ABSTRACT
The ligamentum teres (LT) has traditionally been described as a redundant structure with no contribution to hip biomechanics or function. There has been renewed interest in the LT as a source of hip pathology due to the high prevalence of LT pathology observed at the time of hip arthroscopy. The LT acts a secondary stabilizer to supplement the work of the capsular ligaments and works in a sling-like manner to prevent subluxation of the hip at the extremes of motion. The presence of free nerve endings within the LT indicates a definite role in pain generation, with the LT undergoing various mechanical and histological adaptations to hip pathology.
INTRODUCTION
The ligamentum teres (LT) and its role in hip function has been of constant debate since Professor W.S. Savory first presented a paper to the Cambridge Philosophical Society in April 1874 on its function [1]. It has been established that the LT assumes an important role in the neonatal hip as a stabilizing structure and a conduit for the blood supply of the femoral head [2, 3]. However, traditional orthopedic teaching has been to regard the LT as a redundant or vestigial structure in the adult hip [4]. With the advent of hip arthroscopy in the last few decades there has been renewed interest in the role the LT plays in hip stability and as a generator of hip pain [5].
The recognition of LT pathology (including synovitis, partial and complete tears) at the time of hip arthroscopy is increasingly common with a reported prevalence up to 51% [5–7]. Lesions involving the LT have been said to be the third most common cause of hip pain in athletes undergoing diagnostic arthroscopic procedures [8].
Since the last published reviews of the LT [9, 10], there has been a number of new publications regarding the LT. Our aim has been to gather together this new information in an update review. The purpose of this review is to define the functional role the LT plays in the adult hip with supportive evidence from the literature. Specific focus was given to its role as a hip stabilizer and a pain generator, in addition to other proposed roles such as proprioception, and synovial fluid distribution. In doing so, the authors present an analysis of the anatomy, the histological structure, and the biomechanical function of the LT, and the various changes the LT undergoes in hip pathology.
Hip stabilization
Our current understanding is that the LT acts as a secondary stabilizer of the hip, supplementing the role of the capsular ligaments, and works in a sling-like manner to prevent subluxation of the femoral head at the extremes of motion. To better understand the role of the LT in hip motion, a number of cadaveric studies [11–14] have been performed in the last decade, including the ‘string model’ studies of Martin et al. [12, 13, 15]. This has been aided by a better understanding of anatomy and histology.
In open hip preservation surgery, the LT is routinely transected to facilitate delivery of the femoral head. It has been shown that resection of the LT leads to long-term mild symptoms of instability (giving way of the hip) in almost a quarter of patients, despite other pathologies (cam lesions, pincer lesions, labral tears etc.) being addressed at the time of surgery [16]. This suggests that the LT has a definite role in stabilization of the hip, a role which may be amplified when there is abnormal bone morphology, as occurs in femoroacetabular impingement (FAI) or hip dysplasia, or when the other stabilizing structures, such as the capsule, are deficient, as occurs in capsular laxity or joint hypermobility.
Structural anatomy
Wenger et al. [17] have previously likened the LT to the anterior cruciate ligament (ACL) of the knee. They proposed that the structural anatomy (double bundle) and ultimate load to failure were similar to the ACL and, as such, the LT may play a role in the hip similar to that of the ACL in the knee.
Although it remains unclear whether the LT assumes the same important role in stability of the hip, there are striking anatomical similarities between the two. The LT is a pyramidal structure (Fig. 1) with a mean length of 30–35 mm [11], similar to the ACL. The ligament has a broad origin from almost the entire transverse acetabular ligament and is attached to the ischial and pubic bases by two bands or bundles [18, 19], with the posterior bundle stronger than the anterior bundle. Again, this is similar to the ACL [20]. On the ischial side, the origin of the LT is described as being stronger and marginally broader, extending past the osseous cavity of the acetabulum and onto the periosteum of the ischium and the capsule [21]. Both the LT and the ACL are surrounded by synovium [22], which is commonly found to be inflamed at the time of arthroscopy [23].
Fig. 1.
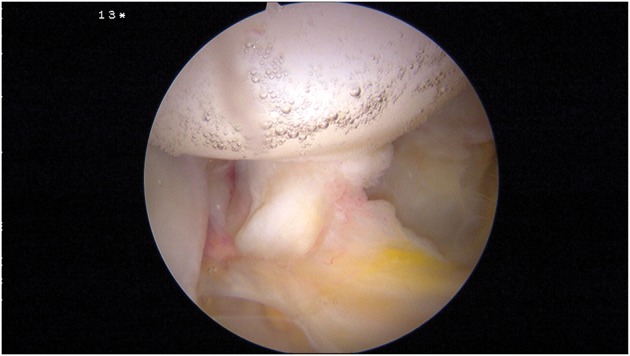
Intra-operative image of the normal LT showing the double bundle anatomy.
