Supplemental Digital Content is Available in the Text.
The link between pain catastrophizing and the differential effect of the components magnification and helplessness on brain morphology in patients with low back pain
Keywords: Pain Catastrophizing, Voxel-Based Morphometry, Magnification, Helplessness, Low back pain
Abstract
Introduction:
Pain catastrophizing (PC), the increased attention to harmful aspects of pain (magnification), and the belief of low controllability (helplessness) has been shown to be important in the maintenance of pain. A growing research on structural alterations in chronic pain revealed an association between PC and brain areas that are involved in affective and cognitive pain processing. However, little is known about a differential effect of the components magnification and helplessness.
Objective:
The aim of this study was to identify brain regions associated with overall PC and with the single components of magnification and helplessness.
Methods:
We investigated 29 patients 6 months after lumbar disk surgery using voxel-based morphometry. Magnification and helplessness were assessed with subscales of the Avoidance-Endurance Questionnaire (AEQ); overall PC was computed using the sum score. The structural brain imaging data were preprocessed and analyzed using SPM8 and VBM8. Multiple regression analyses were performed with PC scales as predictors and depression as covariate.
Results:
Pain catastrophizing was significantly associated with cortical gray matter in brain areas involved in processing attentional, sensory, and affective aspects of pain, including the left posterior cingulate cortex, supplementary motor area, and medial frontal gyrus. In addition, we provide preliminary evidence for brain structure association related to magnification and helplessness.
Conclusion:
This study provides evidence for PC-related structural alterations in patients with low back pain, which are consistent with findings from previous research in different chronic pain disorders. This study is the first to evaluate brain changes related to differential domains of PC.
1. Introduction
Pain catastrophizing (PC) has been shown to be an important predictor for pain, pain-related disability, and accompanying emotional distress among patients with chronic pain19,38,42 as well as a valid prognostic factor in patients with subacute back pain.49 Pain catastrophizing is defined as “an exaggerated negative mental set brought to bear during actual or anticipated painful experience”42 comprising at least 3 components: magnification, which reflects increased attention to possible harmful aspects of pain, cognitions of helplessness, reflecting the belief of lacking or ineffective coping strategies and finally rumination, the perseveration of thoughts of magnification and helplessness. Within a broader stress conception, magnification comprises cognitions of primary appraisals (the evaluation of the stimulus as harmful), whereas helplessness refers to secondary appraisal, the belief in coping possibilities and their successfulness.23 Although the 3 components are positively related,7,43 previous research has shown differential correlations with pain intensity and further outcomes in patients with chronic pain disorders. For example, Sullivan et al.44 reported helplessness as a unique predictor for affective pain intensity in patients with neuropathic pain. More recently, in a large scale study on 844 patients with mixed diagnoses of chronic pain, Craner et al.44 could demonstrate that helplessness and magnification are unique predictors of several pain outcomes, whereas rumination revealed zero-order correlations that disappeared in the multivariate models. With respect to the fact, that PC and moreover, the respective single components are highly important in the experience of pain, there is a need to better understand the mechanisms underlying PC.
A growing evidence from research in functional neuroimaging has shown that overall PC is associated with higher activation in brain regions that are involved in affective processing of pain, attention to pain, and the cognitive control of emotion and cognition.33 Similar findings were reported in studies that examined brain structure alterations in gray matter volume (GMV). For example, Hubbard et al.16 reported negative correlation between PC in patients with migraine and GMV in the left primary somatosensory cortex (S1), medial prefrontal cortex (PFC), and anterior midcingulate regions known to be involved in processing the attentional, sensory, and affective aspects of pain and cognitive inhibitory control. Furthermore, PC scores were significantly associated with cortical thickness in supplementary motor area (SMA), MCC and posterior cingulate cortex (PCC).35 Because the measure used in previous research assessing PC did not distinguish between components such as magnification or helplessness, it is still unclear whether these single components may be, at least partly, associated with different brain regions. A deeper understanding of the role of PC and their subdomains in pain processing should help to improve treatment outcomes in patients with chronic pain.
In this study, we investigated brain structural alterations associated with overall PC and the components, magnification and helplessness, in a homogeneous sample of patients with respect to their disease history. Keeping in mind that magnification reflects an increased attention and awareness of threat appraisal, we expected brain structure associations in regions known to modulate attention and affective reactions, such as the anterior cingulate cortex (ACC) and anterior insula16 and sensory-discriminative aspects of pain somatosensory cortices and PCC.16 By contrast, helplessness that mirrors an evaluation of the inability to control pain experiences effectively should be more associated with the brain in regions such as ventrolateral PFC, ACC,34 and SMA.35
2. Materials and methods
2.1. Subjects
Subjects were recruited from the St. Josef University Hospital of Bochum (Germany). The sample consisted of 29 individuals (n = 14 female) who participated in the physical examination and had signed the informed consent. The inclusion criteria were as follows: age 18 years and older, a lumbar spine surgery 6 months before the study, and low back pain (LBP; Th 12—L5/S1) during the past 3 months. The exclusion criteria were radiation of pain below the knee, an indication for a second operation because of new acute spinal origin of persistent or recurrent pain, severe osteoporosis, autoinflammatory arthritis, cancer, vertebral fracture, inflammatory disease of the spine, or a previous known psychiatric disease (ie, depression, schizophrenia), and insufficient knowledge of the German language. The study was approved by the ethics committee of Ruhr-University of Bochum and was conducted in accordance with the Declaration of Helsinki.
