Abstract
The most effective strategy for preventing influenza is annual vaccination. We analyzed data from the 2005-2011 National Health Interview Survey (NHIS) using the Kaplan-Meier survival analysis procedure to estimate the cumulative proportion of persons reporting vaccination in the 2004-05 through 2010-11 seasons for persons ≥18, 18-49, 50-64, ≥65, persons with high-risk conditions, and health care personnel. We compared vaccination coverage by race/ethnicity within each age and high-risk group. Vaccination coverage among adults ≥18 years increased from 27.4% in the 2005-06 season to 38.1% in the 2010-11 season, with an average increase of 2.2% annually. From the 2005-06 to the 2010-11 seasons, coverage increased by 10-12 percentage points for all groups analyzed except for adults aged ≥65 years. Coverage for the 2010-11 season was 70.2% for adults ≥65 years, 43.7% for 50-64 years, 36.7% for 18-49 years with high-risk conditions, and 55.8% for health care personnel. Coverage in the 2010-11 season was significantly lower among non-Hispanic blacks and Hispanics compared with non-Hispanic whites among most of the adult sub-groups. Vaccination coverage among adults <65 years increased from the 2005-06 through the 2010-11 seasons, but substantial racial and ethnic disparities remained in most age groups. Targeted efforts are needed to improve coverage and reduce disparities.
Keywords: influenza vaccine, vaccination, coverage, high-risk conditions
Introduction
Influenza is a major cause of morbidity and mortality among adults in the United States (1-4). Annual epidemics of influenza typically occur during the late fall through early spring in the United States. Influenza viruses cause disease among persons in all age groups (1). Rates of serious illness and death are higher among adults aged ≥65 years, children younger than 2 years, pregnant women, and persons of any age who have medical conditions that place them at increased risk for complications from influenza (1). Influenza illness burden among healthy adults 18-49 years is an important cause of outpatient medical visits and loss of work days (5-6). Influenza vaccination has been shown to be a cost-effective tool for reducing morbidity and mortality associated with influenza among adults (5, 7-18). The economic impact of influenza illness is substantial. One national study estimated the annual economic burden of seasonal influenza in the United States to be $87.1 billion, including $10.4 billion in direct medical costs (6).
Since the 2010-11 influenza season, the Advisory Committee on Immunization Practices has recommended annual influenza vaccination for all persons 6 months of age and older. Prior to 2010, the adult groups recommended for annual vaccination included persons 50 years and older, pregnant women, persons aged 18-49 years with medical conditions associated with higher risk of complications from influenza infection, health care personnel, and close contacts of high risk persons (19). Healthy adults aged 18-49 years who were not close contacts of persons at high risk were added to those recommended for annual vaccination beginning in the 2010-11 season and the recommendation for adults aged 18-49 years was the major change in recommendations during the study period (1).
The most effective strategy for preventing influenza is annual vaccination. However, vaccination coverage has been suboptimal (1, 20-27). To assess the impact of the current adult influenza vaccination program in the United States and to identify strategies to improve vaccination coverage among adults, we analyzed the data from the 2005-2012 National Health Interview Survey (NHIS). We assessed influenza vaccination coverage among adults by age, high-risk status, and racial/ethnic groups.
Methods
We estimated national influenza vaccination coverage among U.S. adults using 2005-2011 NHIS data, and preliminary, early release NHIS data from January-March 2012. The NHIS is a national cross-sectional household survey that is conducted by the Centers for Disease Control and Prevention (CDC) (26, 28). The survey samples civilian, non-institutionalized populations living in the United States at the time of the survey. Face-to-face interviews are conducted weekly throughout the year with a probability sample of households. The NHIS provides estimates of health indicators, health care utilization and access, and health-related behaviors, and minority racial/ethnic groups (black, Hispanic, and others) were oversampled to allow for more precise estimation of health characteristics in these growing minority populations (26, 28). Seasonal influenza vaccination status was assessed by asking respondents if they had a seasonal influenza vaccination during the past 12 months and what month and year vaccination was received.
We defined high-risk persons as individuals who self-reported one or more of the following: ever being told by a physician they had diabetes, emphysema, coronary heart disease, angina, heart attack or other heart condition; being diagnosed with cancer in the past 12 months (excluding non-melanoma skin cancer) or ever being told by a physician they have lymphoma, leukemia or blood cancer; during the past 12 months, being told by a physician they have chronic bronchitis or weak or failing kidneys; or reporting an asthma episode or attack in the past 12 months. Race/ethnicity is defined as individuals who identified themselves as non-Hispanic white, non-Hispanic black, Hispanic, and others (including Asian, American India/Alaska Native, and multiple races).
Although female respondents were asked if they were pregnant at the time of the interview, estimates of influenza vaccination among pregnant women were not assessed due to survey limitations. Because pregnancy status was determined at the time of interview, currently pregnant women who were not pregnant during the influenza season could not be distinguished from currently pregnant women who were pregnant during the influenza season, and women not pregnant at the time of the survey but pregnant during the influenza season could not be identified. Starting in 2012, the NHIS began collecting information on influenza vaccination before, during, and after a recent or current pregnancy. Other data sources that more specifically ascertain pregnancy status in relation to vaccination histories are available (29-31).
During the 2005-06 through 2008-09 seasons, individuals were classified as health care personnel (HCP) if they were currently employed in a health care occupation or in a health care industry setting, based on standard occupation and industry categories recoded into categories by the National Center for Health Statistics (NCHS) at CDC. Health occupation included health diagnosing occupations, health assessment and treating occupations, health technologists, and health service occupations. Health care settings included hospitals, nursing or personal care facilities, and offices of physicians, dentists, chiropractors, optometrists or other health care practitioners. The NCHS categories of HCP are described further in Walker et al (25). From the 2009-10 to 2010-11 seasons, HCP is defined as adults aged ≥18 years who reported they currently volunteer or work in a hospital, medical clinic, doctor's office, dentist's office, nursing home or some other health-care facility, including part-time and unpaid work in a health care facility as well as professional nursing care provided in the home. The new definition we used in the 2009-10 to 2010-11 seasons is comparable to the definition we used in the 2005-06 through 2008-09 seasons (the agreement rate is about 95% between these two HCP definitions based on the 2010-11 NHIS data).
