Summary
In this Minireview, we provide an epidemiologist’s perspective on the debate and recent advances in determining the relationship between diet and cardiovascular health. We conclude that in order to reduce the global burden of cardiovascular disease, there should be a greater emphasis on improving overall diet quality and food sources of macronutrients such as dietary fats and carbohydrates. In addition, building a strong evidence base through high-quality intervention and observational studies is crucial for effective policy changes, which can greatly improve the food environment and population health.
Introduction
Cardiovascular disease (CVD), specifically coronary heart disease and stroke, is the leading cause of death and disability-adjusted life years for all regions of the world (Roth et al., 2017). In 2015, there were an estimated 422.7 million cases of CVD and 17.92 million CVD deaths globally, which accounted for approximately one third of total deaths (Roth et al., 2017). Between 1990 and 2015, the age-standardized global death rate attributable to CVD dropped by 24%, mainly driven by declines in all high-income and some middle-income countries; however, the total number of CVD deaths increased by 41%, mostly attributable to population growth and aging (Roth et al., 2017). Currently, approximately 80% of CVD deaths occur in low- and middle-income countries (Roth et al., 2017), where health care infrastructures and access to treatment are limited. Therefore, effective approaches for the prevention of CVD are crucial to reduce the future disease burden and improve population health.
Among the many established risk factors for CVD, diet plays an important role (Forouzanfar et al., 2015). In the past several decades, numerous studies have enhanced our understanding of the relationship between diet and cardiovascular health. However, divergent results have created confusion among patients, health professionals, and the general public. A recent study from the Prospective Urban and Rural Epidemiology (PURE) cohort (Dehghan et al., 2017) has generated sensational headlines in the media and stirred debate in the scientific community. This study aimed to clarify the relationship between macronutrient intake and mortality, but the findings appeared to contradict those from previous studies and prevailing dietary recommendations and guidelines. By analyzing self-reported dietary data from more than 135,000 people in 18 countries and following the participants over a 7-year period, the authors concluded that “high carbohydrate intake was associated with higher risk of total mortality, whereas total fat and individual types of fat were related to lower total mortality.” In this Minireview, we described recent advances in nutritional epidemiologic studies of dietary fats and carbohydrates and cardiovascular health. We then discussed methodological issues in the PURE study. Finally, we proposed some opportunities and challenges moving forward.
Recent advances in epidemiologic study designs
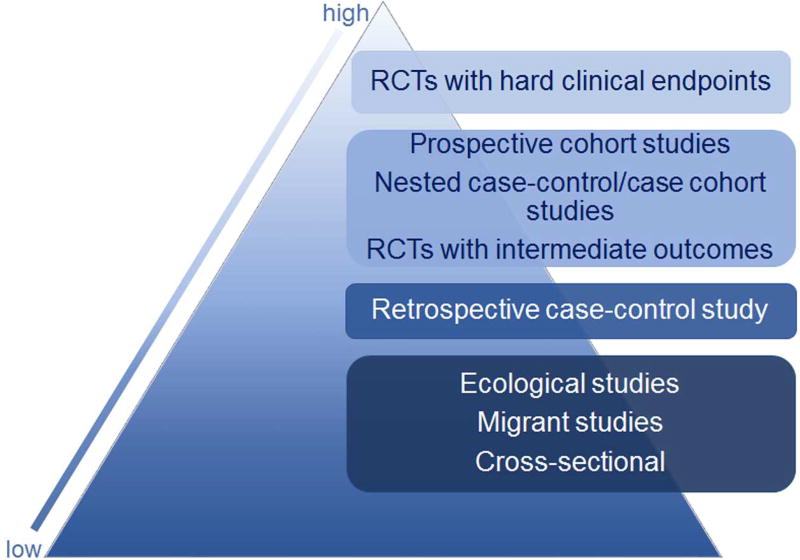
Randomized clinical trials (RCTs), particularly those that are high-quality and double-blind, are the gold standard for determining causation between an exposure and an outcome and thus are the cornerstone for medical guidelines and health policy (Figure 1). A double-blind RCT can minimize or eliminate confounding, which is a major challenge in observational studies. Ideally, RCTs should be used to examine the effect of a nutrient or food on cardiovascular events, in the same way as required for approving new drugs and medical devices. In cases with supplements, RCTs are a practical choice. For example, the Alpha Omega Trial evaluated the effects of n−3 fatty acid supplementation (EPA/DHA and/or alpha-linolenic acid) and cardiovascular events among 4837 patients with myocardial infarction (Kromhout et al., 2010).
Figure 1.
The typical hierarchy of study designs based on ability to infer causality
However, there are multiple reasons why RCTs are not feasible for many nutrients and foods, including macronutrients. To achieve valid results, the difference in intake levels between the treatment and control groups must be biologically meaningful and sustained for a sufficient period. For cardiovascular events, the intervention period would need to be at least several years. Additionally, a large sample size is needed to obtain sufficient statistical power. It is also difficult to maintain a high adherence rate when assigning participants to a diet that differs from their usual diet. For example, the Women’s Health Initiative (WHI) Randomized Controlled Dietary Modification Trial (Howard et al., 2006) studied the effects of decreasing total dietary fat on cancer and CVD outcomes. The study enrolled 48,835 women aged 50–79 years between 1993 and 1998 and randomly assigned them to a low-fat diet (20% of energy intake from fat) or to maintain their usual high-fat diet (37% of energy intake from fat). After a mean follow-up period of 8.1 years, most people in the low-fat group did not achieve the goal to reduce fat to 20% of energy intake. Overall, no significant effect on CVD outcomes was observed. An additional challenge of dietary interventions is that participants cannot be blinded from dietary assignment because they need to change their food choices to achieve the intervention diet. In the WHI, in addition to reducing fat, the intervention group reported significant increases in fiber, vegetables and fruits, total and whole grains, and soy. Thus, it is difficult to isolate the effects of specific macronutrients. Despite these challenges, well-conducted RCTs, if feasible, are essential to examine the effects of nutrients, foods, and dietary patterns on health outcomes and develop evidence-based recommendations. For example, the DASH trial (Dietary Approaches to Stop Hypertension) (Sacks et al., 2001) and the PREDIMED trial (Prevención con Dieta Mediterránea) (Estruch et al., 2013) have provided strong evidence to support the role of healthy dietary patterns in primary prevention of hypertension through adherence to the DASH dietary pattern and cardiovascular disease through adherence to the Mediterranean-style dietary pattern.
