Abstract
Objectives
Examine evidence for different subclasses of posttraumatic stress disorder (PTSD) symptoms in a sample of trauma exposed, low-income, predominantly African American men and women. Assess the relationship between PTSD subclasses with major depressive disorder (MDD) and types of trauma experienced.
Method
Latent class analysis (LCA) using a multivariate normal mixture model on the 17-item PTSD Symptom Scale (PSS) was used to identify latent subclasses of PTSD symptoms (N=5063).
Results
LCA suggested four subclasses of PTSD symptoms: (1) High severity and comorbidity (n= 932, 92.2% current PTSD, 88.7% MDD, 82% both), characterized by high PTSD symptoms, depression, and comorbidity of PTSD and MDD; (2) Moderate severity (n= 1179, 56.5% current PTSD, 53.9% MDD, 34.5% both), which had high avoidance and hyper-vigilance symptoms compared to the other symptoms; (3) Low PTSD and high depression (n= 657, 12.8% current PTSD, 49.9% MDD, 8.8% both) which had high insomnia but otherwise low PTSD symptoms and high depression; and (4) Resilient (n= 2295, 2.0% current PTSD, 16.4% MDD, and 0.6% both) characterized by low mean scores on all PTSD symptoms and depression.
Conclusions
The results suggest avoidance and hyper-vigilance are important -symptoms in PTSD development and insomnia may be an important indicator for depression. The combination of severe insomnia, avoidance, and hyper-vigilance may be key symptoms for comorbidity of PTSD and MDD. Future studies should focus on these symptoms to better target people at high risk for developing PTSD or MDD.
Keywords: Trauma exposure, Depression, Child abuse, Subclass of PTSD symptoms, Comorbidity
Introduction
Posttraumatic stress disorder (PTSD) is a severe trauma-related psychiatric illness often associated with depression. The rate of lifetime PTSD in the veteran population has been estimated to be 10–31% (Kang et al., 2003; Kulka et al., 1990; Tanielian and Jaycox, 2008) with lower rates observed in the general population, estimated to be 5–10% (Kessler et al., 1995). The National Comorbidity Survey of 1995 (Kessler et al., 1995) estimated that 48% individuals who met criteria for PTSD also met criteria for major depressive disorder (MDD). PTSD and MDD are the two most common psychiatric outcomes among individuals with trauma exposure. Symptoms that characterize PTSD include intrusive and fearful memories, flashbacks, emotional numbing, and nightmares of the traumatic events, while symptoms such as emotional detachment, loss of interest, and impaired concentration characterize MDD. The considerable overlap of symptoms of PTSD subjects with other psychiatric diseases has posed significant challenges in diagnosing and treating patients with PTSD.
Previously, PTSD studies mainly focused on veteran populations (Bremner et al., 1992; Dohrenwend et al., 2006; Kang et al., 2003; Wolf et al., 2012). More recently, there has been an increasing interest in studying PTSD in the civilian population (Cloitre et al., 2013, 2014; Gillespie et al., 2009; Nugent et al., 2012; Schwartz et al., 2005). Among civilians, economically disadvantaged African American and Latino populations appear to be exposed to significant amounts of trauma (Alim et al., 2006a; Breslau et al., 1998). In a sample of predominately low-income African American men and women (n=1256), 87.8% reported some form of significant trauma exposure in their lifetime (Gillespie et al., 2009). There is evidence that trauma-related psychopathology contributes to intergenerational patterns of violence (Abram et al., 2004; Byrne et al., 1999; Fullilove et al., 1998; Schwartz et al., 2005, 2004) with potential for psychiatric as well as medical illness and constitutes a major public health problem. Given that there is tremendous heterogeneity in the clinical presentation of PTSD it is of interest to investigate whether certain homogeneous subclasses exist by parsing out the heterogeneity of PTSD symptoms. The findings of such homogeneous subclasses would help to understand the etiology of the disease and may help enhance treatment strategies.
Latent class analysis (LCA) is a powerful data driven statistical method to investigate the structure of heterogeneous diseases. Model based classification methods partition subjects into subclasses such that subjects are homogenous within a subclass while subjects from different subclasses are heterogeneous. LCA is commonly used (Cloitre et al., 2013, 2014; Nugent et al., 2012; Steuwe et al., 2012; Wolf et al., 2012) for obtaining unobserved subclasses (subgroups) of mental disorders such as PTSD based on behavioral symptoms. Breslau and colleagues (Breslau et al., 2005) first applied LCA to investigate the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM-IV) PTSD symptoms from two large urban community samples and reported the presence of three subclasses of subjects based on symptoms, described as: ‘no disturbance’, ‘intermediate disturbance’, and ‘pervasive disturbance’. Nugent and colleagues (Nugent et al., 2012) applied LCA (LCA with continuous scores is often known as latent profile analysis (LPA), however, we use the generic term LCA) on the DSM-IV PTSD symptoms (severity score) to examine heterogeneity among PTSD patients from a subset of subjects described in this manuscript. They reported six different subgroups of PTSD symptom profiles, described as: ‘resilient’, ‘moderate with amnesia’, ‘moderate with diminished interest’, ‘moderate without diminished interest and amnesia’, ‘severe without amnesia’, and ‘severe over all’. They further summarized their findings as ‘resilient’ (1 profile), ‘moderate’ (three profiles), and ‘severe’ (2 profiles) symptoms to be consistent with Breslau and colleagues (Breslau et al., 2005) LCA subclasses.
The goal of the current investigation was to find parsimonious and reproducible latent subclasses of subjects in terms of PTSD symptom severity based on a large dataset (N=5063) with DSM-IV PTSD symptoms in a low-income, trauma exposed, primarily African American population.
