Abstract
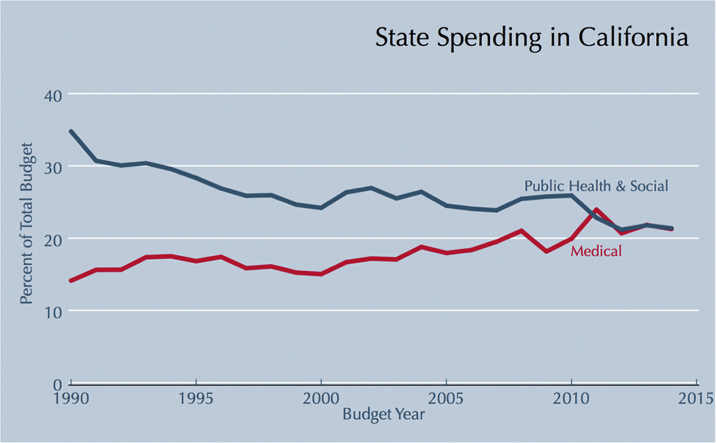
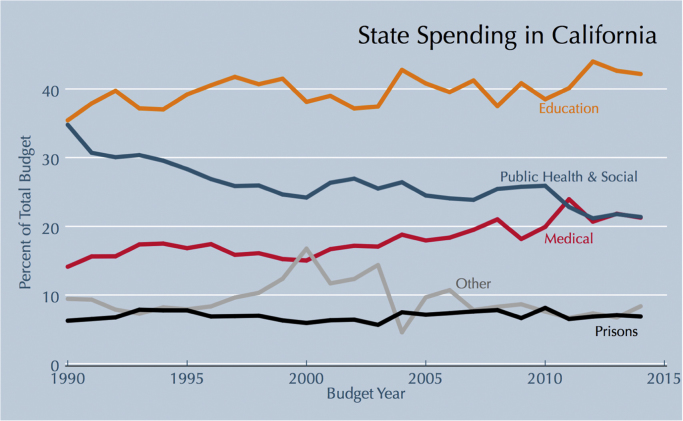
As much as 30% of US health care spending in the United States does not improve individual or population health. To a large extent this excess spending results from prices that are too high and from administrative waste. In the public sector, and particularly at the state level, where budget constraints are severe and reluctance to raise taxes high, this spending crowds out social, educational, and public-health investments. Over time, as spending on medical care increases, spending on improvements to the social determinants of health are starved. In California the fraction of General Fund expenditures spent on public health and social programs fell from 34.8% in fiscal year 1990 to 21.4% in fiscal year 2014, while health care increased from 14.1% to 21.3%. In spending more on healthcare and less on other efforts to improve health and health determinants, the state is missing important opportunities for health-promoting interventions with a strong financial return. Reallocating ineffective medical expenditures to proven and cost-effective public health and social programs would not be easy, but recognizing its potential for improving the public's health while saving taxpayers billions of dollars might provide political cover to those willing to engage in genuine reform. National estimates of the percent of medical spending that does not improve health suggest that approximately $5 billion of California's public budget for medical spending has no positive effect on health. Up to 10,500 premature deaths could be prevented annually by reallocating this portion of medical spending to public health. Alternatively, the same expenditure could help an additional 418,000 high school students to graduate.
Keywords: social determinants of health, education, public health policy, state healthcare spending
Graphical abstract
Highlights
-
•
Medical spending in California rose in 25 years from 14% to 21% of the State budget.
-
•
In this period spending on public health fell by a similar percentage.
-
•
California spends $6 billion annually on healthcare that does not improve health.
-
•
Redirecting this money to tobacco prevention would prevent 12,300 deaths annually.
-
•
Redirecting it to education would help an additional 418,000 students graduate.
1. Introduction
The United States spent $3.2 trillion or $9990 per person on healthcare in 2015 (Centers for Medicare and Medicaid Services, 2015b) and ranks first in the world for per-capita healthcare spending, which is more than double the average within the Organization for Economic Cooperation and Development (OECD) (Organisation for Economic Co-operation and Development, 2015).
Despite this elevated level of healthcare spending, Americans have both shorter life expectancy and poorer health than residents in most other OECD countries (Avendano and Kawachi, 2014, Bezruchka, 2012, National Research Council and Institute of Medicine, 2013). This US health disadvantage has been attributed to a number of cross-country differences, but differences in prices and administrative inefficiencies are major drivers of the excess costs in the US system that are also under policy control. A recent report in The New York Times (Rosenthal, Lu, & Cram, 2013) took note of sharply discordant prices for standard healthcare services in the US compared to other countries. An MRI scan whose cost averages $319 in the Netherlands costs three times that amount in the US; a hip replacement that averages $8000 in Spain costs quintuple that amount in the US; and a dose of Lipitor that averages $6 in New Zealand costs 12 times as much in the US. These examples may be extreme, but they are hardly unique or marginal. The US pays a much higher cost per service delivered than any other developed country (Squires, 2012). In a New England Journal of Medicine commentary, two well-known health economists have pointed out that simply standardizing insurance products could reduce administrative hassles, resulting in savings of $200 billion annually (Fuchs & Milstein, 2011). A report from the Institute of Medicine (Young & Olsen, 2010) estimated $425 billion a year in excessive costs-per-service delivered, including $130 billion in inefficiently delivered services, $190 billion in excessive administrative costs, and $105 billion in prices that are too high (2009 dollars).
Urgent and well-argued calls have been issues for the public health community to engage in a more informed debate about how best to allocate resources to achieve health for all (McDonough, 2016). Important observations are that a much higher fraction of public spending is on healthcare in the US than in peer countries, that a much smaller fraction is on public health and social spending, and that the US lies beyond what economists call “the flat of the curve,” the area at which additional spending on healthcare has little value, and may actually be harmful. Why do these problems persist when they seem so clearly harmful?
There is, in American medicine, a misleading narrative about hard tradeoffs: that reducing spending requires depriving people of coverage, that expanding coverage to new populations requires reducing the benefits of those with existing coverage; that enhancing the benefits will bankrupt the system; and that reducing prices will cost lives. In fact, none of these suggested tradeoffs is confirmed by empirical evidence. The purpose of the analysis here is not to make any firm claims about the impact of reallocating expenditures, but rather to show where the real tradeoffs lie.
