Abstract
Introduction
Older adults are at high risk for stroke and falls, both of which require a large amount of informal caregiving. However, the economic burden of informal caregiving associated with stroke and fall history is not well known.
Methods
Using the 2010 Health and Retirement Study, data on non-institutionalized adults aged ≥65 years (N=10,129) in 2015–2017 were analyzed. Two-part models were used to estimate informal caregiving hours. Based on estimates from the models using a replacement cost approach, the authors derived informal caregiving hours and costs associated with falls in the past 2 years for stroke and non-stroke persons.
Results
Both the prevalence of falls overall and of falls with injuries were higher among people with stroke than those without (49.5% vs 35.1% for falls and 16.0% vs 10.3% for injurious falls, p<0.01). Stroke survivors needed more informal caregiving hours than their non-stroke counterparts, and the number of informal caregiving hours was positively associated with non-injurious falls and even more so with injurious falls. The national burden of informal caregiving (2015 U.S. dollars) associated with injurious falls amounted to $2.9 billion (95% CI=$1.1 billion, $4.7 billion) for stroke survivors (about 0.5 million people), and $6.5 billion (95% CI=$4.3 billion, $8.7 billion) for those who never had a stroke (about 3.6 million people).
Conclusions
In U.S. older adults, informal caregiving hours and costs associated with falls are substantial, especially for stroke survivors. Preventing falls and fall-related injuries, especially among stroke survivors, therefore has potential for reducing the burden of informal caregiving.
INTRODUCTION
Older adults are at high risk for stroke and falls.1–3 Each year in the U.S., one third of adults aged ≥65 years experience a fall.4 An estimated 6.6 million Americans aged ≥20 years are living with a stroke in 2012.1 In 2009, more than two thirds of the one million stroke-related hospitalizations that year were among people aged ≥65 years.1,5 Falls and fall-related injuries are common complications among stroke survivors.6,7 The 2-year risk of falls among stroke survivors was 46%.8
Both stroke and falls rank among the leading causes of disability in the U.S. In terms of their contributions to years lived with disability, falls ranked 15th in the U.S. in 1990 and 11th in 2010, while the rank for stroke changed from 23rd to 17th over the same time period.9 Among those aged ≥65 years, one of five falls are severe incidents, including broken bones and head injuries.10
Not surprisingly, the disabilities caused by stroke and falls frequently are permanent, and care involves support for both the patient’s physical and emotional needs. Thus, stroke and falls often require a large amount of informal caregiving provided by relatives or unpaid nonrelatives in addition to paid professionals.11–15 Stroke survivors in the U.S. used on average 12–22 hours of informal caregiving each week.14 Although a study found the direct medical costs in the U.S. for nonfatal fall injuries among those aged ≥65 years to be $31 billion,16 neither the burden of informal caregiving among those who had fall-related injuries was examined, nor was the economic burden of informal caregiving estimated by stroke and fall status. To address these gaps, in the present study the authors estimate hours of informal caregiving and the economic burden associated with stroke and falls among U.S. older adults using nationally representative samples.
METHODS
Study Sample
The authors used the 2010 Health and Retirement Study (HRS), a biennial, nationally representative longitudinal household survey of U.S. residents aged >50 years.17 The study sample was limited to non-institutionalized individuals aged ≥65 years at the time of the interview (Figure 1, N=10,129).
Figure 1. Process for selecting study population in 2010 Health and Retirement Study.
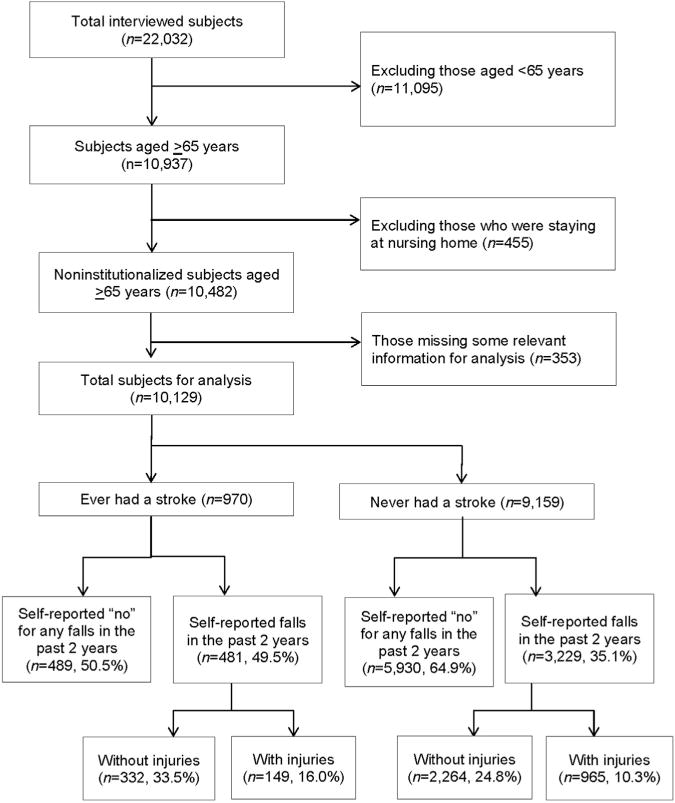
Note: All percentages were weighted by population.