An important anatomic difference between the two ligaments is the base from which they originate. While the ACL arises distinctly from the tibial plateau [20], the LT has an attachment on the adjacent postero-inferior aspect of the acetabular cotyloid fossa which contains fibro-fatty tissue (pulvinar) and small vessels encased in synovium [24]. This ‘pulvinar’ is sometimes found to be hyperemic in the setting of LT synovitis [25], suggesting the synovium of the pulvinar and LT are confluent, and both may be impinged during abnormal rotation of the femoral head. More recently, the LT has been shown to have multiple attachment sites (up to six) from the base of the cotyloid fossa [26]. These anatomic findings alone would suggest the LT plays an integral role in the coaptation of the acetabulum and femoral head in a dynamic manner.
Mechanical properties
A key question regarding the importance of the LT, and its possible similarity to the ACL, relates to its strength and conflicting evidence exists in the literature on this matter. In 2007, Wegner et al. published a frequently cited study in which they determined the ultimate load to failure of the LT was similar to that of the human ACL. The authors, in fact, used a porcine model loading the porcine LTs in custom fixation rings and found that the mean ultimate load to failure of the LT was 882 N, which is similar to a human ACL [17]. More recently, Philippon et al. [27] studied the human LT, using a custom ball and socket fixture and dynamic tensile testing machine, and found a mean ultimate failure load of 204 N, with a mean native length of 32 mm and cross-sectional area of 59 mm2, with mean length of 38 mm at its yield point and 53 mm at its failure point [27]. Furthermore, the LT has a linear stiffness of 16 N/mm and elastic modulus of 9.24 MPa, which is significantly less than a human ACL refuting earlier suggestions of the LT assuming a role similar to the ACL in the knee. However, a limitation here is that cadaveric specimens with a mean age of 54 years were used, which may not reflect the true ultimate load to failure in young adults. In fact, the ultimate load to failure of the cadaveric LTs is more similar to human medial patellofemoral ligament (MPFL) of the knee [28] and the anterolateral ligament of the knee [29], rather than the ACL.
HISTOLOGY
Histologically, the LT is composed of parallel undulating collagen fiber bundles of type I, III, IV and V collagen, along with fibrous and adipose tissue interspersed with blood vessels and nerves [30]. This connective tissue (CT) matrix is surrounded by a layer of investing synovium composed of a single layer of cuboidal cells. This histological structure is similar to the ACL [31], which has a majority composition of type I collagen fibers arranged in parallel undulating bundles. However, it bears similarity to the MPFL in histology also [32], with loose collagen structures interspersed in a dense collagen framework.
Thus, while the LT shares many histological and anatomical similarities to the ACL, its mechanical properties are more similar to the MPFL.
Biomechanical studies of the LT in isolation
In studies where only the LT, femoral head and acetabulum are preserved [11–13], and the hip is stressed until the end point of the LT is reached, it has been found that the range of motion values required to reach such an end-point in simple uni-planar motion are well outside the normal physiological range of motion of the hip—bone to bone contact occurs well before the end point of the LT is reached in uni-planar motion. This suggests the LT is not a primary restraint but rather a secondary checkrein. Its main role appears to be in multi-planar motion, or more natural physiologic motion of the hip, where its end point is reached much earlier, especially in flexion and abduction (similar to a squat position) [13].
The LT moves with the femoral head, much like a sling, and wraps around it in such a way to prevent inferior subluxation with abduction, posterior subluxation with IR and anterior subluxation with ER [12]. The LT becomes taut with ER and lax with IR in flexion [33]. The LT has main effect on limiting rotations in the mid-high flexion position [15]. It is perhaps in these positions (such as standing to sitting, getting into and out of car etc.) where the LT is stressed the most. All the aforementioned studies assume a normal non-dysplastic hip. In the setting of hip dysplasia or capsular laxity, the role of the LT becomes more pronounced in stabilizing the hip [34].
Biomechanical studies of the LT and capsular ligaments
When the femoral head, acetabulum, LT and the capsular ligaments (iliofemoral, pubofemoral and ischiofemoral) are preserved in a cadaveric model the contributions of the LT to hip stability change. van Arkel et al. found that the capsular ligaments provide the primary restraint to IR and ER throughout the complete range of motion of the hip. They found that the LT has a more defined role a secondary restraint in ER during high flexion (>60°) with neutral/full adduction [14], with a minimal contribution in IR and ER FLEX AB. Further they found that the main restraint to the high flex ER position is the lateral iliofemoral ligament, advocating for capsular suturing at the time of LT debridement/repair.