There is at least an implicit, and possibly quite real, tradeoff between US public spending for medical care versus other social services—for which US spending is a much smaller portion of GDP than in other OECD nations (Avendano and Kawachi, 2014, Stuckler et al., 2010). This difference raises the question of whether foregone investment in non-medical social services contributes to poorer health outcomes.
Cross-national studies have observed positive associations between non-medical social spending and population health: on average, countries with greater levels of social spending have longer average life expectancies, lower infant mortality rates, and fewer potential years of life lost (Bradley et al., 2016; Bradley, Elkins, Herrin, & Elbel, 2011; Kangas, 2010). An analysis of 15 European Union countries estimated that a $100 increase in non-medical social-welfare spending was significantly associated with a 0.99% drop in all-cause mortality and a 2.8% decrease in alcohol-related mortality (Stuckler et al., 2010). Within the United States, states with higher per capita non-medical social welfare and education spending had lower rates of suicides and teenage births (Zimmerman, 1987). And states with higher non-health social-to-healthcare spending ratios had significantly better state-level health outcomes for asthma, lung cancer mortality, and limitation in daily activities (Bradley et al., 2015).
Moreover, interventions in public health, education, early childhood development, housing, and transportation have been shown to generate financial returns. For example, these program types generate increased tax revenue from higher earnings and reduced expenditures in law enforcement—that outweigh the cost of the programs (Carlson et al., 2011, Gallivan et al., 2011, Reynolds et al., 2010, Tsemberis, 2010).
But while current evidence indicates that non-medical social spending improves population health at the margin, the same cannot be said for healthcare spending. Several studies have shown that higher per capita spending does not translate to better quality of care or health outcomes (Fisher et al., 2003a, Fisher et al., 2003b, Rothberg et al., 2010), and faster medical spending growth in the US (1970–2002) than in other OECD countries has not resulted in more rapid improvements in health or longevity (White, 2007). Indeed, Institute of Medicine roundtable panelists have estimated that between 20% and 30% of health care spending could be saved without compromising health care quality and health outcomes (Institute of Medicine Roundtable on Evidence-Based Medicine, 2010; Wennberg, Fisher, & Skinner, 2002), a staggering $750-$765 billion in excess health care in 2009, approximately $830-$846 billion in 2015 dollars (Institute of Medicine Roundtable on Evidence-Based Medicine, 2010).
Uncontrolled increases in healthcare spending reduce federal and state budgets for spending on other social programs. For example, rising Medicaid costs have been linked to decreases in higher-education appropriations across states (Fossett and Burke, 2004, Kane and Orszag, 2003), and some US senators have expressed concerns that healthcare expenditures crowded out their states’ abilities to spend on other priorities (The White House, 2009). Furthermore, mid-year state budget adjustments show that states expand health care budgets, often at the expense of other social programs. Of the 16 states that increased their budgets at mid-year in fiscal year (FY) 2015, ten states (63%) increased their Medicaid budget, of which five reduced budget allocations in education, public assistance, or transportation (National Association of State Budget Officers, 2015).
This study uses recent experience in California to examine whether rising medical expenditures are plausibly crowding out other social spending, and if so, what the social opportunity cost of that crowd-out might be.
2. Methods
This analysis uses 25 years of fiscal data from the state of California to assess the crowding-out of non-medical social spending by rapidly increasing health care costs. California was chosen because state Proposition 13 and several state laws make raising taxes difficult, thereby creating a firm budget cap. Moreover, California leans heavily Democratic and has become more so over the study period, suggesting that any reduction in non-medical social spending observed during the 25 years studied cannot be attributed to ideological preferences against such spending.
In California the vast majority of K-12 education resources comes from the state, not local districts, and funding for K-12 education is determined by formulas passed by Propositions 98 (1988) and 111 (1990). An approximate result of this very complex statute is that 40% of the general fund must be spent on K-12 education and community colleges. As a result, one would expect that K-12 education spending as a percentage of annual General-Fund expenditures would remain relatively constant throughout the study period.
As medical spending increases nationally, including in California, the state's effective budget cap implies that less must be spent on the other functions of government, particular on those public health and social expenditures outside of K-12 education.
To test these hypotheses, 25 years of California expenditure data — from FY1990 through FY2014 — were reviewed. Data for this analysis were gathered from Schedule 9: Comparative Statement of Expenditures forms, provided by the California Department of Finance. The General Fund is the principal fund for financing state programs. The primary sources of the General Fund are sales and use taxes, income tax, and corporation taxes (State of California). The General Fund does not include Special Funds and Selected Bond Funds that are restricted for specific government functions or activities. The analyses were focused on General Fund expenditures because spending from this source is determined by the Governor and Legislature and is therefore a modifiable policy outcome from one year to the next. All expenditures were adjusted to 2015 dollars.
General-Fund expenditures were categorized into four main categories:
-
•
healthcare (e.g., healthcare services, state hospitals, rehabilitation, etc.)
-
•
K-12 education
-
•
public health and other social spending; and
-
•
all other expenditures, including corrections and rehabilitation (excluding prison healthcare)
Other social spending included higher-education expenditures, spending on social services, child support services, housing and community development, and so on.
3. Results
Consistent with expectations, public spending in California was relatively flat during this period. From 1990 to 2014, real per-capita spending rose modestly from $2340 to $2880, which represented a large decrease from 9.1% of state GDP to just 4.8%. Also as predicted, spending on K-12 education was well protected, increasing its share of the budget from 37.5% to 42.2%, and hovering very close to 40% for all but the first 2 and last 2 years (See Fig. 1).
Fig. 1.
Non-federal California state spending by category over time. Categories are mutually exclusive and collectively exhaustive.
As shown in Fig. 1, the proportion of the state budget spent on health care increased by 50% from 14.1% to 21.3% over the study period. The largest part of this spending was for Medicaid and other medical benefit payments, 77% of the total in FY2014. Other significant components were for prison healthcare (9.7%), state hospitals (6.6%) and retiree dental benefits (6.4%). Some potentially important components of healthcare spending, such as retiree health benefits, could not be separately identified in the budget. Per capita healthcare spending rapidly increased from $330 in FY1990 to about equal other social spending at $613 in FY2014.