Measures
Stroke survivors were defined as those who self-reported a stroke during their lifetime. HRS survey participants aged ≥65 years were asked whether they had fallen in the last 2 years. Those who reported falling were asked whether they had sustained serious injuries that required medical treatment because of these falls. Based on the responses, two indicator variables were defined. The first variable was whether a respondent self-reported a fall in the last 2 years but did not report severe injuries due to the fall, whereas the second variable was whether a respondent self-reported at least one injurious fall. Stroke survivors without any falls in the last 2 years were used as the baseline. The authors obtained the 2010 HRS data in 2014 and all analyses were conducted between 2015 and 2017.
Informal caregiving was defined as caregiving activities provided by relatives, with or without compensation, or by unpaid non-family members.18 These activities included providing support for activities of daily living or instrumental activities of daily living.19 Weekly hours of informal caregiving were defined as hours provided by all informal caregivers, based on reports by respondents of the number of hours per day and days during the last month that they received informal caregiving. For respondents with multiple informal caregivers, the authors calculated a weekly total of informal caregiving hours using all of these caregivers. The daily hours of informal caregiving per caregiver was limited to a maximum of 16.13,19 Days per month were divided by 4.3 to obtain a weekly average; and for respondents who needed help every day, it was assumed 7 days per week.20
Statistical Analysis
The authors used two-part models to estimate the hours of informal caregiving associated with injurious and non-injurious falls, by stroke status.13,19 Two-part models were applied because 89% of the study sample without stroke and 67% of the study sample with stroke did not utilize informal caregiving (Tables 1 and 2), and the distribution of informal caregiving hours in both groups was skewed. The model was adapted in several previous studies to estimate the economic burden of informal caregiving for chronic diseases, all of which used data with a skewed distribution.13,19,20
Table 1.
Sample Characteristics of People With No History of Stroke: 2010 Health and Retirement Study
| Parameters | Total, % (N=9,159) |
No falls, % (n=5,930) |
Falls in the past 2 yearsa | |||||
|---|---|---|---|---|---|---|---|---|
| Without injury (n=2,264) |
With injury (n=965) |
Total (n=3,229) |
||||||
| % | p-value | % | p-value | % | p-value | |||
| Race/ethnicity | ||||||||
| Non-Hispanic white | 84.7 | 84.0 | 86.5 | 0.008 | 85.0 | 0.380 | 86.1 | 0.004 |
| Non-Hispanic black | 7.4 | 8.2 | 5.9 | <0.001 | 6.1 | 0.015 | 6.0 | <0.001 |
| Hispanic | 6.3 | 6.2 | 6.1 | 0.957 | 7.5 | 0.128 | 6.5 | 0.528 |
| Other races | 1.6 | 1.7 | 1.5 | 0.543 | 1.4 | 0.526 | 1.5 | 0.455 |
| Male | 43.3 | 45.0 | 44.3 | 0.630 | 30.0 | < 0.001 | 40.1 | 0.001 |
| Age, years | ||||||||
| 65–74 | 57.1 | 60.0 | 52.9 | < 0.001 | 48.5 | < 0.001 | 51.6 | < 0.001 |
| 75–84 | 31.5 | 30.3 | 33.7 | 0.008 | 33.8 | 0.043 | 33.7 | 0.001 |
| ≥85 | 11.4 | 9.7 | 13.4 | < 0.001 | 17.7 | < 0.001 | 14.7 | < 0.001 |
| Education | ||||||||
| Less than high school | 20.2 | 19.4 | 20.9 | 0.250 | 23.1 | 0.017 | 21.6 | 0.062 |
| High school | 35.1 | 35.0 | 36.3 | 0.341 | 32.7 | 0.243 | 35.2 | 0.876 |
| Some college | 21.3 | 20.9 | 21.8 | 0.466 | 22.6 | 0.256 | 22.0 | 0.287 |
| College and more | 23.4 | 24.7 | 21.0 | 0.008 | 21.6 | 0.075 | 21.2 | 0.002 |
| Currently married | 56.3 | 58.9 | 53.6 | < 0.001 | 46.8 | < 0.001 | 51.6 | < 0.001 |
| Number of chronic conditionsb | ||||||||
| 0–1 | 22.1 | 26.0 | 16.1 | < 0.001 | 11.8 | < 0.001 | 14.8 | < 0.001 |
