Abstract
Social class gradients in children’s health and development are ubiquitous across time and geography. The authors develop a conceptual framework relating three actions of class—material allocation, salient group identity, and inter-group conflict—to the reproduction of class-based disparities in child health. A core proposition is that the actions of class stratification create variation in children’s mesosystems and microsystems in distinct locations in the ecology of everyday life. Variation in mesosystems (e.g., health care, neighborhoods) and microsystems (e.g., family structure, housing) become manifest in a wide variety of specific experiences and environments that produce the behavioral and biological antecedents to health and disease among children. The framework is explored via a review of theoretical and empirical contributions from multiple disciplines and high-priority areas for future research are highlighted.
Keywords: Children’s health, Social class, Health status disparity, Social theory
PREAMBLE
This paper arises out of a workshop convened in the summer of 2015 by the Eunice Kennedy Shriver National Institute of Child Health and Human Development, of the National Institutes of Health in the United States, and the Economic and Social Research Council and Research Councils UK from the United Kingdom. The meeting of early career and established investigators was titled, “How the social environment gets under the skin – developmental perspectives” and included representatives from demography, economics, epidemiology, family studies, history, psychology, and sociology. One of several working groups from this meeting coalesced around an interest in conceptualizing, defining and measuring the broader socioeconomic environment as it pertains to children’s health. What emerged was a realization of the extent of disciplinary differences in language and frame, as well as an appreciation for the richness of a transdisciplinary perspective on something as complex as social class and health. The product of a year-long discussion and debate is this broad survey of the multileveled and multidimensional mechanisms and processes by which socioeconomic experiences and processes ‘get under the skin’ to affect children’s health and development.
INTRODUCTION
Social class gradients in health are ubiquitous across time and geography. An awareness that social status or position is related to individuals’ health is evident in the writings of Hippocrates, and has been quantitatively described in populations since Petty and Graunt in the 17th century, and Farr in the 19th century counted and summarized deaths and death rates (N. Krieger, 2011). From these earliest systematic collections of population health data was evidence that individuals and groups with greater power, wealth, and prestige typically have better outcomes than those with less or without. These patterns persist into the early 21st century both within and between nations for wide-ranging processes and outcomes including cancers, chronic diseases, infectious diseases, and neurodevelopment.
Concern for social class variation among children engages the concern of scientists, policymakers and families for at least three reasons. First, children occupy a privileged space in most industrialized cultures, being both protected throughout childhood and valued for their future potential. Therefore harm done to children is less tolerated than similar harm done to adults. Second, children ‘receive’ their social class from their families, and as such they are not causally responsible for their status in life. Finally, rapid growth and developmental plasticity make children particularly sensitive to the stimuli of their environments, with lifelong consequences. Stimuli and exposures during critical developmental windows, or cumulatively across childhood can illicit disease and disease processes that persist into adulthood.
The literature documenting and describing the presence of social, economic, and class disparities in child health is abundant. However the literature aiming to explain the how and why—mechanisms and pathways—of the production and maintenance of class gradients in health through time and across geography is less complete. Therefore the structure of this paper integrates the pairing of theory with functional and operational mechanisms and processes. We begin by providing a broad overview of the theoretical foundations of social class, leading to a conceptual framework of children’s health and class-based health disparities that is influenced by bioecological theory. In order to further animate the conceptual framework we provide brief and illustrative examples of empirical research examining the production of class-based gradients in child health. This serves both to summarize key findings and to highlight potential gaps in the literature that are implied by the conceptual framework.
FOUNDATIONS
Theoretical Foundations -- Social Class
Social class refers to the “horizontal stratification of a population” (Gordon, 1949, p. 265) on the basis of factors such as wealth, income, occupation, status, group identification, level of consumption, or family background. Social class is distinct from other sources of stratification in the population stemming from gender, racial or ethnic identity, and religion, although the intersection of class identities with other sources of identity produce additional variation (Bauer, 2014). Social class has strong sociological roots, and has been conceptualized in two primary ways. A Marxist viewpoint conceptualizes social class in relation to the means of production, particularly in terms of whether an individual owns/controls a business, or is a laborer/worker in that business. The second primary conceptualization of social class conceives of social class in terms of a market’s relative distribution of social resources and life chances (Weber, 1978). Common to both conceptualizations of social class is the social relationships underlying stratified groups: social class is not an inherent characteristic of individual persons, but rather emerges through social encounters between individuals and groups, for example between owners and workers, producers and consumers, or individuals and the distributive forces of the market (N. Krieger, Williams, & Moss, 1997; J. W. Lynch & Kaplan, 2000).
Measurement and subsequent delineation of social class location remains a fundamental challenge to research—particularly as it relates to understanding exactly how social class affects children’s health outcomes. As Wright (2007) suggests, a central explanation for the measurement challenge arises from the multidimensionality of social class. Wright contends that social class has six distinct functions or social actions: ‘distributional location’, ‘subjectively salient groups’, ‘life chances’, ‘antagonistic conflicts’, ‘historical variation’, and ‘emancipation’. From these we suggest that a subset of three actions of class are particularly relevant for understanding child health disparities. ‘Distributional location’ and ‘life chances’ both refer to the allocation of or opportunity to acquire material resources. ‘Subjectively salient groups’ refers to the manner by which group affiliation informs identity and location within a structure of inequality. Finally, ‘antagonistic conflict’ seeks to explain how social cleavages create real and powerful antagonism between groups of people.
These three actions of social class become clearer when placing them in the context of current theory exploring macrosystemic dynamics and processes as they relate to health. The allocation of, or opportunity to, acquire material resources action is paralleled by “fundamental cause” theory or the belief that social stratification of individuals within society leads to variation in the money, knowledge, power, and interpersonal resources necessary to prevent and manage illness, resulting in social disparities in health (Link & Phelan, 1995; Phelan, Link, & Tehranifar, 2010). A second theoretical approach dealing with distribution and life chances emerges from political economy, focusing not only on the social hierarchy of resources, status, and power, but on the political and social production of inequality (Navarro & Muntaner, 2004). This perspective goes beyond asking about the health consequences of being poor or non-poor to asking why and how some groups come to have less (or more) than others (N. Krieger, 2011). Political economy draws attention to the values, priorities, and structures of systems which produce the context in which children develop. A third theoretical frame focuses more on salient group identification and inter-group conflict, and the role of relative position within a social hierarchy as the driving force for social class health patterning (Wilkinson & Pickett, 2007). Thus, in this perspective, it is not an absolute level of material resources that produce health, but instead the presence of status inequality between groups, and the psychosocial stress resulting from awareness of one’s location within a more or less unequal hierarchy.
Theoretical foundations – bioecological model of human development
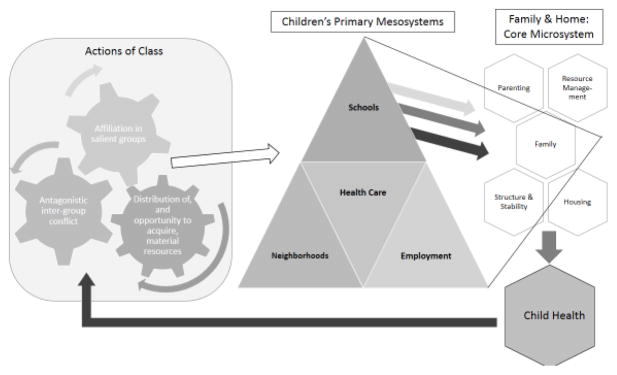
The conceptual framework guiding this manuscript (see Figure) is fundamentally informed by bioecological theory of human development (Bronfenbrenner & Ceci, 1994). A developmental theory is essential for understanding variation in children’s health, like health disparities, because health is a manifestation of development. Regardless of whether the focus is on infant birth weight, motor vehicle-related childhood fatality among toddlers, or any number of specific conditions like diabetes or asthma; children’s health risks and problems typically develop over time, thereby necessitating a developmental theory.
FIGURE.
Conceptual framework for how social class relates to child health and development
The proposed model uses three core ideas from bio-ecological theory. First, our model adopts the concept of proximal process as the primary engine for child health. Bio-ecological theory contends that human development occurs through proximal processes, which are defined as progressively more complex interactions between the child and the persons, objects, and symbols in the child’s environment. For example, the American Academy of Pediatrics (AAP) recommendation for child feeding represents a codified proximal process. The AAP recommends exclusive breastfeeding for the first six months of life (bottle feeding breastmilk or formula is also considered appropriate), with the gradual introduction of solid foods around six months of age, and the addition of healthy snacks around 9 months of age. In this case the proximal process is an interaction between the child and the parent (i.e., feeding behavior) that becomes increasingly complex (i.e., gradual growth in dietary diversity) and is presumed to contribute to optimal physical growth. A simple extension of this idea to child health more broadly suggests that poor health or morbidity results from stagnant or pathogenic interactions between the child and his or her environment such as those illustrated by a parent who provides no solid food to their child for the first year of life, or more extreme conditions such as abuse or maltreatment.
A second feature of bio-ecological theory reflected in the proposed framework (Figure) is the recognition that child development (health) results from nested interactions. This feature is visually depicted in our model in terms of “child health” being nested within the Family and Home Microsystem, with the nesting represented by the same geometric shape used to identify “child health” and distinct elements of family and home. Further, the Family and Home Microsystem is nested within Children’s Primary Mesosystems, a feature illustrated in the model by the placement of the microsystem within the three dimensional space of the mesosystem. Finally, both the Family and Home Microsystem and Children’s Primary Mesosystems are nested within systems of social stratification represented in terms of social class in our model.
The third and last feature of bio-ecological theory captured in this framework is the premise that proximal processes, the drivers of development (health), can be promoted or inhibited by more distal features of children’s environments. This feature is reflected by the arrows flowing from left to right (Figure). Social class and its core actions are posited to operate through two parallel levels of children’s environments. The first level influenced by social class is the mesosystem, which is conceived of as the institutions and establishments that children and their families interact with on a regular basis. Primary mesosystems in children’s lives include schools (childcare through formal education), the health care delivery system, neighborhoods, and employment opportunities for parents. The actions of social class shape Children’s Primary Mesosystems, albeit in complex ways which are illustrated by the “bent arrows”. Just as light entering and exiting a prism is bent based on its naturally-occurring or engineered angles, likewise the effects of social class on children are “bent” or otherwise modified depending on naturally-occurring or engineered features of children’s mesosystems. Children’s Primary Mesosystems, in turn affect the Family and Home Microsystem and the subsequent proximal processes contributing to child health.
