Abstract
We examined the relationship between race-specific rural mortality and the health infrastructure of rural counties in light of America’s recent emergence of a rural mortality penalty. Using the Compressed Mortality File from National Center for Health Statistics (2008–2012) and county-level demographic, socioeconomic, and health care indicators from the Area Health Resource File and the US Census, we created a rural public health infrastructure index which encompasses four types of health care access (public health employees, critical access hospital/rural referral centers, rural health clinics, and emergency departments) within counties. We found that each unit increase in the index is associated with a decline in rural Black mortality, but is associated with an increase in rural White mortality. Policymakers could benefit from focusing on the declining rate of mortality improvement in many rural regions, specifically by trying to better understand how decisions concerning public health spending may influence mortality differently for Black and White residents.
Abbreviations: CAH, critical access hospitals; MSA, metropolitan statistical area; PCMH, patient centered medical home; RUCCs, rural-urban continuum codes
Keywords: Rural mortality penalty, Race-specific mortality, Spatial mortality disparities, Health infrastructure
Highlights
-
•
For the last 25 years, a rural mortality penalty has existed for Blacks and Whites.
-
•
The gap between rural and urban mortality for Black and White residents is growing.
-
•
Public health infrastructure is associated with rural Black and White mortality.
-
•
The role of rural public health infrastructure differs for residents by race.
1. Introduction
Research across the last decade indicates that there was a new trend in macro-level rural-urban mortality in the United States (Cosby et al., 2008; Cossman, James, Cosby, & Cossman, 2010; James & Cossman, 2016). Specifically, many have found that the county-level age-adjusted mortality rates from the last 50 years showed a reversal in the divergence between urban and rural mortality rates. That is, historically, there was an urban mortality penalty—people who lived and died in urban areas had higher mortality rates than those who lived and died in rural areas. In the mid-1980s this trend reversed and now people who live and die in rural areas have higher mortality rates than those who live and die in urban areas. This relationship is also reflected in nascent research on life expectancy (Singh & Siahpush, 2014b), education (Sasson, 2016), and income (Chetty et al., 2016).
The urban mortality penalty arose in the Industrial Revolution and persisted through the 19th and 20th centuries (Haines, 2001) mostly due to infectious and contagious diseases (Omran, 1971, Saloman and Murray, 2002), water quality (Cutler & Miller, 2005), and the poor sewage treatment (Condran & Crimmins-Gardner, 1978) in densely populated (Higgs and Booth, 1979, Preston and Haines, 1991) urban areas. Twentieth century improvements in public health (Higgs and Booth, 1979, Preston and Haines, 1991) reduced mortality rates substantially and resulted in a 50% growth in life expectancy (Smith & Bradshaw, 2006), essentially removing the urban mortality penalty by the late 1940s.
Throughout the middle and latter part of the 20th century, there was no discernible mortality disparity between rural and urban America until the 1980s when the rural mortality penalty emerged. Cossman et al. (2007) showed that there are persistent clusters of mortality in the United States with largely rural areas indicating consistently higher mortality throughout the late 20th century. Additionally, Cossman et al. (2010) found that the rural mortality penalty accounted for 40,201 additional deaths among nonmetropolitan residents in 2005; deaths that could have been avoided if there were no disparities in mortality rates between rural and urban residents. Cossman et al. (2010) anticipated a projected increase in excess deaths through 2015 with heart disease and cancer contributing to about half of them in nonmetropolitan counties. Singh and Siahpush (2014a) also illustrated that mortality rates increased as levels of rurality increased even when controlling for poverty. The gap in mortality rates widened between 1990 and 2009 for all-cause mortality and between 1990 and 2007 for cause-specific mortality, particularly for cardiovascular diseases, certain cancers, chronic obstructive pulmonary disease, diabetes, pneumonia/influenza, nephritis, liver cirrhosis, sudden infant death syndrome, and suicide (Singh & Siahpush, 2014a). Similarly, the gap in life expectancy between rural and urban residents widened between 1969 and 2009, driven by larger increases in life expectancy of metropolitan residents (Singh & Siahpush, 2014b). Evidence of lower life expectancy and higher mortality rates are not the only signs of health disparities between rural and urban areas.
Rural America’s lower life expectancy and higher mortality rates also coincide with a myriad of health related problems. For example, Miller (2011) pointed out a lack of sufficient doctors, dentists, and other health care professionals, and Bauerlein (2014) highlighted the increasing number of rural hospital closures. In fact, “access to quality health services” was selected as the number one health priority according to the Rural Health People 2020 survey respondents (Bolin et al., 2015). Further, nonmetropolitan residents had greater odds of self-reporting fair or poor (vs. good, very good, or excellent) health than metropolitan residents, a disparity that grows with the degree of rurality (across five categories) (Monnat & Pickett, 2011). Smoking status also increases with degree of rurality; for example, in 2012 15.4% of large metropolitan statistical area (MSA) residents, 19.5% of small MSA residents, and 25.6% of non-MSA residents were current smokers with a greater number of non-MSA residents being “every-day smokers” (Blackwell, Lucas, & Clarke, 2014). Singh and Siahpush (2014a) noted a similar pattern in 2010 along with a complementary increase of lung cancers in non-metropolitan areas (Singh, Siahpush, & Williams, 2012). There is also a significant difference in obesity between rural and urban residents where 39.6% of rural residents had a body mass index greater than or equal to 30 while the same was true for 33.4% of urban residents (Befort, Nazir, & Perri, 2012). Even after controlling for “sociodemographic, physical activity, and diet variables,” the significantly greater prevalence of obesity in rural areas still held (Befort et al., 2012, p. 394). Each of these studies demonstrates the poor health services and outcomes for rural residents; however, there are also racial disparities indicating that Black rural residents are even worse off than their White counterparts.