Coincident with the increase in medical spending, the share of other social spending declined from 34.8% in FY1990 to 21.4% in FY2014. Annual per capita spending on non-medical social programs fell from $814 (FY1990) to $616 (FY2014). Taken together, these changes imply that the ratio of social-to-healthcare spending steadily declined from 2.5:1 in FY1990 to almost exactly 1:1 in FY2012 and beyond.
Including K-12 education in the social spending category, we observed that per capita spending on education and other social programs together increased 11.6% from $1,643 in FY1990 to $1,833 in FY2014. Annual per capita spending on healthcare, however, increased 85.8% during the same period. Approximately 70% of General Funds were spent on education and social programs in FY1990 (the highest level throughout the study period). This figure fell to 63.5% in FY2014. Non-medical social spending also decreased as a fraction of state GDP, representing 6.5% of real GDP in FY1990 and only 3.1% of GDP in FY2014. Thus, state investments in education and social programs have not kept pace with increases in healthcare spending during this period.
3.1. Health dividend options
Crowding out social spending limits opportunities to invest in programs that produce high-value and cost-effective outcomes for California. Berwick and Hackbarth (2012) estimate that between 21% and 47% of total healthcare spending are excessive, in that they have no health value (Berwick & Hackbarth, 2012). Applying the low estimate to the proposed $24.9 billion in the California FY2015 budget suggests a potential investible savings of $5.23 billion in fiscal year 2016. This amount represents the opportunity cost of misplaced medical spending, which could be reallocated to improve California's infrastructure, strengthen its workforce, alleviate poverty, and improve population health at no net additional cost (McCullough et al., 2012).
To concretize this opportunity cost, we estimated the health, social welfare, and economic benefits of allocating this $5.23 billion to fund one of three social initiatives in California: 1) funding state tobacco control activities at CDC-recommended levels for 13 years; 2) restoring and expanding the number of high-school counselors in California's public educational system for 10 years; or 3) increasing the number of State Preschool slots for 10 years. One of these 3 proposals could be funded for 10 or 13 years from just one year of reallocated medical spending. Effects on population health, social benefit and net-present economic return are estimated for the several years of funding made possible by one year's reallocation. These 3 interventions were selected to provide a sense of the magnitude and diversity of social and economic benefit that is foregone because of misspent medical costs. Many other evidence-based and high-value programs exist, such as tutoring for English-language learners, family therapy for juvenile offenders or groundwater improvement projects (Washington State Institute for Public Policy, 2015).
Table 1 summarizes the expected benefits of non-medical social programs that can be funded by one year of excess health care spending by the state of California. All three of the illustrative initiatives are cost-effective in the long run, and offer varying impacts on mortality, social outcomes, and economic benefits.
Table 1.
Summary of Expected Returns on Investment for Three Health Dividend Options. One year of excess health care expenditures worth $6.14 billion fully funds programs in each of the sectors below.
| Sector | Social investment | Years funded | Impact on mortality | Other health and social outcomes | Financial return |
|---|---|---|---|---|---|
| Education | Hire 8,443 additional secondary school counselors starting 2016–2017 for 10 years. This would reduce the ratio of students to counselors from 467 to 139. | 10 years | 126 deaths averted annually by 2028 (10 years after initial hires). | 418,000 additional high school graduates by 2028. Graduation rate would increase from 84.3% to 93.7%. | $153-$313 billion lifetime return to society. $81-$104 billion return to government. Benefits include productivity loss averted, and health care, crime, and public assistance costs averted. Benefit to cost ratio=29–60. |
| Public health | Fund comprehensive state tobacco control program at CDC recommended levels ($9.15 per capita) for 13 years (through 2031). | 13 years | 10,500 annual deaths averted in 2028 (end of funding period). | 2.42 percentage point reduction in smoking prevalence from 10.8% in 2014 to 8.4%. (Additional reduction in cigarette consumption per smoker not quantitatively estimated). | $65 billion return to society at end of funding period. Cumulative savings of $11 billion in health care costs from 2016–2028 due to reduction in smoking prevalence & fewer pack years smoked. $2.5 billion savings for CA state in health care costs. Benefit to cost ratio=12.4. |
| Child development | Fund 55,032 additional State Preschool full-day slots for 10 years. This would increase the fraction of income eligible children served from 26% to 35%. | 10 years | 372 deaths averted saved by 2056 (40 years after end of funding period). | 2,036 additional high school graduates per year by 2036-37 (20 years after implementation). Among additional children served by the program, 3.7 percentage point increase in proportion of adults 18–24 with high school degrees. 29% reduction in proportion with less than a high school education. | $25 billion lifetime return to society. $7 billion savings for taxpayers. Benefit to cost ratio=4.8. |
3.1.1. Tobacco prevention and control
California has been a leader in tobacco control and prevention. Since the creation of the state's tobacco control program in 1988, smoking prevalence dropped from 22.7% in 1989 to 12.6% in 2012 (Cox, Barry, Glantz, & Barnes, 2014). However, a recent report by researchers at the UCSF Center for Tobacco Control Research and Education (2014) suggested that California's role as a leader is tenuous due to diminishing revenue for control and prevention (Cox et al., 2014). California is expected to spend $58.9 million on tobacco prevention in FY2015, which represents a small fraction (16.9%) of the $347.9 million recommended by the Centers for Disease Control and Prevention (CDC) (Campaign for Tobacco-Free Kids, 2015).
Exposure to tobacco smoke is responsible for at least 40,000 annual premature deaths and over $13 billion in annual medical care costs in California (Campaign for Tobacco-Free Kids, 2015). By reallocating just one year's worth of $5.23 billion in annual excess health care spending to the state tobacco control program, California can fund prevention and control activities at the CDC-recommended level ($9.15/per capita) for 13 years. Based on an earlier assessment relating per capita expenditures to reductions in smoking (Lightwood and Glantz, 2013), we estimated that funding tobacco control and prevention at the CDC-recommended level would reduce smoking prevalence from 10.8% in 2014 to 8.4% in 2028. Further methodological details about these and the other estimates are available in the Appendix.