Due to the constraints of RCTs, prospective cohort studies are the preferred observational study design to examine the association between diet and CVD (Satija et al., 2015) (Figure 1). With this design, researchers follow a large population of participants for a certain period of time and do not intervene to change dietary habits. In many cohort studies, dietary intake data are collected at baseline when participants are enrolled and CVD and other health outcomes are assessed during follow-up. Dietary data are typically calculated from validated food-frequency questionnaires (FFQs) or 24-hour dietary recalls and are sometimes collected from multiple-day dietary records. The advantages and disadvantages of different dietary measurement methods are extensively discussed elsewhere (Satija et al., 2015; Willett, 2013). Self-reported data are subject to both random and systematic measurement errors. The random errors are typically present in 24-hour recalls and derived from the large day-to-day variation in dietary intake in free-living individuals, which could substantially attenuate the strength of the associations (e.g., correlation coefficients, regression coefficients and relative risks) (Willett, 2013). Therefore, studies often use repeated 24-hour recalls on nonconsecutive days to reduce this type of error (Willett, 2013). FFQs typically have fewer random errors but are subject to systematic errors due to omission of food items and inaccurate nutrient composition databases. One common solution is to use energy-adjusted nutrients in the analysis. Because both the specific nutrients and total energy are derived from the same foods in the FFQ, the measurement errors (over-reporting or under-reporting) in the nutrients and total energy are likely to be correlated (Willett, 2013). Stastistically, the correlated errors can be reduced by adjusting for total energy intake. To address concerns that single-time measures do not represent long-term patterns, more studies are now collecting repeated dietary measures during follow-up. An example is the Nurses’ Health Study, where diet was evaluated every four years using validated semi-quantitative FFQs during more than three decades of follow-up (Bao et al., 2016). Furthermore, repeated dietary measures with validation data also reduce the impact of measurement errors and misclassifications. Detailed methods of measurement error corrections are described elsewhere (Spiegelman, 2016).
Results from prospective cohort studies and RCTs may not be always consistent. For example, a number of cohort studies have reported that antioxidant vitamins (e.g., vitamin C and E) are inversely associated with CVD (Knekt et al., 2004) but most RCTs have indicated that supplementation with these vitamins does not provide beneficial effects (Myung et al., 2013). This discrepancy may be due to the fact that RCTs usually select high-risk populations and the duration of the supplementation is relatively short (3–5 years) compared to observational studies. In addition, residual confounding by socioeconomic status and a more healthy diet and lifestyle in observational studies may partially explain an inverse association between antioxidant vitamins and risk of CVD (Lawlor et al., 2004). It is also likely that antioxidants from high dose supplements have different effects than those from dietary sources where these vitamins come together with other beneficial nutrients such as fiber, minerals, and polyphenols.
Confounding needs to be carefully considered in all observational studies, including prospective cohorts, as participants with different dietary patterns may also differ in other characteristics. All relevant confounders should be carefully identified before study initiation and systematically collected during the study. Residual confounding can be reduced by multivariate regression models with proper adjustment for confounders as well as by stratified analyses or restricting analyses to a specific subgroup. Compared to other observational methods, such as retrospective case-control or cross-sectional studies, prospective cohort studies are less affected by reverse causation, recall bias and selection bias. Reverse causation is reduced because exposures are measured years before the ascertainment of the outcomes. The participants are disease-free at baseline, which reduces recall bias. Incident cases are documented through follow-up, which minimizes selection bias because the cases and non-cases are obtained from the same population. However, biases due to non-differential loss to follow-up and other reasons still need to be considered in cohort studies.
Many prospective cohort studies have been conducted in the USA and Europe, for example, the Framingham Heart Study (Mahmood et al., 2014), Nurses’ Health Study (Bao et al., 2016), and UK Biobank study (Collins, 2012). More cohort studies are now being conducted in developing countries and in populations undergoing rapid nutrition and economic transitions. An example is the China Kadoorie Biobank study which recruited 512,891 adults in 10 regions of China beginning in 2004 (Chen et al., 2011). The study aims to investigate lifestyle, environmental, and genetic determinants of chronic diseases in the Chinese population..
Recently, many cohort studies have formed consortia or initiated pooling projects to increase sample size, evaluate heterogeneity across different populations, and increase generalizability of their findings (Smith-Warner et al., 2006). Multi-center cohort studies are another type of international collaboration which are conducted in various locations under the same or similar protocols. One example is the European Prospective Investigation into Cancer and Nutrition (EPIC) study (Bingham and Riboli, 2004), which recruited half a million participants across 10 European countries and followed them for almost 15 years.
Another advancement in nutritional epidemiology is the ability to measure dietary biomarkers in stored biospecimens (blood, urine or other biofluids) in cohort studies and analyze their relationship with disease outcomes. This may be the only option for estimating intake for nutrients that are not available in food composition tables or that vary widely within the same foods due to variability in production, storage, processing, or preparation. Biomarkers are established for some nutrients (e.g., protein intake by urinary nitrogen, salt intake by urinary sodium/potassium, and essential dietary fatty acids in plasma or erythrocytes); however, there are no specific biomarkers for most individual foods or for total dietary fat or carbohydrate. Additionally, while biomarker measurements are objective and avoid recall bias, these short-term measures may not adequately represent long-term dietary exposure. Therefore, dietary biomarker measurements are complementary to, rather than a replacement for, the self-reported methods in nutritional epidemiologic studies (Satija et al., 2015).
Cardiovascular health effects of dietary fat and carbohydrate
Quality of carbohydrate
Carbohydrates are found in a wide variety of foods and make up the majority of daily energy for most individuals. According to their degree of polymerization and chemical structure, carbohydrates may be divided into sugars, oligosaccharides and polysaccharides, with the latter two also grouped as complex carbohydrate. However, many complex carbohydrates (e.g. potatoes and white bread) still produce a very high glycemic response (Atkinson et al., 2008). Thus, this classification based on chemical distinction has little value for determining the nutritional quality of carbohydrates. The glycemic index (GI) and glycemic load (GL) concepts were developed to rank carbohydrate-rich foods based on the speed and magnitude of their effect on blood glucose levels (Atkinson et al., 2008). GI measures how quickly the carbohydrates in a food raise a person’s blood glucose level, and GL further takes into account the amount of digestible carbohydrate in the food. In large cohort studies, higher dietary GI and GL have been associated with increased risks of type 2 diabetes (Bhupathiraju et al., 2014) and CVD (Ma et al., 2012).
Other useful indicators of carbohydrate quality include the amount and type of dietary fiber and the extent of processing (refined grains versus whole grains). Studies have consistently shown that greater dietary fiber intake is associated with lower risk of both type 2 diabetes (InterAct Consortium, 2015) and CVD (Threapleton et al., 2013; Wu et al., 2015). There is also evidence that whole grains are associated with lower risk of diabetes (Aune et al., 2013) and CVD (Zong et al., 2016). In many populations, added sugar and sugar-sweetened beverages are significant sources of carbohydrates and daily energy, and their detrimental effects on body weight (Malik et al., 2013), obesity, diabetes and CVD have been well-documented (Malik and Hu, 2015).
