This study uses data from the US Nationwide Inpatient Sample to examine the association between regional hospital market concentration and hospital charges in a population of patients undergoing hepatopancreaticobiliary surgical procedures.
Key Points
Question
What is the association between measures of overall hospital market concentration and estimated costs and charges of hepatopancreaticobiliary surgery?
Findings
In this study of 90 995 patients identified in the Nationwide Inpatient Sample from 2003 to 2011, costs of pancreatic resections were 5.5% higher in unconcentrated hospital markets relative to moderately concentrated markets, although overall charges were 8.3% lower in highly concentrated markets. For hepatic resections, hospitals in highly concentrated markets had 8.4% lower costs compared with those in unconcentrated markets and charges that were 13.4% and 10.5% lower compared with moderately and unconcentrated markets, respectively.
Meaning
Higher market concentration may represent the best value proposition for highly complex hepatopancreatic surgery: better quality of care with lower costs.
Abstract
Importance
Trade-offs involved with market competition, overall costs to payers and consumers, and quality of care have not been well defined. Less competition within any given market may enable provider-driven increases in charges.
Objective
To examine the association between regional hospital market concentration and hospital charges for hepatopancreaticobiliary surgical procedures.
Design, Setting, and Participants
This study included all patients undergoing hepatic or pancreatic resection in the Nationwide Inpatient Sample from January 1, 2003, through December 31, 2011. Hospital market concentration was assessed using a variable-radius Herfindahl-Hirschman Index (HHI) in the 2003, 2006, and 2009 Hospital Market Structure files. Data were analyzed from November 19, 2016, through March 2, 2017.
Interventions
Hepatic or pancreatic resection.
Main Outcomes and Measures
Multivariable mixed-effects log-linear models were constructed to determine the association between HHI and total costs and charges for hepatic or pancreatic resection.
Results
Weighted totals of 38 711 patients undergoing pancreatic resection (50.8% men and 49.2% women; median age, 65 years [interquartile range, 55-73 years]) and 52 284 patients undergoing hepatic resection (46.8% men and 53.2% women; median age, 59 years [interquartile range, 49-69 years]) were identified. Higher institutional volume was associated with lower cost of pancreatic resection (−5.4%; 95% CI, −10.0% to −0.5%; P = .03) and higher cost of hepatic resection (13.4%; 95% CI, 8.2% to 18.8%; P < .001). For pancreatic resections, costs were 5.5% higher (95% CI, 0.1% to 11.1%; P = .047) in unconcentrated hospital markets relative to moderately concentrated markets, although overall charges were 8.3% lower (95% CI, −14.0% to −2.3%; P = .008) in highly concentrated markets. For hepatic resections, hospitals in highly concentrated markets had 8.4% lower costs (95% CI, −13.0% to −3.6%; P = .001) compared with those in unconcentrated markets and charges that were 13.4% lower (95% CI, −19.3% to −7.1%; P < .001) compared with moderately concentrated markets and 10.5% lower (95% CI, −16.2% to −4.4%; P = .001) compared with unconcentrated markets.
Conclusions and Relevance
Higher market concentration was associated with lower overall charges and lower costs of pancreatic and hepatic surgery. For complex, highly specialized procedures, hospital market consolidation may represent the best value proposition: better quality of care with lower costs.
Introduction
The association of hospital and surgeon volume with perioperative outcomes has provided the impetus for increased regionalization of surgical care. To this end, many policy researchers have argued that consolidating health systems enables clinicians to coordinate patient care across disciplines. In addition, a higher volume of specific surgical procedures at regional centers has been associated with lower rates of complications and possibly lower overall costs. Other studies, however, have noted that greater competition among hospitals (and conversely, lower hospital market concentration) may lead to faster uptake of novel technologies. Because greater regionalization has been driven, in part, by a national trend toward increasing hospital system consolidation, the interplay between hospital market concentration and the quality and costs of care has not been fully characterized.
In particular, increasing consolidation and regionalization of hospital services may carry financial risks to patients. Specifically, less competition within any given market (ie, greater market concentration) may enable provider-driven increases in charges. Furthermore, greater concentration of specific services within a few hospital systems could even paradoxically result in lower overall quality, further disadvantaging patients. The association among regionalization, market concentration, and patient outcomes can be difficult to interpret because the relationships that hospitals or health systems have with different payers can vary substantially. For example, although hospitals accept Medicare prices (ie, rates are set administratively), they may negotiate with private insurers. As such, drawing broad conclusions regarding the precise trade-offs involved with market concentration, overall costs to payers and consumers, and quality of care can be difficult. To this point, several prior studies have noted marked variations in the levels of hospital cost-to-charge markup while controlling for quality of care and described broad geographic variations in hospital pricing across payers. In one study, Chang et al reported an association between increased hospital market concentration (ie, lower competition) and lower gross charges for common procedures, including bariatric surgery and appendectomy.
For highly specialized procedures, such as pancreaticoduodenectomy and hepatectomy, an emphasis on the volume-outcome association has driven overall improvements in morbidity and mortality during the past several decades. However, most studies to date have almost exclusively focused on the volume-outcome association relative to quality, whereas few if any studies have examined the broader influence of regionalization on costs. The influence of regionalization on procedure-related costs may be particularly important for high-risk, high-cost hepatopancreaticobiliary procedures. As such, the objective of the present study was to examine the association between regional hospital market concentration and hospital charges for hepatopancreaticobiliary surgical procedures using a nationally representative all-payer sample of inpatients.
Methods
Study Population
Patients 18 years and older who underwent elective pancreaticoduodenectomy, total pancreatectomy, partial hepatectomy, or hepatic lobectomy were identified from the Nationwide Inpatient Sample (NIS) from January 1, 2003, through December 31, 2011. Patients were identified using the respective codes from the International Classification of Diseases, Ninth Revision for these procedures (52.7, 52.6, 50.22, and 50.3). The NIS is a stratified random sample of hospitals represented in all state inpatient databases that represents approximately 20% of all hospital discharges in the United States. The NIS is maintained by the Agency for Healthcare Research and Quality and is publicly available, deidentified, and compliant with the Health Insurance Portability and Accountability Act of 1996. The study was approved by the institutional review board of Johns Hopkins University, which did not require informed consent for the use of these data.
Patient comorbidity at the time of surgery was classified using the Charlson Comorbidity Index (CCI) and calculated using a predefined algorithm. Inpatient complications were identified using a previously validated method for administrative data. Hospital length of stay and discharge disposition were dichotomized using previously defined categories. Hospital characteristics, including urban vs rural, region, teaching status, and bed size, were determined using the American Hospital Association Linkage Files provided by the Healthcare Cost and Utilization Project. Annual hospital procedure-specific volume was dichotomized at more than 11 procedures for pancreatic resections and more than 10 procedures for hepatic resections in accordance with previously published studies.
Hospital market concentration was determined using the data reported in the 2003, 2006, and 2009 Hospital Market Structure files, which are assembled by the Agency for Healthcare Research and Quality and linked via hospital identifiers to the NIS data. A hospital market was defined as previously described; to account for the fact that hospital markets can span across counties and other geographic divisions, we decided a priori to define a hospital market by a variable radius around a hospital from which 75% of its discharges were drawn. Hospital concentration within each market was defined by the Herfindahl-Hirschman Index (HHI), which was calculated by summing the squares of the fraction of discharges from each hospital in the market. The HHI is a validated and widely applied metric of market consolidation that indicates the degree to which any one entity (ie, hospital) possesses a disproportionate share. The smaller the HHI, the less concentrated (or more competitive) the market. An HHI greater than or equal to 0.25 was categorized as highly concentrated (ie, noncompetitive); an HHI of 0.15 to 0.25, moderately concentrated (or moderately competitive); and an HHI of less than 0.15, unconcentrated (or highly competitive). Because the dispersion of HHI across urban and rural hospitals varied markedly, the analytic cohort was restricted to urban hospitals only, which performed more than 95% of all estimated resections.
