Key Points
Question
Does either intramedullary nail fixation or locking plate fixation result in less disability 6 months after repair of distal tibia fracture?
Findings
In this randomized clinical trial that included 321 adults with displaced tibial fracture, there was no statistically significant difference in disability ratings between intramedullary nail or locking plate fixation at 6 months (29.8 vs 33.8 points out of a possible 100, respectively).
Meaning
Neither intervention resulted in a superior disability rating at 6 months, so other factors may need to be considered in deciding the optimal approach for displaced fractures of the distal tibia.
Abstract
Importance
The best treatment for fractures of the distal tibia remains controversial. Most such fractures require surgical fixation but outcomes are unpredictable and complications are common.
Objective
To assess disability, quality of life, and complications in patients with displaced tibial fracture treated with intramedullary nail fixation vs locking plate fixation.
Design, Setting, and Participants
A multicenter randomized trial recruiting 321 patients 16 years or older with an acute, displaced, extra-articular fracture of the distal tibia from April 2013 through April 2016 with final follow-up in February 2017. Exclusion criteria included open fractures, fractures involving the ankle joint, contraindication to nailing, or inability to complete questionnaires.
Interventions
Intramedullary nail fixation (nail group; n = 161), a metal rod inserted into the hollow center of the tibia, vs locking plate fixation (plate group; n = 160), a plate attached to the surface of the tibia with fixed-angle screws.
Main Outcomes and Measures
Disability Rating Index (DRI; score range, 0 [no disability] to 100 [complete disability]) at 6 months was the primary outcome measure, with a minimal clinically important difference of 8 points. DRI measurement was also collected at 3 and 12 months. Secondary outcomes were the Olerud-Molander Ankle Score (OMAS), quality of life, and complications (such as infection and further surgery).
Results
Among 321 randomized patients (mean age, 45 years [SD, 16.2]; men, 197 [61%]; had experienced traumatic injury after a fall, 223 [69%]), 258 completed the study. There was no statistically significant difference in the DRI score at 6 months between groups (mean score, 29.8 in the nail group vs 33.8 in the plate group; adjusted difference, 4.0 [95% CI, −1.0 to 9.0], P = .11). There was a statistically significant difference in the DRI score at 3 months in favor of nail fixation (mean score, 44.2 in the nail group and 52.6 in the plate group; adjusted difference, 8.8 [95% CI, 4.3 to 13.2], P < .001), but not at 12 months (mean score, 23.1 in the nail group and 24.0 in the plate group; adjusted difference, 1.9 [95% CI, −3.2 to 6.9], P = .47). Secondary outcomes showed the same pattern, including a statistically significant difference in mean OMAS at 3 and 6 months in favor of nail fixation. There were no statistically significant differences in complications, including the number of postoperative infections (9% in the nail group vs 13% in the plate group). Further surgery was more common in the plate group at 12 months (8% in nail group vs 12% in plate group).
Conclusions and Relevance
Among patients 16 years or older with an acute, displaced, extra-articular fracture of the distal tibia, neither nail fixation nor locking plate fixation resulted in superior disability status at 6 months. Other factors may need to be considered in deciding the optimal approach.
Trial Registration
clinicaltrials.gov Identifier: ISRCTN99771224
This randomized clinical trial compares the effects of locking plate vs intramedullary nail fixation on disability, symptoms, and quality of life among patients with an acute displaced extra-articular distal tibia fracture.
Introduction
The tibia is the most commonly broken major bone in the leg. Injuries require hospital admission, usually require surgery, and result in prolonged periods away from work and social activities. The best treatment for displaced, extra-articular fractures of the distal tibia (specifically the lower third of the tibia) remains controversial. These injuries are particularly difficult to manage due to the limited soft tissue coverage, poor vascularity of the area, and proximity of the fracture to the ankle joint. Infections, nonunion, and malunion are well-recognized complications of fractures of the distal tibia.
Surgical treatment options include intramedullary nail fixation, plate-and-screw fixation, and external fixation. External fixators may be beneficial in selected cases (such as intra-articular or segmental fractures) but the nail and plate options are most commonly used for extra-articular fractures. Mid-shaft fractures of the tibia are generally treated with locked intramedullary nails. However, in the more distal metaphyseal region of the tibia, the nail fixation may be less stable. The bolts or screws that are inserted into the nail may break, malalignment may occur, and there is a risk that the nail will penetrate into the ankle joint. The development of locking plates, for which a thread on the head of the screws locks into the holes in the plate to create a fixed-angle construct, has led to a recent increase in the use of plate fixation. However, plates are not without risks, they require greater soft tissue dissection, which carries a risk of infection, wound breakdown, and damage to the surrounding structures.
The Fixation of Distal Tibia Fractures (FixDT) trial was designed to compare intramedullary nail fixation with locking plate fixation for adult patients with a displaced fracture of the distal tibia (Figure 1).
