Abstract
Although the usefulness of viewing the ocular fundus is well-recognized, ophthalmoscopy is infrequently and poorly performed by most nonophthalmologist physicians, including neurologists. Barriers to the practice of ophthalmoscopy by nonophthalmologists include not only the technical difficulty related to direct ophthalmoscopy, but also lack of adequate training and discouragement by preceptors. Recent studies have shown that digital retinal fundus photographs with electronic transmission and remote interpretation of images by an ophthalmologist are an efficient and reliable way to allow examination of the ocular fundus in patients with systemic disorders such as diabetes mellitus. Ocular fundus photographs obtained without pharmacologic dilation of the pupil using nonmydriatic fundus cameras could be of great value in emergency departments (EDs) and neurologic settings. The Fundus Photography vs Ophthalmoscopy Trial Outcomes in the Emergency Department (FOTO-ED) study showed that ED providers consistently failed to correctly identify relevant ocular funduscopic findings using the direct ophthalmoscope, and that nonmydriatic fundus photography was an effective alternate way of providing access to the ocular fundus in the ED. Extrapolating these results to headache clinics, outpatient neurology clinics, and adult and pediatric primary care settings seems self-evident. As technology advances, nonmydriatic ocular fundus imaging systems will be of higher quality and more portable and affordable, thereby circumventing the need to master the use of the ophthalmoscope. Visualizing the ocular fundus is more important than the method used. Ocular fundus photography facilitates nonophthalmologists' performance of this essential part of the physical examination, thus helping to reestablish the value of doing so.
Case history 1
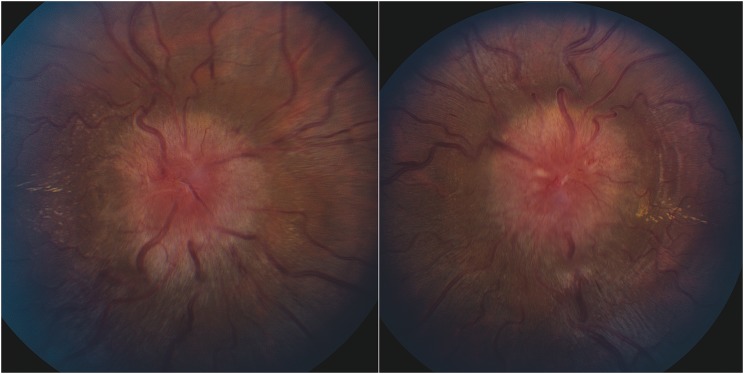
A 28-year-old woman presents to an emergency department (ED) with severe headache, neck pain, and nausea. Her examination is recorded as normal; she is diagnosed with migraine headaches, treated with analgesics, and sent home. Two weeks later, she returns to the same ED complaining of continued headaches and new blurred vision in both eyes. Examination is again recorded as normal and a CT scan of the head without contrast is unremarkable. She is diagnosed again with migraine, and sent home with an outpatient neurology referral. A week later, she is seen in an outpatient neurology clinic, where an electronic medical record indicates a normal neurologic examination, including normal cranial nerves, and she is referred for outpatient ophthalmologic evaluation. By the time she sees the ophthalmologist the following week, her vision is recorded as no perception of light in the right eye and perception of light only in the left eye, with bilateral severe papilledema on ocular funduscopic examination (figure 1). She is sent emergently to the ED, where a brain MRI and magnetic resonance venography are normal with the exception of radiographic signs of elevated intracranial pressure1 and a lumbar puncture confirms an elevated opening pressure of >55 cm H2O with otherwise normal CSF contents, establishing the diagnosis of idiopathic intracranial hypertension (IIH).2,3 Despite immediate surgical intervention for CSF diversion, her vision improves only slightly and she remains legally blind.
Figure 1. Ocular fundus shows severe bilateral papilledema.
Case history 2
A 20-year-old woman goes to an ED with severe headache, neck pain, and nausea. Her chief complaint of headache triggers the acquisition of ocular fundus photographs on a nonmydriatic fundus camera in the ED as part of a research study on the feasibility and usefulness of fundus photographs during routine ED care (figure 2). The photographs are uploaded into the electronic medical record where they are viewed by the ED provider and recognized as showing papilledema. This is confirmed by telemedical assessment of the photographs remotely by an ophthalmologist. The patient's workup occurs immediately in the ED and neuro-ophthalmologic evaluation confirms the diagnosis of IIH and the need for immediate neurosurgical management. The patient maintains excellent central visual acuity with mild peripheral visual field deficits, none of which remains symptomatic or functionally limiting.
Figure 2. Fundus photographs as seen on the patient's electronic medical records, showing severe bilateral papilledema.

