Abstract
Secretogranin III (Scg3) is a member of the granin protein family that regulates the biogenesis of secretory granules. Scg3 was recently discovered as an angiogenic factor, expanding its functional role to extrinsic regulation. Unlike many other known angiogenic factors, the pro-angiogenic actions of Scg3 are restricted to pathological conditions. Among thousands of quantified endothelial ligands, Scg3 has the highest binding activity ratio to diabetic vs. healthy mouse retinas and lowest background binding to normal vessels. In contrast, vascular endothelial growth factor binds to and stimulates angiogenesis of both diabetic and control vasculature. Consistent with its role in pathological angiogenesis, Scg3-neutralizing antibodies alleviate retinal vascular leakage in mouse models of diabetic retinopathy and retinal neovascularization in oxygen-induced retinopathy mice. This review summarizes our current knowledge of Scg3 as a regulatory protein of secretory granules, highlights its new role as a highly disease-selective angiogenic factor, and envisions Scg3 inhibitors as “selective angiogenesis blockers” for targeted therapy.
Keywords: Anti-angiogenesis therapy, Diabetic macular edema, Proliferative diabetic retinopathy, Retinopathy of prematurity, Ligandomics, Comparative ligandomics
Introduction
Secretogranin III (Scg3) was first identified in 1990 as a product of the mouse neuron-specific 1B1075 gene [1], and later renamed secretogranin III (SgIII) based on its biochemical properties [2]. In the next 26 years, Scg3 was exclusively investigated as a vesicle protein that intracellularly regulates the biogenesis of secretory granules. Despite the presence of a classical signal peptide for extracellular trafficking, possible extrinsic regulatory function(s) of Scg3 has been largely ignored. This situation has now changed with the recent discovery that Scg3 is a novel angiogenic and vascular leakage factor with unique disease selectivity [3]. Scg3 was found to selectively bind to and induce angiogenesis of diabetic but not normal vessels. To our knowledge, such high selectivity is a unique property of Scg3, not seen in other angiogenic/leakage factors in diabetes, and raises an interesting question: What may be the selective advantages of a pro-angiogenic factor in terms of its pathological role and therapeutic potential. This review summarizes current knowledge of Scg3 in the biogenesis of secretory granules and emphasizes its new role as a novel endothelial ligand in vascular diseases. We highlight the new trend of developing disease-selective anti-angiogenesis therapies and discuss Scg3 as a highly disease-selective angiogenic factor and its potential for targeted therapy. Other members of Scg3 family covered by several excellent recent reviews [4–7] will be discussed mainly for their related roles in vascular homeostasis.
The granin family
Many hormones, growth factors, neuropeptides, neurotransmitters, and enzymes are secreted from endocrine, neuroendocrine, and neuronal cells through the trans-Golgi network (TGN). Secretion can be constitutive or regulated by external stimulation. Proteins destined for the secretory pathway are synthetized in the rough endoplasmic reticulum, transported to the TGN, and sorted into dense core secretory granules (DCGs), for example, the chromaffin granules of the adrenal medulla. In these DCGs, secretory proteins, such as catecholamines in adrenal chromaffin granules, are highly condensed and can reach levels of 0.5–1.0 mM [8]. Chromogranin A (CgA) in DCGs represents up to 50% of the soluble protein content of adrenal chromaffin granules at concentrations reaching 2 mM [9–11]. The condensation process is part of the biogenesis of secretory granules and requires the coordination of several granin family members, including CgA, chromogranin B (CgB), secretogranin II (SgII or Scg2), and Scg3 [6, 12].
CgA is the founding member of the family and was initially identified in adrenal chromaffin granules in 1967 [10]. Since then, the granin family has been expanded and is now composed of CgA, CgB, Scg2, Scg3, and HISL-19 antigen (SgIV) [13], neuroendocrine secretory protein 7B2 (SgV), NESP55 (SgVI), nerve growth factor inducible protein VGF (SgVII), and proSAAS (SgVIII) [5, 6]. Criteria for the granin family are arbitrarily selected based on their biochemical and structural characteristics rather than sequence homology. Scg3 shares little protein sequence homology with its family members (19–29% identity) (Table 1) or any other proteins. Common properties of the granin family include localization to secretory vesicles, acidic isoelectric point (pI), calcium-binding activity, propensity to form aggregates, and the presence of multiple dibasic cleavage sites. These classification criteria are not entirely unique, and granins typically share several similarities to neuropeptides or prohormones in secretory vesicles [14].
Table 1.
hScg3 (#NM_013243) has low protein sequence homology to other members of the granin family
| Protein name | GenBank accession # | Amino acid identity (%) |
|---|---|---|
| CgA | NM_001275 | 25 |
| CgB | NM_001819 | 19 |
| Scg2 | NM_003469 | 23 |
| 7B2 (SgV) | NM_001144757 | 25 |
| NESP55 (SgVI) | AJ251760 | 23 |
| VGF (SgVII) | NM_003778 | 23 |
| ProSAAS (SgVIII) | NM_0132714 | 29 |
The primary sequence of HISL-19 (SgIV) has not been reported and is excluded from sequence comparison
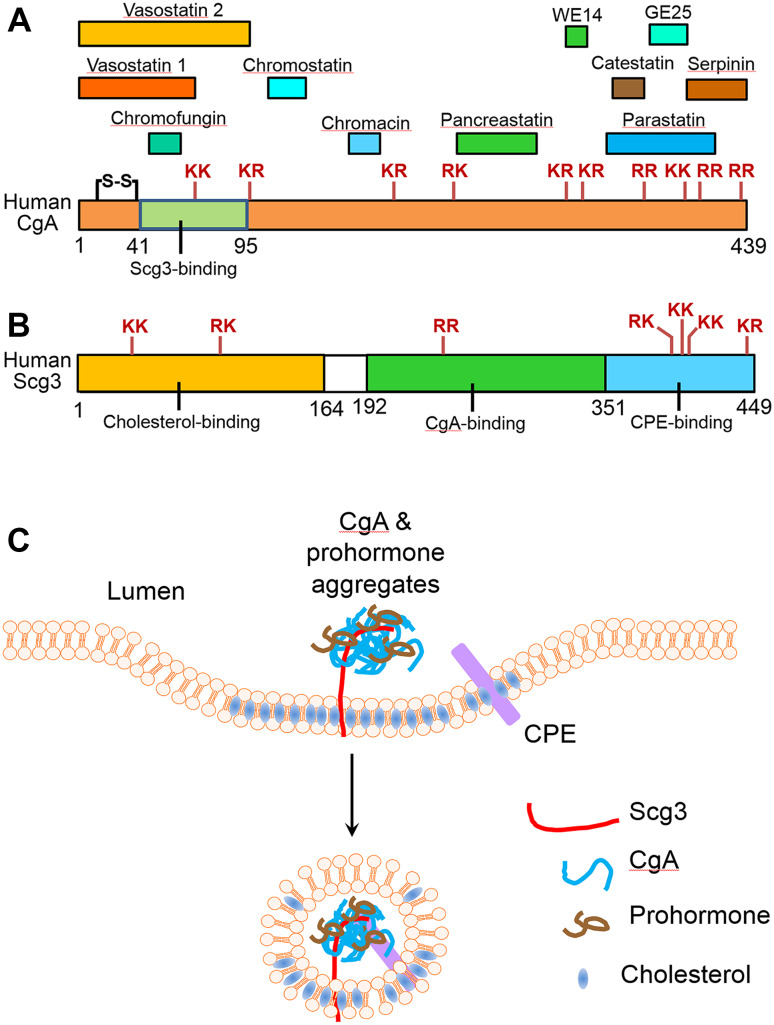
Granins may undergo cell- or tissue-specific processing in secretory granules. CgA can be processed into at least 11 different peptides (Fig. 1a) [5, 15]. The cleaved peptide products are composed of vasostatin 1 and 2, pancreastatin, catestatin, parastatin, chromacin, chromofungin, chromostatin, serpinin, WE14, and GE25. As discussed further below, vasostatin and catestatin have specific roles in regulating angiogenesis. CgB can be cleaved into a number of different peptides, such as PE11 [16], secretolytin [17], and BAM-1745 [18]. Scg2 is a precursor for secretoneurin [19].
Fig. 1.
Human CgA (hCgA) and Scg3, their functional domains, related bioactive peptides, and role in the biogenesis of secretory granules. a Mature hCgA without the signal peptide is 439 amino acids (aa) with a disulfide bond. The positions of ten dibasic peptides are indicated. hCgA is the precursor for at least 11 biologically active peptides: vasostatin I (CgA1–76), vasostatin II (CgA1–131), pancreastatin (CgA250–301), catestatin (CgA352–372), WE14 (CgA324–337), chromofungin (CgA47–66), parastatin (CgA347–419), chromacin (CgA176–197), serpinin (CgA411–436), chromostatin (CgA124–143), and GE25 (CgA375–399). b Mature hScg3 without the signal peptide is 449 aa. No cysteine residue. The positions of seven dibasic peptides are indicated. There is currently no known hScg3-derived biologically active peptide. Scg3 has three functional domains: cholesterol-binding domain (1–164), CgA-binding domain (192–351), and CPE-binding domain (352–449). c A model for Scg3 to regulate the biogenesis of secretory granules. CgA forms aggregates with prohormones in the lumen of the TGN. Scg3 as a linker simultaneously binds to CgA in the aggregates and the cholesterol-rich membrane domains of the TGN. Scg3 also interacts with CPE in the membrane. The complex forms a dense core secretory granule (DCG), which is engulfed by the TGN membrane and released as secretory vesicles
Xenopus Scg3 (xScg3) with a predicted MW of 50 kDa is expressed as a 61- or 63-kDa protein with N-glycosylation and can be processed to 48, 28, and 20 kDa [20]. Only the cleaved products of xScg3 are secreted. Murine Scg3 with a predicted MW of 51 kDa is secreted as a 53.3-kDa protein without proteolytic cleavage [21]. Human Scg3 (hScg3) has a pI of 4.94 and 7 dibasic peptide sites for potential proteolytic cleavage (Fig. 1b), but seems to be secreted also without proteolytic cleavage [22].
