Abstract
Approximately, 50% of human melanomas are driven by BRAF mutations, which produce tumors that are highly immunosuppressive and often resistant to vaccine therapy. We introduced lipid-coated calcium phosphate nanoparticles (LCP NPs) as a carrier to efficiently deliver a tumor-specific antigen, the BRAFV600E peptide, to drive dendritic cell (DC) maturation and antigen presentation in C57BL6 mice. The BRAF peptide vaccine elicited a robust, antigen-specific cytotoxic T cell response and potent tumor growth inhibition in a murine BRAF-mutant melanoma model. Advanced BRAF-specific immune response was illustrated by IFN-γ production assay and cytotoxic T lymphocyte (CTL) assay. Remodeling of immunosuppressive modules within the tumor microenvironment further facilitated CTL infiltration. Thus, using LCP NPs to deliver the BRAF peptide vaccine is a promising strategy for the BRAF-mutant melanoma therapy.
Keywords: BRAF-mutant melanoma, Peptide vaccine, Immunotherapy, Nanoparticles
Introduction
Melanoma is one of the most common forms of skin cancer, with an estimated 76,380 new cases in the USA in 2016 [1]. It accounts for nearly 80% of skin cancer deaths. Despite recent improvements in prevention and early detection, approximately 20% of melanoma patients still die from the disease. Early stage melanoma is curable by surgical resection, but metastasis results in poor prognosis; 5-year survival rates drop from 98 to 17% once melanoma metastasizes. This is largely because metastatic malignancy is refractory to conventional therapies. Hence, new treatment therapies are necessary [2].
Recent advances in immunology and cancer biology, including a better understanding of signaling pathways in cancer progression, have promoted cancer immunotherapy as a new way of halting growth and metastasis [3, 4]. Cancer immunotherapy harnesses the patient’s immune system to combat cancers. The therapy primarily depends on tumor-associated antigens, which are overexpressed during malignant tumor cell development. The immune system is manipulated to recognize tumor-associated antigens and raise a specific immune response against the cancer cells. The typical strategy is to generate a large number of antigen-specific T cells to battle the tumor by using cancer vaccines [5].
A clinically significant event in the field was the identification of driver oncogenic mutations in the BRAF gene, which encodes a serine/threonine-protein kinase BRaf [6]. BRAF inhibitors have been largely studied as clinical therapeutics in BRAF-mutant cancers. The major efficacy of BRAF inhibitors results from BRAF/MEK/ERK signaling inhibition. Vemurafenib and dabrafenib are two structurally unrelated BRAF inhibitors that selectively target V600E, a missense mutation in BRAF. These BRAF inhibitors increased disease-free survival and overall survival (OS), leading to their regulatory approval in 2011 and 2013, respectively [7, 8]. Combined inhibition of BRAF and MEK can reduce disease progression risk by 25% and delay development of resistance compared with BRAF inhibition alone, but cannot prevent emergence [9].
Notably, 50% of human melanomas are driven by BRAF mutations, among which BRAFV600E mutation is the major common one, characterized by aggressive growth and a highly immunosuppressive tumor microenvironment (TME). These tumors are often resistant to immune vaccination therapy [10]. Therefore, inducing a BRAF-mutation-specific and potent T cell response to endogenous antigens remains challenging. The murine BRAFV600E mutant peptide (mBRAF 594-602: FGLANEKSI) for the C57Bl/6 haplotype (H2Db) was designed by modifying amino acids at the 5 and 9 positions to increase binding affinity using the Rammensee epitope prediction model [11]. A previous report on type 1-polarized DCs pulsed with affinity-modified BRAFV600E peptide showed antigen-specific CD8 + T cell responses [12], supporting mutated BRAF as a potential immune system target. However, cell-based vaccination is both costly and less reproducible compared with an injectable chemical dosage of nano-formulation for targeted delivery to the draining LNs. In this study, we aimed to use a BRAF-mutant melanoma in a syngeneic mouse model to study tumor growth inhibition using a tumor-specific BRAF peptide vaccine delivered by DC-targeting nanoparticles (NPs).
Our lab has established a nano-formulation called lipid-calcium-phosphate (LCP) NPs for delivering nucleic acids, peptides, and chemotherapeutic drugs [13, 14]. The NP core, supported by lipid bilayers, may offer efficient encapsulation and delivery of acid and peptides. Injected NPs must overcome both kinetic and physical barriers after administration. This is especially true for peptides and nucleic acids. After the NP formulation is administered, it must protect the cargo molecules from enzymatic degradation by endogenous nucleases. It should also avoid aggregation, which can be accomplished by PEGylation. The BRAF peptide, along with CpG oligodeoxynucleotides (ODN) adjuvant, was formulated in LCP NPs with mannose modification and delivered to the DCs in the LNs. This approach was very effective in inducing an antigen-specific cytotoxic T lymphocyte (CTL) response in the host and significantly inhibited primary BRAF-mutant melanoma growth. Variations in the extent to infiltrated suppressive leukocytes and T cells within the TME were also monitored after vaccination. The simple but sophisticated LCP NP design is an effective vaccine platform with great translational potential. The BRAF peptide vaccine, which has both MHC-I and HLA-restricted properties, acts as a potent immunotherapy for BRAF-mutant melanoma.
Materials and Methods
Materials
Dioleoylphosphatydic acid (DOPA), (±)-N,N,N-trimethyl-2,3-bis(z-octadec-9-ene-oyloxy)-1-propanaminium chloride (DOTAP), 1,2-distearoyl-sn-glycero-3-phosphoethanolamine-N-[amino(polyethylene glycol)-2000 (DSPE-PEG-2000), and 3-(N-succinimidyloxyglutaryl)aminopropyl, polyethyleneglycol-carbamyl distearoylphosphatidyl-ethanolamine (DSPE-PEG-NHS) were purchased from Avanti Polar Lipids (Alabaster, AL). H-2Db-restricted peptides original BRAFV600E (FGLANEKSI), BRAFWT (FGLANVKSI), modified BRAFV600E peptide (pSpSSFGLANEKSI), and control peptide OVA (SIINFEKL) were purchased from Peptide 2.0 (Chantilly, VA). PEG-DSPE-Mannose was synthesized from DSPE-PEG-NHS and 4-Amino phenyl-mannopyranoside. CpG ODN 1826 (5′-TCCATGACGTTCCTGACGTT-3′) and Cy5-labeled ODN (5′-CAAGGGACTGGAAGGCTGGG-3′) were purchased from Sigma Aldrich (St. Louis, MO).
