Abstract
Introduction
The clinical benefit of continued supervised maintenance exercise programs following pulmonary rehabilitation in COPD remains unclear. This systematic review aimed to synthesize the available evidence on the efficacy of supervised maintenance exercise programs compared to usual care following pulmonary rehabilitation completion on health care use and mortality.
Methods
Electronic databases (MEDLINE, Embase, CINAHL, Cochrane Central Register of Controlled Trials, Web of Science, and PEDro) and trial registers (ClinicalTrials.gov and Current Controlled Trials) were searched for randomized trials comparing supervised maintenance exercise programs with usual care following pulmonary rehabilitation completion. Primary outcomes were respiratory-cause hospital admissions, exacerbations requiring treatment with antibiotics and/or systemic corticosteroids, and mortality.
Results
Eight trials (790 COPD patients) met the inclusion criteria, six providing data for meta-analysis. Continued supervised maintenance exercise compared to usual care following pulmonary rehabilitation completion significantly reduced the risk of experiencing at least one respiratory-cause hospital admission (risk ratio 0.62, 95% confidence interval [CI] 0.47–0.81, P<0.001). Meta-analyses also suggested that supervised maintenance exercise leads to a clinically important reduction in the rate of respiratory-cause hospital admissions (rate ratio 0.72, 95% CI 0.50–1.05, P=0.09), overall risk of an exacerbation (risk ratio 0.79, 95% CI 0.52–1.19, P=0.25), and mortality (risk ratio 0.57, 95% CI 0.17–1.92, P=0.37).
Conclusion
In the first systematic review of the area, current evidence demonstrates that continued supervised maintenance exercise compared to usual care following pulmonary rehabilitation reduces health care use in COPD. The variance in the quality of the evidence included in this review highlights the need for this evidence to be followed up with further high-quality randomized trials.
Keywords: pulmonary rehabilitation, health outcomes, supervised maintenance programs, hospitalization, exacerbations
Video abstract
Introduction
Pulmonary rehabilitation is defined as “a comprehensive intervention based on a thorough patient assessment followed by patient-tailored therapies that include, but are not limited to, exercise training, education, and behavior change, designed to improve the physical and psychological condition of people with chronic respiratory disease and to promote the long-term adherence to health-enhancing behaviors.”1 Pulmonary rehabilitation has well-established benefits in improving exercise capacity, health-related quality life, and psychological well-being in chronic lung conditions such as COPD.1,2 The strength of the evidence for these benefits in COPD has led to calls for an end to randomized controlled trials comparing pulmonary rehabilitation with usual care.3 However, the benefits of pulmonary rehabilitation have been shown to be short term2 with the condition of most patients returning to baseline at 12 months.4 Consequently, there is interest in exercise programs that may maintain the initial benefits of pulmonary rehabilitation.5,6
Supervised maintenance exercise programs after pulmonary rehabilitation in COPD appear to be more effective in preserving the improvements in exercise capacity up to 6 months but show no effects with respect to health-related quality of life postrehabilitation.5,7 Exacerbations and hospital admissions are the key events in the management of COPD, but the effects of exercise, particularly supervised maintenance programs following pulmonary rehabilitation, on these outcomes have received little attention. A recent systematic review has highlighted the role of pulmonary rehabilitation in reducing hospitalizations due to COPD exacerbations.8 This supported a previous systematic review that showed a reduction in the risk of hospital readmission when completing pulmonary rehabilitation following exacerbation,9 albeit the quality of this evidence has recently been downgraded due to inconsistencies in the estimates of effect.10 There is increasing interest in assessing these outcomes in response to exercise interventions following pulmonary rehabilitation to identify if the duration of benefits from a pulmonary rehabilitation program alone can be prolonged or rather enhanced during the postrehabilitation period.8 A previous systematic review of supervised maintenance exercise programs following pulmonary rehabilitation in COPD had included studies that reported health care use; however, data were not statistically combined to quantify effect size.5 Despite the availability of new evidence in the area since this review, there remains no systematic review that has synthesized the evidence of the effects of supervised maintenance exercise training programs compared to usual care following pulmonary rehabilitation on outcomes related to health care use. Therefore, the aim of this systematic review was to collate and synthesize all of the available evidence from randomized controlled trials in order to estimate the size of the effect of supervised maintenance exercise programs following pulmonary rehabilitation on health care use.
Methods
The protocol for this study (CRD42016035509) was registered in advance on PROSPERO (International Prospective Register of Systematic Reviews; www.crd.york.ac.uk/PROSPERO/).
Selection criteria
Participants
Adults with a confirmed diagnosis of COPD (in line with national or international criteria, eg, British Thoracic Society, American Thoracic Society/European Respiratory Society, and Global Initiative for Chronic Obstructive Lung Disease) who had completed a pulmonary rehabilitation program.11–13
Intervention
Studies were included if patients were randomized to a supervised maintenance exercise training program following pulmonary rehabilitation.
Comparison
The comparator was any concurrent control group who had completed pulmonary rehabilitation and returned to “usual care.”
Outcomes
Primary outcomes were hospital admissions (respiratory cause), exacerbations requiring treatment with antibiotics and/or systemic corticosteroids, and all-cause mortality.
Secondary outcome measures were hospital admissions (all-cause), outpatient visits, length of hospital stay (respiratory or all-cause), and general practitioner (GP) visits.
Study design
Studies included in this review had to have adhered to the following study designs: parallel-group randomized controlled trials (allocation at individual or cluster level or using quasi-random method) or crossover randomized controlled trials (data up to point of crossover only).
Search strategy
Searches were conducted to identify any relevant completed or ongoing systematic reviews using the following sources: Cochrane Database of Systematic Reviews, Database of Abstracts of Reviews of Effects, and PROSPERO. Published trials were identified through searches on the following bibliographic databases: MEDLINE, Embase, CINAHL, Cochrane Central Register of Controlled Trials, Web of Science, and PEDro. Searches of ongoing trial registers, such as ClinicalTrials.gov and Current Controlled Trials, were also undertaken. Gray literature was also searched via EThOS (British Library) and Conference Proceedings Index (Web of Science Core Collection). Searches were conducted from database inception to August 2017. No limits were set on language or publication status. Search terms were structured around the population (eg, “Lung Diseases, Obstructive”, “COPD”), intervention (eg, “Exercise Therapy”, “exercis* N3 supervi* OR training OR maintenance OR program*”), and study type (eg, “randomised”, “randomized”, “controlled”). An example of a full search strategy for CINAHL is presented in Table S1. Database searching was supplemented by contact with study authors and research groups, forward and backward citation tracking from included studies or previous relevant reviews, with further Internet searching via Google Scholar until August 2017.
Search results were collated using EndNote (Clarivate Analytics, Philadelphia, PA, USA). Duplicate citations were removed prior to independent screening of title and abstracts according to inclusion criteria by two reviewers. Full-text articles were obtained for all studies that were unable to be excluded based on title and abstract, before further independent screening to decide on final eligibility. Discrepancies in study eligibility were resolved through discussion between reviewers.
Data extraction and quality appraisal
Data extraction took place using a modified Cochrane Data Extraction Template including elements adapted from a taxonomy form previously used in randomized controlled trials.14 Data were extracted by one reviewer and checked for accuracy by a second reviewer. List of characteristics extracted from studies is available in the Supplementary materials.
Two reviewers independently assessed the risk of bias for included studies using the Cochrane Risk of Bias Tool with the following domains: random sequence generation, allocation concealment, blinding of outcome assessment, incomplete outcome data, selective outcome reporting, and other bias.15 Each domain was classified as low, unclear, or high with the risk of bias for each study classified using the following criteria: 1) low risk of bias (all criteria were deemed low), 2) medium risk of bias (one criterion graded as high or two criteria graded as unclear), and 3) high risk of bias (more than one criterion was deemed high or more than two criteria graded unclear). Disagreements between reviewers were resolved through further discussion.
Data analysis
All analyses were performed using Review Manager Version 5.3. The primary measures of effect were treated as dichotomous data (defined as the total number of participants in each group who had been hospitalized for respiratory cause, treated for an exacerbation, or died [all-cause]) and interpreted as risk ratios. Rate ratio of hospital admissions (respiratory-cause) and exacerbations was also calculated using the incidence rate in the intervention groups divided by the incidence rate in the control groups. Secondary outcomes of hospital admissions (all-cause), GP visits (all-cause), and outpatient visits were treated as dichotomous outcomes only and were interpreted as risk ratios. Length of hospital admissions (respiratory and all-cause) were analyzed as a continuous outcome and expressed as the between-groups difference in means. All primary and secondary outcomes were analyzed using raw data provided by authors rather than mean values presented in publications. If studies reported the same outcome measures, data were combined statistically using a random-effects meta-analysis. We contacted study authors to obtain missing numerical outcome data, and in cases where studies only reported certain outcomes of health care use, we verified that no additional data were available. The generic inverse-variance random-effects model for rates of hospitalization (respiratory) and exacerbation included the (natural) logarithms of the rate ratios and the standard error of the rate ratio.15 Statistical heterogeneity was assessed by the I2 value. Data were not pooled if heterogeneity was found to be moderate (I2>30%). If heterogeneity was identified, potential sources were explored. Prespecified subgroup analyses included the setting, frequency, and delivery (training level of supervisor, combined with education) of supervised maintenance exercise programs. To test the robustness of findings in primary outcome measures, planned prespecified sensitivity analyses involved the removal of studies categorized as medium or high risk of bias within the Cochrane Risk of Bias Tool.