A quintessential point of the proposed framework is that it steps beyond describing, toward explaining social class variation in children’s health. That is, social class recreates itself through a multistep process. In the first step, social class contributes to the financial and material resources and the sociopolitical dynamics of Children’s Primary Mesosystems, which, in turn, shape children’s Family and Home Microsystems in the second step. In the third and final step, interactions within children’s families and home set proximal processes relevant to health and illness into motion to create children’s health outcomes. Social class can then be recreated because differences in children’s health at birth and accentuated throughout childhood influence the social class children acquire as adults (A. Case, Fertig, & Paxson, 2005; Richards, Chapple-McGruder, Williams, & Kramer, 2015; Taylor, Repetti, & Seeman, 1997).
EMPIRICAL REVIEW
In order to highlight empirical evidence relevant to the theoretical foundations presented above, we briefly review literature illustrating current knowledge for the manner by which class patterns child health. Our review is limited to empirical evidence from high-income countries, recognizing that the manner in which social and economic stratification are experienced in low- and middle-income countries could be substantially different. An overarching objective is to view the extant literature through the lens of the multi-dimensional actions of class as characterized by Wright. Therefore we take this opportunity to characterize current evidence for how these actions of class might be embodied as child health, as well as pointing out areas where fuller examination of the mechanisms connecting class and health might be informative. To aid in focus and coherence in this section, we limit our review to child physical health outcomes. This in no way suggests that class is not relevant to cognitive, socioemotional, or mental health of children; on the contrary we believe these are inter-connected with physical health. We hope that the issues raised in the illustrations and discussions that follow can be readily translated beyond physical health.
Mesosystemic forces that shape child’s environment and family interactions
Employment
Parental employment is a resource that is not evenly distributed in society, but yet has substantial health implications for children. Recent evaluations of the Great Recession provide clear evidence that job loss and unemployment was not equally shared, but rather concentrated in areas with high concentrations of racial and ethnic minorities and individuals with low educational attainment (Thiede & Monnat, 2016). Areas with elevated unemployment experience greater unintentional injury of children (McClure, Kegler, Davey, & Clay, 2015), elevated preterm births (Messer et al., 2008), greater initiation of marijuana by adolescents (Tucker, Pollard, de la Haye, Kennedy, & Green, 2013), and more child maltreatment (Raissian, 2015). These results, connected with others wherein area unemployment is combined with other metrics of area socioeconomic deprivation and linked to health outcomes like morality (Singh & Kogan, 2007) suggest that jobs are a resource, that when scarce, impedes healthy child outcomes.
Jobs are also a distribution channel for additional resources at both the macro and micro levels. At the macro level community job loss has effects for all children, even those whose parents retain their jobs because higher unemployment compromises tax revenues resulting in lower governmental allocations for local health departments (Ye, Leep, & Newman, 2015) as well as education (Gassman-Pines, Gibson-Davis, & Ananat, 2015). Additionally, jobs are also used to distribute financial resources like earnings and health insurance. Indeed, employment-based insurance is the primary source of insurance coverage for Americans (Fronstin, 2013) and substantial evidence documents a close link between job loss and being uninsured (Doty, Collins, Robertson, & Garber, 2011; Lavarreda, Snyder, & Brown, 2013). Other resources that are built into jobs, such as work schedules that can be “flexed” to accommodate children’s needs and are advocated for promoting breastfeeding (Bettinelli, 2012; Hawkins, Griffiths, Dezateux, Law, & Millennium Cohort Study Child Health, 2007), are frequently less available to individuals in lower social classes (Heymann, 2001).
Substantially less research has considered the link of other actions of social class through employment to child health. Theory and research elaborated in the Parenting section of this manuscript documents the possibility of social class variation in parenting that may socialize children to better affiliate with salient occupational groups (white versus blue collar), and potentially serve as a source of intergroup conflict between these occupational groups. If the labor force continues to bifurcate with increasing value placed on science, technology, engineering and math (STEM) fields, pressures placed on children to acquire the characteristics of STEM professionals (i.e., salient group affiliation) may create fertile ground for negative health outcomes in both the short and long term (Saw, Berenbaum, & Okazaki, 2013; Shen, Liao, Abraham, & Weng, 2014). These are promising areas for future research.
Health care system distribution, access, and quality
Access to and interaction with the health care system is shaped by family socioeconomic position and is likely to contribute to class-based inequities in children’s physical health (Millman, 1993). Access to health care is measured in a variety of ways (Penchansky & Thomas, 1981), including having health insurance, access to a usual source of care, or utilization of needed services (Strickland, Jones, Ghandour, Kogan, & Newacheck, 2011). Children from families with lower incomes are less likely to have health insurance, less likely to have had a medical office visit or utilized a hospital outpatient center in the last year (Simpson et al., 2005), and less likely to get all the recommended vaccines (Christakis, Mell, Wright, Davis, & Connell, 2000; Health, Services, Health, & Services, 2003) as compared children from families with higher incomes. Lower income children are also more likely than higher income children to have made trips to the emergency room, had problems getting a necessary treatment or had a referral to a specialist (Simpson et al., 2005), more likely to have delayed care (Olson, Tang, & Newacheck, 2005), experienced increased risk for hospitalizations (Christakis, Mell, Koepsell, Zimmerman, & Connell, 2001), and have higher likelihood of ruptured appendicitis (Jablonski & Guagliardo, 2005).
These differences in access to, and utilization of, care exist despite the fact that, in the US, lower income children are eligible to enroll in public insurance through either Children’s Medicaid or the Children’s Health Insurance Program (CHIP). As of 2013, an estimated 88% of income-eligible children were enrolled in the program (The Urban Institute, 2015). Beginning in January 2014, the Affordable Care Act extended Medicaid eligibility to low income adults (those with incomes <138% of the federal poverty line) in the 32 states that opted into the Medicaid expansion component and provided subsidies for lower-middle income families in all states to purchase insurance, thus potentially covering many more lower-middle income children. It is not yet clear whether having non-Medicaid/CHIP insurance will help ameliorate the inequities in getting timely preventive and medical care. Unlike Children’s Medicaid and CHIP, often private medical insurance through employers or purchased through the ACA requires premiums, deductibles, and co-pays for office visits and medications that can act as a deterrent to seeking care for lower income families.
In this context inequities in access to quality health care may stem primarily from class-based resource allocation processes—for lower middle and middle income children, the high monetary cost of co-pays and premiums are a cost barrier, and for children covered by public health insurance, the monetary cost of health insurance is not the only cost of health care visits. Additional costs include lost wages, transportation costs, and time costs. Other resource allocation pathways could include the shortage of health service providers that accept patients with public insurance (Devoe et al., 2007) or more broadly the presence of geographic health professional shortage areas (Spelke, Zertuche, & Rochat, 2016; Wang & Luo, 2005). However at the intersection of race and class, other actions of class may be at play including inter-group conflict and salient group membership in accessing and delivering high quality healthcare. African American populations, who are disproportionately represented among those with low-incomes, have experienced repeated betrayals of trust by medical and research communities and continue to experience discrimination in the medical setting which likely contributes to higher levels of distrust of medical professionals seen among these populations (Rajakumar, Thomas, Musa, Almario, & Garza, 2009). This distrust may lead to delaying preventative care or treatment.
Strengthening causal inference for the relationship between access to health care and health outcomes requires methods or designs that can overcoming the major sources of confounding that exist between the insured and uninsured populations (Hadley, 2003). Both the Medicaid expansion component and the provision of subsidies to purchase health care could be leveraged as natural or quasi-experiments in order to better understand the impact of access to care on health. A handful of studies have begun to examine the impacts of ACA on health outcomes. These have focused primarily on adult health since adults’ insurance coverage is most affected; however, future studies should examine whether child health responds to changes in parents health coverage through the ACA as lack of insurance has been cited as a source of family stress and a barrier around providing optimal care for children (Devoe et al., 2007).
Neighborhood conditions
Because of historical processes of racial and economic residential segregation, children living in poor families often live in impoverished neighborhoods (Kramer & Hogue, 2009; Reardon & Bischoff, 2011). This means that poverty is not only an individual or family experience, but to the extent that high poverty neighborhoods have fewer amenities and greater social discord, it is also a community experience. In the U.S. in particular, poverty and race go hand-in-hand to impact children’s neighborhood contexts; whereas only 1.4% of white children live in both poor families and poor neighborhoods, 16.8% of black children experience this “double jeopardy” (Osypuk & Acevedo-Garcia, 2010).
Empirically, neighborhood environments have been linked to a wide range of child health outcomes including body mass index (BMI) (Chen & Paterson, 2006), overweight and obesity (Alvarado, 2016; Borrell, Graham, & Joseph, 2016; Sharifi et al., 2016), asthma and (McGrath, Matthews, & Brady, 2006) and blood pressure. (T. Leventhal & Brooks-Gunn, 2004). Much work reports that women living in disadvantaged neighborhoods are more likely to deliver infants preterm or low birth weights (Culhane & Elo, 2005; Margerison-Zilko et al., 2015; Masi, Hawkley, Piotrowski, & Pickett, 2007; Morenoff, 2003; Ncube, Enquobahrie, Albert, Herrick, & Burke, 2016; O’Campo et al., 2008; Vos, Posthumus, Bonsel, Steegers, & Denktas, 2014), suggesting possible intergenerational effects of neighborhood context, whereby the influence of disadvantaged environments on child health begins in utero or prior to conception. A small body of research has examined the specific pathways by which early-life neighborhood exposures influence children’s health. Chen and Paterson (2006) report that lower neighborhood socioeconomic status is associated with lower basal cortisol in adolescence, suggesting that neighborhood disadvantage may dysregulate the hypothalamic-pituitary-adrenal (HPA) axis, which is in turn associated with regulation of many physiological processes and health outcomes.
The ‘neighborhood effects’ literature has been critiqued on numerous counts (Oakes, 2004) including differentiation of selection versus causation, the challenge of identifying effects when there are few poor individuals living in salubrious environments (structural confounding), and measurement of contextual versus compositional features of neighborhoods (Arcaya et al., 2016; Schempf & Kaufman, 2012). Beyond addressing the challenges of causal inference, there are opportunities for enriching the conceptualization of class-based neighborhood effects with respect to the proximal processes for child health. Much of the neighborhood effects literature implicitly or explicitly posits that the drivers of neighborhood health gradients are distributional in nature, focusing on the allocation of resources and services to neighborhoods. However neighborhoods also represent relational spaces where salient group identity and inter-group conflict may play out in ways that impact child health (Cummins, Curtis, Diez-Roux, & Macintyre, 2007; Macintyre, Ellaway, & Cummins, 2002).