Scope of the problem
In 1851, by the light of a candle, Hermann von Helmholtz viewed the living human ocular fundus via direct ophthalmoscopy and ushered in a new era in the field of ophthalmologic diagnosis.4–6 In addition to the obvious importance of viewing the ocular fundus in patients with visual complaints, it became clear by the late 19th century that findings seen on ocular fundus examination could critically inform the diagnosis of neurologic and systemic diseases and alter acute and chronic management.5 Despite the subsequent invention of other methods of examining the back of the eye, such as indirect ophthalmoscopy and slit-lamp biomicroscopy with lens magnification,2 direct ophthalmoscopy remained essentially the only clinical examination technique to view the ocular fundus available to nonophthalmologic physicians. Ophthalmoscopy became integrated into the general physical examination performed by physicians, especially those specializing in primary care, pediatrics, internal medicine, neurology, neurosurgery, and emergency medicine.6,7
Examination of the ocular fundus provides a unique opportunity to directly view CNS tissue and its vasculature. Detection of retinal vascular occlusions, hypertensive and diabetic retinopathy, and red flags for neurologic disorders such as optic disc swelling or pallor not only facilitates appropriate management of a vision-threatening condition, but often reveals an underlying systemic or neurologic disease that has dire implications for a patient's well-being and that otherwise would have been overlooked.2,3
For example, detection of optic disc edema in 2.6% of 1,408 patients presenting to an ED with a chief complaint of headache, neurologic deficit, visual loss, or elevated blood pressure altered patient disposition and contributed to the final diagnosis, confirming the importance of funduscopic examination in the ED.8
It is not surprising that ophthalmoscopy was eventually incorporated into medical education.6,7,9 Examination of the ocular fundus has always been an integral part of the neurologic examination.4,6 The standard core curriculum for medical students' neurologic clerkship10,11 cites funduscopic examination as one of the elements of the neurologic examination that must be taught during the neurology clerkship. Funduscopic examination is also listed in the Neurology Residency Core Curriculum.12,13 In addition, the Accreditation Council for Graduate Medical Education (ACGME) Neurology and Pediatric Neurology Milestones includes “visualizes papilledema” as a Neurologic Examination Milestone.14 Although neither the American Academy of Neurology Headache & Facial Pain Fellowship Core Curriculum15 nor the United Council for Neurologic Subspecialties Headache Medicine Core Curriculum16 specifically mentions this skill, it is implicitly included in the neurologic examination and is of crucial importance in excluding papilledema during the evaluation of a patient with headache. Similarly, the Model of the Clinical Practice of Emergency Medicine (an outline for the core knowledge base required of emergency physicians revised in 201617 and adopted by all 6 national organizations of emergency medicine) lists headache and papilledema as 2 of the critical symptoms or signs (defined as “a symptom or sign of a life-threatening illness or injury with a high probability of mortality if immediate intervention is not begun to prevent further…neurologic instability”) the knowledge of which must be mastered by emergency medicine specialists. Although this article does not specifically mention examination of the ocular fundus in the list of skills integral to the practice of emergency medicine, which does include slit-lamp examination, the same document lists headache, idiopathic intracranial hypertension, and cerebral venous thrombosis among the critical disorders commonly encountered in emergency medicine, indicating that identification of papilledema in the ED is an essential part of the clinical examination.17 The ACGME milestones18 emphasize the ability to perform a physical examination, recognize pertinent physical findings, and perform techniques required for conducting the examination. A wall-mounted or portable ophthalmoscope is listed among the suggested equipment for EDs proposed by the American College of Emergency Physicians (ACEP).19 The ACEP-endorsed clinical policy statement on the evaluation and management of adult patients presenting to the ED with acute, nontraumatic headache, last updated in 2008,20 emphasizes that “the cornerstone of assessing the patient with headache is the medical history and physical examination.” This policy states that “adult patients with headache and exhibiting signs of increased intracranial pressure (e.g., papilledema, absent venous pulsations on funduscopic examination …) should undergo a neuroimaging study before having a lumbar puncture in the ED.”20
Vision changes necessitate a thorough examination of the eye. Most medical specialty societies agree that headaches, acute neurologic deficits, and severely elevated systemic blood pressure measurements also deserve an assessment of the ocular fundus. Yet it is remarkable how infrequently the ocular fundus is examined in situations that are nearly universally acknowledged as requiring this important element of the physical examination.6,21–23 Headache is the fourth most common chief complaint among all patients presenting to the ED and the single most common neurologic complaint,24 but very few studies have evaluated the frequency of ophthalmoscopy and abnormal ocular findings in headache patients. A 2008 study25 reported that funduscopic examination was performed in 48% of 91 adult patients presenting to an ED with sudden, severe headache, but whether the ED providers' interpretations of the funduscopic findings were accurate is unknown. The authors proposed an algorithm for emergency evaluation of severe headache, which included systematic examination of the ocular fundus. A 2013 study26 reported that only 28 of 228 (12%) patients presenting to the ED with a chief complaint of headache had direct ophthalmoscopy performed by ED providers and that none of the ocular fundus abnormalities such as papilledema, optic nerve pallor, or grade IV hypertensive retinopathy present in 8.5% of these headache patients were detected by the ED providers. Considering that over 3 million patients visit an ED for headache each year in the United States,27,28 undetected diagnostically relevant ocular fundus findings may be present in more than 250,000 of them. Considering that a large number of patients with headache and optic nerve head edema have normal brain imaging or may not be imaged, examination of the ocular fundus in all headache patients is essential.2,3
Reports on the frequency of ocular funduscopic examination vary according to the examiner's medical specialty and training level and the patient encounter type. Even neurologists often fail to examine the ocular fundus. A pilot study of 163 headache patients evaluated in the ED, in inpatient units, or in outpatient clinics revealed that funduscopy was performed in only 11% of patients examined by an internal medicine specialist, 20% of patients examined in the ED, and 43% of patients examined by a neurologist.29 However, despite funduscopy being an essential part of any full neurologic examination, funduscopy is rarely if ever performed.6,7,21–23 In a 2010 study of 92 patients presenting to an urgent care center with acute medical conditions for which funduscopy would be clinically relevant, only 15% of patients had an examination of the ocular fundus performed.22 In a study evaluating the overdiagnosis of IIH, 20% of care providers consulted for headaches did not attempt to perform ophthalmoscopy, while 44% of those who examined the ocular fundus misinterpreted the optic nerve appearance as papilledema.30
Barriers to adequate performance of the ocular funduscopic examination
Performing direct ophthalmoscopy is not easy. Ocular fundus examination is listed second in the Stanford Medicine 25 list of difficult examination skills.31 Although the convenience of the instruments and the optical quality of the equipment have improved over the years, direct ophthalmoscopy is still a skill that necessitates extensive training, practice, and maintenance. It requires having the instrument at hand in good working order, with well-charged batteries, a cooperative patient who can maintain fixation, and a physical setting that allows for close proximity to both sides of the patient, often a problem in an ED or hospital locale. The patient's pupil must be of adequate size for viewing or pharmacologic dilation is needed, and the room lights are best dimmed, which is not always possible.2 Pharmacologic dilation of the pupil, routinely utilized by ophthalmologists in their examination of the ocular fundus, is almost never performed in nonophthalmic settings, largely due to lack of access to dilating drops, fear of side effects, and reluctance to wait the necessary 30 minutes for adequate pupillary dilation. Ophthalmoscopy takes longer than most elements of the physical examination, and it is rare these days for a physician to not feel time pressure during patient encounters.32 Preceptors of medical students, residents, fellows, and junior faculty, especially those who were not themselves well-trained or who are not skilled in the procedure, may actually discourage the practice of direct ophthalmoscopy among their trainees.21,33,34 In addition, even if the ocular fundus is visualized, many nonophthalmology practitioners do not recognize what they see or appreciate the implications of what they observe.6
How can technology help us?
