Abstract
Cirrhosis is a prevalent cause of morbidity and mortality, especially for those at an advanced decompensated stage. Cirrhosis development and progression involves several important interorgan communications, and recently, the gut microbiome has been implicated in pathophysiology of the disease. Dysbiosis, defined as a pathological change in the microbiome, has a variable effect on the compensated versus decompensated stage of cirrhosis. Adverse microbial changes, both in composition and function, can act at several levels within the gut (stool and mucosal) and have also been described in the blood and oral cavity. While dysbiosis in the oral cavity could be a source of systemic inflammation, current cirrhosis treatment modalities are targeted toward the gut-liver axis and do not address the oral microbiome. As interventions designed to modulate oral dysbiosis may delay progression of cirrhosis, a better understanding of this process is of the utmost importance. The concept of oral microbiota dysbiosis in cirrhosis is relatively new; therefore, this review will highlight the emerging role of the oral-gut-liver axis and introduce perspectives for future research.
Introduction
Cirrhosis is the end stage of liver disease and is one of the most common causes of morbidity and mortality worldwide (1). Cirrhosis results in a nodular transformation of the liver after several years to decades of inflammation and fibrosis, and, clinically, it has a compensated and a decompensated stage. The disease has an estimated 26.4% mortality per 2-year interval in the US alone and is the 12th leading cause of death (1). Several etiologies, with the most prevalent being viral hepatitis, alcoholic liver disease (ALD), and nonalcoholic fatty liver disease/nonalcoholic steatohepatitis (NAFLD/NASH), can cause cirrhosis. NAFLD is a spectrum of liver disease associated with metabolic syndrome and obesity that consists of simple fatty infiltration (steatosis), inflammation with steatosis (steatohepatitis or NASH), and varying degrees of fibrosis that ultimately lead to cirrhosis. Currently, viral hepatitis (hepatitis C and B) is the leading cause of cirrhosis worldwide; however, NAFLD/NASH is on track to become the most common etiology of chronic liver disease, especially in those with diabetes (2, 3). There is a strong link between the gut microbiota and cirrhosis outcomes, a relationship that needs to be further explored (4–7). Similar to the effect of gut microbiota on cirrhosis, emerging evidence also suggests that there is a possible link between a dysbiotic oral microenvironment and liver diseases. Therefore, it is important to understand the pathogenesis of cirrhosis and the underlying biological factors that can modulate disease outcomes to develop better preventive and treatment strategies. The aim of this review article is to highlight the role of gut microbiome and inflammation in the pathophysiology of cirrhosis and to introduce the oral-gut-liver axis as a new perspective to consider in future research.
Gut microbiota and dysbiosis
The human gut microbiome contains a complex gene pool that arises from the over 1 × 1010 microbes that reside in the human intestine (8). The microbiota is broadly classified by 5 major phyla, namely Firmicutes, Bacteroidetes, Actinobacteria, Proteobacteria, and Verrucomicrobia. Dysbiosis is a term for a microbial imbalance or maladaptation on or inside the body (9) and has been described in patients with cirrhosis. Autochthonous, potentially beneficial taxa — largely comprising members of Firmicutes — are overrepresented in the microbiome of healthy individuals and can serve as biomarkers of a healthy functioning microbiota (10). Taxa within the Firmicutes help digest complex carbohydrates, ferment simple sugars, and, in the process, synthesize short chain fatty acids — including butyrate, propionate, and acetate — that are nutritive to colonocytes. The autochthonous taxa also play a key role in bile acid (BA) homeostasis (11), and alterations in these taxa are associated with mucosal immunological impairment (12), which can encourage the progression of disease processes, including cirrhosis.
Cirrhosis pathophysiology, including gut microbial dysbiosis
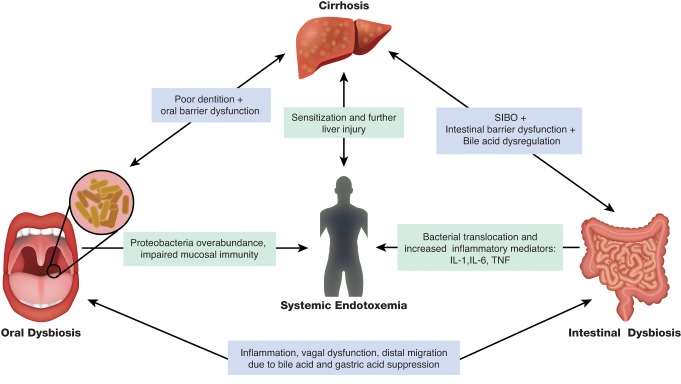
Irrespective of etiology, there are certain common underlying pathways that drive the progression of inflammation in the liver toward fibrosis and subsequent cirrhosis (Figure 1). Upregulation of inflammation and inflammatory mediator–related changes to the liver is postulated to be the primary driver of liver disease. For all cirrhosis etiologies, disease-specific mediators stimulate hepatocytes, hepatic stellate cells (HSCs), Kupffer cells, cholangiocytes, and hepatic T cells to release inflammatory molecules, such as TNF, TGF-β1, and IL-6. These inflammatory mediators activate HSCs to form myofibroblasts that produce collagen, leading to fibrosis and cirrhotic transformation over time (13, 14). In addition to liver inflammation and injury, cirrhosis progression is also associated with an impaired intestinal barrier, systemic inflammation, altered BA profile, and gut dysbiosis.
Figure 1. Proposed relationship between the gut, liver, and the oral cavity.
Inflammation in the oral cavity, liver, and the gut can lead to systemic inflammation, thereby inducing endotoxemia as the result of an increase in the relative abundance of potentially pathogenic microbiota in the gut and oral cavity, along with impaired mucosal and systemic immune response and a dampened ability of the liver to handle these insults. Alterations in bile acid profile, gastric acid suppression and potential neuro-hormonal changes that are inherent in cirrhosis also conspire to generate this systemic proinflammatory milieu. SIBO, small intestinal bacterial overgrowth. Illustrated by Rachel Davidowitz.
Intestinal barrier dysfunction.
The intestinal barrier has several layers of defense, consisting of the mucus layer, tight-junction proteins, physical integrity, and immune surveillance. Studies have demonstrated the complicity of an impaired intestinal barrier in human and animal cirrhosis models, and colonic inflammation has shown to contribute to the increased intestinal permeability in NASH cirrhosis (15–17). In alcoholic cirrhosis, duodenal and jejunal injury has been documented along with increased intercellular space in tight junctions in the distal duodenum (18, 19). Other impairment of intestinal defense mechanisms, such as reduced secretory IgA (20) and generalized reductions in immunity (21), could further weaken the intestinal barrier, resulting in translocation of bacteria and their products. Bacterial products — such as endotoxins, peptidoglycans, and microbial DNA, referred to as pathogen-associated molecular patterns (PAMPs) — gain access to the intestinal immune system due to an increased intestinal permeability. PAMPs interact with innate sensors, including TLRs on the surface of intestinal cells and intracellular NLRs, thereby triggering an inflammatory response characterized by increased generation of cytokines such as IL-1, IL-6, IL-8, and TNF (22, 23). Additionally, bacteria and bacterial products travel to the liver via the portal vein and interact with innate sensors (TLRs and NLRs) of the hepatocytes and Kupffer cells, resulting in further production of inflammatory mediators and cirrhosis (24, 25).