Results
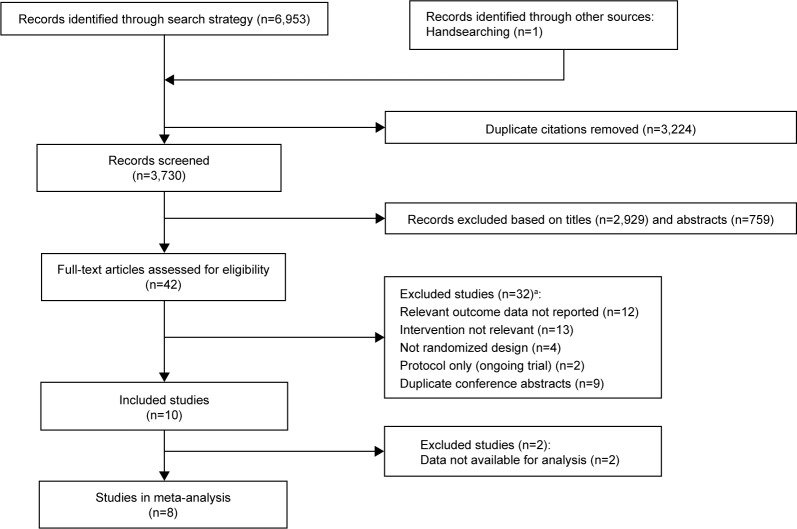
After the removal of duplicates, searches identified 3,730 records to be screened, of which 3,688 records were excluded based on title and abstract (Figure 1). Full texts were obtained for the remaining 42 records. Information on excluded texts and reasons for these can be found in Table S2. Ten records (eight studies) met the inclusion criteria (Table 1), of which six studies had data available for meta-analysis. Two studies were excluded from the meta-analysis due to data not being available in the appropriate format16 and outcome definitions (eg, exacerbation) not meeting review eligibility criteria.17
Figure 1.
Flow diagram of study selection.
Note: aSome studies excluded for multiple reasons.
Table 1.
Characteristics of included studies
| Study (country) | Sample size, gender, age | FEV1% predicted (spirometry), smoking history | Inclusion/exclusion criteria | Study aim, design, unit of allocation | Pulmonary rehabilitation program (setting, components, duration, frequency) | Maintenance program (setting, components, duration, frequency) | Primary outcome (1) and other outcomes and follow-up (2) |
|---|---|---|---|---|---|---|---|
| Ries et al (2003)16 (USA) | 164 participants Int: n=83 Con: n=81 Males: n=89 Females: n=75 Age, mean ± SD All: 67±8 |
FEV1%pred, mean All: 45% No data available for smoking status |
Inclusion: clinical diagnosis of chronic lung disease; chronic symptoms and perceived disability from disease; stable state; no other significant medical or psychiatric conditions that would interfere with program participation; commitment to abstain from smoking | Assess a telephone-based maintenance intervention for retaining benefits following pulmonary rehabilitation RCT, cluster | Exercise and education combined with psychosocial support Twelve 2 h sessions over 8 weeks | Weekly semistructured phone calls and monthly supervised reinforcement sessions (1.5 h supervised exercise, 1.0 h topic review, 0.5 h social time) for 12 months | (1) Pulmonary function, exercise tolerance, dyspnea, depression (2) QoL, health status, health care use |
| Brooks et al (2002)17 (Canada) | 85 participants Int: n=37 Con: n=48 Males: n=50 Females: n=35 Age, mean ± SD Int: 68±1 Con: 68±1 |
FEV1%pred, mean ± SD Int: 32±2% Con: 32±2% All nonsmokers for at least 6 months |
Inclusion: severe stable COPD (FEV1<40% predicted, FEV1/FVC <0.70); completion of inpatient or outpatient rehabilitation; nonsmoker for a minimum of 6 months; aged 49–85 years Exclusion: coexisting conditions that might limit exercise tolerance or cognitive functioning; noncompliance with respiratory rehabilitation; mechanical ventilatory support for any part of the day; inability to communicate in English; living too far away to participate | Compare the effects of two postrehabilitation programs on functional exercise capacity and health-related QoL in patients with COPD RCT, individual | Exercises – breathing, treadmill or cycle exercises, interval and upper extremity training, leisure walking Patient education and psychosocial support included (relaxation and occupational therapies) Inpatient – five times a week for 6 weeks Outpatient – three times a week at the center and at home for 8 weeks | Monthly 2 h group sessions supervised by a physical therapist for 12 months. First hour for discussion around home exercise program, second hour for performing components of the home exercise program under supervision. Phone calls made between visits with standardized questions regarding adherence to home exercises | (1) 6MWT, CRQ (2) Medical outcomes survey: short-form 36, SGRQ, subject compliance, pulmonary function |
| Spencer et al (2010)18 (Australia) | 48 participants Int: n=24 Con: n=24 Males: n=22 Females: n=26 Age, mean ± SD Int: 65±8 Con: 67±7 |
FEV1%pred, mean ± SD Int: 57±21% Con: 60±16% Current smokers Int: n=6 Con: n=5 |
Inclusion: COPD diagnosis; completed an 8 week pulmonary rehabilitation program; FEV1/FVC <70% and FEV1<80% predicted Exclusion: exacerbation in previous month; supplemental oxygen; comorbidities that would prevent performing exercises; clinic patients (pulmonary rehabilitation) | Determine if weekly supervised exercise following pulmonary rehabilitation would maintain functional exercise capacity and QoL RCT, individual | Exercises – 20 min walking, 20 min cycling, 10 min arm cycling, upper and lower limb strength training 8 weeks in a pulmonary rehabilitation gym | Pulmonary rehabilitation gym for 12 months. Supervised exercise 1 day/week with unsupervised exercise 4 days/week. Exercises prescribed in line with exercise undertaken during pulmonary rehabilitation | (1) 6MWT, SGRQ (2) Lung function tests, ISWT, ESWT, HADS, hospital admissions, length of stay and exacerbations |
| Ringbaek et al (2010)19 (Denmark) | 96 participants Int: n=55 Con: n=41 Males: n=31 Females: n=63 Age, mean ± SD Int: 67±1 Con: 69±9 |
FEV1%pred, mean ± SD Int: 36±14% Con: 37±16% Current smokers Int: n=13 Con: n=7 |
Inclusion: stable COPD (FEV1 <80%, FEV1/FVC <70%); motivation for pulmonary rehabilitation; completion of 7 weeks of pulmonary rehabilitation Exclusion: musculoskeletal, cardiac or cognitive problems | Examine whether maintenance training improved long-term effect of pulmonary rehabilitation RCT, individual | Supervised walking and cycling both at 85% of predicted VO2 peak and unsupervised exercise at home Twice a week for 7 weeks with supplementary education once a week | Weekly supervised exercise for the first 6 months, every second week for the next 6 months, and no supervised exercise for the last 6 months. Unsupervised exercise at home encouraged | (1) ESWT, SGRQ (2) Hospitalization (time to first admission, admission rates, days in hospital), exercise adherence, attendance at evaluation visits |
| Wilson et al (2015)20 and Burns et al (2016)21 (UK) | 148 participants Int: n=73 Con: n=75 Males: n=91 Females: n=57 Age, mean ± SD Int: 67±15 Con: 69±9 |
FEV1%pred, mean ± SD All: 41±16% >20 pack-year smoking history No data available on current smoking status | Inclusion: >35 years of age; COPD diagnosis (FEV1<80%); >20 pack-year smoking history; completed at least 60% of pulmonary rehabilitation sessions Exclusion: cardiac or pulmonary disease (other than COPD); myocardial infarction within 6 months or unstable angina; respiratory infection within last 4 weeks; uncontrolled or severe comorbidities; cognitive complications |
Evaluate long-term effect of maintenance exercise on health-related QoL Assess the cost-effectiveness of maintenance exercise following pulmonary rehabilitation on health-related QoL RCT, individual | Exercises – walking, cycling, sit to stand, step-ups, arm exercises with dumbbells. High intensity (85% of maximum capacity) Once a week for 8 weeks (1 h for exercise and 1 h for education). Endurance exercise everyday and strength exercise two more times a week at home | Individually tailored strength and endurance exercises including walking, cycling, sit-to-stand, step-ups, and arm exercises with dumbbells One 2 h (1 h exercise and 1 h education) session every 3 months for 12 months. Same group of patients from original pulmonary rehabilitation. Home exercise program review | (1) CRQ (dyspnea) (2) CRQ (other domains), ESWT, BMI, body fat, HADS, EQ5D |
| Roman et al (2013)22 (Spain) | 71 participants Con: n=23 RHB: n=22 RHBM: n=26 Males: n=58 Females: n=13 Age, mean (95% CI) RHBM: 65 (62–68) RHB: 64 (60–68) Con: 63 (60–66) |
FEV1%pred, mean (95% CI) Con: 60% (56–64) RHB: 60% (55–65) RHBM: 61% (56–66) Current smokers Con: n=8 RHB: n=7 RHBM: n=9 |
Inclusion: 35–74 years old; moderate COPD diagnosis; smokers or nonsmokers Exclusion: musculoskeletal conditions affecting ability to exercise; terminal illness/other severe disease |
Use maintenance postpulmonary rehabilitation to improve QoL in COPD RCT, individual | Exercises – low intensity peripheral muscle training. Abdominal, upper and lower limb exercises, shoulder and full arm circling, weight-lifting, and other exercises. Each exercise repeated 8–10 times over 45 min Three 1 h sessions a week for 12 weeks with 15 min of respiratory physiotherapy every session and 45 min of education during weeks 1, 6+12 | Low intensity peripheral muscle training. One session a week for 9 months | (1) CRQ (2) Pulmonary function, 6MWT, hospital admissions, GP visits, exacerbations |
| Moullec et al (2008)23 and Moullec and Ninot (2010)24 (France) | 40 participants Int: n=14 Con: n=26 Males: n=31 Females: n=9 Age, mean ± SD Int: 63±7 Con: 60±10 |
FEV1%pred, mean ± SD Int: 53±16% Con: 47±19% No data available on smoking status |