If the LT assumes a secondary stabilizing role in the presence of intact capsular ligaments, it may be of more importance when these ligaments are released or lax. This suggestion is supported by the work of O’Donnell et al., who found that routine anterior capsular tightening, using either RF or suture plication, leads to significant improvement in results for patients having partial LT tear debridements [35]. This method has resulted in a lesser re-tear rate than their earlier method of LT debridement alone [36].
The above findings also appear to be consistent with that same group’s previously devised LT test [37]—pain at the extremes of ER/IR in a position of mid flexion and slight abduction. We believe this test reproduces the end-point of the LT at the extreme of the assessed multi-planar motion, with an inflamed, and/or torn LT inciting a pain response within the hip.
Dysplasia of the hip
As the LT has been proposed to be a secondary stabilizer, its role in hip dysplasia is of particular interest, both in developmental dysplasia of the hip (DDH) and FAI. It is perhaps the loss of osseous stability, which increases the importance of the LT as a stabilizer and hence leads to synovitis and/or tears of the LT.
In the setting of DDH it has been shown that the LT undergoes various adaptations including: disruption of the collagen framework; elastic fibers become thicker and more numerous; cells are irregularly distributed and are in different stages of functional activity [38]. Further fibro-cartilaginous metaplasia is seen within the LT which may be secondary to the increased mechanical stress. Interestingly, there appears to be a change in the collagen compositions of the LT in DDH, with an increase in both type III collagen [39] and the ratio of type III to type I collagen [40]. These changes suggest that the LT adapts to increased mechanical stress in DDH by becoming thicker and more elastic. This may lead to an increased propensity to tear. Interestingly, patients with CT disorders (such as Marfans and Ehlers-Danlos syndrome) often have mutations to the genes encoding type III collagen [41], it may be that the upregulation of this particular type of collagen, as is also the case with DDH patients [39, 40], is partly responsible for changes to the LT in such patients, in addition to the capsular laxity.
FEMOROACETABULAR IMPINGEMENT
In the setting of FAI, tear prevalence of up to 51% has been reported at the time of hip arthroscopy [5–7]. In athletes with FAI these numbers are higher with a 70% tear rate (60% partial and 10% complete) which is postulated occur as a result of increased stress on the LT [42]. The precise reason for the increased prevalence of LT tears in this cohort of patients has yet to be fully elucidated. As in the setting of DDH, studies have demonstrated that LT tears are associated with abnormal bone morphology and increased age, with LT tears being more common in patients with a low lateral coverage index (center edge angle—acetabular inclination) [43] and with a lower center edge angle alone [44]. This may be due to the levering effect of the femoral head on the acetabulum causing increased strain in the LT with ultimate failure.
The presence of LT pathology in the setting of FAI often heralds more significant chondral damage to both the femoral and acetabular articular surfaces. There is a 3.1 times higher incidence of chondral damage, particularly to the middle-inferior part of the acetabular fossa and the apex of the femoral head, with the presence of LT tears [44, 45]. Unfortunately, the exact etiology of this association and whether it is more prevalent in cam or pincer impingement has not been borne out in these studies. The question still remains, which comes first the LT tear or the chondral damage?
It is possible that the altered biomechanics created in the setting of FAI subjects the LT to increased damage. It is known that patients with cam impingement typically have reduced internal rotation [46] which may result in tightening of the LT. Many of these patients compensate by externally rotating their hips during hip flexion to account for the cam deformity. It is possible that this maneuver when performed rapidly, as occurs in sporting activity, may predispose a tight and less compliant LT to excess forces resulting in tearing over time. Further, a deficient LT renders the hip less stable particularly during the extremes of motion, as outlined above, which may increase the shear forces on the articular surfaces of both the femoral head and the acetabulum, resulting in accelerated chondral damage.
Benign joint hypermobility
Of particular interest recently has been the pathological changes to the LT in states of capsular laxity and generalized hypermobility. When the capsular ligaments are lax, as occurs in generalized hypermobility, the hip has an increased range of motion, which increases the excursion and endpoints of the LT and possibly leads to its stretching and eventual tearing.
Patients with generalized hypermobility (as defined by a Beighton test score of 4 or more) have a reduced capsular thickness (capsular laxity) and a high prevalence of partial tears of the LT [47]. Further, a thin hip capsule alone is associated with a higher incidence of LT pathology [48].
Athletes are more hypermobile than the general population, with a high incidence of capsular laxity seen in some sports in particular such as golf, running, gymnastics [49]. It is perhaps in this group of athletes where LT damage assumes more significance as a contributor to microinstability [50]. The incidence of chondral damage is high across all sports including golf, dancing, soccer and tennis [49]. It is proposed that the pattern of chondral damage [51] well described in the setting of athletes with capsular laxity [49], may be a result of increased laxity of the capsule and subsequent damage to the LT, which in turn leads to microinstability of the hip and chondral damage. The high prevalence of FAI in athletes [52, 53] compounds this situation by putting the LT at a levering disadvantage. In patients with LT tears who have generalized hypermobility, reconstruction of the LT has improved patient related outcome measures [54, 55].
