Abstract
Background
Failure-to-rescue is defined as the conditional probability of death after a complication, and the failure-to-rescue rate reflects a center’s ability to successfully “rescue” patients after complications. The validity of the failure-to-rescue rate as a quality measure is dependent on the preventability of death and the appropriateness of this measure for use in the trauma population is untested. We sought to evaluate the relationship between preventability and failure-to-rescue in trauma.
Methods
All adjudications from a mortality review panel at an academic level I trauma center from 2005–2015 were merged with registry data for the same time period. The preventability of each death was determined by panel consensus as part of peer review. Failure-to-rescue deaths were defined as those occurring after any registry-defined complication. Univariate and multivariate logistic regression models between failure-to-rescue status and preventability were constructed and time to death was examined using survival time analyses.
Results
Of 26,557 patients, 2,735 (10.5%) had a complication, of whom 359 died for a failure-to-rescue rate of 13.2%. Of failure-to-rescue deaths, 272 (75.6%) were judged to be non-preventable, 65 (18.1%) were judged potentially preventable, and 22 (6.1%) were judged to be preventable by peer review. After adjusting for other patient factors, there remained a strong association between failure-to-rescue status and potentially preventable (odds ratio 2.32, 95% confidence interval, 1.47–3.66) and preventable (odds ratio 14.84, 95% confidence interval, 3.30–66.71) judgment.
Conclusion
Despite a strong association between failure-to-rescue status and preventability adjudication, only a minority of deaths meeting the definition of failure to rescue were judged to be preventable or potentially preventable. Revision of the failure-to-rescue metric before use in trauma care benchmarking is warranted.
Since the introduction of the concept >20 years ago, failure-to-rescue (FTR) has become a widely used metric of quality of care. Failure-to-rescue is defined as death occurring after a complication1 and has been shown to correlate better with inhospital mortality than the complication rates alone after cardiac surgery,2,3 vascular surgery,4,5 general surgery,4,6 pancreatectomy,7,8 pulmonary resection,9 and surgery for head and neck cancer.10 Recently, this relationship also has been demonstrated after traumatic injury.11,12 The FTR rate also is associated more strongly with potentially modifiable factors specific for institutional systems, such as nurse-to-bed ratios,13 nurse education levels,14 and physician board certification status1,15 than complication rates, which are associated more strongly with non-modifiable patient factors such as age or comorbidities.16 FTR rates are therefore, a more desirable measure of quality of care than complication rates because the complication rates reflect patient severity, while the FTR rate reflects allegedly how centers respond to complications once they have occurred.17
From a conceptual standpoint, the term “failure-to-rescue” implies that rescue is possible, and death is, therefore, a failure. But, as with complications and death, not all FTR events are preventable.12,18,19 Additionally in trauma cohorts, the majority of deaths after injury occur without a recorded, preceding complication, thus early traumatic deaths usually do not meet the definition of FTR.20 As trauma center mortality rates and other quality metrics appear to be exerting an increasing role in reimbursement based on pay-for-performance21 and as hospitals devote increasing resources to improving patient safety, a greater understanding of FTR in the trauma population (and possibly in other operative settings as well) is necessary.
In this retrospective cohort study, we aimed to describe the association between FTR status and preventable mortality, as adjudicated by mortality review panels. We hypothesized that after controlling for the characteristics of the demographics and the injury, FTR status would be associated strongly with preventable or potentially preventable deaths. We further intended to define patient characteristics associated with both FTR status and preventability adjudication. Lastly, we also sought to define differences in the timing of death in FTR and non-FTR deaths according to preventability adjudication.
METHODS
After receiving approval from the University of Pennsylvania’s Institutional Review Board, we performed a retrospective, cohort analysis of our institutional trauma registry from 2005–2015. Our trauma center is a mature, academic, urban, level 1 trauma center accredited by the Pennsylvania Trauma Systems Foundation (PTSF), the regulatory body responsible for overseeing all trauma programs throughout the Commonwealth of Pennsylvania.22 As a stipulation for accreditation, Pennsylvania trauma centers require trained registrars to abstract data for all trauma patients and monitor the data for completeness and quality.
All inpatient trauma patients during the study period were included. Patients <18 years of age and those with primary burn wounds were excluded. Demographic information (age, race, sex), physiologic data (admission Glasgow Coma Score [GCS], GCS subscores, systolic blood pressure, pulse, respiratory rate, and temperature), and pre-existing medical conditions were abstracted from the trauma registry, as was the mechanism of injury (blunt versus penetrating) and injury severity as measured by injury severity score (ISS).23 Pre-existing conditions were defined per Pennsylvania Trauma Outcome Study registry definitions24; for the purpose of analysis, patients were categorized as having none, 1–2, or ≥3 pre-existing comorbidities.