Cell lines
Murine BRAF-mutant melanoma cell line BPD6 (BRAFV600E, PTEN−/−, syngeneic with C57BL/6) was obtained from Brent Hanks (Duke Cancer Institute, Durham, NC) and cultivated in RPMI-1640 Medium (Invitrogen, Carlsbad, CA) supplemented with 10% FBS (Invitrogen) and 1% Penicillin/Streptomycin (Invitrogen) at 37 °C and 5% CO2.
Preparation and Characterization of Vaccine Formulation
The LCP NP was synthesized in a water-in-oil reverse micro-emulsion [15]. Ca phase was formed by mixing 600 μL of 2.5 M CaCl2 with or without peptide and/or CpG ODN in a 20 mL Cyclohexane/Igepal CO-520 (71:29, V: V) solution (oil phase). The oil phase was formed by mixing 600 μL of 12.5 mM Na2HPO4 (pH 9.0). We stirred both phases for 5 min then added 400 μL of 20 mM DOPA for 25 min. We then added 40 mL of ethanol and collected cores by centrifugation. Ethanol washes were followed before collection of the cores. Final LCP NPs were formed by mixing 1 mL CaP cores, 100 μL of 20 mM DOTAP, 100 mL cholesterol, 10 mL DSPE-PEG-2000, and 10 μL DSPE-PEG-mannose. After removal of chloroform under reduced pressure, final particles were dispersed in 100 μL of 5% glucose. Transmission electron microscopy (JEOL 100CX II TEM, JEOL, Japan) was used for particle characterization. Particle size and zeta potential were measured with a Malvern Zetasizer Nano ZS in water (Malvern, United Kingdom). DC accumulation of DSPE-PEG-mannose-modified LCP NPs in the draining LNs was investigated by using LCP NPs containing a Cy5-labeled oligonucleotide and flow cytometry analysis of NP uptake in CD11c+ DCs.
Tumor growth inhibition
Female C57BL/6 mice (6–8 weeks old) were purchased from Charles River Laboratories (Wilmington, MA). All animal studies were approved by the IACUC Committee at the University of North Carolina at Chapel Hill (UNC). On day 0, mice were inoculated subcutaneously with 1 × 106 BPD6 cells on their lower flank. Once the tumor volume reached approximately 50 mm3 (0.5 × length × width × height), mice were then randomized into five groups (n = 5–7) as follows: Untreated group (PBS group), Empty LCP NP (Empty group), CpG LCP NPs (CpG group), BRAF LCP NPs (BRAF group), and BRAF + CpG LCP NPs (BRAF + CpG group). Vaccination with LCP NPs was performed on day 10. We monitored tumor size (using digital calipers) and animal weight every 2–3 days. Mice were killed before tumors reached 20 mm in one dimension. At the endpoint, tumors, major organs, and blood samples were harvested and tested. We evaluated anti-tumor efficacy by comparing relative tumor volume (RTV) value and therapeutic group/control group (T/C) ratio. RTV = V t/V 0, V t and V 0 represent the tumor volume measured at each time point interval and Day 0. T/C (%) = RTV of therapeutic group/RTV of control group × 100%. T/C ≤ 42%, active, T/C ≤ 10%, highly active.
In vivo CTL assay
In vivo CTL was conducted per a previously published protocol [16]. Mice were vaccinated with different formulations on the lower flank. Seven days later, the mice were intravenously injected with a mix of 5 × 106 splenocytes, half of which were pulsed by BRAFV600E peptide (10 μM), while the other half were pulsed by OVA peptide (10 μM). The BRAFV600E pulsed cells were labeled with 4 μM carboxyfluorescein succinimidyl ester (CFSE) and OVA-pulsed cells with 0.4 μM CFSE. These two population were referred to as CFSEhigh (BRAFV600E pulsed cells) and CFSElow (OVA-pulsed cells). After 18 h, splenocytes were collected and analyzed by flow cytometry. CFSEhigh and CFSElow, as well as in vivo BRAFV600E specific lysis, were calculated [17]. The experiments were conducted in triplicate. Specific lysis was calculated as follows:
where from naive mice.
ELISPOT assay for IFN-γ production
Mice were vaccinated with different formulations of treatment. Seven days later, spleen and draining LNs were collected into single cells and seeded on the capture antibody-coated 96-well plate. IFN-γ production was measured with BD™ ELISPOT assay system (BD Pharmingen, San Diego, CA) as per the manufacturer’s instructions [18].
Flow cytometry assay
Immune cell populations were analyzed by flow cytometry. Briefly, tumor tissues or LNs were collected using collagenase A at 37 °C for 40-50 min. Single cells were harvested in PBS and stained with fluorescein-conjugated antibodies. Penetration buffer (BD, Franklin Lakes, NJ) was added for any intracellular cytokine staining.
Immunofluorescence staining
Staining was performed following tissue deparaffinization, antigen retrieval, permeabilization, and BSA blocking. Primary and secondary antibodies conjugated with fluorophores (BD, Franklin Lakes, NJ) were incubated overnight at 4 °C. Cell nuclei were counterstained with DAPI (Vector Laboratories Inc., Burlingame, CA). Images were collected using fluorescence microscopy (Nikon, Tokyo, Japan) and analyzed using Image J software. Three fields were randomly selected.
TUNEL Assay
Assay performed following DeadEnd Fluorometric TUNEL System (Promega, Madison, WI) instructions [19] and imaged using fluorescence microscopy. Fluorescently stained FITC (green) positives were defined as TUNEL-positive nuclei. Three fields were randomly selected and quantified.
H&E morphology evaluation and blood chemistry analysis
At the endpoint of the tumor inhibition study, mice with different treatments were all subjected to toxicity assays. Both whole blood and serum were collected. We collected and compared whole blood cellular components and tested for indicators of renal and liver function such as creatinine, blood urea nitrogen (BUN), serum aspartate aminotransferase (AST), and alanine aminotransferase (ALT). Organs were collected and send out for H&E staining by UNC histology facility.
Statistical analysis
We used Prism 5.0 software to conduct one-way ANOVA and a two-tailed Student’s t test and compared the data with those for the PBS control group. p values less than 0.05 were considered significantly different.
