Abstract
Purpose
We sought to evaluate the extent to which childhood physical and/or sexual abuse history is associated with post-traumatic stress disorder (PTSD) during early pregnancy; and to explore the extent to which the childhood abuse-PTSD association is mediated through, or modified by, adult experiences of intimate partner violence (IPV).
Methods
In-person interviews collected information regarding history of childhood abuse and IPV from 2,928 women age 18–49 years old prior to 16 weeks of gestation. PTSD was assessed using the PTSD Checklist-Civilian Version (PCL-C). Multivariate logistic regressions were used to estimate odds ratios (OR) and 95% confidence intervals (CI).
Results
Compared to women with no childhood abuse, the odds of PTSD were increased 4.31-fold for those who reported physical abuse only (95%CI: 2.18–8.49), 5.33-fold for sexual abuse only (95%CI 2.38–11.98) and 8.03-fold for those who reported physical and sexual abuse (95%CI 4.10–15.74). Mediation analysis showed 13% of the childhood abuse-PTSD association was mediated by IPV. Further, high odds of PTSD were noted among women with histories of childhood abuse and IPV compared with women who were not exposed to either (aOR=20.20; 95%CI 8.18–49.85).
Conclusions
Childhood abuse is associated with increased odds of PTSD during early pregnancy. The odds of PTSD were particularly elevated among women with a history of childhood abuse and IPV. Efforts should be made to prevent childhood abuse and mitigate its effects on women’s mental health.
Keywords: Childhood abuse, PTSD, Early pregnancy, Peru
Introduction
Posttraumatic stress disorder (PTSD), a response that occurs following an exposure to extreme traumatic events, is characterized by symptoms of re-experiencing, avoidance, and increased arousal (1). While PTSD research has traditionally examined single index traumas, such as those influenced by a natural disaster, a serious accident, a terrorist act, or war/combat (2, 3) a growing body of research has focused on extended exposure to traumatic life events such as childhood abuse (4–9).
Researchers have demonstrated that childhood physical and/or sexual abuse increases vulnerability to PTSD in adulthood (10). Of note, women are at higher risk than men of becoming victims of childhood sexual abuse globally (20% vs. 8%) (11, 12) and hence at increased risk of PTSD (13). Intimate partner violence (IPV) has also been associated with subsequent risk PTSD (14). Prevalence estimates of PTSD among abused women have ranged from 16% to 85% (15, 16) compared with 5–10% observed among women in the general population (17). Women are at particularly elevated risk for PTSD during their reproductive years, specifically during pregnancy and postpartum periods, with PTSD symptoms likely to reach their peak closer to delivery (18). Although there is substantial evidence of childhood physical and sexual abuse as risk factors for PTSD among men and non-pregnant women (19–21), few have examined this relationship among pregnant women (22–25) and none of the studies included Latin American women. In studies that focused on the antepartum period, only two demonstrated statistically significant associations between childhood sexual abuse and antepartum PTSD; and inferences from these studies are hindered due to incomplete adjustments for potential confounders such as age, race/ethnicity, and comorbid psychiatric disorders including depression (24, 26). In other studies, this association was not significant possibly to lack of adjustment for multivariable confounders, small sample sizes, and variability in assessment of childhood trauma (27, 28). Moreover, prior studies failed to distinguish between types of childhood abuse; and these studies have primarily focused on women residing in high-income countries (29–31).
The burden of childhood trauma brought on by childhood physical and sexual abuse have been reported in Latin America where many children’s lives are characterized by poverty, forced labor, early marriage, neglect and abuse, domestic violence, and home accidents (32). Collectively, these traumatic experiences contribute to approximately 50% of deaths in children under the age of 5 years (32). Recent studies show the worldwide prevalence of childhood sexual abuse range from 2–68% with variations likely due to methodology, sample size, study population, and individual data collection efforts (11–13, 33). A recent study conducted among pregnant Peruvian women found the prevalence of childhood and adulthood abuse to be 69.4% and 39.1%, respectively (34).
Available evidence indicates that those who experienced childhood abuse are more likely to experience intimate partner violence (IPV) (34, 35). IPV, a common type of abuse experienced by women worldwide, is another significant global public health problem with estimated prevalence ranging from 15% to 71% (36–38). However, prior studies have not have explored the risk of PTSD among those who have experienced childhood abuse and IPV. Given (1) the enormous and enduring physical and mental health consequences of childhood abuse across the life course (39–41); and (2) that antenatal care represents the first and often only time many women in low and middle income countries engage with the health care system (42), we evaluated the extent to which history of childhood abuse is associated with PTSD symptoms during early pregnancy among Peruvian women. Further, we explored the extent to which an association of childhood abuse with PTSD is mediated through, or modified by, adult experiences of IPV.
Methods
The present study was drawn from the ongoing Pregnancy Outcomes, Maternal and Infant Study (PrOMIS) cohort. The PrOMIS cohort is designed to examine maternal social and behavioral risk factors of preterm birth, maternal mental health, and other adverse pregnancy outcomes. Participants were recruited during their first trimester between February 2012 and March 2014 at the Instituto Nacional Materno Perinatal (INMP) in Lima, Peru. The INMP is the primary reference establishment for maternal and perinatal care and is operated by the Peruvian Ministry of Health. Eligible women were those reproductive age group (18–49) who initiated prenatal care before 16 weeks of gestation. We excluded those who did not speak and read Spanish or were younger than 18 or older than 49 years of age. The eligibility criteria of initiating prenatal care prior to the completion of 16 weeks of gestation was to mitigate concerns about reverse causality and recall bias while enrolling a study population that is generalizable to the source population of women at INMP. Before setting this threshold, we determined that over 90% of women delivering at INMP initiate prenatal care prior to 16 weeks of gestation. In addition, the national literacy rate for women in Peru is estimated to be 91.4 (UNESCO, 2015). Enrolled participants were interviewed using a structured questionnaire to elicit information regarding sociodemographic, lifestyle characteristics, medical and reproductive histories, and early life experiences. All participants provided written informed consent. The institutional review boards of the INMP, Lima, Peru and the Harvard T.H. Chan School of Public Health Office of Human Research Administration, Boston, MA, approved all study procedures.
Analytical Population and Variable Specification
Details of the study procedures for the PrOMIS cohort study have been previously described (34, 43, 44). The analytical population for this study was derived from 3,045 participants enrolled in the PrOMIS cohort. For the present analysis, we excluded participants with missing childhood abuse history (N=69) and those with missing PTSD scores (N=76). Hence a total of 2,928 participants remained for analysis. The excluded participants did not differ with regards to sociodemographic or lifestyle characteristics from those included in the present analysis.
