Abstract
Falls are a leading cause of injury, hospitalization and even death among older adults. Although various strength and balance exercise interventions have shown moderate reductions in falls incidence among healthy older adults, no significant falls incidence improvements have been consistently seen in frail older adults or in patient groups with an increased falls risk (e.g. people with Parkinson's disease and stroke). This might be due to a lack of task specificity of previous exercise interventions to the recovery actions required to prevent a fall. Perturbation‐based balance training (PBT) is an emerging task‐specific intervention that aims to improve reactive balance control after destabilizing perturbations in a safe and controlled environment. Although early studies were carried out predominantly in research laboratory settings, work in clinical settings with various patient groups has been proliferating. A systematic search of recent PBT studies showed a significant reduction of falls incidence among healthy older adults and certain patient groups (e.g. people with Parkinson's disease and stroke), with clinically relevant reductions in frail older adults. The most practical methods in clinical settings might be treadmill‐based systems and therapist‐applied perturbations, and PBT that incorporates multiple perturbation types and directions might be of most benefit. Although more controlled studies with long‐term follow‐up periods are required to better elucidate the effects of PBT on falls incidence, PBT appears to be a feasible and effective approach to falls reduction among older adults in clinical settings. Geriatr Gerontol Int 2017; 17: 2294–2303..
Keywords: aged, falls, gait, locomotion, postural balance
Introduction
Falls and fall‐related injuries represent a global public health concern for our aging societies. Approximately 30% of people aged >60 years experience a fall in a given year,1, 2 with older age and frailty independently increasing falls risk.2, 3, 4 Older adults with neurological disorders, such as stroke and Parkinson's disease, are at an even higher risk of falling.5 Falls are a leading cause of injury, hospitalization and even death among older adults;1, 6 therefore, evidence‐based interventions for reducing falls and fall‐related injuries in older populations are of great importance.
Moderate reductions in falls risk (approximately 15–20%) have been seen in healthy older adults after exercise interventions including combinations of strength, balance and aerobic exercises.7, 8 However, there is mixed evidence for whether such exercise interventions result in a significant reduction in falls incidence in frail, older adults.9, 10, 11 Importantly, there is limited evidence for falls risk reduction after such strength and balance exercise interventions alone in older adults with Parkinson's disease12, 13 or after a stroke.14 One potential reason for the inconsistency or lack of effectiveness of such general exercise interventions for falls reduction is the lack of task specificity to the recovery actions required to prevent a fall.15, 16 In order to recover balance after a postural disturbance, change‐in‐support movements (e.g. by taking compensatory steps or by grasping nearby objects for support) and counter rotations of body segments can be executed.17, 18 Training that targets such balance recovery mechanisms might be more effective than general exercise.15, 16, 19, 20
The importance of task‐specific training has led to increasing interest in a new approach called perturbation‐based balance training (PBT).21, 22 PBT is a task‐specific intervention that aims to improve reactive balance control (i.e. rapid reactions to instability) after destabilizing perturbations in a safe and controlled environment. Participants are exposed to unexpected balance perturbations (e.g. treadmill accelerations, waist pulls, cable‐based trips, nudge from a therapist etc.; see Fig. 1 for examples) during tasks of daily living, such as standing, walking or rising from a chair.19, 23 The perturbations during PBT are unannounced in order to mimic the accidental and unexpected nature of falls in daily life,21 and ensure that the task‐specific approach of PBT is in concordance with the “specificity of learning” hypothesis.24