Diverse functional roles of granins and their derivative peptides
Granins and their peptides regulate a broad spectrum of biological activities, including secretion, metabolism, vascular homeostasis, blood pressure, cardiac function, cell adhesion and migration, and innate immunity [5–7]. Whereas this review is focused primarily on the roles of granins in secretion and vascular homeostasis, we present below a brief overview of their roles in the regulation of other important biological activities. For a wider coverage of these areas, readers are referred to excellent reviews [5, 6, 15].
CgA-derived pancreastatin possesses multiple dysglycemic activities, including inhibition of glucose-induced insulin release from pancreatic β-cells, inhibition of glucose uptake by adipocytes and hepatocytes, and induction of glycogenolysis [23–25]. These activities have been confirmed in humans and through studies in CgA-knockout mice [26, 27]. CgA-derived catestatin is a potent endogenous antagonist of nicotine cholinergic receptor and inhibits nicotine-evoked catecholamine secretion in an autocrine fashion [28]. Catestatin is also a potent vasodilator by stimulating histamine releases with augmented H1 receptor activity and increased plasma epinephrine [29]. Catestatin stimulates chemotaxis of human peripheral blood monocytes by a pathway involving phosphoinositide-3 kinase and nitric oxide [30]. Catestatin and chromofungin directly inhibit growth of fungi, yeast, and bacteria, and regulate calcium influx in neutrophils [31]. CgA plays an important role in the regulation of blood pressure, either directly or indirectly via its bioactive peptides [32, 33].
Scg2-derived secretoneurin induces the release of neurotransmitters and luteinizing hormone [34, 35], and is a potent chemotactic factor for monocytes, eosinophils, and endothelial cells [36]. In acute T cell-mediated encephalomyelitis, secretoneurin immunoreactivity is associated with a clustering of macrophages but not T lymphocytes [37].
VGF is a multifunctional protein. VGF-deficient mice display a lean, hypermetabolic, and hyperactive phenotype with reduced circulating glucose and insulin [38–40]. Increased sympathetic nervous system activity in VGF-/- mice may be responsible for alterations in energy expenditure and reduced fat storage. Intracerebroventricular administration of VGF-derived peptide TLQP-21 in mice increased energy expenditure and body temperature without altering circulating thyroid hormones (free T3 and T4) and prevented high-fat diet-induced obesity [41, 42]. Intracerebroventricularly injected TLQP-21 inhibited gastric emptying, decreased gastric acid secretion, and reduced ethanol-induced gastric lesion in rats [43–45]. These functional activities were inhibited by cyclooxygenase (COX) inhibitors, suggesting the involvement of prostaglandins. C-terminal VGF-derived peptides suppressed angiotensin II-induced vasopressin secretion, stimulated the release of neuropeptides and neurotrophins, and induced electrical potentiation in hippocampal neurons [46–48].
VGF is abundantly expressed in neurons of both sympathetic and spinal sensory ganglia [49] and upregulated in dorsal root ganglia and spinal cord after sciatic nerve transection or in other neuropathic pain models [50–52]. Intraplantar or intrathecal injection of C-terminal VGF-derived peptides induced hyperalgesia or hypersensitivity in different models of pain [50, 52, 53]. Injection of VGF-derived peptide TLQP-62 or AQEE-30 into the hippocampus in rodents promoted an antidepressant-like activity but did not affect anxiety- or novelty-induced locomotor activity [54, 55]. VGF-deficient mice have increased immobility with impairment in contextual fear-conditional learning and spatial learning [46, 54]. In addition, administration of C-terminal VGF-derived peptide AQEE-30 or LQEQ-19 into the hypothalamus enhanced nitric oxide production and facilitated penile erection in male rats [56, 57]. This functional activity was partially inhibited by pretreatment with a nitric oxide synthase inhibitor. Consistently, male VGF-knockout mice are infertile [38].
The granin 7B2 is critical to regulate the catalytic activity of prohormone convertase 2 (PC2). 7B2 functions as a molecular chaperone that binds to PC2 and prevents its unfolding and aggregation in the secretory vesicles [58]. PorSAAS is a potent inhibitor of PC1/3 [59].
To summarize this section, granins and their derivative peptides play important roles in regulating a large number of physiological and pathological processes. Because there is minimal sequence homology between Scg3 and other granins (Table 1), the diverse activities of the granin family discussed above may have limited implication to guide the functional study of Scg3.
The role of intracellular Scg3 in secretory granule biogenesis
Scg3 is one of the least studied members in the granin family. hScg3 and mouse Scg3 (mScg3) have 449-amino acids with additional signal peptides at their N termini. Scg3 is well conserved during evolution, from fish to mammals; hScg3 and mScg3 share 88.3% identity in protein sequence.
Scg3 is abundantly expressed in the brain [1] and was initially implicated in secretory processes because of coordinated mRNA upregulation of both Scg3 and the prohormone proopiomelanocortin in stimulated pituitary cells [60]. Since then, Scg3 has been exclusively investigated as a granin family member for the biogenesis of secretory granules. Scg3 binds strongly and selectively to CgA at pH 5.5 and 10 mM Ca2+, conditions that mimic the intragranular milieu [61]. Deletion of the Scg3-binding domain in CgA results in CgA missorting to the constitutive pathway, suggesting that Scg3 functions as a sorting/retention receptor for CgA to secretory granules [61]. On the other hand, deletion of the CgA-binding domain from Scg3 does not alter the intracellular trafficking of Scg3, which can still be transported to secretory granules [61]. Despite the absence of a transmembrane domain, Scg3 directly binds to liposomes in a cholesterol-dependent manner [62]. Binding of Scg3 to the secretory granule membranes purified from AtT-20 cells is drastically reduced when cholesterol is depleted from the membrane [62]. Scg3 also binds membrane-associated carboxypeptidase E (CPE) [63]. Both Scg3 and CPE bind the secretory granule membrane in a cholesterol-dependent manner and are localized similarly to the periphery of secretory granules [63]. Thus, Scg3 and CPE are laterally associated with each other on the secretory granule membrane. However, transport of Scg3 to secretory granules is not impaired in CPE-deficient cells [63], suggesting that Scg3 is sorted to the secretory granules in a CPE-independent manner.
A previous study reported that single-nucleotide polymorphisms (SNPs) in the SCG3 gene are associated with obesity in humans [64]. It was suggested that these SNPs affect the secretion of neuropeptides, including neuropeptide Y and proopiomelanocortin, which in turn regulate appetite. However, mice with homozygous deletion of the Scg3 gene have no apparent defects in viability, fertility, locomotor behavior, or obesity [65], suggesting that Scg3 is not essential for the secretion of many vital hormones. In this context, the role of Scg3 in secretory granule biogenesis may be functionally compensated by other granin family members.
A model for Scg3-mediated biogenesis of secretory granules was recently proposed by Hosaka and Watanabe [12]. Immature secretory granules or micro-aggregates, including prohormones and CgA, become tethered to a cholesterol-rich membrane domain in the TGN by Scg3, which simultaneously binds to CgA and cholesterol through different binding domains (Fig. 1c). In parallel, processing enzymes (e.g., CPE) are also recruited to the raft-like microdomains of the TGN membrane. The cholesterol-rich domains join together to form a membrane platform on which the attached micro-aggregates gather to form larger aggregates. The specific interaction between Scg3 and CPE may help to strengthen this assembly. Meanwhile, prohormones in the premature aggregates are cleaved into small fragments by processing enzymes. Depending on the species and cell types, CgA and Scg3 may also be processed [20–22]. Eventually, the secretory granule of mature hormones and granin fragments is engulfed into a membrane compartment and further concentrated to form dense core aggregates (Fig. 1c). This model is based on the binding activity of Scg3 to CgA, cholesterol, and CPE. Many detailed mechanistic steps in secretory granule biogenesis remain elusive. Mammalian Scg3, along with other proteins in the DCGs, is secreted with unknown fate for proteolytic cleavage and begins its next functional adventure as an extracellular regulator.
Scg3 and its family members as novel angiogenic and vascular leakage factors
In a separate line of research, our group developed the first technology of ligandomics for high-throughput identification of cell-wide ligands with simultaneous binding or functional activity quantification [66–68]. We applied ligandomics to a mouse model of diabetic retinopathy (DR) and identified Scg3 as an endothelial ligand with high binding activity to diabetic retinal vasculature [3]. Scg3 was independently verified as a novel angiogenic and vascular leakage factor by endothelial proliferation, migration, tube formation, spheroid sprouting, and permeability assays in vitro [3].
Because several granins have been reported to be angiogenesis regulators or precursor regulators [7, 69], such a role for Scg3 may not be surprising. Circulating full-length CgA and its cleaved peptide vasostatin-1 (CgA1–76) are potent inhibitors against angiogenesis and vascular leakage [70–72]. In contrast, CgA-derived catestatin (CgA352–372) induces endothelial cell proliferation, migration, tube formation, and corneal angiogenesis by activating G protein, MAP kinase, and Akt pathways [73]. Interestingly, blood coagulation converts CgA into catestatin, instead of vasostatin-1, in a thrombin-dependent manner [70]. These findings suggest that circulating full-length CgA and related polypeptides form a delicate balance of anti- and pro-angiogenic factors tightly regulated by proteolysis. Thrombin activation in pathophysiological conditions may tip this balance from anti-angiogenesis to pro-angiogenesis. In normal plasma, circulating CgA and vasostatin-1 levels are typically at ~0.1 and ~0.3–0.4 nM, respectively [70]. The level of catestatin may vary widely, from 0.03 to 0.33 nM or even up to 1.5 nM [32, 74, 75]. It seems possible that this variation may be related to blood coagulation and thrombin-dependent conversion from CgA to catestatin under different pathophysiological conditions.
