Abstract
Background
Prescription drug misuse and its consequences (e.g., overdose) are a major public health concern. While national focus has been on opioids, misuse of sedatives/tranquilizers also occurs. Here we describe the use, correlates, and sources of prescription drugs in a community-based cohort of people who inject drugs (PWID).
Methods
We included participants of the AIDS Linked to the IntraVenous Experience (ALIVE) study in follow-up in 2014. We defined prescription drug use as use of opioids or sedatives/tranquilizers considering both medical “prescribed by a doctor” and non-medical sources “obtained from the street/friend/relative.” Correlates were evaluated separately for opioids and sedatives/tranquilizers using logistic regression and included socioeconomic factors, health conditions, substance use, and health care access.
Results
823 predominantly African-American (90.6%) and male (66.3%) ALIVE participants with a median age of 55 were included. Prevalence of prescription opioid and sedative/tranquilizer use was 25.3% and 16.3% respectively. While the majority (70%) obtained prescription drugs exclusively through medical sources, the 30% who reported any non-medical source were also more likely to use other substances by injection and non-injection routes. PWID reporting prescription drug use (from medical and non-medical sources) were significantly more likely to report other substance use, mental health disorder, and recent contact with health care providers or detoxification facilities.
Conclusions
Prescription drug use was highly prevalent among PWID. While it is difficult to distinguish medically indicated from non-medical use, high levels of prescription drug use in conjunction with other drugs and alcohol heightens the risk for drug overdose and other adverse consequences.
Keywords: prescription drug use, people who inject drugs (PWID), the ALIVE study, substance use
1. Introduction
Over the last two decades, misuse of prescription psychotherapeutic drugs (including opioid analgesics, tranquilizers, sedatives and stimulants) and the related adverse health consequences have reached epidemic proportions in the United States (Centers for Disease Control and Prevention, 2013). Indeed, the prevalence of prescription drug misuse among the general population has increased by nearly 180% over the past 20 years (Manchikanti et al., 2012). In 2015, an estimated 6.4 million people reported misuse of prescription psychotherapeutics (2.4% of the population), 3.8 million of whom reported opioid analgesics as being the primary drug of misuse, followed by tranquilizers, stimulants, and sedatives (Substance Abuse and Mental Health Service Administration, 2015). Related to this, there have been notable increases in prescription drug abuse-related deaths, emergency room and outpatient clinic visits, and hospital admissions, leading to an accompanying significant rise in health care costs (Centers for Disease Control and Prevention, 2013).
Accounting for geographical, cultural and societal differences, the prevalence of prescription drug misuse among the general population is estimated to be approximately 2–6% (Harrell & Broman, 2009; Manchikanti et al., 2012; Substance Abuse and Mental Health Service Administration, 2015), but could be as high as 80–90% among people with underlying substance use disorders (K. M. Johnson, Fibbi, Langer, Silva, & Lankenau, 2013; Lankenau et al., 2007). Moreover, as people who use drugs are more vulnerable due to social disadvantage, stigma, poverty, and unfavorable physical or mental health conditions, the health consequences of prescription drug misuse may be even more severe (Khosla, Juon, Kirk, Astemborski, & Mehta, 2011), including both accidental fatal and non-fatal overdose (K. M. Johnson et al., 2013; Kerr et al., 2007; Khosla et al., 2011) and increased risk for HIV and hepatitis C virus infection (Chaisson, Moss, Onishi, Osmond, & Carlson, 1987; Garfein, Vlahov, Galai, Doherty, & Nelson, 1996; Jose et al., 1993; Kral et al., 2001; Schoenbaum et al., 1989). On the other hand, for people who inject drugs (PWID) prescription drugs may be considered a safer and more predictable alternative to illicit street drugs as they are legal and consistently formulated.
Several prior studies have reported that prescription drug misuse is highly prevalent among PWID in urban settings, such as New York City, New Orleans, Toronto and Baltimore (Firestone & Fischer, 2008; Khosla et al., 2011; Lankenau et al., 2007). A prior report from our cohort of PWID in Baltimore described the street acquisition (and presumed misuse) of prescription drugs, which was strongly linked to use of other substances, such as alcohol, marijuana, or injection drugs (Khosla et al., 2011). This report was limited in that it did not consider alternative sources for obtaining prescription drugs including medical and non-medical sources. It is well recognized that there are multiple behaviors that contribute to the misuse of prescription drugs, even those obtained with a legitimate prescription. Inappropriate or high-volume drug prescriptions by physicians (Centers for Disease Control and Prevention, 2013), manipulation of the system in the form of frequent changes of primary care physicians and pharmacies - often referred to as “doctor shopping” or “pharmacy shopping” (Bouland, Fine, Withers, & Jarvis, 2015; Peirce, Smith, Abate, & Halverson, 2012; Stogner, Sanders, & Miller, 2014) - and repeated emergency room and outpatient clinic visits (Wisniewski, Purdy, & Blondell, 2008) may all drive misuse. With this analysis, we build upon our prior report from Baltimore by further characterizing prescription drug use and adding important information on sources for obtaining prescription drugs in a cohort of current and former PWID in an urban setting in the United States.
