Sir,
We read with enthusiasm the article by Li et al. (2014) that describes how a course of intermittent theta-burst stimulation (iTBS) over the left dorsolateral prefrontal cortex (L-DLPFC) produced robust antidepressant responses compared to sham stimulation in patients with treatment-refractory depression (Li et al., 2014). TBS, a patterned form of repetitive transcranial magnetic stimulation (rTMS) modelled after endogenous hippocampal discharge patterns (Larson and Lynch, 1986; Huang et al., 2005), has been shown to be more efficient than standard rTMS in modulating cortical excitability (Cárdenas-Morales et al., 2009). Preliminary results indicate non-inferiority of 600 pulses/day of iTBS versus 3000 pulses/day of conventional rTMS in treating depression (Blumberger et al., 2017). Li et al. found that iTBS in highly refractory depression led to a mean 33% reduction in the 17-item Hamilton Depression Rating Scale (HDRS17) (Li et al., 2014), and degree of refractoriness predicted reduced efficacy (Li et al., 2014). Higher refractoriness may require more rTMS pulses to produce an antidepressant response, which in turn would necessitate more rTMS sessions per acute course (Yip et al., 2017). Multiple spaced TBS sessions can be applied over a day with selected time intervals between sessions in an effort to accelerate the onset of effect, thereby also reducing the number of days required to complete an acute course (Cazzoli et al., 2012). To begin testing this hypothesis, we conducted an open-label trial of spaced iTBS for the treatment of depression in six patients with the highest level of treatment-refractoriness.
Eligible participants were 21–70 years of age and had major depressive disorder or bipolar II disorder as diagnosed by the Structured Clinical Interview for DSM-5. Participants were required to meet criteria for the highest non-psychotic treatment-refractoriness on the Maudsley Staging Method (MSM, 14/15) (Fekadu et al., 2009) and have a baseline total score of ≥20 on the HDRS17 (Hamilton, 1960) in the current episode. Participants must have received an FDA-approved rTMS treatment course with ≥60 000 pulses of deep rTMS (Levkovitz et al., 2015) or ≥90 000 pulses of conventional rTMS over L-DLPFC and have failed to meet responder criteria (Lisanby et al., 2009). Participants also were required to have failed to respond to an acute course of electroconvulsive therapy and to meet deep brain stimulation inclusion criteria (Filkowski et al., 2016). Participants were excluded if they had a history of a psychotic disorder, substance use disorder, major systemic illness, lesional neurological disorder, or brain implant. We recruited six participants for this trial. Full written informed consent was obtained for all participants. The study was conducted according to the Declaration of Helsinki and approved by the Stanford Institutional Review Board. All participants were profoundly functionally impaired—either unemployed, on disability, or with significantly reduced workloads due to depressive symptoms. Participant demographics, prior treatments, and baseline measures are included in Table 1.
Table 1.
Participant demographics, prior treatments, baseline measures, and results
| Participant ID | Group | ||||||
|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | ||
| General characteristics | |||||||
| Gender | M | F | F | F | M | F | 4 F/2 M |
| Diagnosis at entry | MDD | BPAD Depressed | MDD | MDD | MDDb | MDD | 5 MDD/1 BPAD |
| Age at treatment | 69 | 53 | 66 | 47 | 63 | 38 | 56 (±12.1) |
| Education (years) | 14 | 15 | 16 | 19 | 19 | 22 | 17.5 (±3.0) |
| Unemployed/functionally disabled | Y | Y | Y | Y | Ya | Y | All |
| Psychiatric history | |||||||
| Age at MDD onset | 32 | 18 | 20 | 18 | 33 | 23 | 24 (±6.8) |
| Length of illness (years) | 37 | 35 | 46 | 29 | 30 | 15 | 32 (±10.3) |
| Current depressive apisode (years) | 27 | 15 | 9 | 15 | 8 | 15 | 14.8 (±6.8) |
| Family history of MDD | Y | Y | Y | N | Y | N | 4 Y/2 N |
| Psychiatric hospitalizations | 0 | 5 | 1 | 0 | 2 | 7 | 2.5 (±2.9) |
| Treatment resistance | |||||||