Scg2 is another granin that may regulate angiogenesis. Scg2-derived neuropeptide secretoneurin stimulates endothelial proliferation, migration, tube formation, and corneal angiogenesis by inducing Akt and EKR pathways [19, 76]. Secretoneurin also induces coronary angiogenesis in a rat model of myocardial infarction [77]. However, secretoneurin stimulates vascular endohtelial growth factor receptors (VEGFRs) in coronary endothelial cells, and secretoneurin-induced angiogenesis is abrogated by the antibody against vascular endothelial growth factor (VEGF). Furthermore, secretoneurin increases VEGF binding to endothelial cells, and this binding is blocked by heparanase [77], suggesting that secretoneurin stimulates VEGF binding to heparan sulfate proteoglycans. Thus, secretoneurin-induced angiogenesis is VEGF-dependent.
By contrast, Scg3 appears to be a VEGF-independent angiogenic factor [3]. For example, Scg3 does not upregulate VEGF expression and vice versa. Scg3 does not bind to or activate VEGFRs. These findings suggest that Scg3 and VEGF have distinct receptor signaling pathways.
Scg3 as a highly disease-selective angiogenic factor
Quantitative comparison of the entire ligandome profiles for diseased vs. healthy cells can globally map all disease-associated ligands, including ligands with increased (disease-high) or decreased (disease-low) binding activity in disease conditions. When applied to diabetic and healthy mice, comparative ligandomics systematically identified 353 diabetes-high and 105 diabetes-low retinal endothelial ligands (Fig. 2a, b) [3]. Among a total of 1772 identified ligands, Scg3 emerged as a DR-high ligand with the highest binding activity ratio to diabetic vs. control retina (1731:0 diabetic:control) and lowest binding activity to healthy vasculature (Fig. 2c). Hepatoma-derived growth factor-related protein 3 (Hdgfrp3 or HRP-3) was found as a DR-low ligand with decreased binding to diabetic retinal vessels (48:11,140). VEGF had minimal binding activity change (diabetes-unchanged) to the retina of 4-month-diabetic mice (408:2420). GFP as a negative control showed background binding activity (10:10). These binding activity changes in diabetic retina reflected up- and down-regulation of their cognate receptors that, in the case of Scg3 and HRP-3, have yet to be identified.
Fig. 2.
Comparative ligandomics to identify Scg3 as a disease-selective ligand. a Ligandomics globally maps cell-wide endothelial ligands with simultaneous binding activity quantification in live mice. b Quantitative comparison of the entire ligandome profiles for diabetic vs. healthy retina systematically identifies disease-associated endothelial ligands. c Comparative ligandomics identified Scg3 as a diabetes-high ligand, HRP-3 as a diabetes-low ligand and VEGF as a diabetes-unchanged ligand in 4-month-diabetic mice in terms of their preferential endothelial-binding activity. ***p < 0.0001, χ 2 test, diabetic vs. healthy
The angiogenic activity of DR-high Scg3, DR-low HRP-3, and DR-unchanged VEGF in diabetic and healthy mice was independently characterized to establish the reliability of these binding activity profiling by comparative ligandomics [3]. Scg3 induced corneal angiogenesis in diabetic but not normal mice. HRP-3 stimulated corneal angiogenesis in normal but not diabetic mice. VEGF promoted angiogenesis in both diabetic and normal mice. These three distinct angiogenic activity patterns parallel their binding activity patterns in diabetic and healthy mice (Fig. 2c) [3], strongly supporting the predicting value of comparative ligandomics.
Pathophysiology and molecular mechanisms of diabetic retinopathy
DR is a leading cause of vision loss in working adults, afflicting nearly 93 million people worldwide [78]. DR can be classified into two main stages: non-proliferative DR and proliferative DR (PDR) [79]. PDR is characterized by retinal neovascularization. Diabetic macular edema (DME) and PDR are the two major forms of vision-threatening DR.
The pathogenic mechanisms by which DR and other diabetic vascular complications (DVCs) develop are not fully understood. Hyperglycemia is the primary cause of DR and DVCs through multiple mechanisms, as summarized below.
The activities of protein kinase C (PKC) α, β, δ isoforms are upregulated in diabetic vascular tissues and have been implicated in DVCs. Knockout of PKCβ or PKCδ in mice alleviates retinal ischemia-induced proliferative retinopathy, retinal pericyte apoptosis, mesangial expansion, albuminuria, and atherosclerosis [80–83]. Ruboxistaurin, a PKCβ-selective inhibitor, ameliorates DVCs in preclinical and clinical studies [83–87].
High glucose can result in the formation of advanced glycation end products (AGEs), a heterogeneous group of products that derive from non-enzymatic glycation of proteins and lipids. AGEs not only alter protein structure and function but also bind to receptor for AGEs (RAGE). RAGE activates the pro-inflammatory transcription factor, NF-κB [88]. Overexpression of RAGE in type 1 diabetic mice conferred accelerated diabetic nephropathy [89], and soluble RAGE without the transmembrane domain suppressed diabetic atherosclerosis [90]. These findings implicate the pathological role of RAGE in DVCs.
Intracellular high glucose increases the activity of the sorbitol/polyol pathway, which consumes nicotinamide adenine dinucleotide phosphate (NADPH) [91]. Cytosolic NADPH is necessary to maintain glutathione in its reduced form as a primary intracellular antioxidant. In addition, high glucose inhibits glucose 6-phosphate dehydrogenase, which catalyzes the first intermediary reaction in the pentose phosphate pathway as a primary source of NADPH [92]. The consequences are decreased intracellular NADPH and increased oxidative stress.
Superoxide and other reactive oxygen species (ROS) in vascular cells play a prominent role in endothelial dysfunction. Mitochondrion is a major source of superoxide. High intracellular concentrations of glucose and glucose-derived pyruvate increase the activity of the tricarboxylic acid (TCA) cycle and the flux of electron donors (NADH and FADH2) into the electron transport chain [93]. Coenzyme Q donates excess electrons to molecular oxygen, thereby generating superoxide. In addition, superoxide can be generated by NADPH oxidase, uncoupled endothelial nitric oxide synthase (eNOS), and xanthine oxidoreductase [94, 95].
In addition to oxidative damage, ROS mediates signal transduction that can lead to disruption of endothelial adherens junctions and increased vascular leakage. Adherens junctions are regulated by β-catenin, vascular endothelial cadherin (VE-cadherin), and the actin cytoskeleton [96]. A recent study showed that hyperglycemia induces retinal vascular leakage by activating transglutaminase 2 (TGase2) through ROS [97]. VEGF stimulates TGase2 activity through sequential elevation of intracellular Ca2+ and ROS in endothelial cells. ROS-mediated activation of TGase2 plays a key role in VEGF-induced retinal vascular leakage by stimulating stress fiber formation and VE-cadherin disruption [97]. VEGF can also promote vascular leakage through an ROS-independent pathway. VEGFR2-mediated Src kinase activation promotes phosphorylation of FAK kinase and β-catenin, thereby facilitating VE-cadherin-β-catenin dissociation and EC junctional breakdown [98]. Similarly, the expression of semaphorin 3A, a guidance cue for neuronal axons, is upregulated in diabetic retina. Semaphorin 3A binds the VEGF co-receptor neurophilin-1 (NRP1) to stimulate the phosphorylation of Src, FAK, and VE-cadherin, and increase vascular leakage [99].
The Diabetes Control and Complications Trial (DCCT) and Epidemiology and Diabetes Interventions and Complications (EDIC) studies indicated that hyperglycemia may have long-lasting detrimental effects that are not responsive to subsequent intensive treatment, a phenomenon called “metabolic memory” [100, 101]. Changes in chromatin architecture that sensitize the genome to a diabetic milieu and cause chronic alternations in gene expression are increasingly implicated in metabolic memory of DR and other vasculopathies [102, 103]. These epigenetic regulations are mediated by covalent modifications of either DNA (e.g., cytosine methylation and hydroxymethylation) or histone proteins (e.g., acetylation, methylation, phosphorylation, and ubiquitination) [104]. However, recent studies in diabetic animals showed contradictory results for histone acetylation [105, 106]. One study found reduced global acetylation of retinal histones with activation of histone deacetylases (HDACs) and inhibition of histone acetylase (HAT), while another group showed a significant increase in retinal histone acetylation. The reasons for the discrepancy are unknown.
It is highly likely that multiple intracellular events may jointly contribute to the pathogenesis of DR and other DVCs. The relative importance of individual pathways to DR pathogenesis is not clear. The recent FDA approval of VEGF inhibitor ranibizumab for the treatment of all forms of DR suggests that anti-angiogenesis therapies can reverse some diabetic abnormalities of DR, including vascular leakage.
Molecular mechanisms of Scg3
The distinct binding and angiogenic activity patterns between Scg3 and VEGF in diabetic and control mice suggest that these two factors have different receptor signaling pathways [3]. Indeed, Scg3 does not bind VEGFR1 or VEGFR2, and it does not activate VEGFR2 [3]. Scg3 does not appear to cross talk with the VEGF pathway, and no evidence for any form of mutual or reciprocal regulation of expression levels was found [3]. Furthermore, Scg3 and VEGF activate different intracellular signaling pathways. VEGF induces the phosphorylation of MEK, ERK1/2, Akt, Src, and Stat3, whereas Scg3 activates MEK, ERK1/2 and Src kinases, but not Akt or Stat3 [3]. These findings suggest that Scg3 and VEGF bind to distinct receptors and induce different intracellular signaling pathways, which converge on MEK/ERK and Src to regulate angiogenesis and leakage (Fig. 3). Interestingly, Scg3 promoted endothelial permeability when applied to either the upper or lower chambers of trans-well inserts, suggesting that the Scg3 receptor is expressed on luminal and abluminal surface. This is similar to VEGF receptors that are also expressed on both surfaces of endothelial cells [107]. The putative Scg3 receptor is minimally expressed on normal endothelium, but markedly upregulated by diabetes, leading to the dramatic increase observed for Scg3 binding to diabetic retinal vessels [3]. Precise Scg3 receptor identity and characterization is critical to substantiate the results on Scg3 disease selectivity. Scg3 receptor identity may also allow generation of an aflibercept-like decoy receptor as an alternative strategy for anti-Scg3 therapy of DR [108].