One of the major challenges in such latent class analyses is to decide on the number of subclasses to extract. A commonly used criterion is to choose the number of subclasses that optimizes the goodness-of-fit statistics such as the Bayesian Information Criterion (BIC) (Schwarz, 1978) and the Log-likelihood of the latent class model to the observed data. The parametric bootstrapped likelihood ratio test (BLRT) (McLachlan and Peel, 2000) is another commonly used criterion to extract latent subclasses. However, fit statistics, such as BIC don’t always provide the most interpretable latent subclasses (Cloitre et al., 2013, 2014; Wolf et al., 2012) and BLRT in the framework of LCA is often inconclusive (Nylund et al., 2007). Specifically, when the sample size increases, fit statistics generally tend to lead to a larger number of latent subclasses. This becomes a problem in a large population study such as ours because the above mentioned fit statistics result in over-stratification of the population. Another problem is that the identified subclasses would have poor reproducibility in other studies. We developed a new measure, the Reproducibility Index, to help guide the selection of the number of latent subclasses in order to have greater stability and reproducibility of results in future studies.
In this study, LCA was applied to data for participants from the Grady Trauma Project, a NIH funded project investigating PTSD in an urban population, using scores from the 17-item PTSD Symptom Scale (PSS). Interpretable and reproducible latent subclasses of subjects in terms of PTSD symptoms severity were obtained. We characterized the identified subclasses in terms of PTSD symptom severity, current PTSD and MDD diagnosis, as well as comorbidity of PTSD and MDD. This study also provided an opportunity to assess the relationship be- tween PTSD and trauma exposure scores, such as the childhood trauma questionnaire (CTQ) and traumatic event inventory (TEI), which was important because trauma plays the primary etiologic role for the development of PTSD and comorbidity of PTSD and MDD.
Methods
Study Subjects
The data for this study were collected to increase understanding of psychiatric sequelae of trauma exposure in a low-income, urban population of, predominantly African American men and women. A total of 8091 participants were approached while in the waiting rooms of primary care or obstetrical-gynecological clinics of Grady Memorial Hospital in Atlanta, Georgia, USA. All participants signed informed consent approved by the Emory University Institutional Review Board and the Grady Hospital Research Oversight Committee. Approximately a third of the participants were missing some items of PSS or did not meet a trauma exposure criterion for PTSD diagnosis. We analyzed data for 5063 participants, all of who had complete information on the 17-item PSS and a history of trauma exposure.
Clinical Assessment
All subjects in the study completed the modified PSS (Foa and Tolin, 2000; Schwartz et al., 2005), the Beck Depression Inventory (BDI) (Beck et al., 1961) for depressive symptom assessment, and Childhood Trauma Questionnaire (CTQ) (Bernstein and Fink, 1998) for childhood abuse. Lifetime trauma exposure was assessed by the Traumatic Events Inventory (TEI) (Schwartz et al., 2005).
Modified PTSD Symptom Scale (PSS)
The PSS is a psychometrically valid 17-item self-report scale assessing PTSD symptomatology over the two weeks prior to rating (Foa and Tolin, 2000; Schwartz et al., 2005). Each symptom is rated on a 4-point scale from 0 (not at all) to 3 (very much/almost always) with higher scores indicating more severe symptoms of PTSD. The PSS has been validated with the widely used gold standard measure of PTSD, the Clinician Administered PTSD Scale (CAPS; (Foa et al., 1993; Foa and Tolin, 2000)). The diagnosis of current PTSD (PTSD vs. no PTSD) was determined based on DSM-IV A-E criteria responses to the PSS questionnaire (A, exposure of trauma; B, presence of at least 1 intrusive symptom; C, presence of at least 3 avoidance/numbing symptoms; and D, presence of at least 2 hyperarousal symptoms; and E, symptoms present for at least 1 month).
The Beck Depression Inventory (BDI)
The BDI (Beck et al., 1961) is 21-item self- report inventory measuring depression severity in the previous 2 weeks. Each of the items measures the presence and severity of depressive symptoms that are rated on a scale from 0 to 3. For certain analysis, subjects were classified as having MDD determined by a cutoff score of 15 on the BDI (Craven et al., 1988), which results in optimal sensitivity. The Structured Clinical Interview for DSM-IV (SCID) confirmed the current diagnosis of MDD in a subset of individuals.
Childhood Trauma Questionnaire (CTQ)
The CTQ (Bernstein and Fink, 1998) is a 28-item self-report inventory assessing childhood physical, sexual and emotional abuse. The current brief version (Bernstein and Fink, 1998; Bernstein et al., 2003) of CTQ and the original 70-item CTQ are both consistent, stable over time, with high validity. The CTQ yields a total score and five sub-scale scores, in particular, childhood sexual abuse (items 20–24, 27), childhood physical abuse (item 9,11,12,15,17), childhood emotional abuse (item 3,8,14,18,25), childhood emotional negligence (item 5,7,13,19,28), and childhood physical negligence (item 1,2,4,6,26).
Traumatic Events Inventory (TEI)
The traumatic events inventory (Schwartz et al., 2005) is a measure that assesses lifetime history of trauma exposure, including child abuse and non-child abuse. The TEI assesses past experience and frequency of 13 separate types of traumatic events.
Statistical Analysis
In order to identify homogeneous groups of subjects in terms of PTSD symptoms, we employed a latent class analysis (LCA) with the 17 core symptoms of PTSD, measured by PSS. We performed LCA via model-based classification for normal mixture models (Fraley and Raftery, 2002) with R-package mclust version 5.0.2 (Fraley et al., 2012), which has been shown to outperform traditional classification algorithms (Magidson and Vermunt, 2002). One advantage of normal mixture models (Fraley and Raftery, 2002) with mclust statistical software is that it has several covariance models to choose from (Fraley et al., 2012). Thus, to determine the optimum number of latent subclasses we conducted our analysis using mclust version 5.0.2 with the covariance model ‘EII’ (Fraley et al., 2012). Geometric features of the latent subclasses are spherical with equal size, which provided better qualitative and quantitative differences among the selected subclasses. Classification of subjects was determined based on the estimated posterior probabilities that indicate the likelihood of each subject belonging to each subclass. Subjects were assigned to the subclass for which the posterior probability was highest.
