Abstract
Background
Incidence estimates of sudden cardiac death (SCD) in sub-Saharan Africa (SSA) are unknown.
Method
Over 12 months, the household administrative office and health community committee within neighbourhoods in two health areas of Douala, Cameroon, registered all deaths among 86 188 inhabitants aged >18 years. As part of an extended multi-source surveillance system, the Emergency Medical Service (EMS), local medical examiners and district hospital mortuaries were also surveyed. Whereas two physicians investigated every natural death, two cardiologists reviewed all unexpected natural deaths.
Results
There were 288 all-cause deaths and 27 (9.4%) were SCD. The crude incidence rate was 31.3 [95% confidence interval (CI): 20.3–40.6]/100 000 person-years. The age-standardized rate by the African standard population was 33.6 (95% CI: 22.4–44.9)/100 000 person-years. Death occurred at night in 37% of cases, including 11% of patients who died while asleep. Out-of-hospital sudden cardiac arrest occurred in 63% of cases, 55.5% of which occurred at home. Of the 88.9% cases of witnessed cardiac arrest, 63% occurred in the presence of a family member and cardiopulmonary resuscitation was attempted only in 3.7%.
Conclusion
The burden of SCD in this African population is heavy with distinct characteristics, whereas awareness of SCD and prompt resuscitation efforts appear suboptimal. Larger epidemiological studies are required in SSA in order to implement preventive measures, especially in women and young people.
Keywords: sudden cardiac death, SCD epidemiology, SCD incidence, sub-Saharan Africa
Key Messages
The burden of sudden cardiac death in this African population, which is 33.6 deaths per 100 000 person-years, is close to the incidence reported in several Western and Asian populations.
Prompt cardiopulmonary resuscitation is suboptimal and needs to be developed according to international recommendations.
Specific preventive strategies targeting the most vulnerable groups of young people and women should be deployed.
Introduction
Data on the epidemiology of sudden cardiac death (SCD) in Black African ethnic groups is lacking.1 The rate of diabetes and coronary artery disease (CAD) is on the rise in the developing countries2, thereby sowing the seeds for the sprawling dissemination of SCD in this burgeoning African population of patients with cardiovascular disease (CVD).3 Even though SCD has been reported in Africans,4–13 its epidemiology remains unknown in sub-Saharan Africa (SSA) owing to the lack of prospective cohort surveys. Identifying the demographic and clinical profiles of patients experiencing cardiac arrest may provide opportunities for improving prevention in SSA, where heart diseases are still neglected.14 In this context, the Pan African Society of Cardiology (PASCAR) initiated a surveillance programme throughout Africa.
Methods
Study population and data collection
The study was conducted in Douala, the largest city in Cameroon. The Cameroonian healthcare system is characterized by the division of the country into health districts (Appendix A). A health district (HD) is the operational geographic unit responsible for providing primary healthcare to the population. An HD covers several neighbouring administrative entities: (i) a district hospital with a mortuary, (ii) primary medical centres and (iii) a dialogue and community participating committee. Each HD comprises two or more health areas (HAs). An HA is a territorial subdivision of an HD around a reference healthcare centre managed by a senior general practitioner (GP) and formed by one or several villages or neighbourhoods. Inhabitants of an HA are covered by (i) a primary health centre and (ii) a health community committee (COSA = ‘comité de santé’).
Two HAs were randomly selected among the six HDs in Douala on the condition that only one HA was selected per HD. The two selected HA comprised a total of 171 690 residents in 2013. UN statistics show that the proportion of people >18 years old in Cameroon is 50.2%.15 Thus, we monitored 86 188 inhabitants for all-death occurrence. The proportion of the population living in rural regions is 45.62% (data.worldbank.org/indicator/SP.RUR.TOTL?locations=CM). Given that living conditions differ between rural and urban areas in Cameroon and that the HAs we monitored are in the main city in Cameroon, our results should be interpreted as urban-based data.
