Abstract
Rationale: Approximately 20% of Medicare beneficiaries hospitalized for acute exacerbations of chronic obstructive pulmonary disease (COPD) are readmitted within 30 days of discharge. In addition to implementing penalties for excess readmissions, the U.S. Centers for Medicare and Medicaid Services has developed Bundled Payments for Care Improvement (BPCI) initiatives to improve outcomes and control costs.
Objectives: To evaluate whether a comprehensive COPD multidisciplinary intervention focusing on inpatient, transitional, and outpatient care as part of our institution’s BPCI participation would reduce 30-day all-cause readmission rates for COPD exacerbations and reduce overall costs.
Methods: We performed a pre–postintervention study comparing all-cause readmissions and costs after index hospitalization for Medicare-only patients with acute exacerbation of COPD. The primary outcome was the difference in 30-day all-cause readmission rate compared with historical control subjects; secondary outcomes included the 90-day all-cause readmission rate and also health care costs compared with BPCI target prices.
Results: Seventy-eight consecutive Medicare patients were prospectively enrolled in the BPCI intervention in 2014 and compared with 109 patients in the historical group from 2012. Patients in BPCI were more likely to receive regular follow-up phone calls, pneumococcal and influenza vaccines, home health care, durable medical equipment, and pulmonary rehabilitation, and to attend pulmonary clinic. There was no difference in all-cause readmission rates at 30 days (BPCI, 12 events [15.4%] vs. non-BPCI, 19 events [17.4%]; P = 0.711), and 90 days (21 [26.9%] vs. 37 [33.9%]; P = 0.306). Compared with BPCI target prices, we incurred 4.3% lower 90-day costs before accounting for significant investment from the health system.
Conclusions: A Medicare BPCI intervention did not reduce 30-day all-cause readmission rates or overall costs after hospitalization for acute exacerbation of COPD. Although additional studies enrolling larger numbers of patients at multiple centers may demonstrate the efficacy of our BPCI initiative for COPD readmissions, this is unlikely to be cost effective at any single center.
Keywords: chronic obstructive pulmonary disease, exacerbations, bundled payment, penalties
About one-fifth of all patients hospitalized for an acute exacerbation of chronic obstructive pulmonary disease (COPD) are readmitted within 30 days of discharge, accounting for the majority of COPD-related health care costs (1–5). Significant differences observed in readmission rates by geography and care delivery practices prompted the United States Centers for Medicare and Medicaid Services (CMS) to conclude that up to 75% of these readmissions were preventable (6–8). In late 2014, CMS started penalizing hospitals up to 3% of all Medicare billing for higher than historical rates of readmissions after COPD exacerbations (8, 9).
In addition to penalties for excess readmissions, CMS has developed a number of alternative payment models aimed at reimbursing providers and hospitals based on outcomes rather than volume, including the Bundled Payments for Care Improvement (BPCI) initiative (10). By incentivizing outcomes, CMS aims to align provider and patient interests and reward health care systems for efficient, coordinated, and high-quality care (11). The University of Alabama at Birmingham (UAB) entered a contract with CMS to pilot a BPCI initiative in which payments for all inpatient and outpatient care related to a hospitalization for COPD and the 90-day postacute period would be bundled (10). If aggregate Medicare spending during the episode is below a target price, UAB has the opportunity to share in the savings, and if spending is above the target price, CMS is repaid a portion of the overage.
COPD is a complex multisystem disease with numerous comorbidities, and respiratory-specific therapies have not been successful in reducing readmission rates (12). This has resulted in a number of multidisciplinary, multipronged approaches aimed at increasing patient participation and improving care delivery, although results thus far have been mixed (13–18). In response to the CMS initiative, we initiated a multidisciplinary COPD management program that focuses on inpatient, transitional, and outpatient care; employs a common administrative and scheduling structure; and accepts joint responsibility for both outcomes and costs. We hypothesized that the BPCI intervention would result in a reduction in 30-day all-cause readmission rates after an index admission for acute exacerbations of COPD, and that the improvement in outcomes would result in cost savings compared with historical controls and BPCI target prices. Some of the results in this manuscript have been previously reported in the form of an abstract (19).