Model fit comparison was assessed using three traditional methods (a) log-likelihood; (b) Bayesian information criterion (BIC), a penalized log-likelihood function where the penalty term is based on the number of estimated parameters and the sample size used; and (c) Gap-statistic (Tibshirani et al., 2001), a nonparametric goodness-of-classification measure that takes into account within- and between-class sum-squares obtained from a given number of classes. The higher values of the log-likelihood, BIC and Gap-statistic corresponds to a better fit of the model to the observed data, which guided our selection of the number of latent subclasses. However, the determination of the number of subclasses based on the current fit statistics is often ambiguous, particularly with large data sets, and results in over estimation of the number of subclasses (Baudry et al., 2010). In order to address this issue, we developed an empirical statistical measure to aide in the decision of the number of subclasses. Development of the measure was based on the principle that the number of subclasses should be reproducible when the same latent model is applied to repeated sampling of subsets of data or in other studies. We refer to this measure as the Reproducibility Index and it is described below.
Reproducibility Index
We considered an empirical measure to help guide in determining the number of latent subclasses such that the selected number of subclasses is reproducible in a subsample of the dataset or in other studies. For a given number of subclasses, for example 2, we fit a LCA model for the whole dataset. Then, we took a subsample of the data and fit LCA model to the subsample. Next, we computed the percent of subjects from the subsample whose class membership was the same as the class membership when the total dataset was used. We then computed a weighted sum of these percentages where weights were the proportion of subjects belonging to each subclass of the subsample data. We repeated this process 1000 times, at each time with a subsample of 500 individuals. Finally, we computed the mean of the weighted sum of percentages and referred to this as the Reproducibility Index for determining number of subclasses in the LCA. A Reproducibility Index value of 1 indicated that the number of latent subclasses is perfectly reproducible in a subsample or a smaller dataset. We repeated this procedure up to 9 subclasses and the estimated Reproducibility Index is given in Table 2. Reproducibility Index is promising in the determination of latent subclasses such that the selected number of subclass will be reproducible in other studies.
Table 2.
Summary of Fit Statistics and Reproducibility Measures
| Model (# of Subclasses) | BIC a | Log-likelihood b | Gap-Statistic c | Reproducibiliyd Index |
|---|---|---|---|---|
| 2 | −238.73 | −119.21 | 0.85 | 0.99 |
| 3 | −234.00 | −116.76 | 0.89 | 0.96 |
| 4 | −232.75 | −116.07 | 0.91 | 0.79 |
| 5 | −231.07 | −115.15 | 0.92 | 0.79 |
| 6 | −229.60 | −114.34 | 0.93 | 0.73 |
| 7 | −229.75 | −114.34 | 0.95 | 0.52 |
| 8 | −227.43 | −113.10 | 0.95 | 0.58 |
| 9 | −227.58 | −113.10 | 0.93 | 0.32 |
Bayesian Information Criteria: maximum value provides optimal latent class; values are in thousands
Maximum value provides optimal latent class; values are in thousands
Largest gap-statistic provides optimal number of subclasses
Larger value provides better reproducibility of subclasses and 1 indicates perfect reproducibility
For this study, the number of latent subclasses was determined by first looking at the three traditional methods (BIC, log-likelihood, and gap-statistic) and then using the Reproducibility Index. Finally, interpretability of the remaining latent subclasses was assessed to decide on the optimal number of latent subclasses.
Multiple pairwise comparisons were performed to examine differences in PTSD symptoms, depression symptoms, trauma exposure, and demographics across the identified latent subclasses. To account the classification error we employed BCH method (Bakk et al., 2013) when comparing external variables by latent subclasses. Note that BCH method uses posterior probabilities that indicate the likelihood of each subject belongs to a subclass and which is one of the commonly used method to account classification errors.
Results
There were 5053 subjects that reported their gender of which 3572 were females (70.7%) and 1481 were males (29.3%) (Table 1). Self-identified race was predominantly African American (91.9 %). The mean age of the sample was 40 years (range:18–81) and the majority of the subjects were unemployed at the time of interview (69.1%).
Table 1.
Demographic Characteristic of Subjects
| Demographic | Total Sample (N),% | Male (n),% | Female (n),% |
|---|---|---|---|
| Sex | 5053 | (1481) 29.3% | (3572) 70.7% |
| Age (5034) | 5034 | (1478), 29.4% | (3556), 70.6% |
| 18–24 | (862), 17.1 % | (147), 9.9% | (715), 20.1% |
| 25–34 | (977), 19.4 % | (190), 12.9% | (787), 22.1% |
| 35–44 | (902), 17.9% | (293), 19.8% | (609), 17.1% |
| 45–54 | (1426), 28.3 % | (519), 35.1% | (907), 25.5% |
| 55–65 | (777), 15.4 % | (300), 20.3% | (477), 13.4% |
| > 65 | (90), 1.8% | (29), 2.0% | (61), 1.7% |
| Race/ethnicity (5032) | |||
| African American/Black | (4623), 91.9% | (1339), 90.7% | (3284), 92.4% |
| Latino | (37), 0.007% | (15), 1.0% | (22), 0.6% |
| Asian | (5), 0.1% | (2), 0.1% | (3), 0.1% |
| White | (202), 4.0% | (71), 4.8% | (131), 3.7% |
| Mixed | (100), 2.0% | (28), 1.9% | (72), 2.0% |
| Other | (65), 1.3% | (21), 1.4% | (44), 1.2% |
| Education (n =5029) Did not complete 12th grade | (1120), 22.3% | (336), 22.8% | (784), 22.0% |
| 12th grade or high school graduate | (1736), 34.5 % | (557), 37.8% | (1179), 33.1% |
| Graduate Equivalency diploma (GED) | (251), 5.0% | (88), 6.0% | (163), 4.6% |
| Some college/technical school | (1182), 23.5% | (312), 21.2% | (870), 24.5% |
| Technical school graduate | (225), 4.5% | (44), 3.0% | (181), 5.1% |
| College graduate | (430), 8.6% | (111), 7.5% | (319), 9.0% |
| Graduate school | (85), 1.7% | (24), 1.6% | (61), 1.7% |
| Unemployment | (3470), 69.1 | (1077), 31.0% | (2393), 69.0% |
| (3470) Household monthly income in US$ (4880) 0–249 | (1104), 22.6% | (429), 29.9% | (675), 19.6% |
| 250–499 | (425), 8.7% | (118), 8.2% | (307), 8.9% |
| 500–999 | (1304), 26.7% | (353), 24.6% | (951), 27.6% |
| 1000–1999 | (1306), 26.8% | (317), 22.1% | (989), 28.7% |
| ≥ 2000 | (741), 15.2% | (218), 15.2% | (523), 15.2% |
Thirty-three percent of the participants of the sample (N=5063) met DSM-IV criteria for a current PTSD diagnosis, 43% met criteria for MDD, and 24% had both PTSD and MDD. Among those participants who met PTSD diagnosis criteria, 75% met criteria for MDD. Exploratory data analysis showed that serious life-threatening accidents (48.2%) were the most common form of trauma exposure followed by interpersonal violence such as witnessing violence between parents or caregivers (31.8%), being a victim of attack with a weapon (31.2%) and without a weapon (27.3%), and experiencing sexual assault before age 13 (24.8%). Approximately one fourth (26.9%) of the participants reported trauma exposure due to a natural disaster, 23.1% reported sudden life-threatening illness, and one out of five (21.1%) participants reported physical abuse during childhood. Other forms of trauma exposure were witnessing murder of family members or friends (13.6%), experiencing sexual assault between ages 13 to 17 (14.3%), and sexual assault after age 17 (11.5%).