2. Materials and Methods
2.1 Study population and study design
The AIDS Linked to the IntraVenous Experience (ALIVE) study is a community-based prospective cohort study of current and former PWID, located in Baltimore, Maryland, USA (Vlahov et al., 1991). After the initial recruitment of 2946 participants through extensive community outreach in 1988–1989, subsequent enrollments occurred in 1994–1995, 1998, 2000, and 2005–2008 using similar methods. We place flyers at locations frequented by PWID including opioid treatment programs, syringe service programs, HIV clinics and federally qualified health centers, and study staff participate in health fairs and other community activities. In addition, we rely on word-of-mouth referrals from existing participants. We included participants who were in follow-up after the implementation of a new survey with detailed questions on prescription drug use in January 2014. Throughout 2014, the active cohort included 935 participants, 112 of whom were excluded from the analysis due to missing data on key covariates, leaving 823 for the analysis. The study was approved by the Johns Hopkins University Institution Review Boards (IRB) and all study participants provided a written informed consent.
2.2 Data collection and measurements
The newly implemented survey on prescription drug use was administered using audio computer-assisted self-interview (ACASI) (Macalino, Celentano, Latkin, Strathdee, & Vlahov, 2002). Participants were asked about the types of prescription drugs used (opiates, sedatives, tranquilizers, stimulants and hallucinogens), the route of use (injection vs. non-injection), and the source (prescribed by a doctor, obtained on the street or through friends or family members). All questions reflected behaviors in the prior six months. Exposure variables such as socio-demographic characteristics, health conditions and healthcare utilization were assessed either by structured interviewer-administered questionnaires or, in the case of sensitive risk behavioral information, by ACASI (Macalino et al., 2002). Depressive symptoms were quantified using the Center for Epidemiological Studies - Depression Scale (CES-D), applying the previously described higher cut-off of 23 for this population (Dinwiddie, Reich, & Cloninger, 1992; M. E. Johnson, Fisher, Fenaughty, & Theno, 1998).
2.3 Statistical analysis
Two primary outcomes were examined independently: use of prescription opioids and use of sedatives or tranquilizers (as a combined outcome), respectively. Self-reported sources of prescription drugs were grouped into “prescribed by a doctor” (representing a combination of medical and nonmedical use) and “obtained through sources other than a doctor, including acquisition on the street and through family members or friends” (representing non-medical use) and examined stratified by use of other substances. Stimulants and hallucinogens were not examined due to low frequency of use in the given time period. Prevalence of prescription drug use was first assessed by key correlates of interest reflecting population characteristics, including socioeconomic factors, physical and mental health parameters, access to health care service, substance use (both type and route), and HIV/Hepatitis C (HCV) seropositivity. Bivariate analyses (chi-square test or Fisher exact test) and logistic regression were used to assess the strength of association between selected explanatory variables and the two outcomes. Two separate models were run for use of opioids and sedatives/tranquilizers as a combined outcome. Likelihood ratio (LR) tests were performed to assess and optimize the goodness of fit for both models. To describe factors independently associated with prescription drug use, we included variables in multivariable logistic regression analysis based on known associations with the outcomes from prior literature or variables that demonstrated an association with the outcomes of interest at a level of p<0.05 in our data. In the case of variables that reflected a similar construct, the selection was based on either the strongest point estimate or the most clinically meaningful variable. Age, gender and ethnicity were retained in the adjusted model regardless of their statistical significance. Assuming mixed use patterns, substance use variables were coded as: none, alcohol/marijuana, non-injection cocaine/heroin, injection cocaine/heroin. Tobacco use was highly prevalent, and thus not included in substance use patterns. All analyses were performed using STATA (Version 12; STATA Corporation, College Station, TX, USA).
3. Results
3.1 Characteristics of study participants
Of the 823 included study participants, 66.3% were male, and 90.6% were African-American; the median age was 54.6 years (interquartile range [IQR] 50.1–59.1). Overall, current injection drug use (as defined by active injection in the prior 6 months) was reported by 19.7% of the participants, while 26.4% reported non-injection use of cocaine or heroin (smoked or snorted). Regular alcohol consumption and tobacco use was reported by 47.4% and 75.7% of the participants, respectively, whereas 11.3% reported marijuana use in the prior 6 months. The overall prevalence of HIV and HCV was 33.2% and 83.5%, respectively. Among HIV-infected persons, 86.6% were on antiretroviral therapy.
As shown in Table 1, 562 persons (68.5%) reported no use of any prescription drugs, and 208 (25.3%) and 134 (16.3%) people reported use of prescription opiates and sedatives/tranquilizers, respectively. Eighty-three participants (10.0%) reported use of both opiates and sedatives/tranquilizers (data not shown). The three groups did not differ with respect to health insurance or prescription plan coverage. However, prevalence of both opioid and sedative/tranquilizer use was lower in men, African-Americans, and persons currently employed (see Table 1). Moreover, compared to those not using prescription drugs, participants reporting opioid and sedative/tranquilizer use more often reported emergency room visits, being in an alcohol/drug detoxification program, receiving disability support, active injection drug use, depressive symptoms (CESD scores > 23), being diagnosed with depression, anxiety disorder, manic depression, or schizophrenia, and moderate to severe body pain.