Methods
Study Design
We performed a pre-postintervention study comparing readmissions following an index hospitalization for acute exacerbations of COPD to the University of Alabama at Birmingham hospital. With 1,157 licensed beds, this is one of the 20 largest acute care medical facilities in the United States. Alabama has the second highest prevalence of COPD of any state in the United States. For these reasons, our hospital may be particularly suited to testing the efficacy of a BPCI initiative for COPD at a single medical center.
We included Medicare-only patients prospectively enrolled in the BPCI during its first year (2014) and compared outcomes with patients meeting BPCI criteria during 2012. All participants were fee for service Medicare only, and no dual-eligible Medicare–Medicaid or managed Medicare patients were included. The primary outcome studied was the difference in 30-day all-cause readmission rate, and secondary outcomes included 90-day all-cause readmission rate, 30- and 90-day readmissions due to acute exacerbations of COPD, and also 30- and 90-day health care costs (compared with historical control subjects) as well as the BPCI target price for 90 days. Participants were followed for 1 year postdischarge to calculate time to readmission.
UAB is participating in model 2 of the BPCI involving patients discharged with one of the diagnoses for acute exacerbations of COPD, which include diagnosis-related group (DRG) numbers 190, 191, and 192 (for details, see the online supplement). Data for readmissions were prospectively recorded for the intervention group and extracted from the electronic medical record for control subjects. The study was approved by the UAB Institutional Review Board.
Interventions
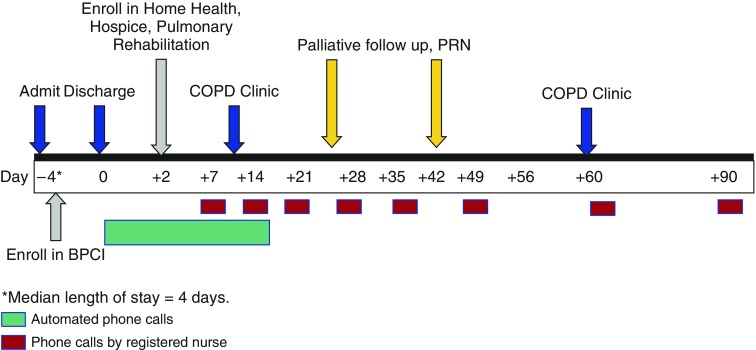
Patients enrolled in the BPCI initiative received standardized care during their admission and the postacute care period (timeline of interventions in Figure 1; for additional details, please see the online supplement). On hospitalization, all patients received a uniform duration of 5 days of antibiotics and systemic steroids (20). All participants were provided patient education material that included red flag symptoms. Active smokers received tobacco cessation counseling (21). Participants were monitored in the COPD clinic within 2 weeks, and case-based referrals were also made to pulmonary rehabilitation, home health, palliative care, and hospice as appropriate. Periodic phone calls were placed (for the timeline, see the online supplement), and deterioration of a patient’s symptoms was relayed to the BPCI health care providers for appropriate action.
Figure 1.
Timeline and interventions to prevent readmission in the Medicare Bundled Payments for Care Improvement initiative. BPCI = Bundled Payments for Care Improvement; COPD = chronic obstructive pulmonary disease; PRN = pro re nata (as needed).
Financial Considerations
We compared total costs for patients enrolled in BPCI during 2014 with the BPCI target price for 90 days as determined by Medicare. Cost calculations for the BPCI have been described elsewhere (8). Briefly, the BPCI base price was based on historical claims for DRG 190–192 from July 1, 2009 to June 30, 2012, which was then risk adjusted for measures of disease severity, predicted and observed readmission rates, and inflation, using the 2013 Consumer Price Index. This base price was then discounted 3% to derive the BPCI target price. As Medicare disallows use of individual patient data, costs for an index admission as well as 30- and 90-day all-cause costs were calculated by summing claims for inpatient and outpatient care submitted to CMS as obtained locally from the UAB Health Services Foundation.
Statistical Analyses
Comparisons between groups were made for continuous variables, using an independent t test or Mann–Whitney U test for nonparametric data, and using the χ2 or Fisher exact test for categorical variables. To assess time to first readmission, Cox proportional hazards analysis was performed. Comparisons were deemed to be statistically significant at a two-tailed α of 0.05 or less. All analyses were performed with the Statistical Package for the Social Sciences (SPSS 22.0; SPSS Inc., Chicago, IL).