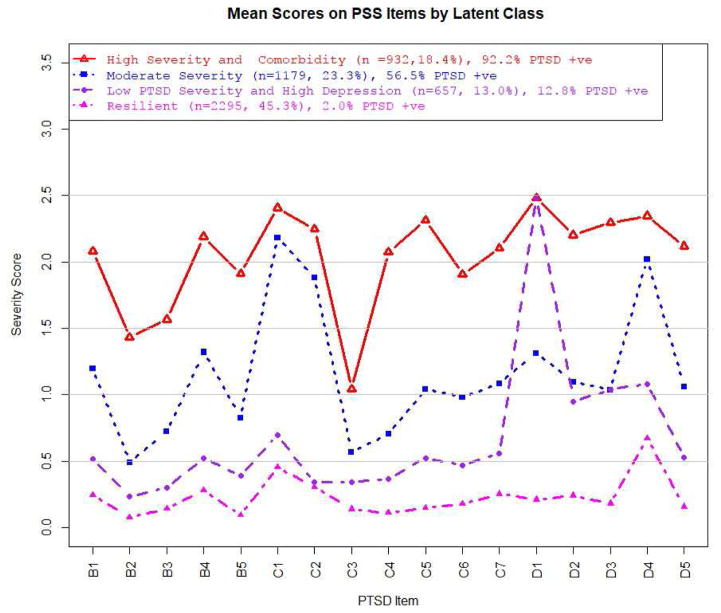
In order to assess model fit, we first examined traditional statistical methods BIC, log-likelihood, and gap-statistic (Table 2). Traditional statistical methods revealed latent subclasses of size two and three to be too small. Next, the Reproducibility Index was used to assess latent subclasses of size 4 – 9 (Table 2). The reproducibility index suggested latent subclasses of size 6 – 9 were too large and would lead to worse reproducibility and stability than smaller latent subclasses. Finally, we assessed interpretability of the latent subclasses for sizes four and five by plotting PTSD symptoms by severity score. The four latent subclass model showed a clear separation in symptom severity and PTSD diagnosis among the identified subclasses whereas the five latent subclass model did not. Thus, we selected the four latent subclass model because it was the most parsimonious, reproducible, and interpretable (Figure 1, Table 3).
Figure 1.
Mean Severity Scores on PSS Itemsa by Latent Subclasses
aB1:Intrusive memories, B2:Nightmares, B3:Flashbacks, B4:Psychologic reactivity, B5:Physiologic reactivity, C1:Avoid thinking, C2:Avoid activities, C3:Amnesia, C4:Diminished interest, C5:Detached, C6:Restricted affect, C7:Foreshortened future, D1:Insomnia, D2:Irritability, D3:Concentration problems, D4:Hypervigilance, D5:Exaggerated startle
Table 3.
PTSD, MDD, and both PTSD and MDD by Four Latent Subclasses
| Latent Subclass | Current PTSD | MDD | PTSD and MDD |
|---|---|---|---|
| High severity and comorbidity subclass (n =932, 18.4%) | 92.2% | 88.7% | 82.0% |
| Moderate severity subclass (n =1179, 23.3% ) | 56.5% | 53.9% | 34.5% |
| Low PTSD and high depression subclass (n=657, 13.0%) | 12.8% | 49.9% | 8.8% |
| Resilient subclass (n = 2295, 45.3%) | 2.0% | 16.4% | 0.6% |
The Four Latent Subclasses
Latent class analysis of the PSS questionnaire revealed four distinct latent subclasses of PTSD symptoms (Figure 1). To better understand differences between the four latent subclasses, mean PSS scores by item, depression, and exposure to lifetime and childhood trauma were assessed.
Subclass 1 - High Severity and Comorbidity
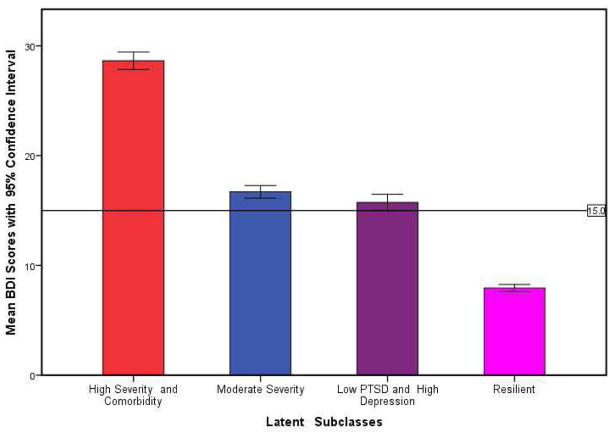
Subclass 1 (n=932, 18.4%) had the highest mean score for all PSS symptoms compared to the other subclasses. Subclass 1 also had the highest mean BDI score indicating, on average, subjects in this subclass were more depressed (Figure 2). Current PTSD and MDD diagnostic status revealed Subclass 1 to have higher rates of PTSD, MDD, and comorbid PTSD and MDD (95.2% PTSD, 88.7% MDD, and 82.0% both, Table 3). Due to the high mean scores of PSS items and high comorbidity of PTSD and MDD diagnosis, Subclass 1 was named high severity and comorbidity subclass.