Fig. 3.
Scg3 and VEGF have distinct receptor signaling pathways. Scg3 does not bind to VEGFR1 or VEGFR2. Scg3 cannot activate VEGFR2. VEGF activates Src, MEK, ERK1/2, Akt, and Stat3, whereas Scg3 induces the phosphorylation of Src, MEK, and ERK1/2, but not Akt or Stat3. Despite the unknown receptor of Scg3, these results suggest that Scg3 and VEGF have different receptor signaling pathways. In this regard, their inhibitors could be used for alternative or combination therapy of diabetic retinopathy
Scg3 as a therapeutic target for vascular diseases
Given that VEGF inhibitors have limited therapeutic efficacy for DR [109, 110], anti-Scg3 therapy with different mechanism of action could improve the efficacy of anti-VEGF-resistant DR through alternative or combination therapy. To investigate the therapeutic potential of Scg3 for DR, we intravitreally injected either Scg3-neutralizing polyclonal or monoclonal antibody (mAb) into streptozotocin-induced diabetic mice. Both antibodies alleviated diabetic retinal vascular leakage [3]. The therapeutic activity of anti-Scg3 mAb to inhibit DR leakage was independently verified in Ins2Akita mice with spontaneous diabetes. These results suggest that Scg3 plays an important role in diabetic retinal vascular leakage and that anti-Scg3 mAb may be further developed for clinical therapy of diabetic macular edema.
Diabetic rodents do not develop PDR, probably because of their relatively short lifespan. Mice with oxygen-induced retinopathy (OIR), a disease model of retinopathy of prematurity (ROP), are often used as a surrogate model of PDR. Both PDR and ROP are characterized by pathological RNV. Intravitreal injection of Scg3-neutralizing polyclonal antibody or mAb prevented RNV in OIR mice [3]. These results suggest that Scg3 exacerbates OIR pathogenesis and that anti-Scg3 mAb has the potential for the therapy of ROP and PDR. Similar to DR, Scg3 expression is not induced in OIR retina [3]. Based on the mechanistic models in Fig. 3, the therapeutic activity of anti-Scg3 antibodies implies that Scg3 binding to OIR vessels may also increase. This notion is yet to be experimentally validated in OIR mice by comparative ligandomics. Nonetheless, it is more appropriate to call Scg3 “disease-associated or selective”, but not “disease-specific”, angiogenic factor.
Of note, Scg2 was also identified as a DR-associated endothelial ligand by comparative ligandomics, albeit with relatively low binding to diabetic vessels (16:0 for diabetic:control) [3]. Furthermore, comparative ligandomics identified pleiotrophin as a DR-high angiogenic factor with relatively low disease selectivity (38:0 for diabetic:control) [3]. The therapeutic potential of pleiotrophin for DR and ROP was demonstrated in a recent study using pleiotrophin-neutralizing antibodies [111]. These findings suggest that comparative ligandomics is capable of identifying different disease-selective angiogenic factors to facilitate biologic drug discovery and development.
A new trend to develop disease-selective angiogenesis blockers
To date, nearly all the conventional angiogenic factors were discovered and verified based on their functional activity on normal vessels, and therefore, their agonists and antagonists target both normal and diseased vessels. For example, VEGF is markedly upregulated in the vitreous fluid of PDR patients by 36–110-fold, whereas its receptor VEGFR1 is induced only by ~1.5-fold [112, 113].
A new trend for anti-angiogenesis drug development is to target angiogenic pathways with high disease selectivity. For instance, a previous study found that CCR3, a G protein-coupled receptor (GPCR) for C-C chemokine ligands, was specifically expressed in choroidal neovascular endothelial cells with undetectable expression in normal vessels [114]. Anti-CCR3 antibodies and small-molecule antagonists inhibited choroidal neovascularization (CNV) induced by laser photocoagulation [114, 115]. However, CCR3 was not upregulated in the animal model of Matrigel-induced CNV, and therapeutic activity of CCR3 inhibitors was not detected in this disease model [116]. CCR3 is also highly expressed on normal eosinophils [117], and ablation of the CCR3 gene dysregulates the trafficking of eosinophils [118]. A recent study suggests that systemic inhibition of CCR3 may be required for CNV therapy [115]. Unfortunately, phase I clinical trial of a CCR3 antagonist was terminated [119], probably due to safety, a major setback to develop a disease-selective angiogenesis blocker. As a result, the advantages of this partially selective angiogenesis blocker have never been fully assessed in patients.
Besides angiogenic factors and their receptors, searches for disease-associated therapeutic targets have been extended to other cell surface and intracellular signaling pathways. One example is that a prion-like protein doppel was uncovered as a tumor endothelial cell-specific surface marker [120]. Doppel overexpression enhanced tumor angiogenesis by promoting VEGFR2 activation [121]. An orally active doppel-binding glycosaminoglycan was successfully developed to target tumor angiogenesis but spare physiological angiogenesis in mice [121]. This tumor-specific angiogenesis blocker has the potential advantage for targeted cancer therapy.
In another study, RUNX1, also called Aml1 or Cbfa2, was identified as a diabetes-associated angiogenic transcriptional factor by differential transcriptome analysis [122]. RUNX1 is markedly upregulated in retinal endothelial cells of PDR patients or OIR mice. Ro5-3335, an inhibitor of RUNX1, significantly inhibited OIR-induced pathological RNV. Thus, therapy targeting RUNX1 may also offer the similar advantage for targeted therapy of DR and ROP.
Like CCR3, Scg3 was discovered as a highly disease-associated angiogenic factor with undetectable binding or angiogenic activity in normal vessels but augmented binding to diseased vessels. Perhaps, the reason why Scg3 has been largely ignored as a cellular ligand for so long is because of its very low binding and angiogenic activity to normal vessels. Because of the disease selectivity, Scg3-neutralizing antibodies could be considered disease-selective angiogenesis blockers (Fig. 4), in some ways similar to selective β adrenergic blockers, for targeted therapy with minimal adverse effects on normal vessels. This advantage is especially important to ROP where therapy is required to block pathological but not physiological/developmental angiogenesis or vasculogenesis. ROP is the most common cause of vision loss in children that currently lacks an approved drug therapy [123]. Anti-VEGF drugs have been approved for other vascular diseases but not ROP. VEGF plays a critical role in vasculogenesis, and VEGF inhibitors can cause severe adverse effects in neonatal or premature retina in animals and humans [124–126]. Indeed, such side effects are predicted from the phenotypes of embryonic lethality in mice with heterozygous VEGF gene ablation [127]. This is in sharp contrast to the normal phenotype of Scg3-/- mice [65]. Therefore, we predict that anti-Scg3 antibodies for ROP therapy will be effective and safe because of its disease selectivity.
Fig. 4.
Non-selective vs. selective angiogenesis blockers. The receptors for selective angiogenic ligands (e.g., Scg3) are expressed only on the diseased but not normal endothelium, whereas the receptors for non-selective angiogenic factors (e.g., VEGF) are expressed on both diseased and normal endothelium. Selective angiogenesis blockers preferentially exert therapeutic activity on diseased vessels with minimal adverse effects on normal vessels. In contrast, non-selective angiogenesis blockers have therapeutic and detrimental effects on diseased and normal vasculature simultaneously
Perspectives
Scg3 is a multifunctional protein. It not only functions as a vesicle protein to regulate the biogenesis of secretory granules but also moonlights as an angiogenic factor. In contrast to many other conventional angiogenic factors, Scg3 is a highly selective angiogenic factor. With the emergence of comparative ligandomics technology, systematic identification of more such endothelial ligands with high disease-selective binding activity is feasible for the first time. Given the high disease selectivity of Scg3, its inhibitors may become the founding members for a new class of selective angiogenesis blockers. The potential of such reagents is supported by strong preclinical results in mice. Future endeavors should be channeled towards obtaining preclinical data in large animals and clinical studies to define the advantages of such selective inhibitors for targeted anti-angiogenesis therapy.
Acknowledgements
This work was supported by National Institutes of Health (NIH) R21EY027065 (WL), NIH Center Core Grant P30-EY014801, and an RPB unrestricted grant.