Childhood Abuse Assessment
In order to elicit information regarding participants’ childhood physical or sexual abuse experiences, we used the Childhood Physical and Sexual Abuse Questionnaire (45) which has been previously used in the Peruvian population (34, 46). The questionnaire consists of eight questions taken from the Center for Disease Control and Prevention Adverse Childhood Experiences Study concerning abuse. Criteria for rating an experience of childhood sexual abuse included reporting that an older person touched them, they were made to touch someone else in a sexual way, or intercourse was attempted or completed, before the age of 18 years. Criterial for childhood physical abuse included reporting that they were hit, kicked, or beaten often and/or their life was seriously threatened, before the age of 18 years. The questions were asked as follows “sometimes parents or other adults hurt children. While you were growing up, that is, during your first 18 years of life, how often did a parent, step-parent, or adult living in your home: (1) Actually push, grab, shove, slap you, or throw something at you? (2) Hit you so hard that you had marks or were injured? and (3) Act in a way that made you afraid that you might be physically hurt? Some people, while growing up in their first 18 years of life, had a sexual experience with an adult or someone at least five years older than themselves. These experiences may have involved a relative family friend or stranger. During the first 18 years of life, did an adult or older relative, family friend or stranger ever: (1) Touch or fondle your body in a sexual way? (2) Have you touch their body in a sexual way? (3) Attempt to have any type of sexual intercourse (oral, anal, or vaginal) with you? (4) Actually have any type of sexual intercourse with you (oral, anal, or vaginal) with you?”
The responses for both sexual and physical abuse were used to create two outcome groups. The first was a mutually exclusive group where individuals were categorized as “no abuse” if they responded “no” to all questions regarding sexual and physical abuse. Those who responded “yes” to only physical abuse questions were categorized as “physical abuse only.” Those who responded “yes” to only sexual abuse questions were categorized as “sexual abuse only.” Participants who responded “yes” to both any physical abuse questions and any sexual abuse questions were categorized under “both physical and sexual abuse.” In addition to the four mutually exclusive groups, a binary outcome variable was created where participants who responded “yes” to any questions of either physical or sexual abuse were classified as having experienced “any abuse.”
Intimate Partner Violence (IPV) Assessment
IPV was assessed using questions adapted from the protocol of Demographic Health Survey Questionnaires and Modules: Domestic Violence Module (47) and the World Health Organization Multi-Country Study on Violence Against Women (37). Women were asked for a range of physical and/or sexual coercive acts used against them by a current or former spouse or intimate partner without their consent during their life. Participants were classified as having experienced physical violence if they endorsed any of the following: being slapped, having her arms twisted or something thrown at her, being pushed or shoved, being hit, kicked, dragged or beaten up, being choked or burnt on purpose, or being threatened or hurt with a weapon (such as, gun, knife, or other object). Sexual violence was defined if participants endorsed any of the following: being physically forced to have sexual intercourse, having had unwanted sexual intercourse because of fear of what the partner might do, and being forced to perform other sexual acts that the respondent found degrading or humiliating. In this study, participants were categorized as having experienced any IPV if they experienced one or more acts of physical or sexual violence at any time from a current or former male partner.
PTSD Assessment
We used the Posttraumatic Stress Disorder Checklist – Civilian Version (PCL-C) to assess the symptomatology and severity of PTSD during the past month. The PCL is a 17-item self-reported questionnaire that is derived from the criteria of the Diagnostic and Statistical Manual of Mental (DSM-IV) and assesses three symptom clusters: re-experiencing the trauma, avoidance and numbing, and hyperarousal (48). For each item, a score of 1 – 5 was assigning to the response categories of “not at all bothersome”, “a little bit bothersome”, “moderately bothersome”, “quite a bit bothersome” and “extremely bothersome”. The total PCL score ranges from 17 to 85 and is used as a severity measure of PTSD. Higher scores indicate more severe PTSD. The PCL-C has shown adequate levels of reliability and diagnostic accuracy when applied to different populations including pregnant women, primary care, and gynecology patients (48–51). A score of 44 was found to yield good diagnostic efficiency with a sensitivity of 94% and a specificity of 86% among a predominantly female trauma sample when compared against a diagnostic gold standard of clinical diagnostic interview (52). Hence, we used a total score of 44 and above to classified participants as having PTSD (53, 54).
Other Covariates
Participants’ age was categorized as follows: 18–20, 21–29, 30–34, and ≥ 35 years. Other sociodemographic variables were categorized as follows: maternal ethnicity (Mestizos of mixed Amerindian and European descent vs. others); educational attainment (≤6, 7–12, and >12 completed years of schooling); marital status (married and living with partner vs. others); employment status (employed vs. not employed); access to basic foods (very hard/hard, somewhat hard, and not very hard); parity (nulliparous vs. multiparous); planned pregnancy (yes vs. no); self-reported health in the past year (good vs. poor); and gestational age at interview (weeks).
Statistical Analyses
Frequency distributions of sociodemographic and reproductive characteristics were examined according to types of childhood abuse. One-way analysis of variance (ANOVA) for continuous variables and Chi-square tests for categorical variables were used to assess statistically significant differences in these characteristics between categories of childhood abuse. Logistic regressions were used to calculate maximum likelihood estimates of odd ratios (OR) and 95% confidence intervals (CIs) of PTSD in relation to history of childhood abuse. The odds of PTSD according to types of childhood abuse (physical abuse only, sexual abuse only, and both physical and sexual abuse) were estimated with women who had no history of childhood abuse (either physical or sexual) serving as the reference group. We included potential confounders of a priori interest (i.e., age at the time of the interview and ethnicity) in multivariable-adjusted logistic regression models on the bases of their hypothesized relationship between exposure (history of childhood abuse) and outcome (PTSD). Final logistic regression models included covariates that altered unadjusted ORs by at least 10%. Prior studies have shown associations of socioeconomic status and depression with childhood abuse (34, 55) and PTSD (56, 57). Given this, we performed a sensitivity analysis on the association between childhood abuse and PTSD after adjusting for these potential confounders. In addition, exploratory mediation analysis was conducted to assess whether the relation between childhood abuse and PTSD could be partially explained through the indirect effects of maternal exposure to intimate partner violence (IPV) (i.e., a hypothesized mediator of early life adversity and mental disorder in adulthood). We considered IPV as potential mediator as IPV may be on the causal pathway between childhood abuse and adulthood PTSD. We followed the four steps in establishing mediation recommended by Baron and Kenny (58). We considered lifetime experiences of IPV as potential mediator. First, we assessed the relation between childhood abuse and PTSD (the direct effect). Second, we evaluated the relation between childhood abuse and IPV (the mediator). Third, we examined the relation between the IPV and PTSD. Finally, we investigated the extent to which experiences of IPV mediated the relation between childhood abuse and PTSD, adjusting for maternal age at interview and maternal ethnicity. Further, given that childhood abuse is associated with increased odds of IPV (34), we examined the joint and independent effect of childhood abuse and experiences of IPV on risk of PTSD. For this analysis, we categorized participants into four groups based on combinations of childhood abuse and IPV. The four resulting categories were as follows: (1) no childhood abuse and no IPV, (2) childhood abuse only, (3) IPV only, and (4) childhood abuse and IPV. Participants with no childhood abuse and no IPV comprised the reference group, against which participants in the other three categories were compared. We explored the presence of effect modification by stratified analyses and by introducing interaction in logistic regression models. Interactions on the additive scale between history of childhood abuse and IPV on the odds of PTSD were formally assessed using the relative excess risk due to interaction (59, 60). All statistical analyses were performed using SAS 9.4 (SAS Institute, Cary, NC, USA) and Stata version 12.0 software (Statacorp, College Station, TX). All reported p values are two tailed with statistical significance set at 0.05.
