Abstract
Key to an understanding of alcohol use disorder (AUD) are the drinking-related reductions that begin in young adulthood and continue throughout the adult lifespan. Research is needed to precisely characterize the form of these reductions, including possible developmental differences across the lifespan. Using U.S.-representative data, we estimated multiple-group Markov models characterizing longitudinal transitions among five drinking statuses and differences in transition patterns across six adult age periods. While past research indicates relative developmental stability in overall AUD-desistance rates, we found far higher rates of Severe-AUD desistance in young adulthood relative to later ages. Especially considering the dramatic change reflected by Severe-AUD desistance (from 6+ symptoms to 0–1 symptoms), this result indicates a substantial developmental shift, with Severe-AUD-desistance rates peaking at 43–50% across ages 25–34 and then dropping to 22–24% across ages 35–55. We discuss implications regarding practical significance of young-adult “maturing out” and predictions regarding lifespan variability in desistance mechanisms.
Keywords: Alcohol Use Disorder, Alcohol-Use-Disorder Severity, Lifespan Development, Maturing Out, Natural Recovery
A key finding informing a developmental understanding of alcohol use disorder (AUD) is the reduction in heavy and problematic drinking that begins in young adulthood and continues throughout subsequent developmental periods (Johnston, O’Malley, Bachman, Schulenberg, & Miech, 2014; Li, Hewitt, & Grant, 2007). Research should prioritize the advancement of a more precise characterization of this developmental phenomenon, particularly to determine the extent this phenomenon reflects desistance from severe forms of problem drinking as opposed to milder forms. An important motivation for studying normative drinking-related reductions is to inform practical efforts aimed at reducing negative impacts of problem drinking, for instance by guiding the design of clinical and public health interventions (National Institute on Alcohol Abuse and Alcoholism [NIAAA], 2008a; Watson & Sher, 1998). However, research is needed to evaluate the extent that developmental drinking-related reductions observed in the population reflect resolution of clinically-significant drinking pathology. This may indicate how useful an empirical understanding of these reductions could be in informing practical efforts to address forms of problem drinking that pose the greatest potential harms to individuals and society. In the interest of this objective, it is noteworthy that the introduction of severity-graded AUD diagnoses in the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5; American Psychiatric Association [APA], 2013) provides a standard approach for differentiating degrees of clinical significance, thereby lending itself well to an investigation of how AUD desistance rates may vary as a function of AUD severity.
Possible Developmental Differences in Patterns of AUD Desistance
Toward characterizing the nature of developmental drinking reductions, attention should be paid to the possibility that the form of drinking reductions that occur may vary across developmental periods of the adult lifespan. While past research suggests that overall rates of AUD desistance are relatively stable across the lifespan (Vergés et al., 2012), insights regarding developmental variability may perhaps be gleaned through an analysis of AUD desistance that differentiates levels of AUD severity. That is, more substantial differences across adult developmental periods may be observed when analyzing developmental differences in rates of AUD desistance from different specific AUD-severity levels.
Interestingly, rationales exist for mutually exclusive alternative hypotheses for such an analysis. On the one hand, there are important reasons to question the practical significance of young-adult drinking-related reductions and to predict that it may be in later development periods that relatively substantial forms of desistance more commonly occur. Given the earlier peaks in normative rates of alcohol consumption and problem drinking that precede young adulthood, it may be expected that the subsequent drinking-related declines observed in young adulthood often reflect relatively unsubstantial changes involving resolution of mildly problematic drinking. Further, it has been argued that the AUD diagnostic system suffers from a developmentally-specific proneness to false-positive diagnoses in the years preceding young adulthood (Caetano & Babor, 2006; Harford et al., 2005), which could artefactually inflate the appearance of young-adult AUD desistance. Moreover, models of AUD subtypes and AUD-course heterogeneity suggest that relatively severe AUDs may tend to persist beyond young adulthood (Zucker, Hicks, & Heitzeg, 2016). These arguments provide a basis for predicting that (1) young adulthood will be characterized by higher rates of desistance from relatively mild AUDs, whereas (2) later developmental periods will be characterized by higher rates of desistance from more severe AUDs.
On the other hand, young adulthood has been characterized as a critical period for “maturing out” of problem behaviors due to the particularly widespread and substantial maturational change that occurs in this period (e.g., Bachman, Wadsworth, O’Malley, & Johnston, 1997). From this perspective, it might be expected that the marked maturation occurring in young adulthood enhances the potential for highly substantial forms of behavior change, including desistance from severe AUDs. In contrast, the relative developmental stability of later developmental periods may be expected to make such dramatic forms of desistance less likely (Jackson & Sartor, 2016). These arguments provide a basis for predicting that young adulthood may be characterized by higher rates of desistance from relatively severe AUDs when compared to later developmental periods.
The current study provides the first empirical investigation of the above mutually exclusive alternative hypotheses.
The current study
The current study provides a developmentally-informed characterization of patterns of AUD desistance, with particular interest in how rates of desistance from different levels of AUD severity (Mild, Moderate, or Severe AUD) may vary across developmental periods of the adult lifespan. Using data from the large, age-heterogeneous sample of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC; Grant, Kaplan, & Stinson, 2005), we analyzed longitudinal transitions in and out of different drinking statuses over a three-year period (between NESARC Waves 1 and 2). The drinking statuses included (1) Abstainer/Low-Risk Drinker, (2) Sub-Diagnostic Risky Drinker, (3) Mild AUD, (4) Moderate AUD, and (5) Severe AUD; thus facilitating characterizations of rates of AUD desistance from three different levels of initial AUD severity (Mild, Moderate, and Severe AUD). Rates of transitions among the five drinking statuses were characterized separately within six different age groups spanning emerging adulthood to late midlife (ages 20–55), thus facilitating characterizations of developmental differences in rates of desistance from Mild, Moderate, and Severe AUD. Further, beyond facilitating our primary objective of characterizing developmental variability in patterns of AUD desistance, this approach more generally provides a rich, developmentally-sensitive account of various forms of drinking-behavior change in a U.S.-representative sample (e.g., also characterizing problem-drinking escalation and AUD onset in different developmental periods).
Method
Participants and Procedures
The current study employed secondary data analysis, using data from NESARC Waves 1 and 2 (Grant et al., 2005). NESARC was funded by the National Institute of Alcoholism and Alcohol Abuse and was conducted via in-person interviews by the U.S. Census Bureau. Wave 1, conducted from 2001–2002, assessed a very large, nationally-representative, highly age heterogeneous sample, with Hispanics, Blacks, and those aged 18–24 over-sampled by design (N=43,093; ages 18 to >90; Mage=46.4; SDage=18.1; 43.0% male; 56.9% Caucasian; 19.3% Hispanic; 19.1% Black). Wave 2, conducted from 2004–2005, retained 80.4% of the initial sample (n=34,653; ages 20 to >90; Mage=49.1; SDage=17.3; 42.0% male; 58.2% Caucasian; 18.4% Hispanic; 19.0% Black). Analyses excluded participants who were not retained at Wave 2 (n=8,440). This was necessary because analyses employed multiple-group models with age groups defined by Wave-2 age (see Measures), and multiple-group modeling does not permit missing data on the grouping variable. Analyses also excluded those who were otherwise missing data on current-study variables (n=207). Finally, analyses excluded those over age 55 (n=11,652) due to sparseness of some drinking statuses and concerns regarding attrition bias in this age range (see Limitations). Compared to those included in analyses (n=22,794), those excluded from analyses (n=20,299) were generally older and had lower levels of alcohol use and AUD symptomatology. With a few exceptions, this general pattern of differences between included versus excluded participants applied across all three of the above exclusion criteria (see Online Supplements Table A1).
Measures
Drinking severity status classification
Using the past-year drinking-related measures described in the below paragraphs, at both Waves 1 and 2, participants were classified into five a priori “drinking statuses.” This classification was informed by guidelines for safe versus risky drinking (NIAAA, 2008b) and DSM-5 (APA, 2013) guidelines for severity-graded AUD diagnoses. The first status, Abstainer/Low-Risk Drinker, comprised non-drinkers and drinkers who neither exceeded guidelines for safe drinking (described below) nor reported any AUD symptoms. The second status, Sub-Diagnostic Risky Drinkers, comprised those who exceeded either weekly or daily guidelines for safe drinking or reported just one AUD symptom. The third, fourth, and fifth statuses were those who, based on DSM-5 guidelines, were classified with Mild AUD (2–3 symptoms), Moderate AUD (4–5 symptoms), and Severe AUD (6 or more symptoms), respectively (although excluding the DSM-5 “craving” symptom, as discussed below). See Table 1 for frequencies of these different drinking statuses overall and within each of the current study’s age groups (and see Online Supplements Table A3 for frequencies of the drinking statuses among participants excluded from analyses).
Table 1.