2.2. Behavioral and clinical measures
Each participant completed a series of self-report questionnaires to measure the following parameters:
Pain Catastrophizing was assessed with 2 of the cognitive subscales, scales of the German version of the Avoidance-Endurance Questionnaire (AEQ).14 Cognitive responses were defined as automatically occurring thoughts, introduced by the question “When I become aware of my pain during the past 14 days, this thought comes to my mind….” The AEQ contains the components of magnification (Catastrophizing Thoughts Subscale, CTS) and helplessness (Help/Hopelessness Scale, HHS). Both scales have shown moderate to high positive correlations,13,14 reflecting overlapping but also distinct variation. The reliability, as indicated by internal consistency, for the overall CTS score in the current sample was 0.96 (Cronbach alpha).
Magnification was assessed with the 3-item scale CTS of the AEQ describing the exaggeration of the possible seriousness of pain sensations (eg, “I can't have a tumor, can I?” and “It isn't a serious illness, is it?”). The items were answered on a 7-point numerical scale that ranges from “never” to “always.” Higher scores indicate a higher tendency of magnification. The CTS has been shown reliable, indicated by internal consistencies between 0.78 and 0.8413,14 and valid with respect to low but positive correlations with pain and disability and moderate to high positive associations with pain anxiety and fear-avoidance beliefs.14
Helplessness was assessed with the 9-item scale HHS of the AEQ assessing automatic cognitions reflecting low effectiveness and low controllability of pain (eg, “Whatever will I do if it gets worse again?” “Nothing helps anymore!”). All 9 items are answered on a 7-point numerical scale that ranges from “never” to “always.” Higher scores indicate more frequent thoughts of helplessness. The HHS has been shown high internal consistency (Cronbach alpha 0.91,14), and positive correlations with pain, disability, and pain-related affective distortion such as pain anxiety and fear of pain-related (re)injury.14,36
2.2.1. Depressive mood
We used the German version of the 21-item Beck Depression Inventory (BDI) (German version Kammer 1983).3,18 The BDI is a self-administered questionnaire that assesses the severity of depressive symptoms. Internal consistency assessments of reliability have been high with Cronbach alpha above 0.90 in most evaluations.2 The sum score of the BDI ranges from 0 to 63; higher scores indicate a higher degree of depressive mood.
2.2.2. Pain variables
Low back pain disease characteristics including self-reported measures of disease duration (months) and ratings of average pain intensity using a 0 to 10 numerical rating scale (NRS; 0, no pain and 10, worst pain imaginable) for the past week and past 3 months were determined.
2.3. Scanning protocol and data processing
A structural high-resolution scan of each participant was acquired using a T1-weighted MPRAGE sequence (Field Of View (FoV): FoV: 250 mm, echo time = 4.18, repetition time = 1990 ms) on a 1.5 T, Siemens Symphony scanner. One hundred sixty sagittal slices with a resolution of 1 × 1 × 1.5 mm were recorded.
Analysis was performed using the SPM8 package (Wellcome Department of Imaging Neuroscience, London, United Kingdom; http://www.fil.ion.ucl.ac.uk/spm) in combination with Matlab 7.9 platform (Mathworks, Sherborn, MA).
Preprocessing has been performed using VBM8 (VBM8 toolbox, download from http://dbm.neuro.uni-jena.de/vbm8/) with default parameters (bias regularization 0.0001 and bias cutoff full width at half maximum 60 mm). Briefly, anatomical images were spatially normalized into the Montreal Neurological Institute space and segmented into gray matter (GM), white matter, and cerebrospinal fluid. Each GM segment was morphed into a customized DARTEL template, which was in stereotactic space of the Montreal Neurological Institute. Finally, the modulated GM segments were smoothed with a Gaussian kernel set at 8-mm full width at half maximum.