Figure 2.
Mean with 95% Confidence Interval of Depression (BDI) Scores by Latent Subclasses
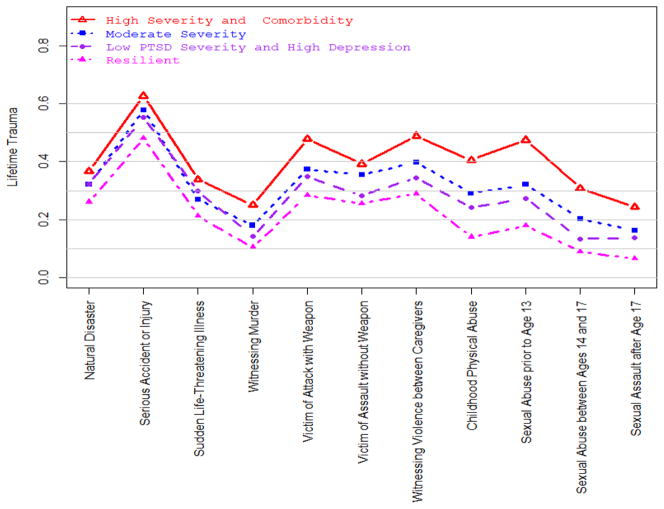
The TEI was used to assess the proportion of subjects in each subclass that experienced eleven specific types of lifetime traumas (Figure 3). For every type of trauma, the high severity and comorbidity subclass had the highest proportion of subjects that experienced that trauma. The largest differences were seen for childhood physical abuse and sexual abuse prior to age 13. The CTQ showed the mean score for the 5 types of childhood trauma (sexual abuse, physical abuse, emotional abuse, emotional neglect, and physical neglect) were also highest for the high severity and comorbidity subclass (Table 5). The results of the TEI and CTQ suggest the high severity and comorbidity subclass experienced the greatest amount of trauma. Significantly higher rates of inter-personal trauma exposure (witnessing violence, victim of attack with weapon, physical and sexual abuse) in the high severity and comorbidity subclass may help explain the high comorbidity between PTSD and MDD (p < 0.040).
Figure 3.
Proportion of Subjects Within each of the Four Latent Subclasses Experienced Different
Table 5.
Trauma (CTQ) Exposure Among the Four Latent Subclasses
| # Times Traumatic Event Occurs | Anova Results | |||||
|---|---|---|---|---|---|---|
|
|
||||||
| Childhood Trauma Type | 1:High severity and comorbidity PTSD (n=932) | 2:Moderate severity PTSD (n=1179) | 3:Low PTSD and high depression PTSD (n=657) | 4:Resilient PTSD (n=2295) | ||
| Ma (SD) | M (SD) | M (SD) | M (SD) | Overall F(df), P-value | Pairwise Comparisons | |
| Sexual Abuse | 10.88 (6.65) | 8.61 (5.42) | 7.69 (4.84) | 6.87 (4.08) | 139.52 (3, 5020), p < 0.001 | 1 > 2 > 3 > 4 |
| Physical Abuse b | 10.48 (5.29) | 8.76 (4.17) | 8.27 (3.88) | 7.28 (3.00) | 148.36 (3, 5020), p < 0.001 | 1 > 2 > 4,1 > 3 > 4 |
| Emotional Abuse | 12.70 (5.91) | 10.08 (4.93) | 8.90 (4.59) | 7.54 (3.66) | 285.65 (3, 5020), p < 0.001 | 1 > 2 > 3 > 4 |
| Emotional | 12.21 (6.08) | 10.22 (5.15) | 9.27 (4.90) | 8.14 (4.23) | 154.55 (3, 5020), p < 0.001 | 1 > 2 > 3 > 4 |
| Physical Negligence c | 8.63 (4.15) | 7.34 (3.24) | 6.77 (2.81) | 6.51 (2.69) | 101.24 (3, 5020), p < 0.001 | 1 > 2 > 3,1 > 2 > 4 |
M= mean, SD = standard deviation
Moderate severity and low PTSD and high depression subclasses differ marginally, p-value =0.051
Moderate severity and low PTSD and high depression subclasses do not differ significantly, p-value =0.23
Subclass 2 - Moderate Severity
Subclass 2 (n=1179, 23.3%) had the second highest means score on all PSS items, except for insomnia, compared to subclasses 3 and 4. Avoidance and hyper-vigilance symptoms were more severe than the other symptoms experienced by this subclass. BDI showed subjects to experience, on average, mild mood disturbances to borderline clinical depression (M = 16.81, SD = 10.02) (Figure 2). Approximately half of the subjects met current diagnosis for PTSD and MDD separately and approximately 30% were diagnosed with both (Table 3). Subclass 2 was termed moderate severity subclass due to the moderate mean PSS scores, PTSD diagnosis, and MDD diagnosis.
The moderate severity subclass had the second highest proportion of subjects that experienced the lifetime traumas assessed by the TEI. Two exceptions were ‘Natural Disaster’ and ‘Sudden Life-Threatening Illness’. CTQ showed the mean scores for each type of childhood trauma was second highest for the moderate severity subclass (Table 5).
Subclass 3 - Low PTSD and High Depression
Mean scores on all PSS items for subclass 3 (n=657, 13.0%) were lower than subclasses 1 and 2 and higher than subclass 4. The one exception was insomnia. Interestingly, subclass 3’s mean score for insomnia was almost equal to the high severity and comorbidity subclass. While mean PSS symptoms for subclass 3 were, with the exception of insomnia, lower than the moderate severity subclass, there was not a significant difference in BDI scores (p = 0.99). The depression experienced in subclass 3 (M = 15.93, SD = 9.60) was approximately equal to that of the moderate severity subclass (M = 16.81, SD = 10.02). Current diagnosis of PTSD, MDD, and comorbid PTSD and MDD revealed subjects had similar rates of MDD to the moderate severity subclass but lower PTSD and comorbidities (Table 3). Hence, subclass 3 was denoted as low PTSD and high depression.
