Abstract
Background:
Shift work can have an impact on the physical and psychological well-being of the healthcare worker, affecting patients as well as their own safety at the workplace. This study was conducted to compare the health outcomes and injuries, along with associated risk factors between the nurses working in rotating night shift (RNS) as compared to day shift (DS) only.
Materials and Methods:
It was a cross-sectional study conducted from June to November 2016 in a tertiary care hospital of Delhi. It involved 275 nurses working in RNS and 275 nurses from DS of various departments, selected through simple random sampling. Standard Shift Work Index Questionnaire (SSI) was used as the study instrument, with selected variables (according to objectives of the study). Data were analyzed using descriptive statistics, Chi-square, t-test, and multivariate regression.
Results:
Female nurses had more sleep disturbance, fatigue, and poor psychological health. Working on a contractual basis, RNS, and living outside the hospital campus were associated with higher odds of having needle stick injury (NSI). The nurses working in RNSs were found to have significantly lower mean scores in job satisfaction (p = 0.04), sleep (p < 0.001), and psychological well-being (p = 0.047) as compared to DS workers.
Conclusions:
Health outcomes among nurses working in RNSs call for the interventions, focused on various factors which can be modified to provide supportive and safer working environment.
Keywords: Health, India, injury, nurse, sleep
Introduction
Healthcare systems are organizations that are established to meet the health needs of people. Work in the health sector is often associated with night shifts and long duty hours in order to provide round the clock services.[1] Nurses have a significant role in healthcare delivery. Night shift nurses are responsible for patient care with little support[2,3] in a difficult working environment under continuous pressure[4] and face problems directly related to working at night.[2,3]
A Greek study noted that the nurses doing night shifts as compared to day shift (DS) nurses experience more severe symptoms of fatigue, sleepiness, and impaired concentration.[5] Rotating night shifts (RNSs) have been found to be one of the most common reasons for the disruption of the sleep–wake cycle, causing poor physical and psychological well-being, as well as unsatisfactory work performance.[6,7] In addition to the above-mentioned outcomes, healthcare workers are exposed to various occupational health hazards, including accidental needle stick injuries (NSIs), which pose a serious risk of infection to healthcare workers with HIV, Hepatitis B, Hepatitis C, and others.[8] Ilhan et al.[8] demonstrated that the percentage of nurses experiencing a sharp or NSI during their professional life was 79.7%. Similar results were shown in another study done by Sharma et al.,[9] which revealed the prevalence of NSI among nurses was found to be 79.5%. A study done in Australia by Winwood et al.[10] demonstrated that the fatigue related to night shifts can increase the risk of human errors and injuries and can negatively affect the quality of patient care.
Although research into occupational health among nursing workforces has reflected deleterious health effects related to shift work, most of these studies represent health workers of developed countries. Nurses in developed countries may have better and safer working conditions than nurses in developing countries. This can be due to greater economic resources and regulatory policy that support quality occupational health and safety precautions in most of the developed countries. The poor health outcomes and injuries can have unwanted consequences in the form of decreased job satisfaction and attrition, which affects the healthcare delivery. These consequences can be manifold in developing countries such as India, where health sector already suffers due to the poor doctor: nurse and nurse: population ratio. Moreover, developing countries have limited qualified human resources compared to disease burden. The implementation of adequate preventive measures to minimize the adverse health effects of shift work are limited and need more research in this area. This study aims to determine if rotating shift work along with nights, compared to DS only, is associated with risk factors predisposing nurses to poor health outcomes and injuries.
Materials and Methods
It was a hospital-based cross-sectional study conducted in a tertiary care hospital in Delhi, conducted over a period of 6 months, from June to November 2016. At this hospital, nurses work in irregular rotating shifts (morning, evening, and night shifts), while a subset of nursing staff does only morning shifts, e.g., working in the outpatient departments (OPDs). The sample size was determined using Fisher's formula for estimating single proportions.[11] The standard normal deviation was set at a 95% confidence level, the prevalence of injuries at 79.5%,[9] with the allowable margin of error of 5%. The Fisher's formula (n = Z2[PQ]/d2) gave a sample size of 275 respondents, considering 10% nonresponse rate.