Abbreviations
- CgA
Chromogranin A
- CCR3
C-C chemokine receptor type 3
- CPE
Carboxypeptidase E
- CNV
Choroidal neovascularization
- DCG
Dense core secretory granule
- DR
Diabetic retinopathy
- HRP-3
Hepatoma-derived growth factor-related protein 3
- mAb
Monoclonal antibody
- OIR
Oxygen-induced retinopathy
- OPD
Open reading frame
- NGS
Next-generation DNA sequencing
- PDR
Proliferative diabetic retinopathy
- RNV
Retinal neovascularization
- ROP
Retinopathy of prematurity
- ROS
Reactive oxygen species
- Scg3
Secretogranin III
- TGN
Trans-Golgi network
- VEGF
Vascular endothelial growth factor
- VEGFR
VEGF receptor
- VGF
Nerve growth factor inducible protein
References
- 1.Ottiger HP, Battenberg EF, Tsou AP, Bloom FE, Sutcliffe JG. 1B1075: a brain- and pituitary-specific mRNA that encodes a novel chromogranin/secretogranin-like component of intracellular vesicles. J Neurosci. 1990;10(9):3135–3147. doi: 10.1523/JNEUROSCI.10-09-03135.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dopazo A, Lovenberg TW, Danielson PE, Ottiger HP, Sutcliffe JG. Primary structure of mouse secretogranin III and its absence from deficient mice. J Mol Neurosci. 1993;4(4):225–233. doi: 10.1007/BF02821554. [DOI] [PubMed] [Google Scholar]
- 3.LeBlanc ME, Wang W, Chen X, Caberoy NB, Guo F, Shen C, et al. Secretogranin III as a disease-associated ligand for antiangiogenic therapy of diabetic retinopathy. J Exp Med. 2017;214(4):1029–1047. doi: 10.1084/jem.20161802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Taupenot L, Harper KL, O’Connor DT. The chromogranin-secretogranin family. N Engl J Med. 2003;348(12):1134–1149. doi: 10.1056/NEJMra021405. [DOI] [PubMed] [Google Scholar]
- 5.Helle KB. The granin family of uniquely acidic proteins of the diffuse neuroendocrine system: comparative and functional aspects. Biol Rev Camb Philos Soc. 2004;79(4):769–794. doi: 10.1017/S146479310400644X. [DOI] [PubMed] [Google Scholar]
- 6.Bartolomucci A, Possenti R, Mahata SK, Fischer-Colbrie R, Loh YP, Salton SR. The extended granin family: structure, function, and biomedical implications. Endocr Rev. 2011;32(6):755–797. doi: 10.1210/er.2010-0027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Helle KB, Corti A. Chromogranin A: a paradoxical player in angiogenesis and vascular biology. Cell Mol Life Sci. 2015;72(2):339–348. doi: 10.1007/s00018-014-1750-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Winkler H, Westhead E. The molecular organization of adrenal chromaffin granules. Neuroscience. 1980;5(11):1803–1823. doi: 10.1016/0306-4522(80)90031-7. [DOI] [PubMed] [Google Scholar]
- 9.Helle KB. The chromogranins. Historical perspectives. Adv Exp Med Biol. 2000;482:3–20. doi: 10.1007/0-306-46837-9_1. [DOI] [PubMed] [Google Scholar]
- 10.Winkler H, Fischer-Colbrie R. The chromogranins A and B: the first 25 years and future perspectives. Neuroscience. 1992;49(3):497–528. doi: 10.1016/0306-4522(92)90222-N. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.O’Connor DT, Frigon RP. Chromogranin A, the major catecholamine storage vesicle soluble protein. Multiple size forms, subcellular storage, and regional distribution in chromaffin and nervous tissue elucidated by radioimmunoassay. J Biol Chem. 1984;259(5):3237–3247. [PubMed] [Google Scholar]
- 12.Hosaka M, Watanabe T. Secretogranin III: a bridge between core hormone aggregates and the secretory granule membrane. Endocr J. 2010;57(4):275–286. doi: 10.1507/endocrj.K10E-038. [DOI] [PubMed] [Google Scholar]
- 13.Neuhold N, Ullrich R. Secretogranin IV immunoreactivity in medullary thyroid carcinoma: an immunohistochemical study of 62 cases. Virchows Arch A Pathol Anat Histopathol. 1993;423(2):85–89. doi: 10.1007/BF01606581. [DOI] [PubMed] [Google Scholar]
- 14.Kelly RB. Pathways of protein secretion in eukaryotes. Science. 1985;230(4721):25–32. doi: 10.1126/science.2994224. [DOI] [PubMed] [Google Scholar]
- 15.D’Amico MA, Ghinassi B, Izzicupo P, Manzoli L, Di Baldassarre A. Biological function and clinical relevance of chromogranin A and derived peptides. Endocr Connect. 2014;3(2):R45–R54. doi: 10.1530/EC-14-0027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lorenz K, Troger J, Gramlich O, Grus F, Hattmannstorfer R, Fischer-Colbrie R, et al. PE-11, a peptide derived from chromogranin B, in the rat eye. Peptides. 2011;32(6):1201–1206. doi: 10.1016/j.peptides.2011.03.011. [DOI] [PubMed] [Google Scholar]
- 17.Strub JM, Garcia-Sablone P, Lonning K, Taupenot L, Hubert P, Van Dorsselaer A, et al. Processing of chromogranin B in bovine adrenal medulla. Identification of secretolytin, the endogenous C-terminal fragment of residues 614–626 with antibacterial activity. Eur J Biochem. 1995;229(2):356–368. doi: 10.1111/j.1432-1033.1995.tb20476.x. [DOI] [PubMed] [Google Scholar]
- 18.Flanagan T, Taylor L, Poulter L, Viveros OH, Diliberto EJ., Jr A novel 1745-dalton pyroglutamyl peptide derived from chromogranin B is in the bovine adrenomedullary chromaffin vesicle. Cell Mol Neurobiol. 1990;10(4):507–523. doi: 10.1007/BF00712845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kirchmair R, Egger M, Walter DH, Eisterer W, Niederwanger A, Woell E, et al. Secretoneurin, an angiogenic neuropeptide, induces postnatal vasculogenesis. Circulation. 2004;110(9):1121–1127. doi: 10.1161/01.CIR.0000139884.81390.56. [DOI] [PubMed] [Google Scholar]
- 20.Holthuis JC, Jansen EJ, Martens GJ. Secretogranin III is a sulfated protein undergoing proteolytic processing in the regulated secretory pathway. J Biol Chem. 1996;271(30):17755–17760. doi: 10.1074/jbc.271.30.17755. [DOI] [PubMed] [Google Scholar]
- 21.Dowling P, Shields W, Rani S, Meleady P, Henry M, Jeppesen P, et al. Proteomic analysis of conditioned media from glucose responsive and glucose non-responsive phenotypes reveals a panel of secreted proteins associated with beta cell dysfunction. Electrophoresis. 2008;29(20):4141–4149. doi: 10.1002/elps.200800152. [DOI] [PubMed] [Google Scholar]
- 22.Rong YP, Liu F, Zeng LC, Ma WJ, Wei DZ, Han ZG. Cloning and characterization of a novel human secretory protein: secretogranin III. Sheng Wu Hua Xue Yu Sheng Wu Wu Li Xue Bao (Shanghai) 2002;34(4):411–417. [PubMed] [Google Scholar]
- 23.Sanchez-Margalet V, Calvo JR, Goberna R. Glucogenolytic and hyperglycemic effect of 33–49 C-terminal fragment of pancreastatin in the rat in vivo. Horm Metab Res. 1992;24(10):455–457. doi: 10.1055/s-2007-1003361. [DOI] [PubMed] [Google Scholar]
- 24.Tatemoto K, Efendic S, Mutt V, Makk G, Feistner GJ, Barchas JD. Pancreastatin, a novel pancreatic peptide that inhibits insulin secretion. Nature. 1986;324(6096):476–478. doi: 10.1038/324476a0. [DOI] [PubMed] [Google Scholar]
- 25.Gonzalez-Yanes C, Sanchez-Margalet V. Pancreastatin modulates insulin signaling in rat adipocytes: mechanisms of cross-talk. Diabetes. 2000;49(8):1288–1294. doi: 10.2337/diabetes.49.8.1288. [DOI] [PubMed] [Google Scholar]
- 26.Gayen JR, Saberi M, Schenk S, Biswas N, Vaingankar SM, Cheung WW, et al. A novel pathway of insulin sensitivity in chromogranin A null mice: a crucial role for pancreastatin in glucose homeostasis. J Biol Chem. 2009;284(42):28498–28509. doi: 10.1074/jbc.M109.020636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.O’Connor DT, Cadman PE, Smiley C, Salem RM, Rao F, Smith J, et al. Pancreastatin: multiple actions on human intermediary metabolism in vivo, variation in disease, and naturally occurring functional genetic polymorphism. J Clin Endocrinol Metab. 2005;90(9):5414–5425. doi: 10.1210/jc.2005-0408. [DOI] [PubMed] [Google Scholar]
- 28.Mahata SK, O’Connor DT, Mahata M, Yoo SH, Taupenot L, Wu H, et al. Novel autocrine feedback control of catecholamine release. A discrete chromogranin a fragment is a noncompetitive nicotinic cholinergic antagonist. J Clin Investig. 1997;100(6):1623–1633. doi: 10.1172/JCI119686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kennedy BP, Mahata SK, O’Connor DT, Ziegler MG. Mechanism of cardiovascular actions of the chromogranin A fragment catestatin in vivo. Peptides. 1998;19(7):1241–1248. doi: 10.1016/S0196-9781(98)00086-2. [DOI] [PubMed] [Google Scholar]
- 30.Egger M, Beer AG, Theurl M, Schgoer W, Hotter B, Tatarczyk T, et al. Monocyte migration: a novel effect and signaling pathways of catestatin. Eur J Pharmacol. 2008;598(1–3):104–111. doi: 10.1016/j.ejphar.2008.09.016. [DOI] [PubMed] [Google Scholar]
- 31.Aslam R, Atindehou M, Lavaux T, Haikel Y, Schneider F, Metz-Boutigue MH. Chromogranin A-derived peptides are involved in innate immunity. Curr Med Chem. 2012;19(24):4115–4123. doi: 10.2174/092986712802430063. [DOI] [PubMed] [Google Scholar]
- 32.O’Connor DT, Kailasam MT, Kennedy BP, Ziegler MG, Yanaihara N, Parmer RJ. Early decline in the catecholamine release-inhibitory peptide catestatin in humans at genetic risk of hypertension. J Hypertens. 2002;20(7):1335–1345. doi: 10.1097/00004872-200207000-00020. [DOI] [PubMed] [Google Scholar]
