Abstract
Introduction
Favorable cardiovascular health (FCH) is associated with healthy longevity and reduced cardiovascular mortality risk. However, limited work has investigated the distribution of FCH in older age or considered the antecedents of FCH. Based on prior work linking psychological well-being with cardiovascular endpoints, higher psychological well-being was hypothesized to be associated with increased likelihood of maintaining FCH over time.
Methods
Data were from the English Longitudinal Study of Ageing. The first study wave (2002–2003) included men and women aged ≥50 years. The analytic sample (N=4,925) was restricted to individuals without baseline cardiovascular disease and with clinical data from three follow-ups through 2013. Psychological well-being was assessed with 17 items from the Control, Autonomy, Satisfaction, and Pleasure scale. FCH was defined as being a non-smoker, diabetes-free, and having healthy levels of blood pressure, cholesterol, and BMI (FCH scores ranged from 0–5). Statistical analyses conducted in 2016–2017 used linear mixed models to examine associations between psychological well-being and FCH scores over time. Secondary analyses examined cardiovascular-related mortality.
Results
Only 1% of participants achieved complete FCH at study baseline. Adjusting for sociodemographic factors and depression, greater psychological well-being was associated with higher FCH scores across time (β=0.05, 95% CI=0.02, 0.08), but not rate of change in FCH. Psychological well-being was also associated with a 29% reduced risk of cardiovascular-related mortality in multivariable-adjusted models.
Conclusions
Findings suggest that psychological well-being is associated with having FCH at older ages, and add to knowledge of assets that may increase likelihood of healthy aging.
INTRODUCTION
Cardiovascular disease (CVD) is the leading cause of death worldwide and the burden of disease is high, especially among adults aged >50 years.1 To delay the onset and progression of CVD, traditional prevention strategies are often used to mitigate risk factors. However, reducing damage imposed by risk factors is neither the same nor as desirable as maintaining health across the lifespan. In fact, once risk factors are established, the probability of experiencing CVD is dramatically increased and medication does not fully restore low risk.2 By contrast, adults who are able to maintain favorable cardiovascular health (FCH), defined by healthy levels of blood pressure and lipids, healthy body weight, being diabetes-free, and avoiding cigarette smoking,3,4 show dramatically reduced risk for CVD and premature death.3–5 Thus, primordial prevention—that is, preventing adverse levels of risk factors from becoming established—may be an effective strategy for fostering cardiovascular health across the lifespan.6
However, it remains unclear how many adults achieve FCH and then maintain it. Based on current estimates, prevalence appears surprisingly low. In one study of women aged 18–39 years, 20% met criteria for having FCH.3 In another study of over 350,000 men and women aged 18–60 years, only 5%–10% were non-smokers with healthy levels of blood pressure and cholesterol.5 Another metric called ideal cardiovascular health has been defined as meeting recommended levels of physical activity and healthy diet in addition to the other factors used to define FCH. Prevalence of ideal cardiovascular health is even lower, with estimated prevalence of <1% in older adults.7–9
Factors that enable individuals to maintain FCH in older age are largely unidentified, although research suggests that psychological factors during childhood may be relevant.10,11 Psychological attributes may be prime candidates because they shape how individuals perceive, interact with, and behave in the world, but are also modifiable by the social environment.12 Researchers have long recognized links between psychological health and CVD, but most focus on how poor psychological functioning (e.g., depression) increases disease risk.13,14 Recent evidence suggests psychological well-being—such as having a sense of purpose and a positive outlook—may reduce disease risk independently of depression or other indicators of psychological distress.15 For example, prospective studies demonstrate that experiencing satisfaction with life, optimism, and positive feelings are associated with reduced risk of heart attack, stroke, and cardiovascular death.16–18 Given these established links with CVD, psychological well-being (hereafter called well-being) may also be associated with an actively healthy profile as characterized by maintaining FCH across time.
Using a primordial prevention framework with data from the English Longitudinal Study of Ageing (ELSA), the prevalence of FCH in older adults and whether well-being predicts FCH is investigated. Low prevalence of FCH is expected. Individuals with higher versus lower well-being levels are expected to have higher FCH scores and show slower declines in FCH as they age. Associations are further hypothesized to be independent of sociodemographic characteristics and depression status, potential confounders identified from prior work.15 In secondary analyses, well-being’s association with cardiovascular-related mortality is examined. Sensitivity analyses test the possibility of reverse causality between FCH and well-being, and well-being’s relationship with the components of FCH.
METHODS
Study Population
Data were from ELSA, a nationally representative cohort study of the community-dwelling English population aged ≥50 years. ELSA participants were recruited from households that participated in the Health Survey for England (an annual national cross-sectional health survey) in 1998, 1999, and 2001.19 All Health Survey for England households that contained at least one person aged ≥50 years who consented to be re-contacted were eligible for ELSA.