Systemic inflammation.
Cirrhosis reflects a state of heightened systemic inflammation (26, 27) that is potentially instigated by the underlying cirrhosis etiology and endotoxemia, as well as superadded sepsis and other infections. In murine models of induced fibrosis, increased bacterial translocation and inflammation have been shown to correlate with gut dysbiosis, supporting gut microbes as a source of inflammatory mediators (28). Additionally, human studies have also implicated gut dysbiosis in cirrhotic liver disease (4); however, the oral mucosa could also serve as another source of inflammation, as discussed below.
BA dysregulation.
BAs are secreted by the liver and exist in two forms, primary BAs (cholic acid [CA] and chenodeoxycholic acid [CDCA]) and secondary BAs (lithocholic [LCA] and deoxycholic acid [DCA]), which are derived from primary BAs in the colon by the colonic microbiome. The physiological role of BAs is to help in digestion of fats, but they are also essential for intestinal homeostasis via their protective effect on the gut microbiome and intestinal epithelial cells (29–31). There is an imbalance of BA synthesis and excretion in cirrhosis, with reduced levels of secondary BAs due to decreased colonic conversion (32, 33). There is evidence that the Firmicutes, particularly those within the Clostridiales cluster, are responsible for the conversion of primary to secondary BAs in the colon (33–35). It is also possible that reduced BA secretion allows migration of oral microbiota downward to the distal gut, thereby potentiating small intestinal bacterial overgrowth. Over the last decade, evaluation of the BA receptor farnesoid X receptor (FXR) has changed our understanding of BA physiology. BAs are natural FXR ligands in the distal ileum, and BA engagement of FXR promotes BA excretion and — more importantly — can induce antimicrobial peptides (35, 36). FXR regulates hepatic 7α hydroxylase, a critical enzyme for BA synthesis (37). Given the ability to control BA metabolism, FXR ligands are now being targeted to treat NASH (38) and have been approved to treat primary biliary cholangitis (39). Animal studies have also pointed toward FXR agonism as a potential strategy to prevent intestinal barrier dysfunction, hepatic inflammation, and fibrosis (40–43). These findings suggest a broader role for BAs in the progression of cirrhosis through modulation of the gut-liver axis, although human studies are needed.
Gut dysbiosis.
Multiple studies in animal models of NAFLD and ALD have shown a clear association between disease and dysbiosis (44, 45). Additionally, there is evidence that the microbiome influences progression of NAFLD, ALD, and viral hepatitis to end-stage liver disease in humans (46, 47), highlighting dysbiosis as a possible common denominator in these diseases. Dysbiosis has been documented in stool, sigmoid colonic mucosa, small intestinal mucosa, ascites, liver, serum, and saliva from cirrhotic patients (4, 5, 7, 12, 48–50), pointing toward a global mucosal immune change in cirrhosis that permits widespread change in the microbiota. In one of the first studies to look at the gut microbiome using current culture-independent techniques, Chen et al. demonstrated that fecal microbiota from cirrhosis patients exhibits a relative reduction in Bacteroidetes, an increase in Proteobacteria and Fusobacteria, but change in Firmicutes compared with microbiome from healthy individuals (5). Additionally, there were differences at the family level, with Streptococcaceae and Veillonellaceae. Streptococcaceae positively correlated with cirrhosis severity, while Lachnospiraceae negatively correlated with disease. Another research group demonstrated differences in microbiota composition in a larger population of cirrhosis patients and showed that these alterations correlated with cognitive dysfunction and outcome (4, 51). Moreover, the authors of these studies presented a potentially new simplified calculation, the cirrhosis dysbiosis ratio (CDR), to interpret dysbiosis in cirrhosis. The CDR was defined as the ratio of autochthonous taxa to potentially pathogenic taxa at the family level and could predict inpatient and outpatient outcomes, with worse scores indicative of more advanced stages of cirrhosis.
In decompensated cirrhosis, the quintessential infection is spontaneous bacterial peritonitis (SBP), which is defined as infection of the ascites fluid without a physical break in the intestinal lining (52) and is usually caused by members of the Enterobacteriaceae. Not surprisingly, a high relative abundance of Enterobacteriaceae has been noted in patients with SBP compared with other microbiota that are increased cirrhotic patients (4, 53). Hepatic encephalopathy (HE) is another widespread complication that represents an altered gut-liver-brain axis in cirrhosis and affects several brain cell types, including astrocytes, microglia, and neurons (54, 55). The microbiome in cirrhotic patients with HE has been noted to have reduced autochthonous bacteria and, more significantly, increased gram-negative bacterial taxa. In HE, it is hypothesized that gut bacterial production of ammonia and inflammatory cytokines affect different parts of the brain. MRI has shown that astrocytic impairment associates with elevated serum ammonia levels, while white matter changes are associated with inflammation (56). Autochthonous taxa and Enterobacteriaceae were linked with ammonia-associated brain MRI changes, while oral taxa such as Porphyromonadaceae were associated with white matter changes (56).
It is assumed that most constituents of the microbiota are bacteria, but emerging evidence suggests the presence of fungi, archaea, and viruses, especially bacteriophages (57). In patients with cirrhosis, a recent study linked fungal diversity to bacterial diversity and suggested that fungi can impact hospitalizations in conjunction with bacterial indices (58). Fungi in cirrhosis are affected differentially with antibiotics and proton pump inhibitors (PPIs). Further studies are needed to define the constituents of the entire microbiome in liver disease.
Changes in gut microbiota have also been linked with 90-day hospitalizations, organ failure, and death in in-patients with cirrhosis; these effects underline the additive impact of microbiota changes in clinically relevant outcomes (4, 6, 49). An interesting aspect of liver disease–associated microbiota changes is the effect of liver transplant on the recipient’s microbiota. The liver transplant is not a perfect model, because posttransplant patients are on antiviral, antibiotic, and immunosuppressive therapies; however, these patients still provide useful information on the impact that replacement of a diseased liver with a healthy liver has on the microbiota. Longitudinal evaluation of patients with liver transplant showed a significant improvement in gut microbiota diversity over time, but the restoration of microbial diversity did not reach the levels observed in age-matched healthy controls (59). Interestingly, changes in Proteobacteria and Firmicutes were related to the level of cognitive improvement after transplant. The evidence above demonstrates that cirrhosis is associated with gut dysbiosis (Table 1); however, other sources of inflammation related to microbiota in cirrhosis may also be relevant in the overall prognostication.
Table 1. Important studies of human microbiome and cirrhosis.
The emerging oral-gut-liver axis
Oral mucosa.
The oral cavity includes lips, tongue, teeth, periodontium, hard and soft palate, floor of the mouth, and buccal mucosa. The oral mucosa is the mucous membrane lining the inside of the oral cavity and consists of a stratified squamous epithelium termed oral epithelium and an underlying connective tissue termed lamina propria. Depending on the location, oral epithelium can be either keratinized or nonkeratinized. Similar to all forms of connective tissue proper, the lamina propria consists of papillary and dense layers with varying amounts of collagen (type I and III), elastin fibers, blood vessels, and nerve tissue.
