Notes
Editorial note
This review question is now being addressed according to a new protocol, published 11 June 2021: https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD014845 For this review, the authors are narrowing the focus to energy labelling, as well as broadening the range of target products to include alcoholic drinks, reflecting recent policy interest in energy labelling on alcohol products.
Abstract
Background
Nutritional labelling is advocated as a means to promote healthier food purchasing and consumption, including lower energy intake. Internationally, many different nutritional labelling schemes have been introduced. There is no consensus on whether such labelling is effective in promoting healthier behaviour.
Objectives
To assess the impact of nutritional labelling for food and non‐alcoholic drinks on purchasing and consumption of healthier items. Our secondary objective was to explore possible effect moderators of nutritional labelling on purchasing and consumption.
Search methods
We searched 13 electronic databases including CENTRAL, MEDLINE and Embase to 26 April 2017. We also handsearched references and citations and sought unpublished studies through websites and trials registries.
Selection criteria
Eligible studies: were randomised or quasi‐randomised controlled trials (RCTs/Q‐RCTs), controlled before‐and‐after studies, or interrupted time series (ITS) studies; compared a labelled product (with information on nutrients or energy) with the same product without a nutritional label; assessed objectively measured purchasing or consumption of foods or non‐alcoholic drinks in real‐world or laboratory settings.
Data collection and analysis
Two authors independently selected studies for inclusion and extracted study data. We applied the Cochrane 'Risk of bias' tool and GRADE to assess the quality of evidence. We pooled studies that evaluated similar interventions and outcomes using a random‐effects meta‐analysis, and we synthesised data from other studies in a narrative summary.
Main results
We included 28 studies, comprising 17 RCTs, 5 Q‐RCTs and 6 ITS studies. Most (21/28) took place in the USA, and 19 took place in university settings, 14 of which mainly involved university students or staff. Most (20/28) studies assessed the impact of labelling on menus or menu boards, or nutritional labelling placed on, or adjacent to, a range of foods or drinks from which participants could choose. Eight studies provided participants with only one labelled food or drink option (in which labelling was present on a container or packaging, adjacent to the food or on a display board) and measured the amount consumed. The most frequently assessed labelling type was energy (i.e. calorie) information (12/28).
Eleven studies assessed the impact of nutritional labelling on purchasing food or drink options in real‐world settings, including purchases from vending machines (one cluster‐RCT), grocery stores (one ITS), or restaurants, cafeterias or coffee shops (three RCTs, one Q‐RCT and five ITS). Findings on vending machines and grocery stores were not interpretable, and were rated as very low quality. A meta‐analysis of the three RCTs, all of which assessed energy labelling on menus in restaurants, demonstrated a statistically significant reduction of 47 kcal in energy purchased (MD −46.72 kcal, 95% CI −78.35, −15.10, N = 1877). Assuming an average meal of 600 kcal, energy labelling on menus would reduce energy purchased per meal by 7.8% (95% CI 2.5% to 13.1%). The quality of the evidence for these three studies was rated as low, so our confidence in the effect estimate is limited and may change with further studies. Of the remaining six studies, only two (both ITS studies involving energy labels on menus or menus boards in a coffee shop or cafeteria) were at low risk of bias, and their results support the meta‐analysis. The results of the other four studies which were conducted in a restaurant, cafeterias (2 studies) or a coffee shop, were not clearly reported and were at high risk of bias.
Seventeen studies assessed the impact of nutritional labels on consumption in artificial settings or scenarios (henceforth referred to as laboratory studies or settings). Of these, eight (all RCTs) assessed the effect of labels on menus or placed on a range of food options. A meta‐analysis of these studies did not conclusively demonstrate a reduction in energy consumed during a meal (MD −50 kcal, 95% CI −104.41, 3.88, N = 1705). We rated the quality of the evidence as low, so our confidence in the effect estimate is limited and may change with further studies.
Six laboratory studies (four RCTs and two Q‐RCTs) assessed the impact of labelling a single food or drink option (such as chocolate, pasta or soft drinks) on energy consumed during a snack or meal. A meta‐analysis of these studies did not demonstrate a statistically significant difference in energy (kcal) consumed (SMD 0.05, 95% CI −0.17 to 0.27, N = 732). However, the confidence intervals were wide, suggesting uncertainty in the true effect size. We rated the quality of the evidence as low, so our confidence in the effect estimate is limited and may change with further studies.
There was no evidence that nutritional labelling had the unintended harm of increasing energy purchased or consumed. Indirect evidence came from five laboratory studies that involved mislabelling single nutrient content (i.e. placing low energy or low fat labels on high‐energy foods) during a snack or meal. A meta‐analysis of these studies did not demonstrate a statistically significant increase in energy (kcal) consumed (SMD 0.19, 95% CI −0.14to 0.51, N = 718). The effect was small and the confidence intervals wide, suggesting uncertainty in the true effect size. We rated the quality of the evidence from these studies as very low, providing very little confidence in the effect estimate.
Authors' conclusions
Findings from a small body of low‐quality evidence suggest that nutritional labelling comprising energy information on menus may reduce energy purchased in restaurants. The evidence assessing the impact on consumption of energy information on menus or on a range of food options in laboratory settings suggests a similar effect to that observed for purchasing, although the evidence is less definite and also of low quality.
Accordingly, and in the absence of observed harms, we tentatively suggest that nutritional labelling on menus in restaurants could be used as part of a wider set of measures to tackle obesity. Additional high‐quality research in real‐world settings is needed to enable more certain conclusions.
Further high‐quality research is also needed to address the dearth of evidence from grocery stores and vending machines and to assess potential moderators of the intervention effect, including socioeconomic status.
Plain language summary
Nutritional labelling to promote healthier consumption and purchasing of food or drinks
A poor diet including excessive energy intake is an important cause of ill health. Nutritional labelling may help people to make healthier food choices.
What is the aim of this review?
This review investigated whether nutritional labels (i.e. labels providing information about nutritional content) persuade people to buy or consume different (healthy) kinds of food. We searched for all available evidence to answer this question and found 28 studies.
Key messages
There is evidence to suggest that nutritional labelling, with energy information (e.g. calorie counts) on menus, may reduce energy purchased in restaurants, but more high‐quality studies are needed to make this finding more certain.
What was studied in the review?
Some studies assessed buying food or drinks from vending machines, grocery stores, restaurants, cafeterias, or coffee shops. Others assessed the amount of food or drink consumed during a snack or meal in an artificial setting or scenario (referred to as laboratory studies or settings).
What are the main results of the review?
Nutritional labelling on restaurant menus reduced the amount of energy (i.e. calories) purchased, but the quality of the three studies that contributed to this finding was low, so our confidence in the effect estimate is limited and may change with further studies. Eight studies assessed this same type of intervention in laboratory settings, but instead of evaluating how much energy participants purchased, these studies evaluated how much energy participants consumed. These studies did not conclusively demonstrate a reduction in energy consumed when menus or foods were labelled, and they were also of low quality.
In addition, six laboratory studies assessed how much energy participants consumed when they were given one food or drink option with or without labels, and five laboratory studies assessed how much energy participants consumed when foods were experimentally labelled as low energy or low fat when they were actually high‐energy foods (i.e. mislabelling). Results from these two groups of studies were inconclusive and of low, or in the case of mislabelling studies, very low quality. We found some studies that assessed labelling on vending machines and grocery stores, but their results were not easy to interpret, so we could not use them to inform this review.
How up‐to‐date is this review?
The evidence is current to 26 April 2017.
Summary of findings
Summary of findings 1. Summary of findings table.
| Nutritional labelling compared to no labelling for healthier food purchasing and consumption | ||||||
| Patient or population: university students/staff and general consumers Setting: real‐world and laboratory settings Intervention: nutritional labelling Comparison: no labelling | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Risk with no labelling | Risk with nutritional labelling | |||||
| Food purchased from vending machines assessed with: diet soda beverages/week Follow‐up: 5 weeks a | Although more beverages were purchased in the labelling group, large baseline imbalances arising from a small number of randomised units meant that an accurate effect size could not be calculated. | — | (1 RCT) | ⊕⊝⊝⊝ Very lowb | Sample size unknown (population purchasing from 3 intervention and 2 control public vending machines) | |
| Food purchased from a grocery store assessed with: calorie‐healthy foods as % of sales Follow‐up: 94 months | Sales performance decreased after labelling was introduced in this interrupted time series study, although this was difficult to interpret because results were measured as health foods as a proportion of overall foods, rather than directly measuring the number of products purchased. | — | (1 ITS study) | ⊕⊝⊝⊝ Very lowc | Sample size unknown (population purchasing from a large chain of grocery stores) | |
| Food purchased in restaurants (labels on menus) assessed with: kcal Follow‐up: range 2 weeks to 19 weeks | The median food purchased in restaurants was 746 kcald | MD 46.72 kcal fewer (78.35 fewer to 15.10 fewer)e | — | 1877 (3 RCTs) | ⊕⊕⊝⊝ Lowf | Six additional studies (one Q‐RCT and 5 ITS studies which took place in a restaurant, cafeterias or coffee shops) also measured purchasing, 2 of which were ITS studies at low risk of bias (which assessed energy labels on menus/menu boards in a coffee shop or cafeteria) and found results consistent with this meta‐analysis. |
| Food consumed in laboratory settings (labels on menus or labels placed on a range of food options) assessed with: kcal | The median food consumed in laboratory settings was 796.4 kcald | MD 50.27 kcal fewer (104.41 fewer to 3.88 more) | — | 1705 (8 RCTs) | ⊕⊕⊝⊝ Lowg | — |
| Food consumed in laboratory settings (single snack food or drink option) assessed with: kcal | The median food consumed in laboratory settings was 316.975 kcald | SMD 0.05 (95% CI −0.17 to 0.27), P = 0.67 | — | 732 (6 RCTs) | ⊕⊕⊝⊝ Lowh | An SMD of 0.05 represents a small effect (Cohen 1988). |
| Potential harms (high‐energy snack foods consumed with misleading low fat/energy labels in laboratory settings) assessed with: kcal | The median food consumed with misleading low fat/energy labels in laboratory settings was 190 kcald | SMD of 0.19 (95% CI −0.14to 0.51), P = 0.25 | — | 831 (5 RCTs) | ⊕⊝⊝⊝ Very lowi | An SMD of 0.19 represents a small effect (Cohen 1988). |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RR: risk ratio; OR: odds ratio. | ||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low quality: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect Very low quality: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect | ||||||
aAll outcomes measuring immediate purchasing or consumption decisions at the point of exposure to the label, although returning customers in non‐laboratory settings may have experienced repeat exposure during the study period. bDowngraded by two levels for very serious risk of bias and one level for a high degree of imprecision given no useful effect estimate could be calculated. cRating begins at 'low' as this is an observational study. Downgraded by one level for serious risk of bias, and one level for indirectness, as outcome was measured as a proportion of overall purchasing rather than directly measured. dMedian value among the control groups in the included studies. e Assuming this result applied consistently to a population average meal of 600 kcal, this would represent a reduction of 7.8% (95% CI 2.5% to 13.1%). f Downgraded by two levels for very serious risk of bias. g Downgraded by one level for imprecision, as the 95% confidence interval included the possibility of no effect and of a meaningful decrease, and by one level for indirectness, as behaviour observed in a laboratory setting may not be applicable to real‐world settings. Although five of the included studies were at unclear risk of bias, we did not downgrade for risk of bias. hDowngraded by one level for serious risk of bias and one level for indirectness, as behaviour observed in a laboratory setting may not be applicable to real‐world settings. iDowngraded one level for serious risk of bias, one level for heterogeneity, one level for indirectness (as behaviour observed in a laboratory setting may not be applicable to real‐world settings) and one level for imprecision (as the 95% confidence interval included the possibility of a meaningful decrease or increase).
Background
Description of the condition
Poor diets contribute to the global prevalence and burden of obesity and preventable diseases including cardiovascular disease, diabetes and many forms of cancer. Worldwide, excess weight is now a problem in countries of all income brackets, with 2.8 million people estimated to die annually as a result of obesity (WHO Obesity Fact Sheet). In the UK, suboptimal diet is one of the leading causes of years of life lost (Newton 2015). Diet‐related disease is a substantial threat to the health of populations and a challenge to the effective and economic provision of health services (Foresight 2007; WHO 2013). However, changing behaviour to halt and reverse rises in these potentially preventable diseases is difficult. While many people want to engage in behaviours that promote good health, including healthy eating, most people find it difficult to implement and maintain them (Ogden 2007). Recognition is growing that these difficulties are in part due to the physical environments that surround us, which can exert considerable influences on our health‐related behaviours, with relatively little conscious engagement (Hollands 2016; Marteau 2012). Altering these environments may provide a catalyst for behaviour change (Das 2012; Marteau 2012). In recent work, stemming from a systematic scoping review (Hollands 2013a; Hollands 2013b), we described a set of interventions to change health‐related behaviours that involve altering the small‐scale physical environment in which that behaviour is performed (Hollands 2017b). This includes interventions that use text and symbols to convey specific information about products and their use – nutritional labelling being one example.
Description of the intervention
Nutritional labels provide information about the nutritional content of a food or drink. The type of information provided varies, for example, with regard to the nutrients such as fat, sugar, salt or energy content. The form of providing information also varies, for example, as a single number, as a proportion of a guideline for daily consumption, or with colours indicative of relative healthiness.
Until recently, most food that was eaten was homemade from raw ingredients, making the content apparent to those planning and preparing a household's meals. Progressively, however, people have been preparing fewer of their meals from scratch; pre‐prepared, often pre‐packaged, meals now form a substantial part of dietary intake in many parts of the world. These meals or snacks are often complex items, consisting of a mix of ingredients that make it difficult for consumers to know their nutritional content.
For several decades, pre‐packaged foods have provided ingredient and nutrient declarations in order to provide consumers with information about the product. In 1967, the US Federal Trade Commission enacted the Fair Packaging and Labelling Act, requiring that food should be "honestly and informatively" labelled (FTC 2016). In 1990, further legislation in the USA (the Nutrition Labelling and Education Act) made nutritional labelling compulsory on all pre‐packaged foods, and nutrient content claims, such as 'low fat', had to meet Food and Drug Administration (FDA) regulations (FDA 1994). In the same year, the European Union passed a directive to guide 'clearly visible' nutritional labelling (EEC 1990). This labelling was not compulsory unless associated with a nutritional claim, although it was widely adopted. In December 2014 the Food Information Regulations superseded the previous directive, making ingredient and nutrition declarations mandatory for most pre‐packaged foods from December 2016 (European Union 2011). These regulations stipulate that manufacturers must provide nutritional information in a consistent format for most pre‐packed foods including information on fat, saturated fat, carbohydrate, total sugars, protein and salt (expressed per 100 g or per 100 ml of the food product).
Additionally, manufacturers are able to repeat information in 'the principal field of vision' i.e. front of pack. This is purely voluntary but, where provided, only information on energy or energy plus fat, saturated fats, sugars and salt can be given, either per 100g or 100 ml and/or per portion. These front‐of‐pack nutritional labelling schemes have usually been designed to guide consumer choice and sometimes include an interpretative component, such as reference to daily intake guidelines or colour coding to indicate relative healthiness. These can supplement, but not replace, the mandatory, back‐of‐pack nutrition declarations. In the UK, for example, a voluntary front‐of‐pack scheme using red, amber and green colour coding according to nutrient content, is widely used. In Sweden, a voluntary front‐of‐pack keyhole label, which aims to help consumers choose healthier foods, has been used for the last 20 years. Norway and Denmark also adopted this approach in 2016 (Nordic Council of Ministers 2016). In Australia and New Zealand, a healthy heart tick symbol has been in use for over 25 years, but in June 2014 a new voluntary front‐of‐pack Health Star Rating System began to gradually take its place (Commonwealth of Australia 2016). This label provides information on energy, saturated fat, sugars, sodium and fibre, together with a rating of the overall nutritional profile, ranging from half a star to five stars.
Other countries, including Canada, Australia and New Zealand, have adopted mandatory nutritional labelling. In Australia and New Zealand, mandatory labelling of all manufactured foods took effect in December 2002 (Food Standards 2002). This requires a nutrition information panel that presents details on energy, fat, saturated fat, protein, carbohydrate, sugar and sodium per serving and per 100 g of food. In Canada, labelling has been mandatory on almost all pre‐packaged foods since December 2007 (Health Canada 2016). This labelling includes a 'Nutrition facts' table, which provides information on the amount of 13 core nutrients and energy in a defined amount of food. In these countries, there are no specific requirements regarding whether the label is placed on the front or back of the pack. Other countries with mandatory nutritional labelling include Mexico, Argentina, Brazil, Chile, Colombia, Ecuador, Paraguay, Uruguay, Israel, Gulf Cooperation Council members, Japan, India, China, Hong Kong, South Korea, Malaysia, Taiwan and Thailand (EUFIC 2013).
In addition to labelling pre‐packaged foods, some countries have introduced labelling on menus. Mandatory energy labelling in restaurants was first introduced in the state of New York (USA) in 2008 (Dumanovsky 2011). In December 2016, the FDA 'final rule' for all states became effective, requiring that energy information be listed on menus and menu boards in chain restaurants with 20 or more locations as well as in all vending machines by May 2017 (FDA 2016). Similarly, the Healthy Menu Choices Act 2015 came into force in January 2017 in Ontario, Canada. Since February 2011, some states of Australia have also implemented a labelling policy, requiring mandatory energy labelling on menus in fast food chains and on vending machines (Obesity Policy Coalition 2014).
In the absence of international agreements, there is considerable variation in both the information provided and the presentation format for nutritional labelling (see Figure 1 a,b,c for some examples of current nutritional labels). In a taxonomy to classify health‐related food labelling, Rayner 2013 divides point‐of‐purchase food labels into two broad classes: 'information' and 'claims'. While useful for organising the broad range of labels on foods, the taxonomy is insufficiently detailed for studying their behavioural impact. For example, it does not discriminate between labels that are numeric, verbal or pictorial in form. Consequently, it is difficult to use this typology to compare interventions across the range of dimensions likely to influence the effectiveness of labels for changing product purchasing and consumption.
1.
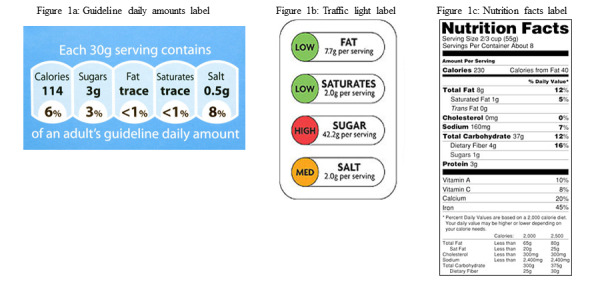
Examples of nutritional labels used in practice
Front‐of‐pack nutritional labelling approaches fall into three broad categories.
Numerical information on nutrient content.
Interpretative labelling, for example the use of colour coding to indicate how healthy products are.
Logos that indicate whether a product meets a pre‐determined guideline regarding healthiness.
In summary, nutritional labelling has been recommended as a means to enable consumers to make healthier choices about what they buy and how much they eat (WHO 2004). However, the evidence for the impact of nutritional labelling on food purchasing and consumption is unclear. Developing a more comprehensive understanding of this impact would inform future policy decisions about the implementation of nutritional labelling. It would also inform our understanding of the relationships between different types of information on food packages and thus inform both future implementation and evaluation of the effects of nutritional labelling.
How the intervention might work
Effects of nutritional labelling
Nutritional labelling may impact on population health by leading to healthier food purchasing and ultimately, healthier consumption. Healthier food purchasing and consumption are defined as:
increased purchasing or consumption of products considered healthy in relation to recognised nutritional guidelines; and/or
decreased purchasing or consumption of products considered less healthy in relation to these standards.
Processes by which nutritional labelling may have an impact on food choices and health
Nutritional labelling has been proposed as an intervention that enables individuals to make healthier choices about the foods they purchase and consume (Cowburn 2005; Dobbs 2014; WHO 2004). Figure 2 shows the logic model explaining the processes by which nutritional labelling might be expected to lead to food purchasing and consumption, resulting in improved health. These include increasing understanding of the healthiness of food and drink, as well as increasing the availability of healthy foods. The setting in which people purchase food (e.g. a grocery store, fast food or other restaurant) (Bollinger 2011; Harnack 2008a), expectations of the taste of the food (Wansink 2004), and food prices (Horgen 2002) may all modify the impact of labels. The cultural context in which the food is purchased or consumed may also have an impact because diets and attitudes to nutrition vary between countries (Brownell 2006), and such differences may have an impact on the behavioural effects of labels. Finally, individual differences in body weight (Wansink 2006 ‐ study 3), socioeconomic status (Malam 2009), gender (Aron 1995), and dietary restraint (i.e. the extent to which an individual is actively trying to restrict their energy intake) may further modify the impact of nutritional labelling.
2.
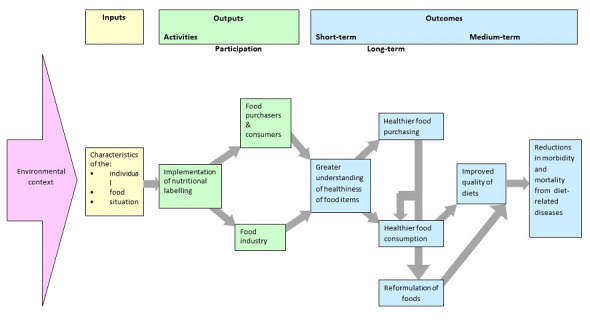
Logic model of the process by which nutritional labelling may have an impact on diets and health
Direct and indirect impact of labels on the individual
The use of nutritional labels may have an impact not only on individuals who purchase or consume the food but also on the restaurant or retailer by altering the range of products available or, on the food industry as a whole, by encouraging the reformulation of products to achieve a healthier nutritional profile on a visible label. Figure 2 indicates the possible impact of nutritional labelling on the behaviour of the food industry directly, through stimulating reformulation of products and indirectly, from changes in consumer purchasing and consumption.
Why it is important to do this review
The large and increasing prevalence of diet‐related disease worldwide requires population‐level interventions to promote healthier diets. Although nutritional labelling has been implemented in North America, Europe and Australasia, there is no consensus on whether it is effective for achieving healthier purchasing and consumption or on which domain, if any, labels are most effective. The variety of schemes implemented may contribute to confusion. The absence of consensus on nutritional labelling policy is reflected in different recommendations and changes to recommendations about implementation that have been made internationally. For example, while the European Union recommended the use of guideline daily amounts with optional "additional forms of expression" (European Commission 2011), the UK Department of Health has recommended subsequent adoption of a labelling system combining elements of guideline daily amounts and traffic light labelling (UK Dept Health 2013). Similarly, while the implementation of a traffic‐light labelling scheme in Australia was recommended (Blewett 2011), subsequently a new interpretative 'Health Stars' scheme has been developed (Australian Dept Health and Aging 2013).
There is a need for robust evidence to support decisions regarding the implementation of nutritional labelling and the development of food policy and programmes globally. Although previous systematic reviews have evaluated the impact of nutritional labelling, they have not restricted primary outcomes to objectively measured food or drink purchasing and consumption behaviours. Some reviews, for example, include studies with both objective and self‐reported behavioural outcomes as well as non‐behavioural outcomes (Campos 2011; Cecchini 2016; Grunert 2007; Mhurchu 2007).
The current review identified and collated existing research evidence concerning the impact of nutritional labels on food purchasing and consumption to assess the beneficial and adverse impacts of nutritional labelling on diets and the factors that moderate these effects.
Objectives
To assess the impact of nutritional labelling for food and non‐alcoholic drinks on purchasing and consumption of healthier items. Our secondary objective was to explore possible effect moderators of nutritional labelling on purchasing and consumption.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs) or quasi‐randomised controlled trials (Q‐RCTs) that compared a labelling intervention with a no‐label (or incomplete label) control. We included quasi‐randomised studies, in which the randomisation sequence was not truly random (Reeves 2011), because of the difficulty of implementing true randomisation at an aggregate, population level. We also considered cluster‐randomised studies, when randomisation is by site (e.g. grocery store).
Other eligible study designs included interrupted time series studies (ITS) that compared purchasing or consumption before and after the implementation of nutritional labelling. In line with the Cochrane Effective Practice and Organisation of Care (EPOC) group recommendations, we only included ITS studies if they had a clearly defined time point at which the intervention occurred and at least three observation periods both before and after the intervention (EPOC 2015). Authors had to present these data within a graph and/or at the very least analyse them using regression analysis, preferably using segmented regression. Based on Cochrane recommendations, we excluded studies that reported only a simple pre‐ and postintervention comparison unless we could make a valid justification for their inclusion or if a re‐analysis could enable the inclusion of data from multiple observations before and after the intervention using repeated measures methods (Cochrane Public Health Review Group 2010; EPOC 2015).
Finally, we also considered controlled before‐and‐after studies (CBA) that measured purchasing or consumption before and after implementation of an intervention in non‐randomised intervention and control groups. To be included in the review, studies needed to have at least two intervention sites and two control sites, and the characteristics of the different groups had to be similar (EPOC 2015).
Types of participants
Adults or children purchasing or consuming food or drink were eligible for inclusion. Purchases included those bought by an individual for their personal consumption, or for consumption by a small group that the individual belonged to, such as their family. Food or drink purchases included those from any retail outlet including grocery stores and other food stores, vending machines, cafeterias and both fast food and non‐fast food restaurants.
Types of interventions
Eligible interventions included the nutritional labelling of a food or a non‐alcoholic drink product. We identified three characteristics of nutritional labelling with a potential impact on behaviour.
Type of nutrient. The label provides information about one or more nutrient or energy contained in the product. These nutrients typically include those for which reductions in intake are recommended, including fat, saturated fat, salt and sugar, and they may also include those for which increases in intake are recommended, such as vitamins or minerals. We did not consider warning labels about product content that pose an immediate health threat to some people, for example 'contains peanuts', to be nutritional labels in the current context. Figure 1c shows the US nutrition facts label indicating a range of nutrients that labels may describe. Although technically not a nutrient, we included energy (e.g. calories) in this category.
Amount of nutrient. Information is given indicating the amount of different types of nutrients or energy contained in the product or in a serving size. This information may be absolute or relative. If absolute, the label would use numeric information about content, for example, 'total fat ‐ 12 grams'. If relative, the label would use a verbal descriptor of the amount of the nutrient or energy contained in the product such as 'lower fat'. However, 'a good source of vitamin C' or 'contains whole grain' would not be considered a nutritional label as 'good' and 'contains' are not descriptors of amount.
Visibility. The labels needed to be visible upon purchase or consumption. In some cases, the label might be placed on the front of product packages or containers. In other cases, the label might not appear on but rather alongside the product. Examples include labels on a shelf where the food or drink is being displayed in a grocery store, on the exterior of a vending machine selling snacks, on the counter from which the food is being served in a cafeteria, or on a restaurant menu from which food is being selected.
We classified nutritional labels that did not have the characteristics specified above as incomplete and considered them ineligible. We only included interventions that combined nutritional labelling with other interventions if we could isolate the impact of the nutritional label. We did not consider logos providing a summary assessment of the healthiness of a product or general health claims to provide nutritional information and so excluded them from this review.
As noted above, the intervention labelling group had to be compared with a no‐labelling (or incomplete) control group. Thus, we excluded studies that only compared two or more different types of labelling schemes without a control group.
Types of outcome measures
Eligible studies had to report an objectively measured behavioural outcome of food or drinks purchased or consumed. Given that alcohol consumption involves different processes from non‐alcoholic drinks, we investigated the impact of nutritional labelling on purchasing and consumption of non‐alcoholic drinks only.
Primary outcomes
The primary outcomes were healthier choices of:
food or drink purchased (i.e. payment with money) from vending machines, supermarkets or grocery stores, restaurants, cafeterias or other contexts in which food and drink for immediate consumption are sold;
food or drinks consumed in real‐world or laboratory settings; and
harm or unintended consequences of nutritional labels, such as increased energy consumption from single nutrient labelling implying a healthier product.
Purchasing
We considered healthier food and drink purchasing to be:
fewer purchases of less healthy items or overall reductions in purchases of less healthy target nutrients or energy;
more purchases of healthier items or overall increases in purchases of healthier target nutrients or energy.
Food and drink purchases could be assessed either at the individual or population group level. In the context of this review, an individual level purchasing outcome measure required direct observation of what was purchased:
from a vending machine; this comprised a record of everything purchased by the individual on that visit, or a record of items, such as chocolate bars, targeted in the intervention;
in a restaurant; this comprised a record of everything purchased by the individual for consumption on that visit, or a record of items, such as soft drinks, targeted in the intervention and purchased for consumption on that visit;
in a grocery store; this comprised a record of everything purchased by the individual on that visit, or a record of items, such as ready meals, targeted by the intervention and purchased on that visit.