The cohort of interest in this study was all patients who died in the hospital, and the primary exposure of interest was the adjudication of preventability as decided by a mortality review panel. At our institution, the panel consists of the trauma medical director, the trauma program director, the performance improvement coordinator, and attending trauma surgeons. In addition to collecting data on injured patients, the PTSF mandates that trauma centers review all deaths to identify opportunities for improvement of care and to judge whether the death was non-preventable, potentially preventable, or preventable (Table I). Cases are first assigned randomly to surgeons not involved in the case for review. Each mortality then is presented at monthly mortality review meetings for discussion and consensus regarding preventability. In the event that consensus cannot be reached, voting by simple majority of surgeons is used. All review determinations of performance improvement are entered prospectively into the database.
Table I.
Mortality preventability classification
| Classification | Criteria |
|---|---|
| Preventable | Anatomic injury or combination of injuries considered survivable |
| Standard protocols not followed with unfavorable consequence | |
| Inappropriate provider care with unfavorable consequence | |
| P values >.5 by Trauma and Injury Severity Score methodology | |
| Potentially preventable | Anatomic injury or combination of injuries considered severe but survivable |
| Standard protocols not followed, possibly resulting in an unfavorable consequence | |
| Suboptimal provider care, possibly resulting in an unfavorable consequence | |
| P values .25–.5 by Trauma and Injury Severity Score methodology | |
| Not preventable | Anatomic injury or combination of injuries considered nonsurvivable with optimal care |
| Standard protocols followed, or if followed, did not result in an unfavorable consequence | |
| Appropriate provider care, or if suboptimal, did not result in an unfavorable consequence | |
| P values <.25 by Trauma and Injury Severity Score methodology |
TRISS, Trauma and Injury Severity Score.
The primary outcome of interest was FTR status. A FTR case was defined as a death after any PTSF-defined complication. In a previous work, we have limited the definition of FTR in trauma patients to those deaths occurring after major complications, with “major” defined as the complications noted in the sentinel publication on FTR1 and those associated with mortality in univariate analyses.20 For the purpose of this work, we expanded the definition of FTR cases to include deaths preceded by any complication, in order to increase the precedence rate and thus include a greater proportion of deaths.17 The definitions of the PTSF 2014 Operational Manual Database Collection System, Appendix 9 were used as complications.22
Baseline variables between FTR and non-FTR cases were examined using the χ2 test for categorical variables and the Mann-Whitney or Kruskal-Wallis test for nonparametric continuous variables. Parametric continuous variables were compared using t test or 1-way ANOVA tests, as appropriate. Univariate logistic regression was used to examine the association between FTR status and patient variables. Variables associated with FTR status and P <.1 were considered for inclusion in a multivariable logistic regression model to test the association between FTR classification and preventability.
To examine the differences in the timing of deaths between FTR and non-FTR cases, survival times were examined using Kaplan-Meier curves. The assumption of proportional hazards was checked, and then log-rank tests for equality of survivor functions were conducted between preventability categories. All statistical analyses were performed using Stata version 14.1 (College Station, TX).
RESULTS
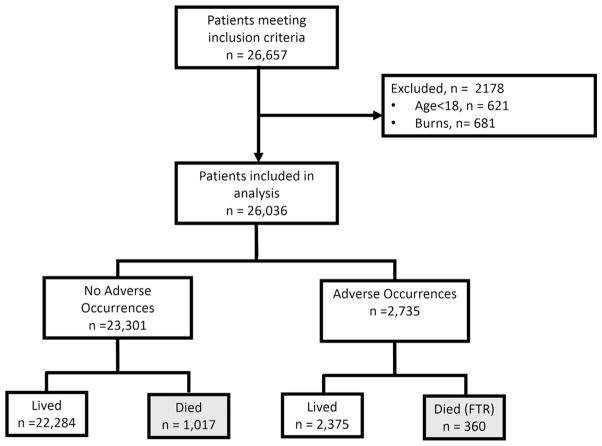
In total, 26,557 patients were evaluated for inclusion in the study. After excluding pediatric patients and those with a primary injury mechanism of burn, 26,036 patients remained in the cohort (Fig 1). Overall, the study population was 54% African-American, 70% male, and with a median age of 40 years (interquartile range [IQR] was 26–56 years). The mechanism of injury was predominantly blunt (78%), with a median injury severity score (ISS) of 5 (IQR 1–13). Complications occurred in 2,735 (10.5%) patients, of whom 360 died for a FTR rate of 13.2%. During the study period, there was a statistically significant decrease in the FTR rate from 17.3% in 2005 to 10.6% in 2015 (P < .01). In total, 1,377 of 26,036 (5.2%) of patients died. In the 1,377 patients who died, 820 (61%) were African-American, 80% were male, and the group had a median age of 40 years (IQR 24–68 years) with a median ISS of 26 (IQR 10–35). The majority of all deaths were considered non-preventable (1,239 or 90.0%), while only a minority were considered potentially preventable (109 or 7.9%) or preventable (24 or 1.7%).