The oral mucosa serves as a gateway between the environment and the body and is the first line of defense against microbes and their products. Similar to the gut microbiota, the oral microbiota can be either beneficial or potentially pathogenic and is kept in balance by the natural defense mechanisms of the oral cavity (60). For example, cell shedding from the epithelial surface layers and salivary secretions can limit excessive bacterial colonization. Salivary immunoglobulins such as IgA, IgG, and IgM — as well as salivary agglutinins, histatins, and lysozyme — all form part of the host defense to bacterial insult (61). The oral microbiome is a complex ecosystem with over 700 bacterial species as well as various viruses and fungi. This complex microbiome colonizes teeth surfaces and all mucosal surfaces, and it exists in a surface-attached community encased in a biofilm called dental plaque (62, 63). Like gut microbiota, oral microbiota can be either aerobic or anaerobic with genera, such as Fusobacterium, Veillonella, and Streptococci, predominating. While most of the gut microbiota is extracellular, several oral pathogens such as Porphyromonas gingivalis (a key stone periodontal bacterium) can be intracellular and more pathogenic. Oral pathogens can be beneficial, exacerbate disease processes (64), or be modulated for beneficial purposes (65).
The periodontium is the specialized tissues that surround and support the teeth and comprises four principal components: gingiva, periodontal ligament, cementum, and alveolar bone proper. The gingiva has tissues that exploit an elaborate immune system to protect the host against microbial insult and external stress (66). Specifically, the gingiva consists of an epithelium with a basement membrane and a connective tissue (lamina propria) that includes a dense network of collagen fibers, blood and lymphatic vessels, nerves, and immune and inflammatory cells. Polymorphonuclear leukocytes (PMNs) within the gingival crevice (the space around the teeth) are the first line of defense against bacteria. Gingival keratinocytes, the main cell type in the gingival epithelial tissues, and the connective tissue macrophages, plasma cells, and T and B cells express a variety of inflammatory and immune mediators, including cytokines, chemokines, and matrix metalloproteinases (MMPs), which together orchestrate innate and adaptive immunity. Collectively, cellular and molecular components of the periodontium provide defense for the gingival crevice and the underlying tissues. Despite the continuous presence of a heavy microbial load, the oral mucosa maintains a balanced tissue homeostasis and displays minimal inflammation in healthy individuals. Failure to control inflammation or coordinate timely termination can lead to chronic conditions such as periodontal disease (66).
Oral mucosal dysfunction, dysbiosis, and periodontal disease.
Periodontal disease is one of the most prevalent oral diseases, affecting almost half of the population (67). In its most basic classification, periodontal disease can be categorized as either gingivitis or periodontitis. Gingivitis defines the inflammation of gingival tissues without alveolar bone loss, whereas periodontitis is accompanied by destruction of alveolar bone. Development of periodontitis is mainly driven by the dysbiotic microbiota engaging multiple innate sensors and activating downstream inflammatory signaling cascades, and by the inability of the host to restrain inflammation due to environmental, genetic, and/or epigenetic factors, all of which in turn promote dysbiosis (68–70). The proposed mechanisms linking periodontal disease and systemic conditions include shared risk factors, direct effects of oral bacteria, and continuous exposure to inflammatory mediators. Besides local tissue effects, periodontitis is also associated with increased risk of several systemic conditions, such as diabetes, cardiovascular and respiratory diseases, pregnancy complications, cancer, and possibly liver diseases (71–75). Therefore, the tightly regulated interaction between the oral microbiota and the host immune system within the oral mucosa is key for maintaining tissue homeostasis and preventing adverse clinical outcomes.
The emerging oral-gut axis and liver disease.
It is routine clinical practice to treat periodontitis prior to liver transplant in order to eliminate all potential infectious foci and reduce the risk of postsurgical complications (76). In addition to potentially affecting transplant outcomes, periodontitis is associated clinically with liver diseases such as precirrhotic NAFLD, cirrhosis, and hepatocellular carcinoma (77). While the studies are still limited and a link between periodontal and liver diseases is not as well established as associations between periodontitis and other systemic conditions, such as diabetes and cardiovascular disease (78), it is likely that similar factors related to the oral microbiota and inflammation connect oral and liver disease, as well. It is possible that the link between the liver and the oral cavity could be via the gut through impaired intestinal permeability that in turn could allow direct translocation of bacteria and/or their products and inflammatory mediators from the oral cavity to the systemic circulation.
In addition to periodontitis, cirrhotic patients exhibit numerous oral issues, such as petechiae (79), candidiasis (79), and xerostomia (79, 80). Although studies on the interaction between cirrhosis and periodontitis are still too limited to make assumptions regarding a potential cause-and-effect relationship, a higher incidence of periodontitis (ranging from 25%–68%) has been reported in cirrhotic patients compared with healthy controls (81, 82), an observation that warrants further investigation. In a retrospective study, Aberg and colleagues showed an association between periodontal disease and progression of chronic liver disease, suggesting that dental disease could play a role in cirrhosis (83). Yoneda et al. found that the Porphyromonas gingivalis (a keystone periodontal pathogen) infection was more common in NAFLD patients with periodontitis compared with non-NAFLD patients (84). Additionally, Yoneda and colleagues noted that Porphyromonas gingivalis infection induced NAFLD and accelerated NAFLD progression to NASH in experimental murine models. Nagao and colleagues investigated the relationship between periodontal disease and the progression of liver fibrosis in hepatitis B– and hepatitis C–associated cirrhosis and reported higher salivary levels of the fimbrillin A genotype Porphyromonas gingivalis in patients who developed liver cirrhosis. The study concluded that periodontal disease may be associated with the progression of viral liver disease (85). Recently, periapical lucency, a sign of periapical periodontitis, has been also associated with a higher prevalence of decompensation, such as ascites, HE, and variceal bleeding (86). With regards to different cirrhosis etiologies, periodontitis prevalence tends to be concentrated in patients with alcoholic cirrhosis, which is frequently accompanied by poor oral hygiene (83, 87, 88).
Qin and colleagues compared the stool microbiome in cirrhotic patients and healthy controls in a prospective study and found higher levels of Streptococcus and Veillonella species in the stool from cirrhotic individuals. Comparison of the stool species of cirrhotics with known bacterial species prevalent in the oral cavity and gut of healthy individuals demonstrated a partial similarity to oral microbes and to ileal microbes of the healthy individuals (89). Qin et al. concluded that oral microbes extend into and/or invade the gut, possibly as the result of the changes in intestinal pH and/or BA dysregulation observed in cirrhosis. This extension of oral microbes into the gut, however, could be related to an epiphenomenon allowed by impaired gastric acid and bile secretion that is prevalent in cirrhosis. Another study, involving the use of omeprazole, further supports a cirrhosis-related extension of the oral microbiota into the gut. Omeprazole is a PPI that works to reduce the secretion of digestive acids in the human stomach, thereby raising gastric pH and allowing the presence of bacteria, which normally would have been killed by the gastric acid. The study characterized stool microbiota before and after a 40 mg daily dose of omeprazole for 14 days in cirrhotic patients and healthy controls. Omeprazole therapy, possibly through increased gastric and intestinal pH, led to a significant increase in the relative abundance of Streptococcaceae in stool from all controls (1% vs. 5%) and all patients with cirrhosis (0% vs. 9%). The elevated levels of Streptococcaceae, which are typically limited to the oral microbiome, in stool after omeprazole correlated with serum gastrin levels, which increased as the result of PPI use (90). While these results are intriguing, current evidence does not directly prove distal migration of oral bacteria to the gut in cirrhotic patients. Additionally, multiple gut dysbiosis experiments lack evidence of migration of oral microbiota in animal models of cirrhosis.