Inclusion: FEV1/FVC <0.7, FEV1 30%–79% predicted; no indication for home oxygen therapy; stable state for the previous 2 months; no change in medication and symptoms for the previous 4 weeks; >40 years of age; no previous pulmonary rehabilitation experience Exclusion: medical or psychiatric disturbances that would hinder program participation; diagnosis of asthma; congestive left heart failure; terminal disease | Determine changes in the emotional and functional dimensions of QoL in COPD 1 year after a pulmonary rehabilitation program with or without a follow-up intervention Quasi-RCT, individual | Twenty inpatient sessions over 4 weeks | Community gymnasium Individualized strength, interval, breathing, and endurance training with nature walking at ventilatory threshold 96 sessions across 12 months. Exercise training (3.5 h/week; 72 sessions); health education (2 h/month; 12 sessions); psychosocial support (with discussion group 1 h/month; 12 sessions) | (1) 6MWT, QoL (SGRQ and WHOQoL-Brief) (2) Six-item questionnaire with a VAS, maximal exercise capacity, physical activity, health care utilization, attendance, pulmonary function |
| Guell et al (2017)25 (Spain) | 138 participants Int: n=68 Con: n=70 Males: n=123 Females: n=15 Age, mean ± SD Int: 64±9 Con: 64±8 |
FEV1%pred, mean ± SD Int: 34±11% Con: 34±9% No data available on smoking status |
Inclusion: COPD diagnosis (grade II–IV severity); clinically stable during previous 4 weeks; 18–75 years old; exsmokers or with intention to quit; BODE index value between 3 and 10 Exclusion: bronchodilator response (FEV1 increment >15% of the baseline value after 200 μg of inhaled bronchodilator); other respiratory diagnoses; severe coronary artery disease; orthopedic diseases limiting mobility; life expectancy <2 years; inability to cooperate |
Assess the efficacy of a supervised maintenance program after pulmonary rehabilitation on improving symptoms, exercise capacity, and health-related QoL compared to just pulmonary rehabilitation on its own RCT, individual | Three hospital-based 2 h sessions a week for 8 weeks. Supplemented with four education sessions and chest physiotherapy 30 min weight-lifting (0.5 kg in each hand, increased by 1 kg a week until peak tolerance), 30 min leg cycling (start at 50% maximum load achieved during initial exercise test, load increased by 10 W if heart rate and oxygen saturation are stable and exercise is tolerated) | Supervised exercise on alternate weeks at hospital for 36 months. Unsupervised home exercise program (3 days a week) similar to hospital program (15 min chest physiotherapy, 30 min arm training, 30 min leg training). Supplemented by structured phone calls from physiotherapists every 15 days Exercise similar to pulmonary rehabilitation. Exercises, if well tolerated, were progressed at hospital visits | 1) BODE index (2) 6MWT, health-related QoL, and CRQ |
Abbreviations: BMI, body mass index; BODE, body mass index, airflow obstruction, dyspnea, and exercise index; Con, control group; Int, intervention group; CRQ, chronic respiratory questionnaire; ESWT, endurance shuttle walk test; EQ5D, Euro Quality of Life Five Dimensions questionnaire; FEV1%pred, forced expiratory volume in 1 s % of predicted; FVC, forced vital capacity; GP, general practitioner; HADS, hospital anxiety and depression scale; ISWT, incremental shuttle walk test; 6MWT, 6 min walk test; QoL, quality of life; RCT, randomized controlled trial; RHB, pulmonary rehabilitation with no maintenance; RHBM, pulmonary rehabilitation with maintenance; SD, standard deviation; SGRQ, St George’s Respiratory Questionnaire; VAS, visual analog scale; WHOQoL-Brief, World Health Organization Quality of Life Brief questionnaire.
Characteristics of included studies
The eight included studies were published between 2002 and 2017 (Table 1). The eight studies, in total, randomized 790 COPD patients (64% males), with study sample sizes ranging between 40 and 164. All stages of COPD severity (airflow limitation) were represented across included studies. All studies, except Moullec et al,23,24 randomized patients to either a control group (usual care) or a supervised maintenance exercise program following pulmonary rehabilitation. Moullec et al23,24 used a quasi-random method, whereby patients were consecutively assigned following pulmonary rehabilitation discharge. All supervised maintenance exercise interventions lasted between 9 and 12 months except for Guell et al25 who provided a program for 36 months. Ringbaek et al19 and Ries et al16 had 6- and 12-month observation periods, respectively, following the completion of supervised maintenance exercise, data for which were not relevant for analysis in this review. Intervention procedures varied considerably between studies with one study providing an intense program of 3.5 h of supervised maintenance exercise a week,23,24 whereas another study provided one supervised maintenance session every 3 months.20,21 More details on interventions for all of the studies are given in Table 1.
Primary and secondary outcomes of this review were determined by either self-reporting of events by patients16,17 or self-report validated through examination of health records.18–25 Health care use was reported as a secondary outcome in the majority of studies16–24 with the publication of one study not reporting relevant outcomes.25 Contact with authors of this study provided unpublished data relevant to this review. None of the studies had outcome data for all planned meta-analyses.
The risk of bias assessment was hindered by poor study reporting. Some studies presented with several unclear risks of bias domains, leading to overall high risk of bias. Due to high attrition rates, the risk of bias in four of the included studies in the meta-analyses was classified as high (Table 2). The only study with a low risk of bias was unable to be included in meta-analyses due to the lack of availability of data.16
Table 2.
Risk of bias assessment
| Study | Random sequence generation | Allocation concealment | Blind outcome assessment | Incomplete outcome data | Selective reporting (reporting bias) | Other bias | Overall risk |
|---|---|---|---|---|---|---|---|
| Ries et al (2003)16 | Low | Low | Low | Low | Low | Low | Low |
| Brooks et al (2002)17 | Low | Low | Unclear | High | Low | Low | Medium |
| Spencer et al (2010)18 | Low | Low | High | Low | Low | Low | Medium |
| Ringbaek et al (2010)19 | Unclear | Unclear | Unclear | Low | Low | Low | High |
| Wilson et al (2015)20 and Burns et al (2016)21 | Low | Low | Low | High | Low | Low | Medium |
| Roman et al (2013)22 | Low | Unclear | Unclear | High | Low | Low | High |
| Moullec et al (2008)23 and Moullec and Ninot (2010)24 | High | High | Unclear | High | Low | Low | High |
| Guell et al (2017)25 | Low | Low | Unclear | High | High | Low | High |
Primary outcomes
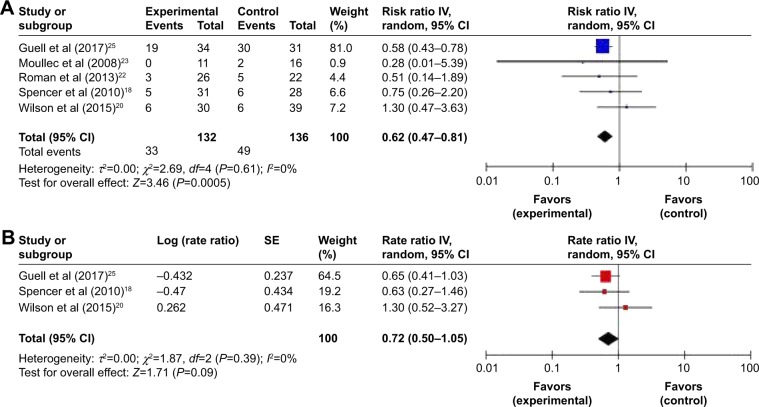
Hospital admissions (respiratory cause)
Meta-analysis of five trials18,20,22–25 demonstrated a statistically significant reduction in the risk of experiencing at least one respiratory-cause hospital admission with continued supervised maintenance exercise following pulmonary rehabilitation (risk ratio 0.62, 95% confidence interval (CI) 0.47–0.81, P<0.001) (Figure 2A). There were no indications of heterogeneity in the findings (I2=0%).
Figure 2.
Trial-level data, effect estimates, and forest plot of comparison for the overall risk (of experiencing at least one event) (A) and incidence rates (B) of respiratory-cause hospitalization.
Abbreviations: CI, confidence interval; IV, inverse variance; SE, standard error.
Three trials provided data on incidence rates,18,20,25 whereby the overall estimate of the average effect suggested a reduction in the rate of respiratory-cause hospital admissions with supervised maintenance exercise (rate ratio 0.72, 95% CI 0.50–1.05, P=0.09, I2=0%) (Figure 2B).
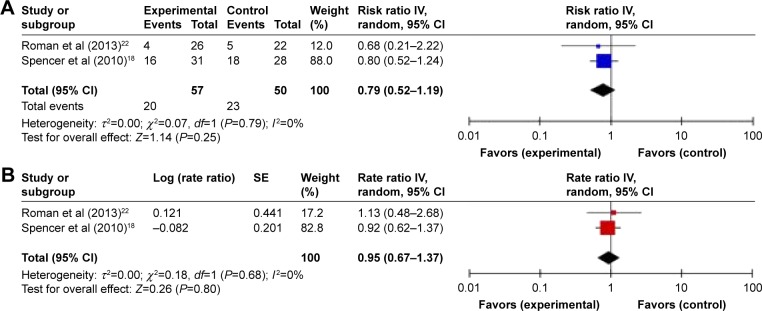
Exacerbations requiring treatment with antibiotics and/or systemic corticosteroids
Meta-analysis of two trials18,22 suggested a reduction in the risk of experiencing at least one exacerbation with supervised maintenance exercise (risk ratio 0.79, 95% CI 0.52–1.19, P=0.25, I2=0%) (Figure 3A). Synthesis of the incidence rates of exacerbations in these studies suggested a minimal effect of supervised maintenance exercise (rate ratio 0.95, 95% CI 0.67–1.37, P=0.80, I2=0%) (Figure 3B).
Figure 3.
Trial-level data, effect estimates, and forest plot of comparison for the overall risk (of experiencing at least one event) (A) and incidence rates (B) of exacerbation requiring treatment with medication.
Abbreviations: CI, confidence interval; IV, inverse variance; SE, standard error.
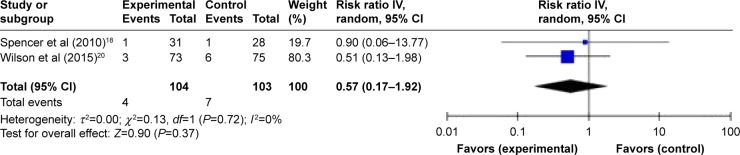
Mortality
Meta-analysis of two trials18,20 suggested a reduction in the risk of all-cause mortality with supervised maintenance exercise, but this was not statistically significant (risk ratio 0.57, 95% CI 0.17–1.92, P=0.37, I2=0%) (Figure 4). The trial by Roman et al22 was omitted from this analysis due to no events occurring in either group during the trial.15
Figure 4.