Results
Baseline characteristics for patients in the BPCI arm and 2012 control subjects are shown in Table 1. The median length of hospital stay for control subjects was 3 days (interquartile range [IQR], 2–5), and 4 days (IQR, 2–5.3) for the BPCI group (P = 0.049). Two patients (1.8%) in the control arm and one (1.3%) in the BPCI arm received invasive mechanical ventilation (P = 0.624). There were two deaths among the control subjects and one in the BPCI group.
Table 1.
Baseline characteristics of patients in Medicare Bundled Payments for Care Improvement and control arms
| BPCI (n = 78) | Control Subjects (n = 109) | P Value | |
|---|---|---|---|
| Age, yr | 72.0 (11.0) | 69.9 (11.3) | 0.207 |
| Sex, female, n (%) | 48 (61.5) | 66 (60.6) | 0.891 |
| Race, African American, n (%) | 21 (26.9) | 33 (30.3) | 0.410 |
| Body mass index, kg/m2 | 27.1 (10.0) | 27.8 (10.2) | 0.694 |
| Smoking history, pack-years | 37.7 (22.7) | 47.2 (30.7) | 0.150 |
| Current smoker, n (%) | 27 (34.6) | 44 (41.1) | 0.369 |
| FEV1, % predicted | 54.4 (23.2) | 49.7 (19.0) | 0.310 |
| FEV1/FVC | 0.55 (0.15) | 0.52 (0.16) | 0.348 |
| Domiciliary oxygen use, n (%) | 40 (51.3) | 47 (43.5) | 0.295 |
| Asthma, n (%) | 9 (11.5) | 18 (16.5) | 0.340 |
| Coronary artery disease, n (%) | 16 (20.5) | 38 (35.5) | 0.027 |
| Atrial fibrillation, n (%) | 14 (17.9) | 17 (15.7) | 0.690 |
| Congestive heart failure, n (%) | 22 (28.2) | 31 (28.7) | 0.941 |
| Cerebrovascular accident, n (%) | 5 (6.4) | 14 (12.8) | 0.151 |
| Hypertension, n (%) | 60 (76.9) | 72 (66.1) | 0.108 |
| Diabetes mellitus, n (%) | 21 (26.9) | 29 (26.6) | 0.961 |
| Chronic kidney disease, n (%) | 12 (15.4) | 6 (5.5) | 0.024 |
| Obstructive sleep apnea, n (%) | 9 (11.5) | 12 (11.0) | 0.910 |
| Gastroesophageal reflux disease, n (%) | 27 (34.6) | 34 (31.2) | 0.623 |
| Depression, n (%) | 17 (21.8) | 30 (27.5) | 0.373 |
| Anxiety, n (%) | 13 (16.7) | 21 (19.3) | 0.650 |
Definition of abbreviation: BPCI = Medicare Bundled Payments for Care Improvement.
All values expressed as mean (SD) unless otherwise stated.
Services
Table 2 illustrates the frequency of individual interventions administered to patients in the two groups. Compared with control subjects, patients in the BPCI arm were more likely to receive influenza and pneumococcal vaccinations, to be referred to pulmonary rehabilitation, to have follow-up appointments scheduled with the pulmonary clinic and to attend those appointments, to receive home care, and to use durable medical equipment including home oxygen. There was no difference in the number of palliative care referrals. Active smokers in the BPCI intervention were significantly more likely to receive smoking cessation counseling.
Table 2.
Comparison of individual interventions
| BPCI (n = 78) | Control Subjects (n = 109) | P Value | |
|---|---|---|---|
| Pneumococcal vaccination, n (%) | 64 (82.1) | 38 (37.3) | <0.001 |
| Influenza vaccination, n (%) | 39 (50.5) | 29 (30.9) | 0.011 |
| Tobacco cessation counseling, n (%)* | 19/27 (70.4) | 12/44 (27.3) | <0.001 |
| Home care, n (%) | 33 (42.3) | 22 (20.0) | 0.001 |
| Durable medical equipment, n (%) | 43 (55.1) | 40 (36.7) | 0.012 |
| Pulmonary rehabilitation referral, n (%) | 13 (16.7) | 5 (4.6) | 0.006 |
| Follow-up pulmonary clinic referral, n (%) | 60 (76.9) | 26 (24.1) | <0.001 |
| Attended pulmonary clinic, n (%) | 50 (64.1) | 23 (21.1) | <0.001 |
| Palliative care, n (%) | 7 (9.0) | 7 (6.4) | 0.513 |
| Follow-up phone calls, n (%) | 78 (100) | 0 (0) | <0.001 |
Definition of abbreviation: BPCI = Medicare Bundled Payments for Care Improvement.
