Abstract
Background
Force platform training with functional electric stimulation aimed at improving balance may be effective in fall prevention for older adults. Aim of the study is to evaluate the effects of the visual-feedback-based force platform balance training with functional electric stimulation on balance and fall prevention in older adults.
Methods
A single-centre, unblinded, randomized controlled trial was conducted. One hundred and twenty older adults were randomly allocated to two groups: the control group (n = 60, one-leg standing balance exercise, 12 min/d) or the intervention group (n = 60, force platform training with functional electric stimulation, 12 min/d). The training was provided 15 days a month for 3 months by physical therapists. Medial–lateral and anterior–posterior maximal range of sway with eyes open and closed, the Berg Balance Scale, the Barthel Index, the Falls Efficacy scale-International were assessed at baseline and after the 3-month intervention. A fall diary was kept by each participant during the 6-month follow-up.
Results
On comparing the two groups, the intervention group showed significantly decreased (p < 0.01) medial–lateral and anterior–posterior maximal range of sway with eyes open and closed. There was significantly higher improvement in the Berg Balance Scale (p < 0.05), the Barthel Index (p < 0.05) and the Falls Efficacy Scale-International (p < 0.05), along with significantly lesser number of injurious fallers (p < 0.05), number of fallers (p < 0.05), and fall rates (p < 0.05) during the 6-month follow-up in the intervention group.
Conclusion
This study showed that the visual feedback-based force platform training with functional electric stimulation improved balance and prevented falls in older adults.
Keywords: Biofeedback, Elderly people, Rehabilitation, Quality of life
Introduction
A fall is defined as an event that results in a person coming to rest inadvertently on the ground, or floor, or other lower level (Hill et al., 2015). Approximately 30% of community-dwelling adults aged 65 years and older fall at least once a year (Hirase et al., 2015). The consequences of falls may be severe, leading to fractures, institutionalization, loss of functional independence, disability, fear of falling, depression and social isolation (Abreu et al., 2015). Therefore, prevention of falls among older adults is a crucial public health challenge.
Balance deficits are one of the known risk factors for falls in older adults (Schmid, Van Puymbroeck & Koceja, 2010). Previous meta-analyses have shown that multifactorial intervention involving balance training could reduce falls (Cameron et al., 2012; Kannus et al., 2005). Some traditional balance exercises like Tai Chi as a single intervention has also shown reduced risk of falls in community-dwelling older adults (Gillespie et al., 2012). Recently, there is a popular balance training method by instructing participants to stand on a force platform and minimizing the center of pressure (COP) movement (Dos Anjos, Lemos & Imbiriba, 2016). Force platform provides a method to quantify and train the ability of maintaining standing position in different circumstances (Srivastava et al., 2009). Older adults tend to rely on exteroceptive information and prioritize the vision on postural control. Visual feedback balance training can enhance sensorimotor integration by a recalibration of the sensory systems contributing to balance control (Hatzitaki et al., 2009). Force platform balance training combined with visual feedback seems to effect to improve balance control and reduce postural sway in older adults (Lakhani & Mansfield, 2015).
The ability of lower extremity muscle to generate adequate force is a fundamental component of maintaining balance and a decrease in muscle strength with aging has been well documented (Moreland et al., 2004). Functional electrical stimulation can increase muscle strength, induce changes in muscle fiber composition and capillary system structure, prevent muscle atrophy due to the prolonged immobilization, decreases pain, and increase functional fitness (Tok et al., 2011). Functional electrical stimulation has been used to improve balance in adults with stroke and was recently shown some effects on balance in older adults (Mignardot et al., 2015).
However, the effects of the visual-feedback-based force platform balance training with functional electric stimulation on the prevention of falls in older adults were unknown. Therefore, the purpose of this study was to evaluate the effects of the visual-feedback-based force platform balance training with functional electric stimulation on the balance and prevention of falls in older adults.
Methods
Participants
This study was conducted at a department of geriatrics in China. Recruitment started in December 2015 and follow-up was completed in January 2017. Inclusion criteria were (1) age 60 and older, (2) ability to walk with or without an assistive device for a minimum of 20 m, (3) ability to see visual feedback from a computer screen, and (4) ability to follow instructions for testing and training (Mini-Mental State Examination, MMSE, >23 points). Subjects were excluded for any of following reasons: (1) neurological disorders, (2) severe psychiatric disorders (Hamilton Depression Scale, HAMD, >21 point, Hamilton Anxiety Scale, HAMA, >20 point), (3) severe musculoskeletal impairment, (4) terminal cardiovascular problems, and (5) participation in other balance training.