Quality of fat
Mounting evidence indicates that different types of fat have divergent effects on health. The American Heart Association Presidential Advisory Report reviewed evidence from RCTs and prospective cohort studies and estimated that replacing 5% of energy intake from saturated fats with equivalent intake from polyunsaturated fats or monounsaturated fats was associated with a 25% and 15% lower risk of CHD, respectively (Sacks et al., 2017). Replacing saturated fats with carbohydrates from refined sources (refined starches and added sugars) was not significantly associated with CHD risk, whereas replacing saturated fats with whole grains was associated with a 9% lower risk of CHD (Sacks et al., 2017). Therefore, when considering the cardiovascular health effects of different types of fat, it is crucial to determine which macronutrients or foods are replacing a reduction in saturated fat. Based on the current evidence, the 2015–2020 Dietary Guidelines for Americans (DGA) eliminated the previous upper limit for total fat intake but recommended reducing saturated fats to less than 10% of calories and replacing them with unsaturated fats (U.S. Department of Health and Human Services and U.S. Department of Agriculture, 2015).
Beyond the single nutrient: the importance of dietary patterns
Studies have evolved from examining individual foods and nutrients towards using dietary patterns to represent the combined effects of foods and beverages in different diets. Dietary pattern analysis accounts for complex interactions among nutrients and foods as well as the cumulative effect of the overall diet, which may be more powerful than each component’s individual effect (Hu, 2002). Extensive evidence from prospective cohort studies has demonstrated that following the Mediterranean-style (Martinez-Gonzalez and Bes-Rastrollo, 2014; Sofi et al., 2014), Dietary Approaches to Stop Hypertension (DASH) (Salehi-Abargouei et al., 2013), and Alternative Healthy Eating Index (AHEI) dietary patterns (Chiuve et al., 2012) is associated with substantially reduced risk of CVD. A recent analysis using repeated dietary measurements every four years from the Nurses' Health Study and Health Professionals Follow-up Study further demonstrated that improved diet quality (according to Mediterranean-style diet, DASH and AHEI scores) was consistently associated with a lower CVD risk in both the short term (subsequent 4 years) and long-term (subsequent 20 years) (Sotos-Prieto et al., 2015). These studies indicate that individual and population cardiovascular health can be substantially improved with greater adherence to healthy dietary patterns. Although there are multiple healthy dietary patterns which differ in their specific components and methodologies for assessing adherence, a healthy dietary pattern is generally high in vegetables, fruits, whole grains, seafood and fatty fish, legumes, and nuts; moderate in low-fat and nonfat dairy products; lower in red and processed meat; and low in refined grains and foods and beverages containing added sugars.
Methodological issues in the PURE study
When interpreting the PURE study findings, it is crucial to consider the study methodology as well as the importance of macronutrient quality and dietary patterns in the context set above. Beginning in 2003, the PURE study collected self-reported dietary data using FFQs at baseline from 135,000 participants in 18 countries. After tracking participants’ health over an average of seven years, researchers found that those with the highest intake of dietary fat (35% of daily calories on average) were 23% less likely to have died than those with the lowest intake (10% of daily calories on average). Oppositely, for carbohydrates, those with the highest intake (77% of daily calories on average) were 28% more likely to have died than those with the lowest intake (46% of daily calories on average). The authors concluded that higher fat intake was associated with decreased mortality while higher carbohydrate intake was associated with increased mortality. Although this study had a large sample size and included participants from many countries, the results need to be interpreted with caution due to the following methodological issues.
First, grouping all carbohydrates together is overly simplistic because different types of carbohydrates have opposing effects on health. Studies have consistently demonstrated that refined carbohydrates are associated with increased risk whereas whole grains are associated with decreased risk of type 2 diabetes (Aune et al., 2013; Hu et al., 2012) and CVD (Zong et al., 2016).
Second, in many developing countries such as those included in the PURE study, people subsist on a “poverty diet” which contains little fat and many refined carbohydrates, such as white rice and refined wheat products. Therefore, when attempting to compare high versus low saturated fat intake, the study actually compared participants with high saturated fat intake to those with high refined carbohydrate intake. The authors reported that saturated fat was not significantly associated with CVD, which is not surprising given that saturated fat was essentially compared with refined carbohydrates in the analyses. In addition, the association between carbohydrate intake and mortality risk was mainly driven by non-CVD mortality, such as deaths from respiratory, liver and infectious diseases. Low-income people in developing countries tend to bear the burden of these types of diseases, as well as consume high-carbohydrate diets. Therefore, an association between high carbohydrate intake and non-CVD mortality is likely to be confounded by poverty, food insecurity, undernutrition and lack of medical care access.
Third, the PURE study population was highly heterogeneous, consisting of participants from rural and urban areas of 18 countries with different levels of socioeconomic development. The dietary patterns, food choices, lifestyle habits, cultural backgrounds, and disease patterns differed considerably across various countries and regions. Therefore, country-specific analyses, region-specific analyses and urban-rural stratified analyses are needed to better understand the observed associations.
Fourth, the macronutrient compositions presented in the PURE study as the healthiest (roughly 50% carbohydrate, 30–35% fat, 15–20% protein) are very close to current dietary recommendations (Food and Agriculture Organization of the United Nations, 2010). Therefore, the PURE study’s conclusion that “global dietary guidelines should be reconsidered in light of these findings” is not supported by its own data.
Finally, the dietary intake data for the Chinese participants, who made up one third of the PURE study sample, were not consistent with data from other studies conducted in China. Fat intake in China has been increasing since the 1990s, coupled with a decrease in carbohydrate intake. In parallel with these dietary changes, rates of obesity, hypertension, and diabetes have increased considerably (Figure 2). National surveys reported that the Chinese population currently consumes an average of 30% of their daily calories from fat. However, the PURE study reported an average total fat intake of 17.7% in the Chinese participants. The PURE study used the same FFQ as the 2002 China National Nutrition and Health Survey. This FFQ has been validated among 271 healthy adults between 1999 and 2001 by comparing the data from the FFQ and 18 days of 24-hour recalls throughout one year. In that validation study, the energy contribution from carbohydrate, fat and protein was 58.8%, 27.3% and 12.9%, respectively. The large discrepancies in dietary data in the PURE study compared to the FFQ validation study and other Chinese national surveys casts doubt on the validity of the PURE study’s dietary assessment procedures. Surprisingly, vegetable oils, which are major sources of dietary fat in Chinese adults, were not on the PURE study’s list of top food contributors for dietary fat.