SUDAAN (Software for the statistical analysis of corrected data, Research Triangle Institute, Research Triangle Park, NC, version 10.01) was used to calculate point estimates and 95% confidence intervals (CIs). We assessed influenza vaccination among adult populations and stratified by race/ethnicity. To better assess influenza vaccination coverage for each season, we reported coverage restricted to individuals interviewed during September through June, and vaccinated during August through May, using the Kaplan-Meier survival analysis procedure. For example, respondents interviewed during September 2010 through June 2011 were analyzed to estimate influenza vaccination received during August 2010 through May 2011. For the 2004-05 season, estimates are based on interviews conducted during January through June 2005, and vaccination received during August 2004 through May 2005 (Starting from 2005, month and year of influenza vaccination was included in the NHIS data), while for the preliminary 2011-12 season estimates, interviews from September 2011 through March 2012, and vaccination received during August 2011 through February 2012 were used (interviews conducted during January through March 2012 are based on the 2012 NHIS early released data). Vaccination status was determined using reported month and year of most recent vaccination as of the end of the month prior to interview. T tests for linear trends in recent years were conducted for each group (coverage in the 2004-05 season was excluded from trend analysis since vaccine shortage occurred in the 2004-05 season and coverage among each group were substantially low). Racial/ethnic differences within each target group were assessed with T tests. All analyses were weighted to reflect the age, sex, and race/ethnicity of the U.S. non-institutionalized, civilian population. All tests were 2-tailed with the significance level set at α<0.05. A new weight variable was created based on how many months of interview data were included in the analyses. Since we restricted to individuals interviewed during September through June for the 2005-06 through 2010-11 seasons and 10 months of interview data were included in the analyses, the new weight variable=final weight*(12/10), while for the 2004-05 season, new weight=final weight*(12/6), and for the 2011-12 season, new weight=final weight*(12/7).
Individuals who refused to answer the influenza vaccination question or did not know their vaccination status (about 1.6% per season) were excluded from the analysis. Vaccination status was imputed for individuals who said they received vaccination but did not report their month and year of vaccination (percentage points imputed ranged 3-5% during the 2004-05 season through the 2011-12 season). Information was imputed from donor pools matched for week of interview, age group, region of residence, and race/ethnicity.
Results
Sample characteristics of the study population by age and high-risk status are given in Table 1. Overall, in the 2004-05 through the 2011-12 seasons, the NHIS analytic sample size ranged from 14,798-25,758 adults.
Table 1. Sample characteristics of participants ≥18 years in the United States, by age, high-risk status, and healthcare personnel -National Health Interview Survey, the 2004-05 through 2010-2011 seasons.
| 2004-05 Seasonaa | 2005-06 Seasonb | 2006-07 Seasonb | 2007-08 Seasonb | 2008-09 Seasonb | 2009-10 Seasonb | 2010-11 Seasonb | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sample size |
Weighted % |
Sample size |
Weighted % |
Sample size |
Weighted % |
Sample size |
Weighted % |
Sample size |
Weighted % |
Sample size |
Weighted % |
Sample size |
Weighted % |
|
| Age group | ||||||||||||||
| ≥18 years | 14,958 | 100.0 | 22,959 | 100.0 | 20,195 | 100.0 | 19,341 | 100.0 | 14,798 | 100.0 | 25,661 | 100.0 | 25,758 | 100.0 |
| 18-64 years | 12,078 | 83.9 | 18,570 | 83.9 | 16,207 | 83.8 | 15,436 | 83.5 | 11,826 | 83.1 | 20,441 | 83.0 | 20,426 | 82.9 |
| 18-49 years | 8,543 | 60.9 | 13,204 | 60.7 | 11,504 | 60.3 | 10,790 | 59.0 | 8,227 | 58.3 | 14,028 | 58.0 | 14,181 | 57.8 |
| 50-64 years | 3,535 | 23.0 | 5,366 | 23.2 | 4,703 | 23.5 | 4,646 | 24.5 | 3,599 | 24.8 | 6,413 | 25.0 | 6,245 | 25.2 |
| ≥65 years | 2,907 | 16.1 | 4,389 | 16.1 | 3,988 | 16.2 | 3,905 | 16.5 | 2,972 | 16.9 | 5,220 | 17.0 | 5,332 | 17.1 |
| Persons with high-risk conditionsc | ||||||||||||||
| 18-64 years | 2,397 | 100.0 | 3,548 | 100.0 | 2,995 | 100.0 | 2,919 | 100.0 | 2,410 | 100.0 | 4,194 | 100.0 | 4,017 | 100.0 |
| 18-49 years | 1,231 | 54.1 | 1,859 | 53.8 | 1,543 | 52.8 | 1,488 | 53.5 | 1,213 | 51.6 | 2,039 | 50.6 | 1,961 | 50.0 |
| 50-64 years | 1,166 | 45.9 | 1,689 | 46.2 | 1,452 | 47.2 | 1,431 | 46.5 | 1,197 | 48.4 | 2,155 | 49.4 | 2,056 | 50.0 |
| Persons without high-risk conditions | ||||||||||||||
| 18-64 years | 9,660 | 100.0 | 14,979 | 100.0 | 13,177 | 100.0 | 12,479 | 100.0 | 8,769 | 100.0 | 16,208 | 100.0 | 15,570 | 100.0 |
| 18-49 years | 7,296 | 76.9 | 11,313 | 76.5 | 9,943 | 76.1 | 9,281 | 74.6 | 6,374 | 72.1 | 11,962 | 74.7 | 11,544 | 74.2 |
| 50-64 years | 2,364 | 23.1 | 3,666 | 23.5 | 3,234 | 23.9 | 3,198 | 25.4 | 2,395 | 27.9 | 4,246 | 25.3 | 4,026 | 25.8 |
| Health-care personneld ≥18 years | 1,020 | 6.8e | 1,638 | 6.9e | 1,484 | 7.2e | 1,490 | 7.6e | 1,185 | 7.6e | 1,860 | 7.8e | 2,112 | 8.2e |
This is based on interviews conducted during January through June 2005.
This is based on interviews conducted during September through June for each influenza season (e.g., the 2005-06 season included persons interviewed during September 2005 through June 2006).
Adults categorized as being at high risk for influenza-related complications self-reported one or more of the following: 1) ever being told by a physician they had diabetes, emphysema, coronary heart disease, angina, heart attack, or other heart condition; 2) having a diagnosis of cancer during the preceding 12 months (excluding non-melanoma skin cancer) or ever being told by a physician they have lymphoma, leukemia, or blood cancer during the previous 12 months; 3) being told by a physician they have chronic bronchitis or weak or failing kidneys; or 4) reporting an asthma episode or attack during the preceding 12 months.
During the 2005-06 through 2008-09 seasons, adults were classified as health-care personnel if they were ≥18 years and currently employed in a health-care occupation or in a health-care--industry setting, on the basis of standard occupation and industry categories recoded in groups by National Center for Health Statistics, Centers for Disease Control & Prevention. From the 2009-10 to 2010-11 seasons, health-care personnel is defined as adults ≥18 years who currently volunteer or work in a hospital, medical clinic, doctor's office, dentist's office, nursing home or some other health-care facility including part-time and unpaid work in a health care facility as well as professional nursing care provided in the home.
This number indicates the percentage of adults ≥18 years who are health-care personnel.
Overall, for all age and high-risk groups, vaccination coverage was substantially lower for the 2004-05 season when a vaccine supply shortage occurred compared to the 2005-2006 season (Table 2). Influenza vaccination coverage among adults aged ≥18 years, 18-64 years, 18-49 years, and 50-64 years increased significantly from 27.4%, 20.0%, 15.2%, and 32.5%, respectively from the 2005-06 season to 38.1%, 31.5%, 26.1%, and 43.7%, respectively in the 2010-11 season, with annual average increases of 2.2%, 2.3%, 2.2%, and 2.3%, respectively (test for trend, p<0.05) (Table 2). The test for linear trend in vaccination coverage from the 2005-06 through 2010-11 seasons among adults aged ≥65 years was not statistically significant. Among adults aged ≥65 years, seasonal vaccination coverage during the 2009-10 season (66.5%) was significantly lower than coverage during the 2008-09 (69.6%) and 2010-11 (70.2%) seasons (p<0.05) (Table 2, Figure).