Results
Affinity-modified BRAF peptide was readily packaged in LCP NPs
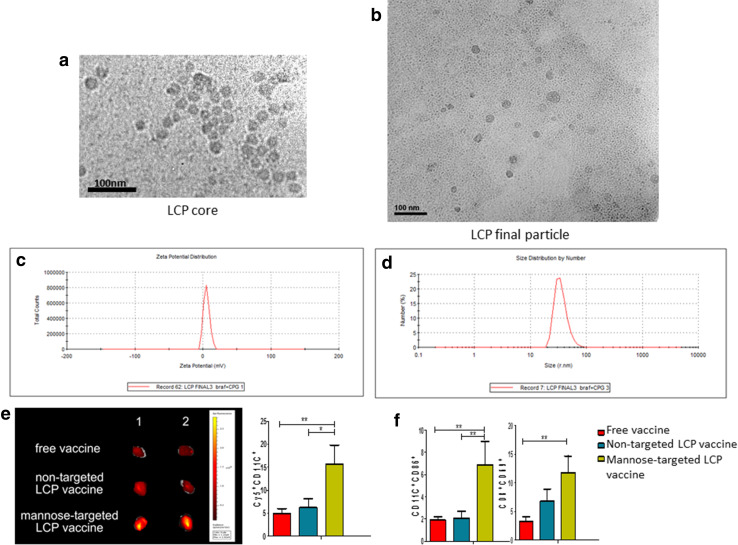
To achieve more efficient vaccination, we co-delivered NPs encapsulating both the tumor-specific antigen and a potent adjuvant to APCs. CpG ODN, a potent adjuvant, could be efficiently encapsulated in LCP NPs; this system was extensively characterized and optimized in our laboratory [20]. On N-terminal of the BRAF peptide, phosphorylated serine residues were designed to facilitate CpG ODN encapsulation. Once the CpG ODN was co-loaded in LCP NPs in a reverse oil-in-water micro-emulsion, amorphous calcium phosphate (CaP) precipitates were formed and then stabilized with DOPA. These so-called CORE particles were then coated with DOTAP/cholesterol and stabilized with DSPE-PEG and DSPE-PEG-mannose. The zeta potential, as determined by a Zetasizer, was approximately 15 mV, which was indicative of full PEGylation of the LCP NPs. Transmission electron microscope (TEM) images were taken to investigate the NP morphology and to confirm the size of the LCP NPs (Fig. 1a–d). The LCP NPs loaded with the modified BRAFV600E peptide and CpG were spherical with a diameter of approximately 30 nm after uranium acetate staining. The encapsulation efficiency was about 60% after optimization. Mannose modification achieved enhanced and prolonged accumulation of the NPs in the LNs, whereas the targeted delivery of NPs to draining LNs facilitated local DC activation (CD11c+CD86+), as well as local T cell activation (CD8+CD69+), thus boosting immune efficiency (Fig. 1e–f).
Fig. 1.
Characterization of the LCP NP-based BRAF peptide vaccine. LCP encapsulating the modified melanoma-specific antigen (BRAFV600E) and adjuvant (CpG ODN) illustrated efficient antigen loading and DC activation. Panels (a) and (b) show TEM images of NP cores and final structure. Size distribution (c) and Zeta potential (d) show NP characteristics. Cy5-labeled NPs show enhanced accumulation in draining LNs and uptake in proximal DCs (e) after mannose-modified LCP encapsulation, which facilitated local DC activation and T cell activation (f). n = 5, *p < 0.05, **p < 0. 01
BRAF peptide vaccine induced an antigen-specific immune response
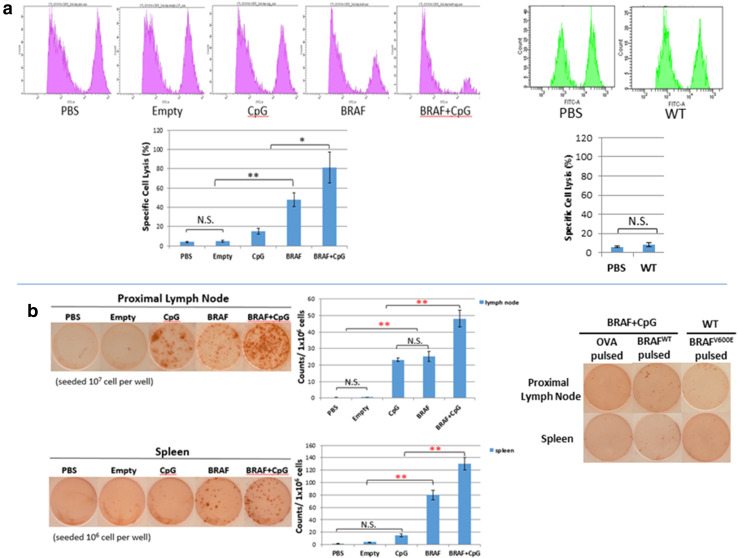
We proceeded to evaluate therapeutic efficacy in the murine BRAF-mutant melanoma syngeneic tumor model. CTLs are responsible for killing tumor cells, while IFN-γ-producing T cells secrete cytokines to modulate the TME. Therefore, an assay for antigen-specific CTL response measured how and how well the vaccine formulation worked, whereas assaying IFN-γ-producing T cells measured systemic T cell function upon antigen presentation [16, 18]. LCP NPs loaded with the modified tumor-specific BRAF-mutant peptide were subcutaneously inoculated in the flank of the mice. CTL assay and ELISPOT assay were performed 1 week later to examine the antigen-specific T cell response and IFN-γ production.
As shown in Fig. 2a, immunization with LCP NPs encapsulating the modified BRAF-mutant peptide or CpG ODN alone boosted modest (approximately 48%) efficacy, whereas vaccination with empty particles or NP encapsulating BRAFWT peptide (the wildtype (WT) group) showed no noticeable BRAF-mutant-specific CTL results. Only the combined group with tumor-specific peptide and adjuvant proved effective (approximately 80% efficacy), indicating robust BRAFV600E-specific responses.
Fig. 2.
Antigen-specific immune response induced by the BRAF peptide vaccine. a In vivo CTL response after vaccination, n = 5. b IFN-γ production after vaccination was measured with ELISPOT assay system. One representative experiment from each group is shown. n = 5, N.S. no significance, *p < 0.05, **p < 0. 01
Moreover, consistent with the CTL assay, we found no significant IFN-γ production of BRAFV600E-pulsed cells in the spleens or LNs of naïve mice or empty NP-vaccinated mice, indicating insufficient BRAFV600E-specific killing (Fig. 2b). Only full vaccination boosted IFN-γ release. OVA-pulsed or BRAFWT-pulsed cells for any group in the spleen or LN also showed no significant IFN-γ production.