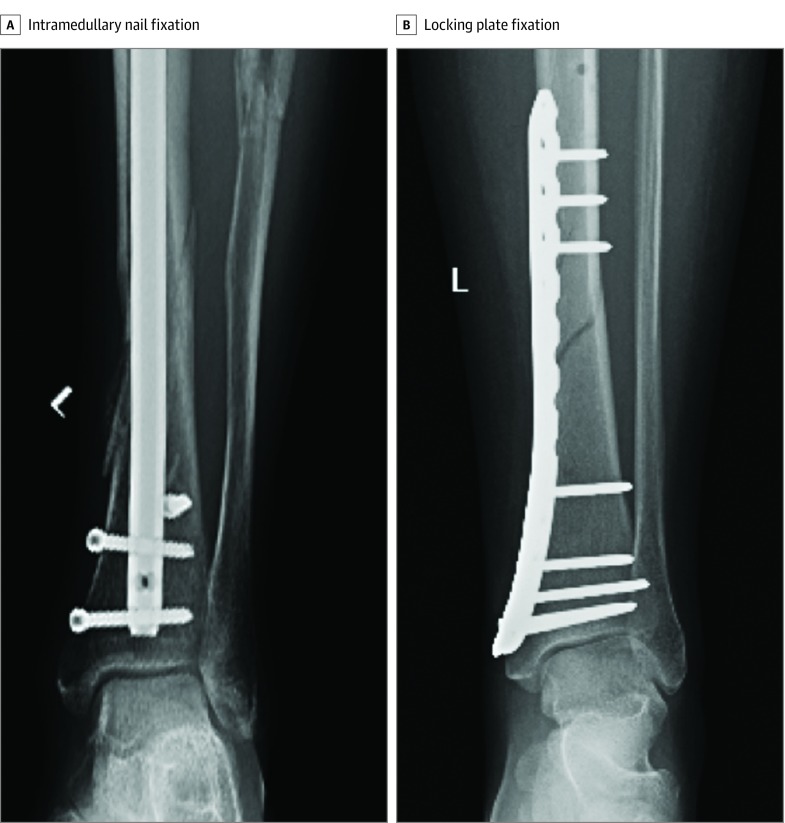
Figure 1. Radiographs of Distal Tibia Fractures Treated With Different Types of Surgical Fixation.
Methods
Study Design and Eligibility Criteria
The National Research Ethics Service approved the study, the approved protocol and statistical analysis plan are available in Supplement 1 and Supplement 2, respectively. The trial was overseen by independent steering and data and safety monitoring committees. This was a multicenter randomized clinical trial in 28 UK trauma hospitals. Young adults and adults 16 years or older (hereafter referred to as adults) with an acute, displaced, extra-articular fracture of the distal tibia were eligible to enter the trial if the treating surgeon believed the patient would benefit from surgical fixation of the fracture (Figure 2). A distal tibial fracture was defined as a fracture extending within 2 “Müller squares” of the ankle joint; Müller defined a square based upon the width of the patient’s own distal tibia, such that this measurement accounts for the different height of different patients. Patients were excluded if the fracture was open (the broken bone was exposed through a breach in the skin), the fracture extended into the ankle joint, there was a contraindication to intramedullary nail fixation (eg, a total knee replacement or previous deformity of the tibia), there was a contraindication to anesthesia, or the patient was unable to complete questionnaires. All patients gave written informed consent.
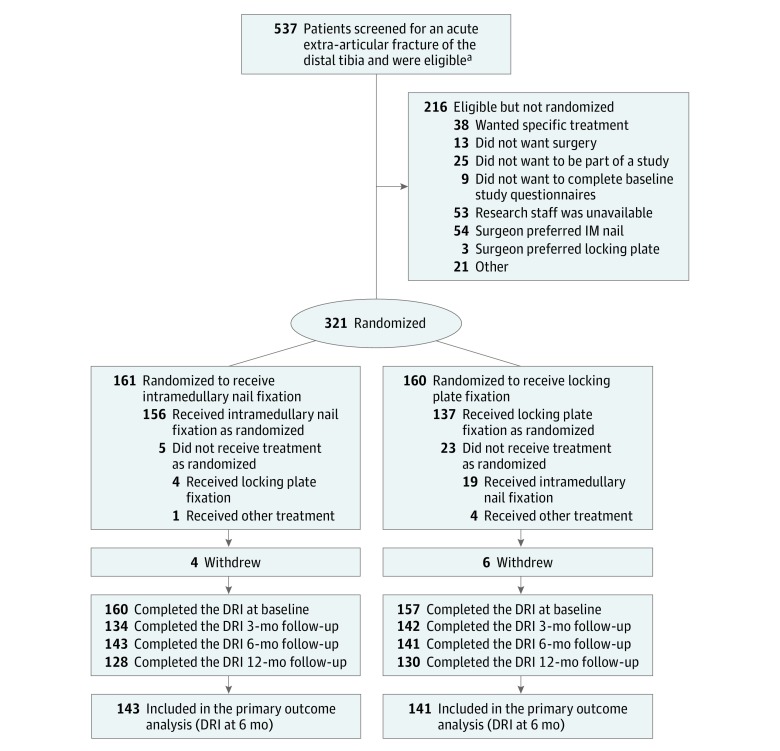
Figure 2. Flow of Patients Though the FixDT Trial.
DRI indicates Disability Rating Index, FixDT, Fixation of Distal Tibia Fractures.
aFull screening data varied by site depending on the case mix seen at that hospital (eg, some hospitals screened children but others only ever saw adult patients). Of screened patients, approximately 23% were excluded due to open fractures, 7% had been treated nonoperatively, 4% had been treated with external fixation, and in 4% the surgeon decided there was a contraindication to nail fixation (eg, patient had total knee replacement).
Randomization and Blinding
The method of fixation was allocated before surgery using a secure, centralized, web-based randomization service via a minimization algorithm provided by an accredited clinical trials unit. The minimization variables were center and age group (above and below 50 years) to improve balance between intervention groups; age was used to differentiate younger patients with normal bone quality who sustained high-energy fractures from older patients with low-energy (fragility) fractures related to osteoporosis. Blinding was ensured by registering patients before the treatment allocation was revealed.
Because the type of fixation used could easily be discerned by the patient due to the clearly visible surgical scars, the patients could not be blinded to their treatment. The treating surgeons could not be blind to the treatment. However, the treating clinical team took no part in the postoperative assessment of the patients, which was performed by independent research associates.
Interventions
Surgery was performed under general or regional anesthesia. All patients had thromboprophylaxis and antibiotic prophylaxis. All of the hospitals in the trial used both intramedullary nail and locking plate fixation as part of their routine clinical practice and all surgeons were familiar with both surgical interventions. Specialist trainees were allowed to operate under consultant supervision.