2.4. Statistical analysis
The smoothed GM images were entered into a voxel-wise multiple regression analysis to investigate the variability in the regional GMV. We excluded all voxels with GM values of <0.1 using absolute threshold masking. Statistical analyses were performed using the general linear model in SPM12. In addition, we used AlphaSim48 to calculate the appropriate, corrected for multiple comparison threshold, cluster size for the whole-brain analysis. 5000 Monte Carlo simulations using AlphaSim with a voxel-level threshold of P < 0.001 were calculated resulting in a cluster of 44 contiguous voxels reflecting a corrected threshold of P < 0.05. Previous studies suggest that total GMV31 and age17,31 are important covariates in VBM. Therefore, both covariates were included in all the following analyses: first, the correlation between the GMV and overall score of PC; second, the correlation between the GMV and the mean of pain magnification; and finally, the correlation between the GMV and the mean of helplessness. In addition, previous studies have reported that depression was highly correlated with PC, and there is also a debate whether catastrophizing is a symptom of depression or a separate construct.10 Therefore, we reran the models including depression as a covariate to control that our results were robust with respect to depression symptoms. Anatomical labeling of brain regions showing significant correlations and the visualization of results was performed using the SPM8 extension XjView (http://www.alivelearn.net/xjview8/) and the Wake Forest University (WFU) (http://fmri.wfubmc.edu/software/pickatlas).21,22,26
In addition, we tested whether the observed differences in the height of correlation between GMV and overall PC (PC-sum score), magnification, and helplessness are significant, using the Pearson and Filon z-score,8 which is part of the cocor package (http://comparingcorrelations.org/). The cocor package covers a broad range of tests, including the comparisons of dependent correlations with either overlapping or nonoverlapping variables.
3. Results
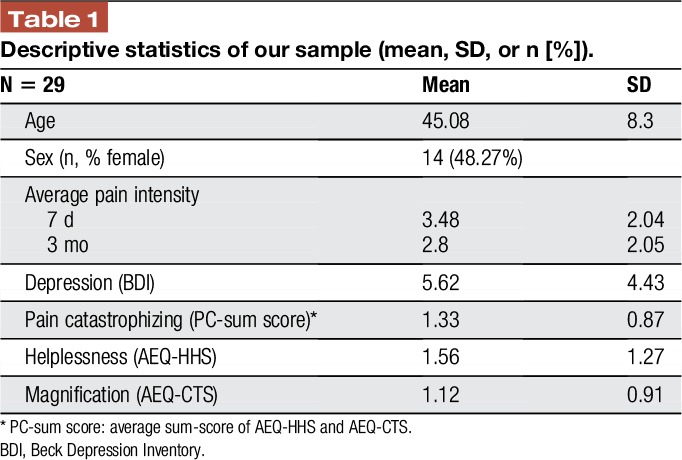
With respect to the behavioral data, we found a positive correlation between overall PC and the BDI (r = 0.468, P = 0.01) and average pain intensity last week (r = 0.437, P = 0.018). In addition, helplessness was significantly positively correlated with BDI (r = 0.588, P = 0.001) and with pain intensity (r = 0.435, P = 0.018) but not with magnification, assessed with the CTS (r = 0.275, P = 0.149). Furthermore, magnification was not significantly correlated with BDI (r = 0.082, P = 0.672) and with pain intensity (r = 0.237, P = 0.216). In addition, no significant correlation was found between magnification and pain duration (r = −0.274; P = 0.151) and between helplessness and pain duration (r = 0.170; P = 0.377). Table 1 reports mean values and SDs for all descriptive variables.
Table 1.
Descriptive statistics of our sample (mean, SD, or n [%]).
3.1. Imaging results
Imaging results showed positive relations between overall PC and GMV in the right MFG/SMA which remained robust, when depression was regressed out. By contrast, a negative correlation between overall PC and GMV in the left PCC merely appeared when we controlled for depression.
A negative correlation between GMV in the left PCC was further seen for magnification, but not for helplessness, irrespective of the control for depression. Furthermore, magnification revealed a positive correlation with GMV in the left MFG, also irrespective of depression.
With respect to helplessness, we found a positive correlation with GMV in the right MFG/SMA, which also remained robust for depression. To note, this positive association was seen for the overall score of PC, even irrespective of depression. No significant correlations were identified in the ACC and PFC. For details (ie, peak coordinates and z values) see Table 2 and Figure 1. In addition, we found no significant correlation between total GMV and pain duration (r = −0.098; P = 0.605). Furthermore, pain duration did not correlate significantly with GMV findings in MFG and PCC. For a complete exploratory result, see the Supplementary Data (Supplementary Table 1, Supplementary Table 2; available online at http://links.lww.com/PR9/A9 and Supplementary Figure 1; http://links.lww.com/PR9/A8).
Table 2.
Bivariate correlations between pain catastrophizing, magnification, and helplessness and regional gray matter volume using age, total GMV, and depression as covariates.