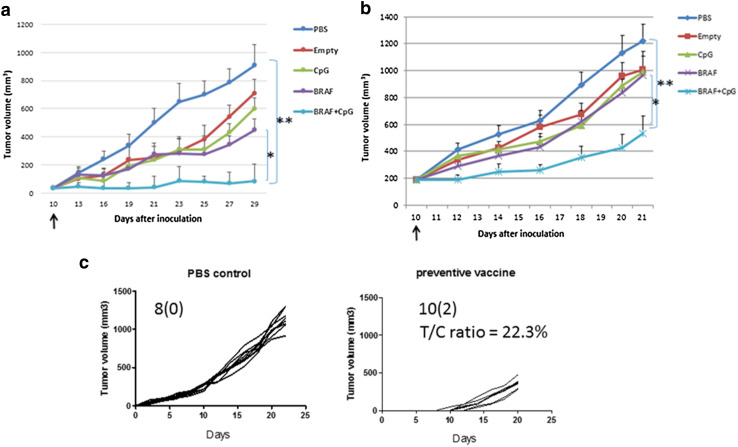
Enhanced T cell infiltration into TME results in a superior anti-tumor vaccination effect
The therapeutic efficacy induced by the BRAF peptide vaccine was evaluated in a BRAF-mutant melanoma model. As Fig. 3 shows, this vaccine showed potent tumor growth inhibition compared with other groups. Empty LCP NPs and LCP NPs encapsulating CpG showed no significant therapeutic effect, whereas LCP NPs encapsulating the BRAF peptide showed modest efficacy, indicating the essential immune function of antigen presenting. Furthermore, the most effective anti-tumor action can only be achieved when using the proper adjuvant. Only the combined full vaccination significantly inhibited tumor growth (p < 0.01). Preventive vaccination further reduced melanoma risk. Giving two vaccination dosages (on day 14 and day 7 boosted), the rate of tumor progression decreased significantly; the T/C ratio was 22.3%. Moreover, two out of ten mice achieved tumor-free survival, compared with the PBS control group, suggesting a potential preventive therapy for translational application.
Fig. 3.
Anti-tumor activity of the BRAF peptide vaccine in murine BRAF-mutant model. Mice were subcutaneously inoculated with either 2 × 105 (a) or 1 × 106 (b) BPD6 cells on day 0. Vaccination with 5% glucose (The PBS group), empty LCP (The Empty group), LCP-CpG (The CpG group), LCP-BRAF peptide (The BRAF group), or LCP-(BRAF + CpG) (The BRAF + CpG group) was given on day 10. Tumor growth was measured every 2–3 days. Five mice from each group were killed on day 29, and tumors, whole blood, and organs were harvested for further study. n = 5, *p < 0.05, **p < 0. 01. Preventive vaccination (n = 10) significantly reduced tumor growth compared with PBS control (n = 8), with T/C ratio of 22.3%. Two animals in the vaccinated group did not grow tumors (c)
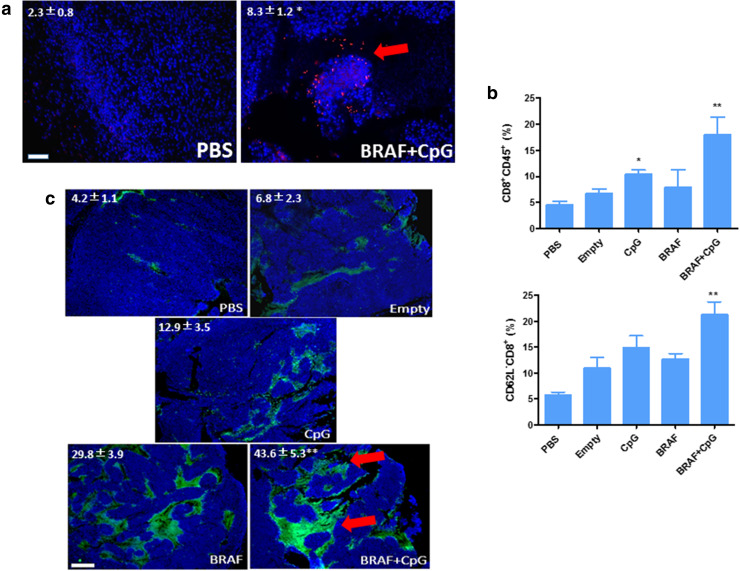
Vaccination’s enhanced anti-tumor effect was accompanied by an increase in CD8+ T cell population in the tumors, as determined by both flow cytometry analysis and immunofluorescence staining (Fig. 4). The tumor tissue slices from mice treated with the BRAF peptide vaccine showed extensive T cell infiltration into the tumor region (Fig. 4a). The tumors were further collected and dispersed into single cells. CD8+ T cell (CD8+CD45+) and T cell activation (CD8+CD62L−) were analyzed with flow cytometry. The results confirm that the CD8+ T cells significantly increased in number upon activation (Fig. 4b). These data suggest that manipulating the antigen-presenting cells could significantly enhance CD8+ T cell activation and proliferation. The antigen-specific CD8+ T cell killing induced potent cell death within the TME, as indicated by TUNEL assay (Fig. 4c).
Fig. 4.
Enhanced T cell infiltration into tumor microenvironment-induced potent CTL killing. a Tissue sections from murine BRAF-mutant model with different treatments were stained for CD8+ (red) and DAPI (blue), then analyzed by immunofluorescence microscopy. Scale bars indicate 200 μm. Arrow indicated infiltrating CTLs. b The percentage of CD8+ T cell (CD8+CD45+) and its activation (CD8+CD62L−) within tumor regions were quantified by flow cytometry. c TUNEL assay indicating apoptotic cell death. Scale bars indicate 300 μm. Arrows indicate apoptotic regions. Numbers in the panel indicate average values of three samples per group, quantified by Image J. *p < 0.05, **p < 0. 01
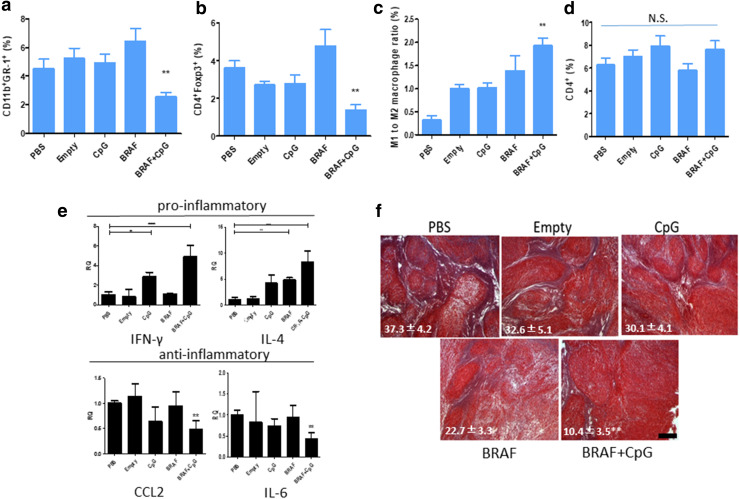
Changes of tumor-infiltrating immune cells and collagen within the TME
To further elucidate BRAF peptide vaccination in improving T cell infiltration, we then evaluated the changes of the related immunosuppressive subsets such as Tregs and MDSCs, which contributed to a complicated interplay network with CD8+ T cell anti-tumor activity within the collagen-rich BRAF-mutant murine model [21]. The accumulation of these immunosuppressive cells was measured by flow cytometry. As shown in Fig. 5a–b, the percentages of Tregs and MDSCs in the BRAF peptide vaccine group were much lower than in other groups. Macrophages are another important component of the suppressive tumor immune microenvironment. As shown in Fig. 5c, vaccination could efficiently stimulate macrophages to an advantageous tumor-suppressive M1 state. Vaccination significantly increased cytokine production of IFN-γ and IL-4 and decreased anti-inflammatory C–C motif chemokine 2 (CCL2) and IL6 production (Fig. 5e). The BRAF control group alone is insufficient to build up Type 1 T helper (Th1) type immunity. Interestingly, it correlated with increased Tregs and MDSCs. Tumor profiling of cytotoxic T cell (CD8+CD45+), T cell activation (CD8+CD62L−), MDSCs (CD11b+Gr1+), Tregs (CD4+Foxp3+), and the M1 (F4/80+Ly6C+) to M2 (F4/80+CD206+) ratio indicated a strong correlation between high levels of MDSCs and Tregs present in TME with loss of T cell function (activation). Furthermore, a significant decrease in collagen after vaccination indicated a change of the TME morphology that favored further CTL infiltration (Fig. 5f). Although we found no significant increase in infiltrating CD4+ T cells after vaccination (Fig. 5d), there was an overall significant remodeling of the suppressive TME in favor of immunotherapy.
