Abstract
Objective
To evaluate cross-sectional associations of sodium and potassium with body mass index (BMI), waist circumference (WC), and body fat and determine whether nativity/duration of US residence modified these associations.
Methods
Sodium and potassium were derived from 24-hour diet recalls from 16,156 US participants of the 2008–2011 Hispanic Community Health Study/Study of Latinos (HCHS/SOL) and from 24-hour urine in 447 HCHS/SOL participants. BMI, WC, and body fat were measured.
Results
500 mg/day higher dietary sodium was cross-sectionally associated with 0.07 kg/m2 higher BMI (p<0.05) and 0.18 cm larger WC (p=0.04). 500 mg/day higher dietary potassium was only associated with lower BMI and smaller WC among those foreign-born with 10+ years in the US (−0.13 kg/m2, p<0.01; and −0.36cm, p=0.01, respectively) and among the US born (−0.62 kg/m2, p<0.01 and −1.42 cm, p<0.01, respectively). 500 mg/day higher urinary sodium was associated with 0.27 kg/m2 higher BMI (p<0.01) and 0.54 kg more body fat (p<0.01).
Conclusions
Sodium intake was associated with higher BMI, WC, and body fat. Potassium intake, was associated with lower BMI and smaller WC among US-born and participants with longer duration of US residence.
Keywords: Sodium, potassium, body mass index, waist circumference, Hispanics
Introduction
Two of every three adults in the United States (US) are either overweight or obese.1 The current obesity epidemic in the US has been at least partly attributed to the increasingly processed diet and its composition, which is not only energy-dense but also rich in sodium and low in potassium.2 Given the ubiquity of sodium in the US diet,3 coupled with lack of potassium, the sodium to potassium (Na-K) ratio has increased over time and is less than ideal.2 While emerging evidence suggests that sodium intake may be associated with obesity, independent of energy,4–12 the relationships of potassium and Na-K ratio with obesity have not been explored in great detail. Findings from limited studies suggest that lower potassium and a higher Na-K ratio are associated with higher rates of obesity.13
Among ethnic minority populations, such as US Hispanics/Latinos, the relationships among sodium, potassium, Na-K ratio, and obesity are particularly pertinent and yet they remain underexplored. Hispanics/Latinos have higher dietary sodium intake, lower dietary potassium intake,14 and higher rates of obesity15 compared with non-Hispanic whites. Further, Hispanics/Latinos have a unique acculturation experience during which their dietary habits and quality tend to worsen with greater duration of residence in the US.16 Thus, understanding how dietary nutrients such as sodium and potassium intake are associated with obesity outcomes among Hispanics/Latinos, one of the fastest-growing segments of the US population, is of great medical and public health interest.
Establishing a direct association between dietary nutrients, sodium in particular, and obesity independent of energy intake is important, yet challenging given the strong correlation between nutrients such as sodium and energy intake. Most prior studies have adjusted for energy intake derived from dietary recall or food frequency questionnaire,4,6,7,9,12,17 both of which are prone to measurement error.18 Fewer studies have explored sodium density (estimated as sodium divided by energy intake) in relation to obesity,8,11 and to our knowledge, no prior study in the US has used the doubly labeled water (DLW) method19 to objectively calculate energy intake and account for it when examining the associations among sodium, potassium, and obesity outcomes.
Using data from the Hispanic Community Health Study/Study of Latinos (HCHS/SOL), we aimed to examine: 1) the associations of dietary sodium, potassium, and Na-K ratio with measures of obesity, and 2) whether these associations varied by duration of US residence. In a subsample, we further examined the associations of 24-urinary sodium, potassium, and Na-K ratio with measures of obesity controlling for DLW derived energy intake.
Methods
Study population
HCHS/SOL
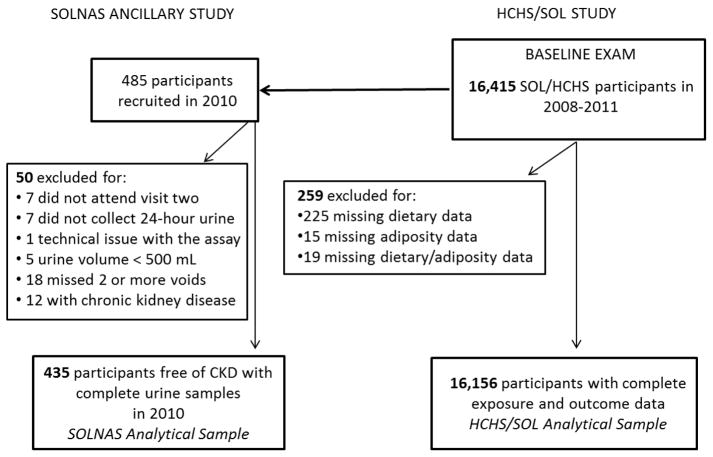
The HCHS/SOL is a a population based cohort study of 16,415 community dwelling self-identified Hispanics/Latinos of diverse heritage. In brief, participants aged 18–74 years were recruited between 2008 and 2011 in areas in proximity to four field centers in: Bronx, NY; Chicago, IL, Miami-Dade, FL; and San Diego, CA. A two-stage area probability sample of households was selected; stratification and over-sampling at each stage was utilized to obtain a diverse and representative sample of Hispanics/Latinos.20 Participants were asked to bring in their current medications for review, to undergo a clinical examination, have fasting blood samples collected, answer questionnaires pertaining to their medical history and health behaviors, including two 24-hour diet recalls. After excluding 259 individuals without at least one exposure and outcome measure of interest, our final analytic cross-sectional HCHS/SOL sample was 16,156 (Figure 1). All participants provided informed consent and the study was approved by each site’s Institutional Review Board. Details have been described elsewhere.20,21
Figure 1.