Figure 1.
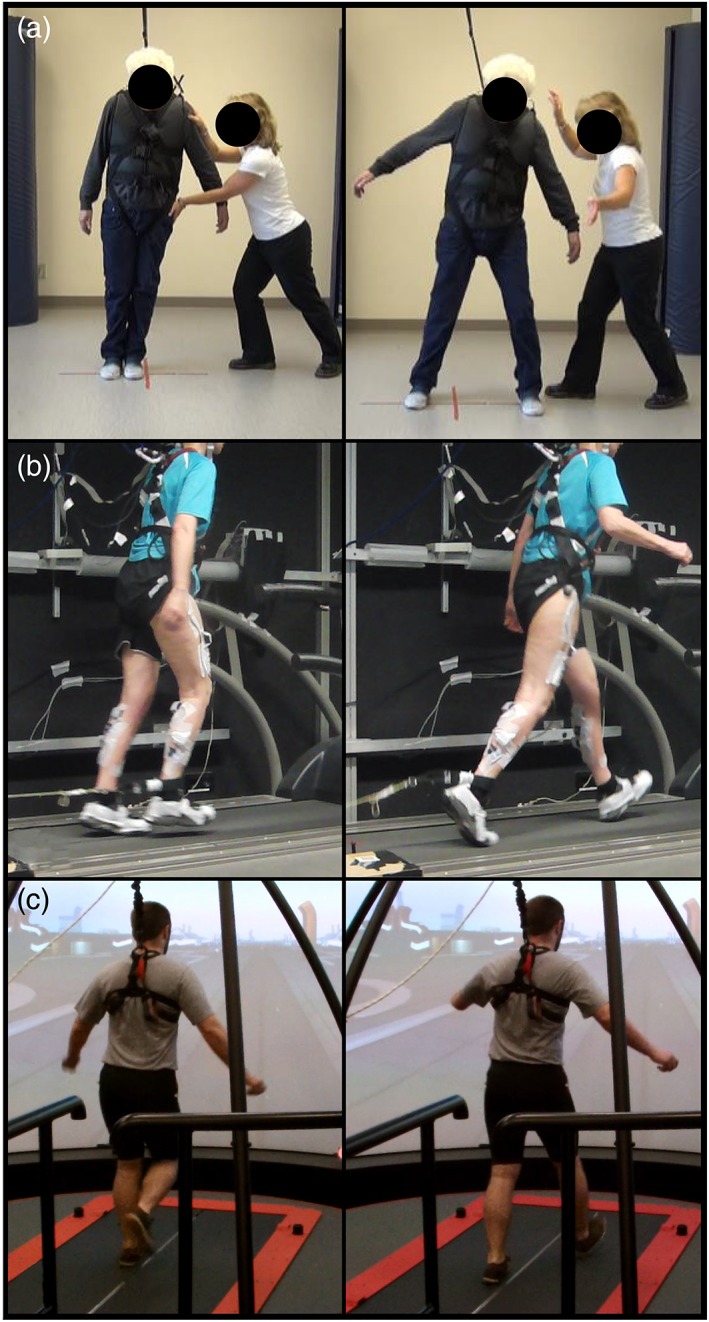
Examples of different types of perturbations used in clinical and research settings. (a) A therapist‐applied lean‐and‐release perturbation in the mediolateral direction. (b) A cable trip perturbation on a standard treadmill causing a forward loss of balance. (c) A treadmill belt acceleration perturbation using the Computer Assisted Rehabilitation Environment (Motekforce Link, Amsterdam, the Netherlands), causing a forward loss of balance.
Despite the diminished reactive gait stability seen in older adults in response to a novel perturbation compared with young adults,25 reactive locomotor adaptation potential (the ability to adapt and improve reactive gait adjustments in a feedback‐driven manner) does not appear to decline with age,26, 27 nor does it appear to be specific to one mode (stance, sit‐to‐stand or gait) of locomotion.28 By capitalizing on older adults’ potential for improvement by providing sufficient and specific stimuli (i.e. PBT), the reactive balance control of older adults could be improved, which might reduce their falls risk. One recent meta‐analysis of randomized controlled trials using PBT indeed reported a significantly lower falls incidence in PBT groups after the interventions,29 with a second meta‐analysis combining studies of PBT with voluntary stepping interventions also reporting reduced falls incidence.30 However, despite this evidence, it is important to consider whether such training is effective and feasible in clinical settings, or whether such benefits are only seen in highly controlled laboratory settings, information that is not yet explored in detail in the literature. Therefore, in the present review, we systematically searched the literature for PBT studies with older adults in order to: (i) examine the characteristics of PBT studies carried out to date with older adults that assessed prospective falls incidence; and (ii) using this evidence from the literature, present and discuss a number of considerations for applying PBT in clinical settings, such as the perturbation characteristics (type, direction, magnitude etc.) and the training program (frequency, volume), that could affect the feasibility and effectiveness of PBT for falls reduction among older adults in clinical settings.
Methods
A systematic literature search with search terms relating to perturbations, training, falls and age with date of publication set at 2002 or later was carried out in PubMed and Web of Science databases (see Appendix S1 for the full search strategy). Studies were selected for inclusion if they carried out PBT with older adults (mean age of ≥60 years), reported post‐intervention falls data and if a control group was included. Studies that carried out PBT, but that did not provide specific details on the intervention, were excluded from the main synthesis. The final search was carried out on 9 January 2017. Additionally, reference lists of the discovered articles, previous reviews and other articles known to the authors were checked. Studies with healthy older adults, high risk or frail older adults, as well as older adults with neurological disorders that met the above criteria, were considered in the current review.
Results and discussion
The complete search and inclusion process can be seen in Figure 2. The search yielded 802 records, and four articles were identified through other sources. After removing duplicates, 672 titles were screened. The title screening excluded 489 records, after which the remaining 183 abstracts were assessed for inclusion. A total of 32 full texts were then assessed, and eight articles met all inclusion criteria. The reasons for exclusion at the full text screening stage can be found in Figure 2. A summary of all included articles can be found in Table 1.
Figure 2.
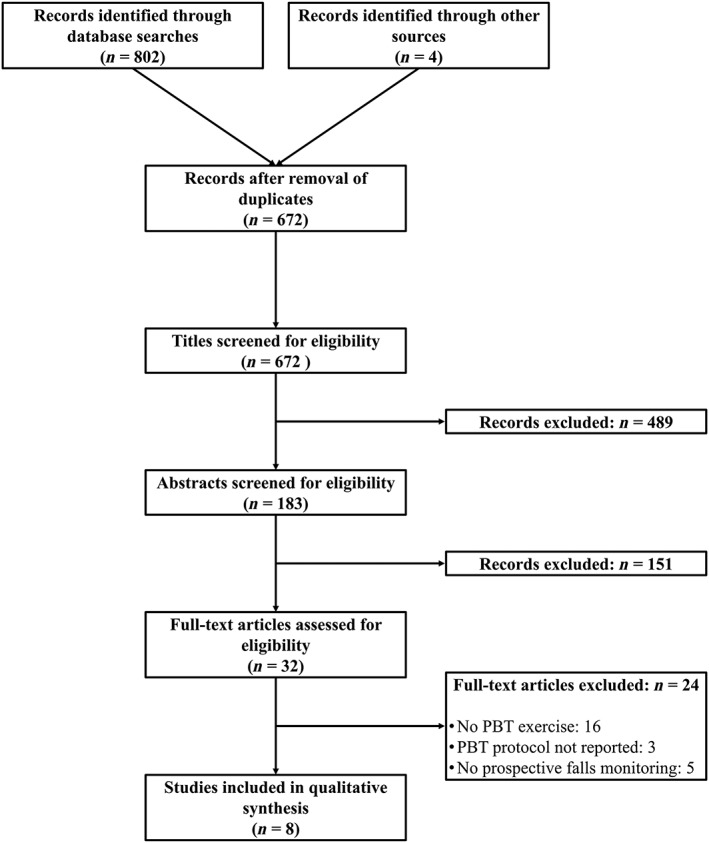
Flowchart of systematic search and article inclusion and exclusion process. PBT, perturbation‐based balance training.