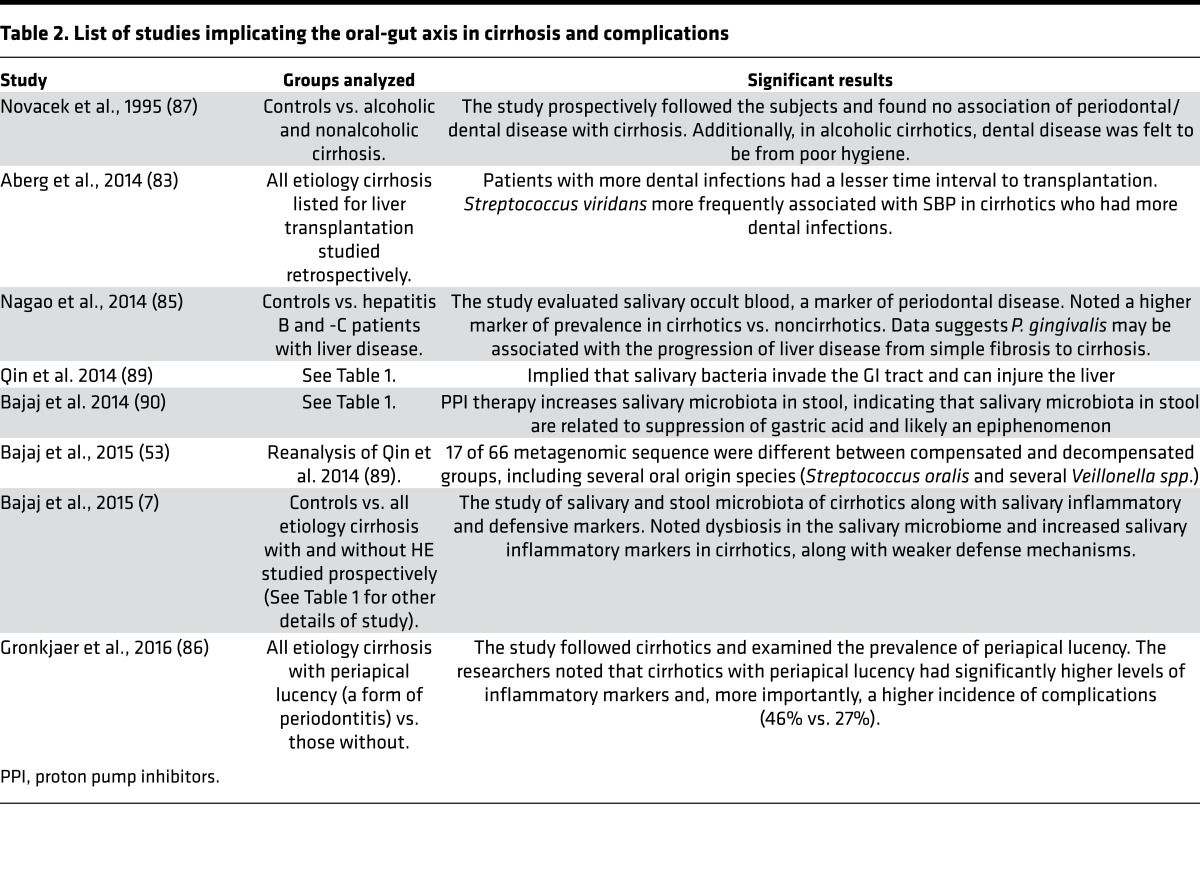
A study on the influence of the oral-gut-liver axis in cirrhosis directly compared the salivary microbiome in cirrhotic patients and healthy controls to the stool microbiome and analyzed salivary inflammation and prediction of 90-day hospitalizations (7). Similar to stool, autochthonous taxa (Lachnospiraceae, Ruminococcaceae, Clostridiales Incertae Sedis XIV) were reduced, while Enterobacteriaceae was increased in the saliva in cirrhotic patients compared with healthy controls. Salivary dysbiosis associated with salivary inflammation and impairment of nonspecific defense mechanisms, such as histatin and lysozyme. Analysis of the predicted functionality of the oral microbiota revealed markedly higher levels of endotoxin and endotoxin-binding protein capacity in saliva from cirrhotic patients compared with saliva from healthy controls. Among the cirrhotic patients, those that were hospitalized with decompensation during the follow-up period (38%) had marked salivary dysbiosis compared with patients who were not hospitalized; therefore, the oral-gut-liver axis may be a major source of inflammatory load in cirrhotic patients (Figure 1). A prospective trial to evaluate the role of periodontal therapy in these cirrhotic patients is underway (NCT03030820). For a list of studies conducted investigating the oral-gut-liver axis, see Table 2.
Table 2. List of studies implicating the oral-gut axis in cirrhosis and complications.
Therapeutic strategies targeting the microbiota in cirrhosis
Given the prominent role of the microbiome in the progression of liver disease toward cirrhosis and in complications of cirrhosis, studies have been conducted in cirrhotic patients to evaluate the effects of modulating the microbiome with probiotics and antibiotics. There is robust evidence that probiotics influence the native microbiome in noncirrhotic patients (91); however, more detailed studies are needed to determine the effects of probiotics in cirrhosis. A randomized controlled trial (RCT) showed that twice daily oral administration of Lactobacillus rhamnosus GG (LGG) for 8 weeks to patients with cirrhosis results in reduced relative abundance of Enterobacteriaceae and increased relative abundance of autochthonous Clostridiales Incertae Sedis XIV and Lachnospiraceae in the stool, indicating less dysbiosis. At the end of 8 weeks, Lactobacillus GG administration reduced endotoxins and inflammatory mediators such as TNF-α (92), providing evidence for further exploration of probiotics as a means of suppressing endotoxemia.
The effects of lactulose on the microbiome has been studied but has not been shown to have a notable effect on reversing dysbiosis (51, 93). Similarly, the effects of the antibiotic rifaximin on the human microbiome has been examined in detail. An 8-week trial of twice-daily oral administration of 550 mg rifaximin in patients with compensated cirrhosis resulted in minor overall changes in microbiota composition, as well as measurable changes in microbiota functionality (94). Evaluation of stool from cirrhotics with a history of HE given lactulose alone revealed minimal changes in microbial composition, while — in those on both lactulose and rifaximin — it revealed changes that were reflective of the underlying liver disease severity rather than the medications themselves (51). However, multiple studies have shown that rifaximin improves cognition and quality of life in cirrhotic patients, suggesting that rifaximin likely modulates the microbiome and reduces inflammation (95, 96). Another therapy being considered for modulating the human microbiome is fecal microbial transplantation (FMT), a concept that has been explored in animal models. For example, Shen et al. engineered rodent gut microbiota with reduced urease activity, thereby decreasing ammonia production, and then introduced this microbiota into rodents that had been depleted of their existing gut microbiota. Compared with animals with a normal flora, animals colonized with the engineered microbiota had reduced mortality and lower fecal ammonia levels (97). Kao and colleagues (98) reported a single case in which a patient with recurrent HE underwent FMT, and this treatment resulted in stool microbiome alterations and improved cognition. In a small pilot study, 8 patients with alcoholic hepatitis underwent FMT and received stool from a donor within their family. One year after FMT, favorable changes to the microbiome were present, and — compared with alcoholic hepatitis patients receiving standard care — patients who underwent FMT had improved mortality (99). A recently published RCT showed that, compared with the standard of care, HE patients that received FMT from a rationally selected donor had improved brain function, a remarkable reduction of both HE recurrence and all hospitalizations, and a restoration of antibiotic-associated loss of diversity (100). Moreover, FMT in patients with recurrent HE was safe overall. Another study using oral capsules for FMT is now underway in the same population (ClinicalTrials.gov, NCT03152188).
