Abstract
This study uses CMS Overall Hospital Quality Star Rating data to estimate associations between hospital characteristics, number and types of measures reported, and the CMS Hospital Quality Star Ratings.
The Centers for Medicare & Medicaid Services (CMS) introduced the Overall Hospital Quality Star Ratings in July 2016 to provide consumers a summary rating of hospital performance using measures already reported to CMS. Hospitals achieve 1 to 5 stars based on 62 measures across 7 weighted measure groups relating to health care quality: mortality, readmissions, safety, patient experience, efficient use of imaging, effectiveness of care, and timeliness of care. To receive a star rating, hospitals must report at least 3 of the 7 measure groups and at least 1 Outcome group (mortality, readmissions, or safety). Within each measure group, at least 3 individual measures must be reported for inclusion of that group. If a hospital does not submit enough measures for a group to be included, the weight from that group is redistributed to the other groups for which the hospital has sufficient data.
Concerns have been raised regarding the measures, methodology, and potential bias toward or against certain hospital types. To assess these concerns, we evaluated associations between hospital characteristics, number and types of measures reported, and the star ratings.
Methods
This study was deemed nonhuman subjects research by the Northwestern University institutional review board. Data from the CMS Overall Hospital Quality Star Ratings database (obtained July 27, 2016), American Hospital Association 2014 Annual Survey of Hospitals, and CMS Fiscal Year 2015 Payment Update Impact File were merged. We examined associations between hospital characteristics (Table), number of individual measures reported, number of group categories (Outcome or other) reported, and the star ratings (4-5 stars [high] vs 1-3 stars [low]) using χ2 analysis and Kruskal-Wallis tests. Two-sided P values less than .05 were used to indicate statistical significance. Analyses were performed using Statistical Analysis Software (SAS Institute), version 9.4.
Table. Hospital Characteristics by Centers for Medicare & Medicaid Services (CMS) Overall Hospital Quality Star Ratings.
| Low CMS Star Rating (1-3 Stars) | High CMS Star Rating (4-5 Stars) | P Valuea | |||
|---|---|---|---|---|---|
| No. of Hospitals | % (95% CI) | No. of Hospitals | % (95% CI) | ||
| Total hospitals | 2593 | 72.3 (70.7-73.7) | 998 | 27.7 (26.3-29.3) | |
| Hospital type | |||||
| Major teaching | 192 | 84.2 (79.5-88.9) | 36 | 15.8 (11.1-20.5) | <.001 |
| Other teaching | 829 | 81.2 (78.8-83.6) | 192 | 18.8 (16.4-21.2) | |
| Community | 1199 | 69.8 (67.6-71.9) | 520 | 30.2 (28.1-32.4) | |
| Critical access | 363 | 66.7 (62.8-70.7) | 181 | 33.3 (29.3-37.2) | |
| Specialtyb | 10 | 12.7 (5.3-20.0) | 69 | 87.3 (80.0-94.7) | |
| No. of beds | |||||
| <100 | 949 | 66.0 (63.6-68.5) | 488 | 34.0 (31.5-36.4) | <.001 |