Because the NIS reports only total billed hospital charges for each inpatient stay, total hospital costs were estimated using cost-to-charge ratios published by the Healthcare Cost and Utilization Project. All financial variables were adjusted for inflation and reported in 2011 dollars using the US Department of Commerce Bureau of Economic Analysis gross domestic product implicit price deflator.
Statistical Analysis
Data were analyzed from November 19, 2016, through March 2, 2017. Continuous variables were examined as means and SDs or medians with interquartile range (IQR) and evaluated using an unpaired t test or nonparametric Kruskal-Wallis test. Categorical variables were compared using the Pearson χ2 test or Fisher exact test as appropriate. Frequency estimates across categories were obtained using sampling weights published by the NIS. Because reported and estimated financial data were highly right-skewed, total hospital costs and charges were log transformed before regression analysis. The association between total hospital costs and charges was evaluated using a multivariable mixed-effects log-linear model with a random intercept included for each hospital. Continuous variables were centered at the mean to preserve model interpretability. Separate independent models for pancreatic and hepatic resections were constructed. An interaction term between hospital volume and HHI category was evaluated but not included in the final model because it did not lead to improvements in model fit (assessed by Aikake information criteria and Bayesian information criteria). Design weights were rescaled to accommodate the hierarchical nature of the model and applied at the patient and hospital levels, as previously described for pooling data across multiple years of the NIS. Model predictions were exponentiated to obtain case-mix–adjusted estimates for total hospital cost and charges. All analyses were conducted using Stata software (version 14.0 MP; StataCorp). P < .05 was used to determine statistical significance.
Results
Patient and Hospital Characteristics
In the defined study period, a weighted total of 38 711 patients underwent a pancreatic resection (50.8% men and 49.2% women) and a weighted total of 52 284 patients underwent hepatic resection (46.8% men and 53.2% women). Among patients undergoing pancreatic resection, median age was 65 years (IQR, 55-73 years); among patients undergoing hepatic resection, 59 years (IQR, 49-69 years). The most common primary payer in both groups was Medicare (18 762 patients undergoing pancreatic resection [48.5%] and 18 249 patients undergoing hepatic resection [34.9%]). Overall, preoperative comorbidity was pronounced as most patients had a CCI greater than 2 (20 314 patients undergoing pancreatic resection [52.5%] and 36 518 patents undergoing hepatic resection [69.8%]). Median hospital length of stay was 11 days (IQR, 8-16 days) for pancreatic resection and 6 days (IQR, 5-8 days) for hepatic resection (Table 1).
Table 1. Demographic and Clinical Characteristics of Patients in the 2003-2011 NIS Undergoing Pancreatic Resection and Hepatic Resectiona.
| Characteristic | Surgical Group by Hospital Market Concentration | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pancreatic Resection | Hepatic Resection | |||||||||
| Unconcentrated (n = 26 407) |
Moderate (n = 5297) |
High (n = 7007) |
Total (N = 38 711) |
P Value | Unconcentrated (n = 38 624) |
Moderate (n = 6007) |
High (n = 7653) |
Total (N = 52 284) |
P Value | |
| Sex | ||||||||||
| Male | 13 352 (67.9) | 2637 (13.4) | 3673 (18.7) | 19 662 | .46 | 18 202 (74.3) | 2803 (11.4) | 3488 (14.2) | 24 493 | .65 |
| Female | 13 055 (68.5) | 2661 (14.0) | 3334 (17.5) | 19 049 | 20 421 (73.5) | 3204 (11.5) | 4165 (15.0) | 27 790 | ||
| Age, median (IQR), y | 64 (55-72) | 65 (55-72) | 67 (58-74) | 65 (55-73) | NA | 58 (48-68) | 60 (52-69) | 62 (51-72) | 59 (49-69) | NA |
| CCI | ||||||||||
| 0 | 4462 (73.0) | 856 (14.0) | 797 (13.0) | 6115 | .054 | 6558 (77.0) | 851 (10.0) | 1104 (13) | 8513 | .09 |
| 1 | 1862 (66.1) | 439 (15.6) | 514 (18.3) | 2815 | 1305 (70.3) | 250 (13.5) | 301 (16.2) | 1857 | ||
| 2 | 6416 (67.8) | 1283 (13.6) | 1767 (18.7) | 9466 | 3988 (73.9) | 713 (13.2) | 696 (12.9) | 5397 | ||
| ≥3 | 13 666 (67.3) | 2719 (13.4) | 3929 (19.3) | 20 314 | 26 773 (73.3) | 4193 (11.5) | 5552 (15.2) | 36 518 | ||
| Procedure type | ||||||||||
| Total pancreatectomy | 2274 (68.4) | 507 (15.2) | 545 (16.4) | 3326 | .74 | NA | NA | NA | NA | NA |
| Pancreaticoduodenectomy | 24 133 (68.2) | 4790 (13.5) | 6462 (18.3) | 35 385 | NA | NA | NA | NA | NA | |
| Lobectomy | NA | NA | NA | NA | NA | 12 708 (75.9) | 1897 (11.3) | 2143 (12.8) | 16 748 | .15 |
| Partial hepatectomy | NA | NA | NA | NA | NA | 25 916 (72.9) | 4110 (11.6) | 5509 (15.5) | 35 536 | |
| No. of in-hospital complications | ||||||||||
| 0 | 16 491 (68.8) | 3209 (13.4) | 4263 (17.8) | 23 963 | .07 | 29 522 (74.8) | 4472 (11.3) | 5493 (13.9) | 39 488 | .05 |
| 1 | 8224 (68.7) | 1600 (13.4) | 2150 (18) | 11 975 | 8052 (71.3) | 1344 (11.9) | 1901 (16.8) | 11 296 | ||
| ≥2 | 1691 (61.0) | 488 (17.6) | 594 (21.4) | 2773 | 1049 (70.0) | 191 (12.7) | 259 (17.3) | 1499 | ||
| Length of stay, median (IQR), d | 10 (8-15) | 12 (9-18) | 12 (9-18) | 11 (8-16) | NA | 6 (5-8) | 6 (5-8) | 6 (5-9) | 6 (5-8) | NA |
| Primary payer | ||||||||||
| Medicare | 12 344 (65.8) | 2567 (13.7) | 3851 (20.5) | 18 762 | .01 | 12 715 (69.7) | 2172 (11.9) | 3362 (18.4) | 18 249 | <.001 |
| Medicaid | 1206 (67.7) | 287 (16.1) | 288 (16.2) | 1781 | 2174 (74.0) | 400 (13.6) | 363 (12.4) | 2937 | ||
| Private | 11 445 (70.8) | 2195 (13.6) | 2524 (15.6) | 16 163 | 21 615 (76.2) | 3170 (11.2) | 3579 (12.6) | 28 365 | ||
| Uninsured | 585 (67.6) | 124 (14.3) | 157 (18.2) | 865 | 922 (82.5) | 86 (7.7) | 111 (9.9) | 1118 | ||
| Other | 827 (72.6) | 125 (11.0) | 188 (16.5) | 1139 | 1198 (74.2) | 179 (11.1) | 238 (14.7) | 1615 | ||
| Quartile of household income | ||||||||||
| First | 5051 (66.4) | 1111 (14.6) | 1440 (18.9) | 7602 | .26 | 7177 (72.3) | 1352 (13.6) | 1392 (14) | 9921 | .006 |
| Second | 6002 (65.3) | 1319 (14.4) | 1865 (20.3) | 9186 | 8582 (71.4) | 1261 (10.5) | 2174 (18.1) | 12 017 | ||
| Third | 7241 (68.6) | 1337 (12.7) | 1972 (18.7) | 10 550 | 10 474 (73.3) | 1510 (10.6) | 2314 (16.2) | 14 298 | ||
| Fourth | 8112 (71.3) | 1530 (13.5) | 1730 (15.2) | 11 373 | 12 390 (77.2) | 1884 (11.7) | 1772 (11.0) | 16 047 | ||
| Discharge disposition | ||||||||||
| Routine | 14 522 (72.8) | 2551 (12.8) | 2879 (14.4) | 19 952 | <.001 | 31 423 (75.6) | 4669 (11.2) | 5484 (13.2) | 41 577 | <.001 |
| Transferred | 2830 (58.1) | 687 (14.1) | 1353 (27.8) | 4871 | 1489 (57.0) | 363 (13.9) | 761 (29.1) | 2613 | ||
| Home health care | 8352 (67.0) | 1759 (14.1) | 2354 (18.9) | 12 465 | 5058 (71.1) | 837 (11.8) | 1223 (17.2) | 7118 | ||
| Died | 693 (50.2) | 286 (20.7) | 401 (29.1) | 1380 | 645 (67) | 133 (13.8) | 185 (19.2) | 962 | ||
| Other | 4 (13.3) | 5 (16.7) | 20 (66.7) | 30 | 9 (64.3) | 5 (35.7) | 0 | 14 | ||
Abbreviations: CCI, Charlson Comorbidity Index; IQR, interquartile range; NA, not applicable; NIS, Nationwide Inpatient Sample.
