Abstract
Despite significant therapeutic advances for HIV-1 infected individuals, a preventative HIV-1 vaccine remains elusive. Studies focusing on early transmission events, including the observation that there is a profound loss of gastrointestinal (GI) CD4+ T cells during acute HIV-1 infection, highlight the importance of inducing HIV-specific immunity within the gut. Here, we report on the generation of cellular and humoral immune responses in the intestines by a mucosally administered, dendritic cell (DC) targeted vaccine. Our results show that nasally delivered α–CD205-p24 vaccine in combination with polyICLC, induced poly-functional immune responses within naso-pulmonary lymphoid sites that disseminated widely to systemic and mucosal (GI tract and the vaginal epithelium) sites. Qualitatively, while α–CD205-p24 prime-boost immunization generated CD4+ T cell responses, heterologous prime-boost immunization with α–CD205-p24 and NYVAC gag-p24 generated high levels of HIV-specific CD4+ and CD8+ T cells within the GI tract. Finally, DC targeting enhanced the amplitude and longevity of vaccine induced immune responses in the GI tract. This is the first report of a nasally delivered, DC targeted vaccine to generate HIV-specific immune responses in the GI tract and will potentially inform the design of preventative approaches against HIV-1 and other mucosal infections.
INTRODUCTION
Despite a dramatic improvement in survival of HIV-1 infected patients with combination antiretroviral therapy (cART), HIV vaccine development remains a global priority. A key feature of HIV-1 transmission includes the preferential targeting of virus to gastrointestinal (GI) lymphocytes during acute HIV-1 (1, 2) and SIV (3) infections, independent of the route of viral inoculation. A recent study demonstrated a strikingly rapid seeding of viral reservoirs, including those in the GI tract, even prior to the appearance of systemic viremia in SIV-infected Rhesus Macaques (4). Therefore, it has been argued that the goal of an effective HIV vaccine should be to interrupt mucosal transmission at its earliest stages and to prevent viral production in mucosal tissues (5).
Targeting antigens to dendritic cells (DC) is a strategy to enhance the effectiveness of vaccination, reviewed in ref (6). Among the DC associated receptors that have been targeted to boost cellular and humoral adaptive immunity are Fcγ receptors (7), MHC II molecules (8), CD40 (9), CD11b (10), CD11c (11) and a number of C type lectins including CD205 (12), CD207 (13), macrophage mannose receptor (14), CLEC9A (15), DCIR2 (16), DC-SIGN (17) and dectin 1 (18). CD205 or DEC-205 targeting is perhaps best studied in the context of HIV-1 vaccine design. This involves engineering an α–CD205-p24 fusion construct which is then administered in combination with an adjuvant such as polyICLC to boost HIV-1 specific immune responses in mice (19), non human primates (20) and humans (21). In the present study, we have used an analogue of Polyriboinosinic-polyribocytoidylic acid (Poly IC) as the adjuvant. PolyIC is a synthetic double-stranded RNA, recognized by TLR3 and other intracellular receptors. A complex of poly IC with poly-L-lysine and carboxymethylcellulose (poly ICLC), is five to 10 times more resistant to hydrolysis by RNAse than the parent poly I:C. Additionally, PolyICLC demonstrates a greater potency for interferon induction than its parent, PolyIC (22). Notably, GI mucosal immunity, highly relevant to HIV-1 vaccine development effort, has never been examined using a DC targeted vaccine.
Our goal here was to induce and detect HIV-1 specific T and B cell responses in the GI tract. We focused on mucosal vaccination as it offers many attractive features including the ease of administration, potential for mass immunization, reduced cost of production, storage and delivery. Additionally, mucosal vaccination is considered superior to systemic vaccination for recruiting cells to local (23), regional (24, 25) and distant mucosal sites (26) for non-HIV and HIV- (and SIV-) specific (27, 28) antigens. In studying the mechanism(s) of protection elicited by mucosal vaccines, we have previously demonstrated that intranasal vaccination licenses T cells (29) and B cells to the GI tract through the induction of gut homing receptors α4 β7 and CCR9. In the present study, we demonstrate that intranasal delivery of an α–CD205-p24 fusion antibody induces and directs HIV-specific T and B cells to the GI tract. Thus, here we define the first study of a DC targeted vaccine to induce GI immune responses directed against HIV. The data presented herein is of relevance to the HIV-1 vaccine development effort as well as for mucosal vaccination against other enteric and pulmonary pathogens.
RESULTS
Intranasal immunization with α–CD205-p24 and poly ICLC induces HIV-specific CD4+ T cell responses in the intestinal lamina propria
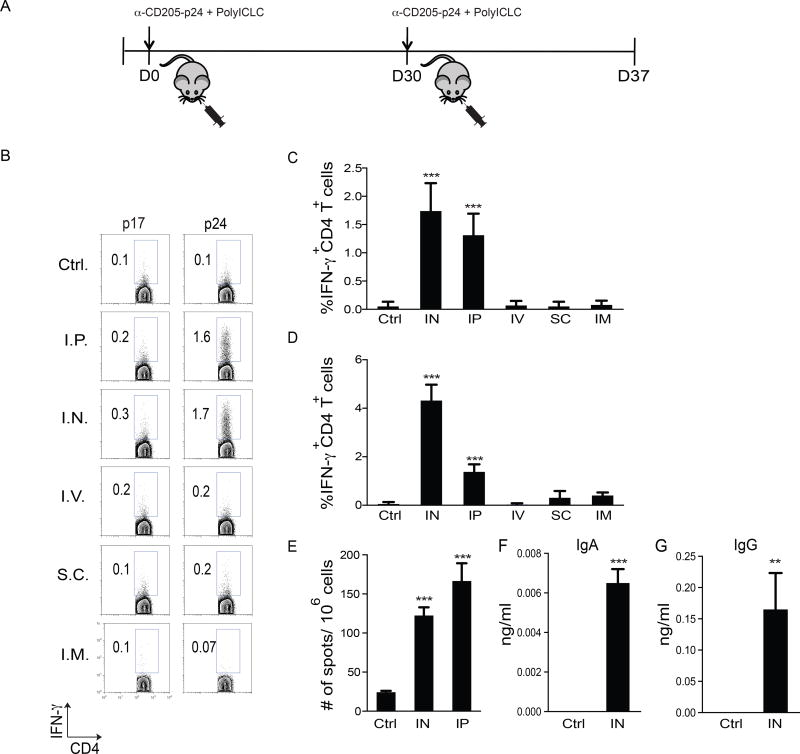
With the goal of inducing HIV-specific immune responses in the GI tract, we compared mucosal and systemic routes of vaccine delivery. C57Bl/6 mice were immunized with 5µg of α–CD205-p24 and 50 µg of polyICLC, administered either intranasally (i.n.), intraperitoneally (i.p.), intravenously (i.v.), subcutaneously (s.c.), or via the intramuscular (i.m.) routes. A booster dose of the vaccine was administered 4 weeks after priming. As a control, α-CD205-empty, which did not carry any antigen, and polyICLC were administered i.p. (Ctrl). One-week post boost, mononuclear cells were isolated from the intestinal lamina propria and spleen (Figure 1a).
Figure 1. Intranasal immunization with α–CD205-p24 and poly ICLC delivered i.n and i.p elicit antigen specific IFN-γ+CD4+ T cell responses in the gastrointestinal (GI) lamina propria.
C57Bl/6 mice were immunized with α-CD205-p24 fusion mAb (5µg) and poly ICLC (50µg). The vaccine was delivered i.p., i.n., i.v., s.c. or i.m in a prime boost manner. α-CD205-empty mAb (5µg) delivered i.p. served as control. Mononuclear cells were isolated from the small intestinal lamina propria (SILP) and spleen one-week post vaccine boost. IFN-γ secretion in response to HIV p24 (immunizing) or p17 (control) peptide pools was evaluated by intracellular cytokine staining.
(A) Shows the schema of immunization.
(B) FACS plots from a representative experiment.
(C, D) Data from three independent experiments (5 mice per group) illustrating the mean levels of IFN-γ-producing CD4+ T cells in the (c) SILP and (d) Spleen. Background (p17) subtracted p24 data are shown. Statistical comparisons to α-CD205-empty (Ctrl) mice are shown.
(E) ELISPOT quantification of p24-specific IgA+ cells in the GI tract following i.n. and i.p. immunization. α-CD205-empty mAb (5µg) delivered i.p. served as control. Mean data from two experiments, 5 mice per group. Statistical comparisons to α-CD205-empty (Ctrl) mice are shown.
(F, G) ELISA quantification of p24-specific (f) IgA and (g) IgG in the serum from the above experiments. Error bars show mean ± SD. ***=p<0.001
IFN-γ producing CD4+ T cells were detected in the small intestinal lamina propria (SILP) following i.n. and i.p. routes of vaccine delivery. In contrast, i.v., s.c., and i.m. vaccination failed to induce detectable levels of antigen specific CD4+ T cells in the SILP (Figures 1b, c). Similar findings were noted in the spleen (Figure 1d). Furthermore, i.n. and i.p immunization induced HIV p24-specific IgA+ B cells in the SILP, as confirmed by ELISPOT (Figure 1e). Since i.n. immunization is clinically feasible, it was explored further and was found to induce p24-specific IgA and IgG antibodies in the serum (Figures 1f ,g)
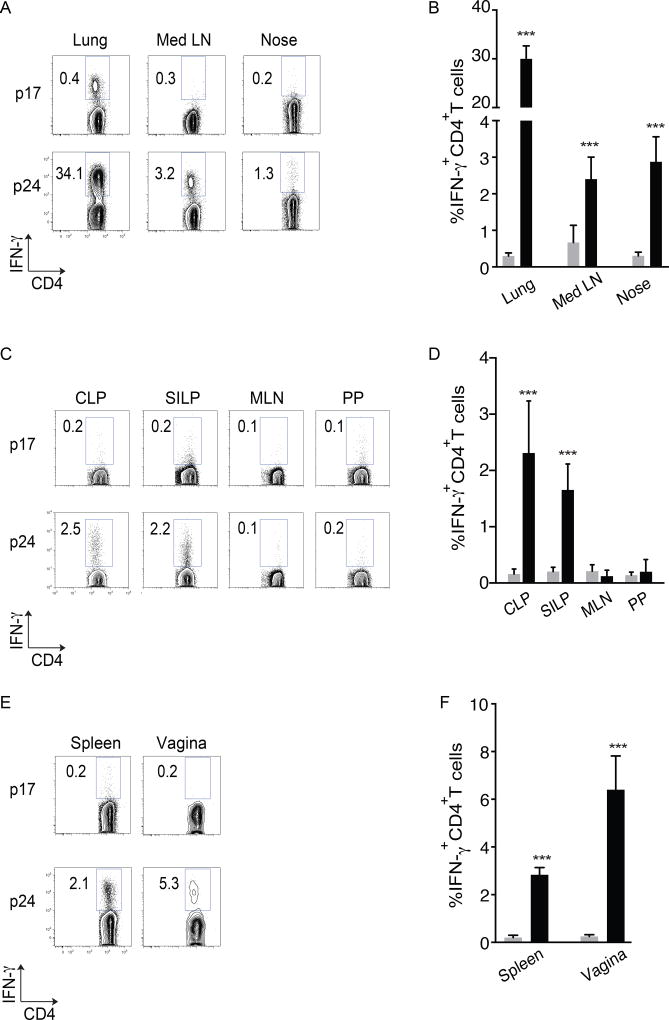
Intranasal immunization induces IFN-γ+CD4+ T cells locally, followed by dissemination to the effector sites of the GI tract
To examine the sites of induction of immunity following i.n. vaccination, we isolated mononuclear cells from the nose, mediastinal LN (Med LN) and lungs of vaccinated mice. HIV-p24 specific CD4+ T cells were readily detectable in lungs, Med LN and nose suggesting a local generation of vaccine induced immune response (Figures 2a,b). In fact, striking frequencies of HIV-specific T cells were detected in the lung, highlighting the potential efficacy of i.n. delivered DC-targeted vaccines against other pulmonary pathogens like pneumonic plague (30).