Poor rural Blacks have the highest mortality rates in the nation (Singh & Siahpush, 2014a). Murray et al., 2005, Murray et al., 2006 also note that there are regional variations in life expectancy, mortality, health care utilization, and insurance that are largely rooted in race, population density, and race-specific socioeconomics. Rural Blacks ranked their health as fair or poor more often than rural Whites or Hispanics or urban Blacks, Whites, or Hispanics, and they also note that education, health insurance, and income above or below the federal poverty level contribute greatly to rural-urban mortality disparities (Probst, Bellinger, Walsemann, Hardin, & Glover, 2011). Recent work by Case and Deaton (2015) indicates increasing mortality among those who are lower educated; however, Snyder (2016) replied to this research by noting that education varies by rural-urban location (e.g., Provasnik et al., 2007) and that many of the trends Case and Deaton (2015) studied need to be examined at smaller areas of geography. Other research found that basic measures of health care infrastructure vary in their effect on mortality across rural sub-regions (i.e., in some regions health care improves mortality and in others social and economic factors are stronger predictors of death) (James, 2014). In a follow-up study exploring racial differences in health care infrastructure and mortality, measures of primary care in rural America are beneficial for White rural mortality, but not for Black rural mortality (James & Cossman, 2016). This begs the question, if typical measures of health care – e.g., primary care physicians, emergency department availability, etc. – do not significantly help the health of the worst off population, what does? We explore the role of public health infrastructure in rural America as a potential explanation.
1.1. Addressing rural-urban mortality disparities
Existing work has shown many contributors to rural-urban mortality differentials. Typical measures of rural-urban areas are rooted in the aggregation of rural-urban continuum codes (RUCCs) (Singh and Siahpush, 2002, Hall et al., 2006), and these studies consistently show a relationship between numerous social and economic factors and population health. Poverty (Hartley, 2004, Burton et al., 2013, Pascoe et al., 2016), income (Probst et al., 2011), segregation (Yang & Matthews, 2015), income inequality (USDA, 2013), and the changing economic opportunities (Council of Economic Advisors, 2010) that come with urbanization and suburbanization (Fan & Song, 2009) all influence mortality disparities and the rural mortality penalty more specifically. However, the most prominent explanation of rural health disadvantages is access to care (Kwan, 2016). That is, the argument is typically made that more rural residents cannot as easily access physicians, hospitals, or testing facilities as can urban residents (Arcury et al., 2005, Chan et al., 2006). It is true that rural residents travel farther for primary (Cossman, Ritchie, & Cosby, 2006a) and specialist care (Cossman, Ritchie, & Cosby, 2006b). For those who are chronically ill, this can combine to a substantial amount of travel for coordinated care (Winters, 2013).
While the Balanced Budget Act of 1997 (US Senate, 1997) tried to rectify some of these disparities with the acknowledgement that rural hospitals need assistance to stay in business, the critical access hospitals (CAH) developed under this bill continue to struggle (Rosko and Mutter, 2010, Joynt et al., 2011). There were high numbers of closures of rural hospitals in the 1980s and 1990s, and we are now seeing a resurgence in CAH closures following the passage and implementation of the Affordable Care Act (Kaufman et al., 2016). Rural referral centers have also been identified and subsidized as high volume acute care rural hospitals that treat a large number of acute cases (HRSA, 2016), particularly for those who are low income. A third component to rural health care comes from rural health clinics, which are federally qualified health clinics certified to receive specialty Medicare and Medicaid reimbursement, improving access to care in rural areas by using non-physicians such as nurse practitioners and physician’s assistants (HRSA, 2006). Lastly, emergency departments are frequently used centers of care in rural places (Baskin, Baker, Bryan, Young, & Powell-Young, 2015).
This patchwork quilt of rural health care has appeared to assuage some of the pressures for rural health care; however, given that rural Black mortality rates are higher than rural White mortality rates (Yang, Jensen, & Haran, 2011; James, 2014; James & Cossman, 2016) perhaps the local public health infrastructure is not equally beneficial across members of different racial groups. It is our contention that this “system” works better for rural Black residents than it does for rural White residents. We know that there are geographic variations in public health spending (Mays & Smith, 2009), but that they exist has not yet been linked to health-related disparities nationwide. Recent studies examined how changes in public health expenditures affected health outcomes, but only in California (Brown, Martinez-Gutierrez, & Navab, 2014) and Georgia (Marton, Sung, & Honore, 2015).
2. Data and methods
Two analyses were conducted. First, descriptive analyses established mortality disparities over time by race and area (urban-rural). Second, ordinary least squares (OLS) multivariable analysis examined factors associated with race-specific mortality rates at one cross-section of time (2008–2012 averaged mortality rates) for rural, urban, and all US counties. We expect the effects of race on mortality are pervasive and would necessitate multiple interaction terms; to facilitate interpretation, we run separate models for White mortality and Black mortality instead.
Mortality data are from the Compressed Mortality File from the National Center for Health Statistics, which tracks county-level mortality in the United States. We used data from 1968–2012 (85,868,225 deaths). The data are all deaths in the US by age group, sex, race, county of death, and cause of death (ICD-8, 9, and 10 codes) (NCHS, 2010). Denominators were calculated using US Census estimates of resident populations ([dataset] National Center for Health Statistics, 2000, [dataset] National Center for Health Statistics, 2001, [dataset] National Center for Health Statistics, 2010). Independent cities in Virginia and other states were collapsed into their respective counties.