Fig 1.
Flow diagram of patients in the study.
When comparing FTR versus non-FTR cases, we found significant differences across a wide range of patient characteristics (Table II). Patients who experienced FTR deaths were older (median age 57.5; IQR 31–77) vs 35 (IQR 23–59) years of age (P < .001), more likely to be female (24% vs 18%, P = .15), and more likely to have sustained blunt trauma (76% vs 44%, P < .001). FTR cases were more physiologically stable as measured by the revised trauma score25 (5.03; IQR 3.51–7.84) vs 2.93 (IQR 0–4.09; P = .001), had a greater injury burden (median ISS 26; IQR 17–38) vs 26 (IQR 10–35; P < .001), and had a greater predicted survival by Trauma and Injury Severity Score (TRISS)25 methodology. FTR cases were more than twice as likely to have undergone an operation (38% vs 15%, P <.001) and had greater durations of stays in the intensive care unit (median 4; IQR 1–10.5) vs 0 (IQR 0–1) days (P <.001). As with non-FTR cases, the majority of FTR cases were classified as non-preventable by panel review; however, a greater proportion of cases in the FTR group were considered potentially preventable (18% vs 4% P < .001) or preventable (6% vs 0.2%, P < .001). Of the 24 deaths judged preventable in the study period, 22 (91%) were FTR deaths.
Table II.
Demographic, physiologic, injury scoring, and clinical outcome variables by failure-to-rescue status among mortalities
| Variable | All mortalities N = 1,377 |
Non-FTR Mortalities N = 1,017 |
FTR Mortalities N = 360 |
P value |
|---|---|---|---|---|
| Median age, y (IQR) | 40 (24–68) | 35 (23–59) | 57.5 (31–77) | <.001 |
| Male, n (%) | 1,108 (80.5) | 834 (82.0) | 274 (76.1) | .015 |
| Race, n (%) | <.001 | |||
| African-American | 820 (59.5) | 670 (65.9) | 150 (41.7) | |
| Caucasian | 469 (34.1) | 296 (29.1) | 174 (48.3) | |
| Other | 87 (6.3) | 51 (5.0) | 36 (10.0) | |
| Pre-existing conditions, n (%) | <.001 | |||
| None | 808 (58.7) | 669 (65.8) | 139 (38.6) | |
| 1–2 | 360 (26.1) | 254 (25.0) | 106 (29.4) | |
| >3 | 209 (15.2) | 94 (9.2) | 115 (31.9) | |
| Blunt mechanism, n (%) | 724 (52.6) | 452 (44.4) | 272 (75.6) | <.001 |
| Mean admission temperature,°C (standard deviation) | 35.9 (1.2) | 35.9 (1.2) | 36.0 (1.1) | .04 |
| Median admission GCS (IQR) | ||||
| Motor | 1 (1–1) | 1 (1–1) | 2 (1–6) | <.001 |
| Verbal | 1 (1–1) | 1 (1–1) | 1 (1–5) | <.001 |
| Eye | 1 (1–1) | 1 (1–1) | 1 (1–4) | <.001 |
| Median revised trauma score (IQR) | 3.2 (0–7.8) | 2.9 (0–4.01) | 5.0 (3.5–7.8) | .001 |
| Median maximum AIS score (IQR) | 5 (3–5) | 4 (1–5) | 4 (4–5) | .001 |
| Median Injury Severity score (IQR) | 26 (11–35) | 26 (10–35) | 26 (17–38) | <.001 |
| Median predicted probability of survival by TRISS (IQR) | 0.3 (0.1–0.5) | 0.2 (0.4–0.5) | 0.6 (0.2–0.9) | <.001 |
| Underwent operation, n (%) | 285 (20.9) | 150 (14.7) | 135 (37.5) | <.001 |
| Median ICU duration of stay, d (IQR) | 0 (0–1) | 0 (0–1) | 4 (1–10.5) | <.001 |
| Preventability adjudication, n (%) | <.001 | |||
| Not preventable | 1,239 (90.0) | 967 (95.1) | 272 (75.6) | |
| Potentially preventable | 109 (7.9) | 44 (4.3) | 65 (18.1) | |
| Preventable | 24 (1.5) | 2 (0.2) | 22 (6.1) | |
| Missing | 5 (0.3) | 4 (0.4) | 1 (0.3) | |
P values result from χ2 test for categorical variables, t test for parametric continuous variables, and the Mann-Whitney test for non-parametric continuous variables.
AIS, Abbreviated Injury Scale; GCS, Glasgow Coma Scale; ICU, intensive care unit; IQR, interquartile ratio; TRISS, Trauma and Injury Severity Score.