Figure 2. Following intranasal immunization, p24 immune responses are generated within nasal and lung tissues and disseminate to mucosal and systemic sites.
(A – F) C57Bl/6 mice were vaccinated i.n. with α-CD205-p24 fusion mAb (5µg) and poly ICLC (50µg) and p24-specific immune responses were evaluated one week post boost.
(A) FACS plots from a representative experiment, illustrating the induction of IFN-γ+CD4+ cells in the lung, mediastinal LN (Med LN) and nose.
(B) Mean data from three independent experiments (5 mice per group). Statistical comparisons to p17 (control) are shown.
(C) FACS plots from a representative experiment, illustrating the induction of IFN-γ+CD4+ cells in the GI effector (CLP and SILP) and inductive (Peyer’s patch- PP and mesenteric LN- MLN) sites.
(D) Mean data from three independent experiments (5 mice per group). Statistical comparisons to p17 (control) are shown.
(E) FACS plots from a representative experiment, illustrating the induction of IFN-γ+CD4+ cells in the spleen and vaginal mucosa.
(F) Mean data from three independent experiments (5 mice per group). Statistical comparisons to p17 (control) are shown.
Error bars show mean ± SD. ***=p<0.001
We hypothesized that GI immune responses were being induced due to the dissemination of antigen specific cells from local sites of induction as opposed to generation of GI immune responses due to swallowed antigen. Accordingly, we examined the inductive (Peyer’s Patches-PP and mesenteric LN-MLN) and effector (SILP and CLP) sites of the GI tract separately. While HIV p24 specific IFN-γ+CD4+ T cells were detected in the SILP and CLP, the PP and MLN of immunized animals did not contain appreciable levels of antigen specific CD4+ T cells (Figures 2c,d). These data demonstrated that the immune response following i.n. vaccination was predominantly noted in the GI effector sites as opposed to the inductive sites. Finally, in addition to the GI tract, we examined the systemic compartments and female reproductive tract and found that i.n. immunization induces HIV-specific CD4+ T cells in the spleen and genital tract in addition to the GI tract (Figures 2e,f).
Combined, these data demonstrate that following i.n. immunization, antigen specific T cells are induced locally within the upper and lower respiratory tracts and disseminate to systemic sites as well as to the gastrointestinal and genital mucosae.
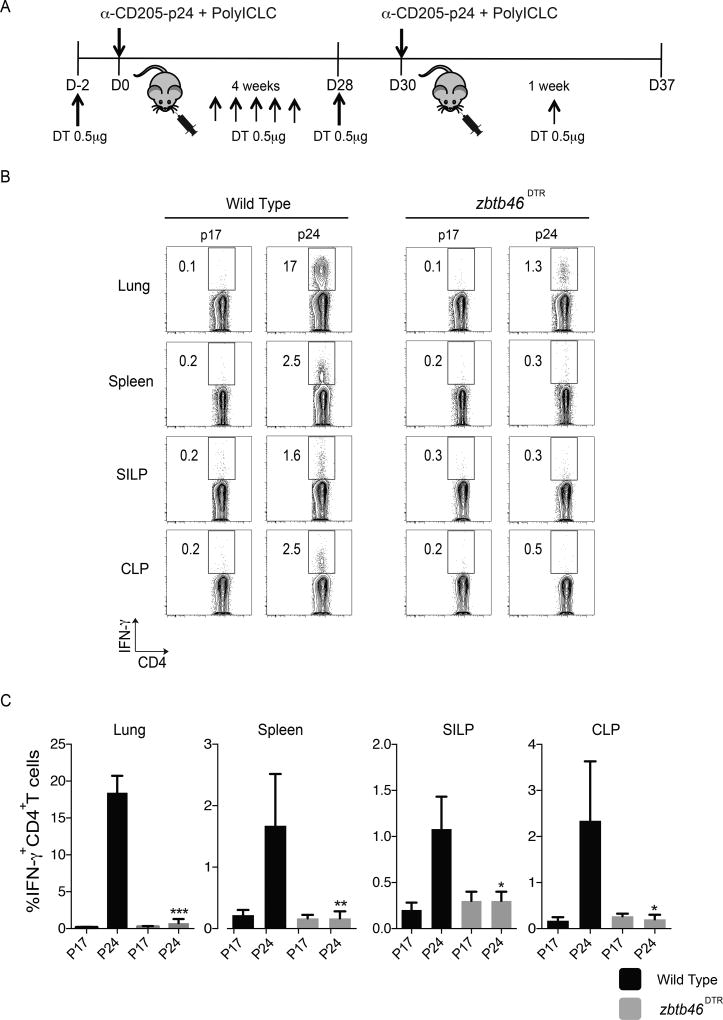
Classical Dendritic cells mediated the induction of IFN-γCD4+ T cells following intranasal vaccination
In order to assess the role of classical dendritic cells (cDC) in our i.n. immunization experiments, zbtb46DTR mice were used. In these mice, a zinc finger transcription factor, Zbtb46, which is specific to cDCs, is conditionally deleted, thus distinguishing cDCs from other cells types expressing CD11c (31).
Chimerization to WT mice was needed to avoid toxicity associated with multiple administrations of diphtheria toxin. Zbtb46DTR chimera and C57Bl/6 WT chimeric mice received 0.5µg of DT i.p. on day -2 prior to vaccination (Figure 3a). Depletion of the cDCs was confirmed in the lungs and spleen of representative mice (data not shown). Both groups of mice were then immunized with α–CD205-p24 (5µg) and polyICLC (50µg) in a prime-boost regimen as described. In order to maintain the deletion of cDCs during the course of immunization, 0.5µg of DT was administered i.p. every 5 days over the priming period and another dose of 0.5µg of DT was administered i.p on day 28 and 4 days following the booster vaccination (Figure 3a). IFN-γ+ T effector responses were strikingly impaired in all of the compartments examined (lung, spleen and GI tract) in Zbtb46DTR but not WT mice (Figures 3b,c) demonstrating that cDCs mediate the effect of i.n. vaccination.
Figure 3. Classical DCs are essential for inducing systemic and mucosal immune responses to intranasal immunization.
Wild type (WT) and zbtb46DTR mice were immunized i.n. with α–CD205-p24 fusion mAb (5µg) and poly ICLC (50µg) in a prime-boost manner. Diphtheria toxin (DT), (0.5µg) was administered i.p., 48 hours prior to immunization and every five days post vaccination. Additional doses of DT were administered on day 28 and 4 days post-boost. IFN-γ secretion in response to HIV gag p24 (immunizing) or p17 (control) peptide pools was evaluated one week post-boost by intracellular cytokine staining.
(A) Shows the schema of immunization
(B) FACS plots from a representative experiment, illustrating the induction of IFN-γ+CD4+ cells in the lung, spleen, SILP and CLP.
(C) Mean data from three independent experiments (5 mice per group) is shown. Statistical comparisons between p24 levels in WT and zbtb46DTR mice are shown. Error bars show mean ± SD. *=p<0.05, **=p<0.01, ***=p<0.001
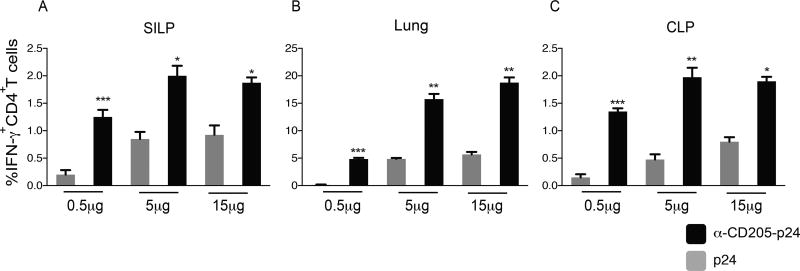
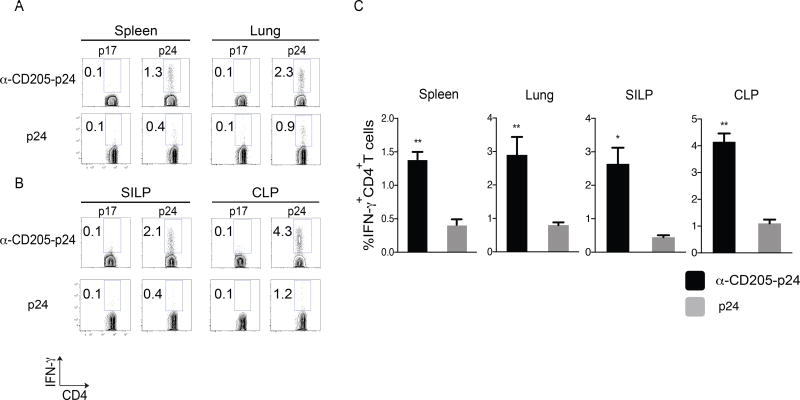
α–CD205-p24 immunization enhances gastrointestinal CD4+ T cell responses relative to untargeted protein immunization
Having shown that i.n. immunization mediated intestinal responses were DC mediated, we wanted to compare the efficacy of DC targeted vaccination with untargeted protein vaccination. C57Bl/6 mice were immunized i.n. with 0.5, 5 and 15 µg of p24 protein plus polyICLC and compared with 0.5, 5 and 15 µg of i.n. delivered α–CD205-p24 and poly ICLC. The DC targeted approach was more potent at inducing antigen-specific immunity within the GI tract compared to untargeted protein vaccination- significantly higher levels of HIV p24-specific, IFN-γ+CD4+ T cells were observed in the lungs, SILP and CLP in the DEC-205 targeted vaccine group compared to untargeted p24 immunized group (Figures 4a - c).