Results
Of the sample of 2,928 participants, 2,100 (71.7%) reported having experienced any physical or sexual abuse during childhood. The prevalence of physical abuse only, sexual abuse only, and both physical and sexual abuse were 38.8%, 7.9%, 24.5%, respectively. Participants’ sociodemographic and lifestyle characteristics reported according to type of childhood abuse are shown in Table 1. The majority of the participants (80.8%) were married or living with their partner. Approximately 53.7% reported being unemployed while 54.6% reported completing 7–12 years of education. Advanced maternal age (≥ 35 years old), nulliparity, and difficulty in accessing basic needs were statistically significantly associated with a history of childhood abuse.
Table 1.
Characteristics of the study population according to types of childhood abuse in Lima, Peru (N = 2,928)
| All participants (N = 2,928) |
No abuse (N = 828) |
Physical abuse only (N = 1,137) |
Sexual abuse only (N = 230) |
Physical and sexual abuse (N = 733) |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|
|||||||
| Characteristics | n | % | n | % | n | % | n | % | n | % | P-value |
| Age (years)a | 28.1 ± 6.3 | 27.7 ± 6.1 | 28.1 ± 6.4 | 28.2 ± 6.5 | 28.7 ± 6.3 | 0.02 | |||||
| Age (years) | |||||||||||
| 18–20 | 160 | 5.5 | 39 | 4.7 | 67 | 5.9 | 15 | 6.3 | 39 | 5.3 | 0.01 |
| 20–29 | 1642 | 56.1 | 508 | 61.4 | 628 | 55.2 | 127 | 53.1 | 379 | 51.7 | |
| 30–34 | 601 | 20.5 | 154 | 18.6 | 233 | 20.5 | 39 | 16.3 | 175 | 23.9 | |
| ≥35 | 525 | 17.9 | 127 | 15.3 | 209 | 18.4 | 49 | 20.5 | 140 | 19.1 | |
| Education (years) | |||||||||||
| ≤6 | 123 | 4.2 | 36 | 4.3 | 48 | 4.2 | 5 | 2.1 | 34 | 4.6 | 0.73 |
| 7–12 | 1600 | 54.6 | 462 | 55.8 | 617 | 54.3 | 124 | 51.9 | 397 | 54.2 | |
| >12 | 1199 | 40.9 | 328 | 39.6 | 470 | 41.3 | 99 | 41.4 | 302 | 41.2 | |
| Mestizo ethnicity | 2199 | 75.1 | 633 | 76.4 | 846 | 74.4 | 179 | 74.9 | 541 | 73.8 | 0.40 |
| Married/living with a partner | 2365 | 80.8 | 685 | 82.7 | 921 | 81.0 | 177 | 74.1 | 582 | 79.4 | 0.17 |
| Employed | 1355 | 46.3 | 379 | 45.8 | 511 | 44.9 | 113 | 47.3 | 352 | 48.0 | 0.48 |
| Access to basic foods | |||||||||||
| Hard | 1453 | 49.6 | 345 | 41.7 | 556 | 48.9 | 124 | 51.9 | 428 | 58.4 | <0.0001 |
| Not very hard | 1473 | 50.3 | 483 | 58.3 | 579 | 50.9 | 106 | 44.4 | 305 | 41.6 | |
| Nulliparous | 1431 | 48.9 | 448 | 54.1 | 542 | 47.7 | 116 | 48.5 | 325 | 44.3 | 0.001 |
| Planned pregnancy | 1209 | 41.3 | 364 | 44.0 | 477 | 42.0 | 91 | 38.1 | 277 | 37.8 | 0.10 |
| Gestational age at interviewa | 9.2 ± 3.5 | 9.3 ± 3.4 | 9.2 ± 3.5 | 9.3 ± 3.3 | 9.2 ± 3.5 | 0.92 | |||||
| Early pregnancy BMI (kg/m2) | |||||||||||
| <18.5 | 57 | 1.9 | 19 | 2.3 | 23 | 2.0 | 4 | 1.7 | 11 | 1.5 | 0.65 |
| 18.5–24.9 | 1403 | 47.9 | 380 | 45.9 | 558 | 49.1 | 119 | 49.8 | 346 | 47.2 | |
| 25–29.9 | 1079 | 36.9 | 321 | 38.8 | 410 | 36.1 | 77 | 32.2 | 271 | 37.0 | |
| ≥30 | 359 | 12.3 | 93 | 11.2 | 142 | 12.5 | 25 | 10.5 | 99 | 13.5 | |
| Intimate partner violenceb | 1066 | 36.4 | 199 | 24.0 | 377 | 33.2 | 98 | 41.0 | 392 | 53.5 | <0.0001 |
| Depression (PHQ-9 ≥10) | 801 | 27.4 | 128 | 15.6 | 349 | 31.0 | 49 | 21.7 | 275 | 37.9 | <0.0001 |
Abbreviations: PHQ-9-Patient Health Questionnaire-9; BMI-body mass index; Due to missing data, percentages may not add up to 100%.;
mean ± SD (standard deviation):
Lifetime intimate partner violence: For continuous variables, P-value was calculated using the ANOVA; for categorical variables, P-value was calculated using the Chi-square test.