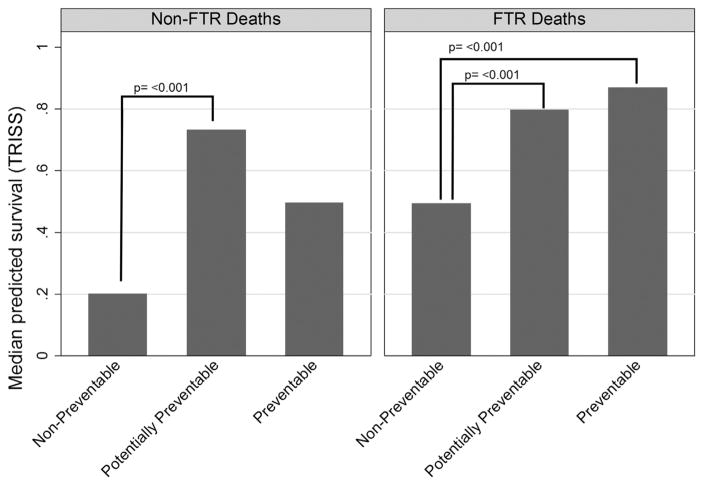
Examining the subset of FTR deaths by preventability status (Table III) revealed several findings. Demographic variables such as age, race, or sex were not associated with adjudication of preventability, nor were characteristics of injury as measured by injury mechanism, ISS, or maximum score on the abbreviated injury scale.26 Presenting physiology as measured by GCS subscore and RTS was, however, associated strongly with preventability in a stepwise fashion, such that the less physiologically compromised the patient was on arrival, the more likely the death was to be considered preventable. This association was reflected in the predicted probabilities of survival as derived from the Trauma and Injury Severity Score (TRISS) and the A Severity Characterization of Trauma (ASCOT) methodology (Fig 2).
Table III.
Demographic, physiologic, injury score and clinical outcomes among failure-to-rescue deaths, by preventability adjudication
| Variable | All FTR deaths N = 359 |
Non–preventable N = 272 |
Potentially preventable N = 65 |
Preventable N = 22 |
P value |
|---|---|---|---|---|---|
| Median age, y (IQR) | 57.5 (31–77) | 56.5 (31–78) | 53 (31–76) | 62.5 (39–74) | .58 |
| Male, n (%) | 273 (76.0) | 205 (75.3) | 49 (75.3) | 19 (86.3) | .51 |
| Race, n (%) | .14 | ||||
| African-American | 150 (41.8) | 114 (41.9) | 29 (44.6) | 7 (31.8) | |
| Caucasian | 173 (29.5) | 136 (50.0) | 27 (41.5) | 10 (45.5) | |
| Other | 36 (10.0) | 22 (0.7) | 9 (13.8) | 5 (22.7) | |
| Pre-existing conditions, n (%) | .42 | ||||
| None | 139 (38.7) | 112 (41.2) | 22 (33.8) | 5 (22.7) | |
| 1–2 | 106 (29.5) | 76 (27.9) | 22 (33.8) | 8 (36.4) | |
| >3 | 115 (32.0) | 84 (30.9) | 21 (32.3) | 9 (40.9) | |
| Blunt mechanism, n (%) | 271 (75.5) | 202 (74.3) | 52 (80.0) | 17 (77.3) | .62 |
| Mean admission Temperature,°C (standard deviation) | 36.0 (1.1) | 36.0 (1.2) | 36.1 (0.8) | 36.0 (1.4) | .68 |
| Median admission GCS (IQR) | |||||
| Motor | 2 (1–6) | 1 (1–6) | 6 (1–6) | 6 (1–6) | .001 |
| Verbal | 5 (1–5) | 1 (1–4) | 5 (1–5) | 5 (1–5) | .001 |
| Eye | 1 (1–4) | 1 (1–4) | 4 (1–4) | 4 (1–4) | .001 |
| Median revised trauma score (IQR) | 5.0 (3.5–7.8) | 4.1 (3.2–7.1) | 7.6 (4.1–7.8) | 7.9 (4.1–7.8) | <.001 |
| Median maximum AIS score (IQR) | 5 (4–5) | 4 (4–5) | 4 (3–5) | 4 (3–5) | .21 |
| Median injury severity score (IQR) | 26 (17–38) | 26 (17.5–38) | 26 (17–38) | 28 (17–38) | .97 |
| Median predicted probability of survival by TRISS (IQR) | 0.6 (0.2–0.9) | 0.5 (0.2–0.9) | 0.8 (0.4–0.9) | 0.9 (0.4–1.0) | .001 |
| Median ICU duration of stay, d (IQR) | 4 (1–10.5) | 3 (1–9) | 9 (2–14) | 15 (5–28) | .001 |
P values result from χ2 test for categorical variables, t test for parametric continuous variables, and the Mann-Whitney test for non-parametric continuous variables.