Table 2.
Influenza vaccination coverage among adults ≥ 18 years by age, high-risk status, and healthcare personnel -National Health Interview Survey, the 2004-05 to 2010-2011 seasons, United States.
| Influenza vaccination coverage | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||||||||
| 2004-05 Seasona | 2005-06 Seasonbb | 2006-07 Seasonb | 2007-08 Seasonb | 2008-09 Seasonb | 2009-10 Seasonb | 2010-11 Seasonb | Total change from 2005-06 season to 2010-11 seasonc | Annual average change from 2005-06 season to 2010-11 season | ||||||||
| % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | |||
| Age group | ||||||||||||||||
| ≥18 years | 20.9 | 20.1, 21.7 | 27.4d | 26.5, 28.3 | 30.2d | 29.3, 31.1 | 33.0d | 32.0, 33.9 | 35.2d | 34.0, 36.4 | 36.9d | 36.0, 37.9 | 38.1 | 37.2, 39.0 | 10.7 | 2.2* |
| 18-64 years | 13.1 | 12.5, 13.8 | 20.0d | 19.2, 20.9 | 23.0d | 22.1, 24.0 | 25.7d | 24.8, 26.7 | 28.2d | 27.0, 29.4 | 30.8d | 29.8, 31.8 | 31.5 | 30.6, 32.5 | 11.5 | 2.3* |
| 18-49 years | 10.2 | 9.4, 11.0 | 15.2d | 14.3, 16.1 | 17.5d | 16.6, 18.6 | 19.3d | 18.3, 20.3 | 22.4d | 21.1, 23.8 | 25.3d | 24.3, 26.4 | 26.1 | 25.0, 27.2 | 10.9 | 2.2* |
| 50-64 years | 21.0 | 19.6, 22.5 | 32.5d | 30.5, 34.6 | 36.9d | 35.0, 38.8 | 41.1d | 39.1, 43.1 | 41.9 | 39.5, 44.3 | 43.3 | 41.6, 45.1 | 43.7 | 42.1, 45.3 | 11.2 | 2.3* |
| ≥65 years | 61.2 | 59.0, 63.5 | 66.0d | 64.0, 68.0 | 67.7 | 65.6, 69.8 | 69.2 | 67.1, 71.3 | 69.6 | 67.3, 71.9 | 66.5d | 64.5, 68.5 | 70.2d | 68.2, 72.1 | 4.2 | 0.9 |
| Persons with high-risk conditionse | ||||||||||||||||
| 18-64 years | 24.8f | 22.9, 26.7 | 33.9df | 31.6, 36.4 | 37.7df | 35.2, 40.4 | 41.8df | 39.2, 44.5 | 41.4f | 38.6, 44.4 | 44.3f | 41.8, 46.8 | 45.6f | 43.1, 48.2 | 11.7 | 2.4* |
| 18-49 years | 17.6f | 15.4, 20.1 | 24.7df | 21.9, 27.9 | 26.5f | 23.3, 30.1 | 31.9df | 28.5, 35.6 | 31.9f | 27.9, 36.2 | 34.9f | 31.8, 38.3 | 36.7f | 33.3, 40.3 | 12.0 | 2.4* |
| 50-64 years | 33.2f | 30.2, 36.4 | 44.3df | 40.6, 48.2 | 49.9df | 46.2, 53.7 | 53.5f | 50.0, 57.2 | 51.2f | 47.3, 55.2 | 53.8f | 50.4, 57.3 | 54.4f | 51.0, 57.9 | 10.1 | 2.1* |
| Persons without high-risk conditions | ||||||||||||||||
| 18-64 years | 10.4 | 9.7, 11.1 | 16.9d | 16.0, 17.8 | 19.9d | 19.0, 20.9 | 21.9d | 20.9, 22.9 | 24.8d | 23.5, 26.2 | 27.5d | 26.4, 28.6 | 28.1 | 27.2, 29.1 | 11.2 | 2.2* |
| 18-49 years | 8.9 | 8.1, 9.7 | 13.7d | 12.8, 14.7 | 16.2d | 15.2, 17.3 | 17.2 | 16.2, 18.2 | 20.8d | 19.4, 22.3 | 23.8d | 22.7, 24.9 | 24.3 | 23.3, 25.4 | 10.6 | 2.1* |
| 50-64 years | 15.3 | 13.8, 17.1 | 27.2d | 25.1, 29.5 | 31.4d | 29.4, 33.5 | 35.8d | 33.4, 38.3 | 37.2 | 34.4, 40.2 | 38.4 | 36.2, 40.7 | 38.8 | 36.9, 40.7 | 11.6 | 2.2* |
| Health-care personnelg ≥18 years | 34.5 | 31.3, 38.0 | 43.5d | 39.9, 47.2 | 47.1 | 43.6, 50.7 | 47.6 | 44.5, 50.8 | 53.1d | 49.1, 57.3 | 60.3d | 57.1, 63.5 | 55.8 | 52.8, 59.0 | 12.3 | 2.5* |
Abbreviation: CI, confidence interval.
p<0.05 by t test for trend analysis from the 2005-06 season through 2010-11 season.
Estimates are based on interviews conducted during January through June 2005, and vaccination received during August 2004 through May 2005.
Estimates are based on interviews conducted during September through June, and vaccination received during August through May for each influenza season (e.g., the 2005-06 season included persons interviewed during September 2005 through June 2006, and vaccinated during August 2005 through May 2006).
Percentage change did not calculate from the 2004-05 season since vaccine supply shortage occurred and vaccination coverage was low during the 2004-05 season.
p<0.05 by t test for comparisons between two seasons with the prior season as the reference group (e.g., 2005-06 vs. 2004-05, 2006-07 vs. 2005-06, 2007-08 vs. 2006-07, 2008-09 vs. 2007-08, 2009-10 vs. 2008-09, and 2010-11 vs. 2009-10).
Adults categorized as being at high risk for influenza-related complications self-reported one or more of the following: 1) ever being told by a physician they had diabetes, emphysema, coronary heart disease, angina, heart attack, or other heart condition; 2) having a diagnosis of cancer during the preceding 12 months (excluding non-melanoma skin cancer) or ever being told by a physician they have lymphoma, leukemia, or blood cancer during the previous 12 months; 3) being told by a physician they have chronic bronchitis or weak or failing kidneys; or 4) reporting an asthma episode or attack during the preceding 12 months.
p<0.05 by t test for comparisons between persons with high-risk conditions and persons without high-risk conditions within the same age group of each season.