Table 1.
Overview of included studies that administered perturbation‐based balance training to older adults
| Study | Design | Participants | Perturbation type | Protocol | Falls monitoring | Main outcome |
|---|---|---|---|---|---|---|
| Mansfield et al 19 | RCT | Healthy, n = 16, 70.3 years (4.7 years) | Moveable platform in four directions | 3 × 30 min/week for 6 weeks | Prospective for 1 year | No significant differences in falls incidence, but not powered for this measure |
| Pai et al 31 | RCT | Healthy, n = 67, 72 years (5.5 years) | Moveable platform simulating a slip | 1 session of 24 slips | Prospective for 1 year | Intervention led to a significant decrease (34% to 15%) in falls incidence, no change in the control group |
| Rosenblatt et al 32 | RCT | Healthy, n = 82, 65.4 years (7.8 years) | Treadmill belt accelerations during standing | 4 × 1 h over 2 weeks | Prospective for 1 year | Significantly fewer (17 vs 31) likely preventable trip‐related falls (17) in the intervention group compared to control group |
| Lurie et al 34 | Randomized pilot study | High risk, n = 26, 81.1 years (6.53 years) | Treadmill belt accelerations and decelerations during standing and walking | 5.84 sessions of 44.25 min (means) | Retrospective: 3 months preceding and 3 months after the intervention | Non‐significant difference in PBT group experiencing falls (19% vs 33%) and injurious falls (8% vs 18%) compared with controls |
| Shimada et al 33 | RCT | High risk, n = 15, 81.8 years (5.9 years) † | Treadmill belt decelerations during walking | 600 min of PBT over 6 months | Prospective for 6 months | Non‐statistically significant decrease (21%) in falls in the PBT group |
| Protas et al 35 | RCT | Parkinson's disease, n = 9, 71.3 years (7.4 years) | Treadmill belt accelerations during standing while facing and sideways | 3× per week for 8 weeks. | Prospective: 2 weeks preceding and 2 weeks after the intervention | The PBT group experienced a significant reduction in falls in the 2 weeks after the training period, in comparison to the 2 weeks before the training |
| Shen and Mak36 | RCT | Parkinson's disease, n = 22, 63.3 years (8.0 years) | Treadmill belt accelerations during stance and therapist pushes during walking | 3–5× per week for 12 weeks of balance training incorporating PBT | Prospective: 12 months after the intervention | Significantly fewer falls during follow up in the PBT group than in the control group |
| Smania et al 37 | RCT | Parkinson's disease, n = 28, 67.64 years (7.41 years) | Standing on foam and moveable platforms while a therapist pulled the participant | 3 × 50mins of balance training with PBT, per week for 7 weeks | Retrospective: 1 month preceding, during and 1 month after the intervention | Significant reduction in falls during and a non‐significant reduction after the intervention in PBT group. The PBT group experienced significantly fewer falls than controls both during and after PBT. |
Age data from all participants who started the intervention (n = 18), just 15 completed the study. PBT, perturbation‐based balance training; RCT, randomized controlled trial.
PBT and falls reduction
Three PBT studies have been carried out with healthy, community‐dwelling older adults that prospectively monitored falls and included a control group.19, 31, 32 Rosenblatt et al. examined the effects of PBT on the falls incidence over 1 year of 82 community‐dwelling women (mean age 65.4 years, SD 7.8 years) who received 2 weeks (four 1‐h sessions) of PBT (treadmill accelerations) compared with a control group.32 During the 1‐year follow up, the control group (n = 80) experienced 31 likely preventable trip‐related falls (i.e. compensatory stepping was possible), compared with a significantly lower 17 likely preventable trip‐related falls in the intervention group.32 Pai et al. also found a significant reduction in falls incidence after PBT in their study (67 community‐dwelling older adults completed the PBT and 1‐year follow up; mean age 72 years, SD 5.5 years).31 Participants were exposed to either just one slip or a single PBT session of 24 unannounced slips. During the follow‐up period of 12 months, the intervention group had a 50% decrease (34% to 15%, P < 0.05) in falls incidence, whereas no change in falls incidence was seen in the control group, who were 2.3‐fold more likely to fall than those in the intervention group in the 12‐month follow‐up period.31 Finally, Mansfield et al. examined the effects of PBT over 6 weeks using a moveable platform during stance to train stepping and grasping reactions in older adults, and found beneficial effects on balance recovery responses to laboratory‐based perturbations.19 The original publication did not report falls data, but prospective falls data were recorded (reported in Mansfield et al. 29). These data did not show significant reductions in falls incidence; however, the study was not powered for this outcome measure.