- 33.Takiyyuddin MA, Parmer RJ, Kailasam MT, Cervenka JH, Kennedy B, Ziegler MG, et al. Chromogranin A in human hypertension. Influence of heredity. Hypertension. 1995;26(1):213–220. doi: 10.1161/01.HYP.26.1.213. [DOI] [PubMed] [Google Scholar]
- 34.You ZB, Saria A, Fischer-Colbrie R, Terenius L, Goiny M, Herrera-Marschitz M. Effects of secretogranin II-derived peptides on the release of neurotransmitters monitored in the basal ganglia of the rat with in vivo microdialysis. Naunyn Schmiedebergs Arch Pharmacol. 1996;354(6):717–724. doi: 10.1007/BF00166897. [DOI] [PubMed] [Google Scholar]
- 35.Zhao E, Basak A, Wong AO, Ko W, Chen A, Lopez GC, et al. The secretogranin II-derived peptide secretoneurin stimulates luteinizing hormone secretion from gonadotrophs. Endocrinology. 2009;150(5):2273–2282. doi: 10.1210/en.2008-1060. [DOI] [PubMed] [Google Scholar]
- 36.Fischer-Colbrie R, Laslop A, Kirchmair R. Secretogranin II: molecular properties, regulation of biosynthesis and processing to the neuropeptide secretoneurin. Prog Neurobiol. 1995;46(1):49–70. doi: 10.1016/0301-0082(94)00060-U. [DOI] [PubMed] [Google Scholar]
- 37.Storch MK, Fischer-Colbrie R, Smith T, Rinner WA, Hickey WF, Cuzner ML, et al. Co-localization of secretoneurin immunoreactivity and macrophage infiltration in the lesions of experimental autoimmune encephalomyelitis. Neuroscience. 1996;71(3):885–893. doi: 10.1016/0306-4522(95)00476-9. [DOI] [PubMed] [Google Scholar]
- 38.Hahm S, Mizuno TM, Wu TJ, Wisor JP, Priest CA, Kozak CA, et al. Targeted deletion of the Vgf gene indicates that the encoded secretory peptide precursor plays a novel role in the regulation of energy balance. Neuron. 1999;23(3):537–548. doi: 10.1016/S0896-6273(00)80806-5. [DOI] [PubMed] [Google Scholar]
- 39.Watson E, Fargali S, Okamoto H, Sadahiro M, Gordon RE, Chakraborty T, et al. Analysis of knockout mice suggests a role for VGF in the control of fat storage and energy expenditure. BMC Physiol. 2009;9:19. doi: 10.1186/1472-6793-9-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Watson E, Hahm S, Mizuno TM, Windsor J, Montgomery C, Scherer PE, et al. VGF ablation blocks the development of hyperinsulinemia and hyperglycemia in several mouse models of obesity. Endocrinology. 2005;146(12):5151–5163. doi: 10.1210/en.2005-0588. [DOI] [PubMed] [Google Scholar]
- 41.Bartolomucci A, La Corte G, Possenti R, Locatelli V, Rigamonti AE, Torsello A, et al. TLQP-21, a VGF-derived peptide, increases energy expenditure and prevents the early phase of diet-induced obesity. Proc Natl Acad Sci USA. 2006;103(39):14584–14589. doi: 10.1073/pnas.0606102103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bartolomucci A, Bresciani E, Bulgarelli I, Rigamonti AE, Pascucci T, Levi A, et al. Chronic intracerebroventricular injection of TLQP-21 prevents high fat diet induced weight gain in fast weight-gaining mice. Genes Nutr. 2009;4(1):49–57. doi: 10.1007/s12263-009-0110-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sibilia V, Pagani F, Bulgarelli I, Tulipano G, Possenti R, Guidobono F. Characterization of the mechanisms involved in the gastric antisecretory effect of TLQP-21, a vgf-derived peptide, in rats. Amino Acids. 2012;42(4):1261–1268. doi: 10.1007/s00726-010-0818-6. [DOI] [PubMed] [Google Scholar]
- 44.Severini C, La Corte G, Improta G, Broccardo M, Agostini S, Petrella C, et al. In vitro and in vivo pharmacological role of TLQP-21, a VGF-derived peptide, in the regulation of rat gastric motor functions. Br J Pharmacol. 2009;157(6):984–993. doi: 10.1111/j.1476-5381.2009.00192.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sibilia V, Pagani F, Bulgarelli I, Mrak E, Broccardo M, Improta G, et al. TLQP-21, a VGF-derived peptide, prevents ethanol-induced gastric lesions: insights into its mode of action. Neuroendocrinology. 2010;92(3):189–197. doi: 10.1159/000319791. [DOI] [PubMed] [Google Scholar]
- 46.Bozdagi O, Rich E, Tronel S, Sadahiro M, Patterson K, Shapiro ML, et al. The neurotrophin-inducible gene Vgf regulates hippocampal function and behavior through a brain-derived neurotrophic factor-dependent mechanism. J Neurosci. 2008;28(39):9857–9869. doi: 10.1523/JNEUROSCI.3145-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Toshinai K, Yamaguchi H, Kageyama H, Matsuo T, Koshinaka K, Sasaki K, et al. Neuroendocrine regulatory peptide-2 regulates feeding behavior via the orexin system in the hypothalamus. Am J Physiol Endocrinol Metab. 2010;299(3):E394–E401. doi: 10.1152/ajpendo.00768.2009. [DOI] [PubMed] [Google Scholar]
- 48.Yamaguchi H, Sasaki K, Satomi Y, Shimbara T, Kageyama H, Mondal MS, et al. Peptidomic identification and biological validation of neuroendocrine regulatory peptide-1 and -2. J Biol Chem. 2007;282(36):26354–26360. doi: 10.1074/jbc.M701665200. [DOI] [PubMed] [Google Scholar]
- 49.Ferri GL, Levi A, Possenti R. A novel neuroendocrine gene product: selective VGF8a gene expression and immuno-localisation of the VGF protein in endocrine and neuronal populations. Brain Res Mol Brain Res. 1992;13(1–2):139–143. doi: 10.1016/0169-328X(92)90053-E. [DOI] [PubMed] [Google Scholar]
- 50.Moss A, Ingram R, Koch S, Theodorou A, Low L, Baccei M, et al. Origins, actions and dynamic expression patterns of the neuropeptide VGF in rat peripheral and central sensory neurones following peripheral nerve injury. Mol Pain. 2008;4:62. doi: 10.1186/1744-8069-4-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Costigan M, Befort K, Karchewski L, Griffin RS, D’Urso D, Allchorne A, et al. Replicate high-density rat genome oligonucleotide microarrays reveal hundreds of regulated genes in the dorsal root ganglion after peripheral nerve injury. BMC Neurosci. 2002;3:16. doi: 10.1186/1471-2202-3-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Riedl MS, Braun PD, Kitto KF, Roiko SA, Anderson LB, Honda CN, et al. Proteomic analysis uncovers novel actions of the neurosecretory protein VGF in nociceptive processing. J Neurosci. 2009;29(42):13377–13388. doi: 10.1523/JNEUROSCI.1127-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Rizzi R, Bartolomucci A, Moles A, D’Amato F, Sacerdote P, Levi A, et al. The VGF-derived peptide TLQP-21: a new modulatory peptide for inflammatory pain. Neurosci Lett. 2008;441(1):129–133. doi: 10.1016/j.neulet.2008.06.018. [DOI] [PubMed] [Google Scholar]
- 54.Hunsberger JG, Newton SS, Bennett AH, Duman CH, Russell DS, Salton SR, et al. Antidepressant actions of the exercise-regulated gene VGF. Nat Med. 2007;13(12):1476–1482. doi: 10.1038/nm1669. [DOI] [PubMed] [Google Scholar]
- 55.Thakker-Varia S, Krol JJ, Nettleton J, Bilimoria PM, Bangasser DA, Shors TJ, et al. The neuropeptide VGF produces antidepressant-like behavioral effects and enhances proliferation in the hippocampus. J Neurosci. 2007;27(45):12156–12167. doi: 10.1523/JNEUROSCI.1898-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Succu S, Cocco C, Mascia MS, Melis T, Melis MR, Possenti R, et al. Pro-VGF-derived peptides induce penile erection in male rats: possible involvement of oxytocin. Eur J Neurosci. 2004;20(11):3035–3040. doi: 10.1111/j.1460-9568.2004.03781.x. [DOI] [PubMed] [Google Scholar]
- 57.Succu S, Mascia MS, Melis T, Sanna F, Melis MR, Possenti R, et al. Pro-VGF-derived peptides induce penile erection in male rats: involvement of paraventricular nitric oxide. Neuropharmacology. 2005;49(7):1017–1025. doi: 10.1016/j.neuropharm.2005.05.015. [DOI] [PubMed] [Google Scholar]
- 58.Lee SN, Lindberg I. 7B2 prevents unfolding and aggregation of prohormone convertase 2. Endocrinology. 2008;149(8):4116–4127. doi: 10.1210/en.2008-0064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Qian Y, Devi LA, Mzhavia N, Munzer S, Seidah NG, Fricker LD. The C-terminal region of proSAAS is a potent inhibitor of prohormone convertase 1. J Biol Chem. 2000;275(31):23596–23601. doi: 10.1074/jbc.M001583200. [DOI] [PubMed] [Google Scholar]
- 60.Holthuis JC, Martens GJ. The neuroendocrine proteins secretogranin II and III are regionally conserved and coordinately expressed with proopiomelanocortin in Xenopus intermediate pituitary. J Neurochem. 1996;66(6):2248–2256. doi: 10.1046/j.1471-4159.1996.66062248.x. [DOI] [PubMed] [Google Scholar]
- 61.Hosaka M, Watanabe T, Sakai Y, Uchiyama Y, Takeuchi T. Identification of a chromogranin A domain that mediates binding to secretogranin III and targeting to secretory granules in pituitary cells and pancreatic beta-cells. Mol Biol Cell. 2002;13(10):3388–3399. doi: 10.1091/mbc.02-03-0040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hosaka M, Suda M, Sakai Y, Izumi T, Watanabe T, Takeuchi T. Secretogranin III binds to cholesterol in the secretory granule membrane as an adapter for chromogranin A. J Biol Chem. 2004;279(5):3627–3634. doi: 10.1074/jbc.M310104200. [DOI] [PubMed] [Google Scholar]