Fig. 5.
Change of TME. The percentage of MDSCs (a), Treg cells (b), M1-to-M2 ratio (c), and CD4+ T cells (d) within tumor regions were quantified by flow cytometry. Rt-PCR elucidated inflammatory cytokine profile within TME (e). Masson’s trichrome staining (f) indicating change in collagen after different treatments. Numbers in the panel indicate average values of three samples per group, quantified by Image J. n = 5. *p < 0.05, **p < 0. 01. Scale bars indicate 300 μm
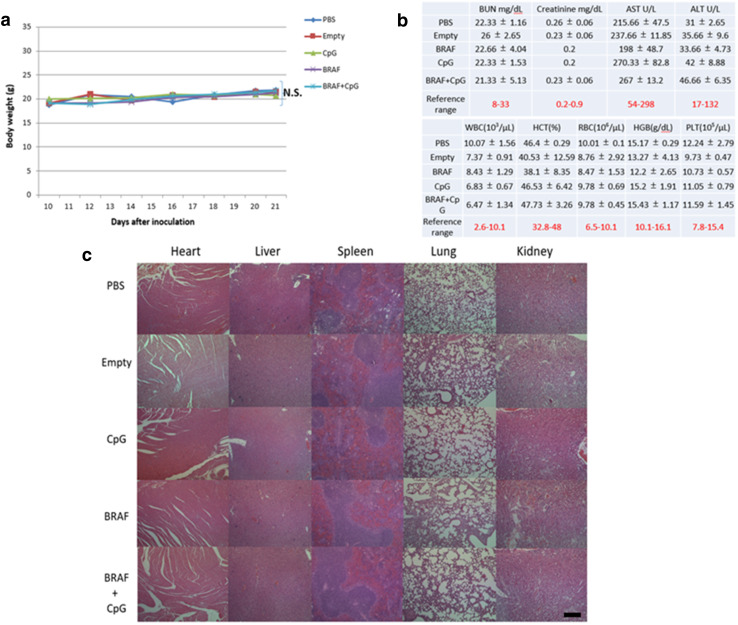
Toxicity evaluation
There was no significant loss in mice body weights, which indicated minor treatment toxicity. No significantly noticeable morphological changes occurred in major organs (Fig. 6). Additionally, serum biochemical value analysis demonstrated normal liver (AST, ALT) and kidney (creatinine, BUN) function. Whole blood cell counts remained constant within normal ranges for all the groups, suggesting that no systemic anemia or inflammation occurred after treatments.
Fig. 6.
Safety profile of the BRAF peptide vaccination. a Body weights of mice in each group. b Whole blood and serum toxicity evaluation. c H&E morphology evaluation. The BPD6-bearing mice were divided into five groups with different treatments. Body weights were evaluated every 2–3 days. Mice were euthanized at the endpoint with blood and major organs collected for blood serum and H&E tests. Scale bars indicate 300 μm. n = 5. N.S.: p > 0.05
Discussion and conclusion
Management of advanced melanoma is still a major challenge, and the development of a better understanding of melanoma biology is essential to design new therapeutic strategies and address present challenges associated with existing therapies. In human diseases, over 50% of melanoma cases have corporates BRAF mutations, and approximately, 90% of these mutations are at codon 600. Almost all of these mutations result from a single nucleotide substitution from glutamic acid to valine (BRAFV600E) [22]. BRAFV600E results in constitutive kinase pathway activation and unstoppable proliferation [23, 24].
Advanced melanoma is aggressively resistant to chemotherapeutic regimens. Many studies into the molecular basis of melanoma survival and proliferation have identified apoptotic resistance of melanoma cells as the underlying cause of chemo-resistance [25]. This is a formidable challenge for devising treatment strategies for advanced melanoma, and until recently, there was little advancement in standards of care. Dacarbazine has been the sole first-line treatment for melanoma since US Food and Drug Administration (FDA) approved its use in 1976. It has demonstrated a response rate of 10–20% in Phase I and Phase II clinical trials, but overall survival benefit has not been clearly established [26–29]. IFN-α, a type I interferon, is used for adjuvant immunotherapy in advanced melanoma; however, improvements in OS are debatable, and the subset of patients who are sensitive to adjuvant therapy has not been identified [30, 31]. High-dose IL-2 was approved in 1998, but again, the response rate is only about 10% and therapy involves grade 3 toxicities [32].
Immunotherapeutic strategies against melanoma have been extensively investigated in recent years. Tremendous excitement was generated as “checkpoint inhibitors” provided improved OS and disease-free survival over conventional chemotherapy regimens. Ipilimumab, a monoclonal antibody targeting CTLA-4, received regulatory approval in 2011, followed by pembrolizumab and nivolumab, antibodies against PD-1, in 2014 [33–36]. However, new challenges rapidly emerged as a proportion of patients demonstrated transitory or no responses against checkpoint inhibitors, while long-term survival and even cure were only attained in a small subset of patients [37]. It is thus extremely crucial to identify the right patient subset that may benefit from immunotherapy. However, no biomarker can currently predict clinical outcome [38].