For intramedullary nail fixation, an intramedullary nail is inserted at the proximal end of the tibia and passed down the hollow center (medullary canal) of the bone to hold the fracture in the correct anatomical position (Figure 1A). The reduction technique, the surgical approach, the type and size of the nail, the configuration of the proximal and distal interlocking screws, and any supplementary device or technique was left to the discretion of the surgeon as per standard clinical practice.
For locking plate fixation, a locking plate is inserted at the distal end of the tibia and passed under the skin onto the surface of the bone (Figure 1B). Again, the details of the reduction technique, the surgical approach, the type and position of the plate, the number and configuration of fixed-angle screws, and any supplementary device or technique was left to the discretion of the surgeon. The only stipulation was that fixed-angle screws must be used in at least some of the distal screw holes—this is standard practice with all distal tibia locking plates. All patients received the same standardized, written physiotherapy advice detailing the exercises they needed to perform for rehabilitation following their injury; patients in both groups were advised to move their toes and ankle and knee joints fully within the limits of their comfort. Details of weight-bearing status were advised by the treating surgeon, but patients were encouraged to bear weight as soon as possible. Any other rehabilitation input beyond the written physiotherapy advice was left to the discretion of the treating clinicians.
Data Collection and Outcome Measures
The research associates at each center performed a clinical assessment and made a record of any early complications at the 6-week routine follow-up appointment. The patient-reported outcome measures, later complications, and resource-use data were collected using questionnaires at 3, 6, and 12 months. Radiographs were taken at 6 weeks and 12 months (or before 12 months if the surgeon considered the fracture to be united).
The primary outcome measure for this study was the Disability Rating Index (DRI) at 6 months, assuming a minimal clinically important difference of 8 points. The DRI is a validated questionnaire that is completed by the patient. It consists of 12 items specifically related to function of the lower limb, which are combined to provide an overall score from 0 (no disability) to 100 (complete disability). The secondary outcome measures were the EuroQol Health-Related Quality-of-Life 3-Level score (EQ-5D-3L; health-state score range, −0.59 [worse possible health] to 1 [perfect health], death = 0), with a minimal clinically important difference of 0.07, and the Olerud-Molander Ankle Score (OMAS) rating of pain and function at the ankle joint (score range, 0 [worst pain and function] to 100 [no pain and best function]). All serious adverse events occurring in the 12 months after surgery were recorded on a standardized complications form. These were categorized as “local complications related to the injury or its treatment,” “systemic complications,” and “unrelated adverse events.” Local complications included infection, vascular and neurological injury, venous thromboembolism, and malunion. Malunion was determined from standard anteroposterior and lateral radiographs of the tibia and fibula taken at 6 weeks and 12 months. Threshold values for malunion were determined by an independent trauma surgeon using OsiriX software (Pixmeo), version 7.5. These were coronal angulation of the tibia greater than 5°, sagittal angulation greater than 10°, and shortening greater than 10 mm. Any other surgery required in relation to the index fracture was recorded, including revision fixation, interventions for nonunion, and removal of symptomatic metalwork. A cost-effectiveness analysis is not reported in this article.
Statistical Analysis
A minimal clinically important difference for the DRI of 8 points was selected to power the study; at an individual patient level, this represents the ability to climb stairs or run, with “some difficulty” vs with “great difficulty.” At a population level, 8 points represents the difference between a “healthy patient” and a “patient with a minor disability.” The standard deviation of the DRI used in the sample size calculation was taken at 6 months from the pilot study and was approximately 20 points. Therefore 264 patients would be sufficient for 90% power at the 5% significance level (using 2-tailed significance testing). Allowing for 20% loss to follow-up, we aimed to recruit 320 patients in total.
The statistical analysis plan was approved by the independent data and safety monitoring committee. The primary outcome analysis investigated differences in the DRI at 6 months after randomization on an intention-to-treat basis, with early outcome analysis at 3 months and late outcome analysis at 12 months; per-protocol analyses were also reported. The primary (adjusted) analysis used a mixed-effects multivariable linear regression, with a random-effect term included to model potential associations within recruiting centers, and fixed effects for preinjury DRI score, age group (<50 years and ≥50 years), and sex (male and female). Unadjusted differences between treatment groups were assessed using a t test, based on a normal approximation for the DRI. Treatment effect estimates were presented with appropriate 95% CIs and all tests were 2-sided with a P value of less than .05 considered significant. No attempt was made to adjust for multiple testing; therefore, secondary analyses should be interpreted as exploratory. Analyses of secondary outcomes followed the same modeling approach as the primary outcome. Pairwise interaction terms between treatment group and both sex (male and female) and age group (<50 years and ≥50 years) were added to the mixed-effects models to test for important subgroup effects. Postoperative complications were compared between intervention groups using Fisher exact test. Where data were not available due to withdrawal of patients, lack of completion of individual data items, or loss to follow-up, the reasons for the missing data were ascertained and patterns assessed to judge plausibility of an assumption that data were missing at random. Sensitivity analyses were undertaken using multiple imputation techniques (imputation by chained equations) to assess the effect of missing data on the primary analysis. To complement the preplanned analysis, a post hoc exploratory analysis using each of the DRI, OMAS, and EQ-5D-3L index scores at all 4 time points was conducted. This analysis combined observed longitudinal data collected at the 4 time points into a single value, the area under the curve (AUC), and facilitated comparisons of the AUCs between treatment groups. Mixed models were used to provide unbiased estimates of the AUCs, and CIs determined from standard errors using asymptotic normality, under the assumption of data being missing at random.16AUCs were estimated by fitting a repeated-measures mixed model, with the same fixed-effects structure as used in the primary analyses (adjusted for preinjury score, sex, and age group), but with a 3-level random-effects structure in which observations (time points) were nested within patients and patients were nested within center. All analyses were undertaken in Stata (StataCorp), version 14.