At a population level, purchasing data had to be derived from sales data supplied by the retailer from till receipts. Such data could be presented as sales of specific items or as total nutrients or energy purchased, calculated from the sales data presented. When studies assessed purchasing in terms of the overall healthiness of the specific product labelled, analyses presented in the research reports needed to indicate which products were considered more or less healthy in line with the labelling given. We excluded studies that evaluated intention to purchase or intention to consume without an objectively assessed measure of the behaviour.
Consumption
We considered healthier food or drink consumption to be:
lower consumption of less healthy foods or an overall reduction in consumption of less healthy target nutrients or energy;
greater consumption of healthier foods or an overall increase in consumption of healthier target nutrients.
Studies had to assess consumption by an objective measure, calculating the amount of a snack or a meal consumed by subtracting the amount of food remaining after consumption from the amount of food served. This was specified as either:
amount of a food or drink consumed; or
total target nutrients or energy consumed as part of a meal.
To assess the absolute healthiness of products forming part of interventions included in this review would require knowledge of the full nutritional content of each product offered to study participants and how it was consumed relative to other components of the diet. Therefore, the definition of a more or less healthy product is based on the relative composition of the items tested, with reference to international dietary guidelines.
Secondary outcomes
There were no secondary outcomes.
Other measures
We also assessed possible moderating effects on the primary outcomes above, presented in the section below on Subgroup analysis and investigation of heterogeneity.
Search methods for identification of studies
Electronic searches
We conducted electronic searches of the following databases.
Cochrane Central Register of Controlled Trials (CENTRAL; 2017, Issue 3) in the Cochrane Library (last searched 12 March 2017).
Cochrane Database of Systematic Reviews (CDSR; 2017, Issue 4) in the Cochrane Library (last searched 12 April 2017).
MEDLINE OvidSP (1946 to 25 April 2017).
Embase OvidSP (1974 to 25 April 2017).
CINAHL EBSCO Host (1981 to 26 April 2017).
Trophi (Evidence for Policy and Practice Information (EPPI) Centre Database; 2004 to 11 August 2017).
PsycINFO OvidSP (1967 to April Week 3 2017 [searched 26 April 2017]).
Applied Social Sciences Index and Abstracts (ASSIA) from Cambridge Scientific Abstracts (CSA) Proquest (1987 to 26 April 2017).
Sociological abstracts (Proquest; 1952 to 26 April 2017).
ABI/INFORM Global (Proquest; 1970s [precise date not available] to 26 April 2017).
SCOPUS Reed Elsevier (1966 to 26 April 2017).
Science Citation Index & Social Science Citation Index (Web of Science Core Collection, Thomson Reuters) (1945 to 26 April 2017).
HMIC (Health Management Information Consortium; OvidSP; 1979 to January 2017 [searched 26 April 2017]).
We also searched trial registries for potentially relevant studies that were completed or in progress (July 2017), using the WHO International Clinical Trials Registry Platform (ICTRP) and ClinicalTrials.gov. We obtained potentially relevant studies from the following clinical trial databases: NCT (ClinicalTrials.gov); Australian New Zealand Clinical Trials Registry (ACTRN) (www.anzctr.org.au); European Union Clinical Trials Register (EUCTR) (www.clinicaltrialsregister.eu/ctr-search/search); Deutsches Register Klinischer Studien (DRKS) German Clinical Trials Register (www.drks.de/drks_web); Nederlands Trial Register (NTR) (www.trialregister.nl/trialreg/index.asp); the International Standard Randomised Controlled Trial Number (ISRCTN) Register (www.isrctn.com); Registro Brasileiro de Ensaios Clínicos (RBR) (www.ensaiosclinicos.gov.br); Sri Lanka Clinical Trials Registry (SLCTR) (www.slctr.lk); the Clinical Trials Registry – India (CTRI) (ctri.nic.in/Clinicaltrials/login.php); Chinese Clinical Trial Register (ChiCTR) (www.chictr.org.cn/abouten.aspx); Iranian Registry of Clinical Trials (IRCT) (www.irct.ir); Japan Primary Registries Network (JPRN) (rctportal.niph.go.jp); Korean Clinical Trial Registry (KCT) (cris.nih.go.kr/cris/index.jsp); and the Thai Clinical Trials Registry (TCTR) (www.clinicaltrials.in.th).
Appendix 1 shows the search strategies for each database. We applied no date or language restrictions.
We screened the reference lists of included studies to identify potential studies. We also conducted forward citation searches on the Web of Science for papers that cited included studies. Furthermore, we screened the reference lists of the systematic reviews found through a search of the Cochrane Database of Systematic Reviews to identify further potentially relevant studies.
Searching other resources
We contacted authors of all included studies and key researchers in the topic area and asked them to identify unpublished or ongoing research in the field. Additionally, we searched the websites of key organisations in the area of health and nutrition, including the following.
Departments of Health for England (www.gov.uk/government/organisations/department-of-health), Scotland (www.gov.scot/Topics/Health), Wales (gov.wales/topics/health/?lang=en), and Northern Ireland (www.health-ni.gov.uk).
Australian Federal and State Departments of Health (www.health.gov.au).
Department of Health for South Africa (www.gov.za/issues/health).
Ministry of Health and Family Welfare for India (mohfw.nic.in).
Health Canada (www.hc-sc.gc.ca/index-eng.php?).
Food Standards Agency, UK (www.food.gov.uk).
European Commission (ec.europa.eu/commission/index_en).
Rudd Centre for Food Policy and Obesity (www.uconnruddcenter.org).
Centers for Disease Control and Prevention (www.cdc.gov).
World Health Organization (who.int/en).
National Institutes for Health Office of Disease Prevention (prevention.nih.gov).
International Obesity Task Force (www.worldobesity.org).
We entered the results generated by the above searches into Endnote X6 bibliographic software and de‐duplicated them.
Data collection and analysis
Selection of studies
Two reviewers independently assessed titles and abstracts of papers for inclusion, resolving any disagreements through discussion. Failure to reach consensus led to discussion with a third reviewer. We obtained full‐text papers of potentially eligible studies identified during the first screening phase, and we assessed them for inclusion using the same procedures as for titles and abstracts.
Data extraction and management
We developed a draft data extraction form based on the Cochrane Public Health template and modified it to allow extraction of data specific to this review. Two reviewers independently piloted the draft to ensure that it enabled reliable and accurate extraction of appropriate data and then independently extracted all data on study and participant characteristics along with results. When a reviewer was an author of an included study, a third reviewer was involved in the data extraction process. If reported, we also extracted data on measures relating to the process of implementing the intervention, including any data on its cost. Once the first phase of data extraction was complete, the first author reconciled the two sets of data extraction forms. Where there were inconsistencies, the two data extractors met to discuss and reach a consensus. Where data were missing or unclear, we contacted study authors. Finally, one author entered the data into RevMan, and a second author checked the data entry.
When multiple papers reported data from the same study, we considered the papers together as one study.
Assessment of risk of bias in included studies
We assessed risk of bias for RCTs using the Cochrane 'Risk of bias' assessment tool (Higgins 2011).
Was allocation sequence randomly generated using an appropriate method (selection bias)?
Was allocation adequately concealed (selection bias)?
Were incomplete outcome data adequately addressed (attrition bias)?
Were reports of the study free of suggestion of selective outcome reporting (reporting bias)?
Were participants and personnel blinded to knowledge of allocated interventions adequately (performance bias)?
Were outcome assessors blinded to allocated intervention (detection bias)?
Was the study apparently free of other problems that could put it at risk of bias?
We considered the RCTs to be at an overall low risk of bias when they met all of the above criteria or when there was not more than one unclear criterion (with no criterion assessed as high risk). We judged studies to be at unclear risk of bias if more than one domain was at unclear risk of bias (with no criterion assessed as high risk) and at high risk of bias if one or more criteria were not adequately met.
For ITS studies, we implemented the Cochrane Public Health Review Group Guidelines for assessing risk of bias (Cochrane Public Health Review Group 2010).
Was the intervention independent of other changes?
Was the shape of the intervention effect pre‐specified (specifically, the purpose of the intervention should be the purpose of the analysis)?
Was the intervention unlikely to affect data collection?
Was knowledge of the allocated interventions adequately prevented during the study?
Were incomplete outcome data adequately addressed?
Was the study free of selective outcome reporting?
Was the study apparently free of other problems that could put it at risk of bias?
We considered ITS studies to be at an overall low risk of bias when they adequately addressed all of the above criteria and at high risk if one or more of the above criteria were not met.
We planned to assess the risk of bias of controlled before‐and‐after studies using the Quality Assessment Tool for Quantitative Studies (EPHPP 2010). As we failed to identify any relevant controlled before‐and‐after studies for inclusion in this review, we do not provide any further details of this tool (for more information see EPHPP 2010).
Measures of treatment effect
Purchase data could be either dichotomous (e.g. a more versus less healthy choice) or continuous (e.g. mean amount of nutrient or energy purchased). Consumption was generally assessed using continuous data (e.g. total nutrients or mean energy consumed). As the included studies reported no dichotomous data, we calculated a mean difference (MD) with 95% confidence intervals (CIs) for each study when possible. In two studies, however, it was only possible to calculate a standardised mean difference (SMD) with 95% CIs because the authors reported only mean kcal and F statistics (Wansink 2006 ‐ study 1; Wansink 2006 ‐ study 3). We calculated combined effect sizes using an MD with 95% CIs when studies used similar interventions and outcomes, or using an SMD when the outcomes differed (e.g. when trials measured outcomes as energy consumed at one meal or over several meals). In both cases, we used a random‐effects model to pool the data.
In order to re‐express effect sizes using a more familiar metric, we calculated the percentage reduction in energy consumed over a typical meal, using an average of 600 kcal as a baseline. This amount was based on mean daily energy intake across the UK population of 1727 kcal or 7226 kJ (standard deviation (SD) 537 kcal or 2247 kJ, using data from the UK National Diet and Nutrition Survey (National Centre for Social Research 2012). Our approach to re‐expressing effect sizes was based on Hollands 2015.
For ITS studies, we aimed to present statistical comparisons of time trends before and after the intervention (EPOC 2015). In all of the ITS studies, we present the results as described by the study authors, typically as regression analyses. When studies also presented data graphically, we did not attempt any re‐analysis using segmented time series regression techniques if the data were already appropriately analysed by the study authors or if we did not consider the study to be of sufficient quality to warrant re‐analysis. We considered one ITS study to be at low risk of bias (Bollinger 2011), but we could not re‐analyse the data presented graphically due to a lack of information. The figures presented weekly calories per transaction, but there were no data on the number of transactions per week; this means that the absolute and relative variability of each point was unknown and could not be modelled with time series to provide unbiased estimates.
Unit of analysis issues
For eligible cluster‐randomised trials, we planned to adjust the data to account for clustering if the study authors had not already done so. However, we only included one cluster‐RCT in the review, and the appropriate data needed to report and adjust the results were not available.
Dealing with missing data
We included all data in the review using an intention‐to‐treat approach where possible. Where studies reported dropouts or withdrawals, we extracted data on the number and reasons for missing data.
Assessment of heterogeneity
In order to deal with inevitable methodological variability among studies that evaluate food or drinks consumed in real‐world or laboratory settings, we took a broader perspective and considered that studies that evaluated labelling as an intervention and energy purchasing or consumption as an outcome were potentially similar enough to be combined in meta‐analyses of purchasing and consumption. We assessed statistical heterogeneity by visually examining the extent to which confidence intervals overlapped. Additionally, we reported the I² statistic, a point estimate of inconsistency, and interpreted the levels of heterogeneity made based on the recommendations of Deeks 2011.
Assessment of reporting biases
We planned to use funnel plots to identify small study effects, which in turn, could indicate publication bias. None of the included meta‐analyses, however, included more than 10 studies, so based on the recommendations of Sterne 2011, we did not carry out this action.
Data synthesis
Where one study reported a number of different types of interventions or outcome measures, we made the following decisions as to which data we would include in the analyses.
For included studies with more than one eligible intervention arm, we combined data when studies contained information about the same product characteristic (e.g. energy), albeit in multiple ways (e.g. varying in whether presented as numbers, colour‐coded, activity‐equivalents, and whether presented with recommended daily energy intake).
Where studies assessed the impact of nutritional labelling adjacent to a range of food products and it was not possible to extract an effect summary for the range of food products, we included the data for the product representing the most complete meal, for example, sales of entrées (as opposed to sales of a side dish) (e.g. Dubbert 1984). If no products represented more or less complete meals, we extracted data for products containing the greatest amount of energy.
Where studies reported a number of outcomes, such as consumption of a range of different nutrients, we used the most frequently reported outcome among the included studies (e.g. Harnack 2008a). Had outcomes been reported in the same study that related to both increased consumption of healthier foods and decreased consumption of less healthy foods, we would have prioritised the latter.
Most included studies reported on energy (described by the study authors as 'calories') as the outcome unit. Some reported on grams or millilitres (e.g. Cavanagh 2014; Roberto 2012; Vermeer 2011), and we converted these to calories using the formula presented in DeGroot 2012. We analysed purchasing and consumption studies separately, as we considered them, a priori, to be different outcomes. In the process of conducting the review, it became apparent that the studies also differed in terms of how many labelled options participants had to choose from and what kind(s) of nutritional content the labels described. Participants had to make absolute judgments when given only one labelled option and relative judgments when provided with a myriad of options labelled differently. Thus, we analysed these studies separately. We employed Review Manager 5 (RevMan 5) to perform meta‐analyses, using the inverse variance approach for continuous data (RevMan 2014). We synthesised data from non‐randomised studies in a narrative summary.
Subgroup analysis and investigation of heterogeneity
We planned subgroup analyses to assess effect modifiers and explore them as sources of heterogeneity. We chose the potential modifiers based on previous research or as considered in the section How the intervention might work. Due to a lack of information reported in the included studies, we were unable to conduct many of the planned subgroup analyses (see Differences between protocol and review). There were, however, sufficient data to explore two possible moderators of the main effects of nutritional labelling: dietary restraint and study country. We used the generic inverse variance approach to pool the MDs or SMDs, both across studies and within subgroups.
Sensitivity analysis
We repeated meta‐analyses, omitting all studies at high or unclear risk of bias.
Summary of findings and assessment of the certainty of the evidence
We prepared the Summary of findings table using the main outcomes evaluated in the included studies and as specified in Primary outcomes: food purchased from vending machines, food purchased from a grocery store, food purchased from a restaurant, cafeteria or coffee shop, food consumed in a laboratory setting (where participants were given a range of options), food consumed in a laboratory setting (where participants were given a single option), and harms (food consumed with misleading labels). All of the participants in these studies were from general populations groups, so may be considered medium risk populations. All comparisons presented in the Summary of findings table evaluate nutritional labelling (broadly) versus no labelling (i.e. it was not the remit of this systematic review to compare the effectiveness of different types of nutritional labels). Some of the summary results were presented as MD while others had to be presented using SMD for reasons described above (Measures of treatment effect).
We used the GRADE system to assess the quality of evidence for each outcome (Schünemann 2011). Using the four standard GRADE levels of quality (high, moderate, low and very low) we assigned evidence from RCTs an initial quality rating of high and evidence from non‐RCTS an initial rating of low. We upgraded (for observational studies only) or downgraded these levels based on our judgments regarding risk of bias, precision, consistency, directness and publication bias. We interpreted the overall quality level for each outcome following definitions provided by Balshem 2011.
We report the quality level assigned for each outcome, along with justification for the decisions, in the Results.
Results
Description of studies
Results of the search
Our search strategy yielded 50,270 unique records. Screening of titles and abstracts resulted in 263 records plus 15 trial registries (i.e. 278 records) that were potentially eligible and whose full text we reviewed. Overall, 28 studies (27 published and 1 unpublished study), presented in 32 papers, met the inclusion criteria (see Figure 3), while we excluded 246 records (Characteristics of excluded studies). We also identified one relevant ongoing study (see Ongoing studies), but no data were available at the time of completing the current review.
3.
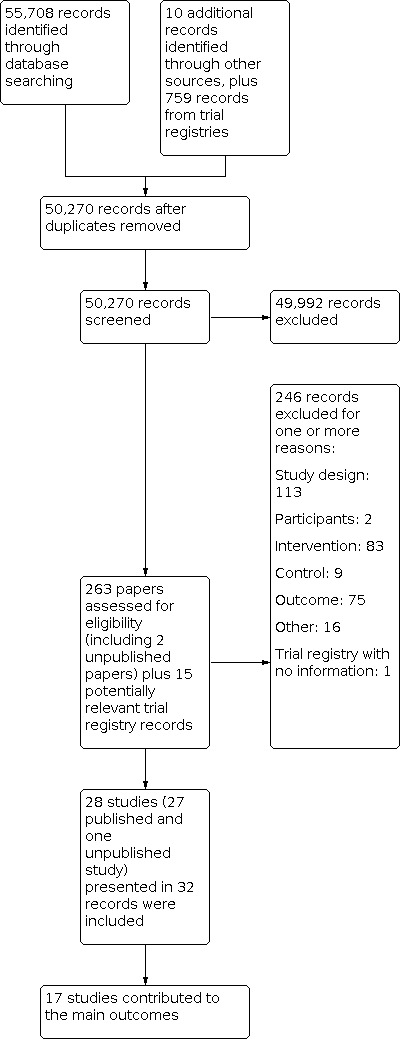
Study flow diagram
Included studies
Study design
Of the 28 studies included in the review, 17 were RCTs: 16 of these were randomised by individual (Cavanagh 2014; Crockett 2014; Ebneter 2013; Ellison 2013; Ellison 2014a; Girz 2012 ‐ study 1; Girz 2012 ‐ study 2; Girz ongoing; Hammond 2013; Harnack 2008a; James 2015Platkin 2014; Roberto 2010; Roberto 2012; Temple 2010; VanEpps 2016), while one was randomised by cluster, with vending machines being the unit of randomisation (Bergen 2006. In addition, there were five Q‐RCTs (Allan 2015; Kral 2002; Vermeer 2011; Wansink 2006 ‐ study 1; Wansink 2006 ‐ study 3), plus six ITS studies (Balasubramanian 2002; Bollinger 2011; Chu 2009; Cioffi 2015; Dubbert 1984; Holmes 2013). Bollinger 2011 was designed as a controlled before‐and‐after study, but it was only possible to extract data at different time periods for the intervention group and not the comparison group, so we treated it as an ITS.
All studies were in high‐income countries, with most (21 studies) taking place in the USA. Four studies took place in Canada, and three in Europe (two in the UK and one in the Netherlands).
Participants
Fourteen studies recruited university students or staff (Bergen 2006; Cavanagh 2014; Chu 2009; Cioffi 2015; Ebneter 2013; Girz 2012 ‐ study 1; Girz 2012 ‐ study 2; Girz ongoing; James 2015; Kral 2002; Platkin 2014; Temple 2010; Wansink 2006 ‐ study 1; Wansink 2006 ‐ study 3), six recruited university students or staff as well as members of the general population (Allan 2015; Ellison 2013; Ellison 2014a; Hammond 2013; Roberto 2010; Roberto 2012), and six recruited from general population groups (Balasubramanian 2002; Bollinger 2011; Dubbert 1984; Harnack 2008a; VanEpps 2016; Vermeer 2011). Of the remaining two studies, Holmes 2013 recruited participants from a high‐income population, while Crockett 2014 actively sought to include lower income groups by recruiting in more socially deprived areas.
Twenty‐six studies included adult participants, one included adolescents and adults (Harnack 2008a), and one study targeted families of young children by labelling a children's menu (Holmes 2013). Four studies explicitly reported recruiting women only (Cavanagh 2014; Ebneter 2013; Kral 2002; Platkin 2014), but the included studies did not consistently describe full details of study participants (including mean age, sex and ethnicity).
Interventions and comparisons
All of the included studies compared at least one form of labelling with no labelling, with most (20/28) evaluating labelling on menus or menu boards, or nutritional labelling placed on, or adjacent to, a range of foods from which participants could choose (Allan 2015; Balasubramanian 2002; Bergen 2006; Bollinger 2011; Chu 2009; Cioffi 2015; Dubbert 1984; Ellison 2013; Ellison 2014a; Girz 2012 ‐ study 1; Girz 2012 ‐ study 2; Girz ongoing, Hammond 2013; Harnack 2008a; Holmes 2013; James 2015; Platkin 2014; Roberto 2010; Temple 2010; VanEpps 2016). The remaining eight studies provided participants with only one food or drink option to choose from (Cavanagh 2014; Crockett 2014; Ebneter 2013; Kral 2002; Roberto 2012; Wansink 2006 ‐ study 1; Wansink 2006 ‐ study 3; Vermeer 2011). In these eight studies, the nutritional label was on the container or packaging, adjacent to the food, or on a display board.
Twelve studies included an intervention arm that assessed absolute energy labels on food or drinks without any other information or formatting, such as the use of colour coding (e.g. traffic light format) (Allan 2015; Bollinger 2011; Cavanagh 2014; Ebneter 2013; Ellison 2013; Ellison 2014a; Girz 2012 ‐ study 1; Girz ongoing, Hammond 2013; Platkin 2014; Roberto 2010; VanEpps 2016). Four of these studies also included an intervention arm that assessed energy information with traffic light format interventions (Ellison 2013; Ellison 2014a; Hammond 2013; VanEpps 2016). Six studies evaluated energy labelling plus other information (e.g. recommendation of daily energy intake or energy density) (Girz 2012 ‐ study 2; Harnack 2008a; James 2015; Kral 2002; Roberto 2010; Vermeer 2011), one of which was also colour coded to the level of energy density (Kral 2002). Five studies evaluated labels that provided information on energy or fat content using terms such as 'high' or 'low' (Balasubramanian 2002; Crockett 2014; Dubbert 1984; Wansink 2006 ‐ study 1; Wansink 2006 ‐ study 3), one of which also used colour coding in the same treatment arm (Crockett 2014).Three studies compared 'nutrition facts' labelling (e.g. total energy, serving size (grams), fat (grams), protein (grams), and carbohydrates (grams)) (Chu 2009; Cioffi 2015; Temple 2010). One study evaluated a 'Smart Choices' label (with information on energy per serving and servings per package) (Roberto 2012), one study evaluated labels with energy information and exercise equivalents (Platkin 2014), one evaluated energy and fat content labelling (Holmes 2013), and one study evaluated a '0 calories 0 carbs' label (Bergen 2006).
Nine of the included studies evaluated a second or third treatment arm that was also eligible for inclusion in this review (Crockett 2014; Ebneter 2013; Ellison 2013; Ellison 2014a; Hammond 2013; Platkin 2014; Roberto 2010; Roberto 2012; VanEpps 2016). Of these, seven had treatment arms that contained information about the same product characteristic in multiple ways (e.g. calories only and calories plus a traffic light format), so we combined these arms as a single labelling intervention (Ellison 2013; Ellison 2014a; Hammond 2013; Platkin 2014; Roberto 2010; Roberto 2012; VanEpps 2016). The other two studies evaluated a second treatment arm, considered separately in this review (low fat or energy labels on high‐fat foods) (Crockett 2014; Ebneter 2013).
Twenty‐five studies used a no‐label control (Allan 2015; Cavanagh 2014; Crockett 2014; Balasubramanian 2002; Bergen 2006; Bollinger 2011; Chu 2009; Cioffi 2015; Dubbert 1984; Ellison 2013; Ellison 2014a; Girz 2012 ‐ study 1; Girz 2012 ‐ study 2; Girz ongoing; Hammond 2013; Harnack 2008a; Holmes 2013; James 2015; Kral 2002; Platkin 2014; Roberto 2010; Roberto 2012; Temple 2010; VanEpps 2016; Vermeer 2011), and three studies included a regular label control (Ebneter 2013; Wansink 2006 ‐ study 1; Wansink 2006 ‐ study 3). Of these three studies, Ebneter 2013 compared 'regular fat M&M's' with additional energy information on the label versus 'regular fat M&M's' without energy information on the label. Wansink 2006 ‐ study 1 compared 'new low fat M&M's label versus a 'new colours on regular M&M'sn label, and Wansink 2006 ‐ study 3 compared a 'Low‐fat Rocky Mountain Granola' label with a 'Regular Rocky Mountain Granola' label.
The included studies aimed to either decrease consumption or purchasing of less healthy foods or increase consumption or purchasing of relatively healthier foods, with the exception of five studies (as reported above) that also assessed the impact of low fat or low energy labels on high‐fat foods (Crockett 2014; Ebneter 2013; Girz 2012 ‐ study 1; Wansink 2006 ‐ study 1; Wansink 2006 ‐ study 3).
Settings
Eleven studies were in real‐world settings (i.e. grocery stores, restaurants, cafeterias, coffee shops or other contexts in which food and drink for immediate consumption are sold) and where participants ordered and paid for their food or drinks as they would normally do in that setting (Allan 2015; Balasubramanian 2002; Bergen 2006; Bollinger 2011; Chu 2009; Cioffi 2015; Dubbert 1984; Ellison 2013; Ellison 2014a; Holmes 2013; VanEpps 2016). Seventeen studies took place in artificial settings or scenarios (i.e. in contexts where participants would not normally order or consume food or drinks, or they did not pay for food or drinks because these were provided by the researchers), broadly considered laboratory settings (Cavanagh 2014; Crockett 2014; Ebneter 2013; Girz 2012 ‐ study 1; Girz 2012 ‐ study 2; Girz ongoing, Hammond 2013; Harnack 2008a; James 2015; Kral 2002; Platkin 2014; Roberto 2010; Roberto 2012; Temple 2010; Vermeer 2011; Wansink 2006 ‐ study 1; Wansink 2006 ‐ study 3).
Twelve studies took place in university laboratories or classrooms (Cavanagh 2014; Ebneter 2013; Girz 2012 ‐ study 1; Girz 2012 ‐ study 2; Girz ongoing, Hammond 2013; James 2015; Kral 2002; Platkin 2014; Roberto 2010; Roberto 2012; Temple 2010), three took place in other university facilities, including an open‐house area (Wansink 2006 ‐ study 1, campus grounds (Bergen 2006), a theatre (Wansink 2006 ‐ study 3), and university‐based restaurants or dining centres (Chu 2009; Cioffi 2015; Ellison 2013; Ellison 2014a). One study took place in community‐based facilities (church halls and hotel conference rooms) for reasons of convenience (Harnack 2008a). Other studies took place in a chain of coffee shops (Bollinger 2011), a hospital coffee shop (Allan 2015), a community restaurant (Holmes 2013) and a community‐based cafeteria (Dubbert 1984). Balasubramanian 2002 was in a major grocery store chain, and VanEpps 2016 in the workplace of a large healthcare company. Although two studies took place in cinemas, we considered these laboratory studies as the participants did not pay for the food or drinks which were provided by the researchers (Crockett 2014; Vermeer 2011).
Outcomes
Within each of the primary outcomes of interest, studies reported the following measures.
Purchasing
There were 11 purchasing studies in real‐world settings.
Bergen 2006 assessed the impact of labelling on drinks purchased from vending machines by measuring the mean number of low‐energy soft drinks sold weekly over a nine‐week period (two‐week baseline period, five‐week intervention period, and two‐week postintervention period).
Balasubramanian 2002 assessed the impact of labelling on 'light' entrées and juices purchased from a grocery store by measuring sales transactions (i.e. the percentage of labelled products bought relative to other products bought) each week over a seven‐year period.
Nine studies assessed the impact of labelling on food or drinks purchased in restaurants, cafeterias or coffee shops. Studies measured the outcome using the mean energy content of items purchased at each meal over a period of time (2 weeks: Ellison 2013; 4 weeks: VanEpps 2016; 41 days: Chu 2009; 2 months: Holmes 2013; 19 weeks: Ellison 2014a), mean weekly energy sales of 45 labelled food items for 12 weeks (Cioffi 2015), the proportion of high‐calorie purchases over a six‐week period (as a percentage of total drinks or snacks sold) (Allan 2015); mean energy of food and drinks bought per sales transaction over 14 months (Bollinger 2011), or the probability of purchasing low‐energy items from three different food categories (vegetables, salads, entrées) during an 18‐week period (Dubbert 1984).