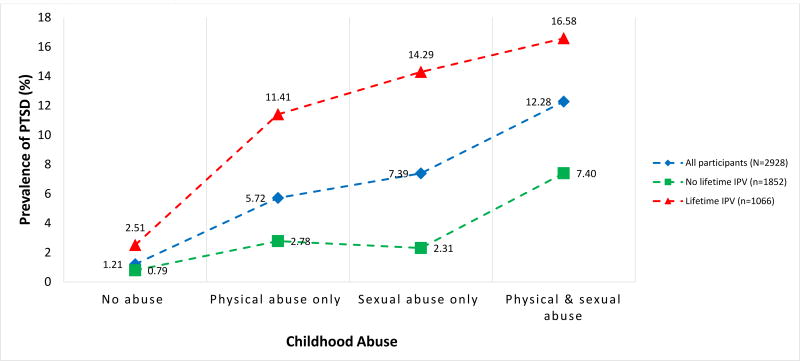
The overall prevalence of PTSD was 6.2%. The prevalence of PTSD was the highest among participants who reported childhood physical and sexual abuse (12.3%), followed by childhood sexual abuse only (7.4%) and childhood physical abuse only (5.7%) (Figure 1). Figure 1 also presents the prevalence of PTSD stratified according to lifetime experiences of IPV. Among women with lifetime IPV, the highest prevalence of PTSD was found among those who reported both childhood physical and sexual abuse (16.6%), followed by childhood sexual abuse only (14.3%) and childhood physical abuse only (11.4%). In contrast, among women who reported no lifetime IPV experiences, the prevalence of PTSD was 7.4% among those who reported childhood physical and sexual abuse, followed by childhood physical abuse only (2.8%) and childhood sexual abuse only (2.3%).
Figure 1.
Prevalence of Posttraumatic Stress Disorder (PTSD) assessed by the PTSD Check List - Civilian Version (PCL-C) among pregnant women (N=2,928)
Abbreviations: IPV, intimate partner violence
As shown in Table 2, a history of childhood physical or sexual abuse was associated with a 7.29-fold increased odds of PTSD (95% CI 3.84–13.87). This association was attenuated but remained strong after adjusting for age, ethnicity and lifetime experiences with IPV (aOR= 5.73; 95% CI 2.99–10.98). As shown in the bottom panel of Table 2, compared with women who experienced no abuse during childhood, the odds of PTSD were increased 4.31-fold for those who reported experiencing physical abuse only (95% CI 2.18–8.49), 5.33-fold for those who reported sexual abuse only (95% CI 2.38–11.98) and 8.03-fold for those who reported experiencing both physical and sexual abuse (95% CI 4.10–15.74) during childhood (Table 2). Further adjustments for difficulty paying for the basics and depression did not materially change the findings (Supplement Table 1).
Table 2.
Association between childhood abuse and posttraumatic stress disorder (PTSD)a assessed by the PTSD Check List - Civilian Version (PCL-C) during pregnancy (N = 2,928)
| No PTSD (N = 2746) |
PTSD (N = 182) |
||||||
|---|---|---|---|---|---|---|---|
|
|
|
||||||
| Childhood abuse | n | % | n | % | Unadjusted OR (95% CI) |
Adjusted OR (95% CI)b |
Adjusted OR (95% CI)c |
| No abuse | 818 | 29.8 | 10 | 5.5 | Reference | Reference | Reference |
| Any abuse | 1928 | 70.2 | 172 | 94.5 | 7.29 (3.84, 13.87) | 7.21 (3.78, 13.74) | 5.73 (2.99, 10.98) |
| Types of abuse | |||||||
| No abuse | 818 | 29.8 | 10 | 5.5 | Reference | Reference | Reference |
| Physical abuse only | 1072 | 39.0 | 65 | 35.7 | 4.96 (2.53, 9.71) | 4.88 (2.49, 9.57) | 4.31 (2.18, 8.49) |
| Sexual abuse only | 213 | 7.8 | 17 | 9.3 | 6.53 (2.95, 14.46) | 6.77 (3.04, 15.06) | 5.33 (2.38, 11.98) |
| Physical & sexual abuse | 643 | 23.4 | 90 | 49.5 | 11.45 (5.91, 22.17) | 11.32 (5.82, 22.00) | 8.03 (4.10, 15.74) |
Abbreviations: OR, odds ratio; CI, confidence interval
PTSD is defined as PCL-C score ≥ 44.
Adjusted for age (years) at interview and maternal ethnicity
Further adjusted for lifetime intimate partner violence
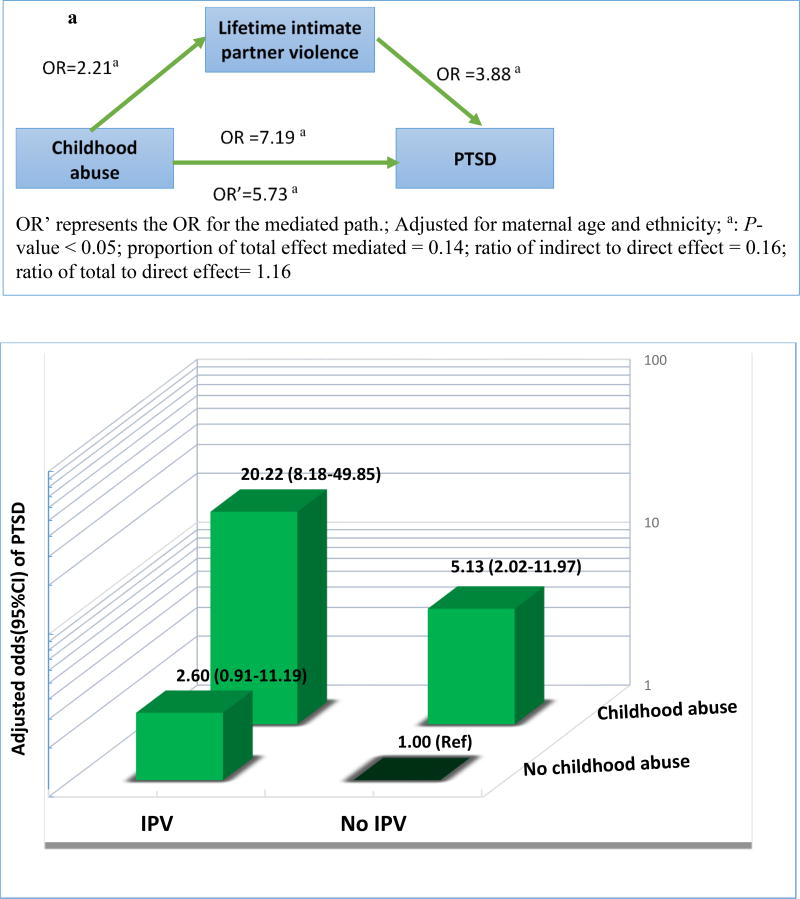
Given that experience of intimate partner violence may be on the causal pathway between childhood abuse and PTSD, we explored the extent to which abuse by an intimate partner is a mediator of the association of childhood abuse with PTSD (Figure 2a); and, if so, to quantify the magnitude of the mediated effect. From these analyses, we found that IPV accounted for only 13% of the indirect effect of the relation between childhood abuse and PTSD. Hence, IPV is not an important mediator of the hypothesized association (61).