Table 1.
Characteristics of study population by prescription drug use
| No prescription drug use | Prescription opiate use+ | Sedative/tranquilizer use+ | |
|---|---|---|---|
| N = 562 (%) | N = 208 (%) | N = 134 (%) | |
| Sociodemographic | |||
| Age | |||
| Median (y) | 54.9 | 54.6 | 51.9 |
| IQR | 50.5 – 59.6 | 49.8 – 58.7 | 46.8 – 57.9 |
| Male gender | 390 (69.4) | 127 (61.1) | 65 (48.5) |
| African-American race | 522 (92.9) | 180 (86.5) | 107 (79.9) |
| Homelessness* | 26 (4.6) | 8 (3.9) | 9 (6.7) |
| Employment* | 104 (18.5) | 23 (11.1) | 13 (9.8) |
| Health Care Access | |||
| Health insurance* | 531 (95.0) | 199 (96.1) | 131 (97.8) |
| Prescription drug plan* | 532 (95.3) | 200 (96.6) | 129 (96.3) |
| Disability support* | 320 (57.1) | 144 (69.2) | 93 (69.4) |
| Usual source of primary health care | 502 (89.3) | 196 (94.2) | 122 (91.0) |
| Emergency room/outpatient visits* | 454 (80.8) | 184 (88.5) | 120 (89.6) |
| Tobacco and Substance Use | |||
| Tobacco use* | 406 (72.2) | 185 (88.9) | 115 (85.8) |
| Substance use* | |||
| None | 279 (49.9) | 48 (23.3) | 29 (21.8) |
| Alcohol, marijuana | 143 (25.6) | 65 (31.6) | 33 (24.8) |
| Snorted/smoked heroin/cocaine | 47 (8.4) | 41 (19.9) | 29 (21.8) |
| Injection drugs | 90 (16.1) | 52 (25.2) | 42 (31.6) |
| Alcohol/drug detoxification* | 148 (26.4) | 118 (56.7) | 77 (57.5) |
| Comorbidity | |||
| Current physical comorbidity* | 61 (11.1) | 30 (15.0) | 14 (11.1) |
| HIV infection | 188 (33.5) | 70 (33.7) | 40 (29.9) |
| Median CD4+ cell count/μL | 446.5 | 458 | 406.5 |
| Median HIV viral load/μL | 40 | 40 | 40 |
| HAART* | 157 (86.7) | 57 (81.4) | 29 (72.5) |
| HCV infection | 469 (83.5) | 180 (86.5) | 102 (76.7) |
| HBV infection | 193 (35.3) | 83 (40.3) | 56 (42.4) |
| CESD score > 23# | 94 (16.8) | 68 (32.7) | 59 (44.0) |
| Depression*∘ | 12 (2.1) | 10 (4.8) | 10 (7.5) |
| Anxiety disorder*∘ | 11 (2.0) | 6 (2.9) | 6 (4.5) |
| Manic depression*∘ | 6 (1.1) | 7 (3.4) | 10 (7.5) |
| Schizophrenia*∘ | 3 (0.5) | 1 (0.5) | 1 (0.8) |
| Ever treated for any mental health condition | 235 (42.0) | 133 (64.6) | 102 (76.7) |
| Body pain* | |||
| None | 139 (24.8) | 21 (10.1) | 12 (9.0) |
| Mild | 251 (44.7) | 81 (38.9) | 50 (37.3) |
| Moderate – Severe | 171 (30.5) | 106 (51.0) | 72 (53.7) |
During the prior 6 months
During the prior week
Self-reported diagnosis
Abbreviations:
CESD, Center of Epidemiologic Studies Depression scale; HAART, highly active antiretroviral therapy; HBV, hepatitis b virus; HCV, hepatitis c virus; IQR, interquartile range; y, years; μL, micro liter
3.2 Self-reported sources of prescription drugs
Table 2 shows the distribution of self-reported sources of prescription drugs overall and for opiates and sedatives/tranquilizers separately, stratified by other substance use. Overall, among the 255 persons reporting any prescription drug use, 70.2% indicated an exclusive medical source (prescription by a doctor), whereas 29.8% reported at least one non-medical source, including acquisition on the street or through friends or family members. Among the 76 persons reporting at least one non-medical source, 25% reported concurrent non-injection use of cocaine or heroin and 48.7% were actively injecting. Of the 179 participants exclusively using medical sources, 31.3% reported no additional substance use, 15.6% reported non-injection and 19% injection drug use.
Table 2.