Two studies have examined the effects of PBT on falls incidence among frail or high‐risk older adults.33, 34 Shimada et al. examined the effects of adding 600 min of PBT to an existing 6‐month physical exercise intervention consisting of balance, strength, endurance, and pain‐relieving exercises on falls incidence in a group of 15 long‐term care facility residents and outpatients at a high risk of falling (4 were patients with Parkinson's disease, 4 were patients who had strokes, 8 were patients with knee osteoarthritis, the remaining 16 had no specific diagnosis).33 Participants were randomized to the normal exercise intervention or PBT plus the normal intervention. During the 6‐month follow‐up period, the number of falls was 21% lower in the intervention group than in the control group, which despite being clinically relevant, was not statistically significantly different (P = 0.384) to the control group.33 Lurie et al. found similar results in 31 older adults who were referred to a physiotherapist for gait and balance training.34 They compared the results of PBT in addition to regular physiotherapy with a control group that received regular physiotherapy consisting of strength, mobility and balance exercises. During the 3‐month follow‐up period, fewer participants in the intervention group experienced falls (19.23% vs. 33.33%, P = 0.227) and injurious falls (7.69% vs. 18.18%, P = 0.243) in comparison with the control group.34 As with Shimada et al., these results were not statistically significant, despite the clinically relevant differences.33 However, this was a pilot study, and was not powered to detect differences in falls incidence. Additionally, the 3‐month follow‐up period might have been too short to detect significant differences.
Three studies have examined the effects of PBT on the incidence of falls in daily life among older adults with Parkinson's disease.35, 36, 37 We do not discuss the above‐detailed study of Shimada et al. here, as only a proportion of the participants had a neurological disorder.33 Protas et al. investigated the effects of 8 weeks’ PBT, in combination with gait training, in nine men with mild‐to‐moderate idiopathic Parkinson's disease, and showed a significant reduction of falls in the 2 weeks after the training period, in comparison with the 2 weeks before the training.35 Smania et al. carried out a similar study in 28 older adults with moderate‐to‐severe Parkinson's disease.37 In that study, 7 weeks’ balance training incorporating PBT was compared with general physical exercise for effects on falls incidence during, and for 1 month after, the intervention.37 PBT led to a significant reduction in falls during and a non‐significant reduction after the intervention compared with the month before.37 In comparison with the control group, the PBT group experienced significantly fewer falls both during and after the intervention.37 Finally, Shen and Mak reported significantly fewer falls in older adults with mild‐to‐moderate Parkinson's disease during a 15‐month follow up after 3 months’ balance training including PBT, compared with participants who had completed strength training.36 Although the results of these studies suggest a beneficial effect of PBT on falls risk in Parkinson's disease, all of the interventions had multiple components, only one of which was PBT, and therefore, the exact effect of PBT is difficult to determine. That being said, one recent study showed that people with Parkinson's disease can adapt their reactive dynamic stability control after perturbations to stance, and retain motor adaptations to a similar degree as healthy older adults over 24 h.38 This suggests that reactive adaptation might not be completely inhibited in Parkinson's disease, which is promising for the clinical implementation of PBT in this patient group.
There has been less research carried out on PBT in other patient populations. One study of the effects of PBT on falls post‐training in people with chronic stroke is currently underway.39 Preliminary results from another non‐randomized study including individuals with subacute stroke show a trend for reduced falls in daily life after PBT.40 In both of the previous stroke studies, a physiotherapist applied perturbations through pushes and nudges. One other previous study of people with chronic stroke incorporated similar PBT exercises into an agility‐based training program.41 A reduced number of falls during laboratory‐based platform perturbations was observed after PBT, but no differences were seen in daily life falls incidence, probably as a result of the study not being powered for this outcome measure.41 Despite these promising results, more research is required to determine the effectiveness and feasibility of PBT for falls reduction in patient groups with an increased falls risk.
Implementing PBT in clinical practice
In this section, we discuss a number of factors that should be considered when implementing PBT in clinical practice. This is done with reference to current research in both laboratory and clinical settings. The included studies in the present review, as well as studies analyzing the effects of PBT on reactive compensatory stepping behavior after laboratory‐based perturbations are discussed, as the effects of PBT can be evaluated more precisely in such laboratory settings.
PBT setups in clinical practice
Although many methods are available for delivering unexpected perturbations, the PBT studies that have been carried out in clinical settings have generally opted for treadmill‐based perturbations33, 34, 35, 36, 42 or therapist‐applied perturbations.39, 40, 41 There are two practical advantages to treadmill‐based setups: the lack of required space and the relative ease of securing a fixed harness system above the treadmill. These studies have used treadmill belt accelerations during stance or walking in order to perturb the participant's balance in a similar manner to a trip or a slip, and this setup appears to be feasible in clinical settings.34 Therapist‐applied perturbations could be considered the most clinically feasible type of perturbations, given the low cost and limited equipment required. These can be either internal perturbations (having the patient carry out a task that causes instability) or external perturbations. External therapist‐applied perturbations can include lean‐and‐release or pushing and pulling the participant in multiple directions.39 The feasibility of PBT in clinical settings is also supported by case studies of patients with progressive supranuclear palsy42 and subacute stroke43 reporting positive outcomes. Once the most feasible setup for PBT has been determined, it is important to consider how to best maximize the effects of PBT.