Study Flow Chart
Study of Latinos: Nutrition & Physical Activity Assessment Study (SOLNAS ancillary study)
In 2010–2012, within months of completing the HCHS/SOL, a sub-set of weight stable HCHS/SOL participants enrolled in the SOLNAS ancillary study,22 designed to assess the measurement error of self-reported energy, protein, sodium, and potassium intake. Spot and 24 hour urine samples were collected at two study visits spanning 12 days. 485 SOLNAS participants attended visit one. Participants arrived at the first visit after a four hour fast and provided a baseline spot urine sample. Participants then ingested a DLW mixture dosed based on body weight23 and provided in-clinic post-DLW spot urine samples at three and four hours. At the end of visit one, participants received a meal replacement beverage and fluids necessary for the DLW measurement process. Additionally participants were given 24-hour urine collection instructions and advised to collect and return the urine at visit two. At visit two, 478 participants who returned, provided two more timed spot urine collections for the DLW measurement; seven participants did not return with 24-hour urine samples. Of the 471 24-hour urine samples, a total of 36 were subsequently excluded for the following reasons: a urine sample <500 mL (n=5), reporting two or more missed urine collections (n=18), technical issues with the laboratory assay (n=1), or the participant has chronic kidney disease (n=12), resulting in a final analytic size of 435 (see Figure 1). The sample included 44 participants who missed 1 void. All participants provided informed consent.
Dietary Measures
Self-reported measures of energy, sodium and potassium
Two 24-hour dietary recalls were collected from the full sample of HCHS/SOL participants within a three month period.24 Scores from the two dietary recalls were averaged; 99% of the sample provided at least one recall. Using the Nutrition Data System for Research software which uses the multiple-pass method,25 values for dietary sodium (mg/day), potassium (mg/day), and energy (kcal/day) were derived. The following measures were further calculated: dietary Na-K ratio as sodium (mmol) divided by potassium (mmol), dietary sodium density as dietary sodium intake (mg) per 1000 kcal per day, and dietary potassium density as dietary potassium intake (mg) per 1000 kcal per day.
Biomarker-based measures of energy, sodium and potassium
From 24-hour urine samples, sodium (mmol) and potassium (mmol) were determined using the ion-selective electrode method (Roche Diagnostics, Indianapolis, IN) at the central HCHS/SOL laboratory at the University of Minnesota. Samples were normalized to a 24-hour period and values for sodium and potassium were converted into mg/day. In brief and described elsewhere,22 DLW, a validated technique known to provide accurate measurement of total energy expenditure,26 was used to estimate total energy intake—valid among weight stable individuals. Deuterium and oxygen-18, two byproducts of the ingested DLW mixture were measured from each spot urine sample using mass spectrometry at the Gas-Isotope-Ratio Mass Spectrometry Laboratory, US Department of Agriculture/Agriculture Research Service Children’s Nutrition Research Center, Baylor College of Medicine, Houston, Texas.27,28 Deuterium and oxygen-18 elimination rates were calculated from the multiple timed spot urine specimen collected over the 12 day period; with the difference between these rates proportional to carbon dioxide production. The Weir equation was used to estimate total energy expenditure (expressed in kcal/day) from the carbon dioxide production rate.23 The following measures were also derived: Na-K ratio as the ratio of urinary sodium (mmol/day) to urinary potassium (mmol/day), sodium density as urinary sodium excrestion (mg) per 1000 kcal (derived from DLW) per day, and potassium density as potassium excretion (mg/day) per 1000 kcal (derived from DLW) per day.
Measures of Obesity
Body mass index (BMI) in kg/m2 was measured in both the full HCHS/SOL sample and the SOLNAS sub-sample and derived from measured weight and height wearing light clothing.21 Waist circumference (WC) in centimeters was measured during the HCHS/SOL study only using standardized reference points. Additionally, in the SOLNAS subsample, DLW methods, described elsewhere,29 were used to measure body fat in kg and percent body fat.
Other Measures
All study participants reported their language preference (Spanish or English), age, sex, and educational attainment (< high school, high school degree, or > than high school). Individuals also reported their incomes grouped as: < $20,000, $20,000 – $50,000, ≥ $50,000, or missing income. Participants were asked to select a category that best described their Hispanic/Latino heritage, with responses including, Central American, Cuban, Dominican, Mexican, Puerto-Rican, South American, more than one group, or other. Additionally, participants reported their nativity and were classified as US born or foreign born (including Puerto Rico). Participants who were identified as foreign-born further reported the duration that they had lived in the US. Nativity/years in the US was classified as: foreign born, < 10 years in the US; foreign born, 10+ years in the US; or US born.
Participants reported their smoking status (never, current, or former) and alcohol consumption (‘heavy drinkers’ were defined as having >7 drinks/week for women and >14 drinks/week for men). Physical activity was self-reported using the modified version of the World Health Organization Global Physical Activity Questionnaire.30 Described elsewhere,31 the Alternative Healty Eating Index-2010 (AHEI-2010, range from 0 to 110) was used to assess overall diet, with higher scores indicating a more healthful diet. Three seated blood pressure (BP) measurements were taken using an automatic sphygmomanometer (OMRON HEM-907 L), and hypertension was defined as having average systolic BP ≥ 140 mmHg or diastolic BP ≥ 90 mmHg, or documented use of anti-hypertension medication. Use of diuretic medication was also noted. Diabetes status/impaired glucose classification was defined as fasting plasma glucose ≥126 mg/dL, a 2 hour postload glucose level ≥200 mg/dL, A1C level ≥6.5%, or documented use of hypoglycemic agents.32 Chronic kidney disease (CKD) was defined as having an estimated glomerular filtration rate <60 ml/min/1.73m2.33 Depressive symptoms were assessed using the Center for Epidemiologic Studies Depression Scale-10 (CESD range 0 to 30).
Statistical Analysis
For our main analysis, among participants of the HCHS/SOL study demographic and clinical characteristics were assessed along with mean dietary sodium, sodium density, potassium, potassium density, and Na-K ratio across categories of nativity/years in the US. T-tests were used to determine whether means differed by nativity/years in the US. Estimates were age-adjusted to the US 2010 census population
Using multiplicative interaction terms within linear regression models we found that nativity/years in the US modified the associations of dietary potassium, potassium density, and Na-K ratio with BMI and WC (p values of interactions < 0.05), but not sodium or sodium density, thus resulting in stratified models for potassium, potassium density, and Na-K ratio. Models were adjusted for: age, sex, Hispanic/Latino heritage, education, income, language preference, study site, smoking, hypertension, diabetes, chronic kidney disease, alcohol use, depression, and physical activity. Models for sodium, potassium, and Na-K ratio were additionally adjusted for dietary energy intake.