| 2–3 | 48.2 | 50.1 | 45.8 | 0.007 | 41.9 | < 0.001 | 44.7 | < 0.001 |
| ≥4 | 29.7 | 23.9 | 38.1 | < 0.001 | 46.3 | < 0.001 | 40.5 | < 0.001 |
| Total non-housing wealth (U.S. $) | ||||||||
| ≤6,000 | 20.5 | 19.2 | 21.9 | 0.060 | 25.2 | 0.003 | 22.9 | 0.007 |
| 6,001–66,000 | 23.3 | 23.1 | 24.2 | 0.330 | 22.7 | 0.828 | 23.8 | 0.521 |
| 66,001–306,000 | 27.2 | 28.1 | 25.3 | 0.039 | 26.1 | 0.349 | 25.5 | 0.061 |
| >306,000 | 29.0 | 29.6 | 28.6 | 0.496 | 26.0 | 0.052 | 27.8 | 0.168 |
| Formal caregiving | ||||||||
| Utilization | 2.3 | 1.4 | 3.3 | 0.002 | 6.3 | <0.001 | 4.1 | <0.001 |
| Hours per week | 0.8 | 0.4 | 0.9 | 0.018 | 3.0 | 0.001 | 1.5 | < 0.001 |
| Informal caregiving | ||||||||
| Utilization | 11.4 | 7.4 | 16.8 | < 0.001 | 23.7 | < 0.001 | 18.9 | < 0.001 |
| Hours per week | 2.8 | 1.7 | 4.1 | < 0.001 | 7.1 | < 0.001 | 5.0 | < 0.001 |
Note: Boldface indicates statistical significance (p<0.05).
p-values compare values in “No falls” column to values in each subcolumn of “Falls in past 2 years.”
Authors included 11 chronic conditions: hypertension; diabetes; cancer; lung disease; heart disease; any emotional, nervous, or psychiatric problems; arthritis; dementia or Alzheimer’s disease; urinary incontinence; visual impairment (corrected eyesight reported as “poor” or “legally blind”); and hearing impairment (corrected hearing ability reported as “poor”).
Table 2.
Sample Characteristics of People Who Had Had a Stroke: 2010 Health and Retirement Study
| Parameters | Total, % (N=970) |
No falls, % (n=489) |
Falls in the past 2 yearsa | |||||
|---|---|---|---|---|---|---|---|---|
| Without injury (n=332) |
With injury (n=149) |
Total (n=481) |
||||||
| % | p-value | % | p-value | % | p-value | |||
| Race/ethnicity | ||||||||
| Non-Hispanic white | 83.0 | 80.4 | 84.3 | 0.158 | 88.8 | 0.010 | 85.7 | 0.035 |
| Non-Hispanic black | 10.8 | 12.9 | 9.5 | 0.170 | 7.1 | 0.030 | 8.7 | 0.066 |
| Hispanic | 4.8 | 5.2 | 4.5 | 0.534 | 4.0 | 0.486 | 4.3 | 0.409 |
| Other races | 1.3 | 1.5 | 1.8 | 0.724 | 0.0 | 0.059 | 1.2 | 0.771 |
| Male | 49.6 | 52.6 | 51.7 | 0.832 | 35.9 | 0.001 | 46.6 | 0.095 |
| Age, years | ||||||||
| 65–74 | 40.5 | 43.8 | 36.3 | 0.063 | 39.0 | 0.311 | 37.1 | 0.053 |
| 75–84 | 39.5 | 36.9 | 44.0 | 0.120 | 38.0 | 0.816 | 42.1 | 0.196 |
| ≥85 | 20.0 | 19.3 | 19.7 | 0.916 | 23.0 | 0.261 | 20.8 | 0.623 |
| Education | ||||||||
| Less than high school | 26.4 | 24.0 | 28.4 | 0.237 | 29.6 | 0.239 | 28.9 | 0.166 |
| High school | 36.5 | 38.2 | 35.6 | 0.476 | 32.8 | 0.249 | 34.7 | 0.312 |
| Some college | 18.4 | 18.0 | 19.2 | 0.664 | 18.1 | 0.980 | 18.8 | 0.703 |
| College and more | 18.7 | 19.8 | 16.8 | 0.344 | 19.5 | 0.959 | 17.6 | 0.456 |
| Currently married | 50.1 | 51.4 | 50.7 | 0.861 | 44.9 | 0.313 | 48.8 | 0.555 |
| Number of chronic conditionsb | ||||||||
| 0–1 | 8.5 | 12.6 | 5.3 | 0.003 | 2.2 | < 0.001 | 4.3 | < 0.001 |
| 2–3 | 38.3 | 46.8 | 29.7 | < 0.001 | 29.5 | 0.003 | 29.6 | < 0.001 |
| ≥4 | 53.2 | 40.6 | 65.0 | < 0.001 | 68.4 | < 0.001 | 66.1 | < 0.001 |
| Total non-housing wealth, U.S. $ | ||||||||
| ≤6,000 | 28.8 | 27.3 | 28.7 | 0.667 | 33.9 | 0.215 | 30.4 | 0.373 |
| 6,001–66,000 | 27.4 | 26.7 | 31.2 | 0.257 | 21.9 | 0.302 | 28.2 | 0.688 |
| 66,001–306,000 | 23.9 | 24.3 | 22.3 | 0.662 | 25.7 | 0.768 | 23.4 | 0.826 |
| >306,000 | 19.9 | 21.7 | 17.8 | 0.240 | 18.5 | 0.510 | 18.1 | 0.225 |
| Formal caregiving | ||||||||
| Utilization | 11.7 | 7.8 | 12.5 | 0.082 | 21.9 | 0.002 | 15.6 | 0.008 |
| Hours per week | 3.6 | 3.8 | 3.3 | 0.766 | 3.6 | 0.915 | 3.4 | 0.808 |
| Informal caregiving | ||||||||
| Utilization | 32.4 | 20.7 | 38.8 | < 0.001 | 56.0 | < 0.001 | 44.3 | < 0.001 |
| Hours per week | 11.3 | 7.1 | 12.9 | 0.008 | 21.1 | 0.001 | 15.5 | < 0.001 |
Note: Boldface indicates statistical significance (p<0.05).