Low PTSD and high depression had the third highest proportion of subjects that experienced all TEI items with the exception of ‘Natural Disaster’ and ‘Sudden Life-Threatening Illness’. There was not a significant difference in proportion that experienced ‘Natural Disaster’ between the moderate severity and low PTSD and high depression subclasses (p = 0.95). The low PTSD and high depression subclass had a higher proportion of subjects that experienced ‘Sudden Life-Threatening Illness’ than moderate severity, but the difference was not statistically significant (p = 0.19). The difference in proportion that experienced ‘Sudden Life-Threatening Illness’ was also not significantly different compared to the high severity and comorbidity subclass (p = 0.18). Mean CTQ scores for all trauma types were lower than the high severity and comorbidity and moderate severity subclasses. There was not a significant difference in mean childhood physical abuse and physical neglect between the moderate severity and low PTSD and high depression subclasses (Table 5). These results suggest a large proportion of trauma exposed subjects did not experience PTSD or depression.
Subclass 4 - Resilient
Subclass 4 (n=2295, 45.3%) had the lowest mean severity score for all PSS items. In addition, the mean BDI score for subclass 4 was significantly lower than the other 3 subclasses (p < 0.001). Current PTSD, MDD, and both PTSD and MDD diagnoses were low (2.0%, 16.4%, and 0.6%, respectively). Due to the low mean PSS scores and depression, subclass 4 was termed the resilient subclass.
The resilient subclass had the lowest proportion of people experience the eleven types of lifetime trauma that were assessed. The resilient subclass had the lowest mean scores for all childhood trauma types. There was not a significant difference in mean scores for childhood physical neglect between the low PTSD and high depression and resilient subclasses.
Demographic Information Across Latent Subclasses
Demographic information of the study participants across the four subclasses is given in Table 4. Chi-squared tests showed gender, race, unemployment rate, education, and income differed across the four latent subclasses (p ≤ 0.010). Multiple pairwise comparison revealed gender only differed between moderate severity and resilient subclasses (p < 0.030). Unemployment rate was significantly higher for the high severity and comorbidity subclass than the other three subclasses (p < 0.001).
Table 4.
Demographic Information Across PTSD Symptoms Subclasses
| Subclasses of PSS Symptom
|
|||||
|---|---|---|---|---|---|
| Demographic | High severity and comorbidity (n=932) | Moderate severity (n=1179) | Low PTSD and high depression (n=657) | Resilient (n=2295) | Chisq p-value |
| Sex (Female, %) | 72.4% | 73.0% | 72.2 % | 68.4% | χ2(3) = 10.5, p = 0.010 |
| Race (AA a, % ) | 89.9% | 91.5% | 91.3% | 93.5 % | χ2(15) = 35.8, p < 0.001 |
| Unemployment (%) | 79.6% | 69.3% | 72.0% | 63.8% | χ2(3) = 80.10, p < 0.001 |
| Age (M, SD b ) | 41.29 (11.79) | 39.17 (13.24) | 42.96 (13.14) | 40.67 (14.35) | F(3, 5032) = 11.40, p < 0.001 |
| Education (%) | |||||
| L12 c | 28.2 % | 22.3% | 19.9% | 20.5% | |
| H12 d | 30.4 % | 34.2% | 34.6% | 36.3% | |
| GED e | 7.5 % | 6.3% | 4.6% | 3.4% | |
| CT f | 21.2% | 24.2% | 24.5% | 23.8% | χ2(18) = 76.1, p < 0.001 |
| TSG g | 5.4% | 3.6% | 5.4% | 4.3% | |
| CG h | 6.3 % | 7.4% | 9.6% | 9.7% | |
| GS l | 1.0 % | 2.0 | 1.4% | 1.9% | |
| Income ($, %) | |||||
| 0–249 | 31.6% | 21.0% | 22.3% | 19.8% | |
| 250–499 | 8.5% | 9.6% | 8.1% | 8.5% | |
| 500–999 | 28.0% | 28.1% | 25.0% | 26.0% | χ2(12) = 81.5, p < 0.001 |
| 1000–1999 | 21.8% | 26.7% | 28.4% | 28.3% | |
| ≥ 2000 | 9.9% | 14.6% | 16.1% | 17.4% | |
African American
M= Mean, SD= standard deviation
Did not complete 12th grade
Completed 12th grade or high school graduate
Graduate equivalence diploma
Some college/technical school
Technical school graduate
College graduate
Graduate school
Discussion
In this study, we conducted a latent class analysis (LCA) using 17 PTSD symptoms, measured by the PSS questionnaire, for 5063 trauma exposed subjects. LCA suggested four subclasses of PTSD symptom severity: (1) High severity and comorbidity , (2) Moderate severity, (3) Low PTSD and high depression, and (4) Resilient.
The high severity and comorbidity subclass reported the most severe PTSD symptoms (including avoidance, hyper-vigilance, and insomnia) and had the highest percentage of participants that met both PTSD and MDD diagnostic criteria. This subclass reported the highest levels of exposure to adult and childhood traumas. The largest difference in proportion of traumas experienced compared to the other subclasses appears to be childhood physical abuse and sexual abuse before age 13. Further investigating childhood trauma in this subclass may aide in understanding the comorbidity of PTSD and MDD.
The moderate severity subclass reported the second highest PTSD symptom severity. The symptoms avoid thinking, avoid activities, and hyper-vigilance were prominent in this subclass compared to other symptoms. Approximately half of the subjects in this subclass met current PTSD or MDD diagnosis of which 34.5% met both. Avoiding thinking, social activities, and hyper-vigilance may be key symptoms to target persons at higher risk for developing PTSD.
The low PTSD and high depression subclass reported low symptom severity for all PTSD symptoms, except insomnia. Furthermore, only 12.8% of the subclass met current PTSD diagnosis whereas 49.9% met MDD diagnosis. Symptom severity reported for insomnia was similar to that of the high severity and comorbidity subclass and significantly lower than the moderate severity subclass.