The nurses work in different units of the hospital, as allocated according to the hospital needs and their qualifications. Out of the total number of nurses, 275 nurses working in RNS and 275 from DS were selected, proportionately from each ward and printed questionnaires were delivered to these nurses. The nurses were stratified into wards based on their representativeness (spread), and then simple random sampling was used to identify respondents among various wards and OPDs. Data were collected using SSI, which is a self-administered and structured questionnaire. The principal investigator explained the purpose and contents of this survey and asked cooperation from the nursing department of the institution. Questionnaires were distributed with a cover page explaining the study purpose, methodology, and instructions on each unit. Respondents were asked to complete the questionnaires in a day or two, without affecting their work at a hospital and return them to the sister in charge (head nurse) of corresponding wards. The investigator collected the filled forms from the sister in charge (head nurse). After paying at least three visits to hospital as a follow-up, the overall response rate was around 88.7%. Out of total 550 forms (275 to RNS nurses and 275 to DS nurses), 480 questionnaires were returned.
Self-administered questionnaires were used to acquire information about sleep and fatigue (33 items), attitudes toward work indicating general job satisfaction (41 items), and general health well-being (47 items). Cronbach's alpha for “poor sleep,” “chronic fatigue, “job satisfaction”, “general health questionnaire (GHQ),” and “injuries” was 0.89, 0.78, 0.83, 0.79, and 0.91, respectively.
The “Standard Shift Work Index”[12] was developed by Barton et al., with the aim to produce a core of questions, covering the selected areas of interest, according to individual researchers. All the measures included are independent of each other, producing individual scores. It provides a battery of self-report questionnaires, which is easy to administer and has good psychometric properties. It can be used to assess the impact of shift systems on the health of workers by measuring (a) outcomes, related to various health problems (physical, mental health, sleep disruption, etc.); (b) modifiers, related to individual's characteristics and circumstances, such as age, marital status, number of dependents in the family; and (c) general, which includes information about work and shift system.[12] In accordance with the aims and objectives of our study, we included the subsections of SSI scales: (1) Demographic profile including personal and work characteristics – age, sex, marital status, the number of dependents living with study participant, occupational rank, residence, and employment status (contractual or regular). (2) Sleep questionnaire: sleep habits were evaluated by a Likert scale ranging from 1 (almost never) to 5 (almost always), “a score of 5 being associated with high sleep disturbance.” (3) Chronic fatigue assessed by using a 1–5-point Likert scale (higher score is an indication of more fatigue). (4) Injuries: sustained at the workplace in the last 1 month and the shift in which they occurred and their potential causes. NSI was defined as “any cut or prick to the study subject in the hospital by a needle which has been used previously on a patient.” (5) Job satisfaction: consists of five items which measure the degree to which the employee is satisfied and happy with the job, assessed with a 7-point score ranging from “strongly disagree” (score 1) to “strongly agree” (score 7). (6) GHQ: multiple-response scale or Likert scale to assess the common mental health problems – “A higher score would indicate poorer psychological health.”
Data were analyzed using Statistical Package for the Social Sciences version 21 (IBM Corp. Released 2012. IBM SPSS Statistics for Windows, Armonk, NY). Completed schedules were included for data processing and analysis. Quantitative variables are presented as mean and standard deviation, while categorical variables were reported as absolute and relative frequencies. The scale score of each item was compared between RNS and DS workers by using the Fisher's exact and Chi-square test for categorical data and unpaired t-test for continuous data.
Exploratory data analyses were conducted to examine the patterns and relationships among dependent variables (SSI scores, NSI) and other predictive variables using appropriate regression with backward elimination approach. Multivariate linear and logistic analyses were done for SSI scores (continuous) and NSI (dichotomous), respectively. Dummy coding of categorical variables (1,0) was done to fit them in predictive modeling. Also, before finalizing the fitted model, the correlation coefficients of all the variables were investigated to ensure the significance of each predictive variable. It is important to state that to finalize the model all the requisite assumptions, i.e., linearity, multivariate normality, etc. were met. For all analyses p value <0.05 was considered to be statistically significant.