p-values compare values in “No falls” column to values in each subcolumn of “Falls in past 2 years.”
Authors included 11 chronic conditions: hypertension; diabetes; cancer; lung disease; heart disease; any emotional, nervous, or psychiatric problems; arthritis; dementia or Alzheimer’s disease; urinary incontinence; visual impairment (corrected eyesight reported as “poor” or “legally blind”); and hearing impairment (corrected hearing ability reported as “poor”).
In the first part of the model, the authors used a logit model to estimate the associations of injurious and non-injurious falls with the likelihood of receiving informal caregiving. In the second part, the authors estimated the associations of injurious and non-injurious falls with hours of informal caregiving among those who used informal care by employing ordinary least squares regression with log-transformed hours of informal caregiving. In both parts of the model, the authors controlled for race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, and other races); age (65–74, 75–84, and ≥85 years); sex (male or female); marital status (currently married or not); education (less than high school, high school graduate, some college graduate, and college and more); numbers of self-reported chronic conditions (zero to one, two to three, and four to 11); net total non-housing wealth (quartiles from the sample); and usage of formal caregiving (currently use formal caregiving or not). The model included 11 chronic conditions: hypertension; diabetes; cancer; lung disease; heart disease; any emotional, nervous, or psychiatric problems; arthritis; dementia; urinary incontinence; visual impairment (corrected eyesight self-reported as “legally blind” or “poor”); and hearing impairment (corrected hearing ability self-reported as “poor”).
The authors estimated two-part models for two separate groups: (1) stroke survivors and (2) those who never had a stroke. A two-part model using the total sample (1 and 2) was also estimated. The conceptual model for the analysis is shown in Appendix Figure 1 (available online). The results from both parts of the model were used to estimate the average marginal associations of injurious and non-injurious falls with weekly hours of informal caregiving. Stata, version 14.0, was used for all analyses.
The authors estimated the economic burden of informal caregiving by adapting a replacement cost approach.13,21 This approach assumes that the value of informal caregiving is equivalent to the typical wage of paid workers who provide similar services.14 The 2015 median hourly wage of home health aides ($10.54) reported by the Bureau of Labor Statistics as the unit cost of informal caregiving was used.13,22 Also, the authors used the federal minimum wage rate ($7.25 per hour) as of 2015 as a lower-bound estimate to conduct a sensitivity analysis.23,24
The authors estimated the national economic burden of informal caregiving associated with injurious and non-injurious falls according to stroke status by using population prevalence estimates among those aged ≥65 years from the 2010 HRS.13 The annual national economic burden of informal caregiving was estimated by multiplying the weekly cost of informal caregiving by the number of individuals with injurious and non-injurious falls in the past 2 years, and the numbers of weeks in 1 year (i.e., 52), assuming that informal caregiving was required for an entire year.
RESULTS
Among the 10,129 study subjects, 970 were stroke survivors (Figure 1). In all, 49.5% of stroke survivors reported that they had had at least one fall in the past 2 years, and 149, or 16.0% of the stroke survivors, had a fall-related injury during this period. In the past 2 years among those who had never had a stroke, 10.3% had an injurious fall, whereas 24.8% had a non-injurious fall. All percentages were weighted by population sampling weight from the 2010 HRS data.