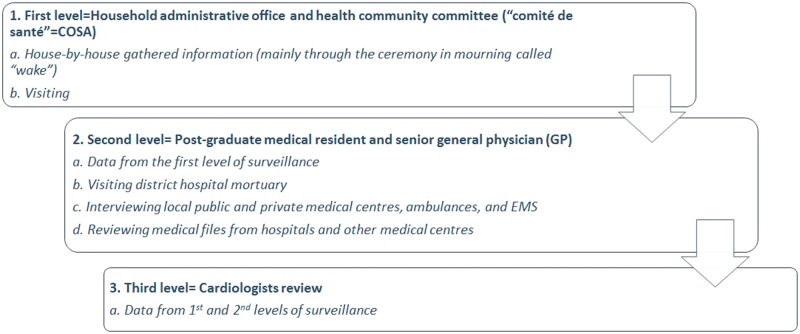
The full study protocol can be found in previous publications.16,17 For the purpose of the study, a three-level case-reporting and ascertainment system was established for SCD surveillance (Figure 1). The first level included the household administrative office and health community committee COSA within the neighbourhoods. At this initial level, specific questionnaires were used to record details of every death. The household administrative office and COSA were responsible for gathering information and completing the questionnaires at this initial level. In Cameroon, the cultural norm in any bereaved family includes hosting a wake, which is attended by all relatives and neighbours. In this way, COSA members living in the neighbourhood are promptly informed of every death within their administrative areas. For the second level of surveillance, a local data-management centre was set up in each HA. Each centre verified all data received from the initial level of surveillance. A post-graduate medical resident and a GP from the district hospital reviewed all natural deaths and selected unexpected deaths. The third level of data management took place at the main study coordinating centre, where at least two cardiologists reviewed all unexpected natural deaths. In the event of disagreement between them, the opinion of a third cardiologist was sought.
Figure 1.
Study surveillance levels: extended multiple sources of death surveillance were conducted at 3 levels. Legend: GP= general physician, EMS=emergency medical service.
To avoid loss of cases, we matched the number of deaths reported by the COSA investigator’s team from the Bonamikano HA and the overall annual mortuary activity at the district hospital of Bonassama, a suburb of Douala. The mortuary in Bonassama district hospital receives almost all cadavers within the district.
Deaths were coded based on the 10th Revision of the International Classification of Diseases (ICD-10). The total number of subjects monitored and their age, sex and vital status (if deceased, the cause of death) were obtained from local administrative offices. To ensure accuracy, the household administrative worker in each office of the public safety bureau was required to collect supplementary information, such as delay from the onset of symptoms to loss of consciousness. If data collection proved difficult, we collected information on the medical history, symptoms and circumstances surrounding each death, using multiple sources to verify the cause of death. This was obtained by the joint effort of one- and two-level case-reporting, from family members, hospital personnel if the decedent died in hospital or from other bystanders. We not only interviewed the decedent’s relatives and witnesses, but we also collected related medical records from the hospitals and the community health offices. In addition to the deaths noted by members of the COSA, we completed the recording by checking all notices of deaths, by visiting the district hospital mortuary of each HA and verifying the medical records from local medical examiners. Interviews of relatives and witnesses were conducted on a weekly basis, ensuring that data were not lost and that recollections gathered were as accurate as possible.
Induced deaths such as those caused by road accidents, intoxication, suicide and other factors were excluded. The final diagnosis of sudden unexpected death was ascertained by at least two cardiologists. Data were recorded in a Case Report Form (see Appendix).
Definition of SCD
We adopted the definition that can be used to ascertain the phenotype in community-based cohort studies as well as investigations conducted in the general population.18 Therefore, established SCD was defined as an unexpected death without obvious extra-cardiac cause, occurring with a rapid witnessed collapse within 1 h after the onset of symptoms, and probable SCD was defined as unexpected death without obvious extra-cardiac cause that occurred within 24 h. In any situation, death should not have occurred in the setting of a prior terminal condition, such as malignancy not in remission or end-stage chronic obstructive lung disease. The term ‘sudden cardiac arrest’ (SCA) was used to describe SCD cases in which specific resuscitation records were available or where the individual had survived a cardiac arrest.
Ethical issues
Approval from the Regional Delegation of the Ministry of Health and local institutions where mortuaries where surveyed was obtained before starting the survey. Confidentiality was maintained in accordance with the Declaration of Helsinki. Informed consent was obtained from the representative of the bereaved family.