For analyses of the SOLNAS sub-sample, we also assessed demographic and clinical characteristics of the SOLNAS sample (reported in Table S1). We repeated similar linear regression models in the SOLNAS sub-sample using the urinary-based biomarkers but did not test for effect modification by nativity/years in US due to a smaller sample size. Models were adjusted for: age, sex, Hispanic/Latino heritage, education, income, language preference, nativity/years in the US, study site, missed urine voids, smoking, hypertension, diabetes, alcohol use, depression, and physical activity. Models for sodium, potassium, and Na-K ratio were additionally adjusted for DLW derived energy intake. Additionally, we conducted a sensitivity analysis by further excluding participants who missed 1 urine void (n=44) or were on diuretic medications, which are known to effect electrolyte excretion (n=28), for a restricted sample of 363 participants. Analyses were conducted in SUDAAN (Version 11.0.1, Research Triangle Institute, NC) to account for the complex survey design and the sampling weights.
Results
Overall, mean age was 41 years old (SE: 0.2), and 52.6% (SE: 0.5) were female (Table 1). In total, 34% (SE: 0.7) had less than a high school education, 76% (SE: 0.9) preferred Spanish to English, 25% (SE: 0.5) had hypertension, and 17% (SE: 0.4) had diabetes. Compared with those born in the US, those foreign born were less likely to have CKD but more likely to have lower educational attainment, lower incomes, prefer Spanish, and have higher AHEI-2010 scores.
Table 1.
Demographic and clinical characteristics overall and by nativity/years in the US, HCHS/SOL
| Overall (N=16,156) | Nativity/Years in the US
|
|||||||
|---|---|---|---|---|---|---|---|---|
| Foreign born, < 10 years in the US (n=3,630) | Foreign born, ≥ 10 years in the US (n=8,964) | US born (n=2,713) | ||||||
|
| ||||||||
| Characteristic | % or mean | SE | % or mean | SE | % or mean | SE | % or mean | SE |
| Age, mean (SE) | 41.1 | 0.2 | 38.6 | 0.4 | 46.9 | 0.3 | 31.3 | 0.3 |
| Female | 52.6 | 0.5 | 54.8 * | 1.0 | 53.9 * | 0.9 | 49.0 | 1.8 |
| Hispanic/Latino heritage | ||||||||
| Central American | 7.3 | 0.5 | 8.8 * | 0.9 | 8.4 * | 0.6 | 1.4 | 0.3 |
| Cuban | 21.1 | 1.7 | 40.0* | 2.9 | 16.5 * | 1.4 | 5.0 | 0.7 |
| Dominican | 9.8 | 0.7 | 8.3 * | 0.9 | 12.3 * | 0.9 | 4.2 | 0.7 |
| Mexican | 36.5 | 1.6 | 30.1 * | 2.3 | 41.0 | 1.7 | 41.0 | 2.0 |
| Puerto Rican | 16.4 | 0.8 | 3.6 * | 0.6 | 13.9 * | 0.8 | 39.1 | 1.8 |
| South American | 5.1 | 0.3 | 7.2 * | 0.7 | 5.3 * | 0.4 | 0.9 | 0.1 |
| More than one/other | 3.9 | 0.3 | 2.0 * | 0.3 | 2.6 * | 0.4 | 8.4 | 1.0 |
| < HS Education | 33.5 | 0.7 | 28.7 * | 1.1 | 37.6 * | 0.9 | 21.9 | 1.3 |
| < $20,000 Income | 42.5 | 0.9 | 47.8 * | 1.4 | 43.5 * | 1.0 | 31.3 | 1.6 |
| Spanish language Preference | 76.4 | 0.9 | 98.2 * | 0.3 | 81.1 * | 1.0 | 25.1 | 1.4 |
| Current smoker | 20.9 | 0.6 | 18.6 * | 1.0 | 19.0 * | 0.8 | 28.1 | 1.4 |
| Heavy drinker | 5.8 | 0.3 | 4.4 * | 0.4 | 5.8 * | 0.4 | 7.9 | 0.9 |
| Physical activity (total METS/week), mean (SE) | 685.1 | 13.4 | 657.7 | 24.6 | 665.5 | 18.6 | 728.2 | 33.3 |
| Energy, Kcal, mean (SE) | 1892.4 | 10.3 | 1951.4 | 18.7 | 1844.7* | 14.1 | 1968.0 | 22.1 |
| AHEAI-20102, mean (SE) | 47.8 | 0.2 | 47.2 * | 0.3 | 48.7 * | 0.2 | 46.4 | 0.3 |
| Hypertension | 25.1 | 0.5 | 24.9 | 0.9 | 24.9 | 0.6 | 24.7 | 1.5 |
| Diabetes | 16.7 | 0.4 | 13.1 | 0.8 | 18.1* | 0.5 | 14.3 | 1.1 |
| Chronic kidney disase | 5.0 | 0.3 | 4.6* | 0.5 | 4.8* | 0.3 | 8.7 | 1.4 |
| CESD1 score, mean (SE) | 7.1 | 0.1 | 6.6* | 0.1 | 6.9* | 0.1 | 7.9 | 0.2 |
All estimates are age adjusted to the US 2010 census population aged 18–74 years
Indicates estimate is significantly different compared with US born as the referent group, p< 0.05
CESD: Center for Epidemiologic Studies Depression scale
AHEI-2010: Alternative Heathy Eating Index 2010, range: 0–110
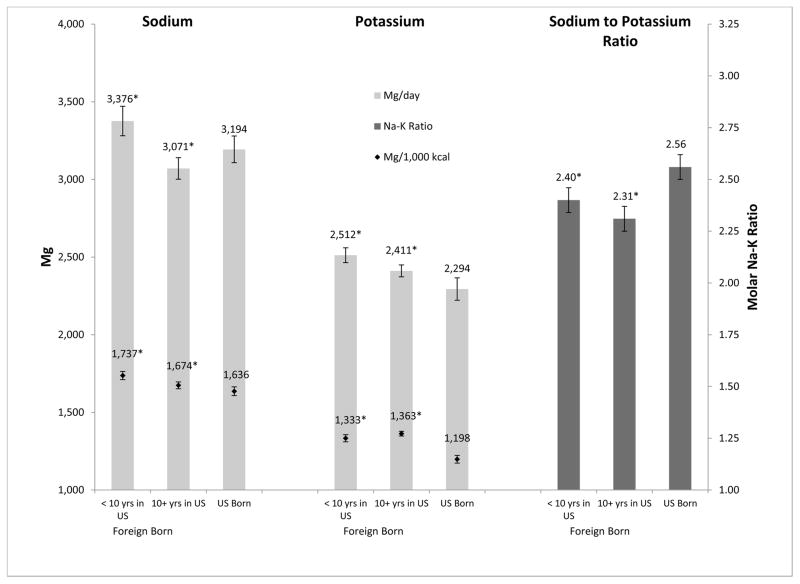
Mean dietary sodium differed by nativity/years in the US (Figure 2) and ranged from 3071 mg/day (SE: 35) among those foreign born with 10+ years in the US, to 3376 mg/day (SE: 47) among the foreign born with < 10 years in the US. Mean dietary potassium and Na-K ratio—both indicators of diet quality—were least favorable (i.e. lower potassium and higher Na-K ratio) among those born in the US. Results from t-tests showed that compared with the US born, those foreign born with < 10 years had higher dietary potassium (2512 mg/day, SE: 23 vs. 2294 mg/day, SE: 33; p<0.01), higher dietary potassium density (1333 per 1000 kcal, SE: 11 vs. 1198 per 1000 kcal, SE: 11; p<0.01), and had lower mean dietary Na-K ratio (2.40, SE: 0.03 vs. 2.56, SE: 0.03; p<0.01).