Consumption
Seventeen studies assessed the impact of labelling on food or drink consumed in artificial or laboratory settings. In 14 of these studies, the outcome was mean energy consumed during a snack, a single meal, or across multiple meals (Crockett 2014; Ebneter 2013; Girz 2012 ‐ study 1; Girz 2012 ‐ study 2; Girz ongoing; Hammond 2013; Harnack 2008a; James 2015; Kral 2002; Platkin 2014; Roberto 2010; Temple 2010; Wansink 2006 ‐ study 1; Wansink 2006 ‐ study 3). Of the three remaining studies, two measured mean grams of food consumed (Cavanagh 2014; Roberto 2012), and one measured mean volume of a drink consumed (Vermeer 2011).
Further details of each study are reported in the table of Characteristics of included studies.
Excluded studies
Of 50,270 records screened, we excluded 49,992 records in the initial screening, and we assessed the full text of 263 papers plus 15 potentially relevant trial registry records (i.e. 278 records) for inclusion (Figure 3). We excluded 246 for not meeting one or more of our inclusion criteria:
113 studies had an ineligible design (i.e. they were not an RCT, Q‐RCT, controlled before‐and‐after study or an ITS study meeting the EPOC criteria for inclusion (EPOC 2015));
83 studies used an intervention that did not include a nutritional label meeting the inclusion criteria or used a multi‐component intervention from which the impact of the label could not be isolated;
76 studies did not assess food purchasing or consumption or used subjective (self‐reported) measures. In all of these cases, we were confident that the excluded studies had not measured relevant outcomes.
In addition:
9 studies didn't include a no label or incomplete label control group, that is, they only compared different labelling schemes;
2 studies were in participants who were not purchasing or consuming food or drink for their personal consumption or for a small group they belonged to; and
1 trial registration did not present enough information to assess eligibility;
16 of the records were registries, conference abstracts or full papers related to already excluded studies.
We report further details in the Characteristics of excluded studies. As over two‐hundred papers were assessed at the full paper stage, we did not include all of these studies in the Characteristics of excluded studies table if they had obvious reasons for exclusion, such as if the study designs were clearly not eligible (e.g. cross‐sectional survey), if the intervention did not assess a nutritional label (e.g. posters on benefits of eating fruit and vegetables), if the studies did not have a no‐label control group, or if studies did not evaluate purchasing or consumption, or only evaluated intention to purchase or consume a food or drink.
Risk of bias in included studies
We present an overview of risk of bias for each study in Figure 4.
4.

Risk of bias summary
Allocation
Of the 17 RCTs, only Crockett 2014 reported an adequate method of both sequence generation and allocation concealment. Seven other RCTs reported an adequate method of sequence generation (e.g. random number generator) but provided no information on the method of allocation concealment (Girz 2012 ‐ study 1; Girz 2012 ‐ study 2; Girz ongoing; James 2015; Platkin 2014; Roberto 2010; Roberto 2012). Seven RCTs reported no information for either criterion (Bergen 2006; Cavanagh 2014; Ebneter 2013; Hammond 2013; Harnack 2008a; Temple 2010; VanEpps 2016). Ellison 2013 and Ellison 2014a reported only that diners were randomly assigned to a table in one of three sections in a restaurant with different intervention or control menus, but authors reported neither the method used to generate the random sequence nor the method of allocation concealment. Ellison 2014a noted that one section of the restaurant with a designated intervention had booth seating, which some parties requested to have, so not all participants were likely randomised. We thus considered this study to be at high risk of bias on this criterion.
In four Q‐RCTs, participants were allocated to intervention or control groups on different days (Kral 2002; Vermeer 2011; Wansink 2006 ‐ study 1; Wansink 2006 ‐ study 3), and in one Q‐RCT, participants were allocated to intervention or control groups on different weeks (Allan 2015).
Blinding
Of the 17 RCTs and 5 Q‐RCTs, 14 studies appropriately blinded the study participants by concealing the purpose of the study and their treatment group, thus mitigating one source of performance bias (Cavanagh 2014; Crockett 2014; Ebneter 2013; Ellison 2013; Ellison 2014a; Hammond 2013; Harnack 2008a; James 2015; Platkin 2014; Roberto 2010; Roberto 2012; Temple 2010; Vermeer 2011; Wansink 2006 ‐ study 3). We assessed blinding to be inadequate in four studies, as some study participants guessed the study purpose or may have been aware of the other treatment group (Allan 2015; Bergen 2006; Kral 2002; Wansink 2006 ‐ study 1). Blinding was unclear in another four RCTs (Girz 2012 ‐ study 1; Girz 2012 ‐ study 2; Girz ongoing; VanEpps 2016).
Most studies did not explicitly state whether study personnel were blinded to the participants' treatment group, but given the nature of the interventions, blinding is unlikely. In addition, the included studies often did not report blinding the outcome assessor; however, when the outcome variable was objectively assessed (e.g. derived from electronic data, or by weighing food), the lack of blinding may not have resulted in detection bias (Allan 2015; Bergen 2006; Cavanagh 2014; Crockett 2014; Ebneter 2013; Ellison 2013; Ellison 2014a; Hammond 2013; Harnack 2008a; James 2015; Kral 2002; Platkin 2014; Roberto 2010; Roberto 2012;Temple 2010; Vermeer 2011; Wansink 2006 ‐ study 1; Wansink 2006 ‐ study 3; VanEpps 2016). The three remaining studies reported no information on blinding or the method of outcome assessment (Girz 2012 ‐ study 1; Girz 2012 ‐ study 2; Girz ongoing).
All six ITS studies objectively measured the outcomes (e.g. electronic data or till receipts), so a lack of blinding of the outcome assessment may not have resulted in detection bias.
Incomplete outcome data
Most of the RCTs, Q‐RCTs and ITS studies evaluated groups of participants within defined observation periods (sometimes with very short time periods, particularly in laboratory experiments). This may explain why there was little evidence of attrition bias. The exceptions to this were three RCTs and two ITS studies. Two of the RCTs did not report the number of participants randomised at the beginning of the study, only the number of observations made (Ellison 2013; Ellison 2014a). In Ebneter 2013, the overall attrition rate was 22%, with no information on attrition by group. Thus, we considered Ellison 2013 and Ellison 2014a to be at unclear risk of bias and Ebneter 2013 to be at high risk of bias. One ITS study was also at unclear risk bias due to a lack of reporting (Balasubramanian 2002), and another ITS study was at high risk of bias due to a high attrition rate (Cioffi 2015).
Selective reporting
We judged most studies to be at low risk of bias with regard to selective reporting given that they fully reported all of the outcomes specified in the Methods section of the papers. Although the availability of a study protocol would have allowed for a more reliable estimate of this, our searches identified only two protocols from the 17 RCTs (Crockett 2014; Hammond 2013). In addition, most of the RCTs and Q‐RCTs reported complete data that could be used to calculate effect sizes. Selective reporting was not clear in one RCT, Girz ongoing, or in one ITS study, Balasubramanian 2002. The ITS study by Cioffi 2015 was at high risk of bias because authors excluded outcome data for some target food items from the analysis.
Other potential sources of bias
Biases specific to interrupted time series studies
Two of the ITS studies reported that the intervention was independent of confounding variables during the study period (Bollinger 2011; Chu 2009), and another two provided no information (Dubbert 1984; Holmes 2013). In Cioffi 2015, the authors noted that "with data observed over many weeks and at various locations, it was impossible to control for all external factors or events that might have occurred over the entire length of the study", and in Balasubramanian 2002, the authors noted that "our models do not incorporate explanatory variables such as price or other type of deals", suggesting that other changes could have occurred during the study period. We considered that the lack of control for potential confounders introduced a high risk of bias.
Other potential threats to validity
In the cluster‐RCT, there were significant baseline differences between the randomised clusters, so we considered this study to be at high risk of bias (Bergen 2006). In one ITS study, it was unclear how investigators selected the participating grocery stores, raising the possibility of selection bias (Balasubramanian 2002). In three studies, data collection occurred during short time periods or during restricted hours of the day (Dubbert 1984; Ellison 2013; Vermeer 2011), so the outcomes may not have been representative of purchasing or consumption. Moreover, in Balasubramanian 2002, the introduction of the Nutrition Labeling and Education Act may have drawn additional attention to signposting throughout the city where the study took place, not just in the stores in question, thus possibly introducing a co‐intervention. We considered these studies to be at high risk of bias for this additional criterion.
Effects of interventions
See: Table 1
Purchasing studies
Purchasing from vending machines
One cluster‐RCT compared sales of drinks in vending machines with and without labels in a university setting (Bergen 2006). The results showed that participants purchased more diet soda from the labelled vending machines (mean 54.4 beverages, SD 16.7) compared to the non‐labelled machines (mean 48.9 beverages, SD 1.8) (Table 2). However, given the small number of vending machines randomised (N = 3), and the large baseline differences in sales between the vending machines, we cannot clearly interpret the study results or calculate an accurate effect size.
1. Study that assessed labelling vs no labelling on drinks purchased from vending machines.
| Reference and study design | Participants and Setting | Intervention/Comparison (sample sizes) | Outcome | Results | Summary effect |
|
Bergen 2006 Cluster‐RCT |
Students and employees at a university Real‐world setting |
Brightly coloured '0 calories, 0 carbs' labels (n = 3 vending machines) vs no labels (n = 2 vending machines)a | Mean number of diet soda beverages (with '0 calories, 0 carbs') purchased from vending machines (weekly) | Mean 54.40 beverages (SD 16.69) vs 48.90 beverages (SD 1.84) | The methods used to analyse the data were not clearly reported and an accurate effect size and confidence intervals could not be calculated.b |
aThe authors also evaluated another intervention ('0 calorie, 0 carbs' plus a motivational poster encouraging the purchase of water and non‐energy‐containing soft drinks) that was not eligible for inclusion in this review. bThere were baseline differences between the groups. In addition, we could not provide a standardised effect due to the impact of small randomised units (vending machines) on estimates of standard deviation.
Using GRADE criteria, we downgraded the evidence by two levels for very serious risk of bias and by one level for a high degree of imprecision. Thus, we considered the quality of the evidence for labelling on drinks purchased from vending machines to be very low, meaning that we have very little confidence in it.
Purchasing from a grocery store
One ITS study with unclear sample sizes assessed the impact of verbal descriptor labels for single nutrients, such as 'low calorie' or 'light' on food purchasing from a grocery store (Balasubramanian 2002). Regression analysis demonstrated that the sales performance of calorie‐healthy foods (e.g. low‐calorie bottled juices and 'light' frozen entrées and dinners) decreased after the implementation of mandatory labelling (Table 3). The results of this longitudinal time series analysis were, however, difficult to interpret because the authors evaluated a percentage of labelled products bought relative to other products, rather than evaluating time trends of the number of products purchased before and after the introduction of labelling.
2. Study that assessed labelling vs no labelling on food or drinks purchased from a grocery store.
| Reference and study design | Participants and setting | Intervention/comparison (sample sizes) | Outcome | Results | Summary effect |
|
Balasubramanian 2002 Interrupted time series |
Customers at a major grocery store chain Real‐world setting |
'Low calorie', 'diet' 'light' label on front of package vs no label (sample sizes not clear)a | Share (%) of sales of different food categories | "Regression models featuring calorie‐healthy foods consistently show [that] the relative sales performance of such items decreased after the onset of [mandatory labelling]": 'low calorie/diet/light' bottled juices = −1.538 (SE 0.191); 'light' frozen entrées = −2.601 (SE 0.373); 'light' frozen dinners = −4.507 (SE 0.963)b | Regression P values of < 0.001 indicated fewer foods with 'calorie healthy' descriptors were purchased. |
aThe authors also evaluated 'vitamin C fortified' bottled juices, 'plus calcium/calcium added' juices, and 'low fat/reduced fat/fat free' cheese and cookies. These data were not eligible for inclusion in this review. bGraphs were not presented for the foods or beverages of interest, so that re‐analysis of the data was not possible from the published paper.
Using GRADE criteria, we downgraded the evidence for this observational study by one level for serious risk of bias and one level for indirectness, because the study measured the outcome indirectly, as a proportion of overall purchasing rather than as a direct quantity. Thus, we considered the quality of the evidence for labelling on drinks purchased from grocery stores to be very low, meaning that we have very little confidence in it.
Purchasing from a restaurant, cafeteria or coffee shop
Nine studies assessed the impact of nutritional labels on menus or menu boards, or nutritional labels placed on, or adjacent to, a range of food or drink options in restaurants, cafeterias or coffee shops (Allan 2015; Bollinger 2011; Chu 2009; Cioffi 2015; Dubbert 1984; Ellison 2013; Ellison 2014a; Holmes 2013; VanEpps 2016). Three of these studies were RCTs (Ellison 2013; Ellison 2014a; VanEpps 2016), one was a Q‐RCT (Allan 2015), and five used ITS analyses (Bollinger 2011; Chu 2009; Cioffi 2015; Dubbert 1984; Holmes 2013). Only three RCTs presented data suitable for calculating effect sizes (Ellison 2013; Ellison 2014a; VanEpps 2016). We present brief descriptions of all nine studies below and in Table 4.
3. Studies that assessed labelling vs no labelling on food or drinks purchased in restaurants, cafeterias or coffee shops.
| Reference and study design | Participants and setting | Intervention/comparison (sample sizes) | Outcome | Results | Summary effect |
|
Allan 2015 Q‐RCT |
Coffee shop customers at academic hospital Real‐world setting |
Energy content of all food and drinks available on point of purchase signs vs. no information (N = 20,516 items purchased) | Proportion of high energy food and drinks purchased (as a percentage of total drinks and snacks sold) | The proportion of high energy snacks purchased was 41% in the intervention and 45% the control group (P = 0.04); the proportion of high energy drinks purchased was 46% in the intervention group and 50% in the control group (P = 0.15). | Effect size and confidence intervals could not be calculated. |
|
Bollinger 2011 Interrupted time series |
Coffee shop customers Real‐world setting |
Energy content on menu and menu boards vs no information (N = 118,480 transactions reported) | Mean kcal of food and drinks purchased per transaction | "Estimates of the effect of calorie posting (calories per transaction): log (beverages and food) = −0.060 (0.001)a–representing a ... decrease in average calories per transaction, equivalent to 14.4 calories" | Regression P value < 0.01 |
|
Chu 2009 Interrupted time series |
Customers at a university dining centre Real‐world setting |
Nutrition facts information on menu board (N = 14,199 entrées sold) vs no label (pre‐intervention: N = 13,951 entrées sold; post‐intervention N = 14,020 entrées sold) | Mean kcal content of entrées purchased per day | Mean energy content of entrées sold at start of the pre‐intervention period: 646.5 kcal with a slope of 0.094 kcal per day. The difference in energy content of entrées sold between the pre‐treatment last day and treatment first day was −12.4 kcal (P = 0.007). Following this reduction, the difference in slope pre‐intervention to intervention was −0.298 kcal per day, and the difference in slope intervention to post‐intervention was 1.512 kcal per day. This means that the average energy content of entrées purchased reduced immediately after the intervention, and gradually increased when the intervention was removed. | Regression P values were 0.56 (pre‐intervention to intervention slope), and 0.013 (intervention to post‐intervention slope). |
|
Cioffi 2015 Interrupted time series |
Customers at a university dining centre Real‐world setting |
Nutrition facts label on pre‐packaged meals and snacks vs no label (sample sizes not reported) | Mean kcal purchased per week from meals and snacks | "Mean [energy] purchased decreased significantly across the 3 [time points] of the pre‐labelling period. However, no such trend was observed in the post‐labelling period." (data compared over 3 time points)."After labelling, the mean energy content of the items purchased per week decreased significantly from 476.2 (SD 8.7) kcals to 445.3 (SD 8.1) kcals per week (p<0.001)." | A statistical comparison of time trends (i.e. slope) before and after the intervention was not reported, so that the overall effectiveness of the intervention is not clear. |
|
Dubbert 1984 Interrupted time series |
Customers at a public cafeteria Real‐world setting |
'Lower calorie' label on green paper with a red dot on right‐hand corner beside food item vs no label (sample sizes of foods purchased is not clear) | Probability of choosing low energy entrées, vegetables, or salads | "The probability of choosing a low [energy] entrée did not differ from baseline." The probability of purchasing lower‐energy vegetables and salads significantly increased compared to the no label baseline conditions (P < 0.001). | A statistical comparison of time trends before and after the intervention was not clearly reported, so that the overall effectiveness of the intervention is not clear. |
|
Ellison 2013 RCT |
Customers at a restaurant Real‐world setting |
1. Energy content on menu (n = 54) 2. Menu with energy content using traffic light format (n = 54) 3. No label (n = 30) |
Mean kcal purchased per meal (including entrées, desserts and drinks) | 756.5 kcal (SD 338.5)b vs 765 kcal (SD 368.0) | MD −8.50 kcal (95% CI −154.85 to 137.85) |
|
Ellison 2014a RCT |
Customers at a restaurant Real‐world setting |
1. Energy content on menu (n = 469) 2. Menu with energy content using traffic light format (n = 591) 3. No label (n = 472) |
Mean kcal purchased per meal (entrées only) | 705.6 kcal (SD 334.7)c vs. 746 kcal (SD 368.0) | MD −40.38 kcal (95% CI −79.21 to −1.55) |
|
Holmes 2013 Interrupted time series |
Families at a restaurant Real‐world setting |
Children's menu with energy and fat content label vs no label (N = 1275 meals)d | Mean kcal purchased per meal | "The calorie and fat menu had the biggest change in calories compared to the control menu (−9.54), but it was not significant." | A statistical comparison of time trends before and after the intervention was not reported, so that the overall effectiveness of the intervention is not clear. |
|
VanEpps 2016 RCT |
Employees at large company buying lunch online Real‐world setting |
1. Energy content on menu (n = 38) 2. Menu with energy content using traffic light format (n = 46) 3. No label (n = 123)e |
Mean kcal purchased per meal | 537.9 kcal (SD 203.9)f vs. 605.3 kcal (SD 222.5) | MD −67.38 kcal (95% CI −126.09 to −8.66) |
aAccounting for effects of week, day of week and weather. bSDs were calculated from P values reported in the text; means and SDs for both intervention groups were combined (intervention 1: 817 kcal (SD 334.6); intervention 2: 696 kcal (SD 334.6)). cSDs were based on Ellison 2013; means and SDs for both intervention groups were combined (intervention 1: 719 kcal (SD 334.6); intervention 2: 695 kcal (SD 334.6)). dThe authors also evaluated two other labelling interventions (a healthy (apple) symbol, and a 'Nutrition Bargain Price') that were not eligible for inclusion in this review. eThe authors also evaluated one other labelling interventions (traffic light labels without energy information) that was not eligible for inclusion in this review. fMeans and SDs (obtained from the study authors) for both intervention groups were combined (intervention 1: 543.8 (SD 180); intervention 2: 533.1 (SD 223.6)).
Of the three RCTs, two took place in the same restaurant under the supervision of the same research team (Ellison 2013; Ellison 2014a). In both studies, groups of customers were randomised to three different menus: a menu labelled with energy information, a menu with energy information in a traffic light format, or a menu with no energy information. In the first study, investigators collected data for two weeks, and in the second study, for 19 weeks. In the third RCT, conducted over a four‐week period, company employees chose lunch items from an online menu from a corporate restaurant with or without energy information, and alone or with a traffic light format (VanEpps 2016). For each of these three RCTs, we combined two of the treatment arms: energy labelling alone, and energy labelling plus a traffic light format. We could then calculate effect sizes for menu labelling versus no‐label comparisons. A meta‐analysis of these three RCTs from restaurants demonstrated a statistically significant reduction of 47 kcal in energy purchased when menus were labelled (MD −46.72 kcal, 95% CI −78.35 to −15.10, P = 0.004, N = 1877; Analysis 1.1; Figure 5) with little evidence of heterogeneity (Chi² = 0.84, P = 0.66, I² = 0%). Assuming an average meal intake of 600 kcal, the size of this effect suggests that energy labelling on menus would reduce energy purchased per meal by 7.8% (95% CI 2.5% to 13.1%).
1.1. Analysis.

Comparison 1: Labelling on menus vs no labelling in restaurants, Outcome 1: Energy (kcal) of food purchased
5.

Forest plot of comparison: Labelling on menus vs no labelling in restaurants, and energy (kcal) of food purchased
We considered two RCTs to be at unclear risk of bias because there was insufficient information available on study methods to make an assessment (Ellison 2013; VanEpps 2016), and we assessed one RCT as being at very high risk of bias (Ellison 2014a). We thus downgraded the evidence two levels for very serious risk of bias. We rated the quality of the evidence for these three studies to be low, so our confidence in the effect estimate is limited, and the estimate may change with further studies.
Of the remaining six studies, one Q‐RCT assessed point‐of‐purchase signs that provided energy information on all snacks and drinks available at a hospital coffee shop (Allan 2015).The signs were randomly presented or not presented for six weeks each. The authors reported that the proportion of high‐calorie snacks purchased (of the total purchases) was significantly lower in the intervention group compared to the control group (41% versus 45%, P = 0.04), but there was no significant difference in the proportion of high‐energy drinks purchased between the intervention and control (46% versus 50%, P = 0.15). While the total number of items purchased over the 12 weeks was 20,516, the study did not provide sample sizes for intervention and control snacks or drinks.
Of the five ITS studies, one evaluated changes before and after mandatory energy food labelling on menus and menu boards in New York City (Bollinger 2011). Using regression analysis, the authors reported an average decrease after labelling in energy purchased from food of 14.4 calories per transaction (P = 0.001) at a coffee shop chain, with a negligible impact on energy from drinks per transaction.
Three ITS studies took place in cafeterias (Chu 2009; Cioffi 2015; Dubbert 1984), but only one statistically compared time trends before and after the implementation of labelling (Chu 2009). This study found that introducing a menu board that adhered to the same format as the FDA nutritional facts label reduced the average energy content of entrées selected by participants immediately after the intervention, and that the energy content of the entrées selected gradually increased after removing the nutrition information (total entrées sold/evaluated = 42,170) (Chu 2009). Cioffi 2015 also reported the effects of a nutrition facts label placed directly on pre‐packaged meals and snacks. The mean energy purchased was higher pre‐intervention than during the intervention, but authors did not report a statistical comparison of time trends before and after the intervention. Dubbert 1984 found that a 'lower calorie selection' label placed near appropriate food items significantly increased the probability of purchasing lower energy vegetables and salads compared to higher energy vegetables and salads (P < 0.001 for both) over baseline conditions. The probability of purchasing a low‐energy entrée did not differ from baseline. A further ITS study assessed the impact of energy and fat information presented on children's menus and reported that, compared with no nutritional labelling, total energy purchased after two months was unchanged (Holmes 2013). However, authors did not report a statistical comparison of time trends before and after the intervention.
We considered two ITS studies to be at low risk of bias (Bollinger 2011; Chu 2009), while one was at unclear risk (Holmes 2013), and two were at high risk (Cioffi 2015; Dubbert 1984). One Q‐RCT was also at high risk of bias (Allan 2015) Both ITS studies considered to be at low risk of bias supported the findings of the meta‐analysis reported above.
Consumption studies
Consumption in laboratory settings
Seventeen studies assessed the impact on consumption of nutritional labels on one or more food items in artificial or laboratory settings (Cavanagh 2014; Crockett 2014; Ebneter 2013; Girz 2012 ‐ study 1; Girz 2012 ‐ study 2; Girz ongoing, Hammond 2013; Harnack 2008a; James 2015; Kral 2002; Platkin 2014; Roberto 2010; Roberto 2012; Temple 2010; Vermeer 2011; Wansink 2006 ‐ study 1; Wansink 2006 ‐ study 3. Eight assessed labelling on menus or on a range of food options, such as at a buffet meal (Girz 2012 ‐ study 2; Girz ongoing, Hammond 2013; Harnack 2008a; James 2015; Platkin 2014; Roberto 2010; Temple 2010) (see Table 5). Six studies assessed the impact of a nutritional label on a snack, drink or meal without providing participants with other options to choose from (Cavanagh 2014; Crockett 2014; Ebneter 2013; Kral 2002; Roberto 2012; Vermeer 2011) (see Table 5). An additional three studies intentionally mislabelled products to detect effects on behaviour, by measuring energy intake of high‐fat snack foods labelled as low fat or low energy (Girz 2012 ‐ study 1; Wansink 2006 ‐ study 1; Wansink 2006 ‐ study 3). We consider these latter three in the section below on potential harms associated with labelling (see also Table 6).
4. Studies that assessed labelling vs no labelling on food or drinks consumed in laboratory settings.
| Reference and study design | Participants and setting | Intervention/comparison (sample sizes) | Outcome | Results | Summary effect |
| Labelling on menus or placed on a range of food options on energy consumed during a meal | |||||
|
Girz 2012 ‐ study 2 RCT |
University students Experimental (laboratory) study at a university |
Energy content on menu plus information on recommended daily energy intake for women and men (n = 60) vs no label (n = 66)a | Mean kcal consumed during a meal (salad and pasta) | 608.2 kcal (SD 350.8)b vs 631.3 kcal (SD 324.0) | MD −23.02 kcal (95% CI −141.28 to 95.24) |
|
Girz ongoing RCT |
University students Experimental (laboratory) study at a university |
Energy content on menu (n = 24) vs no label (n = 25) | Mean kcal consumed during a meal | 433.1 kcal (SD 260.2) vs 426.5 kcal (SD 237.4)c | MD 6.60 kcal (95% CI −133.02 to 146.22) |
|
Hammond 2013 RCT |
Adults Experimental (laboratory) study at a university |
1. Energy content on menu (n = 165) 2. Menu with energy content using a traffic light format (n = 156) 3. Menu with energy, fat, salt, and sugar content using traffic light format (n = 152) vs no label (n = 162) |
Mean kcal consumed during a fast food meal | 761.6 kcal (SD 348.9)d vs 839.6 kcal (SD 318.8) | MD −78.00 kcal (95% CI −136.29 to −19.70) |
|
Harnack 2008a RCT |
Adolescents and adults Experimental study conducted in hotel conference rooms/church hall |
Energy content on menu plus information on recommended daily energy intake for women and men (n = 151) vs no label (n = 150)e | Mean kcal consumed during a fast food meal | 804.7 kcal (SD 423.9) vs 739.0 kcal (SD 358.2) | MD 65.70 kcal (95% CI −22.94 to 154.34) |
|
James 2015 RCT |
Adults, including university students Experimental study at a university |
Energy content on menu plus information on recommended daily energy intake for women and men (n = 99) vs no label (n = 99)f | Mean kcal consumed during a meal | 722.0 kcal (SD 271.6)g vs 770.0 (SD 269.1) | MD −48.00 kcal (95% CI −123.31 to 27.31) |
|
Platkin 2014 RCT |
Female university students Experimental (laboratory) study at a university |
1. Energy content on menu (n = 20) 2. Menu with energy content and exercise equivalents (n = 20) vs no label (n = 22) |
Mean kcal consumed during a fast food meal | 870.1 kcal (SD 375.9)h vs 995.4 (SD 429.4) | MD −125.33 kcal (95% CI −339.26 to 88.59) |
|
Roberto 2010 RCT |
Adults from the community Experimental (classroom) study at a university |
1. Energy content on menu (n = 92) 2. Menu with energy content plus information on recommended daily intake (n = 103) vs no label (n = 92) |
Mean kcal consumed during a meal | 1293.3 kcal (SD 656.8)i vs 1458.9 kcal (SD 724.6) | MD −165.58 kcal (95% CI −340.01 to 8.84) |
|
Temple 2010 RCT |
Adults Experimental (laboratory) study at a university |
Nutrition facts label on foods (n = 23) vs no label (n = 24) | Mean kcal consumed during a meal | 620.4 kcal (SD 203.6) vs 822.8 kcal (SD 408.7)j | MD −202.40 kcal (SD −385.86 to −18.94) |
| Labelling of a single food or drink option on energy consumed during a snack or meal | |||||
|
Cavanagh 2014 RCT |
Female university students Experimental (laboratory) study at a university |
Energy label on chocolate cookie (130 kcal) (n = 62) vs no label (n = 62)k | Mean grams consumed from snack of chocolate chip cookies | 45.1 g (SD 21.50) vs 33.1 g (SD 21.57)l | SMD 0.55 (95% CI 0.19 to 0.91) |
|
Crockett 2014 RCT |
Adults Experimental study at a cinema |
Red 'high fat' label on side of popcorn container (n = 96) vs no label (n = 88)m | Mean kcal consumed from snack of toffee or salted popcorn (high‐fat snack) | 413.5 kcal (SD 307.6)n vs 468.1 kcal (SD 361.9) | SMD −0.16 (95% CI −0.45 to 0.13) |
|
Ebneter 2013 RCT |
Female university students Experimental study at a university |
Energy label ('new colours of regular M&M's, 240 calories per serving"') on glass container containing M&M's (n = 41) vs no energy content label ('new colours of regular M&M's') (n = 38)o | Mean kcal consumed during snack of M&M's (high‐fat snack) | 157.2 kcal (SD 98.5) vs165.9 kcal (SD 141.5) | SMD −0.07 (95% CI −0.51 to 0.37) |
|
Kral 2002 Q‐RCT |
Females Experimental (laboratory) study at a university |
Energy label plus 'colour‐coded' information on level of energy density on an entrée (n = 20) vs no label (n = 20) | Mean kcal consumed from an entrée at breakfast, lunch and dinner | 1534.0 kcal (SD 451.7) vs 1569.0 kcal (SD 335.4) | SMD −0.09 (95% CI −0.71 to 0.53) |
|
Roberto 2012 RCT |
Adults Experimental (laboratory) study at a university |
1. Smart choices label on cereal box (n = 76 analysed) 2. Modified smart choices label (n = 71) vs no label (n = 69) |
Mean grams of high‐sugar breakfast cereal and milk consumed | 225.7 g (SD 138.2)p vs 219.9 g (SD 127.1) | SMD 0.04 (95% CI −0.24 to 0.33) |
|
Vermeer 2011 Q‐RCT |
Adults Experimental study at a cinema |
Portion size and energy content label (display board) (n = 48) vs no label (n = 41) | Mean millilitres of soft drink consumed | 376.3 mL (SD 125.4) vs 382.14 mL (SD 147.6)q | SMD −0.04 (95% CI−0.46 to 0.37) |
aTwo other interventions were combined by the study authors as a 'calorie only' intervention (400 kcal salad and 1200 kcal pasta, and 1200 kcal salad and 400 kcal pasta (although both salad and pasta contained 1200 kcal)). We did not include this data in the above analysis as it involved mislabelling some of the foods (data were not reported separately for consumption of foods that were accurately labelled). bMeans and SDs were reported separately for men and women by the study authors; we have combined these data. cData were obtained from the study authors (Girz ongoing). dMean and SDs for all three intervention groups were combined (intervention 1: 744.2 kcal (SD 368.1); intervention 2: 776.8 kcal (SD 350.9); intervention 3: 764.9 (SD 326.2)). eThe authors also evaluated other labelling interventions (energy information and daily recommended intake plus price modification, and price modification alone) that were not eligible for inclusion in this review. fThe authors also evaluated another intervention (exercise label describing the number of minutes of brisk walking required to burn the energy for each food item), but as this intervention did not present energy content information, it was not eligible for inclusion in this review. gSDs were calculated from confidence intervals. hSDs were calculated from standard errors. Means and SDs for both intervention groups were combined (intervention 1: 898.82 kcal (SD 392); intervention 2: 841.31 kcal (SD 82.07)). iMeans and SDs for both intervention groups were combined (intervention 1: 1334.72 kcal (SD 621); intervention 2: 1256.37 kcal (SD 689)). jData were obtained from the study authors (Temple 2010). kThe authors also evaluated another labelling intervention (high energy label on a low energy cookie) that was not eligible for inclusion in this review. lThese data were converted kcal using formula presented in DeGroot 2012. mThe authors also evaluated another labelling intervention (green 'low fat' label on high fat popcorn) that is not reported here (see Table 6). nMeans and SDs for two types of popcorn (toffee and salted), reported separately in the paper, were combined. oThe authors also evaluated two other labelling interventions (low fat label with and without energy information on high fat snacks) that is not reported here (see Table 6). pMeans and SDs for both intervention groups were combined (intervention 1: 219.21 (SD 133); intervention 2: 232.61 (SD 144)). These data were then converted kcal using formula presented in DeGroot 2012. qThese data were converted kcal using formula presented in DeGroot 2012.