Figure 2.
Trends in energy intake from carbohydrate and fat and corresponding increase in obesity-related chronic diseases in China (1992–2012).
Data on percentage of carbohydrate and fat intake as well as the prevalence of overweight and obesity are from Chinese nutrition and health surveillance reports in 2002 (National Health and Family Planning Commission of the People’s Republic of China, 2004) and 2012 (Chang and Wang, 2016). The surveillance reports used the Chinese cut-off point defining overweight as 24≤BMI<28, and obesity as BMI ≥28. The data extracted here were among adults (>18 years). The prevalence of hypertension in adults was 13.6% in 1991 (Tao et al., 1995), 17.7% in 2002 (Wu et al., 2008), and 33.5% in 2010 (Li et al., 2012). The prevalence of diabetes in adults was 2.5% in 1994 (Pan et al., 1997), 5.5% in 2000 to 2001 (Gu et al., 2003), and 10.9% in 2013 (Wang et al., 2017).
National Health and Family Planning Commission of the People’s Republic of China (2004). The nutrition and health status of the Chinese people [Chinese]. Available at http://www.moh.gov.cn/wsb/pzcjd/200804/21290.shtml.
Chang, J.L., Wang, Y. (2016). Chinese Nutrition and Health Surveillance: 2010–2013 Report [Chinese] (Beijing, China: Peking University Medical Press).
Tao, S., Wu, X., Duan, X., Fang, W., Hao, J., Fan, D., Wang, W., Li, Y. (1995). Hypertension prevalence and status of awareness, treatment and control in China. Chin. Med. J. 108, 483–489.
Wu, Y., Huxley, R., Li, L., Anna, V., Xie, G., Yao, C., Woodward, M., Li, X., Chalmers, J., Gao, R., et al. (2008). Prevalence, awareness, treatment, and control of hypertension in China: data from the China National Nutrition and Health Survey 2002. Circulation 118, 2679–2686.
Li, Y.C., Wang, L.M., Jiang, Y., Li, X.Y., Zhang, M., Hu, N. (2012). Prevalence of hypertension among Chinese adults in 2010 [Chinese]. Chin. J. Prev. Med. 46, 409–413.
Pan, X.R., Yang, W.Y., Li, G.W., Liu, J. (1997). Prevalence of diabetes and its risk factors in china, 1994. National diabetes prevention and control cooperative group. Diabetes Care 20, 1664–1669.
Gu, D., Reynolds, K., Duan, X., Xin, X., Chen, J., Wu, X., Mo, J., Whelton, P.K., He, J.; InterASIA Collaborative Group. (2003). Prevalence of diabetes and impaired fasting glucose in the Chinese adult population: international collaborative study of cardiovascular disease in Asia (InterASIA). Diabetologia 46, 1190–1198.
Wang, L., Gao, P., Zhang, M., Huang, Z., Zhang, D., Deng, Q., Li, Y., Zhao, Z., Qin, X., Jin, D., et al. (2017). Prevalence and ethnic pattern of diabetes and prediabetes in China in 2013. JAMA 317, 2515–2523.
In summary, despite the large study population from multiple countries, the PURE results need to be interpreted in the context of the existing literature and various methodological issues in data collection, analysis and interpretation. Overall, the study results did not appear to challenge the existing recommendations that are focused on healthy sources of fats and carbohydrates.
Opportunities and challenges
Inferring causality in observational studies
Although confounding and bias cannot be completely eliminated from observational studies, causality can still be inferred based on the totality of evidence. When examining causality in observational studies, it is useful to consider the Hill checklist (Hill, 1965): strength, consistency, temporality, biological gradient (dose-response), plausibility, coherence, and experimental evidence. Systematic reviews and meta-analyses are now widely used to summarize relevant literature, synthesize aggregate data and evaluate the totality of evidence. However, poorly designed and executed meta-analyses regarding diet and health can generate misleading findings and spread inaccurate information to the public (Barnard et al., 2017). When conducting and interpreting meta-analyses on diet and health, it is crucial to exercise caution because meta-analyses are susceptible to limitations such as publication bias as well as heterogeneity in quality of included studies (Barnard et al., 2017). Furthermore, to infer causality, findings from different types of exposures (i.e., dietary patterns, foods, nutrients, and biomarkers) and different types of study designs (e.g., animal studies, mechanistic studies in humans, prospective cohort studies, RCTs of intermediate and hard endpoints, and meta-analyses) should be evaluated together. Although RCTs of diet and disease outcomes are challenging in most situations, they should still be considered whenever feasible. Experimental studies are useful to provide insights into the underlying mechanisms and pathways linking diet to health, which is an important element in determining causality. Consistent evidence from different types of study designs is necessary to arrive at a consensus to infer causality and inform policy. For example, trans-fat was consistently associated with higher risk of CHD in observational studies and increased total and LDL cholesterol in small RCTs (Mozaffarian et al., 2009). Evidence from animal experiments also supported the role of trans-fat intake in the development of atherosclerosis (Micha and Mozaffarian, 2009). The consistent evidence from different types of studies provides a strong foundation for the recommendation and policies to reduce trans-fat intake.
Improving diet assessment
Currently, a variety of dietary assessment methods are widely used including FFQs, dietary recalls, dietary records, biochemical measurements and anthropometric measurements. Each method has advantages and disadvantages and may provide complementary information (Satija et al., 2015). The choice of method should be based on the scientific questions as well as the potential available resources. Whenever possible, repeated measures of diet should be collected to improve data quality. New technologies offer the potential to collect data easily and with immediate feedback. The National Cancer Institute developed the web-based Automated Self-Administered 24-hour dietary recall system, which uses digital images to improve participants’ estimation of intake and portion size (Kirkpatrick et al., 2016; Kirkpatrick et al., 2014). Additionally, automatic food image recognition systems have been developed to track dietary intake using mobile applications and cameras on tablets and smartphones (Boushey et al., 2017). However, the validity and feasibility of using these recent methods in large epidemiological studies have not yet been established.
The role of precision nutrition
Recent advances in “omics” technologies have allowed researchers to assess a large number of genomic, epigenomic, transcriptomic, proteomic, metabolomic, and microbiomic traits from biological specimens using high throughput methods. “Systems epidemiology” refers to the integration of such technologies into epidemiological studies (Cornelis and Hu, 2013), and can provide insight into the biological mechanisms underlying diet and health. This approach can also identify biomarkers for specific dietary components, enabling us to achieve better diet and nutritional assessment in free-living populations (Scalbert et al., 2014). Precision nutrition (also called personalized nutrition) aims to use the systems epidemiology approach to prevent diseases by adapting nutrition interventions and recommendations based on individual metabolic profiles and genetic backgrounds.