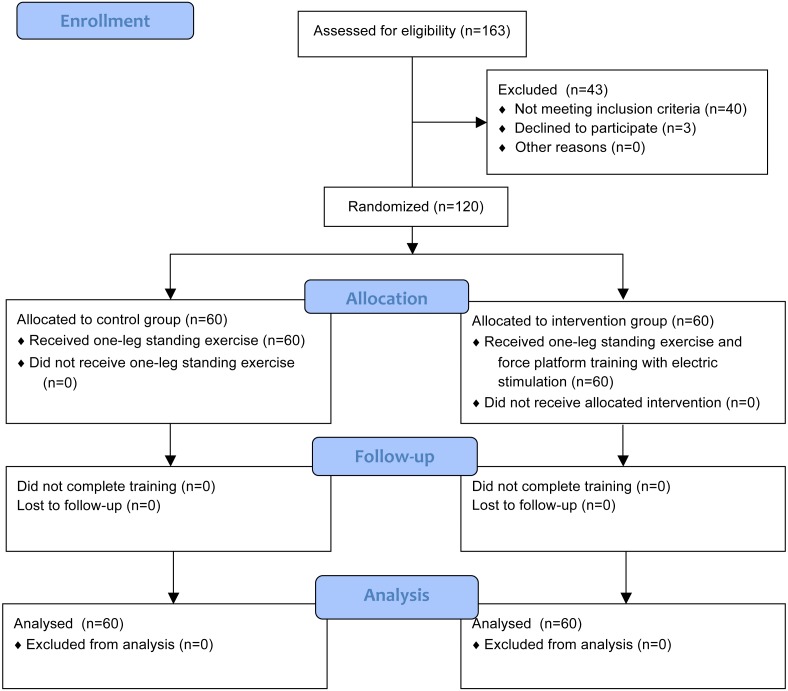
All included participants signed informed consent and they were randomly assigned to the intervention group (IG) or the control group (CG) using computer-generated random numbers. The sequence was concealed until group assignment and baseline measurement was completed. A person unrelated to the study performed the randomization procedure. This study was approved by the Chinese Ethics Committee of Registering Clinical Trials (ChiECRCT-20150041) and was registered at http://www.chictr.org.cn/ (identified: ChiCTR-IOR-16007691). The study design and flow of participants are shown in Fig. 1.
Figure 1. Flow chart for the study.
Intervention
The IG was trained by the computerized force platform with visual feedback (Balance-A, NCC, Shanghai, China) and the functional electrical stimulation with biofeedback (MyoNet-COW, NCC, Shanghai, China).
Participants were instructed to stand barefoot on the force platform in marked foot position (10 cm between heel centers, with an angle of 150 between the long axes of the feet), keeping their arms by their sides. The force platform was connected to a computer and a monitor. The monitor was placed approximately 1 m in front of the participant at eye level. Participants could receive real-time visual feedback of their center of pressure (COP) on the monitor. First, the feedback of their anterior–posterior COP was presented as a fluctuating horizontal line that moved upwards as the COP moved forwards and downwards as the COP moved backwards. A horizontal midline indicating the correct anterior–posterior COP and two horizontal lines indicating 5% skewing of the correct COP were placed on the screen. Participants were told that the feedback line represented the anterior-posterior position of their body and were instructed to keep the line as close to the midline as possible and not exceed the upper and lower boundary lines for 3 min. Then, the feedback of their medial–lateral COP was presented as a fluctuating vertical line. A vertical midline indicating the correct medial–lateral COP and two vertical lines indicating 5% skewing of the correct COP were placed on the screen. Participants were asked to keep the line as close to the midline as possible and to stay in the two vertical boundary lines for 3 min.
After the force platform training, participants were instructed to performed the functional electrical stimulation training in sitting position, with the ankle, knee, and hip joints at 90°. First, Self-adhesive 5 × 5 cm electrodes were placed on each leg with the anode with membrane-depolarizing properties positioned over the proximal part of the tibialis anterior muscle about 5 cm below the head of fibula. The cathode was placed on the distal part of the tibialis anterior muscle about 5 cm above the lateral external malleolus of fibula. The starting stimulation intensity was adjusted to elicit maximal contraction without inducing discomfort. Participants were asked to do the ankle dorsiflexion and received electrical stimulation by the device for 3 min (10 s on and 10 s off, rectangular-wave pulsed currents, 50 Hz). Then, the anode was placed along the middorsal line of shank, over both medial and lateral gastrocnemii. The cathode was attached to the superficial aspect of soleus muscle (5 cm in distance from where the two heads of gastrocnemii join the Achilles tendon). Participants were received electrical stimulation when they did the ankle plantarflexion in 3 min.
In addition, both the IG and the CG performed the one-leg standing balance exercise for 12 min per day. The detailed description of one-leg standing balance exercise can be found in a previous article (Sakamoto et al., 2006). Participants were not allowed to use a walker or cane during the training. The force platform training with functional electric stimulation and the one-leg standing exercise were provided 15 days a month for 3 months by two different specified physical therapists.