Figure 4. DC targeting enhances the amplitude of anti-p24 immune responses in the GI tract compared to untargeted protein vaccination.
C57Bl/6 mice were immunized i.n. with polyICLC, plus either α–CD205-p24 fusion mAb or untargeted p24 protein, both delivered i.n. in a prime-boost regimen, in escalating doses of 0.5µg, 5µg and 15µg. Mean data from three independent experiments (5 mice per group) is shown in (A-C) where in response to HIV gag-p24 or p17 peptide pools, IFN-γ+CD4+ T cells were quantified in the SILP (a), lung (b) and CLP (c). Background (p17) subtracted p24 data are shown. Additionally, statistical comparisons between α-CD205-p24 fusion mAb and p24 are shown. Error bars show mean ± SD. *=p<0.05, **=p<0.01, ***=p<0.001
Intranasal immunization with α–CD205-p24 induced antigen specific Th1 and Th17 responses in the GI tract
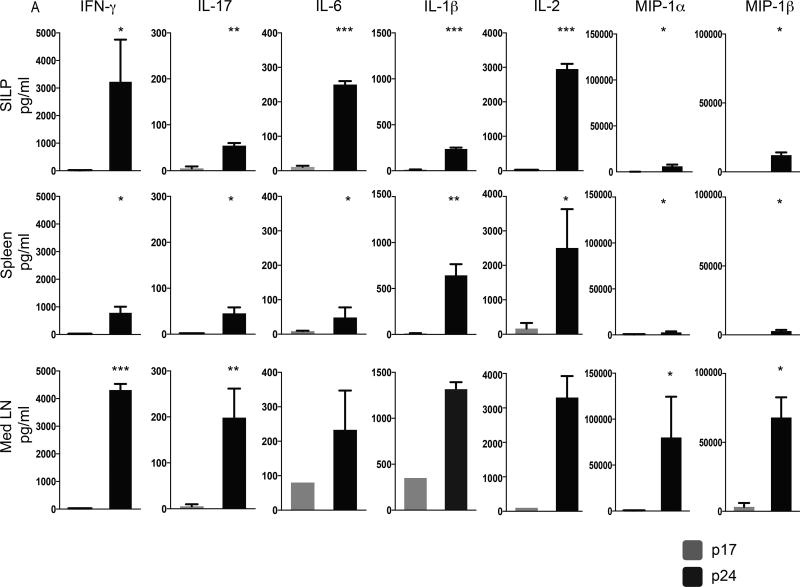
Having established that i.n. vaccination induces antigen specific T cells in the GI effector compartments, the poly-functionality of these cells, considered as a possible correlate of vaccine induced protection (7), was assessed. Mononuclear cells were isolated from the SILP, spleen and MedLN of vaccinated mice and re-stimulated with either p24 or p17 peptide pools and α-CD28 (1µg/ml) for 20 hours. Post re-stimulation the supernatant was collected and cytokine profiles determined using a Bio-Plex mouse cytokine immunoassay. The use of multiplexed ELISA allowed us simultaneous detection of multiple cytokines from a relatively small (~50µl) volume of the sample. Therefore, we chose this method over the conventional, FACS-based study of intracellular cytokines. i.n. immunization induced highly poly-functional CD4+ T cells within local (Med LN), systemic (spleen) and gastrointestinal (SILP and CLP) sites (Figure 5). Specifically, IFN-γ, IL-2, IL-6, IL-17a and IL-1β - cytokines, as well CC chemokines- MIP-1α and MIP-1β were induced post-immunization. Cell yield in the colon was low and was insufficient to provide reliable data. Thus, data from CLP were not included. Thus i.n. immunization with DC-targeted α–CD205-p24 vaccine produced highly polyfunctional T cells in the GI tract
Figure 5. Intranasal immunization with α–CD205-p24 induced predominantly antigen specific Th1 and Th17 responses in the GI tract.
C57Bl/6 mice were immunized i.n. with α–CD205-p24 fusion mAb (5µg) and poly ICLC (50µg) in a prime-boost regimen. One-week post boost, mononuclear cells were isolated from the SILP, spleen, Med LN and CLP and re-stimulated with either p24 or p17 peptide pools and α-CD28 (1µg/ml) for 20 hours. Multiplexed ELISA was used to quantify the levels of secreted IFN-γ, IL-17, IL-6, IL-1β, IL-2, MIP-1α and MIP-1β. Mean data from two individual experiments is shown (5 mice per experiment). Statistical comparisons to p17 control are shown. Error bars show mean ± SD. *=p<0.05, **=p<0.01, ***=p<0.001
Dendritic cell targeting induces long-term memory CD4+ T cells in the GI tract
To test if long-term memory could be detected within the intestinal tract, we examined recall responses in mice immunized with the DC-targeted or untargeted vaccine after 24 weeks of vaccination. Effector-memory cells i.e. T cells producing IFN-γ were readily detected within the spleen, lung, SILP and CLP of mice immunized with the DC targeted vaccine (albeit at a lower frequency in the spleen than at mucosal sites). In contrast, untargeted p24 vaccination induced significantly lower levels of effector-memory cells within the GI compartments or lungs and virtually undetectable levels in the spleen at 24 weeks (Figures 6a – c). Therefore, DC targeting induces long-term memory against p24 protein in the intestinal tissues.
Figure 6. α–CD205-p24 vaccine delivered i.n. induces long term memory in effector sites of the GI tract.
C57Bl/6 mice were immunized in a prime-boost regimen with polyICLC plus either α–CD205-p24 fusion mAb (5µg) or p24 (15µg, the highest dose of untargeted p24 vaccine was chosen). Mice were sacrificed 25 weeks post boost and lymphocytes were isolated from the spleen, lung and the effector sites (SILP and CLP) of the GI tract. IFN-γ+CD4+ T cells were examined by flow cytometry.
(A, B) FACS plots from a representative experiment showing antigen specific IFN-γ+CD4+ T cells in the spleen, lung, SILP and CLP. (C) Mean data from three independent experiments is shown (5 mice per group). Background (p17) subtracted p24 data are shown. Statistical comparisons between α-CD205-p24 fusion mAb and p24 are shown. Error bars show mean ± SD. *p<0.05, **p<0.01, ***p<0.001
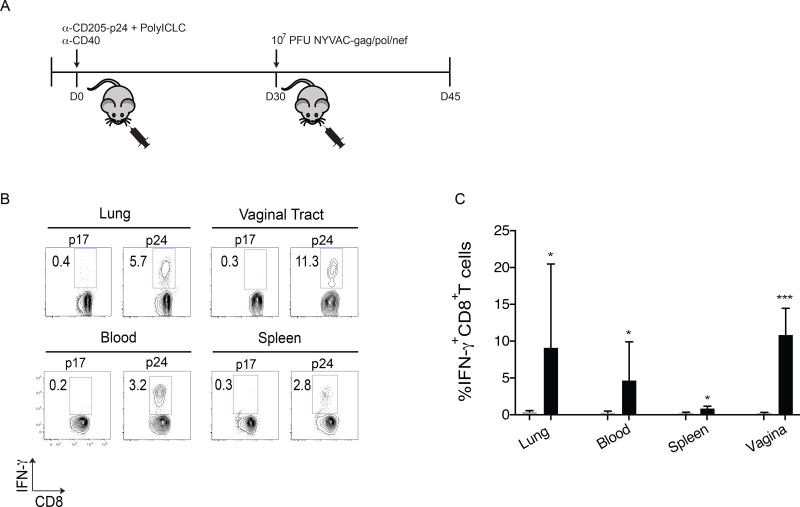
Heterologous α–CD205-p24 prime, NYVAC gag/pol/nef boost immunization, generates p24-specific CD8+ T cells in the systemic and mucosal compartments
α–CD205-p24 prime-boost vaccine used in the present study raised concerns regarding generation of HIV-specific CD4+ T cells in the GI and vaginal tracts, potentially with enhanced susceptibility to the virus (32) Therefore, we wanted to develop a platform to generate HIV-specific CD8+ T cells at these mucosal sites and performed heterologous prime-boost experiments (priming with α–CD205-p24 followed by a NYVAC-gag boost). We hypothesized that vaccinating with DEC-205 targeted vaccine would generate p24-specific helper T cells which could then enhance the induction of CD8+ T cell responses using a poxvirus vector such as NYVAC (33). Using a heterologous prime-boost immunization regimen, first generation C57Bl/6 and Balb/c offspring (F1 mice) were immunized with 25µg of α-CD40, 50µg of polyICLC and 5µg of α–CD205-p24 delivered i.n. For these experiments, F1 hybrid mice (first generation C57Bl/6 and Balb/c offspring) were used since the CD8 response is directed to a defined gag 197-205 peptide presented only on H-2d but not H-2b as shown previously (34). The F1 mice were immunized with 25µg of α-CD40, 50µg of polyICLC and 5µg of α–CD205-p24 delivered i.n. Previous observations have demonstrated that a combination of a TLR ligand and an agonist α-CD40 antibody elicited stronger immunity (19, 35). Therefore, we immunized with a combination of α-CD40 and PolyICLC in these experiments. Four weeks later the mice were administered 107 PFU of NYVAC-gag/pol/nef, delivered i.n. (Figure 7a). Additionally i.p. immunization was also assessed (Supplemental Figure 1). 14 days post boost, IFN-γ+CD8+ T cell responses were observed in the lung, spleen, blood and vaginal tract of the i.n. immunized mice (Figures 7b,c). Unfortunately, poor viability of intestinal mononuclear cells precluded conclusions to be drawn in 2 of 3 experiments of the i.n. immunized group. However, robust levels of intestinal IFN-γ+CD8+ T cells were detected in the GI tract of the i.p. immunized mice. Therefore, we conclude from these experiments that while α–CD205-p24 prime boost immunization generated predominantly CD4+ T cell responses, with a heterologous α–CD205-p24 prime, NYVAC boost immunization regimen, we were able to generate gag p24-specific CD8+ T cells within the systemic compartment as well as mucosal sites.
Figure 7. Heterologous α–CD205-p24 prime, NYVAC gag/pol/nef boost immunization, generates p24-specific CD8+ T cells in the systemic and mucosal compartments.
F1 hybrid (cross between BALB/c females and C57Bl/6 males; heterozygous at all loci) mice were immunized with α–CD205-p24 fusion mAb (5µg), poly ICLC (50µg) and α-CD40 (25µg). After 4 weeks, the mice were administered 107 PFU NYVAC gag/pol/nef delivered i.n. After 2 weeks of boost, IFN-γ secretion was evaluated in CD8+ T cells.
(A) Shows the schema of immunization.
(B) FACS plots from a representative experiment, illustrating the induction of IFN-γ+CD8+ cells in the lung, vaginal tract, blood and spleen.