AIS, Abbreviated Injury Scale; GCS, Glasgow Coma Scale; ICU, intensive care unit; IQR, interquartile ratio; TRISS, Trauma and Injury Severity Score.
Fig 2.
Differences in predicted survival using TRISS methodology by preventability adjudication. FTR, Failure-to-rescue. P-values result from the Kruskal-Wallis test.
In multivariable logistic regression modeling, preventability adjudication remained strongly and statistically associated with FTR status. Relative to non-preventable adjudication, the odds of potentially preventable and preventable adjudications being FTR cases were 2.3 (95% confidence interval [CI], 1.5–3.7) and 14.8 (95% CI, 3.3–66.7), respectively. Other factors associated with FTR status included a blunt mechanism of injury, ISS, revised trauma score, having ≥3 pre-existing conditions and having undergone an operation (Table IV).
Table IV.
Multivariable logistic regression on the outcome of failure-to-rescue status
| Odds ratio | 95% confidence interval | P value | |
|---|---|---|---|
| Preventability Adjudication | |||
| Non-preventable | Ref | ||
| Potentially preventable | 2.32 | 1.47–3.66 | <.001 |
| Preventable | 14.8 | 3.30–66.71 | <.001 |
| Pre-existing conditions | |||
| None | Ref | ||
| 1–2 | 1.01 | 0.7–1.47 | .95 |
| 3 | 2.36 | 1.52–3.65 | <.001 |
| Blunt mechanism | 2.40 | 1.68–3.44 | <.001 |
| Injury severity score | 1.02 | 1.01–1.02 | <.001 |
| Revised trauma score | 1.27 | 1.19–1.36 | <.001 |
| Underwent operation | 2.54 | 1.82–3.54 | <.001 |
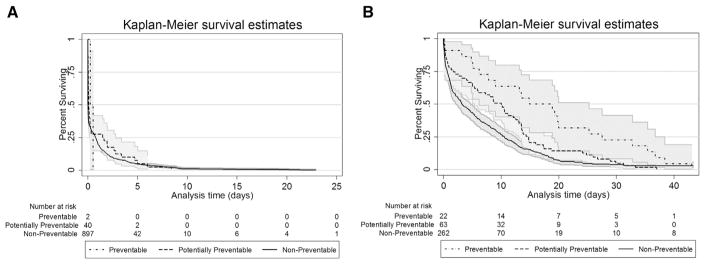
Kaplan-Meier plotting revealed that median survival time was less in the non-FTR group than in the FTR group (0.2 days [95% CI, 0.004–0.79]) vs 5.0 days (95% CI, 0.81–12.8), LR test (P <.001). When stratified by FTR case status, there were no differences in survival time by preventability adjudication in the non-FTR group (non-preventable: 0.2 days [95% CI, 0.1–0.2]) versus potentially preventable: 0.1 days (95% CI, 0.5–0.2) versus preventable: 0.24 days (95% CI, 0.24–unbounded; P = .2). In the FTR group, survival time increased with preventability adjudication (non-preventable: 3.1 days [95% CI, 2.1–4.8]) versus potentially preventable: 10.0 days (95% CI, 5.4–12.5) versus preventable: 14.9 (95% CI, 6.2–25.3; P = .004; Fig 3).
Fig 3.
Survival times with 95% confidence intervals by preventability adjudication in non-failure-to-rescue patients (A) and failure-to-rescue patients (B).
DISCUSSION
In this investigation of deaths after trauma at our level 1 academic institution, we found that nearly all deaths judged preventable were FTR cases. Conversely, we also found that the majority of FTR cases were deemed non-preventable by an expert mortality review. Ideally, when attempting to measure quality of care using outcome metrics, trauma centers should only be judged on the subset of negative outcomes that are truly preventable. Pragmatically, however, the issue of preventability may be difficult to ascertain reliably. In a systematic review of quality indicators often used to evaluate and compare trauma centers, Stelfox et al27 determined that that peer-reviewed preventable death was the quality metric with the most robust evidence in regard to its association with improved outcomes after implementation. Our results, with only 1.7% of all trauma deaths deemed preventable and 7.9% deemed potentially preventable, are consistent with published literature.28
When examining the relationship between preventability and death, deaths judged preventable or potentially preventable had greater predicted survival rates by both TRISS and ASCOT scoring systems than non-preventable deaths. We also found that patients with FTR deaths deemed preventable had a greater predicted survival rate than those deemed potentially preventable or non-preventable. The inverse association between predicted survivability and preventable death suggests that non-patient factors, such as physician decision-making or obstacles to escalation of care may be responsible. In an institutional investigation of the causes of preventable and potentially preventable deaths, Teixiera et al28 determined that preventable deaths usually were due to a delay in treatment, an error in clinical judgment, a missed diagnosis, or a technical error. Focus on these areas, therefore, is more likely to lead to a durable improvement in patient safety and rates of FTR. The finding that the FTR metric, as it is defined currently in the trauma population, includes mostly non-preventable deaths suggests that there is room for improvement with respect to precision and that the FTR metric may not be appropriate.