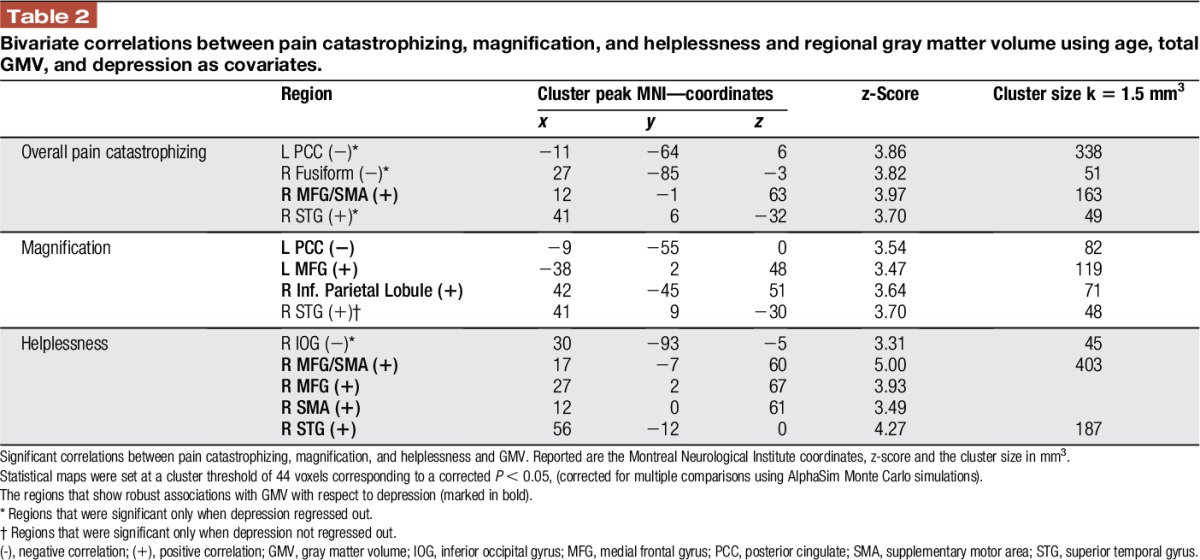
Figure 1.
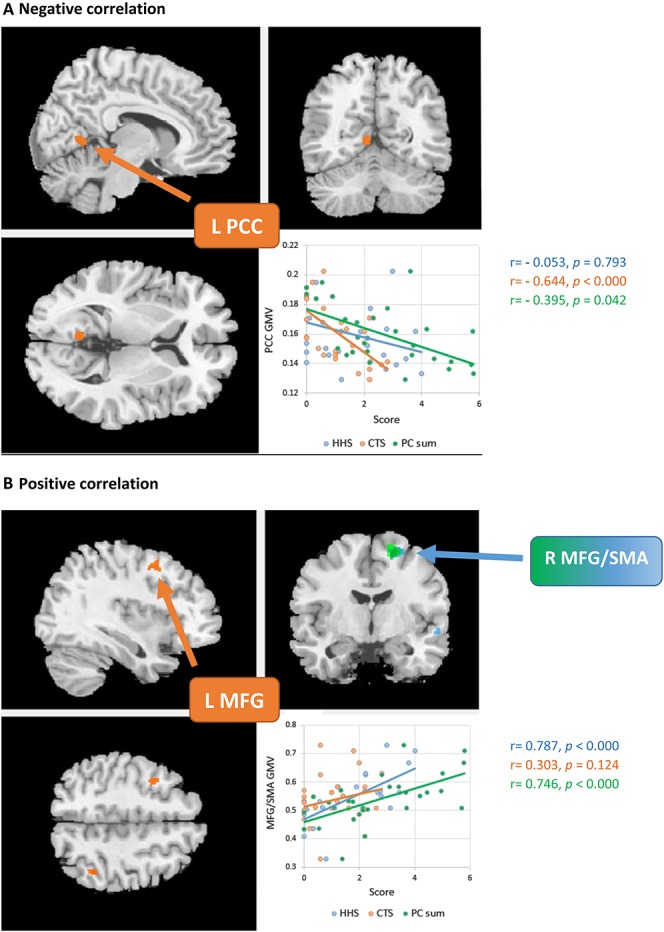
Correlations between pain catastrophizing (PC-sum score), the subscales helplessness (AEQ-HHS) and magnification (AEQ-CTS) and regional gray matter volume. Part A shows that there is a negative correlation between GMV in PCC and magnification, whereas part B shows positive correlation between GMV in MFG/SMA and helplessness. Statistical maps were set at a cluster threshold of 44 voxels corresponding to a corrected P < 0.05, (corrected for multiple comparisons using AlphaSim Monte Carlo simulations). GMV, gray matter volume; MFG, medial frontal gyrus; PCC, posterior cingulate; SMA, supplementary motor area.
When we compared the correlation between regional GMV and all 3 components of PC, we found significant differences in the correlation between GMV in PCC and magnification and helplessness, respectively (z = −2.751, P = 0.003) as well as between GMV in PCC and magnification and overall PC, respectively (z = −1.985, P = 0.024). Although both, the correlation between GMV in PCC and magnification as well as overall PC are significant and with a negative direction, the correlation for magnification was significantly higher than for overall PC. In addition, we found significant differences in the correlation between GMV in the right MFG/SMA and helplessness and magnification, respectively (z = 2.77, P = 0.003) but not between GMV in the right MFG/SMA and helplessness and overall PC, respectively (z = 0.613, P = 0.27). Finally, we found significant differences in the correlation between GMV in the left MFG and helplessness and magnification, respectively (z = 2.0217, P-value = 0.0432). For details (ie, r and P values) see Figure 1.