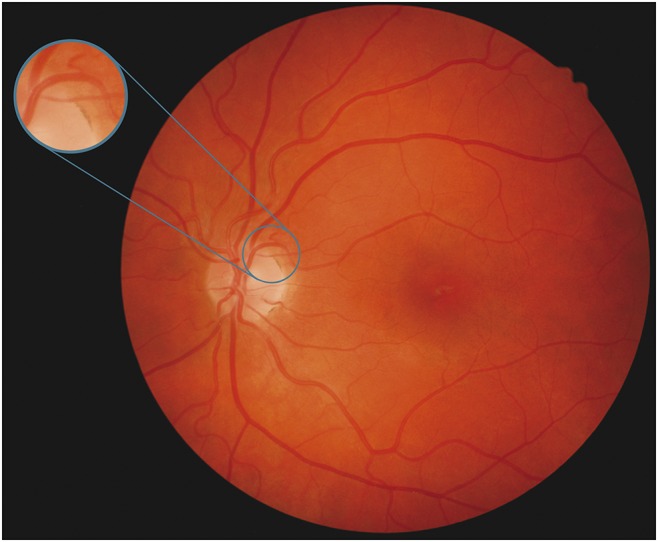
Although there are reasonable concerns about advancements in medical technology contributing to a decline in clinician examination skills,35 innovations in medical technology are one of the driving forces for innovation in medicine. Ocular fundus photography takes advantage of improvements in imaging technology to circumvent the technical obstacle of viewing the ocular fundus with an ophthalmoscope. Retinal photography was first introduced in 1886 (shortly after the ophthalmoscope was first used), became commercially available in 1926, and has been routinely used since the 1950s.36,37 The continued development of the technology has culminated in nonmydriatic high-resolution digital fundus photography. Compact and user-friendly tabletop and handheld digital cameras provide very high-quality photographs showing the entire ocular fundus even without pharmacologic dilation of the pupils (figure 3).36–38 The most recent cameras can directly connect to electronic medical records, allowing immediate and secure transmission of images.37,39,40 Portable smartphone-based ophthalmic cameras combined with applications have also emerged.37
Figure 3. Normal nonmydriatic ocular fundus photograph of the left eye with an inset showing the typical field of view of a direct ophthalmoscope.
Although most smartphone photography to date does not provide high-quality nonmydriatic retinal imaging, expected technical improvements will soon likely allow these cameras to replace the outdated direct ophthalmoscope in the pocket of any medical care provider.
One of the obvious advantages of digital imaging is the possibility of immediate transfer of imaging for remote interpretation. Numerous studies have validated the use of tele-ophthalmology in primary care centers, with remote interpretation of retinal photographs to screen for numerous ocular diseases such as diabetic retinopathy.41 The same can be done for fundus abnormalities relevant to ED care or neurology clinical practice, with appropriate interpretation of transmitted images easily accomplished on the go using a smartphone or a tablet.40 The image quality of nonmydriatic fundus photographs on an iPhone 3G was found to be superior to that of the same photographs on a desktop computer,42 likely because of the advanced features of the smartphone's display and the ease of enlarging and moving images on a smartphone. Smartphones can also video dynamic phenomena such as spontaneous venous pulsations, and new image processing software can accurately reproduce various retinal findings and screen for abnormalities based on artificial intelligence–driven algorithms.37
The FOTO-ED 3-phase study
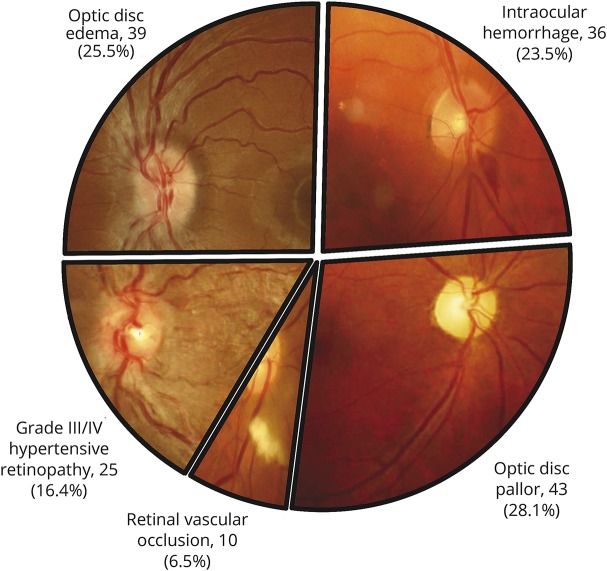
The Fundus Photography vs Ophthalmoscopy Trial Outcomes in the Emergency Department (FOTO-ED) study evaluated whether nonmydriatic ocular fundus photography would be feasible and would improve diagnosis and patient disposition in the ED compared with direct ophthalmoscopy.43–47 The FOTO-ED study included patients presenting to a university hospital ED with headaches, focal neurologic deficits, acute visual changes, or diastolic blood pressure ≥120 mm Hg, symptoms and signs generally accepted as warranting ocular fundus examination. All included patients had nonmydriatic ocular fundus photographs taken by nurse practitioners or a medical student after an average of 10 minutes of training using a commercially available nonmydriatic tabletop digital ocular fundus camera. Photographs were taken at the time of triage in a lighted room and were transmitted electronically to a neuro-ophthalmologist for remote interpretation. Relevant ocular fundus abnormalities were defined as optic disc edema, isolated intraocular hemorrhage, grade III or IV hypertensive retinopathy, retinal vascular occlusion, and optic disc pallor, findings that would change patient ED management and disposition (figure 4 and table).