Frequencies of drinking statuses at Waves 1 and 2 for each of the six age groups used in the current study’s analyses and for the combined current-study sample
| Wave 1 Drinking statuses
|
||||||
|---|---|---|---|---|---|---|
| Abstainer/Low- Risk Drinker |
Sub-Diagnostic Risky Drinker |
Mild AUD (2–3 symptoms) |
Moderate AUD (4–5 symptoms) |
Severe AUD (6+ symptoms) |
Total of non- missing cases |
|
| Age groups used in analyses | ||||||
| Ages 20–24 | 1282 (59.0%) | 438 (20.1%) | 248 (11.4%) | 111 (5.1%) | 95 (4.4%) | 2174 (100.0%) |
| Ages 25–29 | 1489 (54.8%) | 730 (26.9%) | 292 (10.7%) | 123 (4.5%) | 83 (3.1%) | 2717 (100.0%) |
| Ages 30–34 | 1883 (60.7%) | 816 (26.3%) | 267 (8.6%) | 88 (2.8%) | 46 (1.5%) | 3100 (100.0%) |
| Ages 35–39 | 2227 (63.9%) | 899 (25.8%) | 251 (7.2%) | 72 (2.1%) | 38 (1.1%) | 3487 (100.0%) |
| Ages 40–47 | 4182 (68.8%) | 1364 (22.4%) | 368 (6.1%) | 96 (1.6%) | 66 (1.1%) | 6076 (100.0%) |
| Ages 48–55 | 3854 (73.5%) | 1005 (19.2%) | 255 (4.9%) | 64 (1.2%) | 62 (1.2%) | 5240 (100.0%) |
| Combined current sample | 14917 (65.4%) | 5252 (23.0%) | 1681 (7.4%) | 554 (2.4%) | 390 (1.7%) | 22794 (100.0%) |
|
| ||||||
| W2 Drinking statuses
|
||||||
| Abstainer/Low- Risk Drinker |
Sub-Diagnostic Risky Drinker |
Mild AUD (2–3 symptoms) |
Moderate AUD (4–5 symptoms) |
Severe AUD (6+ symptoms) |
Total | |
|
| ||||||
| Age groups used in analyses | ||||||
| Ages 20–24 | 956 (44.0%) | 646 (29.7%) | 346 (15.9%) | 137 (6.3%) | 89 (4.1%) | 2174 (100.0%) |
| Ages 25–29 | 1432 (52.7%) | 834 (30.7%) | 301 (11.1%) | 102 (3.8%) | 48 (1.8%) | 2717 (100.0%) |
| Ages 30–34 | 1792 (57.8%) | 893 (28.8%) | 289 (9.3%) | 81 (2.6%) | 45 (1.5%) | 3100 (100.0%) |
| Ages 35–39 | 2141 (61.4%) | 909 (26.1%) | 289 (8.3%) | 91 (2.6%) | 57 (1.6%) | 3487 (100.0%) |
| Ages 40–47 | 3976 (65.4%) | 1447 (23.8%) | 429 (7.1%) | 130 (2.1%) | 94 (1.5%) | 6076 (100.0%) |
| Ages 48–55 | 3735 (71.3%) | 1013 (19.3%) | 322 (6.1%) | 113 (2.2%) | 57 (1.1%) | 5240 (100.0%) |
| Combined current sample | 14032 (61.6%) | 5742 (25.2%) | 1976 (8.7%) | 654 (2.9%) | 390 (1.7%) | 22794 (100.0%) |
Note. Age groups were defined based on age reported at Wave 2.
Safe versus risky drinking was coded based on established guidelines defining risky as five or more drinks daily or 14 or more drinks weekly for men and as four or more drinks daily or seven or more drinks weekly for women (NIAAA, 2008b). Whether or not participants exceeded these guidelines was determined on the basis of self-reported past-year drinking quantity and frequency and resulting estimates of weekly and daily ethanol intake. Participants were coded positive for exceeding weekly guidelines if their average weekly ethanol intake was estimated to exceed 8.4 oz. of absolute ethanol for men and 4.2 oz. for women (assuming a standard drink containing 0.6 oz. ethanol). Participants were coded as exceeding daily guidelines if their maximum daily ethanol intake was estimated to exceed 2.7 oz. for men and 2.1 oz. for women. Participants were also coded positive for exceeding daily guidelines if they reported one or more past-year occasions of consuming five or more drinks for men and four or more drinks for women. For more details, see NESARC data notes (NIAAA, 2008b).
AUD symptomatology was assessed based on ten of the eleven AUD criteria defined by the DSM-5 (APA, 2013). These included (1) larger amounts or longer periods of alcohol use than expected, (2) persistent desire or unsuccessful efforts to control drinking, (3) much time spent obtaining, using, or recovering from alcohol, (4) alcohol-related failures in major role obligations, (5) social or interpersonal alcohol-related problems, (6) reducing important social, occupational, or recreational activities due to alcohol, (7) alcohol use in physically hazardous situations, (8) continued drinking despite physical or psychological consequences, (9) alcohol tolerance, and (10) alcohol withdrawal. Although alcohol craving is also included among the DSM-5 AUD criteria, this criterion was not used because it was assessed only at NESARC Wave 2 (see Limitations). For details of the AUD criteria assessment, see NESARC data notes (NIAAA, 2008b).
Age groups
Participants were classified into age groups based on NESARC Wave 2 ages, given the current study’s primary interest in how AUD desistance by Wave 2 may vary as a function of age. Six age groups were defined including ages 20–24, 25–29, 30–34, 35–39, 40–47, and 48–55. Although age is merely an imprecise proxy for developmental progression (Rutter, 1989) and opinions vary regarding the age ranges that best represent different developmental periods, we sometimes refer to our age-classifications as roughly representing emerging adulthood at ages 20–24, young adulthood at ages 25–29 and 30–34, and midlife at ages 35–49, 40–47, and 48–55. Age-based classifications were intentionally made broader at older ages to account for the more rapid developmental changes of emerging and young adulthood, as well as the data’s greater sparseness in relatively severe drinking statuses at older ages (e.g., see Table 1).
Sex and race/ethnicity
Analyses included covariates to control for sex and race/ethnicity based on NESARC Wave 1 self-reports. For sex, one binary dummy variable was used to contrast females (coded 1) versus males (coded 0). For race/ethnicity, three binary dummy variables were used to contrast four groups including Caucasian, African-American, Hispanic, and “other,” with Caucasian as the reference category (i.e., with Caucasian coded 0 in all three dummy variables).
Analytic Approach
All models were estimated using Mplus version 7.11 (Muthén & Muthén, 1998–2012). Analyses accounted for the NESARC data’s primary sampling unit, stratum, and population weights, thereby adjusting for sampling-related non-independence of observations and deriving U.S.-representative model estimates (via the Mplus option TYPE=COMPLEX with CLUSTER, STRATIFICATION, and WEIGHT specifications; using Wave-2 sampling-unit, stratum, and population-weight variables, given our analysis of Wave-2 dependent variables and our exclusion of those not retained at Wave 2).
A manifest Markov models (Kaplan, 2008) was estimated to characterize transitions among our five a priori drinking statuses from NESARC Wave 1 to NESARC Wave 2 (i.e., from NESARC’s baseline assessment to the three-year follow-up assessment). To characterize developmental differences in patterns of transitions among the drinking statuses, the Markov model was estimated as a multiple-group model with our age groups (see Measures) as the grouping variable (via the Mplus KNOWNCLASS option; Muthén & Muthén, 1998–2012). Covariates included a binary dummy variable for sex and three binary dummy variables for race/ethnicity (see Measures). These covariates predicted drinking-status membership at both waves, and their effects were freed to vary across the age groups. Model-derived logit estimates of effects of Wave-1 drinking-status membership on Wave-2 drinking-status membership were used to compute transition probabilities and their standard errors via Mplus MODEL CONSTRAINT commands (per guidelines in Mplus manual Chapter 14; Muthén & Muthén, 1998–2012).1 These transition probabilities (see Table 2), ranging from 0 to 1, characterize the model-predicted likelihood of transitioning to a particular drinking status by Wave 2, given membership in a particular drinking status at Wave 1. Importantly, our multiple-group approach allowed computation of transition probabilities separately for each of the six age groups, thereby allowing characterization of developmental differences in patterns of drinking-status-transition probabilities.
Table 2.