| Maudsley Staging Method | 14 | 14 | 14 | 14 | 14 | 14 | 14 |
| Thase and Rush Staging Method | 5 | 5 | 5 | 5 | 5 | 5 | 5 |
| Previous brain stimulation therapy failure | |||||||
| VNS | Y | N | N | N | N | N | 1 Y/5 N |
| ECT (courses) | 1 | 2 | 1 | 1 | 1 | 1 | 1.2 (±0.4) |
| Right unilateral (total sessions) | 0 | 12 | 12 | 10 | 15 | 0 | 8.2 (±6.5) |
| Bilateral (total sessions) | 20 | 28 | 28 | 0 | 18 | 16 | 18.3 (±10.3) |
| TMS (courses) | 2 | 1 | 2 | 2 | 1 | 2 | 1.7 (±0.5) |
| TMS (average sessions per course) | 26 | 37 | 39.5 | 30.5 | 25 | 25 | 30.5 (±6.4) |
| DBS consultation | Y | N | N | Y | Y | Y | 4 Y/2 N |
| Psychotherapy failure | Y | Y | Y | Y | Y | Y | All |
| Ketamine failure | Y | N | N | Y | Y | Y | 4 Y/2 N |
| Baseline clinical assessments | |||||||
| HRSD-17 | 34 | 26 | 29 | 27 | 20 | 37 | 28.8 (±6.0) |
| HRSD-6 | 17 | 15 | 15 | 15 | 14 | 20 | 16 2.2 |
| MADRS | 43 | 36 | 40 | 39 | 29 | 55 | 40.3 (±8.6) |
| BDI-II SR | 39 | 64 | 34 | 47 | 22 | 53 | 43.2 (±14.8) |
| CGI-S | 7 | 7 | 7 | 7 | 7 | 7 | 7 |
| Immediate post-stimulation clinical assessments | |||||||
| HRSD-17 | 3 | 5 | 5 | 8 | 16c | 5 | 7 (±4.7) |
| HRSD-6 | 1 | 2 | 2 | 3 | 12c | 0 | 3.3 (±4.4) |
| MADRS | 1 | 0 | 1 | 6 | 19c | 9 | 6 (±7.3) |
| BDI-II SR | 7 | 3 | 8 | 19 | 23c | 12 | 12 (±7.6) |
| CGI-S | 1 | 1 | 1 | 1 | 5c | 1 | 1.7 (±1.6) |
| Two weeks post-stimulation clinical assessments | |||||||
| HRSD-17 | 17 | 26 | 14 | 18 | 14 | 27 | 19.3 (±5.8) |
| HRSD-6 | 9 | 15 | 7 | 9 | 9 | 16 | 10.8 (±3.7) |
| MADRS | 21 | 35 | 13 | 29 | 38 | 19 | 25.8 (±9.8) |
| BDI-II SR | 21 | 54 | 16 | 27 | 17 | 47 | 30.3 (±16.2) |
| CGI-S | 4 | 7 | 5 | 4 | 4 | 6 | 5 (±1.3) |
| Four weeks post-stimulation clinical assessments | |||||||
| HRSD-17 | 25 | N/Ad | 20 | 26 | 18 | 31 | 24 (±5.1) |
| HRSD-6 | 12 | N/Ad | 10 | 13 | 13 | 18 | 13.2 (±2.9) |
| MADRS | 38 | N/Ad | 21 | 40 | 25 | 43 | 33.4 (±9.8) |
| BDI-II SR | 33 | N/Ad | 23 | 47 | 21 | 54 | 35.6 (±14.5) |
| CGI-S | 6 | N/Ad | 7 | 7 | 5 | 7 | 6.4 (±0.9) |
BDI-II SR = Beck Depression Inventory Self Report; BPAD = Bipolar Affective Disorder; CGI-S = Clinical Global Impression - Severity Scale; DBS = deep brain stimulation; ECT = electroconvulsive therapy; HDRS-17 = Hamilton Rating Scale for Depression 17 point; MADRS = Montgomery-Asberg Depression Rating Scale; N/A = not applicable; MDD = Major Depressive Disorder; TMS = transcranial magnetic stimulation; VNS = vagus nerve stimulation.
aThis subject previously acquired a doctoral degree and was employed as a professional; currently works part time in service industry.
bAt time of enrolment, this subject carried a MDD diagnosis, but was subsequently found to have OCD and withdrew from the study.
cThis subject withdrew from the study following 40 of 50 stimulation sessions.
dThis subject received retreatment prior to this time point.
All participants completed pre-/post-treatment 8-min resting state functional connectivity and structural T1-weighted MRI scans. For the targeting (pre-) scan, a hierarchical clustering algorithm (Drysdale et al., 2017) was applied to each participant’s resting state scan to identify personalized functional subregions within both the L-DLPFC and subcallosal cingulate (SCC) (Fox et al., 2012). The L-DLPFC functional subregion with the strongest anti-correlation with SCC regions was selected as the stimulation target. This L-DLPFC functional target was then localized for each participant using the Localite Neuronavigation System. Participants were then treated with open-label spaced iTBS with 1800 pulses per session at 90% resting motor threshold and depth adjustment to the personalized functional target (Stokes et al., 2005). Each session lasted 10 min followed by a 50-min intersession interval. Our iTBS pulse parameters were identical to those used by Li et al. (3-pulse 50-Hz bursts at 5-Hz for 2-s trains, with trains every 10 s). Ten sessions were applied per day (18 000 pulses/day) for five consecutive days (90 000 total pulses) using a Magventure Magpro X100 system. Depression severity was measured with the HDRS17 at baseline, immediately after the final session, and at 2 and 4 weeks follow-up.