Figure 2.
Age-standardized mean dietary sodium, sodium density, potassium, potassium density and sodium to potassium ratio by nativity/years in the US, HCHS/SOL.
All estimates are age standardized to the US 2010 standard population.
*Mean is significantly different compared with US Born (referent group), p<0.05
From fully-adjusted linear regression models (Table 2), 500 mg/day higher dietary sodium was associated with a 0.07 kg/m2 higher BMI (95% CI: 0.00, 0.15; p<0.05) and a 0.18 cm larger WC (95% CI: 0.00, 0.36; p<0.05). Likewise, a 250 mg/1000 kcal higher dietary sodium density was associated with a 0.07 kg/m2 higher BMI (95% CI: 0.01, 0.14) and a 0.17 cm larger WC (95% CI: 0.01, 0.34).
Table 2.
Associations of dietary sodium and sodium density with body mass index and waist circumference, HCHS/SOL
| Body Mass Index (kg/m2) | Waist Circumference (cm) | |||
|---|---|---|---|---|
| Beta | 95% CI | Beta | 95% CI | |
| Sodium | ||||
| Model 1 | 0.00 | −0.05, 0.05 | 0.11 | −0.01, 0.24 |
| Model 2 | 0.07* | 0.00, 0.15 | 0.18* | 0.00, 0.36 |
| Sodium Density | ||||
| Model 1 | 0.12* | 0.05, 0.18 | 0.31* | 0.13, 0.49 |
| Model 2 | 0.07* | 0.01, 0.14 | 0.17* | 0.01, 0.34 |
Model 1 is adjusted for age, sex, heritage, education, income, language preference, nativity/years in the US, and study site; Model 2 is additionally adjusted for smoking, hypertension, diabetes, chronic, kidney disease, alcohol use, depression, physical activity (total METs/week), and energy intake (in sodium models only)
We modeled 500 mg increments of sodium and 250 mg per 1000 kcal units for sodium density
Indicates estimate is statistically significant, p<0.05
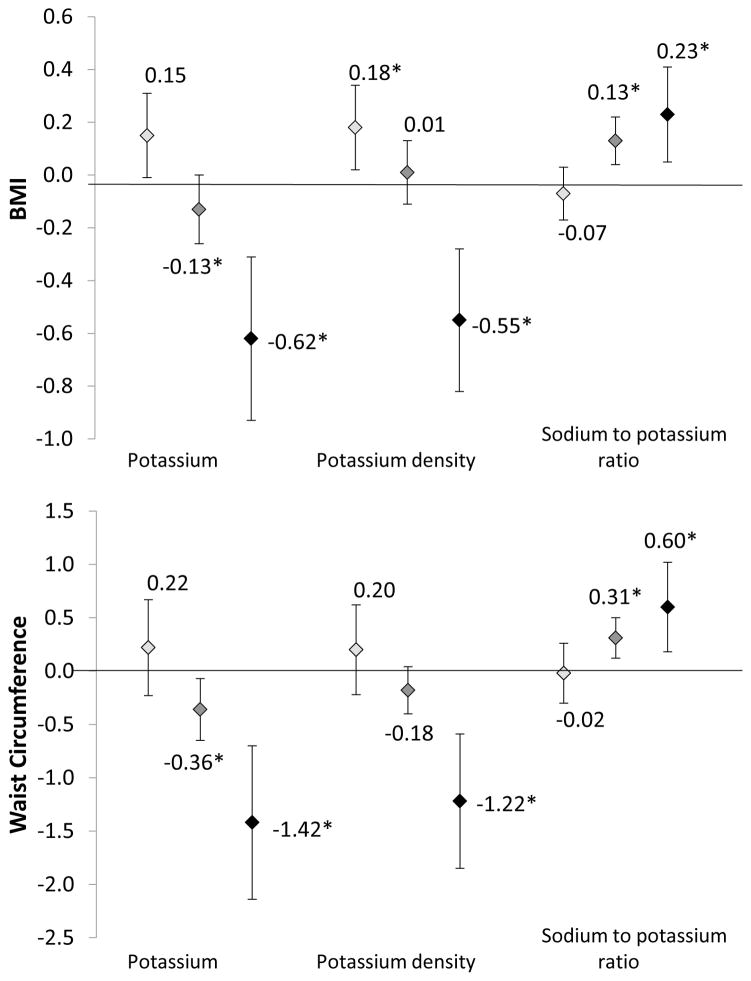
The associations of potassium, potassium density, and Na-K ratio with obesity measures varied by nativity/years in the US (Figure 3 and Table S1). For dietary potassium, a 500 mg/day increment was only associated with lower BMI among the foreign born with 10+ years in the US (−0.13 kg/m2, −0.25, 0.00, p<0.05) and among those US born (−0.62 kg/m2, 95% CI: −0.92, −0.31). For dietary potassium density, a 250 mg/1000 kcal increment was associated with higher BMI among the foreign born with <10 years in the US (0.18 kg/m2, 95% CI: 0.03, 0.34) but not among the foreign born with 10+ years in the US (0.01 km/m2, 95% CI: −0.10, 0.13) and with lower BMI among the US born (−0.55 kg/m2, 95% CI: −0.82, −0.28). For dietary Na-K ratio, a 0.50 unit increment was associated with higher BMI among the foreign born with 10+ years in the US (0.13 kg/m2, 0.04, 0.22) and among the US born (0.23 kg/m2, 95% CI: 0.05, 0.41). Patterns for WC largely mirrored those of BMI.