Trial-level data, effect estimates, and forest plot of comparison for the risk of mortality.
Abbreviations: CI, confidence interval; IV, inverse variance.
Secondary outcomes
Hospital admissions (all-cause)
Meta-analysis of three trials19,20,23 suggested a greater risk of experiencing at least one all-cause hospital admission with supervised maintenance exercise (risk ratio 1.14, 95% CI 0.80–1.62, P=0.48, I2=0%) (Figure S1).
Length of stay (respiratory cause and all-cause)
One trial provided data for length of hospital stay due to respiratory cause18 (mean difference −1.60, 95% CI −4.73 to 1.53, P=0.32), and one trial provided data for length of hospital stay due to all-cause19 (mean difference −0.20, 95% CI −2.31 to 1.91, P=0.85) with both favoring a shorter length of stay with supervised maintenance exercise.
Outpatient visits
Only one trial provided data for outpatient visits.20 The overall estimate of effect suggested a nonsignificant reduction in the risk of experiencing at least one outpatient visit with supervised maintenance exercise (risk ratio 0.78, 95% CI 0.53–1.14, P=0.20).
GP visits
Meta-analysis of three trials18,20,22 suggested a minimal reduction in the number of patients making at least one GP visit with supervised maintenance exercise (risk ratio 0.92, 95% CI 0.75–1.11, P=0.38, I2=0%) (Figure S2).
Sensitivity analyses
As all studies included in the meta-analyses were assessed to have a medium or high risk of bias, we were unable to perform our prespecified sensitivity analyses. However, we deemed that a sensitivity analysis was required on our outcome of the risk of respiratory-cause hospital admissions due to the presence of one study25 that had a substantially longer intervention (and follow-up period) (36 months).
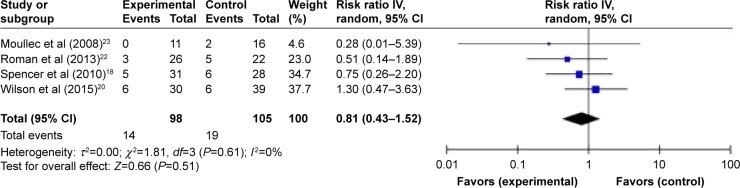
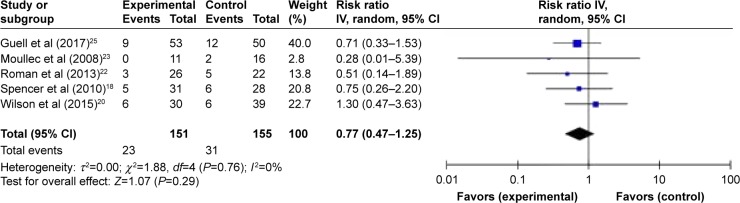
Assessing the number of patients suffering one or more exacerbation between groups (ie, risk ratio) will show the direction of the intervention effect, but it is heavily influenced by the duration of the trial.26 Pooled analyses excluding Guell et al25 led to the loss of statistical significance and reduction in the overall effect of supervised maintenance exercise on the overall risk of experiencing at least one respiratory-cause admission (risk ratio 0.81, 95% CI 0.43–1.52, P=0.51) (Figure 5). Admission data were also retrieved from the study authors for the 1 year follow-up of this study, to allow further scrutiny of the effect of the duration of follow-up. Pooled analyses including the 12-month follow-up of Guell et al25 also led to loss of statistical significance and reduction in the overall effect of supervised maintenance exercise on the overall risk of experiencing at least one respiratory-cause hospital admission (risk ratio 0.77, 95% CI 0.47–1.25, P=0.29) (Figure 6). Due to limited number of completed trials, it was not possible to perform meaningful synthesis of prespecified subgroups on our primary outcomes.
Figure 5.
Sensitivity analyses on trial-level data, effect estimates, and forest plot of comparison for the risk of hospital admission for a respiratory cause excluding Guell et al.25
Abbreviations: CI, confidence interval; IV, inverse variance.
Figure 6.
Sensitivity analyses on trial-level data, effect estimates, and forest plot of comparison for the risk of hospital admission for a respiratory cause including 0–12 months follow-up of Guell et al.25
Abbreviations: CI, confidence interval; IV, inverse variance.
Discussion
To our knowledge, this is the first systematic review to identify eight completed randomized trials that compared the efficacy of supervised maintenance exercise following pulmonary rehabilitation with usual care on health care use in COPD, six of which had relevant data to be synthesized using meta-analysis.
Summary of main findings
Data synthesis of five trials18,20,22–25 suggests that, on average, supervised maintenance exercise following pulmonary rehabilitation significantly reduces the risk of experiencing at least one respiratory-cause hospital admission by 38%. The current available evidence is heavily weighted by one trial,25 whereby the magnitude of the point estimate is sensitive to the inclusion of this trial (due to length of follow-up). Synthesized data from three trials18,20,25 suggest that, on average, supervised maintenance exercise may also have an effect on multiple admissions by reducing the rate of respiratory-cause admissions by 28%. While pooling of studies for other primary measures in this review (relative risk reduction in exacerbations requiring treatment with antibiotics and/or systemic corticosteroids and all-cause mortality of 21% and 43%, respectively) did not translate to statistically significant changes, the point estimates of effect do surpass proposed thresholds of clinical significance.26,27 There is currently no evidence that supervised maintenance exercise following pulmonary rehabilitation has an effect on the risk of all-cause hospital admission or GP visits. Furthermore, there are insufficient data to synthesize the effect of supervised maintenance exercise on outpatient visits or duration of hospital stay following respiratory-cause and all-cause admission.
Strengths and limitations of the review
A strength of this review is that it is the first to conduct comprehensive searches and synthesis of published and unpublished data on health care use during supervised maintenance exercise programs compared to usual care following pulmonary rehabilitation. This review followed a preset, publicly available protocol detailing specific methodology. When the protocol for this review was written however, we did not anticipate the inclusion of trials with substantial differences in study follow-up. The recent study of Guell et al25 has received plaudits for conducting such a long follow-up period of postpulmonary rehabilitation maintenance.28 We feel that this deviation from our protocol in performing sensitivity analysis was strongly justified on the basis that studies with a longer observation period are likely to impact the robustness of our findings.
Extensive efforts were made to contact all trial authors to obtain additional data when outcomes did not appear in the available reports. The retrieval of additional data (beyond the published literature) reflects a key strength of our review. We, however, recognize that two studies16,17 that met review eligibility criteria were not included in our meta-analyses; hence, this must be noted as a limitation. We identified inconsistencies in how our review outcomes were reported. The majority of the studies were limited by expressing hospitalizations/exacerbations as mean number of events per study group only and simply interpreted as a difference in means. However, a small minority of patients who experience multiple events can heavily influence this measure of effect, and the interpretation of such estimates is not as informative as when discrete (count) data are analyzed as ratios. From a statistical point of view, a strength of our review is that our measures of effect make full use of the data that have been collected in the included studies. Clinically, we allow health care practitioners and other relevant stakeholders to be able to interpret the effect of supervised maintenance exercise on the risk of whether a patient experiences an exacerbation and the efficacy of the intervention in reducing multiple events in the same patient.
The proposed minimal clinically important difference in COPD exacerbation frequency is 20%.26,27 As the entire range of the confidence interval for the effect of supervised maintenance exercise on hospitalization rates (ie, severe exacerbation) or risk of an exacerbation treated with antibiotics and/or systemic corticosteroids does not exceed the threshold of clinical usefulness, we cannot exclude the possibility that the reduction is of a magnitude not considered clinically worthwhile. Hence, the available evidence can be considered consistent with either an increase or a decrease in hospitalization rates (ie, severe exacerbation) or risk of an exacerbation as a result of the intervention.
The proportion of missing outcome data compared to observed outcome data in some of the trials20–25 is enough to induce a clinically relevant bias in the observed intervention effects. There is no consensus on how to handle participants in a meta-analysis for whom data are not available.15 We opted for an available case analysis as opposed to intention to treat analysis using imputation. Although our findings do provide an analysis of efficacy, the lack of intention to treat approach precludes an effectiveness analysis of the supervised maintenance exercise.29
Effects estimated from published studies only may be inflated due to bias toward the nonpublication of studies with nonsignificant effects. The fact that all of the included published studies did not report significant effects of supervised maintenance exercise on health care use mitigates concerns about publication bias. All of the trials included in the meta-analyses were classified as having an overall medium or high risk of bias. Therefore, the quality of the overall evidence presented in this review is low. There were many individual domains where the risk of bias was unclear, primarily due to incomplete reporting. It is important to consider that this may not be poor reporting per se, and rather limitations in study design.30 Also, as commonly found in COPD trials, especially those >6 months in duration, many studies were classified as having high attrition bias.31
Comparison with other reviews
No previous systematic review has synthesized data from randomized controlled trials assessing the effects of supervised maintenance exercise following pulmonary rehabilitation on health care use. There were three previous systematic reviews in COPD that had synthesized the available evidence on supervised maintenance programs following pulmonary rehabilitation, but meta-analyses were limited to exercise capacity and quality of life outcomes.5,7,32 Similarities, with regard to the benefits of exercise in our review, can be seen with Moore et al8 where data from randomized controlled trials on health care use following pulmonary rehabilitation alone were synthesized. However, this review did not focus on interventions aiming to maintain exercise regimens following pulmonary rehabilitation but instead evaluated the short- and long-term benefits of initial pulmonary rehabilitation programs on exacerbations compared to no treatment. It was concluded that the delivery of pulmonary rehabilitation to stable COPD patients or patients following acute exacerbations results in reduced rates of hospitalizations compared to usual care. Our findings suggest that continuing maintenance exercise in a supervised manner following pulmonary rehabilitation may further enhance the benefit on certain health care use outcomes.