To estimate the number of deaths averted due to decreased smoking, age- and sex-specific all-cause mortality risk ratios reported by the Surgeon General (U.S. Surgeon General, 2014) were used to calculate current and projected smoking attributable fractions (SAFs) for men and women ages 35–54, 55–64, 65–74, and 75 and over. These SAFs were then applied to projected numbers of deaths in 2028. It was estimated that a 2.42 percentage-point reduction in smoking prevalence would avert 10,500 annual deaths in that year. Reductions in smoking prevalence and intensity would also save Californians $11 billion in health care costs over 13 years, including $2.5 billion paid for out of public funds.
Using age group-specific values of a statistical life (VSL) (Aldy and Viscusi, 2008), it was estimated that 10,500 averted deaths would be valued at $53.7 billion (2015 dollars). Overall, funding state tobacco prevention and control at the CDC recommended level for 13 years is estimated to generate a return to society (health care savings plus statistical value of deaths averted) of $64.9 billion; the expected social benefit-to-cost ratio is 12:1.
3.1.2. High school guidance counselors
California ranks 31st in the nation in high-school graduation rate with only 84.5% of incoming 9th graders graduating with a degree within four years in the latest data (United Health Foundation, 2014). High-school completion increases lifetime earnings and improves long-term health (Hahn et al., 2015). Increasing the number of high-school graduates also generates substantial economic benefits to the state government and society. Lifetime economic benefits per additional high-school graduate—which include increased productivity, and averted crime, healthcare, and welfare costs—have been estimated to range between $347,000 to $718,000 (Community Preventive Services Task Force, 2015b).
A meta-analysis conducted by the US Community Preventive Services Task Force (Task Force) (2011) concluded that mentoring and counseling programs aimed at increasing high-school completion were effective: Students in high-quality mentoring and counseling programs had 2.6 times greater mean adjusted odds of high-school completion compared to comparison group students (The Guide to Community Preventive Services, 2013, Wilson et al., 2011). High-school completion rates for students who participated in these programs were, on average, 9.4 percentage points greater than high-school completion among students in comparison groups (Community Preventive Services Task Force, 2015b). However, notwithstanding their effectiveness, California lost over 1,000 high-school guidance counselors between 2008 and 2011. As of FY2013, California had 4,173 high school guidance counselors, an average of 467 students to each counselor (U.S. Department of Education et al., 2006–2014). The recommended minimum ratio is 250:1 (American School Counselor Association); high-quality programs often have smaller student-counselor ratios.
One year of excess healthcare expenditures ($5.23 billion) can fund 8,443 additional guidance counselors for ten years. This would reduce the student-to-counselor ratio to 156:1 and facilitate frequent contact between students and counselors, consistent with effective interaction frequency from the evaluation literature. Applying the average effect size of mentoring and counseling on projected high-school completion rates, we estimated an additional cumulative 418,000 students would graduate by the end of the ten-year funding period. The projected graduation rate in California would increase from 84.1% to 93.7% by FY2023.
Previous work estimating the effects of education on health (Galea, TracyHoggatt, Dimaggio, & Karpati, 2011) suggests that an increase in high-school graduation of this magnitude would result in 208 deaths averted at the end of the funding period. The total return to society (societal benefits plus statistical value of deaths averted) is projected to be $153-$313 billion. The value of deaths averted is calculated as above (Aldy and Viscusi, 2008), and contributes $2.7 billion to this total. The expected social benefit-to-cost ratio of this program is between 29 and 60 to 1.
3.1.3. Preschool
The Task Force recommends center-based early childhood education (ECE) as an effective intervention for improving long-term health, educational achievement, and social outcomes (Community Preventive Services Task Force, 2015a). Low-income three- and four-year-old children who participated in center-based ECE programs, on average, had improved test scores, greater high-school graduation rates, and lower rates of grade retention, special-education assignment, teen births, and contact with the juvenile and adult criminal justice systems (Kay and Pennucci, 2014). The Task Force concluded that these programs can narrow achievement gaps and promote health equity (Community Preventive Services Task Force, 2015a).
Created in 2008, the California State Preschool Program (CSPP) provides center-based ECE to three- and four-year old children and is “the largest state-funded preschool program in the nation” (California Department of Education, 2015). CSPP funding fell from $445 million in FY2008 to $374 million in FY2011 but has rebounded in recent years in nominal (not real) dollars (California Child Care Resource & Referral Network, 2008–2014). The 2015 budget agreement created 7,030 additional full-day slots and 2,500 additional part-day slots (Child Care Law Center, 2015). The total number of part-day and full-day CSPP slots in FY2015 (~156,600), however, can only serve 26.5% of all income-eligible three- and four-year-old children in the state, and remains 20% below levels of 2007 (Rock et al., 2015). Because of budget cuts, a statewide waiting list for subsidized child care is no longer maintained; before it was eliminated there were 50,000–70,000 children aged 3 or 4 on the list (Rock et al., 2015).
By reallocating one year's worth of excess healthcare expenditures to CSPP, California can fund 55,032 additional full-day slots (at $9,500/slot/year) for ten years. Providing quality ECE to an additional 55,032 children, who represent 9.3% of income-eligible three- and four-year olds in the state, would increase the number of high-school graduates by 2,036 per year by FY2036, and the proportion of young adults with less than a high-school education would fall 28.7%: from 12.9% to 9.2%. We estimated that increases in high-school graduation would contribute to 372 averted deaths by 2056, 40 years after implementing the program. The program is projected to generate $20.5 billion in lifetime economic benefits from higher labor-market earnings, lower crime, and reduced costs in healthcare, grade retention, and special education, roughly $6.6 billion of which would benefit taxpayers. The total return to society (societal benefits plus statistical value of deaths averted) is estimated to be $25.3 billion; the expected benefit-to-cost ratio is 4.8:1.
4. Discussion
These findings suggest that as spending on medical care in California has increased it has crowded out public health and other social spending. In the context of total state spending that has fallen by almost 50% over 25 years as a proportion of state GDP, medical spending has held its own by increasing its share of the state budget. By contrast, funding on other social programs—including public health and the state functions that contribute most to the social determinants of health—have fallen by two-thirds as a proportion of state GDP.