Results
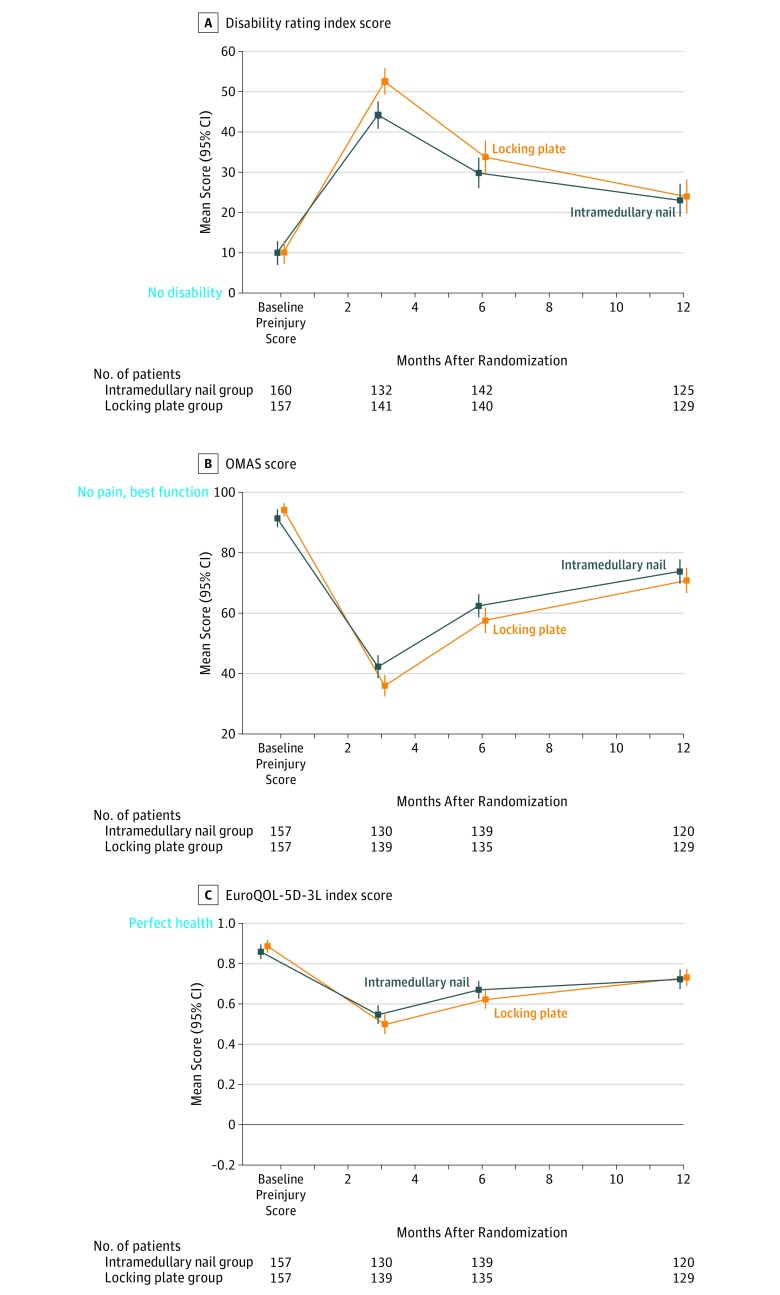
Of 537 screened patients between April 2013 and April 2016, 321 were randomized (161 allocated to receive intramedullary nail fixation [nail group] and 160 allocated to receive locking plate fixation [plate group]). The mean age and sex of consenting patients was similar to those who did not take part in the trial; a t test comparing means of both groups showed no evidence of a difference in age (mean difference, −0.9 [95% CI, −4.1 to 2.3]) and a 2-sample test of proportions showed no evidence of a difference in sex distribution (P = .82). The 2 treatment groups of patients were well matched in both demographics and preinjury disability and ankle and quality-of-life scores (Table 1). The mean age of patients was 45 years, 62% (n = 197) were men, 91% (n = 293) of patients received their allocated treatment and a completion rate of at least 80% was achieved at each follow-up time point. Follow-up was completed in February 2017. In both groups of patients, the DRI score improved over the 12 months following randomization, but did not return to preinjury levels (Figure 3).
Table 1. Baseline Characteristics of Patients Treated With Intramedullary Nail vs Locking Plate Fixation for Displaced Tibial Fracturea.
| Fixation Type, No. of Patients (%) | ||
|---|---|---|
| Intramedullary Nail (n = 161) | Locking Plate (n = 160) |
|
| Age, mean (SD), y | 44.3 (16.3) | 45.8 (16.3) |
| <50 | 97/161 (60) | 97/160 (61) |
| Women | 65/161 (40) | 59/160 (37) |
| Fracture on left side | 67/160 (42) | 75/159 (47) |
| Previous problems on the injured side | 40/160 (25) | 36/159 (23) |
| Mechanism of injury | ||
| Low-energy fallb | 85 (53) | 87 (54) |
| High-energy fall | 27 (17) | 24 (15) |
| Road traffic collision | 15 (9) | 22 (14) |
| Crush injury | 8 (5) | 3 (2) |
| Contact sports injury | 14 (9) | 11 (7) |
| Other | 11 (7) | 12 (8) |
| BMI, mean (SD) | 27.7 (6.2) | 27.7 (6.9) |
| Current smoker | 53/160 (33) | 50/158 (31) |
| Years smoking, mean (SD) | 19 (12) | 26 (14) |
| Alcohol consumption, units per weekc | ||
| 0-7 | 86 (53) | 87 (54) |
| 8-14 | 28 (17) | 24 (15) |
| 15-21 | 28 (17) | 22 (14) |
| >21 | 18 (11) | 22 (14) |
| Diabetes | 6/160 (4) | 7/159 (4) |
| Preinjury score, mean (SD)d | ||
| DRI | 9.9 (19.0) | 10.0 (18.4) |
| Median (IQR) | 1.2 (0-10.6) | 1.6 (0-11.5) |
| OMAS | 91.4 (19.0) | 94.2 (14.0) |
| EQ-5D-3L | 0.860 (0.23) | 0.888 (0.21) |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); DRI, Disability Rating Index; EQ-5D-3L, EuroQol Health-Related Quality of Life 3-Level; OMAS, Olerud-Molander Ankle Score.