Role in pain generation
Degenerative arthritis of the hip is a painful condition. It is proposed that free nerve endings found in the LT [30, 56] mediate a component of the pain response in degenerative arthritis. Further, it is well established that tears or synovitis of the LT alone, without the presence of any other hip pathology, are capable of causing hip pain [8, 10]. Debridement and/or reconstruction of the ligament alone has been shown to be effective in alleviating pain in the majority of patients [23, 54, 55, 57, 58]. This suggests that the LT is in itself a pain generator, mediated by the free nerve endings within the ligament. Radiofrequency ablation and or debridement possibly denudes these free nerve endings, eliminating the source of the painful hip, however, this has not been proven histologically yet.
Histology of free nerve endings
The presence or absence of nerve fibers within the LT has been controversial however more recent studies [30, 59, 60] have definitively shown that most, if not all, LT have nerve fibers, with a mean diameter of 56.5 μm [30], consistent with pain mediating unmyelinated fibers. These free nerve endings are concentrated in the center of the ligament [56] and appear to be of type Iva (nociceptive) variety [56, 60], proving a definite role for the LT as source of pain within the hip. Although concentrated in the center of the ligament, they are sparsely dispersed in the rest of the ligament proper. Thus, any tears or synovitis of the LT, mediate pain by exciting these free nerve endings.
Degenerative arthritis of the hip
In degenerative arthritis of the hip, it has been postulated that the LT assumes a role more consistent with pain-generation [8, 58, 61]. In their study of eleven cadaveric hip joints with degeneration, Samptachalit et al. found that the LT shows a spectrum of degenerative changes similar to tendon pathology. The thinnest LT undergoes near complete disruption of the ligament, intermediate thickness LTs show fatty replacement with and without fibromatous degeneration, fibromatous degeneration with and without mucoid degeneration and eosinophilic change, whereas the thickest LT show mucoid and fibromatous degeneration with microscopic tears [62]. Dehao et al. [30] further found occasional foci of osteochondroid and chondroid changes within the CT component which were more prevalent with more severe degeneration of the hip.
It is possible that in the degenerative hip, in addition to well established foci of pain such as the chondral damage, the structural damage to the LT alone (Fig. 2) is capable of exciting free nerve endings in the ligament. This damage appears to be graded, with mild changes in less affected hips and more severe metaplastic changes to the LT in more affected hips. A causal relationship between the severity of hip arthritis and increasing damage to the LT is yet to be established by radio-histological studies.
Fig. 2.

Intra-operative image of a degenerate LT in the setting of early osteoarthritis of the hip.
Shinohara et al. [63] examined the histological changes in complete LT detachments from the femoral head and found that the transition zone of the femoral head attachment undergoes histological change including loss of type II collagen and aggrecan, and abundance of single-stranded DNA positive chondrocytes. The upregulation of single stranded cells suggests that single stranded DNA damage is amplified in the presence of detachment, indicating that detachment or tears are not a purely mechanical event but rather may result from underlying weakening of the transition zone.
This appears to be consistent with the weakening of the ligament seen in degenerative arthritis. A weakened ligament will conduct more stress and hence excite more pain fibers. Studying if the concentration of free nerve endings in the degenerating LT increase or decrease will help us better understand the contribution of the LT as a pain generator in the degenerating hip. To this effect, a recent study has found that in the setting of arthritis, there is a definite upregulation of free nerve endings in both the capsule and the LT [64].
Interestingly, recent work on the LT has found small arterioles within the ligament proper which provide a blood supply to the ligament. There are numerous small blood vessels within the CT matrix of the ligament with a mean diameter of 182 μm. Most of the smaller arteries are surrounded by a layer of encircling fat [30]. This may provide a cushioning effect to maintain patency of the vessels during hip motion and so preserve an unhindered blood supply to the LT.
It is possible that this unhindered cushioned blood supply is what allows the LT to degenerate in a spectrum-like manner and also allows nourishment of the LT’s free nerve endings despite the presence of bone to bone contact in severe degenerative arthritis.
Role in proprioception
The LT was previously thought to serve a proprioceptive role in the hip, however, the presence or absence of mechanoreceptors within the LT continues to be a subject of debate. There are four types of nerve endings based on Freeman and Wyke’s classification [65]: Type I (Ruffini) low-threshold and slow-adapting; Type II (Pacini) low-threshold and fast-adapting; Type III (Golgi) low-threshold and slow-adapting; and type IV (Free nerve endings) high-threshold nociceptors.