Figure 4. Pie chart shows the distribution of the 153 (11.8%) relevant findings observed among 1,291 patients enrolled in the 3 phases of the Fundus Photography vs Ophthalmoscopy Trial Outcomes in the Emergency Department (FOTO-ED) study.
The photographs in each slice were taken during the study.
Table.
Emergency department (ED) providers' performance with ocular funduscopic examination in the 3 phases of the Fundus Photography vs Ophthalmoscopy Trial Outcomes in the Emergency Department (FOTO-ED) studies
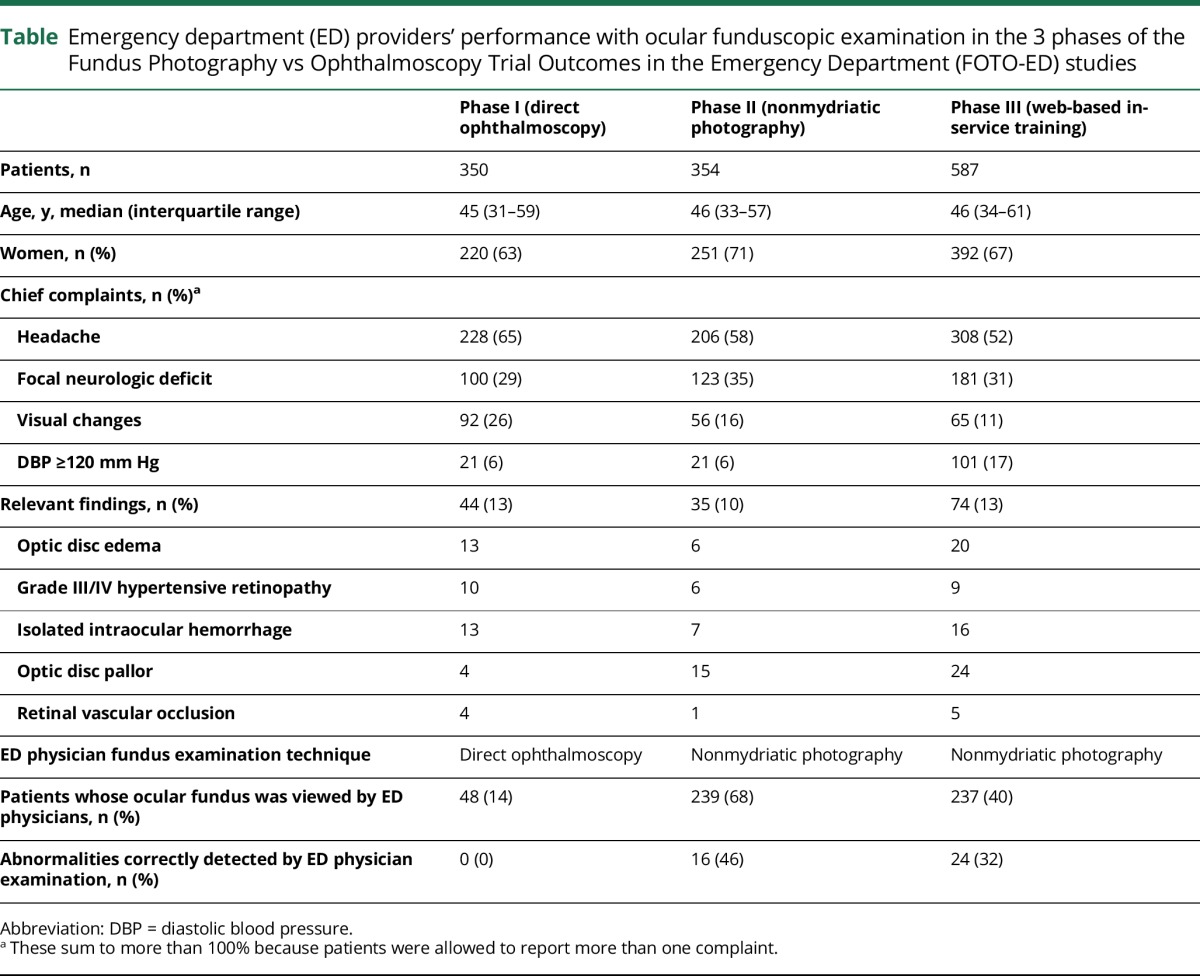
The first phase of the FOTO-ED study evaluated the routine clinical use of direct ophthalmoscopy by ED providers.43 The photographs were not made accessible to the ED providers whose behavior regarding examination of the ocular fundus with an ophthalmoscope and interpretation of findings was recorded by an external observer. This phase demonstrated that direct ophthalmoscopy was infrequently and poorly performed by ED providers. Review of the fundus photographs by a neuro-ophthalmologist revealed relevant ocular findings in 44 of the 350 enrolled patients (13%; 95% confidence interval [CI] 9%–17%). The ED providers only performed ocular funduscopic examination using a direct ophthalmoscope in 48 of the 350 enrolled patients (14%; 95% CI 10%–18%). Eleven of the 44 relevant findings were known prior to the ED evaluation and an additional 6 were identified by an ophthalmologist during a consultation in the ED, leaving 27 patients with relevant findings on photography who neither had an ophthalmology consultation requested nor were diagnosed by the ED providers. Thus, 82% (95% CI 65%–93%) of the findings unknown at the time of presentation to the ED were missed by routine ED care, and the ED providers themselves missed 100% of the relevant findings, even when they tried to use the direct ophthalmoscope, which was infrequently. This first phase of the FOTO-ED study clearly demonstrated the superiority of nonmydriatic fundus photography interpreted by neuro-ophthalmologists to routine direct ophthalmoscopy by ED providers. The study also showed that nonmydriatic fundus photography was feasible in the ED without altering ED routine flow.44 Both patients and those taking the photographs found the process agreeable and brief (mean ease, speed, and comfort rating ≥8.7 out of 10 for all; median photography time, 1.9 minutes; interquartile range 1.3–2.9 minutes, representing less than 0.5% of the patient's total ED visit time). The photographs were of good quality and provided adequate examination of the ocular fundus to allow for identification of relevant findings in 97% of enrolled patients in at least one eye.45
The second phase of the FOTO-ED study evaluated the routine use of nonmydriatic ocular fundus photography as interpreted by the ED providers.46 The photographs were automatically transferred into the ED folder of the patient's electronic medical record and the ED providers were alerted that photographs were available by an eye icon appearing on the list of tests performed for each patient. There was no incentive to encourage the ED providers to open the photography folder and the ED providers did not receive any specific education regarding how to interpret fundus photographs. Of the 354 enrolled patients in phase II, 35 (10%; 95% CI 7%–13%) had relevant findings identified on the fundus photographs by a neuro-ophthalmologist. The ED providers reviewed the photographs in 239 patients (68%), which was much higher than their 14% frequency of examination of the ocular fundus with the direct ophthalmoscopy in phase I. Importantly, they identified relevant abnormalities in 16 of 35 patients (sensitivity 46%; 95% CI 29%–63%), which was also much better than the 0% detection rate with only the direct ophthalmoscope in phase I. The ED providers also correctly identified 289 of 319 ocular fundus photographs as normal (specificity 96%; 95% CI 87%–94%), which they believed was particularly helpful (e.g., allowing exclusion of papilledema in a patient with headaches).