Results of the six-age-group manifest Markov model of drinking severity status transitions from NESARC Wave 1 to Wave 2: Within-age-group transition probabilities and one-standard-error ranges around transition probabilities
| Ages 20–24 (n=2174) | |||||
|---|---|---|---|---|---|
| W2 Abstainer/Low- Risk Drinker (n=956) |
W2 Sub-Diagnostic Risky Drinker (n=646) |
W2 Mild AUD (2–3 symptoms) (n=346) |
W2 Moderate AUD (4–5 symptoms) (n=137) |
W2 Severe AUD (6+ symptoms) (n=89) |
|
| W1 Abstainer/Low-Risk Drinker (n=1282) | 0.448 | 0.310 | 0.152 | 0.067 | 0.022 |
| (0.419–0.477) | (0.286–0.334) | (0.136–0.168) | (0.055–0.079) | (0.015–0.029) | |
| W1 Sub-Diagnostic Risky Drinker (n=438) | 0.127 | 0.486 | 0.264 | 0.058 | 0.065 |
| (0.109–0.145) | (0.453–0.519) | (0.232–0.296) | (0.044–0.072) | (0.049–0.081) | |
| W1 Mild AUD (2–3 symptoms) (n=248) | 0.085 | 0.387 | 0.319 | 0.124 | 0.085 |
| (0.068–0.102) | (0.344–0.43) | (0.28–0.358) | (0.093–0.155) | (0.062–0.108) | |
| W1 Moderate AUD (4–5 symptoms) (n=111) | 0.054 | 0.278 | 0.387 | 0.161 | 0.120 |
| (0.034–0.074) | (0.232–0.324) | (0.33–0.444) | (0.113–0.209) | (0.083–0.157) | |
| W1 Severe AUD (6+ symptoms) (n=95) | 0.037 | 0.248 | 0.260 | 0.185 | 0.270 |
| (0.02–0.054) | (0.19–0.306) | (0.205–0.315) | (0.135–0.235) | (0.202–0.338) | |
| Ages 25–29 (n=2717) | |||||
| W2 Abstainer/Low- Risk Drinker (n=1432) |
W2 Sub-Diagnostic Risky Drinker (n=834) |
W2 Mild AUD (2–3 symptoms) (n=301) |
W2 Moderate AUD (4–5 symptoms) (n=102) |
W2 Severe AUD (6+ symptoms) (n=48) |
|
| W1 Abstainer/Low-Risk Drinker (n=1489) | 0.655 | 0.253 | 0.061 | 0.024 | 0.007 |
| (0.624–0.686) | (0.225–0.281) | (0.05–0.072) | (0.016–0.032) | (0.004–0.01) | |
| W1 Sub-Diagnostic Risky Drinker (n=730) | 0.230 | 0.540 | 0.180 | 0.031 | 0.019 |
| (0.207–0.253) | (0.512–0.568) | (0.156–0.204) | (0.02–0.042) | (0.01–0.028) | |
| W1 Mild AUD (2–3 symptoms) (n=292) | 0.122 | 0.426 | 0.276 | 0.121 | 0.055 |
| (0.101–0.143) | (0.385–0.467) | (0.239–0.313) | (0.085–0.157) | (0.035–0.075) | |
| W1 Moderate AUD (4–5 symptoms) (n=123) | 0.101 | 0.335 | 0.335 | 0.157 | 0.072 |
| (0.075–0.127) | (0.28–0.39) | (0.271–0.399) | (0.109–0.205) | (0.033–0.111) | |
| W1 Severe AUD (6+ symptoms) (n=83) | 0.076 | 0.349 | 0.211 | 0.279 | 0.085 |
| (0.048–0.104) | (0.284–0.414) | (0.161–0.261) | (0.212–0.346) | (0.053–0.117) | |
| Ages 30–34 (n=3100) | |||||
| W2 Abstainer/Low- Risk Drinker (n=1792) |
W2 Sub-Diagnostic Risky Drinker (n=893) |
W2 Mild AUD (2–3 symptoms) (n=289) |
W2 Moderate AUD (4–5 symptoms) (n=81) |
W2 Severe AUD (6+ symptoms) (n=45) |
|
| W1 Abstainer/Low-Risk Drinker (n=1883) | 0.682 | 0.242 | 0.059 | 0.012 | 0.004 |
| (0.658–0.706) | (0.221–0.263) | (0.047–0.071) | (0.007–0.017) | (0.002–0.006) | |
| W1 Sub–Diagnostic Risky Drinker (n=816) | 0.228 | 0.573 | 0.164 | 0.024 | 0.011 |
| (0.207–0.249) | (0.548–0.598) | (0.144–0.184) | (0.017–0.031) | (0.005–0.017) | |
| W1 Mild AUD (2–3 symptoms) (n=267) | 0.141 | 0.463 | 0.228 | 0.129 | 0.038 |
| (0.114–0.168) | (0.423–0.503) | (0.195–0.261) | (0.097–0.161) | (0.019–0.057) | |
| W1 Moderate AUD (4–5 symptoms) (n=88) | 0.114 | 0.266 | 0.282 | 0.216 | 0.121 |
| (0.069–0.159) | (0.211–0.321) | (0.216–0.348) | (0.157–0.275) | (0.064–0.178) | |
| W1 Severe AUD (6+ symptoms) (n=46) | 0.130 | 0.368 | 0.306 | 0.096 | 0.100 |
| (0.081–0.179) | (0.272–0.464) | (0.216–0.396) | (0.045–0.147) | (0.048–0.152) | |
| Ages 35–39 (n=3487) | |||||
| W2 Abstainer/Low- Risk Drinker (n=2141) |
W2 Sub-Diagnostic Risky Drinker (n=909) |
W2 Mild AUD (2–3 symptoms) (n=289) |
W2 Moderate AUD (4–5 symptoms) (n=91) |
W2 Severe AUD (6+ symptoms) (n=57) |
|
| W1 Abstainer/Low-Risk Drinker (n=2227) | 0.726 | 0.205 | 0.057 | 0.008 | 0.003 |
| (0.707–0.745) | (0.188–0.222) | (0.047–0.067) | (0.005–0.011) | (0.001–0.005) | |
| W1 Sub-Diagnostic Risky Drinker (n=899) | 0.284 | 0.513 | 0.147 | 0.037 | 0.020 |
| (0.264–0.304) | (0.487–0.539) | (0.128–0.166) | (0.027–0.047) | (0.014–0.026) | |
| W1 Mild AUD (2–3 symptoms) (n=251) | 0.159 | 0.410 | 0.336 | 0.057 | 0.038 |
| (0.134–0.184) | (0.363–0.457) | (0.293–0.379) | (0.04–0.074) | (0.022–0.054) | |
| W1 Moderate AUD (4–5 symptoms) (n=72) | 0.081 | 0.184 | 0.464 | 0.175 | 0.096 |
| (0.05–0.112) | (0.128–0.24) | (0.39–0.538) | (0.124–0.226) | (0.058–0.134) | |
| W1 Severe AUD (6+ symptoms) (n=38) | 0.085 | 0.141 | 0.252 | 0.228 | 0.293 |
| (0.047–0.123) | (0.08–0.202) | (0.162–0.342) | (0.142–0.314) | (0.166–0.42) | |
| Ages 40–47 (n=6076) | |||||
| W2 Abstainer/Low- Risk Drinker (n=3976) |
W2 Sub-Diagnostic Risky Drinker (n=1447) |
W2 Mild AUD (2–3 symptoms) (n=429) |
W2 Moderate AUD (4–5 symptoms) (n=130) |
W2 Severe AUD (6+ symptoms) (n=94) |
|
| W1 Abstainer/Low-Risk Drinker (n=4182) | 0.783 | 0.170 | 0.034 | 0.006 | 0.007 |
| (0.771–0.795) | (0.159–0.181) | (0.029–0.039) | (0.004–0.008) | (0.005–0.009) | |
| W1 Sub-Diagnostic Risky Drinker (n=1364) | 0.255 | 0.534 | 0.169 | 0.031 | 0.010 |
| (0.239–0.271) | (0.512–0.556) | (0.153–0.185) | (0.024–0.038) | (0.007–0.013) | |
| W1 Mild AUD (2–3 symptoms) (n=368) | 0.111 | 0.460 | 0.285 | 0.092 | 0.052 |
| (0.094–0.128) | (0.426–0.494) | (0.254–0.316) | (0.072–0.112) | (0.037–0.067) | |
| W1 Moderate AUD (4–5 symptoms) (n=96) | 0.072 | 0.306 | 0.258 | 0.187 | 0.177 |
| (0.045–0.099) | (0.246–0.366) | (0.205–0.311) | (0.139–0.235) | (0.119–0.235) | |
| W1 Severe AUD (6+ symptoms) (n=66) | 0.104 | 0.138 | 0.122 | 0.136 | 0.500 |
| (0.064–0.144) | (0.086–0.19) | (0.07–0.174) | (0.089–0.183) | (0.425–0.575) | |
| Ages 48–55 (n=5240) | |||||
| W2 Abstainer/Low- Risk Drinker (n=3735) |
W2 Sub-Diagnostic Risky Drinker (n=1013) |
W2 Mild AUD (2–3 symptoms) (n=322) |
W2 Moderate AUD (4–5 symptoms) (n=113) |
W2 Severe AUD (6+ symptoms) (n=57) |
|
| W1 Abstainer/Low-Risk Drinker (n=3854) | 0.816 | 0.150 | 0.024 | 0.006 | 0.004 |
| (0.802–0.83) | (0.137–0.163) | (0.02–0.028) | (0.004–0.008) | (0.002–0.006) | |
| W1 Sub-Diagnostic Risky Drinker (n=1005) | 0.269 | 0.552 | 0.123 | 0.042 | 0.015 |
| (0.249–0.289) | (0.529–0.575) | (0.107–0.139) | (0.033–0.051) | (0.01–0.02) | |
| W1 Mild AUD (2–3 symptoms) (n=255) | 0.121 | 0.378 | 0.287 | 0.180 | 0.034 |
| (0.097–0.145) | (0.334–0.422) | (0.249–0.325) | (0.133–0.227) | (0.021–0.047) | |
| W1 Moderate AUD (4–5 symptoms) (n=64) | 0.140 | 0.318 | 0.257 | 0.160 | 0.125 |
| (0.094–0.186) | (0.242–0.394) | (0.194–0.32) | (0.113–0.207) | (0.071–0.179) | |
| W1 Severe AUD (6+ symptoms) (n=62) | 0.090 | 0.133 | 0.132 | 0.312 | 0.333 |
| (0.051–0.129) | (0.08–0.186) | (0.083–0.181) | (0.22–0.404) | (0.249–0.417) | |
Note. Transition probability estimates are in bold and are followed in parentheses by one-standard-error ranges around the estimate (with a lower bound of the estimate minus one standard error of the estimate and an upper bound of the estimate plus one standard error of the estimate). Note. Colored cells indicate the “simple” transition probabilities that were later summed to compute the “combined” transition probabilities that are contrasted in tests of primary interest in Table 3, per our definition of AUD desistance as a transition from one of the AUD statuses at Wave 1 to either the Abstainer/Low-Risk-Drinker status or the Sub-Diagnostic Risky Drinker status at Wave 2. Transition probabilities in blue cells were later summed to index desistance from Mild AUD, transition probabilities in red cells were later summed to index desistance from Moderate AUD, and transition probabilities in green cells were later summed to index desistance from Severe AUD.