Prescription drug source by drug category and substance use category
| Prescription drugs overall | Prescription opiates | Sedatives/Tranquilizers | |||||||
|---|---|---|---|---|---|---|---|---|---|
| N = 255 (%) | N = 206 (%) | N = 127 (%) | |||||||
|
| |||||||||
| Medical source | Non-medical source+ | Both | Medical source | Non-medical source+ | Both | Medical source | Non-medical source+ | Both | |
| No additional substance use | 56 (31.3) | 4 (7.8) | 3 (12.0) | 43 (25.9) | 3 (10.3) | 2 (18.2) | 26 (36.6) | 2 (5.4) | 1 (5.3) |
| Alcohol or marijuana | 61 (34.1) | 10 (19.6) | 3 (12.0) | 62 (37.4) | 3 (10.3) | 0 (0.0) | 23 (32.4) | 7 (18.9) | 3 (15.8) |
| Non-injection cocaine or heroin | 28 (15.6) | 14 (27.5) | 5 (20.0) | 29 (17.5) | 8 (27.6) | 4 (36.4) | 11 (15.5) | 12 (32.4) | 3 (15.8) |
| Injection drug use | 34 (19.0) | 23 (45.1) | 14 (56.0) | 32 (19.2) | 15 (51.8) | 5 (45.4) | 11 (15.5) | 16 (43.3) | 12 (63.1) |
| Total | 179 (70.2) | 51 (20.0) | 25 (9.8) | 166 (80.6) | 29 (14.1) | 11 (5.3) | 71 (55.9) | 37 (29.1) | 19 (15.0) |
Drugs obtained on the street, from a friend or a family member
Looking at patterns by prescription drug type, among sedatives/tranquilizer users, a larger proportion reported acquisition through non-medical sources compared to opiate users (44.1% vs. 19.4%). Among the 206 people using prescription opiates, 80.6% reported acquisition exclusively through medical sources. Of the 40 individuals indicating at least one non-medical source for prescription opiates, 30% reported non-injection use of cocaine or heroin, and 50% were actively injecting. Sedative/tranquilizer use was reported by 127 persons, 55.9% of whom reported medical sources only, and 44.1% of whom reported at least one non-medical source. Of the 56 individuals indicating at least one non-medical source, 26.8% reported use of non-injection cocaine or heroin, and 50% were actively injecting.
3.3 Correlates of prescription drug use
Table 3 shows the unadjusted correlates of prescription drug use, stratified by drug type. Correlates were similar for both prescription opiates and sedatives/tranquilizers. Overall, use was less common among men (OR 0.73 for opiates and OR 0.41 for sedatives/tranquilizers), African-Americans (OR 0.56 and OR 0.31), and those aged 50 years and older (OR 0.85 and OR 0.44); however, associations with sex and age were not statistically significant for opiates. Prescription drug use was significantly more common among those reporting other substance use, such as alcohol or marijuana (OR 2.62 and OR 1.94), non-injection cocaine or heroin (OR 4.74 and OR 4.82), injection of cocaine or heroin (OR 2.90 and OR 3.78), but also among individuals who reported body pain (OR 3.80 and OR 4.08 for moderate to severe pain), being in an alcohol/drug detoxification program (OR 3.24 and OR 2.91), or being recently treated in an emergency room (OR 2.12 and OR 1.97). Prescription drug use was also more common among participants who reported having been treated for a mental health disorder (OR 2.29 and OR 4.16) or having been diagnosed with depression (OR 1.88 and 3.38), anxiety disorder (OR 1.37 and 2.42), or manic depression (OR 2.11 and 7.90); however, associations were not statistically significant for opiates. Interestingly, there was no association between prescription drug use and general health care access, as measured by health insurance coverage and current prescription drug plan; however, prescription opiate use was more common in those reporting a usual source of care and a consistent health care provider (OR 2.04 and OR 1.12). There was no association of prescription drug use and HIV or HCV status or any other physical comorbidity.
Table 3.