Given the shifting emphasis away from social spending and public health, one might expect that health outcomes have worsened, at least relative to what they might have otherwise have been. And indeed, evidence suggests that, not only does the US lag other countries in life expectancy despite greater national wealth (National Research Council & Institute of Medicine, 2013), but that increases in life expectancy in the US have been both slow and uneven in recent decades (Chetty et al., 2016). From 1985 to 2010, life expectancy increased by only 3.9 years in the United States, substantially less than the average increase in other developed countries, which was 6.2 years during this time (Organisation for Economic Co-operation & Development, 2016). California beat the US national average, achieving a 5.3 year increase (Institute for Health Metrics and Evaluation, 1985–2010), but this was still nearly a full year less than the average of peer countries. (Only one state--New York--achieved an average increase in life expectancy on par with peer countries). All in all, the evidence suggests that both in California and in the US as a whole, health outcomes have deteriorated relative to what they could have been during this period.
Some have argued that resources for healthcare and other social spending originate from distinct sources, and that it makes no sense to compare spending across categories. Yet, as Emanuel and Fuchs (2008) have argued, such claims are misperceptions that distort important policy discussions (Emanuel & Fuchs, 2008). Governments pay for increases in healthcare costs by taxing, borrowing, or, most commonly, reducing services from other sectors (Emanuel and Fuchs, 2008, Fossett and Burke, 2004). This analysis shows that in California, public health and other non-medical social spending declined as healthcare spending increased, and no surprise: a persistent reluctance to raise taxes, even in a state government controlled entirely by Democrats, imposes a firm cap on total expenditures.
Increasing medical spending also creates challenging political constraints. In 2009 Republicans complained that there had been a 40% increase in state funding in the previous 6 years, and rhetorically asked voters what they had to show for it (Devore, 2009). The number itself was wildly off, but their sophistry contained a kernel of truth: voters were being asked to pay more for medical care for poor people, current and retired state employees, and those in long-term care facilities. Given that Medi-Cal enrollment was flat over this period, the cost increases were almost entirely attributable to increasing cost of service, not greater coverage: most voters could not see the benefits (Tatum, 2014).
Yet while economists debate how much, if any, medical benefit is purchased with each annual increase in expenditures, this much is clear: population health is not improving as fast as it could. During the period analyzed here, 1990–2014, US performance in life expectancy worsened relative to other OECD countries. In 1990, US life expectancy at birth (75.3) was in the broad middle of the pack (Organisation for Economic Co-operation and Development, 2016). US life expectancy (76.7) had fallen to the bottom quartile by 2000, continued to fall in ranking through 2014 (78.9), and fell by 0.1 years the following year (Organisation for Economic Co-operation and Development, 2016, Xu et al., 2016).
The analysis here has important limitations. Many of the policy decisions that would help to constrain unnecessary medical spending lie outside of the control of the California State government. Some, like a law compelling price transparency for pharmaceuticals and medical procedures, are within relatively easy political reach for the state legislature. Although price transparency—in which the public has a right to know the prices paid for medical services—is not a panacea, it is also a necessary first step in any reasonable cost-control measure. Most states have received a grade of “F” in price transparency by an independent watchdog group, but 6 states do better, including 3—Colorado, Maine, and New Hampshire—who get an “A” (Brantes & Delbanco, 2016). At the same time, more meaningful action on prices may require active negotiation by the Federal Government over pharmaceutical prices in Medicare and Medicaid, which is currently barred by law. Better aligning physician compensation with the health benefit of services provided would require reform of the Resource-Based Relative Value Scale Updating Committee, a logistically easy though politically challenging administrative fix at the Federal level (Laugesen, 2014). The experience of the VA suggests that there is also room for competitive pricing in the procurement of medical devices and other supplies (Coulam, Feldman, & Dowd, 2011). California can take meaningful steps to restrain or reverse excessive prices and administrative costs in medical care, but it is limited in what it can achieve on its own.
Even if California were to achieve a significant reduction in the cost of the medical care it pays for, it isn’t clear that this money would be reallocated to social spending and public health. The analysis here suggests that increases in medical spending have co-occurred with decreases in social and public health spending, but this analysis cannot demonstrate causality nor guarantee reversibility.
Although not the focus of this analysis, there is clearly uncertainty around the potential healthcare savings and effectiveness of the educational and public-health interventions modeled here. The point of this analysis is to provide a point estimate of the tradeoffs of high medical spending with spending in social and public health areas. Healthcare waste (e.g., overtreatment, pricing failures, and administrative complexity, etc.) represents 21% to 47% total healthcare spending in the United States. In the absence of state-specific estimates, we applied the lowest percentage to California's healthcare budget but recognize that identifying healthcare savings is a more complicated task. We also acknowledge that point estimates reported in this study do not reflect secondary effects of social investments that impact other areas. For example, investing in additional preschool slots can reduce smoking risks and generate additional savings for the state (D’Onise, Lynch, & McDermott, 2011). Point estimates, therefore, may underestimate the true impact of investing in these programs.
Because testing specific hypotheses is beyond the scope of this study, confidence intervals and p-values are not reported. The evaluation literature on which this analysis rests reports confidence intervals and sources of uncertainty. The citations provided, and in particular high-level evidence reviews such as the Community Guide (Crosby, 2005), the Washington State Institute for Public Policy (Washington State Institute for Public Policy, 2015), and others provide helpful points of entry into this rich literature.
It should be noted that three initiatives highlighted in this paper (i.e., preschool, high school guidance counselors, and tobacco prevention and control) are evidence-based interventions that have been shown to generate health, social, and economic benefits to participants and society. As in healthcare, not all spending on social services produces the intended benefits and is cost-effective. This paper presents the potential gains of shifting spending from low-value activities to high-value interventions. It demonstrates that high-value investments can be found in public health, early childhood education, and other sectors, but does not advocate for categorical spending shifts from one sector to another without evidence on the relative effectiveness and costs of programs (Homer,Hirsch, & Fisher, 2016; Woolf & Aron, 2016).
Several previous papers have documented the costs of wasteful medical spending in dollar terms. The objective of this paper is to begin a process of expressing the costs of wasteful medical spending in human terms—the implicit effects on the smokers who do not quit and on the high-school students who drop out. Perhaps if these costs were better understood in these human terms, it would be less commonplace for policy-makers to shrug off the nearly trillion dollars in wasteful spending every year.