Statistical analysis
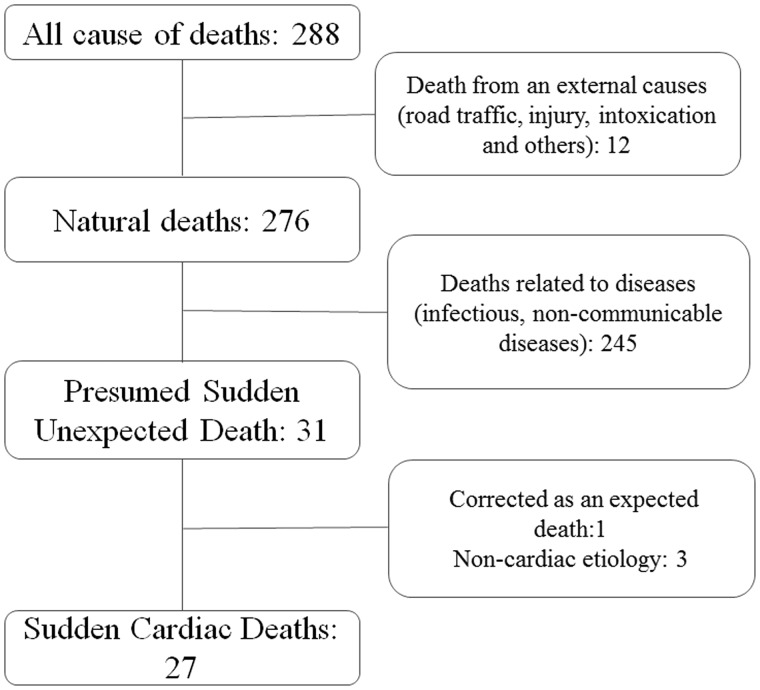
All-cause deaths reported by COSA were cautiously analysed in order to classify them with a special focus on SCD cases, as illustrated in the flow chart (Figure 2). The approximate number of inhabitants per age group was calculated based on the national census data for men and women. The crude 12-month incidence of SCD was assessed by dividing the number of cases registered during the timeframe of the survey by the total number of inhabitants in the same age range, standardized for 100 000 inhabitants. Standard errors and 95% confidence intervals (CIs) around the point estimates were calculated. Continuous variables were presented with the medians and inter-quartiles (with difference between the 25th and 75th percentiles). The differences in age between men and women in the ‘Bonamikano’ and ‘Cité des Palmiers’ HAs were assessed by a non-parametric Wilcoxon test. The comparison of incidence rates between the two HA surveyed in Douala is also presented in Table 1. Differences among SCD cases between men and women as well as regions were tested using a one-sample binomial test, which allowed us to test whether the proportion of SCD cases on a two-level categorical-dependent variable differed from a hypothetical value. The Adjusted SCD incidence rates with the African age-distribution population were calculated. Characteristics of people suffering SCD are presented as frequencies with the corresponding percentages in Table 2.
Figure 2.
Flow-chart of all-death population. Note: Every death was studied at the 3-level of surveillance by COSA members, GP, and cardiologists with an expertise in sudden death. COSA= “comité de santé ”, GP= general physician.
Table 1.
Crude SCD incidence rate between women, men and health areas
| Characteristics | Men | Women | P | Bonamikano* | Cité des palmiers* | p | Total |
|---|---|---|---|---|---|---|---|
| Population size | 42 664 | 43 525 | – | 25 086 | 61 103 | – | 86 189 |
| SCD deaths | 14 | 13 | – | 11 | 16 | – | 27 |
| Median age (interval inter-quartile) | 56 (42) | 35 (16) | 0.15 | 65 (37) | 34.5 (25) | 0.05 | 46 (37) |
| Incidence rate of SCD (per 100 000 person-years) | 29.9 | 32.8 | 0.34 | 43.9 | 26.2 | 0.85 | 31.3 |
| Confidence Interval (per 100 000 person-years) | (21.6–44.6) | (19.2–40.6) | – | (30.9–56.9) | (16.2–36.2) | – | (20.3–41.3) |
SCD= sudden cardiac death.
Health areas where the survey was conducted.
Results
A cohort of 86 188 inhabitants was followed. The overall mortality rate was 334 deaths/100 000 person-years and sudden unexplained death represented 36 cases per 100 000 inhabitants per year. Sudden extra-cardiac death accounted for 1% of total mortality. Of these three patients who experienced extra-cardiac unexpected deaths, one had a haemorrhagic stroke and the second died from postpartum haemorrhage. The last died the day after delivery, pulmonary embolism being suspected as the cause.