Some recent histological studies [66, 67] have shown that there is a lack of any of the Type I-III mechanoreceptors in either the LT or the hip joint capsule. However, Moraes et al. [64] found all four types of mechanoreceptors in the labrum, capsule and the LT, and an upregulation of these receptors in the setting of arthrosis.
It is possible that the suggested proprioceptive role of the LT is mediated by the presence of mechanoreceptors, however, the free nerve endings themselves may subserve a proprioceptive role in the painful hip.
Role in synovial fluid distribution
Under normal physiologic loads, the hip joint is lubricated by fluid film lubrication [68]. The LT, by virtue of its intraarticular position and its motion with femoral head rotation, has proposed to have a ‘windshield wiper’ effect to facilitate synovial fluid distribution [4]. It is possible that as the femoral head rotates, the LT acting in a sling-like manner, distributes synovial fluid across the femoral head surface, much the same way as a windshield wiper of the car. This may allow for more equal distribution of synovial fluid across the hip joint, however, this has not yet been proven. Although this theory has often been quoted, the original source of the theory is uncertain.
Synovitis is being increasingly recognized as central to degenerative arthritis of the hip [69, 70]. It is possible that in degenerative arthritis of the hip, due to the increased fluid secondary to synovitis and the thickening and metaplasia of the LT as previously discussed, the LT is both weaker and at a mechanical disadvantage to distribute the increased volume of synovial fluid within the early degenerate hip. This may affect the proper lubrication of the hip, and accelerate damage to the hip cartilage.
CONCLUSION
The LT is not a redundant structure in the adult hip. Its primary role appears to be as a secondary stabilizer to supplement the work of the capsular ligaments, particularly in mid-flexion, abduction/adduction and rotation. It may have a more defined role to prevent subluxation in a sling function around the femoral head. It acts as a source of pain within the hip joint, a role subserved by the free nerve endings in the ligament, and undergoes mechanical and histological transformations based on hip pathology. These same free nerve endings may serve a secondary proprioceptive role in the painful hip. Further, the LT may act to distribute synovial fluid within the hip joint.
FUNDING
No funding has been received to support this work.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1. Savory WS. The use of the ligamentum teres of the hip-joint. J Anat Physiol 1874; 8: 291–6. [PMC free article] [PubMed] [Google Scholar]
- 2. McKibbin B. Anatomical factors in the stability of the hip joint in the newborn. Bone Joint J 1970; 52: 148–59. [PubMed] [Google Scholar]
- 3. Chandler SB, Kreuscher PH.. A study of the blood supply of the ligamentum teres and its relation to the circulation of the head of the Femur. J Bone Joint Surg Am 1932; 14: 834–46. [Google Scholar]
- 4. Phillips A, Bartlett G, Norton M. et al. Ligamentum teres: vital or vestigial? Orthop Proc 2012; 94-B(Supp XLII): 1. [Google Scholar]
- 5. Botser IB, Martin DE, Stout CE. et al. Tears of the ligamentum teres: prevalence in hip arthroscopy using 2 classification systems. Am J Sports Med 2011; 39(Suppl): 117S–25S. [DOI] [PubMed] [Google Scholar]
- 6. Gray AJ, Villar RN.. The ligamentum teres of the hip: an arthroscopic classification of its pathology. Arthroscopy 1997; 13: 575–8. [DOI] [PubMed] [Google Scholar]
- 7. Devitt BM, Smith B, Stapf R. et al. The reliability of commonly used arthroscopic classifications of ligamentum teres pathology. J Hip Preserv Surg 2017; 4: 187–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Byrd JWT, Jones KS.. Traumatic rupture of the ligamentum teres as a source of hip pain. Arthroscopy 2004; 20: 385–91. [DOI] [PubMed] [Google Scholar]
- 9. Bardakos NV, Villar RN.. The ligamentum teres of the adult hip. J Bone Joint Surg Br 2009; 91: 8–15. [DOI] [PubMed] [Google Scholar]
- 10. O’Donnell JM, Pritchard M, Salas AP. et al. The ligamentum teres—its increasing importance. J Hip Preserv Surg 2014; 1: 3–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Demange MK, Kakuda CMS, Pereira CAM. et al. Influence of the femoral head ligament on hip mechanical function. Acta Ortopédica Bras 2007; 15: 187–90. [Google Scholar]