Implications for clinical practice
Based on the evidence presented in this review, it would currently be unwise to make specific recommendations on clinical care within this area. Due to the low precision (wide confidence intervals) in our effect estimates, only one of our meta-analyses translated to a statistically significant difference in health care use as a result of supervised maintenance exercise. However, early indications are promising, whereby the current point estimates of effect in some of the outcomes (eg, exacerbation rate) would be large enough to be classified as clinically significant. These clinically significant findings could have large implications for future postrehabilitation care. While there are proposals that “one size does not fit all” with pulmonary rehabilitation maintenance,28 supervised maintenance exercise will likely play an important part in future practice recommendations. Arguably, the funding and reimbursement of supervised maintenance programs may largely depend on evaluations of cost-effectiveness. In theory, offering continued supervised maintenance exercise programs following pulmonary rehabilitation may not be cost-effective in the short term due to the initial outlay of setting up a program;21,33 however, the potential reductions in health care use in the medium to long term seen within this review may be large enough to produce a favorable cost–benefit ratio to health care budgets. This review highlights the importance of this active area of research and upon completion of further studies, its influence on future clinical practice.
Implications for future research
The findings of our meta-analyses must be interpreted in relation to quality and quantity of available evidence. The low precision of the individual study estimates (as a result of small sample sizes and hence low number of events) widens the confidence intervals for the point estimates of effect, highlighting the important impact that further research could have.
Further randomized trials addressing the current uncertainty about the effects of supervised maintenance exercise versus usual care on outcomes such as mortality and risk of exacerbation would need to be large (in sample size and/or a duration of follow-up ≥12 months). None of the included studies reported an a priori sample size calculation to determine the effect of supervised maintenance exercise on outcomes related to health care use.18,20,22,25 Future studies should include an appropriately powered sample size calculation based on proposed minimal clinically important differences. These studies should also adopt proper statistical analysis of outcomes (particularly exacerbations). Typical distribution of COPD exacerbations data and recommended statistical approaches have been discussed elsewhere.34,35 To facilitate critical appraisal and interpretation, future randomized trials would also benefit from adhering to Consolidated Standards of Reporting Trials (CONSORT) guidelines.
Our findings have general applicability to all stable COPD patients referred to pulmonary rehabilitation. As none of the included trials stratified randomization by COPD severity, it is unclear whether our findings are equally applicable to all stages of COPD severity or exacerbation status. Further research is required to ascertain the effects of supervised maintenance exercise programs following early rehabilitation programs where patients are inherently considered to have a greater baseline risk of health care use. Similarly, our review was limited to patients with a diagnosis of COPD; efficacy of exercise maintenance options for other chronic respiratory conditions requires attention.
During our searches, we identified two protocols of randomized trials (based in the USA and Canada) that meet our eligibility criteria (Table S3).36,37 Compared to usual care following pulmonary rehabilitation, one study36 is randomizing patients to Tai Chi classes, or a walking group for a 6-month period, while another study37 is randomizing patients to a 12-month community exercise program. An update on the synthesis of the available evidence would be encouraged upon completion of the trials. For the design and delivery of new trials, research teams should note recent recommendations from the Australian and New Zealand Pulmonary Rehabilitation Guidelines6 that maintenance programs of monthly or three monthly supervised exercises (or less frequently) are insufficient to maintain exercise capacity or quality of life. It is reasonable to suggest that this frequency of supervised maintenance exercise compared with usual care is also unlikely to benefit outcomes related to health care use. However, we recognize that there is growing interest in different approaches to maintain the benefits of pulmonary rehabilitation, for example, telerehabilitation,38 telecoaching,39 and pedometer feedback.40
Conclusion
This systematic review and meta-analysis suggests that supervised maintenance exercise programs compared to usual care following pulmonary rehabilitation may be beneficial in reducing health care use. However, the quality of the available evidence was variable. This outlines the requirement for methodologically sound and large studies to provide more precise estimates for the effects of postpulmonary rehabilitation maintenance.
Supplementary materials
Methods
Data extraction
The following study characteristics were extracted: methods of the study (date/title of the study, aim of study, study design, unit of allocation, duration of study, duration of intervention, primary outcome, secondary outcomes, and funding source), participants (population description, demographics, inclusion criteria, exclusion criteria, method of recruitment of participants, total number randomized, clusters, baseline imbalances, withdrawal and exclusions, and subgroups reported), intervention and where relevant comparator (group name, number randomized to group-sample size, description, venue numbers/locations, duration and frequency of maintenance exercise training period, delivery, providers, co-interventions, compliance/adherence, and defined parameters of usual care), and outcomes (outcome name, outcome type, outcome definition, person measuring/reporting, unit of measurement, scales [upper and lower limits], outcome tool validation, imputation of missing data, assumed risk estimate, and level of power).
Trial-level data, effect estimates, and forest plot of comparison for the risk of all-cause hospital admission.
Abbreviations: CI, confidence interval; IV, inverse variance.
Trial-level data, effect estimates, and forest plot of comparison for the risk of GP visits.
Abbreviations: CI, confidence interval; GP, general practitioner; IV, inverse variance.
Table S1.
Example search strategy of a bibliographic database (CINAHL)
| Number | Search term | Field |
|---|---|---|
| 1 | Lung diseases, obstructive | MH (explode) |
| 2 | Lung diseases, interstitial | MH (explode) |
| 3 | Pulmonary fibrosis | MH (explode) |
| 4 | COPD | TX |
| 5 | Chronic obstructive pulmonary disease | TX |
| 6 | COAD | TX |
| 7 | COBD | TX |
| 8 | Emphysem* | TX |
| 9 | Chronic bronchitis | TX |
| 10 | Cystic fibrosis | TX |
| 11 | Pneumoconiosis | TX |
| 12 | Sarcoidosis | TX |
| 13 | Asthma | TX |
| 14 | Bronchiectasis | TX |
| 15 | Alveolitis | TX |
| 16 | Histiocytosis | TX |
| 17 | Granulomatosis | TX |
| 18 | Bagassosis | TX |
| 19 | Asbestosis OR byssinosis OR siderosis OR silicosis OR berylliosis OR anthracosilicosis | TX |
| 20 | Scleroderma | TX |
| 21 | 1 OR 2 OR 3 OR 4 OR 5 OR 6 OR 7 OR 8 OR 9 OR 10 OR 11 OR 12 OR 13 OR 14 OR 15 OR 16 OR 17 OR 18 OR 19 OR 20 | |
| 22 | Exercise therapy | MH (explode) |
| 23 | Activities of daily living | MH (explode) |
| 24 | Rehabilitation research | MH |
| 25 | Physical and rehabilitation medicine | MH (explode) |
| 26 | Physical fitness | MH |
| 27 | Exercise movement techniques | MH (explode) |
| 28 | Telerehabilitation | MH |
| 29 | Rehabilitation N2 pulmonary OR respiratory OR physical OR early | TI, AB |
| 30 | Exercis* N3 supervi* OR training OR maintenance OR program* | TI, AB |
| 31 | Physical activit* | TI, AB |
| 32 | Maintenance N2 intervention OR group OR exercise OR program* OR training | TI, AB |
| 33 | 22 OR 23 OR 24 OR 25 OR 26 OR 27 OR 28 OR 29 OR 30 OR 31 OR 32 | |
| 34 | Randomised | TI, AB |
| 35 | Randomized | TI, AB |
| 36 | Randomly | TI, AB |
| 37 | Trial | TI, AB |
| 38 | Controlled | TI, AB |
| 39 | 34 OR 35 OR 36 OR 37 OR 38 | |
| 40 | 21 AND 33 AND 39 |
Notes: Searches encompassed other chronic lung conditions as part of a wider review.
Truncation operator.
Table S2.
Characteristics of excluded studies
| Study | Reason(s) for exclusion |
|---|---|
| Andrews et al (2015)1 | Not a randomized trial |
| Bernocchi et al (2016)2 | Intervention not relevant (unsupervised) |
| Berry et al (2003)3 | Outcomes not applicable |
| Bertolini et al (2016)4 | Not randomized; outcomes not applicable; intervention not relevant (unsupervised) |
| Brooks et al (2002)5 | Outcomes not applicable |
| Browne et al (2013)6 | Conference abstract – full text included |
| Carrieri-Kohlman et al (2005)7 | Intervention not relevant (did not include pulmonary rehabilitation) |
| Cejudo et al (2014)8 | Conference abstract – full text included; outcomes not applicable |
| Cejudo et al (2014)9 | Conference abstract – full text included; outcomes not applicable |
| Cruz et al (2016)10 | Intervention not relevant (behavioral feedback intervention-unsupervised) |
| Desveaux et al (2016)11 | Ongoing trial – data not available |
| du Moulin et al (2009)12 | Intervention not relevant (unsupervised); outcomes not applicable |
| Eisner and van Straten (2003)13,a | Conference title only |
| Elliott et al (2004)14 | Outcomes not applicable |
| Fu et al (2016)15 | Intervention not relevant (no exercise intervention post-pulmonary rehabilitation) |
| Gomez et al (2006)16 | Conference abstract – full text included |
| Guell et al (2000)17 | Intervention not relevant (control group did not receive pulmonary rehabilitation) |
| Heppner et al (2006)18 | Not a randomized trial |
| Hill and McDonald (2004)19 | Outcomes not applicable |
| Kotrach et al (2016)20 | Intervention not relevant (unsupervised) |
| Linneberg et al (2012)21 | Outcomes not applicable |
| Martinez et al (2008)22 | Conference abstract – full text included |
| Moy et al (2015)23 | Ongoing trial – data not available |
| Perumal et al (2010)24 | Not a randomized trial |
| Pleguezuelos et al (2013)25 | Intervention not relevant (unsupervised); outcomes not applicable |
| Ries et al (2008)26 | Intervention not relevant (unsupervised and control group received additional care); outcomes not applicable |
| Ringbaek et al (2009)27 | Conference abstract – full text included |
| Rodriguez-Trigo et al (2011)28 | Conference abstract – full text included |
| Scalvini et al (2016)29 | Intervention not relevant (unsupervised) |
| Spencer et al (2007)30 | Conference abstract – full text included |
| Spencer et al (2009)31 | Conference abstract – full text included |
| Swerts et al (1990)32 | Outcomes not applicable |
| van Wetering et al (2010)33 | Intervention not relevant (control group did not receive pulmonary rehabilitation); outcomes not applicable |
| Vasilopoulou et al (2017)34 | Intervention not relevant (control group did not receive pulmonary rehabilitation) |
Notes: Abstract and full text were nonretrievable.