Maximizing long‐term effects of PBT
One key factor that might determine how successful PBT can be for reducing falls is the extent to which participants retain improvements in reactive balance control they have made during training over the weeks, months and years after training. In PBT studies, the long‐term effects can be determined through prospective falls monitoring or perturbation recovery performance assessed in a laboratory setting. These improvements could be enhanced ability to increase the base of support by stepping, decreased reaction time to perturbations or improved counter rotation to control the center of mass.18, 44 This retention can be affected by a combination of the perturbation type and magnitude, but also the training volume. Previous studies reported that both healthy older adults and patients with Parkinson's disease, after experiencing a single session of perturbations, showed at least partial retention of reactive balance control improvements over short periods of 24 h.27, 38 Studies with healthy older adults have also shown retention over longer periods of 6,45, 46 9 and 12 months46 in laboratory settings. Retention in compensatory step length has also been shown in patients with Parkinson's up to 2 months after a 2‐week long PBT intervention.47 Retention over such long time periods indicates that PBT provides a strong stimulus for the neuromuscular system, which could indicate that high training volumes might not be necessary to maximize retention. Bhatt et al. also investigated the effect of experiencing a single slip perturbation 3 months after a perturbation session on retention at 6 months.45 Their results show that such a “booster” session helped participants to retain improvements in reactive balance control.45 These findings are potentially important for clinical practice, as they show that after an initial training period, long‐term retention of the benefits of PBT is possible and can be enhanced with short additional sessions.
Perturbation magnitudes
One way to maximize the effects of PBT is to use perturbations of appropriate magnitude. In the aforementioned studies, a variety of magnitudes were used, that were either fixed or progressive with training. High‐magnitude perturbations, where participants initially require support from the harness to regain stability, appear to trigger fast and significant adaptation in recovery behavior, and long‐term retention of motor adaptations.31, 45, 46, 48 However, studies based in clinical settings have generally used a more progressive increase in perturbation magnitude, starting with lower‐magnitude perturbations and progressing based on the supervising physiotherapist's judgement.34, 37 Although perturbation magnitudes that result in participants requiring support from the harness have been shown to be effective, these might not always be appropriate for specific groups, such as frail older adults or people with neurological conditions, as physical injury is possible even if the safety harness is used to prevent a fall to the floor. Additionally, high‐magnitude perturbations might not be tolerated by some frail individuals, which could increase withdrawal from the program. It is not yet clear how much perturbation magnitude impacts motor learning and retention. In young adults, exposure to smaller‐magnitude perturbations can improve stability control after larger‐magnitude perturbations.49 However, it has also been shown that younger adults can recover more effectively from an overground slip after high‐, rather than low‐, magnitude perturbation experience.50 Given the mixed evidence in young adults, and the benefits of both approaches shown in older adults, selecting perturbation magnitudes that are safe and tolerable while still challenging for the participant appears to be a reasonable choice for clinical applications.
Perturbation directions
Second to the perturbation magnitude, the direction of perturbation should be considered. In the studies discussed above, two studies applied perturbations that caused a loss of balance in the backward direction.31, 33 Another study applied only perturbations leading to a forward loss of balance,32 whereas three studies applied perturbations in both directions.34, 35, 36 Although the impact of perturbation direction on falls incidence or types of falls experienced is not known, there is evidence to suggest that adaptation to perturbations in one direction might not transfer and benefit reactive balance control in another direction.27, 38 Perturbations in the mediolateral directions should also be considered when applying PBT in clinical settings, because of the reduced mediolateral stability seen in older adults.51 This reduced mediolateral stability can also be seen during forward compensatory stepping, where older adults often struggle to stabilize the leg, and keep from falling sideways.52, 53 Although repetition of one single perturbation might improve certain mechanisms of balance control that can be transferred to other tasks (e.g. counter rotations or rapid stepping to enlarge the base of support), it seems reasonable to suggest that multidirectional perturbations that target several balance recovery strategies might be the most advantageous for falls reduction in older adults.
PBT frequency and volume
The optimal frequency and volume of PBT for falls reduction among older adults must be considered. Although the duration of training sessions in previous studies has not always been described, most report sessions of 50 min to 1 h. The frequency and training load varies to a greater extent from just single sessions to multiple sessions over a number of months. It is important for future research to determine the minimum effective dose for falls reduction in different participant and patient groups, as this would minimize the time and financial commitment required for PBT in clinical settings. As aforementioned, this might depend on the magnitude of perturbations used. With high‐magnitude perturbations, relatively low PBT volume might be required for long‐term benefits.31, 45, 46, 48 With lower‐magnitude perturbations, which might be more feasible with frail, older adults or different patient groups, longer training periods might be required in order to result in a significant reduction in falls incidence.