4. Discussion
As hypothesized, overall PC as well as both subcomponents of magnification and helplessness were significantly associated with cortical GM in brain areas involved in processing attentional, sensory, and affective aspects of pain, including the left PCC, STG, and MFG/SMA. In addition, the behavioural results of the current study are in line with previous studies investigating the different aspects of PC in patients with subacute and chronic pain.7,14,36,42 These data support the idea that PC is a multifaceted construct comprising pain-related cognitions such as magnification and helplessness which share overlapping as well as distinct parts of variance and are differently related to pain outcomes. To our knowledge, no study to date has examined brain structure association related to overall PC and the components of helplessness and magnification in patients with LBP.
4.1. Brain regions associated with overall pain catastrophizing
Our VBM analysis yields evidence that overall PC was significantly positively associated with GMV in the right MFG that is known to play a role in processing of negative emotion.29 The association in this region was robust with respect to depression. Gray matter volume in this area was also positively correlated with helplessness but not with magnification. When we compared the height of these correlations, we found no significant differences between helplessness and overall PC. Comparable results were found in previous research that reported positive correlation between SMA and overall PC.35 However, the authors reported that this correlation was no longer significant after control for helplessness. This supports the idea that the right MFG/SMA is merely associated with helplessness but not with overall PC.
Of interest, negative correlations between overall PC and GMV were only found when depression was used as an extra regressor. This raises the possibility that any observed negative correlations with overall PC are actually a function of removing depression. However, we found a negative association between overall PC and GMV in the PCC; this region is known to be a central part of the default mode network6 and commonly activated during processing of painful as well as emotional stimuli. In addition, our results are in line with findings from previous functional imaging studies in reporting positive correlations between individual PC scores and PCC activation.37 In addition, GMV in the left PCC has been reported to be negatively correlated with migraine pain intensity.16 Patients suffering from migraine headaches are more likely to display higher levels of PC compared with migraine-free individuals.15,16 Our results in this study are in line with earlier studies that reported structural abnormalities in several brain regions in patients with chronic pain, eg, the GMV of patients with chronic back pain was reduced in the dorsolateral PFC and the right thalamus,1,39 in the ACC and insula27,28 as well as in the PCC compared with healthy controls.5 However, only 1 study reported correlations between PC and reduced cortical GM in the dorsolateral PFC, medial PFC, inferior frontal gyrus, middle temporal gyrus, and S1.16 These discrepant findings may be attributed to the fact that the authors investigated PC in patients with migraine disease and that in some diagnoses, disease variables may play a more important role in the relation between PC and brain abnormalities.32
4.2. Brain regions associated with magnification
One important goal of our study was to investigate the association between GMV and the single components of PC, magnification, and helplessness. Concerning magnification, we found a strong association with GMV in the left PCC. To note, GMV in the left PCC was merely associated with overall PC (when depression was regressed out) and with magnification, but not with helplessness. The negative correlation between PCC and magnification was also robust after control for depression. These findings are in accordance with findings from functional imaging studies showing a strong relationship between PC and an activation in the PCC in patients with LBP and fibromyalgia.10,24 In addition, the PCC plays a prominent role in the processing of emotionally salient stimuli,25 and activation of the PCC is correlated with severity of anxiety symptoms in mood and anxiety disorders.4 However, further evidence suggests that the PCC plays an important role in regulating the focus of attention11 and that it is involved in orienting the body towards innocuous and noxious somatosensory stimuli.47 As Sullivan and colleagues proposed,41 we may conceptualize PC as automatic cognitions in the sense of primary and secondary appraisal sensu Lazarus and Folkman (1984).23 Primary appraisal involves attending to and evaluating the meaning of a situation, whereas secondary appraisal refers to an evaluation of possible coping strategies and their effectiveness or controllability. Gray matter volume association with the PCC may provide a possible explanation for the behavioral data of previous studies reporting that high catastrophizing individuals show increased attention to pain and a certain inability to divert attention from pain.40,46
4.3. Brain regions associated with helplessness
Concerning helplessness, our results revealed a significant positive association between GMV in the right MFG/SMA and helplessness. These findings are consistent with previous structural magnetic resonance imaging research demonstrating a positive correlation between helplessness and cortical thickness in this region.35 In addition, our results are in line with previous research showing that right MFG is involved in negative emotions such as fearful faces processing9 and the imagination of shame-related situations.29 It may be speculated that experiencing helplessness and hopelessness when trying to cope with pain may elicit or increase feelings of shame. Negative emotion in general in patients with chronic pain was significantly positively correlated with PC.30 Lateralization of GMV with respect to the subdomains of PC is of further interest. Although helplessness displayed associations with the right MFG/SMA, magnification revealed a positive relation with the left MFG. Talati and Hirsch45 reported effects of lateralization in the MFG with respect to decision making and executive functions, although the relation to catastrophizing and its subdomains remains unclear. Further research is warranted to explore possible effects of lateralization and subdomains of PC.
This study might have some limitations. The design is cross sectional; hence, it is not possible to determine whether the relationship between GMV alterations and PC is causal and, if so, to determine the direction of the relationship between pain psychology and brain structure. An additional limitation of our study is the absence of a control group. It remains unclear whether the GMV associations identified in our study are specific to PC in CLBP or exist in the general population. However, studies without control group can also be helpful for identifying trends that can be studied more in-depth. Thus, longitudinal studies will be important to fully confirm the hypothesis that PC can alter GMV. In addition, VBM is very helpful in detecting macrochanges in regional brain morphology; the correlating changes in cytoarchitecture remain to be fully elucidated.