The first ELSA interview (Wave 1) in 2002–2003 included 11,391 men and women.19 Follow-up interviews with the original cohort members occurred in 2004–2005 (Wave 2), 2006–2007 (Wave 3), 2008–2009 (Wave 4), 2010–2011 (Wave 5), and 2012–2013 (Wave 6); response rates ranged from 73%–82% across waves.19 Clinical health examinations were performed in conjunction with interviews during Waves 2, 4, and 6; thus, measures of FCH were available only at these waves with Wave 2 serving as the present study’s baseline.
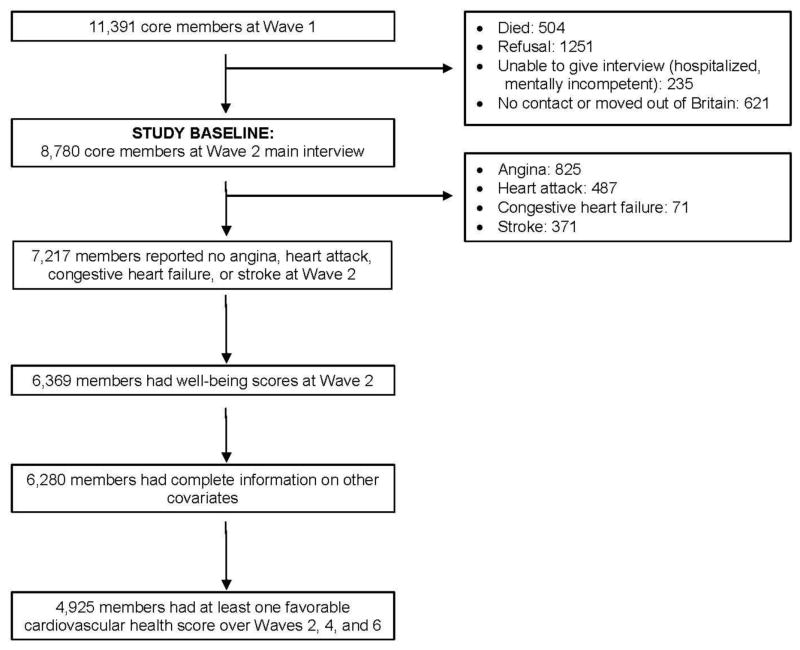
At Wave 2, there were 8,780 core ELSA members who participated in the main interview. Excluding individuals with baseline CVD (n=1,563; i.e., self-reported doctor-diagnosed angina, heart attack, congestive heart failure, or stroke), missing information on well-being or covariates (n=937), and without at least one FCH measure (n=1,355) resulted in an analytic sample of 4,925 participants (Figure 1). Excluded versus included participants tended to be older, more likely to be men and non-white, have lower levels of education, earn less income, and have lower baseline well-being.
Figure 1.
Sample size flow chart.19
This study complies with the Declaration of Helsinki. ELSA has been approved by various ethics committees, including the London Multicentre Research Ethics Committee. All participants provided informed consent.
Measures
Well-being was assessed with items from the 19-item Control, Autonomy, Satisfaction, Pleasure (CASP-19) scale during each wave of ELSA. The CASP-19 assesses psychological functioning in older adults and was originally generated and validated in the United Kingdom with 264 people of “early old age” (aged 65–75 years).20 It is a summative scale covering four domains: control, autonomy, pleasure, and self-realization. Each item is scored on a 4-point scale describing how much each statement applies; higher scores represent greater well-being. The CASP-19 has demonstrated good internal consistency and construct validity in ELSA and other samples.20,21
To prevent physical health from confounding the association between well-being and FCH, two items related to health were removed (My age prevents me from doing the things I would like to and My health stops me from doing things I want to do). Internal consistency reliability was good for this 17-item scale (α=0.87). The CASP-17 from Wave 2 was used in analyses to correspond with the wave in which FCH was first assessed. If participants completed at least nine of the 17 items, then missing values were imputed with the mean value of non-missing items (only 275 individuals [5.58%] required imputed CASP-17 values; most [n=197] were missing only a single item). Analyses considered CASP-17 as either a continuous (mean=39.60, SD=7.26, range, 0–51) or categorical variable. The latter used tertiles based on the analytic sample’s distribution of scores to assess the possibility of discontinuous effects (low: <38; moderate: 38 to <44; high: ≥44).
