Abstract
Aims
To test the hypothesis that among non-treatment-seeking emerging adults (EA) who both use marijuana and have alcohol binges, a brief, longitudinally-delivered, developmentally-based motivational intervention would show greater reductions in the use of these two substances compared with a health education control condition.
Design
Parallel, two group, randomized controlled trial with follow-up interventions conducted at 1, 3, 6, and 9 months and final assessments at 12 and 15 months.
Setting
Hospital-based research unit in the United States.
Participants
Community-based 18–25 year olds who reported at least monthly binge drinking and at least weekly marijuana use.
Intervention
Motivational intervention focused primarily on themes of emerging adulthood (identity exploration, instability, self-focus, feeling in-between, a sense of possibilities) and the subjects' relationship to substance use (n=110) compared with an attention-matched health education control condition (n=116).
Measurements
The primary outcomes were days of binge alcohol, marijuana and dual use day as measured using the Timeline Followback Method analyzing the treatment by time interaction to determine relative differences in the rate of change between intervention arms.
Findings
At baseline, the mean rate (days / 30) of binge drinking was 5.23 (± 4.31), of marijuana use was 19.4 (± 10.0), and of dual (same day) use was 4.11 (± 4.13). Relative to baseline, there were reductions in the rate of binge alcohol use, marijuana use, and days of combined binge alcohol and marijuana use (p < .001) at all follow-up assessments. However, the treatment by time interaction was not statistically significant for alcohol (p = .37), for marijuana (p=.07), or for dual use (p=.55). Averaged over all follow-ups, mean reductions in binge, marijuana, and dual use days were 1.16, 1.45, and 1.08, respectively, in the health education arm, and 1.06, 1.69, and 0.96 in MI. Bayes factors were < .01 for frequency of binge alcohol use and frequency of dual binge alcohol and marijuana, and .016 for marijuana use.
Conclusions
A brief, longitudinally-delivered, developmentally-based motivational intervention for young adults did not produce reductions in binge alcohol, marijuana use, or dual use days relative to a control condition.
Keywords: alcohol, cannabis, multiple substance use disorders, brief intervention, emerging adults
Introduction
Worldwide, marijuana is used by nearly 182 million people for nonmedical purposes1 and globally nearly 6% of all deaths are attributable to harmful alcohol use2. In the United States, alcohol and marijuana are the most commonly used substances in the United States, with 138.3 and 22.2 million current users, respectively, aged 12 and above in 20153. The highest rates of use are among young adults between 18 and 25 years of age, where 37.7% report binge drinking and 19.6% report marijuana use in the last month, with men having higher rates than women4,5. There is also high rates of dual use in this age group as 80% of marijuana users also consume alcohol6, and up to 55% of alcohol users use marijuana7–13. Despite these high rates of substance use, and the well-known attendant problems associated with use—including psychosocial problems14–25, injuries13,26–28, accidents14,26,29,30, and health effects26,27,31–37—few alcohol or marijuana users seek specialty treatment38.
The prevalence of substance use, including alcohol and marijuana use, and other risk behavior peaks between the ages of 18 to 25, a period characterized by behavioral change, and identity consolidation. Some authors have termed this period “emerging adulthood” to capture the transition from adolescence to adulthood39, a time of defining one’s identity before settling into the roles of adult life. Behavioral risk-taking including substance use are forms of exploration and sensation-seeking that will likely later be constrained by growing economic, occupational, and familial concerns. Substance use is often part of the experimentation that occurs during the emerging adulthood period. Over this developmental period however, many in this age group experience an increasing awareness of how risk-taking behaviors will adversely impact future “adult” responsibilities39. This awareness, acceptance, and behavioral stabilization are central features of the transition to adulthood40.
Despite its explanatory utility in understanding the high rates of substance use in 18–25 year olds, the theory of emerging adulthood has not been explored as a possible framework for substance use interventions for young adults. Being able to consider their substance use in a developmental context may help young adults see the connections and longer-term impact between their use and the other areas of their life, and begin to make different choices because of this increased awareness. To date, brief motivational interventions (BMIs), not linked to developmental issues, have been tested over the past two decades for non-treatment-seeking persons, because of their limited contact time and low cost. Brief interventions have proven efficacious for decreasing alcohol consumption when applied in outpatient settings to hazardous and unhealthy drinkers41–46 across age groups, but have been ineffective for alcohol dependent persons not seeking treatment. In emerging adults47,48, recent meta-analyses have found small effects when examining the utility of BMI for alcohol use. Brief interventions have also addressed marijuana use among non-treatment-seekers in randomized trials, demonstrating efficacy among adolescents49–53, men (Stephens et al54,55, young persons opportunistically approached during primary care visits56, and community-recruited, non-treatment-seeking, young adult women57. Marijuana use reductions have been modest and attenuate over time, abstinence occurred rarely, and marijuana-related problems did not diminish significantly57. In some studies, readiness-to-change influenced treatment efficacy as persons with a desire to quit showed greater and more durable responses57,58. Of note, although many interventions target only a single substance, or target substance use generally59, participants are often polysubstance users9,49,56.
Among dual users—who are at heightened risk for psychosocial21–25,29 and mental health effects10,33–37—brief motivational interventions have modestly reduced both alcohol and marijuana use in adult populations9,60–62. A review of BMIs for alcohol among college students looking for secondary effects on marijuana use found no direct intervention effects on marijuana, but did find that as alcohol use decreased, marijuana use decreased as well63. In summary, in both hazardous alcohol use and marijuana brief intervention studies, the effect size is modest, treatment effects fade43,64 in the months following intervention, and the optimal timing and number of community-based booster sessions remain open to further research.
Based on this literature, we believed a brief intervention, which incorporated motivational interviewing strategies and techniques, to explicitly address emerging adult identity exploration themes—one of which was substance use—might offer an innovative lever to reduce risk-prone dual alcohol and marijuana consumption in a non-treatment seeking group. That is, we developed a brief motivational intervention addressing substance use that purposefully occurred within a broader conversation about age-specific life events prevalent in this young adult group65. Our goal was to help participants explore their future lives, expectations and developmental tasks, and to realize their goals and work towards those goals66, and how substance use might hold them back as they move into adulthood. Because other work with severe drug and alcohol users demonstrated that long-term, quarterly monitoring through regular brief “check-ups” is feasible, improves engagement and retention, and is effective in drug use reduction51,67,68, we developed an intervention that provides longitudinal contacts over nine months, longer than previous studies, a reorientation in keeping with primary medical care delivery.
The purpose of this randomized controlled trial was to test the hypothesis that among non-treatment-seeking emerging adults (EA) who both use marijuana and have alcohol binges, a brief, longitudinally-delivered, EA-themed motivational intervention would result in fewer binge alcohol and marijuana use days relative to a health education control condition over 15 months.
Methods
Design
Parallel, two group, randomized controlled trial with follow-up interventions conducted at 1, 3, 6, and 9-, months and final assessments at 12 and 15 months.
Participants
Study participants were enrolled between January 2012 and May 2016 in a “health behaviors study” among young adults. Participants were recruited via Southern New England Craigslist and Facebook advertising, and through advertisements placed in local college newspapers, on public transportation, and on commercial radio. Advertisements were worded slightly differently depending on the medium, but all included the 18–25 age requirement, mention of a research study about health behaviors, and the question “Have you recently used alcohol or marijuana?” Interested individuals called the study number or emailed the study address to receive a call back and were given a 10-minute anonymous phone screen. The screen included questions about basic demographics, substance use, sexual activity, mental health, and general health. Eligible individuals were invited for an in-person interview at the research site and offered compensation ($40)69,70.
Eligibility criteria for the study included being 18–25 years old, English-speaking, at least monthly binge drinking (4 or more drinks in a 2-hour period for women, 5 or more for men) and at least weekly marijuana use in the past three months, no drug use (other than nicotine, marijuana, or alcohol) once a week or more, living within 30 minutes of the research site and contact information for at least two verifiable locator persons. Of the 2,645 individuals screened by phone, 2,002 were ineligible. The most common reasons for ineligibility were not using both substances at the study threshold levels (976), having suicidal ideation (234), being outside the age range (148), cocaine or opioid use (81), and living at a distance (53). The remaining individuals were ineligible for other or multiple reasons. The 643 eligible persons were invited for an interview and 402 were either not interested (n=47 actively refused; n=54 passively refused, i.e. said they would call back to schedule an appointment, but never did), or did not keep a scheduled appointment (n=301) at the hospital-based research site.