Unless otherwise indicated, data are expressed as weighted number (percentage) of row totals for each surgical group. Estimated counts were rounded to the nearest unit, and thus, totals across categories may differ from the calculated sums. P values were calculated using an unpaired t test or nonparametric Kruskal-Wallis test for continuous variables and the Pearson χ2 test or Fisher exact test for categorical variables.
Most patients (31 065 [80.2%] for pancreatic resection; 40 354 [77.2%] for hepatic resection) underwent a resection in a hospital in the largest bed size category (ie, >200 beds for nonteaching hospitals and >500 beds for teaching hospitals). A comparable proportion of patients underwent a resection in a teaching hospital (32 751 [84.6%] for pancreatic resection; 44 998 [86.1%] for hepatic resection) and in a high-volume center (27 450 [70.9%] for pancreatic resection; 41 673 [79.7%] for hepatic resection). Among patients who underwent a pancreatic resection at a high-volume center, most procedures were at a center in an unconcentrated market (22 802 [83.1%]). Among patients who underwent a pancreatic resection at a low-volume center, many of these procedures were performed at a center in a highly concentrated market (4739 [42.1%]). A similar pattern was also observed among patients undergoing hepatic resection, with 34 999 resections (84.0%) at a high-volume center in unconcentrated markets and 4475 resections (42.2%) at a low-volume center in highly concentrated markets.
Inpatient Costs and Charges
The overall unadjusted median charge for a pancreatic resection was $90 989 (IQR, $63 785-$147 517), whereas the total median unadjusted cost was $31 033 (IQR, $22 995-$45 636). Overall median inpatient charges and costs for hepatic resection were $60 394 (IQR, $40 965-$94 139) and $20 734 (IQR, $14 908-$29 699), respectively.
When hospitals were stratified by market concentration, median unadjusted charges for pancreatic resection ranged from $85 886 (IQR, $59 550-$149 160) in highly concentrated markets to $101 580 (IQR, $69 272-$162 866) in moderately concentrated markets. Overall median unadjusted costs for patients undergoing pancreatic resection varied slightly less, from $29 902 (IQR, $22 068-$45 195) in highly concentrated markets to $32 463 (IQR, $23 254-$46 579) in moderately concentrated markets.
Unadjusted charges for hepatic resection varied similarly across these strata, with median charges ranging from $51 942 (IQR, $34 895-$81 285) in highly concentrated markets to $62 439 (IQR, $43 113-$97 890) in unconcentrated markets. Median costs ranged from $17 938 (IQR, $13 024-$26 076) in moderately concentrated markets to $21 651 (IQR, $15 870-$30 563) in unconcentrated markets (Table 2).
Table 2. Characteristics of Hospitals in the 2003-2011 NIS Performing Pancreatic Resections and Hepatic Resectionsa.
| Characteristic | Surgical Group by Hospital Market Concentration | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Pancreatic Resection | Hepatic Resection | ||||||||||
| Unconcentrated (n = 26 407) |
Moderate (n = 5297) |
High (n = 7007) |
Total (N = 38 711) |
P Value | Unconcentrated (n = 38 624) |
Moderate (n = 6007) |
High (n = 7653) |
Total (N = 52 284) |
P Value | ||
| Hospital region | |||||||||||
| Northeast | 1780 (60) | 247 (8.3) | 942 (31.7) | 2969 | .11 | 1923 (51.7) | 503 (13.5) | 1293 (34.8) | 3719 | .005 | |
| Midwest | 7423 (72.4) | 936 (9.1) | 1894 (18.5) | 10 252 | 10 921 (78.7) | 1012 (7.3) | 1944 (14.0) | 13 877 | |||
| South | 9188 (62.8) | 2535 (17.3) | 2917 (19.9) | 14 639 | 12 851 (68.5) | 2953 (15.7) | 2962 (15.8) | 18 766 | |||
| West | 8016 (73.9) | 1580 (14.6) | 1254 (11.6) | 10 851 | 12 928 (81.2) | 1539 (9.7) | 1454 (9.1) | 15 921 | |||
| Hospital volume | |||||||||||
| Low | 3605 (32) | 2917 (25.9) | 4739 (42.1) | 11 261 | <.001 | 3625 (34.2) | 2511 (23.7) | 4475 (42.2) | 10611 | <.001 | |
| High | 22 802 (83.1) | 2380 (8.7) | 2268 (8.3) | 27 450 | 34 999 (84.0) | 3497 (8.4) | 3177 (7.6) | 41673 | |||
| Hospital bed size | |||||||||||
| Small | 1648 (68.9) | 324 (13.6) | 419 (17.5) | 2391 | .007 | 3194 (73.9) | 523 (12.1) | 605 (14.0) | 4322 | .06 | |
| Medium | 2647 (50.4) | 973 (18.5) | 1635 (31.1) | 5254 | 4618 (60.7) | 1188 (15.6) | 1802 (23.7) | 7608 | |||
| Large | 22 111 (71.2) | 4000 (12.9) | 4954 (15.9) | 31 065 | 30 812 (76.4) | 4296 (10.6) | 5246 (13) | 40 354 | |||
| Teaching status | |||||||||||
| Nonteaching | 1705 (28.6) | 1167 (19.6) | 3088 (51.8) | 5960 | <.001 | 3126 (42.9) | 1122 (15.4) | 3037 (41.7) | 7286 | <.001 | |
| Teaching | 24 702 (75.4) | 4130 (12.6) | 3920 (12.0) | 32 751 | 35 498 (78.9) | 4885 (10.9) | 4615 (10.3) | 44 998 | |||
| Total hospital costs, median (IQR), $ | 30 998 (23 250-45 533) |
32 463 (23 254-46 579) |
29 902 (22 068-45 195) |
31 033 (22 995-45 636) |
NA | 21 651 (15 870-30 563) |
17 938 (13 024-26 076) |
17 959 (12 575-27 183) |
20 734 (14 908-29 699) |
NA | |
| Total hospital charges, median (IQR), $ | 89 919 (64 518-144 465) |
101 580 (69 272-162 866) |
85 886 (59 550-149 160) |
90 989 (63 785-147 517) |
NA | 62 439 (43 113-97 890) |
55 219 (37 288-87 036) |
51 942 (34 895-81 285) |
60 394 (40 965-94 139) |
NA | |
Abbreviations: IQR, interquartile range; NA, not applicable; NIS, Nationwide Inpatient Sample.