Offered to active smokers only.
Readmissions
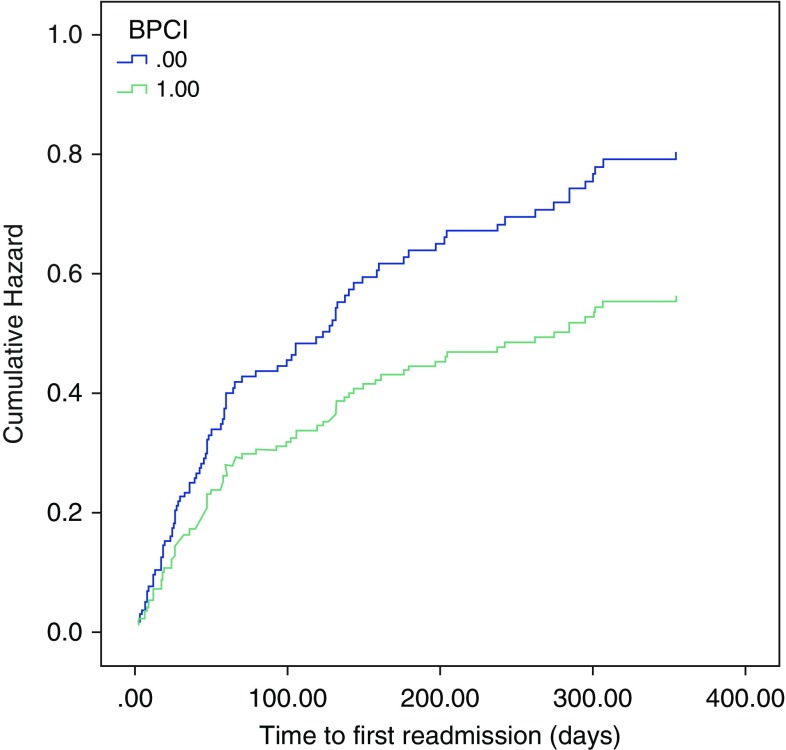
There was no difference in the primary outcome of 30-day all-cause readmissions (BPCI, 12 events [15.4%] vs. non-BPCI = 19 events [17.4%]; P = 0.711). There was also no difference in the 90-day all-cause readmission rates (21 events [26.9%] vs. 37 events [33.9%]; P = 0.224). There were no differences in readmission due to acute exacerbations of COPD at 30 days (11 events [14.1%] vs. 13 events [11.9%]; P = 0.661) and at 90 days (16 events [20.5%] vs. 26 events [23.9%]; P = 0.589). There was also no difference in the time to first readmission between BPCI and control patients (239 [157] vs. 213 [153] d; unadjusted hazard ratio, 0.70; 95% confidence interval, 0.45–1.07; P = 0.101) (Figure 2).
Figure 2.
Comparison of time to first readmission in the Medicare Bundled Payments for Care Improvement (BPCI) and control arms. Compared with control subjects, patients in the BPCI arm had a greater time to first readmission (239 [157] vs. 213 [153] d; unadjusted hazard ratio, 0.70 [95% confidence interval, 0.45–1.07]; P = 0.101).
Costs
The total target price for the patients enrolled in BPCI during 2014 was $1,047,464.26 whereas actual total CMS expenditures were $1,002,299.23; a net savings of $45,165.03 (4.3%). The net reconciliation by DRG codes was a savings of $18,396.28 (3.2%) for DRG 190, a savings of $37,532.91 (10.6%) for DRG 191, and a loss of $10,764.16 (8.5%) for DRG 192. However, these savings did not account for $250,000 in additional costs for the hospital system, incurred in hiring a full-time nurse practitioner and nurse and an additional part-time nurse, and the costs of telephone calls, printed materials, and physician effort. Individual patient cost data were available for hospital and posthospital care at our institution only, and there was no difference in the per-patient costs for the index admission in the BPCI group as compared with 2012 control subjects (Table 3).