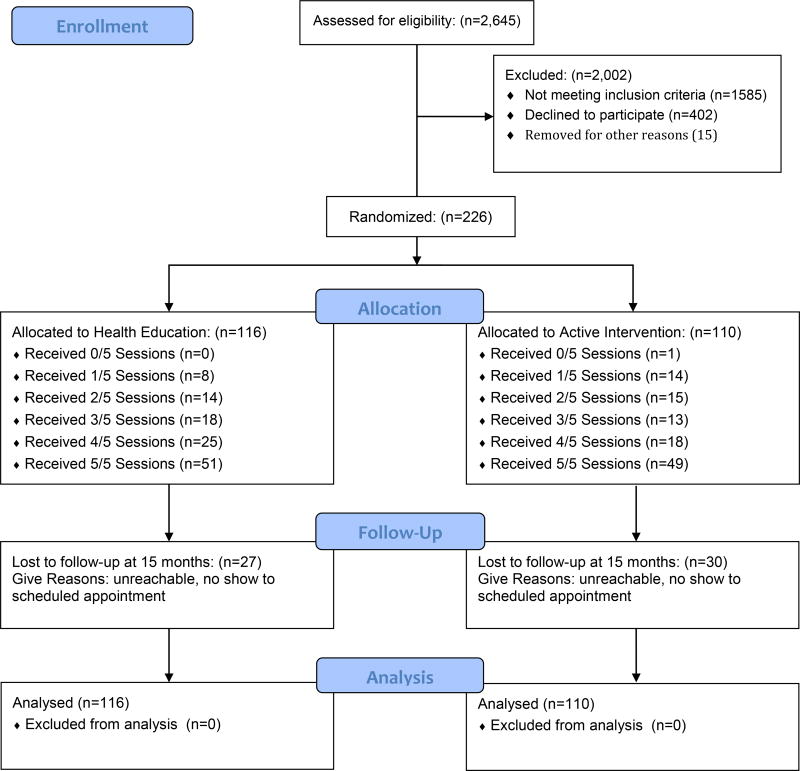
Two hundred and forty-one persons provided written informed consent and completed a baseline interview (the study was approved by the Institutional Review Board of a research hospital in Southern New England) after which 13 persons were found to be ineligible and 2 withdrew their participation. The final sample randomized for this trial included 226 persons (Figure 1).
Figure 1.
CONSORT Flow Diagram
Procedure
Schedule of the Intervention
Following the baseline assessment, participants were randomized to the active emerging adulthood motivational intervention (EA) condition or the health education (HE) condition 1:1 using random assignment software administrated by the research statistician, which generated a blocked random assignment sequence. The research assistants conducting study assessments were blind to the randomization. Study interventionists retrieved group assignment just prior to meeting with each participant for their initial intervention session. For each participant, five individual intervention sessions (EA or HE) were scheduled with a same-sex interventionist, each lasting approximately 20–30 minutes. The initial session was conducted on the same day immediately following the baseline assessment. The subsequent intervention sessions were conducted at 1-, 3-, 6-, and 9-months with follow-up assessments preceding each of these intervention sessions; follow-up assessments alone were also completed at 12-, and 15-months following the baseline assessment. Research staff performing the assessments was blinded to assigned condition. All assessments and intervention sessions were completed at the research site or by phone. Participants were compensated $40 for each of the first five assessment/intervention combined visits, $50 for the final two assessments, with a $50 bonus if all were completed. Participants were also entered into a raffle for movie or concert tickets during months in which they completed an assessment; one winner was chosen each calendar month.
Therapist Training, Adherence Coding, and Session Attendance
Therapist Training
Four interventionists—two women and two men, three clinical psychologists and one masters level clinician—conducted the study interventions. Because participants might be more comfortable speaking about certain issues with a therapist of the same gender, most specifically relationship issues, sexual, or traumatic experiences71,72 that might relate to emerging adult themes, we matched participant and therapist by gender. Two ninety-minute training sessions for intervention staff included: 1) a didactic presentation including a brief overview of the study and an overview of alcohol and marijuana use and consequences; 2) a demonstration role play of each intervention (EA and HE); and 3) opportunity for the study interventionists to practice the intervention using scripted role plays. Each interventionist demonstrated proficiency with two pilot participants in each condition prior to actual study recruitment.
Adherence Coding
After an initial training about the manual and the intervention and once inter-rater reliability was established, coders independent of this study rated adherence to the manual by each rating a set of audiotaped sessions (33% of EA sessions, 11% of HE sessions), using a study-specific coding instrument. . For the EA sessions, therapists were fully adherent 88.2% of the time. Therapists were fully adherent to the HE sessions 97.4% of the time. An additional rating assessing the presence of EA elements in the HE sessions was coded using a 1–10 scale, with 1 being “no EA treatment elements” present. The HE sessions were rated 1.04 for presence of EA treatment elements.
Session Attendance
Female participants assigned to EA participated in an average of 4.31 of 5 sessions, those assigned to HE participated in an average of 4.22 sessions. Male participants assigned to EA participated in an average of 3.13 of 5 sessions, those assigned to HE participated in an average of 3.49 sessions. The average length of the EA sessions was 26 minutes, and of the HE sessions was 22 minutes.
Intervention
Initial EA Session
The initial EA session focused primarily on emerging adulthood, allowing time towards the end for the development of a substance use Change Plan if the participant was interested in making a change. The session was based around the framing identity question— “Where do you see yourself in the next 1–5 years, and how do your current behaviors fit with these goals?” The beginning of the session was focused on describing the developmental phase of emerging adulthood, highlighting the themes associated with this phase (identity exploration, instability, self-focus, feeling in-between and a sense of possibilities39), and probing for examples from the participant’s own experiences when these themes played out and for the participant’s beliefs about what constitutes “completion” of the stage of emerging adulthood – that is, when did the participant think they would be a “developed” adult. Two worksheets—an Emerging Adults Circle Worksheet, which profiled various areas of the participant’s life and generated a discussion about which areas felt stable and which areas the participant would like to improve upon, and a Thoughts About Emerging Adulthood worksheet, which gave the participant a place to document what life events are in transition, and where a participant would like her/his life to be in both 1- and 5-years—were created to help explore experiences, values and beliefs, and to encourage the participant to think about their current experiences as part of the path that will lead to their desired future. The second half of the initial EA session focused on experimentation and risk behavior, and pulled for the participant’s own definition of these two concepts, the differences between them, their experiences with experimentation and risk, and what the participant expected their attitude toward experimentation/risk behavior to be like in 1- and 5-years. Blending the first and second halves of the discussion allowed the interventionist to highlight areas in which current substance use and/or other risk behaviors interfered with stated values and goals. The interventionist highlighted these areas of friction/conflict in a motivational interviewing-consistent manner, stating that what the participant chooses to do is up to them, but that the goal of the sessions was to encourage the participant to recognize that each of their experiences involves a choice s/he is making (what we called “micro-decisions”), and that these choices help or hinder progress towards stated goals for moving toward adulthood. At the end of the session, both Session 1 worksheets were provided to the participant to take home, and the next study appointment was set. If a participant was interested in reducing or eliminating substance use, the interventionist helped the participant create a Change Plan around this.
Second EA Session
During the second session a month later, the interventionist checked in with the participant about any “emerging adult” moments they might have had over the past month, where the participant recognized one of the themes discussed during the first session, or when they were more fully aware of making a decision in a deliberate and intentional manner. Interventionists supported participants’ reports that they were more aware of their decision process to use (or not use) and felt more in control and engaged with their decisions.
After a brief check-in about the previous month, the interventionist asked permission to review some of the substance-use related information the participant provided during the study assessment. The interventionist used this feedback to highlight “not-so-good-aspects” of the participant’s substance use, completing a standard motivational interviewing Decisional Balance worksheet, and to explore the participant’s interest in making changes in their substance use. For participants interested in making a change, the interventionist and the participant completed a standard Change Plan. As this was not a treatment intervention and participants were not obligated to reduce or quit their substance use, for those participants who did not want to change their substance use, the interventionist adapted the Change Plan process for any health behavior change the participant was interested in making as a way to model the process used when making a substance use-related change. Through the discussion of the Change Plan, participants specified the change to be made, the steps involved in the change, and ways in which others might be helpful. Participants were asked to generate potential barriers to change and to problem-solve ways to address those barriers. At the end of the session, Decisional Balance and Change Plan worksheets were given to all participants and the next study appointment was set. For those participants who did not complete a Change Plan, either for a substance-use related plan or another health behavior, the process for completing the Change Plan was described in case they were interested in completing the worksheet on their own before the next session.