Consistent with past work, FCH was defined by five components: (1) No self-reported doctor diagnosis of high blood pressure, systolic blood pressure ≤120 mm Hg, and diastolic blood pressure ≤80 mm Hg; (2) No self-reported doctor diagnosis of high cholesterol and total cholesterol <200 mg/dL; (3) BMI <25 kg/m2; (4) No self-reported doctor diagnosis of diabetes (fasting glucose was assessed, but many participants were missing that information so it was not included in the FCH criteria); and (5) Non-smoker (either never or formerly smoked cigarettes).3 A total FCH score was created at each wave (ranging from 0 to 5) by totaling the number of healthy components maintained by individuals. Although this FCH score weighs each component equally, this straightforward approach is useful when tracking cardiovascular health over time (versus developing a clinical risk score).22 Moreover, considering cardiovascular health in aggregate may improve predictions based on any single component.4 If participants developed CVD during a follow-up wave, they were assigned a FCH score of 0 for that wave and subsequent waves. Medication use for high blood pressure, high cholesterol, and diabetes is often included as part of the FCH score. However, ELSA participants answered questions about medication use only if they indicated being diagnosed with the condition. For this reason, medication use provided nearly identical information to diagnosis and was not included in the FCH score. Another definition of cardiovascular health has been proposed that takes diet and physical activity into account23; however, because those health behaviors may be a pathway linking well-being to cardiovascular outcomes,15 they were not included.
Nurses clinically assessed blood pressure, cholesterol (fasting when possible), height, and weight during examinations at Waves 2, 4, and 6. Blood samples were analyzed in the Royal Victoria Infirmary.24 The average time between nurse examinations was 3.91 years (SD=0.57) for Waves 2 and 4, and 3.79 years (SD=0.49) for Waves 4 and 6. Information on self-reported doctor-diagnosed cardiovascular conditions (high blood pressure, high cholesterol, and diabetes) and cigarette smoking status (current smoker, former smoker, or never smoker) was assessed during interviews.
Baseline covariates were self-reported at Wave 2. Age was measured continuously in years, with participants aged >90 years assigned the value of 91 to preserve confidentiality. Gender was categorized as men or women; race was categorized as white or non-white. SES was assessed by educational attainment (university degree or equivalent, higher education but not university degree, A-level [national school exam at age 18 years, high school equivalent], O-level [national school exam at age 16 years], or less than O-level) and total weekly income (measured continuously). Participants also self-reported doctor-diagnosed depression status (depressed, non-depressed).
Statistical Analysis
SAS, version 9.4, was used to conduct analyses during 2016–2017 (p<0.05 significance level, two-tailed). Distributions of baseline (Wave 2) characteristics and FCH scores across baseline tertiles of well-being were examined. Next, the prevalence of FCH at each wave and the extent to which FCH scores changed over follow-up was examined. Primary analyses used linear mixed models to evaluate associations between Wave 2 well-being and FCH scores across time. Well-being was examined as either a continuous (standardized) or categorical (tertiled) variable. A set of models was fit adjusted first for age, gender, and race; second, SES (education and income) was added; third, depression diagnosis was added. Given healthier individuals may be more likely to undergo exams at subsequent waves, these models also accounted for attrition by weighting with a revisit propensity score. This score was calculated from a logistic regression as the probability of having two or three exams given all relevant factors at baseline including age, gender, race, education, income, and depression diagnosis. Using this score, inverse probabilities of multiple exams were created and members of the analytic sample were weighted to account for bias because of missing data.25 To assess consistency of health-related effects of CASP-17 as compared with other indicators of well-being that have been used previously,18 secondary analyses used logistic regression to determine if CASP-17 was related to reduced risk of cardiovascular-related death, among individuals free from baseline CVD and with complete data regarding well-being, covariates, and death (N=5,944). Sensitivity analyses considered potential for reverse causality by testing whether Wave 2 FCH scores predicted well-being levels through Wave 6, as well as well-being’s relationship with individual components of FCH in logistic regression.
RESULTS
Participants were on average aged 64.6 years (SD=8.7 years, range, 52–91 years), with 2,139 men and 2,786 women (56.6%); most were white (98.9%). Individuals with higher well-being levels at Wave 2 were more likely to be white, be more highly educated, earn higher incomes, and less likely to be depressed (Table 1). Baseline well-being was also associated with higher FCH scores at each assessment (rWave2 =0.05, rWave4 =0.09, rWave6 =0.05, all ps<0.01). Trajectories of FCH scores across time for each well-being tertile are shown in Appendix Figure 1.
Table 1.