Unadjusted correlates of prescription drug use
| Prescription opiates | Sedatives/Tranquilizers | |||
|---|---|---|---|---|
| OR (95% CI) | P | OR (95% CI) | P | |
| Sociodemographic | ||||
| Age 50 years and older | 0.85 (0.59 – 1.21) | 0.37 | 0.44 (0.30 – 0.65) | < 0.01 |
| Male gender | 0.73 (0.53 – 1.01) | 0.06 | 0.41 (0.28 – 0.59) | < 0.01 |
| African-American race | 0.56 (0.34 – 0.92) | 0.02 | 0.31 (0.19 – 0.52) | < 0.01 |
| Homelessness* | 0.75 (0.34 – 1.66) | 0.48 | 1.58 (0.73 – 3.40) | 0.25 |
| Employed* | 0.59 (0.36 – 0.95) | 0.03 | 0.53 (0.29 – 0.97) | 0.04 |
| Health Care Access | ||||
| Health insurance coverage* | 1.24 (0.56 – 2.76) | 0.59 | 2.29 (0.69 – 7.56) | 0.18 |
| Prescription drug plan* | 1.38 (0.59 – 3.20) | 0.46 | 1.19 (0.45 – 3.12) | 0.73 |
| Usual source of care / primary care physician | 2.04 (1.08 – 3.85) | 0.03 | 1.12 (0.59 – 2.13) | 0.74 |
| Emergency room visits* | 2.12 (1.51 – 2.98) | < 0.01 | 1.97 (1.33 – 2.91) | < 0.01 |
| Outpatient clinic visits* | 1.33 (0.89 – 1.98) | 0.15 | 1.77 (1.07 – 2.94) | 0.03 |
| Tobacco and Substance Use | ||||
| Tobacco use* | 3.01 (1.89 – 4.81) | < 0.01 | 2.01 (1.20 – 3.36) | 0.01 |
| Substance use* | ||||
| Alcohol, marijuana | 2.62 (1.72 – 3.99) | < 0.01 | 1.94 (1.14 – 3.29) | 0.02 |
| Non-injection cocaine or heroin use+ | 4.74 (2.85 – 7.88) | < 0.01 | 4.82 (2.70 – 8.60) | < 0.01 |
| Injection drug use | 2.90 (1.85 – 4.54) | < 0.01 | 3.78 (2.25 – 6.34) | < 0.01 |
| Alcohol and/or drug detoxification program* | 3.24 (2.34 – 4.49) | < 0.01 | 2.91 (2.0 – 4.25) | < 0.01 |
| Comorbidities | ||||
| Any physical comorbidity | 1.11 (0.78 – 1.56) | 0.57 | 1.33 (0.88 – 2.03) | 0.18 |
| HIV positive | 1.03 (0.74 – 1.44) | 0.85 | 0.83 (0.56 – 1.25) | 0.38 |
| HCV positive | 1.38 (0.88 – 2.16) | 0.16 | 0.59 (0.38 – 0.93) | 0.02 |
| CESD score >23# | 2.08 (1.46 – 2.96) | < 0.01 | 3.53 (2.38 – 5.23) | < 0.01 |
| Depression*∘ | 1.88 (0.84 – 4.22) | 0.12 | 3.38 (1.50 – 7.63) | < 0.01 |
| Anxiety disorder*∘ | 1.37 (0.52 – 3.66) | 0.53 | 2.42 (0.90 – 6.48) | 0.08 |
| Manic depression*∘ | 2.11 (0.79 – 5.62) | 0.14 | 7.90 (2.95 – 21.14) | < 0.01 |
| Schizophrenia*∘ | 0.99 (0.10 – 9.54) | 0.99 | 1.73 (0.18 – 16.73) | 0.64 |
| Ever treated for any mental health condition | 2.29 (1.65 – 3.17) | < 0.01 | 4.16 (2.71 – 6.39) | < 0.01 |
| Body pain* | < 0.01 | < 0.01 | ||
| Mild | 2.07 (1.23 – 3.48) | 2.13 (1.10 – 4.12) | ||
| Moderate - severe | 3.80 (2.27 – 6.36) | 4.08 (2.14 – 7.77) | ||
| Any registered disability* | 1.66 (1.18 – 2.32) | < 0.01 | 1.59 (1.07 – 2.36) | 0.02 |
Snorted cocaine, crack, snorted heroin or smoked heroin
During the prior 6 months
During the prior week
Self-reported diagnosis
Abbreviations:
CESD, Center for Epidemiologic Studies Depression Scale; HCV, hepatitis c virus
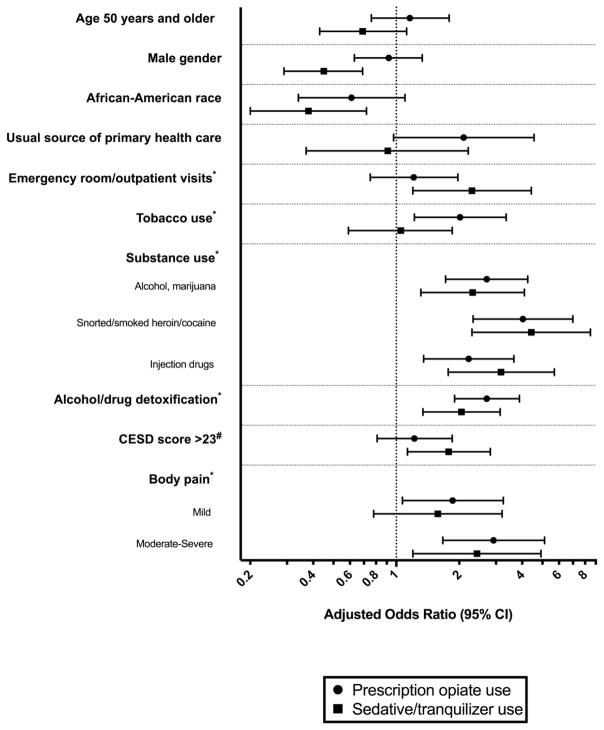
Associations for non-medical use of opiates and sedatives/tranquilizers remained similar after adjustment in the multivariable analysis. For both prescription opiates and sedatives/tranquilizers, non-medical use remained significantly associated with moderate to severe pain body pain and other substance use including alcohol or marijuana use, non-injection use of cocaine or heroin, and injection of cocaine or heroin. Furthermore, both prescription opiate and sedative/tranquilizer use remained significantly more common in those who reported having recently attended an alcohol/drug detoxification program or being treated in an outpatient facility. However, after adjustment, associations of non-medical prescription drug use with mental health conditions such as depression, anxiety disorder and manic depression were no longer significant. Figure 1 illustrates the adjusted odds ratios with 95% confidence intervals, and supplemental Table 4 shows the quantitative results of the multivariable analysis.