Other work investigating the contributions of patient demographics to complication and mortality rates have reported that the elderly have been shown to have greater mortality rates29 and poorer outcomes30 after injury than younger patients. With respect to race, African-American patients have been shown to have greater rates of complications and mortality than patients of other races, even when controlling for injury severity and co-morbid diseases.31 Additionally, some studies have demonstrated that women are less likely than men to develop complications after trauma, but women who do have a greater mortality rate than similarly injured men.32 In the subset of FTR deaths, patient factors that might be expected to be associated either positively or negatively with preventability status, such as patient demographics, injury severity score, and pre-existing conditions, were not different between groups. This finding is in keeping with the FTR theorem, in which the occurrence of a complication can be considered as a marker of patient complexity, because patients with complications are similarly complex, the subsequent FTR cohort is relatively insensitive to differences in patient demographics.1,16
In survival analysis, we found that there was clear separation of timing between FTR and non-FTR cases. Nearly 75% of non-FTR cases survived <1 day, whereas the median survival for FTR cases was ≈5 days. This finding was not unexpected, because many of the complications that create opportunity for FTR events take time to develop. Within FTR deaths, there was clear separation of Kaplan-Meier curves by preventability judgments such that on average, the longer a patient survived after the injury, the more likely the eventual death was to be judged preventable. It may be that many deaths that occur immediately after arrival to the trauma bay are perceived to be secondary to progression of unsurvivable injury, and therefore may be more likely to be considered non-preventable.33 Greater durations of stay also may allow for greater interaction between the patient and the trauma center, thereby increasing the opportunity for suboptimal patient care to occur.
As with any retrospective cohort study, our work has limitations. First, because only data from a single institution were used, the results may not be generalizable to institutions with varying patient populations and processes of care and efforts of quality improvement. Furthermore, we did not investigate all patient characteristics that have been shown elsewhere to be associated with FTR, such as insurance status,34 transfusion requirement, or admission lactate. It should be noted, however, that our complication rate, death rate, and preventability adjudications parallel closely those of other published studies, and thus we suspect our findings may in fact reflect a general paradigm. Second, the relatively low-moderate interrater reliability of classification of deaths by internal mortality review panels is a known limitation of this methodology. Because the adjudications reached by our review panel are not necessarily those that would have been reached by independent external reviewers, the association between FTR status and preventability adjudication will need to be confirmed in other cohorts or by blinded non-biased reviewers. Investigation of this question using independent external reviewers is an important step to eliminate potential bias in the determination of preventability. Finally, issues of preventability aside, this work does not address the “appropriateness” of deaths that occurred. For example, death may be an appropriate outcome after de-escalation of care for an elderly patient with multiple comorbidities at the request of family members. In this circumstance, failure to allow death would in fact represent a breakdown of the system35 and a worse quality of care. In other words, the preventable must be distinguished from the inevitable36 and because any interventions made by hospitals will likely be costly and time- and resource-intensive,37 appropriate and attainable targets must first be identified.
In conclusion, although we find strong evidence that those deaths identified as FTR by the traditional definition are associated strongly with potentially preventable and preventable adjudications by mortality panel review, the majority of FTR deaths were deemed to be non-preventable, suggesting that a better understanding of what is truly a failure of medical care is needed for FTR to be considered an accurate measure of hospital quality in the trauma population. As hospital quality and quality of care become increasingly common household terms, dissemination of what really is and is not high-quality care is of vital importance.
Acknowledgments
Supported by Award Number K12 HL 109009 from the National Heart, Lung, and Blood Institute.
Footnotes
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung, and Blood Institute or the National Institutes of Health.
All authors have made substantial contributions to all of the following: (1) the conception and design of the study, or acquisition of data, or analysis and interpretation of data, (2) drafting the article or revising it critically for important intellectual content, (3) final approval of the version to be submitted.
Presented as an abstract at the 11th Academic Surgical Congress in Jacksonville, FL, February 2–4, 2016.