Unless otherwise indicated, data are expressed as weighted number (percentage) of row totals for each surgical group. Estimated counts were rounded to the nearest unit, and thus, totals across categories may differ from the calculated sums. P values are calculated using an unpaired t test or nonparametric Kruskal-Wallis test for continuous variables and the Pearson χ2 test or Fisher exact test for categorical variables.
Several patient-level factors were associated with variation in costs and charges. Specifically, a CCI greater than 2 was associated with 4.6% higher costs (95% CI, 2.2%-7.1%; P < .001) and 4.7% higher charges (95% CI, 2.3%-7.3%; P < .001) for patients undergoing pancreatic resection and with 14.7% higher costs (95% CI, 12.3%-17.2%; P < .001) and 14.1% higher charges (95% CI, 11.7%-16.6%; P < .001) for patients undergoing hepatic resection (reference, CCI = 0). A nonroutine discharge disposition was uniformly associated with higher costs and charges for pancreatic and hepatic resection (all P < .05), as was an extended length of stay (P < .001) (Table 3). For pancreatic resection, private insurance was associated with slightly lower costs (−2.8%; 95% CI, −4.7% to −0.9%; P = .004) and lower charges (−2.7%; 95% CI, −4.6% to −0.8%; P = .006) compared with Medicare. In contrast, for hepatic resection, lack of insurance was associated with slightly higher costs (6.8%; 95% CI, 1.8%-12.0%; P = .007) and higher charges (6.7%; 95% CI, 1.7%-11.9%; P = .008) compared with Medicare. Compared with a nonextended length of stay, an extended length of stay was also associated with a nearly 2-fold increase in costs (204.4%; 95% CI, 198.7%-210.2%; P < .001) and charges (204.3%; 95% CI, 198.5%-210.2%; P < .001) among patients undergoing pancreatic resection and in costs (193.5%; 95% CI, 188.7%-198.4%; P < .001) and charges (193.1%; 95% CI, 188.2%-198.0%; P < .001) among patients undergoing hepatic resection.
Table 3. Results of Multivariable Mixed-Effects Log-Linear Models of Total Hospital Costs and Charges for Inpatient Care of Patients Undergoing Pancreatic Resection and Hepatic Resection.
| Factor | Surgical Group | |||||||
|---|---|---|---|---|---|---|---|---|
| Pancreatic Resection | Hepatic Resection | |||||||
| Proportional Change in Costs (95% CI) | P Valuea | Proportional Change in Charges (95% CI) | P Valuea | Proportional Change in Costs (95% CI) | P Valuea | Proportional Change in Charges (95% CI) | P Valuea | |
| Sex | ||||||||
| Male | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA |
| Female | 0.954 (0.940-0.969) | <.001 | 0.954 (0.940-0.969) | <.001 | 0.941 (0.928-0.955) | <.001 | 0.941 (0.927-0.954) | <.001 |
| Age, y | 0.998 (0.997-0.999) | <.001 | 0.998 (0.997-0.999) | <.001 | 0.998 (0.998-0.999) | <.001 | 0.998 (0.998-0.999) | <.001 |
| CCI | ||||||||
| 0 | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA |
| 1 | 1.034 (1.006-1.063) | .02 | 1.036 (1.007-1.065) | .02 | 0.995 (0.956-1.035) | .79 | 0.990 (0.952-1.031) | .64 |
| 2 | 1.013 (0.989-1.038) | .28 | 1.017 (0.993-1.042) | .17 | 1.129 (1.100-1.159) | <.001 | 1.123 (1.094-1.153) | <.001 |
| ≥3 | 1.046 (1.022-1.071) | <.001 | 1.047 (1.023-1.073) | <.001 | 1.147 (1.123-1.172) | <.001 | 1.141 (1.117-1.166) | <.001 |
| Total pancreatectomy | 1 [Reference] | NA | 1 [Reference] | NA | NA | NA | NA | NA |
| Pancreaticoduodenectomy | 0.93 (0.880-0.984) | .01 | 0.929 (0.877-0.983) | .01 | NA | NA | NA | NA |
| Lobectomy | NA | NA | NA | NA | 1 [Reference] | NA | 1 [Reference] | NA |
| Partial hepatectomy | NA | NA | NA | NA | 0.872 (0.858-0.886) | <.001 | 0.873 (0.860-0.887) | <.001 |
| No. of in-hospital complications | ||||||||
| 0 | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA |
| 1 | 1.107 (1.089-1.126) | <.001 | 1.106 (1.087-1.124) | <.001 | 1.120 (1.101-1.141) | <.001 | 1.118 (1.098-1.139) | <.001 |
| ≥2 | 1.425 (1.373-1.480) | <.001 | 1.426 (1.373-1.482) | <.001 | 1.446 (1.375-1.521) | <.001 | 1.442 (1.370-1.517) | <.001 |
| Length of stay | ||||||||
| Nonextended | 1 [Reference] | 1 [Reference] | 1 [Reference] | 1 [Reference] | ||||
| Extended | 2.044 (1.987-2.102) | <.001 | 2.043 (1.985-2.102) | <.001 | 1.935 (1.887-1.984) | <.001 | 1.931 (1.882-1.980) | <.001 |
| Primary payer | ||||||||
| Medicare | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA |
| Medicaid | 0.993 (0.955-1.032) | .72 | 0.982 (0.944-1.021) | .36 | 1.023 (0.991-1.057) | .16 | 1.021 (0.989-1.054) | .21 |
| Private | 0.972 (0.953-0.991) | .004 | 0.973 (0.954-0.992) | .006 | 1.004 (0.988-1.021) | .64 | 1.004 (0.988-1.021) | .60 |
| Uninsured | 0.966 (0.919-1.016) | .18 | 0.971 (0.922-1.022) | .26 | 1.068 (1.018-1.120) | .007 | 1.067 (1.017-1.119) | .008 |
| Other | 1.078 (1.014-1.146) | .02 | 1.068 (1.002-1.137) | .04 | 1.106 (1.045-1.171) | .001 | 1.103 (1.041-1.169) | .001 |
| Discharge disposition | ||||||||
| Routine | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA |
| Transferred | 1.279 (1.244-1.314) | <.001 | 1.287 (1.252-1.324) | <.001 | 1.283 (1.237-1.330) | <.001 | 1.286 (1.240-1.335) | <.001 |