Figure 1.
Independent correlates of prescription drug use: results from multivariable logistic regression
*During the prior 6 months
#During the prior week
4. Discussion
Our study demonstrated that nearly a third of this population of urban current and former PWID reported use of prescription drugs, many of whom were using prescription opiates, sedatives and tranquilizers while also using illicit drugs. In addition to this strong association between use of prescription drugs and use of other illicit drugs, persons who used prescription drugs were also more likely to have mental health conditions, and recent interactions with a health care provider. These results build upon prior findings from this cohort on street-acquired prescription drug use (Khosla et al., 2011) by characterizing prescription drug use from all sources, including physicians, friends/family and the street. Indeed, we found that among those using prescription drugs, a high proportion were obtaining opiates (80%) or sedatives/tranquilizers (56%) from a medical source, which is consistent with previous reports among PWID (Peirce et al., 2012; Substance Abuse and Mental Health Service Administration, 2015; Wisniewski et al., 2008) and consistent with the observation that prescription drug use was correlated with engagement in care, though interestingly not with the prevalence of comorbidities.
While the prevalence of prescription drug use among PWID in urban settings in the US has been consistently higher than what has been reported in the general population (Lankenau et al., 2007), the magnitude has been variably reported, ranging from as low as 3% to as high as 85% (Harrell & Broman, 2009; K. M. Johnson et al., 2013; Lankenau et al., 2007; Manchikanti et al., 2012). Consistent with these previous studies among PWID in urban settings in the United States (Lankenau et al., 2007), prescription drug use among PWID in Baltimore was more common among those who were white, female and younger. This is particularly noteworthy, as it differs from the traditional composition of our study population which is predominantly African-American, male and older with a median age of 55 years. Given the underrepresentation of white, younger, female PWID in our sample, the true prevalence of prescription drug misuse among PWID in Baltimore may be greater than estimated in our study.
Similar to prior work (Huang et al., 2006; Khosla et al., 2011; Lankenau et al., 2007), there were strong associations of use of prescription drugs with depressive symptoms, mental health disorders, and chronic pain. These associations combined with associations observed between use of prescription drugs and recent mental health diagnosis may indicate at least some medically indicated use. On the other hand, while the majority of prescription drugs were obtained from medical sources in this population, we cannot rule out misuse of drugs acquired through a medical source given some of the associations observed. Prior work has demonstrated that legitimate prescriptions may be an important source of misuse, reflected in frequent changes of health care providers (e.g., “doctor shopping” and “pharmacy shopping”; (Nelson, Juurlink, & Perrone, 2015)). In our data, this was supported by the strong association between prescription drug use and frequent emergency room visits, even though a high percentage of the participants reported seeing mostly the same physician (Bouland et al., 2015; Khosla et al., 2011).
Moreover, a non-trivial proportion of our sample acquired prescription drugs from a non-medical source including friends, family members or on the street. Prescription drug use in general was also more common among people who also reported other drug use, including alcohol and marijuana, and particularly among those who reported cocaine or heroin use. Also, acquisition from a non-medical source was more common among those using other substances particularly heroin and cocaine and was more frequently reported for sedatives/tranquilizers compared with opioids. Thus, although we cannot draw definitive conclusions about medically vs. not medically indicated use from our data, the combination of use that we observed likely reflects some combination of legitimate use and misuse–i.e., reflecting both use of these substances to get high and also the high burden of untreated mental health conditions in this population. PWID are vulnerable to under-treatment as a result of both poor health care access and provider biases regarding prescribing sedatives/tranquilizers to people with a history of injection drug use.
Prescription drugs, including opioids and sedatives/tranquilizers play an important role in the management of somatic and psychiatric disease (Huang et al., 2006). However, the prevalence of prescription drug use disorder has been increasing over the past decade (Han, Compton, Jones, & Cai, 2015), reflecting a complex array of issues including high levels of use without a prescription, inappropriate prescribing patterns (high frequency, high intensity), perceived safety, and under-treatment of pain and depression (Manchikanti et al., 2012). The situation is likely even more complicated in populations with a history of active injection of heroin and or cocaine as some might be using prescription drugs for self-treatment of withdrawal and others may be self-medicating for pain, depression or other somatic symptoms (Nelson et al., 2015). Regardless of the reason, the medically indicated use of prescription drugs among those with history or active injection drug use in the context of competing mental health and other chronic conditions requires close management by a health care provider, because any prescription drug use may be a risk factor for continued or relapsing heroin use (Knowlton, Nguyen, Robinson, Harrell, & Mitchell, 2015). Moreover, the high levels of use among those using and injecting illicit drugs including heroin and cocaine heightens the risk for overdose and other adverse outcomes in this population.