Study excluded due to presentation as a conference title only in search results.
Table S3.
Ongoing studies
| Study name or title | Study period (start and end dates) (country) | Study design | Participants | Intervention and comparison | Relevant outcomes |
|---|---|---|---|---|---|
| LEAP: design and rationale of a randomized controlled trial of Tai Chi23 | August 2012 to September 2017 (USA) | Randomized controlled trial (2:2:1 ratio) | 90 COPD patients who have just been discharged from pulmonary rehabilitation | 1. Tai Chi (1 h, twice a week for 3 months, then once a week for 3 months. A total of 36 classes) 2. Usual care (general recommendations for exercise) 3. Walking group (same frequency and duration as Tai Chi) |
Hospital admissions (respiratory) and acute exacerbations (use of corticosteroids and/or antibiotics verified by medical records) |
| Effects of a community-based, postrehabilitation exercise program in COPD: protocol for a randomized controlled trial with embedded process evaluation11 | November 2012 to August 2018 (Canada) | Randomized controlled trial | 100 COPD patients who have completed pulmonary rehabilitation within the last 2 weeks | 1. Usual care (standard home exercise instructions postpulmonary rehabilitation) 2. Community-based exercise program (1 h, minimum of two sessions per week (option to do more) for 1 year) |
Exacerbations (self-reported) |
Abbreviation: LEAP, long-term exercise after pulmonary rehabilitation.
References
- 1.Andrews SM, Carter M, Deoghare H, Mills PK, van Gundy K, Jain VV. Pulmonary rehabilitation maintenance program prevents accelerated FEV1 decline and may prevent exacerbations in patients with severe COPD. Am J Respir Crit Care Med. 2015;191:A2013. [Google Scholar]
- 2.Bernocchi P, Scalvini S, Baratti D, et al. A multidisciplinary telehealth program in patients with combined chronic obstructive pulmonary disease and chronic heart failure: study protocol for a randomized controlled trial. Trials. 2016;17(1):462. doi: 10.1186/s13063-016-1584-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Berry MJ, Rejeski WJ, Adair NE, Ettinger WH, Zaccaro DJ, Sevick MA. A randomized, trolled trial comparing long-term and short-term exercise in patients with chronic obstructive pulmonary disease. J Cardiopulm Rehabil. 2003;23:60–68. doi: 10.1097/00008483-200301000-00011. [DOI] [PubMed] [Google Scholar]
- 4.Bertolini GN, Ramos D, Leite MR, et al. Effects of a home-based exercise program after supervised resistance training in patients with chronic obstructive pulmonary disease. Medicina. 2016;49:331–337. [Google Scholar]
- 5.Brooks D, Krip B, Mangovski-Alzamora S, Goldstein RS. The effect of postrehabilitation programmes among individuals with chronic obstructive pulmonary disease. Eur Respir J. 2002;20:20–29. doi: 10.1183/09031936.02.01852001. [DOI] [PubMed] [Google Scholar]
- 6.Browne P, Olive S, Staunton L, et al. The effects of maintenance schedules following pulmonary rehabilitation in patients with chronic obstructive pulmonary disease. Thorax. 2013;68(Suppl 3):A16. doi: 10.1136/bmjopen-2014-005921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Carrieri-Kohlman V, Nguyen HQ, Donesky-Cuenco D, Demir-Deviren S, Neuhaus J, Stulbarg MS. Impact of brief or extended exercise training on the benefit of a dyspnea self-management program in COPD. J Cardiopulm Rehabil. 2005;25:275–284. doi: 10.1097/00008483-200509000-00009. [DOI] [PubMed] [Google Scholar]
- 8.Cejudo P, Galdiz B, Puy C, et al. Evaluation of a maintenance 3-year follow-up pulmonary rehabilitation program. Eur Respir J. 2014;44:1708. [Google Scholar]
- 9.Cejudo P, Galdiz B, Puy C, et al. Outcomes evaluation of a maintenance 3-year follow-up pulmonary rehabilitation programme. Am J Respir Crit Care Med. 2014;189:A3645. [Google Scholar]
- 10.Cruz J, Marques A, Brooks D. Walk2Bactive: a randomized controlled trial of a physical activity-focused behavioural intervention beyond pulmonary rehabilitation in chronic obstructive pulmonary disease. Chron Respir Dis. 2016;13(1):57–66. doi: 10.1177/1479972315619574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Desveaux L, Beauchamp MK, Lee A, Ivers N, Goldstein R, Brooks D. Effects of a community-based, post-rehabilitation exercise program in COPD: protocol for a randomized controlled trial with embedded process evaluation. JMIR Res Protoc. 2016;5(2):e63. doi: 10.2196/resprot.5435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.du Moulin M, Taube K, Wegscheider K, Behnke M, van den Bussche H. Home-based exercise training as maintenance after outpatient pulmonary rehabilitation. Respiration. 2009;77(2):139–145. doi: 10.1159/000150315. [DOI] [PubMed] [Google Scholar]
- 13.Eisner B, van Straten J. The decline in acute hospitalizations for COPD patients in a pulmonary rehab maintenance program. Presented at the National COPD Conference; Arlington, VA, USA. November 14–15, 2003. [Google Scholar]
- 14.Elliott M, Watson C, Wilkinson E, Musk AW, Lake FR. Short- and long-term hospital and community exercise programmes for patients with chronic obstructive pulmonary disease. Respirology. 2004;9(3):345–351. doi: 10.1111/j.1440-1843.2004.00595.x. [DOI] [PubMed] [Google Scholar]
- 15.Fu JJ, Min J, Yu PM, McDonald VM, Mao B. Study design for a randomised controlled trial to explore the modality and mechanism of Tai Chi in the pulmonary rehabilitation of chronic obstructive pulmonary disease. BMJ Open. 2016;6(8):e011297. doi: 10.1136/bmjopen-2016-011297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gomez A, Roman M, Larraz C, et al. Efficacy of respiratory rehabilitation on patients with moderate COPD in primary care and maintenance of benefits at 2 years. Aten Primaria. 2006;38(4):230–233. doi: 10.1157/13092346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Guell R, Casan P, Belda J, et al. Long-term effects of outpatient rehabilitation of COPD: a randomized trial. Chest. 2000;117(4):976–983. doi: 10.1378/chest.117.4.976. [DOI] [PubMed] [Google Scholar]
- 18.Heppner PS, Morgan C, Kaplan RM, Ries AL. Regular walking and long-term maintenance of outcomes after pulmonary rehabilitation. J Cardiopulm Rehabil. 2006;26(1):44–53. doi: 10.1097/00008483-200601000-00010. [DOI] [PubMed] [Google Scholar]
- 19.Hill C, McDonald C. A maintenance program post pulmonary rehabilitation improved exercise tolerance in patients with COPD. Respirology. 2004;9:A8. [Google Scholar]
- 20.Kotrach H, Dajczman E, Baltzan MA, et al. A randomized controlled pilot study using a virtual game system (VGS) as a home-based exercise modality following pulmonary rehabilitation (PR) in patients with COPD. Am J Respir Crit Care Med. 2016;193:A4530. [Google Scholar]
- 21.Linneberg A, Rasmussen M, Buch TF, et al. A randomised study of the effects of supplemental exercise sessions after a 7-week chronic obstructive pulmonary disease rehabilitation program. Clin Respir J. 2012;6(2):112–119. doi: 10.1111/j.1752-699X.2011.00256.x. [DOI] [PubMed] [Google Scholar]
- 22.Martinez G, Thogersen J, Brondum E, Ringbaek T, Lange P. Effect of maintenance training after 7 weeks rehabilitation programme. Berlin: European Respiratory Society Annual Congress; 2008. [Google Scholar]
- 23.Moy ML, Wayne PM, Litrownik D, et al. Long-term exercise after pulmonary rehabilitation (LEAP): design and rationale of a randomized controlled trial of Tai Chi. Contemp Clin Trials. 2015;45(Pt B):458–467. doi: 10.1016/j.cct.2015.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Perumal SD, Ni N, O’Driscoll MF, Joyce R, Mc TJ. Efficacy of a maintenance programme on patients with COPD following pulmonary rehabilitation. Irish J Med Sci. 2010;179:S482. [Google Scholar]
- 25.Pleguezuelos E, Perez ME, Guirao L, et al. Improving physical activity in patients with COPD with urban walking circuits. Respir Med. 2013;107:1948–1956. doi: 10.1016/j.rmed.2013.07.008. [DOI] [PubMed] [Google Scholar]
- 26.Ries AL, Make BJ, Reilly JJ. Pulmonary rehabilitation in emphysema. Proc Am Thorac Soc. 2008;5:524–529. doi: 10.1513/pats.200707-093ET. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ringbaek T, Broendum E, Martinez G, Thoegersen J, Lange P. Effect of maintenance training after 7-weeks rehabilitation programme on hospitalisation. Vienna: European Respiratory Society Annual Congress; 2009. [Google Scholar]
- 28.Rodriguez-Trigo G, Cejudo P, Puy C, et al. Long term pulmonary rehabilitation programs for chronic obstructive pulmonary disease (COPD). Two years follow-up. Eur Respir J. 2011;38:3645. [Google Scholar]
- 29.Scalvini S, Bernocchi P, Baratti D, et al. Multidisciplinary telehealth program for patients affected by chronic heart failure and chronic obstructive pulmonary disease. Eur J Heart Fail. 2016;18:94. doi: 10.1186/s13063-016-1584-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Spencer L, Alison J, McKeough Z. Maintenance of exercise capacity following pulmonary rehabilitation in COPD: a randomised controlled trial. Stockholm: European Respiratory Society Annual Congress; 2007. [Google Scholar]
- 31.Spencer LM, Alison JA, McKeough ZJ. Do supervised weekly exercise programs maintain functional exercise capacity and quality of life, twelve months after pulmonary rehabilitation in COPD? BMC Pulm Med. 2009;7:7. doi: 10.1186/1471-2466-7-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Swerts PM, Kretzers LM, Terpstra-Lindeman E, Verstappen FT, Wouters EF. Exercise reconditioning in the rehabilitation of patients with chronic obstructive pulmonary disease: a short- and long-term analysis. Arch Phys Med Rehabil. 1990;71(8):570–573. [PubMed] [Google Scholar]
- 33.van Wetering CR, Hoogendoorn M, Mol SJ, Rutten-van Molken MP, Schols AM. Short- and long-term efficacy of a community-based COPD management programme in less advanced COPD: a randomised controlled trial. Thorax. 2010;65(1):7–13. doi: 10.1136/thx.2009.118620. [DOI] [PubMed] [Google Scholar]
- 34.Vasilopoulou M, Papaioannou AI, Kaltsakas G, et al. Home-based maintenance tele-rehabilitation reduces the risk for AECOPD, hospitalizations and emergency department visits. Eur Respir J. 2017;49(5):1602129. doi: 10.1183/13993003.02129-2016. [DOI] [PubMed] [Google Scholar]
Acknowledgments
We acknowledge the cooperation of authors (Rosa Guell, Pilar Cejudo Ramos, Lissa Spencer, Miguel Roman, Magdalena Esteva, Thomas Ringbaek, Ed Wilson, and Greg Moullec) of the included studies in this review for providing data in a format appropriate for analyses. We also thank Marilyn Moy, Laura Desveaux, and Dina Brooks for providing updates on their current ongoing trials related to this review. This review was conducted during Alex R Jenkins’ PhD studentship, which was part of the Doctoral Training Alliance Applied Biosciences for Health Programme.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Spruit M, Singh S, Garvey C, et al. An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med. 2013;188(8):13–64. doi: 10.1164/rccm.201309-1634ST. [DOI] [PubMed] [Google Scholar]