Recently, gene-environment interaction studies have provided evidence that the genetic risk of obesity, diabetes, and CVD can be mitigated by physical activity and healthy diets. Healthy dietary patterns have been found to reduce the effects of genetic variants on type 2 diabetes (Cornelis and Hu, 2012) and CVD (Do et al., 2011; Parnell et al., 2014). On the other hand, the detrimental effects of an unhealthy diet may be augmented by genetic susceptibility. For example, in a study of three U.S. cohorts, the genetic effect on obesity risk was stronger in participants with high sugar-sweetened beverage intake (Qi et al., 2012).
High-throughput metabolomics studies in cohorts of different populations have found that higher plasma levels of branched chain amino acids (including leucine, isoleucine and valine) and aromatic amino acids (including tyrosine and phenylalanine) were associated with an increased risk of type 2 diabetes (Guasch-Ferre et al., 2016; Lu et al., 2016; Qiu et al., 2016). Lipid metabolites (such as ceramides, cholesterol esters, monounsaturated fatty acid, omega-6 fatty acids, and docosahexaenoic acids) (Toledo et al., 2017; Wang et al., 2017; Wurtz et al., 2015) and amino acids (such as phenylalanine and tryptophan) (Wurtz et al., 2015; Yu et al., 2017) have also been associated with CVD risk. Trimethylamine-N-oxide, a metabolite produced by the interaction of gut bacteria with dietary intake of phosphatidylcholine and carnitine, components typically found in a meat-based diet, has also been associated with CVD (Koeth et al., 2013; Tang et al., 2013), although the results are not entirely consistent.
Omics technologies have offered promising opportunities in nutritional epidemiologic studies to assess individuals’ characteristics including the genome, epigenome, metabolome, and microbiome. However, it is still premature to prescribe personalized diets for prevention of CVD based on these individual characteristics. The rapid advances in wearable devices, mobile applications, big data analytics, and innovative educational and behavioral interventions will aid the development of precision prevention to improve both individual and population health (O'Sullivan et al., 2017).
Informing evidence-based guidelines
The DGA are largely based on extensive review of current evidence and are established through multiple methods such as original and existing systematic reviews, meta-analyses, food pattern modeling, and descriptive data analysis. Following the evolution in nutritional sciences, dietary guidelines are shifting their focus from individual nutrients to food quality and overall dietary patterns. The 2015–2020 DGA recommend multiple eating patterns including the Mediterranean-style pattern, healthy vegetarian pattern, and healthy USDA pattern and emphasize that these patterns can be tailored to individuals’ cultural and food preferences and health conditions. Furthermore, a large body of evidence has demonstrated that regular physical activity is beneficial for reducing the risk of chronic diseases (U.S. Department of Health and Human Services, 2008). Therefore, the 2015–2020 DGA also include a key recommendation to “Meet the Physical Activity Guidelines for Americans”. It is important to consider the combined effects of diet and physical activity in an overall healthy lifestyle. Studies in different populations have demonstrated that adherence to a combination of healthy lifestyle factors (including but not limited to a generally healthy diet, being physically active, not smoking, and maintaining a healthy weight) has a profound impact on improving cardiovascular health (Stampfer et al., 2000; Odegaard et al., 2011; Carlsson et al., 2013; Veronese et al., 2016; Lv et al., 2017).
Conclusions and Future Perspectives
Nutritional epidemiology has greatly enhanced our understanding of the complex relationship between diet and cardiovascular health. Due to the constraints in conducting RCTs with nutrients and foods, large prospective cohort studies have been the predominant nutritional epidemiologic study design. Understanding the unique design and analytic issues in the field is crucial when interpreting findings and determining the validity of findings from different types of studies. Biases and confounding issues need to be carefully considered and the totality of evidence should be thoroughly evaluated to reach a consensus and inform policy. To achieve better cardiovascular health, existing evidence strongly supports an overall healthy dietary pattern that emphasizes quality and healthy sources of fats and carbohydrates rather than the absolute amounts of fats or carbohydrates in the diet. Building a strong evidence base through high-quality observational and intervention studies is critical for effective policy changes, which can greatly improve the food environment and population health. With recent advances in study design, dietary assessment methods, omics technologies, and big data analytics, the field of nutritional epidemiology is evolving rapidly and will continue to play an indispensable role in furthering our understanding of the role of diet in cardiovascular health and in translating nutritional sciences into policies and practice.
This review provides a nutritional epidemiologic perspective on the recent debate and advances in determining the relationship between diet and cardiovascular health. To reduce the global cardiovascular disease burden, high-quality intervention and observational studies are needed to inform policies to improve overall diet quality and dietary sources of fats and carbohydrates.
Acknowledgments
We thank Liting Sheng for helping with the figures. A.P. was supported by the National Key Research and Development Program of China (2017YFC0907504). X. L. is supported by the National Key Research and Development Program of China (2017YFC0909700) and the Chinese Academy of Sciences (ZDBS-SSW-DQC-02). F.B.H. was supported by the National Institute of Health grants (R01 DK102896, R01 HL060712, and R01 HL118264).
Dr. Frank Hu has received research support from the California Walnut Commission and an honorarium from Metagenics.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declaration of Interests
An Pan, Xu Lin and Elena Hemler declare no competing interests.