Subjective reports of sleep disturbance (insomnia) have indicated that 70–91% of patients with PTSD had difficulty falling or staying asleep (Maher et al., 2006). Furthermore, evidence suggests people that experience insomnia have a ten-fold risk of developing depression compared with those who sleep well (Taylor et al., 2005). High symptom severity of insomnia in the high severity and comorbidity subclass supports previous findings effect of insomnia on PTSD and depression. The difference in insomnia severity and current diagnosis of PTSD and MDD in the moderate severity versus low PTSD and high depression subclasses is of particular interest. The moderate severity subclass had significantly lower severity scores on insomnia compared to the low PTSD and high depression subclass. However, there was not a significant difference in people meeting current MDD diagnosis. These results indicate insomnia may be an important symptom for MDD in persons that do not meet PTSD diagnosis, such as in the low PTSD and high depression subclass. From the moderate severity subclass we see that high symptom severity for insomnia is not crucial for MDD. However, avoidance and hyper-vigilance symptom severity is high for this class, similar to the high severity and comorbidity subclass, which may indicate the importance of these symptoms in persons that develop PTSD.
Future research should focus on better understanding insomnia, avoiding thinking, avoiding activities, and hyper-vigilance. The goal is to better understand how these symptoms relate to current PTSD and MDD diagnosis. By understanding these symptoms, we may become better equipped to target persons at high risk of developing PTSD, MDD, or both.
Strengths of the study include a large civilian dataset with detailed information on PTSD symptoms, depression, and traumas experienced in childhood and adulthood. The application of rigorous statistical methods to identify subclasses of PTSD symptoms is another strength. One of the limitations of this study is the absence of treatment to further validate subclasses by responses to treatments as this is a cross-sectional study. A large longitudinal study with treatment or clinical courses could facilitate further evaluation of the latent subclasses. The study is also limited by the use of self-report measures and retrospective reports of childhood trauma (CTQ). Several studies have found strong convergence between the CTQ and more objective measures of abuse (Carpenter et al., 2011; Hyman et al., 2005). Finally, the dataset was comprised primarily of African American subjects with low socioeconomic status. While these data may not generalize to all traumatized populations, they are representative of other large urban samples (Alim et al., 2006b), which have been understudied in PTSD research.
Acknowledgments
Source of Funding
This research is supported by the U.S. National Institutes of Health (NIH) grant 5R01 MH079448-06, MH098212, MH092576, and HHMI. The content is solely the responsibility of the authors and does not necessarily represent the official views of NIH.
Footnotes
Conflicts of Interest:
The authors have no financial disclosures to make or no conflict of interests to report.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Abram K, Teplin L, Charles D, Longworth S, McClelland G, Dulcan M. Posttraumatic stress disorder and trauma in youth in juvenile detention. Archives of General Psychiatry. 2004;61(4):403–410. doi: 10.1001/archpsyc.61.4.403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alim TN, Charney DS, Mellman TA. An overview of posttraumatic stress disorder in african americans. Journal of Clinical Psychology. 2006a;62(7):801–813. doi: 10.1002/jclp.20280. [DOI] [PubMed] [Google Scholar]
- Alim TN, Graves E, Mellman TA, Aigbogun N, Gray E, Lawson W, Charney DS. Trauma exposure, posttraumatic stress disorder and depression in an african-american primary care population. Journal of the National Medical Association. 2006b;98(10):1630–1636. [PMC free article] [PubMed] [Google Scholar]
- Bakk Z, Tekle FB, Vermunt JK. Estimating the association between latent class membership and external variables using bias-adjusted three-step approaches. Sociological Methodology. 2013;43(1):272–311. [Google Scholar]
- Baudry JP, Raftery AE, Celeux G, Lo K, Gottardo R. Combining mixture components for clustering. J Comput Graph Statist. 2010;19(2):332–353. doi: 10.1198/jcgs.2010.08111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck A, Ward C, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of General Psychiatry. 1961;4(6):561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Bernstein D, Fink L. Childhood Trauma Questionnaire: A Retrospective Self-report. Harcourt Brace & Company; 1998. [Google Scholar]
- Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, Stokes J, Handelsman L, Medrano M, Desmond D, Zule W. Development and validation of a brief screening version of the childhood trauma questionnaire. Child Abuse and Neglect. 2003;27(2):169– 190. doi: 10.1016/s0145-2134(02)00541-0. [DOI] [PubMed] [Google Scholar]
- Bremner J, Southwick S, Brett E, Fontana A, Rosenheck R, Charney D. Dissociation and posttraumatic stress disorder in vietnam combat veterans. Am J Psychiatry. 1992;149(3):328–32. doi: 10.1176/ajp.149.3.328. [DOI] [PubMed] [Google Scholar]
- Breslau N, Kessler R, Chilcoat H, Schultz L, Davis G, Andreski P. Trauma and posttraumatic stress disorder in the community: The 1996 detroit area survey of trauma. Archives of General Psychiatry. 1998;55(7):626–632. doi: 10.1001/archpsyc.55.7.626. [DOI] [PubMed] [Google Scholar]
- Breslau N, Reboussin B, Anthony J, Storr C. The structure of posttraumatic stress disorder: Latent class analysis in 2 community samples. Archives of General Psychiatry. 2005;62(12):1343–1351. doi: 10.1001/archpsyc.62.12.1343. [DOI] [PubMed] [Google Scholar]
- Byrne CA, Resnick HS, Kilpatrick DG, Best CL, Saunders BE. The socioeconomic impact of interpersonal violence on women. Journal of Consulting and Clinical Psychology. 1999;67(3):362–366. doi: 10.1037//0022-006x.67.3.362. [DOI] [PubMed] [Google Scholar]