Contrasts of primary interest
Although results provide information regarding a variety of drinking-related transitions and how they may vary across age groups, of primary interest to the current study were contrasts across age groups in rates of AUD desistance from the three different levels of AUD severity. We defined AUD desistance as transitioning from an AUD status at Wave 1 to a non-AUD status at Wave 2. Thus, we defined Mild-AUD desistance as including transitions from Mild AUD to either Abstainer/Low-Risk Drinker or Sub-Diagnostic Risky Drinker (transitions highlighted in blue in Table 2), we defined Moderate-AUD desistance as including transitions from Moderate AUD to either Abstainer/Low-Risk Drinker or Sub-Diagnostic Risky Drinker (transitions highlighted in red in Table 2), and we defined Severe-AUD desistance as including transitions from Severe AUD to either Abstainer/Low-Risk Drinker or Sub-Diagnostic Risky Drinker (transitions highlighted in green in Table 2).
Thus, in order to test developmental variability in the above three desistance transitions of interest, we first computed “combined” transition probabilities reflecting the sum of multiple “simple” transition probabilities (via Mplus MODEL CONSTRAINT commands; Muthén & Muthén, 1998–2012). For example, separately for each age group, we computed the probability of Severe-AUD desistance as the sum of (1) the probability of transitioning from Severe-AUD to Abstainer/Low-Risk-Drinker plus (2) the probability of transitioning from Severe-AUD to Sub-Diagnostic-Risky-Drinker (the sum of the two transition probabilities highlighted in green for each age group in Table 2).2 After computing this Severe-AUD-desistance probability separately for each age group, we conducted Wald χ2 tests of whether the magnitude of this probability varied significantly across the age groups (via the Mplus MODEL TEST function; Muthén & Muthén, 1998–2012), thereby assessing developmental differences in rates of Severe-AUD desistance. Parallel procedures were carried out to assess developmental differences in rates of Mild-AUD desistance and developmental differences in rates of Moderate-AUD desistance.
Results
Table 2 presents age-group-specific transition probabilities from our primary six-age-group manifest Markov model of drinking-status transitions. It is noteworthy that highly similar results were obtained in multiple supplemental variations of our primary model (see Online Supplements B and C),3 and a very similar pattern of transition probabilities was found in descriptive within-age-group cross-tabulations of Wave-1 drinking status by Wave-2 drinking status (see Online Supplements Appendix D), all of which bolsters confidence in the robustness of our primary results. While the full model results in Table 2 provide information about a variety of forms of drinking-related change across the adult lifespan, below we describe our tests of primary interest assessing developmental differences in rates of AUD desistance from three different levels of AUD severity.
Follow-up tests of primary interest: Age variability in AUD desistance from Mild, Moderate, and Severe AUD
Very broad initial omnibus tests confirmed that there were significant differences across the six age groups (a) among the full set of transition probabilities presented in Table 2 (χ2(100)=656.783 (p<.001)) and (b) among probabilities of the three AUD-desistance transitions of primary interest (χ2(15)=29.036 (p=.016)). Thus, as presented in Table 3, three more specific omnibus tests were conducted to assess age-group differences in probabilities of the three AUD-desistance transitions of interest (Mild-, Moderate-, and Severe-AUD desistance, respectively). These tests showed non-significant age-group differences in rates of desistance from Mild AUD (χ2(5)=8.179 (p=.147)) and in rates of desistance from Moderate AUD (χ2(5)=8.179 (p=.147)), but showed significant age-group differences in rates of desistance from Severe AUD (χ2(5)=11.165 (p=.048)).
Table 3.
Age-group contrasts of desistance-related transition probabilities of primary interest: Comparing the six age groups on AUD desistance from three AUD-severity levels
| Age groups
|
|||||||
|---|---|---|---|---|---|---|---|
| Omnibus Wald χ2 tests | Ages 20–24 (n=2174) |
Ages 25–29 (n=2717) |
Ages 30–34 (n=3100) |
Ages 35–39 (n=3487) |
Ages 40–47 (n=6076) |
Ages 48–55 (n=5240) |
|
| Desistance from Mild AUD | χ2(5)=8.179 (p=.147) | 0.47 | 0.545 | 0.61 | 0.57 | 0.57 | 0.50 |
| (0.43–0.52) | (0.51–0.60) | (0.56– 0.65) | (0.523– 0.62) | (0.54– 0.60) | (0.45– 0.55) | ||
|
| |||||||
| Desistance from Moderate AUD | χ2(5)=6.770 (p=.238) | 0.33 | 0.44 | 0.38 | 0.27 | 0.38 | 0.46 |
| (0.29–0.38) | (0.38–0.50) | (0.31– 0.45) | (0.20– 0.33) | (0.31– 0.44) | (0.38– 0.53) | ||
|
| |||||||
| Desistance from Severe AUDa | χ2(5)=11.165 (p=.048) | 0.29ab | 0.43a | 0.50a | 0.23b | 0.24b | 0.22b |
| (0.23–0.35) | (0.36– 0.49) | (0.40– 0.60) | (0.16– 0.30) | (0.19– 0.30) | (0.15–0.29) | ||
Note. Each main cell contains bolded transition probability estimates followed in parentheses by one-standard-error ranges around the estimate (with a lower bound of the estimate minus one standard error of the estimate and an upper bound of the estimate plus one standard error of the estimate). Note. Colored cells indicate probabilities of desistance from Mild (blue), Moderate (red), and Severe (green) AUD, where desistance was defined as transitions from these AUD statuses at Wave 1 to either the Abstainer/Low-Risk Drinker status or the Sub-Diagnostic Risky Drinker Status at Wave 2 (see Analytic Approach). The above shading corresponds to the shading in Table 2 in order to aid the reader in observing how “simple” transition probabilities in Table 2 were summed to compute the “combined” transition probabilities contrasted across age groups here in Table 3. Note. Prior to conducting the above tests, broader omnibus tests showed significant differences across the six age groups (a) among the full set of transition probabilities presented in Table 2 (χ2(100)=656.783 (p<.001)) and (b) among probabilities of the three AUD-desistance transitions of primary interest (χ2(15)=29.036 (p=.016)). Thus, as tabled above, we proceeded to conducting the three more specific omnibus tests of age-group differences in rates of the three AUD-desistance transitions of primary interest. Only the omnibus test for Severe-AUD desistance was significant, so only for Severe-AUD desistance were follow-up pairwise comparisons among the age groups conducted. Based on these pairwise age-group comparisons, age-group-specific Severe-AUD desistance probabilities that do not share a letter as a postscript were found to differ significantly.
Note that rates of desistance from Severe AUD were also very close to significantly lower at ages 20–24 when compared to both ages 25–29 (p=.112) and ages 30–34 (p=.053).
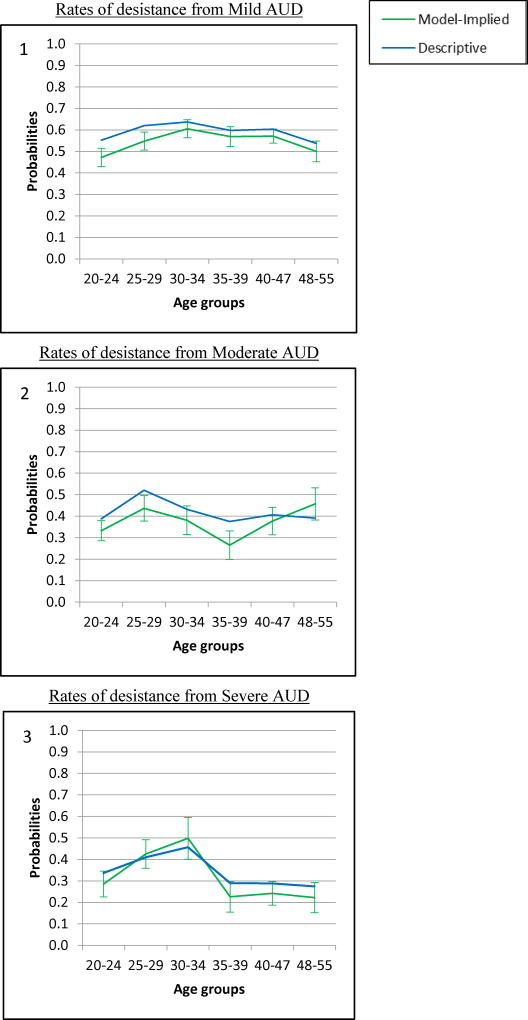
Thus, follow-up tests of pairwise differences among the age groups were conducted only for rates of desistance from Severe AUD. Results indicated that Severe-AUD desistance was more likely to occur in young adulthood than in midlife. Specifically, rates of Severe-AUD desistance were significantly higher at both ages 25–29 and 30–34 when compared to ages 35–39, 40–47, and 48–55 (see Table 3). As illustrated in Panel 3 of Figure 1, it was quite a substantial decrease in Severe-AUD desistance rates that was observed to occur from young adulthood to midlife, with a peak of 43–50% across the two age groups spanning ages 25–34, followed by a drop to 22–24% across the three age groups spanning ages 35–55.