In addition, the TME supported tumor cell survival despite drug exposure and resulted in innate and acquired drug resistance [5, 39]. TME refers to nonmalignant stroma cells that coexist with the neoplastic epithelial cells, including extracellular matrix, cytokines, and growth factors [40]. In addition to initiating multidrug resistance and supporting the tumorigenic process, a permissive microenvironment also acts as a physical barrier that limits the penetration of therapeutic agents, thus inhibiting their anticancer efficacy. Therefore, the complicated nature of the TME suggests that NP-based codelivery of multiple agents for tumor cell-specific targeting and killing may not overcome microenvironment barriers. Combining one regimen targeting and modulating TME-associated drug resistance with another regimen targeting and killing tumor cells holds promise to synergistically improve the therapeutic outcome of cancer treatment [41–43].
In the present work, vaccination using NP delivery effectively treated aggressive growth of BRAF-mutant melanoma. By predicting peptide-MHC class I binding using artificial neural networks (the NetMHC 4.0 developed by Technical University of Denmark [44, 45]), we identified the murine BRAFV600E peptide FGLANEKSI as a strong binder with binding affinity of 104.92 nM and 0.07% rank (strong binders are defined as having %rank < 0.5, and weak binders with %rank < 2). In vivo studies demonstrated that a single vaccination can induce a strong antigen-specific CTL response and potent tumor growth inhibition for approximately 2 weeks. Again, our LCP NPs provided enhanced vaccination efficacy. LCP, as a Ca2+ reservoir, could effectively modify the intracellular calcium dynamics that drive DC maturation for antigen presentation in a timely manner [46]. This advantage allowed the DCs to orchestrate cytokine production and antigen presentation to induce a potent immune response.
CD8+ T cell-mediated immunity was one crucial mechanism for enhanced anti-tumor immunity [47]. BRAF peptide vaccination induced a local enhancement of tumor-specific T cell infiltration, thus facilitating immune response activation, resulting in a long-term sustained effect. After vaccination, cytotoxic T cells increasingly infiltrated TME derived inflammatory cytokines such as IFN-γ and IL-4 and therefore amplified macrophage polarization. The inflammatory TME facilitated further Ly6C+ monocyte differentiation into M1-like functional phenotypes (F4/80+Ly6C+). These M1 state macrophages were recruited predominantly to the site of cancer. These key effector cells in the TME boosted local tumor antigen uptake and provided protection against tumor cells. Vaccination, when given at an early stage of tumor progression (tumor volume approximately 50 mm3 or smaller), would effectively skew immune reactions toward Th1 type. Our data showed a significant decrease in anti-inflammatory cytokines such as CCL2 and IL6. The Th1 type TME promoted effective CTL infiltration rather than activation of Tregs. These cytokine mediators regulated the expansion, migration, and activation of immune suppressive cells in a combinatorial manner. The attraction of CCL2 to MDSCs is well documented [48]. Increased IL6 signaling also promotes MDSCs proliferation once infiltrated. Our vaccine data suggested a potential immunotherapy by blocking IL6 or CCL2 within TME at an early stage of melanoma progression; we have studies ongoing to test this hypothesis. In addition, for BRAF-mutant melanoma, tumor stroma within immunosuppressive TME supported tumor cell growth. Fibroblast Activation Protein (FAP+) stroma cells are the major source of collagen production [42, 49]. Our unpublished follow-up work indicates that FAP+ stroma cells neighboring tumor cells also harbor BRAF mutations and that BRAF vaccination depletes these FAP+ cells, which improves CD8+ T cells’ functions within the TME. Although we found no significant increase in TME infiltrating CD4+ T cells after vaccination, one approach to improve efficacy is to co-load BRAF class II peptides into the same NP delivery system, thereby enhancing the T helper cell memory response. Overall, the modified TME would further enable syngeneic mono-antibody or chemotherapeutic nano-therapy, providing a promising strategy of combining immune therapy with chemotherapy. Thus, targeting TME-changing motifs along with efficient vaccination is a viable future research direction. We are currently working on applying BRAF peptide vaccination on genetically engineered BRAF-mutant murine model, and plan to test this on a humanized murine model.
Dysplastic nevi, also known as unusual-looking benign (noncancerous) moles, are common among Caucasians [50]. These atypical moles greatly increase the risk of developing melanoma, even if there is no family history of melanoma [51]. The BRAF peptide vaccine, which is HLA-restricted, may thus be developed as a preventive vaccination for use alongside regular exams. Therapeutic vaccines, along with adoptive T cell therapy and CAR-T cell therapy, are some of the novel strategies currently being explored in clinical trials [51, 52]. NPs can thus be potentially exploited as efficient drug-delivery vehicles and may reduce the side effects associated with some of the present therapeutics [53]. Theoretically, NP platforms can be exploited for combinatorial therapy by designing multimodal particles to further clinical translation.
Acknowledgements
The work was supported by NIH Grants CA149387 and CA198999. Leaf Huang is a Senior Visiting Scholar of the State Key Laboratory of Molecular Engineering of Polymers, Fudan University, China.