Distribution of Participant Characteristics by Tertiles of Well-being
| Variable | Low CASP-17 Scores <38 (N=1,633) n (%) |
Moderate CASP-17 Scores 38–<44 (N=1,622) n (%) |
High CASP-17 Scores ≥44 (N=1,670) n (%) |
p-value |
|---|---|---|---|---|
| Mean age (years) at Wave 2 (SD) | 64.70 (9.21) | 64.6 (8.68) | 64.4 (8.19) | 0.51 |
| Gender | 0.27 | |||
| Men | 734 (45.0) | 700 (43.2) | 705 (42.2) | |
| Women | 899 (55.1) | 922 (56.8) | 965 (57.8) | |
| Race | 0.01 | |||
| White | 1,604 (98.2) | 1,607 (99.1) | 1,658 (99.3) | |
| Non-white | 29 (1.78) | 15 (0.92) | 12 (0.72) | |
| Education at Wave 2 | <0.0001 | |||
| University degree | 165 (10.1) | 234 (14.4) | 297 (17.8) | |
| Higher education, no degree | 189 (11.6) | 211 (13.0) | 246 (14.7) | |
| A-level | 114 (6.98) | 114 (7.03) | 122 (7.31) | |
| O-level | 297 (18.2) | 337 (20.8) | 331 (19.8) | |
| Less than O-level | 868 (53.2) | 726 (44.8) | 674 (40.4) | |
| Mean weekly income at Wave 2 (SD) | 249.6 (169.6) | 302.8 (223.4) | 345.5 (292.8) | <0.0001 |
| Depression status at Wave 2 | <0.0001 | |||
| Depressed | 194 (11.9) | 94 (5.8) | 56 (3.35) | |
| Non-depressed | 1,439 (88.1) | 1,528 (94.2) | 1,614 (96.7) | |
| Mean total FCH score at Wave 2 (SD) | 2.38 (0.83) | 2.48 (0.84) | 2.48 (0.79) | 0.002 |
| Mean total FCH score at Wave 4 (SD) | 2.12 (1.06) | 2.30 (1.03) | 2.30 (0.96) | <0.0001 |
| Mean total FCH score at Wave 6 (SD) | 2.02 (1.13) | 2.19 (1.11) | 2.14 (1.07) | 0.004 |
Notes: N=4,925. Percentages refer to the proportion of individuals within each well-being tertile with that characteristic. p-value comes from chi-square or ANOVA. Boldface indicates statistical significance (p<0.05).
CASP-17, 17-item Control, Autonomy, Satisfaction, Pleasure scale; FCH, favorable cardiovascular health
Approximately 1% of participants achieved FCH in each wave (i.e., healthy status on all components; Appendix Table 1). The vast majority of participants were healthy on only two (45%–52%) or three components (26%–30%) at any given wave. Moreover, most participants showed no change in FCH scores across time (Appendix Table 2). Indeed, 56% of participants had the same level of FCH at Waves 2 and 6.
Linear mixed models examined baseline well-being’s association with FCH scores across time and initially included an interaction term for well-being X time. However, the interaction was not statistically significant in any model, indicating well-being was not related to rate of change in FCH across time. As a result, the interaction term was removed from models reported here. These show higher well-being levels were consistently associated with higher FCH scores over time (Table 2). This association held in minimally adjusted models and when adjusting for SES and depression. Similar findings were evident with well-being tertiles. For example, in the multivariable-adjusted model, both moderate (β=0.11, 95% CI=0.04, 0.17, p<0.05) and high (β=0.09, 95% CI=0.02, 0.15, p<0.05) well-being levels were positively associated with FCH scores across time (but well-being level did not interact significantly with time to predict FCH).
Table 2.
Relationship Between Wave 2 Well-being and FCH Scores From Waves 2, 4, and 6
| Variable | β (95% CI)
|
||
|---|---|---|---|
| Model 1a | Model 2b | Model 3c | |
| Well-being (standardized) at Wave 2 | 0.07 (0.05, 0.10) | 0.05 (0.03, 0.08) | 0.05 (0.02, 0.08) |
| Time | −0.04 (−0.05, −0.04) | −0.04 (−0.05, −0.04) | −0.04 (−0.05, −0.04) |
| Age at Wave 2 | −0.01 (−0.01, −0.01) | −0.005 (−0.01, −0.002) | −0.005 (−0.01, −0.002) |
| Gender (women as reference) | −0.04 (−0.08, 0.01) | −0.07 (−0.12, −0.02) | −0.07 (−0.12, −0.02) |
| Race (whites as reference) | 0.15 (−0.08, 0.38) | 0.15 (−0.08, 0.38) | 0.15 (−0.08, 0.37) |
| Education (less than O-level as reference) at Wave 2 | |||
| University degree | 0.23 (0.15, 0.31) | 0.23 (0.15, 0.31) | |
| Higher education, not university degree | 0.10 (0.02, 0.17) | 0.10 (0.02, 0.17) | |
| A-level | 0.15 (0.05, 0.24) | 0.15 (0.05, 0.25) | |
| O-level | 0.15 (0.09, 0.22) | 0.15 (0.09, 0.22) | |
| Income at Wave 2 | 0.07 (0.04, 0.10) | 0.07 (0.03, 0.10) | |
| Depression status (non-depressed as reference) at Wave 2 | −0.03 (−0.13, 0.07) | ||
Notes: N=4,925. Boldface indicates statistical significance (p<0.05).