This study has important limitations: Due to the cross-sectional study design, we cannot establish temporality or causality of the observed associations. Moreover, our outcome represents a composite of use and misuse because we cannot definitively differentiate between medical use of prescription drugs and misuse among those who acquired drugs from a medical source.
These limitations notwithstanding, our results provide evidence that there is need for detailed assessment of prescription drug use in the context of polysubstance use patterns in this disproportionally affected population. Coordinated, multifaceted and comprehensive approaches are needed to successfully address the opioid epidemic. Due to the chronic, relapsing nature of drug addiction, long-term recovery is the best possible and desirable outcome (Huang et al., 2006; Nelson et al., 2015). Gaining more insight into the sources, drug-seeking behavior, and correlates for prescription drug misuse may help to close the gap between prevention and management of prescription drug misuse, especially in the highly vulnerable population of PWID.
Supplementary Material
Highlights.
Prescription drug misuse is highly prevalent among people who inject drugs.
There was significant polysubstance use in association with prescription drug use
Depression and body pain may be undertreated among PWID.
Prescription drug misuse among PWID may be underestimated.
Acknowledgments
Funding: AA was supported by the Swiss National Science Foundation (SNF) [P2ZHP3_148715] and the Prof. Dr. Max Cloëtta Foundation/Uniscientia Foundation, Vaduz, Liechtenstein [Clinical Medicine Plus].
Funding
This work was supported by the Swiss National Science Foundation (SNF) [grant number P2ZHP3_148715] (AA); the Prof. Dr. Max Cloëtta Foundation/Uniscientia Foundation, Vaduz, Liechtenstein [grant name Clinical Medicine Plus] (AA); and the National Institutes on Drug Abuse [grant numbers 4 R01 DA012568, 5 U01 DA036297] (AGA, GDK, SHM). The funders had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
A special acknowledgement goes to the staff and study participants of the ALIVE study, without whom this analysis would not have been possible.
Abbreviations
- ALIVE
AIDS Linked to the IntraVenous Experience
- ACASI
Audio computer-assisted self-interview
- CES-D
Center for Epidemiological Studies - Depression Scale
- LR
Likelihood ratio
- PWID
People who inject drugs
Footnotes
Contributors
AA and SHM conceptualized the manuscript, conducted the analysis and drafted the initial report. AGA assisted with the analysis. GDK and BLG provided critical feedback into the development of the survey and the manuscript. All authors approved the final version for the manuscript.
Conflict of Interest
All authors declare that they have no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Bouland DT, Fine E, Withers D, Jarvis M. Prescription Medication Obtainment Methods and Misuse. J Addict Med. 2015;9(4):281–285. doi: 10.1097/ADM.0000000000000130. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. [Accessed 09/30/15];CDC Prescription Drug Abuse Report 2013. 2013 Retrieved from: http://www.cdc.gov/HomeandRecreationalSafety/pdf/HHS_Prescription_Drug_Abuse_Report_09.2013.pdf.
- Chaisson RE, Moss AR, Onishi R, Osmond D, Carlson JR. Human immunodeficiency virus infection in heterosexual intravenous drug users in San Francisco. Am J Public Health. 1987;77(2):169–172. doi: 10.2105/ajph.77.2.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dinwiddie SH, Reich T, Cloninger CR. Psychiatric comorbidity and suicidality among intravenous drug users. J Clin Psychiatry. 1992;53(10):364–369. [PubMed] [Google Scholar]
- Firestone M, Fischer B. A qualitative exploration of prescription opioid injection among street-based drug users in Toronto: behaviours, preferences and drug availability. Harm Reduct J. 2008;5:30. doi: 10.1186/1477-7517-5-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garfein RS, Vlahov D, Galai N, Doherty MC, Nelson KE. Viral infections in short-term injection drug users: the prevalence of the hepatitis C, hepatitis B, human immunodeficiency, and human T-lymphotropic viruses. Am J Public Health. 1996;86(5):655–661. [Google Scholar]
- Han B, Compton WM, Jones CM, Cai R. Nonmedical Prescription Opioid Use and Use Disorders Among Adults Aged 18 Through 64 Years in the United States, 2003–2013. Jama. 2015;314(14):1468–1478. doi: 10.1001/jama.2015.11859. [DOI] [PubMed] [Google Scholar]
- Harrell ZA, Broman CL. Racial/ethnic differences in correlates of prescription drug misuse among young adults. Drug Alcohol Depend. 2009;104(3):268–271. doi: 10.1016/j.drugalcdep.2009.05.017. [DOI] [PubMed] [Google Scholar]