Outcome measures
Primary outcome: Fall rates during 6 months follow-up. Participants using daily fall diaries recorded the number of falls from the day training started until the follow-up ended. The research staff contacted each participant monthly to maximize compliance with the fall diaries. The fall rates are the total number of falls per person in 6 months.
Secondary outcomes: The number of injurious fallers and the number of fallers in 6 months follow-up. Falls were classified as injurious if they resulted in a physical injury including bruising, laceration, dislocation, fracture, loss of consciousness, or if the patient reported persistent pain (Haines et al., 2011).
COP-based balance parameters were measured using the force platform. Participants were asked to stand still on the force platform for 30 s with their eyes open, then they were asked to close their eyes for 30 s. The following parameters were calculated: maximum range of sway in the medial–lateral and anterior–posterior directions. The maximum range of sway was calculated from the distance between the maximum and minimum COP displacement for each direction. The reliability and validity of COP-based parameters have been tested among older adults (Li et al., 2016b).
The Berg Balance Scale (BBS) was used as a functional balance measure. It consists of 14 items that are scored on a scale of 0–4 and is reliable and valid in elderly people. The maximum score is 56, and people with scores below 45 show a risk of falling (Nick et al., 2016). The Falls Efficacy Scale-International (FES-I) was a widely accepted tool for accessing the fear of falling. It consists of 16 items that are scored on a scale of 0–4 and the higher scores indicate high concern about falling (Delbaere et al., 2010). The ability to perform activities of daily living was assessed using the Barthel Index (BI), which is a valid and reliable tool. The maximum score is 100 and the higher scores represent greater independence (Ali et al., 2015). The COP-based parameters, BBS, FES-I, and BI were tested by a therapist initially and after 3 months of balance training. The therapist was blinded to the information about the groups to which the participants belonged.
The sample size estimate was based on extrapolations from our pilot studies and other related promising pilot work (Li et al., 2016c; Mirelman et al., 2013). Power calculations indicated that a sample size of 120 (60 in each group) would have 80% power to detect a between-group difference of 20% in the fall rates after intervention with a significance level of 0.05 and a dropout rate of 10%.
Data analysis
Independent-sample t-tests and Chi-square tests were used for baseline comparisons between the IG and CG. Chi-square tests were used to compare sex distributions and fallers in the year before the intervention between the two groups. The group differences in outcome measures were analyzed by two-factor analysis of variance. The between-subject factor was the treatment and the within-subject factor was time. Post hoc Bonferroni tests were performed to compare post-training and baseline measures in each group of patients. Fall rates and the proportion of patients who had falls and injurious falls were compared by Chi-square tests during the 6-month follow-up. Data was analyzed using SPSS (version 21, IBM, New York, USA) and considered significant at p < 0.05.
Results
A flowchart outlining study participation is shown in Fig. 1. A total of 143 inpatients were assessed for eligibility and 120 underwent randomization (60 in each group). No patients dropped out and no training-related adverse events occurred.
The baseline characteristics of the participants are summarized in Table 1. There were no significant differences between the two groups in terms of age, sex, BMI, blood pressure, number of medications, fallers in the previous year, MMSE, HAMD, and HAMA (p > 0.05).
Table 1. Baseline characteristics of the participants.
| Characteristic | Intervention group (n = 60) | Control group (n = 60) | P value |
|---|---|---|---|
| Age, mean (SD), years | 69.5 (6.0) | 70.6 (5.5) | 0.292 |
| Females, n | 29 | 27 | 0.714 |
| BMI, mean (SD), kg/m2 | 24.01 (3.4) | 24.55 (2.7) | 0.335 |
| Systolic BP, mean (SD), mmHg | 146 (13.4) | 148 (13.6) | 0.239 |
| Diastolic BP, mean (SD), mmHg | 83 (10.1) | 81 (8.5) | 0.601 |
| Number of medications, mean (SD) | 5.3 (2.3) | 5.5 (1.9) | 0.696 |
| Fallers in previous 12 months, n | 24 | 21 | 0.572 |
| MMSE, mean (SD), score | 26.9 (1.6) | 27.3 (1.7) | 0.342 |
| HAMA, mean (SD), score | 10.4 (3.1) | 11.1 (4.1) | 0.309 |
| HAMD, mean (SD), score | 13.6 (4.1) | 12.8 (3.8) | 0.275 |
Notes.
- SD
- standard deviation
- BMI
- body mass index
- BP
- blood pressure
- MMSE
- Mini-Mental State Examination
- HAMD
- Hamilton Depression Scale
- HAMA
- Hamilton Anxiety Scale
The results of baseline and post-training balance assessment are given in Table 2. No significant difference was found between the two groups at baseline of BI, BBS, FES-I, and COP-based parameters (p > 0.05).