Figure 1. Plots of differences across age groups in rates of AUD desistance from (1) Mild AUD, (2) Moderate AUD, and (3) Severe AUD.
Green lines show model-derived transition-probability estimates with bars showing one-standard-error ranges around the estimate. Blue lines show transition probabilities based on simple descriptive cross-tabulations of Wave-1 drinking status by Wave-2 drinking status within age groups.
It is noteworthy that Severe-AUD desistance was also very close to significantly lower for emerging adults (i.e., at ages 20–24) when compared to young adults at both ages 25–29 (p=.095) and ages 30–34 (p=.055). Thus, there appeared to be elevated rates of Severe-AUD desistance during young adulthood relative to both earlier and later developmental periods (see Panel 3 of Figure 1), although significance testing most clearly supported this young-adult elevation in relation to the lower rates observed in the later midlife age groups.
Other noteworthy post-hoc conclusions
Aside from the above tests of primary substantive interest, there are additional noteworthy patterns of findings suggested by the full set of age-group-specific transition probabilities presented in Table 2. We discuss some such patterns here, although we do not provide statistical tests of these patterns in order to distinguish these relatively tentative post-hoc conclusions from our above a priori hypothesis tests of primary substantive interest (those presented in Table 3). While our tests of primary interest showed significantly elevated rates of Severe-AUD desistance in young adulthood, examination of the overall pattern in Table 2 suggests that this may be primarily attributable to young-adult elevations in transitions from Severe-AUD to sub-diagnostic risky drinking as opposed to abstinence/low-risk-drinking. Indeed, greater elevations during young adulthood (ages 25–29 and 30–34) are observed for transitions from the Severe-AUD status to the Sub-Diagnostic-Risky-Drinker status than for transitions from the Severe-AUD status to the Abstainer/Low-Risk-Drinker status. However, while young adulthood does show a particularly pronounced pattern of more frequent desistance to sub-diagnostic risky drinking as opposed to abstinence/low-risk-drinking, it is noteworthy that this is a somewhat pervasive pattern across all developmental periods. In fact, across all age groups and all initial AUD severity levels, AUD desistance more often resulted in a transition to the Sub-Diagnostic-Risky-Drinker status compared to the Abstainer/Low-Risk-Drinker status. Another noteworthy pattern is an age-related increase in rates of stability of low-risk statuses, suggesting a lifespan-developmental decrease in problem-drinking escalation and AUD onset. Particularly dramatic increases across ascending age groups were observed for the probability of remaining an abstainer/low-risk-drinker from Wave 1 to Wave 2. More modest increases were also observed for those who either remained a sub-diagnostic risky drinker or declined from this status to become an abstainers/low-risk-drinker (as opposed to escalating to one of the three AUD statuses).
Additional post-hoc considerations pertained to the generalizability of our findings across demographic subgroups of sex and race/ethnicity. As presented in Online Supplements Appendices F-J, we re-estimated our manifest Markov model within subgroups of females, males, Caucasians, African-Americans, and Hispanics; although we did not conduct follow-up tests in these subgroups to parallel our full-sample tests of primary interest (those presented in Table 3). Results regarding age differences in patterns of AUD desistance appeared somewhat robust across the demographic subgroups, with some noteworthy exceptions. Regarding sex differences, males were most consistent with the full-sample pattern of (1) relative stability in rates of Mild- and Moderate-AUD desistance and (2) substantially elevated rates of Severe-AUD desistance in young adulthood (see Online Supplements Figure F1). In contrast, while females also showed relative developmental stability in rates of Mild-AUD desistance, they showed far higher rates of Moderate-AUD desistance in young adulthood than in later periods, with a more modest young-adult spike in rates of Severe-AUD desistance only at ages 30–34 (see Online Supplements Figure G1). Regarding race/ethnicity differences, Caucasians were most consistent with the full-sample pattern of (1) relative stability in rates of Mild- and Moderate-AUD desistance and (2) substantially elevated rates of Severe-AUD desistance in young adulthood (see Online Supplements Figure H1). In contrast, while Hispanics also showed relative developmental stability in rates of Mild-AUD desistance, they showed a complex pattern of declines in Moderate-AUD desistance rates from young adulthood to midlife that was interrupted by a substantial spike in the midlife age group of 40–47 (see Online Supplements Figure I1). In addition, although Hispanics showed elevated rates of Severe-AUD desistance during young adulthood (consistent with full-sample results), this was limited to an extremely substantial spike in rates during the young-adult period of ages 30–34, with extremely low rates in the preceding young-adult period of ages 25–29. Finally, while African-Americans also showed relative developmental stability in rates of Mild-AUD desistance, they showed elevated rates of both Moderate- and Severe-AUD desistance during young adulthood. For Moderate-AUD desistance, they showed a somewhat substantial spike in rates across both young-adult periods of ages 25–29 and 30–34. In contrast, for Severe-AUD desistance, they showed an extremely substantial spike in rates in only the young-adult period of ages 25–29, with extremely low rates in the following young-adult period of ages 30–34 (see Online Supplements Figure J1).
Discussion
Although epidemiologic data clearly show a pattern of age-related reduction in alcohol use and related pathology beginning in young adulthood and continuing throughout the adult lifespan, little past research has been done to clarify the precise form of these changes or to assess the extent to which the form of these changes varies across developmental periods. We used data from the U.S.-representative NESARC sample to investigate this issue. We estimated manifest Markov models to characterize longitudinal transitions among drinking statuses and to characterize developmental variability in transition patterns across six different developmentally-informed age groups spanning ages 20–24 to ages 48–55. While our results provide a rich, developmentally-sensitive account of various forms of drinking-behavior change (see Table 2), our primary objective was to test lifespan-developmental differences in rates of AUD desistance from different levels of AUD severity (as presented in Table 3). Findings indicated that rates of desistance from Severe AUD were far higher in young adulthood than in later developmental periods (while desistance from less severe AUDs varied less substantially by age). Especially given the dramatic change reflected by the Severe-AUD-desistance transition (a reduction from at least six AUD symptoms to either zero or one symptom), it is particularly remarkable to note the substantial magnitude of developmental variability in this transition that is indicated by our findings. Specifically, Severe-AUD desistance rates peaked at around 43–50% for the two age groups spanning ages 25–34 and then dropped to around 22–24% for the three age groups spanning ages 35–55.
The Clinical Significance of the Young-Adult “Maturing Out” Phenomenon
By resolving the severity of AUDs in this study, we were able to demonstrate that the well-documented reductions in alcohol consumption and problem drinking that occur in young adulthood (i.e., “maturing out”) represent a more clinically and practically significant phenomenon than previously recognized. As noted in the Introduction, some models of AUD subtypes and related heterogeneity in AUD course (e.g., developmentally-limited vs. -persistent AUDs) can confer an expectation that much of the desistance occurring in young adulthood will be from relatively mild AUDs, whereas desistance from more severe AUDs may be expected more often in later developmental periods (Martin, Chung, & Langenbucher, 2016; Zucker et al., 2016). To the contrary, our finding appear to indicate a substantial prevalence of severe yet developmentally-limited AUD, although admittedly without establishing the long-term stability of these changes. Future work should therefore extend our analyses to data that span longitudinally throughout the adult life course (i.e., following individuals from early to late adulthood).
Past research has also provided reason to question the practical/clinical significance of young-adult “maturing out” based on concerns about developmentally-specific diagnostic errors around this age period. Specifically, it has been suggested that a considerable amount of the observed elevations in AUD rates in the years preceding young adulthood may reflect “false-positive” diagnoses owing to problems with certain specific AUD criteria (e.g., elevated erroneous endorsements of the “tolerance” and “withdrawal” criteria; Caetano & Babor, 2006; Harford et al., 2005). Such false-positive diagnoses in the years preceding young adulthood could, in turn, lead to spurious observations of desistance as individuals transition to young adulthood. While these measurement concerns are likely valid and may indeed enhance the overall appearance of young-adult AUD desistance, it is unlikely that this explains the current study’s evidence for widespread young-adult desistance from Severe AUD, given the magnitude of symptom change required for Severe-AUD desistance (a reduction from 6 or more to less than 2 symptoms). Thus, our results show widespread young-adult desistance specifically from a form of AUD that is likely to reflect a clinically-significant condition and unlikely to reflect measurement-related diagnostic error.