References
- U.S. Department of Health and Human Services and U.S. Department of Agriculture. 2015 – 2020 Dietary Guidelines for Americans. (8) 2015 Dec; Available at https://health.gov/dietaryguidelines/2015/guidelines/
- Atkinson FS, Foster-Powell K, Brand-Miller JC. International tables of glycemic index and glycemic load values: 2008. Diabetes Care. 2008;31:2281–2283. doi: 10.2337/dc08-1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aune D, Norat T, Romundstad P, Vatten LJ. Whole grain and refined grain consumption and the risk of type 2 diabetes: a systematic review and dose-response meta-analysis of cohort studies. Eur. J. Epidemiol. 2013;28:845–858. doi: 10.1007/s10654-013-9852-5. [DOI] [PubMed] [Google Scholar]
- Bao Y, Bertoia ML, Lenart EB, Stampfer MJ, Willett WC, Speizer FE, Chavarro JE. Origin, methods, and evolution of the three Nurses' Health Studies. Am. J. Public Health. 2016;106:1573–1581. doi: 10.2105/AJPH.2016.303338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnard ND, Willett WC, Ding EL. The misuse of meta-analysis in nutrition research. JAMA. 2017;318:1435–1436. doi: 10.1001/jama.2017.12083. [DOI] [PubMed] [Google Scholar]
- Bhupathiraju SN, Tobias DK, Malik VS, Pan A, Hruby A, Manson JE, Willett WC, Hu FB. Glycemic index, glycemic load, and risk of type 2 diabetes: results from 3 large US cohorts and an updated meta-analysis. Am. J. Clin. Nutr. 2014;100:218–232. doi: 10.3945/ajcn.113.079533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bingham S, Riboli E. Diet and cancer--the European Prospective Investigation into Cancer and Nutrition. Nat. Rev. Cancer. 2004;4:206–215. doi: 10.1038/nrc1298. [DOI] [PubMed] [Google Scholar]
- Boushey CJ, Spoden M, Zhu FM, Delp EJ, Kerr DA. New mobile methods for dietary assessment: review of image-assisted and image-based dietary assessment methods. Proc. Nutr. Soc. 2017;76:283–294. doi: 10.1017/S0029665116002913. [DOI] [PubMed] [Google Scholar]
- Carlsson AC, Wändell PE, Gigante B, Leander K, Hellenius ML, de Faire U. Seven modifiable lifestyle factors predict reduced risk for ischemic cardiovascular disease and all-cause mortality regardless of body mass index: a cohort study. Int. J. Cardiol. 2013;168:946–952. doi: 10.1016/j.ijcard.2012.10.045. [DOI] [PubMed] [Google Scholar]
- Chen Z, Chen J, Collins R, Guo Y, Peto R, Wu F, Li L. China Kadoorie Biobank of 0.5 million people: survey methods, baseline characteristics and long-term follow-up. Int. J. Epidemiol. 2011;40:1652–1666. doi: 10.1093/ije/dyr120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiuve SE, Fung TT, Rimm EB, Hu FB, McCullough ML, Wang M, Stampfer MJ, Willett WC. Alternative dietary indices both strongly predict risk of chronic disease. J. Nutr. 2012;142:1009–1018. doi: 10.3945/jn.111.157222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins R. What makes UK Biobank special? Lancet. 2012;379:1173–1174. doi: 10.1016/S0140-6736(12)60404-8. [DOI] [PubMed] [Google Scholar]
- Cornelis MC, Hu FB. Gene-environment interactions in the development of type 2 diabetes: recent progress and continuing challenges. Annu. Rev. Nutr. 2012;32:245–259. doi: 10.1146/annurev-nutr-071811-150648. [DOI] [PubMed] [Google Scholar]
- Cornelis MC, Hu FB. Systems epidemiology: a new direction in nutrition and metabolic disease research. Curr. Nutr. Rep. 2013;2 doi: 10.1007/s13668-013-0052-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dehghan M, Mente A, Zhang X, Swaminathan S, Li W, Mohan V, Iqbal R, Kumar R, Wentzel-Viljoen E, Rosengren A, et al. Associations of fats and carbohydrate intake with cardiovascular disease and mortality in 18 countries from five continents (PURE): a prospective cohort study. Lancet. 2017;390:2050–2062. doi: 10.1016/S0140-6736(17)32252-3. [DOI] [PubMed] [Google Scholar]
- Do R, Xie C, Zhang X, Mannisto S, Harald K, Islam S, Bailey SD, Rangarajan S, McQueen MJ, Diaz R, et al. The effect of chromosome 9p21 variants on cardiovascular disease may be modified by dietary intake: evidence from a case/control and a prospective study. PLoS Med. 2011;8:e1001106. doi: 10.1371/journal.pmed.1001106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Estruch R, Ros E, Salas-Salvado J, Covas MI, Corella D, Aros F, Gomez-Gracia E, Ruiz-Gutierrez V, Fiol M, Lapetra J, et al. Primary prevention of cardiovascular disease with a Mediterranean diet. N. Engl. J. Med. 2013;368:1279–1290. doi: 10.1056/NEJMc1806491. [DOI] [PubMed] [Google Scholar]
- Food and Agriculture Organization of the United Nations. Fats and fatty acids in human nutrition: report of an expert consultation. FAO Food and Nutrition Paper 91; Rome: 2010. [Accessed on January 9, 2018]. http://www.who.int/nutrition/publications/nutrientrequirements/fatsandfattyacids_humannutrition/en/ [PubMed] [Google Scholar]
- Forouzanfar MH, Alexander L, Anderson HR, Bachman VF, Biryukov S, Brauer M, Burnett R, Casey D, Coates MM, Cohen A, et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386:2287–2323. doi: 10.1016/S0140-6736(15)00128-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guasch-Ferre M, Hruby A, Toledo E, Clish CB, Martinez-Gonzalez MA, Salas-Salvado J, Hu FB. Metabolomics in prediabetes and diabetes: a systematic review and meta-analysis. Diabetes Care. 2016;39:833–846. doi: 10.2337/dc15-2251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill AB. The environment and disease: association or causation? Proc. R. Soc. Med. 1965;58:295–300. [PMC free article] [PubMed] [Google Scholar]
- Howard BV, Van Horn L, Hsia J, Manson JE, Stefanick ML, Wassertheil-Smoller S, Kuller LH, LaCroix AZ, Langer RD, Lasser NL, et al. Low-fat dietary pattern and risk of cardiovascular disease: the Women's Health Initiative Randomized Controlled Dietary Modification Trial. JAMA. 2006;295:655–666. doi: 10.1001/jama.295.6.655. [DOI] [PubMed] [Google Scholar]
- Hu EA, Pan A, Malik V, Sun Q. White rice consumption and risk of type 2 diabetes: meta-analysis and systematic review. BMJ. 2012;344:e1454. doi: 10.1136/bmj.e1454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu FB. Dietary pattern analysis: a new direction in nutritional epidemiology. Curr. Opin. Lipidol. 2002;13:3–9. doi: 10.1097/00041433-200202000-00002. [DOI] [PubMed] [Google Scholar]