Check-up Intervention Sessions (Sessions 3, 4 and 5)
Participants assigned to the EA group received reinforcement or “check-up” sessions with the original interventionist at 3-, 6- and 9-months. Interventionists reviewed information from the previous sessions, including the participant’s views of change and exploration related to emerging adulthood, and ”not-so-good-things” about substance use, and explored updates to these areas, again incorporating feedback about current substance use levels from the study assessment. As in Session 2, there was more focus during Sessions 3, 4 and 5 on the participant’s current substance use, how this related to 1-and 5-year goals, and their current stance related to changing substance use. Change Plans from earlier sessions, if created, were reviewed, barriers to completing the Change Plan were discussed and problem-solved, and successful completion of the Change Plan was supported. If the participant indicated that the goals set in the previous session were fully met, the interventionist assisted in determining whether further goals should be set, and explored strategies to help the participant maintain their achieved goals. At each of the check-in sessions, participants were encouraged to consider developing a Change Plan if they had not already done so, and for those who chose to complete the worksheet, the interventionist followed the same procedure as described above.
Health Education Control
A Health Education intervention served as the control condition73–75. The duration and timing of these five sessions was identical to the EA condition. The five sessions covered: 1) sleep and sleep hygiene, 2) food and nutrition, 3) exercise, 4) health prevention (colds and flus) and 5) stress and stress management. These sessions were primarily didactic and consisted of handouts and videos reviewed by the interventionist, followed by a brief discussion as to whether participants had been exposed to this information in the past and provision of local and web-based resources about the topic.
Measures
Outcomes
The primary outcomes were days of binge alcohol use, marijuana and dual use.
Covariates
Participants were asked to provide demographic information, including age, race/ethnicity, and gender. School status was collected with the question “Are you currently in school?” Response options were “Full time, part time, not in school.” Employment status was queried with “Are you currently working?” with response options “Full time, part time, unemployed or laid off and looking for work, unemployed or laid off and not looking for work, on disability.”
Alcohol and Marijuana Use
At the baseline assessment participants were asked to recall the 90 days prior to the interview using the Timeline FollowBack (TLFB) method76. Participants indicated days in which they used alcohol and/or marijuana and the quantity of alcohol used on drinking days. We defined binge alcohol use as 4 or more drinks for women, 5 or more for men, in a two-hour period. At the 1-, 3-, 6-, 9-, 12-, and 15-month assessments, the TLFB was used to assess marijuana and alcohol use since the date of the participant’s previous assessment. Other measures included age of initiation of alcohol and marijuana use, which was assessed by asking, “How old were you when you had your first drink of alcohol (other than a few sips)?” and “How old were you when you first tried marijuana?” Alcohol use and cannabis use DSM-IV-TR diagnoses were assessed using the SCID77. The Short Inventory of Problems (SIP) for alcohol adverse consequences78 and the Marijuana Problem Severity (MPS)79 scales, each assessing problems in the past 90 days, were completed. Desire to reduce alcohol or marijuana use was assessed by adapting the Thoughts About Abstinence Scale80 which asked participants to rate their current desire to reduce using a 1 to 10 scale with 1 being “no desire” and 10 being “a very great desire.” Participants were asked about desire to reduce marijuana and alcohol separately.
Statistical Analysis
We present descriptive statistics to summarize the baseline characteristics of participants. We used random effects logistic regression to determine if loss to follow-up was systematically associated with treatment assignment, demographic characteristics, or baseline levels of substance use. We express the outcomes as count variables giving days of use per 30 TLFB days. An examination of the distributions indicated over dispersion (variance > mean). Therefore we used random effects negative binomial regression to estimate and test the effects of intervention. For each outcome we estimated intervention effects as the treatment by linear time, and treatment by unconditional time interaction effects. In the unconditional time models, each follow-up assessment was represented as separate dummy variables. We used likelihood ratio difference in chi-square (LR2) tests to test the statistical significance of intervention effects and to compare nested models. We present results for the best fitting model (treatment by linear time or treatment by unconstrained time).
The primary outcomes were days of binge drinking, marijuana and dual use day as measured using the Timeline Followback Method. Our primary outcomes analysis of alcohol and marijuana use was guided by intent-to-treat principles. The results we report used all available data and maximum likelihood estimation which is robust under the assumption of missing at random (MAR). Planned covariates included age, gender, and ethnicity as potential confounders. Age was included because the population studied is transitioning from minority to majority status. Gender was included because of known differences in alcohol metabolism and sociocultural differences in definitions of appropriate alcohol use. Ethnicity was included because different racial/ethnic groups have been shown to have different rates of alcohol and marijuana use81. Additionally, the SIP and MPS scales were included as covariates in models evaluating the effects of intervention on binge alcohol and marijuana use, respectively. Models also included any variables that significantly (p < .10) predicted loss to follow-up. Coefficients for the treatment by time interaction give the relative difference in the rate of change between intervention arms. Under the hypothesis that active treatment will reduce frequency of substance use more for those in active intervention than those in the control condition, we would expect these coefficients to be < 1.0 and statistically significant. The study was powered to detect differences of about 20% in rates of use. Based on means and standard deviations reported in prior brief motivational interventions this would approximate standardized reductions in mean rates of about .4 at end of treatment. To further describe substantive effect sizes, we also report between group differences in predicted rates of use. The rates reported assume a random effect of 0 and are evaluated with all variables other than treatment condition and time evaluated at their mean. Based on model BIC statistics we calculated and report Bayes factors82. Bayes factors can be used to compare the likelihood of two or more models, given the observed data. As calculated here, Bayes factors < 1 favor the null model, and Bayes factors < .3 are generally interpreted to indicate no difference between intervention groups. All statistical analyses were conducted in Stata 14.183.
Results
Sample and Follow-up
Participants averaged 21.2 (± 2.02) years of age, 55.3% were male, 65.5% were non-Latino White, 10.6% were African-American, 12.4% were Hispanic, and 11.5% identified other racial or ethnic origins (Table 1). Almost half (47.4%) were full-time students, 14.2% were part-time students, and 38.5% were not enrolled in school. About 15.0% reported they worked full-time and 38.9% worked part-time. Mean age of initiating alcohol and marijuana use was 15.3 (± 2.22) and 15.2 (± 2.45), respectively.
Table 1.
Demographic Characteristics, Substance Use Behaviors, and Follow-Up Rates (n = 226).
| n (%) | Mean (± SD) | Median | Range | |
|---|---|---|---|---|
| Age | 21.2 (± 2.02) | 21 | 18 – 25 | |
| Gender (Male) | 125 (55.3%) | |||
| Race/Ethnicity | ||||
| Caucasian | 148 (65.5%) | |||
| African-American | 24 (10.6%) | |||
| Hispanic | 28 (12.4%) | |||
| Other | 26 (11.5%) | |||
| School Status | ||||
| Full-Time | 107 (47.4%) | |||
| Part-Time | 32 (14.2%) | |||
| Not Enrolled | 87 (38.5%) | |||
| Employment Status | ||||
| Full-Time | 34 (15.0%) | |||
| Part-Time | 88 (38.9%) | |||
| Other | 104 (46.0%) | |||
| Age Initiated Alcohol Use | 15.3 (± 2.22) | 15 | 8 – 21 | |
| Age Initiated MJ Use | 15.2 (± 2.45) | 15 | 7 – 24 | |
| Alcohol Use Ratea | 9.00 (± 5.60) | 9 | 1 – 30 | |
| Binge Drinking Ratea | 5.23 (± 4.31) | 4 | 0 – 27 | |
| Marijuana Use Ratea | 19.4 (± 10.0) | |||
| Dual Binge & MJ Ratea | 4.11 (± 4.13) | |||
| SIP | 6.92 (± 6.19) | |||
| MJ Problem Severity | 5.22 (± 3.55) | |||
| Desire to Reduce Alc. Use | 145 (64.2%) | |||
| Desire to Reduce MJ Use | 159 (70.4%) | |||
| Observed @ 1-Mo | 195 (86.3%) | |||
| Observed @ 3-Mo | 178 (78.8%) | |||
| Observed @ 6-Mo | 173 (76.6%) | |||
| Observed @ 9-Mo | 162 (71.7%) | |||
| Observed @ 12-Mo | 161 (71.2%) | |||
| Observed @ 15-Mo | 160 (70.8%) | |||
| # of Post BL Assessments | 4.55 (± 1.98) | 6 | 0 – 6 | |
| Obs. @ 1+ Assessments | 211 (93.4%) |
Days of use / 30 TLFB days assessed using a 90-Day TLFB.
At baseline, the mean rate (days / 30) of alcohol use was 9.00 (± 5.60), the mean rate of binge drinking was 5.23 (± 4.31), the mean rate of marijuana use was 19.4 (± 10.0), and the mean rate of dual (binge drinking and marijuana on the same day) use was 4.11 (± 4.13). Mean scores on the SIP and MPS were 6.92 (± 6.19) and 5.22 (± 3.55), respectively. Thirty-five persons (15.5%) met DSM criteria for alcohol dependence, and 64 (28.3%) for marijuana dependence. One hundred forty-five (64.2%) expressed some desire to reduce use of alcohol and 159 (70.4%) expressed some desire to reduce use of marijuana. Follow-up rates were 86.3%, 78.8%, 76.6%, 71.7%, 71.2%, and 70.8% at 1-, 3-, 6-, 9-, 12-, and 15-months, respectively. On average, participants completed 4.55 (± 1.98) follow-up assessments and 93.4% were observed on at least 1 follow-up. At the 15-month interview, the completion rate was 70.8%.