5. Studies that assessed potential harms (indirectly): 'low fat' or low energy labels on high‐energy snacks.
| Reference and study design | Participants and setting | Intervention/comparison (sample sizes) | Outcome | Results | Summary effect |
|
Crockett 2014 RCT |
Adults Experimental study at a cinema |
Green 'low fat' label on side of container containing high‐fat popcorn (n = 103) vs no label (n = 88) | Mean kcal consumed from snack of popcorn | 402.44 kcal (SD 288.68) vs 468.07 kcal (SD 361.93) | SMD −0.20 (95% CI −0.48 to 0.08) |
|
Ebneter 2013 RCT |
Female university students Experimental study at a university |
Low fat label ('new low fat M&M's') on glass container containing M&M's (n = 49) vs no energy information label ('new colours of regular M&M's') (n = 38) | Mean kcal consumed during snack of M&M's | 192.34 kcal (SD 145.53) vs165.88 kcal (SD 141.5) | SMD 0.18 (95% CI−0.25 to 0.61) |
|
Girz 2012 ‐ study 1 RCT |
Female university students Experimental (laboratory) study at a university |
Lower energy label (600 kcal) on high‐energy salad and pasta (actually 1200 kcal) (n = 56) vs no label (n = 49)a | Mean kcal consumed during a meal (salad and pasta) | 400.26 kcal (SD 199.8) vs 420.19 kcal (SD 233.69) | SMD −0.09 (95% CI −0.47 to 0.29) |
|
Wansink 2006 ‐ study 1 Q‐RCT |
Students and their families Experimental study at a university |
Low fat label ('new low fat M&M's') on glass container containing M&M's vs no energy information label ('new colours of regular M&M's') (n = 269 overall (n by group not reported)) | Mean kcal consumed from snack of M&M's | Mean 244 kcal (SD not reported) vs 190 kcal (SD not reported) | SMD 0.44 (95% CI 0.20 to 0.68)b |
|
Wansink 2006 ‐ study 3 Q‐RCT |
University staff, graduates and undergraduates Experimental study at a university |
Low fat label ('Low‐Fat Rocky Mountain Granola') on zip lock bag vs no label ('Regular Rocky Mountain Granola') (n = 66 overall (n by group not reported)) | Mean kcal consumed from snack of granola | Mean 249 kcal (SD not reported) vs 165 kcal (SD not reported) | SMD 0.69 (95% CI 0.20 to 1.18)c |
aData were extracted for those who chose pasta or salad when it was inaccurately as '600 calories'. bSMD was calculated based on F‐test data reported in the text. cSMD was calculated based on F‐test data reported in the text.
Energy consumed during a meal with a range of available food options
A meta‐analysis of eight RCTs did not conclusively demonstrate a reduction in energy consumed when menus (7 studies) or a range of foods (1 study) were labelled (MD −50.27 kcal, 95% CI −104.41to 3.88, P = 0.07, N = 1705; Analysis 2.1; Figure 6; Girz 2012 ‐ study 2; Girz ongoing, Hammond 2013; Harnack 2008a; James 2015; Platkin 2014; Roberto 2010; Temple 2010), and there was moderate heterogeneity between the studies (Chi² = 13.06, P = 0.07, I² = 46%). The pooled result shows a positive effect for labelling, although the 95% confidence interval crosses the line of no effect. Assuming an average meal intake of 600 kcal, the size of this effect suggests that energy labelling of menus or food would reduce consumption per meal by 8.4% (95% CI −0.7% to 17.4%).
2.1. Analysis.

Comparison 2: Labelling on menus or placed on a range of food options vs no labelling in laboratory settings, Outcome 1: Energy (kcal) consumed during a meal
6.

Forest plot of comparison: Labelling on menus or placed on a range of food options vs. no labelling in laboratory settings, and energy (kcal) consumed
A pre‐planned sensitivity analysis, including the three studies judged to be at low risk of bias (James 2015; Platkin 2014; Roberto 2010), resulted in an increased effect size (MD −72.04 kcal, 95% CI −137.84 to −6.25, P = 0.03, N = 547; Analysis 3.1) with little evidence of heterogeneity (Chi² = 1.73, P = 0.42, I² = 0%). This equated to a per meal reduction of 12.0% (95% CI 1.0% to 23.0%), again assuming an average meal intake of 600 kcal.
3.1. Analysis.

Comparison 3: Labelling on menus vs no labelling in laboratory settings (studies with a low risk of bias), Outcome 1: Energy (kcal) consumed during a meal
Of the eight RCTs that evaluated this outcome, we considered three to be at low risk of bias (James 2015; Platkin 2014; Roberto 2010), while five were at unclear risk due to there being insufficient information on study methods to make an assessment (Girz 2012 ‐ study 2; Girz ongoing; Hammond 2013; Harnack 2008a; Temple 2010).
Using GRADE criteria, we downgraded the evidence one level for imprecision (as the 95% confidence interval included the possibility of no effect and of a meaningful decrease) and one level for indirectness (as behaviour observed in a laboratory setting may not be applicable to real‐world settings). Although five of the included studies were at unclear risk of bias, we did not downgrade for risk of bias. Thus, we considered quality of the evidence for the impact of labelling on menus or multiple foods on energy consumption to be low, meaning that our confidence in the effect estimate is limited, and the estimate may change with further studies.
Energy consumed during a snack or meal with a single food or drink option
Four RCTs (Cavanagh 2014; Crockett 2014; Ebneter 2013; Roberto 2012), plus two Q‐RCTs (Kral 2002; Vermeer 2011), assessed the impact of labelling on energy (kcal) consumption when participants were offered a single food option: cookies, high‐sugar breakfast cereal, chocolate, popcorn, an entrée, or soft drinks. In these studies, the nutritional label was placed on the container or packaging, adjacent to the food, or presented on a display board. A meta‐analysis of these six studies did not demonstrate a statistically significant reduction in energy consumed with labelling, but the confidence intervals were wide, suggesting uncertainty in the true effect size (SMD 0.05, 95% CI −0.17 to 0.27, P = 0.67, N = 732; Analysis 4.1), and the effect size was small (see Cohen 1988). Heterogeneity between the studies was moderate, principally due to Cavanagh 2014, which differed in using low‐energy (as opposed to high‐energy) snack foods (Chi² = 10.28, P = 0.07, I² = 51%). Within this analysis there is a probable lack of consistency in the distributions of values associated with measures of meal compared to snack consumption, which is a potential limitation, affecting the extent to which the SD units can be equated across the studies; however, we are confident that alternative analysis options would not affect our overall conclusions. The results were similar in a sensitivity analysis that included only the two studies we judged to be at low risk of bias (SMD −0.06, 95% CI −0.26 to 0.15, P = 0.57, N = 400; Analysis 5.1; Crockett 2014; Roberto 2012), with little evidence of heterogeneity (Chi² = 0.98, P = 0.32, I² = 0%).
4.1. Analysis.

Comparison 4: Labelling of a single food or drink option vs no labelling in laboratory settings, Outcome 1: Energy (kcal) consumption
5.1. Analysis.

Comparison 5: Labelling of a single food or drink option vs no labelling in laboratory settings (studies at low risk of bias), Outcome 1: Energy (kcal) consumption
Of the four RCTs and two Q‐RCTs that evaluated this outcome, we considered two RCTs to be at low risk of bias (Crockett 2014; Roberto 2012), one RCT to be at unclear risk of bias (given insufficient information reported to enable an assessment) (Cavanagh 2014), and one RCT and the two Q‐RCTs to be at high risk of bias (Ebneter 2013; Kral 2002; Vermeer 2011).
Using GRADE criteria, we downgraded the evidence one level for serious risk of bias and one level for indirectness, as behaviour observed in a laboratory setting may not be applicable to real‐world settings. Although the confidence intervals were wide, this did not affect the overall rating. Thus, we considered the quality of the evidence for the impact of labelling of a single food or drink option on energy consumption to be low, meaning that our confidence in the effect estimate is limited, and that the estimate may change with further studies.
Subgroup analyses
We conducted pre‐planned subgroup analyses by dietary restraint and by study country. We performed separate analyses for studies that provided a range of food options and for studies that provided single food options. No analyses demonstrated statistically significant differences, but the confidence intervals were wide, suggesting uncertainty in the true effect size.
For studies providing multiple food options, the pooled effect size for restrained eaters was MD 20.87 kcal (95% CI −37.44 to 79.18, P = 0.48, N = 129; Girz 2012 ‐ study 2; Girz ongoing), and for unrestrained eaters the MD was 10.98 kcal (95% CI −38.85 to 60.81, P = 0.67, N = 138; Girz 2012 ‐ study 2; Girz ongoing), with the test for subgroup differences showing no significant effect (Chi² = 0.06, df = 1, P = 0.80, I² = 0%); see Analysis 6.1.
6.1. Analysis.

Comparison 6: Consumption in laboratory settings: subgroup analysis by dietary restraint (studies providing a range of food options), Outcome 1: Energy (kcal) consumed during a meal
Of the studies that provided single food options, only one study reported data for restrained and unrestrained eaters, presenting the results as standardised mean energy consumption. The effect size for restrained eaters was SMD −0.44 (95% CI −0.94 to 0.05) (sample size not reported), and for unrestrained eaters it was SMD 0.03 (95% CI −0.34 to 0.39) (sample size not reported) (Crockett 2014), with the test for subgroup differences showing no significant effect (Chi² = 2.24, df = 1, P = 0.13, I² = 55%); see Analysis 7.1.
7.1. Analysis.

Comparison 7: Consumption in laboratory settings: subgroup analysis by dietary restraint (study providing a single food option), Outcome 1: Energy (kcal) consumed during a snack
For studies providing multiple food options, the pooled effect size for US studies was MD −70.57 kcal (95% CI −167.65 to 26.52, P = 0.15, N = 895; Harnack 2008a; James 2015; Platkin 2014; Roberto 2010; Temple 2010). The effect size for studies conducted in other countries was MD −58.18 kcal (95% CI −107.15 to −9.21; Girz 2012 ‐ study 2; Girz ongoing; Hammond 2013), with the test for subgroup differences showing no significant effect (Chi² = 0.05, df = 1, P = 0.82, I² = 0%); see Analysis 8.1.
8.1. Analysis.

Comparison 8: Consumption in laboratory settings: subgroup analysis by study country (studies providing a range of food options), Outcome 1: Energy (kcal) consumed during a snack/meal
For studies providing a single food option, the pooled effect size for US studies was SMD 0.14 (95% CI −0.17 to 0.45, P = 0.37, N = 459; Cavanagh 2014; Ebneter 2013; Kral 2002; Roberto 2012), and for studies conducted in other countries the SMD was −0.12 (95% CI −0.36 to 0.11, P = 0.31, N = 273; Crockett 2014; Vermeer 2011), with the test for subgroup differences showing no significant effect (Chi² = 1.75, df = 1, P = 0.19, I² = 43%); see Analysis 9.1.
9.1. Analysis.

Comparison 9: Consumption in laboratory settings: subgroup analysis by study country (studies providing single food option), Outcome 1: Energy (kcal) consumed during a snack/meal
Potential harms associated with labelling
Based on the analyses described above, there is no evidence that nutritional labelling has the unintended harm of increasing energy purchased or consumed.
Indirect evidence concerning potential harm comes from five studies that involve mislabelling content for a single nutrient (Crockett 2014; Ebneter 2013; Girz 2012 ‐ study 1; Wansink 2006 ‐ study 1; Wansink 2006 ‐ study 3). Two Q‐RCTs examined the impact of low fat labels on energy consumption of high‐energy snack foods (chocolate and granola) (Wansink 2006 ‐ study 1; Wansink 2006 ‐ study 3), and one RCT evaluated the impact of low energy labels on energy consumption of high‐fat foods (a pasta dish and an energy dense salad) (Girz 2012 ‐ study 1). In addition, two RCTs evaluated treatment arms in which high‐fat snack foods carried a low fat label (Crockett 2014; Ebneter 2013). In one of these studies a treatment group received toffee and salted popcorn with a green low fat label (Crockett 2014), and in the other study, a treatment group received a chocolate confectionery coated with hard candy shell (M&M's) labelled as 'low fat' (without any other energy information) (Ebneter 2013). A meta‐analysis of these five studies did not demonstrate a statistically significant increase in energy (kcal) consumed with mislabelling, but the confidence intervals are wide, suggesting uncertainty in the true effect size (SMD 0.19, 95% CI −0.14 to 0.51, P = 0.25, N = 718), and the effect size was small (see Cohen 1988). There was also a high degree of heterogeneity between the studies (Chi² =17.44, P = 0.002, I² = 77%); see Analysis 10.1.
10.1. Analysis.

Comparison 10: Low fat (or energy) labelling vs no labelling on high‐energy foods, Outcome 1: Energy (kcal) consumed during a snack/meal in laboratory settings
Only one of the five studies was at low risk of bias (Crockett 2014), while one was at unclear risk (Girz 2012 ‐ study 1), and the other three were at high risk of bias (Ebneter 2013; Wansink 2006 ‐ study 1; Wansink 2006 ‐ study 3).
Using GRADE criteria, we downgraded the evidence one level for serious risk of bias, one level for heterogeneity, and one level for indirectness, as behaviour observed in a laboratory setting may not be applicable to real‐world settings. In addition, the 95% confidence interval included the possibility of a meaningful decrease or increase; however, the quality score was already very low, and we could not reduce it further to recognise this imprecision. Thus, we judged the quality of the evidence for studies of mislabelling on energy consumption to be very low, meaning we have very little confidence in the results presented, and the true effect is likely to be substantially different from the estimate of effect.
Discussion
Summary of main results
Purchasing food or drinks in real‐world settings (vending machines, grocery stores, restaurants, cafeterias or coffee shops)
Eleven studies, comprising five RCTs and six interrupted time series (ITS) studies, assessed the impact of nutritional labels on menus or menu boards, or nutritional labels placed on, or adjacent to, a range of food or drink options, on purchasing in real‐world settings. One cluster‐RCT assessed purchasing from vending machines; one ITS study, from grocery stores; and three RCTs, one Q‐RCT and five ITS, from restaurants and cafeterias. We could not interpret study results on vending machines and grocery stores and considered the evidence to be of very low quality. A meta‐analysis of the three RCTs, all of which assessed energy labelling in restaurants, demonstrated a statistically significant reduction of 47 kcal in energy purchased when menus were labelled. Assuming an average meal of 600 kcal, this represents a 7.8% reduction (95% CI 2.5% to 13.1%) in energy purchasing. Applying the GRADE system, we considered the quality of the evidence for these three studies as low, so our confidence in the effect estimate is limited and may change with further studies. Of the remaining six studies, we considered only two (both ITS studies involving energy labels on menus or menu boards) to be at low risk of bias, and their results support the meta‐analysis. The other four studies which were conducted in a restaurant, cafeterias (2 studies) or a coffee shop, did not clearly report their results, so we considered them to be at high risk of bias.
Consumption of food or drinks in laboratory settings
Seventeen studies, comprising 13 RCTs and 4 Q‐RCTs, assessed the impact of nutritional labelling on consumption of food or drink in an artificial settings or scenarios (referred to as laboratory settings in this review).
Of these, eight RCTs assessed the effect of labels on menus, or labels placed on a range of food options, on energy consumed during a meal. A meta‐analysis of these eight studies did not conclusively demonstrate a reduction in energy consumed when menus or foods were labelled, but the results favoured nutritional labelling. Assuming an average meal intake of 600 kcal, the size of this effect suggests that energy labelling of menus or food would reduce consumption per meal by about 8.4% (95% CI −0.7% to 17.4%). Applying the GRADE system, we considered the quality of the evidence for this group of studies to be low, meaning that our confidence in the effect estimate is limited and that the estimate may change with further studies. In a pre‐planned sensitivity analysis including only the three studies at low risk of bias, we found a statistically significant reduction of 72 kcal in energy consumed, equating to a reduction of 12.0% per meal (95% CI 1% to 23%). Further studies at low risk of bias are needed to increase confidence in this effect size.
Six laboratory studies (four RCTs and two Q‐RCTs) assessed the impact of labelling a single food or drink option (cookies, high‐sugar breakfast cereal, chocolate, popcorn, an entrée, or soft drinks) on energy consumed during a snack or meal. A meta‐analysis of these six studies did not demonstrate a statistically significant difference in energy (kcal) consumed with labelling, and in any case the effect size was small (Cohen 1988). However, the confidence intervals were wide, suggesting uncertainty in the true effect size. Applying the GRADE system, we considered the quality of the evidence for this group of studies to be low, so our confidence in the effect estimate is limited and may change with further studies. The results were similar in a sensitivity analysis that included only two studies at low risk of bias.
Subgroup analysis exploring possible moderating effects (restrained eaters and unrestrained eaters; studies conducted in the USA and studies conducted in other countries) did not show a difference in impact of nutritional labelling. However, these analyses were likely underpowered due to the small number of studies in each subgroup.
Potential harms associated with labelling
Based on the analyses described above, there was no evidence that nutritional labelling had the unintended harm of increasing energy purchased or consumed. Indirect evidence concerning potential harm came from five laboratory studies that involved mislabelling content for a single nutrient (i.e. placing low energy or low fat labels on high‐energy foods) during a snack or meal. A meta‐analysis of these five studies did not demonstrate a statistically significant increase in energy (kcal) consumed, and the effect size was small (Cohen 1988). However, the confidence intervals were wide, suggesting uncertainty in the true effect size. We considered the quality of the evidence from these studies to be very low, providing very little confidence in the effect estimate.
Overall completeness and applicability of evidence
We used an extensive search strategy involving a comprehensive range of databases and other sources and, whilst possible, it is unlikely that we missed relevant references. In addition, we included only studies with objectively assessed outcomes, thus increasing the applicability of the evidence to actual behaviour. However, the applicability of the evidence was limited by several study characteristics. Most (21/28) studies took place in the USA and none were in low‐ or middle‐income countries. Furthermore, many of the studies took place in university settings (19/28), and 17 took place in artificial or laboratory settings. While the review results are necessarily limited to the foods and drinks evaluated in the included studies, these encompassed a range of foods including fast food and other meals, soft drinks and snacks. The extent to which the results of this review are applicable beyond North American university settings or laboratory settings is uncertain. For one of the meta‐analyses (Analysis 4.1), we acknowledge that the probable lack of consistency in the distributions of values associated with the different outcome measures is a potential limitation, constraining the extent to which the SD units are comparable across the studies.
One of the strengths of this review is that we included all types of nutritional labels. This review, however, did not set out to compare labels in terms of content or format. Thus, the results apply to nutritional labelling in general.
Quality of the evidence
We assessed the quality of the evidence included in this review as low or very low using GRADE criteria. These low ratings were largely due to the large number of studies with a high risk of bias, imprecision in the pooled effect estimates, and unknown applicability of laboratory studies to real‐world settings.
Potential biases in the review process
At least two independent reviewers were involved in the selection of studies and in the data extraction and quality assessment processes, thus reducing the potential for reviewer error and bias. We sought published and unpublished studies in any language, thus reducing the potential for language and publication biases. It is possible that we failed to identify all relevant research for inclusion in the review, although we took steps to reduce this possibility by citation searching and contacting researchers in the field regarding eligible studies. We also made a number of changes to the review after writing the protocol, although we provided a rationale for these changes in Differences between protocol and review. In addition, we could have re‐analysed the graphs in some of the interrupted time series studies using segmented time series regression techniques, although in most cases data presented in the graphs were inadequate to enable this. However, even when adequate data were available, we did not do this because we considered most studies to be at high risk of bias.
Agreements and disagreements with other studies or reviews
We identified 12 systematic reviews that concern nutritional labelling (Bleich 2017; Campos 2011; Cantu‐Jungles 2017; Cecchini 2016; Cowburn 2005; Grech 2015; Grunert 2007; Harnack 2008b; Mhurchu 2007; Shemilt 2017; Sinclair 2014; Swartz 2011), nine of which assessed at least one type of behavioural outcome (i.e. purchasing or consumption). Of the three reviews that did not report behavioural outcomes, two evaluated outcomes such as consumer knowledge and understanding of nutritional labelling (Campos 2011; Cowburn 2005). The third review aimed to assess behavioural outcomes, but it included no studies that evaluated these types of outcomes (Mhurchu 2007). Despite differences in assessed outcomes between these latter three reviews and our review, all three studies found evidence to support nutritional labelling that is understandable and accessible as a means to promote healthier food choices in different consumer groups such as children, adolescents or older people (Campos 2011).
Of the nine reviews that assessed at least one type of behavioural outcome (Bleich 2017; Cantu‐Jungles 2017; Cecchini 2016; Grech 2015; Grunert 2007; Harnack 2008b; Shemilt 2017; Sinclair 2014; Swartz 2011), none had the same inclusion criteria as our review in terms of the interventions, study design or outcomes evaluated here, making comparisons between these and the current review difficult. There were also major differences between some of these reviews and ours in terms of data comparison and analysis. Unlike previous reviews, ours differentiated the impacts of nutritional labels used in different physical contexts, including vending machines, grocery stores, and cafeterias, restaurants or coffee shops. We also considered the impacts on purchasing and the impacts on consumption separately. These previous reviews assessed a range of outcomes (including 'choice', 'selection', 'foods ordered' or 'intentions') and several contexts (including real‐world settings, laboratory settings or in response to hypothetical scenarios).
The five systematic reviews we judged most similar to ours were Bleich 2017; Cantu‐Jungles 2017; Swartz 2011, Sinclair 2014, and Cecchini 2016. Swartz 2011 assessed the impact of energy labels on menus in restaurants but included only non‐RCTs. Based on a narrative synthesis of seven studies, the authors concluded that energy labelling on menus did not decrease energy purchasing or consumption. Three of the studies included in that review also met the inclusion criteria for our review. We judged them as having poor quality, and they did not present data that we could clearly interpret or use to estimate effect sizes.
Bleich 2017 assessed the effectiveness of menu labelling on calories offered, ordered, purchased, or consumed in restaurant, cafeteria, and laboratory settings. The authors concluded that the impact of menu labelling on encouraging lower calorie purchases remains unclear. This systematic review substantially differed from our review in that it included a number of types of study designs that did not meet our eligibility criteria, and it did not include a meta‐analysis or quality assessment of the included studies.
Similarly, Cantu‐Jungles 2017 examined the effect of restaurant menu labelling on calories and nutrients chosen by adults in restaurants or simulated settings. Their meta‐analysis of 14 studies showed no effect of menu labelling on calories chosen, either ordered or consumed (MD −0.21 calories (95% CI: −1.36 to 0.94). The authors did, however, report a significant difference of −115.2 calories when the meta‐analysis was restricted to studies conducted in laboratory settings. As above, this systematic review substantially differed from our review despite the authors using a modified version of our review protocol (Crockett 2011). For example, before‐and‐after controlled studies were included in the Cantu‐Jungles 2017 review which we also assessed, but that we found did not meet EPOC requirements for implementation in at least two intervention and two control sites. Moreover, this review did not report a full quality assessment of the individual studies or summarise the quality of evidence using the GRADE system. In addition, purchasing and consumption outcomes were not treated separately, as in the current review, as we considered them, a priori, to be different outcomes.
Sinclair 2014 also assessed the impact of nutritional labelling on menus. A meta‐analysis of six studies (with 24 comparisons) resulted in a significant reduction in energy consumed (MD −41 kcal (95% CI −79 to −3) compared to no intervention. These results were consistent with the effects we found in our review. Our analysis of consumption also included five out of six of the studies included in Sinclair 2014 (of the total eight studies in our meta‐analysis); the sixth study failed to meet our inclusion criteria.
Similar to our review, Cecchini 2016 aimed to assess the effectiveness of food labelling for increasing the selection of healthier products and reducing energy intake. Unlike our review, the authors included a heterogeneous range of labels, including logos such as the healthy choice tick, serving size labels, as well as labels with nutrient information (guideline daily amounts, or GDA), and a mix of outcomes including purchasing intentions, an outcome we excluded from our review due to validity concerns. Moreover, the authors excluded studies that evaluated menu labelling. Cecchini 2016 reported a significant increase in the number of people making a healthier choice and a non‐significant decrease in calorie intake. Differences in our review methods have allowed us to form stronger conclusions. For example, our search strategy retrieved seven more RCTs, despite having narrower inclusion criteria.
Authors' conclusions
Implications for practice.
The results from a small body of low quality evidence suggest that nutritional labelling comprising energy information on menus may reduce energy purchased in restaurants. The evidence assessing the impact on consumption of energy information on menus or placed on a range of food options in laboratory settings suggests a similar effect to that observed for purchasing, although the evidence is less definite and also of low quality. Considered alongside other reviews, we tentatively suggest that nutritional labelling on menus in restaurants could be used as part of a broader range of interventions to increase the impact of efforts to support healthier food consumption across populations.
Implications for research.
The evidence available for this review was limited in quality and quantity. Further high‐quality studies are needed to address the dearth of evidence from grocery stores and vending machines and to assess the impact of nutritional labels varying in content and format on purchasing and consumption. In addition, further research is needed to test the effects of single versus multiple labelled food options to assess associations between labelling, food options and behaviour.