Figure 3.
Fully-adjusted associations of dietary potassium, potassium density, and sodium to potassium ratio with body mass index and waist circumference, stratified by nativity/years in the US, HCHS/SOL.
Models are adjusted for age, sex, heritage, education, income, language preference, study site, smoking, hypertension, diabetes, chronic kidney disease, alcohol use, depression, physical activity (total METs/week), and energy intake (except for in potassium density models).
We modeled 500 mg increments of potassium, 250 mg per 1000 kcal unit increments for potassium density, and 0.50 unit increments of sodium to potassium ratio (mmol/mmol)
 Foreign Born < 10 years in US
Foreign Born < 10 years in US
 Foreign Born 10+ years in US
Foreign Born 10+ years in US
◆ US born
Demographic and clinical characteristics of SOLNAS participants are shown in Table S2. Among SOLNAS participants, in fully-adjusted linear regression models (Table 3), a 500 mg/day higher urinary sodium excretion was associated with 0.27 kg/m2 higher BMI (95% CI: 0.08, 0.45), 0.54 kg higher body fat (95% CI: 0.15, 0.93), and 0.35 higher percent body fat (95% CI: 0.11, 0.58). A 250 mg/1000 kcal increment of urinary sodium density was associated with 0.39 (95% CI: 0.09, 0.68) higher percent body fat. Urinary potassium and potassium density were not associated with BMI, body fat, or percent body fat in fully adjustment models. However, a 0.50 increment of urinary Na-K ratio was associated with a 0.23 kg/m2 higher BMI (95% CI: 0.04, 0.41), a 0.48 kg higher body fat (95% CI: 0.10, 0.86), and a 0.34 higher percent body fat (95% CI: 0.12, 0.57). Results from the sensitivity analysis restricted to those without any missing urine voids and not on diuretic medications were unchanged (not shown).
Table 3.
Associations of 24-hr urinary sodium, potassium, and sodium to potassium ratio with body mass index, body fat, and percent body fat, SOLNAS (N=435).
| Body Mass Index (kg/m2) | Body Fat (kg) | Percent Body Fat | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| Beta | 95% CI | Beta | 95% CI | Beta | 95% CI | |
| Sodium | ||||||
| Model 1 | 0.46* | 0.26, 0.66 | 0.83* | 0.41, 1.25 | 0.40* | 0.16, 0.64 |
| Model 2 | 0.27* | 0.08, 0.45 | 0.54* | 0.15, 0.93 | 0.35* | 0.11, 0.58 |
| Sodium density | ||||||
| Model 1 | 0.11 | −0.14, 0.37 | 0.33 | −0.18, 0.84 | 0.37* | 0.06, 0.68 |
| Model 2 | 0.12 | −0.13, 0.37 | 0.37 | −0.11, 0.86 | 0.39* | 0.09, 0.68 |
| Potassium | ||||||
| Model 1 | 0.56* | 0.11, 1.02 | 0.93* | 0.04, 1.82 | 0.37 | −0.09, 0.83 |
| Model 2 | 0.22 | −0.17, 0.60 | 0.41 | −0.37, 1.20 | 0.26 | −0.20, 0.73 |
| Potassium density | ||||||
| Model 1 | −0.32 | −0.80, 0.16 | −0.49 | −1.35, 0.37 | 0.10 | −0.39, 0.58 |
| Model 2 | −0.39 | −0.88, 0.10 | −0.55 | −1.44, 0.34 | 0.07 | −0.44, 0.59 |
| Sodium: Potassium | ||||||
| Model 1 | 0.25* | 0.04, 0.45 | 0.51* | 0.07, 0.94 | 0.34* | 0.10, 0.59 |
| Model 2 | 0.23* | 0.04, 0.41 | 0.48* | 0.10, 0.86 | 0.34* | 0.12, 0.57 |
Model 1 is adjusted for age, sex, heritage, education, income, language preference, nativity/years in the US, study site, and missing 1 urine void; Model 2 is additionally adjusted for smoking, hypertension, diabetes, alcohol use, depression, physical activity (total METs/week), and energy intake (in sodium and potassium models only)
We modeled 500 mg increments of sodium and potassium, 250 mg per 1000 kcal unit increments for sodium density and potassium density, and 0.50 unit increments of sodium to potassium ratio (mmol/mmol)
Indicates estimate is statistically significant, p<0.05
Discussion
In the current study of over 16,000 diverse US Hispanics/Latinos, sodium was associated with measures of obesity—independent of energy intake. Each 500 mg increment of daily dietary sodium was significantly associated with a 0.07 kg/m2 higher BMI and 0.18 cm larger WC. The associations of dietary potassium, potassium density, and Na-K ratio with BMI and WC were stronger in magnitude with more years spent in the US. For example, whereas higher dietary potassium was not associated with BMI or WC among the foreign-born with <10 years in the US, higher dietary potassium was associated with 0.13 kg/m2 lower BMI and 0.36 cm smaller WC among foreign-born with 10+ years in the US, among the US born it was association with 0.62kg/m2 lower BMI and 1.42 cm smaller WC. The magnitude of the associations between urinary-based markers, especially sodium and Na-K ratio, and measures of obesity were much stronger, and independent of DLW derived energy expenditure, suggesting a direct relationship.
Sodium is ubiquitous in the US food supply,3 and therefore highly correlated with energy intake.34 High sodium diets are also known to increase fluid intake,35 such as the consumption of sugary drinks36 which in turn may contribute to weight gain.37 Thus, the sodium—obesity relationship has largely been attributed to indirect downstream processes related to increased energy intake. However, emerging evidence suggests a direct relationship between sodium and obesity exists independent of energy intake.4–12,17,38,39 For example, in a population based UK sample that assessed sodium using 24-hour urine, 400 mg per day higher sodium (or one gram of salt) was independently associated with greater fat mass in children by 0.73 kg and in adults by 0.91 kg even after controlling for energy intake using DLW.39 In agreement with such findings, our study, which was the first of its kind in the US to use objective measures of both sodium and energy, found a strong and direct association between sodium and measures of obesity, independent of energy intake.