| 100-299 | 1062 | 76.7 (73.4-77.9) | 341 | 24.3 (22.1-26.6) | |
| 300-499 | 367 | 75.8 (72.0-79.6) | 117 | 24.2 (20.4-28.0) | |
| ≥500 | 215 | 80.5 (75.7-85.3) | 52 | 19.4 (14.7-24.2) | |
| Percentage of DSH paymentsc | |||||
| Q1 (≤18.1) | 433 | 57.1 (53.6-60.6) | 325 | 42.8 (39.4-46.4) | <.001 |
| Q2 (18.2-26.0) | 532 | 70.3 (67.0-73.5) | 225 | 29.7 (26.5-33.0) | |
| Q3 (26.1-35.5) | 583 | 76.9 (73.9-79.9) | 175 | 23.1 (20.1-26.1) | |
| Q4 (>35.5) | 669 | 88.4 (86.1-90.7) | 88 | 11.6 (9.3-13.9) | |
| Joint Commission accredited | |||||
| Yes | 1943 | 72.6 (68.2-74.1) | 734 | 27.4 (25.9-31.8) | .39 |
| No | 650 | 71.1 (70.9-74.3) | 264 | 28.9 (25.7-29.1) | |
| No. of Outcome measure groups reportedd | |||||
| 1 of 3 | 117 | 54.4 (47.8-61.1) | 98 | 45.6 (38.9-52.2) | <.001 |
| 2 of 3 | 474 | 68.8 (65.3-72.3) | 215 | 31.2 (27.7-34.7) | |
| 3 of 3 | 2002 | 74.5 (72.9-76.2) | 685 | 25.5 (23.8-27.1) | |
| No. of other groups reportede | |||||
| 0 of 4 | 1 | 50.0 (0.0-100.0) | 1 | 50.0 (0.0-100.0) | .30 |
| 1 of 4 | 124 | 79.0 (72.6-85.4) | 33 | 21.0 (14.6-27.4) | |
| 2 of 4 | 241 | 70.3 (65.4-75.1) | 102 | 29.7 (24.9-34.6) | |
| 3 of 4 | 380 | 72.7 (68.8-76.5) | 143 | 27.3 (23.5-31.2) | |
| 4 of 4 | 1847 | 72.0 (70.2-73.7) | 719 | 28.0 (26.3-29.8) | |
| Total measures reported, No. | |||||
| Q1 (<39) | 599 | 66.9 (63.8-70.0) | 296 | 33.1 (30.0-36.2) | <.001 |
| Q2 (39-52) | 719 | 74.0 (71.3-76.8) | 252 | 26.0 (23.2-28.7) | |
| Q3 (53-57) | 733 | 75.7 (73.0-78.4) | 235 | 24.3 (21.6-27.0) | |
| Q4 (>57) | 542 | 71.6 (68.4-74.8) | 215 | 28.4 (25.2-31.6) | |
Abbreviation: DSH, disproportionate share hospital.
χ2 test.
Specialty hospitals self-identified as cardiac, orthopedic, surgical, cancer, or other specialty primary service type.
Critical access hospitals are excluded from the CMS Impact File due to payment through alternative mechanism.
Outcome groups defined by CMS consisted of mortality, readmissions, and safety. To be eligible to receive a CMS star rating, hospitals had to report at least 3 measures in at least 1 Outcome group.
Other groups defined by CMS consisted of patient experience, efficient use of medical imaging, effectiveness of care, and timeliness of care.
Results
Of 3591 hospitals receiving a star rating, 4 or 5 stars were awarded to 15.8% of major teaching hospitals, 18.8% of other teaching hospitals, 30.2% of community hospitals, 33.3% of critical access hospitals, and 87.3% of specialty hospitals (P < .001 for all compared with specialty hospitals) (Table). Smaller hospitals more frequently achieved a high star rating compared with larger hospitals (No. of beds: <100, 34.0%; 100-299, 24.3%; 300-499, 24.2%; ≥500, 19.4%; P < .001). Hospitals with lower disproportionate share payments achieved a high star rating more frequently (Q1, 42.8%; Q2, 29.7%; Q3, 23.1%; Q4, 11.6%; P < .001). Specialty hospitals comprised 2.2% of hospitals but accounted for 41.1% of 5-star hospitals.