Further limitation should be considered regarding the overall score for PC. Helplessness and magnification were positively but not significantly correlated in our sample, although moderate to high correlations were reported for these scales in previous research.13,14 Low to moderate correlations between the subcomponents of PC were further reported by the validation study of the Pain Catastrophizing Scale (PCS),43 one of the most used measures of magnification and helplessness. With respect to the high internal consistency of the overall PCS score, the authors concluded that the subcomponents “can be viewed as different dimensions of the same construct.”43 Thus, the impact different aspects of PC, such as magnification and helplessness, will have on different pain outcomes7 or on the activity of distinguishable brain circuits remains an important research topic that should be addressed in future studies.
Another limitation is that we did not include a measure for rumination, a further aspect of PC.43 The role of rumination, the perseveration of negative thoughts on causes, and consequences of pain in the maintenance of pain and disability is still under debate.7 However, Kucyi et al.20 reported data on an enhanced medial prefrontal-default mode network due to pain rumination in patients with chronic pain. Thus, further research on the role of pain rumination in structural brain alterations in patients with chronic pain disorders is warranted.
However, an important strength of this study is the homogeneity of our sample regarding the disease history: All subjects underwent a first lumbar disk surgery 6 months before the study. We excluded patients who suffered from pain radiating below the knee or showed signs indicating the necessity of a second operation besides other possible specific causes of LBP (ie, an inflammatory disease of the spine).12 Selecting a homogeneous patient sample regarding the disease history is important because different subpopulations may have diverse coping strategies that can influence their pain outcomes. For example, pain conditions with a neuropathic etiology are often distinct from other painful conditions without damage to the nervous system.39 A further strength of our study is the control for potential confounders, as catastrophizing is known to be strongly associated with depressive symptoms; the possible influence of depression was statistically removed.10 However, given the considerable conceptual overlap between depression and helplessness (negative cognitions) and the high correlation between them, including depression as a covariate may change the results of helplessness far more than magnification. Therefore, we reran the analyses without depression as a covariate to confirm that our results are not a function of controlling for depression.
5. Conclusion
Our results indicate that in a sample of patients with LBP 6 months after a primary lumbar spine surgery, GM brain associations with regions involved in the affective and cognitive processing of pain vary with respect to overall PC, whereas the subcomponents of magnification and helplessness seem to share some variance but also display unique parts in the association with these brain regions. Even the behavioural data indicated that both domains of PC are differentially related to pain and depression. These findings may help us to better understand the neuronal correlates of PC with the components of more attention-related aspects of magnification and helplessness, which reflects inefficiency of coping and perceived uncontrollability of pain.
Disclosures
The authors have no conflicts of interest to declare.
Appendix A. Supplemental Digital Content
Supplemental digital content associated with this article can be found online at http://links.lww.com/PR9/A9 and http://links.lww.com/PR9/A8.
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Web site (www.painjournalonline.com).
References
- [1].Apkarian AV, Sosa Y, Sonty S, Levy RM, Harden RN, Parrish TB, Parrish TB, Gitelman DR. Chronic back pain is associated with decreased prefrontal and thalamic gray matter density. J Neurosci 2004;24:10410–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol 1988;56:893–7. [DOI] [PubMed] [Google Scholar]
- [3].Beck AT, Ward CH, Mendelson M, Mock J, Erbauch J. An inventory for measuring depression. Arch Gen Psychiatry 1961;4:561–71. [DOI] [PubMed] [Google Scholar]
- [4].Bench CJ, Friston KJ, Brown RG, Scott LC, Frackowiak RS, Dolan RJ. The anatomy of melancholia–focal abnormalities of cerebral blood flow in major depression. Psychol Med 1992;22:607–15. [DOI] [PubMed] [Google Scholar]
- [5].Buckalew N, Haut MW, Morrow L, Weiner D. Chronic pain is associated with brain volume loss in older adults: preliminary evidence. Pain Med 2008;9:240–8. [DOI] [PubMed] [Google Scholar]