While the biological rationale for this association has not been fully explored, the conventional wisdom that all calories are metabolically equivalent regardless of macronutrient composition is being questioned. For example, a study by Ebbeling et al,40 showed that isocaloric diets differing in macronutrient composition elicited different declines in resting and total energy expenditure. Similarly, experimental studies in rats showed that high sodium diets induce higher adiposity compared with rats with isocaloric low sodium diets.41 Consistent with this animal model, we found that a 500 mg/day higher urinary sodium excretion was significantly associated with 0.54 kg more body fat. Additionally, we found that urinary sodium density, a relative measure, was associated with percent body fat, a measure of body composition, but not absolute body fat in kg. Taken together, these results suggest that sodium in itself is associated with increased fat mass, while sodium density is associated with body composition. Though we cannot say for sure why this is the case, the authors note that both sodium density and percent body fat are relative measures.
In our study, potassium, a nutrient positively associated with healthfulness of diet,42 was negatively associated with BMI and WC, but showed stronger magnitude with longer duration of US residence. In the context of the acculturation process, the current findings may be the consequence of worsening of dietary habits as subjects become more acculturated (as with greater time in the US).16 Therefore, we speculate that among individuals with fewer years in the US, potassium may not necessarily reflect diet quality and healthfulness to the extent that it does in a diet among individuals with greater years spent in the US. This would explain the lack of associations between dietary potassium and measures of obesity among the foreign-born with < 10 years in the US. In our study, overall dietary summary scores were indeed higher (i.e. more healthy) among Hispanics/Latinos who were foreign-born vs. US born. Consistent with this speculation, adjusted for age and energy, we found that dietary potassium was a weaker predictor of AHEI dietary summary score among the foreign born with <10 years in the US than among the foreign born with 10+ years in the US or among the US born (data not shown). In the SOLNAS subsample, neither urinary potassium nor potassium density was associated with obesity, though we were underpowered to test for effect modification by nativity/years in the US.
Similar to potassium, the associations between Na-K ratio—another indicator of diet qualty42—and measures of obesity also varied by nativity/years in the US, such that the associations were only significant in those with longer years in the US. To our knowledge this has not been previously documented and may again reflect Na-K ratio, similar to potassium, as being a better indicator of healthfulness of diet in more acculturated US Hispanics/Latinos. Results from the SOLNAS subsample showed a strong positive association among urinary Na-K ratio with all measures of obesity including: BMI, body fat, and percent body fat. For example, we found a 0.50 unit increase in Na-K to be associated with 0.23 kg/m2 higher BMI, 0.48 kg more body fat, and 0.34 greater body fat percent. Consistent with our findings, spot urine Na-K ratio —a more easily available approach to measuring Na-K ratio—was also shown to be independently associated with percent total body fat measured using DXA in a multi-ethnic US cohort.5
The current study is not without limitations. First, given the cross-sectional design we could not establish temporality. Sodium reduction is often indicated in the treatment of certain chronic conditions such as hypertension, diabetes, and CKD. Yet, we were unable to account for potential dietary modifications made by these individuals, due to the cross-sectional design of the study. Further, our main measures of sodium and potassium were derived via 24-hour dietary recall, which is subject to measurement error.22 However, we also found similar associations using density measures, which are less error prone.22 Further, we were able to repeat our analyses using objective biomarkers from 24-hour urine in the SOLNAS sub-sample, and found consistent associations and sometimes stronger in magnitude. However, even the 24-hour urine biomarker measure has limitations,18 as it only reflects sodium intake on one day and is not necessarily reflective of habitual sodium intake. Finally, though we used nativity/years in the US as a proxy measure for acculturation,43 we acknowledge that this measure may not accurately reflect the dynamic acculturation process.
Despite such limitations, our study has several notable strengths. To our knowledge, this was the first study of its kind conducted in a population based sample of diverse US Hispanics/Latinos. The sample was large and comprised of mostly immigrants. Thus, we were adequately powered to test for interactions by length of time in the US. Our study included multiple dietary measures each with differing strengths. For example, though dietary sodium collected via diet recall is prone to measurement error, sodium density is a more accurate marker of true sodium density.
In the current sample, dietary sodium density only over-estimates urinary sodium density by 6%.44 Likewise, it has been noted that potassium, potassium density, and particularly Na-K ratio derived from self-reported measures capture intake quite well.44,45 In addition to our multiple measures of diet, this study also made use of multiple measures of obesity, including BMI, waist circumference, body fat, and percent body fat. In general, our results were robust across multiple nutrient markers—dietary and urinary biomarkers, measures of obesity, and sensitivity analyses.
Conclusions
In the current population based study of US Hispanics/Latinos, higher sodium intake was associated with higher BMI, WC, and body fat. Lower potassium intake and higher Na-K ratio were more strongly associated with higher BMI and WC with longer duration of US residence. Although the mechanisms underlying such relationships have not been adequately explored, our findings along with other studies suggest that sodium may be directly related to measures of obesity, above and beyond energy intake. Future studies investigating the longitudinal relationship among intakes of sodium, potassium, Na-K ratio, and changes in measures of obesity are warranted.
Supplementary Material
What is already known about this subject?
Emerging evidence suggests that sodium is associated with measures measures of obesity.
What does your study add?
Higher sodium was associated with higher BMI, waist circumference, and more body fat among diverse US Hispanics.
Lower potassium and higher sodium to potassium ratio was associated with higher BMI and waist circumference with stronger associations among Hispanics with longer duration of US residence.
Acknowledgments
Funding Information: The Study of Latinos: Nutrition & Physical Activity Assessment Study was supported by R01HL095856 from the National Heart, Lung, and Blood Institute. The Hispanic Community Health Study/Study of Latinos was carried out as a collaborative study supported by contracts from the National Heart, Lung, and Blood Institute (NHLBI) to the University of North Carolina (N01-HC65233), University of Miami (N01-HC65234), Albert Einstein College of Medicine (N01-HC65235), Northwestern University (N01-HC65236), and San Diego State University (N01-HC65237).
Tali Elfassy was supported by the American Heart Association post-doctoral fellowship (17POST32490000) and the T32 training grant from the National Institutes of Health, National Heart, Lung, and Blood Institute (HL 007426). Dr. Zeki Al Hazzouri was supported by a grant from the National Institutes of Health, National Institute on Aging (K01AG047273).
Footnotes
Clinical Trial Registration: This trial is registered at clinicaltrials.gov as NCT02060344
Disclosures: The authors have no disclosures or conflicts of interests to report.
Author Contributions: Dr. Elfassy conducted the statistical analyses for this study. Drs. Elfassy and Zeki Al Hazzouri interpreted the data and drafted the manuscript. Drs. Elfassy, Mossavar-Rahmani, Van Horn, Gellman, Sostres-Alvarez, Schneiderman, Daviglus, Beasley, Llabre, Shaw, Prado, Florez, and Zeki Al Hazzouri contributed to the methodological aspects of this study.