An example of the importance of salient group identity in neighborhoods concerns the production of local social norms. Neighborhood, community, and school social norms influence health behaviors such as tobacco and alcohol use among adolescents (Chuang, Ennett, Bauman, & Foshee, 2005, 2009; Eisenberg & Forster, 2003; Ennett, Flewelling, Lindrooth, & Norton, 1997; Frohlich, Potvin, Gauvin, & Chabot, 2002; Lipperman-Kreda, Grube, & Paschall, 2010; Lovato et al., 2010). The notion of salient groups may also come into play as a moderator of “neighborhood effects” if individuals’ interactions with their neighborhood’s service, physical, or social environment differs depending on their affiliation with other salient class-based groups. For example, the role of school environments on children’s BMI appears to differ by household-or neighborhood-level socioeconomic status (Carroll-Scott et al., 2015).
Much less attention has been paid to investigating the role of class-based antagonistic or inter-group conflict within neighborhoods and their effects on child health. For example, one line of inquiry could investigate how potentially conflict-generating processes such as gentrification and urban re-development, affordable housing, zoning, ordinances regarding property upkeep, policing programs (e.g., “stop and frisk”, decriminalization of marijuana), etc. affect the health of both the “beneficiaries” and “victims” of such programs. A few studies have attempted to explore the effects of neighborhood change and gentrification on birth outcomes (Huynh & Maroko, 2014; Margerison-Zilko et al., 2015), but this work is in its infancy and remains in need of advances in exposure measurement and replication.
The relatively large literature on factors such as social capital, social control, and collective efficacy could represent actions relevant to both salient group identity and inter-group conflict processes of class. Because collective efficacy may be strengthened in areas of racial, ethnic, or class homogeneity, identification with salient groups could promote cohesion. On the other hand, cross-class efforts at social control—for example around expectations for behavioral or aesthetic norms such as yard care—could result in inter-group conflict. While some empirical work has found that social cohesion, social control, and/or collective efficacy are associated with better health in adults, little work has examined these characteristics with respect to children’s physical health. Such work could follow the model of Donnelly and colleagues (2016) who found that adolescents who grew up in neighborhoods with high collective efficacy exhibited fewer depression and anxiety symptoms compared to those who grew up in neighborhoods with lower collective efficacy.
Education System
Educational attainment is one of the strongest predictors of adult morbidity and mortality (Hummer & Lariscy, 2011), and the expansion of compulsory education has been called among the most important health intervention instituted in countries around the globe (Desai & Alva, 1998; Machado-Rodrigues et al., 2014). While the association between education and health and longevity is widely documented, debate about the causal direction of education and health exists (J. L. Lynch & von Hippel, 2016). The lifecourse and transgenerational reproduction of education and health represent complex dynamics, and while health selection and residual confounding are not unimportant, the bulk of the evidence is consistent with a causal beneficial effect of greater education on health (Heckman, 2006; Montez & Friedman, 2015).
Though the link between education and cognitive development in children is most evident, educational policies and institutions can also directly impact child physical health through policies of mandatory vaccination or physical exams, and programs promoting physical education and nutrition. For example, schools can facilitate the delivery of services to children who are food insecure and lack health and dental care. In the U.S., the National School Lunch Program (NSLP) provides free or subsidized lunch (and often breakfast) for families at or below 185 percent of the federal poverty line (National School Lunch Program, 2012). Research has suggested that food insecurity is associated with obesity, lower energy, and more internalizing behavior problems in children (Weinreb et al., 2002); therefore providing meals during the school months may reduce negative health outcomes, improve concentration and provide a reliable source of nutrition and food for low-income children..
Educational systems also afford opportunities for children to be tested for vision, dental, and health issues through various screening programs. Most of these screenings are mandated by states and provide an avenue for identification and referral for identified with conditions that may be problematic to their learning. Unfortunately, the effectiveness and the amount of services vary from state to state with many of the highest need schools providing fewer services. Even though the infrastructure exists for providing services across class groups, as discussed previously in the section on neighborhood effects, there are still stark differences in how these children fare in poorer schools with large income gaps in achievement and unmet needs still present (Reardon, 2011).
Beyond the service environment of schools, the quality of school infrastructure could also affect health in class-dependent manner. Poorly funded schools are often built in areas and of materials that may be high in toxicants (e.g. lead and mercury) that have consequences for achievement (Miranda, Kim, Reiter, Galeano, & Maxson, 2009) and behavior (Dietrich, Douglas, Succop, Berger, & Bornschein, 2001). There appear to be no safe levels of lead exposure for the developing child (Centers for Disease Control and Prevention, 2012) and lead can be found in old buildings and contaminated soil. Almost every major city in the U.S. is dealing with the issue of lead exposure (Amato et al., 2012) in children and how both the home and school environment relate to exposure is important for understanding class disparities in children’s health.
Services such as school lunches and health screening represent one way that educational institutions and education-related policy seek to buffer or address disparities in the allocation of resources to children. The programs are successful to the extent that supply of needed services meet the distribution and intensity of demand. One emerging area of relevance for class and race-based disparities that arise from a different action of class is concern about the ‘school to prison pipeline’ and the disproportionate representation of poor black boys in school disciplinary events (Wald & Losen, 2003). One explanation for the disparate rate of school suspension of low income black and Latino children is conflicting expectations about ‘normal’ behavior and unequal tolerance for deviation from class-based norms (Skiba, R.S., Nardo, & Peterson, 2002).
Microsystemic forces that shape children’s interaction within family contexts
Parenting and Family Resource Management
Kohn and Schooler (1983) were among the first to comment upon and document social class variation in parenting activities. They argued that parents in middle- and upper-class families valued promoting children’s independence, decision-making and self-direction, whereas lower-class families valued or prioritized children’s deference to authority, rule-following and conformity. Kohn and Schooler surmised these distinct parenting values were held to prepare children for the occupation they would likely occupy in the future. Subsequent research has used class-based differences in parenting style to explain associations between childhood socioeconomic status and child and adult health outcomes including BMI trajectories (Lane, Bluestone, & Burke, 2013), and adult metabolic function (Lehman, Taylor, Kiefe, & Seeman, 2005).
Lareau (2002) presented compelling ethnographic evidence suggesting that middle-class parents take a fundamentally different approach to parenting than working class parents, and that differences in parenting were manifest in children’s own beliefs. “Concerted cultivation,” the form of parenting manifest by middle class parents, was characterized in terms of purposeful nurturance of children’s special gifts and interests through organized and structured activities. Children raised under this parenting model articulated feeling “special” because of the activities organized by their parents, and feeling “bored” if time was not sufficiently filled with structured activities. By contrast, “accomplishment of natural growth,” the approach to parenting observed by lower class families, was characterized in terms of parents providing basic care and allowing the child to grow. Children raised under this parenting model had a more “go with the flow” everyday experience that responded more to emergent experiences than planned events.
Analysis of the Early Childhood Longitudinal Study, Kindergarten Class (ECLS-K) reported that fully 50% of the variance in their measure of “concerted cultivation” was explained by multiple indicators of socioeconomic status, with the strongest effect leveraged by parental educational attainment (Cheadle & Amato, 2011). This logic is consistent with Wright’s notion of subjectively salient experiences. That is, class generates children’s subjectively salient experiences—one of which can be exposure to systematically different parenting styles or practices; this exposure helps steer children’s identity as being located on the lower (or higher) end of a system of economic stratification.
Parenting is closely related to the topic of family resource management, which, according to the National Council of Family Relations, focuses on “decisions individuals and families make about developing and allocating physical, psychological and social resources such as time, money, material assets, and energy.” Lareau’s (2002) work on class variation applies here as well. “Concerted cultivation” parenting expends more financial resources and structured time; by contrast, maintenance of kinship networks with family, including liberal opportunity for emergent play and interaction with older and younger peers within the family is exercised more deliberately by parents embracing “accomplishment of natural growth.”
Although not written under the general framework of “family resource management,” Wither Opportunities (Duncan & Murnane, 2011) draws substantial attention to how socioeconomic status creates substantial differences in how distinct household resources are allocated. This logic aligns closely with Wright’s view of class as generating an unequal allocation of resources and/or life chances. When the focus is placed on using financial resources to provide children with enriching experiences like sports or travel, individuals in the upper quintiles of household earnings spend between four and 10-times the amount of money (on sports and travel, respectively) than individuals in comparably sized families in the lowest quintiles of household earnings (Kaushal, Magnuson, & Waldfogel, 2011). In terms of the allocation of family time, mothers with higher levels of educational attainment spend more time engaging in literacy activities with their children and taking them to novel locations like museums (Phillips, 2011). The increasing emphasis placed on allocating time and financial resources to enriching children’s development has contributed to an expansion of the academic achievement gap between rich and poor (Reardon, 2011) and leads some to contend that “class differences in childrearing is on the rise” (Miller, 2015).
No research we know of has explored the notion of class as generating subjectively salient groups when examining parenting practices and child health. The extant literature relating class-based parenting activities to children’s health inequalities is more closely aligned with Wright’s view of class as producing an uneven allocation of resources and life chances. One prime example is that parents of different social classes vary in their ability to ensure access to healthy foods and also engage in varied feeding practices; both are key factors shaping children’s diet and development of healthy eating habits—two critical proximal processes—which are then reflected in outcomes such as overweight or obesity (Rhee, 2008). Overall, this literature is relatively nascent and deserves further attention; additionally, exploring class through the lens of subjectively salient groups would enrich future research on this topic.
Family structure, stability, and interpersonal dynamics
Family structure – in terms of number and relationship of caregivers –is strongly associated with socioeconomic status, and has been consistently associated with indicators of child health and development. Children living in single or stepparent homes are generally in worse health (Bramlett & Blumberg, 2007; Carr & Springer, 2010; Mauldon, 1990; Montgomery, Kiely, & Pappas, 1996), show elevated levels of health vulnerability (Dawson, 1991), participate in fewer routine medical and dental visits (Anne Case & Paxson, 2001), and have worse access to preventative health care (Gorman & Braverman, 2008) than their counterparts living in two biological parent families. Child health is further stratified by parental cohabitation status. For example the risk of asthma diagnosis is highest among children of single mothers, intermediate among children of cohabiting mothers, and lowest among children of married mothers (Harknett, 2009). A similar pattern is evident for birth weight: the highest weights at birth are found among infants born to married mothers, intermediate weights among infants born to cohabiting mothers, and lowest weights among infants born to single mothers (Kane, 2016).