Figure 2.
a) Assessing the mediating role of intimate partner violence (IPVA) on the association between childhood abuse and post-traumatic stress disorder (PTSD); Figure 2b) Independent and joint effect of childhood abuse and IPV on the odds of PTSD
History of childhood abuse was more strongly related PTSD risk than abuse by an intimate partner. As shown in Figure 2b, using multivariate adjusted models compared to women with no history of childhood abuse and no history of lifetime IPV (i.e., the reference group), women who experienced childhood abuse only had 5.13-fold elevated odds of PTSD (95% CI 2.02–12.97). The corresponding odds of PTSD for women who experienced IPV only was 2.60 (95%CI 0.91–11.19). Women with a joint positive history of both childhood abuse and IPV had 20.20 increased odds of PTSD (95%CI 8.18–49.85). Although these analyses suggest greater-than-additive effect of history of childhood abuse and IPV on the odds of PTSD (i.e., synergy index=3.03 (95%CI 1.67–5.51), the statistical test for significance of the multiplicative interaction term did not reach statistical significance (P=0.753).
Discussion
The present study extends the literature by documenting substantially increased odds of PTSD among pregnant women with a history of childhood abuse. A history of any childhood physical or sexual abuse was associated with 5.73-fold increased odds of PTSD after adjusting for confounders including lifetime experiences of IPV. Compared with women who experienced no abuse during childhood, the odds of PTSD were 8.03-fold higher among those who reported experiencing both physical and sexual abuse during childhood. Lifetime abuse by an intimate partner was not found to be an important mediator of the child abuse and PTSD association. However, we observed evidence suggestive of a greater than additive effect of a combined history of child abuse and IPV on the odds of PTSD. This finding indicates that women with a joint positive history of child abuse and IPV had particularly high odds (aOR 20.20; 95%CI 8.18–49.85) of IPV as compared with women who had no history of child abuse and IPV.
Our findings are consistent with previous studies that identified childhood physical and sexual abuse as specific risk factors for PTSD among non-pregnant women and men (19–21). In a prospective study of children followed into young adulthood, a history of physical abuse (OR=1.75; 95%CI 1.20–3.00) and sexual abuse (OR=2.34; 95%CI 1.50–3.70) were associated with increased odds of lifetime PTSD (22). Similarly, in their analysis of data from the Detroit Area Survey of Trauma, Breslau and colleagues found that a history of childhood trauma was associated with increased odds of PTSD (OR=2.06; 95%CI1.18–3.60) (23). In addition, our findings showed IPV is not an important mediator of the association between childhood abuse and PTSD. As such, IPV did not explain the association between childhood abuse and PTSD. Childhood abuse is thought to disrupt neurodevelopmental processes that respond to stress including the serotonin system, the hypothalamic-pituitary-adrenal axis, and childhood brain development (62). These neurobiological effects may influence the subsequent development of psychiatric disorders, including PTSD (63).
As noted earlier, only a few researchers have examined the association between a history of childhood abuse and PTSD among pregnant women. Seng et al, in their study of 1,259 pregnant women, found the prevalence of PTSD to be 11.4% in women physically or sexually abused as adults, 16.0% in women exposed to childhood physical or sexual abuse and 39.0% in those exposed to both childhood and adult physical and sexual abuse (P<0.001) (24). Similarly, Lev-Wiesel et al, in their study of Israeli pregnant women, found that those with a history of childhood abuse had higher mean PTSD scores (assessed using PTSD Symptoms Scale) as compared with women who had no history abuse (mean (standard deviation): 1.47 (0.51) vs. 1.22 (0.29), P<0.001) (25). Our findings and those of some researchers (25, 64), however, are dissimilar to findings reported by Morland et al (28). In their study of 101 pregnant women seeking prenatal care in Hawaii, USA, the authors observed no evidence of a statistical significant association of childhood abuse with prevalent PTSD (28). Inferences from this study, however, are limited in part, by the very small sample size; and by possibly uncontrolled confounding including from unmeasured indicators of socioeconomic status. In a recent meta-analysis of 5 previous studies, recent evidence suggests an association between childhood sexual abuse and PTSD among pregnant or postpartum women (41). On balance, available evidence, although sparse, underscores the enduring effects of childhood abuse on PTSD among pregnant women, a population known to be particularly vulnerable to experiencing psychiatric disorders (24, 25, 64).
Some limitations should be considered when interpreting our findings. First, childhood abuse and IPV histories were assessed by self-report. Consequently, these measures may be subjected to non-systematic errors in recall, as well as systematic non-disclosure leading to misclassification. It has been noted that individuals are likely to minimize experiences of past violence rather than suggest that they had experienced violence in their lifetime (65). Hence, it is likely that errors in recall of violence exposures may have led to underestimation of reported associations. Additionally, our questionnaires have not been previously validated in our study population. To help mitigate these limitations, well-trained interviewers used standard questionnaires to collect information from all study participants. Additionally, we worked to assure that interviewers and study participants were blinded as to specific study hypotheses. Third, despite controlling for confounders, we cannot rule out the possibility of residual confounding by unmeasured covariates. Fourth, by including only reproductive age group (18–49), it is possible that our estimates of child abuse might be underestimated. There is some evidence to indicate that childhood abuse can be particularly higher in pregnant teens. Future studies need to include teenage mothers who might be at an increased risk of childhood abuse. Fifth, our study did not include other aspects of child abuse such as emotional abuse, and this may have attenuated the association. Lastly, sampling bias may be present in our hospital-based study may not be generalizable to all women.