References
- 1.Yang L, Colditz GA. PRevalence of overweight and obesity in the united states, 2007–2012. JAMA Internal Medicine. 2015;175(8):1412–1413. doi: 10.1001/jamainternmed.2015.2405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cordain L, Eaton SB, Sebastian A, et al. Origins and evolution of the Western diet: health implications for the 21st century. The American journal of clinical nutrition. 2005 Feb;81(2):341–354. doi: 10.1093/ajcn.81.2.341. [DOI] [PubMed] [Google Scholar]
- 3.Mattes RD, Donnelly D. Relative contributions of dietary sodium sources. J Am Coll Nutr. 1991 Aug;10(4):383–393. doi: 10.1080/07315724.1991.10718167. [DOI] [PubMed] [Google Scholar]
- 4.Hulthen L, Aurell M, Klingberg S, Hallenberg E, Lorentzon M, Ohlsson C. Salt intake in young Swedish men. Public health nutrition. 2010 May;13(5):601–605. doi: 10.1017/S1368980009991431. [DOI] [PubMed] [Google Scholar]
- 5.Jain N, Minhajuddin AT, Neeland IJ, Elsayed EF, Vega GL, Hedayati SS. Association of urinary sodium-to-potassium ratio with obesity in a multiethnic cohort. The American journal of clinical nutrition. 2014 May;99(5):992–998. doi: 10.3945/ajcn.113.077362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Larsen SC, Angquist L, Sorensen TI, Heitmann BL. 24h urinary sodium excretion and subsequent change in weight, waist circumference and body composition. PloS one. 2013;8(7):e69689. doi: 10.1371/journal.pone.0069689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Libuda L, Kersting M, Alexy U. Consumption of dietary salt measured by urinary sodium excretion and its association with body weight status in healthy children and adolescents. Public health nutrition. 2012 Mar;15(3):433–441. doi: 10.1017/S1368980011002138. [DOI] [PubMed] [Google Scholar]
- 8.Raisanen JP, Silaste ML, Kesaniemi YA, Ukkola O. Increased daily sodium intake is an independent dietary indicator of the metabolic syndrome in middle-aged subjects. Annals of medicine. 2012 Sep;44(6):627–634. doi: 10.3109/07853890.2011.585657. [DOI] [PubMed] [Google Scholar]
- 9.Song HJ, Cho YG, Lee H-J. Dietary sodium intake and prevalence of overweight in adults. Metabolism. 2013 May;62(5):703–708. doi: 10.1016/j.metabol.2012.11.009. [DOI] [PubMed] [Google Scholar]
- 10.Yi SS, Kansagra SM. Associations of sodium intake with obesity, body mass index, waist circumference, and weight. American journal of preventive medicine. 2014 Jun;46(6):e53–55. doi: 10.1016/j.amepre.2014.02.005. [DOI] [PubMed] [Google Scholar]
- 11.Yoon YS, Oh SW. Sodium density and obesity; the Korea National Health and Nutrition Examination Survey 2007–2010. European journal of clinical nutrition. 2013 Feb;67(2):141–146. doi: 10.1038/ejcn.2012.204. [DOI] [PubMed] [Google Scholar]
- 12.Zhu H, Pollock NK, Kotak I, et al. Dietary sodium, adiposity, and inflammation in healthy adolescents. Pediatrics. 2014 Mar;133(3):e635–642. doi: 10.1542/peds.2013-1794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cai X, Li X, Fan W, et al. Potassium and Obesity/Metabolic Syndrome: A Systematic Review and Meta-Analysis of the Epidemiological Evidence. Nutrients. 2016;8(4):183. doi: 10.3390/nu8040183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Angell SY, Yi S, Eisenhower D, et al. Sodium intake in a cross-sectional, representative sample of New York City adults. American journal of public health. 2014 Dec;104(12):2409–2416. doi: 10.2105/AJPH.2013.301542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Daviglus ML, Talavera GA, Aviles-Santa ML, et al. Prevalence of major cardiovascular risk factors and cardiovascular diseases among Hispanic/Latino individuals of diverse backgrounds in the United States. Jama. 2012 Nov 7;308(17):1775–1784. doi: 10.1001/jama.2012.14517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ayala GX, Baquero B, Klinger S. A systematic review of the relationship between acculturation and diet among Latinos in the United States: implications for future research. Journal of the American Dietetic Association. 2008 Aug;108(8):1330–1344. doi: 10.1016/j.jada.2008.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yi SS, Firestone MJ, Beasley JM. Independent associations of sodium intake with measures of body size and predictive body fatness. Obesity (Silver Spring, Md) 2015 Jan;23(1):20–23. doi: 10.1002/oby.20912. [DOI] [PubMed] [Google Scholar]
- 18.Cogswell ME, Mugavero K, Bowman BA, Frieden TR. Dietary Sodium and Cardiovascular Disease Risk - Measurement Matters. The New England journal of medicine. 2016 Jun 1; doi: 10.1056/NEJMsb1607161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schoeller DA. Recent advances from application of doubly labeled water to measurement of human energy expenditure. The Journal of nutrition. 1999 Oct;129(10):1765–1768. doi: 10.1093/jn/129.10.1765. [DOI] [PubMed] [Google Scholar]
- 20.Lavange LM, Kalsbeek WD, Sorlie PD, et al. Sample design and cohort selection in the Hispanic Community Health Study/Study of Latinos. Ann Epidemiol. 2010 Aug;20(8):642–649. doi: 10.1016/j.annepidem.2010.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sorlie PD, Aviles-Santa LM, Wassertheil-Smoller S, et al. Design and implementation of the Hispanic Community Health Study/Study of Latinos. Ann Epidemiol. 2010 Aug;20(8):629–641. doi: 10.1016/j.annepidem.2010.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mossavar-Rahmani Y, Shaw PA, Wong WW, et al. Applying Recovery Biomarkers to Calibrate Self-Report Measures of Energy and Protein in the Hispanic Community Health Study/Study of Latinos. American journal of epidemiology. 2015;181(12):996–1007. doi: 10.1093/aje/kwu468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Weir JB. New methods for calculating metabolic rate with special reference to protein metabolism. The Journal of physiology. 1949 Aug;109(1–2):1–9. doi: 10.1113/jphysiol.1949.sp004363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Siega-Riz AM, Sotres-Alvarez D, Ayala GX, et al. Food-group and nutrient-density intakes by Hispanic and Latino backgrounds in the Hispanic Community Health Study/Study of Latinos. The American journal of clinical nutrition. 2014 Jun;99(6):1487–1498. doi: 10.3945/ajcn.113.082685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhao G, Ford ES, Mokdad AH. Racial/ethinic variation in hypertension-related lifetsyle behaviours among US women with self-reported hypertension. Journal of Human Hypertension. 2008;22:608–616. doi: 10.1038/jhh.2008.52. [DOI] [PubMed] [Google Scholar]