Our Findings in the Context of Other Research on Adult-Developmental Differences in Patterns of Problem-Drinking Change
While our findings are highly novel, they confirm and substantially extend conclusions of previous research. In the single past study to our knowledge with an objective similar to ours, Lee, Chassin, and Villalta (2013) conducted a latent transition analysis of drinking status transitions in a high-risk community sample with a relatively limited sample size (N=844) and age range (17–40). Their results showed that, in young adulthood, problem-drinking reductions were most common among those initially in the most severe of four problem-drinking statuses; whereas, in the later period of early midlife, initial severity was not significantly related to the likelihood of problem-drinking reductions. While our findings are consistent with Lee et al.’s, the current study substantially extends theirs, facilitating a number of novel and important empirical insights. Specifically, Lee et al.’s analyses were far less differentiated on problem-drinking severity, failing to even distinguish sub-diagnostic from supra-diagnostic problem drinkers (65% of their most “severe” drinker status met AUD diagnostic criteria). In contrast, our analyses differentiated multiple levels of supra-diagnostic AUD severity via DSM-5 AUD-severity grading (APA, 2013). Also, unlike Lee et al.’s study, “desistance” transitions in our study truly reflected AUD desistance in that those who desisted had transitioned from meeting AUD diagnostic criteria to not meeting AUD diagnostic criteria. These two features substantially enhance the interpretability and clinical/practical relevance of our findings. In addition, while Lee et al. characterized desistance only in young adulthood and early midlife without statistical tests of age differences, our analyses contrasted six developmental periods spanning much of the adult lifespan, with formal tests of age differences in desistance rates. These novel and important features of the current study were facilitated by our use of the very large, highly age heterogeneous NESARC sample, which also provided U.S.-representative data to enhance generalizability of findings.
Other research advancing an understanding of lifespan-developmental differences in patterns of problem-drinking change includes Vergés et al.’s (2012) work “deconstructing the age-prevalence curve.” Vergés et al. assessed changes across the lifespan in rates of AUD persistence, AUD onset, and AUD recurrence; with the objective of understanding their unique contributions to overall age-related reductions in alcohol-dependence rates. Their results showed especially marked age reductions in new onsets. Thus, they emphasized the implication that, while the decreases in AUD rates observed over the lifespan may be assumed to indicate developmental increases in AUD desistance, their results indicate a considerable impact of developmental reductions in AUD onsets (Vergés et al., 2012). In contrast, regarding AUD desistance, they concluded that there was relative developmental stability across the lifespan based on nonsignificant age effects on persistence rates. However, their descriptive results appear to indicate a modest peak in the prevalence of AUD desistance during young adulthood. Specifically, based on their persistence rates, it can be inferred that rates of desistance peaked at 72% by ages 28–32 and then declined to a low of 55% by ages 43–52, remaining somewhat low thereafter. Thus, while risk for AUD onset may decrease throughout the lifespan, the potential for desistance from an existing AUD may peak in young adulthood. The latter notion is supported and extended by the current study’s findings, as our results indicate a young-adult peak in potential for AUD desistance especially for those with a Severe AUD.
Possible Implications Regarding Lifespan Differences in Mechanisms of AUD Desistance
Beyond the current study and others described above, surprisingly little work has been done toward understanding developmental differences across the adult lifespan in patterns and predictors of problem-drinking desistance. Advancing this area of research is important, given the clear evidence that unique insights into psychopathology can be gleaned by taking a developmentally-informed perspective (Chassin, Sher, Hussong, & Curran, 2013; Cicchetti & Toth, 2009; NIAAA, 2008a). Further, a lifespan-developmental approach to desistance research can help address the need for increased empirical attention to problem drinking in midlife and older adults (Chassin, Sher, Hussong, & Curran, 2013; NIAAA, 2008a), which is of particular importance given the increases in older-adult problem drinking projected to coincide with the aging of the “baby boomer” generation (Gfroerer, Penne, Pemberton, & Folsom, 2003; Han, Gfroerer, Colliver, & Penne, 2009).
By showing lifespan-developmental differences in patterns of problem-drinking desistance, our findings suggest a likely utility of future lifespan-developmental research aimed at understanding mechanisms of desistance and how they may vary across the lifespan. Future research should investigate (1) whether different mechanisms tend to spur desistance in different developmental periods and (2) whether this can explain the current study’s evidence for different patterns of desistance in different developmental periods. Given our evidence that desistance from Severe AUD is especially common in young adulthood, future research may reveal that there are certain mechanisms that (1) operate predominantly in young adulthood and (2) are particularly capable of spurring desistance from Severe AUD. This would suggest that research should prioritize efforts to advance a richer understanding of how these particular mechanisms of desistance operate during young adulthood. This could prove to be a rather fruitful inroad toward informing clinical and public health interventions targeting severe problem drinkers.
In contemplating specific ways that desistance mechanisms may vary developmentally, predictions can be based on Watson and Sher’s (1998) review highlighting dramatic conceptual differences between the “maturing out” and “natural recovery” literatures. The “maturing out” literature, focused on young adulthood, has largely viewed problem drinking reductions as stemming from the rapid contextual changes occurring in this period. Particular emphasis has been placed on young-adult transitions into adult roles (marriage, parenthood, full-time employment; Bachman et al., 1997) and accompanying contextual changes that pose incompatibility with certain forms of alcohol involvement (Watson & Sher, 1998; Yamaguchi & Kandel, 1985a, 1985b). Importantly, these processes are rarely conceptualized as involving acknowledgement or concern regarding one’s drinking (Jackson & Sartor, 2016; Watson & Sher, 1998). A starkly different view of desistance comes from the “natural recovery” literature, which has investigated precursors of desistance mostly in midlife samples (e.g., Mage=41 [SD=9.1] in a review by Sobell et al. [2000]). Informed in part by models of behavior change (e.g., Stall & Biernacki’s [1986] “stages of spontaneous remission”), this literature often views desistance as stemming from an accumulation of drinking consequences that can prompt (1) deliberate reappraisals of one’s drinking, then (2) self-identification as a problem drinker (i.e., problem recognition), and then (3) targeted efforts to change drinking habits (Klingemann & Sobell, 2007).
Predictions regarding developmental variability in desistance mechanisms can stem from the premise that the maturing out and natural recovery literatures may both offer valid models of desistance, but with maturing-out models applying more to young adulthood and natural-recovery models applying more to later developmental periods (Lee & Sher, in press). That is, desistance in young adulthood may tend to occur as a byproduct of the maturational role changes that characterize this period, whereas desistance in later periods may tend to stem from more deliberate and drinking-specific processes of problem recognition and effortful change. In light of our current findings, an additional prediction is that the role changes that may be especially central to young-adult desistance may also be particularly impactful in ameliorating relatively severe AUDs. Of course, basing such predictions on the current study’s findings is quite speculative at present. Little research exists to date investigating lifespan-developmental differences in desistance mechanisms, let alone whether this can explain lifespan-developmental differences in patterns of desistance (such as those found here). Future research pursing these lines of inquiry could offer key insights toward tailoring interventions both for different developmental periods and for different AUD-severity levels.
An example of how such work could inform interventions pertains to potential clinical applications of role incompatibility theory (Yamaguchi & Kandel, 1985a, 1985b), a theory commonly applied in conceptualizing young-adult role-transition effects (e.g., Bachman et al., 1997; Curran, Muthen, & Harford, 1998; Derrick & Leonard, 2016; Gotham et al., 2003; Lee, Chassin, & MacKinnon, 2010; Schulenberg, Maggs, & O’Malley, 2003; Staff et al., 2010). If future research confirms that processes of role-incompatibility resolution drive a spike in Severe-AUD desistance during young adulthood, it would follow that a richer understanding of role-incompatibility resolution could yield key practical insights. Clinical applications may involve enhancing and guiding ongoing role-incompatibility-resolution processes among young adults or activating such processes in later developmental periods where this may be less likely to occur naturally. The integration of role-incompatibility themes into clinical practice is consistent with motivational enhancement approaches that aim to illuminate and leverage discrepancies of patients’ problem behaviors with their goals and values (e.g., Miller & Rollnick, 2002). Although this example is currently quite speculative, it illustrates the notion that lifespan-developmental desistance research could inform the design of interventions targeting problem drinkers of different developmental periods.
Limitations
Although this study makes a substantial contribution toward advancing a more developmentally-informed understanding of AUD desistance across the adult lifespan, there are important limitations that should be acknowledged.
Exclusion of participants over age 55
One key limitation was the failure to extend our analyses into older adulthood. We excluded those over age 55 due to sparseness of some drinking statuses and concerns regarding attrition bias. Regarding sparseness, Online Supplements Table A3 shows extremely low prevalence rates in some drinking statuses among those over age 55. Further, Online Supplements Table D1 shows how this sparseness problem is compounded when considering drinking-status transitions representing specific combinations of Wave 1 and Wave 2 statuses. Regarding our concerns about attrition bias, ancillary descriptive analyses of transition probabilities show a dramatic increase in rates of Severe-AUD desistance that begins at ages 55–69 and becomes extremely pronounced at ages 70+ (see Online Supplements Figure D1). While this may reflect a true phenomenon, a highly plausible alternative explanation is that, among older participants with Wave-1 Severe AUD, retention by Wave 2 may have been substantially more likely for those who did versus did not desist. AUD chronicity may be particularly related to attrition at these older ages, for instance, due to chronicity-related health problems or mortality (Adams & Smith, 1995; Chatfield, Brayne, & Matthews, 2005; Gossop et al., 2007; O’Connell, Chin, Cunningham, & Lawlor, 2003; Radler & Ryff, 2010). Such attrition bias could substantially inflate estimates of Severe-AUD desistance at these older ages, so we excluded those over age 55 to avoid potentially misleading results. This concern was supported by additional attrition-bias analyses we conducted of age-group-specific differences between those retained versus not retained at Wave 2. Indeed, although our overall attrition-bias analyses described in Participants and Procedures showed lower Wave-1 alcohol consumption and AUD symptoms among those not retained at Wave 2 (see Online Supplements Table A1), this pattern reversed with age, with older-adult-specific contrasts showing higher Wave-1 alcohol consumption and AUD symptoms among those not retained at Wave 2 (see Online Supplements Table A2).