(C) Mean data from three independent experiments (5 mice per group) summarizing IFN-γ+CD8+ T cells in the lung, Blood, Spleen and vagina. Statistical comparisons to p17 (control) are shown. Error bars show mean ± SD. *=p<0.05, ***=p<0.001
DISCUSSION
The global impact of HIV infection is staggering. Since it was recognized over 34 years ago (36), the HIV pandemic has resulted in the infection of nearly 60 million people worldwide, nearly half of who have died from the disease. It is widely accepted that while substantial advances have been made in the field of HIV therapeutics, an effective HIV vaccine would be the optimum solution for the ultimate control of the global AIDS pandemic (37).
The present study was guided by three principles. First, given the profound effect of HIV-1 infection on GI-resident CD4+ T cells (1, 3) our goal was to induce HIV-1 specific immune responses in the GI mucosa. Second, targeting DC-specific lectins and endocytic receptors has been demonstrated to enhance the potency, magnitude and longevity of vaccine induced systemic immune responses (12, 19, 38, 39), therefore we wanted to adopt a DC-targeted approach to enhance mucosal immunity. Third, since mucosal routes of vaccine delivery are superior to systemic routes in inducing mucosal immune responses (28, 40–42), we wanted to immunize across a mucosal surface to induce HIV-1 specific cells in the gut. Combined, here we provide the first study of a mucosally delivered, DC-targeted vaccine to generate HIV-1 specific immune responses in the GI tract.
Although, to date no evidence exists that CD4+ T cell activation or vaccine-induced CD4+ T cells result in heightened HIV-1 acquisition or viremia after infection (43, 44), α–CD205-p24 prime-boost vaccine used in the present study raises concerns regarding generation of HIV-specific CD4+ T cells in the GI and vaginal tracts, potentially with enhanced susceptibility to the virus (32). In particular, our data need to be evaluated in the context of the STEP (HVTN 502/Merck 023) Trial- a multicenter phase IIb study of Ad5 HIV-1 clade B gag/pol/nef vaccine compared with placebo (45). The study was halted prematurely in 2007 due to lack of vaccine efficacy despite inducing IFN-γ ELISPOT responses in the peripheral blood. A similar Phambili/HVTN 503 study, also using the Merck Ad5 vaccine did not reveal increased susceptibility to HIV as was seen in the Step Trial, but the study was scientifically inconclusive due to premature discontinuation of the trial (46). Post-hoc analyses of the Step trial revealed a higher rate of HIV infection in uncircumcised men, seropositive for Ad5 prior to vaccine administration. A number of theories were proposed to understand the correlates of increased susceptibility to HIV seen in this sub-group of Step Trial volunteers. These included the possibility that the vaccine increased the number of activated CD4+ T cells in the peripheral blood, lymphoid tissue or mucosal sites and created potential targets for HIV-1. Subsequent analyses of peripheral blood T cells have debunked the possibility that expansion, activation or homing of Ad5-specific CD4+ T cells was responsible for increased susceptibility to HIV seen in the Step Trial (47, 48). Since mucosal sampling was not included in the Step Trial, analyses of the mucosa became available recently from a different study where rhesus macaques were immunized with rAd5-gag/pol/nef vaccine (rAd5), similar to the vaccine used in the Step Trial. This study also has revealed no increase in the phenotype, frequency or trafficking of Ad5-specific CD4+ T lymphocytes to mucosal target sites following rAd5 vaccination of rhesus monkeys with baseline Ad5 immunity (49). These studies provide evidence against the hypothesis that recruitment of vector-specific CD4+ T cells to mucosal sites led to increased HIV-1 acquisition in Ad5-seropositive, uncircumcised vaccinees in the Step study. A number of additional findings that have emerged from the analyses of Step Trial data which may explain the lack of vaccine efficacy. These include reduced vaccine-specific immunity in Ad5 seropositive individuals (45), narrow epitope recognition by CD8+ T cells (44), and the induction of intestinal microbiota polyreactive HIV non-neutralizing gp-41 reactive antibody repertoire response to HIV Env DNA- rAD5 vaccine (50). Another key feature that has been highlighted by the Step Trial is the fact that HIV vaccine efficacy studies need to incorporate evaluation of mucosal immune responses in their study design (44). This is an aspect that our study attempts to address.
In contrast to the Step Trial, The RV 144 efficacy trial conducted in Thailand provided encouraging evidence that an HIV vaccine could provide modest level of protection against HIV acquisition- 31.2% at 42 months of follow up (43). Immune correlates of protection demonstrated that IgG antibodies to V1V2 loops in the HIV envelope correlated inversely with the rate of HIV-1 infection (51). Notably, again HIV-specific CD4+ T cells were not associated with infection risk in these analyses. In contrast, studies done on a sub-group of RV 144 vaccine recipients confirmed the presence of V2-specific, polyfunctional effector CD4+ T cells (52).
Further proof that HIV-specific CD4+ T cells are not associated with increase risk of disease acquisition comes from the Pre-exposure Prophylaxis Initiative (iPrEx) trial. In this study T cell responses to HIV-1 Gag, Protease, Integrase, Reverse transcriptase, Vif and Nef antigens were examined in exposed-sero negative subjects. IFN-g+CD4+ and - CD8+ responses against Vif- and Integrase were associated with reduced HIV-1 infection risk (53).
Together, based on these data, we infer that although there has been a theoretical risk, the abundance of scientific evidence refutes the claim that HIV-specific CD4+ T cells enhance susceptibility to HIV-1 infection. In fact, we would argue that since the vast majority of neutralizing antibodies and cytotoxic T cells are critically dependent on CD4+ T cell help, inducing specific, potent, broad and long-lived CD4+ T cell response will be essential in the HIV-1 vaccine effort. This was the rationale behind the heterologous prime-boost experiments (priming with α–CD205-p24 followed by a NYVAC-gag boost) in our study. We hypothesized that vaccinating with DEC-205 targeted vaccine would generate robust levels of p24-specific helper T cells which could then enhance the induction of CD8+ T cell responses using a poxvirus vector such as NYVAC (33), A recent phase 1b clinical trial with recombinant adenovirus 5–vectored prime, followed by NYVAC boost showed enhanced vaccine immunogenicity and further validated our rationale (54). In confirmation of our hypothesis, we detected significant numbers (~10–20% of all CD8+ T cells) of p24-specific CD8+ T cells in both the GI tract and the vaginal mucosa. This is the first demonstration of DEC-205 prime, NYVAC boost vaccination and given the robust generation of CD8+ T cells at mucosal surfaces.
The migration of cells to the gut in response to sensitization in the lung (and vice versa) led to the proposal of a “common mucosal immunological system” by Bienenstock et al in 1978 (55). In support of this hypothesis, we have recently demonstrated that intranasal vaccination can target lung DCs to induce gut homing receptors α4β7 and CCR9 and recruit vaccine-primed, antigen-specific, T cells to the GI tract (29). Further, administration of an adjuvant such as polyICLC appeared to boost the expression of α4β7-on T cells following i.n. vaccination (29). In the present study we show that an i.n. delivered α–CD205-p24 vaccine induces gag-p24 specific cells in the inductive sites of the upper (nose associated lymphoid tissue) and lower (Med LN) respiratory tract but not the GI tract (PP and MLN). Interestingly, in addition to effector respiratory sites (lung), gag p24-specific T cells could also be detected in the effector sites of GI (SILP and CLP) and genital (vaginal mucosa) tracts. Although we did not test for the expression of α4β7 (targeting to the gut) or α4β1 (targeting to the vaginal mucosa), our data echo recent findings by Stary et al who show that nasal vaccination against Chlamydia trachomatis targets CD4+ T cells to the vaginal mucosa and offers protection against genital chlamydia infection (56). It follows therefore, that i.n. vaccine induced immune responses, generated locally within the upper and lower respiratory tracts are disseminated widely to other mucosal sites. Thus, the present study provides further functional evidence of i.n. vaccine induced DC-mediated mucosal cross talk.
A number of immunomodulatory agents including toxin based adjuvants, cytokines, CpG DNA, α-Gal-cer, chitosan and non-replicative delivery systems, reviewed in ref (57) have been tested as mucosal adjuvants. We chose microbial mimic and TLR-3 ligand, poly ICLC as an adjuvant based on its enhanced potency compared to other adjuvants when co-administered with protein antigens (22). Furthermore, polyICLC has an established safety record in cancer patients (58–60) and, in a recent study by our lab, polyICLC, administered subcutaneously to a group of human volunteers demonstrated excellent safety (61). This, combined with the data presented here supports the use of polyICLC as a mucosal adjuvant for further studies.
Our study establishes that intranasal vaccine induced immunity is mediated by zbtb46-dependent classical DCs. Additionally, two other features of DC targeting with intranasal vaccines stand out here. First, DC-targeting boosts the amplitude of vaccine-induced mucosal immunity. Second, DC targeting results in a striking increase in the longevity of mucosal immune responses. We speculate that enhanced longevity of DEC-205 targeted immune response could be due to a stronger priming effect. Alternatively, since DEC-205 is expressed in the intestinal epithelium (62), we hypothesize that epithelial DEC-205 signals could maintain the longevity of DEC205 DC-primed mucosal immune responses. We are in the process of testing this hypothesis and if proven, this could make DEC-205 targeting particularly relevant for mucosal vaccines.
Several characteristics of T cells such as phenotype, function, antigen-specificity and MHC restriction have been investigated as potential correlates of immune protection after vaccination (7). Recent data however, suggests that the quality of the immune response, measured through increased levels of antigen-specific polyfunctional T cells capable of producing multiple, relevant cytokines, is a better correlate of sustained protective immunity (63). The use of multiplexed ELISA allowed us simultaneous detection of multiple cytokines from a relatively small (~50µl) volume of the sample. Therefore, we chose this method over the conventional, FACS-based study of intracellular cytokines. Our study demonstrates that i.n. vaccination with α–CD205-p24 vaccine generated polyfunctional T cells, both systemic and mucosal, capable of producing TH1, TH2 and TH17 cytokines as well as β-chemokines. While vaccine induced IFN-γ and IL-2 production is perhaps best studied, there is evidence that β chemokines such as MIP-1 α and MIP-1 β are associated with a better clinical status in HIV-1 infected patients (64). Additionally, IL-17 producing CD4+ T cells have been associated with protective efficacy of vaccines against tuberculosis (65) and rotavirus infections (66), while reduced intestinal IL-17a production is associated with loss of mucosal integrity and with SIV disease progression in Rhesus Macaques (67, 68). The induction of IL-17 producing cells by our α–CD205-p24 vaccine is particularly interesting in this context and worthy of further examination.