- 26.Buchowski MS. Doubly Labeled Water Is a Validated and Verified Reference Standard in Nutrition Research. The Journal of nutrition. 2014 Feb-26;144(5):573–574. doi: 10.3945/jn.114.191361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wong WW, Lee LS, Klein PD. Deuterium and oxygen-18 measurements on microliter samples of urine, plasma, saliva, and human milk. The American journal of clinical nutrition. 1987 May;45(5):905–913. doi: 10.1093/ajcn/45.5.905. [DOI] [PubMed] [Google Scholar]
- 28.Wong WW, Clarke LL, Llaurador M, Klein PD. A new zinc product for the reduction of water in physiological fluids to hydrogen gas for 2H/1H isotope ratio measurements. European journal of clinical nutrition. 1992 Jan;46(1):69–71. [PubMed] [Google Scholar]
- 29.Bhutani S, Racine N, Shriver T, Schoeller DA. Special Considerations for Measuring Energy Expenditure with Doubly Labeled Water under Atypical Conditions. Journal of obesity & weight loss therapy. 2015 Jul-30;5(Suppl 5):002. doi: 10.4172/2165-7904.S5-002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.World Health Organization. Global Physical Activity Surveillance. [Accessed Dec 24, 2015];Chronic Diseases and Health Promotion. 2015 http://www.who.int/chp/steps/GPAQ/en/
- 31.Chiuve SE, Fung TT, Rimm EB, et al. Alternative Dietary Indices Both Strongly Predict Risk of Chronic Disease. The Journal of nutrition. 2012 Jun 1;142(6):1009–1018. doi: 10.3945/jn.111.157222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.American Diabetes A. Diagnosis and Classification of Diabetes Mellitus. Diabetes Care 2010 -/Revised;33(Suppl 1):S62–S69. doi: 10.2337/dc10-S062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. American journal of kidney diseases: the official journal of the National Kidney Foundation. 2002 Feb;39(2 Suppl 1):S1–266. [PubMed] [Google Scholar]
- 34.Whelton PK, Appel LJ, Sacco RL, et al. Sodium, blood pressure, and cardiovascular disease: further evidence supporting the American Heart Association sodium reduction recommendations. Circulation. 2012 Dec 11;126(24):2880–2889. doi: 10.1161/CIR.0b013e318279acbf. [DOI] [PubMed] [Google Scholar]
- 35.He FJ, Markandu ND, Sagnella GA, MacGregor GA. Effect of salt intake on renal excretion of water in humans. Hypertension. 2001 Sep;38(3):317–320. doi: 10.1161/01.hyp.38.3.317. [DOI] [PubMed] [Google Scholar]
- 36.Grimes CA, Wright JD, Liu K, Nowson CA, Loria CM. Dietary sodium intake is associated with total fluid and sugar-sweetened beverage consumption in US children and adolescents aged 2–18 y: NHANES 2005–2008. The American journal of clinical nutrition. 2013 Jul;98(1):189–196. doi: 10.3945/ajcn.112.051508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Schulze MB, Manson JE, Ludwig DS, et al. Sugar-sweetened beverages, weight gain, and incidence of type 2 diabetes in young and middle-aged women. Jama. 2004 Aug 25;292(8):927–934. doi: 10.1001/jama.292.8.927. [DOI] [PubMed] [Google Scholar]
- 38.Hoffmann IS, Cubeddu LX. Salt and the metabolic syndrome. Nutrition, metabolism, and cardiovascular diseases: NMCD. 2009 Feb;19(2):123–128. doi: 10.1016/j.numecd.2008.02.011. [DOI] [PubMed] [Google Scholar]
- 39.Ma Y, He FJ, MacGregor GA. High Salt Intake: Independent Risk Factor for Obesity? Hypertension. 2015 Aug 3; doi: 10.1161/HYPERTENSIONAHA.115.05948. [DOI] [PubMed] [Google Scholar]
- 40.Ebbeling CB, Swain JF, Feldman HA, et al. Effects of dietary composition on energy expenditure during weight-loss maintenance. Jama. 2012 Jun 27;307(24):2627–2634. doi: 10.1001/jama.2012.6607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fonseca-Alaniz MH, Brito LC, Borges-Silva CN, Takada J, Andreotti S, Lima FB. High dietary sodium intake increases white adipose tissue mass and plasma leptin in rats. Obesity (Silver Spring, Md) 2007 Sep;15(9):2200–2208. doi: 10.1038/oby.2007.261. [DOI] [PubMed] [Google Scholar]
- 42.Loftfield E, Yi S, Immerwahr S, Eisenhower D. Construct validity of a single-item, self-rated question of diet quality. Journal of nutrition education and behavior. 2015 Mar-Apr;47(2):181–187. doi: 10.1016/j.jneb.2014.09.003. [DOI] [PubMed] [Google Scholar]
- 43.Thomson MD, Hoffman-Goetz L. Defining and measuring acculturation: a systematic review of public health studies with Hispanic populations in the United States. Social science & medicine (1982) 2009 Oct;69(7):983–991. doi: 10.1016/j.socscimed.2009.05.011. [DOI] [PubMed] [Google Scholar]
- 44.Mossavar-Rahmani Y, Sotres-Alvarez D, Wong WW, et al. Applying recovery biomarkers to calibrate self-report measures of sodium and potassium in the Hispanic Community Health Study/Study of Latinos. J Hum Hypertens. 02/16/online 2017. [Google Scholar]
- 45.Freedman LS, Commins JM, Moler JE, et al. Pooled Results From 5 Validation Studies of Dietary Self-Report Instruments Using Recovery Biomarkers for Potassium and Sodium Intake. American journal of epidemiology. 2015;181(7):473–487. doi: 10.1093/aje/kwu325. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.