The levels of healthcare spending by states and the US are a result of specific policy choices (Zimmerman, 2013). They reflect decisions not to negotiate over the price of pharmaceuticals, to avoid price transparency, and to prohibit the use of cost-effectiveness analyses in health priority setting. These decisions—and many others—impact the cost of medical care in the US Average prices for patented drugs in other industrialized countries were less than 40% of those in the US in 2007 (the price gap was greater for drugs classified as “essential” for each country's population) (Schweitzer & Comanor, 2011); the US spends far more for specialty physician services relative to other countries (Laugesen & Glied, 2011); and the US fails to capture market-based efficiencies from a standard benefits packages—a change that by itself has been estimated to save the US $200 billion annually (McGinnis, 2010). California’s experience demonstrates that these policy choices have consequences, including for the public’s health. Voters are sometimes castigated for their unwillingness to accept that political decisions have consequences. But the blame cannot be laid all at the feet of the voters. Experts can help them by better articulating and explaining the consequences of alternative policy choices.
It lies beyond the scope of this paper to prescribe approaches to limiting wasteful medical spending, but three ideas, briefly sketched, indicate the range of possibilities. First, California could request a waiver to allow it to negotiate pharmaceutical prices. A second idea would be for the state to more aggressively expand programs that address the upstream determinants of health, and have been shown to more than pay for themselves in terms of reduced Medicaid expenditures. For example, both asthma home remediation and cognitive behavior therapy have been shown to generate more savings to local and state government than they cost to administer. In essence, this idea would involve borrowing from future returns of social investments to make those investments today. Third, California could directly control prices more effectively, for example by adapting Maryland's All-Payer model, which, recently strengthened, is now estimated to save that state $300 million over the next 5 years (Centers for Medicare and Medicaid Services, 2015a). Combining aspects of these ideas, one simulation has found that healthcare costs could be realistically be reduced by 15% over 25 years (Homer et al., 2016). Progress takes time and requires political effort, but a payoff like this is both achievable and dramatic.
5. Conclusions
Reducing waste and unnecessary cost increases in the US healthcare system is politically difficult. Yet precisely for this reason it is essential to be clear-eyed about the costs of doing nothing. Making progress politically will require an energized coalition of those who could benefit from change and all who care about good governance. Creating this energy requires careful articulation of the true opportunity costs of unnecessary medical spending.
Footnotes
Supplementary data associated with this article can be found in the online version at doi:10.1016/j.ssmph.2017.01.004.
Contributor Information
Linda Diem Tran, Email: Diem.tl@gmail.com.
Frederick J. Zimmerman, Email: fredzimmerman@ucla.edu.
Jonathan E. Fielding, Email: jfieldin@ucla.edu.
Appendix A. Supplementary material
Supplementary material
References
- Aldy J.E., Viscusi W.K. Adjusting the value of a statistical life for age and cohort effects. Review of Economics and Statistics. 2008;90:573–581. [Google Scholar]
- American School Counselor Association, The role of the professional school counselor. In A.S.C. Association (Ed.). Alexandria, VA.
- Avendano M., Kawachi I. Why do Americans have shorter life expectancy and worse health than do people in other high-income countries? Annual Review of Public Health. 2014;35:307–325. doi: 10.1146/annurev-publhealth-032013-182411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berwick D.M., Hackbarth A.D. Eliminating waste in US health care. JAMA. 2012;307:1513–1516. doi: 10.1001/jama.2012.362. [DOI] [PubMed] [Google Scholar]
- Bezruchka S. The Hurrider I Go the Behinder I Get: The deteriorating international ranking of US health status. Annual Review of Public Health. 2012;33(33) doi: 10.1146/annurev-publhealth-031811-124649. (157-+) [DOI] [PubMed] [Google Scholar]
- Bradley E.H., Canavan M., Rogan E., Talbert-Slagle K., Ndumele C., Taylor L. Variation in health outcomes: the role of spending on social services, public health, and health care, 2000–09. Health Affairs. 2016;35:760–768. doi: 10.1377/hlthaff.2015.0814. [DOI] [PubMed] [Google Scholar]
- Bradley, E.H., Canavan, M., Rogan, E., Talbert-Slagle, K., Taylor, L., Ndumele, C., et al. (2015). State variation in health and social spending and impact on health. Academy health annual research meeting. Minneapolis, MN
- Bradley E.H., Elkins B.R., Herrin J., Elbel B. Health and social services expenditures: Associations with health outcomes. BMJ Quality Safety. 2011;20:826–831. doi: 10.1136/bmjqs.2010.048363. [DOI] [PubMed] [Google Scholar]
- Brantes, F.d., Delbanco, S., 2016. Report card on state price transparency laws. Newtown, CT: Health Care Incentives Improvement Institute.
- California Child Care Resource & Referral Network (2008–2014). Child care funding allocations 2008–2013 Fiscal Years (in millions).
- California Department of Education (2015). Child care and development programs. Sacramento, CA: 〈http://www.cde.ca.gov/sp/cd/op/cdprograms.asp〉 Accessed 05.12.15.
- Campaign for Tobacco-Free Kids, 2015. Broken promises to our children: A state-by-state look at the 1998 state tobacco settlement 17 years later.
- Carlson D., Haveman R., Kaplan T., Wolfe B. The benefits and costs of the Section 8 housing subsidy program: A framework and estimates of first-year effects. Journal of Policy Analysis and Management. 2011;30:233–255. [Google Scholar]
- Centers for Medicare & Medicaid Services, 2015a. Maryland all-payer model. Innovation models. Baltimore, MD: Centers for Medicare & Medicaid Services. 〈https://innovation.cms.gov/initiatives/Maryland-All-Payer-Model/〉 Accessed 13.12.16
- Centers for Medicare & Medicaid Services . Centers for Medicare & Medicaid Services; Baltimore, MD: 2015. National health expenditures 2015 highlights. [Google Scholar]
- Chetty R., Stepner M., Abraham S., Lin S., Scuderi B., Turner N. The association between income and life expectancy in the United States, 2001–2014. JAMA. 2016;315:1750–1766. doi: 10.1001/jama.2016.4226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Child Care Law Center, 2015. Analysis of child care provisions in the california state budget for Fiscal Year (FY) 2015-2016. Child Care Law Center.
- Community Preventive Services Task Force, 2015a. Health equity: Center-based early childhood education. Atlanta, GA: The Community Guide. 〈https://www.thecommunityguide.org/findings/promoting-health-equity-through-education-programs-and-policies-center-based-early-childhood〉 Accessed 08.06.15.