High quality studies are also needed on the effectiveness of nutritional labelling alongside other interventions to promote healthy diets. This might include price interventions (e.g. Ellison 2014a; Harnack 2008a), availability of more healthy options (Grech 2015; Hollands 2017a), reductions in portion size (Hollands 2015; Marteau 2015), and product reformulation (Public Health England 2015). The evidence base would also be improved by the use of high‐quality randomised controlled trials with evaluations of long‐term effects and clear reporting of methods, including those relating to risk of bias.
There was a notable absence of evidence assessing potential moderators of the effect of nutritional labelling on behaviour. In particular, any meaningful examination of the potential moderating role of socioeconomic status, will require, at minimum, studies to report these details at the study level, and preferably to stratify results by socioeconomic status subgroups. A further notable absence in the evidence base was assessment of nutritional labelling in low‐ and middle‐income countries. Given that energy‐dense diets are becoming cheaper and more accessible in these countries, with corresponding rising rates of obesity (Brownell 2006; Ng 2014; Yach 2006), an evaluation of the effectiveness of nutritional labelling and other interventions to promote healthier food purchasing and consumption is warranted.
Future research would benefit from a more diverse logic model that takes account of possible wider impacts of nutritional labelling. These include impacts upon those producing and selling food, who may decide to reformulate or adjust the choice of items available, as well as the impact of labelling on consumer behaviour when applied in combination with other interventions.
What's new
| Date | Event | Description |
|---|---|---|
| 16 June 2021 | Amended | Editorial note amended |
History
Protocol first published: Issue 9, 2011 Review first published: Issue 2, 2018
| Date | Event | Description |
|---|---|---|
| 15 June 2021 | Amended | Published note added, linking this review to a new protocol of a review to supersede this one. |
| 11 October 2018 | Amended | Published note added in response to recent retraction of several studies by Brian Wansink |
Notes
From the author team, 10 October, 2018, in response to recent retraction of several studies by Brian Wansink
On the 19th September 2018, JAMA, JAMA Internal Medicine and JAMA Pediatrics retracted six articles on which Brian Wansink (John Dyson Professor of Marketing at Cornell University), was an author (https://media.jamanetwork.com/news-item/jama-network-retracts-6-articles-that-included-dr-brian-wansink-as-author/). Given seven previous retractions, this means that 13 of his articles have been retracted as of 10th October 2018 (http://retractiondatabase.org/RetractionSearch.aspx#?auth%3dWansink). The retracted articles are listed at the end of this note.
None of the 13 retracted articles authored by Wansink were included in this Cochrane review. The results and conclusions of the review are therefore not affected.
Other articles on which Wansink is an author, and which have not been retracted, were included in this review. It includes 28 studies, of which two studies were authored by Wansink.
The effects reported in this review are uncertain, attributable in part to evidence that is at significant risk of bias with, at best, GRADE ratings of ‘low’ (meaning that further research is very likely to have an important impact on our confidence in estimated effects). These retractions do, however, introduce additional uncertainty regarding the veracity of other studies Wansink has authored, including those contributing to this review. Should any study included in this review be retracted, we will withdraw that study’s data from updated meta‐analyses conducted as part of future updates of this Cochrane review. Gareth Hollands and Theresa Marteau, on behalf of the author team Retracted studies (as of 10th October 2018)
Wansink B, Tal A, Shimizu M (2012). First foods most: after 18‐hour fast, people drawn to starches first and vegetables last. Arch Intern Med. 172(12): 961‐963.
Tal A, Wansink B (2013). Fattening fasting: hungry grocery shoppers buy more calories, not more food. JAMA Intern Med. 173(12): 1146‐1148.
Tal A, Zuckerman S, Wansink B (2014). Watch what you eat: action‐related television content increases food intake. JAMA Intern Med. 174(11): 1842‐1843.
Wansink B, Cheney MM (2005). Super Bowls: serving bowl size and food consumption. JAMA. 293(14): 1727‐1728.
Wansink B, Payne C, Werle C (2008). Consequences of belonging to the “clean plate club”. Arch Pediatr Adolesc Med. 162(10): 994‐995.
Hanks AS, Just DR, Wansink B (2013). Preordering school lunch encourages better food choices by children. JAMA Pediatr. 167(7): 673‐674.
Vuorinen A‐L, Strahilevitz MA, Wansink B, Safer DL (2017). Shifts in the Enjoyment of Healthy and Unhealthy Behaviors Affect Short‐ and Long‐Term Postbariatric Weight Loss. Bariatric Surgical Practice and Patient Care. 12(1): 35–42.
Wansink B, Just DR, Payne CR, Klinger MZ (2012). Attractive names sustain increased vegetable intake in schools. Prev Med. 55(4):330‐332.
Wansink B, Westgren R (2003). Profiling taste‐motivated segments. Appetite. 41(3): 323‐7.
Sigirci O, Rockmore M, Wansink B (2016). How Traumatic Violence Permanently Changes Shopping Behavior. Front. Psychol. 7:1298.
Sigirci O, Wansink B (2015). Low prices and high regret: how pricing influences regret at all‐you‐can‐eat buffets. BMC Nutrition 1:36.
Wansink B, Park S‐B (2002). Sensory Suggestiveness and Labeling: Do Soy Labels Bias Taste? Journal of Sensory Studies. 17(5): 483‐491.
Wansink B, Just DR, Payne CR (2012). Can Branding Improve School Lunches? Arch Pediatr Adolesc Med. 166(10): 967‐968.
Acknowledgements
Emma Norris, Ocean Blue and Chandrika Cyril worked as research assistants on the review, assisting with the search and selection of studies as well as data entry.
Joana Vasconcelos was the second assessor for one of papers and assisted with addressing some reviewers comments.
Stephan Dombrowski and Mike Rayner gave helpful feedback on an early draft of the review.
Appendices
Appendix 1. Search strategies
| Cochrane Central Register of Controlled Trials and Cochrane Database of Systematic Reviews (CDSR)(Cochrane Library, Wiley) | |
| #1 | MeSH descriptor: [Food Packaging] explode all trees |
| #2 | label$ or content$ sign$ or symbol$ or ticket$ or sticker$ or diet$ or health$ or calori$ or nutritio$ or guideline daily amount$ or recommended daily amount$ or nutrient reference value$ or nutrient daily value$:ti,ab,kw (Word variations have been searched) |
| #3 | #1 and #2 |
| #4 | food pack$:ti,ab,kw (Word variations have been searched) |
| #5 | MeSH descriptor: [Product Labeling] explode all trees |
| #6 | food$ or fat$ or sugar$ or salt or diet$ or health$ or calori$ or nutritio$ or guideline daily amount$ or recommended daily amount$ or nutrient reference value$ or nutrient daily value$ or snack$ or eat$:ti,ab,kw (Word variations have been searched) |
| #7 | #5 and #6 |
| #8 | (((soft or sugar? or sweet* or carbonated or energy or sport? or diet or flavo?red or fruit* or milk* or dairy or yoghurt or caffein* or cold or hot or nonalcohol* or non‐alcohol*) near/3 (drink? or beverage?)) or soda? or flavo?red water? or fruit water? or cordial? or squash? or juice? or smoothie? or milkshake? or tea or teas or coffee?) |
| #9 | #5 and #8 |
| #10 | MeSH descriptor: [Food Labeling] explode all trees |
| #11 | ((Nutritio$ or Nutrient$) near (label$ or content$ sign$ or symbol$ or ticket$ or sticker$)):ti,ab,kw (Word variations have been searched) |
| #12 | nutrition$ information or nutrient$ information:ti,ab,kw (Word variations have been searched) |
| #13 | Food$ label$ or food$ content$ label$ or food$ content$ sign$ or food$ content symbol$ or food$ content$ tag$ or food$ content$ ticket$ or food$ content$ sticker$:ti,ab,kw (Word variations have been searched) |
| #14 | traffic light$:ti,ab,kw (Word variations have been searched) |
| #15 | guideline daily amount$ or nutrient reference value$ or nutrient daily value$:ti,ab,kw (Word variations have been searched) |
| #16 | (recommended dietary allowance$ near (label$ or content$ sign$ or symbol$ or information or ticket$ or sticker$)):ti,ab,kw (Word variations have been searched) |
| #17 | Healthy choice:ti,ab,kw (Word variations have been searched) |
| #18 | ((Calorific or calorie$ or caloric) and (label$ or content$ sign$ or symbol$ or ticket$ or sticker$)):ti,ab,kw (Word variations have been searched) |
| #19 | ((Calorific or calorie$ or caloric) next information):ti,ab,kw (Word variations have been searched) |
| #20 | (fat near (label$ or content$ sign$ or symbol$ or tag$ or ticket$ or sticker$)):ti,ab,kw (Word variations have been searched) |
| #21 | (salt near (label$ or content$ sign$ or symbol$ or tag$ or ticket$ or sticker$)):ti,ab,kw (Word variations have been searched) |
| #22 | (sugar near (label$ or content$ sign$ or symbol$ or tag$ or ticket$ or sticker$)):ti,ab,kw (Word variations have been searched) |
| #23 | (menu near (label$ or content$ sign$ or symbol$ or tag$ or ticket$ or sticker$)):ti,ab,kw (Word variations have been searched) |
| #24 | (menu and (nutritional content$ or nutritional information or traffic light$ or guideline daily amount or GDA or healthy choice or calorie or fat or sugar or salt)):ti,ab,kw (Word variations have been searched) |
| #25 | (Label$ near/2 (legislation$ or regulation$ or policies or policy)):ti,ab,kw (Word variations have been searched) |
| #26 | (Drink* label* or Drink* content* label* or Drink* content* sign* or Drink* content symbol* or Drink* content* tag* or Drink* content* ticket* or Drink* content* sticker*):ti,ab,kw |
| #27 | ((((soft or sugar? or sweet* or carbonated or energy or sport? or diet or flavo?red or fruit* or milk* or dairy or yoghurt or caffein* or cold or hot or nonalcohol* or non‐alcohol*) near/3 (drink? or beverage?)) or soda? or flavo?red water? or fruit water? or cordial? or squash? or juice? or smoothie? or milkshake? or tea or teas or coffee?) and (label* or content* sign* or symbol* or ticket* or sticker*)):ti,ab,kw |
| #28 | #3 or #4 or #7 or #9 or #10 or #11 or #12 or #13 or #14 or #15 or #16 or #17 or #18 or #19 or #20 or #21 or #22 or #23 or #24 or #25 or #26 or #27 |
| #29 | MeSH descriptor: [Food Habits] explode all trees |
| #30 | MeSH descriptor: [Feeding Behavior] this term only |
| #31 | MeSH descriptor: [Food Preferences] explode all trees |
| #32 | MeSH descriptor: [Eating] explode all trees |
| #33 | MeSH descriptor: [Diet] explode all trees |
| #34 | MeSH descriptor: [Choice Behavior] this term only |
| #35 | (intak$ or consume or consumes or consumption or consumed or eat$ or diet$):ti,ab,kw (Word variations have been searched) |
| #36 | (food near (preference$ or habit$ or behavio?r$ or choice$ or decision$ or decid$ or inclin$ or lik$ or choos$ or select$ or pick$)):ti,ab,kw (Word variations have been searched) |
| #37 | ((drink* or beverage*) near (preference$ or habit$ or behavio?r$ or choice$ or decision$ or decid$ or inclin$ or lik$ or choos$ or select$ or pick$)):ti,ab,kw |
| #38 | #29 or #30 or #31 or #32 or #33 or #34 or #35 or #36 |
| #39 | MeSH descriptor: [Restaurants] explode all trees |
| #40 | purchas$ or buy$ or sale$ or vend$ or sell$:ti,ab,kw (Word variations have been searched) |
| #41 | shop$ or store$ or supermarket$ or market$ or outlet$ or retailer$ or point of purchase:ti,ab,kw (Word variations have been searched) |
| #42 | restaurant$ or cafe$ or bar$ or canteen$ or cafeteria$ or dinner hall$ or dining area$ or dining room$ or refector$ or eatery or mess or buffet or bistro$ or eating place$:ti,ab,kw (Word variations have been searched) |
| #43 | #39 or #40 or #41 or #42 |
| #44 | #28 and (#38 or #43) |
| Medline (OvidSP) | |
| 1 | exp Food packaging/ and (label$ or content$ sign$ or symbol$ or ticket$ or sticker$ or diet$ or health$ or calori$ or nutritio$ or guideline daily amount$ or recommended daily amount$ or nutrient reference value$ or nutrient daily value$).ti,ab. |
| 2 | food pack$.ab,ti. |
| 3 | exp Product labelling/ and (food$ or fat$ or sugar$ or salt or diet$ or health$ or calori$ or nutritio$ or guideline daily amount$ or recommended daily amount$ or nutrient reference value$ or nutrient daily value$ or snack$ or eat$).ti,ab. |
| 4 | exp Food Labeling/ |
| 5 | ((Nutritio$ or Nutrient$) adj5 (label$ or content$ sign$ or symbol$ or ticket$ or sticker$)).ab,ti. |
| 6 | (nutrition$ information or nutrient$ information).ti,ab. |
| 7 | (Food$ label$ or food$ content$ label$ or food$ content$ sign$ or food$ content symbol$ or food$ content$ tag$ or food$ content$ ticket$ or food$ content$ sticker$).ab,ti. |
| 8 | traffic light$.ab,ti. |
| 9 | (guideline daily amount$ or nutrient reference value$ or nutrient daily value$).ab,ti. |
| 10 | (recommended dietary allowance$ adj5 (label$ or content$ sign$ or symbol$ or information or ticket$ or sticker$)).ab,ti. |
| 11 | ((Calorific or calorie$ or caloric) and (label$ or content$ sign$ or symbol$ or ticket$ or sticker$)).ab,ti. |
| 12 | ((Calorific or calorie$ or caloric) adj information).ab,ti. |
| 13 | (fat adj5 (label$ or content$ sign$ or symbol$ or tag$ or ticket$ or sticker$)).ab,ti. |
| 14 | (salt adj5 (label$ or content$ sign$ or symbol$ or tag$ or ticket$ or sticker$)).ab,ti. |
| 15 | (sugar adj5 (label$ or content$ sign$ or symbol$ or tag$ or ticket$ or sticker$)).ab,ti. |
| 16 | (menu and (label$ or content$ sign$ or symbol$ or tag$ or ticket$ or sticker$)).ab,ti. |
| 17 | (menu and (nutritional content$ or nutritional information or traffic light or guideline daily amount or GDA or healthy choice or calorie or fat or sugar)).ab,ti. |
| 18 | (Label$ adj2 (legislation$ or regulation$ or policies or policy)).ti,ab. |
| 19 | Healthy choice.ab,ti. |
| 20 | exp Product labelling/ and (((soft or sugar? or sweet$ or carbonated or energy or sport? or diet or flavo?red or fruit$ or milk$ or dairy or yoghurt or caffein$ or cold or hot or nonalcohol$ or non‐alcohol$) adj3 (drink? or beverage?)) or soda? or flavo?red water? or fruit water? or cordial? or squash? or juice? or smoothie? or milkshake? or tea or teas or coffee?).ab,ti. |
| 21 | (Drink$ label$ or Drink$ content$ label$ or Drink$ content$ sign$ or Drink$ content symbol$ or Drink$ content$ tag$ or Drink$ content$ ticket$ or Drink$ content$ sticker$).ab,ti. |
| 22 | ((((soft or sugar? or sweet$ or carbonated or energy or sport? or diet or flavo?red or fruit$ or milk$ or dairy or yoghurt or caffein$ or cold or hot or nonalcohol$ or non‐alcohol$) adj3 (drink? or beverage?)) or soda? or flavo?red water? or fruit water? or cordial? or squash? or juice? or smoothie? or milkshake? or tea or teas or coffee?) and (label$ or content$ sign$ or symbol$ or ticket$ or sticker$)).ab,ti. |
| 23 | 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22 |
| 24 | exp Food Preferences/ |
| 25 | exp Food Habits/ |
| 26 | exp Feeding Behavior/ |
| 27 | exp Eating/ |
| 28 | exp Diet/ |
| 29 | exp Choice Behavior/ |
| 30 | (intak$ or consume or consumes or consumption or consumed or eat$ or diet$).ti,ab. |
| 31 | (food adj5 (preference$ or habit$ or behavio?r$ or choice$ or decision$ or decid$ or inclin$ or lik$ or choos$ or select$ or pick$)).ab,ti. |
| 32 | ((drink? or beverage?) adj5 (preference$ or habit$ or behavio?r$ or choice$ or decision$ or decid$ or inclin$ or lik$ or choos$ or select$ or pick$)).ab,ti. |
| 33 | 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 |
| 34 | exp Restaurants/ |
| 35 | (purchas$ or buy$ or sale$ or vend$ or sell$).ab,ti. |
| 36 | (shop$ or store$ or supermarket$ or market$ or outlet$ or retailer$ or point of purchase).ab,ti. |
| 37 | (restaurant$ or cafe$ or bar$ or canteen$ or cafeteria$ or dinner hall$ or dining area$ or dining room$ or refector$ or eatery or mess or buffet or bistro$ or eating place$).ab,ti. |
| 38 | 34 or 35 or 36 or 37 |
| 39 | 23 and (33 or 38) |
| Embase (OvidSP) | |
| 1 | Food packaging/ and (label$ or content$ sign$ or symbol$ or ticket$ or sticker$ or diet$ or health$ or calori$ or nutritio$ or guideline daily amount$ or recommended daily amount$ or nutrient reference value$ or nutrient daily value$).ti,ab. |
| 2 | food pack$.ab,ti. |
| 3 | ((Nutritio$ or Nutrient$) adj5 (label$ or content$ sign$ or symbol$ or ticket$ or sticker$)).ab,ti. |
| 4 | (nutrition$ information or nutrient$ information).ti,ab. |
| 5 | (Food$ label$ or food$ content$ label$ or food$ content$ sign$ or food$ content symbol$ or food$ content$ tag$ or food$ content$ ticket$ or food$ content$ sticker$).ab,ti. |
| 6 | traffic light$.ab,ti. |
| 7 | (guideline daily amount$ or nutrient reference value$ or nutrient daily value$).ab,ti. |
| 8 | (recommended dietary allowance$ adj5 (label$ or content$ sign$ or symbol$ or information or ticket$ or sticker$)).ab,ti. |
| 9 | ((Calorific or calorie$ or caloric) and (label$ or content$ sign$ or symbol$ or ticket$ or sticker$)).ab,ti. |
| 10 | ((Calorific or calorie$ or caloric) adj information).ab,ti. |
| 11 | (fat adj5 (label$ or content$ sign$ or symbol$ or tag$ or ticket$ or sticker$)).ab,ti. |
| 12 | (salt adj5 (label$ or content$ sign$ or symbol$ or tag$ or ticket$ or sticker$)).ab,ti. |
| 13 | (sugar adj5 (label$ or content$ sign$ or symbol$ or tag$ or ticket$ or sticker$)).ab,ti. |
| 14 | (menu and (label$ or content$ sign$ or symbol$ or tag$ or ticket$ or sticker$)).ab,ti. |
| 15 | (menu and (nutritional content$ or nutritional information or traffic light or guideline daily amount or GDA or healthy choice or calorie or fat or sugar)).ab,ti. |
| 16 | (Label$ adj2 (legislation$ or regulation$ or policies or policy)).ti,ab. |
| 17 | Healthy choice.ab,ti. |
| 18 | (Drink$ label$ or Drink$ content$ label$ or Drink$ content$ sign$ or Drink$ content symbol$ or Drink$ content$ tag$ or Drink$ content$ ticket$ or Drink$ content$ sticker$).ab,ti. |
| 19 | ((((soft or sugar? or sweet$ or carbonated or energy or sport? or diet or flavo?red or fruit$ or milk$ or dairy or yoghurt or caffein$ or cold or hot or nonalcohol$ or non‐alcohol$) adj3 (drink? or beverage?)) or soda? or flavo?red water? or fruit water? or cordial? or squash? or juice? or smoothie? or milkshake? or tea or teas or coffee?) and (label$ or content$ sign$ or symbol$ or ticket$ or sticker$)).ab,ti. |
| 20 | 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 |
| 21 | food preference/ |
| 22 | feeding behavior/ or drinking behavior/ |
| 23 | food intake/ or eating habit/ or energy consumption/ or portion size/ |
| 24 | Eating/ |
| 25 | exp *Diet/ |
| 26 | health behavior/ and (food$ or eat$ or diet$).ti,ab. |
| 27 | (intak$ or consume or consumes or consumption or consumed or eat$ or diet$).ti,ab. |
| 28 | (food adj5 (preference$ or habit$ or behavio?r$ or choice$ or decision$ or decid$ or inclin$ or lik$ or choos$ or select$ or pick$)).ab,ti. |
| 29 | ((drink? or beverage?) adj5 (preference$ or habit$ or behavio?r$ or choice$ or decision$ or decid$ or inclin$ or lik$ or choos$ or select$ or pick$)).ab,ti. |
| 30 | 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 |
| 31 | catering service/ |
| 32 | (purchas$ or buy$ or sale$ or vend$ or sell$).ab,ti. |
| 33 | (shop$ or store$ or supermarket$ or market$ or outlet$ or retailer$ or point of purchase).ab,ti. |
| 34 | (restaurant$ or cafe$ or bar$ or canteen$ or cafeteria$ or dinner hall$ or dining area$ or dining room$ or refector$ or eatery or mess or buffet or bistro$ or eating place$).ab,ti. |
| 35 | 31 or 32 or 33 or 34 |
| 36 | 20 and (30 or 35) |
| PsycINFO (OvidSP) | |
| 1 | exp Food/ and (label$ or content$ sign$ or symbol$ or tickets$ or diet$ or health$ or calori$ or nutri$ or health$ or calori$ or nutritio$ or guideline daily amount$ or recommended daily amount$ or nutrient reference value$ or nutrient daily values).ti,ab. |
| 2 | food pack$.ab,ti. |
| 3 | ((Nutritio$ or Nutrient$) adj5 (label$ or content$ sign$ or symbol$ or ticket$ or sticker$)).ab,ti. |
| 4 | (nutrition$ information or nutrient$ information).ti,ab. |
| 5 | (Food$ label$ or food$ content$ label$ or food$ content$ sign$ or food$ content symbol$ or food$ content$ tag$ or food$ content$ ticket$ or food$ content$ sticker$).ab,ti. |
| 6 | traffic light$.ab,ti. |
| 7 | (guideline daily amount$ or nutrient reference value$ or nutrient daily value$).ab,ti. |
| 8 | (recommended dietary allowance$ adj5 (label$ or content$ sign$ or symbol$ or information or ticket$ or sticker$)).ab,ti. |
| 9 | ((Calorific or calorie$ or caloric) and (label$ or content$ sign$ or symbol$ or ticket$ or sticker$)).ab,ti. |
| 10 | ((Calorific or calorie$ or caloric) adj information).ab,ti. |
| 11 | (fat adj5 (label$ or content$ sign$ or symbol$ or tag$ or ticket$ or sticker$)).ab,ti. |
| 12 | (salt adj5 (label$ or content$ sign$ or symbol$ or tag$ or ticket$ or sticker$)).ab,ti. |
| 13 | (sugar adj5 (label$ or content$ sign$ or symbol$ or tag$ or ticket$ or sticker$)).ab,ti. |
| 14 | (menu and (label$ or content$ sign$ or symbol$ or tag$ or ticket$ or sticker$)).ab,ti. |
| 15 | (menu and (nutritional content$ or nutritional information or traffic light or guideline daily amount or GDA or healthy choice or calorie or fat or sugar)).ab,ti. |
| 16 | (Label$ adj2 (legislation$ or regulation$ or policies or policy)).ti,ab. |
| 17 | Healthy choice.ab,ti. |
| 18 | exp "beverages (nonalcoholic)"/ and (label$ or content$ sign$ or symbol$ or tickets$ or diet$ or health$ or calori$ or nutri$ or health$ or calori$ or nutritio$ or guideline daily amount$ or recommended daily amount$ or nutrient reference value$ or nutrient daily values).ti,ab. |
| 19 | (Drink$ label$ or Drink$ content$ label$ or Drink$ content$ sign$ or Drink$ content symbol$ or Drink$ content$ tag$ or Drink$ content$ ticket$ or Drink$ content$ sticker$).ab,ti. |
| 20 | ((((soft or sugar? or sweet$ or carbonated or energy or sport? or diet or flavo?red or fruit$ or milk$ or dairy or yoghurt or caffein$ or cold or hot or nonalcohol$ or non‐alcohol$) adj3 (drink? or beverage?)) or soda? or flavo?red water? or fruit water? or cordial? or squash? or juice? or smoothie? or milkshake? or tea or teas or coffee?) and (label$ or content$ sign$ or symbol$ or ticket$ or sticker$)).ab,ti. |
| 21 | 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 |
| 22 | exp Food Preferences/ |
| 23 | exp Eating Behavior/ |
| 24 | exp Food Intake/ |
| 25 | exp Eating/ |
| 26 | exp Diets/ |
| 27 | exp Choice Behavior/ |
| 28 | (intak$ or consume or consumes or consumption or consumed or eat$ or diet$).ti,ab. |
| 29 | (food adj5 (preference$ or habit$ or behavio?r$ or choice$ or decision$ or decid$ or inclin$ or lik$ or choos$ or select$ or pick$)).ab,ti. |
| 30 | ((drink? or beverage?) adj5 (preference$ or habit$ or behavio?r$ or choice$ or decision$ or decid$ or inclin$ or lik$ or choos$ or select$ or pick$)).ab,ti. |
| 31 | 22 or 23 or 24 or 26 or 27 or 28 or 29 or 30 |
| 32 | restaurant.mp. |
| 33 | (purchas$ or buy$ or sale$ or vend$ or sell$).ab,ti. |
| 34 | (shop$ or store$ or supermarket$ or market$ or outlet$ or retailer$ or point of purchase).ab,ti. |
| 35 | (restaurant$ or cafe$ or bar$ or canteen$ or cafeteria$ or dinner hall$ or dining area$ or dining room$ or refector$ or eatery or mess or buffet or bistro$ or eating place$).ab,ti. |
| 36 | 32 or 33 or 34 or 35 |
| 37 | 21 and (31 or 36) |
| HMIC (OvidSP) | |
| 1 | food packaging/ |
| 2 | (packaging/ or product labelling/) and (label$ or content$ sign$ or symbol$ or ticket$ or sticker$ or diet$ or health$ or calori$ or nutritio$ or guideline daily amount$ or recommended daily amount$ or nutrient reference value$ or nutrient daily value$).ti,ab. |
| 3 | label$.mp. and (food$ or fat$ or sugar$ or salt or diet$ or health$ or calori$ or nutri$ or guideline daily amount$ or recommended daily amount$ or nutrient reference value$ or nutrient daily value$).ti,ab. |
| 4 | food pack$.ab,ti. |
| 5 | ((Nutritio$ or Nutrient$) adj5 (label$ or content$ sign$ or symbol$ or ticket$ or sticker$)).ab,ti. |
| 6 | (nutrition$ information or nutrient$ information).ti,ab. |
| 7 | (Food$ label$ or food$ content$ label$ or food$ content$ sign$ or food$ content symbol$ or food$ content$ tag$ or food$ content$ ticket$ or food$ content$ sticker$).ab,ti. |
| 8 | traffic light$.ab,ti. |
| 9 | (guideline daily amount$ or nutrient reference value$ or nutrient daily value$).ab,ti. |
| 10 | (recommended dietary allowance$ adj5 (label$ or content$ sign$ or symbol$ or information or ticket$ or sticker$)).ab,ti. |
| 11 | Healthy choice.ab,ti. |
| 12 | ((Calorific or calorie$ or caloric) and (label$ or content$ sign$ or symbol$ or ticket$ or sticker$)).ab,ti. |
| 13 | ((Calorific or calorie$ or caloric) adj information).ab,ti. |
| 14 | (fat adj5 (label$ or content$ sign$ or symbol$ or tag$ or ticket$ or sticker$)).ab,ti. |
| 15 | (salt adj5 (label$ or content$ sign$ or symbol$ or tag$ or ticket$ or sticker$)).ab,ti. |
| 16 | (sugar adj5 (label$ or content$ sign$ or symbol$ or tag$ or ticket$ or sticker$)).ab,ti. |
| 17 | (menu and (label$ or content$ sign$ or symbol$ or tag$ or ticket$ or sticker$)).ab,ti. |
| 18 | (menu and (nutritional content$ or nutritional information or traffic light or guideline daily amount or GDA or healthy choice or calorie or fat or sugar)).ab,ti. |
| 19 | (Label$ adj2 (legislation$ or regulation$ or policies or policy)).ti,ab. |
| 20 | (Drink$ label$ or Drink$ content$ label$ or Drink$ content$ sign$ or Drink$ content symbol$ or Drink$ content$ tag$ or Drink$ content$ ticket$ or Drink$ content$ sticker$).ab,ti. |