Much of the literature on families in the U.S. has transitioned away from simple dichotomies of biological parent families versus all other types (single parent, step family, gay/lesbian family), and now commonly distinguish families according to other criteria related to family processes and parental dynamics, such as parental stability, father involvement, and/or quality of parental relationships (Carr & Springer, 2010). For example, instability in parental relationships is associated with worse child health (Bzostek & Beck, 2011) and family instability mediates at least a portion of the association between maternal depression and lower levels of childhood health (Turney, 2011). Father’s multiple-partner fertility is also linked with poorer childhood health, and this association is mediated at least at in part by a reduction in the frequency of father’s engagement with his child on a weekly basis (Bronte-Tinkew, Horowitz, & Scott, 2009). However higher levels of engagement of fathers who reside in the home—regardless of whether they are biological or “social” fathers (meaning, men who are romantically involved with the mother and take on the social role of fatherhood)—are positively associated with child health (Bzostek, 2008). No studies we are aware of have examined children’s physical health across heterosexual and gay/lesbian families, but, there is evidence suggesting children’s mental health is not significantly different across heterosexual parent families and same-sex parent families (Patterson, 2006; Stacey & Biblarz, 2001). Siblings are also an integral part of families-of-origin, and potentially make important contributions to children’s health. Older siblings can function as an additional source of learning and socialization for younger siblings, and can directly and indirectly influence the behaviors and attitudes of younger siblings, which may in turn be linked with health.
Sibling interactions can spur social-cognitive development while sibling conflict is linked with deviance and substance use (McHale, Updegraff, & Whiteman, 2012); presence or absence of high-quality sibling relationships, comprised of warmth, closeness, and lack of conflict, also mediate the association between single-parent family structure and children’s substance abuse, sexual risk behaviors, and risk of contracting a sexually transmitted infection (East & Khoo, 2005). Having multiple siblings is generally associated with a dilution of family resources (McHale et al., 2012); this may also adversely impact a child’s health.
As with other microsystem processes, much of the literature on class, family structure and child health has been grounded in a life chances and/or unequal distribution of resources framework. In contrast, we suspect the class actions of subjectively salient groups could generate new insights. Social classes generate subjectively salient experiences such as growing up in an economically disadvantaged single parent family. These experiences in turn critically shape the schema people use to locate themselves and others within a system of economic stratification. As an example, we speculate social isolation and support at the family-level could reflect class-based processes generating subjectively salient experiences, such as multiple spells of unemployment that prompts a series of residential moves, putting family members at risk of social isolation. At a more basic level, social isolation and social support have powerful and enduring effects on health. The literature on adult health shows this very clearly [see for example (House, Landis, & Umberson, 1988; House, Umberson, & Landis, 1988)]. Some evidence along these lines has been shown for health early on in the life course. Low-income children whose mothers are socially isolated exhibit higher rates of serious accidents, injuries, and poisonings (Leininger, Ryan, & Kalil, 2009). Maternal perceptions of instrumental support predict higher levels of child health (Turney, 2013), whereas greater household chaos (meaning, a crowded, noisy, and unpredictable environment) predict lower levels of child health (Dush, Schmeer, & Taylor, 2013). In sum, health is likely maximized among children who belong to a family in which both the parent-child and sibling relationships are characterized by high levels of closeness and warmth, as well as high levels of social support which may buffer the child from the full effects of stressful events.
Housing
While family structure, dynamics, and resources are primary elements of the microsystem, the intimate physical context of family life is the home, and this environment is also part of children’s microsystems. As a source of protection from the elements, animals and insects, and a place to safely store valuables and food, housing is—in Maslow’s hierarchy of needs—a fundamental human necessity. A lack of housing, or, homelessness, is associated with higher levels of food insecurity and poor nutrition for children, as well as increased behavioral problems and developmental delays, relative to housed poor children (Wood, Valdez, Hayashi, & Shen, 1990). For housed children, the quality and stability of the built structure and utility services provided to households can also affect health. Quinn and colleagues (2010) found that children living in homes with more infrastructure and service stressors had lower self-rated health, reduced controllability of asthma, and more unplanned medical visits. Exposure to dust mites and indoor air mold appear to increase risk for the development and exacerbation of asthma in children (Jaakkola, Hwang, & Jaakkola, 2005; Johnston, 2000). There is also strong evidence for the negative effect of specific toxicants in the home, such as lead, on children’s health outcomes. Lead paint dust is well-known to cause severe and irreversible cognitive development problems (J. Krieger & Higgins, 2002) and surveillance data indicates that dangerously high levels of lead are 12 times as common for low income children compared to higher income children (6% vs 0.5%) (Raymond, Wheeler, & Brown, 2014).
Crowding is an additional housing feature that is more prevalent among lower-income populations and has been associated with increased risk for childhood respiratory (Baker, Taylor, & Henderson, 1998) and gastrointestinal diseases (McCallion et al., 1996), potentially due to a higher degree of infectious disease transmission among individuals living in crowded conditions (Tama Leventhal & Newman, 2010). Crowding has also been associated with inadequate sleep among adults (Chambers, Pichardo, & Rosenbaum, 2014) and lack of personal space is thought to contribute to social and emotional challenges among adults and children; however, few studies have looked at this specifically (Tama Leventhal & Newman, 2010). Housing quality and instability can also indirectly affect children’s health through their impact on family processes such as high levels of parental stress or depression and increased parental conflict (in the wake of job loss or persistent poverty for example) (Haurin, Parcel, & Haurin, 2002; Tama Leventhal & Newman, 2010).
Overall, the literature on class-based differences in housing and child health rely on an allocation and distribution action of class as the motivating process. Whether salient group affiliation (e.g. from residence in particular housing class such as public housing) or inter-group conflict (e.g. as might arise in mixed income housing developments) further transmits class differences to child health disparities is unclear but potentially enlightening.
Embodying social environments
In summary there is varied evidence for the manner in which the actions of social class shape and affect the meso- and microsystem environments to which children are most exposed. To the extent that the class-based influence on these environments affects the critical proximal processes of child health and development, the social environment may be physically embodied as illness or wellness. These processes are evident across the lifecourse of individuals, but because of the transgenerational nature of class, may also be communicated from one generation to the next. Most efforts to examine the actions of class implicitly frame the question in terms of differential allocation or distribution of necessary resources. This is clearly a potent and intuitive action. However opportunities may exist for further understanding actions of class – and possible unintended consequences of social policies – including the production of salient group experiences and antagonistic inter-group conflicts. If these sources of experience also serve as proximal processes they too become part of the reproduction of class and class-based health disparities.
HIGH PROFILE TARGETS FOR FUTURE RESEARCH
In the end, what contributions are made by this high level review focused on how social class “gets under the skin” to affect children’s health, and what next steps are needed? First, although the idea of socioeconomic differences in children’s health is not new (e.g. Evans, Miller, & Seeman, 2012), this paper provides one way to organize the broad domains of relevant research and theory across multiple disciplines into a coherent conceptual model. The fact that there is clear theoretical rationale and corroborating empirical evidence for many of the pathways proposed in the model (Figure) speaks to its potential utility for building an integrated understanding of population variability in children’s health. Second, despite its high level nature, this review points to several discrete ideas, such as the importance of the conceptual meaning of social class and its diverse modes of action that have unique and distinct implications for children’s health. Another discrete and unique point uncovered by this review is the diverse means by which social class “gets under the skin”. Psychosocial stress and the biologic sequelae are meaningful and deserving of attention. However, we also highlight other conceptually more direct and potentially actionable pathways, such as paraoccupational exposure to disease agents or differential exposure or vulnerability to environmental toxicants (e.g., proximity to hazardous sites), aging infrastructure (e.g., recent Flint water problems), and poor housing stocks. Finally, this review illustrates the complexity of child health and development and the corresponding need to work across boundaries separating disciplines and the worlds of “discovery” and “practice” to protect the health of all children.
Contributions notwithstanding, this review highlights multiple areas for additional work. The upcoming areas highlight ways of operationalizing Wright’s actions of social class and “high priority” areas for future basic and policy research. The identified items are considered “high priority” for several different reasons; either because the item addresses a basic critical gap in the knowledge base, because it would generate substantial impact, or because it would open doors that have historically been closed.
Operationalizing Wright’s Actions of Social Class
The framework linking social class to child health and the evidence provided in the empirical review above highlight the importance of creating theoretical and empirical clarity about how the three different actions of social class influence child health. Thus, it is necessary to consider how one might operationalize the framework and what difficulties might arise in the process. The biggest lesson from our framework is that researchers should use different indicators of social class depending on the actions being tested. Some health pathways will call for distributional indicators such as income, wealth, or education; others will need to be more focused on salient groups or antagonistic conflicts using occupational prestige or latent classifications of groups as indicators. In addition, researchers need to be sensitive to the way that different spatial and temporal scales influence indicators of social class. For instance, social class might be operationalized at the level of individual persons, households, or spatially across neighborhoods, each reflecting a distinct manifestation of social class, and each measuring different aspects of the distribution of resources, status and power. Similarly, many measures are temporally dynamic throughout the life course of an individual, across generations within families, and through history of successive cohorts, necessitating attention to the timing of measurement (Kane & Lam, 2011).
For example, technological progress has shifted the relative social position of people with different levels of educational attainment. Cohorts born in the early twentieth century in the United States had low high school and college completion rates of approximately 10 and 6 per cent respectively (Bailey & Dynarski, 2011). The relative prevalence and earnings of each group has changed dramatically as more people attended secondary schools and universities. High school graduates have seen a relative decline in their wage premium compared to 8th grade graduates from 35 percent in the early twentieth century to 20 percent or less by the end of the twentieth century. College graduates, on the other hand, have seen an increase in their wage premium versus high school graduates from 31 percent in 1950 to 62 percent in 2005 suggesting an increase in the relative status and resources returned from a fixed level of education (Goldin & Katz, 2000, 2007). These variations over time are also matched by spatial variations in high school and college completion rates and the relative status and wage premium of degrees (Goldin & Katz, 2000; Snyder & Dillow, 2015). Cohort and period influences on these various indicators of social class highlight the importance of contextualizing studies in time and space when analyzing how social class influences child health; explicitly examining cohort and period patterns in child health trends may contribute to our understanding of the dynamics of child health disparities.
Basic Research
The first high priority area for research is the need for more studies that use experimental or quasi-experimental designs. The vast majority of studies covered in this review are based on observational, albeit complex observational, designs such as those deployed in the National Longitudinal Study of Adolescent to Adult Health (Add Health) and Early Childhood Longitudinal Program (ECLS) studies that use rigorous sampling procedures and multimodal data collection techniques. Nevertheless, strong causal inference demands random assignment to change agents or designs that mimic these features. Experimental studies of overt attempts to manipulate some feature of socioeconomic position do exist. The Perry Preschool Project, for example, allocated educational resources and family wrap-around services to promote parental labor force engagement in low-income families. The program essentially simulated an upward shift in social position through the provision of sustained high-quality childcare for low income children and resources to enhance human capital for parents. Long-term evaluations of the Perry Preschool Project demonstrate a substantial return on investment in terms of benefits to individual children and broader societal benefits (Heckman, Moon, Pinto, Savelyev, & Yavitz, 2010; Nores, Belfield, Barnett, & Schweinhart, 2005). In contrast results from the Moving to Opportunity program, another simulation of an upward shift in social position by allowing impoverished families to move into better (albeit still low income) neighborhoods, are mixed. Specifically, results indicated greater rates of depression and other behavioral health outcomes (i.e., PTSD and conduct disorder) among boys who moved, but reduced rates of depression and conduct disorder among girls who moved (Kessler et al., 2014). More recent results suggest economic effects in young adulthood varied by the age of the child at the time of intervention, with positive economic outcomes in young adulthood for children who moved before age 13, but either null or detrimental effects for moves after age 13 (Chetty, Hendren, & Katz, 2015). Together, these findings highlight the complex, and often unintended consequences of social interventions and the importance of their timing in the life course.