- InterAct Consortium. Dietary fibre and incidence of type 2 diabetes in eight European countries: the EPIC-InterAct Study and a meta-analysis of prospective studies. Diabetologia. 2015;58:1394–1408. doi: 10.1007/s00125-015-3585-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirkpatrick SI, Potischman N, Dodd KW, Douglass D, Zimmerman TP, Kahle LL, Thompson FE, George SM, Subar AF. The use of digital images in 24-hour recalls may lead to less misestimation of portion size compared with traditional interviewer-administered recalls. J. Nutr. 2016;146:2567–2573. doi: 10.3945/jn.116.237271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirkpatrick SI, Subar AF, Douglass D, Zimmerman TP, Thompson FE, Kahle LL, George SM, Dodd KW, Potischman N. Performance of the Automated Self-Administered 24-hour Recall relative to a measure of true intakes and to an interviewer-administered 24-h recall. Am. J. Clin. Nutr. 2014;100:233–240. doi: 10.3945/ajcn.114.083238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koeth RA, Wang Z, Levison BS, Buffa JA, Org E, Sheehy BT, Britt EB, Fu X, Wu Y, Li L, et al. Intestinal microbiota metabolism of L-carnitine, a nutrient in red meat, promotes atherosclerosis. Nat. Med. 2013;19:576–585. doi: 10.1038/nm.3145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kromhout D, Giltay EJ, Geleijnse JM. n−3 fatty acids and cardiovascular events after myocardial infarction. N. Engl. J. Med. 2010;363:2015–2026. doi: 10.1056/NEJMoa1003603. [DOI] [PubMed] [Google Scholar]
- Lawlor DA, Davey Smith G, Kundu D, Bruckdorfer KR, Ebrahim S. Those confounded vitamins: what can we learn from the differences between observational versus randomised trial evidence? Lancet. 2004;363:1724–1727. doi: 10.1016/S0140-6736(04)16260-0. [DOI] [PubMed] [Google Scholar]
- Lu Y, Wang Y, Ong CN, Subramaniam T, Choi HW, Yuan JM, Koh WP, Pan A. Metabolic signatures and risk of type 2 diabetes in a Chinese population: an untargeted metabolomics study using both LC-MS and GC-MS. Diabetologia. 2016;59:2349–2359. doi: 10.1007/s00125-016-4069-2. [DOI] [PubMed] [Google Scholar]
- Lv J, Yu C, Guo Y, Bian Z, Yang L, Chen Y, Tang X, Zhang W, Qian Y, Huang Y, Wang X, Chen J, Chen Z, Qi L, Li L, China Kadoorie Biobank Collaborative Group Adherence to healthy lifestyle and cardiovascular diseases in the Chinese population. J. Am. Coll. Cardiol. 2017;69:1116–1125. doi: 10.1016/j.jacc.2016.11.076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma XY, Liu JP, Song ZY. Glycemic load, glycemic index and risk of cardiovascular diseases: meta-analyses of prospective studies. Atherosclerosis. 2012;223:491–496. doi: 10.1016/j.atherosclerosis.2012.05.028. [DOI] [PubMed] [Google Scholar]
- Mahmood SS, Levy D, Vasan RS, Wang TJ. The Framingham Heart Study and the epidemiology of cardiovascular disease: a historical perspective. Lancet. 2014;383:999–1008. doi: 10.1016/S0140-6736(13)61752-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malik VS, Hu FB. Fructose and cardiometabolic health: what the evidence from sugar-sweetened beverages tells us. J. Am. Coll. Cardiol. 2015;66:1615–1624. doi: 10.1016/j.jacc.2015.08.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malik VS, Pan A, Willett WC, Hu FB. Sugar-sweetened beverages and weight gain in children and adults: a systematic review and meta-analysis. Am. J. Clin. Nutr. 2013;98:1084–1102. doi: 10.3945/ajcn.113.058362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez-Gonzalez MA, Bes-Rastrollo M. Dietary patterns, Mediterranean diet, and cardiovascular disease. Curr. Opin. Lipidol. 2014;25:20–26. doi: 10.1097/MOL.0000000000000044. [DOI] [PubMed] [Google Scholar]
- Micha R, Mozaffarian D. Trans fatty acids: effects on metabolic syndrome, heart disease and diabetes. Nat. Rev. Endocrinol. 2009;5:335–344. doi: 10.1038/nrendo.2009.79. [DOI] [PubMed] [Google Scholar]
- Mozaffarian D, Aro A, Willett WC. Health effects of trans-fatty acids: experimental and observational evidence. Eur. J. Clin. Nutr. 2009;63:S5–S21. doi: 10.1038/sj.ejcn.1602973. [DOI] [PubMed] [Google Scholar]
- Myung SK, Ju W, Cho B, Oh SW, Park SM, Koo BK, Park BJ, Korean Meta-Analysis Study Group Efficacy of vitamin and antioxidant supplements in prevention of cardiovascular disease: systematic review and meta-analysis of randomised controlled trials. BMJ. 2013;346:f10. doi: 10.1136/bmj.f10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Odegaard AO, Koh WP, Gross MD, Yuan JM, Pereira MA. Combined lifestyle factors and cardiovascular disease mortality in Chinese men and women: the Singapore Chinese health study. Circulation. 2011;124:2847–2854. doi: 10.1161/CIRCULATIONAHA.111.048843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Sullivan A, Henrick B, Dixon B, Barile D, Zivkovic A, Smilowitz J, Lemay D, Martin W, German JB, Schaefer SE. 21st century toolkit for optimizing population health through precision nutrition. Crit. Rev. Food Sci. Nut. 2017 doi: 10.1080/10408398.2017.1348335. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parnell LD, Blokker BA, Dashti HS, Nesbeth PD, Cooper BE, Ma Y, Lee YC, Hou R, Lai CQ, Richardson K, et al. CardioGxE, a catalog of gene-environment interactions for cardiometabolic traits. BioData Min. 2014;7:21. doi: 10.1186/1756-0381-7-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qi Q, Chu AY, Kang JH, Jensen MK, Curhan GC, Pasquale LR, Ridker PM, Hunter DJ, Willett WC, Rimm EB, et al. Sugar-sweetened beverages and genetic risk of obesity. N. Engl. J. Med. 2012;367:1387–1396. doi: 10.1056/NEJMoa1203039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiu G, Zheng Y, Wang H, Sun J, Ma H, Xiao Y, Li Y, Yuan Y, Yang H, Li X, et al. Plasma metabolomics identified novel metabolites associated with risk of type 2 diabetes in two prospective cohorts of Chinese adults. Int. J. Epidemiol. 2016;45:1507–1516. doi: 10.1093/ije/dyw221. [DOI] [PubMed] [Google Scholar]