| Home health care | 1.129 (1.108-1.151) | <.001 | 1.133 (1.111-1.156) | <.001 | 1.166 (1.142-1.191) | <.001 | 1.169 (1.144-1.193) | <.001 |
| Died | 1.557 (1.469-1.651) | <.001 | 1.564 (1.474-1.659) | <.001 | 1.854 (1.725-1.992) | <.001 | 1.866 (1.735-2.007) | <.001 |
| Other | 1.130 (0.871-1.465) | .36 | 1.195 (0.906-1.577) | .21 | 1.708 (1.072-2.720) | .02 | 1.778 (1.079-2.932) | .02 |
| Quartile of household income | ||||||||
| First | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA |
| Second | 1.000 (0.977-1.023) | .97 | 0.996 (0.973-1.019) | .73 | 0.991 (0.971-1.011) | .37 | 0.990 (0.970-1.010) | .32 |
| Third | 0.990 (0.966-1.015) | .44 | 0.983 (0.958-1.008) | .18 | 0.998 (0.977-1.019) | .84 | 0.994 (0.974-1.015) | .58 |
| Fourth | 1.007 (0.985-1.030) | .55 | 1.000 (0.978-1.023) | .97 | 0.987 (0.966-1.007) | .21 | 0.984 (0.964-1.005) | .13 |
| Hospital region | ||||||||
| Northeast | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA |
| Midwest | 1.015 (0.944-1.090) | .69 | 0.936 (0.838-1.046) | .24 | 0.991 (0.916-1.073) | .82 | 0.895 (0.810-0.989) | .03 |
| South | 0.944 (0.878-1.015) | .12 | 0.928 (0.830-1.036) | .18 | 0.939 (0.868-1.016) | .12 | 0.895 (0.810-0.989) | .03 |
| West | 1.242 (1.148-1.345) | <.001 | 1.372 (1.221-1.541) | <.001 | 1.178 (1.085-1.279) | <.001 | 1.300 (1.169-1.446) | <.001 |
| Hospital teaching status | ||||||||
| Nonteaching | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA |
| Teaching | 1.023 (0.972-1.078) | .39 | 0.958 (0.898-1.022) | .19 | 1.062 (1.010-1.117) | .02 | 1.016 (0.954-1.082) | .62 |
| Hospital bed size | ||||||||
| Small | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA |
| Medium | 0.961 (0.884-1.044) | .34 | 1.089 (0.980-1.210) | .11 | 0.960 (0.888-1.038) | .31 | 1.033 (0.934-1.142) | .53 |
| Large | 0.947 (0.875-1.024) | .17 | 1.136 (1.029-1.254) | .01 | 0.938 (0.874-1.007) | .08 | 1.083 (0.991-1.183) | .08 |
| Year (centered) | 1.010 (1.002-1.018) | .01 | 1.041 (1.030-1.052) | <.001 | 1.022 (1.014-1.030) | <.001 | 1.056 (1.045-1.067) | <.001 |
| Hospital market concentration | ||||||||
| Unconcentrated | 1.055 (1.001-1.111) | .047 | 0.965 (0.899-1.035) | .32 | 1.051 (0.996-1.109) | .07 | 0.967 (0.899-1.041) | .37 |
| Moderate | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA |
| High | 1.016 (0.967-1.067) | .53 | 0.917 (0.860-0.977) | .008 | 0.963 (0.913-1.015) | .16 | 0.866 (0.807-0.929) | <.001 |
| Hospital volume | ||||||||
| Low | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA |
| High | 0.946 (0.900-0.995) | .03 | 0.955 (0.889-1.026) | .21 | 1.134 (1.082-1.188) | <.001 | 1.070 (1.002-1.142) | .04 |
| Intraclass correlation | 0.417 (0.380-0.456) | NA | 0.613 (0.582-0.642) | NA | 0.387 (0.350-0.425) | NA | 0.590 (0.559-0.620) | NA |
Abbreviations: CCI, Charlson Comorbidity Index; NA, not applicable.
Calculated using 2-tailed tests.
For pancreatic resection, a higher institutional volume was associated with a 5.4% lower cost (95% CI, −10.0% to −0.5%; P = .03). In contrast, for hepatic resection, higher institutional volume was associated with 13.4% higher costs (95% CI, 8.2%-18.8%; P < .001) and 7.0% higher charges (95% CI, 0.2%-14.2%; P = .04). Of note, median household income quartile and hospital bed size were not associated with variation in costs for pancreatectomy or hepatectomy (Table 3).
For each hospital, unadjusted means and SEs of overall costs and charges were plotted according to procedure type (eFigures 1 and 2 in the Supplement). The HHI group corresponding to moderate hospital market concentration was initially used as a reference to assess the impact of more or less market concentration on costs and charges. An unconcentrated hospital market was associated with a 5.5% higher cost of pancreatic resection (95% CI, 0.1%-11.1%; P = .047); however, highly concentrated hospital markets had overall 8.3% lower charges (95% CI, −14.0% to −2.3%; P = .008) than those in less concentrated markets (Table 3). For hepatic resection, hospitals in highly concentrated markets had 8.4% lower costs (95% CI, −13.0% to −3.6%; P = .001) than those in unconcentrated markets. In addition, hospitals in highly concentrated markets also had 13.4% lower charges than those in moderately concentrated markets (95% CI, −19.3% to −7.1%; P < .001) (Table 3) and 10.5% lower charges (95% CI, −16.2% to −4.4%; P = .001) than those in unconcentrated markets.
In subanalyses examining the interaction between hospital volume and hospital market concentration, a 15.8% lower adjusted charge (95% CI, −25.7% to −5.6%; P = .007) and an 11.6% lower adjusted cost (95% CI, −18.4% to −4.2%; P = .003) were associated with highly concentrated markets compared with unconcentrated markets for pancreatic resection in high-volume centers. Similar trends were observed for hepatic resection in high-volume centers, with highly concentrated hospital markets associated with 22.7% lower adjusted charges (95% CI, −31.1% to −13.1%; P < .001) and 9.1% lower adjusted costs (95% CI, −16.8% to −0.7%; P = .04) compared with unconcentrated markets.