Abbreviations
- CCL2
C-C Motif chemokine 2
- CFSE
Carboxyfluorescein succinimidyl ester
- DOPA
Dioleoylphosphatydic acid
- DOTAP
(±)-N,N,N-Trimethyl-2,3-bis(z-octadec-9-ene-oyloxy)-1-propanaminium chloride
- DSPE-PEG-2000
1,2-Distearoyl-sn-glycero-3-phosphoethanolamine-N-[amino(polyethylene glycol)-2000
- DSPE-PEG-NHS
3-(N-succinimidyloxyglutaryl) aminopropyl, polyethyleneglycol-carbamyl-distearoylphosphatidylethanolamine
- FAP
Fibroblast activation protein
- LCP NP
Lipid-coated calcium phosphate nanoparticle
- ODN
Oligodeoxynucleotides
- OS
Overall survival
- TEM
Transmission electron microscope
- Th1
Type 1 T helper
- TME
Tumor microenvironment
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2016. CA Cancer J Clin. 2016;66(1):7–30. doi: 10.3322/caac.21332. [DOI] [PubMed] [Google Scholar]
- 2.Gloster HM, Jr, Brodland DG. The epidemiology of skin cancer. Dermatol Surg. 1996;22(3):217–226. doi: 10.1111/j.1524-4725.1996.tb00312.x. [DOI] [PubMed] [Google Scholar]
- 3.Smyth MJ, Dunn GP, Schreiber RD. Cancer immunosurveillance and immunoediting: the roles of immunity in suppressing tumor development and shaping tumor immunogenicity. Adv Immunol. 2006;90:1–50. doi: 10.1016/S0065-2776(06)90001-7. [DOI] [PubMed] [Google Scholar]
- 4.Miao L, Li J, Liu Q, et al. Transient and local expression of chemokine and immune checkpoint traps to treat pancreatic cancer. ACS Nano. 2017;11(9):8690–8706. doi: 10.1021/acsnano.7b01786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Klemm F, Joyce JA. Microenvironmental regulation of therapeutic response in cancer. Trends Cell Biol. 2015;25(4):198–213. doi: 10.1016/j.tcb.2014.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sithanandam G, Kolch W, Duh FM, et al. Complete coding sequence of a human B-raf cDNA and detection of B-raf protein kinase with isozyme specific antibodies. Oncogene. 1990;5(12):1775–1780. [PubMed] [Google Scholar]
- 7.Chapman PB, Hauschild A, Robert C, et al. Improved survival with vemurafenib in melanoma with BRAF V600E mutation. N Engl J Med. 2011;364(26):2507–2516. doi: 10.1056/NEJMoa1103782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hauschild A, Grob JJ, Demidov LV, et al. Dabrafenib in BRAF-mutated metastatic melanoma: a multicentre, open-label, phase 3 randomised controlled trial. Lancet. 2012;380(9839):358–365. doi: 10.1016/S0140-6736(12)60868-X. [DOI] [PubMed] [Google Scholar]
- 9.Long GV, Stroyakovskiy D, Gogas H, et al. Combined BRAF and MEK inhibition versus BRAF inhibition alone in melanoma. N Engl J Med. 2014;371(20):1877–1888. doi: 10.1056/NEJMoa1406037. [DOI] [PubMed] [Google Scholar]
- 10.Junttila MR, de Sauvage FJ. Influence of tumour micro-environment heterogeneity on therapeutic response. Nature. 2013;501(7467):346–354. doi: 10.1038/nature12626. [DOI] [PubMed] [Google Scholar]
- 11.Rammensee H, Bachmann J, Emmerich NP, et al. SYFPEITHI: database for MHC ligands and peptide motifs. Immunogenetics. 1999;50(3–4):213–219. doi: 10.1007/s002510050595. [DOI] [PubMed] [Google Scholar]
- 12.Cintolo JA, Datta J, Xu S, et al. Type I-polarized BRAF-pulsed dendritic cells induce antigen-specific CD8 + T cells that impact BRAF-mutant murine melanoma. Melanoma Res. 2016;26(1):1–11. doi: 10.1097/CMR.0000000000000203. [DOI] [PubMed] [Google Scholar]
- 13.Guo X, Huang L. Recent advances in nonviral vectors for gene delivery. Acc Chem Res. 2012;45(7):971–979. doi: 10.1021/ar200151m. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liu Q, Das M, Liu Y, et al. Targeted drug delivery to melanoma. Adv Drug Deliv Rev. 2017 doi: 10.1016/j.addr.2017.09.016. [DOI] [PubMed] [Google Scholar]
- 15.Li J, Chen YC, Tseng YC, et al. Biodegradable calcium phosphate nanoparticle with lipid coating for systemic siRNA delivery. J Control Release. 2010;142(3):416–421. doi: 10.1016/j.jconrel.2009.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Xu Z, Ramishetti S, Tseng YC, et al. Multifunctional nanoparticles co-delivering Trp2 peptide and CpG adjuvant induce potent cytotoxic T-lymphocyte response against melanoma and its lung metastasis. J Control Release. 2013;172(1):259–265. doi: 10.1016/j.jconrel.2013.08.021. [DOI] [PubMed] [Google Scholar]
- 17.Reddy R, Zhou F, Nair S, et al. In vivo cytotoxic T lymphocyte induction with soluble proteins administered in liposomes. J Immunol. 1992;148(5):1585–1589. [PubMed] [Google Scholar]
- 18.Czerkinsky CC, Nilsson LA, Nygren H, et al. A solid-phase enzyme-linked immunospot (ELISPOT) assay for enumeration of specific antibody-secreting cells. J Immunol Methods. 1983;65(1–2):109–121. doi: 10.1016/0022-1759(83)90308-3. [DOI] [PubMed] [Google Scholar]
- 19.Chen WS, Xu PZ, Gottlob K, et al. Growth retardation and increased apoptosis in mice with homozygous disruption of the Akt1 gene. Genes Dev. 2001;15(17):2203–2208. doi: 10.1101/gad.913901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Xu Z, Wang Y, Zhang L, et al. Nanoparticle-delivered transforming growth factor-beta siRNA enhances vaccination against advanced melanoma by modifying tumor microenvironment. ACS Nano. 2014;8(4):3636–3645. doi: 10.1021/nn500216y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lu Y, Miao L, Wang Y, et al. Curcumin micelles remodel tumor microenvironment and enhance vaccine activity in an advanced melanoma model. Mol Ther. 2016;24(2):364–374. doi: 10.1038/mt.2015.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bamford S, Dawson E, Forbes S, et al. The COSMIC (Catalogue of Somatic Mutations in Cancer) database and website. Br J Cancer. 2004;91(2):355–358. doi: 10.1038/sj.bjc.6601894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Davies H, Bignell GR, Cox C, et al. Mutations of the BRAF gene in human cancer. Nature. 2002;417(6892):949–954. doi: 10.1038/nature00766. [DOI] [PubMed] [Google Scholar]
- 24.Pratilas CA, Taylor BS, Ye Q, et al. (V600E)BRAF is associated with disabled feedback inhibition of RAF-MEK signaling and elevated transcriptional output of the pathway. Proc Natl Acad Sci USA. 2009;106(11):4519–4524. doi: 10.1073/pnas.0900780106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Soengas MS, Lowe SW. Apoptosis and melanoma chemoresistance. Oncogene. 2003;22(20):3138–3151. doi: 10.1038/sj.onc.1206454. [DOI] [PubMed] [Google Scholar]
- 26.Avril MF, Aamdal S, Grob JJ, et al. Fotemustine compared with dacarbazine in patients with disseminated malignant melanoma: a phase III study. J Clin Oncol. 2004;22(6):1118–1125. doi: 10.1200/JCO.2004.04.165. [DOI] [PubMed] [Google Scholar]