SCD population
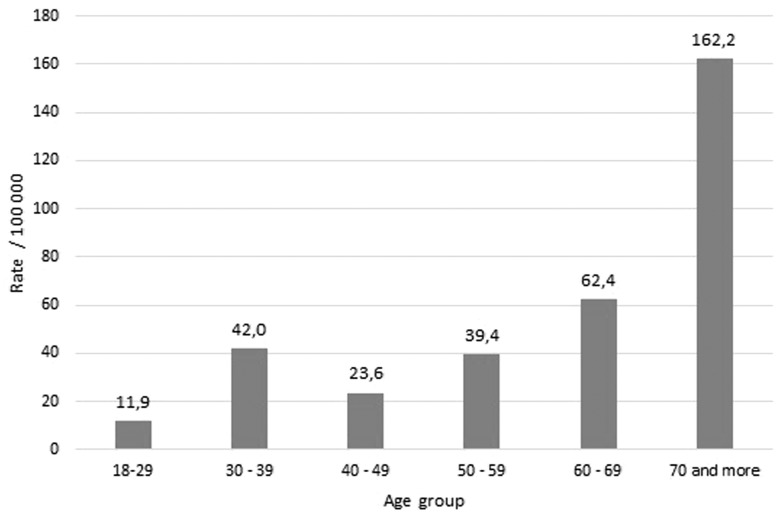
As shown in Table 1, 27 persons suffered SCD, of whom 13 (48.1%) were women. The median age was 46.0 (37) years, 56 (42) years for men and 35 (16) years for women (p = 0.051). The crude incidence rate of SCD was 31.3 (95% CI: 20.3–41.3)/100 000 person-years. The incidence in men and in women was 29.9 and 32.8/100 000 person-years, respectively (p = 0.847). The age-standardized rate by the African standard population was 33.6 (95% CI: 22.2–44.9)/100 000 person-years. Except for the 30- to 39-year-old age group, the distribution linearly and steadily increased with age and peaked in those older than 69 years (Figure 3). Of the 27 SCD cases, 12 (44.4%) were categorized as established, since cardiac arrest occurred within 1 h after the onset of symptoms.
Figure 3.
Age-based Incidence of Sudden Cardiac Death.
Nocturnal death accounted for 37.0% of all SCD, of which 11.1% occurred during sleep (Table 2). One non-competitive female athlete aged 35 years died while exercising. Out-of-hospital cardiac arrest (OHCA) was reported in 17 (63.0%) subjects. Fifteen (55.5%) deaths occurred at home (Table 2): five were found dead (or presumably so) at the scene and brought directly to a mortuary, and the remaining 10 cases were transported by taxi/cab to emergency care centres without any resuscitation attempts. Cardiac arrest was witnessed by others in 24 (88.9%) patients, but only one (3.7%) attempt at cardiopulmonary resuscitation (CPR) was made, unsuccessfully, in a hospitalized patient.
Table 2.
SCD patients’ characteristics
| Variables | N (%) | |
|---|---|---|
| Time of death | Day | 16 (59.3) |
| Night | 10 (37.0) | |
| Unknown | 1 (3.7) | |
| Timeframe | Less than 1 hour | 13 (48.1) |
| Less than 24 hours | 14 (51.9) | |
| Likelihood | Established | 12 (44.4) |
| Probable | 15 (55.6) | |
| Place of death | IHCA | 10 (37.0) |
| Home | 15 (55.6) | |
| At work | 1 (3.7) | |
| Public place | 1 (3.7) | |
| Witness | Family | 17 (63.0) |
| Others* | 7 (25.9) | |
| No witness | 3 (11.1) | |
| Activity | Asleep | 3 (11.1) |
| Resting | 23 (85.2) | |
| Sport-related | 1 (3.7) | |
| Known medical history | Hypertension | 6 (22.2) |
| Diabetes | 3 (11.1) | |
| Heart failure | 4 (14.8) | |
| Dilated CM | 2 (7.4) | |
| Acute myocardial infarction | 2 (7.4) | |
| Other addiction | 1 (3.7) | |
| Tropical disease | 1 (3.7) | |
| HIV infection | 2 (7.4) | |
| Imaging tests available | ECG | No |
| 2D echo | 2 (7.4) | |
| LVEF | No | |
| Known medications | CV drugs | No |
| Other drugs | No | |
IHCA= in-hospital cardiac arrest, DM= dilated cardiomyopathy, HIV= human immunodeficiency virus, ECG= electrocardiogram, LVEF= left ventricular ejection fraction, CV= cardiovascular.
Other people who are not a relative.
Association with CVD
Hypertension and diabetes were known to be present in 22.2% and 11.1% of victims, respectively. One 65-year-old man experienced witnessed chest pain consistent with an acute coronary syndrome before he lost consciousness. The day before, he had already reported the same chest discomfort. Heart failure (HF) was diagnosed in four (14.8%) patients, but no data concerning left ventricular ejection fraction (LVEF) were available. ECG recording was not available in any cases and 2-D Echo was documented in only two patients (Table 2).