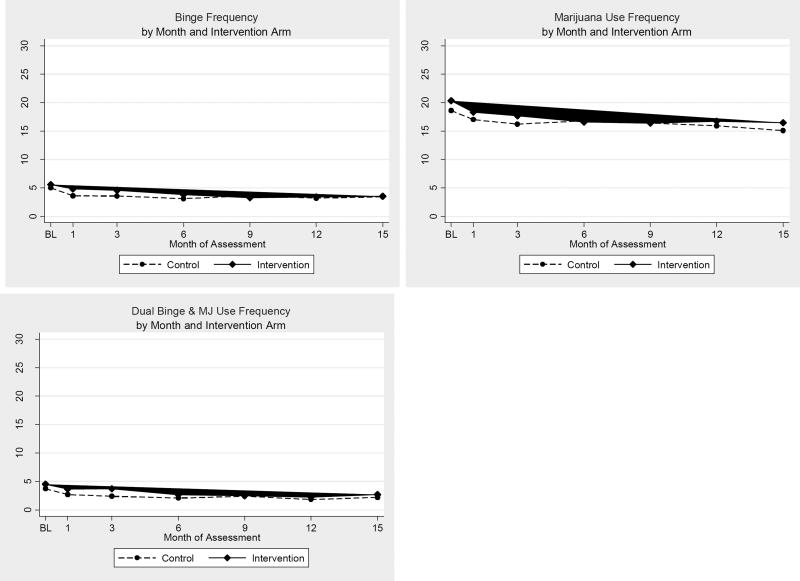
We observed statistically significant reductions in the rate binge alcohol use (LR2 = 84.74, df = 6, p < .001), marijuana use (LR2 = 58.62, df = 6, p < .001), and days of combined binge alcohol and marijuana use (LR2 = 25.50, df = 6, p < .001). Relative to baseline, rates of use on all three outcomes was significantly lower at all follow-up assessments in the combined sample. Figure 2 plots the observed mean rates for the outcome variables by month and treatment arm. For both study arms, the observed mean rates of use decrease between baseline and 1-month, but thereafter the growth trajectories exhibit little change during months 1 to 15.
Figure 2.
Mean 30-Day Rates of Binge Drinking and Marijuana Use by Month of Assessment and Intervention Condition.
We ran random effects logistic regression models individually evaluating all variables described in Table 1 as predictors of loss to follow-up. Males had a significantly higher likelihood of being lost to follow-up than females (OR = 3.96, 95%CI 1.50; 10.43, z = −2.78, p = .005). Loss to follow-up was not associated significantly (p > .10) with any of the other evaluated baseline characteristics.
Outcome Analysis
For days of binge alcohol use (LR2 = 33.23, df = 10, p < .001) and days of dual use (LR2 = 37.86, df = 10, p < .001) the unconstrained time model fit the data significantly better than the linear time model. The unconstrained time model did not fit the data significantly (LR2 = 13.62, df = 10, p = .191) better than the linear time model when evaluating the effects of intervention on days of marijuana use. Results for the best fitting negative binomial regression models are given in Table 2.
Table 2.
Random-Effects Negative Binomial Regression Models Testing the Effect of Intervention on the 30 Day Rate of Binge Alcohol Use, Marijuana Use, and Dual Binge and Marijuana Use (n = 226).
| BINGE ALCOHOL USE | MARIJUANA USE | DUAL SUBSTANCE USE | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|||||||||
| IRR | 95%CI | p = | IRR | 95%CI | p = | IRR | 95%CI | p = | |
| Age | 0.94 | (0.80 – 0.98) | 0.005 | 1.04 | (1.00 – 1.09) | 0.060 | 0.97 | (0.92 – 1.02) | 0.211 |
| Gender (Male) | 1.19 | (0.98 – 1.44) | 0.084 | 1.59 | (1.33 – 1.91) | <0.001 | 1.31 | (1.06 – 1.63) | 0.014 |
| Race/Ethnicity | |||||||||
| African-American | 0.99 | (0.72 – 1.36) | 0.954 | 1.08 | (0.81 – 1.44) | 0.582 | 1.09 | (0.76 – 1.56) | 0.637 |
| Latino | 0.85 | (0.64 – 1.14) | 0.272 | 0.69 | (0.53 – 0.90) | 0.006 | 0.97 | (0.70 – 1.35) | 0.875 |
| Other | 0.83 | (0.62 – 1.12) | 0.225 | 0.94 | (0.72 – 1.24) | 0.686 | 0.86 | (0.63 – 1.19) | .368 |
| Caucasian [REF] | [1.00] | [1.00] | |||||||
| Short Inventory Problems | 1.03 | (1.01 – 1.05) | <0.001 | NA | 1.03 | (1.01 – 1.05) | .003 | ||
| MJ Problem Severity | NA | 1.10 | (0.99 – 1.04) | .273 | 0.98 | (0.95 – 1.01) | .259 | ||
| Unconstrained Time | |||||||||
| Month 1 | 0.67 | (0.55 – 0.81) | <0.001 | NA | 0.67 | (0.53 – 0.83) | <0.001 | ||
| Month 3 | 0.67 | (0.56 – 0.81) | <0.001 | NA | 0.60 | (0.47 – 0.75) | <0.001 | ||
| Month 6 | 0.61 | (0.50 – 0.74) | <0.001 | NA | 0.55 | (0.43 – 0.71) | <0.001 | ||
| Month 9 | 0.68 | (0.56 – 0.83) | <0.001 | NA | 0.62 | (0.49 – 0.79) | <0.001 | ||
| Month 12 | 0.61 | (0.49 – 0.75) | <0.001 | NA | 0.48 | (0.37 – 0.63) | <0.001 | ||
| Month 15 | 0.63 | (0.78 – 1.23) | <0.001 | NA | 0.58 | (0.45 – 0.74) | <0.001 | ||
| Linear Time | NA | 0.98 | (0.95 – 1.36) | 0.155 | NA | ||||
| Intervention | 0.98 | (0.78 – 1.23) | 0.874 | 1.14 | (0.95 – 1.35) | 0.155 | 1.05 | (0.81 – 1.36) | .736 |
| Int. by Unconstrained Time | |||||||||
| Int. X Month 1 | 1.17 | (0.897 – 1.52) | 0.255 | NA | 1.01 | (0.74 – 1.39) | 0.941 | ||
| Int. X Month 3 | 1.09 | (0.83 – 1.43) | 0.543 | NA | 1.16 | (0.84 – 1.61) | 0.377 | ||
| Int. X Month 6 | 1.04 | (0.78 – 1.39) | 0.771 | NA | 0.97 | (0.69 – 1.38) | 0.876 | ||
| Int. X Month 9 | 0.82 | (0.60 – 1.10) | 0.185 | NA | 0.80 | (0.56 – 1.14) | 0.218 | ||
| Int. X Month 12 | 0.88 | (0.65 – 1.20) | 0.422 | NA | 0.89 | (0.61 – 1.30) | 0.561 | ||
| Int. X Month 15 | 0.86 | (0.63 – 1.17) | 0.337 | NA | 0.81 | (0.56 – 1.17) | 0.270 | ||
| Int. by Linear Time | NA | 0.99 | (0.98 – 1.01) | 0.075 | NA | ||||
| Constant | 17.4 | (6.08 – 49.9) | <0.001 | 2.14 | (0.80 – 5.72) | 0.127 | 6.29 | (1.87 – 21.1) | 0.003 |
NA = We present results from the best fitting model testing the treatment by time interaction. The SIP was included in models involving binge alcohol use, and the MPS was included in models involving marijuana use.
Controlling for age, gender, ethnicity, and the SIP, the treatment by time interaction effect on days of binge alcohol use was not statistically significant (LR2 = 6.49, df = 6, p = .371). Coefficients for time give the expected factor change in the number of binge alcohol days for persons in the control arm; relative to baseline, persons in the control arm had significantly lower rates of binge alcohol use at all follow-up assessments. The coefficient for the main effect of treatment gives the factor difference in the number of binge alcohol use days at baseline; the OR was 0.98 and not statistically significant (p = .874). Coefficients for the treatment by time interaction indicate that those randomized to intervention had slightly smaller reductions in binge alcohol use at 1-, 3-, and 6-months, but slightly larger reductions at 9-, 12-, and 15-month assessments (Table 2), although the substantive magnitude of between group differences is small and does not approach statistically significant levels at any follow-up assessment.