We found that childhood abuse is highly prevalent and is associated with increased odds of PTSD during early pregnancy independent of lifetime IPV experiences. Further we found that women with a history of child abuse and abuse by an intimate partner had particularly high odds of PTSD. These findings have important clinical and public health implications. For many women in low and middle-income countries, antenatal care is typically the first and only interaction with the health care system. As such, antenatal care represents critically important opportunities for health care providers to identify women exposed and burdened with the myriad of adverse physical and mental health consequences of interpersonal violence. Better understanding of how early life adversity (including childhood abuse) may increase risk of PTSD, other psychopathologies, and adverse reproductive outcomes may yield new insights and provide the impetus for developing and delivering more comprehensive and effective obstetric care. On the basis of our findings and available literature, we argue that there is a need to integrate screening for history of abuse in antenatal care. There is also a need to develop trauma-informed care for survivors of abuse who are suffering from psychiatric disorders through integrated antenatal care programs. Screening for psychiatric disorders among pregnant women who have experienced abuse will promote greater awareness and identify those individuals who would benefit from further mental health evaluation and treatment. Efforts should be made to prevent childhood abuse, identify those who have been victims, and connect those experiencing adverse outcomes with specific care designed to mitigate adverse health effects.
Supplementary Material
Acknowledgments
This research was supported by awards from the National Institutes of Health (NIH) (R01-HD-059835 and T37-MD0001449). The authors wish to thank the dedicated staff of Asociacion Civil Proyectos en Salud (PROESA), Peru and Instituto Nacional Materno Perinatal (INMP), Peru for their expert technical assistance with this research. Sincere gratitude is extended to all women who participated in the PrOMIS cohort study as they have made invaluable personal contributions to shaping future developments in public health and global health policy.
Abbreviations and acronyms
- PTSD
post-traumatic stress disorder
- IPV
intimate partner violence
- PCL-C
PTSD Checklist-Civilian Version
- OR
odds ratios
- CI
confidence intervals
- PrOMIS
Pregnancy Outcomes, Maternal and Infant Study
- INMP
Instituto Nacional Materno Perinatal
- ANOVA
analysis of variance
- PHQ-9
Patient Health Questionnaire-9
- BMI
body mass index
References
- 1.APA. American Psychiatric Association. Diagnostic and statistical manual of mental disorders DSM-V. Washington, DC: American Psychiatric Association; 2013. Available from: http://www.psychiatryonline.com/DSMPDF/dsm-iv.pdf. [Google Scholar]
- 2.Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):617–27. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kessler RC, Ustun TB, editors. WHO. The WHO World Mental Health Surveys: Global Perspectives on the Epidemiology of Mental Disorders. New York: Cambridge University Press; 2008. p. 580. [Google Scholar]
- 4.Breslau N, Kessler R, Chilcoat H, Schultz L, Davis G, Andreski P. Trauma and posttraumatic stress disorder in the community: the 1996 Detroit Area Survey of Trauma. Archives of General Psychiatry. 1998;55(7):626–32. doi: 10.1001/archpsyc.55.7.626. [DOI] [PubMed] [Google Scholar]
- 5.Baker CK, Norris FH, Diaz DM, Perilla JL, Murphy AD, Hill EG. Violence and PTSD in Mexico: gender and regional differences. Soc Psychiatry Psychiatr Epidemiol. 2005;40(7):519–28. doi: 10.1007/s00127-005-0921-2. [DOI] [PubMed] [Google Scholar]
- 6.Benítez CIP, Vicente B, Zlotnick C, Kohn R, Johnson J, Valdivia S, et al. Estudio epidemiológico de sucesos traumáticos, trastorno de estrés post-traumático y otros trastornos psiquiátricos en una muestra representativa de Chile. Salud Mental. 2009;32(2):145–53. [PMC free article] [PubMed] [Google Scholar]
- 7.Lowe SR, Galea S, Uddin M, Koenen KC. Trajectories of posttraumatic stress among urban residents. Am J Community Psychol. 2014;53(1–2):159–72. doi: 10.1007/s10464-014-9634-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rivera-Vélez G, González-Viruet M, Martínez-Taboas A, Pérez-Mojica D. Post-traumatic stress disorder, dissociation, and neuropsychological performance in Latina victims of childhood sexual abuse. Journal of Child Sexual Abuse. 2014;23(1):55–73. doi: 10.1080/10538712.2014.864746. [DOI] [PubMed] [Google Scholar]
- 9.Seiler A, Kohler S, Ruf-Leuschner M, Landolt M. Adverse Childhood Experiences, Mental Health, and Quality of Life of Chilean Girls Placed in Foster Care: An Exploratory Study. Psychological Trauma: Theory, Research, Practice, and Policy. 2015 doi: 10.1037/tra0000037. [DOI] [PubMed] [Google Scholar]
- 10.McLaughlin KA, Conron KJ, Koenen KC, Gilman SE. Childhood adversity, adult stressful life events, and risk of past-year psychiatric disorder: a test of the stress sensitization hypothesis in a population-based sample of adults. Psychol Med. 2010;40(10):1647–58. doi: 10.1017/S0033291709992121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pereda N, Guilera G, Forns M, Gomez-Benito J. The prevalence of child sexual abuse in community and student samples: a meta-analysis. Clin Psychol Rev. 2009;29(4):328–38. doi: 10.1016/j.cpr.2009.02.007. [DOI] [PubMed] [Google Scholar]
- 12.Stoltenborgh M, van Ijzendoorn MH, Euser EM, Bakermans-Kranenburg MJ. A global perspective on child sexual abuse: meta-analysis of prevalence around the world. Child Maltreat. 2011;16(2):79–101. doi: 10.1177/1077559511403920. [DOI] [PubMed] [Google Scholar]
- 13.Andrews G, Corry J, Slade T, Issakidis C, Swanston H. Child sexual abuse. In: Ezzati M, Lopez A, Rodgers A, Murray C, editors. Comparative quantification of health risks : global and regional burden of disease atrributable to selected major risk factors. Vol. 2. Geneva: World Health Organization; 2004. pp. 1851–940. [Google Scholar]
- 14.Lagdon S, Armour C, Stringer M. Adult experience of mental health outcomes as a result of intimate partner violence victimisation: a systematic review. European journal of psychotraumatology. 2014;5 doi: 10.3402/ejpt.v5.24794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Coker AL, Smith PH, McKeown RE, King MJ. Frequency and correlates of intimate partner violence by type: physical, sexual, and psychological battering. Am J Public Health. 2000;90(4):553–9. doi: 10.2105/ajph.90.4.553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Golding J. Intimate partner violence as a risk factor for mental disorders: A meta-analysis. Journal of Family Violence. 1999;14:99–132. [Google Scholar]
- 17.Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52(12):1048–60. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- 18.Onoye JM, Shafer LA, Goebert DA, Morland LA, Matsu CR, Hamagami F. Changes in PTSD symptomatology and mental health during pregnancy and postpartum. Arch Womens Ment Health. 2013;16(6):453–63. doi: 10.1007/s00737-013-0365-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McLeer S, Dixon J, Henry D, Ruggiero K, Escovitz K, Niedda T, et al. Psychopathology in non-clinically referred sexually abused children. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37(12):1326–33. doi: 10.1097/00004583-199812000-00017. [DOI] [PubMed] [Google Scholar]