Table 2. Effects of force platform balance training with visual feedback on balance.
| Parameters | Intervention group (n = 60) | Control group (n = 60) | |||||
|---|---|---|---|---|---|---|---|
| Baseline | Post-training | pa | Baseline | Post-training | pa | pb | |
| BI | 93.1 (2.6) | 96.3 (3.2) | <0.001 | 93.9 (2.1) | 95.1 (2.7) | 0.005 | 0.026 |
| BBS | 44.5 (5.1) | 50.1 (3.1) | <0.001 | 45.2 (4.7) | 48.7 (3.7) | <0.001 | 0.027 |
| FES-I | 31.4 (8.2) | 22.9 (7.5) | <0.001 | 32.1 (8.6) | 26.4 (8.1) | <0.001 | 0.015 |
| Eyes open | |||||||
| MML, cm | 3.81 (1.05) | 2.14 (0.34) | <0.001 | 3.57 (0.56) | 2.74 (0.38) | <0.001 | 0.001 |
| MAP, cm | 2.63 (0.52) | 1.25 (0.65) | <0.001 | 2.45 (0.75) | 1.85 (0.15) | <0.001 | <0.001 |
| Eyes closed | |||||||
| MML, cm | 1.86 (0.79) | 0.83 (0.25) | <0.001 | 1.56 (0.94) | 1.03 (0.47) | <0.001 | 0.004 |
| MAP, cm | 2.49 (0.87) | 1.86 (0.44) | <0.001 | 2.54 (0.61) | 2.16 (0.73) | 0.002 | 0.007 |
Notes.
Data are mean (SD).
p values for within group comparisons (p < 0.05).
p values for treatment × time interaction (p < 0.05).
- BI
- Barthel Index
- BBS
- Berg Balance Scale
- FES-I
- Falls Efficacy Scale-International
- MML
- medial–lateral maximal range of sway
- MAP
- anterior–posterior maximal range of sway
The BI score and BBS score were both increased in the IG (from 93.1 ± 2.6 to 96.3 ± 3.2, from 44.5 ± 5.1 to 50.1 ± 3.1) and CG (from 93.9 ± 2.1 to 95.1 ± 2.7, from 45.2 ± 4.7 to 48.7 ± 3.7) after training and the BBS scores in both groups were increased more than 45. There were significant differences between two groups (p < 0.05). The FES-I score in the IG (from 31.4 ± 8.2 to 22.9 ± 7.5) and in the CG (from 32.1 ± 8.6 to 26.8 ± 8.1) also reduced and there were significant differences between two groups (p < 0.05). The FES-I score in the IG < 23 indicated low concern about falling.
The maximal range of sway in the medial–lateral and anterior–posterior directions were reduced in both the groups with eyes open and eyes closed conditions at the end of the 3 months training. The medial–lateral maximal range of sway reduced from 3.81 ± 1.05 to 2.14 ± 0.34 and the anterior–posterior maximal range of sway reduced from 2.63 ± 0.52 to 1.25 ± 0.65 in eyes open in the IG. In the CG they were reduced from 3.57 ± 0.56 to 2.74 ± 0.38 and from 2.45 ± 0.75 to 1.85 ± 0.15. The medial–lateral maximal range of sway reduced from 1.86 ± 0.79 to 0.83 ± 0.25 and the anterior–posterior maximal range of sway reduced from 2.49 ± 0.87 to 1.86 ± 0.54 in eyes closed in the IG. In the CG they were reduced from 1.56 ± 0.94 to 1.03 ± 0.47 and from 2.54 ± 0.61 to 2.16 ± 0.73. There was significant difference between two groups (p < 0.01).
Table 3 shows the number of injurious fallers, the number of fallers, and fall rates in 6 months follow-up. It was found that the number of injurious fallers during the 6 months follow-up in the IG (5) was less than the CG (13) and the difference between the two groups was statistically significant (p < 0.05). The number of fallers in the IG (8) was also less than the CG (17) during the 6 months follow-up and there were significant differences between two groups (p < 0.05). The fall rates in IG were 33.3% and in CG were 53.3% during the 6 months follow-up. There were significant differences between two groups (p < 0.05).
Table 3. Effects of force platform balance training with visual feedback on fall.
| IG (n = 60) | CG (n = 60) | P value | |
|---|---|---|---|
| Injurious fallers, n | 5 | 13 | 0.041 |
| Fallers, n | 8 | 17 | 0.043 |
| Fall rates, % | 33.3 | 53.3 | 0.027 |
Notes.
P values are given for difference between groups.
- IG
- intervention group
- CG
- control group
Discussion
The results of this randomized, controlled study showed that the visual-feedback-based force platform training with functional electric stimulation can significantly improve balance and prevent falls in older adults. The results also showed a positive effect of the training on activities of daily living and the reduction of falling fear. To the best of our knowledge, this is the first study using the visual-feedback-based force platform training with functional electric stimulation to test the effects on the balance and prevention of falls in older adults.