For marijuana use days, the treatment by linear time interaction effect was not statistically significant (LR2 = 3.23, df = 1, p = .072). When comparing intervention groups with respect to rates of marijuana use the treatment by time interaction effect was not statistically significant. Substantively, persons randomized to active intervention had slightly (OR = 0.99, 95%CI 0.98; 1.01) but not significantly larger linear reductions in marijuana use days over the 15 month follow-up than those randomized to HE.
The overall effect of intervention on dual use was also not statistically significant (LR2 = 4.95, df = 6, p = .550). Coefficients estimating intervention effects on dual use days were directionally inconsistent across time, substantively small, and none approached statistically significant levels (Table 2). There was evidence of unintended treatment effects or harms in either treatment group.
Using the largest difference at any time point which directionally favored the intervention arm, those randomized to EA were predicted to have about a .6 day larger reduction in binge drinking at 9-months, a 1.47 day larger reduction in days of marijuana use at 15 months, and a .5 day larger reduction in dual use at 15 months. Relative to common baseline standard deviations, these represent differences of about .14, .15, and .12, respectively. For all models, the BIC statistic favored the null model. Bayes factors were < .01 for frequency of binge alcohol use and frequency of dual binge alcohol and marijuana, and .016 for marijuana use.
We conducted an auxiliary analysis testing for treatment effects among persons expressing any desire to reduce alcohol use (n = 145) for alcohol outcomes or any desire to reduce marijuana (n = 159) when analyzing rate of marijuana use. Neither the treatment by linear time nor the treatment by unconditional time interactions approached statistically significant levels in any of these comparisons. Tests for treatment by linear time interactions were (LR2 = 1.96, df = 1, p = .172) for rate of binge drinking, and (LR2 = 1.15, df = 1, p = .284) for rate of using marijuana. Test statistics for the treatment by unconstrained time interactions were (LR2 = 6.52, df = 6, p = .368), and (LR2 = 9.65, df = 6, p = .472) for binge alcohol use, and rate of marijuana use, respectively. We used persons who had a desire to quit either using either alcohol or marijuana (n = 188) when evaluating dual substance use. Again, neither the treatment by linear time (LR2 = 2.84, df = 1, p = .091) nor treatment by unconstrained time (LR2 = 4.45, df = 6, p = .615) was statistically significant.
Discussion
In this randomized controlled trial among non-treatment-seeking young adults who used both alcohol and marijuana, a brief, multi-session, longitudinally-delivered intervention based on emerging adulthood theory did not produce greater reductions in binge alcohol, marijuana use or dual use days relative to a health education control condition. Our study focused on the age group with the highest alcohol and marijuana use prevalence nationally, had important strengths in that it included students and non-students, was half female, and had wide ethnic diversity.
There is evidence supporting a variety of effective intervention approaches for adult alcohol and marijuana users who are interested in treatment to cease or reduce use84,85. Yet among the 19.8 million Americans aged 12 years or older who have used marijuana, fewer than 5% seek formal drug treatment38. Similarly there are 136.9 million who have used alcohol in the past month and 60.1 million binge drinkers, yet only about 4% of binge drinkers and fewer than 2% of all current drinkers seek formal alcohol treatment38. Most young adults who use marijuana also do not perceive a need for reduction or treatment and do not seek care86. Non-treatment-seekers are often not ready to stop using, or may be ambivalent about stopping because seeking treatment implies that they have a “drug problem.” They may experience few negative consequences or a social environment supporting their use, or under-estimate that adverse life experience may indeed be related to substance use. It is possible that frequent users may deny problems related to their use to reduce cognitive dissonance while continuing to use heavily87. Still, previous work suggests that many users may, upon review, decide to change their substance use even if they are initially ambivalent88. Despite using clinicians experienced with motivational interventions, our intervention, with its added focus on developmental issues salient for this age group, did not help participants with behavior change, even those who had some desire to reduce either alcohol or marijuana.
There have been reports of brief interventions to reduce marijuana or binge alcohol use among persons not ready to approach formal treatment45,52,88,89. Other BMIs have reduced marijuana52,88,89 or binge alcohol use among young adults for short periods45. Although BMIs targeting dual alcohol and marijuana use in incarcerated adolescents90, adult ED patients62, and young adults with psychological distress and depression60,61 were shown to reduce alcohol and/or marijuana use, the effects were small61 and notable reductions in one or both substances were also noted in the comparison groups91.
Our lack of treatment effect may have multiple explanations. First, these young adults might believe substance use is normative. Dual users may socialize with other dual users, reinforcing the perceived norm of substance use. In addition, during the years of this study the social environment for marijuana use became less disapproving92 and the national discussion around legalizing marijuana increased notably so there may be greater resistance to change because marijuana is more socially acceptable and viewed as harmless. Still, with a mean age of 20, this young cohort might taper their use post-study participation as they get older and have greater life responsibilities93. Second, our participants had high rates of marijuana use, on average 19 days per month, with relatively high rates of marijuana-related problems and drug dependence; more intensive interventions may be needed for heavier users. Participants reported having few problems related to alcohol use, thereby lowering their motivation to reduce. Third, dual use participants may be more invested in substance use as a form of experimentation during this life period. Fourth, dual users may be experiencing some potentiation effect such that marijuana enhances the use of alcohol and vice versa, leading to a disinterest in reducing or quitting either. Dual users may be using these substances as forms of “coping” with more bothersome psychological symptoms94. Finally, perhaps the emerging adults here with an average age of 20 may still be too young to successfully reflect on their own risk behaviors and the emerging adult framework had little resonance. Therefore, while this self-reflective type of intervention may not work for them, perhaps it would be more effective with a slightly older group who have entered adulthood.
Among variables that influence treatment efficacy, willingness to alter one’s substance use behaviors has been important. Recent work has found that lower readiness-to-change predicts reduced intervention efficacy among young adult alcohol users95,96 and prolonged time in the “contemplation stage” can increase use97, although among non-treatment-seeking marijuana users followed naturalistically, initial change goal was a poor predictor of outcome98. In this study, readiness to reduce alcohol or marijuana did not influence treatment outcomes. Dupont et al.,97 suggested the scope of motivational interventions be widened to explore the reasons unmotivated individuals remain engaged in interventions despite making no meaningful change.
This trial had limitations. Substance use outcomes were based on self-report, although they were assessed by trained staff using validated instruments and procedures to aid recall and minimize bias. Second, we did not measure other potential moderating variables (e.g., social support). Third, we had a broader marijuana use inclusion criterion than other studies. Fourth, we did not use MITI coding for motivational interviewing fidelity ratings because quantifying the MI evoking change elements measured on the MITI were not central to our intervention99. Therefore, it cannot be determined whether our negative findings can be attributed to motivational interviewing here; rather, they may be attributed to either the developmental approach and/or our variation of standard motivational interviewing-based treatment. Fifth, the intervention sessions reviewed for treatment manual adherence were randomly chosen but because many were performed by phone, creating technical difficulties with recording, and some participants refused to allow recording, the sessions reviewed may not be representative of all sessions. Finally, only one-third of study-eligible young adults enrolled in this trial, reducing generalizability.
Despite having a high prevalence of marijuana and binge alcohol use young adults typically do not seek help for substance-related problems, but their high dual use warrants attention and intervention. Our findings suggest that an emerging-adult focused, motivational EA intervention for substance use did not influence rates of alcohol or marijuana use beyond an attention-matched control condition. Gaining a better understanding of the treatment components needed to change the behavior of the wide range of young adults who do not seek more formal treatment is important to reduce the impact of dual substance use in this age group.
Acknowledgments
This study was funded by the National Institute on Alcohol Abuse and Alcoholism (R01AA020509). Trial registered at clinicaltrials.gov; Clinical Trial # NCT01473719, https://clinicaltrials.gov/ct2/show/NCT01473719. Registration prior to participant enrollment.
Footnotes
The authors declare no conflict of interest.