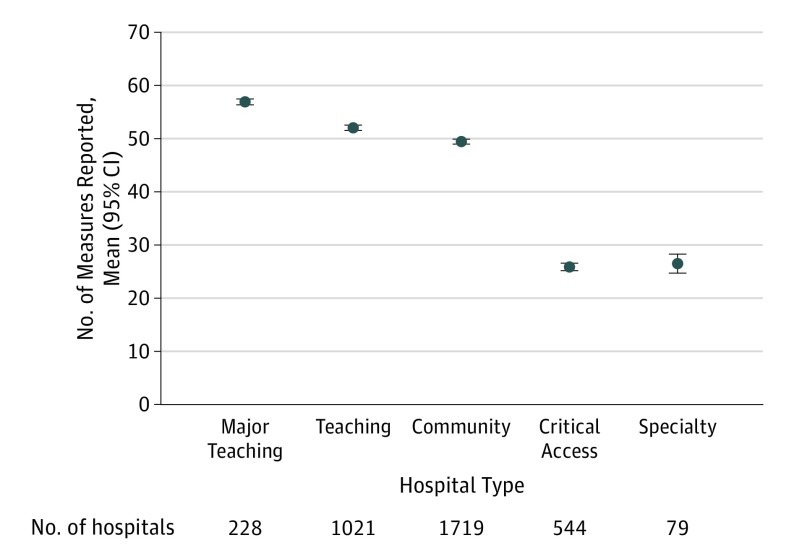
Hospitals reported a mean of 46.6 (75.2%) of 62 possible measures. Major teaching (mean, 56.9), other teaching (mean, 52.1), and community hospitals (mean, 49.5) reported approximately twice as many measures as critical access (mean, 25.9) and specialty hospitals (mean, 26.5; P < .001) (Figure). Hospitals reporting more Outcome measures less frequently received a high star rating: high star ratings were given to 46.9% of hospitals reporting the minimum threshold of 1 Outcome measure group, 31.2% of hospitals reporting 2 Outcome measure groups, and 25.5% of hospitals reporting all 3 Outcome measure groups (P < .001) (Table). Star ratings were based on the minimum eligibility threshold of only 3 of 7 measure groups for 49.4% of specialty and 33.3% of critical access hospitals; whereas, 94.3% of major teaching, 80.8% of other teaching, and 96% of community hospitals reported all 7 measure groups.
Figure. Mean No. of Hospital Quality Measures Reported (of 62 Total Possible Measures) by Hospital Typea.
aError bars represent 95% CIs. Includes hospitals that met the reporting threshold of at least 3 measures within at least 1 Outcome group (mortality, readmissions, safety). Using the Kruskal-Wallis test, P<.001 for all pairwise comparisons except between critical access and specialty hospitals (P = .96).
Discussion
Hospitals less frequently received a high star rating if they were larger, academic hospitals or cared for a higher proportion of disproportionate share patients. Specialty and critical access hospitals more frequently earned high star ratings compared with acute care hospitals. Critical access hospitals and some specialty hospitals (ie, certain cancer centers) are exempt from reporting-based payment incentives through the CMS Inpatient Quality Reporting system and may not collect many measures used in the star ratings. Consequently, specialty and critical access hospitals reported systematically fewer measures. Although hospital type influenced the number and type of measures reported, the study was limited by the inability to determine whether differences in individual measure reporting by hospital type explained the differences in star ratings.
Because the measures used as the basis for calculating the star ratings differed by hospital type, failure to account for these differences may limit the utility of the star ratings, particularly when comparing different hospital types.
Section Editor: Jody W. Zylke, MD, Deputy Editor.
References
- 1.QualityNet Comprehensive Methodology Report, v2.0. 2016; https://www.qualitynet.org/dcs/ContentServer?c=Page&pagename=QnetPublic%2FPage%2FQnetTier3&cid=1228775957165. August 16, 2016.
- 2.Bilimoria KY, Barnard C. The new CMS Hospital Quality Star Ratings: the stars are not aligned. JAMA. 2016;316(17):1761-1762. [DOI] [PubMed] [Google Scholar]
- 3.QualityNet Statistical Analysis System (SAS) package. https://www.qualitynet.org/dcs/ContentServer?c=Page&pagename=QnetPublic%2FPage%2FQnetTier3&cid=1228775958130. Accessed 8/14/2016.
- 4.US Government Publishing Office Federal Register 2015: rules and regulations. https://www.gpo.gov/fdsys/pkg/FR-2015-08-17/pdf/2015-19049.pdf. Accessed September 22, 2016.