During the 2005-06 through 2008-09 seasons, adults were classified as health-care personnel if they were ≥18 years and currently employed in a health-care occupation or in a health-care--industry setting, on the basis of standard occupation and industry categories recoded in groups by National Center for Health Statistics, Centers for Disease Control & Prevention. From the 2009-10 to 2010-11 seasons, health-care personnel is defined as adults ≥18 years who currently volunteer or work in a hospital, medical clinic, doctor's office, dentist's office, nursing home or some other health-care facility including part-time and unpaid work in a health care facility as well as professional nursing care provided in the home. Vaccination coverage for the 2009-10 and 2010-11 seasons among health-care personnel were 57.5%, and 57.4%, respectively if the old health-care personnel definition of 2005-06 through 2008-09 seasons was used.
Figure 1. Influenza Vaccination Coverage Among Adult Populations, the 2004-2005 to 2011-2012 Seasons.
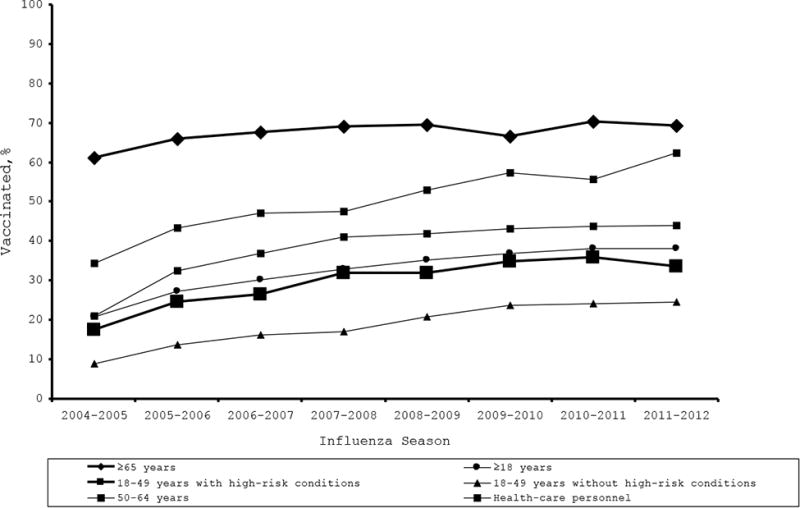
Among adults with high-risk conditions, vaccination coverage for adults aged 18-64 years, 18-49 years, and 50-64 years significantly increased from 33.9%, 24.7%, and 44.3%, respectively in the 2005-06 season to 45.6%, 36.7%, and 54.4%, respectively in the 2010-11 season, with annual average increases of 2.4%, 2.4%, and 2.1%, respectively (test for trend, p<0.05) (Table 2, Figure).
Among adults without high-risk conditions, vaccination coverage for adults aged 18-64 years, 18-49 years, and 50-64 years significantly increased from 16.9%, 13.7%, and 27.2%, respectively in the 2005-06 season to 28.1%, 24.3%, and 38.8%, respectively in the 2010-11 season (test for trend, p<0.05) (Table 2). For all years, within each age group, coverage was significantly lower among those without high-risk conditions compared with those with high-risk conditions (Table 2).
Among HCP, coverage significantly increased from the 2005-06 season to the 2010-11 season, with an annual average increase of 2.5% (test for trend, p<0.05) (Table 2, Figure). Vaccination coverage for the 2009-10 and 2010-11 seasons among HCP were 60.3%, and 55.8%, respectively (Figure, Table 2). For the 2010-11 season, influenza vaccination coverage among HCP was significantly lower for Hispanics and non-Hispanic blacks compared to non-Hispanic whites (Table 3).
Table 3.
Influenza vaccination coverage among adults ≥18 years by age, high-risk status, healthcare personnel, and race/ethnicitya-National Health Interview Survey, the 2010-11 season, United States.
| Influenza vaccination coverage | ||||||||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| Non-Hispanic white | Non-Hispanic black | Hispanic | Othersb | |||||
| % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | |
| Age group | ||||||||
| ≥18 years | 41.1 | 39.9, 42.3 | 32.1c | 29.5, 34.8 | 28.8c | 27.0, 30.7 | 37.4 | 34.0, 41.1 |
| 18-64 years | 33.4 | 32.2, 34.7 | 28.0c | 25.4, 30.9 | 25.4c | 23.6, 27.3 | 33.1 | 29.7, 36.8 |
| 18-49 years | 26.7 | 25.3, 28.2 | 25.2 | 22.3, 28.3 | 23.3c | 21.3, 25.4 | 28.4 | 25.1, 32.1 |
| 50-64 years | 46.1 | 44.2, 48.1 | 35.1c | 30.7, 40.0 | 34.1c | 29.8, 38.8 | 45.7 | 37.7, 54.5 |
| ≥65 years | 72.0 | 69.9, 74.0 | 60.5c | 54.4, 66.7 | 64.7 | 57.1, 72.1 | 67.2 | 58.3, 75.9 |
| Persons with high-risk conditionsd | ||||||||
| 18-64 years | 46.4 | 43.5, 49.5 | 44.1 | 37.3, 51.6 | 42.6 | 36.9, 48.8 | 48.1 | 37.2, 60.5 |
| 18-49 years | 34.5 | 30.4, 39.0 | 42.1 | 32.5, 53.2 | 41.7 | 34.4, 49.8 | 33.4 | 23.4, 46.3 |
| 50-64 years | 57.0 | 52.9, 61.3 | 46.2c | 38.4, 54.8 | 43.6c | 34.7, 53.6 | 72.8 | 46.4, 93.4 |
| Persons without high-risk conditions | ||||||||
| 18-64 years | 30.2 | 28.9, 31.5 | 23.6c | 21.1, 26.4 | 22.1c | 20.2, 24.3 | 30.3 | 26.9, 34.0 |
| 18-49 years | 25.4 | 24.0, 26.9 | 22.0c | 19.3, 25.0 | 21.0c | 18.9, 23.3 | 27.5 | 24.0, 31.3 |
| 50-64 years | 41.3 | 39.0, 43.6 | 28.8c | 23.8, 34.5 | 28.7c | 23.9, 34.2 | 39.1 | 30.7, 48.9 |
| Health-care personnele | ||||||||
| ≥18 years | 58.6 | 54.8, 62.4 | 43.7c | 36.2, 52.1 | 45.2c | 36.5, 54.9 | 66.8 | 56.4, 77.0 |
Abbreviation: CI, confidence interval.
This table is based on interviews conducted during September 2010 through June 2011, and vaccination received during August 2010 through May 2011.
Others included Asian, American India/Alaska Native, and multiple races.
p<0.05 by t test for comparisons between racial/ethnic groups with non-Hispanic white as the reference group.
Adults categorized as being at high risk for influenza-related complications self-reported one or more of the following: 1) ever being told by a physician they had diabetes, emphysema, coronary heart disease, angina, heart attack, or other heart condition; 2) having a diagnosis of cancer during the preceding 12 months (excluding non-melanoma skin cancer) or ever being told by a physician they have lymphoma, leukemia, or blood cancer during the previous 12 months; 3) being told by a physician they have chronic bronchitis or weak or failing kidneys; or 4) reporting an asthma episode or attack during the preceding 12 months.
During the 2010-11 season, health care personnel is defined as adults ≥18 years who currently volunteer or work in a hospital, medical clinic, doctor's office, dentist's office, nursing home or some other health-care facility including part-time and unpaid work in a health care facility as well as professional nursing care provided in the home.