Values may not sum to treatment group totals due to missing data.
Low-energy falls were from a height of less than 2 m.
One unit = 8 mL pure alcohol.
Score ranges: DRI, 0 (no disability) to 100 (complete disability); EQ-5D-3L, −0.59 (worse possible health) to 1 (perfect health), death is 0; OMAS, 0 (worst pain and function) to 100 (no pain and best function).
Figure 3. Overall Trends in Disability Rating Index, OMAS, and EQ-5D-3L Scores for Intramedullary Nail vs Locking Plate Fixation for Displaced Distal Tibia Fracture.
EQ-5D-3L indicates EuroQol Health-Related Quality of Life 3-Level score; OMAS, Olerud and Molander ankle score. Score range for each questionnaire: Disability Rating Index, 0 (no disability) to 100 (complete disability); OMAS, 0 (worst pain and function) to 100 (no pain and best function); and EQ-5D-3L, −0.59 (worse possible health) to 1 (perfect health) and death is 0. Preinjury scores were collected after the injury at baseline for all patients before surgery to reflect the patients’ preinjury status for all questionnaires.
Some patients were not included in the trial because of a preference for one treatment or the other. Only 38 patients expressed a preference, of whom 23 preferred an intramedullary nail fixation and 15 a locking plate fixation. However, there was a stronger treatment preference among the surgeons; 57 potentially eligible patients were excluded, 54 of whom were because the surgeon had a preference to use a nail fixation.
Primary Analysis
At the primary outcome of 6 months, on an intention-to-treat basis, the mean DRI score was 29.8 in the nail group and 33.8 in the plate group. The adjusted difference was not statistically significant (4.0 [95% CI, −1.0 to 9.0; P = .11]). For the secondary analysis at 3 months, the mean DRI score was 44.2 in the nail group vs 52.6 in the plate group, with an adjusted difference of 8.8 (95% CI, 4.3 to 13.2; P < .001). For the analysis at 12 months, the mean DRI score was 23.1 in the nail group vs 24.0 in the plate group, with an adjusted difference of 1.9 (95% CI, −3.2 to 6.9; P = .47).
Secondary Analysis
The secondary outcome measures showed the same pattern at each time point. Figure 3 shows the change in outcome scores over time graphically and Table 2 shows the actual numbers. The adjusted estimate of the treatment effect for the OMAS at 6 months was −6.0 (95% CI, −11.2 to −0.7; P = .03) in favor of the nail group (mean score: nail group, 62.4 [SD, 23.1] vs plate group, 57.6 [SD, 24.9]). The adjusted difference of the EQ-5D-3L score at 6 months was −0.06 (95% CI, −0.12 to −0.01; P = .03) in favor of the nail group (mean score: nail group, 0.67 [SD, 0.27] vs plate group, 0.62 [SD, 0.28]). So, the secondary outcome measures were statistically significantly different at 3 and 6 months, but there was no significant difference at 12 months.
Table 2. Patient-Reported Outcome Measures Among Patients Treated With Intramedullary Nail vs Locking Plate Fixation for Displaced Distal Tibial Fracture at All Time Points.
| Outcome | Intramedullary Nail (n = 161) |
Locking Plate (n = 160) |
Difference in Means | ||||||
|---|---|---|---|---|---|---|---|---|---|
| No. of Patients | Mean (95% CI) | Median (IQR) | No. of Patients | Mean (95% CI) | Median (IQR) | Unadjusted | Adjusted (95% CI)a |
P Value | |
| Primary Outcome | |||||||||
| DRI scoreb | |||||||||
| 6 mo | 142 | 29.8 (26.0 to 33.7) |
23.2 (10.6 to 43.4) |
140 | 33.8 (29.7 to 37.9) |
27.4 (13.4 to 52.7) |
4 (−1.6 to 9.6) |
4.0 (−1.0 to 9.0) |
.11 |
| Secondary Outcome | |||||||||
| DRI scoreb | |||||||||
| 3 mo | 132 | 44.2 (40.8 to 47.6) |
42.6 (28.7 to 55.2) |
141 | 52.6 (49.3 to 55.9) |
52.3 (37.6 to 66.5) |
8.4 (3.6 to 13.1) |
8.8 (4.3 to 13.2) |
<.001 |
| 12 mo | 125 | 23.1 (18.9 to 27.2) |
13.3 (5.6 to 35.9) |
129 | 24.0 (19.7 to 28.3) |
15.0 (5.2 to 32.6) |
0.9 (−5.0 to 6.8) |
1.9 (−3.2 to 6.9) |
.47 |
| OMASb | |||||||||
| 3 mo | 130 | 42.3 (38.4 to 46.1) |
139 | 36.0 (32.4 to 39.5) |
−6.3 (−11.5 to −1.1) |
−7.0 (−12.0 to −2.0) |
.006 | ||
| 6 mo | 139 | 62.4 (58.5 to 66.3) |
135 | 57.6 (53.3 to 61.8) |
−4.9 (−10.6 to 0.9) |
−6.0 (−11.2 to −0.7) |
.03 | ||
| 12 mo | 120 | 73.8 (69.7 to 77.9) |
129 | 70.8 (66.6 to 75.0) |
−3 (−8.8 to 2.9) |
−3.6 (−9.1 to 1.9) |
.19 | ||
| EQ-5D-3L scoreb | |||||||||
| 3 mo | 134 | 0.55 (0.50 to 0.59) |