The third phase of the FOTO-ED study was a quality improvement project performed to determine whether a 30-minute web-based educational module would improve the ED providers' performance.47 Consistent with previous phases of the FOTO-ED study, 12.6% (74) of the 587 patients presenting to the ED with eligible chief complaints had relevant findings on ocular fundus photographs. Trained ED providers reviewed 45% of photographs and correctly identified abnormal images in 67% of cases and normal images in 80% of cases before training, compared with 43%, 45%, and 83%, respectively, after training. Untrained ED providers reviewed 35% of photographs and correctly identified abnormal findings in 50% of cases and normal images in 79% of normal cases. This study confirmed that ED providers perform much better with fundus photography than with direct ophthalmoscopy, especially to identify normal fundus photographs. However, the in-service training did not result in significant improvement in the interpretation of these photographs.
The 3 phases of the FOTO-ED study clearly showed that most ED providers consistently fail to correctly identify relevant ocular funduscopic findings using the direct ophthalmoscope, and that nonmydriatic fundus photography is an effective alternate way of providing access to the ocular fundus in the ED. A total of 1,291 patients were included in the 3 phases of the FOTO-ED study, among whom 153 (12%) had relevant findings on fundus photographs that altered the ED management of these patients. The ED providers were not able to identify any of the relevant findings in phase I without the help of an ophthalmologist consultant, but they recognized 40 of the 109 (36.7%) relevant findings when given access to fundus photographs in phases II and III. They also correctly identified 448 out of the 515 (87%) normal images, which was believed to be very helpful, particularly in patients with headaches in whom papilledema could be easily and reliably excluded.
Future applications
The FOTO-ED study triggered a great deal of interest and enthusiasm not only from ED providers, but medical students, residents, and nonophthalmology physicians such as neurologists. Indeed, the findings of the FOTO-ED study can likely be extrapolated to other nonophthalmologic settings.48,49 Numerous other studies have now validated the use of cameras in clinical settings other than adult EDs.50–54 The feasibility and reliability of nonmydriatic fundus photography in children as young as 22 months was demonstrated in a pediatric ophthalmology clinic.50 A subsequent study validated the use of a tabletop nonmydriatic camera in children ages 5–12 years in a pediatric ED.51 Another study showed that relatively good images of the optic disc could be obtained in children as young as 2 years without pupillary dilation using a smartphone attached to an ophthalmoscope.52
The applications of this technology in neurology settings are multiple and go beyond the assessment of papilledema in headache patients. For example, recognition of grade III/IV hypertensive retinopathy is important in numerous neurologic emergencies.43,53,54 Ocular fundus photography may also prove useful in the risk stratification of patients presenting with suspected TIA or stroke48,55–57 or in critically ill patients in whom identification of ocular fundus abnormalities may affect acute management and prognosis.58
New inexpensive, portable, easy-to-operate fundus cameras have revolutionized retinal screening programs, which have grown exponentially over the last decade. Tele-ophthalmology screening is now the standard of care in linking remote areas to ophthalmologists.41 Neurology clinics, primary care offices, urgent care centers, and EDs can use any of the nonmydriatic cameras that connect directly to electronic medical records and integrate fundus photographs into a patient's systematic evaluation. Although the hope is that most physicians will learn to accurately interpret the photographs themselves, remote interpretation by an ophthalmologist is always possible, facilitated by the integrated Internet connection capability of most recent cameras. Obtaining a fundus photograph does not replace an ophthalmologic consultation in patients with visual complaints, when the diagnosis is not obvious, or when the photograph is of poor quality. Rather, such photographs should be considered an integral part of the clinical examination that should prove helpful in triaging patients appropriately.