Influenza vaccination coverage for the 2010-11 season by race and ethnicity, age group, and high risk status is shown in Table 3. Vaccination coverage among most adult sub-groups was significantly lower for Hispanics and non-Hispanic blacks compared with non-Hispanic whites (Table 3). Coverage for the 2010-11 season among adults 18-64 years with high-risk conditions was similar across racial/ethnic groups.
Preliminary vaccination coverage for the 2011-12 season is shown in the figure. Preliminary vaccination coverage estimates for the 2011-12 season were similar to the 2010-11 season estimates among age and high-risk groups, except for increase in coverage among HCP from 55.8% (52.8, 58.9) in the 2010-11 season to 62.4% (58.3, 66.6) in the 2011-12 season.
Discussion
Our study indicates that influenza vaccination coverage among adults significantly increased over five influenza seasons through 2010-11, but varied by age group and whether respondents reported health conditions associated with risk for complications from influenza infection. Vaccination coverage among all groups recommended for vaccination remains suboptimal (including HCP). Coverage was lower than the 90% Healthy People 2020 target for persons 18-64 years with high-risk conditions, persons aged ≥65 years, and HCP (32). Vaccination coverage was substantially lower for all age and high-risk groups in the 2004-05 season due to the vaccine supply shortage which occurred during that season (33).
Overall, by the 2010-11 season, the first season during which all adults were recommended for influenza vaccination, vaccination coverage among adults ≥18 years was 38% with vaccination estimates steadily increasing from the 2005-06 season through the 2010-2011 season. Coverage also increased steadily from the 2005-06 season through the 2010-2011 season among healthy adults aged 18-49 year, the group added in 2010 to those for whom annual vaccination is recommended by the Advisory Committee on Immunization Practices (1). This group was added given the known significant morbidity and economic impact of influenza in working age adults (12). In addition, the universal vaccination recommendation also eliminates the need to determine whether each person has one or more specific indications for vaccination and emphasizes the importance of preventing influenza among persons of all ages (1). Continuing annual monitoring of vaccination coverage among adults ≥18 years is important to assess the impact of the vaccination program and to focus efforts on groups with lagging coverage.
Influenza vaccination uptake remains low among adults for whom vaccination has long been recommended, especially adults younger than 65 years of age who have high-risk medical conditions. In the 2010-11 season, vaccination coverage among adults 18-64 years with high-risk conditions was only 45.6%. This is substantially lower than the 90% Healthy People 2020 target for this risk group. The universal influenza vaccination recommendation may help improve vaccination coverage among this age group in future seasons, but continued focus to ensure vaccination among high-risk groups is essential as they are at the greatest risk of influenza-related hospitalization and death (34, 35). Primary care physicians, medical subspecialists, and other health care professionals and vaccination providers, including pharmacists, should work together to ensure that persons at high-risk are assessed for their vaccine needs, receive a strong recommendation for vaccination and are either vaccinated by the recommending provider or referred to another provider if they do not provide influenza vaccination services.
Vaccination coverage for adults aged ≥65 years did not significantly increase linearly during the 2005-06 season (66.0%) through 2010-11 seasons (70.2%), and the preliminary estimate for 2011-12 was similar to 2010-11. The lack of change in influenza vaccination coverage in this age group indicates that new approaches are needed if increases in influenza vaccination are to occur and reach the 90% Healthy People 2020 target. Reasons for the lack of change in coverage are not well understood. One recent study indicated that the majority (67%) of adults aged ≥65 years who are vaccinated receive their influenza vaccination in a clinical setting, which is significantly higher than those aged 18-49 years (54%) and 50-64 years (56%) (36). One potential reason for the level coverage in recent years might be related to system or operational factors affecting the number of persons that can be vaccinated in clinical settings and the failure to implement interventions to promote immunization. An increase in vaccination in alternative settings (e.g., community immunizers, health department clinics, pharmacies, and educational settings) may help improve influenza vaccination; however, individuals must be motivated to seek out vaccination, and an increase in the proportion of older persons receiving influenza vaccinations in retail settings was not associated with an increase in vaccination coverage (36, 37). A provider's recommendation remains one of the most important determinants of vaccination (36, 37).
Trivalent seasonal influenza vaccination coverage declined during the 2009-10 season among adults aged ≥65 years. One of the possible reasons is that adults aged ≥65 were not in the first priority groups for limited doses of the influenza A (H1N1) 2009 monovalent vaccine, although they were included in targeted groups once vaccine supply increased (38). Lower coverage in older adults might reflect confusion regarding the influenza A (H1N1) 2009 monovalent vaccine recommendations and the continued strong recommendation to vaccinate all elderly with seasonal influenza vaccine.
Influenza vaccination coverage among HCP increased by twelve percentage points from the 2005-06 through 2010-11 seasons, although a similar increase was observed for all adults aged 18-64 years. HCP are exposed to influenza both at work and in the community. Vaccination of this group is especially important given their exposure to many high risk patients and the fact that HCP often work while ill (39-42). Despite influenza vaccination being recommended annually for HCP by the Advisory Committee on Immunization Practices and numerous medical, nursing and pharmacy professional organizations, and being part of the Standards for Adult Immunization Practices (43), vaccination coverage remains suboptimal. Low awareness of the federal vaccination recommendations for seasonal influenza vaccination among HCP may have affected vaccination coverage. One study showed that only about 45-50% of HCP correctly reported being in the target groups recommended to receive annual influenza (Unpublished data, and CDC-sponsored population-based internet panel surveys in the 2010-11 influenza season). Factors that may increase vaccination coverage among HCP include convenient access to vaccination during all shifts and at no cost to HCP, health care facility leadership support for vaccination efforts, providing feedback to HCP on vaccination levels at their workplace, and education of HCP that emphasizes the importance of HCP vaccination for patient safety, the effectiveness and safety of influenza vaccine (44). Worksite vaccination could significantly increase seasonal vaccination coverage among HCP; however, one study showed that one-third of health care settings did not offer on-site vaccination for HCP (44).
Our study showed that vaccination coverage among most adult sub-groups that were analyzed was significantly higher among non-Hispanic white compared with non-Hispanic blacks and Hispanics. Racial/ethnic disparities in influenza vaccination have been described in previous studies (21, 23-26, 45). Multiple factors likely contribute to these racial/ethnic disparities, including differences in attitudes toward vaccination and preventive care, propensity to seek and accept vaccination, variations in likelihood that providers recommend vaccination, and differences in quality of care received by racial/ethnic populations (1, 24, 25, 46-51). Broad use of interventions to remove barriers to access and to make offering of vaccination in health care and other settings a routine practice are important components of efforts to reduce these disparities (51, 52). Efforts to reduce disparities may be most important for older adult age groups given smaller disparities in adults aged 18-49 years.