Linear mixed models adjusted for age, gender, and race.
Linear mixed models adjusted for Model 1 characteristics and SES (education, income).
Linear mixed models adjusted for Model 2 characteristics and depression status.
FCH, favorable cardiovascular health
Secondary analyses examined whether baseline well-being was associated with cardiovascular-related mortality. During approximately 8 years of follow-up, 162 cardiovascular-related deaths (2.73%) occurred. Consistent with findings regarding FCH, a one SD higher baseline well-being level was associated with nearly 30% lower multivariable-adjusted odds of dying from CVD (Table 3). The pattern was similar when considering well-being tertiles. Individuals in the highest versus lowest well-being tertile had up to 35% lower multivariable-adjusted odds of cardiovascular death (OR=0.65, 95% CI=0.43, 0.99). Similar associations were evident for moderate well-being levels (OR=0.56, 95% CI=0.37, 0.84).
Table 3.
Association Between Wave 2 Well-being and Cardiovascular-related Mortality in Individuals Without Baseline CVD
| Variable | OR (95% CI)
|
||
|---|---|---|---|
| Model 1 | Model 2 | Model 3 | |
| Well-being (standardized) at Wave 2 | 0.72 (0.61, 0.85) | 0.73 (0.61, 0.87) | 0.71 (0.59, 0.84) |
| Age at Wave 2 | 1.15 (1.13, 1.18) | 1.15 (1.13, 1.17) | 1.15 (1.13, 1.17) |
| Gender (women as reference) | 1.73 (1.25, 2.42) | 1.80 (1.28, 2.53) | 1.80 (1.28, 2.52) |
| Race (whites as reference) | 0.91 (0.12, 7.16) | 1.05 (0.15, 7.58) | 1.05 (0.15, 7.37) |
| Education (less than O-level as reference) at Wave 2 | |||
| University degree | 0.42 (0.19, 0.94) | 0.43 (0.19, 0.97) | |
| Higher education, not university degree | 1.47 (0.90, 2.43) | 1.47 (0.90, 2.42) | |
| A-level | 0.90 (0.45, 1.81) | 0.89 (0.44, 1.80) | |
| O-level | 0.68 (0.39, 1.18) | 0.68 (0.39, 1.18) | |
| Income at Wave 2 | 1.05 (0.97, 1.14) | 1.05 (0.97, 1.14) | |
| Depression status (non-depressed as reference) at Wave 2 | 0.40 (0.12, 1.37) | ||
Notes: N=5,944. 162 deaths. Boldface indicates statistical significance (p<0.05).
Logistic regression models adjusted for age, gender, and race.
Logistic regression models adjusted for Model 1 characteristics and SES (education, income).
Logistic regression models adjusted for Model 2 characteristics and depression status.
CVD, cardiovascular disease
Sensitivity analyses evaluated whether total FCH score at Wave 2 predicted well-being in subsequent waves (through Wave 6). In all models, Wave 2 FCH score was positively associated with well-being at each time point (β=0.54, 95% CI=0.29, 0.79, p<0.05). Time was significantly associated with declines in well-being (p<0.05). However, the interaction between FCH score X time was not statistically significant, suggesting effects of time on rate of change in well-being did not depend on initial FCH. Moreover, baseline well-being was individually associated with healthier diabetes status, smoking status, and blood pressure, but not cholesterol and BMI (Appendix Table 3).
DISCUSSION
Although FCH is associated with healthier aging and reduced risk of CVD, limited research has examined its distribution in older age and psychosocial antecedents. This study investigated the prevalence of FCH and whether well-being was associated with the presence and maintenance of FCH across approximately 8 years in older adults. Consistent with past findings,5 few people achieved or maintained FCH in older adulthood. Furthermore, cardiovascular health remained relatively stable during older age such that there was limited change in FCH scores. Changes that occurred were primarily characterized by declines in FCH rather than improvements. Nonetheless, as expected, men and women with higher baseline levels of well-being were more likely to have healthier FCH levels across all time points, adjusting for sociodemographic characteristics and depression. However, well-being was not related to rate of change in FCH, perhaps because there was relatively little change occurring. In line with prior work18 and providing further support for the notion that well-being is associated with better cardiovascular health, individuals with greater initial well-being were also less likely to die from cardiovascular-related mortality during follow-up.