Humoral immunity can completely suppress viremia in humanized mice (69, 70), SIV-infected Rhesus Macaques (71) and, in combination with viral inducers, decrease rebound from latent reservoirs of HIV-1 in humanized mice (72). Additionally, as discussed above, the RV-144 Thai trial (43) has demonstrated that vaccine recipients who produced V2-loop antibodies were 31% less likely to get HIV-infected (73). Therefore, although the focus of the present study was induction of T cell immunity, we also investigated vaccine-induced humoral response in the GI mucosa. Notably, antigen targeting to DCs has previously been shown to elicit long-lived T cell help for antibody responses (74). Our study found that the i.n. administered, DC-targeted vaccine induced antigen specific IgA secreting B cells in the intestinal lamina propria. We are planning a more detailed investigation on GI humoral immunity elicited by DC-targeted vaccines.
We would like to mention an important caveat here- how these findings will translate to protection against human infection are unclear at this point and additional studies of in-vivo protection are needed. However, to our knowledge, there are no challenge models to test the efficacy of vaccine-induced, HIV-specific immune responses within the murine GI tract. The Vaccinia-gag model, previously used in the lab (19) is less relevant for delivery across the GI mucosa. As more studies examine the induction of HIV-specific immune responses in the GI tract, the creation of a GI-specific challenge model will become increasingly relevant.
In summary our study is the first demonstration of a DC cell targeted, mucosally delivered vaccine to induce HIV-1 specific immunity in the GI tract. The data presented herein offers insights into future research in identifying preventative strategies not only against HIV-1 infection but also against other enteric and pulmonary pathogens.
MATERIALS & METHODS
Mice
C57Bl/6 mice (B6) and Balb/c mice were purchased from Taconic Labs or bred at Rockefeller University. F1 hybrid mice (cross between BALB/c females and C57Bl/6 males; heterozygous at all loci), were bred at in-house. Zbtb46DTR mice were kindly provided by Dr. M. Nussenszweig (Rockefeller University, New York). All mice were maintained in specific pathogen–free conditions and used at 6–8 weeks unless otherwise specified. Protocols were approved by the Rockefeller University Animal Care and Use Committee.
Construction and production of fusion mAbs
DNA for HIV gag-p24 (aa 133–363 derived from HIV isolate BH10) was cloned in frame into the COOH terminus of the heavy chains of α–mouse-DEC205 as described previously (19). The fusion α–CD205-p24 mAb was produced by transient transfection (calcium phosphate) in 293T cells in serum-free DMEM supplemented with Nutridoma SP (Roche Applied Science). The mAbs were purified on protein G columns (GE Healthcare Bio-Sciences Corp.) and characterized by SDS/PAGE and Western blotting using α-mouse IgG1-HRP (Southern Biotech) or HRP-α-gag-p24 (ImmunoDiagnostics). mAb binding was verified on CHO cells stably transfected with the respective receptor by FACS using phycoerythrin-conjugated goat α-mouse IgG (Jackson ImmunoResearch). Unconjugated α–DEC-205 mAb expressed by stably transfected CHO cells was similarly purified. Recombinant NYVAC-encoding HIV BX08gp120-IIIBGag/Pol/Nef is a replication incompetent vector, kindly provided by Dr. Giuseppe Pantaleo (Centre Hospitalier Universitaire Vaudois (CHUV) Lausanne, Switzerland) and prepared as previously described (75).
Soluble gag-p24 protein
Soluble FLAG gag-p24 protein (76) was expressed by CHO cells and purified from culture supernatant using anti-FLAG M1 Affinity gel (Sigma-Aldrich) following the manufacturer’s instructions. All proteins had <0.125 endotoxin units/µg using a Limulus Amebocyte Lysate assay, QCL-1000 (Bio Whittaker, Walkersville, MD).
HIV gag peptides
Overlapping (staggered by 4 aa) gag p17 and p24 15-mer peptides were obtained from the NIH AIDS Reference Reagent Program (catalog no. 8117). Peptides, including the H-2Kd binding peptide p24 197–205 (34), were also synthesized by the Proteomics Resource Center at The Rockefeller University. As previously described (19), the 30- and 60-member gag p17 and p24 libraries were divided into 3 and 5 pools of 9 to 12 peptides, respectively. The respective gag p17 peptide pools span from aa 1–51 (pool 1), aa 41–91 (pool 2), and aa 81–135 (pool 3) of the HIV gag p17 protein. The respective gag p24 peptide pools span from aa 125–183 (pool 1), aa 173–231 (pool 2), aa 221–279 (pool 3), aa 269–327 (pool 4), and aa 317–363 (pool 5) of the HIV gag p24 protein. Response to individual pools has been mapped previously in our lab (19). Also, previous work from the lab has demonstrated that CD8+ T cell responses elicited by pooled p24 peptides were comparable to the 197-205 nonamer peptides (15). Hence, in the present study, we combined all three p17 peptide pools and all five p24 peptide pools together while testing for recall responses.
Immunization
Mice were injected by various routes including i.n., i.p., i.v., i.m. or s.c. (in the hind footpads) with the indicated doses of fusion α–CD205-p24 mAb, unconjugated α–CD205-empty mAb, or HIV gag-p24 protein along with stimuli for DC maturation-polyICLC (Oncovir) 50 µg, and when indicated- 25µg of agonist α–CD40 mAb (35). Unless otherwise specified, vaccines were delivered in a prime-boost fashion with the booster given 4 weeks after priming. Mice were sacrificed 7 weeks after the booster dose. For determining long term immune responses, mice were sacrificed 25 weeks post-boost.
Isolation of mononuclear cells from various organs and cell preparation
Mice were euthanized and the mononuclear cells were isolated from the following organs:
Intestinal mononuclear cell isolation
As previously described (77), small and large intestines were removed in toto and placed in cold HBSS media containing 5% FCS. The intestines were carefully cleaned from the mesentery and flushed of fecal content. Peyer’s patches were removed and analyzed separately where indicated. Intestines were opened longitudinally and then cut into 1cm pieces. The intestinal tissue was incubated with 1.3 mM EDTA (Cellgro) in HBSS at 37°C for 20 min. The EDTA incubation step was repeated a second time. The supernatants containing intestinal epithelial cell (IEC) with some superficial villi cells, referred to as the “IEC fraction”, were not used in the present study. To isolate the lamina propria lymphocytes (LPL), the remaining intestinal tissue was minced and transferred to conical tubes. The minced pieces were resuspended in 20 ml of complete RPMI containing 0.125 mg/ml of collagenase (Sigma) and shaken at 200 rpm for 50 min at 37°C. The tissue suspension was collected and passed through a 70-µm cell strainer and the cells were pelleted by centrifugation at 1600 rpm. The cells were then resuspended and layered onto a 20/80 % Percoll (GE biochemicals) gradient, centrifuged and collected, washed and resuspended in complete RPMI media. These purified cells constituted the small intestinal lamina propria (SILP) or colonic lamina propria (CLP) lymphocyte population.
Lung mononuclear cell isolation
The pulmonary circulation was perfused with saline to remove the intravascular pool of cells. Lungs were carefully separated from thymic and cardiovascular remnants and removed in toto. Organs were thoroughly minced using iridectomy scissors and incubated for 60 min in digestion medium containing 0. 5 mg/ml of collagenase (Sigma) in a humidified incubator at 37°C and 5% CO2. In the last 5 min, 10 mM EDTA was added. Tissue fragments were disrupted mechanically by pipetting and passed through a 70-µm cell strainer and mononuclear cells were washed twice in RPMI. The cells were then layered onto a 20/80 % Percoll gradient, centrifuged and collected, washed and resuspended in complete RPMI media.
Spleen and LN cell isolation
The spleen and LN were harvested in RPMI media with 5% FCS and digested at 37°C in the presence of 400units/ml of collagenase D (Sigma-Aldrich) or 25 minutes. In the last 5 min, 10 mM EDTA was added. Spleen but not LN samples went through subsequent ACK lysis (Gibco), were washed twice and counted.
Vaginal mononuclear cell isolation
The vaginal tract was excised, cut into fine pieces and incubated in collagenase (Sigma) at 0.5mg/ml at 37°C for 1 h. Tissue was then homogenized, filtered and washed. The resulting cell suspension was layered on a 20/80% Percoll gradient and the interface was collected to obtain an enriched mononuclear cell population.
Peripheral blood mononuclear cell isolation
Blood was obtained from the experimental mice by cardiac puncture in heparinized syringes. Mononuclear cells were obtained by layering on Histopaque (Sigma).
Nasal mononuclear cell isolation
Nose associated lymphoid tissue was isolated as described previously (78). Briefly, the entire nose was dissected out, mechanically disrupted using blunt scissors and transferred to conical tubes. The tissue fragments were digested in 10 ml of RPMI containing 0.3 mg/ml of collagenase (Sigma-Aldrich, St. Louis, MO) and agitated at 200 rpm for 60 minutes at 37°C. The tissue suspension was collected and passed through a 70-µm cell strainer and the cells were pelleted by centrifugation at 1600 rpm for 5 minutes. The resulting cell suspension was layered on a 20/80% Percoll gradient and the interface was collected to obtain an enriched mononuclear cell population.
Recall responses to gag-p24 peptides
As described previously (79), 2–5 × 105 mononuclear cells isolated from various organs were incubated for 6 hours at 37°C with pooled p17 or p24 peptides at a final concentration of 1µg/ml in the presence of α-CD28 antibody (clone 37.51; American Type Culture Collection), final concentration of 2µg/mL. Notably, since our lab has previously demonstrated that the CD4+ T cell response was noted to p24 peptides in pools 1 and 3 and the CD8+ T cell response was directed to p24 peptides in pool 2 (which contained a previously defined gag 197–205 peptide sequence presented on H-2Kd) (19), in the present study, mononuclear cells were incubated with the entire reactive HIV gag-p24 or nonreactive HIV gag-p17 15-mer peptide mix. After one hour of incubation, Brefeldin A (Sigma-Aldrich) was added to a final concentration of 10µg/mL for the 5 remaining hours to allow intracellular cytokine accumulation. For all subsequent steps cells were washed and stained in ice cold PBS with 2% FCS.
Surface staining and intracellular cytokine staining (ICS)
Cells were incubated with α-mouse-CD3, CD4 or CD8 mAbs (all purchased from BD PharMingen) and Aqua LIVE/DEAD fixable (Invitrogen) for 20 min at 4°C after blocking Fcγ receptor with α–CD16/CD23 antibody (ebioscience). Following fixation with Cytofix/Cytoperm Plus™ (BD PharMingen), cells were stained for intracellular IFN-γ (BD Pharmingen) for 30 min at 4°C. Data were collected using BD LSR II and analyzed by FlowJo (Tree Star, Ashland, OR). Dead cell were excluded from the analyses, CD3-gated live CD4+ T cells and CD8+ T cells were analyzed for the expression of IFN-γ as indicated in individual experiments.