Other considerations
Falls tend to occur in daily life during execution of movement (e.g. walking or transferring from standing to sitting), and rarely occur during quiet standing.1, 54, 55 Therefore, perturbations should be applied during tasks, such as walking,33, 34 weight shifting39, 56 and rising from a chair.57 Falls can also occur in varied environmental circumstances that pose sensory and mechanical challenges to balance control (e.g. in the dark/dim light or in the presence of obstacles that impede stepping), and can occur when the individual is distracted. Therefore, PBT programs should consider adding sensory, environmental and cognitive challenges during training to help to promote generalizability of improved reactive balance control to realistic situations.39, 57
Future research directions
Based on the PBT studies discussed in the present review, a number of methodological issues should be addressed in the future. First, the intervention was not always standardized across participants because of the individualization based on ability and physiotherapist judgement.33, 34, 36, 37 Although these studies showed the feasibility of PBT in clinical practice, conclusions related to the optimal perturbation number and type are difficult to make. Second, the falls monitoring follow‐up period differed between studies, with four studies following participants for 6 or 12 months, and three studies with a follow‐up period between 1 and 3 months. This makes comparisons across different interventions more difficult with regard to long‐term benefits of PBT. As these interventions differed greatly and were carried out in different subject groups, it is difficult to determine the components of PBT that affect long‐term retention in PBT‐induced adaptations. Therefore, more controlled studies of PBT with long‐term follow up are required to better determine the effects of different PBT components on motor adaptation, retention and falls.
Conclusion
PBT appears to be a feasible approach to reducing falls among older adults in clinical settings. Based on the current evidence, it appears that treadmill‐based systems and therapist‐applied perturbations might be the most practical methods in clinical settings, and PBT that incorporates multiple perturbation types and directions might be of most benefit.
Disclosure statement
The authors declare no conflict of interest.
Supporting information
Appendix S1 Search Strategy.
Acknowledgements
CM was funded by the Kootstra Talent Fellowship awarded by the Center for Research Innovation, Support and Policy (CRISP), and by the NUTRIM Graduate Program of Maastricht University Medical Center+. AM holds a New Investigator Award from the Canadian Institutes of Health Research (MSH‐141983).
References
- 1. Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med 1988; 319 (26): 1701–1707. [DOI] [PubMed] [Google Scholar]
- 2. Talbot LA, Musiol RJ, Witham EK, Metter EJ. Falls in young, middle‐aged and older community dwelling adults: Perceived cause, environmental factors and injury. BMC Public Health 2005; 5: 86 https://doi.org/10.1186/1471‐2458‐5‐86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kojima G, Kendrick D, Skelton DA, Morris RW, Gawler S, Iliffe S. Frailty predicts short‐term incidence of future falls among British community‐dwelling older people: A prospective cohort study nested within a randomised controlled trial. BMC Geriatr 2015; 15 (1): 155 https://doi.org/10.1186/s12877‐015‐0152‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Gale CR, Cooper C, Aihie SA. Prevalence and risk factors for falls in older men and women: The English longitudinal study of ageing. Age Ageing 2016. https://doi.org/10.1093/ageing/afw129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Homann B, Plaschg A, Grundner M et al. The impact of neurological disorders on the risk for falls in the community dwelling elderly: A case‐controlled study. BMJ Open 2013; 3 (11): e003367 https://doi.org/10.1136/bmjopen‐2013‐003367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Terroso M, Rosa N, Marques AT, Simoes R. Physical consequences of falls in the elderly: A literature review from 1995 to 2010. Eur Rev Aging Phys Act 2014; 11 (1): 51–59. [Google Scholar]
- 7. Gillespie LD, Robertson MC, Gillespie WJ et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev 2012; 9: CD007146 https://doi.org/10.1002/14651858.CD007146.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Sherrington C, Whitney JC, Lord SR, Herbert RD, Cumming RG, Close JC. Effective exercise for the prevention of falls: A systematic review and meta‐analysis. J Am Geriatr Soc 2008; 56 (12): 2234–2243. [DOI] [PubMed] [Google Scholar]
- 9. de Labra C, Guimaraes‐Pinheiro C, Maseda A, Lorenzo T, Millan‐Calenti JC. Effects of physical exercise interventions in frail older adults: A systematic review of randomized controlled trials. BMC Geriatr 2015; 15 (1): 154 https://doi.org/10.1186/s12877‐015‐0155‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Faber MJ, Bosscher RJ, Chin APMJ, van Wieringen PC. Effects of exercise programs on falls and mobility in frail and pre‐frail older adults: A multicenter randomized controlled trial. Arch Phys Med Rehabil 2006; 87 (7): 885–896. [DOI] [PubMed] [Google Scholar]