Among both stroke survivors and those who never had a stroke, those who had a fall in the past 2 years were more likely to be non-Hispanic white, and to have four or more chronic health conditions, than those who had no falls in the past 2 years (Tables 1 and 2). Also, those who had a fall in the past 2 years were more likely to use informal and formal caregiving services than those who did not have a fall during this period. Among stroke survivors, age, education, marital status, and net total non-housing wealth did not differ significantly between those who had had and those who had not had a fall during the period of interest (Table 2). In addition, among those who had never had a stroke, those who had a fall in the past 2 years were less likely to be married, less likely to be male, and older than their counterparts who did not fall in the past 2 years (Table 1).
Stroke survivors used more hours of informal caregiving than their non-stroke counterparts did. Although stroke survivors used an average of 11.3 hours of informal caregiving per week, their non-stroke counterparts reported only 2.8 hours (p<0.01; Appendix Figure 2, available online). Hours of informal caregiving were positively associated with non-injurious falls and even more with injurious falls. Among those without stroke, people with no falls in the past 2 years reported an average of 1.7 hours of informal caregiving; this number was 4.1 hours for those with a fall but no injury and 7.1 hours for those with a fall that caused an injury (p<0.01; Table 1). A similar pattern was seen for stroke survivors; those without a fall in the past 2 years averaged 7.1 hours of informal caregiving per week, whereas those with non-injurious falls used 12.9 hours and those with a fall causing an injury used 21.1 hours (p<0.01; Table 2; Appendix Figure 2, available online).
Table 3 shows the estimates from the two-part models for hours of informal caregiving and economic burden associated with falls and fall-related injuries. After controlling for potential confounders, among people with stroke the weekly duration of informal caregiving was 10.5 hours (p<0.01) higher for those with injurious falls than it was for those who had not fallen in the past 2 years. Employing the median wage of home health aides in 2015 ($10.54/hour), and using for comparison adults with no falls, the authors estimated that a stroke survivor who had fall-related injuries on average had an additional economic burden of $5,777 per year (95% CI=$2,247, $9,306) for informal caregiving. Applying the results to the estimated U.S. population of stroke patients from the 2010 HRS, the economic burden of informal caregiving associated with fall-related injuries among elderly stroke survivors (about 0.5 million people) was $2.9 billion per year (95% CI=$1.1 billion, $4.7 billion). For people without stroke, in comparison with those without falls, hours of weekly informal caregiving due to non-injurious falls and to injurious falls equaled 1.7 (p<0.01), corresponding to an annual national economic burden of $8.1 billion (95% CI=$4.6 billion, $11.5 billion), and 3.3 (p<0.01), respectively, the latter corresponding to an annual national economic burden of $6.5 billion (95% CI=$4.3 billion, $8.7 billion).
Table 3.
Estimated Incremental Hours and Economic Burden of Informal Caregiving Associated With Falls With and Without Injuries, per Person
| Modela/Fall statusb | Burden of informal caregiving
|
||
|---|---|---|---|
| Annual economic burden
|
|||
| Weekly hoursc,d | Per patient ($)d,e | National estimates ($ billion)d,f | |
| Stroke | |||
|
| |||
| Falls without injuries | 5.26 (−0.94, 11.46) | 2,883 (−515, 6,281) | 3.17 (−0.57, 6.91) |
|
| |||
| Fall with injuries | 10.54 (4.10, 16.98) | 5,777 (2,247, 9,306) | 2.89 (1.12, 4.65) |
|
| |||
| Non-stroke | |||
|
| |||
| Falls without injuries | 1.70 (0.97, 2.42) | 932 (532, 1,326) | 8.11 (4.63, 11.54) |
|
| |||
| Fall with injuries | 3.28 (2.17, 4.39) | 1,798 (1,189, 2,406) | 6.47 (4.28, 8.66) |
|
| |||
| Total | |||
|
| |||
| Falls without injuries | 2.12 (1.34, 2.90) | 1,162 (734, 1,589) | 11.50 (7.27, 15.74) |
|
| |||
| Fall with injuries | 4.06 (3.02, 5.11) | 2,225 (1,655, 2,801) | 9.35 (6.95, 11.76) |
Note: Boldface indicates statistical significance (p<0.05).
Authors conducted three two-part models separately, using different samples. The first model used stroke survivors only, the second used only those who never had a stroke, and the last model used all samples.
Fall status is the main independent variable. Other independent variables used in the model is shown in footnote c.
Estimated results are from two-part models with adjustment for race; gender; age; marital status; education; number of chronic diseases (0–1, 2–3, and >4); net total non-housing wealth; and usage of formal caregiving.
Numbers in parentheses are the 95% CIs.
Per-patient annual economic burden of informal caregiving associated with falls with and without injuries were estimated by multiplying total weekly hours by 52 weeks and then multiplying the product by median wages for health aides ($10.54/hour) supplied by the 2015 U.S. Bureau of Labor Statistics.