References
- 1.World Health Organization. The health and social effects of nonmedical cannabis use. Geneva, Switzerland: 2016. [Google Scholar]
- 2.World Health Organization. Alcohol Fact Sheet. 2015 Jan; http://www.who.int/mediacentre/factsheets/fs349/en/
- 3.Center for Behavioral Health Statistics and Quality. Substance Abuse and Mental Health Services Administration; 2016. Key substance use and mental health indicators in the United States: Results from the 2015 National Survey on Drug Use and Health. (HHS Publication No. SMA 16-4984, NSDUH Series H-51) Retrieved from http://www.samhsa.gov/data/ [Google Scholar]
- 4.Center for Behavioral Health Statistics and Quality. Substance Abuse and Mental Health Services Administration; 2015. Behavioral health trends in the United States: Results from the 2014 National Survey on Drug Use and Health. (HHS Publication No. SMA 15-4927, NSDUH Series H-50) Retrieved from http://www.samhsa.gov/data/ [Google Scholar]
- 5.Johnston LD, M OMP, Bachman JG, Schulenberg JE, Miech RA. Monitoring the Future national survey results on drug use, 1975–2014: Volume 2, College students and adults ages 19–55. Ann Arbor, MI: Institute for Social Research, The University of Michigan; 2015. [Google Scholar]
- 6.Pape H, Rossow I, Storvoll EE. Under double influence: assessment of simultaneous alcohol and cannabis use in general youth populations. Drug Alcohol Depend. 2009;101(1–2):69–73. doi: 10.1016/j.drugalcdep.2008.11.002. [DOI] [PubMed] [Google Scholar]
- 7.Booth BM, Kirchner JE. Correlates and 6-month outcomes for co-occurring cannabis use in rural and urban at-risk drinkers. Substance Use & Misuse. 2001;36(6–7):717–733. doi: 10.1081/ja-100104087. [DOI] [PubMed] [Google Scholar]
- 8.Earleywine M, Newcomb MD. Concurrent versus simultaneous polydrug use: prevalence, correlates, discriminant validity, and prospective effects on health outcomes. Exp Clin Psychopharmacol. 1997;5(4):353–364. doi: 10.1037//1064-1297.5.4.353. [DOI] [PubMed] [Google Scholar]
- 9.Magill M, Barnett NP, Apodaca TR, Rohsenow DJ, Monti PM. The role of marijuana use in brief motivational intervention with young adult drinkers treated in an emergency department. J Stud Alcohol Drugs. 2009;70(3):409–413. doi: 10.15288/jsad.2009.70.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Midanik LT, Tam TW, Weisner C. Concurrent and simultaneous drug and alcohol use: results of the 2000 National Alcohol Survey. Drug Alcohol Depend. 2007;90(1):72–80. doi: 10.1016/j.drugalcdep.2007.02.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shillington AM, Clapp JD. Heavy alcohol use compared to alcohol and marijuana use: do college students experience a difference in substance use problems? J Drug Educ. 2006;36(1):91–103. doi: 10.2190/8PRJ-P8AJ-MXU3-H1MW. [DOI] [PubMed] [Google Scholar]
- 12.Substance Abuse and Mental Health Services Administration. The NSDUH Report: Concurrent Illicit Drug and Alcohol Use. Rockville, MD: Office of Applied Studies; 2009. [Google Scholar]
- 13.Woolard R, Nirenberg TD, Becker B, et al. Marijuana use and prior injury among injured problem drinkers. Acad Emerg Med. 2003;10(1):43–51. doi: 10.1111/j.1553-2712.2003.tb01975.x. [DOI] [PubMed] [Google Scholar]
- 14.Wechsler H, Lee JE, Kuo M, Seibring M, Nelson TF, Lee H. Trends in college binge drinking during a period of increased prevention efforts. Findings from 4 Harvard School of Public Health College Alcohol Study surveys: 1993–2001. J Am Coll Health. 2002;50(5):203–217. doi: 10.1080/07448480209595713. [DOI] [PubMed] [Google Scholar]
- 15.Connor J, Gray A, Kypri K. Drinking history, current drinking and problematic sexual experiences among university students. Aust N Z J Public Health. 2010;34(5):487–494. doi: 10.1111/j.1753-6405.2010.00595.x. [DOI] [PubMed] [Google Scholar]
- 16.White A, Hingson R. The burden of alcohol use: excessive alcohol consumption and related consequences among college students. Alcohol research : current reviews. 2013;35(2):201–218. [PMC free article] [PubMed] [Google Scholar]
- 17.Powers J, Duffy L, Burns L, Loxton D. Binge drinking and subsequent depressive symptoms in young women in Australia. Drug Alcohol Depend. 2016;161:86–94. doi: 10.1016/j.drugalcdep.2016.01.019. [DOI] [PubMed] [Google Scholar]
- 18.Mason-Jones AJ, Cabieses B. Alcohol, binge drinking and associated mental health problems in young urban Chileans. PLoS One. 2015;10(4):e0121116. doi: 10.1371/journal.pone.0121116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aertgeerts B, Buntinx F. The relation between alcohol abuse or dependence and academic performance in first-year college students. J Adolesc Health. 2002;31(3):223–225. doi: 10.1016/s1054-139x(02)00362-2. [DOI] [PubMed] [Google Scholar]
- 20.Wolaver AM. Effects of heavy drinking in college on study effort, grade point average, and major choice. Contemporary Economic Policy. 2002;20(4):415–428. [Google Scholar]
- 21.Zwerling C, Ryan J, Orav EJ. The efficacy of preemployment drug screening for marijuana and cocaine in predicting employment outcome. JAMA. 1990;264(20):2639–2643. [PubMed] [Google Scholar]
- 22.Fergusson DM, Horwood LJ, Beautrais AL. Cannabis and educational achievement. Addiction. 2003;98(12):1681–1692. doi: 10.1111/j.1360-0443.2003.00573.x. [DOI] [PubMed] [Google Scholar]
- 23.Chun TH, Spirito A, Hernandez L, et al. The significance of marijuana use among alcohol-using adolescent emergency department patients. Acad Emerg Med. 2010;17(1):63–71. doi: 10.1111/j.1553-2712.2009.00615.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lynskey M, Hall W. The effects of adolescent cannabis use on educational attainment: a review. Addiction. 2000;95(11):1621–1630. doi: 10.1046/j.1360-0443.2000.951116213.x. [DOI] [PubMed] [Google Scholar]
- 25.Patton GC, Coffey C, Lynskey MT, et al. Trajectories of adolescent alcohol and cannabis use into young adulthood. Addiction. 2007;102(4):607–615. doi: 10.1111/j.1360-0443.2006.01728.x. [DOI] [PubMed] [Google Scholar]
- 26.Hingson RW, Zha W, Weitzman ER. Magnitude of and trends in alcohol-related mortality and morbidity among U.S. college students ages 18–24, 1998–2005. J Stud Alcohol Drugs Suppl. 2009;(16):12–20. doi: 10.15288/jsads.2009.s16.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mundt MP, Zakletskaia LI, Brown DD, Fleming MF. Alcohol-induced memory blackouts as an indicator of injury risk among college drinkers. Inj Prev. 2012;18(1):44–49. doi: 10.1136/ip.2011.031724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Macdonald S, Anglin-Bodrug K, Mann RE, et al. Injury risk associated with cannabis and cocaine use. Drug Alcohol Depend. 2003;72(2):99–115. doi: 10.1016/s0376-8716(03)00202-3. [DOI] [PubMed] [Google Scholar]
- 29.Lehman WE, Simpson DD. Employee substance use and on-the-job behaviors. J Appl Psychol. 1992;77(3):309–321. doi: 10.1037/0021-9010.77.3.309. [DOI] [PubMed] [Google Scholar]
- 30.Kypri K, Paschall MJ, Langley J, Baxter J, Cashell-Smith M, Bourdeau B. Drinking and alcohol-related harm among New Zealand university students: findings from a national Web-based survey. Alcohol Clin Exp Res. 2009;33(2):307–314. doi: 10.1111/j.1530-0277.2008.00834.x. [DOI] [PubMed] [Google Scholar]
- 31.Moore BA, Augustson EM, Moser RP, Budney AJ. Respiratory effects of marijuana and tobacco use in a U.S. sample. J Gen Intern Med. 2005;20(1):33–37. doi: 10.1111/j.1525-1497.2004.40081.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Taylor DR, Fergusson DM, Milne BJ, et al. A longitudinal study of the effects of tobacco and cannabis exposure on lung function in young adults. Addiction. 2002;97(8):1055–1061. doi: 10.1046/j.1360-0443.2002.00169.x. [DOI] [PubMed] [Google Scholar]
- 33.Fergusson DM, Horwood LJ, Swain-Campbell N. Cannabis use and psychosocial adjustment in adolescence and young adulthood. Addiction. 2002;97(9):1123–1135. doi: 10.1046/j.1360-0443.2002.00103.x. [DOI] [PubMed] [Google Scholar]
- 34.Grant BF, Stinson FS, Dawson DA, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004;61(8):807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- 35.Hall W, Babor TF. Cannabis use and public health: assessing the burden. Addiction. 2000;95(4):485–490. doi: 10.1046/j.1360-0443.2000.9544851.x. [DOI] [PubMed] [Google Scholar]