Manipulation of the gut microbiota has been shown to change oral microbiota composition. In an RCT, Krasse and colleagues found that administration of probiotics twice daily for 2 weeks significantly reduced gingivitis (101). Matsuoka and colleagues noted a significant reduction in total plaque bacteria and Porphyromonas gingivalis after administration of Lactobacillus salivarius; however, bacterial levels returned to baseline after the treatment was stopped (102). Similarly, Teughels and colleagues found that probiotic treatment in patients with chronic periodontitis reduced plaque score, bleeding, gingival scores, and markers of inflammation during the period of probiotic administration (65). Gingivitis-associated inflammation was studied by Twetman and colleagues, who found that 2 weeks of oral probiotics significantly reduced the levels of IL-8 and TNF-α in the crevicular fluid during therapy; however, these changes were reversed after probiotic administration was stopped (103). Together, these studies indicate that the oral microbiome can be modulated with probiotics in noncirrhotic patients. While there is ample evidence for modulation of the fecal microbiome with probiotics in cirrhosis, further studies are needed regarding the oral microbial milieu.
Conclusion
There is growing evidence that gut dysbiosis aids in the pathogenesis of liver cirrhosis and contributes to the overall systemic inflammatory milieu. Further studies are needed to meaningfully study the functional aspects of these microbial changes that serve as potential mediators of the microbe-host interactions. Similar to the gut microbiome, emerging evidence suggests that the oral microbiome influences changes in the liver; therefore, having a better understanding of the oral-gut-liver represents an exciting new research frontier. Given the ease of sampling, combined with the depth of information that can be retrieved from the oral microbiome, such studies may signal a significant shift in our approach to elucidating the role of the microbiome in liver disease (104). The oral cavity has potential to be considered an additional factor in future discussions on the impact of microbiota on cirrhosis-associated complications.
Acknowledgments
The manuscript was supported by US VA Merit Review I0CX001076 and NIDDK RO1DK089713 (to JSB) and also by National Institute of Dental and Craniofacial Research grant DE025037 (to SES).
Version 1. 10/05/2017
Electronic publication
Footnotes
Conflict of interest: The authors have declared that no conflict of interest exists.
Published: October 5, 2017
Reference information: JCI Insight. 2017;2(19):e94416. https://doi.org/10.1172/jci.insight.94416.
Contributor Information
Chathur Acharya, Email: chathur.acharya@vcuhealth.org.
Sinem Esra Sahingur, Email: ssahingur@vcu.edu.
References
- 1.Scaglione S, et al. The epidemiology of cirrhosis in the United States: A Population-based Study. J Clin Gastroenterol. 2015;49(8):690–696. doi: 10.1097/MCG.0000000000000208. [DOI] [PubMed] [Google Scholar]
- 2.Younossi ZM, et al. Changes in the prevalence of the most common causes of chronic liver diseases in the United States from 1988 to 2008. Clin Gastroenterol Hepatol. 2011;9(6):524–530. doi: 10.1016/j.cgh.2011.03.020. .e1; quiz e60. [DOI] [PubMed] [Google Scholar]
- 3.Browning JD, et al. Prevalence of hepatic steatosis in an urban population in the United States: impact of ethnicity. Hepatology. 2004;40(6):1387–1395. doi: 10.1002/hep.20466. [DOI] [PubMed] [Google Scholar]
- 4.Bajaj JS, et al. Altered profile of human gut microbiome is associated with cirrhosis and its complications. J Hepatol. 2014;60(5):940–947. doi: 10.1016/j.jhep.2013.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen Y, et al. Characterization of fecal microbial communities in patients with liver cirrhosis. Hepatology. 2011;54(2):562–572. doi: 10.1002/hep.24423. [DOI] [PubMed] [Google Scholar]
- 6.Bajaj JS, et al. Gut microbiota alterations can predict hospitalizations in cirrhosis independent of diabetes mellitus. Sci Rep. 2015;5:18559. doi: 10.1038/srep18559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bajaj JS, et al. Salivary microbiota reflects changes in gut microbiota in cirrhosis with hepatic encephalopathy. Hepatology. 2015;62(4):1260–1271. doi: 10.1002/hep.27819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Turnbaugh PJ, Ley RE, Hamady M, Fraser-Liggett CM, Knight R, Gordon JI. The human microbiome project. Nature. 2007;449(7164):804–810. doi: 10.1038/nature06244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tamboli CP, Neut C, Desreumaux P, Colombel JF. Dysbiosis in inflammatory bowel disease. Gut. 2004;53(1):1–4. doi: 10.1136/gut.53.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nava GM, Stappenbeck TS. Diversity of the autochthonous colonic microbiota. Gut Microbes. 2011;2(2):99–104. doi: 10.4161/gmic.2.2.15416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schnabl B, Brenner DA. Interactions between the intestinal microbiome and liver diseases. Gastroenterology. 2014;146(6):1513–1524. doi: 10.1053/j.gastro.2014.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bajaj JS, et al. Colonic mucosal microbiome differs from stool microbiome in cirrhosis and hepatic encephalopathy and is linked to cognition and inflammation. Am J Physiol Gastrointest Liver Physiol. 2012;303(6):G675–G685. doi: 10.1152/ajpgi.00152.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bataller R, Brenner DA. Liver fibrosis. J Clin Invest. 2005;115(2):209–218. doi: 10.1172/JCI24282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhou WC, Zhang QB, Qiao L. Pathogenesis of liver cirrhosis. World J Gastroenterol. 2014;20(23):7312–7324. doi: 10.3748/wjg.v20.i23.7312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pendyala S, Neff LM, Suárez-Fariñas M, Holt PR. Diet-induced weight loss reduces colorectal inflammation: implications for colorectal carcinogenesis. Am J Clin Nutr. 2011;93(2):234–242. doi: 10.3945/ajcn.110.002683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brignardello J, Morales P, Diaz E, Romero J, Brunser O, Gotteland M. Pilot study: alterations of intestinal microbiota in obese humans are not associated with colonic inflammation or disturbances of barrier function. Aliment Pharmacol Ther. 2010;32(11–12):1307–1314. doi: 10.1111/j.1365-2036.2010.04475.x. [DOI] [PubMed] [Google Scholar]
- 17.Tiihonen K, Ouwehand AC, Rautonen N. Effect of overweight on gastrointestinal microbiology and immunology: correlation with blood biomarkers. Br J Nutr. 2010;103(7):1070–1078. doi: 10.1017/S0007114509992807. [DOI] [PubMed] [Google Scholar]