Stool and Serum gag-specific IgG and IgA
Stool was collected from vaccinated and control mice and suspended in 1ml of PBS containing protease inhibitor (Roche). Serum was prepared by cardiac bleed, followed by serum separation using microtainer tubes (BD Biosciences). Stool and Serum gag-specific ELISA was performed by coating NUNC plates (Apogent) with 2 µg/ml of gag p24 recombinant protein in ELISA coating buffer overnight at 4°C. Plates were washed 3 times with PBS and blocked with Blocking solution (1× PBS, 5% goat serum, and 0.1% Tween-20) for 1 h at 37°C, followed by sample addition at serial 10-fold titration (dilutions made into blocking solution) for 2 h at room temperature, followed by 3 subsequent washes. A 1:10,000 dilution of goat anti–mouse IgG HRP (Jackson ImmunoResearch) or goat anti-mouse IgA HRP (Life technologies) was added according to standard protocols for 1 h at 37°C, the plate was washed 3 times before addition of 100 µl 1X TMB Substrate Solution (eBioscience) stopped with addition of 2N sulfuric acid, and read at 450/470 nm.
Multiplexed ELISA for polyfunctional T cells
One-week post boost, the vaccinated mice were sacrificed and mononuclear cells were isolated from the local (Med LN), systemic (spleen) and GI mucosal (SILP) compartments and re-stimulated with either p24 or p17 peptide pools and α-CD28 (1µg/ml) for 20 hours. The supernatant was collected and analyzed using a Bio-Plex Pro™ Mouse Cytokine 23-plex assay (Biorad). Briefly, the Bio-Plex assay is an immunoassay, based on magnetic beads, consisting of a sandwich ELISA. Capture antibodies directed against the desired biomarkers were covalently coupled to beads. Coupled beads (50µl) were added to the supernatant (50µl) and incubated for 1 hr at room temperature. After a series of washes to remove unbound protein, a biotinylated detection antibody (25µl) was added and incubated at room temperature for 30 minutes. The final detection complex was formed with the addition of a streptavidin-phycoerthrin (SA-PE) conjugate. The samples were re-suspended in assay buffer at a volume of 125µl. Phycoerytherin served as a fluorescent reporter. The fluorescence was measured in a Luminex-based reader (Biorad). The data was analyzed using Bio-Plex data Pro software™.
ELISPOT
Plates were coated with 5µg/ml gag-p24 protein overnight. Following washing, plates were blocked with RPMI media containing 10% FBS (Gibco), 1% non essential amino acids (Gibco), 1% anti-anti cocktail (Gibco), and 0.1% 2- mercaptoethanol (Gibco). Cells were plated in a concentration of 1-2X 106 cells per well (GI) in triplicate and cultured for 24 hours at 37°C, washed, and isotype specific antibody was detected using HRP-conjugated goat anti-mouse IgA secondary (Southern Biotech). Spots were developed using BD ELISPOT AEC substrate set (551951) according to manufacturers protocol. Spots were quantified using a CTL-ImmunoSpot Analyzer and Software.
Statistical Analysis
Data reported in the figures represent the average of at least three independent experiments. Error bars represent the SD. Statistical analysis using the unpaired t-test between 2 groups was done using Prism software.
Supplementary Material
F1 hybrid (BALB/c females X C57Bl/6 males) mice were immunized in a heterologous prime-boost regimen with α–CD205-p24 mAb (5µg), poly ICLC (50µg) and α-CD40 (25µg) and boosted with 107 PFU NYVAC gag/pol/nef delivered i.p. 2 weeks post boost, IFN-γ secretion was evaluated in CD8+ T cells.
(A) FACS plots from a representative experiment, illustrating the induction of IFN-γ+CD8+ cells in the SILP, vagina, blood and spleen.
(B) Mean data from three independent experiments is shown (5 mice per group).
Error bars show mean ± SD. **=p<0.005, ***=p<0.001
Acknowledgments
We would like to acknowledge two dear colleagues in this paper. First and foremost, this work was inspired by late Dr. Ralph Steinman. The work was initiated and developed in his laboratory. Second, this project was closely done with the help of late Dr. Yoonkyung Do. Additionally, we would like to thank Dr. Dr. Chae Gyu Park for help with the reagents. This work was supported by grants from the American Gastroenterology Association Elsevier Award (S.M.), The Rockefeller University Clinical and Translation science award pilot project from NIH/NCRR (5UL1RR024143-05) National Institutes of Health (S.M.), and The Leona M. and Harry B. Helmsley Charitable Trust, (S.M)
References
- 1.Mehandru S, Poles MA, Tenner-Racz K, Horowitz A, Hurley A, Hogan C, et al. Primary HIV-1 infection is associated with preferential depletion of CD4+ T lymphocytes from effector sites in the gastrointestinal tract. The Journal of experimental medicine. 2004;200(6):761–70. doi: 10.1084/jem.20041196. Epub 2004/09/15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guadalupe M, Reay E, Sankaran S, Prindiville T, Flamm J, McNeil A, et al. Severe CD4+ T-cell depletion in gut lymphoid tissue during primary human immunodeficiency virus type 1 infection and substantial delay in restoration following highly active antiretroviral therapy. Journal of virology. 2003;77(21):11708–17. doi: 10.1128/JVI.77.21.11708-11717.2003. Epub 2003/10/15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brenchley JM, Schacker TW, Ruff LE, Price DA, Taylor JH, Beilman GJ, et al. CD4+ T cell depletion during all stages of HIV disease occurs predominantly in the gastrointestinal tract. The Journal of experimental medicine. 2004;200(6):749–59. doi: 10.1084/jem.20040874. Epub 2004/09/15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Whitney JB, Hill AL, Sanisetty S, Penaloza-MacMaster P, Liu J, Shetty M, et al. Rapid seeding of the viral reservoir prior to SIV viraemia in rhesus monkeys. Nature. 2014;512(7512):74–7. doi: 10.1038/nature13594. Epub 2014/07/22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Neutra MR, Kozlowski PA. Mucosal vaccines: the promise and the challenge. Nature reviews Immunology. 2006;6(2):148–58. doi: 10.1038/nri1777. Epub 2006/02/24. [DOI] [PubMed] [Google Scholar]
- 6.Kastenmuller W, Kastenmuller K, Kurts C, Seder RA. Dendritic cell-targeted vaccines - hope or hype? Nature reviews Immunology. 2014;14(10):705–11. doi: 10.1038/nri3727. Epub 2014/09/06. [DOI] [PubMed] [Google Scholar]
- 7.Thakur A, Pedersen LE, Jungersen G. Immune markers and correlates of protection for vaccine induced immune responses. Vaccine. 2012;30(33):4907–20. doi: 10.1016/j.vaccine.2012.05.049. Epub 2012/06/05. [DOI] [PubMed] [Google Scholar]
- 8.Carayanniotis G, Barber BH. Adjuvant-free IgG responses induced with antigen coupled to antibodies against class II MHC. Nature. 1987;327(6117):59–61. doi: 10.1038/327059a0. Epub 1987/05/07. [DOI] [PubMed] [Google Scholar]
- 9.Palumbo RN, Nagarajan L, Wang C. Recombinant monomeric CD40 ligand for delivering polymer particles to dendritic cells. Biotechnology progress. 2011;27(3):830–7. doi: 10.1002/btpr.595. Epub 2011/05/04. [DOI] [PubMed] [Google Scholar]
- 10.Mascarell L, Bauche C, Fayolle C, Diop OM, Dupuy M, Nougarede N, et al. Delivery of the HIV-1 Tat protein to dendritic cells by the CyaA vector induces specific Th1 responses and high affinity neutralizing antibodies in non human primates. Vaccine. 2006;24(17):3490–9. doi: 10.1016/j.vaccine.2006.02.009. Epub 2006/03/10. [DOI] [PubMed] [Google Scholar]
- 11.Castro FV, Tutt AL, White AL, Teeling JL, James S, French RR, et al. CD11c provides an effective immunotarget for the generation of both CD4 and CD8 T cell responses. European journal of immunology. 2008;38(8):2263–73. doi: 10.1002/eji.200838302. Epub 2008/07/25. [DOI] [PubMed] [Google Scholar]
- 12.Bonifaz LC, Bonnyay DP, Charalambous A, Darguste DI, Fujii S, Soares H, et al. In vivo targeting of antigens to maturing dendritic cells via the DEC-205 receptor improves T cell vaccination. The Journal of experimental medicine. 2004;199(6):815–24. doi: 10.1084/jem.20032220. Epub 2004/03/17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Idoyaga J, Cheong C, Suda K, Suda N, Kim JY, Lee H, et al. Cutting edge: langerin/CD207 receptor on dendritic cells mediates efficient antigen presentation on MHC I and II products in vivo. J Immunol. 2008;180(6):3647–50. doi: 10.4049/jimmunol.180.6.3647. Epub 2008/03/07. [DOI] [PubMed] [Google Scholar]
- 14.Apostolopoulos V, Barnes N, Pietersz GA, McKenzie IF. Ex vivo targeting of the macrophage mannose receptor generates anti-tumor CTL responses. Vaccine. 2000;18(27):3174–84. doi: 10.1016/s0264-410x(00)00090-6. Epub 2000/06/17. [DOI] [PubMed] [Google Scholar]
- 15.Idoyaga J, Lubkin A, Fiorese C, Lahoud MH, Caminschi I, Huang Y, et al. Comparable T helper 1 (Th1) and CD8 T-cell immunity by targeting HIV gag p24 to CD8 dendritic cells within antibodies to Langerin, DEC205, and Clec9A. Proceedings of the National Academy of Sciences of the United States of America. 2011;108(6):2384–9. doi: 10.1073/pnas.1019547108. Epub 2011/01/26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Klechevsky E, Flamar AL, Cao Y, Blanck JP, Liu M, O'Bar A, et al. Cross-priming CD8+ T cells by targeting antigens to human dendritic cells through DCIR. Blood. 2010;116(10):1685–97. doi: 10.1182/blood-2010-01-264960. Epub 2010/06/10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tacken PJ, de Vries IJ, Gijzen K, Joosten B, Wu D, Rother RP, et al. Effective induction of naive and recall T-cell responses by targeting antigen to human dendritic cells via a humanized anti-DC-SIGN antibody. Blood. 2005;106(4):1278–85. doi: 10.1182/blood-2005-01-0318. Epub 2005/05/10. [DOI] [PubMed] [Google Scholar]
- 18.Carter RW, Thompson C, Reid DM, Wong SY, Tough DF. Preferential induction of CD4+ T cell responses through in vivo targeting of antigen to dendritic cell-associated C-type lectin-1. J Immunol. 2006;177(4):2276–84. doi: 10.4049/jimmunol.177.4.2276. Epub 2006/08/05. [DOI] [PubMed] [Google Scholar]