The new generation of medical students embraces new technology and already prefers nonmydriatic fundus photography to direct ophthalmoscopy.33,34,49 Obtaining a photograph in a few seconds instead of trying to visualize the ocular fundus with a direct ophthalmoscope allows providers to focus on the findings and their implications for diagnosis and management rather than on the technique of mastering ophthalmoscopy. Traditional medical school and residency curricula should include interpretation of ocular fundus photography as an educational tool.49 Restoring the ocular fundus examination to its appropriate place in general and neurologic physical examinations will undoubtedly enhance patient care and prevent medical errors and adverse events.59,60 Our first patient was irreversibly blind because 2 ED providers and 1 neurologist failed to attempt an ocular fundus examination. The incurred medicolegal fees alone would cover the price of at least 120 excellent digital cameras. Downstream expenses saved by prevention of patient morbidity would likely justify widespread implementation of this technology.
The usefulness of viewing the ocular fundus is well-recognized, and fundus photography can circumvent the major obstacle of using an ophthalmoscope. The emergence of digital cameras capable of providing high-quality photographs without pharmacologic dilation of the pupils makes it possible for nonophthalmologists to easily visualize the ocular fundus in a timely fashion and reestablishes the value of doing so.
Glossary
- ACEP
American College of Emergency Physicians
- ACGME
Accreditation Council for Graduate Medical Education
- CI
confidence interval
- ED
emergency department
- FOTO-ED
Fundus Photography vs Ophthalmoscopy Trial Outcomes in the Emergency Department
- IIH
idiopathic intracranial hypertension
Author contributions
Valérie Biousse: participated in the design of the study, in the analysis and interpretation of the data, and in the drafting and critical revision of the manuscript. Beau B. Bruce: participated in the design of the study, in the collection, analysis, and interpretation of the data, and in the critical revision of the manuscript. Nancy J. Newman: participated in the design of the study, in the analysis and interpretation of the data, and in the drafting and critical revision of the manuscript.
Study funding
Supported in part by Research to Prevent Blindness (Department of Ophthalmology) and NIH grants P30-EY006360 (Department of Ophthalmology), K23-EY019341 (B. Bruce), and UL1-RR025008 (V. Biousse).
Disclosure
V. Biousse is a consultant for Gensight Biologics (France) and received research support from the NIH/PHS (P30-EY006360), NIH (R01-NS089694), and Research to Prevent Blindness. B. Bruce served as a consultant for MedImmune (data safety and monitoring board) and Bayer (medicolegal), has provided expert testimony on optic disc edema, and received research support via his institution from Teva Pharmaceuticals, Pfizer, Novartis, and the NIH (P30-EY006360, R01-NS089694). N. Newman is a consultant for Gensight Biologics (France) and Santhera Pharmaceuticals (Switzerland), serves on the Data Safety Monitoring Board for a Quark Pharmaceuticals (Israel) clinical trial, has provided expert testimony on optic disc edema, and has received research support from NIH grants (R01-089694, P30-EY006360) and Research to Prevent Blindness Lew R. Wasserman Merit Award. Go to Neurology.org/N for full disclosures.
References
- 1.Bidot S, Saindane AM, Peragallo JH, Bruce BB, Newman NJ, Biousse V. Brain imaging in idiopathic intracranial hypertension. J Neuro Ophthalmol 2015;35:400–411. [DOI] [PubMed] [Google Scholar]
- 2.Biousse V, Newman NJ. Neuro-ophthalmology Illustrated. 2nd ed. New York: Thieme; 2016. [Google Scholar]
- 3.Biousse V, Newman NJ. Diagnosis and clinical features of common optic neuropathies. Lancet Neurol 2016;15:1355–1367. [DOI] [PubMed] [Google Scholar]
- 4.Sherman SE. The history of the ophthalmoscope. Doc Ophthalmol 1989;71:221–228. [DOI] [PubMed] [Google Scholar]
- 5.Verghese A, Charlton B, Cotter B, Kugler J. A history of physical examination texts and the conception of bedside diagnosis. Trans Am Clin Climatol Assoc 2011;122:290–311. [PMC free article] [PubMed] [Google Scholar]
- 6.Mackay DD, Garza PS, Bruce BB, Newman NJ, Biousse V. The demise of direct ophthalmoscopy: a modern clinical challenge. Neurol Clin Pract 2015;4:150–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Benbassat J, Polak BC, Javitt JC. Objectives of teaching direct ophthalmoscopy to medical students. Acta Ophthalmol 2012;90:503–507. [DOI] [PubMed] [Google Scholar]
- 8.Sachdeva V, Vasseneix C, Hage R, et al. Optic nerve head edema among patients presenting to the emergency department. Neurology (in press, 2018). [DOI] [PMC free article] [PubMed]
- 9.Stern GA. Teaching ophthalmology to primary care physicians: The Association of University Professors of Ophthalmology Education Committee. Arch Ophthalmol 1995;113:722–724. [DOI] [PubMed] [Google Scholar]
- 10.Gelb DJ, Gunderson CH, Henry KA, Kirshner HS, Józefowicz RF; Consortium of Neurology Clerkship Directors and the Undergraduate Education Subcommittee of the American Academy of Neurology. The neurology clerkship core curriculum. Neurology 2002;58:849–852. [DOI] [PubMed] [Google Scholar]
- 11.American Academy of Neurology, Association of University Professors of Neurology, American Neurological Association. Neurology clerkship core curriculum guidelines. Available at: aan.com/uploadedFiles/4CME_and_Training/2Training/3Fellowship_Resources/5Core_Curricula/skilz.pdf. Accessed September 25, 2017.