- 63.Hosaka M, Watanabe T, Sakai Y, Kato T, Takeuchi T. Interaction between secretogranin III and carboxypeptidase E facilitates prohormone sorting within secretory granules. J Cell Sci. 2005;118(Pt 20):4785–4795. doi: 10.1242/jcs.02608. [DOI] [PubMed] [Google Scholar]
- 64.Tanabe A, Yanagiya T, Iida A, Saito S, Sekine A, Takahashi A, et al. Functional single-nucleotide polymorphisms in the secretogranin III (SCG3) gene that form secretory granules with appetite-related neuropeptides are associated with obesity. J Clin Endocrinol Metab. 2007;92(3):1145–1154. doi: 10.1210/jc.2006-1808. [DOI] [PubMed] [Google Scholar]
- 65.Kingsley DM, Rinchik EM, Russell LB, Ottiger HP, Sutcliffe JG, Copeland NG, et al. Genetic ablation of a mouse gene expressed specifically in brain. EMBO J. 1990;9(2):395–399. doi: 10.1002/j.1460-2075.1990.tb08123.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.LeBlanc ME, Wang W, Caberoy NB, Chen X, Guo F, Alvarado G, et al. Hepatoma-derived growth factor-related protein-3 is a novel angiogenic factor. PLoS One. 2015;10(5):e0127904. doi: 10.1371/journal.pone.0127904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Guo F, Ding Y, Caberoy N, Alvarado G, Wang F, Chen R, et al. ABCF1 extrinsically regulates retinal pigment epithelial cell phagocytosis. Mol Biol Cell. 2015;26(12):2311–2320. doi: 10.1091/mbc.E14-09-1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ding Y, Caberoy NB, Guo F, LeBlanc ME, Zhang C, Wang W, et al. Reticulocalbin-1 facilitates microglial phagocytosis. PLoS One. 2015;10(5):e0126993. doi: 10.1371/journal.pone.0126993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Tota B, Angelone T, Cerra MC. The surging role of chromogranin A in cardiovascular homeostasis. Front Chem. 2014;2:64. doi: 10.3389/fchem.2014.00064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Crippa L, Bianco M, Colombo B, Gasparri AM, Ferrero E, Loh YP, et al. A new chromogranin A-dependent angiogenic switch activated by thrombin. Blood. 2013;121(2):392–402. doi: 10.1182/blood-2012-05-430314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ferrero E, Scabini S, Magni E, Foglieni C, Belloni D, Colombo B, et al. Chromogranin A protects vessels against tumor necrosis factor alpha-induced vascular leakage. FASEB J. 2004;18(3):554–556. doi: 10.1096/fj.03-0922fje. [DOI] [PubMed] [Google Scholar]
- 72.Blois A, Srebro B, Mandala M, Corti A, Helle KB, Serck-Hanssen G. The chromogranin A peptide vasostatin-I inhibits gap formation and signal transduction mediated by inflammatory agents in cultured bovine pulmonary and coronary arterial endothelial cells. Regul Pept. 2006;135(1–2):78–84. doi: 10.1016/j.regpep.2006.04.007. [DOI] [PubMed] [Google Scholar]
- 73.Theurl M, Schgoer W, Albrecht K, Jeschke J, Egger M, Beer AG, et al. The neuropeptide catestatin acts as a novel angiogenic cytokine via a basic fibroblast growth factor-dependent mechanism. Circ Res. 2010;107(11):1326–1335. doi: 10.1161/CIRCRESAHA.110.219493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ji L, Pei ZQ, Ma DF, Zhang J, Su JS, Gao XD, et al. Prognostic value of circulating catestatin levels for in-hospital heart failure in patients with acute myocardial infarction. Zhonghua Xin Xue Guan Bing Za Zhi. 2012;40(11):914–919. [PubMed] [Google Scholar]
- 75.Meng L, Wang J, Ding WH, Han P, Yang Y, Qi LT, et al. Plasma catestatin level in patients with acute myocardial infarction and its correlation with ventricular remodelling. Postgrad Med J. 1050;2013(89):193–196. doi: 10.1136/postgradmedj-2012-131060. [DOI] [PubMed] [Google Scholar]
- 76.Kirchmair R, Gander R, Egger M, Hanley A, Silver M, Ritsch A, et al. The neuropeptide secretoneurin acts as a direct angiogenic cytokine in vitro and in vivo. Circulation. 2004;109(6):777–783. doi: 10.1161/01.CIR.0000112574.07422.C1. [DOI] [PubMed] [Google Scholar]
- 77.Albrecht-Schgoer K, Schgoer W, Holfeld J, Theurl M, Wiedemann D, Steger C, et al. The angiogenic factor secretoneurin induces coronary angiogenesis in a model of myocardial infarction by stimulation of vascular endothelial growth factor signaling in endothelial cells. Circulation. 2012;126(21):2491–2501. doi: 10.1161/CIRCULATIONAHA.111.076950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Yau JW, Rogers SL, Kawasaki R, Lamoureux EL, Kowalski JW, Bek T, et al. Global prevalence and major risk factors of diabetic retinopathy. Diabetes Care. 2012;35(3):556–564. doi: 10.2337/dc11-1909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Wong TY, Cheung CM, Larsen M, Sharma S, Simo R. Diabetic retinopathy. Nat Rev Dis Primers. 2016;2:16012. doi: 10.1038/nrdp.2016.12. [DOI] [PubMed] [Google Scholar]
- 80.Suzuma K, Takahara N, Suzuma I, Isshiki K, Ueki K, Leitges M, et al. Characterization of protein kinase C beta isoform’s action on retinoblastoma protein phosphorylation, vascular endothelial growth factor-induced endothelial cell proliferation, and retinal neovascularization. Proc Natl Acad Sci USA. 2002;99(2):721–726. doi: 10.1073/pnas.022644499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Geraldes P, Hiraoka-Yamamoto J, Matsumoto M, Clermont A, Leitges M, Marette A, et al. Activation of PKC-delta and SHP-1 by hyperglycemia causes vascular cell apoptosis and diabetic retinopathy. Nat Med. 2009;15(11):1298–1306. doi: 10.1038/nm.2052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Ohshiro Y, Ma RC, Yasuda Y, Hiraoka-Yamamoto J, Clermont AC, Isshiki K, et al. Reduction of diabetes-induced oxidative stress, fibrotic cytokine expression, and renal dysfunction in protein kinase Cbeta-null mice. Diabetes. 2006;55(11):3112–3120. doi: 10.2337/db06-0895. [DOI] [PubMed] [Google Scholar]
- 83.Harja E, Chang JS, Lu Y, Leitges M, Zou YS, Schmidt AM, et al. Mice deficient in PKCbeta and apolipoprotein E display decreased atherosclerosis. FASEB J. 2009;23(4):1081–1091. doi: 10.1096/fj.08-120345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Aiello LP, Bursell SE, Clermont A, Duh E, Ishii H, Takagi C, et al. Vascular endothelial growth factor-induced retinal permeability is mediated by protein kinase C in vivo and suppressed by an orally effective beta-isoform-selective inhibitor. Diabetes. 1997;46(9):1473–1480. doi: 10.2337/diab.46.9.1473. [DOI] [PubMed] [Google Scholar]
- 85.Ishii H, Jirousek MR, Koya D, Takagi C, Xia P, Clermont A, et al. Amelioration of vascular dysfunctions in diabetic rats by an oral PKC beta inhibitor. Science. 1996;272(5262):728–731. doi: 10.1126/science.272.5262.728. [DOI] [PubMed] [Google Scholar]
- 86.Aiello LP, Vignati L, Sheetz MJ, Zhi X, Girach A, Davis MD, et al. Oral protein kinase c beta inhibition using ruboxistaurin: efficacy, safety, and causes of vision loss among 813 patients (1,392 eyes) with diabetic retinopathy in the Protein Kinase C beta Inhibitor-Diabetic Retinopathy Study and the Protein Kinase C beta Inhibitor-Diabetic Retinopathy Study 2. Retina. 2011;31(10):2084–2094. doi: 10.1097/IAE.0b013e3182111669. [DOI] [PubMed] [Google Scholar]
- 87.Tuttle KR, Bakris GL, Toto RD, McGill JB, Hu K, Anderson PW. The effect of ruboxistaurin on nephropathy in type 2 diabetes. Diabetes Care. 2005;28(11):2686–2690. doi: 10.2337/diacare.28.11.2686. [DOI] [PubMed] [Google Scholar]
- 88.Yan SF, Ramasamy R, Schmidt AM. The RAGE axis: a fundamental mechanism signaling danger to the vulnerable vasculature. Circ Res. 2010;106(5):842–853. doi: 10.1161/CIRCRESAHA.109.212217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Yamamoto Y, Kato I, Doi T, Yonekura H, Ohashi S, Takeuchi M, et al. Development and prevention of advanced diabetic nephropathy in RAGE-overexpressing mice. J Clin Investig. 2001;108(2):261–268. doi: 10.1172/JCI11771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Park L, Raman KG, Lee KJ, Lu Y, Ferran LJ, Jr, Chow WS, et al. Suppression of accelerated diabetic atherosclerosis by the soluble receptor for advanced glycation endproducts. Nat Med. 1998;4(9):1025–1031. doi: 10.1038/2012. [DOI] [PubMed] [Google Scholar]
- 91.Brownlee M. Biochemistry and molecular cell biology of diabetic complications. Nature. 2001;414(6865):813–820. doi: 10.1038/414813a. [DOI] [PubMed] [Google Scholar]