The maximal range of sway in the medial–lateral and anterior–posterior directions were reduced significantly in the IG indicated that participants could control their center of pressure more stably and accurately. This meant these participants improved the ability to maintain the standing position in static circumstances and the ability to maintain standing while experiencing internally produced perturbations associated with movements of their extremities (Barclay-Goddard et al., 2004). The learning of balance skills was facilitated by the use of visual feedback. Visual information on how the center of pressure is situated and on how it moves during different tasks serves as a tool to improve the volitional postural control. This result was consistent with the motor learning theory that emphasized the role of feedback in the learning of motor skills (Sihvonen, Sipila & Era, 2004). The results of the BBS showed improvement in the performance of functional balance after training. These indicated that the participants improved their ability of balance when they did some real-life meaningful activities such as transfers and stair climbing after training. These meant that the positive effect of training on balance was founded in both functional balance measures as well as laboratory measures. Some previous studies also used other scales to test the effect of the visual-feedback-based balance training on balance. For example, Schwenk et al. (2014) tested thirty-three older adults using visual feedback technique and founded the Timed-up-and-go improved significantly in the IG.
This study evaluated effect of training not only on balance but also on the ability to perform the activities of daily living. The results of the BI showed that the IG significantly improved the ability to perform activities of daily living after training. This means they can perform everyday actions more safely and independently. Srivastava et al. (2009) also reported that the BI scores were improved in forty-five stroke survivors after four weeks visual-feedback-based force platform training. Meanwhile, the results of the FES-I showed the less concerned about falls in the IG compared with the CG after training. The consequences of fear of falling include falling, restriction or avoidance of daily activities, loss of independence, reduction in social activity, depression and a reduction in quality of life (Kendrick et al., 2014). The reduction in fear of falling improved not only the confidence regarding falls but also the confidence in social activities. This indicated that this training might have positive effect on life quality of older adults.
It should be noted the BBS score for the IG group was raised to a level that have less risk to fall as previously mentioned in the Methods section (Nick et al., 2016). The FES-I score in the IG also reached a level that has low concern about falling after three months training (Delbaere et al., 2010). This study found that the fallers and fall rates were both decreased significantly in the IG during six months follow-up. This indicated the visual-feedback-based force platform training with functional electric stimulation could prevent falls in older adults. Previous studies have tested the effect of visual-feedback-based force platform training as a single intervention for fall prevention in older adults. Although these studies showed that the force platform training could improve balance, they found that the force platform training singly might have not significant effect on prevention of falls. For example, Wolf et al. (2003) found no significant difference between training group and education group in the rate of falls after 15 weeks training and 4-month follow-up in community-dwelling older adults. Sihvonen et al. (2004) found no significant difference in number of fallers between two groups after 4 weeks training and 1-year follow-up in 27 older women living in residential care. They only found the recurrent falls were significantly decreased in the IG compared to the CG. This maybe because visual-feedback-based force platform training emphasizes more on the improvement of the organization of sensory information related to postural control and has no significant effects on ankle muscles function (Hagedorn & Holm, 2010). But humans need to generate appropriate torques at the ankle joint to control body sway while standing upright and the decrease in the maximal strength of ankle muscles are considered a main cause of postural instability (Cattagni et al., 2014). In this study, the tibialis anterior muscle and triceps surae muscle were trained by the functional electrical stimulation. It has been proved the functional electrical stimulation can increase muscle function of lower limbs in older adults (Maggioni et al., 2010). A meta-analysis included 24 trials showed that electrical stimulation improved the functional motor ability and normality of movement in patients with stroke (Pomeroy et al., 2006). In addition, this study used randomization and set strict exclusion criteria to minimize other risk factors’ affection on falls, for example, HAMD and HAMA showed no significant difference between the two groups at the baseline. Besides, the IG in this study was given a total of 13.5 h training which was more than twice the training duration of previous studies (Sihvonen et al., 2004). So the visual-feedback-based force platform training with functional electric stimulation showed the positive effects on the prevention of falls in older adults in this study. Furthermore, the injurious fallers were also decrease significantly in the IG during six months follow-up. The reasons for reduction of the injurious fallers were not only the decreased fallers number but also the improved ability to restore balance in response to obstacles and sudden perturbations in the walking as the improved muscle function of low limbs (Pomeroy et al., 2006).
There were limitations in the present study. First of all, a randomized controlled trial with a double-blind study design was not possible because of the nature of the intervention. So the study designed some methods to reduce the bias. For instance, the different exercises were conducted by different physical therapists and data were collected by a specified person who was blinded to the grouping condition. Secondly, this study did not use other functional balance measures (such as Timed Up-and-Go) and muscle strength measures. Meanwhile, Virtual Reality (VR) as a novel technology can provide visual, vestibular, and somatosensory feedback (Li et al., 2016a). It can also provide a mimic environment that the participant thinks real and environment factor is an independent risk factor of falls (Collado-Mateo et al., 2017; Fu et al., 2015). So future study should add VR and more measures into the training to get more enhanced effects and evidences. Finally, this study did not recruit some frail older adults because of the strict inclusion and exclusion criteria. So future study needed to evaluate the effect of the training on the frail older adults.