Multiple linear regression was done to identify the demographic and individual variables associated with the SSI score. The independent variables which were explored in regression analyses were: age (<35, 36–40, >40), gender (male/female), marital status (single/married), number of dependents in the family (0, 1/2, ≥3), residence (inside campus/outside), occupational rank (sister in charge/staff nurse), and employment status (contractual or regular), working shift (RNS or DS), and mean years of experience.
The association between the NSI and selected characteristics, which have been described above, was analyzed by means of logistic regression and expressed as adjusted odds ratio (AOR) with a confidence interval at 95% (95% CI). The AOR measures the strength of association between the characteristics of the study population and NSI. Positive OR means that the odds for the occurrence of NSI were greater when exposed to an increased value of covariates analyzed.
Ethical considerations
The aim and objectives of the study were explained and informed consent was taken from all the participants. The option to opt out of the study at any stage of the interview was kept open without any clause. The institutional ethical clearance for the study was obtained (F. No. 11/IEC/MAMC/2016) and complete confidentiality regarding nurses' information was maintained through all the stages of the study.
Results
Table 1 shows the comparison of sleep, fatigue, NSI, job satisfaction, and GHQ scores between the two groups. RNS nurses were found to have lower mean scores of sleep quantity and quality than DS nurses. The difference was statistically significant while working in both morning (p value < 0.001) and afternoon shifts (p value = 0.07). RNS reported higher mean score of fatigue compared to the DS nurses, but it was not statistically significant. However, the NSIs within last 1 month were significantly higher among RNS nurses (p value < 0.001). More than three-fourths of the nurses in both groups reported to have experienced a NSI in their career and almost half of the nurses who have had NSI in recent past had attributed fatigue as the main cause of injury. RNS nurses were found to have lower scores in both job satisfaction and psychological health, with statistically significant difference (p = 0.04), as shown in Table 1.
Table 1.
Comparison of sleep, fatigue, NSI, job satisfaction, and general health questionnaire scores
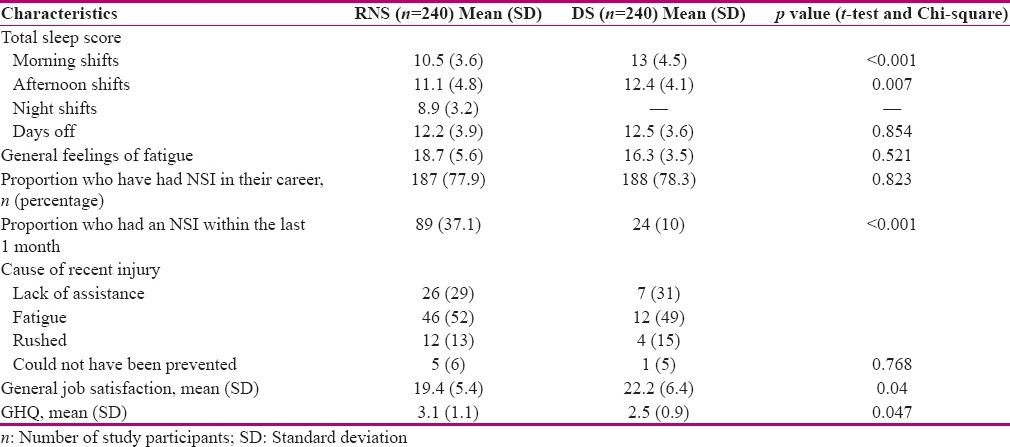
Table 2 shows the multiple regression analysis for various health outcomes. Sleep disturbances were found to be associated with female gender, residence outside the campus, and increased with the number of dependents in the family. Fatigue was more among the females, married respondents, and RNS nurses. Nurses who were staying outside the hospital campus and were doing RNS had lower job satisfaction compared to another group. Poor psychological scores were associated with the female gender and number of dependents in the family.
Table 2.