Past studies have considered how psychosocial factors in childhood relate to FCH in adulthood,10 but this is the first study to prospectively investigate adult psychosocial factors in relation to attaining and maintaining cardiovascular health in old age. No other longitudinal studies have examined well-being in relation to FCH. One previous study reported associations between optimism and ideal cardiovascular health, but the cross-sectional design limited conclusions about the direction of the relationship.26 However, the current study is the only one that investigates how psychosocial factors in older adulthood might contribute to achieving and maintaining FCH over time.
The sizes of associations in this study were modest, but even small effect sizes can have important implications at the population level, especially if effects compound or accumulate over time.27–29 Although the relationship between well-being and health is likely bidirectional, most research has investigated whether health leads to changes in psychological states rather than the reverse. However, evidence suggests well-being may precede important health outcomes and that it can be enhanced through intervention.30 Preliminary studies also demonstrate that well-being interventions are feasible in at-risk populations and promote physical as well as psychological health.31 If well-being can be shown to contribute causally to achieving FCH, then it may serve as a target for intervention with the goal of improving lifetime ability to attain and maintain cardiovascular health.32
One theoretical model posits that well-being relates to healthy cardiovascular functioning not only by buffering the cardiotoxic effects of stress, but also by enhancing biological and behavioral functioning.15 Although biological and behavioral pathways were not tested because of limited follow-up, such analyses would be useful in future studies. Unlike other markers of cardiovascular health,23 the FCH metric has the advantage of keeping the potential mediating factors of physical activity and diet separate from the definition of cardiovascular health.
Limitations
Study limitations include self-reported data and a homogeneous sample of white English adults aged >50 years. Without additional diversity, conclusions cannot be broadly generalized. Moreover, individuals included versus excluded from the analytic sample tended to be younger, more socioeconomically advantaged, and healthier. Well-being and FCH later in life were considered, which is a time when behavioral and other tendencies are well-established. This may result in conservative tests of the hypotheses because relatively few people in the ELSA cohort made it to older age with complete FCH. It may be informative to assess well-being in younger cohorts when both the prevalence of FCH may be higher and interventions to improve cardiovascular health may be more effective because psychological and behavioral factors are not as well entrenched. Finally, because of how medication use was assessed in ELSA, analyses could not thoroughly account for it.
Study strengths include a prospective design that not only excluded people with pre-existing CVD, but also examined cardiovascular-related mortality as a secondary outcome. Additionally, the possibility of reverse causality was evaluated and potential confounders were controlled. Notably, adding depression status to the models did not alter conclusions, suggesting that well-being’s effects are more than the mere absence of depression.
CONCLUSIONS
Current findings build upon past work indicating that well-being is associated with reduced CVD risk.15 Beyond reducing risk for disease, this study illustrates that well-being is also associated with maintaining healthier cardiovascular functioning. These findings contribute to a more comprehensive definition of what it means to enjoy cardiovascular health and highlight psychological factors that may be important for healthy aging.
Supplementary Material
Acknowledgments
This work was supported by the National Institute on Aging of NIH in Bethesda, Maryland (Award Number R03AG046342). ESZ was supported by a training grant from the National Cancer Institute (Award Number 3R25CA057711). The content is solely the responsibility of the authors and does not necessarily represent the views of NIH. No funding from industry was received.