Conclusions
This study showed that the visual-feedback-based force platform training with functional electric stimulation could improve balance and activities of daily living in older adults, thereby preventing falls. The visual-feedback-based force platform training with functional electric stimulation was feasible with good adherence and few adverse events. A future larger study is needed to test the effects of the visual-feedback-based force platform training with functional electric stimulation.
Supplemental Information
Funding Statement
This study was funded by Science and Technology Commission of Shanghai Municipality (No. 13DZ1941606). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Contributor Information
Shu-Yan Chen, Email: chenshuyan@xinhuamed.com.cn.
Jing Sheng, Email: jingsheng60@126.com.
Shao-Jun Ma, Email: dabian2017@sina.com.
Additional Information and Declarations
Competing Interests
The authors declare there are no competing interests.
Author Contributions
Zhen Li wrote the paper, prepared figures and/or tables, reviewed drafts of the paper.
Xiu-Xia Wang analyzed the data, contributed reagents/materials/analysis tools.
Yan-Yi Liang conceived and designed the experiments, reviewed drafts of the paper.
Shao-Jun Ma and Shu-Yan Chen performed the experiments.
Jing Sheng conceived and designed the experiments.
Clinical Trial Ethics
The following information was supplied relating to ethical approvals (i.e., approving body and any reference numbers):
This study was approved by the Chinese Ethics Committee of Registering Clinical Trials. Approval No. ChiECRCT-20150041.
Data Availability
The following information was supplied regarding data availability:
The raw data has been provided as Supplemental File.
Clinical Trial Registration
The following information was supplied regarding Clinical Trial registration:
ChiCTR-IOR-16007691.
References
- Abreu et al. (2015).Abreu HC, Reiners AA, Azevedo RC, Silva AM, Abreu D, Oliveira A. Incidence and predicting factors of falls of older inpatients. Revista De Saude Publica. 2015;49 doi: 10.1590/S0034-8910.2015049005549. Article 37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ali et al. (2015).Ali TF, Warkentin LM, Gazala S, Wagg AS, Padwal RS, Khadaroo RG, Acute Care and Emergency Surgery (ACES) Group Self-reported outcomes in individuals aged 65 and older admitted for treatment to an acute care surgical service: a 6-month prospective cohort study. Journal of the American Geriatrics Society. 2015;63(11):2388–2394. doi: 10.1111/jgs.13783. [DOI] [PubMed] [Google Scholar]
- Barclay-Goddard et al. (2004).Barclay-Goddard R, Stevenson T, Poluha W, Moffatt ME, Taback SP. Force platform feedback for standing balance training after stroke. Cochrane Database of Systematic Reviews. 2004;4 doi: 10.1002/14651858.CD004129.pub2. Article CD004129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cameron et al. (2012).Cameron ID, Gillespie LD, Robertson MC, Murray GR, Hill KD, Cumming RG, Kerse N. Interventions for preventing falls in older people in care facilities and hospitals. Cochrane Database of Systematic Reviews. 2012;12 doi: 10.1002/14651858.CD005465.pub3. Article CD005465. [DOI] [PubMed] [Google Scholar]
- Cattagni et al. (2014).Cattagni T, Scaglioni G, Laroche D, Van Hoecke J, Gremeaux V, Martin A. Ankle muscle strength discriminates fallers from non-fallers. Frontiers in Aging Neuroscience. 2014;6 doi: 10.3389/fnagi.2014.00336. Article 336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collado-Mateo et al. (2017).Collado-Mateo D, Dominguez-Muñoz FJ, Adsuar JC, Merellano-Navarro E, Gusi N. Exergames for women with fibromyalgia: a randomised controlled trial to evaluate the effects on mobility skills, balance and fear of falling. PeerJ. 2017;5:e3211. doi: 10.7717/peerj.3211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delbaere et al. (2010).Delbaere K, Close JC, Mikolaizak AS, Sachdev PS, Brodaty H, Lord SR. The Falls Efficacy Scale International (FES-I). A comprehensive longitudinal validation study. Age and Ageing. 2010;39(2):210–216. doi: 10.1093/ageing/afp225. [DOI] [PubMed] [Google Scholar]
- Dos Anjos, Lemos & Imbiriba (2016).Dos Anjos F, Lemos T, Imbiriba LA. Does the type of visual feedback information change the control of standing balance? European Journal of Applied Physiology and Occupational Physiology. 2016;116:1771–1779. doi: 10.1007/s00421-016-3434-7. [DOI] [PubMed] [Google Scholar]