- 27.Crosby T, Fish R, Coles B, et al. Systemic treatments for metastatic cutaneous melanoma. Cochrane Database Syst Rev. 2002 doi: 10.1002/14651858.CD001215. [DOI] [PubMed] [Google Scholar]
- 28.Falkson CI, Ibrahim J, Kirkwood JM, et al. Phase III trial of dacarbazine versus dacarbazine with interferon alpha-2b versus dacarbazine with tamoxifen versus dacarbazine with interferon alpha-2b and tamoxifen in patients with metastatic malignant melanoma: an Eastern Cooperative Oncology Group study. J Clin Oncol. 1998;16(5):1743–1751. doi: 10.1200/JCO.1998.16.5.1743. [DOI] [PubMed] [Google Scholar]
- 29.Middleton MR, Grob JJ, Aaronson N, et al. Randomized phase III study of temozolomide versus dacarbazine in the treatment of patients with advanced metastatic malignant melanoma. J Clin Oncol. 2000;18(1):158–166. doi: 10.1200/JCO.2000.18.1.158. [DOI] [PubMed] [Google Scholar]
- 30.Mocellin S, Pasquali S, Rossi CR, et al. Interferon alpha adjuvant therapy in patients with high-risk melanoma: a systematic review and meta-analysis. J Natl Cancer Inst. 2010;102(7):493–501. doi: 10.1093/jnci/djq009. [DOI] [PubMed] [Google Scholar]
- 31.Theofilopoulos AN, Baccala R, Beutler B, et al. Type I interferons (alpha/beta) in immunity and autoimmunity. Annu Rev Immunol. 2005;23:307–336. doi: 10.1146/annurev.immunol.23.021704.115843. [DOI] [PubMed] [Google Scholar]
- 32.Schwartzentruber DJ, Lawson DH, Richards JM, et al. gp100 peptide vaccine and interleukin-2 in patients with advanced melanoma. N Engl J Med. 2011;364(22):2119–2127. doi: 10.1056/NEJMoa1012863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hodi FS, O’Day SJ, McDermott DF, et al. Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med. 2010;363(8):711–723. doi: 10.1056/NEJMoa1003466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Robert C, Schachter J, Long GV, et al. Pembrolizumab versus ipilimumab in advanced melanoma. N Engl J Med. 2015;372(26):2521–2532. doi: 10.1056/NEJMoa1503093. [DOI] [PubMed] [Google Scholar]
- 35.Hassel JC. Ipilimumab plus nivolumab for advanced melanoma. Lancet Oncol. 2016;17(11):1471–1472. doi: 10.1016/S1470-2045(16)30409-0. [DOI] [PubMed] [Google Scholar]
- 36.Wolchok JD, Kluger H, Callahan MK, et al. Nivolumab plus ipilimumab in advanced melanoma. N Engl J Med. 2013;369(2):122–133. doi: 10.1056/NEJMoa1302369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Schadendorf D, Hodi FS, Robert C, et al. Pooled analysis of long-term survival data from phase II and phase III trials of ipilimumab in unresectable or metastatic melanoma. J Clin Oncol. 2015;33(17):1889–1894. doi: 10.1200/JCO.2014.56.2736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Topalian SL, Taube JM, Anders RA, et al. Mechanism-driven biomarkers to guide immune checkpoint blockade in cancer therapy. Nat Rev Cancer. 2016;16(5):275–287. doi: 10.1038/nrc.2016.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Miao L, Guo S, Lin CM, et al. Nanoformulations for combination or cascade anticancer therapy. Adv Drug Deliv Rev. 2017;115:3–22. doi: 10.1016/j.addr.2017.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Nelson CM, Bissell MJ. Of extracellular matrix, scaffolds, and signaling: tissue architecture regulates development, homeostasis, and cancer. Annu Rev Cell Dev Biol. 2006;22:287–309. doi: 10.1146/annurev.cellbio.22.010305.104315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Conniot J, Silva JM, Fernandes JG, et al. Cancer immunotherapy: nanodelivery approaches for immune cell targeting and tracking. Front Chem. 2014;2:105. doi: 10.3389/fchem.2014.00105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Miao L, Liu Q, Lin CM, et al. Targeting tumor-associated fibroblasts for therapeutic delivery in desmoplastic tumors. Cancer Res. 2017;77(3):719–731. doi: 10.1158/0008-5472.CAN-16-0866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hu K, Miao L, Goodwin TJ, et al. Quercetin remodels the tumor microenvironment to improve the permeation, retention, and antitumor effects of nanoparticles. ACS Nano. 2017;11(5):4916–4925. doi: 10.1021/acsnano.7b01522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Andreatta M, Nielsen M. Gapped sequence alignment using artificial neural networks: application to the MHC class I system. Bioinformatics. 2016;32(4):511–517. doi: 10.1093/bioinformatics/btv639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Nielsen M, Lundegaard C, Worning P, et al. Reliable prediction of T-cell epitopes using neural networks with novel sequence representations. Protein Sci. 2003;12(5):1007–1017. doi: 10.1110/ps.0239403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tseng YC, Xu Z, Guley K, et al. Lipid-calcium phosphate nanoparticles for delivery to the lymphatic system and SPECT/CT imaging of lymph node metastases. Biomaterials. 2014;35(16):4688–4698. doi: 10.1016/j.biomaterials.2014.02.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Medzhitov R, Janeway CA., Jr Decoding the patterns of self and nonself by the innate immune system. Science. 2002;296(5566):298–300. doi: 10.1126/science.1068883. [DOI] [PubMed] [Google Scholar]
- 48.Umansky V, Sevko A. Tumor microenvironment and myeloid-derived suppressor cells. Cancer Microenviron. 2013;6(2):169–177. doi: 10.1007/s12307-012-0126-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lo A, Wang LC, Scholler J, et al. Tumor-promoting desmoplasia is disrupted by depleting FAP-expressing stromal cells. Cancer Res. 2015;75(14):2800–2810. doi: 10.1158/0008-5472.CAN-14-3041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rigel DS, Carucci JA. Malignant melanoma: prevention, early detection, and treatment in the 21st century. CA Cancer J Clin. 2005;50(4):215–236. doi: 10.3322/canjclin.50.4.215. [DOI] [PubMed] [Google Scholar]
- 51.Restifo NP, Dudley ME, Rosenberg SA. Adoptive immunotherapy for cancer: harnessing the T cell response. Nat Rev Immunol. 2012;12(4):269–281. doi: 10.1038/nri3191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Porter DL, Levine BL, Kalos M, et al. Chimeric antigen receptor-modified T cells in chronic lymphoid leukemia. N Engl J Med. 2011;365(8):725–733. doi: 10.1056/NEJMoa1103849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Allen TM, Cullis PR. Drug delivery systems: entering the mainstream. Science. 2004;303(5665):1818–1822. doi: 10.1126/science.1095833. [DOI] [PubMed] [Google Scholar]