Experiments like the Perry Preschool Project and the Moving to Opportunity program make a valuable contribution to the literature, but they also have shortcomings. A simple shortcoming is that “health” is an atypical outcome in many of these projects; consequently, research designed to delineate variation in meaningful and age-appropriate health outcomes across assignment groups is needed. Perhaps the greatest shortcoming of existing experimental work is the inability to attend to distinct putative effects of competing elements or actions of social class. Building on Wright’s work we propose three distinct functions or modes of action, minimally, (Figure) that require isolation to understand how manipulations to social position may produce health outcomes. Consider, for example, the complex and presumably counter-intuitive findings from Kessler and colleagues (2014) evaluation of the Moving to Opportunity program: residential relocation is ripe with stressors ranging from the simple moving logistics, to all the nuances of acquiring familiarity in your new community (e.g., finding products in the local supermarket, finding your way to basic services) and the social stressors of losing contact with some acquaintances while trying to build new ones. This reality highlights a basic confound in the Moving to Opportunity experimental group: they all “benefited from resource allocation” but they were also all reallocated (to varying degrees) to a different social group and confronted with sources of group conflict.
Data linkage initiatives (and the resulting ‘Big Data’) are another high priority research activity stimulated by this review. Definitive studies designed to capture nuanced conceptual features of the actions of class, multiple pathways to child health, an array of developmentally appropriate health outcomes, and the myriad of possible behavioral and biological mediators are typically not feasible. Moreover, even if feasible, collecting these data in a single study would be inefficient because they already exist in several distinct areas such as income tax returns, school records, electronic medical records, personal health information maintained in proprietary applications (e.g., physical activity apps such as Fitbit, INike, Runkeeper), county land use records and other sources that will undoubtedly grow as technology expands. Consequently, the current problem is not necessarily the absence of data, but rather the ability to harvest and integrate existing data. Indeed advancements in bioinformatics and expansion of comprehensive health information exchanges provide substantial potential for linking studies of the social world with useful child health outcomes. Of course such tools are not a panacea, recognizing that medical records are not typically collected for research purposes, and that information maintained in health information exchanges is only relevant to users of health services. Nevertheless, recognizing that some health information exchanges like those by major insurers such as Kaiser Permanente boast greater than 90% of covered lives within specific catchment areas, harnessing the strength of these tools for research is necessary.
Policy Research
Research to identify potential competing or conflicting commitments within policies is needed. Policy makers interested in protecting or promoting children’s health oftentimes have multiple commitments to balance. Self-evidently, the development of any given policy whose express purpose is to improve child health demonstrates a commitment to child health. However, in the real world riddled with limited resources, competing world views on who is responsible for child health, and what “health” really means, any policy maker will quickly confront other commitments. Possible competing commitments can be pragmatic (e.g., concerns about losing the next election), moralistic (e.g., all children deserve basic health care), ideological (e.g., the ability to provide services under the policy should be determined through a competitive process), or political (e.g., I want to keep a friendly relationship with “Entity A”, who opposes the proposed policy). While some commitments may compete, others may clearly conflict. Consider, for example, federal policy supporting Head Start. The policy is clearly committed to children (and families) living in poverty. Nevertheless competing commitments related to accountability, such as grantees’ ability to meet performance standards (e.g. section 641A to Title 42 of US Code 9836A) and requirements for active parent involvement (e.g. section 642 of Title 42 of US Code 9837) can result in Head Start agencies screening out children who are most in need.
Research or critical analyses of underlying conceptual mechanisms targeted in policies intended to benefit children’s health (either in the short or long term) is needed. As others have noted (Komro, Burris, & Wagenaar, 2014), very few policies have been evaluated for their putative effects on child and family health outcomes. One illustration of this need is the conflicting and counter-intuitive adolescent mental and behavioral health findings previously described from the Moving to Opportunity program (Kessler et al., 2014). The findings that male adolescents receiving the opportunity to move to a better neighborhood experienced poorer (rather than better) mental and behavioral health outcomes than their peers in the control group does not make sense from a “Class as Inadequate Access to Resources” perspective. But, the results make more sense when viewed from a “Class as group affiliation” or “Class as group conflict” perspectives. Similarly, the putative value of various policy approaches to “school choice”, whether through voucher systems to private schools or transportation options within district, such policies are predicated on a view of class wherein access to resources is viewed as the key criterion, whereas consequences resulting from disruptions to group affiliation and potential shifts in group conflict are given less attention. Conversely, policy attempts driven more by perspectives of class as group affiliation or attempts to minimize group conflict, such as strategies to build social capital have been presumed to yield greater health benefits than those focused on resource allocation (Scheffler & Brown, 2008). Researchers should evaluate ongoing and new policy experiments like state’s willingness to adopt Medicaid expansion, school choice and the array of social welfare programs to determine whether or how they are affecting children’s health (Komro et al., 2014). More importantly, such results—informed by analysis plans that capture variation in the distinct modes of action underlying social class—would ensure delivery of clear information to decision makers as to why specific elements of, or entire, policies help or harm children’s health.
In sum, explaining the ubiquitous finding of social class gradients in child health is complex and the possible causes operate across many levels and domains; yet the posited causal processes producing the gradient need not be seen as a ‘black box’ of invisible steps. Our conceptual model is certainly a vast over-simplification, but by bringing together the theoretical perspectives and empirical evidence of multiple disciplines it offers one possible view of testable (and in some cases actionable) pathways and mechanisms by which social class ‘gets under the skin’ to affect children’s health and development.
Acknowledgments
The Eunice Kennedy Shriver National Institute Of Child Health & Human Development of the National Institutes of Health provided support for MRK (K01HD074726), JBK (K99/R00 HD075860), PDK (R01HD061294), and JGG (R01HD061010); CMZ received support from National Heart, Lung, and Blood Institute (K01HL128843); EBS received support from the Economic and Social Research Council (ES/L010267/1).
Contributor Information
Michael R. Kramer, Department of Epidemiology, Rollins School of Public Health, Emory University, 1518 Clifton Road, NE, Atlanta, GA 30322.
Eric B. Schneider, Department of Economic History, London School of Economics and Political Science.
Jennifer B. Kane, Department of Sociology, University California, Irvine
Claire Margerison-Zilko, Department of Epidemiology and Biostatistics, College of Human Medicine, Michigan State University.
Jessica Jones-Smith, Department of International Health, Johns Hopkins Bloomberg School of Public Health.
Katherine King, Department of Community and Family Medicine, Duke University.
Pamela Davis-Kean, Department of Psychology, University of Michigan.
Joseph G. Grzywacz, Department of Family & Child Sciences, Florida State University.
REFERNCES
- Alvarado SE. Neighborhood disadvantage and obesity across childhood and adolescence: Evidence from the NLSY children and young adults cohort (1986–2010) Soc Sci Res. 2016;57:80–98. doi: 10.1016/j.ssresearch.2016.01.008. [DOI] [PubMed] [Google Scholar]
- Amato MS, Moore CF, Magzamen S, Imm P, Havlena JA, Anderson HA, Kanarek MS. Lead exposure and educational proficiency: moderate lead exposure and educational proficiency on end-of-grade examinations. Annals of epidemiology. 2012;22(10):738–743. doi: 10.1016/j.annepidem.2012.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arcaya MC, Tucker-Seeley RD, Kim R, Schnake-Mahl A, So M, Subramanian SV. Research on neighborhood effects on health in the United States: A systematic review of study characteristics. Soc Sci Med. 2016;168:16–29. doi: 10.1016/j.socscimed.2016.08.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey MJ, Dynarski SM. Gains and gaps: Changing inequality in US college entry and completion. NBER Working Papers. 2011;(17633) [Google Scholar]
- Baker D, Taylor H, Henderson J. Inequality in infant morbidity: causes and consequences in England in the 1990s. ALSPAC Study Team. Avon Longitudinal Study of Pregnancy and Childhood. Journal of epidemiology and community health. 1998;52(7):451–458. doi: 10.1136/jech.52.7.451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauer GR. Incorporating intersectionality theory into population health research methodology: challenges and the potential to advance health equity. Soc Sci Med. 2014;110:10–17. doi: 10.1016/j.socscimed.2014.03.022. [DOI] [PubMed] [Google Scholar]