- Roth GA, Johnson C, Abajobir A, Abd-Allah F, Abera SF, Abyu G, Ahmed M, Aksut B, Alam T, Alam K, et al. Global, regional, and national burden of cardiovascular diseases for 10 causes, 1990 to 2015. J. Am. Coll. Cardiol. 2017;70:1–25. doi: 10.1016/j.jacc.2017.04.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sacks FM, Svetkey LP, Vollmer WM, Apple LJ, Bray GA, Harsha D, Obarzanek E, Conlin PR, Miller ER, 3rd, Simons-Morton DG, Karanja N, Lin PH, DASH-Sodium Collaborative Research Group Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. N. Engl. J. Med. 2001;344:3–10. doi: 10.1056/NEJM200101043440101. [DOI] [PubMed] [Google Scholar]
- Sacks FM, Lichtenstein AH, Wu JHY, Appel LJ, Creager MA, Kris-Etherton PM, Miller M, Rimm EB, Rudel LL, Robinson JG, et al. Dietary fats and cardiovascular disease: a presidential advisory from the American Heart Association. Circulation. 2017;136:e1–e23. doi: 10.1161/CIR.0000000000000510. [DOI] [PubMed] [Google Scholar]
- Salehi-Abargouei A, Maghsoudi Z, Shirani F, Azadbakht L. Effects of Dietary Approaches to Stop Hypertension (DASH)-style diet on fatal or nonfatal cardiovascular diseases--incidence: a systematic review and meta-analysis on observational prospective studies. Nutrition. 2013;29:611–618. doi: 10.1016/j.nut.2012.12.018. [DOI] [PubMed] [Google Scholar]
- Satija A, Yu E, Willett WC, Hu FB. Understanding nutritional epidemiology and its role in policy. Adv. Nutr. 2015;6:5–18. doi: 10.3945/an.114.007492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scalbert A, Brennan L, Manach C, Andres-Lacueva C, Dragsted LO, Draper J, Rappaport SM, van der Hooft JJ, Wishart DS. The food metabolome: a window over dietary exposure. Am. J. Clin. Nutr. 2014;99:1286–1308. doi: 10.3945/ajcn.113.076133. [DOI] [PubMed] [Google Scholar]
- Smith-Warner SA, Spiegelman D, Ritz J, Albanes D, Beeson WL, Bernstein L, Berrino F, van den Brandt PA, Buring JE, Cho E, et al. Methods for pooling results of epidemiologic studies: the Pooling Project of Prospective Studies of Diet and Cancer. Am. J. Epidemiol. 2006;163:1053–1064. doi: 10.1093/aje/kwj127. [DOI] [PubMed] [Google Scholar]
- Sofi F, Macchi C, Abbate R, Gensini GF, Casini A. Mediterranean diet and health status: an updated meta-analysis and a proposal for a literature-based adherence score. Public Health Nutr. 2014;17:2769–2782. doi: 10.1017/S1368980013003169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sotos-Prieto M, Bhupathiraju SN, Mattei J, Fung TT, Li Y, Pan A, Willett WC, Rimm EB, Hu FB. Changes in diet quality scores and risk of cardiovascular disease among US men and women. Circulation. 2015;132:2212–2219. doi: 10.1161/CIRCULATIONAHA.115.017158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spiegelman D. Evaluating public health interventions: 4. The Nurses' Health Study and methods for eliminating bias attributable to measurement error and misclassification. Am. J. Public Health. 2016;106:1563–1566. doi: 10.2105/AJPH.2016.303377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stampfer MJ, Hu FB, Manson JE, Rimm EB, Willett WC. Primary prevention of coronary heart disease in women through diet and lifestyle. N. Engl. J. Med. 2000;343:16–22. doi: 10.1056/NEJM200007063430103. [DOI] [PubMed] [Google Scholar]
- Tang WH, Wang Z, Levison BS, Koeth RA, Britt EB, Fu X, Wu Y, Hazen SL. Intestinal microbial metabolism of phosphatidylcholine and cardiovascular risk. N. Engl. J. Med. 2013;368:1575–1584. doi: 10.1056/NEJMoa1109400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Threapleton DE, Greenwood DC, Evans CE, Cleghorn CL, Nykjaer C, Woodhead C, Cade JE, Gale CP, Burley VJ. Dietary fibre intake and risk of cardiovascular disease: systematic review and meta-analysis. BMJ. 2013;347:f6879. doi: 10.1136/bmj.f6879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toledo E, Wang DD, Ruiz-Canela Lopez M, Clish CB, Razquin C, Zheng Y, Guasch-Ferre M, Hruby A, Corella D, Gomez-Gracia E, et al. Plasma lipidomic profiles and cardiovascular events in a randomized intervention trial with the Mediterranean diet. Am. J. Clin. Nutr. 2017;106:973–983. doi: 10.3945/ajcn.116.151159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veronese N, Li Y, Manson JE, Willett WC, Fontana L, Hu FB. Combined associations of body weight and lifestyle factors with all cause and cause specific mortality in men and women: prospective cohort study. BMJ. 2016;355:i5855. doi: 10.1136/bmj.i5855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang DD, Toledo E, Hruby A, Rosner BA, Willett WC, Sun Q, Razquin C, Zheng Y, Ruiz-Canela M, Guasch-Ferre M, et al. Plasma ceramides, Mediterranean diet, and incident cardiovascular disease in the PREDIMED Trial (Prevencion con Dieta Mediterranea) Am. J. Clin. Nutr. 2017;135:2028–2040. doi: 10.1161/CIRCULATIONAHA.116.024261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willett WC. Nutritional Epidemiology. New York, USA: Oxford University Press; 2013. [Google Scholar]
- Wu Y, Qian Y, Pan Y, Li P, Yang J, Ye X, Xu G. Association between dietary fiber intake and risk of coronary heart disease: a meta-analysis. Clin. Nutr. 2015;34:603–611. doi: 10.1016/j.clnu.2014.05.009. [DOI] [PubMed] [Google Scholar]
- Wurtz P, Havulinna AS, Soininen P, Tynkkynen T, Prieto-Merino D, Tillin T, Ghorbani A, Artati A, Wang Q, Tiainen M, et al. Metabolite profiling and cardiovascular event risk: a prospective study of 3 population-based cohorts. Circulation. 2015;131:774–785. doi: 10.1161/CIRCULATIONAHA.114.013116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu E, Ruiz-Canela M, Guasch-Ferre M, Zheng Y, Toledo E, Clish CB, Salas-Salvado J, Liang L, Wang DD, Corella D, et al. Increases in plasma tryptophan are inversely associated with incident cardiovascular disease in the Prevencion con Dieta Mediterranea (PREDIMED) Study. J. Nutr. 2017;147:314–322. doi: 10.3945/jn.116.241711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao WH, Huang ZP, Zhang X, He L, Willett W, Wang JL, Hasegawa K, Chen JS. Reproducibility and validity of a Chinese food frequency questionnaire. Biomed. Environ. Sci. 2010;23(suppl):1–38. [Google Scholar]
- Zong G, Gao A, Hu FB, Sun Q. Whole grain intake and mortality from all causes, cardiovascular disease, and cancer: a meta-analysis of prospective cohort studies. Circulation. 2016;133:2370–2380. doi: 10.1161/CIRCULATIONAHA.115.021101. [DOI] [PMC free article] [PubMed] [Google Scholar]