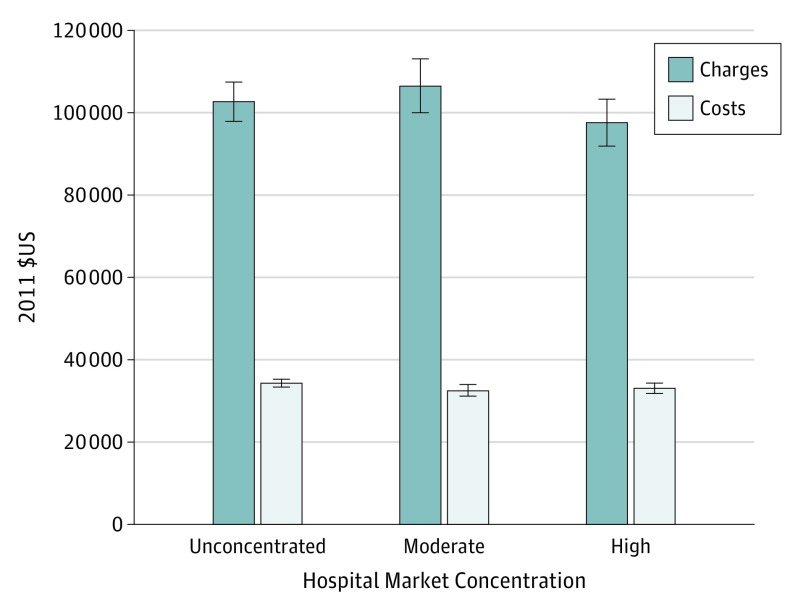
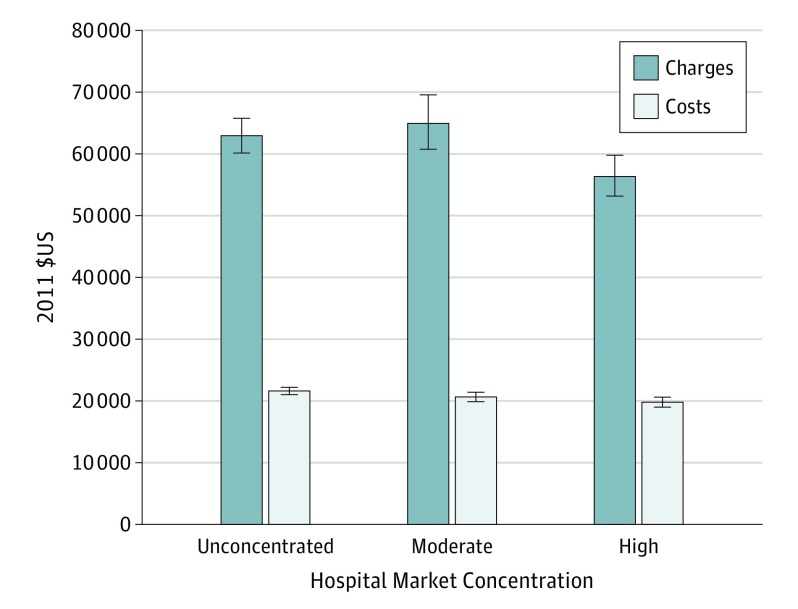
After adjustment, total hospital charges for patients undergoing pancreatic resection varied from $96 844 (95% CI, $91 257-$102 755) in highly concentrated markets to $105 660 (95% CI, $99 257-$112 477) in moderately concentrated markets (Figure 1). Similarly, total hospital charges for hepatic resection ranged from $55 982 (95% CI, $52 756-$59 405) in highly concentrated markets to $64 647 (95% CI, $60 445-$69 140) in moderately concentrated markets (Figure 2). Of the total variation in hospital costs and charges for pancreatic and hepatic resection, 38% to 61% was accounted for by within-hospital variation (Table 3).
Figure 1. Adjusted Total Charges and Costs of Pancreatic Resection by Herfindahl-Hirschman Index (HHI) Category.
The HHI was calculated by summing the squares of the fraction of all discharges from each hospital within a market. Error bars indicate 95% CIs.
Figure 2. Adjusted Total Charges and Costs of Hepatic Resection by Herfindahl-Hirschman Index (HHI) Category.
The HHI was calculated by summing the squares of the fraction of all discharges from each hospital within a market. Error bars indicate 95% CIs.
Discussion
Greater hospital surgical volume has been associated with improved outcomes, including lower mortality, fewer complications, and even improved survival among patients with cancer. Critics of consolidation in the health care system have argued, however, that diminished competition creates a seller’s market that can enable hospitals to set prices, leaving patients with fewer and fewer options for receiving care. To date, few reports have specifically examined whether increasing hospital market concentration at high-volume centers (thereby reducing interhospital competition) is associated with adverse financial implications for patients and payers. As such, the goal of the present study was to define the association between hospital market concentration and total inpatient costs and charges for pancreatic and hepatic operations. Using 9 years of the Healthcare Cost and Utilization Project’s NIS in conjunction with the Hospital Market Structure files, a multivariable mixed-effects log-linear model was constructed adjusting for patient- and hospital-level factors. The data demonstrated that overall charges ranged from 10.5% to 13.4% lower in highly concentrated markets compared with charges in an unconcentrated or moderately concentrated hospital market. Specifically, among patients undergoing a pancreatic resection, lower hospital market concentration was associated with 5.5% greater costs, but increased hospital concentration was associated with 8.3% lower overall charges. Similarly, among patients undergoing a hepatic resection, hospitals in highly concentrated markets had a mean lower cost of 8.4% than hospitals in unconcentrated markets.
Consistent with previous reports, data from the present study noted that higher patient comorbidity, extended length of stay, and nonroutine discharge were associated with higher costs and charges. Furthermore, the occurrence of an inpatient complication was associated with a 10% to 45% increase in the cost and charge. In general, no regional geographical variation was noted in overall costs or charges after pancreatic or hepatic surgery. We did note an increase of 1% to 2% per year in overall adjusted hospital costs for pancreatic and hepatic resections, respectively. Perhaps of more interest, overall adjusted annual charges increased even more sharply (4% and 5% per year, respectively). These findings highlight the general trend in overall hospital costs and payments to providers in the years leading up to the passage of the Affordable Care Act. Furthermore, these estimates are consistent with the trends in nationwide health care expenditures for other surgical and nonsurgical medical expenditures.
We specifically chose hepatopancreatic surgery to assess the interplay between surgical regionalization and costs and charges. As complex surgical procedures, pancreatic and liver operations have been the focus of regionalization efforts. In particular, pancreatic and liver procedures are very sensitive to the volume-outcome effect, with a wide variation in complications, length of stay, and readmission. As such, the present study sought to quantify the net financial impact of market concentration (which is reflective of competition and regional consolidation) for these complex procedures. The largest contributors to inpatient hospital costs were postoperative complications and prolonged length of stay. The derived estimates of increased costs due to complications among patients undergoing pancreatic or hepatic resection were comparable to the increased costs reported from other single- and multiple-institutional studies. Similarly, previous studies have also reported an association of cost with length of stay. The association of length of stay with costs and charges was interesting in that highly concentrated hospital markets (ie, those reflective of high regionalization with less between-hospital competition) generally had a lower cost of care despite likely caring for patients with higher-acuity illness. In fact, several previous studies have noted a sometimes paradoxical relationship between regionalization of patients with higher-acuity illness for highly specialized procedures (ie, greater hospital consolidation) and overall lower costs. Although the explanation is undoubtedly multifactorial and likely to be associated with lower complications at these centers, it may also be associated with a shorter length of stay. Specifically, multiple high-volume, specialized centers have adopted enhanced recovery after surgery pathways, which have successfully reduced length of stay and overall hospital costs.
Although regionalization of hepatopancreatic surgery to high-volume centers has been associated with increased gains in quality, Ho and colleagues reported that regionalization has also resulted in larger price increases. In a separate study, Gani and Pawlik noted that the overall incidence of complications was lower in higher-volume centers after hepatic surgery; however, costs associated with care of complications were higher than in low-volume centers. In another study by Glick et al conducted on 653 hospitals performing heart valve surgery and 1898 hospitals delivering care for acute myocardial infarction, the authors found that hospitals facing greater competition did not demonstrate better-quality measured performance for heart value surgery or acute myocardial infarction care. For both diagnoses, competition by number of hospitals correlated positively with cost. As such, the authors concluded that hospitals delivering cardiac care did not seem to compete meaningfully on publicly reported quality metrics or costs. The present study expands on this previous work, examining the topic as it relates to another set of high-cost procedures, and specifically defined an association of market concentration with costs and charges among patients undergoing hepatopancreatic surgery.