| 21 | ((((soft or sugar? or sweet$ or carbonated or energy or sport? or diet or flavo?red or fruit$ or milk$ or dairy or yoghurt or caffein$ or cold or hot or nonalcohol$ or non‐alcohol$) adj3 (drink? or beverage?)) or soda? or flavo?red water? or fruit water? or cordial? or squash? or juice? or smoothie? or milkshake? or tea or teas or coffee?) and (label$ or content$ sign$ or symbol$ or ticket$ or sticker$)).ab,ti. |
| 22 | 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 |
| 23 | exp food habits/ |
| 24 | feeding behaviour/ |
| 25 | exp Diet/ |
| 26 | (intak$ or consume or consumes or consumption or consumed or eat$ or diet$).ti,ab. |
| 27 | (food adj5 (preference$ or habit$ or behavio?r$ or choice$ or decision$ or decid$ or inclin$ or lik$ or choos$ or select$ or pick$)).ab,ti. |
| 28 | ((drink? or beverage?) adj5 (preference$ or habit$ or behavio?r$ or choice$ or decision$ or decid$ or inclin$ or lik$ or choos$ or select$ or pick$)).ab,ti. |
| 29 | 23 or 24 or 25 or 26 or 27 or 28 |
| 30 | restaurants/ or canteens/ or dining rooms/ or snack bars/ |
| 31 | (purchas$ or buy$ or sale$ or vend$ or sell$).ab,ti. |
| 32 | (shop$ or store$ or supermarket$ or market$ or outlet$ or retailer$ or point of purchase).ab,ti. |
| 33 | (restaurant$ or cafe$ or bar$ or canteen$ or cafeteria$ or dinner hall$ or dining area$ or dining room$ or refector$ or eatery or mess or buffet or bistro$ or eating place$).ab,ti. |
| 34 | 30 or 31 or 32 or 33 |
| 35 | 22 and (29 or 34) |
| CINAHL (EBSCOHost) | |
| S33 | S19 AND (S27 or S32) |
| S32 | S28 OR S29 OR S30 OR S31 |
| S31 | AB "restaurant*" OR "cafe*" OR "bar*" OR "canteen*" OR "cafeteria*" OR "dining room" OR "refector*" OR "mess*" OR "buffet*" OR bistro* OR "eating place*" OR "dining hall" |
| S30 | AB "shop*" OR "store*" OR "supermarket*" OR "market*" OR "outlet*" OR "retailer*" OR "point of purchase" |
| S29 | AB "purchas*" OR "buy*" OR "sale*" OR "vend" OR "sell" |
| S28 | MH "Restaurants" |
| S27 | S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 |
| S26 | AB ( AB ("drink intake" or "beverage intake" or drink consum* or beverage consum*) ) OR AB ( (drink? or beverage?) AND ( "preference*" OR "habit*" OR "behav*" OR "decision*" OR "decid*" OR "inclin*" OR "lik*" OR "select*" OR "choos*" OR "pick*" ) ) |
| S25 | AB "food" AND AB ( "preference*" OR "habit*" OR "behav*" OR "decision*" OR "decid*" OR "inclin*" OR "lik*" OR "select*" OR "choos*" OR "pick*" ) |
| S24 | AB "food intake" OR "food consum*" OR "eat*" OR "diet*" |
| S23 | MH "Diet+" |
| S22 | MH "Eating Behavior+" |
| S21 | MH "Food Habits" |
| S20 | MH "Food Preferences" |
| S19 | S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 OR S12 OR S13 OR S14 OR S15 OR S16 OR S17 OR S18 |
| S18 | ((((soft or sugar? or sweet* or carbonated or energy or sport? or diet or flavo?red or fruit* or milk* or dairy or yoghurt or caffein* or cold or hot or nonalcohol* or non‐alcohol*) N3 (drink? or beverage?)) or soda? or flavo?red water? or fruit water? or cordial? or squash? or juice? or smoothie? or milkshake? or tea or teas or coffee?) and (label* or content* sign* or symbol* or ticket* or sticker*)) |
| S17 | AB Drink* label* or Drink* content* label* or Drink* content* sign* or Drink* content symbol* or Drink* content* tag* or Drink* content* ticket* or Drink* content* sticker* |
| S16 | MH "Product Labeling+" AND AB ( (((soft or sugar? or sweet$ or carbonated or energy or sport? or diet or flavo?red or fruit$ or milk$ or dairy or yoghurt or caffein$ or cold or hot or nonalcohol$ or non‐alcohol$) N3 (drink? or beverage?)) or soda? or flavo?red water? or fruit water? or cordial? or squash? or juice? or smoothie? or milkshake? or tea or teas or coffee?) ) |
| S15 | AB "menu" N5 AB ( "label*" OR "content*" OR "sign*" OR "symbol*" OR "ticket*" OR "sticker*" ) |
| S14 | AB "sugar" N5 AB ( "label*" OR "content*" OR "sign*" OR "symbol*" OR "ticket*" OR "sticker*" ) |
| S13 | AB "salt" N5 AB ( "label*" OR "content*" OR "sign*" OR "symbol*" OR "ticket*" OR "sticker*" ) |
| S12 | AB "fat" N5 AB ( "label*" OR "content*" OR "sign*" OR "symbol*" OR "ticket*" OR "sticker*" ) |
| S11 | AB "calori*" N1 AB "information" |
| S10 | AB (calorific OR calorie* OR caloric) AND AB ( "label*" OR "content*" OR "sign*" OR "symbol*" OR "ticket*" OR "sticker*" ) |
| S9 | AB "healthy choice*" |
| S8 | AB "guideline daily amount*" |
| S7 | AB "traffic light*" |
| S6 | AB "food label*" OR "food content* label*" OR "food content* sign*" OR "food content* sticker*" OR "food content* symbol*" OR "food content* tag*" OR "food content* ticket*" OR "food content sticker*" |
| S5 | AB nutritio* N5 AB ( "label*" OR "content*" OR "sign*" OR "symbol*" OR "ticket*" OR "sticker*") |
| S4 | MH "Food Labeling" |
| S3 | MH "Product Labeling+" AND AB ( "food*" OR "fat*" OR "sugar*" OR "salt*" OR "diet*" OR "health*" OR "calori*" OR "nutrit*" OR "guideline daily amount*" ) |
| S2 | AB "food pack*" |
| S1 | MH "Food Packaging+" AND AB ( "label*" OR "content*" OR "sign*" OR "symbol*" OR "sticker*" OR "diet*" OR "health*" OR "calori*" OR "nutrit*" OR "guideline daily amount*" ) |
| Science Citation Index & Social Science Citation Index (Web of Science Core Collection) | |
| # 34 | #33 AND #23 |
| # 33 | #32 OR #28 |
| # 32 | #31 OR #30 OR #29 |
| # 31 | TI=("restaurant*" or "cafe*" or "bar*" or "canteen*" or "cafeteria*" or "din* hall*" or "dining area*" or "dining room*" or "refector*" or "eatery" or "mess" or "buffet*" or "bistro*" or "eating place*") |
| # 30 | TI=("shop*" or "store*" or "supermarket*" or "market*" or "outlet*" or "retailer*" or "point of purchas*") |
| # 29 | TI=("purchas*" or "buy*" or "sale*" or "vend*" or "sell*") |
| # 28 | #27 OR #26 OR #25 OR #24 |
| # 27 | TI=("drink preference*" OR "drink habit*") OR TI=((drink? or beverage?) NEAR/5 (preference* or habit* or behavio* or choice* or decision* or decid* or inclin* or lik* or choos* or select* or pick*)) |
| # 26 | TI=(food* NEAR/5 (preference* or habit* or behavio* or choice* or decision* or decid* or inclin* or lik* or choos* or select* or pick*)) |
| # 25 | TI=("intak*" or "consume*" or "consumption" or "eat*" or "diet*") |
| # 24 | TI=("food preference*"or "food habits*" or "feeding behave*" or "eating" or "diet*" or "choice behav*") |
| # 23 | #22 OR #21 OR #20 OR #19 OR #18 OR #17 OR #16 OR #15 OR #14 OR #13 OR #12 OR #11 OR #10 OR #9 OR #8 OR #7 OR #6 OR #5 OR #4 OR #3 OR #2 OR #1 |
| # 22 | TS=(((((soft or sugar? or sweet* or carbonated or energy or sport? or diet or flavo?red or fruit* or milk* or dairy or yoghurt or caffein* or cold or hot or nonalcohol* or non‐alcohol*) NEAR3 (drink? or beverage?)) or soda? or "flavo?red water?" or "fruit water?" or cordial? or squash? or juice? or smoothie? or milkshake? or tea or teas or coffee?) and (label* or content* sign* or symbol* or ticket* or sticker*))) |
| # 21 | TS=("Drink* label*" or "Drink* content* label*" or "Drink* content* sign*" or "Drink* content symbol*" or "Drink* content* tag*" or "Drink* content* ticket*" or "Drink* content* sticker*") |
| # 20 | TS=("product packag*") AND TS=((((soft or sugar? or sweet* or carbonated or energy or sport? or diet or flavo?red or fruit* or milk* or dairy or yoghurt or caffein* or cold or hot or nonalcohol* or non‐alcohol*) NEAR3 (drink? or beverage?)) or soda? or flavo?red water? or fruit water? or cordial? or squash? or juice? or smoothie? or milkshake? or tea or teas or coffee?)) |
| # 19 | TS=("Label*"NEAR/2 ("legislation*" or "regulation*" or "policies*" or "policy*")) |
| # 18 | TS=("menu" and ("nutritional content*" or "nutritional information" or "traffic light*" or "guideline daily amount*" or "GDA*" or "healthy choice*" or "calori*" or "fat" or "salt" or "sugar")) |
| # 17 | TS=("menu" NEAR/5 ("label*" or "content* sign*" or "symbol*" or "tag*" or "ticket*" or "sticker*")) |
| # 16 | TS=("sugar" NEAR/5 ("label*" or "content* sign*" or "symbol*" or "tag*" or "ticket*" or "sticker*")) |
| # 15 | TS= ("salt" NEAR/5 ("label*" or "content* sign*" or "symbol*" or "tag*" or "ticket*" or "sticker*")) |
| # 14 | TS=(fat NEAR/5 ("label*" or "content* sign*" or "symbol*" or "tag*" or "ticket*" or "sticker*")) |
| # 13 | TS=(("Calorific" or "calorie*" or "caloric*") NEAR/1 "information") |
| # 12 | TS=(("Calorific" or "calorie*" or "caloric*") and ("label*" or "content* sign*" or "symbol*" or "ticket*" or "sticker*")) |
| # 11 | TS=("healthy choice*") |
| # 10 | TS=("recommended dietary allowance*" NEAR/5 ("label*" or "content* sign*" or "symbol*" or "information" or "ticket*" or "sticker*")) |
| # 9 | TS=("guideline daily amount*" or "nutrient reference value*" or "nutrient daily value*") |
| # 8 | TS=("traffic light*") |
| # 7 | TS=("food* label*" or "food* content* label*" or "food* content* sign*" or "food* content* symbol*" or "food* content* tag*" or "food* content* ticket*" or "food* content* sticker*") |
| # 6 | TS=("nutrition* information" or "nutrient* information") |
| # 5 | TS=(("Nutritio*" or "Nutrient*") NEAR/5 ("label*" or "content* sign*" or "symbol*" or "ticket*" or "sticker*")) |
| # 4 | TS= ("food label*") |
| # 3 | TI=(label*) and TS= ("food*" or "fat*" or "sugar*" or "salt*" or "diet*" or "health*" or "calori*" or "nutritio*" or "guideline daily amount*" or "recommended daily amount*" or "nutrient reference value*" or "nutrient daily value*" or "snack*" or "eat*") |
| # 2 | TS=("food pack*") |
| # 1 | TS=("food packag*") and TS=("label*" or "content* sign*" or "symbol*" or "ticket*" or "sticker*" or "diet*" or "health*" or "calori*" or "nutritio*" or "guideline daily amount*" or "recommended daily amount*" or "nutrient reference value*" or "nutrient daily value*") |
| Scopus | |
| 1. ( ( ( TITLE‐ABS‐KEY ( ( "Label*" W/2 ( "legislation*" OR "regulation*" OR "policies*" OR "policy*" ) ) ) ) OR ( TITLE‐ABS‐KEY ( ( "menu" AND ( "nutritional content*" OR "nutritional information" OR "traffic light*" OR "guideline daily amount*" OR "GDA*" OR "healthy choice*" OR "calori*" OR "fat" OR "salt" OR "sugar" ) ) ) ) OR ( TITLE‐ABS‐KEY ( ( menu W/5 ( "label*" OR "content* sign*" OR "symbol*" OR "tag*" OR "ticket*" OR "sticker*" ) ) ) ) OR ( TITLE‐ABS‐KEY ( ( sugar W/5 ( "label*" OR "content* sign*" OR "symbol*" OR "tag*" OR "ticket*" OR "sticker*" ) ) ) ) OR ( TITLE‐ABS‐KEY ( ( salt W/5 ( "label*" OR "content* sign*" OR "symbol*" OR "tag*" OR "ticket*" OR "sticker*" ) ) ) ) OR ( TITLE‐ABS‐KEY ( ( fat W/5 ( "label*" OR "content* sign*" OR "symbol*" OR "tag*" OR "ticket*" OR "sticker*" ) ) ) ) OR ( TITLE‐ABS‐KEY ( ( ( "Calorific" OR "calorie*" OR "caloric*" ) near/1 "information" ) ) ) ) OR ( ( TITLE‐ABS‐KEY ( ( ( "Calorific" OR "calorie*" OR "caloric*" ) AND ( "label*" OR "content* sign*" OR "symbol*" OR "ticket*" OR "sticker*" ) ) ) ) OR ( TITLE‐ABS‐KEY ( "healthy choice*" ) ) OR ( TITLE‐ABS‐KEY ( ( "recommended dietary allowance*" W/5 ( "label*" OR "content* sign*" OR "symbol*" OR "information" OR "ticket*" OR "sticker*" ) ) ) ) OR ( TITLE‐ABS‐KEY ( "guideline daily amount*" OR "nutrient reference value*" OR "nutrient daily value*" ) ) OR ( TITLE‐ABS‐KEY ( "traffic light*" ) ) OR ( TITLE‐ABS‐KEY ( "food* label*" OR "food* content* label*" OR "food* content* sign*" OR "food* content* symbol*" OR "food* content* tag*" OR "food* content* ticket*" OR "food* content* sticker*" ) ) OR ( TITLE‐ABS‐KEY ( "nutrition* information" OR "nutrient* information" ) ) ) OR ( ( TITLE‐ABS‐KEY ( ( ( "Nutritio*" OR "Nutrient*" ) W/5 ( "label*" OR "content* sign*" OR "symbol*" OR "ticket*" OR "sticker*" ) ) ) ) OR ( TITLE‐ABS‐KEY ( "food label*" ) ) OR ( ( TITLE‐ABS‐KEY ( label* ) AND TITLE‐ABS‐KEY ( "food*" OR "fat*" OR "sugar*" OR "salt*" OR "diet*" OR "health*" OR "calori*" OR "nutritio*" OR "guideline daily amount*" OR "recommended daily amount*" OR "nutrient reference value*" OR "nutrient daily value*" OR "snack*" OR "eat*" ) ) ) OR ( TITLE‐ABS‐KEY ( "food pack*" ) ) OR ( ( TITLE‐ABS‐KEY ( "food packag*" ) AND TITLE‐ABS‐KEY ( "label*" OR "content* sign*" OR "symbol*" OR "ticket*" OR "sticker*" OR "diet*" OR "health*" OR "calori*" OR "nutritio*" OR "guideline daily amount*" OR "recommended daily amount*" OR "nutrient reference value*" OR "nutrient daily value*" ) ) ) ) ) AND ( ( ( TITLE ( "food preference*" OR "food habits*" OR "feeding behave*" OR "eating" OR "diet*" OR "choice behav*" ) ) OR ( TITLE ( ( "intak*" OR "consume*" OR "consumption" OR "eat*" OR "diet*" ) ) ) OR ( TITLE ( ( food* W/5 ( preference* OR habit* OR behavio* OR choice* OR decision* OR decid* OR inclin* OR lik* OR choos* OR select* OR pick* ) ) ) ) ) OR ( ( TITLE ( "purchas*" OR "buy*" OR "sale*" OR "vend*" OR "sell*" ) ) OR ( TITLE ( ( "shop*" OR "store*" OR "supermarket*" OR "market*" OR "outlet*" OR "retailer*" OR "point of purchas*" ) ) ) OR ( TITLE ( ( "restaurant*" OR "cafe*" OR "bar*" OR "canteen*" OR "cafeteria*" OR "din* hall*" OR "dining area*" OR "dining room*" OR "refector*" OR "eatery" OR "mess" OR "buffet*" OR "bistro*" OR "eating place*" ) ) ) ) ) AND ( EXCLUDE ( SUBJAREA , "BIOC " ) OR EXCLUDE ( SUBJAREA , " CHEM " ) OR EXCLUDE ( SUBJAREA , " ENVI " ) OR EXCLUDE ( SUBJAREA , " PHAR " ) OR EXCLUDE ( SUBJAREA , " ENGI " ) OR EXCLUDE ( SUBJAREA , " MATE " ) OR EXCLUDE ( SUBJAREA , " IMMU " ) OR EXCLUDE ( SUBJAREA , " CENG " ) OR EXCLUDE ( SUBJAREA , " ARTS " ) OR EXCLUDE ( SUBJAREA , " COMP " ) OR EXCLUDE ( SUBJAREA , " VETE " ) OR EXCLUDE ( SUBJAREA , " PHYS " ) OR EXCLUDE ( SUBJAREA, " ENER " ) OR EXCLUDE ( SUBJAREA 2. ( TITLE‐ABS‐KEY ( ( ( ( ( soft OR sugar? OR sweet* OR carbonated OR energy OR sport? OR diet OR flavo?red OR fruit* OR milk* OR dairy OR yoghurt OR caffein* OR cold OR hot OR nonalcohol* OR non‐alcohol* ) W/5 ( drink? OR beverage? ) ) OR soda? OR "flavo?red water?" OR "fruit water?" OR cordial? OR squash? OR juice? OR smoothie? OR milkshake? OR tea OR teas OR coffee? ) AND ( label* OR content* AND sign* OR symbol* OR ticket* OR sticker* ) ) OR "drink* label*" OR "drink* content* label*" OR "drink* content* sign*" OR "drink* content* symbol*" OR "drink* content* tag*" OR "drink* content* ticket*" OR "drink* content* sticker*" OR "beverage* label*" OR "beverage* content* label*" OR "beverage* content* sign*" OR "beverage* content* symbol*" OR "beverage* content* tag*" OR "beverage* content* ticket*" OR "beverage* content* sticker*" ) ) AND ( TITLE ( "food preference*" OR "DRINK PREFERENCE*" OR "BEVERAGE PREFERENCE*" OR "food habits*""DRINK HABIT*" OR "BEVERAGE HABIT*" OR "feeding behavi*" OR "drinking behave*" OR "eating" OR "diet*" OR "choice behav*" ) OR TITLE ( "intak*" OR "consume*" OR "consumption" OR "eat*" OR "diet*" ) OR TITLE ( ( food* OR drink* OR beverage* ) W/5 ( preference* OR habit* OR behavio* OR choice* OR decision* OR decid* OR inclin* OR lik* OR choos* OR select* OR pick* ) ) OR TITLE ( "purchas*" OR "buy*" OR "sale*" OR "vend*" OR "sell*" ) OR TITLE ( "shop*" OR "store*" OR "supermarket*" OR "market*" OR "outlet*" OR "retailer*" OR "point of purchas*" ) OR TITLE ( "restaurant*" OR "cafe*" OR "bar*" OR "canteen*" OR "cafeteria*" OR "din* hall*" OR "dining area*" OR "dining room*" OR "refector*" OR "eatery" OR "mess" OR "buffet*" OR "bistro*" OR "eating place*" ) ) AND ( EXCLUDE ( SUBJAREA, "AGRI" ) OR EXCLUDE ( SUBJAREA, "BIOC" ) OR EXCLUDE ( SUBJAREA, "PHAR" ) OR EXCLUDE ( SUBJAREA, "CHEM" ) OR EXCLUDE ( SUBJAREA, "ENVI" ) OR EXCLUDE ( SUBJAREA, "ENGI" ) OR EXCLUDE ( SUBJAREA, "CENG" ) OR EXCLUDE ( SUBJAREA, "IMMU" ) OR EXCLUDE ( SUBJAREA, "MATH" ) OR EXCLUDE ( SUBJAREA, "VETE" ) OR EXCLUDE ( SUBJAREA, "MATE" ) OR EXCLUDE ( SUBJAREA, "PHYS" ) OR EXCLUDE ( SUBJAREA, "COMP" ) ) 3. 1 OR 2 |
|
|
ASSIA, Sociological Abstracts & ABI Inform (Proquest) |
|
| S6 | S4 AND S5 |
| S5 | ((AB,TI("food preference*" OR "drink preference*" OR "beverage preference*" OR "food habits*" OR "drink habit*" OR "beveragepreference*" OR "feeding behavio*" OR "drinking behavio*" OR "eating" OR "diet*" OR "choice behav*") OR (AB,TI("food*" OR drink* OR beverage*) N/2 AB,TI("preference*" OR "habit*" OR "behavio*" OR "choice*" OR "decision*" OR "decid*" OR "consump*"))) OR ((AB,TI("food*" OR drink* OR beverage*) AND AB,TI("purchas*" OR "buy*" OR "sale*" OR "vend*" OR "sell*")) OR (AB,TI("food*" OR drink* OR beverage*) AND AB,TI("shop*" OR "store*" OR "supermarket*" OR "point of purchas*")) OR (AB,TI("food*" OR drink* OR beverage*) and AB,TI("restaurant*" OR "cafe*" OR "canteen*" OR "cafeteria*" OR "din* hall*" OR "din* area*" OR "dining room*" OR "refector*" OR "buffet*" OR "bistro*")))) AND AB,TI(label* OR content* sign* OR symbol* OR ticket* OR sticker*) |
| S4 | S1 OR S2 OR S3 |
| S3 | AB,TI(((soft or sugar? or sweet* or carbonated or energy or sport? or diet or flavo?red or fruit* or milk* or dairy or yoghurt or caffein* or cold or hot or nonalcohol* or non‐alcohol*) N/3 (drink? or beverage?)) or soda? or flavo?red water? or fruit water? or cordial? or squash? or juice? or smoothie? or milkshake? or tea or teas or coffee?) AND AB,TI(label* or content* sign* or symbol* or ticket* or sticker*) |
| S2 | AB,TI("drink* label*" OR "drink* content* label*" OR "drink* content* sign*" OR "drink* content* symbol*" OR "drink* content* tag*" OR "drink* content* ticket*" OR "drink* content* sticker*" or "beverage* label*" OR "beverage* content* label*" OR "beverage* content* sign*" OR "beverage* content* symbol*" OR "beverage* content* tag*" OR "beverage* content* ticket*" OR "beverage* content* sticker*") |
| S1 | ALL("drink* packag*" or "beverage package*") AND ALL("label*" OR "content* sign*" OR "symbol*" OR "ticket*" OR "sticker*" OR "diet*" OR "health*" OR "calori*" OR "nutritio*" OR "guideline daily amount*" OR "recommended daily amount*" OR "nutrient reference value*" OR "nutrient daily value*") |
| TROPHI | |
| 1 | Focus of the report: healthy eating OR obesity |
| 2 | Freetext (All but Authors): label |
| 3 | Freetext (All but Authors): labels |
| 4 | Freetext (All but Authors): labelling |
| 5 | Freetext (All but Authors): labeling |
| 6 | Freetext (All but Authors): sign |
| 7 | Freetext (All but Authors): signs |
| 8 | Freetext (All but Authors): symbol |
| 9 | Freetext (All but Authors): symbols |
| 10 | Freetext (All but Authors): ticket |
| 11 | Freetext (All but Authors): tickets |
| 12 | Freetext (All but Authors): sticker |
| 13 | Freetext (All but Authors): stickers |
| 14 | Freetext (All but Authors): pack |
| 15 | Freetext (All but Authors): packs |
| 16 | Freetext (All but Authors): packaging |
| 17 | 2 OR 3 OR 4 OR 5 OR 6 OR 7 OR 8 OR 9 OR 10 OR 11 OR 12 OR 13 OR 14 OR 15 OR 16 |
| 18 | Freetext (All but Authors): food |
| 19 | Freetext (All but Authors): foods |
| 20 | Freetext (All but Authors): nutrition |
| 21 | Freetext (All but Authors): nutritional |
| 22 | Freetext (All but Authors): nutrient |
| 23 | Freetext (All but Authors): nutrients |
| 24 | Freetext (All but Authors): drink |
| 25 | Freetext (All but Authors): drinks |
| 26 | Freetext (All but Authors): beverage |
| 27 | Freetext (All but Authors): beverages |
| 28 | 18 OR 19 OR 20 OR 21 OR 22 OR 23 OR 24 OR 25 OR 26 OR 27 |
| 29 | 1 AND 17 AND 28 |
| 30 | 24 OR 25 OR 26 OR 27 |
| 31 | 1 AND 17 AND 30 |
| ClinicalTrials.gov | |
| food labeling OR food labelling OR food labels OR food label OR labeling of food OR labelling of food OR labeling of foods OR labelling of foods | |
| drink labeling OR drink labelling OR drink labels OR drink label OR labeling OF drink OR labelling of drink | |
| drinks labeling OR drinks labelling OR drinks labels OR drinks label OR labeling of drinks OR labelling or drinks | |
| beverage labeling OR beverage labelling OR beverage labels OR beverage label OR labeling of beverages OR labelling of beverages | |
| nutritional labeling OR nutritional labelling OR nutritional labels OR nutritional label | |
| nutrition labeling OR nutrition labelling OR nutrition labels OR nutrition label | |
| nutrient labeling OR nutrient labelling OR nutrient labels OR nutrient label | |
| calorie labeling OR calorie labelling OR calorie labels OR calorie label | |
| menu labeling OR menu labelling OR menu labels OR menu label | |
| point of purchase labeling OR point of purchase labelling OR point of purchase labels OR point of purchase label | |
| front of pack labeling OR front of pack labelling OR front of pack labels OR front of pack label | |
| (food OR foods OR drink OR drinks OR beverage OR beverages OR nutritional OR nutrition OR nutrient OR nutrients OR calorie OR menu OR purchase OR pack) AND (labeling OR labelling) | |
| (food OR foods OR drink OR drinks OR beverage OR beverages OR nutritional OR nutrition OR nutrient OR nutrients OR calorie OR menu OR purchase OR pack) AND (label OR labels) | |
| WHO International Clinical Trials Registry Platform (ICTRP) | |
| food labeling OR food labelling OR food labels OR food label OR labeling of food OR labelling of food OR labeling of foods OR labelling of foods | |
| drink labeling OR drink labelling OR drink labels OR drink label OR labeling OF drink OR labelling of drink | |
| drinks labeling OR drinks labelling OR drinks labels OR drinks label OR labeling of drinks OR labelling or drinks | |
| beverage labeling OR beverage labelling OR beverage labels OR beverage label OR labeling of beverages OR labelling of beverages | |
| nutritional labeling OR nutritional labelling OR nutritional labels OR nutritional label | |
| nutrition labeling OR nutrition labelling OR nutrition labels OR nutrition label | |
| nutrient labeling OR nutrient labelling OR nutrient labels OR nutrient label | |
| calorie labeling OR calorie labelling OR calorie labels OR calorie label | |
| menu labeling OR menu labelling OR menu labels OR menu label | |
| point of purchase labeling OR point of purchase labelling OR point of purchase labels OR point of purchase label | |
| front of pack labeling OR front of pack labelling OR front of pack labels OR front of pack label |
Data and analyses
Comparison 1. Labelling on menus vs no labelling in restaurants.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Energy (kcal) of food purchased | 3 | 1877 | Mean Difference (IV, Random, 95% CI) | ‐46.72 [‐78.35, ‐15.10] |
Comparison 2. Labelling on menus or placed on a range of food options vs no labelling in laboratory settings.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Energy (kcal) consumed during a meal | 8 | 1705 | Mean Difference (IV, Random, 95% CI) | ‐50.27 [‐104.41, 3.88] |
Comparison 3. Labelling on menus vs no labelling in laboratory settings (studies with a low risk of bias).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 3.1 Energy (kcal) consumed during a meal | 3 | 547 | Mean Difference (IV, Random, 95% CI) | ‐72.04 [‐137.84, ‐6.25] |
Comparison 4. Labelling of a single food or drink option vs no labelling in laboratory settings.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 4.1 Energy (kcal) consumption | 6 | 732 | Std. Mean Difference (IV, Random, 95% CI) | 0.05 [‐0.17, 0.27] |
Comparison 5. Labelling of a single food or drink option vs no labelling in laboratory settings (studies at low risk of bias).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 5.1 Energy (kcal) consumption | 2 | 400 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.06 [‐0.26, 0.15] |
Comparison 6. Consumption in laboratory settings: subgroup analysis by dietary restraint (studies providing a range of food options).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 6.1 Energy (kcal) consumed during a meal | 2 | 267 | Mean Difference (IV, Random, 95% CI) | 15.48 [‐20.08, 51.04] |
| 6.1.1 Restrained eaters | 2 | 129 | Mean Difference (IV, Random, 95% CI) | 20.87 [‐37.44, 79.18] |
| 6.1.2 Unrestrained eaters | 2 | 138 | Mean Difference (IV, Random, 95% CI) | 10.98 [‐38.85, 60.81] |
Comparison 7. Consumption in laboratory settings: subgroup analysis by dietary restraint (study providing a single food option).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 7.1 Energy (kcal) consumed during a snack | 1 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.17 [‐0.63, 0.28] | |
| 7.1.1 Restrained eaters | 1 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.44 [‐0.94, 0.05] | |
| 7.1.2 Urestrained eaters | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.03 [‐0.34, 0.39] |
Comparison 8. Consumption in laboratory settings: subgroup analysis by study country (studies providing a range of food options).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 8.1 Energy (kcal) consumed during a snack/meal | 8 | 1705 | Mean Difference (IV, Random, 95% CI) | ‐50.28 [‐104.42, 3.87] |
| 8.1.1 Studies conducted in the USA | 5 | 895 | Mean Difference (IV, Random, 95% CI) | ‐70.57 [‐167.65, 26.52] |
| 8.1.2 Studies conducted in other countries | 3 | 810 | Mean Difference (IV, Random, 95% CI) | ‐58.18 [‐107.15, ‐9.21] |
Comparison 9. Consumption in laboratory settings: subgroup analysis by study country (studies providing single food option).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 9.1 Energy (kcal) consumed during a snack/meal | 6 | 732 | Std. Mean Difference (IV, Random, 95% CI) | 0.05 [‐0.17, 0.27] |
| 9.1.1 Studies conducted in the USA | 4 | 459 | Std. Mean Difference (IV, Random, 95% CI) | 0.14 [‐0.17, 0.45] |
| 9.1.2 Studies conducted in other countries | 2 | 273 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.12 [‐0.36, 0.11] |
Comparison 10. Low fat (or energy) labelling vs no labelling on high‐energy foods.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 10.1 Energy (kcal) consumed during a snack/meal in laboratory settings | 5 | 718 | Std. Mean Difference (IV, Random, 95% CI) | 0.19 [‐0.14, 0.51] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Allan 2015.