142 | 0.50 (0.45 to 0.55) |
−0.05 (−0.12 to 0.02) |
−0.06 (−0.12 to 0.00) |
.07 | ||
| 6 mo | 143 | 0.67 (0.63 to 0.71) |
141 | 0.62 (0.58 to 0.67) |
−0.05 (−0.11 to 0.01) |
−0.06 (−0.12 to −0.01) |
.03 | ||
| 12 mo | 128 | 0.72 (0.67 to 0.77) |
130 | 0.73 (0.69 to 0.77) |
0.01 (−0.06 to 0.07) |
−0.02 (−0.07 to 0.05) |
.52 | ||
| Post Hoc AUC Analyses | |||||||||
| DRI scoreb | 160 | 351 (318 to 384) |
159 | 407 (371 to 437) |
56 (6 to 102) |
57 (12 to 103) |
.01 | ||
| OMASb | 160 | 765 (731 to 797) |
158 | 713 (683 to 749) |
48 (2 to 94) |
52 (7 to 96) |
.02 | ||
| EQ-5D-3L scoreb | 160 | 8.09 (7.69 to 8.50) |
159 | 7.71 (7.31 to 8.12) |
0.38 (−0.19 to 0.95) |
0.42 (−0.14 to 0.98) |
.15 | ||
Abbreviations: AUC, area under curve; DRI, Disability Rating Index; EQ-5D-3L, EuroQol Health-Related Quality of Life 3-Level; IQR, interquartile range; OMAS, Olerud-Molander Ankle Score.
Mixed-effects regression model based on intention-to-treat analysis approach with allocated treatment group, age group, and sex as fixed effects, and recruiting site as a random effect.
Score ranges: DRI, 0 (no disability) to 100 (complete disability); EQ-5D-3L, −0.59 (worse possible health) to 1 (perfect health), death is 0; OMAS, 0 (worst pain and function) to 100 (no pain and best function).
The secondary per-protocol analysis, analyzing patients in groups according to the treatment received, showed the same pattern of results as the primary intention-to-treat analysis. At the primary end point of 6 months the mean DRI score was 30.2 in the nail group and 34.0 in the plate group. The adjusted difference was not statistically significant (3.4 [95% CI, −1.1 to 7.8]; P = .15). At 3 months, the mean DRI score was 44.6 in the nail group vs 51.9 in the plate group, with an adjusted difference of 7.5 (95% CI, 3.6 to 11.3; P < .001). For the analysis at 12 months, the mean DRI score was 22.9 in the nail group vs 24.1 in the plate group, with an adjusted difference of 0.9 (95% CI, −3.3 to 5.0; P = .68). At 6 months there was no significant interaction between age and treatment group. In the subgroup of patients younger than 50 years, the mean DRI score was 25.6 in the nail group vs 31.1 in the plate group (adjusted difference, 5.4 [95% CI, −1.0 to 11.8]). In the subgroup of patients 50 years and older, the mean DRI score was 35.9 in the nail group vs 38.2 in the plate group (adjusted difference, 2.0 [95% CI, −6.0 to 10.0]); P for interaction = .52. There was also no significant interaction between sex and treatment group (P = .38). There was a very low level of missing data in all patient-reported outcome measures at all time points; hence, the results of the imputation analysis presented in eTable 1 in Supplement 3 result in very similar estimates of treatment effects.
Table 3 shows the postoperative complications at the 6-week assessment and further surgical interventions associated with the fracture in each group. There were no statistically significant differences in the rate of complications. Surgical debridement for deep infection was rare (1 of 161 patients in the nail group vs 5 of 160 patients in the plate group; P value for Fisher exact test = .12), but treatment with antibiotics for superficial wound healing complications was more common (14 of 157 patients in the nail group 9% [95% CI, 5% to 15%] vs 21 of 157 patients in the plate group 13% [95% CI, 8% to 20%]; P for Fisher exact test = .21). However, there were more secondary operations in the plate group vs the nail group. Of those patients allocated to the nail group, 34% (53/157) reported being fully weight bearing at the 6-week follow-up appointment compared with only 15% (23/157) of those allocated to the plate group (P < .001 for Fisher exact test; absolute rate difference, 19% [95% CI, 10% to 28%]). There were similar numbers of systemic complications in both groups of the trial, but there were numerically more reported unrelated serious adverse events over the duration of the trial among those allocated to the plate group (n = 80 events) than the nail group (n = 46 events).
Table 3. Patient-Reported Postoperative Complications at 6-Week Assessment and Further Related Surgery Within 12 Months of Initial Treatment Among Patients Receiving Intramedullary Nail vs Locking Plate Fixation for Displaced Distal Tibial Fracturea.