- Community Preventive Services Task Force, 2015b. Promoting health equity through education programs and policies: High school completion programs. The community guide. Atlanta, GA: Centers for Disease Control and Prevention. 〈http://www.thecommunityguide.org/healthequity/education/highschoolcompletion.html〉 Accessed 01.06.15.
- Coulam R.F., Feldman R.D., Dowd B.E. Competitive pricing and the challenge of cost control in medicare. Journal of health politics, policy and law. 2011;36:649–689. doi: 10.1215/03616878-1334677. [DOI] [PubMed] [Google Scholar]
- Cox, E., Barry, R., Glantz, S.A., & Barnes, R.L. (2014). Tobacco control in California, 2007–2014: A resurgent tobacco industry while inflation erodes the california tobacco control program
- Crosby R.A. The guide to community preventive services: What works to promote health? Task force on community preventive services. American Journal of Preventive Medicine. 2005;28:305–306. [Google Scholar]
- Devore, C., 2009. Huge tax increases are roiling California GOP. Human Events. Eagle Publishing.
- D’Onise K., Lynch J.W., McDermott R.A. Can attending preschool reduce the risk of tobacco smoking in adulthood? The effects of Kindergarten Union participation in South Australia. Journal of Epidemiology Community Health. 2011;65:1111–1117. doi: 10.1136/jech.2009.101840. [DOI] [PubMed] [Google Scholar]
- Emanuel E.J., Fuchs V.R. Who really pays for health care? The myth of “shared responsibility”. Jama. 2008;299:1057. doi: 10.1001/jama.299.9.1057. [DOI] [PubMed] [Google Scholar]
- Fisher E.S., Wennberg D.E., Stukel T.A., Gottlieb D.J., Lucas F.L., Pinder E.L. The implications of regional variations in Medicare spending. Part 1: The content, quality, and accessibility of care. Annals of Internal Medicine. 2003;138:273–287. doi: 10.7326/0003-4819-138-4-200302180-00006. [DOI] [PubMed] [Google Scholar]
- Fisher E.S., Wennberg D.E., Stukel T.A., Gottlieb D.J., Lucas F.L., Pinder E.L. The implications of regional variations in Medicare spending. Part 2: Health outcomes and satisfaction with care. Annals of Internal Medicine. 2003;138:288–298. doi: 10.7326/0003-4819-138-4-200302180-00007. [DOI] [PubMed] [Google Scholar]
- Fossett J.W., Burke C.E. Rockefeller Institute of Government; Albany, NY: 2004. Medicaid and state budgets in FY 2004: Why medicaid is so hard to cut. [Google Scholar]
- Fuchs V.R., Milstein A. The $640 billion question: Why does cost-effective care diffuse so slowly? New England Journal of Medicine. 2011;364:1985–1987. doi: 10.1056/NEJMp1104675. [DOI] [PubMed] [Google Scholar]
- Galea S., Tracy M., Hoggatt K.J., Dimaggio C., Karpati A. Estimated deaths attributable to social factors in the United States. American Journal of Public Health. 2011;101:1456–1465. doi: 10.2105/AJPH.2010.300086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallivan F., Ang-Olson J., Liban C., Kusumoto A. Cost-effective approaches to reduce greenhouse gas emissions through public transportation in Los Angeles, California. Transportation Research Record: Journal of the Transportation Research Board. 2011;2217:19–29. [Google Scholar]
- Hahn R.A., Knopf J.A., Wilson S.J., Truman B.I., Milstein B., Johnson R.L. Programs to increase high school completion: A community guide systematic health equity review. American Journal of Preventive Medicine. 2015;48:599–608. doi: 10.1016/j.amepre.2014.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Homer, J., 2016. Rethinking the Bradley Ratio. Investment & Financing, Strategy. Cambridge, MA: ReThink Health. http://www.rethinkhealth.org/the-rethinkers-blog/rethinking-the-bradley-ratio/ (accessed December 10, 2016).
- Homer J., Milstein B., Hirsch G.B., Fisher E.S. Combined regional investments could substantially enhance health system performance and be financially affordable. Health Affects (Millwood) 2016;35:1435–1443. doi: 10.1377/hlthaff.2015.1043. [DOI] [PubMed] [Google Scholar]
- Institute for Health Metrics and Evaluation, 1985–2010. Life expectancy, obesity, and physical activity.In IHME_county_data_LifeExpectancy_Obesity_PhysicalActivity_CALIFORNIA (Ed.). Seattle, WA: Institute for Health Metrics and Evaluation. http://www.healthdata.org/us-health/data-download Accessed 12.12.16.
- Institute of Medicine Roundtable on Evidence-Based Medicine . In: The healthcare imperative: Lowering costs and improving outcomes: Workshop series summary. Yong P., Saunders R., Olsen L., editors. The National Academies Press; Washington, DC: 2010. [PubMed] [Google Scholar]
- Kane T., Orszag P. The Brookings Institution; Washington, DC: 2003. Funding restrictions at Public Universities: Effects and policy implications. [Google Scholar]
- Kangas O. One hundred years of money, welfare and death: Mortality, economic growth and the development of the welfare state in 17 OECD countries 1990–2000. International Journal of Social Welfare. 2010;19:S42–S59. [Google Scholar]
- Kay, N., Pennucci, A., 2014. Early childhood education for low-income students: A review of the evidence and benefit-cost analysis. Olympia, WA: Washington State Institute for Public Policy.