All participants tolerated the therapy with no major adverse events. Participant 5 stopped treatment after completing Day 4 (receiving 72 000 pulses) due to perceived lack of effect, but followed through with measures and is included in all results. See Table 1 for depression ratings. There was a mean 76% reduction in HDRS17 from 28.8 ± 6.0 (mean ± standard deviation) at baseline to 7 ± 4.7 after the final session [repeated ANOVA, F(2,10) = 19.58, P < 0.001]. Five of six participants qualified as responders (≥50% decrease in the HDRS17), and four participants were in full remission (HDRS17 ≤ 7) from depression by the final treatment session. At the 2-week follow-up visit, two participants remained responders, and there was a persistent 33% reduction on the HDRS17 (Dunnett’s test, P < 0.05) across all six participants. At the 4-week time point, all participants no longer met responder criteria. Of note, Participant 5 who did not acutely respond to the treatment was later found to have obsessive-compulsive disorder (Yale-Brown Obsessive Compulsive Scale of 20) as his long-standing primary diagnosis, which he did not disclose at study entry. L-DLPFC is an ineffective therapeutic target for OCD (Berlim et al., 2013) and an alternative target is required (Dunlop et al., 2016).
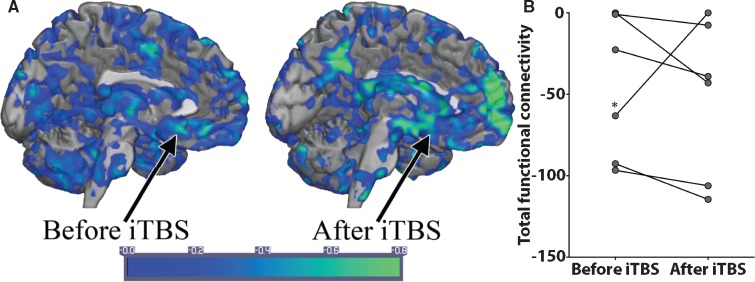
Pre- and post-treatment neuropsychological testing data were available for five participants. Using non-parametric t-tests, performance at post-test either remained unchanged or improved in working memory, executive function, verbal learning and verbal memory domains. One participant had a transient visual memory decrement that renormalized on repeat testing. Five of six participants demonstrated an increased magnitude in anti-correlation between the functional subregions of the L-DLPFC and SCC after iTBS (Fig. 1). A participant with comorbid Parkinson’s disease (Participant 3) taking levodopa demonstrated a reduction in anti-correlation magnitude, which may be due to altered functional connectivity in depressed patients with Parkinson's disease (Wei et al., 2017). If this participant is excluded, the change in functional connectivity is significant [t(4) = −3.024, P < 0.05]. If included, the change in functional connectivity is not significant. A separate analysis of whole brain connectivity changes showed similar findings. Individual participants functional connectivity maps (Fisher’s R-Z transformed) displayed increasing anti-correlations after iTBS in many SCC voxels (see Fig. 1A for representative participant). The paired t-test values of these iTBS-associated changes ranged from −2.18 to −7.62 but did not survive multiple comparisons corrections.
Figure 1.
Personalized and targeted iTBS establishes new anti-correlations between L-DLPFC and SCC. (A) A representative participant’s Fisher’s R-Z transform map of anti-correlations between the L-DLPFC before and after iTBS. The arrow indicates the approximate location of SCC. (B) Total anti-correlation functional connectivity between L-DLPFC and SCC increases in magnitude after iTBS in five of six participants. Negative numbers on the vertical axis indicate the magnitude of anti-correlation. *The one participant in which the anticorrelation was reduced in magnitude had a diagnosis of Parkinson’s disease and was taking levodopa.