- [6].Buckner RL, Andrews-Hanna JR, Schacter DL. The brain's default network: anatomy, function, and relevance to disease. Ann N Y Acad Sci 2008;1124:1–38. [DOI] [PubMed] [Google Scholar]
- [7].Craner JR, Gilliam WP, Sperry JA. Rumination, magnification, helplessness: how do different aspects of pain catastrophizing relate to pain severity and functioning? Clin J Pain 2016;32:1028–35. [DOI] [PubMed] [Google Scholar]
- [8].Diedenhofen B, Musch J. Cocor: a comprehensive solution for the statistical comparison of correlations. PLoS One 2015;10:e0121945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Fusar-Poli P, Placentino A, Carletti F, Landi P, Allen P, Surguladze S, Benedetti F, Abbamonte M, Gasparotti R, Barale F, Perez J, McGuire P, Politi P. Functional atlas of emotional faces processing: a voxel-based meta-analysis of 105 functional magnetic resonance imaging studies. J Psychiatry Neurosci 2009;34:418–32. [PMC free article] [PubMed] [Google Scholar]
- [10].Gracely RH, Geisser ME, Giesecke T, Grant MAB, Petzke F, Williams DA, Clauw DJ. Pain catastrophizing and neural responses to pain among persons with fibromyalgia. Brain 2004;127:835–43. [DOI] [PubMed] [Google Scholar]
- [11].Hahn B, Ross TJ, Stein EA. Cingulate activation increases dynamically with response speed under stimulus unpredictability. Cereb Cortex 2007;17:1664–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Hamilton L, Macgregor A, Warmington V, Pinch E, Gaffney K. The prevalence of inflammatory back pain in a UK primary care population. Rheumatology (Oxford) 2014;53:161–4. [DOI] [PubMed] [Google Scholar]
- [13].Hasenbring M, Marienfeld G, Kuhlendahl D, Soyka D. Risk factors of chronicity in lumbar disc patients. A prospective investigation of biologic, psychologic, and social predictors of therapy outcome. Spine 1994;19:2759–65. [DOI] [PubMed] [Google Scholar]
- [14].Hasenbring MI, Hallner D, Rusu AC. Fear-avoidance- and endurance-related responses to pain: development and validation of the avoidance-endurance questionnaire (AEQ). Eur J Pain 2009;13:620–8. [DOI] [PubMed] [Google Scholar]
- [15].Holroyd KA, Drew JB, Cottrell CK, Romanek KM, Heh V. Impaired functioning and quality of life in severe migraine: the role of catastrophizing and associated symptoms. Cephalalgia 2007;27:1156–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Hubbard CS, Khan SA, Keaser ML, Mathur VA, Goyal M, Seminowicz DA. Altered brain structure and function correlate with disease severity and pain catastrophizing in migraine patients. eNeuro 2014;1:e20.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Isaacs EB, Edmonds CJ, Chong WK, Lucas A, Morley R, Gadian DG. Brain morphometry and IQ measurements in preterm children. Brain 2004;127:2595–607. [DOI] [PubMed] [Google Scholar]
- [18].Kammer D. Eine Untersuchung der psychometrischen Eigenschaften des deutschen Beck-Depressionsinventars (BDI). Diagnostica 1983;29:48–60. [Google Scholar]
- [19].Keefe FJ, Lumley M, Anderson T, Lynch T, Studts JL, Carson KL. Pain and emotion: new research directions. J Clin Psychol 2001;57:587–607. [DOI] [PubMed] [Google Scholar]
- [20].Kucyi A, Moayedi M, Weissman-Fogel I, Goldberg MB, Freeman BV, Tenenbaum HC, Davis KD. Enhanced medial prefrontal-default mode network functional connectivity in chronic pain and its association with pain rumination. J Neurosci 2014;34:3969–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Lancaster JL, Rainey LH, Summerlin JL, Freitas CS, Fox PT, Evans AC, Toga AW, Mazziotta JC. Automated labeling of the human brain: a preliminary report on the development and evaluation of a forward-transform method. Hum Brain Mapp 1997;5:238–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Lancaster JL, Woldorff MG, Parsons LM, Liotti M, Freitas CS, Rainey L, Kochunov PV, Nickerson D, Mikiten SA, Fox PT. Automated Talairach atlas labels for functional brain mapping. Hum Brain Mapp 2000;10:120–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Lazarus RS, Folkman S. Stress, appraisal, and coping. New York: Springer, 1984. [Google Scholar]
- [24].Lloyd D, Findlay G, Roberts N, Nurmikko T. Differences in low back pain behavior are reflected in the cerebral response to tactile stimulation of the lower back. Spine 2008;33:1372–7. [DOI] [PubMed] [Google Scholar]
- [25].Maddock RJ. The retrosplenial cortex and emotion: new insights from functional neuroimaging of the human brain. Trends Neurosci 1999;22:310–6. PII: S0166–2236(98)01374-5/. [DOI] [PubMed] [Google Scholar]
- [26].Maldjian JA, Laurienti PJ, Kraft RA, Burdette JH. An automated method for neuroanatomic and cytoarchitectonic atlas-based interrogation of fMRI data sets. NeuroImage 2003;19:1233–9. [DOI] [PubMed] [Google Scholar]
- [27].May A. Chronic pain may change the structure of the brain. PAIN 2008;137:7–15. [DOI] [PubMed] [Google Scholar]