- 36.King RA, Schwab-Stone M, Flisher AJ, et al. Psychosocial and risk behavior correlates of youth suicide attempts and suicidal ideation. J Am Acad Child Adolesc Psychiatry. 2001;40(7):837–846. doi: 10.1097/00004583-200107000-00019. [DOI] [PubMed] [Google Scholar]
- 37.Patton GC, Coffey C, Carlin JB, Degenhardt L, Lynskey M, Hall W. Cannabis use and mental health in young people: cohort study. BMJ. 2002;325(7374):1195–1198. doi: 10.1136/bmj.325.7374.1195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Substance Abuse and Mental Health Services Administration. Results from the 2013 National Survey on Drug Use and Health: Summary of National Findings. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2014. NSDUH Series H-48, HHS Publication No. (SMA) 14-4863. [Google Scholar]
- 39.Arnett JJ. Emerging adulthood: A theory of development from the late teens through the twenties. Am Psychol. 2000;55(5):469–480. [PubMed] [Google Scholar]
- 40.Greene A, Wheatley S, Aldava J. Stages on life’s way: adolescents’ implicit theories of the life course. J Adolesc Res. 1992;7(3):364–381. [Google Scholar]
- 41.Wilk AI, Jensen NM, Havighurst TC. Meta-analysis of randomized control trials addressing brief interventions in heavy alcohol drinkers. J Gen Intern Med. 1997;12(5):274–283. doi: 10.1046/j.1525-1497.1997.012005274.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Moyer A, Finney JW, Swearingen CE, Vergun P. Brief interventions for alcohol problems: a meta-analytic review of controlled investigations in treatment-seeking and non-treatment-seeking populations. Addiction. 2002;97(3):279–292. doi: 10.1046/j.1360-0443.2002.00018.x. [DOI] [PubMed] [Google Scholar]
- 43.Vasilaki EI, Hosier SG, Cox WM. The efficacy of motivational interviewing as a brief intervention for excessive drinking: a meta-analytic review. Alcohol Alcohol. 2006;41(3):328–335. doi: 10.1093/alcalc/agl016. [DOI] [PubMed] [Google Scholar]
- 44.Maisto SA, Conigliaro J, McNeil M, Kraemer K, Conigliaro RL, Kelley ME. Effects of two types of brief intervention and readiness to change on alcohol use in hazardous drinkers. J Stud Alcohol. 2001;62(5):605–614. doi: 10.15288/jsa.2001.62.605. [DOI] [PubMed] [Google Scholar]
- 45.Appiah-Brempong E, Okyere P, Owusu-Addo E, Cross R. Motivational interviewing interventions and alcohol abuse among college students: a systematic review. Am J Health Promot. 2014;29(1):e32–42. doi: 10.4278/ajhp.130502-LIT-222. [DOI] [PubMed] [Google Scholar]
- 46.Dermen KH, Thomas SN. Randomized controlled trial of brief interventions to reduce college students' drinking and risky sex. Psychol Addict Behav. 2011;25(4):583–594. doi: 10.1037/a0025472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Huh D, Mun EY, Larimer ME, et al. Brief motivational interventions for college student drinking may not be as powerful as we think: an individual participant-level data meta-analysis. Alcohol Clin Exp Res. 2015;39(5):919–931. doi: 10.1111/acer.12714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Foxcroft DR, Coombes L, Wood S, Allen D, Almeida Santimano NM, Moreira MT. Motivational interviewing for the prevention of alcohol misuse in young adults. Cochrane Database Syst Rev. 2016;7:CD007025. doi: 10.1002/14651858.CD007025.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Martin G, Copeland J. The adolescent cannabis check-up: randomized trial of a brief intervention for young cannabis users. J Subst Abuse Treat. 2008;34(4):407–414. doi: 10.1016/j.jsat.2007.07.004. [DOI] [PubMed] [Google Scholar]
- 50.Walker DD, Stephens R, Roffman R, et al. Randomized controlled trial of motivational enhancement therapy with nontreatment-seeking adolescent cannabis users: a further test of the teen marijuana check-up. Psychol Addict Behav. 2011;25(3):474–484. doi: 10.1037/a0024076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Walker DD, Stephens RS, Blevins CE, Banes KE, Matthews L, Roffman RA. Augmenting brief interventions for adolescent marijuana users: The impact of motivational check-ins. J Consult Clin Psychol. 2016;84(11):983–992. doi: 10.1037/ccp0000094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.McCambridge J, Strang J. The efficacy of single-session motivational interviewing in reducing drug consumption and perceptions of drug-related risk and harm among young people: results from a multi-site cluster randomized trial. Addiction. 2004;99(1):39–52. doi: 10.1111/j.1360-0443.2004.00564.x. [DOI] [PubMed] [Google Scholar]
- 53.Dupont HB, Candel MJ, Kaplan CD, van de Mheen D, de Vries NK. Assessing the Efficacy of MOTI-4 for Reducing the Use of Cannabis Among Youth in the Netherlands: A Randomized Controlled Trial. J Subst Abuse Treat. 2016;65:6–12. doi: 10.1016/j.jsat.2015.11.012. [DOI] [PubMed] [Google Scholar]
- 54.Stephens R, Roffman R, Fearer S, Williams C, Burke R. The marijuana check-up: promoting change in ambivalent marijuana users. Addiction. 2007;102(6):947–957. doi: 10.1111/j.1360-0443.2007.01821.x. [DOI] [PubMed] [Google Scholar]
- 55.Walker DD, Stephens RS, Towe S, Banes K, Roffman R. Maintenance Check-ups Following Treatment for Cannabis Dependence. J Subst Abuse Treat. 2015;56:11–15. doi: 10.1016/j.jsat.2015.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Laporte C, Vaillant-Roussel H, Pereira B, et al. Cannabis and Young Users-A Brief Intervention to Reduce Their Consumption (CANABIC): A Cluster Randomized Controlled Trial in Primary Care. Ann Fam Med. 2017;15(2):131–139. doi: 10.1370/afm.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Stein MD, Hagerty CE, Herman DS, Phipps MG, Anderson BJ. A brief marijuana intervention for non-treatment-seeking young adult women. J Subst Abuse Treat. 2011;40(2):189–198. doi: 10.1016/j.jsat.2010.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Palfai TP, Tahaney K, Winter M, Saitz R. Readiness-to-change as a moderator of a web-based brief intervention for marijuana among students identified by health center screening. Drug Alcohol Depend. 2016;161:368–371. doi: 10.1016/j.drugalcdep.2016.01.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Barnett E, Sussman S, Smith C, Rohrbach LA, Spruijt-Metz D. Motivational Interviewing for adolescent substance use: a review of the literature. Addict Behav. 2012;37(12):1325–1334. doi: 10.1016/j.addbeh.2012.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hides L, Carroll S, Scott R, Cotton S, Baker A, Lubman DI. Quik Fix: a randomized controlled trial of an enhanced brief motivational interviewing intervention for alcohol/cannabis and psychological distress in young people. Psychother Psychosom. 2013;82(2):122–124. doi: 10.1159/000341921. [DOI] [PubMed] [Google Scholar]
- 61.Satre DD, Leibowitz A, Sterling SA, Lu Y, Travis A, Weisner C. A randomized clinical trial of Motivational Interviewing to reduce alcohol and drug use among patients with depression. J Consult Clin Psychol. 2016;84(7):571–579. doi: 10.1037/ccp0000096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Woolard R, Baird J, Longabaugh R, et al. Project reduce: reducing alcohol and marijuana misuse: effects of a brief intervention in the emergency department. Addict Behav. 2013;38(3):1732–1739. doi: 10.1016/j.addbeh.2012.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.White HR, Jiao Y, Ray AE, et al. Are there secondary effects on marijuana use from brief alcohol interventions for college students? J Stud Alcohol Drugs. 2015;76(3):367–377. doi: 10.15288/jsad.2015.76.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hettema J, Steele J, Miller WR. Motivational interviewing. Annu Rev Clin Psychol. 2005;1:91–111. doi: 10.1146/annurev.clinpsy.1.102803.143833. [DOI] [PubMed] [Google Scholar]
- 65.Shulman S, Nurmi JE. Understanding emerging adulthood from a goal-setting perspective. New Dir Child Adolesc Dev. 2010;2010(130):1–11. doi: 10.1002/cd.277. [DOI] [PubMed] [Google Scholar]
- 66.Norberg MM, Hides L, Olivier J, Khawar L, McKetin R, Copeland J. Brief interventions to reduce Ecstasy use: a multi-site randomized controlled trial. Behav Ther. 2014;45(6):745–759. doi: 10.1016/j.beth.2014.05.006. [DOI] [PubMed] [Google Scholar]