Limitations
The present study should be considered in light of several limitations. The use of administrative data provides a large, generalizable cohort; however, the data are subject to limitations, including possible inadequate risk adjustment. Our analysis also used reported charges and cost-to-charge ratios compiled by the Healthcare Cost and Utilization Project that differ from the total payments collected by hospitals (and by extension, the true societal cost of the procedures under study). However, prior research using complete financial data from a subset of NIS hospitals found that cost-to-charge ratios (which we used) are highly correlated with payment-to-charge estimators for Medicare, Medicaid, and private insurance. In addition, hospital market concentration was ascribed based on the linkage of the years available in the Hospital Market Structure file using the most recent HHI data available for each year. The definition of a market also relied on a radius of a hospital’s total number of discharges and may not have accounted for a subset of patients who traveled longer distances to receive care. Previous data have suggested, however, that as hospital markets extend beyond geographic divisions, such as counties, state lines, or metropolitan areas, overall distance is likely to be a better estimation of a true market. Finally, in this analysis, we focused on charges by hospitals rather than actual payments for surgical procedures. The dynamics between providers (ie, supply-side factors) and third-party payers (ie, demand-side factors), in turn, determine the negotiated rates for individual hospitals (the equilibrium price of surgical care). Our goal was to determine how hospital consolidation (which alters hospital market concentration) was associated with charges, which constitute the supply side of this equilibrium. Additional analyses that evaluate the influence of market consolidation of insurance providers on payments are needed to elucidate the other portion of this question.
Conclusions
Higher market concentration was associated with lower overall charges and lower costs of pancreatic and hepatic surgery. These findings support the notion that increased hospital market consolidation and regionalization may represent the best value proposition for highly complex surgical procedures: better quality of care with control of costs and charges.
eFigure 1. Unadjusted Mean Costs for Pancreatic Resection and Hepatic Resection by HHI, Clustered by Hospital, With SEs
eFigure 2. Unadjusted Mean Charges for Pancreatic Resection and Hepatic Resection by HHI, Clustered by Hospital, With SEs
References
- 1.Birkmeyer JD, Siewers AE, Finlayson EVA, et al. Hospital volume and surgical mortality in the United States. N Engl J Med. 2002;346(15):1128-1137. doi: 10.1056/NEJMsa012337 [DOI] [PubMed] [Google Scholar]
- 2.Sahni NR, Dalton M, Cutler DM, Birkmeyer JD, Chandra A. Surgeon specialization and operative mortality in United States: retrospective analysis. BMJ. 2016;354(July):i3571-i3579. doi: 10.1136/bmj.i3571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dranove D, Shanley M, White WD. Price and concentration in hospital markets: the switch from patient-driven to payer-driven competition. J Law Econ. 1993;36(1, pt 1):179-204. doi: 10.1086/467270 [DOI] [Google Scholar]
- 4.Cutler DM, Scott Morton F. Hospitals, market share, and consolidation. JAMA. 2013;310(18):1964-1970. doi: 10.1001/jama.2013.281675 [DOI] [PubMed] [Google Scholar]
- 5.Sethi RKV, Henry AJ, Hevelone ND, Lipsitz SR, Belkin M, Nguyen LL. Impact of hospital market competition on endovascular aneurysm repair adoption and outcomes. J Vasc Surg. 2013;58(3):596-606. doi: 10.1016/j.jvs.2013.02.014 [DOI] [PubMed] [Google Scholar]
- 6.Wright JD, Tergas AI, Hou JY, et al. Effect of regional hospital competition and hospital financial status on the use of robotic-assisted surgery. JAMA Surg. 2016;151(7):612-620. doi: 10.1001/jamasurg.2015.5508 [DOI] [PubMed] [Google Scholar]
- 7.Xu T, Wu AW, Makary MA. The potential hazards of hospital consolidation: implications for quality, access, and price. JAMA. 2015;314(13):1337-1338. doi: 10.1001/jama.2015.7492 [DOI] [PubMed] [Google Scholar]
- 8.Mutter RL, Wong HS, Goldfarb MG. The effects of hospital competition on inpatient quality of care. Inquiry. 2008;45(3):263-279. [DOI] [PubMed] [Google Scholar]
- 9.Maeda JLK, Mosher Henke R, Marder WD, Karaca Z, Friedman BS, Wong HS. Variation in hospital inpatient prices across small geographic areas. Am J Manag Care. 2014;20(11):907-916. [PubMed] [Google Scholar]
- 10.Schneider JE, Li P, Klepser DG, Peterson NA, Brown TT, Scheffler RM. The effect of physician and health plan market concentration on prices in commercial health insurance markets. Int J Health Care Finance Econ. 2008;8(1):13-26. doi: 10.1007/s10754-007-9029-4 [DOI] [PubMed] [Google Scholar]
- 11.Gani F, Ejaz A, Makary MA, Pawlik TM. Hospital markup and operation outcomes in the United States. Surgery. 2016;160(1):169-177. doi: 10.1016/j.surg.2016.03.014 [DOI] [PubMed] [Google Scholar]
- 12.Carey K, Burgess JF Jr, Young GJ. Hospital competition and financial performance: the effects of ambulatory surgery centers. Health Econ. 2011;20(5):571-581. doi: 10.1002/hec.1617 [DOI] [PubMed] [Google Scholar]
- 13.Chang DC, Shiozawa A, Nguyen LL, et al. Cost of inpatient care and its association with hospital competition. J Am Coll Surg. 2011;212(1):12-19. doi: 10.1016/j.jamcollsurg.2010.09.014 [DOI] [PubMed] [Google Scholar]
- 14.Ho V, Short MN, Ku-Goto M-H. Can centralization of cancer surgery improve social welfare? Forum Health Econ Policy. 2013;15(2):1-25. doi: 10.1515/fhep-2012-0016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Steiner C, Elixhauser A, Schnaier J. The Healthcare Cost and Utilization Project: an overview. Eff Clin Pract. 2002;5(3):143-151. [PubMed] [Google Scholar]
- 16.Stagg V. CHARLSON: Stata Module to Calculate Charlson Index of Comorbidity. College Station, TX: Statistical Software Components; 2006. [Google Scholar]
- 17.Iezzoni LI, Daley J, Heeren T, et al. Identifying complications of care using administrative data. Med Care. 1994;32(7):700-715. doi: 10.2307/3766163 [DOI] [PubMed] [Google Scholar]
- 18.Okunrintemi V, Gani F, Pawlik TM. National trends in postoperative outcomes and cost comparing minimally invasive versus open liver and pancreatic surgery. J Gastrointest Surg. 2016;20(11):1836-1843. doi: 10.1007/s11605-016-3267-z [DOI] [PubMed] [Google Scholar]
- 19.Birkmeyer JD, Dimick JB. Potential benefits of the new Leapfrog standards: effect of process and outcomes measures. Surgery. 2004;135(6):569-575. doi: 10.1016/j.surg.2004.03.004 [DOI] [PubMed] [Google Scholar]
- 20.Dimick JB, Cowan JA Jr, Knol JA, Upchurch GR Jr. Hepatic resection in the United States: indications, outcomes, and hospital procedural volumes from a nationally representative database. Arch Surg. 2003;138(2):185-191. [DOI] [PubMed] [Google Scholar]
- 21.Meguid RA, Ahuja N, Chang DC. What constitutes a “high-volume” hospital for pancreatic resection? J Am Coll Surg. 2008;206(4):622.e1-622.e9. doi: 10.1016/j.jamcollsurg.2007.11.011 [DOI] [PubMed] [Google Scholar]
- 22.Landefeld JS, Parker RP BEA's chain indexes, time series, and measures of long-term economic growth. Surv Curr Business May 1997:58-68.