- [28].May A. Structural brain imaging: a window into chronic pain. Neuroscientist 2011;17:209–20. [DOI] [PubMed] [Google Scholar]
- [29].Michl P, Meindl T, Meister F, Born C, Engel RR, Reiser M, Hennig-Fast K. Neurobiological underpinnings of shame and guilt: a pilot fMRI study. Soc Cogn Affect Neurosci 2014;9:150–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Ong AD, Zautra AJ, Reid MC. Psychological resilience predicts decreases in pain catastrophizing through positive emotions. Psychol Aging 2010;25:516–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Pell GS, Briellmann RS, Chan CHP, Pardoe H, Abbott DF, Jackson GD. Selection of the control group for VBM analysis: influence of covariates, matching and sample size. NeuroImage 2008;41:1324–35. [DOI] [PubMed] [Google Scholar]
- [32].Piche M, Chen J, Roy M, Poitras P, Bouin M, Rainville P. Thicker posterior insula is associated with disease duration in women with irritable bowel syndrome (IBS) whereas thicker orbitofrontal cortex predicts reduced pain inhibition in both IBS patients and controls. J Pain 2013;14:1217–26. [DOI] [PubMed] [Google Scholar]
- [33].Quartana PJ, Campbell CM, Edwards RR. Pain catastrophizing: a critical review. Expert Rev Neurother 2009;9:745–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Salomons TV, Johnstone T, Backonja M, Shackman AJ, Davidson RJ. Individual differences in the effects of perceived controllability on pain perception: critical role of the prefrontal cortex. J Cogn Neurosci 2007;19:993–1003. [DOI] [PubMed] [Google Scholar]
- [35].Salomons TV, Moayedi M, Weissman-Fogel I, Goldberg MB, Freeman BV, Tenenbaum HC, Davis KD. Perceived helplessness is associated with individual differences in the central motor output system. Eur J Neurosci 2012;35:1481–7. [DOI] [PubMed] [Google Scholar]
- [36].Scholich SL, Hallner D, Wittenberg RH, Hasenbring MI, Rusu AC. The relationship between pain, disability, quality of life and cognitive-behavioural factors in chronic back pain. Disabil Rehabil 2012;34:1993–2000. [DOI] [PubMed] [Google Scholar]
- [37].Seminowicz DA, Davis KD. Cortical responses to pain in healthy individuals depends on pain catastrophizing. PAIN 2006;120:297–306. [DOI] [PubMed] [Google Scholar]
- [38].Severeijns R, Vlaeyen JW, van den Hout MA, Weber WE. Pain catastrophizing predicts pain intensity, disability, and psychological distress independent of the level of physical impairment. Clin J Pain 2001;17:165–72. [DOI] [PubMed] [Google Scholar]
- [39].Smallwood RF, Laird AR, Ramage AE, Parkinson AL, Lewis J, Clauw DJ, Williams DA, Schmidt-Wilcke T, Farrell MJ, Eickhoff SB, Robin DA. Structural brain anomalies and chronic pain: a quantitative meta-analysis of gray matter volume. J Pain 2013;14:663–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Spanos NP, Radtke-Bodorik HL, Ferguson JD, Jones B. The effects of hypnotic susceptibility, suggestions for analgesia, and the utilization of cognitive strategies on the reduction of pain. J Abnorm Psychol 1979;88:282–92. [DOI] [PubMed] [Google Scholar]
- [41].Sullivan MJ, D'Eon JL. Relation between catastrophizing and depression in chronic pain patients. J Abnormal Psychol 1990;99:260–3. [DOI] [PubMed] [Google Scholar]
- [42].Sullivan MJ, Thorn B, Haythornthwaite JA, Keefe F, Martin M, Bradley LA, Lefebvre JC. Theoretical perspectives on the relation between catastrophizing and pain. Clin J Pain 2001;17:52–64. [DOI] [PubMed] [Google Scholar]
- [43].Sullivan MJL, Bishop SR, Pivik J. The pain catastrophizing scale: development and validation. Psychol Assess 1995;7:524–32. [Google Scholar]
- [44].Sullivan MJL, Lynch ME, Clark AJ. Dimensions of catastrophic thinking associated with pain experience and disability in patients with neuropathic pain conditions. PAIN 2005;113:310–5. [DOI] [PubMed] [Google Scholar]
- [45].Talati A, Hirsch J. Functional specialization within the medial frontal gyrus for perceptual go/no-go decisions based on “what,” “when,” and “where” related information: an fMRI study. J Cogn Neurosci 2005;17:981–93. jcn99609 981.993//. [DOI] [PubMed] [Google Scholar]
- [46].van Damme S, Crombez G, Eccleston C. Disengagement from pain: the role of catastrophic thinking about pain. PAIN 2004;107:70–6. [DOI] [PubMed] [Google Scholar]
- [47].Vogt BA. Pain and emotion interactions in subregions of the cingulate gyrus. Nat Rev Neurosci 2005;6:533–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Ward BD. Simultaneous inference for FMRI data. Available at: http://afni.nimh.nih.gov/pub/dist/doc/manual/AlphaSim.pdf. Accessed 19 June, 2000.
- [49].Wertli MM, Eugster R, Held U, Steurer J, Kofmehl R, Weiser S. Catastrophizing-a prognostic factor for outcome in patients with low back pain: a systematic review. Spine J 2014;14:2639–57. [DOI] [PubMed] [Google Scholar]