| Study characteristics | ||
| Methods | Setting: one public coffee shop on a large academic hospital site, UK Design: quasi‐randomised controlled trial Recruitment: all coffee shop customers during the study period were participants Allocation to group: sign display (or absence thereof) was allocated by week using sealed envelopes |
|
| Participants | General customers (primarily healthcare workers and university staff) | |
| Interventions | Intervention: point‐of‐purchase signs indicating the energy content of every drink and snack (6 weeks) Control: no point‐of‐purchase signs (6 weeks) |
|
| Outcomes | Sales of high energy snacks and drinks (presented as a proportion) | |
| Notes | The intervention signs were displayed for 6 randomly allocated weeks over a 12‐week period. The final allocation sequence was: C‐C‐I‐C‐I‐I‐C‐C‐I‐C‐I‐I. The number of items purchased during the study period was 20,516. This study was funded by the Scottish Government's Chief Scientist's Office | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Sign display (or absence thereof) was randomised by week. 12 envelopes containing the instructions 'I' or 'C' were selected at random by an independent observer |
| Allocation concealment (selection bias) | Low risk | Envelopes were sealed (no other information was reported) |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Given that intervention and comparison were in the same coffee shop, it is possible that customers, particularly repeat customers, would have observed that there was an intervention during the different weeks (not blinded) |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The outcome (proportion of high energy drinks and snacks purchased) was objectively obtained from electronic data, so that blinding of outcome assessment was not applicable in this study |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All available data were collected and analysed |
| Selective reporting (reporting bias) | Low risk | All relevant outcomes reported in the Methods section are reported in the Results section |
| Other bias | Unclear risk | Sample sizes for the intervention and control weeks were not reported (i.e. it is not clear if participant outcomes vary across the weeks of the study) |
Balasubramanian 2002.
| Study characteristics | ||
| Methods | Setting: major grocery store chain in a large city, USA Design: interrupted time series Recruitment: existing sales data Allocation to intervention: naturally occurring pre‐ and post‐Nutrition Labelling Education Act (NLEA, 1990) legislation |
|
| Participants | General customers | |
| Interventions | Pre NLEA labelling: no enforced labelling (sample size not reported) NLEA* labelling: 'Nutrition Facts' panel on side or back of product with descriptors on front of pack (sample size not reported) *The NLEA regulations allowed a choice of several descriptions for a given nutrient such as 'low fat', 'reduced fat', 'light' Overall, 2684 item sales analysed |
|
| Outcomes | Sales performance of different categories of food with various types of labels (obtained from electronic sales data) | |
| Notes | This study was conducted from 14 September 1989 to 14 May 1997, with data collected on a weekly basis. "Sales transactions were aggregated across stores to derive the weekly category share for the healthy [products] associated with a given nutrient", and then the authors conducted a regression analysis. Data on 'low‐calorie' bottled juices, 'light' frozen entrées, and 'light' frozen dinners (i.e. items deemed to be 'calorie healthy' by the study authors) were extracted from this study. Information on funding was not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | The outcome (sales performance of different categories of labelled food) was objectively obtained from electronic data, so that blinding of outcome assessment was not applicable in this study |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Details of incomplete outcome data are not presented; the authors stated that "we tried to analyse the data within the constraints imposed by the pervasive problem of missing data" |
| Selective reporting (reporting bias) | Unclear risk | The Methods section does not specify which categories of food were to be included in the analysis |
| Was the intervention independent of other changes? | High risk | The authors noted that "our models do not incorporate explanatory variables such as price or other type of deals", suggesting that other changes could have occurred during the study period |
| Was the shape of the intervention effect pre‐specified? | Low risk | A regression model compared pre‐intervention and the post‐intervention phase, with an exact date of intervention reported. The authors provided a hypotheses specifying the expected effect of the intervention |
| Was the intervention unlikely to affect data collection? | Low risk | Sources and methods of data collection were the same before and after the intervention: electronic sales data |
| Other bias | High risk | Data from a number of stores belonging to one grocery chain were included, but it is unclear how the stores were selected. The introduction of legislation may have drawn additional attention to signposting throughout the city, not just the stores in question (thus possibly introducing a co‐intervention) |
Bergen 2006.
| Study characteristics | ||
| Methods | Setting: university campus buildings, USA Design: cluster‐randomised controlled trial (by vending machine) Recruitment: convenience sample Allocation to group: vending machines were randomly assigned but no information was reported on how this was achieved |
|
| Participants | University students and staff members | |
| Interventions | Intervention 1: brightly coloured (colour not specified) shelf label (2 inch × 5 inch, or 5 cm × 12.5 cm) stating: "0 calorie, 0 carbs" (on water, diet and regular fizzy drinks) (n = 3 vending machines) Intervention 2: brightly coloured shelf label stating "0 calorie, 0 carbs" plus a motivational poster encouraging the purchase of water and non‐energy‐containing soft drinks (n = 3 vending machines) Control: vending machines in similar location to the intervention machines selling similar but unlabelled drinks (n = 2 vending machines) |
|
| Outcomes | Sales of water, diet and regular fizzy drinks (soda) | |
| Notes | This study had a 2‐week baseline period, a 5‐week intervention period, and a 2‐week post‐intervention period. Results from intervention 2 did not meet inclusion criteria for this review so were not included. Data on sales of diet soda extracted from this study. This project was funded in part by the Dorothy Epstein Nutrition Fellows award | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported. The authors only stated that "the vending machines were randomly assigned to one of three conditions" |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Given that intervention and comparison machines were on the same university campus, it is possible that participants would have observed that there were different labels at different machines (not blinded) |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The outcome (mean number of drinks sold) was objectively obtained from electronic data, so that blinding of outcome assessment was not applicable in this study |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | It appears that all available data were collected and analysed: "the totals of each type of beverage sold and machine revenue were electronically tracked at each location at the end of each period" |
| Selective reporting (reporting bias) | Low risk | All relevant outcomes reported in the Methods section are reported in the Results section |
| Other bias | High risk | The mean number of drinks sold at baseline from comparison vending machines was substantially lower than in the intervention vending machine |
Bollinger 2011.
| Study characteristics | ||
| Methods | Setting: 222 New York City (NYC) Starbucks coffee shops before‐and‐after NYC energy labelling legislation and 94 comparison stores in Boston and Philadelphia, USA Design: controlled before‐and‐after study (treated as an ITS as data were collected from multiple time points before and after the intervention) Recruitment: convenience sample of Starbucks customers Allocation to group: naturally occurring NYC legislation with Boston and Philadelphia as comparisons |
|
| Participants | Customers at Starbucks coffee shops | |
| Interventions | Intervention: energy (kcal) information on menus and menu boards in a font and format that was at least as prominent as price (sample size not reported) Control: no energy information on menus and menu boards (sample size not reported) |
|
| Outcomes | Energy (kcal) from food and drinks per transaction, obtained from electronic sales data and 'Starbucks card' holder data | |
| Notes | The authors collected data for all transactions "for a period of time 3 months before and 11 months after energy posting commenced (i.e., January 1, 2008–February 28, 2009). There are over 100 million transactions in the data set." The data were analysed by the authors using regression analysis. Figure 1 in the paper also presents the time series data in graphical form for food and drinks separately. We extracted regression information on combined data for food and drinks. Information on funding was not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | The outcome (mean kcal per transaction) was objectively obtained from electronic data, so that blinding of outcome assessment was not applicable in this study |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Given that the authors observed "every transaction at Starbucks company stores in NYC from January 1, 2008 to February 28, 2009", it appears that the data set are complete |
| Selective reporting (reporting bias) | Low risk | All relevant outcomes reported in the Methods section are reported in the Results section |
| Was the intervention independent of other changes? | Low risk | The authors did not mention if any other historic events occurred during the study period, but they addressed other potentially confounding variables in regression analyses, including seasonality, day‐of‐week, holiday times, and climate. In addition, "to control for other factors affecting transactions, [the authors] also observe every transaction at Starbucks company stores in Boston and Philadelphia, where there was no calorie posting" |
| Was the shape of the intervention effect pre‐specified? | Low risk | A regression model compared pre‐intervention and the post‐intervention phase, with an exact date of intervention reported |
| Was the intervention unlikely to affect data collection? | Low risk | Sources and methods of data collection were the same before and after the intervention: electronic sales data |
| Other bias | Low risk | No other potential threats to validity identified |
Cavanagh 2014.
| Study characteristics | ||
| Methods | Setting: university campus, USA Design: randomised controlled trial Recruitment: recruited through an introductory psychology course; participants received a course credit for participation Allocation to groups: no information on sequence generation was reported (the authors only stated that they used a 2 × 2 × 3 between subjects design) |
|
| Participants | 188 female undergraduate students, overall mean age not reported; 70.7% were Caucasian (understood to be white), 15.4% African‐American and 13.9% Asian | |
| Interventions | Intervention 1: Kashi logo (a brand associated with 'healthful' eating) and a nutrition facts label with low energy (kcal) information (i.e. 130 kcal – the actual amount of kcal in each cookie) (n = 31) Intervention 2: Kashi logo and nutrition facts label with high energy (kcal) information (i.e. 260 kcal – twice the actual amount of kcal in each cookie) (n = 32) Control 1: Kashi logo and no nutrition facts label (n = 31) Intervention 3: Nabisco logo (a brand associated with 'unhealthful' eating) and nutrition facts label with low energy (kcal) information (i.e. 130 kcal – the actual amount of kcal in each cookie) (n = 31) Intervention 4: Nabisco logo and nutrition facts label with high energy (kcal) information (i.e. 260 kcal – twice the actual amount of kcal in each cookie) (n = 32) Control 2: Nabisco logo and no nutrition facts label (n = 31) |
|
| Outcomes | Mean grams consumed assessed by weighing the portion served and portion remaining | |
| Notes | Each participant was given three oatmeal and dark chocolate chip cookies, each of which was broken in half (i.e. all participants actually received a Kashi cookie that was 130 kcal, even though some were labelled as Nabisco cookies). In a post hoc analysis by the study authors, data were combined for intervention 1 and 3, and compared with combined control 1 and 2 (no label control groups). This is the data we have extracted for this review. Information on funding was not reported. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported. The authors only stated that "participants were ... randomly assigned to one of the two brand conditions and one of the three calorie information conditions before they arrived at the laboratory" |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | The participants were told that the purpose of the study was to examine taste‐perceptions in snack foods. Personnel are likely to have been aware of the different labels and which participants saw which labels |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The outcome (mean grams of cookies eaten) was objectively assessed, so that blinding of outcome assessment was not applicable in this study |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | It appears that all participants were included in the analyses |
| Selective reporting (reporting bias) | Low risk | All relevant outcomes reported in the Methods section are reported in the Results section. Additional post hoc analyses were also presented |
| Other bias | Low risk | No other potential threats to validity identified |
Chu 2009.
| Study characteristics | ||
| Methods | Setting: university dining centre, USA Design: interrupted time series Recruitment: convenience sample of customers Allocation to group: none, set periods for each intervention stage |
|
| Participants | Customers (largely college students) at a university dining centre | |
| Interventions | Pre‐intervention: no energy information; entrée descriptions posted on a 31 inch × 37 inch (79 cm × 94 cm) board for a 14‐day period (n = 13,951 entrées sold) Intervention: information on energy, serving size, fat (grams), protein (grams) and carbs (grams) on a menu board (5 inch × 3 inch – or 12.7 × 7.6 cm – board) (n = 14,199 entrees sold) Post‐intervention: no energy information; entrée descriptions posted on 8.5 inch × 11 inch (21.6 cm × 27.9 cm) floor stand as typically in cafeteria before study (n = 14,020 entrées sold) |
|
| Outcomes | Energy content of entrées sold per day (e.g. salads, soups, sandwiches, deli foods, pizza, and other hot entrées), assessed by electronically collected sales data, with nutritional content calculated using software | |
| Notes | 12 hot entrées were targeted in this study (not specified). It was conducted between 25 October and 8 December 2004. The study involved a 14‐day pre‐intervention period, a 14‐day intervention period, and a 13‐day postintervention period. Data points were reported for each day (41 days). The authors used 'piecewise' regression to "test differences in average daily energy content of entrées purchased by dining center patrons for pretreatment vs treatment period and treatment vs posttreatment period." Figure 1 in the paper also presents the time series data in graphical form. Information on funding was not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | The outcome (mean energy content of the entrées purchased) was objectively obtained from electronic data, so that blinding of outcome assessment was not applicable in this study |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There was no attrition |
| Selective reporting (reporting bias) | Low risk | All relevant outcomes reported in the Methods section are reported in the Results section |
| Was the intervention independent of other changes? | Low risk | The authors stated that "there were no other dining centres in the campus offering nutrition information, no campus‐wide nutrition education promoting the use of nutrition labels was active at the time of the study, and there was no known extraneous event occurring at about same time that could have changed purchasing behaviour." |
| Was the shape of the intervention effect pre‐specified? | Low risk | A regression model compared the pre‐intervention and post‐intervention phases. The authors provided a hypotheses specifying the expected effect of the intervention |
| Was the intervention unlikely to affect data collection? | Low risk | Sources and methods of data collection were the same before and after the intervention: electronic sales data |
| Other bias | Low risk | No other potential threats to validity identified |
Cioffi 2015.
| Study characteristics | ||
| Methods | Setting: 20 dining centres on a campus of Cornell University, USA Design: interrupted time series Recruitment: convenience sample of customers Allocation to group: none, set periods for intervention |
|
| Participants | Customers at a university dining centre | |
| Interventions | Pre‐labelling: no nutritional labelling of pre‐packaged "Fresh‐Take" meals and snacks (sample size not reported) Labelling: 'Nutrition Facts' labels on pre‐packaged meals and snacks, including information on serving size, energy, energy from fat, total fat, saturated fat, transfat, total cholesterol, sodium, total carbohydrates (including dietary fibre and sugars), and protein (sample size not reported) |
|
| Outcomes | Energy purchased per week assessed from electronically collected sales data | |
| Notes | 63 (unspecified) food items were labelled. This study was conducted for 3 semesters pre‐labelling (fall 2006, spring 2007 and fall 2007) and 3 semesters post‐labelling (spring 2008, fall 2008 and spring 2009). The final result was a 12‐week set of data for each semester (3 data points before and 3 date points after the intervention). "Mixed models were used to determine if there was a significant trend or a difference in the proportion of sales within the sample (the dependent variables) based on calories or fat." Figure 1 in the paper also presents the time series data in graphical form. The authors stated the study was supported by funds provided by DNS, Cornell University | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | The outcome (mean total kcal purchased) was objectively obtained from electronic data, so that blinding of outcome assessment was not applicable in this study |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Sales data for locations unavailable at second time point excluded and not accounted for. Target items not available at all locations for the whole period (18/63; 28%) were also excluded from the analysis. No information was provided as to whether excluded locations were similar to included locations in terms of customer base and sales |
| Selective reporting (reporting bias) | High risk | Outcome data from some target items that were not available at all locations for the whole study period were excluded from the analysis |
| Was the intervention independent of other changes? | High risk | The authors noted that "with data observed over many weeks and at various locations, it was impossible to control for all external factors or events that might have occurred over the entire length of the study." |
| Was the shape of the intervention effect pre‐specified? | Low risk | The point of analysis is the point of intervention. The study was exploratory with no predictions as to the direction of the effect |
| Was the intervention unlikely to affect data collection? | Low risk | Sources and methods of data collection were the same before and after the intervention: electronic sales data |
| Other bias | Low risk | The authors noted that their analysis was "weakened by the lack of information about the changes in purchasing patterns and sales data among all available foods (labelling, non‐labelling, pre‐packaged, or customised) before and after the nutrition labels were added to our sample" |
Crockett 2014.
| Study characteristics | ||
| Methods | Setting: a cinema in south London, UK Design: randomised controlled study Recruitment: on street recruitment by interviewers from a research agency Allocation to group: a random number generator was used to assign participants to condition |
|
| Participants | 325 participants were randomised, of whom 38 were excluded 51% were aged 18‐34 years, 36% were male, 37% were weight concerned, and 50% were overweight or obese |
|
| Interventions | Intervention 1: green 'low fat' label on the side of a bag of toffee or salted popcorn (n = 103) Intervention 2: red 'high fat' label on the side of a bag of toffee or salted popcorn (n = 96) The bags of popcorn were given to the participants as they entered the cinema Control: no label (n = 88) |
|
| Outcomes | Popcorn consumption as an absolute objective measure of energy (kcal) | |
| Notes | Six sets of results were presented by the study authors (3 treatment conditions × 2 types of popcorn). In our meta‐analysis, data were extracted for red 'high fat' label vs no label (combining data on salted and toffee popcorn consumption). We also extracted data on the 'low fat label' vs no label to evaluate potential harm, as the popcorn (both salted and toffee) served in this cinema was considered to be a high‐fat snack food. Subgroup analyses were conducted by the study authors to explore impact of weight concern, body weight and social deprivation on the effect of labels on consumption. The study was funded by a National Institute for Health Research Postdoctoral Fellowship award | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Pre‐determined random number sequence. Participants were given study numbers on the basis of the order in which they arrived at the cinema |
| Allocation concealment (selection bias) | Low risk | Researchers giving out the cards with the study numbers did not know the randomisation for that number. Another researcher then allocated the participants to a group based on the number on their card |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants were not aware of the true purpose of the study, nor that researchers were going to assess their consumption. Study personnel were aware of allocation of participants when explaining the study. However, one of three researchers explained the intervention to each of the three groups, minimising the opportunity for one researcher to treat participants differently according to group. Additionally, the same script was used by all personnel regardless of which group they were dealing with |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Assessors were aware of group allocation when assessing energy consumption, but food intake measurement appears to have been objective (weight of popcorn left over from a serving), so lack of blinding may not have influenced the results |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 325 participants were recruited, 38 (12%) of whom were excluded from the analyses of the effect of labelling on consumption due to multiple attendances (n = 14), not leaving their popcorn bags (n = 13) or for failure to consume any popcorn (n = 11) |
| Selective reporting (reporting bias) | Low risk | All relevant outcomes reported in the Methods section are reported in the Results section. A protocol was provided by the lead author and the primary outcome reported (relevant to this systematic review) and is presented in the published paper |
| Other bias | Low risk | No other potential threats to validity identified |
Dubbert 1984.
| Study characteristics | ||
| Methods | Setting: cafeteria located near a large medical centre and between a business area and middle‐class residential neighbourhood, USA Design: interrupted time series Recruitment: convenience sample; seated customers were approached and asked if they would be willing to answer a few questions about the foods they selected during peak Tuesday hours of 5.30‐7.30 pm Allocation to group: customer clusters of evening sessions, with each intervention having 3 sessions for a total of 15 sessions |
|
| Participants | Cafeteria customers | |
| Interventions | Baseline: no labels (sample size not reported) Intervention: 'Lower calorie selection' labels on bright green paper with a bright red dot on the upper right‐hand corner and placed near food items (sample size not reported) 'Baseline 2': no labels (sample size not reported) |
|
| Outcomes | The probability of choosing low energy food items (entrées, vegetables and salads) was assessed using electronic register sales data. Energy (kcal) content was calculated by the study authors using a caloric estimate list | |
| Notes | The authors stated that "purchases of more than 14,300 entrees, vegetables, and salads by 6,970 customers were unobtrusively monitored via the cash register inventory control system during 15 evening observations." (15 time points were reported). The authors stated that a "linear logistic regression analysis was used to compute chi‐square tests of the overall effects of labelling and food type (vegetable, salad, entrées) on the probability of choosing a low calorie food". Figure 1 in the paper also presents the time series data in graphical form. Information on funding was not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | The outcome (probability of purchasing low energy items from each of three food categories) was objectively obtained from electronic data, so that blinding of outcome assessment was not applicable in this study |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | It appears that all observations were included in the analysis |
| Selective reporting (reporting bias) | Low risk | All relevant outcomes reported in the Methods section are reported in the Results section |
| Was the intervention independent of other changes? | Unclear risk | No information was provided on confounding variables/historic events during the study period |
| Was the shape of the intervention effect pre‐specified? | Low risk | The point of analysis included the point of intervention |
| Was the intervention unlikely to affect data collection? | Low risk | The sources and methods of data collection were the same before and after the intervention: electronic data |
| Other bias | High risk | The data collection periods were very limited comprising 15 Tuesday evenings between 5.30 and 7.30 pm. Although the full opening hours and days for the cafeteria are not given, these periods may represent only a small proportion of the sales at the cafeteria |
Ebneter 2013.
| Study characteristics | ||
| Methods | Setting: university campus, USA Design: randomised controlled trial Recruitment: advertised as a market research study; participants received a course credit for participation Allocation to groups: no information on sequence generation was reported |
|
| Participants | 175 female undergraduate students of the University of Hawaii, mean age 20.86 (4.32) years. 71.8% were in the normal weight range, 14.4% were overweight, 6.3% were obese, and 7.5% were underweight (BMI ≤ 18.5 kg/m²) | |
| Interventions | Intervention 1: label stating "new colours of low fat M&M's 240 calories, 1.69 oz [28.3 g], ~55 M&M's" (n = 47) Control 1: label stating "new colour of low fat M&M's" with no energy information (n = 49) Intervention 2: label stating "new colours of regular M&M's, 240 calories per serving, 1.69 oz [28.3 g], ~55 M&M's" (n = 41) Control 2: label stating "new colours of regular M&M's" with no energy information (n = 38) |
|
| Outcomes | Energy (kcal) consumption assessed by weighing portion served and portion remaining and calculating energy contained in the portion consumed | |
| Notes | It is not clear how many sessions were conducted to complete this study, or where the study was conducted on campus. Data were extracted on intervention 2 vs control 2, and potential harms were considered by extracting data from control 1 (as M&M's were not actually low fat) vs control 2. Information on funding was not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported. The authors only stated that participants "were randomly assigned to one of four experimental conditions." |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants were told that the study was a taste‐rating exercise for market research and were thus unaware of the nature of the study. Personnel are likely to have been aware of the different labels and which participants saw which labels |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Not reported, but food intake measurement appears to have been objective (weight of M&M's left over from a serving), so lack of blinding may not have influenced the results |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Although 224 participants were recruited and participated, 175 (78%) were able to recall the label they saw and were included in the analysis. The rates of participants randomised to each group were not reported, so that attrition rates across groups are uncertain |
| Selective reporting (reporting bias) | Low risk | All relevant outcomes reported in the Methods section are reported in the Results section |
| Other bias | Low risk | No other potential threats to validity identified |
Ellison 2013.
| Study characteristics | ||
| Methods | Setting: a restaurant at Oklahoma State University campus, USA Design: randomised controlled study Recruitment: convenience sample of diners attending the restaurant Allocation to groups: the restaurant was split into three sections, each with a unique menu treatment. Upon arrival, a party of diners were randomly assigned to a table in one of the three sections |
|
| Participants | Restaurant customers (N = 138 observations); 70% were aged 18‐34.9 years, 18% were aged 35‐54.9 years, and 12% were older than 55; 56% were female; 63% were university students; 44% had an annual income less than USD 25,000, 40% had an income between USD 25,000 and 99,999 | |
| Interventions | Intervention 1: menu with energy information (kcal) in parentheses before each item's price (n = 54) Intervention 2: menu with energy information (kcal) in parentheses before each item's price plus a green, yellow, or red traffic light symbol indicating specific energy level ranges (n = 54) Control: menu with no nutritional information (n = 30) |
|
| Outcomes | Energy (kcal) purchased, calculated from receipts | |
| Notes | Diners could choose from 51 menu options including soups, salads, burgers, sandwiches, pasta, vegetarian dishes, meat dishes as well as deserts and drinks. Survey data were collected for 2 weeks during the 2010 fall semester. Data were combined for intervention 1 and intervention 2 and compared with the control. Information on funding was not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The authors only reported that "patrons were randomly assigned to one of three menu treatments" |
| Allocation concealment (selection bias) | Unclear risk | It is not clear who allocated the customers, or how allocation how participant allocation was concealed |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | The authors stated that the diners were unaware their dining choices had been recorded, however, personnel working in the restaurant would know which section of the restaurant the diners were randomised to |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Not reported, but outcome seems to have been objective (energy (kcal) purchased, calculated from receipts collected by researchers), so lack of blinding may not have influenced the results |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | It is not stated how many were randomised ‐ only that there were 138 observations |
| Selective reporting (reporting bias) | Low risk | All relevant outcomes reported in the Methods section are reported in the Results section |
| Other bias | Unclear risk | Data were collected during a short observation period (2 weeks) |
Ellison 2014a.