2.1. Dependent variable
The 2000 Standard Million was used to age-adjust the mortality rates using 11 age categories (younger than 1 year, 1 to 4 years, 5 to 14 years, 15 to 24 years, 25 to 34 years, 35 to 44 years, 45 to 54 years, 55 to 64 years, 65 to 74 years, 75 to 84 years, and 85 years and older). The proportion of each age group of the total population is used as a weight in each region in the age-adjusted mortality rate calculations. Using this method, the urban and rural mortality rates are based on the same standard population distribution, which permits direct comparisons across counties (Siegel & Swanson, 2004). Essentially, this means that the effect of age has been removed from analysis and counties with aging populations can easily be compared with counties with younger populations. Beale codes were used to classify counties as urban or rural as outlined in James (2014). Definitions of urban and rural were taken from Ingram and Franco (2012). Urban classifications (codes 0–3) comprise about 83% of the US population, while rural codes (4–9) comprise about 17% of the total US population (Cromartie & Parker, 2016). White and Black-specific averaged mortality rates for 2008–2012 are used as the dependent variable in the multivariable analysis. Multiple years are averaged together to account for a low number of Black deaths in some US counties. Mortality data from the CDC do not permit longitudinal analyses of other racial or ethnic categories; therefore, we have no distinction available to us for Hispanics, and other minority groups cannot be studied. For example, there are many counties that would not have enough Native Americans and would not experience enough Native American mortality to calculate stable rates.
2.2. Independent variables
County-level demographic, socioeconomic, and health care indicators are used as the independent variables in the OLS multivariable analyses. These early- to mid-2000 variables come from the Area Health Resource File and are from previous years to account for lag (Area Health Resources Files (AHRF), 2014–2015). We lag the independent variables under the assumption that most effects on mortality are long-term and not immediate. For example, if economic inequality increases one’s risk of dying, it does so over the life course and not concurrent with death; as such, a lag in the independent variables is appropriate.
Demographic measures include percent female (2006), percent Black (2006), percent in poverty (2005), percent aged 65 years and older (2006), percent of the county with a college degree (2006), economic inequality (Gini index, 2005), and dummy variables for region (i.e., Northeast, Midwest, West, South (ref)). The primary independent variable is a rural public health infrastructure index. The rural public health infrastructure index is comprised of four types of public health care that are important in rural America, and it is measured on a continuum of zero to three. Each type of public health care is binary, indicating the presence (1) or absence (0) of this type of care in each county. The rural health care measures are: (1) public health employees (1,0), (2) critical access hospital/rural referral center (1,0), (3) rural health clinic (1,0), and (4) emergency department (1,0). If a county has one of these health care options it is given a score of one, if it has two types it is given a score of two, if it has three or more types it is given a score of three. Alternatively, if a county has none of these types of health care it is assigned a score of zero. We focus specifically on the influence of our rural public health infrastructure index in rural counties; however, we also test it separately in urban and all US counties. Analyses were conducted in SPSS 22.0 (IBM, 2013), and the file was split by RUCC designation as well as by race.
3. Results
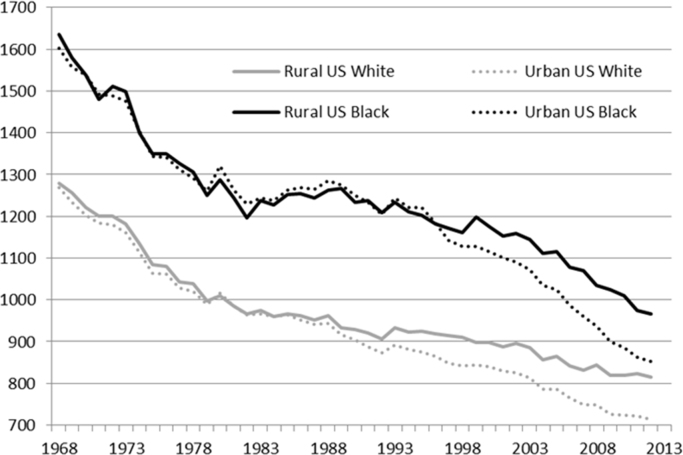
Fig. 1 depicts the descriptive results over time of Black and White mortality in rural and urban America. Clearly, the mortality rates for rural Blacks and Whites are consistently higher than their same-race, urban counterparts, and have been for more than two decades. Additionally, rural Black mortality is more than 150/100,000 deaths higher than that of rural White mortality in recent years. The racial gap is even larger in previous years, peaking at a difference of approximately 300/100,000 from 1987 through 1992. The trend lines in Fig. 1 confirm the large and persistent racial disparity in rural mortality rates in America.
Fig. 1.
Urban-Rural Mortality Rates by Race, 1968–2012.
The second analytical technique is an OLS regression model testing the effects of the rural public health infrastructure index on Black and White-specific mortality from 2008–2012, controlling for basic socioeconomic and demographic factors, for rural, urban, and all US counties. Many interesting results emerge. Table 1 shows the full models for rural counties. The larger the percentage of females in a given county, the higher the mortality rate for Whites; however, this effect is not significant for Blacks. As the percent of Black residents in a rural county increases, White mortality significantly increases while Black mortality significantly decreases. As the percent in poverty increases, mortality for both rural Whites and rural Blacks significantly increases. As the percent of persons age 65+ increases, rural White mortality significantly decreases while rural Black mortality significantly increases. As the percent of those with a college degree increases, rural White mortality decreases, but rural Black mortality is not significantly affected. The Gini index results show a key racial disparity in its effect on mortality. As economic inequality increases, so too does White mortality; however, the relationship is not statistically significant for rural Black mortality. White mortality is significantly higher in the South compared to other census regions, while Black mortality is only significantly lower in the West with no regional difference between the Northeast or Midwest and the South.
Table 1.