National estimates were derived by multiplying the per capita annual economic burden of informal caregiving times the national estimate of people with stroke and without stroke aged ≥65 years from the 2010 Health and Retirement Study by their experience with falling.
When the lower-bound value estimates of informal caregiving ($7.25/hour) was used, the economic burden of informal caregiving associated with fall-related injuries among elderly stroke survivors was about $2.0 billion per year, and the annual burden associated with falls without injuries among the same population was about $2.2 billion (Appendix Table 3, available online). For those who never had a stroke, the annual national economic burden of informal caregiving associated with falls without injuries and falls with injuries was $5.6 billion and $4.5 billion, respectively.
DISCUSSION
In this study, the authors found that both non-injurious falls and falls that produced an injury were positively associated with the burden of informal caregiving among older adults in the U.S. Although stroke survivors without falls in the past 2 years reported an average 7.1 hours a week of informal caregiving, the estimates of an additional weekly 10.5 hours of informal caregiving associated with injurious falls for stroke survivors suggests that injurious falls more than doubled the informal caregiving burden among stroke survivors who experienced such falls.
This study has some significant strengths, including being the first study examining the costs of informal caregiving associated with falls among older adults. The findings may suggest potential economic benefit to society associated with fall intervention programs. Several types of fall prevention interventions are known to reduce the risk of falling among older adults. Group and home-based exercise programs as well as interventions involving an assessment of home safety have been shown to reduce the rate of falls and risk of falling.25 A home safety assessment, including the addition of grab bars near a tub, shower, and a toilet, and installation of railings on both sides of stairs,10 can help maintain the independent living of care recipients.26
In addition, the present study examined the burden of informal caregiving associated with falls by stroke status and found that the stroke survivors with injurious falls used more informal caregiving than stroke survivors without falls. This finding underscores the importance of fall prevention policies, guidelines, and programs that are tailored to specific post-stroke deficits among elderly survivors of stroke.27 Although general fall precautions are insufficient for stroke survivors, stroke-specific interventions to prevent falls are not well developed yet.28 Because the post-stroke deficits vary by location of stroke and damaged brain, it is important to develop a patient-specific fall prevention program among stroke survivors. For instance, those who have had a left-sided stroke generally have right-sided weakness, including right-side visual deficits.28 Putting the right side of the bed against a wall and thus ensuring getting out of bed from the left side (unaffected side) may prevent falls for those who have had a left-side stroke.28 The findings also emphasize the value of benefits of a healthcare plan, which helps stroke survivors manage their recovery.
Another strength of this study is its use of a nationally representative data set and two-part models to estimate the economic burden of informal caregiving. Because the data are able to provide population estimates, one could estimate the national-level burden of informal caregiving associated with falls. Those with injurious falls used more informal caregiving hours than those whose falls did not cause an injury. However, the number of older adults suffering a fall that did not cause injury was substantially larger than the number who were injured in a fall. As a consequence, the national estimates showed that the economic burden of informal caregiving associated with falls that did not cause an injury was higher than the economic burden with injurious falls ($12.0 billion vs $9.6 billion). This finding emphasizes the importance of preventing both injurious and non-injurious falls.
Limitations
There are some limitations to this study that should be noted. First, the study used self-reported information about falls, stroke, and other chronic conditions. Thus, there could be a self-reporting bias in the data. Although the authors tried to control many chronic health conditions, there is still a possibility that omitted variables, such as mobility issues, which can be correlated with both falls and informal caregiving, might have caused possible bias in the analyses. The authors assumed activities of daily living/instrumental activities of daily living, which is highly correlated with mobility, as mediators between fall and informal caregiving in the conceptual model, and did not use them for a predictor of informal caregiving.
Another limitation is that the self-reported fall indicators captured falls in the past 2 years without information on timing. Unlike a stroke, which usually leaves long-term disability after its onset, non-injurious fall status 1–2 years earlier may not be associated with the current burden of informal caregiving. Also, although it was assumed that typically stroke preceded recent falls in the sample, the authors acknowledge that some people may have had a first-ever stroke in the past 2 years and had a fall before they had a stroke.
Because the authors do not have a proper unit cost measure for an opportunity cost approach, which estimates the value of informal caregivers’ foregone time, they could not compare the results from a replacement cost approach to the results from the opportunity cost approach. A range of estimates is provided by using a federal minimum wage as a lower-bound estimate and a median wage of home health aide as a baseline estimate. The latter may be conservative because the cost of hiring a home health aide can include taxes and fringe benefits as well as agency fees.
One should also note that this study could not compare the burden of informal caregiving before and after falls. After injurious falls, older adults may need to move into formal services rather than using informal care as they did before because of higher demands of caregiving.29 Examining the needs for informal and formal caregiving before and after falls would be an important topic.