References
- 1.Silber JH, Williams SV, Krakauer H, Schwartz JS. Hospital and patient characteristics associated with death after surgery. A study of adverse occurrence and failure to rescue. Medical Care. 1992;30:615–29. doi: 10.1097/00005650-199207000-00004. [DOI] [PubMed] [Google Scholar]
- 2.Ahmed EO, Butler R, Novick RJ. Failure-to-rescue rate as a measure of quality of care in a cardiac surgery recovery unit: A five-year study. Ann Thoracic Surg. 2014;97:147–52. doi: 10.1016/j.athoracsur.2013.07.097. [DOI] [PubMed] [Google Scholar]
- 3.Reddy HG, Shih T, Englesbe MJ, et al. Analyzing “failure to rescue”: is this an opportunity for outcome improvement in cardiac surgery? Ann Thorac Surg. 2013;95:1976–81. doi: 10.1016/j.athoracsur.2013.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ghaferi AA, Birkmeyer JD, Dimick JB. Variation in hospital mortality associated with inpatient surgery. N Engl J Med. 2009;361:1368–75. doi: 10.1056/NEJMsa0903048. [DOI] [PubMed] [Google Scholar]
- 5.Waits SA, Sheetz KH, Campbell DA, et al. Failure to rescue and mortality following repair of abdominal aortic aneurysm. J Vascular Surg. 2014;59:909–914. e1. doi: 10.1016/j.jvs.2013.10.078. [DOI] [PubMed] [Google Scholar]
- 6.Silber JH, Rosenbaum PR, Williams SV, et al. The relationship between choice of outcome measure and hospital rank in general surgical procedures: implications for quality assessment. Int J Qual Health Care. 1997;9:193–200. doi: 10.1093/intqhc/9.3.193. [DOI] [PubMed] [Google Scholar]
- 7.Ghaferi AA, Osborne NH, Birkmeyer JD, Dimick JB. Hospital characteristics associated with failure to rescue from complications after pancreatectomy. J Am Coll Surg. 2010;211:325–30. doi: 10.1016/j.jamcollsurg.2010.04.025. [DOI] [PubMed] [Google Scholar]
- 8.Amini N, Spolverato G, Kim Y, Pawlik TM. Trends in hospital volume and failure to rescue for pancreatic surgery. J Gastro Surg. 2015;19:1581–92. doi: 10.1007/s11605-015-2800-9. [DOI] [PubMed] [Google Scholar]
- 9.Farjah F, Backhus L, Cheng A, et al. Failure to rescue and pulmonary resection for lung cancer. J Thoracic Cardiovasc Surg. 2014;149:1365–71. doi: 10.1016/j.jtcvs.2015.01.063. [DOI] [PubMed] [Google Scholar]
- 10.Mulvey CL, Pronovost PJ, Gourin CG. Hospital volume and failure to rescue after head and neck cancer surgery. Otolaryngol Head Neck Surg. 2015;152:783–9. doi: 10.1177/0194599815570026. [DOI] [PubMed] [Google Scholar]
- 11.Haas B, Gomez D, Hemmila MR, Nathens AB. Prevention of complications and successful rescue of patients with serious complications: characteristics of high-performing trauma centers. J Trauma. 2011;70:575–82. doi: 10.1097/TA.0b013e31820e75a9. [DOI] [PubMed] [Google Scholar]
- 12.Glance L, Dick A, Meredith J, Mukamel D. Variation in hospital complication rates and failure-to-rescue for trauma patients. Ann Surg. 2011;253:811–6. doi: 10.1097/SLA.0b013e318211d872. [DOI] [PubMed] [Google Scholar]
- 13.Aiken LH, Clarke SP, Sloane DM, et al. Hospital nurse staffing and patient mortality, nurse burnout, and job satisfaction. JAMA. 2002;288:1987–93. doi: 10.1001/jama.288.16.1987. [DOI] [PubMed] [Google Scholar]
- 14.Aiken LH, Clarke SP, Cheung RB, et al. Education levels of hospital nurses and surgical patient mortality. JAMA. 2003;290:1617–23. doi: 10.1001/jama.290.12.1617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Silber JH, Kennedy SK, Evan-Shoshan O, et al. Anesthesiologist Board Certification and patient outcomes. Anesthesiology. 2002;96:1044–52. doi: 10.1097/00000542-200205000-00004. [DOI] [PubMed] [Google Scholar]
- 16.Silber JH, Rosenbaum PR, Ross RN. Comparing the contributions of groups of predictors: which outcomes vary with hospital rather than patient characteristics? JASA. 1995;90:7–18. [Google Scholar]
- 17.Silber JH, Romano PS, Rosen AK, et al. Failure-to-rescue comparing definitions to measure quality of care. Medical Care. 2007;45:918–25. doi: 10.1097/MLR.0b013e31812e01cc. [DOI] [PubMed] [Google Scholar]
- 18.Zafar SN, Shah AA, Zogg CK, et al. Morbidity or mortality? Variations in trauma centres in the rescue of older injured patients. Injury. 2016;47:1091–7. doi: 10.1016/j.injury.2015.11.044. [DOI] [PubMed] [Google Scholar]
- 19.Silber JH, Rosenbaum PR, Romano PS, et al. Hospital teaching intensity, patient race, and surgical outcomes. Arch Surg. 2009;144:113–20. doi: 10.1001/archsurg.2008.569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Holena DN, Earl-Royal E, Delgado MK, et al. Failure to rescue in trauma: coming to terms with the second term. Injury. 2016;47:77–82. doi: 10.1016/j.injury.2015.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hashmi ZG, Schneider EB, Castillo R, et al. Benchmarking trauma centers on mortality alone does not reflect quality of care: implications for pay-for-performance. J Trauma Acute Care Surg. 2014;76:1184–91. doi: 10.1097/TA.0000000000000215. [DOI] [PubMed] [Google Scholar]
- 22.Foundation PTS. Pennsylvania Trauma Systems Foundation. 2015 Available from http://www.ptsf.org.