- Bettinelli ME. Breastfeeding policies and breastfeeding support programs in the mother’s workplace. J Matern Fetal Neonatal Med. 2012;25(Suppl 4):81–82. doi: 10.3109/14767058.2012.715033. [DOI] [PubMed] [Google Scholar]
- Borrell LN, Graham L, Joseph SP. Associations of Neighborhood Safety and Neighborhood Support with Overweight and Obesity in US Children and Adolescents. Ethn Dis. 2016;26(4):469–476. doi: 10.18865/ed.26.4.469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bramlett MD, Blumberg SJ. Family structure and children’s physical and mental health. Health Affairs. 2007;26(2):549–558. doi: 10.1377/hlthaff.26.2.549. [DOI] [PubMed] [Google Scholar]
- Bronfenbrenner U, Ceci SJ. Nature-nuture reconceptualized in developmental perspective: A bioecological model. Psychological Review. 1994;101(4):568–586. doi: 10.1037/0033-295x.101.4.568. [DOI] [PubMed] [Google Scholar]
- Bronte-Tinkew J, Horowitz A, Scott ME. Fathering with multiple partners: Links to children’s well-being in early childhood. Journal of Marriage and Family. 2009;71(3):608–631. [Google Scholar]
- Bzostek SH. Social Fathers and Child Well-Being. Journal of Marriage and Family. 2008;70(4):950–961. [Google Scholar]
- Bzostek SH, Beck AN. Familial instability and young children’s physical health. Social Science & Medicine. 2011;73(2):282–292. doi: 10.1016/j.socscimed.2011.04.014. [DOI] [PubMed] [Google Scholar]
- Carr D, Springer KW. Advances in families and health research in the 21st century. Journal of Marriage and Family. 2010;72(3):743–761. [Google Scholar]
- Carroll-Scott A, Gilstad-Hayden K, Rosenthal L, Eldahan A, McCaslin C, Peters SM, Ickovics JR. Associations of Neighborhood and School Socioeconomic and Social Contexts With Body Mass Index Among Urban Preadolescent Students. Am J Public Health. 2015;105(12):2496–2502. doi: 10.2105/AJPH.2015.302882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Case A, Fertig A, Paxson C. The lasting impact of childhood health and circumstance. J Health Econ. 2005;24(2):365–389. doi: 10.1016/j.jhealeco.2004.09.008. [DOI] [PubMed] [Google Scholar]
- Case A, Paxson C. Mothers and others: who invests in children’s health? Journal of health economics. 2001;20(3):301–328. doi: 10.1016/s0167-6296(00)00088-6. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. CDC response to Advisory Committee on Childhood Lead Poisoning Prevention recommendations in “Low Level Lead Exposure Harms Children: A Renewed Call of Primary Prevention”. 2012. Retrieved from Atlanta, GA. [Google Scholar]
- Chambers EC, Pichardo MS, Rosenbaum E. Sleep and the housing and neighborhood environment of urban Latino adults living in low-income housing: the AHOME study. Behavioral sleep medicine. 2014:1–16. doi: 10.1080/15402002.2014.974180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheadle JE, Amato PR. A Quantitative Assessment of Lareau’s Qualitative Conclusions About Class, Race, and Parenting. Journal of Family Issues. 2011;32(5):679–706. [Google Scholar]
- Chen E, Paterson LQ. Neighborhood, family, and subjective socioeconomic status: How do they relate to adolescent health? Health Psychol. 2006;25(6):704–714. doi: 10.1037/0278-6133.25.6.704. [DOI] [PubMed] [Google Scholar]
- Chetty R, Hendren N, Katz LF. The effects of exposure to better neighborhoods on children: New evidence from the Moving to Opportunity experiment. 2015;(w21156) doi: 10.1257/aer.20150572. [DOI] [PubMed] [Google Scholar]
- Christakis DA, Mell L, Koepsell TD, Zimmerman FJ, Connell FA. Association of lower continuity of care with greater risk of emergency department use and hospitalization in children. Pediatrics. 2001;107(3):524–529. doi: 10.1542/peds.107.3.524. [DOI] [PubMed] [Google Scholar]
- Christakis DA, Mell L, Wright JA, Davis R, Connell FA. The association between greater continuity of care and timely measles-mumps-rubella vaccination. Am J Public Health. 2000;90(6):962–965. doi: 10.2105/ajph.90.6.962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chuang YC, Ennett ST, Bauman KE, Foshee VA. Neighborhood influences on adolescent cigarette and alcohol use: mediating effects through parent and peer behaviors. J Health Soc Behav. 2005;46(2):187–204. doi: 10.1177/002214650504600205. [DOI] [PubMed] [Google Scholar]
- Chuang YC, Ennett ST, Bauman KE, Foshee VA. Relationships of adolescents’ perceptions of parental and peer behaviors with cigarette and alcohol use in different neighborhood contexts. J Youth Adolesc. 2009;38(10):1388–1398. doi: 10.1007/s10964-009-9424-x. [DOI] [PubMed] [Google Scholar]
- Culhane JF, Elo IT. Neighborhood context and reproductive health. Am J Obstet Gynecol. 2005;192(5 Suppl):S22–29. doi: 10.1016/j.ajog.2005.01.071. [DOI] [PubMed] [Google Scholar]
- Cummins S, Curtis S, Diez-Roux AV, Macintyre S. Understanding and representing ‘place’ in health research: a relational approach. Soc Sci Med. 2007;65(9):1825–1838. doi: 10.1016/j.socscimed.2007.05.036. [DOI] [PubMed] [Google Scholar]
- Dawson DA. Family structure and children’s health and well-being: Data from the 1988 National Health Interview Survey on Child Health. Journal of Marriage and the Family. 1991:573–584. [Google Scholar]
- Desai S, Alva S. Maternal education and child health: Is there a strong causal relationship? Demography. 1998;35(1):71–81. [PubMed] [Google Scholar]
- Devoe JE, Baez A, Angier H, Krois L, Edlund C, Carney PA. Insurance + access not equal to health care: typology of barriers to health care access for low-income families. Ann Fam Med. 2007;5(6):511–518. doi: 10.1370/afm.748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dietrich KN, Douglas RM, Succop PA, Berger OG, Bornschein RL. Early exposure to lead and juvenile delinquency. Neurotoxicology and teratology. 2001;23(6):511–518. doi: 10.1016/s0892-0362(01)00184-2. [DOI] [PubMed] [Google Scholar]
- Donnelly L, McLanahan S, Brooks-Gunn J, Garfinkel I, Wagner BG, Jacobsen WC, … Gaydosh L. Cohesive Neighborhoods Where Social Expectations Are Shared May Have Positive Impact On Adolescent Mental Health. Health Aff (Millwood) 2016;35(11):2083–2091. doi: 10.1377/hlthaff.2016.0721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doty MM, Collins SR, Robertson R, Garber T. When unemployed means uninsured: the toll of job loss on health coverage, and how the Affordable Care Act will help. Issue Brief (Commonw Fund) 2011;18:1–18. [PubMed] [Google Scholar]
- Duncan GJ, Murnane RJ, editors. Whither opportunity?: rising inequality, schools, and children’s life chances. New York: Russell Sage Foundation; 2011. [Google Scholar]
- Dush CMK, Schmeer KK, Taylor M. Chaos as a social determinant of child health: Reciprocal associations? Social Science & Medicine. 2013;95:69–76. doi: 10.1016/j.socscimed.2013.01.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- East PL, Khoo ST. Longitudinal pathways linking family factors and sibling relationship qualities to adolescent substance use and sexual risk behaviors. Journal of Family Psychology. 2005;19(4):571. doi: 10.1037/0893-3200.19.4.571. [DOI] [PubMed] [Google Scholar]
- Eisenberg ME, Forster JL. Adolescent smoking behavior: measures of social norms. Am J Prev Med. 2003;25(2):122–128. doi: 10.1016/s0749-3797(03)00116-8. [DOI] [PubMed] [Google Scholar]
- Ennett ST, Flewelling RL, Lindrooth RC, Norton EC. School and neighborhood characteristics associated with school rates of alcohol, cigarette, and marijuana use. J Health Soc Behav. 1997;38(1):55–71. [PubMed] [Google Scholar]
- Evans GW, Miller CE, Seeman T. How poverty gets under the skin: A life course perspective. In: King R, Maholmes V, editors. Oxford Handbook of Poverty and Child Development. Oxford: Oxford University Press; 2012. [Google Scholar]
- Frohlich KL, Potvin L, Gauvin L, Chabot P. Youth smoking initiation: disentangling context from composition. Health Place. 2002;8(3):155–166. doi: 10.1016/s1353-8292(02)00003-5. [DOI] [PubMed] [Google Scholar]
- Fronstin P. Sources of health insurance and characteristics of the uninsured: analysis of the March 2013 Current Population Survey. EBRI Issue Brief. 2013;(390):1, 4–34. [PubMed] [Google Scholar]
- Gassman-Pines A, Gibson-Davis CM, Ananat EO. How Economic Downturns Affect Children’s Development: An Interdisciplinary Perspective on Pathways of Influence. Child Development Perspectives. 2015;9(4):233–238. doi: 10.1111/cdep.12137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldin C, Katz LF. Education and Income in the Early Twentieth Century: Evidence from the Prairies. The Journal of Economic History. 2000;60(03):782–818. [Google Scholar]
- Goldin C, Katz LF. The Race between Education and Technology: The Evolution of U.S. Educational Wage Differentials, 1890 to 2005. NBER Working Paper. 2007;(12984) [Google Scholar]
- Gordon MM. Social class in American sociology. American Journal of Sociology. 1949;55:262–268. doi: 10.1086/220535. [DOI] [PubMed] [Google Scholar]
- Gorman BK, Braverman J. Family structure differences in health care utilization among US children. Social Science & Medicine. 2008;67(11):1766–1775. doi: 10.1016/j.socscimed.2008.09.034. [DOI] [PubMed] [Google Scholar]
- Hadley J. Sicker and poorer--the consequences of being uninsured: a review of the research on the relationship between health insurance, medical care use, health, work, and income. Med Care Res Rev. 2003;60(2 Suppl):3S–75S. doi: 10.1177/1077558703254101. discussion 76S–112S. [DOI] [PubMed] [Google Scholar]
- Harknett K. Why are children with married parents healthier? The case of pediatric asthma. Population Research and Policy Review. 2009;28(3):347–365. [Google Scholar]
- Haurin DR, Parcel TL, Haurin RJ. Does homeownership affect child outcomes? Real Estate Economics. 2002;30(4):635–666. [Google Scholar]
- Hawkins SS, Griffiths LJ, Dezateux C, Law C Millennium Cohort Study Child Health G. The impact of maternal employment on breast-feeding duration in the UK Millennium Cohort Study. Public Health Nutr. 2007;10(9):891–896. doi: 10.1017/S1368980007226096. [DOI] [PubMed] [Google Scholar]
- Health, U. D. o., Services, H., Health, U. D. o., & Services, H. National healthcare disparities report. Rockville (MD): Agency for Healthcare Research and Quality; 2003. [Google Scholar]
- Heckman JJ. Skill formation and the economics of investing in disadvantaged children. Science. 2006;312(5782):1900–1902. doi: 10.1126/science.1128898. [DOI] [PubMed] [Google Scholar]