Discussion
Epidemiological data concerning premature cardiac death are scant in SSA. Using day-by-day surveillance of all deaths that occurred in two areas of Douala, we found a crude incidence rate of 31.3 SCD per 100 000 person-years in the adult population. Although the complexity of Cameroon creates barriers to obtaining nationwide data, the nature of the government household administrative system (Figure 1) enhances the reliability of collecting complete and accurate data on specific study populations. Compared with the COSA registry, the mortuary registry revealed 3% fewer corpses among the population living in the HAs. Thus, data gathered by investigators in this setting of ‘house-by-house’ information collection were considered to be more exhaustive. The incidence obtained in this study is very similar to that in a study conducted in China,19 especially in the region of Kemalayi, where the standard of living lies between the socio-economic extremes of the areas of Douala surveyed in the present study.
Pattern of SCD in Cameroon
African populations are young and the third national census in Cameroon found that 64.2% of people are aged under 25 years old.20 Accordingly, the median age of premature cardiac death in our study, i.e. 46 years, is lower than that in Western countries. Moreover, the subgroup from the area ‘Cité des Palmiers’ had a median age of 34 years (Table 1), which is lower than any other age reported to date worldwide.3,21–25 Although, the incidence of SCD increased with age (Figure 3), the number of deaths over age 40 was not greater than those aged under 40 years. We therefore hypothesize that the proportion of patients without CAD—mainly inherited arrhythmogenic diseases—is higher in this African population compared with Western populations where CAD accounts for about 80% of all SCD in adults.26 Reinier et al. confirmed that Blacks had a higher prevalence of non-coronary cardiac risk factors for SCA such as congenital and rheumatic heart diseases as well as hypertension, diabetes, and renal insufficiency may play an important role in the high rate of premature cardiac death in SSA.1 This pattern may impact the nature of diagnostic and preventive strategies to be developed in SSA. For instance, the use of a broader spectrum of SCA risk factors including LVH, renal impairment and specific ECG parameters might provide new opportunities for lowering the heavy SCA burden in Africans.
Several studies on SCA have reported more than a two-fold higher incidence in men than in women.27 In Lower Saxony (Germany)23 and in the Paris registry,28 31% of victims were women. In the San Francisco (US) registry29 and the Guangzhou city (China) cohort, the incidence of SCD was nearly as high in women as in men.19 The sex ratio in our study revealed that women are likely to have the same risk of SCD as men. This trend was also observed in the Oregon study but with a slightly greater incidence in men (57% male vs 43% female).30 Gender-related trends appear to have changed, possibly owing to a shift in gender distribution in the prevalence of mortality from CAD.24 Specific factors might explain the high proportion of premature deaths in African women: (i) the illiteracy rate is high among women, resulting in little awareness about CVD prevention; and (ii) women are socio-economically more dependent on their family or spouse’s incomes and, as a result, may benefit less from primary as well as secondary prevention policies, especially where pay-out-of-pocket policies for healthcare prevail.31 This trend in CVD mortality has already been observed in many parts of the world.24 Indeed, studies have shown that women with CVD such as myocardial infarction (MI) wait longer than men after the onset of symptoms to seek care.32,33 Lack of awareness, more ambiguous MI signs and symptoms, and social isolation may contribute to these delays.32,34
OHCA was the commonest scenario, occurring mainly at home in the presence of witnesses in the vast majority of cases. Unfortunately, none of victims was saved even by chest-compression-only CPR. In contrast to developed countries and even in some African settings such as Maiduguri (Nigeria), the Douala SCD registry did not record any unsuccessful attempts at CPR, with only one case recorded. Bougouin et al.35 found 45% of CPR attempts in OHCA in Greater Paris and Talle et al.13 reported 52% of rescue efforts among in-hospital patients with a success rate of 8.2%. This emphasizes the need for widespread CPR awareness programmes so that both medical staff and the public at large are capable of administering such affordable assistance. Moreover, many of these patients were dropped off at the EMS by taxi/cabs without any measure being taken towards ensuring that they reached the medical facilities alive (Appendix B). Although most hospitals and tertiary medical centres in Cameroon have ambulances, they are not well equipped and few have a defibrillator. Even the advanced cardiac life support (ACLS) emergency medical response system, the so-called ‘SAMU de DOUALA’, which is the governmental EMS, has still not attained this objective after more than 15 years of existence. The reasons for this unacceptable inability to treat cardiac arrest are as follows: lack of minimal resuscitation equipment such as catheters for perfusion, emergency drugs (parenteral anti-arrhythmic drugs, adrenaline, dobutamine and others) in ambulances; lack of defibrillator; high cost of healthcare in pay-out-of-pocket settings; difficulty in reaching the operator centralizing calls before dispatch to the available medical staff owing to impaired telephone network; inability of laypersons to grasp the urgency of the situation; absence of facilities and medical personnel capable of performing ACLS; corruption, which is believed by many to adversely affect healthcare delivery.36 The latter three factors account largely for the low number of reported cases of CPR attempts, and therefore the low rate of aborted SCA in SSA. Sport-related SCD was reported in one young female (Table 2), representing an annual incidence of 1.15 cases per 100 000 person-years, which is in accordance with reported incidence estimates in the literature.37 There have been very few studies in this specific population of Black athletes living in Africa38,39 so sport-related population-based studies are needed.