This work provides preliminary evidence for treatment of highly refractory depression with high-dose spaced iTBS. It was previously thought that depression at this level required invasive neuromodulation (Bergfeld et al., 2016) because these interventions deliver constant stimulation (Williams et al., 2016). Our study is limited by small sample size and lack of a sham control group; however, individuals with high refractoriness, such as those included in this study, have been previously shown to have no response to sham TBS (Li et al., 2014). An additional new observation is that application of 18 000 pulses of patterned iTBS over 10 sessions separated by 50-min intersession intervals applied across a single day is preliminarily safe. This is the first study to our knowledge that reports this quantity of rTMS pulses applied to a human brain in one day. Although Li et al. used identical pulse parameters, the maximum number of iTBS pulses was limited to 1800 per day. Further, the total number of iTBS pulses delivered over the 2-week treatment was 18 000, compared to the 90 000 delivered over 5 days in the current study. Given the efficacy of this iTBS protocol with a mean 76% reduction in HDRS17 scores and response in five of six participants, this suggests the possibility that treatment-refractory depression non-responsive to stimulation of L-DLPFC may be a result of under-dosing (Li et al., 2014; Yip et al., 2017). Individuals with highly refractory depression may require more TMS pulses in a given day (Li et al., 2014) and/or more total pulses (Yip et al., 2017) than individuals with mild-moderate treatment-refractory depression.
Additionally, in contrast to ≥24-h spacing of TBS sessions in Li et al., this study implemented 50-min intersession intervals, which may enhance the efficacy of TBS. This approach was modelled after animal studies that showed hour-long intervals may be optimal for producing long term potentiation via TBS (Kramár et al., 2012; Lynch et al., 2013). In addition to optimization of the iTBS parameters, we used a personalized targeting approach based on identifying functional subunits of the L-DLPFC that are anti-correlated with SCC. This approach was developed as the functional connectivity of TMS targets has been shown to be related to efficacy in studies of motor physiology (Nettekoven et al., 2015); furthermore, the functional connectivity of SCC is associated with severity of treatment-refractory depression (Greicius et al., 2007) and stimulation sites within L-DLPFC with the highest anticorrelation with SCC are associated with greater efficacy (Fox et al., 2012, 2014). In line with these reports, we found strengthened anti-correlations between DLPFC and SCC in five of six patients after TBS.
Optimized iTBS parameters with individual-level functional targeting described herein may offer a non-invasive and rapid approach that is effective even in cases of highly treatment-refractory depression. Larger controlled trials are underway to further test this hypothesis.
Funding
This work was supported by the Avy L. and Robert L. Miller Foundation, Stanford Psychiatry Chairman’s Small Grant, Stanford CNI Innovation Award, NIH T32 035165, NIH UL1 TR001085, Stanford Medical Scholars Research Scholarship, NARSAD Young Investigator Award and the Gordie Brookstone Fund.
References
- Bergfeld IO, Mantione M, Hoogendoorn ML, Ruhé HG, Notten P, van Laarhoven J, et al. Deep brain stimulation of the ventral anterior limb of the internal capsule for treatment-resistant depression: a randomized clinical trial. JAMA Psychiatry 2016; 73: 456–64. [DOI] [PubMed] [Google Scholar]
- Berlim MT, Neufeld NH, Van den Eynde F. Repetitive transcranial magnetic stimulation (rTMS) for obsessive-compulsive disorder (OCD): an exploratory meta-analysis of randomized and sham-controlled trials. J Psychiatr Res 2013; 47: 999–1006. [DOI] [PubMed] [Google Scholar]
- Blumberger DM, Vila-Rodriguez F, Daskalakis ZJ, Giacobbe P, Lam RW, Kennedy SH, et al. Design of the theta burst versus high frequency rTMS effectiveness evaluation in depression (THREE-D) non-inferiority trial. Brain Stimul 2017; 10: 424. [Google Scholar]
- Cárdenas-Morales L, Nowak DA, Kammer T, Wolf RC, Schönfeldt-Lecuona C. Mechanisms and applications of theta-burst rTMS on the human motor cortex. Brain Topogr 2009; 22: 294–306. [DOI] [PubMed] [Google Scholar]
- Cazzoli D, Müri RM, Schumacher R, von Arx S, Chaves S, Gutbrod K, et al. Theta burst stimulation reduces disability during the activities of daily living in spatial neglect. Brain 2012; 135 (Pt 11): 3426–39. [DOI] [PubMed] [Google Scholar]