No financial disclosures were reported by the authors of this paper.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;385(9963):117–171. doi: 10.1016/S0140-6736(14)61682-2. https://doi.org/10.1016/S0140-6736(14)61682-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liu K, Colangelo LA, Daviglus ML, et al. Can antihypertensive treatment restore the risk of cardiovascular disease to ideal levels?: the Coronary Artery Risk Development in Young Adults (CARDIA) Study and the Multi-Ethnic Study of Atherosclerosis (MESA) J Am Heart Assoc. 2015;4(9):e002275. doi: 10.1161/JAHA.115.002275. https://doi.org/10.1161/JAHA.115.002275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Daviglus ML, Stamler J, Pirzada A, et al. Favorable cardiovascular risk profile in young women and long-term risk of cardiovascular and all-cause mortality. JAMA. 2004;292(13):1588–1592. doi: 10.1001/jama.292.13.1588. https://doi.org/10.1001/jama.292.13.1588. [DOI] [PubMed] [Google Scholar]
- 4.Lloyd-Jones DM, Leip EP, Larson MG, et al. Prediction of lifetime risk for cardiovascular disease by risk factor burden at 50 years of age. Circulation. 2006;113(6):791–798. doi: 10.1161/CIRCULATIONAHA.105.548206. https://doi.org/10.1161/CIRCULATIONAHA.105.548206. [DOI] [PubMed] [Google Scholar]
- 5.Stamler J, Stamler R, Neaton JD, et al. Low risk-factor profile and long-term cardiovascular and noncardiovascular mortality and life expectancy: findings for 5 large cohorts of young adult and middle-aged men and women. JAMA. 1999;282(21):2012–2018. doi: 10.1001/jama.282.21.2012. https://doi.org/10.1001/jama.282.21.2012. [DOI] [PubMed] [Google Scholar]
- 6.Strasser T. Reflections on cardiovascular diseases. Interdiscip Sci Rev. 1978;3:225–230. https://doi.org/10.1179/030801878791925921. [Google Scholar]
- 7.Folsom AR, Yatsuya H, Nettleton JA, Lutsey PL, Cushman M, Rosamond WD. Community prevalence of ideal cardiovascular health, by the American Heart Association definition, and relationship with cardiovascular disease incidence. J Am Coll Cardiol. 2011;57(16):1690–1696. doi: 10.1016/j.jacc.2010.11.041. https://doi.org/10.1016/j.jacc.2010.11.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shay CM, Ning H, Allen NB, et al. Status of cardiovascular health in U.S. adults: prevalence estimates from the National Health and Nutrition Examination Surveys (NHANES) 2003–2008. Circulation. 2012;125(1):45–56. doi: 10.1161/CIRCULATIONAHA.111.035733. https://doi.org/10.1161/CIRCULATIONAHA.111.035733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fang J, Yang Q, Hong Y, Loustalot F. Status of cardiovascular health among adult Americans in the 50 States and the District of Columbia, 2009. J Am Heart Assoc. 2012;1(6):e005371. doi: 10.1161/JAHA.112.005371. https://doi.org/10.1161/JAHA.112.005371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Appleton AA, Buka SL, Loucks EB, Rimm EB, Martin LT, Kubzansky LD. A prospective study of positive early-life psychosocial factors and favorable cardiovascular risk in adulthood. Circulation. 2013;127(8):905–912. doi: 10.1161/CIRCULATIONAHA.112.115782. https://doi.org/10.1161/CIRCULATIONAHA.112.115782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pulkki-Raback L, Elovainio M, Hakulinen C, et al. Cumulative effect of psychosocial factors in youth on ideal cardiovascular health in adulthood: The Cardiovascular Risk in Young Finns study. Circulation. 2015;131(3):245–253. doi: 10.1161/CIRCULATIONAHA.113.007104. https://doi.org/10.1161/CIRCULATIONAHA.113.007104. [DOI] [PubMed] [Google Scholar]
- 12.Kubzansky LD, Winning A, Kawachi I. Affective states and health. In: Berkman L, Kawachi I, Glymour MM, editors. Social epidemiology: New perspectives on social determinants of global population health. New York: Oxford University Press; 2014. pp. 320–364. https://doi.org/10.1093/med/9780195377903.003.0009. [Google Scholar]
- 13.Chida Y, Steptoe A. The association of anger and hostility with future coronary heart disease: A meta-analytic review of prospective evidence. J Am Coll Cardiol. 2009;53(11):936–946. doi: 10.1016/j.jacc.2008.11.044. https://doi.org/10.1016/j.jacc.2008.11.044. [DOI] [PubMed] [Google Scholar]
- 14.Rugulies R. Depression as a predictor for coronary heart disease: A review and meta-analysis. Am J Prev Med. 2002;23(1):51–61. doi: 10.1016/s0749-3797(02)00439-7. https://doi.org/10.1016/S0749-3797(02)00439-7. [DOI] [PubMed] [Google Scholar]
- 15.Boehm JK, Kubzansky LD. The heart’s content: The association between positive psychological well-being and cardiovascular health. Psychol Bull. 2012;138(4):655–691. doi: 10.1037/a0027448. https://doi.org/10.1037/a0027448. [DOI] [PubMed] [Google Scholar]