| No. of Events/Total Patients (%) | Absolute Risk Reduction, % (95% CI)b |
P Value | ||
|---|---|---|---|---|
| Intramedullary Nail (n = 161) | Locking Plate (n = 160) |
|||
| At 6-wk Assessment | ||||
| Infection symptoms identified | 20/157 (13) | 32/157 (20) | 8 (−1 to 16) | .09 |
| Erythema | 16/20 (80) | 27/32 (84) | 4 (−17 to 26) | .72 |
| Persistent serous drainage | 4/20 (20) | 12/32 (38) | 18 (−7 to 42) | .23 |
| Purulent drainage | 4/20 (20) | 6/32 (19) | −1 (−23 to 21) | >.99 |
| Dehiscence | 2/20 (10) | 8/32 (25) | 15 (−5 to 35) | .34 |
| Treated with antibiotics | 14/157 (9) | 21/157 (13) | 4 (−2 to 11) | .21 |
| Neurological injury | 8/157 (5) | 4/157 (3) | −3 (−7 to 2) | .38 |
| Vascular injury | 1/157 (1) | 0/157 (0) | −1 (−2 to 2) | >.99 |
| Tendon injury | 0/157 (0) | 2/157 (1) | 1 (−1 to 3) | .50 |
| Complex regional pain syndrome | 0/157 (0) | 1/157 (1) | 1 (−2 to 2) | >.99 |
| Deep vein thrombosis | 1/157 (1) | 2/157 (1) | 1 (−2 to 3) | >.99 |
| Pulmonary embolism | 1/157 (1) | 0/157 (0) | −1 (−2 to 2) | >.99 |
| Within 12 mo of Leaving the Treating Hospital | ||||
| Metalwork removal | 11/161 (7) | 14/160 (9) | 2 (−4 to 8) | .54 |
| Surgical debridement | 1/161 (1) | 5/160 (3) | 3 (−1 to 5) | .12 |
| Revision of internal fixation | 2/161 (1) | 5/160 (3) | 2 (−1 to 5) | .28 |
| Other operative procedure | 4/161 (2) | 3/160 (2) | 0 (−4 to 3) | >.99 |
| Additional surgery on distal tibia | 13/161 (8) | 19/160 (12) | 4 (−3 to 10) | .27 |
Values may not sum to treatment group totals due to missing data.
Fisher exact test; absolute risk reductions are for plate group relative to intramedullary nail group.
Post Hoc Analysis
Repeated-measures, mixed-effects post hoc regression analysis was used to calculate marginal means, which provide estimates and 95% CIs of AUCs for each treatment group (Table 2). For those patients allocated to the nail group, the AUC was 351 (95% CI, 316 to 380) and, for those allocated to the plate group, the AUC was 407 (95% CI, 374 to 438). The between-group difference was 57 DRI units (95% CI, 12 to 103). A t test comparing the values between groups yielded a P value of .01, indicating a statistically significant difference in the AUC between treatment groups.
Discussion
This multicenter trial of patients with a fracture of the distal tibia found no significant difference between intramedullary nail fixation and locking plate fixation in disability rating at 6 months or 12 months. However, patients in the nail group reported less disability earlier in their rehabilitation at 3 months. Secondary outcomes showed a similar pattern with better ankle function and improved health-related quality of life at 3 months and 6 months in the patients with a nail fixation, but no evidence of a difference at 12 months. However, these secondary analyses should be interpreted as exploratory and require further research.
A systematic review of the literature showed 6 other randomized clinical trials comparing nail with plate fixation for this injury. Two trials, involving 64 with nail fixation and 104 patients with plate fixation, found no difference in functional scores but showed a difference in wound complications, with more infections in the plate group. However, both these trials used traditional “nonlocking” plates rather than the newer fixed-angle locking devices. Modern locking plates are designed to be inserted using minimally invasive techniques, which may reduce the risk of wound complications. The third trial randomized 111 patients either to intermedullary nail fixation or locking plate fixation. The investigators found no difference in the time to union on radiographs but this was a single-center investigation and more than 20% of the patients in the trial were lost to follow-up. A fourth trial also compared intramedullary nail fixation with minimally invasive plate fixation. This trial did not find any difference in the Foot Function Index, but only 25 patients were included in total. The remaining 2 trials compared the results of external fixation (a different technique in which pins or wires are inserted into the bone and attached to a frame outside the skin) with both plate fixation and intramedullary nail fixation. The first of these trials concluded that “all achieved similar good functional results” but the different techniques may have different rates of complications. However, there were only 28 patients in each group in this trial. The final trial also concluded that all 3 methods were “efficient methods for treating distal tibia fractures” but that their complication profiles were different. This study was too small to draw firm conclusions with only 137 patients distributed across all 3 groups. In summary, previous trials have indicated that different forms of fixation for patients with a fracture of the distal tibia may have different complication profiles but failed to show a difference in functional outcomes. However, each of these trials was considerably smaller than the FixDT trial and so may not have been large enough to detect a clinically important difference between intramedullary nail fixation and locking plate fixation.
This study has several limitations. Two hundred sixteen potentially eligible patients were not randomized, which could pose a risk to the external validity (generalizability) of the trial. However, most of these patients were excluded for logistical reasons (eg, no research staff available at the weekend), good clinical reasons (eg, declined any surgery), or the patient declined the trial because they “did not want to be part of a research study” or “fill out questionnaires.” Of more potential concern were patients who were not included in the trial because of a preference for one treatment or the other. This did not seem to be common among the patients. However, there was a stronger treatment preference among the surgeons. This does suggest that there was a preconceived preference for nail fixation, at least among surgeons in some centers. However, if patients deemed “suitable only for a nail” were excluded, despite being eligible according to the trial criteria, this is only likely to have reduced the relative benefit of nail fixation compared with locking plate fixation. Other possible limitations included postrandomization crossover of patients from one group to the other. However, these were less than anticipated. Ninety one percent of patients received the treatment to which they had been allocated. Similarly, some loss to follow-up was expected. However, the sample size was inflated to account for loss to follow-up of 20%, and more than 80% of patients provided primary outcome scores at every time point.
Conclusions
Among patients 16 years or older with an acute, displaced, extra-articular fracture of the distal tibia, neither nail fixation nor locking plate fixation resulted in superior disability status at 6 months. Other factors may need to be considered in deciding the optimal approach.