OLS Regression of 2008–12 Age-Adjusted Mortality Rates per 100,000 Regressed on Population, Economic, and Health Care Index in Rural US Counties.
| Variable |
Rural White Mortality |
Rural Black Mortality |
||||
|---|---|---|---|---|---|---|
| Unstd. Coeff. (Std. Error) | Std. Coeff. (t-stat.) | Unstd. Coeff. (Std. Error) | Std. Coeff. (t-stat.) | |||
| Constant | 429.651 | – | *** | -432.293 | – | |
| (54.394) | (544.078) | |||||
| Percent Female | 10.347 | 0.159 | 18.184 | 0.043 | ||
| (1.105) | (9.361) | *** | (10.957) | (1.660) | ||
| Percent Black | 0.635 | -0.064 | -4.700 | -0.077 | * | |
| (0.203) | (-3.125) | ** | (1.984) | (-2.369) | ||
| Percent Poverty | 4.189 | 0.192 | *** | 17.302 | 0.119 | *** |
| (0.469) | (8.936) | (4.970) | (3.481) | |||
| Percent Age 65+ | -3.470 | -.094 | *** | 30.501 | 0.108 | *** |
| (0.678) | (-5.119) | (7.748) | (3.937) | |||
| Percent College | -8.869 | -0.345 | *** | 2.151 | 0.013 | |
| (0.478) | (-18.556) | (4.951) | (0.435) | |||
| Gini Index | 99.393 | 0.138 | *** | -144.078 | -0.027 | |
| (12.362) | (8.040) | (141.596) | (-1.018) | |||
| South (ref) | – | – | – | – | ||
| – | – | – | – | |||
| Northeast | -82.010 | -0.118 | *** | -71.156 | -0.017 | |
| (12.219) | (-6.712) | (116.345) | (-0.612) | |||
| Midwest | -101.889 | -0.338 | *** | 28.866 | 0.014 | |
| (6.416) | (-15.881) | (66.787) | (0.432) | |||
| West | -85.663 | -0.211 | *** | -373.086 | -0.123 | *** |
| (8.251) | (-10.382) | (90.577) | (-4.119) | |||
| Rural Public Health | 8.885 | 0.061 | *** | -62.532 | -0.061 | |
| Infrastructure Index | (2.420) | (3.671) | (26.348) | (-2.373) | ** | |
| R-Square | 0.488 | 0.045 | ||||
*.05 level, **.01 level, ***.001 level
The focal point of this work is on the role of rural public health care infrastructure. The rural public health infrastructure index, comprised of four predominant types of health care in rural America, reveals another difference in association with mortality. The rural public health infrastructure index is significantly associated with both rural White and Black mortality; however, the effects are in opposite directions. That is, with each unit increase in the rural public health infrastructure index, Black mortality decreases by 63 deaths per 100,000, but for rural Whites, increases in the rural public health infrastructure index are associated with increased mortality risk. According to Table 2, the rural public health infrastructure index is not significant in models examining White or Black mortality in only urban counties or for White mortality across all US counties; however, it is significant in both rural White and rural Black mortality models (as seen in Table 1) along with all US counties for Black mortality. This evidence further supports our contention that this “system” of rural health care is beneficial for rural Black mortality.
Table 2.
Comparison of Standardized and Unstandardized Rural Health Care Index Coefficients Across Rural, Urban, and U.S. Classifications for White and Black Mortality, 2008–2012.
| Variable | White Mortality, 2008-12 |
|||||
|---|---|---|---|---|---|---|
| RURAL | URBAN | US | ||||
| Rural Public Health Infrastructure Index | Unstd. Coeff. | Std. Coeff. | Unstd. Coeff. | Std. Coeff. | Unstd. Coeff. | Std. Coeff. |
| (Std. Error) | (t-stat.) | (Std. Error) | (t-stat.) | (Std. Error) | (t-stat.) | |
| 8.885 | 0.061 | -4.478 | -0.036 | 0.245 | 0.002 | |
| (2.420) | (3.671) | (2.655) | (-1.687) | (2.069) | (0.119) | |
| Variable | Black Mortality, 2008-12 | |||||
| RURAL | URBAN | US | ||||
| Rural Public Health Infrastructure Index | Unstd. Coeff. | Std. Coeff. | Unstd. Coeff. | Std. Coeff. | Unstd. Coeff. | Std. Coeff. |
| (Std. Error) | (t-stat.) | (Std. Error) | (t-stat.) | (Std. Error) | (t-stat.) | |
| -62.532 | -0.061 | -13.997 | -0.030 | -44.178 | -0.052 | |
| (26.348) | (-2.373) | (15.385) | (-0.910) | (16.996) | (-2.599) | |
Bold coefficients indicate statistical significance at the .05 level or higher.
Perhaps the most interesting finding is that this relatively traditional model of mortality shown in Table 1, which is frequently used to explain White mortality (48.8% of the variance explained), does not explain Black mortality (4.5% of the variance explained). For spatial mortality research to remain a viable area of exploration, researchers must determine how to estimate models that will explain this difference. Why do our models explain rural White mortality, but not rural Black mortality? What is fascinating is that the public health infrastructure indicates improvements in rural Black mortality, but the model is explaining very little variance in rural Black mortality. We have to discern the appropriate measures for identifying differentials within the rural Black population as it pertains to their mortality rates. We have explored segregation and employment variables, but with no improvement in the models. The next step likely is to include health behavior data; however, looking at aggregated individual health behavior and socioeconomic data might not capture the nuances underlying these clearly ecological patterns in rural mortality.