- Heckman JJ, Moon SH, Pinto R, Savelyev PA, Yavitz A. The rate of return to the HighScope Perry Preschool Program. Journal of public economics. 2010;94:114–128. doi: 10.1016/j.jpubeco.2009.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heymann J. The Widening Gap. New York, NY: Basic Books; 2001. [Google Scholar]
- House JS, Landis KR, Umberson D. Social relationships and health. Science. 1988;241(4865):540–545. doi: 10.1126/science.3399889. [DOI] [PubMed] [Google Scholar]
- House JS, Umberson D, Landis KR. Structures and processes of social support. Annual Review of Sociology. 1988:293–318. [Google Scholar]
- Hummer RA, Lariscy JT. Educational attainment and adult mortality. In: Rogers RG, Crimmins EM, editors. International Handbook of Adult Mortality. Netherlands: Springer; 2011. [Google Scholar]
- Huynh M, Maroko AR. Gentrification and preterm birth in New York City, 2008–2010. J Urban Health. 2014;91(1):211–220. doi: 10.1007/s11524-013-9823-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaakkola JJ, Hwang B-F, Jaakkola N. Home dampness and molds, parental atopy, and asthma in childhood: a six-year population-based cohort study. Environmental health perspectives. 2005:357–361. doi: 10.1289/ehp.7242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jablonski KA, Guagliardo MF. Pediatric appendicitis rupture rate: a national indicator of disparities in healthcare access. Popul Health Metr. 2005;3(1):4. doi: 10.1186/1478-7954-3-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston R. Clearing the air: asthma and indoor air exposures. Washington, DC: National Academy Press; 2000. [PubMed] [Google Scholar]
- Kane JB. Marriage Advantages in Perinatal Health: Evidence of Marriage Selection or Marriage Protection? Journal of Marriage and Family. 2016;78(1):212–229. doi: 10.1111/jomf.12257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kane JB, Lam CB. A Promising Approach to Future Biosocial Research on the Family: Considering the Role of Temporal Context. In: Booth A, McHale SM, Landale NS, editors. Biosocial Foundations of Family Processes. New York, NY: Springer New York; 2011. pp. 247–264. [Google Scholar]
- Kaushal N, Magnuson K, Waldfogel J. How is family income related to investments in children’s learning? In: Duncan GJ, Murnane RJ, editors. Whither Opportunity?: Rising Inequality, Schools, and Children’s Life Chances. New York: Russell Sage; 2011. pp. 187–206. [Google Scholar]
- Kessler RC, Duncan GJ, Gennetian LA, Katz LF, Kling JR, Sampson NA, … Ludwig J. Associations of Housing Mobility Interventions for Children in High-Poverty Neighborhoods With Subsequent Mental Disorders During Adolescence. Jama-Journal of the American Medical Association. 2014;311:937–947. doi: 10.1001/jama.2014.607. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Kohn ML, Schooler C. Work and personality: an inquiry into the impact of social stratification. Ablex Pub; 1983. [Google Scholar]
- Komro Ka, Burris S, Wagenaar AC. Social Determinants of Child Health: Concepts and Measures for Future Research. Health Behavior and Policy Review. 2014;1:432–445. doi: 10.14485/HBPR.1.6.1. [DOI] [Google Scholar]
- Kramer MR, Hogue CR. Is segregation bad for your health? Epidemiologic reviews. 2009;31:178–194. doi: 10.1093/epirev/mxp001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger J, Higgins DL. Housing and health: time again for public health action. American Journal of Public Health. 2002;92(5):758–768. doi: 10.2105/ajph.92.5.758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger N. Epidemiology and the people’s health: Theory and context. New York: Oxford University Press; 2011. [Google Scholar]
- Krieger N, Williams DR, Moss NE. Measuring social class in US public health research: Concepts, methodologies, and guidelines. Annual Review of Public Health. 1997;18:341–378. doi: 10.1146/annurev.publhealth.18.1.341. [DOI] [PubMed] [Google Scholar]
- Lane SP, Bluestone C, Burke CT. Trajectories of BMI from early childhood through early adolescence: SES and psychosocial predictors. Br J Health Psychol. 2013;18(1):66–82. doi: 10.1111/j.2044-8287.2012.02078.x. [DOI] [PubMed] [Google Scholar]
- Lareau A. Invisible inequality: Social class and childbearing in black families and white families. American Sociological Review. 2002;67(5):747–776. [Google Scholar]
- Lavarreda SA, Snyder S, Brown ER. The effects of the Great Recession on health insurance: changes in the uninsured population from 2007 to 2009. Policy Brief UCLA Cent Health Policy Res. 2013;(PB2013-5):1–8. [PubMed] [Google Scholar]
- Lehman BJ, Taylor SE, Kiefe CI, Seeman TE. Relation of childhood socioeconomic status and family environment to adult metabolic functioning in the CARDIA study. Psychosom Med. 2005;67(6):846–854. doi: 10.1097/01.psy.0000188443.48405.eb. [DOI] [PubMed] [Google Scholar]
- Leininger LJ, Ryan RM, Kalil A. Low-income mothers’ social support and children’s injuries. Social Science & Medicine. 2009;68(12):2113–2121. doi: 10.1016/j.socscimed.2009.03.013. [DOI] [PubMed] [Google Scholar]
- Leventhal T, Brooks-Gunn J. A randomized study of neighborhood effects on low-income children’s educational outcomes. Dev Psychol. 2004;40(4):488–507. doi: 10.1037/0012-1649.40.4.488. [DOI] [PubMed] [Google Scholar]
- Leventhal T, Newman S. Housing and child development. Children and Youth Services Review. 2010;32(9):1165–1174. [Google Scholar]
- Link BG, Phelan J. Social conditions as fundamental causes of disease. J Health Soc Behav. 1995;(Spec No):80–94. [PubMed] [Google Scholar]
- Lipperman-Kreda S, Grube JW, Paschall MJ. Community norms, enforcement of minimum legal drinking age laws, personal beliefs and underage drinking: an explanatory model. J Community Health. 2010;35(3):249–257. doi: 10.1007/s10900-010-9229-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovato CY, Zeisser C, Campbell HS, Watts AW, Halpin P, Thompson M, … Brown KS. Adolescent smoking: effect of school and community characteristics. Am J Prev Med. 2010;39(6):507–514. doi: 10.1016/j.amepre.2010.08.019. [DOI] [PubMed] [Google Scholar]
- Lynch JL, von Hippel PT. An education gradient in health, a health gradient in education, or a confounded gradient in both? Soc Sci Med. 2016;154:18–27. doi: 10.1016/j.socscimed.2016.02.029. [DOI] [PubMed] [Google Scholar]
- Lynch JW, Kaplan GA. Socioeconomic Factors. In: Berkman LF, Kawachi I, editors. Social Epidemiology. New York: Oxford University Press; 2000. pp. 13–35. [Google Scholar]
- Machado-Rodrigues AM, Santana A, Gama A, Mourão I, Nogueira H, Rosado V, Padez C. Parental perceptions of neighborhood environments, BMI, and active behaviors in girls aged 7–9 years. American Journal of Human Biology. 2014;26(5):670–675. doi: 10.1002/ajhb.22577. [DOI] [PubMed] [Google Scholar]
- Macintyre S, Ellaway A, Cummins S. Place effects on health: how can we conceptualise, operationalise and measure them? Social Science & Medicine. 2002;55(1):125–139. doi: 10.1016/s0277-9536(01)00214-3. [DOI] [PubMed] [Google Scholar]
- Margerison-Zilko C, Cubbin C, Jun J, Marchi K, Fingar K, Braveman P. Beyond the cross-sectional: neighborhood poverty histories and preterm birth. Am J Public Health. 2015;105(6):1174–1180. doi: 10.2105/ajph.2014.302441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masi CM, Hawkley LC, Piotrowski ZH, Pickett KE. Neighborhood economic disadvantage, violent crime, group density, and pregnancy outcomes in a diverse, urban population. Soc Sci Med. 2007;65(12):2440–2457. doi: 10.1016/j.socscimed.2007.07.014. S0277-9536(07)00407-8 [pii] [DOI] [PubMed] [Google Scholar]
- Mauldon J. The effect of marital disruption on children’s health. Demography. 1990;27(3):431–446. [PubMed] [Google Scholar]
- McCallion W, Murray L, Bailie A, Dalzell A, O’Reilly D, Bamford K. Helicobacter pylori infection in children: relation with current household living conditions. Gut. 1996;39(1):18–21. doi: 10.1136/gut.39.1.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McClure R, Kegler S, Davey T, Clay F. Contextual Determinants of Childhood Injury: A Systematic Review of Studies With Multilevel Analytic Methods. Am J Public Health. 2015;105(12):e37–43. doi: 10.2105/AJPH.2015.302883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGrath JJ, Matthews KA, Brady SS. Individual versus neighborhood socioeconomic status and race as predictors of adolescent ambulatory blood pressure and heart rate. Soc Sci Med. 2006;63(6):1442–1453. doi: 10.1016/j.socscimed.2006.03.019. [DOI] [PubMed] [Google Scholar]
- McHale SM, Updegraff KA, Whiteman SD. Sibling relationships and influences in childhood and adolescence. Journal of Marriage and Family. 2012;74(5):913–930. doi: 10.1111/j.1741-3737.2012.01011.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messer LC, Vinikoor LC, Laraia BA, Kaufman JS, Eyster J, Holzman C, … O’Campo P. Socioeconomic domains and associations with preterm birth. Soc Sci Med. 2008;67(8):1247–1257. doi: 10.1016/j.socscimed.2008.06.009. [DOI] [PubMed] [Google Scholar]
- Miller CC. The New York Times. 2015. Dec 17, Class Differences in Child-Rearing Are on the Rise. [Google Scholar]
- Millman M. Committee on Monitoring Access to Personal Health Care Services. Washington, DC: National Academy Press; 1993. [Google Scholar]
- Miranda ML, Kim D, Reiter J, Galeano MAO, Maxson P. Environmental contributors to the achievement gap. NeuroToxicology. 2009;30:1019–1024. doi: 10.1016/j.neuro.2009.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montez JK, Friedman EM. Educational attainment and adult health: under what conditions is the association causal? Soc Sci Med. 2015;127:1–7. doi: 10.1016/j.socscimed.2014.12.029. [DOI] [PubMed] [Google Scholar]
- Montgomery LE, Kiely JL, Pappas G. The effects of poverty, race, and family structure on US children’s health: data from the NHIS, 1978 through 1980 and 1989 through 1991. American Journal of Public Health. 1996;86(10):1401–1405. doi: 10.2105/ajph.86.10.1401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morenoff JD. Neighborhood mechanisms and the spatial dynamics of birth weight. AJS. 2003;108(5):976–1017. doi: 10.1086/374405. [DOI] [PubMed] [Google Scholar]
- National School Lunch Program. National School Lunch Program. 2012 Retrieved from http://www.fns.usda.gov/sites/default/files/NSLPFactSheet.pdf.