The association between SCD and cardiovascular risk factors follows the overall trend towards an increased burden of CVD in SSA.3 Indeed, 30% of adults in SSA are likely to have hypertension whereas diabetes kills about 9% of people.3 In our study, patients were known to have hypertension and/or diabetes in proportions that indicate the need for preventive measures to be taken.
Implications
The disparities in the trends by sex and age in this Black African population compared with many Western and Asian populations surveyed recently point to opportunities for prevention and interventions. First, the relatively high incidence of SCD in women underscores the fact that the healthcare community should be increasingly prepared to implement strategic programmes for women. Second, in contrast to the increased incidence distribution by age noted in the literature, young African adults aged under 40 years are as exposed to premature CVD deaths as older people, although the prevalence of atherosclerosis is almost non-existent in the first four decades of life. Therefore, preventive strategies should be set up to screen for any inherited electrical cardiac disorders that represent the leading cause of SCD in young persons. Another key issue is to develop advanced resuscitation techniques by supplying equipment and training personnel, and developing protocols for ACLS CPR. Research focusing on needs assessment, prognostication and cost-effectiveness should be encouraged.40
Finally, because persons dying suddenly of CVD do so increasingly outside hospital and mainly with bystanders (63% of cases, Table 2) who do not know how to provide lifesaving actions, public health policies should be directed at implementing awareness about the usefulness of basic life support (BLS) CPR and proposing nationwide programmes on BLS training to improve survival from SCA. For instance, training courses might be introduced in schools and universities as a part of normal curricula. The reported cases of resuscitated SCA in remote African settings11,13 call for such measures to be taken. This would no doubt involve close collaboration between public and private stakeholders.
Strengths and limitations
The major strength of this study lies in its extensive nature. Being a population-based surveillance programme for SCD, it provides accurate information about the burden of SCD. The method of home-by-home surveillance provides powerful hands-on data rather than the potentially inaccurate documentation that death certificates offer. However, several limitations merit discussion. First, it would have been better to provide more clinical data. Second, although their impact on the results would probably not be great in the context of studying the global burden of SCD in a population-based cohort, autopsies were not performed systematically to determine the exact cause of death. Third, the small number of SCD cases reported in this study limits the accurate estimation of the incidence rate (CI 95%: 20.3–41.3) and also provides a somewhat lacking clinical characterization of index cases. Fourth, the follow-up of 12 months is too short to estimate trends. Fifth, given that living conditions differ in rural and urban areas, our urban-based community survey cannot be generalized to the whole Cameroonian population. Finally, comprehensive assessment of symptoms prior to cardiac arrest is an important new direction towards pre-emptive risk stratification and short-term prevention of SCD.41 Unfortunately, we did not register any aborted cardiac death in order to explore victims for symptoms they may have had prior to the event.
Conclusion
The incidence of SCD in Cameroon is such that urgent preventive strategies are required. Young people and women are the populations who should primarily be targeted. On the other hand, the population at large should be made aware of how lifesaving resuscitation can be given, and this should be a priority at the national level.
Funding
A.B. received a grant from the French non-governmental organization ‘Association pour la Recherche CardioVasculaire’ (ARCV) to conduct the survey.