- Laugesen M.J. The resource-based relative value scale and physician reimbursement policy. CHEST Journal. 2014;146:1413–1419. doi: 10.1378/chest.13-2367. [DOI] [PubMed] [Google Scholar]
- Laugesen M.J., Glied S.A. Higher fees paid to US physicians drive higher spending for physician services compared to other countries. Health Affairs. 2011;30:1647–1656. doi: 10.1377/hlthaff.2010.0204. [DOI] [PubMed] [Google Scholar]
- Lightwood J., Glantz S.A. The effect of the California tobacco control program on smoking prevalence, cigarette consumption, and healthcare costs: 1989–2008. PLoS One. 2013;8:e47145. doi: 10.1371/journal.pone.0047145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCullough J.C., Zimmerman F.J., Fielding J.E., Teutsch S.M. A health dividend for America: The opportunity cost of excess medical expenditures. American Journal of Preventive Medicine. 2012;43:650–654. doi: 10.1016/j.amepre.2012.08.013. [DOI] [PubMed] [Google Scholar]
- McDonough J.E. Shorter lives and poorer health on the campaign trail. American Journal of Public Health. 2016;106:395–397. doi: 10.2105/AJPH.2016.303069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGinnis M. Taking stock: Numbers and policies. In: Yong P., Saunders R., Olsen L., editors. The healthcare imperative: Lowering costs and improving outcomes: Workshop series summary. The National Academies Press; Washington, DC: 2010. pp. 585–589. [PubMed] [Google Scholar]
- National Association of State Budget Officers, 2015. Table 10. Fiscal 2015 mid-year program area adjustments by value (Millions). In T.F.S.o.S.-S. 2015 (Ed.). Washington, DC: National Association of State Budget Officers.
- U.S. Surgeon General, 2014. The Health Consequences of Smoking---50 Years of Progress: A Report of the Surgeon General. Rockville, MD: Public Health Service, U.S. Department of Health and Human Services
- National Research Council and Institute of Medicine . National Academy of Sciences; Washington, DC: 2013. U.S. health in international perspective: Shorter lives poorer health. [PubMed] [Google Scholar]
- Organisation for Economic Co-operation and Development (2015). OECD.Stat. 〈http://stats.oecd.org/index.aspx?DataSetCode=HEALTH_STAT〉 Accessed 03.07.15.
- Organisation for Economic Co-operation and Development, 2016. OECD.Stat - Life expectancy: Total population at birth. Health status dataset. 〈http://stats.oecd.org/Index.aspx?datasetcode=SOCX_AGG〉 Accessed 12.12.16.
- Reynolds A.J., Magnuson K.A., Ou S.-R. Preschool-to-third grade programs and practices: A review of research. Children and Youth Services Review. 2010;32:1121–1131. doi: 10.1016/j.childyouth.2009.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rock, L., Crow, S., Pham, H.V., 2015. Baby steps: Recession cuts, restoration, and what’s next for California’s child care system. San Francisco: Next Generation.
- Rosenthal J.A., Lu X., Cram P. Availability of consumer prices from US hospitals for a common surgical procedure. JAMA Intern Med. 2013;173:427–432. doi: 10.1001/jamainternmed.2013.460. [DOI] [PubMed] [Google Scholar]
- Rothberg M.B., Cohen J., Lindenauer P., Maselli J., Auerbach A. Little evidence of correlation between growth in health care spending and reduced mortality. Health Affairs. 2010;29:1523–1531. doi: 10.1377/hlthaff.2009.0287. [DOI] [PubMed] [Google Scholar]
- Schweitzer S.O., Comanor W.S. Prices of pharmaceuticals in poor countries are much lower than in wealthy Countries. Health Affairs. 2011;30:1553–1561. doi: 10.1377/hlthaff.2009.0923. [DOI] [PubMed] [Google Scholar]
- Squires, D. (2012). Explaining high health care spending in the United States: An international comparison of supply, utilization, prices, and quality. New York: The Commonwealth Fund. State of California, D.o.F., Finance Glossary of Accounting and Budgeting Terms Sacramento, CA
- Stuckler D., Basu S., McKee M. Budget crises, health, and social welfare programmes. BMJ. 2010;340:c3311. doi: 10.1136/bmj.c3311. [DOI] [PubMed] [Google Scholar]
- Tatum, A., 2014. Healthcare – unsustainable California: The top 10 issues facing the golden state. Stanford, CA: United States Common Sense.
- The Guide to Community Preventive Services, 2013. Promoting health equity through education programs and policies: High school completion programs. 〈http://www.thecommunityguide.org/healthequity/education/highschoolcompletion.html〉 Accessed 6.20.16.
- The White House (2009). . Fiscal Responsibility Summit. Washington, DC
- Tsemberis S. Housing First: Ending homelessness, promoting recovery and reducing costs. How to house the homeless. 2010:37–56. [Google Scholar]
- United Health Foundation (2014). America’s health rankings. United Health Foundation 〈http://www.americashealthrankings.org/CA/Graduation〉 Accessed 06.07.15.
- U.S. Department of Education, National Center for Education Statistics, & Common Core of Data (CCD), 2006-2014. State nonfiscal public Elementary/Secondary Education Survey. Washington, DC.
- Washington State Institute for Public Policy, 2015. Benefit-cost results. Olympia, WA: Washington State Institute for Public Policy. http://www.wsipp.wa.gov/BenefitCost Accessed 04.05.15.
- Wennberg J.E., Fisher E.S., Skinner J.S. Geography and the debate over Medicare reform. Health Aff (Millwood) Suppl Web Exclusives. 2002 doi: 10.1377/hlthaff.w2.96. (W96-114) [DOI] [PubMed] [Google Scholar]
- White C. Health care spending growth: How different is the United States from the rest of the OECD? Health Affairs. 2007;26:154–161. doi: 10.1377/hlthaff.26.1.154. [DOI] [PubMed] [Google Scholar]
- Wilson, S.J., Lipsey, M., Tanner-Smith, E., Huang, C.H., Steinka-Fry, K.T., 2011. Dropout prevention and intervention programs: Effects on school completion and dropout among school-aged children and youth: A systematic review.
- Woolf, S., Aron, L., 2016. The U.S. Health disadvantage and the role of spending. Health affairs blog. Bethesda, MD: Project HOPE.
- Xu, J., Murphy, S.L., Kochanek, K.D., Arias, E., 2016. Mortality in the United States, 2015. Hyattsville, MD: National Center for Health Statistics.
- Young P.L., Olsen L. The National Academies Press, Institute of Medicine; Washington: 2010. The healthcare imperative: Lowering costs and improving outcomes. [PubMed] [Google Scholar]
- Zimmerman F.J. Habit, custom, and power: A multi-level theory of population health. Soc Sci Med. 2013;80:47–56. doi: 10.1016/j.socscimed.2012.12.029. [DOI] [PubMed] [Google Scholar]
- Zimmerman S.L. State-level public policy as a predictor of individual and family well-being. Women Health. 1987;12:161–188. doi: 10.1300/j013v12n03_09. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material