CONCLUSIONS
This study found that the economic burden of informal caregiving associated with falls was substantial among both stroke survivors and those who had never had a stroke. Stroke survivors are more likely to have both falls in general and injurious falls in the past 2 years. Falls are associated with a greater burden of informal caregiving among stroke survivors than among those who had not experienced a stroke. Developing strategies for preventing falls and fall-related injuries among older adults, especially among stroke survivors, has the potential for reducing the burden of informal caregiving in the U.S.
Supplementary Material
Acknowledgments
Publication of this article was supported by the U.S. Centers for Disease Control and Prevention (CDC), an Agency of the U.S. Department of Health and Human Services, and the Association for Prevention Teaching and Research (APTR) Cooperative Agreement No. 1U36 OE000005.
The findings and conclusions in this publication are those of the authors and do not necessarily represent the official position of the CDC.
Footnotes
This article is part of a supplement issue titled The Economics of Hypertension and Cardiovascular Disease.
No financial disclosures were reported by the authors of this paper.
SUPPLEMENTAL MATERIAL
Supplemental materials associated with this article can be found in the online version at https://doi.org/10.1016/j.amepre.2017.07.020.
References
- 1.Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics—2016 update: a report from the American Heart Association. Circulation. 2016;133(4):e38–e360. doi: 10.1161/CIR.0000000000000350. https://doi.org/10.1161/CIR.0000000000000350. [DOI] [PubMed] [Google Scholar]
- 2.CDC. Stroke facts. www.cdc.gov/stroke/facts.htm. Published 2015. Accessed January 18, 2017.
- 3.NIH Senior Health. Falls and older adults. https://nihseniorhealth.gov/falls/aboutfalls/01.html. Published 2013. Accessed January 18, 2017.
- 4.Stevens JA, Ballesteros MF, Mack KA, Rudd RA, DeCaro E, Adler G. Gender differences in seeking care for falls in the aged Medicare population. Am J Prev Med. 2012;43(1):59–62. doi: 10.1016/j.amepre.2012.03.008. https://doi.org/10.1016/j.amepre.2012.03.008. [DOI] [PubMed] [Google Scholar]
- 5.Hall MJ, Levant S, DeFrances CJ. Hospitalization for stroke in U.S. hospitals, 1989–2009. NCHS Data Brief. 2012;95:1–8. [PubMed] [Google Scholar]
- 6.Wagner LM, Phillips VL, Hunsaker AE, Forducey PG. Falls among community-residing stroke survivors following inpatient rehabilitation: a descriptive analysis of longitudinal data. BMC Geriatr. 2009;9(1):46. doi: 10.1186/1471-2318-9-46. https://doi.org/10.1186/1471-2318-9-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hyndman D, Ashburn A, Stack E. Fall events among people with stroke living in the community: circumstances of falls and characteristics of fallers. Arch Phys Med Rehabil. 2002;83(2):165–170. doi: 10.1053/apmr.2002.28030. https://doi.org/10.1053/apmr.2002.28030. [DOI] [PubMed] [Google Scholar]
- 8.Divani AA, Vazquez G, Barrett AM, Asadollahi M, Luft AR. Risk factors associated with injury attributable to falling among elderly population with history of stroke. Stroke. 2009;40(10):3286–3292. doi: 10.1161/STROKEAHA.109.559195. https://doi.org/10.1161/STROKEAHA.109.559195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Murray CJ, Atkinson C, Bhalla K, et al. The state of U.S. health, 1990–2010: burden of diseases, injuries, and risk factors. JAMA. 2013;310(6):591–608. doi: 10.1001/jama.2013.13805. https://doi.org/10.1001/jama.2013.13805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.CDC. Important facts about falls. www.cdc.gov/homeandrecreationalsafety/falls/adultfalls.html. Published 2016. Accessed January 18, 2017.