4. Discussion
Overall, the rural mortality penalty has been affecting both Black and White residents for the past twenty-five years; however, rural Blacks have consistently borne the brunt of it. Although urban Blacks showed slightly higher mortality rates than rural Blacks at the onset of the White rural mortality penalty approximately thirty years ago, the gap between rural-urban Blacks has been growing since the Black rural mortality penalty began. The gap between White rural-urban mortality also seems to be widening since the White rural mortality penalty began in the 1980s. Urban Black mortality rates appear to be approaching those of the rural White rates with a sharper decline in urban Black mortality rates and a more modest decline of rural White mortality rates. These widening gaps between rural and urban residents by race coincide with recently reported growing disparities in life expectancy (Singh & Siahpush, 2014b) and all-cause mortality and numerous major causes of death (Singh & Siahpush, 2014a).
The OLS regression models provided several interesting results. First, they showed that as the percent of females in a rural county increases, rural White mortality increases while rural Black mortality is not significantly affected. This finding is consistent with recent research that details the alarming rise in morbidity and mortality, particularly for rural White women (Case & Deaton, 2015). The second finding from the OLS regression model indicates that as the percent of the Black population increases, both White and Black rural mortality change, but rural White mortality increases while rural Black mortality decreases. Third, as poverty increases, both White and Black mortality significantly increase, but rural Black mortality does so at a greater magnitude. Similarly, Singh and Siahpush (2014a) found distinct differences in rural-urban mortality disparities when they analyzed poverty and race together. Poor non-metropolitan Black residents had the highest all-cause and premature mortality rates in their sample (Singh & Siahpush, 2014a). Black residents are less likely to have a regular source of care as well (Litaker, Koroukian, & Love, 2005); in fact, not having a usual source of care was also associated with being uninsured, unemployed, or with incomes placing them at the poor or near-poor poverty level. Fourth, as the percent of those 65 and older increase, rural White mortality decreases while rural Black mortality increases—that is, having an older population in the county is associated with decreased age-adjusted mortality for Whites, but increased age-adjusted mortality for Blacks. While the Black-White mortality crossover literature suggests a decline in mortality risk for older Blacks and an increase for Whites, the age at which this crossover occurs has been increasing since the late 1960s (Masters, 2012); as such, our findings are to be expected for age 65+ while using an age variable such as age 80+ may indicate a crossover effect instead. Fifth, the percent of those in a county with a college degree and a county’s economic inequality matter for rural White mortality, as increases in percent of those with a college degree is associated with decreases in rural White mortality and economic inequality is associated with substantial increases in rural White mortality. At the same time, the percent of those with a college degree and economic inequality do not significantly affect Black mortality either positively or negatively in our model. Deaton and Lubotsky (2003) have investigated this issue and found that the fraction of the population that is Black has more to do with mortality risk than does inequality, consistent with our findings. In cases where inequality does matter, it is often a breakdown of trust and social cohesion in the community (Deaton & Lubotsky, 2003). It is plausible that this is precisely where the unique rural aspect comes into play for Black mortality. Given that the overwhelming proportion of rural America is White, Black rural communities may thrive in the areas of trust and cohesion.
The main interest of this study focuses on the rural public health infrastructure index, which encompasses four types of rural health care access (i.e., public health employees, critical access hospital/rural referral centers, rural health clinics, and emergency departments) within counties. It is our contention that this “system” works better for rural Black residents than it does for rural White residents. This proposition is supported by the results presented in Table 2 showing the lack of significance of the rural public health infrastructure index in only urban counties and for all US counties for Whites while being significant for Whites and Blacks in rural counties and Blacks in all US counties. That each unit increase in the rural public health infrastructure index is associated with a decline in rural Black mortality, but an increase in rural White mortality, points to a difference in the role of public health infrastructure in rural areas by race. If a rural county has three or more indicators it can reduce Black mortality by approximately 200 deaths per 100,000, lowering it to a level comparable to that of White rural mortality. The rural regions with the largest dearth of public health infrastructure are RUCCs 8 and 9, the most remote and least populated counties in the nation. These two RUCC classifications include 659 counties, 26% of which score a zero on the rural public health infrastructure index, and 55% score either a zero or one. Compared with RUCCs 4–7 (1368 counties), only 6% score a zero and 29% score a zero or one on the index, respectively. This provides evidence that the bulk of the access to public health care for rural Black Americans is in these four regions.
4.1. Limitations
We did not take individual- or contextual-level health behaviors such as smoking, drinking, or obesity (diet/exercise) or individual-level socioeconomic variables into account. Future research will need to shift from contextual to individual-level analysis. Another measure that could be included in future work would be the rate of insurance, especially for periods prior to full implementation of the Affordable Care Act. While we combined several public health measures into an index, in the future it may make sense to allow the individual measures to vary in their effect on mortality – to see if the public health infrastructure problem is more focused in some measures than in others. Finally, James (2014) has already shown that there are variations in mortality across rural regions; so future work can take those gradations into account as well.
5. Conclusions
The rural mortality penalty exists for both White and Black-specific mortality rates, but the onset of the Black rural mortality penalty happened nearly 10 years later than the White penalty. This penalty appears to be expanding within both races, starting later for Blacks, but catching up with a faster growth rate. We found that public health infrastructure—or lack thereof—plays a role in how Black and White residents experience rural mortality differently. For rural Blacks, a stronger public health infrastructure is associated with reductions in the likelihood of mortality, while for rural Whites, a stronger public health infrastructure is associated with increases in the likelihood of mortality. For rural Whites access to care also potentially means increased access to opioids, which would not necessarily prove to be positive for long-term health and mortality. One potential caveat is that in areas of the country where there is extreme poverty among Blacks, even the most basic of public health needs are not being met. Blacks who are living in abject poverty may be experiencing poverty at a much more dismal level than Whites who are living in poverty; therefore, the public health infrastructure cannot work as effectively for both racial groups.