- 67.Scott CK, Dennis ML. Results from two randomized clinical trials evaluating the impact of quarterly recovery management checkups with adult chronic substance users. Addiction. 2009;104(6):959–971. doi: 10.1111/j.1360-0443.2009.02525.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Dennis M, Scott CK, Funk R. An experimental evaluation of recovery management checkups (RMC) for people with chronic substance use disorders. Eval Program Plann. 2003;26(3):339–352. doi: 10.1016/S0149-7189(03)00037-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Caviness CM, Tzilos G, Anderson BJ, Stein MD. Synthetic Cannabinoids: Use and Predictors in a Community Sample of Young Adults. Subst Abus. 2015;36(3):368–373. doi: 10.1080/08897077.2014.959151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Tzilos GK, Reddy MK, Caviness CM, Anderson BJ, Stein MD. Getting higher: co-occurring drug use among marijuana-using emerging adults. J Addict Dis. 2014;33(3):202–209. doi: 10.1080/10550887.2014.950024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Sterling RC, Gottheil E, Weinstein SP, Serota R. Therapist/patient race and sex matching: treatment retention and 9-month follow-up outcome. Addiction. 1998;93(7):1043–1050. doi: 10.1046/j.1360-0443.1998.93710439.x. [DOI] [PubMed] [Google Scholar]
- 72.Landes SJ, Burton JR, King KM, Sullivan BF. Women's Preference of Therapist Based on Sex of Therapist and Presenting Problem: An Analogue Study. Couns Psychol Q. 2013;26(3–4):330–342. doi: 10.1080/09515070.2013.819795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Stein MD, Herman DS, Moitra E, et al. A preliminary randomized controlled trial of a distress tolerance treatment for opioid dependent persons initiating buprenorphine. Drug Alcohol Depend. 2015;147:243–250. doi: 10.1016/j.drugalcdep.2014.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Uebelacker LA, Tremont G, Gillette LT, et al. Adjunctive yoga v. health education for persistent major depression: a randomized controlled trial. Psychol Med. 2017:1–13. doi: 10.1017/S0033291717000575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Uebelacker LA, Weisberg RB, Herman DS, et al. Pilot Randomized Trial of Collaborative Behavioral Treatment for Chronic Pain and Depression in Persons Living with HIV/AIDS. AIDS Behav. 2016;20(8):1675–1681. doi: 10.1007/s10461-016-1397-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Sobell L, Sobell M. Timeline Followback User's Guide: A Calendar Method for Assessing Alcohol and Drug Use. Toronto, Ontario, Canada: Addiction Research Foundation; 1996. [Google Scholar]
- 77.First M, Spitzer R, Williams J, Gibbon M. Structured clinical interview for DSM-IV - patient version. New York, NY: NY State Psychiatric Institute; 1995. [Google Scholar]
- 78.Miller W, Tonigan J, Longabaugh R. Project MATCH Monograph Series. Vol. 4. Rockville, MD: National Institute on Alcohol and Alcoholism; 1995. The Drinker Inventory of Consequences: an instrument for assessing adverse consequence of alcohol abuse. DHHS Publication No. 95-3911. [Google Scholar]
- 79.Stephens RS, Roffman RA, Curtin L. Comparison of extended versus brief treatments for marijuana use. J Consult Clin Psychol. 2000;68(5):898–908. [PubMed] [Google Scholar]
- 80.Marlatt GA, Curry S, Gordon JR. A longitudinal analysis of unaided smoking cessation. J Consult Clin Psychol. 1988;56(5):715–720. doi: 10.1037//0022-006x.56.5.715. [DOI] [PubMed] [Google Scholar]
- 81.Stone AL, Becker LG, Huber AM, Catalano RF. Review of risk and protective factors of substance use and problem use in emerging adulthood. Addict Behav. 2012;37(7):747–775. doi: 10.1016/j.addbeh.2012.02.014. [DOI] [PubMed] [Google Scholar]
- 82.Wagenmakers EJ. A practical solution to the pervasive problems of p values. Psychon Bull Rev. 2007;14(5):779–804. doi: 10.3758/bf03194105. [DOI] [PubMed] [Google Scholar]
- 83.Stata Statistical Software: Release 14.1 [computer program] College Park, TX: StataCorp LP; 2016. [Google Scholar]
- 84.Budney AJ, Roffman R, Stephens RS, Walker D. Marijuana dependence and its treatment. Addict Sci Clin Pract. 2007;4(1):4–16. doi: 10.1151/ascp07414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Carey KB, Scott-Sheldon LA, Carey MP, DeMartini KS. Individual-level interventions to reduce college student drinking: a meta-analytic review. Addict Behav. 2007;32(11):2469–2494. doi: 10.1016/j.addbeh.2007.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Caldeira KM, Kasperski SJ, Sharma E, et al. College students rarely seek help despite serious substance use problems. J Subst Abuse Treat. 2009;37(4):368–378. doi: 10.1016/j.jsat.2009.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Peretti-Watel P. Neutralization theory and the denial of risk: some evidence from cannabis use among French adolescents. Br J Sociol. 2003;54(1):21–42. doi: 10.1080/0007131032000045888. [DOI] [PubMed] [Google Scholar]
- 88.Stephens RS, Roffman RA, Fearer SA, Williams C, Burke RS. The Marijuana Check-up: promoting change in ambivalent marijuana users. Addiction. 2007;102(6):947–957. doi: 10.1111/j.1360-0443.2007.01821.x. [DOI] [PubMed] [Google Scholar]
- 89.Walker DD, Roffman RA, Stephens RS, Wakana K, Berghuis J, Kim W. Motivational enhancement therapy for adolescent marijuana users: a preliminary randomized controlled trial. J Consult Clin Psychol. 2006;74(3):628–632. doi: 10.1037/0022-006X.74.3.628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Stein LA, Lebeau R, Colby SM, Barnett NP, Golembeske C, Monti PM. Motivational interviewing for incarcerated adolescents: effects of depressive symptoms on reducing alcohol and marijuana use after release. J Stud Alcohol Drugs. 2011;72(3):497–506. doi: 10.15288/jsad.2011.72.497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.de Gee EA, Verdurmen JE, Bransen E, de Jonge JM, Schippers GM. A randomized controlled trial of a brief motivational enhancement for non-treatment-seeking adolescent cannabis users. J Subst Abuse Treat. 2014;47(3):181–188. doi: 10.1016/j.jsat.2014.05.001. [DOI] [PubMed] [Google Scholar]
- 92.Sussman S, Dent C. Five-year prospective prediction of marijuana use cessation of youth at continuation high schools. Addict Behav. 2004;29:1237–1243. doi: 10.1016/j.addbeh.2004.03.024. [DOI] [PubMed] [Google Scholar]
- 93.Terry-McElrath YM, O'Malley PM, Johnston LD, Bray BC, Patrick ME, Schulenberg JE. Longitudinal patterns of marijuana use across ages 18–50 in a US national sample: A descriptive examination of predictors and health correlates of repeated measures latent class membership. Drug Alcohol Depend. 2017;171:70–83. doi: 10.1016/j.drugalcdep.2016.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Foster DW, Buckner JD, Schmidt NB, Zvolensky MJ. Multisubstance Use Among Treatment-Seeking Smokers: Synergistic Effects of Coping Motives for Cannabis and Alcohol Use and Social Anxiety/Depressive Symptoms. Subst Use Misuse. 2016;51(2):165–178. doi: 10.3109/10826084.2015.1082596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Carey KB, Henson JM, Carey MP, Maisto SA. Which heavy drinking college students benefit from a brief motivational intervention? J Consult Clin Psychol. 2007;75(4):663–669. doi: 10.1037/0022-006X.75.4.663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Fromme K, Corbin W. Prevention of heavy drinking and associated negative consequences among mandated and voluntary college students. J Consult Clin Psychol. 2004;72(6):1038–1049. doi: 10.1037/0022-006X.72.6.1038. [DOI] [PubMed] [Google Scholar]
- 97.Dupont HB, Candel M, Lemmens P, Kaplan CD, van de Mheen D, De Vries NK. Stages of Change Model has Limited Value in Explaining the Change in Use of Cannabis among Adolescent Participants in an Efficacious Motivational Interviewing Intervention. J Psychoactive Drugs. 2017:1–10. doi: 10.1080/02791072.2017.1325030. [DOI] [PubMed] [Google Scholar]
- 98.Hughes J, Peters E, Callas P, Budney A, Livingston A. Attempts to stop or reduce marijuana use in non-treatment seekers. Drug Alcohol Depend. 2008;97(1–2):180–184. doi: 10.1016/j.drugalcdep.2008.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Moyers TB, Manuel JK, Ernst D. Motivational Interviewing Treatment Integrity Coding Manual. 2014 doi: 10.1016/j.jsat.2016.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]