- Fu et al. (2015).Fu AS, Gao KL, Tung AK, Tsang WW, Kwan MM. Effectiveness of exergaming training in reducing risk and incidence of falls in frail older adults with a history of falls. Archives of Physical Medicine and Rehabilitation. 2015;96(12):2096–2102. doi: 10.1016/j.apmr.2015.08.427. [DOI] [PubMed] [Google Scholar]
- Gillespie et al. (2012).Gillespie LD, Robertson MC, Gillespie WJ, Sherrington C, Gates S, Clemson LM, Lamb SE. Interventions for preventing falls in older people living in the community. Cochrane Database of Systematic Reviews. 2012;9 doi: 10.1002/14651858.CD007146.pub2. Article CD007146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagedorn & Holm (2010).Hagedorn DK, Holm E. Effects of traditional physical training and visual computer feedback training in frail elderly patients. A randomized intervention study. European Journal of Physical and Rehabilitation Medicine. 2010;46:159–168. [PubMed] [Google Scholar]
- Haines et al. (2011).Haines TP, Hill AM, Hill KD, McPhail S, Oliver D, Brauer S, Hoffmann T, Beer C. Patient education to prevent falls among older hospital inpatients: a randomized controlled trial. Archives of Internal Medicine. 2011;171(6):516–524. doi: 10.1001/archinternmed.2010.444. [DOI] [PubMed] [Google Scholar]
- Hatzitaki et al. (2009).Hatzitaki V, Amiridis IG, Nikodelis T, Spiliopoulou S. Direction-induced effects of visually guided weight-shifting training on standing balance in the elderly. Gerontology. 2009;55:145–152. doi: 10.1159/000142386. [DOI] [PubMed] [Google Scholar]
- Hill et al. (2015).Hill AM, McPhail SM, Waldron N, Etherton-Beer C, Ingram K, Flicker L, Bulsara M, Haines TP. Fall rates in hospital rehabilitation units after individualised patient and staff education programmes: a pragmatic, stepped-wedge, cluster-randomised controlled trial. Lancet. 2015;385(9987):2592–2599. doi: 10.1016/S0140-6736(14)61945-0. [DOI] [PubMed] [Google Scholar]
- Hirase et al. (2015).Hirase T, Inokuchi S, Matsusaka N, Okita M. Effects of a balance training program using a foam rubber pad in community-based older adults: a randomized controlled trial. Journal of Geriatric Physical Therapy. 2015;38(2):62–70. doi: 10.1519/JPT.0000000000000023. [DOI] [PubMed] [Google Scholar]
- Kannus et al. (2005).Kannus P, Sievanen H, Palvanen M, Järvinen T, Parkkari J. Prevention of falls and consequent injuries in elderly people. Lancet. 2005;366(9500):1885–1893. doi: 10.1016/S0140-6736(05)67604-0. [DOI] [PubMed] [Google Scholar]
- Kendrick et al. (2014).Kendrick D, Kumar A, Carpenter H, Zijlstra GA, Skelton DA, Cook JR, Stevens Z, Belcher CM, Haworth D, Gawler SJ, Gage H, Masud T, Bowling A, Pearl M, Morris RW, Iliffe S, Delbaere K. Exercise for reducing fear of falling in older people living in the community. Cochrane Database of Systematic Reviews. 2014;11 doi: 10.1002/14651858.CD009848.pub2. Article CD009848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lakhani & Mansfield (2015).Lakhani B, Mansfield A. Visual feedback of the centre of gravity to optimize standing balance. Gait and Posture. 2015;41:499–503. doi: 10.1016/j.gaitpost.2014.12.003. [DOI] [PubMed] [Google Scholar]
- Li et al. (2016a).Li Z, Han XG, Sheng J, Ma SJ. Virtual reality for improving balance in patients after stroke: a systematic review and meta-analysis. Clinical Rehabilitation. 2016a;30(5):432–440. doi: 10.1177/0269215515593611. [DOI] [PubMed] [Google Scholar]
- Li et al. (2016b).Li Z, Liang YY, Wang L, Sheng J, Ma SJ. Reliability and validity of center of pressure measures for balance assessment in older adults. Journal of Physical Therapy Science. 2016b;28(4):1364–1367. doi: 10.1589/jpts.28.1364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li et al. (2016c).Li Z, Wang HM, Sheng J, Ma SJ. Effectiveness of force platform balance training with visual feedback in aged Chinese: a pilot study. International Journal of Clinical and Experimental Medicine. 2016c;9(2):4163–4167. [Google Scholar]
- Maggioni et al. (2010).Maggioni MA, Cè E, Rampichini S, Ferrario M, Giordano G, Veicsteinas A, Merati G. Electrical stimulation versus kinesitherapy in improving functional fitness in older women: a randomized controlled trial. Archives of Gerontology and Geriatrics. 2010;50(3):e19–e25. doi: 10.1016/j.archger.2009.04.015. [DOI] [PubMed] [Google Scholar]