- 18.Bode JC, Bode C, Heidelbach R, Dürr HK, Martini GA. Jejunal microflora in patients with chronic alcohol abuse. Hepatogastroenterology. 1984;31(1):30–34. [PubMed] [Google Scholar]
- 19.Such J, et al. Ultrastructural characteristics of distal duodenum mucosa in patients with cirrhosis. Eur J Gastroenterol Hepatol. 2002;14(4):371–376. doi: 10.1097/00042737-200204000-00006. [DOI] [PubMed] [Google Scholar]
- 20.Saitoh O, et al. Increased prevalence of intestinal inflammation in patients with liver cirrhosis. World J Gastroenterol. 1999;5(5):391–396. doi: 10.3748/wjg.v5.i5.391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tritto G, et al. Evidence of neutrophil functional defect despite inflammation in stable cirrhosis. J Hepatol. 2011;55(3):574–581. doi: 10.1016/j.jhep.2010.11.034. [DOI] [PubMed] [Google Scholar]
- 22.Carvalho FA, Aitken JD, Vijay-Kumar M, Gewirtz AT. Toll-like receptor-gut microbiota interactions: perturb at your own risk! Annu Rev Physiol. 2012;74:177–198. doi: 10.1146/annurev-physiol-020911-153330. [DOI] [PubMed] [Google Scholar]
- 23.Trinchieri G, Sher A. Cooperation of Toll-like receptor signals in innate immune defence. Nat Rev Immunol. 2007;7(3):179–190. doi: 10.1038/nri2038. [DOI] [PubMed] [Google Scholar]
- 24.Seki E, Schnabl B. Role of innate immunity and the microbiota in liver fibrosis: crosstalk between the liver and gut. J Physiol (Lond) 2012;590(3):447–458. doi: 10.1113/jphysiol.2011.219691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Aoyama T, Paik YH, Seki E. Toll-like receptor signaling and liver fibrosis. Gastroenterol Res Pract. 2010;2010:192543. doi: 10.1155/2010/192543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Navasa M, et al. Tumor necrosis factor and interleukin-6 in spontaneous bacterial peritonitis in cirrhosis: relationship with the development of renal impairment and mortality. Hepatology. 1998;27(5):1227–1232. doi: 10.1002/hep.510270507. [DOI] [PubMed] [Google Scholar]
- 27.Tazi KA, Quioc JJ, Saada V, Bezeaud A, Lebrec D, Moreau R. Upregulation of TNF-α production signaling pathways in monocytes from patients with advanced cirrhosis: possible role of Akt and IRAK-M. J Hepatol. 2006;45(2):280–289. doi: 10.1016/j.jhep.2006.02.013. [DOI] [PubMed] [Google Scholar]
- 28.Gómez-Hurtado I, et al. Gut microbiota dysbiosis is associated with inflammation and bacterial translocation in mice with CCl4-induced fibrosis. PLoS One. 2011;6(7):e23037. doi: 10.1371/journal.pone.0023037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kurdi P, Kawanishi K, Mizutani K, Yokota A. Mechanism of growth inhibition by free bile acids in lactobacilli and bifidobacteria. J Bacteriol. 2006;188(5):1979–1986. doi: 10.1128/JB.188.5.1979-1986.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Islam KB, et al. Bile acid is a host factor that regulates the composition of the cecal microbiota in rats. Gastroenterology. 2011;141(5):1773–1781. doi: 10.1053/j.gastro.2011.07.046. [DOI] [PubMed] [Google Scholar]
- 31.Hamer HM, De Preter V, Windey K, Verbeke K. Functional analysis of colonic bacterial metabolism: relevant to health? Am J Physiol Gastrointest Liver Physiol. 2012;302(1):G1–G9. doi: 10.1152/ajpgi.00048.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Vlahcevic ZR, Buhac I, Bell CC, Swell L. Abnormal metabolism of secondary bile acids in patients with cirrhosis. Gut. 1970;11(5):420–422. doi: 10.1136/gut.11.5.420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kakiyama G, et al. Modulation of the fecal bile acid profile by gut microbiota in cirrhosis. J Hepatol. 2013;58(5):949–955. doi: 10.1016/j.jhep.2013.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kakiyama G, et al. Colonic inflammation and secondary bile acids in alcoholic cirrhosis. Am J Physiol Gastrointest Liver Physiol. 2014;306(11):G929–G937. doi: 10.1152/ajpgi.00315.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ridlon JM, Kang DJ, Hylemon PB. Bile salt biotransformations by human intestinal bacteria. J Lipid Res. 2006;47(2):241–259. doi: 10.1194/jlr.R500013-JLR200. [DOI] [PubMed] [Google Scholar]
- 36.Inagaki T, et al. Regulation of antibacterial defense in the small intestine by the nuclear bile acid receptor. Proc Natl Acad Sci U S A. 2006;103(10):3920–3925. doi: 10.1073/pnas.0509592103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kim I, et al. Differential regulation of bile acid homeostasis by the farnesoid X receptor in liver and intestine. J Lipid Res. 2007;48(12):2664–2672. doi: 10.1194/jlr.M700330-JLR200. [DOI] [PubMed] [Google Scholar]
- 38.Forner L, Larsen T, Kilian M, Holmstrup P. Incidence of bacteremia after chewing, tooth brushing and scaling in individuals with periodontal inflammation. J Clin Periodontol. 2006;33(6):401–407. doi: 10.1111/j.1600-051X.2006.00924.x. [DOI] [PubMed] [Google Scholar]
- 39.Nevens F, et al. A placebo-controlled trial of obeticholic acid in primary biliary cholangitis. N Engl J Med. 2016;375(7):631–643. doi: 10.1056/NEJMoa1509840. [DOI] [PubMed] [Google Scholar]
- 40.van Baarlen P, et al. Human mucosal in vivo transcriptome responses to three lactobacilli indicate how probiotics may modulate human cellular pathways. Proc Natl Acad Sci U S A. 2011;108(suppl 1):4562–4569. doi: 10.1073/pnas.1000079107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Verbeke L, et al. The FXR agonist obeticholic acid prevents gut barrier dysfunction and bacterial translocation in cholestatic rats. Am J Pathol. 2015;185(2):409–419. doi: 10.1016/j.ajpath.2014.10.009. [DOI] [PubMed] [Google Scholar]
- 42.Verbeke L, et al. FXR agonist obeticholic acid reduces hepatic inflammation and fibrosis in a rat model of toxic cirrhosis. Sci Rep. 2016;6:33453. doi: 10.1038/srep33453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fiorucci S, et al. The nuclear receptor SHP mediates inhibition of hepatic stellate cells by FXR and protects against liver fibrosis. Gastroenterology. 2004;127(5):1497–1512. doi: 10.1053/j.gastro.2004.08.001. [DOI] [PubMed] [Google Scholar]
- 44.Yan AW, et al. Enteric dysbiosis associated with a mouse model of alcoholic liver disease. Hepatology. 2011;53(1):96–105. doi: 10.1002/hep.24018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.De Minicis S, et al. Dysbiosis contributes to fibrogenesis in the course of chronic liver injury in mice. Hepatology. 2014;59(5):1738–1749. doi: 10.1002/hep.26695. [DOI] [PubMed] [Google Scholar]
- 46.Quigley EM, Stanton C, Murphy EF. The gut microbiota and the liver. Pathophysiological and clinical implications. J Hepatol. 2013;58(5):1020–1027. doi: 10.1016/j.jhep.2012.11.023. [DOI] [PubMed] [Google Scholar]