Table 3.
Institute costs incurred over 30 and 90 days
| BPCI (n = 78) |
Control Subjects (n = 109) |
|||||||
|---|---|---|---|---|---|---|---|---|
| Total | Index Hospitalization | Inpatient Postindex Event | Outpatient Postindex Event | Total | Index Hospitalization | Inpatient Postindex Event | Outpatient Postindex Event | |
| 30-d costs | 6,486 (4,974) | 4,970 (2,703) Range (1,191–13,875) | 1,389 (4,385) | 127 (722) | 5,784 (4,392) | 5,020 (3,706) Range (902–18,934) | 729 (2,367) | 34 (133) |
| Range (1,191–30,153) | Range (0–22,320) | Range (0–4,792) | Range (902–20,303) | Range (0–14,058) | Range (0–1,041) | |||
| 90-d costs | 7,755 (5,768) | 2,608 (5,237) | 177 (766) | 7,849 (7,839) | 2,748 (6,479) | 82 (211) | ||
| Range (1,191–30,153) | Range (0–22,320) | Range (0–4,792) | Range (902–51,582) | Range (0–43,905) | Range (0–1,227) | |||
Definition of abbreviation: BPCI = Medicare Bundled Payments for Care Improvement.
All data expressed as mean (U.S. dollars) and standard deviation. All values expressed in U.S. dollars. None of the comparisons between case subjects and control subjects were statistically significantly different at a two-sided α of 0.05.
Discussion
We report that a comprehensive disease management program developed specifically for patients enrolled in the first CMS BPCI initiative focused on COPD hospitalizations had no statistically significant impact on the risk of all-cause or COPD-related readmissions within 30 or 90 days at a single large academic medical center. Although the intervention resulted in a 4.3% cost savings compared with BPCI target prices, this does not include the costs incurred to support the program, which far exceeded this benefit.
Even before the implementation of BPCI by Medicare, a number of comprehensive programs to decrease the rate of COPD hospitalizations were tested in the United States. Some of these studies suggested benefits, but there were significant differences in the interventions used, study size, duration of follow-up, and outcomes measured, which preclude direct comparisons with our results.
Bourbeau and colleagues implemented a weekly education program for 2 months followed by monthly telephone calls for high-risk patients and showed a 39.8% reduction in hospitalizations due to acute exacerbations of COPD (13). A pre–postintervention study of patients monitored by a COPD nurse navigator also showed improvements, including a 34% decrease in all-cause admissions at 1 year (22).
A multicenter, randomized study by Rice and colleagues using COPD education, an action plan for self-treatment of exacerbations, and monthly telephone calls found a 34% absolute reduction in 1-year hospitalizations and emergency room visits (15). However, a large follow-up randomized controlled study by Fan and colleagues was prematurely terminated because of higher mortality in the intervention arm (18). None of these studies recruited patients during hospitalization for COPD exacerbation.
A few studies have recruited patients during an initial hospitalization for COPD, and again the results have been mixed (14, 16, 23, 24). None of these studies examined 30-day readmission rates, the key time point used to determine CMS penalties. A study by Jennings and colleagues found no difference in 30-day readmission rates compared with usual care, but focused only on readmissions due to acute exacerbations of COPD, and not on readmissions for other conditions that are included in the CMS Hospital Readmissions Reduction Program (17).
Whereas there is an urgent need to reduce hospital readmissions, there is some controversy as to how many of these events related to complex chronic medical conditions are indeed preventable, in contrast to other single-disease conditions penalized by CMS such as hip surgery outcomes (25). Studies suggest that Medicare’s estimate that 75% of readmissions after an acute exacerbation of COPD are potentially preventable might be an overestimate, and that this figure might be as low as 25% (26, 27). It is also not clear whether the focus on COPD is justified as all Medicare patients suffer a 20% readmission rate within 30 days, and although an early readmission is thought to reflect problems in quality of care (28), there are no studies examining this issue in COPD.
In our study, the length of hospital stay was slightly longer in the BPCI arm than in the control arm. The reasons for this are not certain, although it is possible that greater awareness of the bundled payment initiative among providers could have led to a more conservative approach and delayed discharge. Despite this, we did not observe greater costs in the BPCI arm. We speculate that the electronic order set used during the bundle period streamlined care, reducing costs somewhat, including rapid switchover to oral steroids and the use of inexpensive and oral antibiotics whenever possible. It is also possible that the absence of cost differences was a reflection of the relatively small sample size.