- 23.Baker S, O’Niell B, Haddon W, Jr, Long W. The Injury Severity Score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14:187–96. [PubMed] [Google Scholar]
- 24.Pennsylvania Outcomes and Performance Improvement Measurement System (POPIMS) Operations Manual. Camp Hill, PA: Pennsylvania Trauma Systems Foundation; 2015. [Google Scholar]
- 25.Champion HR, Sacco WJ, Carnazzo AJ, et al. Trauma score. Crit Care Med. 1981;9:672–6. doi: 10.1097/00003246-198109000-00015. [DOI] [PubMed] [Google Scholar]
- 26.Committee on Medical Aspects of Automotive Safety. Rating the severity of tissue damage. I. The Abbreviate Scale. JAMA. 1971;215:277–80. doi: 10.1001/jama.1971.03180150059012. [DOI] [PubMed] [Google Scholar]
- 27.Stelfox H, Straus S, Nathens A, Bobranska-Artiuch B. Evidence for quality indicators to evaluate adult trauma care: a systematic review. Crit Care Med. 2011;39:846–59. doi: 10.1097/CCM.0b013e31820a859a. [DOI] [PubMed] [Google Scholar]
- 28.Teixiera PG, Inaba K, Hadjizacharia P, et al. Preventable or potentially preventable mortality at a mature trauma center. J Trauma. 2007;63:1338–47. doi: 10.1097/TA.0b013e31815078ae. [DOI] [PubMed] [Google Scholar]
- 29.Mondello S, Cantrell A, Italiano D, et al. Complications of trauma patients admitted to the ICU in level I academic trauma centers in the United States. BioMed Research International. 2014;2014:7. doi: 10.1155/2014/473419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Haas B, Gomez D, Xiong W, et al. External benchmarking of trauma center performance: have we forgotten our elders? Ann Surg. 2011;253:144–50. doi: 10.1097/SLA.0b013e3181f9be97. [DOI] [PubMed] [Google Scholar]
- 31.Chang D, Handly N, Abdullah F, et al. The occurrence of potential patient safety events among trauma patients: are they random? Ann Surg. 2008;247:327–34. doi: 10.1097/SLA.0b013e31815aab0d. [DOI] [PubMed] [Google Scholar]
- 32.Haider A, Crompton J, Oyetunji T, et al. Females have fewer complications and lower mortality following trauma than similarly injured males: a risk adjusted analysis of adults in the National Trauma Data Bank. Surgery. 2009;146:308–15. doi: 10.1016/j.surg.2009.05.006. [DOI] [PubMed] [Google Scholar]
- 33.Newgard CD. The validity of using multiple imputation for missing out-of-hospital data in a state trauma registry. Acad Emerg Med. 2006;13:314–24. doi: 10.1197/j.aem.2005.09.011. [DOI] [PubMed] [Google Scholar]
- 34.Bell TM, Zarzour BL. Insurance status is a predictor of failure to rescue in trauma patients at both safety net and non-safety net hospitals. J Trauma Acute Care Surg. 2013;75:728–33. doi: 10.1097/TA.0b013e3182a53aaa. [DOI] [PubMed] [Google Scholar]
- 35.Wakeam E, Hyder JA. Raising the bar for failure to rescue. Critical appraisal of current measurement and strategies to catalyze improvement. JAMA Surg. 2015;150:1023–4. doi: 10.1001/jamasurg.2015.1933. [DOI] [PubMed] [Google Scholar]
- 36.Pronovost PJ, Colantuoni E. Measuring preventable harm: helping science keep pace with policy. JAMA. 2009;301:1273–5. doi: 10.1001/jama.2009.388. [DOI] [PubMed] [Google Scholar]
- 37.Kao LS. Rescuing failures: can large data sets provide the answer? JAMA Surgery. 2014;149:124. doi: 10.1001/jamasurg.2013.3674. [DOI] [PubMed] [Google Scholar]