- 11. Fairhall N, Sherrington C, Lord SR et al. Effect of a multifactorial, interdisciplinary intervention on risk factors for falls and fall rate in frail older people: A randomised controlled trial. Age Ageing 2014; 43 (5): 616–622. [DOI] [PubMed] [Google Scholar]
- 12. Canning CG, Sherrington C, Lord SR et al. Exercise for falls prevention in Parkinson disease: A randomized controlled trial. Neurology 2015; 84 (3): 304–312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Allen NE, Canning CG, Sherrington C et al. The effects of an exercise program on fall risk factors in people with Parkinson's disease: A randomized controlled trial. Mov Disord 2010; 25 (9): 1217–1225. [DOI] [PubMed] [Google Scholar]
- 14. Verheyden GS, Weerdesteyn V, Pickering RM et al. Interventions for preventing falls in people after stroke. Cochrane Database Syst Rev 2013; 5: CD008728 https://doi.org/10.1002/14651858.CD008728.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Oddsson LIE, Boissy P, Melzer I. How to improve gait and balance function in elderly individuals ‐ compliance with principles of training. Eur Rev Aging Phys Act 2007; 4 (1): 15–23. [Google Scholar]
- 16. Grabiner MD, Crenshaw JR, Hurt CP, Rosenblatt NJ, Troy KL. Exercise‐based fall prevention: Can you be a bit more specific? Exerc Sport Sci Rev 2014; 42 (4): 161–168. [DOI] [PubMed] [Google Scholar]
- 17. Hof AL. The equations of motion for a standing human reveal three mechanisms for balance. J Biomech 2007; 40 (2): 451–457. [DOI] [PubMed] [Google Scholar]
- 18. Maki BE, McIlroy WE. Change‐in‐support balance reactions in older persons: An emerging research area of clinical importance. Neurol Clin 2005; 23 (3): 751–783 vi‐vii. [DOI] [PubMed] [Google Scholar]
- 19. Mansfield A, Peters AL, Liu BA, Maki BE. Effect of a perturbation‐based balance training program on compensatory stepping and grasping reactions in older adults: A randomized controlled trial. Phys Ther 2010; 90 (4): 476–491. [DOI] [PubMed] [Google Scholar]
- 20. Carty CP, Cronin NJ, Nicholson D et al. Reactive stepping behaviour in response to forward loss of balance predicts future falls in community‐dwelling older adults. Age Ageing 2015; 44 (1): 109–115. [DOI] [PubMed] [Google Scholar]
- 21. Pai YC, Bhatt TS. Repeated‐slip training: An emerging paradigm for prevention of slip‐related falls among older adults. Phys Ther 2007; 87 (11): 1478–1491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Maki BE, Cheng KC, Mansfield A et al. Preventing falls in older adults: New interventions to promote more effective change‐in‐support balance reactions. J Electromyogr Kinesiol 2008; 18 (2): 243–254. [DOI] [PubMed] [Google Scholar]
- 23. Pai YC, Bhatt T, Wang E, Espy D, Pavol MJ. Inoculation against falls: Rapid adaptation by young and older adults to slips during daily activities. Arch Phys Med Rehabil 2010; 91 (3): 452–459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Bachman JC. Specificity vs. generality in learning and performing two large muscle motor tasks. Res Q Am Assoc Health Phys Educ Recreation 1961; 32 (1): 3–11. [Google Scholar]
- 25. Süptitz F, Catala MM, Brüggemann GP, Karamanidis K. Dynamic stability control during perturbed walking can be assessed by a reduced kinematic model across the adult female lifespan. Hum Mov Sci 2013; 32 (6): 1404–1414. [DOI] [PubMed] [Google Scholar]
- 26. Bohm S, Mademli L, Mersmann F, Arampatzis A. Predictive and reactive locomotor adaptability in healthy elderly: A systematic review and meta‐analysis. Sports Med 2015; 45 (12): 1759–1777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Dijkstra BW, Horak FB, Kamsma YP, Peterson DS. Older adults can improve compensatory stepping with repeated postural perturbations. Front Aging Neurosci 2015; 7: 201 https://doi.org/10.3389/fnagi.2015.00201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. McCrum C, Essers JMN, Jie L‐J, Liu W‐Y, Meijer K. Commentary: Older adults can improve compensatory stepping with repeated postural perturbations. Front Aging Neurosci 2016; 8: 111 https://doi.org/10.3389/fnagi.2016.00111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Mansfield A, Wong JS, Bryce J, Knorr S, Patterson KK. Does perturbation‐based balance training prevent falls? Systematic review and meta‐analysis of preliminary randomized controlled trials. Phys Ther 2015; 95 (5): 700–709. [DOI] [PubMed] [Google Scholar]
- 30. Okubo Y, Schoene D, Lord SR. Step training improves reaction time, gait and balance and reduces falls in older people: A systematic review and meta‐analysis. Br J Sports Med 2016. https://doi.org/10.1136/bjsports‐2015‐095452. [DOI] [PubMed] [Google Scholar]
- 31. Pai YC, Bhatt T, Yang F, Wang E. Perturbation training can reduce community‐dwelling older adults' annual fall risk: A randomized controlled trial. J Gerontol A Biol Sci Med Sci 2014; 69 (12): 1586–1594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Rosenblatt NJ, Marone J, Grabiner MD. Preventing trip‐related falls by community‐dwelling adults: A prospective study. J Am Geriatr Soc 2013; 61 (9): 1629–1631. [DOI] [PubMed] [Google Scholar]
- 33. Shimada H, Obuchi S, Furuna T, Suzuki T. New intervention program for preventing falls among frail elderly people ‐ the effects of perturbed walking exercise using a bilateral separated treadmill. Am J Phys Med Rehab 2004; 83 (7): 493–499. [DOI] [PubMed] [Google Scholar]