Multivariate linear regression analysis of the factors associated with sleep, chronic fatigue, job satisfaction, and GHQ scores
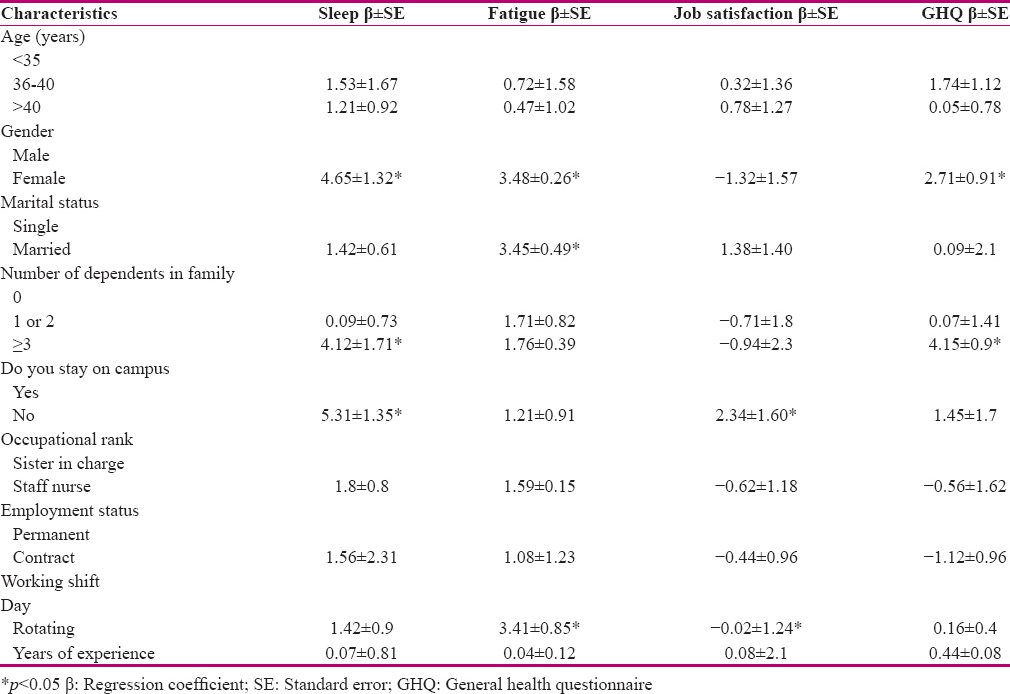
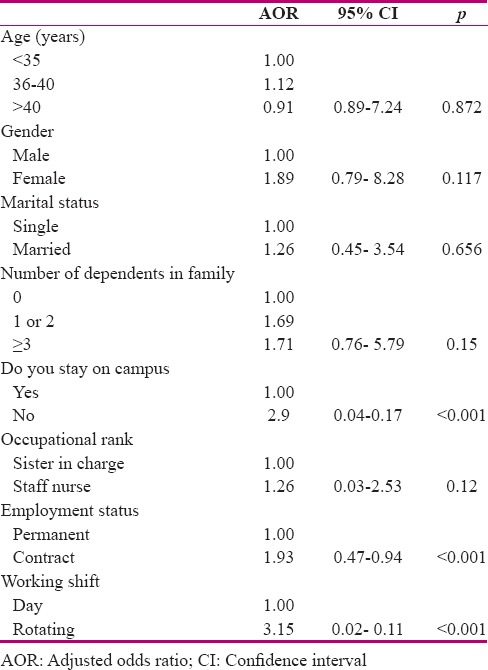
Table 3 shows the AORs and 95% confidence intervals of the factors found to be associated with the NSIs from a final multivariate logistic regression model. Living outside the campus of the hospital was associated with higher odds of experiencing work-related injury [AOR 4.9; 95% confidence interval (CI) 0.04-0.17]. Study subjects working on contractual basis had higher odds of injuries as compared to the permanent staff (AOR 1.93; CI 0.07-0.24). The rotating shift was associated with higher odds of NSIs (AOR 5.71; 95% CI 0.02-0.11).
Table 3.