Final Trial Protocol
Statistical Analysis Plan
eTable 1. Patient-Reported Outcome Measures: Summary Statistics, Unadjusted and Adjusted Treatment Effects at All Time Points Using Multiple Imputation
References
- 1.Digby JM, Holloway GM, Webb JK. A study of function after tibial cast bracing. Injury. 1983;14(5):432-439. [DOI] [PubMed] [Google Scholar]
- 2.Drosos G, Karnezis IA, Bishay M, Miles AW. Initial rotational stability of distal tibial fractures nailed without proximal locking: the importance of fracture type and degree of cortical contact. Injury. 2001;32(2):137-143. [DOI] [PubMed] [Google Scholar]
- 3.Kneifel T, Buckley R. A comparison of 1 versus 2 distal locking screws in tibial fractures treated with unreamed tibial nails: a prospective randomized clinical trial. Injury. 1996;27(4):271-273. [DOI] [PubMed] [Google Scholar]
- 4.Obremskey WT, Medina M. Comparison of intramedullary nailing of distal third tibial shaft fractures: before and after traumatologists. Orthopedics. 2004;27(11):1180-1184. [DOI] [PubMed] [Google Scholar]
- 5.Boenisch UW, de Boer PG, Journeaux SF. Unreamed intramedullary tibial nailing—fatigue of locking bolts. Injury. 1996;27(4):265-270. [DOI] [PubMed] [Google Scholar]
- 6.Mosheiff R, Safran O, Segal D, Liebergall M. The unreamed tibial nail in the treatment of distal metaphyseal fractures. Injury. 1999;30(2):83-90. [DOI] [PubMed] [Google Scholar]
- 7.AOTrauma Müller AO classification of fractures—long bones. https://aotrauma.aofoundation.org/Structure/search-center/Pages/AOSearchResults.aspx?k=muller+classification+of+fractures+-+long+bones&include=Top%2fspeciality%2faotrauma. Accessed October 17, 2017.
- 8.Salén BA, Spangfort EV, Nygren AL, Nordemar R. The Disability Rating Index: an instrument for the assessment of disability in clinical settings. J Clin Epidemiol. 1994;47(12):1423-1435. [DOI] [PubMed] [Google Scholar]
- 9.Brooks R. EuroQol: the current state of play. Health Policy. 1996;37(1):53-72. [DOI] [PubMed] [Google Scholar]
- 10.Dolan P. Modeling valuations for EuroQol health states. Med Care. 1997;35(11):1095-1108. [DOI] [PubMed] [Google Scholar]
- 11.Walters SJ, Brazier JE. Comparison of the minimally important difference for 2 health state utility measures: EQ-5D and SF-6D. Qual Life Res. 2005;14(6):1523-1532. [DOI] [PubMed] [Google Scholar]
- 12.Olerud C, Molander H. A scoring scale for symptom evaluation after ankle fracture. Arch Orthop Trauma Surg. 1984;103(3):190-194. [DOI] [PubMed] [Google Scholar]
- 13.Parsons H, Bruce J, Achten J, Costa ML, Parsons NR. Measurement properties of the Disability Rating Index in patients undergoing hip replacement. Rheumatology (Oxford). 2015;54(1):64-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mauffrey C, McGuinness K, Parsons N, Achten J, Costa ML. A randomised pilot trial of “locking plate” fixation vs intramedullary nailing for extra-articular fractures of the distal tibia. J Bone Joint Surg Br. 2012;94(5):704-708. [DOI] [PubMed] [Google Scholar]
- 15.White IR, Royston P, Wood AM. Multiple imputation using chained equations: issues and guidance for practice. Stat Med. 2011;30(4):377-399. [DOI] [PubMed] [Google Scholar]
- 16.Im GI, Tae SK. Distal metaphyseal fractures of tibia: a prospective randomized trial of closed reduction and intramedullary nail vs open reduction and plate and screws fixation. J Trauma. 2005;59(5):1219-1223. [DOI] [PubMed] [Google Scholar]
- 17.Vallier HA, Cureton BA, Patterson BM. Randomized, prospective comparison of plate vs intramedullary nail fixation for distal tibia shaft fractures. J Orthop Trauma. 2011;25(12):736-741. [DOI] [PubMed] [Google Scholar]
- 18.Vallier HA, Cureton BA, Patterson BM. Factors influencing functional outcomes after distal tibia shaft fractures. J Orthop Trauma. 2012;26(3):178-183. [DOI] [PubMed] [Google Scholar]
- 19.Guo JJ, Tang N, Yang HL, Tang TS. A prospective, randomised trial comparing closed intramedullary nailing with percutaneous plating in the treatment of distal metaphyseal fractures of the tibia. J Bone Joint Surg Br. 2010;92(7):984-988. [DOI] [PubMed] [Google Scholar]
- 20.Polat A, Kose O, Canbora K, Yanık S, Guler F. Intramedullary nailing vs minimally invasive plate osteosynthesis for distal extra-articular tibial fractures: a prospective randomized clinical trial. J Orthop Sci. 2015;20(4):695-701. [DOI] [PubMed] [Google Scholar]
- 21.Fang JH, Wu YS, Guo XS, Sun LJ. Comparison of 3 minimally invasive methods for distal tibia fractures. Orthopedics. 2016;39(4):e627-e633. [DOI] [PubMed] [Google Scholar]
- 22.Li Y, Jiang X, Guo Q, Zhu L, Ye T, Chen A. Treatment of distal tibial shaft fractures by 3 different surgical methods: a randomized, prospective study. Int Orthop. 2014;38(6):1261-1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Final Trial Protocol
Statistical Analysis Plan
eTable 1. Patient-Reported Outcome Measures: Summary Statistics, Unadjusted and Adjusted Treatment Effects at All Time Points Using Multiple Imputation