- Huang B, Dawson DA, Stinson FS, Hasin DS, Ruan WJ, Saha TD, … Grant BF. Prevalence, correlates, and comorbidity of nonmedical prescription drug use and drug use disorders in the United States: Results of the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2006;67(7):1062–1073. doi: 10.4088/jcp.v67n0708. [DOI] [PubMed] [Google Scholar]
- Johnson KM, Fibbi M, Langer D, Silva K, Lankenau SE. Prescription drug misuse and risk behaviors among young injection drug users. J Psychoactive Drugs. 2013;45(2):112–121. doi: 10.1080/02791072.2013.785811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson ME, Fisher DG, Fenaughty A, Theno SA. Hepatitis C virus and depression in drug users. Am J Gastroenterol. 1998;93(5):785–789. doi: 10.1111/j.1572-0241.1998.225_a.x. [DOI] [PubMed] [Google Scholar]
- Jose B, Friedman SR, Neaigus A, Curtis R, Grund JP, Goldstein MF, … Des Jarlais DC. Syringe-mediated drug-sharing (backloading): a new risk factor for HIV among injecting drug users. AIDS. 1993;7(12):1653–1660. doi: 10.1097/00002030-199312000-00017. [DOI] [PubMed] [Google Scholar]
- Kerr T, Fairbairn N, Tyndall M, Marsh D, Li K, Montaner J, Wood E. Predictors of non-fatal overdose among a cohort of polysubstance-using injection drug users. Drug Alcohol Depend. 2007;87(1):39–45. doi: 10.1016/j.drugalcdep.2006.07.009. [DOI] [PubMed] [Google Scholar]
- Khosla N, Juon HS, Kirk GD, Astemborski J, Mehta SH. Correlates of non-medical prescription drug use among a cohort of injection drug users in Baltimore City. Addict Behav. 2011;36(12):1282–1287. doi: 10.1016/j.addbeh.2011.07.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knowlton AR, Nguyen TQ, Robinson AC, Harrell PT, Mitchell MM. Pain Symptoms Associated with Opioid Use among Vulnerable Persons with HIV: An exploratory study with implications for palliative care and opioid abuse prevention. J Palliat Care. 2015;31(4):228–233. doi: 10.1177/082585971503100404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kral AH, Bluthenthal RN, Lorvick J, Gee L, Bacchetti P, Edlin BR. Sexual transmission of HIV-1 among injection drug users in San Francisco, USA: risk-factor analysis. Lancet. 2001;357(9266):1397–1401. doi: 10.1016/S0140-6736(00)04562-1. [DOI] [PubMed] [Google Scholar]
- Lankenau SE, Sanders B, Bloom JJ, Hathazi DS, Alarcon E, Tortu S, Clatts M. Prevalence and Patterns of Prescription Drug Misuse among Young Ketamine Injectors. J Drug Issues. 2007;37(3):717–736. doi: 10.1177/002204260703700311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macalino GE, Celentano DD, Latkin C, Strathdee SA, Vlahov D. Risk behaviors by audio computer-assisted self-interviews among HIV-seropositive and HIV-seronegative injection drug users. AIDS Educ Prev. 2002;14(5):367–378. doi: 10.1521/aeap.14.6.367.24075. [DOI] [PubMed] [Google Scholar]
- Manchikanti L, Helm S, 2nd, Fellows B, Janata JW, Pampati V, Grider JS, Boswell MV. Opioid epidemic in the United States. Pain Physician. 2012;15(3 Suppl):ES9–38. [PubMed] [Google Scholar]
- Nelson LS, Juurlink DN, Perrone J. Addressing the Opioid Epidemic. Jama. 2015;314(14):1453–1454. doi: 10.1001/jama.2015.12397. [DOI] [PubMed] [Google Scholar]
- Peirce GL, Smith MJ, Abate MA, Halverson J. Doctor and pharmacy shopping for controlled substances. Med Care. 2012;50(6):494–500. doi: 10.1097/MLR.0b013e31824ebd81. [DOI] [PubMed] [Google Scholar]
- Schoenbaum EE, Hartel D, Selwyn PA, Klein RS, Davenny K, Rogers M, … Friedland G. Risk factors for human immunodeficiency virus infection in intravenous drug users. N Engl J Med. 1989;321(13):874–879. doi: 10.1056/NEJM198909283211306. [DOI] [PubMed] [Google Scholar]
- Stogner JM, Sanders A, Miller BL. Deception for drugs: self-reported “doctor shopping” among young adults. J Am Board Fam Med. 2014;27(5):583–593. doi: 10.3122/jabfm.2014.05.140107. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Service Administration. [Accessed 02/24/17];Key Substance Use and Mental Health Indicators in the United States: Results from the 2015 National Survey on Drug Use and Health. 2015 Retrieved from: https://www.samhsa.gov/data/sites/default/files/NSDUH-FFR1-2015/NSDUH-FFR1-2015/NSDUH-FFR1-2015.pdf.
- Vlahov D, Anthony JC, Munoz A, Margolick J, Nelson KE, Celentano DD, Solomon L, Polk BF. The ALIVE study, a longitudinal study of HIV-1 infection in intravenous drug users: description of methods and characteristics of participants. NIDA Res Monogr. 1991;109:75–100. [PubMed] [Google Scholar]
- Wisniewski AM, Purdy CH, Blondell RD. The epidemiologic association between opioid prescribing, non-medical use, and emergency department visits. J Addict Dis. 2008;27(1):1–11. doi: 10.1300/J069v27n01_01. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.