- 12. Martin RL, Kivlan BR, Clemente FR.. A cadaveric model for ligamentum teres function: a pilot study. Knee Surg Sports Traumatol Arthrosc 2013; 21: 1689–93. [DOI] [PubMed] [Google Scholar]
- 13. Kivlan BR, Richard Clemente F, Martin RL. et al. Function of the ligamentum teres during multi-planar movement of the hip joint. Knee Surg Sports Traumatol Arthrosc 2013; 21: 1664–8. [DOI] [PubMed] [Google Scholar]
- 14. van Arkel RJ, Amis AA, Cobb JP. et al. The capsular ligaments provide more hip rotational restraint than the acetabular labrum and the ligamentum teres: an experimental study. Bone Joint J 2015; 97-B: 484–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Martin HD, Hatem MA, Kivlan BR. et al. Function of the ligamentum teres in limiting hip rotation: a cadaveric study. Arthroscopy 2014; 30: 1085–91. [DOI] [PubMed] [Google Scholar]
- 16. Phillips AR, Bartlett G, Norton M. et al. Hip stability after ligamentum teres resection during surgical dislocation for cam impingement. Hip Int J Clin Exp Res Hip Pathol Ther 2012; 22: 329–34. [DOI] [PubMed] [Google Scholar]
- 17. Wenger D, Miyanji F, Mahar A. et al. The mechanical properties of the ligamentum teres: a pilot study to assess its potential for improving stability in children’s hip surgery. J Pediatr Orthop 2007; 27: 408–10. [DOI] [PubMed] [Google Scholar]
- 18. Perumal V, Woodley SJ, Nicholson HD.. Ligament of the head of femur: a comprehensive review of its anatomy, embryology, and potential function. Clin Anat N Y N 2016; 29: 247–55. [DOI] [PubMed] [Google Scholar]
- 19. Keene GS, Villar RN.. Arthroscopic anatomy of the hip: an in vivo study. Arthroscopy 1994; 10: 392–9. [DOI] [PubMed] [Google Scholar]
- 20. Giuliani JR, Kilcoyne KG, Rue J-PH.. Anterior cruciate ligament anatomy: a review of the anteromedial and posterolateral bundles. J Knee Surg 2009; 22: 148–54. [DOI] [PubMed] [Google Scholar]
- 21. Rao J, Zhou YX, Villar RN.. Injury to the ligamentum teres. Mechanism, findings, and results of treatment. Clin Sports Med 2001; 20: 791–799-vii. [DOI] [PubMed] [Google Scholar]
- 22. Gardner E, Gray DJ.. Prenatal development of the human hip joint. Am J Anat 1950; 87: 163–211. [DOI] [PubMed] [Google Scholar]
- 23. de SA D, Phillips M, Philippon MJ. et al. Ligamentum Teres injuries of the hip: a systematic review examining surgical indications, treatment options, and outcomes. Arthrosc J Arthrosc Relat Surg 2014; 30: 1634–41. [DOI] [PubMed] [Google Scholar]
- 24. Petersilge CA. Chronic adult hip pain: MR arthrography of the hip. RadioGraphics 2000; 20: S43–52. [DOI] [PubMed] [Google Scholar]
- 25. Porthos Salas A, O’Donnell JM.. Ligamentum teres injuries - an observational study of a proposed new arthroscopic classification. J Hip Preserv Surg 2015; 2: 258–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Mikula JD, Slette EL, Chahla J. et al. Quantitative anatomic analysis of the native ligamentum teres. Orthop J Sports Med 2017; 5: 2325967117691480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Philippon MJ, Rasmussen MT, Turnbull TL. et al. Structural properties of the native ligamentum teres. Orthop J Sports Med 2014; 2: 2325967114561962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kader DF, Rajeev A.. A review of functional anatomy and surgical reconstruction of medial patellofemoral ligament. J Arthrosc Joint Surg 2014; 1: 5–10. [Google Scholar]
- 29. Helito CP, Demange MK, Bonadio MB. et al. Anatomy and Histology of the Knee Anterolateral Ligament. Orthop J Sports Med [Internet] 2013; 1: 232596711351354 [cited 2017 Feb 23]. Available at: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4555517/. Accessed: 7 March 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Dehao BW, Bing TK, Young JLS.. Understanding the ligamentum teres of the hip: a histological study. Acta Ortop Bras 2015; 23: 29–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Strocchi R, de Pasquale V, Gubellini P. et al. The human anterior cruciate ligament: histological and ultrastructural observations. J Anat 1992; 180(Pt 3): 515–9. [PMC free article] [PubMed] [Google Scholar]
- 32. Veteto A, Marberry K, Kondrashov P.. The histological structure of the medial patellofemoral ligament: implications in knee stability and pain generation (914.9). FASEB J 2014; 28(1 Suppl): 914.9. [Google Scholar]