- 47.Acharya C, Bajaj JS. Gut microbiota and complications of liver disease. Gastroenterol Clin North Am. 2017;46(1):155–169. doi: 10.1016/j.gtc.2016.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mutlu EA, et al. Colonic microbiome is altered in alcoholism. Am J Physiol Gastrointest Liver Physiol. 2012;302(9):G966–G978. doi: 10.1152/ajpgi.00380.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Chen Y, et al. Gut dysbiosis in acute-on-chronic liver failure and its predictive value for mortality. J Gastroenterol Hepatol. 2015;30(9):1429–1437. doi: 10.1111/jgh.12932. [DOI] [PubMed] [Google Scholar]
- 50.Chen Y, Ji F, Guo J, Shi D, Fang D, Li L. Dysbiosis of small intestinal microbiota in liver cirrhosis and its association with etiology. Sci Rep. 2016;6:34055. doi: 10.1038/srep34055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bajaj JS, et al. Linkage of gut microbiome with cognition in hepatic encephalopathy. Am J Physiol Gastrointest Liver Physiol. 2012;302(1):G168–G175. doi: 10.1152/ajpgi.00190.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Tandon P, Garcia-Tsao G. Bacterial infections, sepsis, and multiorgan failure in cirrhosis. Semin Liver Dis. 2008;28(1):26–42. doi: 10.1055/s-2008-1040319. [DOI] [PubMed] [Google Scholar]
- 53.Bajaj JS, Betrapally NS, Gillevet PM. Decompensated cirrhosis and microbiome interpretation. Nature. 2015;525(7569):E1–E2. doi: 10.1038/nature14851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Vilstrup H, et al. Hepatic encephalopathy in chronic liver disease: 2014 Practice Guideline by the American Association for the Study of Liver Diseases and the European Association for the Study of the Liver. Hepatology. 2014;60(2):715–735. doi: 10.1002/hep.27210. [DOI] [PubMed] [Google Scholar]
- 55.Kang DJ, et al. Gut microbiota drive the development of neuroinflammatory response in cirrhosis in mice. Hepatology. 2016;64(4):1232–1248. doi: 10.1002/hep.28696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ahluwalia V, et al. Impaired gut-liver-brain axis in patients with cirrhosis. Sci Rep. 2016;6:26800. doi: 10.1038/srep26800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lloyd-Price J, Abu-Ali G, Huttenhower C. The healthy human microbiome. Genome Med. 2016;8(1):51. doi: 10.1186/s13073-016-0307-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Bajaj JS, et al. Fungal dysbiosis in cirrhosis. Gut. [published online ahead of print June 3, 2017]. https://doi.org/10.1136/gutjnl-2016-313170. [Google Scholar]
- 59.Bajaj JS, et al. Liver transplant modulates gut microbial dysbiosis and cognitive function in cirrhosis. Liver Transpl. 2017;23(7):907–914. doi: 10.1002/lt.24754. [DOI] [PubMed] [Google Scholar]
- 60.Lamont RJ, Hajishengallis G. Polymicrobial synergy and dysbiosis in inflammatory disease. Trends Mol Med. 2015;21(3):172–183. doi: 10.1016/j.molmed.2014.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sahingur SE, Cohen RE. Analysis of host responses and risk for disease progression. Periodontol 2000. 2004;34:57–83. doi: 10.1046/j.0906-6713.2002.003425.x. [DOI] [PubMed] [Google Scholar]
- 62.Hojo K, Nagaoka S, Ohshima T, Maeda N. Bacterial interactions in dental biofilm development. J Dent Res. 2009;88(11):982–990. doi: 10.1177/0022034509346811. [DOI] [PubMed] [Google Scholar]
- 63.Pérez-Chaparro PJ, et al. Newly identified pathogens associated with periodontitis: a systematic review. J Dent Res. 2014;93(9):846–858. doi: 10.1177/0022034514542468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Avila M, Ojcius DM, Yilmaz O. The oral microbiota: living with a permanent guest. DNA Cell Biol. 2009;28(8):405–411. doi: 10.1089/dna.2009.0874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Teughels W, Loozen G, Quirynen M. Do probiotics offer opportunities to manipulate the periodontal oral microbiota? J Clin Periodontol. 2011;38(suppl 11):159–177. doi: 10.1111/j.1600-051X.2010.01665.x. [DOI] [PubMed] [Google Scholar]
- 66.Ebersole JL, et al. Aging, inflammation, immunity and periodontal disease. Periodontol 2000. 2016;72(1):54–75. doi: 10.1111/prd.12135. [DOI] [PubMed] [Google Scholar]
- 67.Eke PI, et al. Update on Prevalence of Periodontitis in Adults in the United States: NHANES 2009 to 2012. J Periodontol. 2015;86(5):611–622. doi: 10.1902/jop.2015.140520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Crump KE, Sahingur SE. Microbial nucleic acid sensing in oral and systemic diseases. J Dent Res. 2016;95(1):17–25. doi: 10.1177/0022034515609062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Hajishengallis G. Immunomicrobial pathogenesis of periodontitis: keystones, pathobionts, and host response. Trends Immunol. 2014;35(1):3–11. doi: 10.1016/j.it.2013.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Bartold PM, Van Dyke TE. Periodontitis: a host-mediated disruption of microbial homeostasis. Unlearning learned concepts. Periodontol 2000. 2013;62(1):203–217. doi: 10.1111/j.1600-0757.2012.00450.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ide M, Papapanou PN. Epidemiology of association between maternal periodontal disease and adverse pregnancy outcomes — systematic review. J Periodontol. 2013;84(4 suppl):S181–S194. doi: 10.1902/jop.2013.134009. [DOI] [PubMed] [Google Scholar]
- 72.Lalla E, Papapanou PN. Diabetes mellitus and periodontitis: a tale of two common interrelated diseases. Nat Rev Endocrinol. 2011;7(12):738–748. doi: 10.1038/nrendo.2011.106. [DOI] [PubMed] [Google Scholar]
- 73.Linden GJ, Lyons A, Scannapieco FA. Periodontal systemic associations: review of the evidence. J Periodontol. 2013;84(4 suppl):S8–S19. doi: 10.1902/jop.2013.1340010. [DOI] [PubMed] [Google Scholar]
- 74.Schenkein HA, Loos BG. Inflammatory mechanisms linking periodontal diseases to cardiovascular diseases. J Periodontol. 2013;84(4 suppl):S51–S69. doi: 10.1902/jop.2013.134006. [DOI] [PubMed] [Google Scholar]
- 75.Sahingur SE, Yeudall WA. Chemokine function in periodontal disease and oral cavity cancer. Front Immunol. 2015;6:214. doi: 10.3389/fimmu.2015.00214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Martin P, DiMartini A, Feng S, Brown R, Fallon M. Evaluation for liver transplantation in adults: 2013 practice guideline by the American Association for the Study of Liver Diseases and the American Society of Transplantation. Hepatology. 2014;59(3):1144–1165. doi: 10.1002/hep.26972. [DOI] [PubMed] [Google Scholar]