In future research, it will be important to keep aging-related attrition bias in mind as a methodological concern that is particularly critical in studies on the increasingly important topic of older-adult problem drinking (Han et al., 2009; NIAAA, 2008a). Thus, it will be important to establish strategies for addressing this concern, such as supplementing self-reports with collateral reports (e.g., spouse, peers, adult children) and archival data (e.g., health-care records).
Note, however, that while this issue precluded investigation of desistance beyond age 55, it is unlikely that such attrition bias spuriously produced this study’s conclusion of elevated Severe-AUD desistance in young adulthood. It is true that AUD-chronicity-driven attrition may have occurred even among participants included in analyses. However, if present, such age-related attrition bias would likely diminish rather than enhance our evidence for elevated Severe-AUD desistance in young adulthood. With such attrition bias increasing at older ages and thus affecting midlife more than young-adult participants, our results would increasingly under-represent the extent of Severe-AUD chronicity in older age groups. That is, this bias would cause rates of Severe-AUD desistance to be more inflated in midlife than in young adulthood, thus reducing rather than enhancing the appearance of greater Severe-AUD desistance in young adulthood.
Choices regarding our drinking-status classification
Any choices regarding how to distinguish among drinking statuses would bring certain advantages and disadvantages. We chose to make less nuanced distinctions among drinking statuses at the lower end of the alcohol-involvement/problem-drinking “spectrum” and more nuanced distinctions among drinking statuses at the higher end of this spectrum. This approach brings key advantages that are particularly important in light of our primary interest in characterizing patterns of AUD desistance from different levels of AUD severity. Of course, making more nuanced distinctions among drinking statuses at the lower end of this spectrum (e.g., differentiating abstainers from low-risk drinkers) would likely provide additional information beyond our results (e.g., how often AUD desistance results in abstinence versus low-risk drinking and whether or not this varies by age). However, such questions are at best tangential to those of primary interest in our study, and attempting to address them through increasing our number of drinking statuses would limit modeling feasibility and complicate our presentation of results. Nonetheless, for the interested reader, it should be noted that Online Supplements Appendix E presents descriptive information on nine smaller drinking-related groups from which our five drinking statuses were comprised, including descriptive information on age-group specific rates of transitions among these nine drinking-related groups.
Limitations of the NESARC dataset for cohort comparisons and characterizing individual life-course development
While offering many critical advantages for the purposes of the current study, there are certain limitations of the NESARC dataset that correspond to limitations of the current study’s analyses. Although longitudinal, NESARC has a relatively short follow-up period (i.e., three years), which provides minimal opportunity to examine cohort effects across equivalent ages. While, ideally, it would be useful to conduct age-period-cohort analyses that could disambiguate the influence of these three conceptually distinct but correlated factors (e.g., Kerr, Greenfield, Bond, Ye, & Rehm, 2009), data sets that are adequately prospective, heterogeneous with respect to age and historical period, and diagnostically informative are currently lacking. However, the potential importance of both cohort and period effects should be considered when seeking to generalize findings across different historical periods.
In addition, there is minimal information in the NESARC data about participants’ lifetime course of problem-drinking and AUD prior to their assessments at NESARC Waves 1 and 2. While NESARC does assess “prior to past year” AUD symptomatology at Wave 1, utilizing these data to characterize pre-Wave-1 course of AUD may be hazardous due to established concerns about the reliability of lifetime assessments of AUD, as well as other disorders (e.g., Haeny, Littlefield, & Sher, 2014; Moffitt et al., 2010). Nonetheless, while lacking data on individual changes across the adult lifespan, the current study’s contrasts of age groups across the adult lifespan do provide novel insights toward informing lifespan-developmental models of problem drinking and AUD.
Lack of the craving symptom in AUD diagnoses
Another limitation is the absence of craving from the AUD diagnostic algorithm, due to the fact that this symptom was not assessed in NESARC at Wave 1. Differences in the algorithm used (in this case, 2 out of 10 symptoms, compared to the “official” DSM-5 algorithm defined by 2 out of 11 symptoms) can lead to differences in chronicity estimates (Vergés, Steinley, Trull, & Sher, 2010). Although it is not possible to establish agreement in desistance rates between these definitions using the NESARC data, it is possible to compare their prevalence rates at Wave 2. Prevalence rates were fairly similar (DSM-5 AUD: 10.78%; modified DSM-5 AUD: 10.45%), and only 106 participants (i.e., 2.98% of those with DSM-5 AUD) were misclassified by the modified algorithm. This provides evidence supporting the use of the current algorithm as a very good approximation to DSM-5.
Lack of tests of mechanisms of AUD desistance
While our results advanced an understanding of patterns of AUD desistance across the adult lifespan, we did not incorporate predictors representing potential mechanisms of AUD desistance. Thus, our interpretation of findings as potentially reflecting developmental differences in desistance mechanisms is indeed highly speculative at present. However, we view the current study as a key first step in a larger line of lifespan-developmental desistance research, with investigations of developmental differences in AUD-desistance mechanisms being a clear next step.
Supplementary Material
Acknowledgments
This research was supported by National Institute on Alcohol Abuse and Alcoholism grants K99-AA024236 to Matthew R. Lee and K05-AA017242 to Kenneth J. Sher.
Footnotes
In logit parameterization, Mplus reports transition probabilities, including within different levels of a KNOWNCLASS grouping variable (e.g., levels of our age-group variable; in TECH15 output [Muthén & Muthén, 1998–2012]), but transition-probability standard errors are not included. Thus, we were able to confirm that our transition probabilities computed via MODEL CONSTRAINT precisely matched those reported by Mplus. Further, computing these transition probabilities facilitated formal tests of how they differed among age groups.
By including separate drinking statuses for Abstainers/Low-Risk-Drinkers and Sub-Diagnostic Risky Drinkers but then combining them in our follow-up tests of AUD desistance transitions, we aimed to strike a balance between (1) providing a relatively rich depiction of various forms of drinking-related change in our overall results (see Table 2) and (2) achieving clear and appropriate tests of our AUD-desistance-related hypotheses of primary interest (see Table 3).
Although our primary analysis used Wave-2 age to define the grouping variable and therefore required exclusion of participants who were not retained at Wave 2 (see Participants and Procedures), highly similar results were obtained in a supplemental model that used Wave-1 age to define the grouping variable and thereby allowed inclusion of participants who were not retained at Wave 2 (see Online Supplements Appendix B). In addition, although our primary analysis controlled for covariate effects of sex and race/ethnicity, it is noteworthy that very similar results were obtained from an analysis without covariates (see Online Supplements Appendix C).
Contributor Information
Matthew R. Lee, Department of Psychological Sciences, University of Missouri, Columbia
Cassandra L. Boness, Department of Psychological Sciences, University of Missouri, Columbia
Yoanna E. McDowell, Department of Psychological Sciences, University of Missouri, Columbia
Alvaro Vergés, Escuela de Psicología, Pontificia Universidad Católica de Chile.