- 20.Schumm JA, Briggs-Phillips M, Hobfoll SE. Cumulative interpersonal traumas and social support as risk and resiliency factors in predicting PTSD and depression among inner-city women. J Trauma Stress. 2006;19(6):825–36. doi: 10.1002/jts.20159. [DOI] [PubMed] [Google Scholar]
- 21.Huth-Bocks AC, Krause K, Ahlfs-Dunn S, Gallagher E, Scott S. Relational trauma and posttraumatic stress symptoms among pregnant women. Psychodyn Psychiatry. 2013;41(2):277–301. doi: 10.1521/pdps.2013.41.2.277. [DOI] [PubMed] [Google Scholar]
- 22.Widom CS. Posttraumatic Stress Disorder in Abused and Neglected Children Grown Up. American Journal of Psychiatry. 1999;156:1223–9. doi: 10.1176/ajp.156.8.1223. [DOI] [PubMed] [Google Scholar]
- 23.Breslau N, Chilcoat HD, Kessler RC, Davis GC. Previous exposure to trauma and PTSD effects of subsequent trauma: results from the Detroit Area Survey of Trauma. The American journal of psychiatry. 1999;156(6):902–7. doi: 10.1176/ajp.156.6.902. [DOI] [PubMed] [Google Scholar]
- 24.Seng JS, Sperlich M, Low LK. Mental health, demographic, and risk behavior profiles of pregnant survivors of childhood and adult abuse. J Midwifery Womens Health. 2008;53(6):511–21. doi: 10.1016/j.jmwh.2008.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lev-Wiesel R, Daphna-Tekoah S, Hallak M. Childhood sexual abuse as a predictor of birth-related posttraumatic stress and postpartum posttraumatic stress. Child abuse & neglect. 2009;33(12):877–87. doi: 10.1016/j.chiabu.2009.05.004. [DOI] [PubMed] [Google Scholar]
- 26.Lev-Wiesel R, Daphna-Tekoah S, Hallak M. Childhood sexual abuse as a predictor of birth-related posttraumatic stress and postpartum posttraumatic stress. Child Abuse Negl. 2009;33(12):877–87. doi: 10.1016/j.chiabu.2009.05.004. [DOI] [PubMed] [Google Scholar]
- 27.Lang AJ, Gartstein MA, Rodgers CS, Lebeck MM. The impact of maternal childhood abuse on parenting and infant temperament. J Child Adolesc Psychiatr Nurs. 2010;23(2):100–10. doi: 10.1111/j.1744-6171.2010.00229.x. [DOI] [PubMed] [Google Scholar]
- 28.Morland L, Goebert D, Onoye J, Frattarelli L, Derauf C, Herbst M, et al. Posttraumatic stress disorder and pregnancy health: preliminary update and implications. Psychosomatics. 2007;48(4):304–8. doi: 10.1176/appi.psy.48.4.304. [DOI] [PubMed] [Google Scholar]
- 29.Yampolsky L, Lev-Wiesel R, Ben-Zion IZ. Child sexual abuse: is it a risk factor for pregnancy? J Adv Nurs. 2010;66(9):2025–37. doi: 10.1111/j.1365-2648.2010.05387.x. [DOI] [PubMed] [Google Scholar]
- 30.Seng JS, Low LK, Sperlich M, Ronis DL, Liberzon I. Post-traumatic stress disorder, child abuse history, birthweight and gestational age: a prospective cohort study. BJOG. 2011;118(11):1329–39. doi: 10.1111/j.1471-0528.2011.03071.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lukasse M, Henriksen L, Vangen S, Schei B. Sexual violence and pregnancy-related physical symptoms. BMC Pregnancy Childbirth. 2012;12:83. doi: 10.1186/1471-2393-12-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.UNICEF. The state of Latin American and Carribbean Children 2008. 2008 [Google Scholar]
- 33.Barth J, Bermetz L, Heim E, Trelle S, Tonia T. The current prevalence of child sexual abuse worldwide: a systematic review and meta-analysis. Int J Public Health. 2013;58(3):469–83. doi: 10.1007/s00038-012-0426-1. [DOI] [PubMed] [Google Scholar]
- 34.Barrios YV, Gelaye B, Zhong Q, Nicolaidis C, Rondon MB, Garcia PJ, et al. Association of childhood physical and sexual abuse with intimate partner violence, poor general health and depressive symptoms among pregnant women. PLoS One. 2015;10(1):e0116609. doi: 10.1371/journal.pone.0116609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.McKinney CM, Caetano R, Ramisetty-Mikler S, Nelson S. Childhood family violence and perpetration and victimization of intimate partner violence: findings from a national population-based study of couples. Ann Epidemiol. 2009;19(1):25–32. doi: 10.1016/j.annepidem.2008.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Garcia-Moreno C, Heise L, Jansen HA, Ellsberg M, Watts C. Public health. Violence against women. Science. 2005;310(5752):1282–3. doi: 10.1126/science.1121400. [DOI] [PubMed] [Google Scholar]
- 37.Garcia-Moreno C, Jansen HA, Ellsberg M, Heise L, Watts CH. Prevalence of intimate partner violence: findings from the WHO multi-country study on women's health and domestic violence. Lancet. 2006;368(9543):1260–9. doi: 10.1016/S0140-6736(06)69523-8. [DOI] [PubMed] [Google Scholar]
- 38.Perales MT, Cripe SM, Lam N, Sanchez SE, Sanchez E, Williams MA. Prevalence, types, and pattern of intimate partner violence among pregnant women in Lima, Peru. Violence Against Women. 2009;15(2):224–50. doi: 10.1177/1077801208329387. [DOI] [PubMed] [Google Scholar]
- 39.Lindert J, von Ehrenstein OS, Grashow R, Gal G, Braehler E, Weisskopf MG. Sexual and physical abuse in childhood is associated with depression and anxiety over the life course: systematic review and meta-analysis. International journal of public health. 2014;59(2):359–72. doi: 10.1007/s00038-013-0519-5. [DOI] [PubMed] [Google Scholar]
- 40.Rich-Edwards JW, Mason S, Rexrode K, Spiegelman D, Hibert E, Kawachi I, et al. Physical and sexual abuse in childhood as predictors of early-onset cardiovascular events in women. Circulation. 2012;126(8):920–7. doi: 10.1161/CIRCULATIONAHA.111.076877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wosu AC, Gelaye B, Williams MA. Childhood sexual abuse and posttraumatic stress disorder among pregnant and postpartum women: review of the literature. Arch Womens Ment Health. 2015;18(1):61–72. doi: 10.1007/s00737-014-0482-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fisher J, Cabral de Mello M, Patel V, Rahman A, Tran T, Holton S, et al. Prevalence and determinants of common perinatal mental disorders in women in low- and lower-middle-income countries: a systematic review. Bull World Health Organ. 2012;90(2):139G–49G. doi: 10.2471/BLT.11.091850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhong QY, Wells A, Rondon MB, Williams MA, Barrios YV, Sanchez SE, et al. Childhood abuse and suicidal ideation in a cohort of pregnant Peruvian women. Am J Obstet Gynecol. 2016;215(4):501 e1–8. doi: 10.1016/j.ajog.2016.04.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gelaye B, Kajeepeta S, Zhong QY, Borba CP, Rondon MB, Sanchez SE, et al. Childhood abuse is associated with stress-related sleep disturbance and poor sleep quality in pregnancy. Sleep Med. 2015;16(10):1274–80. doi: 10.1016/j.sleep.2015.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Felitti V, Anda R, Nordenberg D, Williamson D, Spitz A, Edwards V, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine. 1998;14(4):245–58. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 46.Gelaye B, Do N, Avila S, Carlos Velez J, Zhong QY, Sanchez SE, et al. Childhood Abuse, Intimate Partner Violence and Risk of Migraine Among Pregnant Women: An Epidemiologic Study. Headache. 2016;56(6):976–86. doi: 10.1111/head.12855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.DHS. Demographic Health Survey questionnaires and modules: Domestic violence module. [Accessed on September 19, 2014];2005 Available at : http://www.measuredhs.com/aboutsurveys/dhs/modules_archive.cfm.