Policymakers could likely benefit from focusing on the declining rate of mortality improvement in many rural regions, and specifically trying to better understand how their decisions concerning public health spending may influence rural mortality differently for Black and White residents. Along with the importance of hospitals and/or clinics in rural areas is the implementation of health care technology. Given the shortages of health care in many rural counties, including that of specialist care, innovative methods of delivery such as telemedicine and patient centered medical homes are vital for providing access to cardiologists, psychiatrists, and other doctors that may reside several counties away. Additionally, the Patient Centered Medical Home (PCMH) model of care provides rural residents the opportunity for patient centered care giving them both more agency in maintaining their own health and/or managing chronic disease, and assistance in care coordination.
Conflicts of interest
Authors report no.
Footnotes
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Contributor Information
Jeralynn Cossman, Email: jscossman@mail.wvu.edu.
Wesley James, Email: wljames1@memphis.edu.
Julia Kay Wolf, Email: jkwolf@mix.wvu.edu.
References
- Arcury T.A., Preisser J.S., Gesler W.M., Powers J.M. Access to transportation and health care utilization in a rural region. The Journal of Rural Health. 2005;21(1):31–38. doi: 10.1111/j.1748-0361.2005.tb00059.x. [DOI] [PubMed] [Google Scholar]
- Area Health Resources Files (AHRF). US Department of Health and Human Services, Health Resources and Services Administration, Bureau of Health Workforce, Rockville, MD. 2014–2015.
- Baskin L.W., Baker J.R., Bryan T.L., Young G.Q., Powell-Young Y.M. Rural health and the nonemergency use of emergency medical services. Nursing Clinics of North America. 2015;50(3):613–619. doi: 10.1016/j.cnur.2015.05.014. [DOI] [PubMed] [Google Scholar]
- Bauerlein V. Rural hospitals feel pinch. The Wall Street Journal. 2014 〈http://www.wsj.com/articles/rural-hospitals-feel-pinch-1399852667〉 (May 11) (Retrieved June 21, 2016 from) [Google Scholar]
- Befort C.A., Nazir N., Perri M.G. Prevalence of obesity among adults from rural and urban areas of the United States: Findings from NHANES (2005–2008) The Journal of Rural Health. 2012;28(4):392–397. doi: 10.1111/j.1748-0361.2012.00411.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blackwell, D.L., Lucas, J.W., & Clarke, T.C. (2014). Summary health statistics for U.S. adults: National Health Interview Survey, 2012. National Center for Health Statistics. Vital Health Statistics 10(260). Retrieved June 10, 2016 from 〈http://www.cdc.gov/nchs/data/series/sr_10/sr10_260.pdf〉. [PubMed]
- Bolin J.N., Bellamy G.R., Ferdinand A.O., Vuong A.M., Kash B.A., Schulze A., Helduser J.W. Rural healthy people 2020: New decade, same challenges. The Journal of Rural Health. 2015;31(3):326–333. doi: 10.1111/jrh.12116. [DOI] [PubMed] [Google Scholar]
- Brown T.T., Martinez-Gutierrez M.S., Navab B. The impact of changes in county public health expenditures on general health in the population. Health Economics, Policy and Law. 2014;9(3):251–269. doi: 10.1017/S1744133114000024. [DOI] [PubMed] [Google Scholar]
- Burton L.M., Lichter D.T., Baker R.S., Eason J.M. Inequality, family processes, and health in the “new” rural America. American Behavioral Scientist. 2013;57(8):1128–1151. [Google Scholar]
- Case A., Deaton A. Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proceedings of the National Academy of Sciences. 2015;112(49):15078–15083. doi: 10.1073/pnas.1518393112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan L., Hart G., Goodman D.C. Geographic access to health care for rural Medicare beneficiaries. The Journal of Rural Health. 2006;22(2):140–146. doi: 10.1111/j.1748-0361.2006.00022.x. [DOI] [PubMed] [Google Scholar]
- Chetty R., Stepner M., Abraham S., Lin S., Scuderi B., Turner N., Bergeron A., Cutler D. The association between income and life expectancy in the United States, 2001–2014. JAMA. 2016;315(16):1750–1766. doi: 10.1001/jama.2016.4226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Condran G.A., Crimmins-Gardner E. Public health measures and mortality in US cities in the late nineteenth century. Human Ecology. 1978;6(1):27–54. doi: 10.1007/BF00888565. [DOI] [PubMed] [Google Scholar]
- Cosby A.G., Neaves T.T., Cossman R.E., Cossman J.S., James W.L., Feierabend N., Mirvis D.M., Jones C.A., Farrigan T. Preliminary evidence for an emerging nonmetropolitan mortality penalty in the United States. American J. Public Health. 2008;98(8):1470–1472. doi: 10.2105/AJPH.2007.123778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cossman J.S., Cossman R.E., James W.L., Campbell C.R., Blanchard T.C., Cosby A.G. Persistent clusters of mortality in the United States. American J of Public Health. 2007;97(12):2148–2150. doi: 10.2105/AJPH.2006.093112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cossman J.S., James W.L., Cosby A.G., Cossman R.E. Underlying causes of the emerging nonmetropolitan mortality penalty. American Journal of Public Health. 2010;100(8):1417–1419. doi: 10.2105/AJPH.2009.174185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cossman J.S., Ritchie J.B., Cosby A.G. Driving to doctors: Access to primary care physicians in Mississippi (Health Policy Brief) Mississippi Health Policy Research Center. 2006 http://www.nemsahec.msstate.edu/publications/policybriefs/drivetimedocs.pdf [Google Scholar]
- Cossman J.S., Ritchie J.B., Cosby A.G. Driving to doctors: Access to specialists in Mississippi (Health Policy Brief) Mississippi Health Policy Research Center. 2006 http://www.nemsahec.msstate.edu/publications/policybriefs/drivetimespecs.pdf [Google Scholar]
- Council of Economic Advisors (2010). Strengthening the Rural Economy. Executive Office of the President of the United States. Retrieved June 10, 2016 from 〈http://www.usda.gov/documents/Rural_America_final.pdf〉.