- 19.Trumpfheller C, Finke JS, Lopez CB, Moran TM, Moltedo B, Soares H, et al. Intensified and protective CD4+ T cell immunity in mice with anti-dendritic cell HIV gag fusion antibody vaccine. The Journal of experimental medicine. 2006;203(3):607–17. doi: 10.1084/jem.20052005. Epub 2006/03/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Flynn BJ, Kastenmuller K, Wille-Reece U, Tomaras GD, Alam M, Lindsay RW, et al. Immunization with HIV Gag targeted to dendritic cells followed by recombinant New York vaccinia virus induces robust T-cell immunity in nonhuman primates. Proceedings of the National Academy of Sciences of the United States of America. 2011;108(17):7131–6. doi: 10.1073/pnas.1103869108. Epub 2011/04/07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bozzacco L, Trumpfheller C, Siegal FP, Mehandru S, Markowitz M, Carrington M, et al. DEC-205 receptor on dendritic cells mediates presentation of HIV gag protein to CD8+ T cells in a spectrum of human MHC I haplotypes. Proceedings of the National Academy of Sciences of the United States of America. 2007;104(4):1289–94. doi: 10.1073/pnas.0610383104. Epub 2007/01/19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stahl-Hennig C, Eisenblatter M, Jasny E, Rzehak T, Tenner-Racz K, Trumpfheller C, et al. Synthetic double-stranded RNAs are adjuvants for the induction of T helper 1 and humoral immune responses to human papillomavirus in rhesus macaques. PLoS pathogens. 2009;5(4):e1000373. doi: 10.1371/journal.ppat.1000373. Epub 2009/04/11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yanagita M, Hiroi T, Kitagaki N, Hamada S, Ito HO, Shimauchi H, et al. Nasopharyngeal-associated lymphoreticular tissue (NALT) immunity: fimbriae-specific Th1 and Th2 cell-regulated IgA responses for the inhibition of bacterial attachment to epithelial cells and subsequent inflammatory cytokine production. J Immunol. 1999;162(6):3559–65. [PubMed] [Google Scholar]
- 24.Sandoval F, Terme M, Nizard M, Badoual C, Bureau MF, Freyburger L, et al. Mucosal imprinting of vaccine-induced CD8(+) T cells is crucial to inhibit the growth of mucosal tumors. Science translational medicine. 2013;5(172):172ra20. doi: 10.1126/scitranslmed.3004888. Epub 2013/02/15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Langermann S, Palaszynski S, Sadziene A, Stover CK, Koenig S. Systemic and mucosal immunity induced by BCG vector expressing outer-surface protein A of Borrelia burgdorferi. Nature. 1994;372(6506):552–5. doi: 10.1038/372552a0. [DOI] [PubMed] [Google Scholar]
- 26.Velge-Roussel F, Marcelo P, Lepage AC, Buzoni-Gatel D, Bout DT. Intranasal immunization with Toxoplasma gondii SAG1 induces protective cells into both NALT and GALT compartments. Infection and immunity. 2000;68(2):969–72. doi: 10.1128/iai.68.2.969-972.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hawiger D, Inaba K, Dorsett Y, Guo M, Mahnke K, Rivera M, et al. Dendritic cells induce peripheral T cell unresponsiveness under steady state conditions in vivo. The Journal of experimental medicine. 2001;194(6):769–79. doi: 10.1084/jem.194.6.769. Epub 2001/09/19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Belyakov IM, Isakov D, Zhu Q, Dzutsev A, Berzofsky JA. A novel functional CTL avidity/activity compartmentalization to the site of mucosal immunization contributes to protection of macaques against simian/human immunodeficiency viral depletion of mucosal CD4+ T cells. J Immunol. 2007;178(11):7211–21. doi: 10.4049/jimmunol.178.11.7211. Epub 2007/05/22. [DOI] [PubMed] [Google Scholar]
- 29.Ruane D, Brane L, Reis BS, Cheong C, Poles J, Do Y, et al. Lung dendritic cells induce migration of protective T cells to the gastrointestinal tract. The Journal of experimental medicine. 2013;210(9):1871–88. doi: 10.1084/jem.20122762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Do Y, Didierlaurent AM, Ryu S, Koh H, Park CG, Park S, et al. Induction of pulmonary mucosal immune responses with a protein vaccine targeted to the DEC-205/CD205 receptor. Vaccine. 2012;30(45):6359–67. doi: 10.1016/j.vaccine.2012.08.051. Epub 2012/09/06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Meredith MM, Liu K, Darrasse-Jeze G, Kamphorst AO, Schreiber HA, Guermonprez P, et al. Expression of the zinc finger transcription factor zDC (Zbtb46, Btbd4) defines the classical dendritic cell lineage. The Journal of experimental medicine. 2012;209(6):1153–65. doi: 10.1084/jem.20112675. Epub 2012/05/23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Douek DC, Brenchley JM, Betts MR, Ambrozak DR, Hill BJ, Okamoto Y, et al. HIV preferentially infects HIV-specific CD4+ T cells. Nature. 2002;417(6884):95–8. doi: 10.1038/417095a. Epub 2002/05/03. [DOI] [PubMed] [Google Scholar]
- 33.Harari A, Bart PA, Stohr W, Tapia G, Garcia M, Medjitna-Rais E, et al. An HIV-1 clade C DNA prime, NYVAC boost vaccine regimen induces reliable, polyfunctional, and long-lasting T cell responses. The Journal of experimental medicine. 2008;205(1):63–77. doi: 10.1084/jem.20071331. Epub 2008/01/16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mata M, Travers PJ, Liu Q, Frankel FR, Paterson Y. The MHC class I-restricted immune response to HIV-gag in BALB/c mice selects a single epitope that does not have a predictable MHC-binding motif and binds to Kd through interactions between a glutamine at P3 and pocket D. J Immunol. 1998;161(6):2985–93. Epub 1998/09/22. [PubMed] [Google Scholar]
- 35.Ahonen CL, Doxsee CL, McGurran SM, Riter TR, Wade WF, Barth RJ, et al. Combined TLR and CD40 triggering induces potent CD8+ T cell expansion with variable dependence on type I IFN. The Journal of experimental medicine. 2004;199(6):775–84. doi: 10.1084/jem.20031591. Epub 2004/03/10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pneumocystis pneumonia--Los Angeles. MMWR Morbidity and mortality weekly report. 1981;30(21):250–2. Epub 1981/06/05. [PubMed] [Google Scholar]
- 37.Crunkhorn S. Infectious disease: Towards an effective HIV vaccine. Nature reviews Drug discovery. 2015;14(4):238. doi: 10.1038/nrd4786. Epub 2015/04/02. [DOI] [PubMed] [Google Scholar]
- 38.Nchinda G, Amadu D, Trumpfheller C, Mizenina O, Uberla K, Steinman RM. Dendritic cell targeted HIV gag protein vaccine provides help to a DNA vaccine including mobilization of protective CD8+ T cells. Proceedings of the National Academy of Sciences of the United States of America. 2010;107(9):4281–6. doi: 10.1073/pnas.1000621107. Epub 2010/02/18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cheong C, Choi JH, Vitale L, He LZ, Trumpfheller C, Bozzacco L, et al. Improved cellular and humoral immune responses in vivo following targeting of HIV Gag to dendritic cells within human anti-human DEC205 monoclonal antibody. Blood. 2010;116(19):3828–38. doi: 10.1182/blood-2010-06-288068. Epub 2010/07/30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Belyakov IM, Ahlers JD. Functional CD8+ CTLs in mucosal sites and HIV infection: moving forward toward a mucosal AIDS vaccine. Trends in immunology. 2008;29(11):574–85. doi: 10.1016/j.it.2008.07.010. Epub 2008/10/08. [DOI] [PubMed] [Google Scholar]
- 41.Belyakov IM, Ahlers JD, Nabel GJ, Moss B, Berzofsky JA. Generation of functionally active HIV-1 specific CD8+ CTL in intestinal mucosa following mucosal, systemic or mixed prime-boost immunization. Virology. 2008;381(1):106–15. doi: 10.1016/j.virol.2008.08.019. Epub 2008/09/17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gallichan WS, Rosenthal KL. Long-lived cytotoxic T lymphocyte memory in mucosal tissues after mucosal but not systemic immunization. The Journal of experimental medicine. 1996;184(5):1879–90. doi: 10.1084/jem.184.5.1879. Epub 1996/11/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rerks-Ngarm S, Pitisuttithum P, Nitayaphan S, Kaewkungwal J, Chiu J, Paris R, et al. Vaccination with ALVAC and AIDSVAX to prevent HIV-1 infection in Thailand. The New England journal of medicine. 2009;361(23):2209–20. doi: 10.1056/NEJMoa0908492. Epub 2009/10/22. [DOI] [PubMed] [Google Scholar]
- 44.McElrath MJ, De Rosa SC, Moodie Z, Dubey S, Kierstead L, Janes H, et al. HIV-1 vaccine-induced immunity in the test-of-concept Step Study: a case-cohort analysis. Lancet. 2008;372(9653):1894–905. doi: 10.1016/S0140-6736(08)61592-5. Epub 2008/11/18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Buchbinder SP, Mehrotra DV, Duerr A, Fitzgerald DW, Mogg R, Li D, et al. Efficacy assessment of a cell-mediated immunity HIV-1 vaccine (the Step Study): a double-blind, randomised, placebo-controlled, test-of-concept trial. Lancet. 2008;372(9653):1881–93. doi: 10.1016/S0140-6736(08)61591-3. Epub 2008/11/18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gray G, Buchbinder S, Duerr A. Overview of STEP and Phambili trial results: two phase IIb test-of-concept studies investigating the efficacy of MRK adenovirus type 5 gag/pol/nef subtype B HIV vaccine. Current opinion in HIV and AIDS. 2010;5(5):357–61. doi: 10.1097/COH.0b013e32833d2d2b. Epub 2010/10/28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hutnick NA, Carnathan DG, Dubey SA, Makedonas G, Cox KS, Kierstead L, et al. Baseline Ad5 serostatus does not predict Ad5 HIV vaccine-induced expansion of adenovirus-specific CD4+ T cells. Nature medicine. 2009;15(8):876–8. doi: 10.1038/nm.1989. Epub 2009/07/22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.O'Brien KL, Liu J, King SL, Sun YH, Schmitz JE, Lifton MA, et al. Adenovirus-specific immunity after immunization with an Ad5 HIV-1 vaccine candidate in humans. Nature medicine. 2009;15(8):873–5. doi: 10.1038/nm.1991. Epub 2009/07/22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Masek-Hammerman K, Li H, Liu J, Abbink P, La Porte A, O'Brien KL, et al. Mucosal trafficking of vector-specific CD4+ T lymphocytes following vaccination of rhesus monkeys with adenovirus serotype 5. Journal of virology. 2010;84(19):9810–6. doi: 10.1128/JVI.01157-10. Epub 2010/08/06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Williams WB, Liao HX, Moody MA, Kepler TB, Alam SM, Gao F, et al. HIV-1 VACCINES. Diversion of HIV-1 vaccine-induced immunity by gp41-microbiota cross-reactive antibodies. Science. 