- Drysdale AT, Grosenick L, Downar J, Dunlop K, Mansouri F, Meng Y, et al. Resting-state connectivity biomarkers define neurophysiological subtypes of depression. Nat Med 2017; 23: 28–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunlop K, Woodside B, Olmsted M, Colton P, Giacobbe P, Downar J. Reductions in cortico-striatal hyperconnectivity accompany successful treatment of obsessive-compulsive disorder with dorsomedial prefrontal rTMS. Neuropsychopharmacology 2016; 41: 1395–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fekadu A, Wooderson SC, Markopoulou K, Cleare AJ. The maudsley staging method for treatment-resistant depression: prediction of longer-term outcome and persistence of symptoms. J Clin Psychiatry 2009; 70: 952–7. [DOI] [PubMed] [Google Scholar]
- Filkowski MM, Mayberg HS, Holtzheimer PE. Considering eligibility for studies of deep brain stimulation for treatment-resistant depression: insights from a clinical trial in unipolar and bipolar depression. J ECT 2016; 32: 122–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox MD, Buckner RL, Liu H, Chakravarty MM, Lozano AM, Pascual-Leone A. Resting-state networks link invasive and noninvasive brain stimulation across diverse psychiatric and neurological diseases. Proc Natl Acad Sci USA 2014; 111: E4367–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox MD, Buckner RL, White MP, Greicius MD, Pascual-Leone A. Efficacy of transcranial magnetic stimulation targets for depression is related to intrinsic functional connectivity with the subgenual cingulate. Biol Psychiatry 2012; 72: 595–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greicius MD, Flores BH, Menon V, Glover GH, Solvason HB, Kenna H, et al. Resting-state functional connectivity in major depression: abnormally increased contributions from subgenual cingulate cortex and thalamus. Biol Psychiatry 2007; 62: 429–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatr 1960; 23: 56–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang YZ, Edwards MJ, Rounis E, Bhatia KP, Rothwell JC. Theta burst stimulation of the human motor cortex. Neuron 2005; 45: 201–6. [DOI] [PubMed] [Google Scholar]
- Kramár EA, Babayan AH, Gavin CF, Cox CD, Jafari M, Gall CM, et al. Synaptic evidence for the efficacy of spaced learning. Proc Natl Acad Sci USA 2012; 109: 5121–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larson J, Lynch G. Induction of synaptic potentiation in hippocampus by patterned stimulation involves two events. Science 1986; 232: 985–8. [DOI] [PubMed] [Google Scholar]
- Levkovitz Y, Isserles M, Padberg F, Lisanby SH, Bystritsky A, Xia G, et al. Efficacy and safety of deep transcranial magnetic stimulation for major depression: a prospective multicenter randomized controlled trial. World Psychiatry 2015; 14: 64–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li CT, Chen MH, Juan CH, Huang HH, Chen LF, Hsieh JC, et al. Efficacy of prefrontal theta-burst stimulation in refractory depression: a randomized sham-controlled study. Brain 2014; 137 (Pt 7): 2088–98. [DOI] [PubMed] [Google Scholar]
- Lisanby SH, Husain MM, Rosenquist PB, Maixner D, Gutierrez R, Krystal A, et al. Daily left prefrontal repetitive transcranial magnetic stimulation in the acute treatment of major depression: clinical predictors of outcome in a multisite, randomized controlled clinical trial. Neuropsychopharmacology 2009; 34: 522–34. [DOI] [PubMed] [Google Scholar]
- Lynch G, Kramár EA, Babayan AH, Rumbaugh G, Gall CM. Differences between synaptic plasticity thresholds result in new timing rules for maximizing long-term potentiation. Neuropharmacology 2013; 64: 27–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nettekoven C, Volz LJ, Leimbach M, Pool EM, Rehme AK, Eickhoff SB, et al. Inter-individual variability in cortical excitability and motor network connectivity following multiple blocks of rTMS. Neuroimage 2015; 118: 209–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stokes MG, Chambers CD, Gould IC, Henderson TR, Janko NE, Allen NB, et al. Simple metric for scaling motor threshold based on scalp-cortex distance: application to studies using transcranial magnetic stimulation. J Neurophysiol 2005; 94: 4520–7. [DOI] [PubMed] [Google Scholar]
- Wei L, Hu X, Zhu Y, Yuan Y, Liu W, Chen H. Aberrant intra- and internetwork functional connectivity in depressed Parkinson's disease. Sci Rep 2017; 7: 2568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams NR, Short EB, Hopkins T, Bentzley BS, Sahlem GL, Pannu J, et al. Five-year follow-up of bilateral epidural prefrontal cortical stimulation for treatment-resistant depression. Brain Stimul 2016; 9: 897–904. [DOI] [PubMed] [Google Scholar]
- Yip AG, George MS, Tendler A, Roth Y, Zangen A, Carpenter LL. 61% of unmedicated treatment resistant depression patients who did not respond to acute TMS treatment responded after four weeks of twice weekly deep TMS in the Brainsway pivotal trial. Brain Stimul 2017; 10: 847–9. [DOI] [PubMed] [Google Scholar]