Strengths and Limitations
The current analysis offers a number of important strengths compared with these prior reports. First, we specifically designed our study to capture the key outcomes that impact CMS readmission penalties. Second, our comprehensive program included a number of interventions that have individually been shown to decrease the risk of exacerbations (although not necessarily readmission) but that were not uniformly implemented in previous studies including tobacco cessation counseling (13, 15, 17, 18, 22), discharge planning (23), COPD education (13–16, 18, 22), social services referral (23), home health services (14, 23), comorbidity assessment (14, 17), periodic telephone calls (13–15, 17, 18, 23), pulmonary rehabilitation (24), immunization, follow-up with a pulmonologist, and referral to palliative services when appropriate.
None of the previous studies aimed at preventing readmissions assessed the cost-effectiveness of their interventions. Although our total costs were less than the BPCI price targets, this did not include the additional personnel and administrative costs necessary to coordinate the BPCI initiative and more closely monitor patients.
Our study has several limitations. We acknowledge that our study was underpowered to exclude a statistically significant difference in readmission rates. However, the annual patient volumes for COPD admissions we reported at our 1,157-bed acute care hospital reflect the volumes at many large tertiary centers, suggesting that the number of patients admitted annually for an acute exacerbation of COPD to any one center might be inadequate to demonstrate a reduction in the 30-day readmission rate or meaningful cost savings. For perspective, to detect a 5% reduction in the absolute risk of readmission at 30 days from 20% to 15%, which could be considered clinically significant, a sample size of more than 1,800 would be required.
In addition to small sample size, our readmission rates were already lower than national rates and this likely influenced our findings although we did not have a specific prevention program until we implemented the bundle initiative.
We also do not have patient-specific information on readmission rates at other hospitals. However, the Medicare costs do factor in readmissions at any hospital in the country as well as outpatient costs, and the captured CMS costs we report are complete for the determination of costs relative to target price. We did not adjust for disease severity in the pre- and postintervention groups; however, the diagnosis of acute exacerbation by DRG codes does factor in illness severity (2). Participants were not randomized as this is precluded by the retrospective payment design of the BPCI agreement.
Conclusions
A multidisciplinary intervention focusing on inpatient, transitional, and outpatient care as part of our institution’s participation in a Medicare BPCI initiative did not result in a reduction in 30-day all-cause readmissions, and did not result in substantial cost savings. Although larger, multicenter studies may be able to demonstrate a clinically meaningful reduction in the 30-day readmission rate and associated health care costs using these BPCI interventions, COPD may not rank among the most productive targets for efforts to reduce overall 30-day hospital readmission rates at any single center.
Supplementary Material
Footnotes
Disclaimer: The statements contained in this article are solely those of the authors and do not necessarily reflect the views or policies of U.S. Centers for Medicare and Medicaid Services. The authors assume responsibility for the accuracy and completeness of the information contained in this document.
Author Contributions: Study design: S.P.B., J.M.W., M.T.D.; statistical analyses: S.P.B. and M.T.D.; data interpretation: S.P.B., J.M.W., A.S.I., D.P.K., T.M.P., L.T.L., E.M.A., J.G.S., C.C.B., and M.T.D.; manuscript writing: S.P.B. and M.T.D.; critical review of the manuscript for important intellectual content: S.P.B., J.M.W., A.S.I., D.P.K., T.M.P., L.T.L., E.M.A., J.G.S., J.K.N., C.C.B., and M.T.D. S.P.B. had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
This article has an online supplement, which is accessible from this issue’s table of contents at www.atsjournals.org.