- 2.McCarthy B, Casey D, Devane D, Murphy K, Murphy E, Lacasse Y. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2015;(2):CD003793. doi: 10.1002/14651858.CD003793.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lacasse Y, Cates CJ, McCarthy B, et al. This Cochrane Review is closed: deciding what constitutes enough research and where next for pulmonary rehabilitation in COPD. Cochrane Database Syst Rev. 2015;(11):ED000107. doi: 10.1002/14651858.ED000107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mador MJ, Patel AN, Nadler J. Effects of pulmonary rehabilitation on activity levels in patients with chronic obstructive pulmonary disease. J Cardiopulm Rehabil. 2011;31(1):52–59. doi: 10.1097/HCR.0b013e3181ebf2ef. [DOI] [PubMed] [Google Scholar]
- 5.Beauchamp MK, Evans R, Janaudis-Ferreira T, Goldstein RS, Brooks D. Systematic review of supervised exercise programs after pulmonary rehabilitation in individuals with COPD. Chest. 2013;144(4):1124–1133. doi: 10.1378/chest.12-2421. [DOI] [PubMed] [Google Scholar]
- 6.Alison JA, McKeough ZJ, Johnston K, et al. Australian and New Zealand pulmonary rehabilitation guidelines. Respirology. 2017;22:800–819. doi: 10.1111/resp.13025. [DOI] [PubMed] [Google Scholar]
- 7.Busby AK, Reese RL, Simon SR. Pulmonary rehabilitation maintenance interventions: a systematic review. Am J Health Behav. 2014;38(3):321–330. doi: 10.5993/AJHB.38.3.1. [DOI] [PubMed] [Google Scholar]
- 8.Moore E, Palmer T, Newson R, Majeed A, Quint JK, Soljak MA. Pulmonary rehabilitation as a mechanism to reduce hospitalizations for acute exacerbations of COPD: a systematic review and meta-analysis. Chest. 2016;150(4):837–859. doi: 10.1016/j.chest.2016.05.038. [DOI] [PubMed] [Google Scholar]
- 9.Puhan MA, Gimeno-Santos E, Scharplatz M, et al. Pulmonary rehabilitation following exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2011;(10):CD005305. doi: 10.1002/14651858.CD005305.pub3. [DOI] [PubMed] [Google Scholar]
- 10.Puhan MA, Gimeno-Santos E, Cates CJ, et al. Pulmonary rehabilitation following exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2016;(12):CD005305. doi: 10.1002/14651858.CD005305.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.British Thoracic Society . Chronic Obstructive Pulmonary Disease in Over 16s: Diagnosis and Management. London: British Thoracic Society; 2011. [Google Scholar]
- 12.American College of Physicians, American College of Chest Physicians, American Thoracic Society et al. Diagnosis and management of stable chronic obstructive pulmonary disease: a clinical practice guideline update from the American College of Physicians, American College of Chest Physicians, American Thoracic Society, and European Respiratory Society. Ann Intern Med. 2011;155(3):179–191. doi: 10.7326/0003-4819-155-3-201108020-00008. [DOI] [PubMed] [Google Scholar]
- 13.Global Initiative for Chronic Obstructive Lung Disease Global Strategy for the Diagnosis, Management, and Prevention of COPD – 2016. [Accessed December 12, 2017]. Available from: http://goldcopd.org/global-strategy-diagnosis-management-prevention-copd-2016/
- 14.Lamb SE, Becker C, Gillespie LD, et al. Reporting of complex interventions in clinical trials: development of a taxonomy to classify and describe fall-prevention interventions. Trials. 2011;12:125. doi: 10.1186/1745-6215-12-125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.2. The Cochrane Collaboration. 2009. [Accessed April 18, 2017]. webpage on the Internet. [updated September 2009]. Available from: http://handbook.cochrane.org/v5.0.2/
- 16.Ries AL, Kaplan RM, Myers R, et al. Maintenance after pulmonary rehabilitation in chronic lung disease. Am J Respir Crit Care Med. 2003;167(6):880–888. doi: 10.1164/rccm.200204-318OC. [DOI] [PubMed] [Google Scholar]
- 17.Brooks D, Krip B, Mangovski-Alzamora S, Goldstein RS. The effect of postrehabilitation programmes among individuals with chronic obstructive pulmonary disease. Eur Respir J. 2002;20:20–29. doi: 10.1183/09031936.02.01852001. [DOI] [PubMed] [Google Scholar]
- 18.Spencer L, Alison JA, McKeough ZJ. Maintaining benefits following pulmonary rehabilitation: a randomised controlled trial. Eur Respir J. 2010;35(3):571–577. doi: 10.1183/09031936.00073609. [DOI] [PubMed] [Google Scholar]
- 19.Ringbaek T, Brondum E, Martinez G, et al. Long-term effects of 1-year maintenance training on physical functioning and health status in patients with COPD. J Cardiopulm Rehabil. 2010;30(1):47–52. doi: 10.1097/HCR.0b013e3181c9c985. [DOI] [PubMed] [Google Scholar]
- 20.Wilson AM, Browne P, Olive S, et al. The effects of maintenance schedules following pulmonary rehabilitation in patients with chronic obstructive pulmonary disease: a randomised controlled trial. BMJ Open. 2015;5(3):e005921. doi: 10.1136/bmjopen-2014-005921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Burns DK, Wilson ECF, Browne P, et al. The cost effectiveness of maintenance schedules following pulmonary rehabilitation in patients with chronic obstructive pulmonary disease: an economic evaluation alongside a randomised controlled trial. Appl Health Econ Health Policy. 2016;14(1):105–115. doi: 10.1007/s40258-015-0199-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Roman M, Larraz C, Gomez A, et al. Efficacy of pulmonary rehabilitation in patients with moderate chronic obstructive pulmonary disease: a randomized controlled trial. BMC Fam Pract. 2013;14:21. doi: 10.1186/1471-2296-14-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Moullec G, Ninot G, Varray A, Desplan J, Hayot M, Prefaut C. An innovative maintenance follow-up program after a first inpatient pulmonary rehabilitation. Respir Med. 2008;102(4):556–566. doi: 10.1016/j.rmed.2007.11.012. [DOI] [PubMed] [Google Scholar]
- 24.Moullec G, Ninot G. An integrated programme after pulmonary rehabilitation in patients with chronic obstructive pulmonary disease: effect on emotional and functional dimensions of quality of life. Clin Rehabil. 2010;24(2):122–136. doi: 10.1177/0269215509346088. [DOI] [PubMed] [Google Scholar]
- 25.Guell MR, Cejudo P, Ortega F, et al. Benefits of long-term pulmonary rehabilitation maintenance program in severe COPD patients: 3 year follow-up. Am J Respir Crit Care Med. 2017;195(5):622–629. doi: 10.1164/rccm.201603-0602OC. [DOI] [PubMed] [Google Scholar]
- 26.Wedzicha JA, Miravitlles M, Hurst JR, et al. Management of COPD exacerbations: a European Respiratory Society/American Thoracic Society guideline. Eur Respir J. 2017;49(3):1600791. doi: 10.1183/13993003.00791-2016. [DOI] [PubMed] [Google Scholar]
- 27.Jones PW, Beeh KM, Chapman KR, et al. Minimally clinically important differences in pharmacological trials. Am J Respir Crit Care Med. 2014;189(3):250–255. doi: 10.1164/rccm.201310-1863PP. [DOI] [PubMed] [Google Scholar]
- 28.Rochester C, Spruit M. Maintaining the benefits of pulmonary rehabilitation. The Holy Grail. Am J Respir Crit Care Med. 2017;195(5):548–551. doi: 10.1164/rccm.201609-1925ED. [DOI] [PubMed] [Google Scholar]
- 29.Aaron SD, Fergusson D, Marks GB, et al. Counting, analysing and reporting exacerbations of COPD in randomised controlled trials. Thorax. 2008;63(8):122–128. doi: 10.1136/thx.2007.082636. [DOI] [PubMed] [Google Scholar]
- 30.Kjaergard LL, Villumsen J, Gluud C. Reported methodologic quality and discrepancies between large and small randomized trials in meta-analyses. Ann Intern Med. 2001;135(11):982–989. doi: 10.7326/0003-4819-135-11-200112040-00010. [DOI] [PubMed] [Google Scholar]
- 31.Welsh EJ, Cates CJ, Poole P. Combination inhaled steroid and long-acting beta2-agonist versus tiotropium for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2013;(5):CD007891. doi: 10.1002/14651858.CD007891.pub3. [DOI] [PubMed] [Google Scholar]
- 32.Soysa S, McKeough Z, Spencer L, et al. Effects of maintenance programs on exercise capacity and quality of life in chronic obstructive pulmonary disease. Phys Ther Rev. 2012;17:335–345. [Google Scholar]
- 33.Griffiths TL, Phillips CJ, Davies S, Burr ML, Campbell IA. Cost effectiveness of an outpatient multidisciplinary pulmonary rehabilitation programme. Thorax. 2001;56(10):779–784. doi: 10.1136/thorax.56.10.779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Keene ON, Jones MR, Lane PW, Anderson J. Analysis of exacerbation rates in asthma and chronic obstructive pulmonary disease: example from the TRISTAN study. Pharm Stat. 2007;6(2):89–97. doi: 10.1002/pst.250. [DOI] [PubMed] [Google Scholar]
- 35.Keene ON, Calverley PM, Jones PW, Vestbo J, Anderson JA. Statistical analysis of exacerbation rates in COPD: TRISTAN and ISOLDE revisited. Eur Respir J. 2008;32(1):17–24. doi: 10.1183/09031936.00161507. [DOI] [PubMed] [Google Scholar]
- 36.Moy ML, Wayne PM, Litrownik D, et al. Long-term exercise after pulmonary rehabilitation (LEAP): design and rationale of a randomized controlled trial of Tai Chi. Contemp Clin Trials. 2015;45:458–467. doi: 10.1016/j.cct.2015.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Desveaux L, Beauchamp MK, Lee A, Ivers N, Goldstein R, Brooks D. Effects of a community-based, post-rehabilitation exercise program in COPD: protocol for a randomized controlled trial with embedded process evaluation. JMIR Res Protoc. 2016;5(2):e63. doi: 10.2196/resprot.5435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Vasilopoulou M, Papaioannou AI, Kaltsakas G, et al. Home-based maintenance tele-rehabilitation reduces the risk for AECOPD, hospitalizations and emergency department visits. Eur Respir J. 2017;49(5):1602129. doi: 10.1183/13993003.02129-2016. [DOI] [PubMed] [Google Scholar]
- 39.Nguyen HQ, Gill DP, Wolpin S, Steele BG, Benditt JO. Pilot study of a cell phone-based exercise persistence intervention post-rehabilitation for COPD. Int J Chron Obstruct Pulmon Dis. 2009;4:301–313. doi: 10.2147/copd.s6643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cruz J, Brooks D, Marques A. Walk2Bactive: a randomised controlled trial of a physical activity-focused behavioural intervention beyond pulmonary rehabilitation in chronic obstructive pulmonary disease. Chron Respir Dis. 2016;13(1):57–66. doi: 10.1177/1479972315619574. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Trial-level data, effect estimates, and forest plot of comparison for the risk of all-cause hospital admission.