- Cromartie, J., & Parker, T. (2016). Rural classifications. Economic Research Service, US Department of Agriculture. Retrieved June 21, 2016 〈http://www.ers.usda.gov/data-products/rural-urban-continuum-codes.aspx〉.
- Cutler D., Miller G. The role of public health improvements in health advances: The twentieth century United States. Demography. 2005;42(1):1–22. doi: 10.1353/dem.2005.0002. [DOI] [PubMed] [Google Scholar]
- Deaton A., Lubotsky Mortality, inequality and race in American cities and states. Social Science Medicine. 2003;56(6):1139–1153. doi: 10.1016/s0277-9536(02)00115-6. [DOI] [PubMed] [Google Scholar]
- Fan Y., Song Y. Is sprawl associated with a widening urban-suburban mortality gap? Journal of Urban Health. 2009;86(5):708–728. doi: 10.1007/s11524-009-9382-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haines M.R. The urban mortality transition in the United States, 1800–194. 0 Annales de Démographie Historique (Paris) 2001;101:33–64. [Google Scholar]
- Hall S.A., Kaufman J.S., Ricketts T.C. Defining urban and rural areas in US epidemiologic studies. Journal of Urban Health. 2006;83(2):162–175. doi: 10.1007/s11524-005-9016-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartley D. Rural health disparities, population health, and rural culture. American Journal of Public Health. 2004;94(10):1675–1678. doi: 10.2105/ajph.94.10.1675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health Resources and Service Administration Comparison of the Rural Health Clinic and Federally Qualified Health Center Programs. United States Department of Health and Human Services. 2006 〈http://www.hrsa.gov/ruralhealth/policy/confcall/comparisonguide.pdf〉 (Retrieved June 11, 2016 from) [Google Scholar]
- Health Resources and Service Administration. (n.d.) (2016). Rural Referral Centers. U.S. Department of Health and Human Services. Retrieved June 11 from 〈http://www.hrsa.gov/opa/eligibilityandregistration/hospitals/ruralreferralcenters/index.html〉.
- Higgs R., Booth D. Mortality differentials within large American cities in 1890. Human Ecology. 1979;7(4):353–370. [PubMed] [Google Scholar]
- IBM Corp. Released . IBM Corp; Armonk, NY: 2013. IBM SPSS statistics for Windows, Version 22.0. [Google Scholar]
- Ingram, D.D., & Franco, S.J. (2012). NCHS urban-rural classification scheme for counties. National Center for Health Statistics. Vital Health Statistics 2(154). Retrieved August 26, 2013 from 〈http://www.cdc.gov/nchs/data/series/sr_02/sr02_154.pdf〉. [PubMed]
- James W.L. All rural places are not created equal: Revisiting the rural mortality penalty in the United States. American Journal of Public Health. 2014;104(11):2122–2129. doi: 10.2105/AJPH.2014.301989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- James W.L., Cossman J.S. Long-term trends in Black and White mortality in the rural United States: Evidence of a race-specific rural mortality penalty. The Journal of Rural Health. 2016;00:1–11. doi: 10.1111/jrh.12181. [DOI] [PubMed] [Google Scholar]
- Joynt K.E., Harris Y., Orav J., Jha A.K. Quality of care and patient outcomes in critical access rural hospitals. The Journal of the American Medical Association. 2011;306(1):45–52. doi: 10.1001/jama.2011.902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufman B.G., Thomas S.R., Randolph R.K., Perry J.R., Thompson K.W., Holmes G.M., Pink G.H. The rising rate of rural hospital closures. The Journal of Rural Health. 2016;32(1):35–43. doi: 10.1111/jrh.12128. [DOI] [PubMed] [Google Scholar]
- Kwan M.-P., editor. Geographies of health, disease, and well-being: Recent advances in theory and method. Routledge; 2016. [Google Scholar]
- Litaker D., Koroukian S.M., Love T.E. Context and healthcare access: Looking beyond the individual. Medical Care. 2005;43(6):531–540. doi: 10.1097/01.mlr.0000163642.88413.58. [DOI] [PubMed] [Google Scholar]
- Marton J., Sung J., Honore P. Does more public health spending buy better health? Health Services Research and Managerial Epidemiology. 2015:2. doi: 10.1177/2333392815580750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masters R.K. Uncrossing the U.S. black-white mortality crossover: The role of cohort forces in life course mortality risk. Demography. 2012;49:773–796. doi: 10.1007/s13524-012-0107-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mays G.P., Smith S.A. Geographic variation in public health spending: Correlates and consequences. Health Services Research. 2009;44(5p2):1796–1817. doi: 10.1111/j.1475-6773.2009.01014.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monnat S.M., Pickett C.B. Rural/urban differences in self-rated health: Examining the roles of county size and metropolitan adjacency. Health Place. 2011;17:311–319. doi: 10.1016/j.healthplace.2010.11.008. [DOI] [PubMed] [Google Scholar]
- Miller, D. (2011). Health Care Workforce Shortages Critical in Rural America. Council of State Governments. Retrieved June 21, 2016 from 〈http://knowledgecenter.csg.org/kc/content/health-care-workforce-shortages-critical-rural-america〉.