The CDC publishes estimates of influenza vaccination coverage from several data sources, including the Behavioral Risk Factor Surveillance System (BRFSS), National Immunization Survey, internet panel surveys, and NHIS (29). For adults, the estimates from BRFSS provide timely national and state-specific estimates that are available by the time the next influenza vaccination campaigns begin. Internet panel surveys provide timely estimates (in-season and rapid post-season) for the general population and rarer populations of HCP and pregnant women while also providing information on knowledge, attitudes and behaviors related to influenza vaccination. Estimates from NHIS are not as timely, but may provide more valid national estimates than estimates from telephone and internet panel surveys. The NHIS is a national household survey conducted mostly by face-to-face interviews with higher response rates (60-70%) than the BRFSS, a telephone survey with lower response rates (50-60%) (23, 26, 28, 53, 54). For assessing national trends, other advantages of NHIS include availability of a more complete set of high-risk conditions and longer availability to provide season-specific estimates using self-reported month and year of most recent influenza vaccination (since 2005 for NHIS compared to 2008 for BRFSS).
Thus, the NHIS provides a means to assess the potential validity of estimates from more timely data sources. Influenza vaccination coverage in the 2010-11 season based on the BRFSS data was somewhat higher compared to NHIS estimates (40.5% vs. 38.1% for adults aged ≥18 years, 30.5% vs. 26.1% for adults aged 18-49 years, and 44.5% vs. 43.7 for adults aged 50-64 years), and lower for adults ≥65 years (66.6% from BRFSS vs. 70.2% from NHIS). While NHIS estimates for adults aged ≥65 years appear stable in recent seasons aside from a dip during 2009-10, BRFSS estimates for this age group appear to indicate a possible decline, with estimates of 74% for 2008-09, 67% for 2010-11, and 65% for 2011-12 (53). However, both data sources indicate coverage in older adults is in the range of 65-70% with much room for improvement. Ongoing comparisons of NHIS and other sources of influenza vaccination coverage are needed; over several seasons, these comparisons will provide a better assessment of the validity of signals in trends and disparities identified from other data sources. Factors that may contribute to the differences in estimated vaccination coverage between NHIS and other data sources include more representative sample frame and higher response rates for NHIS, survey mode (in-person for NHIS, telephone or internet for others), and differences in survey operations and weighting procedures. Starting in 2008, BRFSS began adding samples of persons in households with only cellular telephone service in each state to the landline telephone sampling frame (55).
The findings in this report are subject to limitations. Influenza vaccination status and high-risk conditions were self-reported and were not validated with medical records. However, self-reported seasonal influenza vaccination status among older adults has been shown to have relatively high agreement with vaccination status ascertained from medical records, with a range of a 5-11 percentage point higher estimates based on self-reported vaccination status compared to estimates based on vaccination status from medical records (56-58). For the 2009-10 season when both seasonal vaccine and the influenza A (H1N1) 2009 monovalent vaccine were both available, it is possible that some persons may have confused receipt of the influenza A (H1N1) 2009 monovalent vaccination and seasonal influenza vaccination, with potential for over- or under-estimation of coverage for seasonal vaccine in 2009-10. NHIS response rates were 60-70%, and it is possible that non-response bias may remain after weighting adjustments.
Influenza vaccination coverage in all groups recommended for vaccination remains suboptimal. Substantial improvement in annual influenza vaccination of recommended groups is needed to maximally reduce the health impact of influenza. Expanded access through greater use of complimentary settings and vaccine providers, and better use of evidence-based practices at medical sites (e.g., standing orders, and reminder/recall notification) are important to improve influenza vaccination coverage further (43).
Acknowledgments
The authors thank Mr. Ajay Yesupriya, Dr. Carolyn S. Neal, the Research Data Center, National Center for Health Statistics, Centers for Disease Control and Prevention; and Dr. Stacie, M. Greby, Dr. Helen Ding, Dr. Jun Zhang, Ms. Alissa O'Halloran, Mr. David Yankey, and other members of the Adult and Flu Vaccine Coverage Monitoring Team for their important contributions to the paper.
Abbreviations
- NHIS
National Health Interview Survey
- BRFSS
Behavioral Risk Factor Surveillance System
- HCP
Health care personnel
Footnotes
Disclaimer: The findings and conclusions in this presentation are those of the authors and do not necessarily represent the views of CDC.
Author Contributions: Dr. Lu had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: Lu, Singleton, Euler, Bridges Analysis and interpretation of data: Lu, Singleton, Euler, Williams, Bridges Drafting of the manuscript: Lu, Singleton, Euler, Williams, Bridges Critical revision of the manuscript for important intellectual content: Lu, Singleton, Euler, Williams, Bridges Study supervision: Lu, Singleton, Bridges
References
- 1.Fiore AE, Uyeki TM, Broder K, Finelli L, Euler GL, Singleton JA, et al. Prevention and control of influenza: recommendations of the Advisory Committee on Immunization Practices. MMWR. 2010;59(RR08):1–62. [PubMed] [Google Scholar]
- 2.Thompson WW, Shay DK, Weintraub E, et al. Mortality associated with influenza and respiratory syncytial virus in the United States. JAMA. 2003;289(2):179–186. doi: 10.1001/jama.289.2.179. [DOI] [PubMed] [Google Scholar]
- 3.Thompson WW, Shay DK, Weintraub E, et al. Influenza-associated hospitalization in the United States. JAMA. 2004;292(11):1333–1340. doi: 10.1001/jama.292.11.1333. [DOI] [PubMed] [Google Scholar]
- 4.Bridges CB, Katz JM, Levandowski RL, Cox NJ. Vaccines. fifth. Elsevier Saunders; Philadelphia, PA: 2007. Inactivated influenza vaccine; pp. 259–290. [Google Scholar]
- 5.Bridges CB, Thompson WW, Meltzer MI, Reeve GR, Talamonti WJ, Cox NJ, et al. Effectiveness and cost-benefit of influenza vaccination of healthy working adults: A randomized controlled trial. JAMA. 2000;284(13):1655–63. doi: 10.1001/jama.284.13.1655. [DOI] [PubMed] [Google Scholar]