Multivariate logistic regression analysis of factors associated with NSIs
Discussion
Results of the present study showed that there was a significant difference between RNS and DS nurses regarding the sleep scores, NSIs, job satisfaction, and general well-being scores. Similarly, another study also demonstrated the significant association of RNS with decreased sleep scores, job satisfaction, and psychological health (assessed with general health questionnaire).[13] The literature agrees in indicating that RNS work imposes circadian strain and leads to a greater number of physical and psychological symptoms in the form of elevated scores on the majority of the SSI scales, such as sleep, chronic fatigue, and general health questionnaire.[14,15]
This study also explored the association between RNSs and NSIs, which were found to be statistically significant. This finding is in accordance with research findings by Johns et al., which reported that healthcare workers while doing night shifts are at a higher risk of sustaining accidental injuries than day workers.[16] However, most of the literature reveals that injuries are found to be associated more with the increased work hours, rather than the type of shift.[8,17] In our sample, nurses working in RNSs revealed that their duty time was sometimes extended leading to work for few extra hours as compared to DS nurses, who had a fixed time schedule in OPDs. This finding is in accordance with the results of studies done by Olds et al. and Ilhan et al.[8,17]
In addition to the above findings, our study revealed the association of SSI score as well as NSI with various demographic and individual variables by using multivariate regression models. Female nursing personnel had higher scores on most of the SSI scales, such as in terms of disturbed sleep, fatigue, and poor psychological health. Nurses with family responsibilities were found to have more disturbed sleep and poor GHQ scores. The greater number of dependents in the family leads to higher physical and emotional demands, leading to overexertion and affecting quality and quantity of sleep. This finding is in accordance with other authors.[14]
In this study, decreased job satisfaction was found to be associated with rotating shift duty and residing outside the hospital premises. The possible explanation for this association is the increased stress among nurses living outside hospital campus, considering the amount of time required to reach workplace every day along with doing rotating shifts, which can lead to job dissatisfaction. The association between rotating shift duty and poor job satisfaction has been demonstrated in many studies.[13,18] This study showed that the nurses who had a contractual appointment, staying outside hospital campus and doing RNS had higher odds of having NSI. This can be attributed to the fact that nurses working on a contractual basis and staying outside experience more stress, job insecurity, and have less experience as compared to the permanent staff.
Interpretation of this study's results is limited by the cross-sectional, self-administered design. This study was based on self-reported information from the study subjects regarding their employment, illness, and injury experiences. Owing to lack of external validation of their responses, results may be subject to potential inaccuracies related to the inability of respondents to recall information correctly. Moreover, results were based on observation over the study period, which may vary over different periods of time.
Conclusion
This study confirmed previous research and identified factors that can be targeted for the development of more effective shift work adaptation programs in a healthcare setting. This study revealed some modifiable targets for improving shift work adaptation, such as sleep, fatigue, job satisfaction, and general health. These can be modified by including appropriate interventions in their training itself, such as behavioral changes for good sleep hygiene, counseling, and periodic screening for general well-being. Prevention of NSIs is the best strategy, but setting up of adequate surveillance mechanism in every hospital is also necessary. In addition to that, fixed timing and duration of duty hours in case of rotating shifts can also contribute to lesser human errors and better job satisfaction.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
The authors are thankful to the nursing personnel working in Lok Nayak Hospital, Maulana Azad Medical College, New Delhi, for their cooperation, which made this research possible.