- 34. Lurie JD, Zagaria AB, Pidgeon DM, Forman JL, Spratt KF. Pilot comparative effectiveness study of surface perturbation treadmill training to prevent falls in older adults. BMC Geriatr 2013; 13: 49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Protas EJ, Mitchell K, Williams A, Qureshy H, Caroline K, Lai EC. Gait and step training to reduce falls in Parkinson's disease. NeuroRehabilitation 2005; 20 (3): 183–190. [PubMed] [Google Scholar]
- 36. Shen X, Mak MK. Technology‐assisted balance and gait training reduces falls in patients with Parkinson's disease: A randomized controlled trial with 12‐month follow‐up. Neurorehabil Neural Repair 2015; 29 (2): 103–111. [DOI] [PubMed] [Google Scholar]
- 37. Smania N, Corato E, Tinazzi M et al. Effect of balance training on postural instability in patients with idiopathic Parkinson's disease. Neurorehabil Neural Repair 2010; 24 (9): 826–834. [DOI] [PubMed] [Google Scholar]
- 38. Peterson DS, Dijkstra BW, Horak FB. Postural motor learning in people with Parkinson's disease. J Neurol 2016; 263 (8): 1518–1529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Mansfield A, Aqui A, Centen A et al. Perturbation training to promote safe independent mobility post‐stroke: Study protocol for a randomized controlled trial. BMC Neurol 2015; 15: 87 https://doi.org/10.1186/s12883‐015‐0347‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Mansfield A, Schinkel‐Ivy A, Danells CJ et al. Does perturbation training prevent falls after discharge from stroke rehabilitation? A prospective cohort study with historical control. Paper presented at: 2016. Canadian Stroke Congress; 2016; Québec City, QC, Canada. [DOI] [PMC free article] [PubMed]
- 41. Marigold DS, Eng JJ, Dawson AS, Inglis JT, Harris JE, Gylfadottir S. Exercise leads to faster postural reflexes, improved balance and mobility, and fewer falls in older persons with chronic stroke. J Am Geriatr Soc 2005; 53 (3): 416–423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Suteerawattananon M, MacNeill B, Protas EJ. Supported treadmill training for gait and balance in a patient with progressive supranuclear palsy. Phys Ther 2002; 82 (5): 485–495. [PubMed] [Google Scholar]
- 43. Mansfield A, Inness EL, Komar J et al. Training rapid stepping responses in an individual with stroke. Phys Ther 2011; 91 (6): 958–969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Pijnappels M, Bobbert MF, van Dieën JH. Push‐off reactions in recovery after tripping discriminate young subjects, older non‐fallers and older fallers. Gait Posture 2005; 21 (4): 388–394. [DOI] [PubMed] [Google Scholar]
- 45. Bhatt T, Yang F, Pai YC. Learning to resist gait‐slip falls: Long‐term retention in community‐dwelling older adults. Arch Phys Med Rehabil 2012; 93 (4): 557–564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Pai YC, Yang F, Bhatt T, Wang E. Learning from laboratory‐induced falling: Long‐term motor retention among older adults. Age 2014; 36 (3): 1367–1376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Jöbges M, Heuschkel G, Pretzel C, Illhardt C, Renner C, Hummelsheim H. Repetitive training of compensatory steps: A therapeutic approach for postural instability in Parkinson's disease. J Neurol Neurosurg Psychiatry 2004; 75 (12): 1682–1687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Bhatt T, Espy D, Yang F, Pai YC. Dynamic gait stability, clinical correlates, and prognosis of falls among community‐dwelling older adults. Arch Phys Med Rehabil 2011; 92 (5): 799–805. [DOI] [PubMed] [Google Scholar]
- 49. Patel P, Bhatt T. Adaptation to large‐magnitude treadmill‐based perturbations: Improvements in reactive balance response. Physiol Rep 2015; 3 (2): e12247 https://doi.org/10.14814/phy2.12247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Liu X, Bhatt T, Pai YC. Intensity and generalization of treadmill slip training: High or low, progressive increase or decrease? J Biomech 2016; 49 (2): 135–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Maki BE, Edmondstone MA, McIlroy WE. Age‐related differences in laterally directed compensatory stepping behavior. J Gerontol A Biol Sci Med Sci 2000; 55 (5): M270–M277. [DOI] [PubMed] [Google Scholar]
- 52. McIlroy WE, Maki BE. Age‐related changes in compensatory stepping in response to unpredictable perturbations. J Gerontol A Biol Sci Med Sci 1996; 51 (6): M289–M296. [DOI] [PubMed] [Google Scholar]
- 53. Singer JC, Prentice SD, McIlroy WE. Age‐related challenges in reactive control of mediolateral stability during compensatory stepping: A focus on the dynamics of restabilisation. J Biomech 2016; 49 (5): 749–755. [DOI] [PubMed] [Google Scholar]
- 54. Robinovitch SN, Feldman F, Yang Y et al. Video capture of the circumstances of falls in elderly people residing in long‐term care: An observational study. Lancet 2013; 381 (9860): 47–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Berg WP, Alessio HM, Mills EM, Tong C. Circumstances and consequences of falls in independent community‐dwelling older adults. Age Ageing 1997; 26 (4): 261–268. [DOI] [PubMed] [Google Scholar]
- 56. Mansfield A, Peters AL, Liu BA, Maki BE. A perturbation‐based balance training program for older adults: Study protocol for a randomised controlled trial. BMC Geriatr 2007; 7: 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Pavol MJ, Runtz EF, Pai YC. Young and older adults exhibit proactive and reactive adaptations to repeated slip exposure. J Gerontol A Biol Sci Med Sci 2004; 59 (5): 494–502. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1 Search Strategy.