- 6.Molinari NA, Ortega-Sanchez IR, Messonnier ML, et al. The annual impact of seasonal influenza in the US: measuring disease burden and costs. Vaccine. 2007;25(27):5086–5096. doi: 10.1016/j.vaccine.2007.03.046. [DOI] [PubMed] [Google Scholar]
- 7.Mullooly JP, Bridges CB, Thompson WW, Chen J, Weintraub E, Jackson LA, et al. Influenza- and RSV-associated hospitalizations among adults. Vaccine. 2007;25(5):846–855. doi: 10.1016/j.vaccine.2006.09.041. [DOI] [PubMed] [Google Scholar]
- 8.Kissling E, Valenciano M I-MOVE case-control studies team. Early estimates of seasonal influenza vaccine effectiveness in Europe among target groups for vaccination: results from the I-MOVE multicentre case-control study, 2011/12. Euro Surveill. 2012 Apr 12;17(15) [PubMed] [Google Scholar]
- 9.Jimenez-Jorge S, de Mateo S, Pozo F, Casas I, Garcia Cenoz M, Castilla J, et al. Early estimates of the effectiveness of the 2011/12 influenza vaccine in the population targeted for vaccination in Spain, 25 December 2011 to 19 February 2012. Euro Surveill. 2012 Mar 22;17(12) [PubMed] [Google Scholar]
- 10.Vu T, Farish S, Jenkins M, Kelly H. A meta-analysis of effectiveness of influenza vaccine in persons aged 65 years and over living in the community. Vaccine. 2002;20(13-14):1831–1836. doi: 10.1016/s0264-410x(02)00041-5. [DOI] [PubMed] [Google Scholar]
- 11.Govaert TM, Thijs CT, Masurel N, Sprenger MJ, Dinant GJ, Knottnerus JA. The efficacy of influenza vaccination in elderly individuals. A randomized double-blind placebo-controlled trial. JAMA. 1994 Dec 7;272(21):1661–5. [PubMed] [Google Scholar]
- 12.Gatwood J, Meltzer MI, Messonnier M, Ortega-Sanchez IR, Balkrishnan R, Prosser LA. Seasonal influenza vaccination of healthy working-age adults: a review of economic evaluations. Drugs. 2012 Jan 1;72(1):35–48. doi: 10.2165/11597310-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 13.Fireman B, Lee J, Lewis N, Bembom O, van der Laan M, Baxter R. Influenza vaccination and mortality: differentiating vaccine effects from bias. Am J Epidemiol. 2009 Sep 1;170(5):650–6. doi: 10.1093/aje/kwp173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fedson DS, Houck P, Bratzler D. Hospital-based influenza and pneumococcal vaccination: Sutton's law applied to prevention. Infect Control Hosp Epidemiol. 2000;21(11):692–699. doi: 10.1086/501716. [DOI] [PubMed] [Google Scholar]
- 15.Ohmit SE, Victor JC, Rotthoff JR, et al. Prevention of antigenically drifted influenza by inactivated and live attenuated vaccines. N Engl J Med. 2006;355(24):2513–22. doi: 10.1056/NEJMoa061850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Baguelin M, Jit M, Miller E, Edmunds WJ. Health and economic impact of the seasonal influenza vaccination programme in England. Vaccine. 2012 May 14;30(23):3459–62. doi: 10.1016/j.vaccine.2012.03.019. [DOI] [PubMed] [Google Scholar]
- 17.Williams WW. Managed care can improve pneumococcal and influenza vaccination levels. HMO Practice. 1997;2(4):174–175. [PubMed] [Google Scholar]
- 18.Fedson DS. Adult immunization: Summary of the National Vaccine Advisory Committee Report. JAMA. 1994;272(14):1133–1137. doi: 10.1001/jama.272.14.1133. [DOI] [PubMed] [Google Scholar]
- 19.Fiore AE, Shay DK, Broder K, Iskander JK, Uyeki TM, Mootrey G, et al. Prevention and control of influenza: recommendations of the Advisory Committee on Immunization Practices. MMWR. 2009;58(RR08):1–52. [PubMed] [Google Scholar]
- 20.Nichol KL. Ten-year durability and success of an organized program to increase influenza and pneumococcal vaccination rates among high-risk adults. Am J Med. 1998;105(5):385–392. doi: 10.1016/s0002-9343(98)00293-9. [DOI] [PubMed] [Google Scholar]
- 21.Egede LE, Zheng D. Racial/Ethnic differences in influenza vaccination coverage in high-risk adults. Am J Public Health. 2003;93(12):2074–2078. doi: 10.2105/ajph.93.12.2074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Singleton JA, Wortley PM, Lu PJ. Influenza vaccination of persons with cardiovascular disease in the United States. Texas Heart Institute Journal. 2004;31(1):1–6. [PMC free article] [PubMed] [Google Scholar]
- 23.Lu PJ, Singleton JA, Rangel MC, et al. Influenza vaccination trends among adults 65 years or older in the United States, 1989-2002. Arch Intern Med. 2005;165(16):1849–1856. doi: 10.1001/archinte.165.16.1849. [DOI] [PubMed] [Google Scholar]
- 24.Singleton JA, Santibanez TA, Wortley PM. Influenza and pneumococcal vaccination of adults aged ≥ 65: racial/ethnic differences. Am J Prev Med. 2005;29(5):412–20. doi: 10.1016/j.amepre.2005.08.012. [DOI] [PubMed] [Google Scholar]
- 25.Walker FJ, Singleton JA, Lu PJ, et al. Influenza vaccination of health care workers in the United States, 1989-2002. Infect Control Hosp Epidemiol. 2006;27(3):257–265. doi: 10.1086/501538. [DOI] [PubMed] [Google Scholar]
- 26.Lu PJ, Bridges CB, Euler GL, Singleton JA. Influenza vaccination of recommended adult populations, U.S., 1989-2005. Vaccine. 2008;26(14):1786–1793. doi: 10.1016/j.vaccine.2008.01.040. [DOI] [PubMed] [Google Scholar]
- 27.Ding H, Lu PJ, Euler GL, Furlow C, Bryan LN, Bardenheier B, et al. Interim Results: State-Specific Seasonal Influenza Vaccination Coverage --- United States, August 2009—January 2010. MMWR. 2010;59(16):477–484. [PubMed] [Google Scholar]
- 28.Centers for Disease Control and Prevention (CDC) National Center for Health Statistics, Centers for Disease Control and Prevention; Hyattsville, MD: [Accessed August 30, 2012]. 2011. National Health Interview Survey. Available at: ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Dataset_Documentation/NHIS/2010/srvydesc.pdf. [Google Scholar]
- 29.Centers for Disease Control and Prevention (CDC) Centers for Disease Control and Prevention; Atlanta, GA: [Accessed January 30, 2013]. 2011. Influenza vaccination coverage—FluVaxView. Available at: http://www.cdc.gov/flu/professionals/vaccination/vaccinecoverage.htm. [Google Scholar]
- 30.Ahluwalia IB, Jamieson DJ, D'Angelo DV, Singleton JA, Santibanez TA, Euler GL, et al. Seasonal influenza and 2009 H1N1 influenza vaccination coverage among pregnant women – 10 States, 2009—10 influenza season. MMWR. 2010;59(47):1541–5. [PubMed] [Google Scholar]
- 31.Ding H, Santibanez TA, Jamieson DJ, et al. Influenza vaccination coverage among pregnant women – National 2009 H1N1 Survey (NHFS) Am J Obstet Gynecol. 2011;204(6 Suppl 1):S96–106. doi: 10.1016/j.ajog.2011.03.003. [DOI] [PubMed] [Google Scholar]