Douglas L. Steinley, Department of Psychological Sciences, University of Missouri, Columbia
Kenneth J. Sher, Department of Psychological Sciences, University of Missouri, Columbia
References
- Adams WL, Smith NS. Epidemiology of problem drinking among elderly people. The International Journal of the Addictions. 1995;30(13–14):1693–1716. doi: 10.3109/10826089509071053. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5. Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- Bachman JG, Wadsworth KN, O’Malley PM, Johnston LD. Smoking, drinking, and drug use in young adulthood: The impacts of new freedoms and new responsibilities. Hillsdale, NJ, England: Lawrence Erlbaum Associates, Inc; 1997. [Google Scholar]
- Caetano R, Babor TF. Diagnosis of alcohol dependence in epidemiological surveys: An epidemic of youthful alcohol dependence or a case of measurement error? Addiction. 2006;101(SUPPL. 1):111–114. doi: 10.1111/j.1360-0443.2006.01599.x. http://doi.org/10.1111/j.1360-0443.2006.01599.x. [DOI] [PubMed] [Google Scholar]
- Chassin L, Sher KJ, Hussong A, Curran P. The developmental psychopathology of alcohol use and alcohol disorders: Research achievements and future directions. Development and Psychopathology. 2013;25(4pt2):1567–1584. doi: 10.1017/S0954579413000771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chatfield MD, Brayne CE, Matthews FE. A systematic literature review of attrition between waves in longitudinal studies in the elderly shows a consistent pattern of dropout between differing studies. Journal of Clinical Epidemiology. 2005;58(1):13–19. doi: 10.1016/j.jclinepi.2004.05.006. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Toth SL. The past achievements and future promises of developmental psychopathology: The coming of age of a discipline. Journal of Child Psychology and Psychiatry. 2009;50(1–2):16–25. doi: 10.1111/j.1469-7610.2008.01979.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curran PJ, Muthen BO, Harford TC. The influence of changes in marital status on developmental trajectories of alcohol use in young adults. Journal of Studies on Alcohol. 1998;59:647–658. doi: 10.15288/jsa.1998.59.647. [DOI] [PubMed] [Google Scholar]
- Derrick J, Leonard K. Substance Use in Committed Relationships. In: Sher KJ, editor. The Oxford handbook of substance use and substance use disorders. New York, NY: Oxford University Press; 2016. [Google Scholar]
- Gfroerer J, Penne M, Pemberton M, Folsom R. Substance abuse treatment need among older adults in 2020: the impact of the aging baby-boom cohort. Drug and Alcohol Dependence. 2003;69(2):127–135. doi: 10.1016/s0376-8716(02)00307-1. [DOI] [PubMed] [Google Scholar]
- Gossop M, Neto D, Radovanovic M, Batra A, Toteva S, Musalek M, Skutle A, Goos C. Physical health problems among patients seeking treatment for alcohol use disorders: a study in six European cities. Addiction Biology. 2007;12(2):190–196. doi: 10.1111/j.1369-1600.2007.00066.x. [DOI] [PubMed] [Google Scholar]
- Gotham HJ, Sher KJ, Wood PK. Alcohol involvement and developmental task completion during young adulthood. Journal of Studies on Alcohol. 2003;64:32–42. doi: 10.15288/jsa.2003.64.32. [DOI] [PubMed] [Google Scholar]
- Grant BF, Kaplan KK, Stinson FS. Source and Accuracy Statement for the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2005. [Google Scholar]
- Haeny AM, Littlefield AK, Sher KJ. Repeated diagnoses of lifetime alcohol use disorders in a prospective study: insights into the extent and nature of the reliability and validity problem. Alcoholism: Clinical and Experimental Research. 2014;38(2):489–500. doi: 10.1111/acer.12237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han B, Gfroerer JC, Colliver JD, Penne MA. Substance use disorder among older adults in the United States in 2020. Addiction. 2009;104(1):88–96. doi: 10.1111/j.1360-0443.2008.02411.x. [DOI] [PubMed] [Google Scholar]
- Harford TC, Grant BF, Yi H, Chen CM. Patterns of DSM-IV alcohol abuse and dependence criteria among adolescents and adults: Results from the 2001 national household survey on drug abuse. Alcoholism: Clinical and Experimental Research. 2005;29:810–828. doi: 10.1097/01.ALC.0000164381.67723.76. [DOI] [PubMed] [Google Scholar]
- Jackson KM, Sartor CE. The natural course of substance use and dependence. In: Sher KJ, editor. The Oxford handbook of substance use and substance use disorders. New York, NY: Oxford University Press; 2016. [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE, Miech RA. Monitoring the Future national survey results on drug use, 1975–2013: Volume II, college students and adults ages 19–55. Ann Arbor: Institute for Social Research, The University of Michigan; 2014. [Google Scholar]
- Kaplan D. An overview of Markov chain methods for the study of stage-sequential developmental processes. Developmental Psychology. 2008;44(2):457. doi: 10.1037/0012-1649.44.2.457. [DOI] [PubMed] [Google Scholar]
- Kerr WC, Greenfield TK, Bond J, Ye Y, Rehm J. Age-period-cohort modelling of alcohol volume and heavy drinking days in the US National Alcohol Surveys: divergence in younger and older adult trends. Addiction. 2009;104(1):27–37. doi: 10.1111/j.1360-0443.2008.02391.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klingemann HK, Sobell LC. Promoting Self-Change from Addictive Behaviors: Practical Implications for Policy, Prevention, and Treatment. New York, NY: Springer; 2007. [Google Scholar]
- Lee MR, Chassin L, MacKinnon D. The effect of marriage on young adult heavy drinking and its mediators: Results from two methods of adjusting for selection into marriage. Psychology of Addictive Behaviors. 2010;24:712–718. doi: 10.1037/a0020983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee MR, Chassin L, Villalta IK. Maturing out of alcohol involvement: Transitions in latent drinking statuses from late adolescence to adulthood. Development and Psychopathology. 2013;25(4pt1):1137–1153. doi: 10.1017/S0954579413000424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee MR, Sher KJ. “Maturing out” of binge and problem drinking. Alcohol Research: Current Reviews. (in press) [PMC free article] [PubMed] [Google Scholar]
- Li TK, Hewitt BG, Grant BF. Is there a future for quantifying drinking in the diagnosis, treatment, and prevention of alcohol use disorders? Alcohol and Alcoholism. 2007;42(2):57–63. doi: 10.1093/alcalc/agl125. [DOI] [PubMed] [Google Scholar]
- Martin CS, Chung T, Langenbucher J. Historical and Cultural Perspectives on Substance Use and Substance Use Disorders. In: Sher KJ, editor. Oxford handbook of substance use and substance use disorders. New York, NY: Oxford University Press; 2016. [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Preparing people for change. 2. New York: Guilford Press; 2002. [Google Scholar]
- Moffitt TE, Caspi A, Taylor A, Kokaua J, Milne BJ, Polanczyk G, Poulton R. How common are common mental disorders? Evidence that lifetime prevalence rates are doubled by prospective versus retrospective ascertainment. Psychological Medicine. 2010;40(6):899–909. doi: 10.1017/S0033291709991036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide. Seventh. Los Angeles, CA: Muthén & Muthén; 1998–2012. [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. The National Institute on Alcohol Abuse and Alcoholism Five Year Strategic Plan: FY09-14 “Alcohol Across the Lifespan”. 2008a. [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. Wave 2 NESARC data notes. 2008b. [Google Scholar]
- O’Connell H, Chin AV, Cunningham C, Lawlor B. Alcohol use disorders in elderly people-redefining an age old problem in old age. BMJ. 2003;327(7416):664–667. doi: 10.1136/bmj.327.7416.664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radler BT, Ryff CD. Who participates? Accounting for longitudinal retention in the MIDUS National Study of Health and Well-Being. Journal of Aging and Health. 2010;22(3):307–311. doi: 10.1177/0898264309358617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutter M. Age as an ambiguous variable in developmental research: Some epidemiological considerations from developmental psychopathology. International Journal of Behavioral Development. 1989;12(1):1–34. [Google Scholar]
- Schulenberg J, Maggs JL, O’Malley PM. How and why the understanding of developmental continuity and discontinuity is important: The sample case of long-term consequences of adolescent substance use. In: Mortimer JT, Shanahan M, editors. Handbook of the life course. New York: Kluwer Academic/Plenum Publishers; 2003. pp. 413–436. [Google Scholar]
- Sobell LC, Ellingstad TP, Sobell MB. Natural recovery from alcohol and drug problems: Methodological review of the research with suggestions for future directions. Addiction. 2000;95(5):749–764. doi: 10.1046/j.1360-0443.2000.95574911.x. [DOI] [PubMed] [Google Scholar]
- Staff J, Schulenberg JE, Maslowsky J, Bachman JG, O’Malley PM, Maggs JL, Johnston LD. Substance use changes and social role transitions: Proximal developmental effects on ongoing trajectories from late adolescence through early adulthood. Development and Psychopathology. 2010;22:917–932. doi: 10.1017/S0954579410000544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stall R, Biernacki P. Spontaneous remission from the problematic use of substances: An inductive model derived from a comparative analysis of the alcohol, opiate, tobacco, and food/obesity literatures. Substance Use & Misuse. 1986;21(1):1–23. doi: 10.3109/10826088609063434. [DOI] [PubMed] [Google Scholar]
- Vergés A, Jackson KM, Bucholz KK, Grant JD, Trull TJ, Wood PK, Sher KJ. Deconstructing the age-prevalence curve of alcohol dependence: Why “maturing out” is only a small piece of the puzzle. Journal of Abnormal Psychology. 2012;121(2):511–523. doi: 10.1037/a0026027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vergés A, Steinley D, Trull TJ, Sher KJ. It’s the algorithm! Why differential rates of chronicity and comorbidity are not evidence for the validity of the abuse-dependence distinction. Journal of Abnormal Psychology. 2010;119:650–661. doi: 10.1037/a0020116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson AL, Sher KJ. Resolution of alcohol problems without treatment: methodological issues and future directions of natural recovery research. Clinical Psychology: Science and Practice. 1998;5:1–18. [Google Scholar]
- Yamaguchi K, Kandel DB. Dynamic relationships between premarital cohabitation and illicit drug use: An event-history analysis of role selection and role socialization. American Sociological Review. 1985a;50:530–546. [Google Scholar]
- Yamaguchi K, Kandel DB. On the resolution of role incompatibility: A life event history analysis of family roles and marijuana use. American Journal of Sociology. 1985b;90:1284–1325. [Google Scholar]
- Zucker RA, Hicks BM, Heitzeg MM. Alcohol use and the alcohol use disorders over the life course: A cross-level developmental review. In: Cicchetti D, editor. Developmental psychopathology: Risk, disorder, and adaptation. Vol. 3. Hoboken, NJ: Wiley; 2016. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.