- 92.Xu Y, Zhang Z, Hu J, Stillman IE, Leopold JA, Handy DE, et al. Glucose-6-phosphate dehydrogenase-deficient mice have increased renal oxidative stress and increased albuminuria. FASEB J. 2010;24(2):609–616. doi: 10.1096/fj.09-135731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Giacco F, Brownlee M. Oxidative stress and diabetic complications. Circ Res. 2010;107(9):1058–1070. doi: 10.1161/CIRCRESAHA.110.223545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Lassegue B, San Martin A, Griendling KK. Biochemistry, physiology, and pathophysiology of NADPH oxidases in the cardiovascular system. Circ Res. 2012;110(10):1364–1390. doi: 10.1161/CIRCRESAHA.111.243972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Breton-Romero R, Lamas S. Hydrogen peroxide signaling in vascular endothelial cells. Redox Biol. 2014;2:529–534. doi: 10.1016/j.redox.2014.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Sukriti S, Tauseef M, Yazbeck P, Mehta D. Mechanisms regulating endothelial permeability. Pulm Circ. 2014;4(4):535–551. doi: 10.1086/677356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Lee YJ, Jung SH, Kim SH, Kim MS, Lee S, Hwang J, et al. Essential role of transglutaminase 2 in vascular endothelial growth factor-induced vascular leakage in the retina of diabetic mice. Diabetes. 2016;65(8):2414–2428. doi: 10.2337/db15-1594. [DOI] [PubMed] [Google Scholar]
- 98.Chen XL, Nam JO, Jean C, Lawson C, Walsh CT, Goka E, et al. VEGF-induced vascular permeability is mediated by FAK. Dev Cell. 2012;22(1):146–157. doi: 10.1016/j.devcel.2011.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Cerani A, Tetreault N, Menard C, Lapalme E, Patel C, Sitaras N, et al. Neuron-derived semaphorin 3A is an early inducer of vascular permeability in diabetic retinopathy via neuropilin-1. Cell Metab. 2013;18(4):505–518. doi: 10.1016/j.cmet.2013.09.003. [DOI] [PubMed] [Google Scholar]
- 100.Diabetes Control Complications Trial/Epidemiology of Diabetes Interventions Complications Research Group. Lachin JM, Genuth S, Cleary P, Davis MD, Nathan DM. Retinopathy and nephropathy in patients with type 1 diabetes four years after a trial of intensive therapy. N Engl J Med. 2000;342(6):381–389. doi: 10.1056/NEJM200002103420603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Nathan DM, Cleary PA, Backlund JY, Genuth SM, Lachin JM, Orchard TJ, et al. Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes. N Engl J Med. 2005;353(25):2643–2653. doi: 10.1056/NEJMoa052187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Brasacchio D, Okabe J, Tikellis C, Balcerczyk A, George P, Baker EK, et al. Hyperglycemia induces a dynamic cooperativity of histone methylase and demethylase enzymes associated with gene-activating epigenetic marks that coexist on the lysine tail. Diabetes. 2009;58(5):1229–1236. doi: 10.2337/db08-1666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Kowluru RA. Diabetic retinopathy, metabolic memory and epigenetic modifications. Vis Res. 2017 doi: 10.1016/j.visres.2017.02.011. [DOI] [PubMed] [Google Scholar]
- 104.Keating ST, Plutzky J, El-Osta A. Epigenetic changes in diabetes and cardiovascular risk. Circ Res. 2016;118(11):1706–1722. doi: 10.1161/CIRCRESAHA.116.306819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Zhong Q, Kowluru RA. Role of histone acetylation in the development of diabetic retinopathy and the metabolic memory phenomenon. J Cell Biochem. 2010;110(6):1306–1313. doi: 10.1002/jcb.22644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Kadiyala CS, Zheng L, Du Y, Yohannes E, Kao HY, Miyagi M, et al. Acetylation of retinal histones in diabetes increases inflammatory proteins: effects of minocycline and manipulation of histone acetyltransferase (HAT) and histone deacetylase (HDAC) J Biol Chem. 2012;287(31):25869–25880. doi: 10.1074/jbc.M112.375204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Stefanini MO, Wu FT, Mac Gabhann F, Popel AS. The presence of VEGF receptors on the luminal surface of endothelial cells affects VEGF distribution and VEGF signaling. PLoS Comput Biol. 2009;5(12):e1000622. doi: 10.1371/journal.pcbi.1000622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Holash J, Davis S, Papadopoulos N, Croll SD, Ho L, Russell M, et al. VEGF-Trap: a VEGF blocker with potent antitumor effects. Proc Natl Acad Sci USA. 2002;99(17):11393–11398. doi: 10.1073/pnas.172398299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Stewart MW. Treatment of diabetic retinopathy: recent advances and unresolved challenges. World J Diabetes. 2016;7(16):333–341. doi: 10.4239/wjd.v7.i16.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Diabetic Retinopathy Clinical Research Network. Wells JA, Glassman AR, Ayala AR, Jampol LM, Aiello LP, et al. Aflibercept, bevacizumab, or ranibizumab for diabetic macular edema. N Engl J Med. 2015;372(13):1193–1203. doi: 10.1056/NEJMoa1414264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Wang W, LeBlanc ME, Chen X, Chen P, Ji Y, Brewer M, et al. Pathogenic role and therapeutic potential of pleiotrophin in mouse models of ocular vascular disease. Angiogenesis. 2017 doi: 10.1007/s10456-017-9557-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Aiello LP, Avery RL, Arrigg PG, Keyt BA, Jampel HD, Shah ST, et al. Vascular endothelial growth factor in ocular fluid of patients with diabetic retinopathy and other retinal disorders. N Engl J Med. 1994;331(22):1480–1487. doi: 10.1056/NEJM199412013312203. [DOI] [PubMed] [Google Scholar]
- 113.Matsunaga N, Chikaraishi Y, Izuta H, Ogata N, Shimazawa M, Matsumura M, et al. Role of soluble vascular endothelial growth factor receptor-1 in the vitreous in proliferative diabetic retinopathy. Ophthalmology. 2008;115(11):1916–1922. doi: 10.1016/j.ophtha.2008.06.025. [DOI] [PubMed] [Google Scholar]
- 114.Takeda A, Baffi JZ, Kleinman ME, Cho WG, Nozaki M, Yamada K, et al. CCR3 is a target for age-related macular degeneration diagnosis and therapy. Nature. 2009;460(7252):225–230. doi: 10.1038/nature08151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Nagai N, Ju M, Izumi-Nagai K, Robbie SJ, Bainbridge JW, Gale DC, et al. Novel CCR3 antagonists are effective mono- and combination inhibitors of choroidal neovascular growth and vascular permeability. Am J Pathol. 2015;185(9):2534–2549. doi: 10.1016/j.ajpath.2015.04.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Li Y, Huang D, Xia X, Wang Z, Luo L, Wen R. CCR3 and choroidal neovascularization. PLoS One. 2011;6(2):e17106. doi: 10.1371/journal.pone.0017106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Murphy K. Janeway’s immunobiology. 9. New York: GS Garland Science, Taylor & Francis Group; 2017. [Google Scholar]
- 118.Humbles AA, Lu B, Friend DS, Okinaga S, Lora J, Al-Garawi A, et al. The murine CCR3 receptor regulates both the role of eosinophils and mast cells in allergen-induced airway inflammation and hyperresponsiveness. Proc Natl Acad Sci USA. 2002;99(3):1479–1484. doi: 10.1073/pnas.261462598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.ClinicalTrial.gov. GW824575 first time in human (ClinicalTrials.gov Identifier: NCT01551771). https://clinicaltrials.gov/ct2/show/NCT01551771?term=age-related+macular+degeneration+AND+CCR3&rank=1
- 120.Seaman S, Stevens J, Yang MY, Logsdon D, Graff-Cherry C, St Croix B. Genes that distinguish physiological and pathological angiogenesis. Cancer Cell. 2007;11(6):539–554. doi: 10.1016/j.ccr.2007.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Al-Hilal TA, Chung SW, Choi JU, Alam F, Park J, Kim SW, et al. Targeting prion-like protein doppel selectively suppresses tumor angiogenesis. J Clin Investig. 2016;126(4):1251–1266. doi: 10.1172/JCI83427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Lam JD, Oh DJ, Wong LL, Amarnani D, Park-Windhol C, Sanchez AV, et al. Identification of RUNX1 as a mediator of aberrant retinal angiogenesis. Diabetes. 2017 doi: 10.2337/db16-1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Hellstrom A, Smith LE, Dammann O. Retinopathy of prematurity. Lancet. 2013;382(9902):1445–1457. doi: 10.1016/S0140-6736(13)60178-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Lepore D, Quinn GE, Molle F, Baldascino A, Orazi L, Sammartino M, et al. Intravitreal bevacizumab versus laser treatment in type 1 retinopathy of prematurity: report on fluorescein angiographic findings. Ophthalmology. 2014;121(11):2212–2219. doi: 10.1016/j.ophtha.2014.05.015. [DOI] [PubMed] [Google Scholar]
- 125.Lutty GA, McLeod DS, Bhutto I, Wiegand SJ. Effect of VEGF trap on normal retinal vascular development and oxygen-induced retinopathy in the dog. Investig Ophthalmol Vis Sci. 2011;52(7):4039–4047. doi: 10.1167/iovs.10-6798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Tokunaga CC, Mitton KP, Dailey W, Massoll C, Roumayah K, Guzman E, et al. Effects of anti-VEGF treatment on the recovery of the developing retina following oxygen-induced retinopathy. Investig Ophthalmol Vis Sci. 2014;55(3):1884–1892. doi: 10.1167/iovs.13-13397. [DOI] [PubMed] [Google Scholar]
- 127.Ferrara N, Carver-Moore K, Chen H, Dowd M, Lu L, O’Shea KS, et al. Heterozygous embryonic lethality induced by targeted inactivation of the VEGF gene. Nature. 1996;380(6573):439–442. doi: 10.1038/380439a0. [DOI] [PubMed] [Google Scholar]