- 77.Han P, Sun D, Yang J. Interaction between periodontitis and liver diseases. Biomed Rep. 2016;5(3):267–276. doi: 10.3892/br.2016.718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Li X, Kolltveit KM, Tronstad L, Olsen I. Systemic diseases caused by oral infection. Clin Microbiol Rev. 2000;13(4):547–558. doi: 10.1128/CMR.13.4.547-558.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Silva Santos PS, Fernandes KS, Gallottini MH. Assessment and management of oral health in liver transplant candidates. J Appl Oral Sci. 2012;20(2):241–245. doi: 10.1590/S1678-77572012000200020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Guggenheimer J, Eghtesad B, Close JM, Shay C, Fung JJ. Dental health status of liver transplant candidates. Liver Transpl. 2007;13(2):280–286. doi: 10.1002/lt.21038. [DOI] [PubMed] [Google Scholar]
- 81.Silva Santos PS, Fernandes KS, Gallottini MH. Assessment and management of oral health in liver transplant candidates. J Appl Oral Sci. 2012;20(2):241–245. doi: 10.1590/S1678-77572012000200020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Grønkjær LL. Periodontal disease and liver cirrhosis: a systematic review. SAGE Open Med. 2015;3:2050312115601122. doi: 10.1177/2050312115601122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Aberg F, Helenius-Hietala J, Meurman J, Isoniemi H. Association between dental infections and the clinical course of chronic liver disease. Hepatol Res. 2014;44(3):349–353. doi: 10.1111/hepr.12126. [DOI] [PubMed] [Google Scholar]
- 84.Yoneda M, et al. Involvement of a periodontal pathogen, Porphyromonas gingivalis on the pathogenesis of non-alcoholic fatty liver disease. BMC Gastroenterol. 2012;12:16. doi: 10.1186/1471-230X-12-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Nagao Y, Kawahigashi Y, Sata M. Association of periodontal diseases and liver fibrosis in patients with HCV and/or HBV infection. Hepat Mon. 2014;14(12):e23264. doi: 10.5812/hepatmon.23264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Grønkjær LL, et al. Presence and consequence of tooth periapical radiolucency in patients with cirrhosis. Hepat Med. 2016;8:97–103. doi: 10.2147/HMER.S113485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Novacek G, et al. Dental and periodontal disease in patients with cirrhosis — role of etiology of liver disease. J Hepatol. 1995;22(5):576–582. doi: 10.1016/0168-8278(95)80453-6. [DOI] [PubMed] [Google Scholar]
- 88.Raghava KV, Shivananda H, Mundinamane D, Boloor V, Thomas B. Evaluation of periodontal status in alcoholic liver cirrhosis patients: a comparative study. J Contemp Dent Pract. 2013;14(2):179–182. doi: 10.5005/jp-journals-10024-1296. [DOI] [PubMed] [Google Scholar]
- 89.Qin N, et al. Alterations of the human gut microbiome in liver cirrhosis. Nature. 2014;513(7516):59–64. doi: 10.1038/nature13568. [DOI] [PubMed] [Google Scholar]
- 90.Bajaj JS, et al. Systems biology analysis of omeprazole therapy in cirrhosis demonstrates significant shifts in gut microbiota composition and function. Am J Physiol Gastrointest Liver Physiol. 2014;307(10):G951–G957. doi: 10.1152/ajpgi.00268.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Hemarajata P, Versalovic J. Effects of probiotics on gut microbiota: mechanisms of intestinal immunomodulation and neuromodulation. Therap Adv Gastroenterol. 2013;6(1):39–51. doi: 10.1177/1756283X12459294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Bajaj JS, et al. Randomised clinical trial: Lactobacillus GG modulates gut microbiome, metabolome and endotoxemia in patients with cirrhosis. Aliment Pharmacol Ther. 2014;39(10):1113–1125. doi: 10.1111/apt.12695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Bajaj JS, et al. A longitudinal systems biology analysis of lactulose withdrawal in hepatic encephalopathy. Metab Brain Dis. 2012;27(2):205–215. doi: 10.1007/s11011-012-9303-0. [DOI] [PubMed] [Google Scholar]
- 94.Bajaj JS, et al. Modulation of the metabiome by rifaximin in patients with cirrhosis and minimal hepatic encephalopathy. PLoS One. 2013;8(4):e60042. doi: 10.1371/journal.pone.0060042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Sanyal A, et al. Randomised clinical trial: rifaximin improves health-related quality of life in cirrhotic patients with hepatic encephalopathy — a double-blind placebo-controlled study. Aliment Pharmacol Ther. 2011;34(8):853–861. doi: 10.1111/j.1365-2036.2011.04808.x. [DOI] [PubMed] [Google Scholar]
- 96.Bajaj JS, Barrett AC, Bortey E, Paterson C, Forbes WP. Prolonged remission from hepatic encephalopathy with rifaximin: results of a placebo crossover analysis. Aliment Pharmacol Ther. 2015;41(1):39–45. doi: 10.1111/apt.12993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Shen TC, et al. Engineering the gut microbiota to treat hyperammonemia. J Clin Invest. 2015;125(7):2841–2850. doi: 10.1172/JCI79214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Kao D, et al. Fecal microbiota transplantation in the management of hepatic encephalopathy. Hepatology. 2016;63(1):339–340. doi: 10.1002/hep.28121. [DOI] [PubMed] [Google Scholar]
- 99.Philips CA, et al. Healthy donor fecal microbiota transplantation in steroid-ineligible severe alcoholic hepatitis: A Pilot Study. Clin Gastroenterol Hepatol. 2017;15(4):600–602. doi: 10.1016/j.cgh.2016.10.029. [DOI] [PubMed] [Google Scholar]
- 100.Bajaj JS, et al. Fecal Microbiota Transplant from a Rational Stool Donor Improves Hepatic Encephalopathy: A Randomized Clinical Trial. Hepatology. doi: 10.1002/hep.29306. [published online ahead of print June 6, 2017]. https://doi.org/10.1002/hep.29306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Krasse P, Carlsson B, Dahl C, Paulsson A, Nilsson A, Sinkiewicz G. Decreased gum bleeding and reduced gingivitis by the probiotic Lactobacillus reuteri. Swed Dent J. 2006;30(2):55–60. [PubMed] [Google Scholar]
- 102.Matsuoko T, et al. Effect of oral Lactobacillus salivarius TI2711 (LS1) administration on periodontopathic bacteria in subgingival plaque. Nihon Shishubyo Gakkai Kaishi. 2006;48(4):315–324. doi: 10.2329/perio.48.315. [DOI] [Google Scholar]
- 103.Twetman S, Derawi B, Keller M, Ekstrand K, Yucel-Lindberg T, Stecksen-Blicks C. Short-term effect of chewing gums containing probiotic Lactobacillus reuteri on the levels of inflammatory mediators in gingival crevicular fluid. Acta Odontol Scand. 2009;67(1):19–24. doi: 10.1080/00016350802516170. [DOI] [PubMed] [Google Scholar]
- 104.Patel VC, Shawcross DL. Salivary microbiota-immune profiling in cirrhosis: could this be the noninvasive strategy that will revolutionize prognostication in hepatology? Hepatology. 2015;62(4):1001–1003. doi: 10.1002/hep.27870. [DOI] [PubMed] [Google Scholar]