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Centers for Medicare and Medicaid Services (CMS), Department of Health and Human Services (HHS) Medicare program; hospital inpatient prospective payment systems for acute care hospitals and the long-term care hospital prospective payment system and Fiscal Year 2014 rates; quality reporting requirements for specific providers; hospital conditions of participation; payment policies related to patient status; final rules. Fed Regist. 2013;78:50495–51040. [PubMed] [Google Scholar]
- 2.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360:1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 3.Blanchette CM, Dalal AA, Mapel D. Changes in COPD demographics and costs over 20 years. J Med Econ. 2012;15:1176–1182. doi: 10.3111/13696998.2012.713880. [DOI] [PubMed] [Google Scholar]
- 4.Mannino DM, Homa DM, Akinbami LJ, Ford ES, Redd SC. Chronic obstructive pulmonary disease surveillance: United States, 1971–2000. MMWR Surveill Summ. 2002;51:1–16. [PubMed] [Google Scholar]
- 5.Mannino DM, Braman S. The epidemiology and economics of chronic obstructive pulmonary disease. Proc Am Thorac Soc. 2007;4:502–506. doi: 10.1513/pats.200701-001FM. [DOI] [PubMed] [Google Scholar]
- 6.Gerhardt G, Yemane A, Hickman P, Oelschlaeger A, Rollins E, Brennan N. Medicare readmission rates showed meaningful decline in 2012. Medicare Medicaid Res Rev. 2013;3:2. doi: 10.5600/mmrr.003.02.b01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Epstein AM, Jha AK, Orav EJ. The relationship between hospital admission rates and rehospitalizations. N Engl J Med. 2011;365:2287–2295. doi: 10.1056/NEJMsa1101942. [DOI] [PubMed] [Google Scholar]
- 8.Feemster LC, Au DH. Penalizing hospitals for chronic obstructive pulmonary disease readmissions. Am J Respir Crit Care Med. 2014;189:634–639. doi: 10.1164/rccm.201308-1541PP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Anonymous. Readmission reduction has begun and the penalties will escalate. Hosp Case Manag. 2013;21:45–47. [PubMed] [Google Scholar]
- 10.Centers for Medicare and Medicaid Services (CMS)Bundled Payments for Care Improvement (BPCI) Initiative: general information [updated 2017 Jan 9; accessed 2017 Jan 10]. Available from: https://innovation.cms.gov/initiatives/bundled-payments/
- 11.Press MJ, Rajkumar R, Conway PH. Medicare’s new bundled payments: design, strategy, and evolution. JAMA. 2016;315:131–132. doi: 10.1001/jama.2015.18161. [DOI] [PubMed] [Google Scholar]
- 12.Marchetti N, Criner GJ, Albert RK. Preventing acute exacerbations and hospital admissions in COPD. Chest. 2013;143:1444–1454. doi: 10.1378/chest.12-1801. [DOI] [PubMed] [Google Scholar]
- 13.Bourbeau J, Julien M, Maltais F, Rouleau M, Beaupré A, Bégin R, Renzi P, Nault D, Borycki E, Schwartzman K, et al. Chronic Obstructive Pulmonary Disease Axis of the Respiratory Network Fonds de la Recherche en Santé du Québec. Reduction of hospital utilization in patients with chronic obstructive pulmonary disease: a disease-specific self-management intervention. Arch Intern Med. 2003;163:585–591. doi: 10.1001/archinte.163.5.585. [DOI] [PubMed] [Google Scholar]
- 14.Casas A, Troosters T, Garcia-Aymerich J, Roca J, Hernández C, Alonso A, del Pozo F, de Toledo P, Antó JM, Rodríguez-Roisín R, et al. CHRONIC Project. Integrated care prevents hospitalisations for exacerbations in COPD patients. Eur Respir J. 2006;28:123–130. doi: 10.1183/09031936.06.00063205. [DOI] [PubMed] [Google Scholar]
- 15.Rice KL, Dewan N, Bloomfield HE, Grill J, Schult TM, Nelson DB, Kumari S, Thomas M, Geist LJ, Beaner C, et al. Disease management program for chronic obstructive pulmonary disease: a randomized controlled trial. Am J Respir Crit Care Med. 2010;182:890–896. doi: 10.1164/rccm.200910-1579OC. [DOI] [PubMed] [Google Scholar]