References
- 1.Bajraktarov S, Novotni A, Manusheva N, Nikovska DG, Miceva-Velickovska E, Zdraveska N, et al. Main effects of sleep disorders related to shift work—opportunities for preventive programs. EPMA J. 2011;2:365–70. doi: 10.1007/s13167-011-0128-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Campbell A, Nilsson K, Andersson E. Night duty as an opportunity for learning. J Adv Nurs. 2008;62:346–53. doi: 10.1111/j.1365-2648.2008.04604.x. [DOI] [PubMed] [Google Scholar]
- 3.Nilsson K, Campbell A, Anderson E. Night nursing: Staff's working experiences. BMC Nurs. 2008;7:13. doi: 10.1186/1472-6955-7-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Adib-Hajbaghery M, Khamechian M, Alavi NM. Nurses' perception of occupational stress and its influencing factors: A qualitative study. Iranian J Nurs Midwifery Res. 2012;17:352–9. [PMC free article] [PubMed] [Google Scholar]
- 5.Korompeli A, Chara T, Chrysoula L, Sourtzi P. Sleep disturbance in nursing personnel working shifts. Nurs Forum. 2013;48:45–53. doi: 10.1111/nuf.12005. [DOI] [PubMed] [Google Scholar]
- 6.Costa G. Shift work and health: Current problems and preventive actions. Saf Health Work. 2010;1:112–3. doi: 10.5491/SHAW.2010.1.2.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Costa G, Accattoli MP, Garbarino S, Magnavita N, Rosselli F. Sleep disorders, and work: Guidelines for health surveillance, risk management, and prevention. Med Lav. 2013;104:251–66. [PubMed] [Google Scholar]
- 8.Ilhan MN, Durukan E, Aras E, Turkoglu S, Aygun R. Long working hours increase the risk of sharp and needlestick injury in nurses: The need for new policy implication. J Adv Nurs. 2006;56:563–8. doi: 10.1111/j.1365-2648.2006.04041.x. [DOI] [PubMed] [Google Scholar]
- 9.Sharma R, Rasania SK, Verma A, Singh S. Study of prevalence and response to needle stick injuries among healthcare workers in a Tertiary Care Hospital in Delhi, India. Indian J Community Med. 2010;35:74–7. doi: 10.4103/0970-0218.62565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Winwood PC, Winefield AH, Lushington K. Work-related fatigue and recovery: The contribution of age, domestic responsibilities, and shiftwork. J Adv Nurs. 2006;56:438–49. doi: 10.1111/j.1365-2648.2006.04011.x. [DOI] [PubMed] [Google Scholar]
- 11.Pourhoseingholi MA, Vahedi M, Rahimzadeh M. Sample size calculation in medical studies. Gastroenterology and Hepatology from bed to bench. 2013;6:14. [PMC free article] [PubMed] [Google Scholar]
- 12.Barton J, Spelten E, Totterdell P, Smith L, Folkard S. Is there an optimum number of night shifts? Relationship between sleep, health and well-being. Work and Stress. 1995;9:109–23. doi: 10.1080/02678379508256545. [DOI] [PubMed] [Google Scholar]
- 13.Ferri P, Guida M, Marcheselli L, Balduzzi S, Magnani D, Lorenzo RD. The impact of shift work on the psychological and physical health of nurses in a general hospital: A comparison between rotating night shifts and day shifts. Risk Management and Healthcare Policy. 2016;9:203–11. doi: 10.2147/RMHP.S115326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Korompeli A, Muurlink O, Tzavara C, Velonakis E, Lemonidou C, Sourtzi P. Influence of shiftwork on Greek nursing personnel. Saf Health Work. 2014:73–9. doi: 10.1016/j.shaw.2014.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Burch JB, Tom J, Zhai Y, Criswell L, Leo E, Ogoussan K. Shiftwork impacts and adaptation among health care workers. Occup Med. 2009;59:159–66. doi: 10.1093/occmed/kqp015. [DOI] [PubMed] [Google Scholar]
- 16.Johns MM, Wolman DM, Ulmer C, editors. Resident duty hours: Enhancing sleep, supervision, and safety. National Academies Press; 2009. [PubMed] [Google Scholar]
- 17.Olds DM, Clarke SP. The effect of work hours on adverse events and errors in health care. J Saf Res. 2010;41:153–62. doi: 10.1016/j.jsr.2010.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gouzou M, Karanikola M, Lemonidou C, Papathanassoglou E, Giannakopoulou M. Measuring professional satisfaction and nursing workload among nursing staff at a Greek Coronary Care Unit. Rev Esc Enferm USP. 2015;49:15–21. doi: 10.1590/S0080-6234201500000003. [DOI] [PubMed] [Google Scholar]