- Navarro V, Muntaner C. Political and economic determinants of populatin health and well-being: Controversies and developments. Amityville, NY: Baywood Pub Co; 2004. [Google Scholar]
- Ncube CN, Enquobahrie DA, Albert SM, Herrick AL, Burke JG. Association of neighborhood context with offspring risk of preterm birth and low birthweight: A systematic review and meta-analysis of population-based studies. Soc Sci Med. 2016;153:156–164. doi: 10.1016/j.socscimed.2016.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nores M, Belfield CR, Barnett WS, Schweinhart L. Updating the Economic Impacts of the High/Scope Perry Preschool Program. Educational Evaluation and Policy Analysis. 2005;27:245–261. doi: 10.3102/01623737027003245. [DOI] [Google Scholar]
- O’Campo P, Burke JG, Culhane J, Elo IT, Eyster J, Holzman C, … Laraia BA. Neighborhood deprivation and preterm birth among non-Hispanic Black and White women in eight geographic areas in the United States. Am J Epidemiol. 2008;167(2):155–163. doi: 10.1093/aje/kwm277. [DOI] [PubMed] [Google Scholar]
- Oakes JM. The (mis)estimation of neighborhood effects: causal inference for a practicable social epidemiology. Soc Sci Med. 2004;58(10):1929–1952. doi: 10.1016/j.socscimed.2003.08.004. S0277953603004131 [pii] [DOI] [PubMed] [Google Scholar]
- Olson LM, Tang S-fS, Newacheck PW. Children in the United States with discontinuous health insurance coverage. New England Journal of Medicine. 2005;353(4):382–391. doi: 10.1056/NEJMsa043878. [DOI] [PubMed] [Google Scholar]
- Osypuk TL, Acevedo-Garcia D. Beyond individual neighborhoods: A geography of opportunity perspective for understanding racial/ethnic health disparities. Health Place. 2010 doi: 10.1016/j.healthplace.2010.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson CJ. Children of lesbian and gay parents. Current directions in psychological science. 2006;15(5):241–244. [Google Scholar]
- Penchansky R, Thomas JW. The concept of access: definition and relationship to consumer satisfaction. Med Care. 1981;19(2):127–140. doi: 10.1097/00005650-198102000-00001. [DOI] [PubMed] [Google Scholar]
- Phelan JC, Link BG, Tehranifar P. Social conditions as fundamental causes of health inequalities: theory, evidence, and policy implications. J Health Soc Behav. 2010;(51 Suppl):S28–40. doi: 10.1177/0022146510383498. [DOI] [PubMed] [Google Scholar]
- Phillips M. Parenting, time use, and disparities in academic outcomes. In: Duncan GJ, Murnane RJ, editors. Whither Opportunity?: Rising Inequality, Schools, and Children’s Life Chances. New York: Russell Sage; 2011. [Google Scholar]
- Quinn K, Kaufman JS, Siddiqi A, Yeatts KB. Stress and the city: housing stressors are associated with respiratory health among low socioeconomic status Chicago children. Journal of Urban Health. 2010;87(4):688–702. doi: 10.1007/s11524-010-9465-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raissian KM. Does unemployment affect child abuse rates? Evidence from New York State. Child Abuse Negl. 2015;48:1–12. doi: 10.1016/j.chiabu.2015.06.008. [DOI] [PubMed] [Google Scholar]
- Rajakumar K, Thomas SB, Musa D, Almario D, Garza MA. Racial differences in parents’ distrust of medicine and research. Arch Pediatr Adolesc Med. 2009;163(2):108–114. doi: 10.1001/archpediatrics.2008.521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raymond J, Wheeler W, Brown MJ. Lead Screening and Prevalence of Blood Lead Levels in Children Aged 1–2 Years — Child Blood Lead Surveillance System, United States, 2002–2010 and National Health and Nutrition Examination Survey, United States, 1999–2010. Morbidity and Mortality Weekly Report. 2014;63(2):36–42. [PubMed] [Google Scholar]
- Reardon SF. The widening academic achievement gap between rich and poor: New evidence and possible explanations. In: Duncan GJ, Murnane RJ, editors. Whither Opportunity?: Rising Inequality, Schools, and Children’s Life Chances. New York: Russell Sage; 2011. [Google Scholar]
- Reardon SF, Bischoff K. Income inequality and income segregation. AJS; American journal of sociology. 2011;116(4):489–514. doi: 10.1086/657114. [DOI] [PubMed] [Google Scholar]
- Rhee K. Childhood overweight and the relationship between parent behaviors, parenting style, and family functioning. The ANNALS of the American Academy of Political and Social Science. 2008;615(1):11–37. [Google Scholar]
- Richards JL, Chapple-McGruder T, Williams BL, Kramer MR. Does neighborhood deprivation modify the effect of preterm birth on children’s first grade academic performance? Soc Sci Med. 2015;132:122–131. doi: 10.1016/j.socscimed.2015.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saw A, Berenbaum H, Okazaki S. Influences of personal standards and perceived parental expectations on worry for Asian American and White American college students. Anxiety Stress Coping. 2013;26(2):187–202. doi: 10.1080/10615806.2012.668536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheffler RM, Brown TT. Social capital, economics, and health: new evidence. Health Economics Policy and Law. 2008;3:321–331. doi: 10.1017/S1744133108004593. [DOI] [PubMed] [Google Scholar]
- Schempf AH, Kaufman JS. Accounting for context in studies of health inequalities: a review and comparison of analytic approaches. Ann Epidemiol. 2012;22(10):683–690. doi: 10.1016/j.annepidem.2012.06.105. [DOI] [PubMed] [Google Scholar]
- Sharifi M, Sequist TD, Rifas-Shiman SL, Melly SJ, Duncan DT, Horan CM, … Taveras EM. The role of neighborhood characteristics and the built environment in understanding racial/ethnic disparities in childhood obesity. Prev Med. 2016;91:103–109. doi: 10.1016/j.ypmed.2016.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen FC, Liao KY, Abraham WT, Weng CY. Parental pressure and support toward Asian Americans’ self-efficacy, outcome expectations, and interests in stereotypical occupations: Living up to parental expectations and internalized stereotyping as mediators. J Couns Psychol. 2014;61(2):241–252. doi: 10.1037/a0036219. [DOI] [PubMed] [Google Scholar]
- Simpson L, Owens PL, Zodet MW, Chevarley FM, Dougherty D, Elixhauser A, McCormick MC. Health care for children and youth in the United States: annual report on patterns of coverage, utilization, quality, and expenditures by income. Ambulatory Pediatrics. 2005;5(1):6–e20. doi: 10.1367/A04-119R.1. [DOI] [PubMed] [Google Scholar]
- Singh GK, Kogan MD. Widening socioeconomic disparities in US childhood mortality, 1969 2000. Am J Public Health. 2007;97(9):1658–1665. doi: 10.2105/AJPH.2006.087320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skiba RJ, RSM, Nardo AC, Peterson RL. The color of discipline: Sources of racial and gender disproportionality in school punishment. Urban Review. 2002;34(4):317–342. [Google Scholar]
- Snyder TD, Dillow SA. Digest of Education Statistics, 2013. 2015 Retrieved from http://nces.ed.gov/pubsearch/pubsinfo.asp?pubid=2015011.
- Spelke B, Zertuche AD, Rochat R. Obstetric Provider Maldistribution: Georgia, USA, 2011. Matern Child Health J. 2016;20(7):1333–1340. doi: 10.1007/s10995-016-1999-8. [DOI] [PubMed] [Google Scholar]
- Stacey J, Biblarz TJ. (How) does the sexual orientation of parents matter? American Sociological Review. 2001:159–183. [Google Scholar]
- Strickland BB, Jones JR, Ghandour RM, Kogan MD, Newacheck PW. The medical home: health care access and impact for children and youth in the United States. Pediatrics. 2011;127(4):604–611. doi: 10.1542/peds.2009-3555. [DOI] [PubMed] [Google Scholar]
- Taylor SE, Repetti RL, Seeman T. Health psychology: what is an unhealthy environment and how does it get under the skin? Annu Rev Psychol. 1997;48:411–447. doi: 10.1146/annurev.psych.48.1.411. [DOI] [PubMed] [Google Scholar]
- The Urban Institute. Tabulations of the Urban Institute Health Policy Center’s ACS Medicaid/CHIP Eligibility Simulation Model. 2015 Retrieved from http://www.insurekidsnow.gov/professionals/reports/index.html.
- Thiede BC, Monnat SM. The Great Recession and America’s geography of unemployment. Demographic Research. 2016;35:891–927. doi: 10.4054/DemRes.2016.35.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tucker JS, Pollard MS, de la Haye K, Kennedy DP, Green HD., Jr Neighborhood characteristics and the initiation of marijuana use and binge drinking. Drug Alcohol Depend. 2013;128(1–2):83–89. doi: 10.1016/j.drugalcdep.2012.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turney K. Maternal depression and childhood health inequalities. Journal of Health and Social Behavior. 2011;52(3):314–332. doi: 10.1177/0022146511408096. [DOI] [PubMed] [Google Scholar]
- Turney K. Perceived instrumental support and children’s health across the early life course. Social Science & Medicine. 2013;95:34–42. doi: 10.1016/j.socscimed.2012.08.017. [DOI] [PubMed] [Google Scholar]
- Vos AA, Posthumus AG, Bonsel GJ, Steegers EA, Denktas S. Deprived neighborhoods and adverse perinatal outcome: a systematic review and meta-analysis. Acta Obstet Gynecol Scand. 2014;93(8):727–740. doi: 10.1111/aogs.12430. [DOI] [PubMed] [Google Scholar]
- Wald J, Losen DJ. Defining and redirecting a school-to-prison pipeline. New Dir Youth Dev. 2003;(99):9–15. doi: 10.1002/yd.51. [DOI] [PubMed] [Google Scholar]
- Wang F, Luo W. Assessing spatial and nonspatial factors for healthcare access: towards an integrated approach to defining health professional shortage areas. Health Place. 2005;11(2):131–146. doi: 10.1016/j.healthplace.2004.02.003. [DOI] [PubMed] [Google Scholar]
- Weber M. Economy and society: An outline of interpretive sociology. Univ of California Press; 1978. [Google Scholar]
- Weinreb L, Wehler C, Perloff J, Scott R, Hosmer D, Sagor L, Gundersen C. Hunger: its impact on children’s health and mental health. Pediatrics. 2002;110(4):e41. doi: 10.1542/peds.110.4.e41. [DOI] [PubMed] [Google Scholar]
- Wilkinson RG, Pickett KE. The problems of relative deprivation: why some societies do better than others. Soc Sci Med. 2007;65(9):1965–1978. doi: 10.1016/j.socscimed.2007.05.041. [DOI] [PubMed] [Google Scholar]
- Wood DL, Valdez RB, Hayashi T, Shen A. Health of homeless children and housed, poor children. Pediatrics. 1990;86(6):858–866. [PubMed] [Google Scholar]
- Wright EO, editor. Approaches to Class Analysis. New York: Cambridge University Press; 2007. [Google Scholar]
- Ye J, Leep C, Newman S. Reductions of budgets, staffing, and programs among local health departments: results from NACCHO’s economic surveillance surveys, 2009–2013. J Public Health Manag Pract. 2015;21(2):126–133. doi: 10.1097/PHH.0000000000000074. [DOI] [PubMed] [Google Scholar]