- 12.Neurology Residency Core Curriculum (American Academy of Neurology). Available at: acgme.org/Specialties/Milestones/pfcatid/37/Neurology. Accessed September 25, 2017.
- 13.American Board of Psychiatry & Neurology. Neurology core competencies outline. 2000. Available at: abpn.com/wp-content/uploads/2015/02/2011_core_N_MREE.pdf. Accessed September 25, 2017.
- 14.The Accreditation Council for Graduate Medical Education, The American Board of Psychiatry and Neurology. The neurology milestone project. 2015. Available at: acgme.org/Specialties/Milestones/pfcatid/37/Neurology. Accessed September 25, 2017.
- 15.Headache and Facial Pain Fellowship Core Curriculum (American Academy of Neurology). Available at: aan.com/uploadedFiles/Website_Library_Assets/Documents/8Membership/3People/5Sections/1Drop_down_for_33_sections/Headache_and_Facial_Pain/Fellowship%20Core%20Curricula.pdf. Accessed September 25, 2017.
- 16.United Council for Neurologic Subspecialties. Headache medicine core curriculum. Available at: ucns.org/globals/axon/assets/3672.pdf. Accessed September 25, 2017.
- 17.Counselman FL, Babu K, Edens MA, et al. ; 2016 EM Model Review Task Force, Beeson MS, Keehbauch JN; American Board of Emergency Medicine. The 2016 model of the clinical practice of emergency medicine. J Emerg Med 2017;52:846–849. [DOI] [PubMed] [Google Scholar]
- 18.The Accreditation Council for Graduate Medical Education, The American Board of Emergency Medicine. The emergency medicine milestone project. 2015. Available at: acgme.org/Specialties/Milestones/pfcatid/7/Emergency%20Medicine. Accessed September 25, 2017.
- 19.American College of Emergency Medicine. Emergency department planning and resource guidelines. 2014. Available at: acep.org/uploadedFiles/ACEP/Practice_Resources/policy_statements/ED_Planning_Policy_FINAL_040914.pdf. Accessed September 25, 2017.
- 20.Edlow JA, Panagos PD, Godwin SA, Thomas TL, Decker WW; American College of Emergency Physicians. Clinical policy: critical issues in the evaluation and management of adult patients presenting to the emergency department with acute headache. Ann Emerg Med 2008;52:407–436. [DOI] [PubMed] [Google Scholar]
- 21.Roberts E, Morgan R, King D, Clerkin L. Funduscopy: a forgotten art? Postgrad Med J 1999;75:282–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dalay S, Umar F, Saeed S. Funduscopy: a reflection upon medical training? Clin Teach 2013;10:103–106. [DOI] [PubMed] [Google Scholar]
- 23.Wu EH, Fagan MJ, Reinert SE, Diaz JA. Self-confidence in and perceived utility of the physical examination: a comparison of medical students, residents, and faculty internists. J Gen Intern Med 2007;22:1725–1730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pitts SR, Niska RW, Xu J, Burt CW. National Hospital Ambulatory Medical Care Survey: 2006 emergency department summary. Natl Health Stat Report 2008:1–38. [PubMed] [Google Scholar]
- 25.Breen DP, Duncan CW, Pope AE, Gray AJ, Al-Shahi Salman R. Emergency department evaluation of sudden, severe headache. QJM 2008;101:435–443. [DOI] [PubMed] [Google Scholar]
- 26.Thulasi P, Fraser CL, Biousse V, Wright DW, Newman NJ, Bruce BB. Nonmydriatic ocular fundus photography among headache patients in an emergency department. Neurology 2013;80:432–437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lucado J, Paez K, Elixhauser A. Headaches in U.S. Hospitals and Emergency Departments, 2008: Statistical Brief #111. 2011 May. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs [Internet]. Rockville, MD: Agency for Healthcare Research and Quality; 2006. [PubMed] [Google Scholar]
- 28.Goldstein JN, Camargo CA Jr, Pelletier AJ, Edlow JA. Headache in United States emergency departments: demographics, work-up and frequency of pathological diagnoses. Cephalalgia 2006;26:684–690. [DOI] [PubMed] [Google Scholar]
- 29.Golombievski E, Doerrler MW, Ruland SD, McCoyd MA, Biller J. Frequency of direct funduscopy upon initial encounters for patients with headaches, altered mental status, and visual changes: a pilot study. Front Neurol 2015;6:233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fisayo A, Bruce BB, Newman NJ, Biousse V. Overdiagnosis of idiopathic intracranial hypertension. Neurology 2016;86:341–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Stanford Medicine 25. Available at: stanfordmedicine25.stanford.edu/. Accessed September 25, 2017.