Abbreviations: CI, confidence interval; IV, inverse variance.
Trial-level data, effect estimates, and forest plot of comparison for the risk of GP visits.
Abbreviations: CI, confidence interval; GP, general practitioner; IV, inverse variance.
Table S1.
Example search strategy of a bibliographic database (CINAHL)
| Number | Search term | Field |
|---|---|---|
| 1 | Lung diseases, obstructive | MH (explode) |
| 2 | Lung diseases, interstitial | MH (explode) |
| 3 | Pulmonary fibrosis | MH (explode) |
| 4 | COPD | TX |
| 5 | Chronic obstructive pulmonary disease | TX |
| 6 | COAD | TX |
| 7 | COBD | TX |
| 8 | Emphysem* | TX |
| 9 | Chronic bronchitis | TX |
| 10 | Cystic fibrosis | TX |
| 11 | Pneumoconiosis | TX |
| 12 | Sarcoidosis | TX |
| 13 | Asthma | TX |
| 14 | Bronchiectasis | TX |
| 15 | Alveolitis | TX |
| 16 | Histiocytosis | TX |
| 17 | Granulomatosis | TX |
| 18 | Bagassosis | TX |
| 19 | Asbestosis OR byssinosis OR siderosis OR silicosis OR berylliosis OR anthracosilicosis | TX |
| 20 | Scleroderma | TX |
| 21 | 1 OR 2 OR 3 OR 4 OR 5 OR 6 OR 7 OR 8 OR 9 OR 10 OR 11 OR 12 OR 13 OR 14 OR 15 OR 16 OR 17 OR 18 OR 19 OR 20 | |
| 22 | Exercise therapy | MH (explode) |
| 23 | Activities of daily living | MH (explode) |
| 24 | Rehabilitation research | MH |
| 25 | Physical and rehabilitation medicine | MH (explode) |
| 26 | Physical fitness | MH |
| 27 | Exercise movement techniques | MH (explode) |
| 28 | Telerehabilitation | MH |
| 29 | Rehabilitation N2 pulmonary OR respiratory OR physical OR early | TI, AB |
| 30 | Exercis* N3 supervi* OR training OR maintenance OR program* | TI, AB |
| 31 | Physical activit* | TI, AB |
| 32 | Maintenance N2 intervention OR group OR exercise OR program* OR training | TI, AB |
| 33 | 22 OR 23 OR 24 OR 25 OR 26 OR 27 OR 28 OR 29 OR 30 OR 31 OR 32 | |
| 34 | Randomised | TI, AB |
| 35 | Randomized | TI, AB |
| 36 | Randomly | TI, AB |
| 37 | Trial | TI, AB |
| 38 | Controlled | TI, AB |
| 39 | 34 OR 35 OR 36 OR 37 OR 38 | |
| 40 | 21 AND 33 AND 39 |
Notes: Searches encompassed other chronic lung conditions as part of a wider review.
Truncation operator.
Table S2.
Characteristics of excluded studies
| Study | Reason(s) for exclusion |
|---|---|
| Andrews et al (2015)1 | Not a randomized trial |
| Bernocchi et al (2016)2 | Intervention not relevant (unsupervised) |
| Berry et al (2003)3 | Outcomes not applicable |
| Bertolini et al (2016)4 | Not randomized; outcomes not applicable; intervention not relevant (unsupervised) |
| Brooks et al (2002)5 | Outcomes not applicable |
| Browne et al (2013)6 | Conference abstract – full text included |
| Carrieri-Kohlman et al (2005)7 | Intervention not relevant (did not include pulmonary rehabilitation) |
| Cejudo et al (2014)8 | Conference abstract – full text included; outcomes not applicable |
| Cejudo et al (2014)9 | Conference abstract – full text included; outcomes not applicable |
| Cruz et al (2016)10 | Intervention not relevant (behavioral feedback intervention-unsupervised) |
| Desveaux et al (2016)11 | Ongoing trial – data not available |
| du Moulin et al (2009)12 | Intervention not relevant (unsupervised); outcomes not applicable |
| Eisner and van Straten (2003)13,a | Conference title only |
| Elliott et al (2004)14 | Outcomes not applicable |
| Fu et al (2016)15 | Intervention not relevant (no exercise intervention post-pulmonary rehabilitation) |
| Gomez et al (2006)16 | Conference abstract – full text included |
| Guell et al (2000)17 | Intervention not relevant (control group did not receive pulmonary rehabilitation) |
| Heppner et al (2006)18 | Not a randomized trial |
| Hill and McDonald (2004)19 | Outcomes not applicable |
| Kotrach et al (2016)20 | Intervention not relevant (unsupervised) |
| Linneberg et al (2012)21 | Outcomes not applicable |
| Martinez et al (2008)22 | Conference abstract – full text included |
| Moy et al (2015)23 | Ongoing trial – data not available |
| Perumal et al (2010)24 | Not a randomized trial |
| Pleguezuelos et al (2013)25 | Intervention not relevant (unsupervised); outcomes not applicable |
| Ries et al (2008)26 | Intervention not relevant (unsupervised and control group received additional care); outcomes not applicable |
| Ringbaek et al (2009)27 | Conference abstract – full text included |
| Rodriguez-Trigo et al (2011)28 | Conference abstract – full text included |
| Scalvini et al (2016)29 | Intervention not relevant (unsupervised) |
| Spencer et al (2007)30 | Conference abstract – full text included |
| Spencer et al (2009)31 | Conference abstract – full text included |
| Swerts et al (1990)32 | Outcomes not applicable |
| van Wetering et al (2010)33 | Intervention not relevant (control group did not receive pulmonary rehabilitation); outcomes not applicable |
| Vasilopoulou et al (2017)34 | Intervention not relevant (control group did not receive pulmonary rehabilitation) |
Notes: Abstract and full text were nonretrievable.
Study excluded due to presentation as a conference title only in search results.
Table S3.
Ongoing studies
| Study name or title | Study period (start and end dates) (country) | Study design | Participants | Intervention and comparison | Relevant outcomes |
|---|---|---|---|---|---|
| LEAP: design and rationale of a randomized controlled trial of Tai Chi23 | August 2012 to September 2017 (USA) | Randomized controlled trial (2:2:1 ratio) | 90 COPD patients who have just been discharged from pulmonary rehabilitation | 1. Tai Chi (1 h, twice a week for 3 months, then once a week for 3 months. A total of 36 classes) 2. Usual care (general recommendations for exercise) 3. Walking group (same frequency and duration as Tai Chi) |
Hospital admissions (respiratory) and acute exacerbations (use of corticosteroids and/or antibiotics verified by medical records) |
| Effects of a community-based, postrehabilitation exercise program in COPD: protocol for a randomized controlled trial with embedded process evaluation11 | November 2012 to August 2018 (Canada) | Randomized controlled trial | 100 COPD patients who have completed pulmonary rehabilitation within the last 2 weeks | 1. Usual care (standard home exercise instructions postpulmonary rehabilitation) 2. Community-based exercise program (1 h, minimum of two sessions per week (option to do more) for 1 year) |
Exacerbations (self-reported) |
Abbreviation: LEAP, long-term exercise after pulmonary rehabilitation.