- 11.Joo H, Dunet DO, Fang J, Wang G. Cost of informal caregiving associated with stroke among the elderly in the United States. Neurology. 2014;83(20):1831–1837. doi: 10.1212/WNL.0000000000000986. https://doi.org/10.1212/WNL.0000000000000986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Joo H, George MG, Fang J, Wang G. A literature review of indirect costs associated with stroke. J Stroke Cerebrovasc Dis. 2014;23(7):1753–1763. doi: 10.1016/j.jstrokecerebrovasdis.2014.02.017. https://doi.org/10.1016/j.jstrokecerebrovasdis.2014.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hickenbottom SL, Fendrick AM, Kutcher JS, Kabeto MU, Katz SJ, Langa KM. A national study of the quantity and cost of informal caregiving for the elderly with stroke. Neurology. 2002;58(12):1754–1759. doi: 10.1212/wnl.58.12.1754. https://doi.org/10.1212/WNL.58.12.1754. [DOI] [PubMed] [Google Scholar]
- 14.Joo H, Zhang P, Wang G. Cost of informal care for patients with cardiovascular disease or diabetes: current evidence and research challenges. Qual Life Res. 2017;26(6):1379–1386. doi: 10.1007/s11136-016-1478-0. https://doi.org/10.1007/s11136-016-1478-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Faes MC, Reelick MF, Joosten-Weyn Banningh LW, Gier M, Esselink RA, Olde Rikkert MG. Qualitative study on the impact of falling in frail older persons and family caregivers: foundations for an intervention to prevent falls. Aging Ment Health. 2010;14(7):834–842. doi: 10.1080/13607861003781825. https://doi.org/10.1080/13607861003781825. [DOI] [PubMed] [Google Scholar]
- 16.Burns ER, Stevens JA, Lee R. The direct costs of fatal and non-fatal falls among older adults—United States. J Safety Res. 2016;58:99–103. doi: 10.1016/j.jsr.2016.05.001. https://doi.org/10.1016/j.jsr.2016.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.HRS 2010 fat (final v3.0) and core (final v4.0) public use dataset. University of Michigan; 2014. Health and Retirement Study. [Google Scholar]
- 18.Gure TR, Kabeto MU, Blaum CS, Langa KM. Degree of disability and patterns of caregiving among older Americans with congestive heart failure. J Gen Intern Med. 2008;23(1):70–76. doi: 10.1007/s11606-007-0456-1. https://doi.org/10.1007/s11606-007-0456-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Langa KM, Vijan S, Hayward RA, et al. Informal caregiving for diabetes and diabetic complications among elderly Americans. J Gerontol B Psychol Sci Soc Sci. 2002;57(3):S177–S186. doi: 10.1093/geronb/57.3.s177. https://doi.org/10.1093/geronb/57.3.S177. [DOI] [PubMed] [Google Scholar]
- 20.Joo H, Fang J, Losby JL, Wang G. Cost of informal caregiving for patients with heart failure. Am Heart J. 2015;169(1):142–148. doi: 10.1016/j.ahj.2014.10.010. https://doi.org/10.1016/j.ahj.2014.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dewey HM, Thrift AG, Mihalopoulos C, et al. Informal care for stroke survivors: results from the North East Melbourne Stroke Incidence Study (NEMESIS) Stroke. 2002;33(4):1028–1033. doi: 10.1161/01.str.0000013067.24300.b0. https://doi.org/10.1161/01.STR.0000013067.24300.B0. [DOI] [PubMed] [Google Scholar]
- 22.Bureau of Labor Statistics. Occupational employment statistics: occupational employment and wages, May 2015. www.bls.gov/oes/current/oes311011.htm. Published May 2015. Accessed January 9, 2017.
- 23.Arno PS, Levine C, Memmott MM. The economic value of informal caregiving. Health Aff (Millwood) 1999;18(2):182–188. doi: 10.1377/hlthaff.18.2.182. https://doi.org/10.1377/hlthaff.18.2.182. [DOI] [PubMed] [Google Scholar]
- 24.Wage and hour division, U.S. Department of Labor. Changes in basic minimum wages in non-farm employment under state law: selected years 1968 to 2016. www.dol.gov/whd/state/stateMinWageHis.htm. Published 2016. Accessed May 31, 2017.
- 25.Gillespie LD, Robertson MC, Gillespie WJ, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2012;9:CD007146. doi: 10.1002/14651858.CD007146.pub3. https://doi.org/10.1002/14651858.cd007146.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Agree EM, Freedman VA, Cornman JC, Wolf DA, Marcotte JE. Reconsidering substitution in long-term care: when does assistive technology take the place of personal care? J Gerontol B Psychol Sci Soc Sci. 2005;60(5):S272–S280. doi: 10.1093/geronb/60.5.s272. https://doi.org/10.1093/geronb/60.5.S272. [DOI] [PubMed] [Google Scholar]
- 27.Winstein CJ, Stein J, Arena R, et al. Guidelines for adult stroke rehabilitation and recovery: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2016;47(6):e98–e169. doi: 10.1161/STR.0000000000000098. https://doi.org/10.1161/STR.0000000000000098. [DOI] [PubMed] [Google Scholar]
- 28.Quigley PA. Redesigned fall and injury management of patients with stroke. Stroke. 2016;47(6):e92–e94. doi: 10.1161/STROKEAHA.116.012094. https://doi.org/10.1161/STROKEAHA.116.012094. [DOI] [PubMed] [Google Scholar]
- 29.Roe B, Howell F, Riniotis K, Beech R, Crome P, Ong BN. Older people and falls: health status, quality of life, lifestyle, care networks, prevention and views on service use following a recent fall. J Clin Nurs. 2009;18(16):2261–2272. doi: 10.1111/j.1365-2702.2008.02747.x. https://doi.org/10.1111/j.1365-2702.2008.02747.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