- 23.Houchens R, Chu B, Steiner C. Hierarchical Modeling Using HCUP Data: HCUP Methods Series. Rockville, MD: Agency for Healthcare Research and Quality: 2007. Report 2007-01. [Google Scholar]
- 24.Riall TS, Nealon WH, Goodwin JS, Townsend CM Jr, Freeman JL. Outcomes following pancreatic resection: variability among high-volume providers. Surgery. 2008;144(2):133-140. doi: 10.1016/j.surg.2008.03.041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Brill S. Bitter pill: how outrageous pricing and egregious profits are destroying ou health care. Time. 2013;181(8):16-24, 26, 28 passim. [PubMed] [Google Scholar]
- 26.Ejaz A, Kim Y, Spolverato G, Taylor R, Hundt J, Pawlik TM. Understanding drivers of hospital charge variation for episodes of care among patients undergoing hepatopancreatobiliary surgery. HPB (Oxford). 2015;17(11):955-963. doi: 10.1111/hpb.12452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nelson-Williams H, Gani F, Kilic A, et al. Factors associated with interhospital variability in inpatient costs of liver and pancreatic resections. JAMA Surg. 2016;151(2):155-163. doi: 10.1001/jamasurg.2015.3618 [DOI] [PubMed] [Google Scholar]
- 28.Ho V, Dugan J, Ku-Goto M-H. Why are hospital prices rising? Health Manag Policy Innovation. 2013;1(4):1-16. [Google Scholar]
- 29.Gani F, Azoulay D, Pawlik TM. Evaluating trends in the volume-outcomes relationship following liver surgery: does regionalization benefit all patients the same? J Gastrointest Surg. 2017;21(3):463-471. doi: 10.1007/s11605-016-3316-7 [DOI] [PubMed] [Google Scholar]
- 30.Nathan H, Cameron JL, Choti MA, Schulick RD, Pawlik TM. The volume-outcomes effect in hepato-pancreato-biliary surgery: hospital versus surgeon contributions and specificity of the relationship. J Am Coll Surg. 2009;208(4):528-538. doi: 10.1016/j.jamcollsurg.2009.01.007 [DOI] [PubMed] [Google Scholar]
- 31.Schneider EB, Ejaz A, Spolverato G, et al. Hospital volume and patient outcomes in hepato-pancreatico-biliary surgery: is assessing differences in mortality enough? J Gastrointest Surg. 2014;18(12):2105-2115. doi: 10.1007/s11605-014-2619-9 [DOI] [PubMed] [Google Scholar]
- 32.Hyder O, Sachs T, Ejaz A, Spolverato G, Pawlik TM. Impact of hospital teaching status on length of stay and mortality among patients undergoing complex hepatopancreaticobiliary surgery in the USA. J Gastrointest Surg. 2013;17(12):2114-2122. doi: 10.1007/s11605-013-2349-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hyder O, Dodson RM, Nathan H, et al. Influence of patient, physician, and hospital factors on 30-day readmission following pancreatoduodenectomy in the United States. JAMA Surg. 2013;148(12):1095-1102. doi: 10.1001/jamasurg.2013.2509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Spolverato G, Ejaz A, Kim Y, et al. Readmission incidence and associated factors after a hepatic resection at a major hepato-pancreatico-biliary academic centre. HPB (Oxford). 2014;16(11):972-978. doi: 10.1111/hpb.12262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Short MN, Aloia TA, Ho V. The influence of complications on the costs of complex cancer surgery. Cancer. 2014;120(7):1035-1041. doi: 10.1002/cncr.28527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Enestvedt CK, Diggs BS, Cassera MA, Hammill C, Hansen PD, Wolf RF. Complications nearly double the cost of care after pancreaticoduodenectomy. Am J Surg. 2012;204(3):332-338. doi: 10.1016/j.amjsurg.2011.10.019 [DOI] [PubMed] [Google Scholar]
- 37.Robinson JC, Luft HS. The impact of hospital market structure on patient volume, average length of stay, and the cost of care. J Health Econ. 1985;4(4):333-356. [DOI] [PubMed] [Google Scholar]
- 38.Vollmer CM., Jr The economics of pancreas surgery. Surg Clin North Am. 2013;93(3):711-728. doi: 10.1016/j.suc.2013.02.010 [DOI] [PubMed] [Google Scholar]
- 39.Bond-Smith G, Belgaumkar AP, Davidson BR, Gurusamy KS. Enhanced recovery protocols for major upper gastrointestinal, liver and pancreatic surgery. Cochrane Database Syst Rev. 2016;2:CD011382. doi: 10.1002/14651858.CD011382.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kennedy EP, Rosato EL, Sauter PK, et al. Initiation of a critical pathway for pancreaticoduodenectomy at an academic institution—the first step in multidisciplinary team building. J Am Coll Surg. 2007;204(5):917-923. doi: 10.1016/j.jamcollsurg.2007.01.057 [DOI] [PubMed] [Google Scholar]
- 41.Page AJ, Ejaz A, Spolverato G, et al. Enhanced recovery after surgery protocols for open hepatectomy—physiology, immunomodulation, and implementation. J Gastrointest Surg. 2015;19(2):387-399. doi: 10.1007/s11605-014-2712-0 [DOI] [PubMed] [Google Scholar]
- 42.Page AJ, Gani F, Crowley KT, et al. Patient outcomes and provider perceptions following implementation of a standardized perioperative care pathway for open liver resection. Br J Surg. 2016;103(5):564-571. doi: 10.1002/bjs.10087 [DOI] [PubMed] [Google Scholar]
- 43.Ho V, Town RJ, Heslin MJ. Regionalization versus competition in complex cancer surgery. Health Econ Policy Law. 2007;2(pt 1):51-71. doi: 10.1017/S1744133106006256 [DOI] [PubMed] [Google Scholar]
- 44.Gani F, Pawlik TM. Assessing the costs associated with volume-based referral for hepatic surgery. J Gastrointest Surg. 2016;20(5):945-952. doi: 10.1007/s11605-015-3071-1 [DOI] [PubMed] [Google Scholar]
- 45.Glick DB, Wroblewski K, Apfelbaum S, Dauber B, Woo J, Tung A. The relationship between competition and quality in procedural cardiac care. Anesth Analg. 2015;120(1):220-229. doi: 10.1213/ANE.0000000000000456 [DOI] [PubMed] [Google Scholar]
- 46.Haut ER, Pronovost PJ, Schneider EB. Limitations of administrative databases. JAMA. 2012;307(24):2589-2590. doi: 10.1001/jama.2012.6626 [DOI] [PubMed] [Google Scholar]
- 47.Smith MW, Friedman B, Karaca Z, Wong HS. Predicting inpatient hospital payments in the United States: a retrospective analysis. BMC Health Serv Res. 2015;15(1):372. doi: 10.1186/s12913-015-1040-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gresenz CR, Rogowski J, Escarce JJ. Updated variable-radius measures of hospital competition. Health Serv Res. 2004;39(2):417-430. doi: 10.1111/j.1475-6773.2004.00235.x [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure 1. Unadjusted Mean Costs for Pancreatic Resection and Hepatic Resection by HHI, Clustered by Hospital, With SEs
eFigure 2. Unadjusted Mean Charges for Pancreatic Resection and Hepatic Resection by HHI, Clustered by Hospital, With SEs