- 48.Weathers F, Litz B, Herman D, Huska J, Keane T. The Annual Convention of the International Society for Traumatic Stress Studies. San Antonio, TX: 1993. The PTSD Checklist (PCL): Reliability, Validity, and Diagnostic Utility. [Google Scholar]
- 49.Mueser KT, Rosenberg SD, Fox L, Salyers MP, Ford JD, Carty P. Psychometric evaluation of trauma and posttraumatic stress disorder assessments in persons with severe mental illness. Psychological Assessment. 2001;13(1):110–7. doi: 10.1037//1040-3590.13.1.110. [DOI] [PubMed] [Google Scholar]
- 50.Wilkins KC, Lang AJ, Norman SB. Synthesis of the psychometric properties of the PTSD checklist (PCL) military, civilian, and specific versions. Depression and anxiety. 2011;28(7):596–606. doi: 10.1002/da.20837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Conybeare D, Behar E, Solomon A, Newman MG, Borkovec TD. The PTSD Checklist-Civilian Version: reliability, validity, and factor structure in a nonclinical sample. Journal of Clinical Psychology. 2012;68(6):699–713. doi: 10.1002/jclp.21845. [DOI] [PubMed] [Google Scholar]
- 52.Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD Checklist (PCL) Behaviour research and therapy. 1996;34(8):669–73. doi: 10.1016/0005-7967(96)00033-2. [DOI] [PubMed] [Google Scholar]
- 53.Freedy JR, Steenkamp MM, Magruder KM, Yeager DE, Zoller JS, Hueston WJ, et al. Post-traumatic stress disorder screening test performance in civilian primary care. Family practice. 2010;27(6):615–24. doi: 10.1093/fampra/cmq049. [DOI] [PubMed] [Google Scholar]
- 54.Jonas DE, Cusack K, Forneris CA, Wilkins TM, Sonis J, Middleton JC, et al. AHRQ Comparative Effectiveness Reviews. Rockville (MD): 2013. Psychological and Pharmacological Treatments for Adults With Posttraumatic Stress Disorder (PTSD) [PubMed] [Google Scholar]
- 55.Font SA, Maguire-Jack K. Pathways from childhood abuse and other adversities to adult health risks: The role of adult socioeconomic conditions. Child Abuse Negl. 2016;51:390–9. doi: 10.1016/j.chiabu.2015.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.DeSalvo KB, Hyre AD, Ompad DC, Menke A, Tynes LL, Muntner P. Symptoms of posttraumatic stress disorder in a New Orleans workforce following Hurricane Katrina. J Urban Health. 2007;84(2):142–52. doi: 10.1007/s11524-006-9147-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.O'Donnell M, Creamer M, Pattison P. Posttraumatic stress disorder and depression following trauma: understanding comorbidity. Am J Psychiatry. 2004;161(8):1390–6. doi: 10.1176/appi.ajp.161.8.1390. [DOI] [PubMed] [Google Scholar]
- 58.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. Journal of personality and social psychology. 1986;51(6):1173–82. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 59.VanderWeele T, Knol M. A tutorial on interaction. Epidemiologic Methods. (3) 2014:33–72. [Google Scholar]
- 60.Rothman KJ, Greenland S, Lash TL. Modern Epidemiology, 3rd Edition. Philadelphia, PA: Lippincott, Williams & Wilkins; 2012. [Google Scholar]
- 61.Fairchild AJ, McQuillin SD. Evaluating mediation and moderation effects in school psychology: a presentation of methods and review of current practice. J Sch Psychol. 2010;48(1):53–84. doi: 10.1016/j.jsp.2009.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Teicher MH, Andersen SL, Polcari A, Anderson CM, Navalta CP, Kim DM. The neurobiological consequences of early stress and childhood maltreatment. Neuroscience & Biobehavioral Reviews. 2003;27(1–2):33–44. doi: 10.1016/s0149-7634(03)00007-1. [DOI] [PubMed] [Google Scholar]
- 63.Watts-English T, Fortson BL, Gibler N, Hooper SR, Bellis MDD. The Psychobiology of Maltreatment in Childhood. Journal of Social Issues. 2006;62(4):717–36. [Google Scholar]
- 64.Seng JS, Rauch SA, Resnick H, Reed CD, King A, Low LK, et al. Exploring posttraumatic stress disorder symptom profile among pregnant women. Journal of psychosomatic obstetrics and gynaecology. 2010;31(3):176–87. doi: 10.3109/0167482X.2010.486453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ellsberg MC, Winkvist A, Pena R, Stenlund H. Women's strategic responses to violence in Nicaragua. Journal of epidemiology and community health. 2001;55(8):547–55. doi: 10.1136/jech.55.8.547. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.