- Mignardot et al. (2015).Mignardot JB, Deschamps T, Le Goff CG, Roumier FX, Duclay J, Martin A, Sixt M, Pousson M, Cornu C. Neuromuscular electrical stimulation leads to physiological gains enhancing postural balance in the pre-frail elderly. Physiological Reports. 2015;3(7):e12471. doi: 10.14814/phy2.12471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mirelman et al. (2013).Mirelman A, Rochester L, Reelick M, Nieuwhof F, Pelosin E, Abbruzzese G, Dockx K, Nieuwboer A, Hausdorff JM. V-TIME: a treadmill training program augmented by virtual reality to decrease fall risk in older adults: study design of a randomized controlled trial. BMC Neurology. 2013;13:15. doi: 10.1186/1471-2377-13-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moreland et al. (2004).Moreland JD, Richardson JA, Goldsmith CH, Clase CM. Muscle weakness and falls in older adults: a systematic review and meta-analysis. Journal of the American Geriatrics Society. 2004;52:1121–1129. doi: 10.1111/j.1532-5415.2004.52310.x. [DOI] [PubMed] [Google Scholar]
- Nick et al. (2016).Nick N, Petramfar P, Ghodsbin F, Keshavarzi S, Jahanbin I. The effect of yoga on balance and fear of falling in older adults. PM&R. 2016;8(2):145–151. doi: 10.1016/j.pmrj.2015.06.442. [DOI] [PubMed] [Google Scholar]
- Pomeroy et al. (2006).Pomeroy VM, King L, Pollock A, Baily-Hallam A, Langhorne P. Electrostimulation for promoting recovery of movement or functional ability after stroke. Cochrane Database of Systematic Reviews. 2006;2 doi: 10.1161/01.STR.0000236634.26819.cc. Article CD003241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sakamoto et al. (2006).Sakamoto K, Nakamura T, Hagino H, Endo N, Mori S, Muto Y, Harada A, Nakano T, Itoi E, Yoshimura M, Norimatsu H, Yamamoto H, Ochi T, Committee on Osteoporosis of The Japanese Orthopaedic Association Effects of unipedal standing balance exercise on the prevention of falls and hip fracture among clinically defined high-risk elderly individuals: a randomized controlled trial. Journal of Orthopaedic Science. 2006;11(5):467–472. doi: 10.1007/s00776-006-1057-2. [DOI] [PubMed] [Google Scholar]
- Schmid, Van Puymbroeck & Koceja (2010).Schmid AA, Van Puymbroeck M, Koceja DM. Effect of a 12-week yoga intervention on fear of falling and balance in older adults: a pilot study. Archives of Physical Medicine and Rehabilitation. 2010;91:576–583. doi: 10.1016/j.apmr.2009.12.018. [DOI] [PubMed] [Google Scholar]
- Schwenk et al. (2014).Schwenk M, Grewal GS, Honarvar B, Schwenk S, Mohler J, Khalsa DS, Najafi B. Interactive balance training integrating sensor-based visual feedback of movement performance: a pilot study in older adults. Journal of NeuroEngineering and Rehabilitation. 2014;11 doi: 10.1186/1743-0003-11-164. Article 164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sihvonen, Sipila & Era (2004).Sihvonen SE, Sipila S, Era PA. Changes in postural balance in frail elderly women during a 4-week visual feedback training: a randomized controlled trial. Gerontology. 2004;50:87–95. doi: 10.1159/000075559. [DOI] [PubMed] [Google Scholar]
- Sihvonen et al. (2004).Sihvonen S, Sipila S, Taskinen S, Era P. Fall incidence in frail older women after individualized visual feedback-based balance training. Gerontology. 2004;50(6):411–416. doi: 10.1159/000080180. [DOI] [PubMed] [Google Scholar]
- Srivastava et al. (2009).Srivastava A, Taly AB, Gupta A, Kumar S, Murali T. Post-stroke balance training: role of force platform with visual feedback technique. Journal of the Neurological Sciences. 2009;287(1–2):89–93. doi: 10.1016/j.jns.2009.08.051. [DOI] [PubMed] [Google Scholar]
- Tok et al. (2011).Tok F, Aydemir K, Peker F, Safaz I, Taşkaynatan MA, Ozgül A. The effects of electrical stimulation combined with continuous passive motion versus isometric exercise on symptoms, functional capacity, quality of life and balance in knee osteoarthritis: randomized clinical trial. Rheumatology International. 2011;31(2):177–181. doi: 10.1007/s00296-009-1263-2. [DOI] [PubMed] [Google Scholar]
- Wolf et al. (2003).Wolf SL, Barnhart HX, Kutner NG, McNeely E, Coogler C, Xu T, Atlanta FICSIT Group Selected as the best paper in the 1990s: reducing frailty and falls in older persons: an investigation of tai chi and computerized balance training. Journal of the American Geriatrics Society. 2003;51(12):1794–1803. doi: 10.1046/j.1532-5415.2003.51566.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The following information was supplied regarding data availability:
The raw data has been provided as Supplemental File.