- Murray C.J.L., Kulkarni S., Ezzati M. Eight Americas: New perspectives on US health disparities. American Journal of Preventive Medicine. 2005;29(5 suppl 1):4–10. doi: 10.1016/j.amepre.2005.07.031. [DOI] [PubMed] [Google Scholar]
- Murray C.J.L., Kulkarni S., Michaud C., Tomijima N., Bulzacchelli M.T., Iandiorio T.J., Ezzati M. Eight Americas: Investigating mortality disparities across races, counties, and race-counties in the United States. PLoS Med. 2006;3(9):e260. doi: 10.1371/journal.pmed.0030260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [dataset] National Center for Health Statistics . US Department of Health and Human Services; 2000. Compressed Mortality File: 1968-88. Hyattsville, MD: Centers for Disease Control and Prevention. [Google Scholar]
- [dataset] National Center for Health Statistics . US Department of Health and Human Services; 2001. Compressed Mortality File: 1989-98. Hyattsville, MD: Centers for Disease Control and Prevention. [Google Scholar]
- [dataset] National Center for Health Statistics . US Department of Health and Human Services; 2010. Compressed Mortality File: 1999–2007. Hyattsville, MD: Centers for Disease Control and Prevention. [Google Scholar]
- Omran A.R. The epidemiological transition: A theory of the epidemiology of population change. The Milbank Memorial Fund Quarterly. 1971;49(4):509–538. [PubMed] [Google Scholar]
- Pascoe J.M., Wood D.L., Duffee J.H., Kuo A. Mediators and adverse effects of child poverty in the United States. Pediatrics. 2016;137(4):e20160340. doi: 10.1542/peds.2016-0340. [DOI] [PubMed] [Google Scholar]
- Preston S.H., Haines M.R. Princeton University Press; Princeton, NJ: 1991. Fatal years: Child mortality in late nineteenth-century America. [Google Scholar]
- Probst J.C., Bellinger J.D., Walsemann K.M., Hardin J., Glover S.H. Higher risk of death in rural Blacks and Whites than urbanites is related to lower incomes, education, and health coverage. Health Affairs. 2011;30(10):1872–1879. doi: 10.1377/hlthaff.2011.0668. [DOI] [PubMed] [Google Scholar]
- Provasnik S., KewalRamani A., McLaughlin Coleman M., Gibertson L., Herring W., Xie W. Institute of Education Sciences, US Department of Education; Washington, DC: 2007. Status of education in rural America (NCES 2007-040). National Center for Education Statistics. [Google Scholar]
- Rosko M.D., Mutter R.L. Inefficiency differences between critical access hospitals and prospectively paid rural hospitals. Journal of Health Politics, Policy and Law. 2010;35(1):95–126. doi: 10.1215/03616878-2009-042. [DOI] [PubMed] [Google Scholar]
- Saloman J.A., Murray C.J.L. The epidemiologic transition revisited: Compositional models for causes of death by age and sex. Population and Development Review. 2002;28(2):205–228. [Google Scholar]
- Sasson I. Trends in life expectancy and lifespan variation by educational attainment: United States, 1990–2010. Demography. 2016;53(2):269–293. doi: 10.1007/s13524-015-0453-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegel J.S., Swanson D., editors. The methods and materials of demography. 2nd ed. Elsevier Science and Technology Books; Amsterdam, the Netherlands: 2004. [Google Scholar]
- Singh G.K., Siahpush M. Increasing rural-urban gradients in US suicide mortality, 1970–199. 7 American Journal of Public Health. 2002;92(7):1161–1167. doi: 10.2105/ajph.92.7.1161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh G.K., Siahpush M. Widening rural-urban disparities in all-cause mortality and mortality from major causes of death in the USA, 1969–2009. Journal of Urban Health. 2014;91(2):272–292. doi: 10.1007/s11524-013-9847-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh G.K., Siahpush M. Widening rural-urban disparities in life expectancy, U.S., 1969–2009. American Journal of Preventive Medicine. 2014;46(2):e19–e29. doi: 10.1016/j.amepre.2013.10.017. [DOI] [PubMed] [Google Scholar]
- Singh G.K., Siahpush M., Williams S.D. Changing urbanization patterns in US lung cancer mortality, 1950–2007. Journal of Community Health. 2012;37(2):412–420. doi: 10.1007/s10900-011-9458-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith D.W., Bradshaw B.S. Variation in life expectancy during the twentieth century of the United States. Demography. 2006;43(4):647–657. doi: 10.1353/dem.2006.0039. [DOI] [PubMed] [Google Scholar]
- Snyder S.E. Urban and rural divergence in mortality trends: A comment on Case and Deaton. Proceedings of the National Academy of Sciences. 2016;113(7) doi: 10.1073/pnas.1523659113. (E815-E815) [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Department of Agriculture (2013). . Rural America at a Glance: 2013 Edition (Economic Brief, No. 24). Economic Research Service. Retrieved June 10, 2016 from 〈http://www.ers.usda.gov/media/1216457/eb-24_single-pages.pdf〉.
- United States Senate (1997). H.R. 2015, Balanced Budget Act of 1997. 105th Congress, 1st Session. Edition statement. Washington: Government Printing Office.
- Winters C.A., editor. Rural nursing: Concepts, theory, and practice. 4th ed. Springer Publishing Company; New York: 2013. [Google Scholar]
- Yang T.-C., Jensen L., Haran M. Social capital and human mortality: Explaining the rural paradox with county-level mortality data. Rural Sociology. 2011;76(3):347–374. doi: 10.1111/j.1549-0831.2011.00055.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang T.-C., Matthews S.A. Death by segregation: Does the dimension of racial segregation matter? PLoS One. 2015;10(9):e0138489. doi: 10.1371/journal.pone.0138489. [DOI] [PMC free article] [PubMed] [Google Scholar]