- Carpenter LL, Shattuck TT, Tyrka AR, Geracioti TD, Price L. Effect of childhood physical abuse on cortisol stress response. Psychopharmacology. 2011;214(1):367–375. doi: 10.1007/s00213-010-2007-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cloitre M, Garvert DW, Brewin CR, Bryant RA, Maercker A. Evidence for proposed icd-11 ptsd and complex ptsd: a latent profile analysis. European Journal of Psychotraumatology. 2013;4(20706) doi: 10.3402/ejpt.v4i0.20706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cloitre M, Garvert DW, Weiss B, Carlson EB, Bryant RA. Distinguishing ptsd, complex ptsd, and borderline personality disorder: A latent class analysis. European Journal of Psychotraumatology. 2014;5(25097) doi: 10.3402/ejpt.v5.25097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craven J, Rodin G, Littlefield C. The beck depression inventory as a screening device for major depression in renal dialysis patients. Int J Psychiatry Med. 1988;18(4):365–74. doi: 10.2190/m1tx-v1ej-e43l-rklf. [DOI] [PubMed] [Google Scholar]
- Dohrenwend B, Turner J, Turse N, Adams B, Koenen KC, Marshall R. The psychological risks of vietnam for u.s. veterans: A revisit with new data and methods. Science (New York, NY) 2006;313(5789):979–982. doi: 10.1126/science.1128944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foa EB, Riggs DS, Dancu CV, Rothbaum BO. Reliability and validity of a brief instrument for assessing post-traumatic stress disorder. Journal of Traumatic Stress. 1993;6(4):459–473. [Google Scholar]
- Foa EB, Tolin DF. Comparison of the ptsd symptom scale-interview version and the clinician-administered ptsd scale. Journal of Traumatic Stress. 2000;13(2):181–191. doi: 10.1023/A:1007781909213. [DOI] [PubMed] [Google Scholar]
- Fraley C, Raftery AE. Model-based clustering, discriminant analysis, and density estimation. J Amer Statist Assoc. 2002;97(458):611–631. [Google Scholar]
- Fraley C, Raftery AE, Murphy TB, Scrucca L. Technical Report No 597. 597 Department of Statistics, University of Washington; 2012. mclust version 4 for r: Normal mixture modeling for model-based clustering, classification, and density estimation. [Google Scholar]
- Fullilove M, Hon V, Jimenez W, Parsons C, Green L, Fullilove R. Injury and anomie: effects of violence on an inner-city community. American Journal of Public Health. 1998;88(6):924–927. doi: 10.2105/ajph.88.6.924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillespie CF, Bradley B, Mercer K, Smith AK, Conneely K, Gapen M, Weiss T, Schwartz AC, Cubells JF, Ressler KJ. Trauma exposure and stress-related disorders in inner city primary care patients. General hospital psychiatry. 2009;31(6):504–14. doi: 10.1016/j.genhosppsych.2009.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyman SM, Garcia M, Kemp K, Mazure CM, Sinha R. A gender specific psychometric analysis of the early trauma inventory short form in cocaine dependent adults. Addictive Behaviors. 2005;30(4):847– 852. doi: 10.1016/j.addbeh.2004.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang HK, Natelson BH, Mahan CM, Lee KY, Murphy FM. Post- traumatic stress disorder and chronic fatigue syndrome-like illness among gulf war veterans: a population-based survey of 30,000 veterans. American Journal of Epidemiology. 2003;157(2):141–148. doi: 10.1093/aje/kwf187. [DOI] [PubMed] [Google Scholar]
- Kessler R, Sonnega A, Bromet E, Hughes M, Nelson C. Posttraumatic stress disorder in the national comorbidity survey. Archives of General Psychiatry. 1995;52(12):1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Kulka RA, Schlenger WE, Fairbank JA, Hough RL, Jordan BK, Marmar CR, Weiss DS. Trauma and the Vietnam war generation: Report of findings from the National Vietnam Veterans Readjustment Study. Brunner/Mazel; 1990. [Google Scholar]
- Magidson J, Vermunt J. Latent class models for clustering: A comparison with k-means. Canadian Journal of Marketing Research. 2002;20:37–44. [Google Scholar]
- Maher M, Rego S, Anis G. Sleep disturbances in patients with post-traumatic stress disorder: epidemiology, impact and approaches to management. CNS Drugs. 2006;20(7):567–590. doi: 10.2165/00023210-200620070-00003. [DOI] [PubMed] [Google Scholar]
- McLachlan G, Peel D. Finite mixture models. Wiley-Interscience; New York: 2000. Wiley Series in Probability and Statistics: Applied Probability and Statistics. [Google Scholar]
- Nugent NR, Koenen KC, Bradley B. Heterogeneity of posttraumatic stress symptoms in a highly traumatized low income, urban, african american sample. Journal of Psychiatric Research. 2012;46(12):1576–1583. doi: 10.1016/j.jpsychires.2012.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nylund KL, Asparouhov T, Muthén BO. Deciding on the number of classes in latent class analysis and growth mixture modeling: a Monte Carlo simulation study. Struct Equ Model. 2007;14(4):535–569. [Google Scholar]
- Schwartz A, Bradley R, Ressler K, Sexton M, Sherry A. Treating posttraumatic stress disorder in urban african american mental health patients. J Amer Psychoanal Assn. 2004;52(2):464–465. [PubMed] [Google Scholar]
- Schwartz AC, Bradley RL, Sexton M, Sherry A, Ressler KJ. Posttraumatic stress disorder among african americans in an inner city mental health clinic. Psychiatric Services. 2005;56(2):212–215. doi: 10.1176/appi.ps.56.2.212. [DOI] [PubMed] [Google Scholar]
- Schwarz G. Estimating the dimension of a model. Ann Statist. 1978;6(2):461–464. [Google Scholar]
- Steuwe C, Lanius RA, Frewen PA. Evidence for a dissociative subtype of ptsd by latent profile and confirmatory factor analyses in a civilian sample. Depression and Anxiety. 2012;29(8):689–700. doi: 10.1002/da.21944. [DOI] [PubMed] [Google Scholar]
- Tanielian T, Jaycox LH. Invisible wounds of war. Rand Corporation; 2008. pp. 1–66. [Google Scholar]
- Taylor D, Lichstein K, Durrence H, Reidel B, Bush A. Epidemiology of insomnia, depression, and anxiety. Sleep. 2005;28(11):1457–1464. doi: 10.1093/sleep/28.11.1457. [DOI] [PubMed] [Google Scholar]
- Tibshirani R, Walther G, Hastie T. Estimating the number of clusters in a data set via the gap statistic. J R Stat Soc Ser B Stat Methodol. 2001;63(2):411–423. [Google Scholar]
- Wolf E, Miller M, Reardon A, Ryabchenko K, Castillo D, Freund R. A latent class analysis of dissociation and posttraumatic stress disorder: Evidence for a dissociative subtype. Archives of General Psychiatry. 2012;69(7):698–705. doi: 10.1001/archgenpsychiatry.2011.1574. [DOI] [PMC free article] [PubMed] [Google Scholar]