Supplementary Material
Acknowledgements
We thank Ms Nicole Massoh, Colince Ebouele Epoh, Mr Gilbert Loh-Loh and Ms Ernestine Ngo Nken for their precious work in the COSA investigating team; Dr Mohammed A. Talle and Dr Bo Gregers Winkel for their scientific collaboration; Mr Ray Cooke for copyediting the manuscript; the French organization ‘Association pour la Recherche CardioVasculaire (ARCV)’ for its financial support; and the Pan African Society of Cardiology (PASCAR, www.pascar.org) for its scientific caution.
Conflict of interest: The authors have no conflicts of interest to declare.
References
- 1. Reinier K, Nichols GA, Huertas-Vazquez A. et al. Distinctive clinical profile of blacks versus whites presenting with sudden cardiac arrest. Circulation 2015;132:380–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Okrainec K, Banerjee DK, Eisenberg MJ.. Coronary artery disease in the developing world. Am Heart J 2004;148:7–15. [DOI] [PubMed] [Google Scholar]
- 3. Mensah GA, Sampson U, Roth GA. et al. Mortality from cardiovascular diseases in sub-Saharan Africa, 1990–2013: a systematic analysis of data from the Global Burden of Disease Study 2013. Cardiovasc J Afr 2015;26:S6–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ouali S, Boughzela E, Haggui A. et al. Clinical and electrophysiological profile of Brugada syndrome in the Tunisian population. Pacing Clin Electrophysiol PACE 2011;34:47–53. [DOI] [PubMed] [Google Scholar]
- 5. Brink PA, Schwartz PJ.. Of founder populations, long QT syndrome, and destiny. Heart Rhythm Off J Heart Rhythm Soc 2009;6:S25–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Rotimi O, Fatusi AO, Odesanmi WO.. Sudden cardiac death in Nigerians: the Ile-Ife experience. West Afr J Med 2004;23:27–31. [DOI] [PubMed] [Google Scholar]
- 7. Schneider J, Bezabih K.. Causes of sudden death in Addis Ababa, Ethiopia. Ethiop Med J 2001;39:323–40. [PubMed] [Google Scholar]
- 8. Rotimi O, Ajayi AA, Odesanmi WO. et al. Sudden unexpected death from cardiac causes in Nigerians: a review of 50 autopsied cases. Int J Cardiol 1998;63:111–15. [DOI] [PubMed] [Google Scholar]
- 9. Arthur JT. Sudden deaths: cardiac and non-cardiac in children in Accra. West Afr J Med 1995;14:108–11. [PubMed] [Google Scholar]
- 10. Bonny A, Tonet J, Fontaine G. et al. Brugada syndrome in pure black Africans. J Cardiovasc Electrophysiol 2008;19:421–6. [DOI] [PubMed] [Google Scholar]
- 11. Bonny A, Amougou SN, Noah Noah D. et al. Sudden cardiac death in low-resource settings: lessons from a resuscitated cardiac arrest. Cardiovasc J Afr 2015;26:91–5. [DOI] [PubMed] [Google Scholar]
- 12. Akinwusi PO, Komolafe AO, Olayemi OO. et al. Pattern of sudden death at Ladoke Akintola University of Technology Teaching Hospital, Osogbo, South West Nigeria. Vasc Health Risk Manag 2013;9:333–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Talle MA, Bonny A, Bakki B. et al. Sudden cardiac death: clinical perspectives from the University of Maiduguri Teaching Hospital, Nigeria. World J Cardiovasc Dis 2015;5:95–106. [Google Scholar]
- 14. Chin A. Sudden cardiac death in Africa. Cardiovasc J Afr 2014;25:151–2. [PMC free article] [PubMed] [Google Scholar]
- 15. Cameroon Statistics: Demographic Indicators. UNICEF http://www.unicef.org/infobycountry/cameroon_statistics.html (27 February 2017, date last accessed).
- 16. Bonny A, Ngantcha M., Amougou SN. et al. Rationale and design of the Pan-African Sudden Cardiac Death survey: the Pan-African SCD study. Cardiovasc J Afr 2014;25:176–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bonny A, Noah Noah D, Ngantcha M. et al. Epidemiology of sudden cardiac death in Cameroon: rationale and design of the Douala-SUD survey. Arch Cardiovasc Dis 2014;107:433–42. [DOI] [PubMed] [Google Scholar]
- 18. Fishman GI, Chugh S, DiMarco JP. et al. Sudden cardiac death prediction and prevention report from a national heart, lung, and blood institute and heart rhythm society workshop. Circulation 2010;122:2335–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hua W, Zhang LF, Wu YF. et al. Incidence of sudden cardiac death in China: analysis of four regional populations. J Am Coll Cardiol 2009;54:1110–18. [DOI] [PubMed] [Google Scholar]
- 20.RGPH, 3e. La population du Cameroun en 2010. 2010.