- 33. Cerezal L, Kassarjian A, Canga A. et al. Anatomy, biomechanics, imaging, and management of ligamentum teres injuries. RadioGraphics 2010; 30: 1637–51. [DOI] [PubMed] [Google Scholar]
- 34. Martin RRL, Martin HD. Function and clinical relevance of the ligamentum teres: a current concept. Current Orthopaedic Practice 2015; 26: 425–28. http://journals.lww.com/c-orthopaedicpractice/Fulltext/2015/07000/Function_and_clinical_relevance_of_the_ligamentum.19.aspx [Google Scholar]
- 35. Amenabar T, O’Donnell J.. Successful treatment of isolated, partial thickness ligamentum teres (LT) tears with debridement and capsulorrhaphy. Hip Int J Clin Exp Res Hip Pathol Ther 2013; 23: 576–82. [DOI] [PubMed] [Google Scholar]
- 36. Haviv B, O’Donnell J.. Arthroscopic debridement of the isolated ligamentum teres rupture. Knee Surg Sports Traumatol Arthrosc off J ESSKA 2011; 19: 1510–3. [DOI] [PubMed] [Google Scholar]
- 37. O’Donnell J, Economopoulos K, Singh P. et al. The ligamentum teres test: a novel and effective test in diagnosing tears of the ligamentum teres. Am J Sports Med 2014; 42: 138–43. [DOI] [PubMed] [Google Scholar]
- 38. Ipplito E, Ishii Y, Ponseti IV.. Histologic, histochemical, and ultrastructural studies of the hip joint capsule and ligamentum teres in congenital dislocation of the hip. Clin Orthop 1980; 146: 246–58. [PubMed] [Google Scholar]
- 39. Jensen BA, Reimann I, Fredensborg N.. Collagen type III predominance in newborns with congenital dislocation of the hip. Acta Orthop Scand 1986; 57: 362–5. [DOI] [PubMed] [Google Scholar]
- 40. Oda H, Igarashi M, Hayashi Y. et al. Soft tissue collagen in congenital dislocation of the hip. Biochemical studies of the ligamentum teres of the femur and the hip joint capsule. Nihon Seikeigeka Gakkai Zasshi 1984; 58: 331–8. [PubMed] [Google Scholar]
- 41. Castori M. Ehlers-danlos syndrome, hypermobility type: an underdiagnosed hereditary connective tissue disorder with mucocutaneous, articular, and systemic manifestations. ISRN Dermatol 2012; 2012: 751768.http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3512326/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Philippon M, Schenker M, Briggs K. et al. Femoroacetabular impingement in 45 professional athletes: associated pathologies and return to sport following arthroscopic decompression. Knee Surg Sports Traumatol Arthrosc 2007; 15: 908–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Domb BG, Martin DE, Botser IB.. Risk factors for ligamentum teres tears. Arthrosc J Arthrosc Relat Surg 2013; 29: 64–73. [DOI] [PubMed] [Google Scholar]
- 44. Chahla J, Soares EAM, Devitt BM. et al. Ligamentum teres tears and femoroacetabular impingement: prevalence and preoperative findings. Arthroscopy 2016; 32: 1293–7. [DOI] [PubMed] [Google Scholar]
- 45. Kaya M, Suziki T, Minowa T. et al. Ligamentum teres injury is associated with the articular damage pattern in patients with femoroacetabular impingement. Arthrosc J Arthrosc Relat Surg 2014; 30: 1582–7. [DOI] [PubMed] [Google Scholar]
- 46. Pun S, Kumar D, Lane NE.. Femoroacetabular impingement. Arthritis Rheumatol Hoboken NJ 2015; 67: 17–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Devitt B. A prospective study exploring the relationship between hip capsular thickness and joint hypermobility: forewarned is forearmed. J Hip Preserv Surg 2016; 3(Suppl 1): [cited 2017 Feb 3]. Available at: https://academic.oup.com/jhps/article/3/suppl_1/hnw030.070/2353007/A-Prospective-Study-Exploring-the-Relationship. Accessed: 7 March 2017. [Google Scholar]
- 48. Devitt BM, Smith B, Stapf R. et al. Generalized joint hypermobility is predictive of hip capsular thickness. Orthop J Sports Med 2017; 5: 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Philippon MJ, Schenker ML.. Athletic hip injuries and capsular laxity. Oper Tech Orthop 2005; 15: 261–6. [Google Scholar]
- 50. Kalisvaart MM, Safran MR.. Microinstability of the hip—it does exist: etiology, diagnosis and treatment. J Hip Preserv Surg 2015; 2: 123–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Beck M, Kalhor M, Leunig M. et al. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br 2005; 87: 1012–8. [DOI] [PubMed] [Google Scholar]