- 16.Bucknall CE, Miller G, Lloyd SM, Cleland J, McCluskey S, Cotton M, Stevenson RD, Cotton P, McConnachie A. Glasgow Supported Self-Management Trial (GSuST) for patients with moderate to severe COPD: randomised controlled trial. BMJ. 2012;344:e1060. doi: 10.1136/bmj.e1060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jennings JH, Thavarajah K, Mendez MP, Eichenhorn M, Kvale P, Yessayan L. Predischarge bundle for patients with acute exacerbations of COPD to reduce readmissions and ED visits: a randomized controlled trial. Chest. 2015;147:1227–1234. doi: 10.1378/chest.14-1123. [DOI] [PubMed] [Google Scholar]
- 18.Fan VS, Gaziano JM, Lew R, Bourbeau J, Adams SG, Leatherman S, Thwin SS, Huang GD, Robbins R, Sriram PS, et al. A comprehensive care management program to prevent chronic obstructive pulmonary disease hospitalizations: a randomized, controlled trial. Ann Intern Med. 2012;156:673–683. doi: 10.7326/0003-4819-156-10-201205150-00003. [DOI] [PubMed] [Google Scholar]
- 19.Bhatt SP, Wells JM, Iyer AS, Kirkpatrick dP, Parekh TM, Anderson EM, Sanders JG, Nichols JK, Blackburn CC, Dransfield MT. An integrated practice unit model to reduce 30-day readmission for COPD: Results from a Medicare Bundled Payments for Care Improvement initiative [abstract] Am J Respir Crit Care Med. 2016;193:A1118. [Google Scholar]
- 20.Leuppi JD, Schuetz P, Bingisser R, Bodmer M, Briel M, Drescher T, Duerring U, Henzen C, Leibbrandt Y, Maier S, et al. Short-term vs conventional glucocorticoid therapy in acute exacerbations of chronic obstructive pulmonary disease: the REDUCE randomized clinical trial. JAMA. 2013;309:2223–2231. doi: 10.1001/jama.2013.5023. [DOI] [PubMed] [Google Scholar]
- 21.Iyer AS, Bhatt SP, Garner JJ, Wells JM, Trevor JL, Patel NM, Kirkpatrick D, Williams JC, Dransfield MT. Depression is associated with readmission due to acute exacerbation of chronic obstructive pulmonary disease. Ann Am Thorac Soc. 2016;13:197–203. doi: 10.1513/AnnalsATS.201507-439OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dajczman E, Robitaille C, Ernst P, Hirsch AM, Wolkove N, Small D, Bianco J, Stern H, Palayew M. Integrated interdisciplinary care for patients with chronic obstructive pulmonary disease reduces emergency department visits, admissions and costs: a quality assurance study. Can Respir J. 2013;20:351–356. doi: 10.1155/2013/187059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lainscak M, Kadivec S, Kosnik M, Benedik B, Bratkovic M, Jakhel T, Marcun R, Miklosa P, Stalc B, Farkas J. Discharge coordinator intervention prevents hospitalizations in patients with COPD: a randomized controlled trial. J Am Med Dir Assoc. 2013;14:450.e1–6. doi: 10.1016/j.jamda.2013.03.003. [DOI] [PubMed] [Google Scholar]
- 24.Greening NJ, Williams JE, Hussain SF, Harvey-Dunstan TC, Bankart MJ, Chaplin EJ, Vincent EE, Chimera R, Morgan MD, Singh SJ, et al. An early rehabilitation intervention to enhance recovery during hospital admission for an exacerbation of chronic respiratory disease: randomised controlled trial. BMJ. 2014;349:g4315. doi: 10.1136/bmj.g4315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Morris MS, Deierhoi RJ, Richman JS, Altom LK, Hawn MT. The relationship between timing of surgical complications and hospital readmission. JAMA Surg. 2014;149:348–354. doi: 10.1001/jamasurg.2013.4064. [DOI] [PubMed] [Google Scholar]
- 26.van Walraven C, Bennett C, Jennings A, Austin PC, Forster AJ. Proportion of hospital readmissions deemed avoidable: a systematic review. CMAJ. 2011;183:E391–E402. doi: 10.1503/cmaj.101860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.van Walraven C, Jennings A, Forster AJ. A meta-analysis of hospital 30-day avoidable readmission rates. J Eval Clin Pract. 2012;18:1211–1218. doi: 10.1111/j.1365-2753.2011.01773.x. [DOI] [PubMed] [Google Scholar]
- 28.Ashton CM, Del Junco DJ, Souchek J, Wray NP, Mansyur CL. The association between the quality of inpatient care and early readmission: a meta-analysis of the evidence. Med Care. 1997;35:1044–1059. doi: 10.1097/00005650-199710000-00006. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.