- 32.Healthy People 2020. U.S. Department of Health and Human Services; Washington, DC: [Accessed May 16, 2013]. 2011. Topics & Objectives – Immunization and Infectious Diseases. http://www.healthypeople.gov/2020/topicsobjectives2020/objectiveslist.aspx?topicid=23. [Google Scholar]
- 33.Interim influenza vaccination recommendations, 2004--05 influenza season. MMWR. 2004;53(39):923–4. [PubMed] [Google Scholar]
- 34.Dao CN, Kamimoto L, Nowell M, Reingold A, Gershman K, Meek J, et al. Adult hospitalizations for laboratory-positive influenza during the 2005-2006 through 2007-2008 seasons in the United States. J Infect Dis. 2010 Sep 15;202(6):881–8. doi: 10.1086/655904. [DOI] [PubMed] [Google Scholar]
- 35.Gilca R, De Serres G, Boulianne N, Ouhoummane N, Papenburg J, Douville-Fradet M, et al. Risk factors for hospitalization and severe outcomes of 2009 pandemic H1N1 influenza in Quebec, Canada. Influenza Other Respi Viruses. 2011 Jul;5(4):247–55. doi: 10.1111/j.1750-2659.2011.00204.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kennedy ED, Santibanez TA, Bryan LN, Wortley PM, Euler GL, Singleton JA. Place of influenza vaccination among adults-United States, 2010-2011 influenza season. MMWR. 2011;60(23):781–785. [PubMed] [Google Scholar]
- 37.Nichol KL, MacDonald R, Hauge M. Factors associated with influenza and pneumococcal vaccination behavior among high-risk adults. J Gen Intern Med. 1996;11(11):673–677. doi: 10.1007/BF02600158. [DOI] [PubMed] [Google Scholar]
- 38.Use of influenza A (H1N1) 2009 monovalent vaccine: recommendations of the Advisory Committee on Immunization Practices (ACIP), 2009. MMWR. 2009;58(No. RR-10):1–8. [PubMed] [Google Scholar]
- 39.Salgado CD, Farr BM, Hall KK, et al. Influenza in the acute hospital setting. Lancet Infect Dis. 2002;2(3):145–155. doi: 10.1016/s1473-3099(02)00221-9. [DOI] [PubMed] [Google Scholar]
- 40.Hayward AC, Harling R, Wetten S, Johnson AM, Munro S, Smedley J, et al. Effectiveness of an influenza vaccine programme for care home staff to prevent death, morbidity, and health service use among residents: cluster randomised controlled trial. BMJ. 2006;333(7581):1241–1244. doi: 10.1136/bmj.39010.581354.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wilde JA, McMillan JA, Serwint J, Butta J, O'Riordan MA, Steinhoff MC. Effectiveness of influenza vaccine in health care professionals: a randomized trial. JAMA. 1999 Mar 10;281(10):908–13. doi: 10.1001/jama.281.10.908. [DOI] [PubMed] [Google Scholar]
- 42.Shefer AM, Atkinson W, Friedman C, Kuhar DT, Mootrey G, Bialek SR, et al. Immunization of health-care personnel: recommendations of the Advisory Committee on Immunization Practices (ACIP) MMWR Recomm Rep. 2011 Nov 25;60(RR-7):1–45. [PubMed] [Google Scholar]
- 43.Poland GA, Shefer AM, McCauley M, Webster PS, Whitley-Williams PN, Peter G. Standards for adult immunization practices. Am J Prev Med. 2003;25(2):144–150. doi: 10.1016/s0749-3797(03)00120-x. [DOI] [PubMed] [Google Scholar]
- 44.Harris K, Maurer J, Black C, Euler G, Kadiyala S. Workplace efforts to promote influenza vaccination among healthcare personnel and their association with uptake during the 2009 pandemic influenza A (H1N1) Vaccine. 2011 Apr 5;29(16):2978–2985. doi: 10.1016/j.vaccine.2011.01.112. [DOI] [PubMed] [Google Scholar]
- 45.Pleis JR, Gentleman JF. Using the National Health Interview Survey: time trends in influenza vaccinations among targeted adults. Eff Clin Pract. 2002 May-Jun;5(3 Suppl):E3. [PubMed] [Google Scholar]
- 46.Lindley MC, Wortley PM, Winston CA, Bardenheier BH. The role of attitudes in understanding disparities in adult influenza vaccination. Am J Prev Med. 2006;31(4):281–5. doi: 10.1016/j.amepre.2006.06.025. [DOI] [PubMed] [Google Scholar]
- 47.Link MW, Ahluwalia IB, Euler GL, et al. Racial and ethnic disparities in influenza vaccination coverage among adults during the 2004–2005 season. Am J Epidemiol. 2006;163(6):571–8. doi: 10.1093/aje/kwj086. [DOI] [PubMed] [Google Scholar]
- 48.Bach PB, Pham HH, Schrag D, Tate RC, Hargraves JL. Primary care physicians who treat blacks and whites. N Engl J Med. 2004;351(6):575–84. doi: 10.1056/NEJMsa040609. [DOI] [PubMed] [Google Scholar]
- 49.Schneider EC, Zaslavsky AM, Epstein AM. Racial disparities in the quality of care for enrollees in medicare managed care. JAMA. 2002;287(10):1288–94. doi: 10.1001/jama.287.10.1288. [DOI] [PubMed] [Google Scholar]
- 50.Gemson DH, Elinson J, Messeri P. Differences in physician prevention practice patterns for white and minority patients. J Community Health. 1988;13(1):53–64. doi: 10.1007/BF01321480. [DOI] [PubMed] [Google Scholar]
- 51.Fiscella K. Anatomy of racial disparity in influenza vaccination. Health Serv Res. 2005;40(2):539–50. doi: 10.1111/j.1475-6773.2005.00371.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Task Force on Community Prevention Services The guide to community preventive services. New York, NY: Oxford University Press; 2005. [Google Scholar]
- 53.Lu PJ, Callahan DB, Ding H, Euler GL. Influenza A (H1N1) 2009 monovalent vaccination among adults aged 25-64 years with asthma--United States, 2010. Am J Prev Med. 2011;41(6):619–626. doi: 10.1016/j.amepre.2011.08.004. [DOI] [PubMed] [Google Scholar]
- 54.BRFSS Summary Data Quality Report. Atlanta, Georgia: U.S. Department of Health and Human Services, CDC; [Accessed October 22, 2012]. 2011. Centers for Disease Control and Prevention (CDC) Available at: http://www.cdc.gov/brfss/data_documentation.htm. [Google Scholar]
- 55.Hu SS, Balluz L, Battaglia MP, Frankel MR. Improving public health surveillance using a dual-frame survey of landline and cell phone numbers. Am J Epidemiol. 2011 Mar 15;173(6):703–11. doi: 10.1093/aje/kwq442. [DOI] [PubMed] [Google Scholar]
- 56.Donald RM, Baken L, Nelson A, Nichol KL. Validation of self-report of influenza and pneumococcal vaccination status in elderly outpatients. Am J Prev Med. 1999;16(3):173–177. doi: 10.1016/s0749-3797(98)00159-7. [DOI] [PubMed] [Google Scholar]
- 57.Zimmerman RK, Raymund M, Janosky JE, Nowalk MP, Fine MJ. Sensitivity and specificity of patient self-report of influenza and pneumococcal polysaccharide vaccinations among elderly outpatients in diverse patient care strata. Vaccine. 2003;21(13-14):1486–1491. doi: 10.1016/s0264-410x(02)00700-4. [DOI] [PubMed] [Google Scholar]
- 58.Mangtani P, Shah A, Roberts JA. Validation of influenza and pneumococcal vaccine status in adults based on self-report. Epidemiol Infect. 2007 Jan;135(1):139–43. doi: 10.1017/S0950268806006479. [DOI] [PMC free article] [PubMed] [Google Scholar]