- 52. Newman JT, Saroki AJ, Briggs KK. et al. Return to elite level of play and performance in professional Golfers after arthroscopic hip surgery. Orthop J Sports Med [Internet] 2016; 4: 232596711664353 [cited 2017 Feb 24]. Available at: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4837663/. Accessed: 7 March 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Singh PJ, O'Donnell JM.. The outcome of hip arthroscopy in Australian football league players: a review of 27 hips. Arthroscopy 2010; 26: 743–9. [DOI] [PubMed] [Google Scholar]
- 54. Chandrasekaran S, Martin TJ, Close MR. et al. Arthroscopic reconstruction of the Ligamentum Teres: a case series in four patients with connective tissue disorders and generalized ligamentous laxity. J Hip Preserv Surg 2016; 3: 358–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Hammarstedt JE, Redmond JM, Gupta A. et al. Arthroscopic ligamentum teres reconstruction of the hip in Ehlers-Danlos syndrome: a case study. Hip Int 2015; 25: 286–91. [DOI] [PubMed] [Google Scholar]
- 56. Haversath M, Hanke J, Landgraeber S. et al. The distribution of nociceptive innervation in the painful hip: a histological investigation. Bone Joint J 2013; 95-B: 770–6. [DOI] [PubMed] [Google Scholar]
- 57. Amenabar T, O'Donnell J.. Arthroscopic ligamentum teres reconstruction using semitendinosus tendon: surgical technique and an unusual outcome. Arthrosc Tech 2012; 1:e169–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Philippon MJ, Pennock A, Gaskill TR.. Arthroscopic reconstruction of the ligamentum teres. J Bone Joint Surg Br 2012; 94-B: 1494–8. [DOI] [PubMed] [Google Scholar]
- 59. Leunig M, Beck M, Stauffer E. et al. Free nerve endings in the ligamentum capitis femoris. Acta Orthop Scand 2000; 71: 452–4. [DOI] [PubMed] [Google Scholar]
- 60. Sarban S, Baba F, Kocabey Y. et al. Free nerve endings and morphological features of the ligamentum capitis femoris in developmental dysplasia of the hip. J Pediatr Orthop Part B 2007; 16: 351–6. [DOI] [PubMed] [Google Scholar]
- 61. Yamamoto Y, Usui I.. Arthroscopic surgery for degenerative rupture of the ligamentum teres femoris. Arthroscopy 2006; 22: 689.e1–e3. [DOI] [PubMed] [Google Scholar]
- 62. Sampatchalit S, Barbosa D, Gentili A. et al. Degenerative changes in the ligamentum teres of the hip: cadaveric study with magnetic resonance arthrography, anatomical inspection, and histologic examination. J Comput Assist Tomogr 2009; 33: 927–33. LWW [cited 2017 Jan 27]. Available at: http://journals.lww.com/jcat/Fulltext/2009/11000/Degenerative_Changes_in_the_Ligamentum_Teres_of.20.aspx. Accessed: 7 March 2017. [DOI] [PubMed] [Google Scholar]
- 63. Shinohara Y, Kumai T, Higashiyama I. et al. Histological and molecular characterization of the femoral attachment of the human ligamentum capitis femoris. Scand J Med Sci Sports 2014; 24:e245–53. [DOI] [PubMed] [Google Scholar]
- 64. Moraes MR, Cavalcante ML, Leite JA. et al. The characteristics of the mechanoreceptors of the hip with arthrosis. J Orthop Surg 2011; 6: 58.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Freeman MA, Wyke B.. Articular reflexes at the ankle joint: an electromyographic study of normal and abnormal influences of ankle-joint mechanoreceptors upon reflex activity in the leg muscles. Br J Surg 1967; 54: 990–1001. [DOI] [PubMed] [Google Scholar]
- 66. Muratli HH, Biçimoğlu A, Tabak YA. et al. Mechanoreceptor evaluation of hip joint capsule and ligamentum capitis femoris in developmental hip dysplasia: a preliminary study. J Pediatr Orthop Part B 2004; 13: 299–302. [DOI] [PubMed] [Google Scholar]
- 67. Desteli EE, Gülman AB, Imren Y. et al. Comparison of mechanoreceptor quantities in hip joints of developmental dysplasia of the hip patients with normal hips. Hip Int J Clin Exp Res Hip Pathol Ther 2014; 24: 44–8. [DOI] [PubMed] [Google Scholar]
- 68. O’Kelly J, Unsworth A, Dowson D. et al. A study of the role of synovial fluid and its constituents in the friction and lubrication of human hip joints. Eng Med 1978; 7: 73–83. [Google Scholar]
- 69. Mathiessen A, Conaghan PG.. Synovitis in osteoarthritis: current understanding with therapeutic implications. Arthritis Res Ther 2017; 19: 18.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Scanzello CR, Goldring SR.. The role of synovitis in osteoarthritis pathogenesis. Bone 2012; 51: 249–57. [DOI] [PMC free article] [PubMed] [Google Scholar]