- 16.Boehm JK, Peterson C, Kivimaki M, Kubzansky LD. Heart health when life is satisfying: Evidence from the Whitehall II cohort study. Eur Heart J. 2011;32:2672–2677. doi: 10.1093/eurheartj/ehr203. https://doi.org/10.1093/eurheartj/ehr203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Davidson KW, Mostofsky E, Whang W. Don’t worry, be happy: Positive affect and reduced 10-year incident coronary heart disease: The Canadian Nova Scotia Health Survey. Eur Heart J. 2010;31(9):1065–1070. doi: 10.1093/eurheartj/ehp603. https://doi.org/10.1093/eurheartj/ehp603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tindle HA, Chang YF, Kuller LH, et al. Optimism, cynical hostility, and incident coronary heart disease and mortality in the Women’s Health Initiative. Circulation. 2009;120(8):656–662. doi: 10.1161/CIRCULATIONAHA.108.827642. https://doi.org/10.1161/CIRCULATIONAHA.108.827642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Steptoe A, Breeze E, Banks J, Nazroo J. Cohort Profile: The English Longitudinal Study of Ageing. Int J Epidemiol. 2013;42(6):1640–1648. doi: 10.1093/ije/dys168. https://doi.org/10.1093/ije/dys168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hyde M, Wiggins RD, Higgs P, Blane DB. A measure of quality of life in early old age: The theory, development and properties of a needs satisfaction model (CASP-19) Aging Ment Health. 2003;7(3):186–194. doi: 10.1080/1360786031000101157. https://doi.org/10.1080/1360786031000101157. [DOI] [PubMed] [Google Scholar]
- 21.Wiggins RD, Netuveli G, Hyde M, Higgs P, Blane D. The evaluation of a self-enumerated Scale of Quality of Life (CASP-19) in the context of research on ageing: A combination of exploratory and confirmatory approaches. Soc Indic Res. 2008;89(1):61–77. https://doi.org/10.1007/s11205-007-9220-5. [Google Scholar]
- 22.Lloyd-Jones DM. Improving the cardiovascular health of the U.S. population. JAMA. 2012;307(12):1314–1316. doi: 10.1001/jama.2012.361. https://doi.org/10.1001/jama.2012.361. [DOI] [PubMed] [Google Scholar]
- 23.Lloyd-Jones DM, Hong Y, Labarthe D, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: The American Heart Association’s strategic impact goal through 2020 and beyond. Circulation. 2010;121(4):586–613. doi: 10.1161/CIRCULATIONAHA.109.192703. https://doi.org/10.1161/CIRCULATIONAHA.109.192703. [DOI] [PubMed] [Google Scholar]
- 24.Graig R, Deverill C, Pickering K. Quality control of blood saliva and urine analytes. In: Spronston K, Mindell J, editors. Health Survey for England 2004, Methodology and Documentation. London: The Information Centre; 2006. pp. 34–41. [Google Scholar]
- 25.Seaman SR, White IR. Review of inverse probability weighting for dealing with missing data. Stat Methods Med Res. 2013;22(3):278–295. doi: 10.1177/0962280210395740. https://doi.org/10.1177/0962280210395740. [DOI] [PubMed] [Google Scholar]
- 26.Hernandez R, Kershaw KN, Siddique J, et al. Optimism and cardiovascular health: Multi-Ethnic Study of Atherosclerosis (MESA) Health Behav Policy Rev. 2015;2(1):62–73. doi: 10.14485/HBPR.2.1.6. https://doi.org/10.14485/HBPR.2.1.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Friedman HS, Booth-Kewley S. The ‘disease-prone personality’: a meta-analytic view of the construct. Am Psychol. 1987;42(6):539–555. doi: 10.1037//0003-066x.42.6.539. https://doi.org/10.1037/0003-066X.42.6.539. [DOI] [PubMed] [Google Scholar]
- 28.Roberts BW, Kuncel NR, Shiner R, Caspi A, Goldberg LR. The power of personality: the comparative validity of personality traits, socioeconomic status, and cognitive ability for predicting important life outcomes. Perspect Psychol Sci. 2007;2(4):313–345. doi: 10.1111/j.1745-6916.2007.00047.x. https://doi.org/10.1111/j.1745-6916.2007.00047.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Abelson RP. A variance explanation paradox: when a little is a lot. Psychol Bull. 1985;97(1):129–133. https://doi.org/10.1037/0033-2909.97.1.129. [Google Scholar]
- 30.Bolier L, Haverman M, Westerhof GJ, Riper H, Smit F, Bohlmeijer E. Positive psychology interventions: A meta-analysis of randomized controlled studies. BMC Public Health. 2013;13:119. doi: 10.1186/1471-2458-13-119. https://doi.org/10.1186/1471-2458-13-119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Huffman JC, Mastromauro CA, Boehm JK, et al. Development of a positive psychology intervention for patients with acute cardiovascular disease. Heart Int. 2011;6:47–54. doi: 10.4081/hi.2011.e14. https://doi.org/10.4081/hi.2011.e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Boehm JK, Vie LL, Kubzansky LD. The promise of well-being interventions for improving health risk behaviors. Curr Cardiovasc Risk Rep. 2012;6(6):511–519. https://doi.org/10.1007/s12170-012-0273-x. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.