- 32.Chi J, Artandi M, Kugler J, et al. The five-minute moment. Am J Med 2016;129:792–795. [DOI] [PubMed] [Google Scholar]
- 33.Kelly LP, Garza PS, Bruce BB, Graubart EB, Newman NJ, Biousse V. Teaching ophthalmoscopy to medical students (the TOTeMS study). Am J Ophthalmol 2013;156:1056–1061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mackay DD, Garza PS, Bruce BB, et al. Teaching ophthalmoscopy to medical students (TOTeMS) II: a one-year retention study. Am J Ophthalmol 2014;157:747–748. [DOI] [PubMed] [Google Scholar]
- 35.Jauhar S. The demise of the physical exam. N Engl J Med 2006;354:548–551. [DOI] [PubMed] [Google Scholar]
- 36.Bennett TJ, Barry CJ. Ophthalmic imaging today: an ophthalmic photographer's viewpoint: a review. Clin Exp Ophthalmol 2009;37:2–13. [DOI] [PubMed] [Google Scholar]
- 37.Panwar N, Huang P, Lee J, et al. Fundus photography in the 21st century: a review of recent technological advances and their implications for worldwide healthcare. Telemed J E Health 2016;22:198–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pérez MA, Bruce BB, Newman NJ, Biousse V. The use of retinal photography in nonophthalmic settings and its potential for neurology. Neurologist 2012;18:350–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bidot S, Bruce BB, Newman NJ, Biousse V. Nonmydriatic retinal photography in the evaluation of acute neurologic conditions. Neurol Clin Pract 2013;3:527–531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bruce BB, Newman NJ, Pérez MA, Biousse V. Non-mydriatic ocular fundus photography and telemedicine: past, present, and future. Neuro-ophthalmology 2013;37:51–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gupta A, Cavallerano J, Sun JK, Silva PS. Evidence for telemedicine for diabetic retinal disease. Semin Ophthalmol 2017;32:22–28. [DOI] [PubMed] [Google Scholar]
- 42.Lamirel C, Bruce BB, Wright DW, Newman NJ, Biousse V. Nonmydriatic digital ocular fundus photography on the iPhone 3G: the FOTO-ED study. Arch Ophthalmol 2012;130:939–940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bruce BB, Lamirel C, Wright DW, et al. Nonmydriatic ocular fundus photography in the emergency department. N Engl J Med 2011;364:387–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bruce BB, Lamirel C, Biousse V, et al. Feasibility of nonmydriatic ocular fundus photography in the emergency department: phase I of the FOTO-ED study. Acad Emerg Med 2011;18:928–933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bruce BB, Thulasi P, Fraser CL, et al. Diagnostic accuracy and use of nonmydriatic ocular fundus photography by emergency physicians: phase II of the FOTO-ED study. Ann Emerg Med 2013;62:28–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lamirel C, Bruce BB, Wright DW, Delaney KP, Newman NJ, Biousse V. Quality of nonmydriatic digital fundus photography obtained by nurse practitioners in the emergency department: the FOTO-ED study. Ophthalmology 2012;119:617–624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bruce BB, Bidot S, Hage R, et al. Fundus photography vs. ophthalmoscopy outcomes in the emergency department (FOTO-ED) phase III: web-based, in-service training of emergency providers. Neuro-Ophthalmology (in press 2018). [DOI] [PMC free article] [PubMed]
- 48.Bruce BB, Biousse VB, Newman NJ. Nonmydriatic ocular fundus photography in neurologic emergencies. JAMA Neurol 2015;72:455–459. [DOI] [PubMed] [Google Scholar]
- 49.Mackay DD, Garza PS. Ocular fundus photography as an educational tool. Semin Neurol 2015;35:496–505. [DOI] [PubMed] [Google Scholar]
- 50.Toffoli D, Bruce BB, Lamirel C, Henderson AD, Newman NJ, Biousse V. Feasibility and quality of nonmydriatic fundus photography in children. J AAPOS 2011;15:567–572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ivan Y, Ramgopal S, Cardenas-Villa M, et al. Feasibility of the digital retinography system camera in the pediatric emergency department. Pediatr Emerg Care 2017. [DOI] [PubMed] [Google Scholar]
- 52.Day LM, Wang SX, Huang CJ. Nonmydriatic fundoscopic imaging using the pan optic iExaminer system in the pediatric emergency department. Acad Emerg Med 2017;24:587–594. [DOI] [PubMed] [Google Scholar]
- 53.Henderson AD, Biousse V, Newman NJ, Lamirel C, Wright DW, Bruce BB. Grade III or Grade IV hypertensive retinopathy with severely elevated blood pressure. West J Emerg Med 2012;13:529–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Muiesan ML, Salvetti M, Paini A, et al. Ocular fundus photography with a smartphone device in acute hypertension. J Hypertens 2017;35:1660–1665. [DOI] [PubMed] [Google Scholar]
- 55.Cheung CY, Chen C, Wong TY. Ocular fundus photography as a tool to study stroke and dementia. Semin Neurol 2015;35:481–490. [DOI] [PubMed] [Google Scholar]
- 56.Wang JJ, Baker ML, Hand PJ, et al. Transient ischemic attack and acute ischemic stroke: associations with retinal microvascular signs. Stroke 2011;42:404–408. [DOI] [PubMed] [Google Scholar]
- 57.Vuong LN, Thulasi P, Biousse V, et al. Ocular fundus photography of patients with focal neurologic deficits in an emergency department. Neurology 2015;85:256–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Garza PS, Fajoles-Vasseneix C, Clough L, et al. Handheld ocular fundus photography in acute subarachnoid hemorrhage: the FOTO-ICU study. Presented at the North American Neuro-Ophthalmology Society annual meeting; March 1, 2016: Tucson, AZ.
- 59.Kugler J, Verghese A. The physical exam and other forms of fiction. J Gen Intern Med 2010;25:756–757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Verghese A, Charlton B, Kassirer JP, Ramsey M, Ioannidis JP. Inadequacies of physical examination as a cause of medical errors and adverse events: a collection of vignettes. Am J Med 2015;128:1322–1324. [DOI] [PubMed] [Google Scholar]