2015;349(6249):aab1253. doi: 10.1126/science.aab1253. Epub 2015/08/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Haynes BF, Gilbert PB, McElrath MJ, Zolla-Pazner S, Tomaras GD, Alam SM, et al. Immune-correlates analysis of an HIV-1 vaccine efficacy trial. The New England journal of medicine. 2012;366(14):1275–86. doi: 10.1056/NEJMoa1113425. Epub 2012/04/06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.de Souza MS, Ratto-Kim S, Chuenarom W, Schuetz A, Chantakulkij S, Nuntapinit B, et al. The Thai phase III trial (RV144) vaccine regimen induces T cell responses that preferentially target epitopes within the V2 region of HIV-1 envelope. J Immunol. 2012;188(10):5166–76. doi: 10.4049/jimmunol.1102756. Epub 2012/04/25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kuebler PJ, Mehrotra ML, McConnell JJ, Holditch SJ, Shaw BI, Tarosso LF, et al. Cellular immune correlates analysis of an HIV-1 preexposure prophylaxis trial. Proceedings of the National Academy of Sciences of the United States of America. 2015;112(27):8379–84. doi: 10.1073/pnas.1501443112. Epub 2015/06/24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bart PA, Huang Y, Karuna ST, Chappuis S, Gaillard J, Kochar N, et al. HIV-specific humoral responses benefit from stronger prime in phase Ib clinical trial. The Journal of clinical investigation. 2014;124(11):4843–56. doi: 10.1172/JCI75894. Epub 2014/10/02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bienenstock J, McDermott M, Befus D, O'Neill M. A common mucosal immunologic system involving the bronchus, breast and bowel. Advances in experimental medicine and biology. 1978;107:53–9. doi: 10.1007/978-1-4684-3369-2_7. Epub 1978/01/01. [DOI] [PubMed] [Google Scholar]
- 56.Stary G, Olive A, Radovic-Moreno AF, Gondek D, Alvarez D, Basto PA, et al. VACCINES. A mucosal vaccine against Chlamydia trachomatis generates two waves of protective memory T cells. Science. 2015;348(6241):aaa8205. doi: 10.1126/science.aaa8205. Epub 2015/06/20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Harandi AM, Medaglini D. Mucosal adjuvants. Current HIV research. 2010;8(4):330–5. doi: 10.2174/157016210791208695. Epub 2010/04/01. [DOI] [PubMed] [Google Scholar]
- 58.Krown SE, Kerr D, Stewart WE, 2nd, Field AK, Oettgen HF. Phase I trials of poly(I,C) complexes in advanced cancer. Journal of biological response modifiers. 1985;4(6):640–9. Epub 1985/12/01. [PubMed] [Google Scholar]
- 59.Morse MA, Chapman R, Powderly J, Blackwell K, Keler T, Green J, et al. Phase I study utilizing a novel antigen-presenting cell-targeted vaccine with Toll-like receptor stimulation to induce immunity to self-antigens in cancer patients. Clinical cancer research : an official journal of the American Association for Cancer Research. 2011;17(14):4844–53. doi: 10.1158/1078-0432.CCR-11-0891. Epub 2011/06/03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Okada H, Kalinski P, Ueda R, Hoji A, Kohanbash G, Donegan TE, et al. Induction of CD8+ T-cell responses against novel glioma-associated antigen peptides and clinical activity by vaccinations with {alpha}-type 1 polarized dendritic cells and polyinosinic-polycytidylic acid stabilized by lysine and carboxymethylcellulose in patients with recurrent malignant glioma. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2011;29(3):330–6. doi: 10.1200/JCO.2010.30.7744. Epub 2010/12/15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Caskey M, Lefebvre F, Filali-Mouhim A, Cameron MJ, Goulet JP, Haddad EK, et al. Synthetic double-stranded RNA induces innate immune responses similar to a live viral vaccine in humans. The Journal of experimental medicine. 2011;208(12):2357–66. doi: 10.1084/jem.20111171. Epub 2011/11/09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Witmer-Pack MD, Swiggard WJ, Mirza A, Inaba K, Steinman RM. Tissue distribution of the DEC-205 protein that is detected by the monoclonal antibody NLDC-145. II. Expression in situ in lymphoid and nonlymphoid tissues. Cellular immunology. 1995;163(1):157–62. doi: 10.1006/cimm.1995.1110. Epub 1995/06/01. [DOI] [PubMed] [Google Scholar]
- 63.Graw F, Regoes RR. Predicting the impact of CD8+ T cell polyfunctionality on HIV disease progression. Journal of virology. 2014;88(17):10134–45. doi: 10.1128/JVI.00647-14. Epub 2014/06/27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Cocchi F, DeVico AL, Yarchoan R, Redfield R, Cleghorn F, Blattner WA, et al. Higher macrophage inflammatory protein (MIP)-1alpha and MIP-1beta levels from CD8+ T cells are associated with asymptomatic HIV-1 infection. Proceedings of the National Academy of Sciences of the United States of America. 2000;97(25):13812–7. doi: 10.1073/pnas.240469997. Epub 2000/11/30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Khader SA, Bell GK, Pearl JE, Fountain JJ, Rangel-Moreno J, Cilley GE, et al. IL-23 and IL-17 in the establishment of protective pulmonary CD4+ T cell responses after vaccination and during Mycobacterium tuberculosis challenge. Nature immunology. 2007;8(4):369–77. doi: 10.1038/ni1449. Epub 2007/03/14. [DOI] [PubMed] [Google Scholar]
- 66.Smiley KL, McNeal MM, Basu M, Choi AH, Clements JD, Ward RL. Association of gamma interferon and interleukin-17 production in intestinal CD4+ T cells with protection against rotavirus shedding in mice intranasally immunized with VP6 and the adjuvant LT(R192G) Journal of virology. 2007;81(8):3740–8. doi: 10.1128/JVI.01877-06. Epub 2007/01/26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Cecchinato V, Trindade CJ, Laurence A, Heraud JM, Brenchley JM, Ferrari MG, et al. Altered balance between Th17 and Th1 cells at mucosal sites predicts AIDS progression in simian immunodeficiency virus-infected macaques. Mucosal immunology. 2008;1(4):279–88. doi: 10.1038/mi.2008.14. Epub 2008/12/17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Xu H, Wang X, Liu DX, Moroney-Rasmussen T, Lackner AA, Veazey RS. IL-17-producing innate lymphoid cells are restricted to mucosal tissues and are depleted in SIV-infected macaques. Mucosal immunology. 2012;5(6):658–69. doi: 10.1038/mi.2012.39. Epub 2012/06/07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Horwitz JA, Halper-Stromberg A, Mouquet H, Gitlin AD, Tretiakova A, Eisenreich TR, et al. HIV-1 suppression and durable control by combining single broadly neutralizing antibodies and antiretroviral drugs in humanized mice. Proceedings of the National Academy of Sciences of the United States of America. 2013;110(41):16538–43. doi: 10.1073/pnas.1315295110. Epub 2013/09/18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Klein F, Halper-Stromberg A, Horwitz JA, Gruell H, Scheid JF, Bournazos S, et al. HIV therapy by a combination of broadly neutralizing antibodies in humanized mice. Nature. 2012;492(7427):118–22. doi: 10.1038/nature11604. Epub 2012/10/30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Barouch DH, Whitney JB, Moldt B, Klein F, Oliveira TY, Liu J, et al. Therapeutic efficacy of potent neutralizing HIV-1-specific monoclonal antibodies in SHIV-infected rhesus monkeys. Nature. 2013;503(7475):224–8. doi: 10.1038/nature12744. Epub 2013/11/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Halper-Stromberg A, Lu CL, Klein F, Horwitz JA, Bournazos S, Nogueira L, et al. Broadly neutralizing antibodies and viral inducers decrease rebound from HIV-1 latent reservoirs in humanized mice. Cell. 2014;158(5):989–99. doi: 10.1016/j.cell.2014.07.043. Epub 2014/08/19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Rolland M, Edlefsen PT, Larsen BB, Tovanabutra S, Sanders-Buell E, Hertz T, et al. Increased HIV-1 vaccine efficacy against viruses with genetic signatures in Env V2. Nature. 2012;490(7420):417–20. doi: 10.1038/nature11519. Epub 2012/09/11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Boscardin SB, Hafalla JC, Masilamani RF, Kamphorst AO, Zebroski HA, Rai U, et al. Antigen targeting to dendritic cells elicits long-lived T cell help for antibody responses. The Journal of experimental medicine. 2006;203(3):599–606. doi: 10.1084/jem.20051639. Epub 2006/03/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Gomez CE, Najera JL, Jimenez V, Bieler K, Wild J, Kostic L, et al. Generation and immunogenicity of novel HIV/AIDS vaccine candidates targeting HIV-1 Env/Gag-Pol-Nef antigens of clade C. Vaccine. 2007;25(11):1969–92. doi: 10.1016/j.vaccine.2006.11.051. Epub 2007/01/17. [DOI] [PubMed] [Google Scholar]
- 76.Bozzacco L, Trumpfheller C, Huang Y, Longhi MP, Shimeliovich I, Schauer JD, et al. HIV gag protein is efficiently cross-presented when targeted with an antibody towards the DEC-205 receptor in Flt3 ligand-mobilized murine DC. European journal of immunology. 2010;40(1):36–46. doi: 10.1002/eji.200939748. Epub 2009/10/16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Mucida D, Park Y, Kim G, Turovskaya O, Scott I, Kronenberg M, et al. Reciprocal TH17 and regulatory T cell differentiation mediated by retinoic acid. Science. 2007;317(5835):256–60. doi: 10.1126/science.1145697. Epub 2007/06/16. [DOI] [PubMed] [Google Scholar]
- 78.Lee H, Ruane D, Law K, Ho Y, Garg A, Rahman A, et al. Phenotype and function of nasal dendritic cells. Mucosal immunology. 2015;8(5):1083–98. doi: 10.1038/mi.2014.135. Epub 2015/02/12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Trumpfheller C, Caskey M, Nchinda G, Longhi MP, Mizenina O, Huang Y, et al. The microbial mimic poly IC induces durable and protective CD4+ T cell immunity together with a dendritic cell targeted vaccine. Proc Natl Acad Sci USA. 2008;105(7):2574–9. doi: 10.1073/pnas.0711976105. Epub 2008/02/08. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
F1 hybrid (BALB/c females X C57Bl/6 males) mice were immunized in a heterologous prime-boost regimen with α–CD205-p24 mAb (5µg), poly ICLC (50µg) and α-CD40 (25µg) and boosted with 107 PFU NYVAC gag/pol/nef delivered i.p. 2 weeks post boost, IFN-γ secretion was evaluated in CD8+ T cells.
(A) FACS plots from a representative experiment, illustrating the induction of IFN-γ+CD8+ cells in the SILP, vagina, blood and spleen.
(B) Mean data from three independent experiments is shown (5 mice per group).
Error bars show mean ± SD. **=p<0.005, ***=p<0.001