- 21. Mehra R. Global public health problem of sudden cardiac death. J Electrocardiol 2007;40:118–22. [DOI] [PubMed] [Google Scholar]
- 22. Murakoshi N, Aonuma K, Epidemiology of arrhythmias and sudden cardiac death in Asia. Circ J Off J Jpn Circ Soc 2013;77:2419–31. [DOI] [PubMed] [Google Scholar]
- 23. Martens E, Sinner MF, Siebermair J. et al. Incidence of sudden cardiac death in Germany: results from an emergency medical service registry in Lower Saxony. Europace 2014;16:1752–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Gerber Y, Jacobsen SJ, Frye RL. et al. Secular trends in deaths from cardiovascular diseases: a 25-year community study. Circulation 2006;113:2285–92. [DOI] [PubMed] [Google Scholar]
- 25. Fender EA, Henrikson CA, Tereshchenko L, Racial differences in sudden cardiac death. J Electrocardiol 2014;47:815–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Huikuri HV, Castellanos A, Myerburg RJ.. Sudden death due to cardiac arrhythmias. N Engl J Med 2001;345:1473–82. [DOI] [PubMed] [Google Scholar]
- 27. Kim C, Fahrenbruch CE, Cobb LA. et al. Out-of-hospital cardiac arrest in men and women. Circulation 2001;104:2699–2703. [DOI] [PubMed] [Google Scholar]
- 28. Jouven X, Desnos M, Guerot C. et al. Predicting sudden death in the population: the Paris Prospective Study I. Circulation 1999;99:1978–83. [DOI] [PubMed] [Google Scholar]
- 29. Steinhaus DA, Vittinghoff, Moffat E. et al. Characteristics of sudden arrhythmic death in a diverse, urban community. Am Heart J 2012;163:125–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Chugh SS, Jui J, Gunson K. et al. Current burden of sudden cardiac death: multiple source surveillance versus retrospective death certificate-based review in a large U.S. community. J Am Coll Cardiol 2004;44:1268–75. [DOI] [PubMed] [Google Scholar]
- 31. Reinier K, Thomas E, Andrusiek. et al. Socioeconomic status and incidence of sudden cardiac arrest. CMAJ Can Med Assoc J 2011;183:1705–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Marrugat JS. Mortality differences between men and women following first myocardial infarction. JAMA 1998;280:1405–9. [DOI] [PubMed] [Google Scholar]
- 33. Vaccarino V, Parsons L, Every NR. et al. Sex-based differences in early mortality after myocardial infarction: National Registry of Myocardial Infarction 2 Participants. N Engl J Med 1999;341:217–25. [DOI] [PubMed] [Google Scholar]
- 34. Sonke GS, Beaglehole R.. Sex differences in case fatality before and after admission to hospital after acute cardiac events: analysis of community based coronary heart disease register. BMJ 1996;313:853–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Bougouin W, Lamhaut L, Marijon E. et al. Characteristics and prognosis of sudden cardiac death in Greater Paris: population-based approach from the Paris Sudden Death Expertise Center (Paris-SDEC). Intensive Care Med 2014;40:846–54. [DOI] [PubMed] [Google Scholar]
- 36. Okafor UV. Challenges in critical care services in Sub-Saharan Africa: perspectives from Nigeria. Indian J Crit Care Med 2009;13:25–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Harmon KG, Drezner JA, Wilson MG, Sharma S.. Incidence of sudden cardiac death in athletes: a state-of-art-review. Br J Sports Med 2014;9:38–72. [DOI] [PubMed] [Google Scholar]
- 38. Marijon E, Tafflet M, Celermajer DS. et al. Sports-related sudden death in the general population. Circulation 2011;124:672–81. [DOI] [PubMed] [Google Scholar]
- 39. Marijon E, Uy-Evanado A, Reinier K. et al. Sudden cardiac death during sports activity in middle age. Circulation 2015;131:1384–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Riviello ED, Letchford S, Achieng L, Newton M.. Critical care in resource-poor settings: lessons learned and future directions. Critical Care Medicine 2011;39:860–7. [DOI] [PubMed] [Google Scholar]
- 41. Marijon E, Uy-Evanado, Dumas F. et al. Warning symptoms are associated with survival from sudden cardiac arrest. Ann Intern Med 2016;164:23–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.