| Study characteristics | ||
| Methods | Setting: a restaurant at the Oklahoma State University campus, USA Design: randomised controlled trial Recruitment: convenience sample of diners attending the restaurant Allocation to groups: the restaurant was split into three sections, each with a unique menu treatment. Upon arrival, a party of diners were randomly assigned to a table in one of the three sections |
|
| Participants | Restaurant customers (N = 1532 usable observations); no participant characteristics were reported | |
| Interventions | Intervention 1: menu with energy information (kcal) in parentheses before each item's price (n = 469 usable observations) Intervention 2: menu with energy information (kcal) in parentheses before each item's price plus a green, yellow, or red traffic light symbol indicating specific energy level ranges (n = 591 usable observations) Control: menu with no nutritional information (n = 472 usable observations) |
|
| Outcomes | Energy (kcal) purchased, calculated from receipts | |
| Notes | This study also included a price manipulation experiment; we extracted data reported over the entire experiment, including all observations regardless of the price of the food. Diners could choose from 51 menu options including soups, salads, burgers, pasta and meat dishes. Data were collected over a 19‐week period (August to November 2010). Data were combined for intervention 1 and intervention 2 and compared with the control. Information on funding was not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | The authors only reported that "upon entering the restaurant, a lunch‐party was randomly assigned to one of three menu treatments." The authors noted that people assigned to the energy plus traffic light treatment group were in a section of the restaurant with booth seating, which some parties requested to have (so not all participants may have been randomised) |
| Allocation concealment (selection bias) | Unclear risk | It is not clear who allocated the customers, or how participant allocation was concealed |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | The authors stated that the restaurant patrons were unaware of the study, and that waiting staff were instructed to refrain from telling diners about the study. Personnel working in the restaurant would know what section of the restaurant the diners were randomised to |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Not reported, but outcome seems to have been objective (energy (kcal) purchased, calculated from receipts collected by researchers), so lack of blinding may not have influenced the results |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | The total number of eligible observations was not reported, only that there were 1532 'usable' observations |
| Selective reporting (reporting bias) | Low risk | All relevant outcomes reported in the Methods section are reported in the Results section |
| Other bias | Low risk | No other potential threats to validity identified |
Girz 2012 ‐ study 1.
| Study characteristics | ||
| Methods | Setting: university laboratory, Canada Design: randomised controlled study Recruitment: students enrolled in introductory psychology who consented to participation in the study Allocation to groups: a random number generator was used to assign participants to condition |
|
| Participants | Female psychology (university) students (n = 149). Mean age 19.11 (SD 1.82) years. 87 were restrained eaters and 62 were unrestrained eaters | |
| Interventions | Intervention 1: energy label on menu indicating low‐energy salad (600 kcal) and high‐energy pasta (1200 kcal) ‐ although both salad and pasta were 1200 kcal (n = 51) Intervention 2: energy label on menu indicating high‐energy salad (1200 kcal) and low‐energy pasta (600 kcal) ‐ although both salad and pasta were 1200 kcal (n = 47) Control: menu with no energy information (n = 49) |
|
| Outcomes | Energy (kcal) consumed. No details were reported as to how these measurements were made | |
| Notes | The duration of study was not reported. Subgroup analysis was conducted by the study authors to explore the impact of the intervention in more and less restrained eaters. The Restraint Scale was used to categorise participants as restrained eaters (scoring 15 or higher) or unrestrained eaters (scoring below 15). Data from intervention 1 and 2 were extracted for those who chose pasta or salad when it was mislabelled as '600 kcal', and analysed together vs control to measure potential harm. Information on funding was not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number generator used |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Participants were told that they would be rating a potential new menu item for a local restaurant. As this information was given to students in a psychology course by researchers, participants may have suspected that researchers were interested in some other outcome. Participants were debriefed to assess whether they guessed the nature of the study, but it is not clear what the outcome of this was |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information reported on blinding or how outcome was assessed |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data incomplete, numbers reported in one table suggest two participants lost from the analyses, although this is a small number so unlikely to bias results |
| Selective reporting (reporting bias) | Low risk | All relevant outcomes reported in the Methods section are reported in the Results section |
| Other bias | Low risk | No other potential threats to validity identified |
Girz 2012 ‐ study 2.
| Study characteristics | ||
| Methods | Setting: university laboratory, Canada Design: randomised controlled trial Recruitment: students enrolled in introductory psychology who consented to participation in the study Allocation to groups: a random number generator was used to assign participants to condition |
|
| Participants | Undergraduate students (n = 254) enrolled in the introductory psychology class. 138 (54%) females and 116 males (45.7%) Mean age of females was 18.69 (2.87) years and of males was 18.71 (1.79) years |
|
| Interventions | Intervention 1: energy label on menu indicating low‐energy salad (400 kcal) and high‐energy pasta (1200 kcal) or high‐energy salad (1200 kcal) and low‐energy pasta (400 kcal) ‐ although both salad and pasta were 1200 kcal (n = 128) Intervention 2: energy label on menu indicating high‐energy salad (1200 kcal) and high‐energy pasta (1200 kcal) plus information on the recommended daily energy intake of 2000 kcal for women and 2400 kcal for men, presented at the bottom of the menu (n = 60) Control: menu with no energy information (n = 66) |
|
| Outcomes | Energy consumed, with no detail as to how these measurements were made | |
| Notes | Duration of study was not reported. Subgroup analysis was conducted by the study authors to explore the impact of the intervention in more and less restrained eaters. The Restraint Scale was used to categorise participants as restrained eaters (scoring 15 or higher) or unrestrained eaters (scoring below 15). The effect of labelling on males and females also explored. Data were extracted for intervention 2 vs control. We did not include intervention 1 in this review as it involved mislabelling some of the foods, and data were not reported separately on consumption of foods that were accurately labelled and consumption of foods that were mislabelled. Information on study funding was not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number generator used |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Participants were told that they would be rating a potential new menu item for a local restaurant. As this information was given to students in a psychology course by researchers, participants may have suspected that researchers were interested in some other outcome. Participants were debriefed to assess whether they guessed the nature of the study, but it is not clear what the outcome of this was |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information reported on blinding or how outcome was assessed |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No attrition evident from tables; all participants accounted for |
| Selective reporting (reporting bias) | Low risk | All relevant outcomes reported in the Methods section are reported in the Results section |
| Other bias | Low risk | No other potential threats to validity identified |
Girz ongoing.
| Study characteristics | ||
| Methods | Setting: university laboratory, Canada Design: randomised controlled trial Recruitment: students enrolled in introductory psychology who consented to participation in the study Allocation to groups: a random number generator was used to assign participants to condition |
|
| Participants | Undergraduate psychology students (n = 49 included in the analysis) | |
| Interventions | Intervention: foods (pizza, soup) presented with energy labels (n = 24) Control: foods (pizza, soup) presented without energy labels (n = 25) |
|
| Outcomes | Energy (kcal) consumption | |
| Notes | Unpublished study; the authors provided study data. This study comprised six study groups with combinations of interventions in terms of labelling and ordering behaviour. Only two groups described above were eligible for inclusion in this review | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number generator used |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Full data provided for all those allocated in intervention and comparison |
| Selective reporting (reporting bias) | Unclear risk | Not reported |
| Other bias | Unclear risk | Not enough methodological information was reported to asses if there were other potential sources of bias |
Hammond 2013.
| Study characteristics | ||
| Methods | Setting: university, Canada Design: randomised controlled trial Recruitment: via newspaper, online and bus advertisements Allocation to group: no information on sequence generation was reported |
|
| Participants | 666 adults from Ontario (Canada), of whom 31 were excluded. Of those included, 36% were aged 18‐34 years, 49% were aged 35‐65 years, and 15% were aged over 65. 71% were white and 17% had no more than high school education, 64% had a college or university education and 19% had postgraduate level education | |
| Interventions | Intervention 1: menu with energy information (kcal) (n = 165) Intervention 2: menu with energy (kcal) content using a traffic light format, indicating whether the energy content was high (red), medium (orange) or low (green) (n = 156) Intervention 3: menu with energy (kcal), fat, salt, and sugar information using a traffic light format for each item (n = 152) Control: menu with no nutritional information (n = 162) |
|
| Outcomes | Consumption of energy (kcal), fat, salt and sugar assessed by weighing food served and food remaining after consumption and estimating energy and nutrients in what was consumed based on nutritional content of choices given by the retailer | |
| Notes | No detailed information regarding where the study took place (other than at a university), but it was a separate location from the fast food chain (Subway) where food was purchased on behalf of the participants. The study was conducted between November 2010 and June 2011. Data were combined for Interventions 1, 2 and 3, and compared with the control. This study was funded by a research grant from the Canadian Cancer Society Research Institute | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported. The authors only stated that "participants were randomised to receive one of four menus". One study menu was implemented on each evening that the study ran with the study menus being implemented on a recurring sequence from one to four. It is not stated whether participants were randomised to receive a particular menu (rather than to a particular evening) nor whether a random allocation sequence was used |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | The authors stated that "participants were blinded to the study condition." There was no information on blinding of personnel; however it seems unlikely that they could be blinded from the knowledge of which intervention was being implemented on a given evening |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Not reported, but outcome seems to have been objective (weighing food), so lack of blinding may not have influenced the results |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 31/666 (5%) participants were excluded from the analysis: 26 for not ordering a meal and 5 for missing data or for failing to meet the study protocol (excluded participants were not reported by treatment group). This low exclusion rate was unlikely to have affected the results |
| Selective reporting (reporting bias) | Low risk | All relevant outcomes reported in the Methods section are reported in the Results section. This study was registered with ClinicalTrials.gov (NCT01948752), and the outcomes reported are presented in the published paper |
| Other bias | Low risk | No other potential threats to validity identified |
Harnack 2008a.
| Study characteristics | ||
| Methods | Setting: community‐conference rooms at local hotels and the basement of a church (settings where the experiment took place, but not part of the experiment per se), USA Design: randomised controlled trial Recruitment: advertisements in local newspapers and flyers in community locations and in person at high schools Allocation to groups: no information on sequence generation was reported |
|
| Participants | Adolescents and adults recruited from suburban and urban populations in the local community including a high school whose students regularly ate fast food. Total number of participants recruited is not given although 605 participants completed the study procedures, of whom 301 were in the two study groups included in this review Age: 16‐25 years: 25% (n = 147); 26‐40 years: 19% (n = 115), 41‐60 years: 42% (n = 248); > 60 years: 14% (n = 84) Gender: male 41% (n = 241), female 59% (n = 353) Ethnicity: Hispanic/Latino 3% (n = 20); Non‐Hispanic/Latino, 97% (n = 567) |
|
| Interventions | Intervention 1: menu with energy (kcal) information on a bright yellow background plus recommendation of daily energy intake for men and women in a box on the right‐hand bottom corner of the menu (n = 151) Intervention 2: menu with no energy label, but with value pricing (the unit cost decreases as portion size increases) (n = 143) Intervention 3: menu with energy (kcal) information plus recommendation of daily energy intake (as above) and value pricing (n = 150) Control: menu with no energy labelling and no value pricing (n = 150) |
|
| Outcomes | Nutrient composition of meal purchased and consumed: absolute measure of the energy and nutritional content (fat, saturated fat, carbohydrate, protein, fibre, vitamin C and calcium) were calculated using a food composition table available from the McDonald's corporation in combination with the gram weight information for the amount of each food item selected and consumed | |
| Notes | Participants chose items available from a McDonalds lunch/dinner menu, and research staff drove to nearby McDonald's restaurant to purchase meals ordered by the participants. Study sessions were held on weekday and weekend evenings (4:50 pm to 7:30 pm) between October 2005 and April 2006. Subgroup analyses were conducted by the study authors for: men and women; those who reported seeing the intervention menus and those who did not; those who reported that nutrition was important to them and those who did not; and those who reported that price was important to them and those who did not. Information about randomisation and raw data for subgroup analyses requested, but no response from author. Data were extracted on intervention 1 vs control. Interventions 2 and 3, which involved a price component, were not eligible for inclusion in this review. The research was supported by a NIDDK grant | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported. The authors only stated that "a randomised controlled 2 × 2 factorial experiment was conducted...". |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants were blinded to the purpose of the study through a cover story. At the end they were questioned to ascertain whether they had noticed the menu manipulations and ascertained the purpose of the study. There is no indication as to whether personnel were blinded to allocated intervention |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Not reported, but outcome seems to have been objective (weighing food), so lack of blinding may not have influenced the results |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 605 participants are reported to have completed the study procedures, and of these, 11 (1.8%) were excluded from the analysis because "they knew before participating in the study that calories might be listed or price would be modified on the menu, or knew that they would not have to pay for their meal." No information was reported regarding the number of participants who dropped out in each group. This low exclusion rate was unlikely to have affected the results |
| Selective reporting (reporting bias) | Low risk | All relevant outcomes reported in the Methods section are reported in the Results section |
| Other bias | Low risk | No other potential threats to validity identified |
Holmes 2013.
| Study characteristics | ||
| Methods | Setting: restaurant at a country club, USA Design: interrupted time series design Recruitment: all children's meals sold during study period were included in the analysis Allocation to groups: none, set periods for intervention |
|
| Participants | Participants were those buying children's meals at the restaurant of a family‐oriented private club | |
| Interventions | Intervention 1: menu with energy (kcal) and fat (gram) information (sample size not reported). Intervention 2: healthy (apple) symbol on menu to denote 'healthier' choices (sample size not reported). Intervention 3: Nutrition Bargain Price (NBP) on menu. "The NBP equals the monetary price divided by a nutrition scaling factor (completeness score). By adjusting the price by nutritional quality, a more immediate indicator of the nutritional cost/reward of the combination, is provided." (sample size not reported) Control: no nutritional information on menu (sample size not reported) Overall, 1275 meals analysed |
|
| Outcomes | Changes in purchasing of energy and fat in children's meals as a consequence of nutritional labelling | |
| Notes | The study was conducted from October 2010 to May 2011 with two month pre‐intervention and two month post‐intervention periods. Patrons could buy combo meals, such as chicken and fries, mini cheese pizza and fruit salad, grilled cheese and potato chips, spaghetti and fresh fruit, hotdog and applesauce, or a corn dog with carrots and celery ‐ or an a la carte menu including a peanut butter and jelly sandwich, spaghetti with butter or a cheeseburger, with the following sides: pretzels or celery and peanut butter. The authors conducted regression analysis, with corrections to account for sales from repeat customers, and the likely correlation between such sales. Data were extracted on intervention 1 vs control. Interventions 2 and 3 were not eligible for inclusion in this review. Funding was received from the Virginia Tech College of Agriculture and Life Sciences | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | The outcome (total energy and fat selected by families) was objectively obtained from electronic data, so that blinding of outcome assessment was not applicable in this study |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | It appears that all observations were included in the analysis |
| Selective reporting (reporting bias) | Low risk | All relevant outcomes reported in the Methods section are reported in the Results section |
| Was the intervention independent of other changes? | Unclear risk | No information was provided on confounding variables/historic events during the study period |
| Was the shape of the intervention effect pre‐specified? | Low risk | The point of analysis included the point of intervention |
| Was the intervention unlikely to affect data collection? | Low risk | The sources and methods of data collection were the same before and after the intervention: electronic data |
| Other bias | Low risk | No other potential threats to validity identified |
James 2015.
| Study characteristics | ||
| Methods | Setting: 2 private dining rooms located within a university, USA Design: randomised controlled study Recruitment: via word of mouth, flyers placed around the university campus, university newsletter Allocation: no information on sequence generation was reported |
|
| Participants | Customers attending a dining room who were between 18 and 30 years of age. Demographic information for the total sample is not reported, but the percentage of females across the group varied between 54% and 57%, between 85% and 95% were white and between 74% and 79% were college students | |
| Interventions | Intervention 1: menu with energy (kcal) information plus information on recommended daily energy intake for women and men (n = 99) Intervention 2: each menu item presented with the number of minutes brisk walking required to burn off the energy in the item (n = 102) Control: menu with no energy information (n = 99) |
|
| Outcomes | Energy consumed during the meal assessed by weighing the food served before and after consumption | |
| Notes | All menus contained the same fast food and beverage options including burgers, salads, a chicken sandwich, chicken nuggets, chicken strips, french fries, desserts, condiments, water, and a choice of sodas. The study was conducted from January to June 2012. Data were extracted on Intervention 1 vs control. Intervention 2 was not eligible for inclusion in this review as it did not present data on nutrient content. The study was partly supported by a Graduate Senate grant from the university | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number generator used to generate stratified randomisation sequence (author communication) |
| Allocation concealment (selection bias) | Unclear risk | It is not clear whether the random sequence was concealed from personnel |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | The authors stated that participants were blinded to the study purpose. It is not stated whether the personnel would have known the group to which participants were randomised, but it would seem likely as they would see the menu given to each participant and so would be aware of how these varied |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Not reported, but outcome seems to have been objective (weighing food), so lack of blinding may not have influenced the results |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All 300 participants randomised completed the intervention and there is no indication of missing data for the outcome of interest in this review |
| Selective reporting (reporting bias) | Low risk | All relevant outcomes reported in the Methods section are reported in the Results section |
| Other bias | Low risk | No other potential threats to validity identified |
Kral 2002.
| Study characteristics | ||
| Methods | Setting: university campus laboratory, USA Design: quasi‐randomised controlled study Recruitment: campus newspaper Allocation to group: participants were assigned to groups based on the day of the week that they were available for their sessions |
|
| Participants | 40 healthy weight women aged 18‐32 years | |
| Interventions | Intervention: label (110 mm × 120 mm), which was colour‐coded according to the level of energy density; the label included information on level of energy density (low, medium, or high), the actual value of energy density (1.25 kcal/g, 1.50 kcal/g, or 1.75 kcal/g), and the weight (g) and energy content per serving (n = 20) Control: no labels (n = 20) |
|
| Outcomes | Daily energy intake from main entrées (breakfast, lunch and dinner); food was weighed to assess the consumption in grams and kJ | |
| Notes | Each meal included a main entrée, which was manipulated in energy density, and several low‐energy compulsory foods, which were standard in amount and type across all test sessions. Entrées consisted of an Apple Bake Crisp for breakfast, a pasta salad with yogurt dressing for lunch, and a pasta bake for dinner. The authors stated that "test sessions were scheduled on the same day of the week for four weeks." Subject group and condition of energy density (low, medium, high) were entered as fixed factors in the model, and subjects were treated as a random factor. In the meta‐analyses we entered the data assessing the effect of nutritional labelling on energy (kcal) consumption of a high‐energy meal. The study was supported by the National Institutes of Health grants | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quasi‐randomised. Participants were assigned to one of two groups (information or no‐information group) based on the day of the week that they were available for their sessions |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Thirteen subjects (65%) in the information group correctly discerned that the purpose of the study was to investigate the influence of energy density on the amount of food eaten – none guessed in control group |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Not reported, but outcome seems to have been objective (weighing food), so lack of blinding may not have influenced the results |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts during study, with 2 participants withdrawing before study started |
| Selective reporting (reporting bias) | Low risk | All relevant outcomes reported in the Methods section are reported in the Results section |
| Other bias | Low risk | No other potential threats to validity identified |
Platkin 2014.
| Study characteristics | ||
| Methods | Setting: university conference room, USA Design: randomised controlled trial Recruitment: on a university campus through announcements in lectures and through electronic bulletin boards Allocation to groups: randomised using a random number generator |
|
| Participants | Overweight or obese women (n = 62) Mean age: 21.87 (SD 3.03), range 18‐33 Ethnicity: 45.16% Hispanic or Latino; 27.42% Black/African American; 4.84% Caribbean non‐Hispanics; 8.06% Asian/Pacific Islander; 3.23% white Non‐Hispanic; 9.68% mixed race; 1.61% don't know/not sure Mean BMI: 28.42 kg/m² (SD 3.10) Education: 82% of all participants had a high school degree/equivalency, some college or a 2‐year college degree |
|
| Interventions | Intervention 1: menu with energy (kcal) information (n = 20) Intervention 2: menu with energy (kcal) information and with exercise equivalents (n = 20) Control: menu with no energy information (n = 22) |
|
| Outcomes | Energy (kcal) consumption during a meal; measured by weighing leftover food | |
| Notes | Food offered was fast food from Burger King. Participants attended twice for baseline and intervention meal. Subgroup analysis was conducted by the study author for restrained vs unrestrained eaters. A repeated measures analysis of variance was conducted. Data were combined from intervention 1 and 2 and compared with the control. This study was a thesis dissertation |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number generator used |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants were told that the study would assess factors influencing eating habits at fast food restaurants. Efforts were made to minimise contact between participants and thus the possibility of observation of differences in labelling provided. Researchers would have been aware of allocation when providing the menus |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Not reported, but outcome seems to have been objective (weighing food), so lack of blinding may not have influenced the results |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No evident attrition from cited participant numbers at both time points |
| Selective reporting (reporting bias) | Low risk | All relevant outcomes reported in the Methods section are reported in the Results section |
| Other bias | Low risk | No other potential threats to validity identified |
Roberto 2010.
| Study characteristics | ||
| Methods | Setting: university classroom in a building not related to eating, USA Design: randomised controlled trial Recruitment: word of mouth, newspaper advertisements and Internet postings Allocation to groups: a random number generator produced randomisation lists stratified by sex |
|
| Participants | Members of the general public in New Haven, Connecticut (n = 295) Female: 50% Mean age: 30.5 (SD 12.4) years Ethnicity: 54.6% white Education: 3.8% less than a high school education, 11.4% completed high school or general equivalency diploma (GED), 32.2% completed some college, 30.1% completed 4 years of college, and 22.5% had a graduate degree |
|
| Interventions | Intervention 1: menu with energy (kcal) information in column to right of menu item (n = 97, n =92 included in the analysis) Intervention 2: menu with energy (kcal) information in column to right of menu item plus information about recommended daily energy intake given at the top of the menu: ''The recommended daily caloric intake for an average adult is 2000 calories'' (n = 110, n = 103 included in the analysis) Control: menu with no energy information (n = 96, n = 92 included in the analysis) |
|
| Outcomes | Energy (kcal) consumed during a meal; objectively assessed using restaurant supplied information to assess energy content of meal ordered and then subtracting energy content of food remaining after the meal – where necessary weighing remaining portions | |
| Notes | Participants could choose items from menus from 2 restaurants (Au Bon Pain and a local, non‐chain restaurant). Menu items included all salads, dressings, sandwiches, wraps, and selected beverages and desserts from Au Bon Pain, and also mozzarella sticks, french fries, pizza, hamburgers, and cheesecake from the local restaurant. The study took place between June and August of 2009. Data were combined from intervention 1 and 2 and compared with the control. The study was funded by grants from the Rudd Foundation and the Robert Wood Johnson Foundation | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A randomisation list was used |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | The purpose of the study in investigating nutritional labelling was concealed from participants with a cover story. The different interventions were hidden from participants as the study took place in partitioned spaces. It is not clear if personnel were blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Not reported, but outcome seems to have been objective (weighing food), so lack of blinding may not have influenced the results |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low dropout with reasons given: 6/96 (6%) lost to follow‐up in no energy label group; 4/97 (4%) lost to follow‐up in energy label group; 9/110 (8%) lost to follow‐up in energy + information group. Of 303 randomised participants, 295 (97%) were included in the analysis |
| Selective reporting (reporting bias) | Low risk | All relevant outcomes reported in the Methods section are reported in the Results section |
| Other bias | Low risk | No other potential threats to validity identified |
Roberto 2012.
| Study characteristics | ||
| Methods | Setting: university laboratory 'not affiliated with eating or weight research', USA Design: randomised controlled trial Recruitment: via flyers, word of mouth, and craigslist.com postings Allocation to groups: randomly generated allocation sequence, stratified by gender |
|
| Participants | Members of the general public (n = 243) Mean age 26 (SD 10) years, range 18‐72 years, 63% female, 59% Caucasian (understood to be white), 22% Asian, 11% African‐American, 4% Hispanic, and 4% reported 'other' Mean BMI 23.2 (SD 4.52), 22% of sample obese Education: 42% had attended some college, 27% had a four year college degree, 22% had a graduate degree, 4% had a 2‐year college degree, 4% had a high school/GED degree only and 1% did not complete high school |
|
| Interventions | Intervention 1: front‐of‐package standard smart choices label including a green check mark, the statement 'Smart Choices Program Guiding Food Choices,' and the information: "120 calories per serving and 11 servings per package" (n = 76 analysed) Intervention 2: front‐of‐package modified Smart Choices logo which included a green check mark, the statement 'Smart Choices Program Guiding Food Choices,' and the following information: "120 calories per 3/4 cup serving and 11 servings per package" (n = 71 analysed) Control: no label (n = 69 analysed) |
|
| Outcomes | Grams of cereal and milk consumed; measured by weighing each participant's cereal box | |
| Notes | The participants were offered a breakfast cereal during the experiment. The study was conducted between August 2007 and August 2008. Data were combined from intervention 1 and 2 and compared with the control. The study was supported in part by funding from the Rudd Foundation | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number generator was used |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants were told they would be taking part in a focus group about the cereal in front of them and would have a chance to eat the cereal (so blinded to the purpose of the study), but it is unclear whether personnel were blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Not reported, but outcome seems to have been objective (weighing food), so lack of blinding may not have influenced the results |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 27/243 (11%) participants were excluded because they correctly identified that the study was testing the influence of nutrition information on their perceptions and/or behaviour. Data were not reported by group although the authors stated that the "proportion of individuals excluded did not differ significantly across study conditions (p = .451)" |
| Selective reporting (reporting bias) | Low risk | All relevant outcomes reported in the Methods section are reported in the Results section |
| Other bias | Low risk | No other potential threats to validity identified |
Temple 2010.
| Study characteristics | ||
| Methods | Setting: university laboratory, USA Design: randomised controlled trial Recruitment: flyers posted on campuses Allocation to groups: no information on sequence generation was reported |
|
| Participants | 47 participants, mean age 29.9 (SD 1.5) years, 23 males and 24 females, mean BMI 25.9 (SD 0.6) kg/m², 91% had completed some college education | |
| Interventions | Intervention: nutritional labels on foods based on US Department of Agriculture format (n = 23) Control: no label on food (n = 24) All participants also watched videos, either on how to read nutritional labels or about the organic food movement |
|
| Outcomes | Energy (kcal) consumed during lunch; measured by weighing leftover food | |
| Notes | Participants were offered a buffet lunch (small salad bar, a sandwich bar, and side items including chips (crisps), chocolate bars, yogurt, fruit, water, soft drinks, white and chocolate milk, and juice). The study (involving single lunch sessions) was conducted between May and August 2009. Study data were obtained from the authors. The authors also conducted subgroup analyses for males and females. The study was funded by start‐up funds through the university | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported. The authors only stated that "participants were randomly assigned to one of two video groups ... and one of two labelling conditions." |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants were told the purpose of the study was to explore the effect of labels and a video on consumption (so blinded to the purpose of the study). No information given to suggest whether or not personnel were blind to the intervention that participants received |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Not reported, but outcome seems to have been objective (weighing food), so lack of blinding may not have influenced the results |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No information to indicate that there was any data missing among those recruited |
| Selective reporting (reporting bias) | Low risk | All relevant outcomes reported in the Methods section are reported in the Results section |
| Other bias | Low risk | No other potential threats to validity identified |
VanEpps 2016.
| Study characteristics | ||
| Methods | Setting: a large health care company, USA Design: randomised controlled trial Recruitment: e‐mail to randomly selected employees Allocation to groups: no information on sequence generation was reported |
|
| Participants | 249 participants (employees) who placed 901 orders, mean age 40.6 (SD 11.09) years, 60% female, mean BMI 27.5 (SD 6.19) kg/m², 81% white | |
| Interventions | Intervention 1: traffic light labels on lunch menu items based on US Department of Agriculture guideline (n = 42) Intervention 2: energy (kcal) content on lunch menu items (n = 38) Intervention 3: energy (kcal) content and traffic light labels on lunch menu items (n = 46) Control: no label on lunch menu items (n = 123) |
|
| Outcomes | Energy (kcal) ordered during lunch | |
| Notes | Participants were required to order an online meal for which they received a USD 3 discount on each lunch ordered throughout the study (up to 3 lunch orders per week). There were 13 different meal options including sandwiches with side dishes, wraps with side dishes, and entrée‐sized salads, as well as drinks (30 different options including sodas, juices, teas and water), snacks, and desserts (e.g. chips, fresh fruit, brownies). The study was conducted over 4 weeks. The authors also conducted regression analysis by BMI, males and females, and for 'non‐dieting' and 'dieting' individuals. Data were extracted for interventions 2 and 3 (combined) vs control. Intervention 1 was not eligible for inclusion in this review as it did not present data on nutrient content. Additional study data were obtained from the authors. The study was funded by one of the author's personal research funds | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported. The authors only stated that "we randomly assigned participants to one of these four menu conditions" |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Not reported, but outcome was objective (food purchased), so lack of blinding may not have influenced the results |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data were reported for all participants randomised (those who placed at least one order appear to have been randomised) |
| Selective reporting (reporting bias) | Low risk | All relevant outcomes reported in the Methods section are reported in the Results section |
| Other bias | Low risk | Participants could make more than one order, so each outcome is not necessarily independent, which may inflate the SE estimate. The data received from the authors were adjusted for covariates |
Vermeer 2011.
| Study characteristics | ||
| Methods | Setting: cinema, the Netherlands Design: quasi‐randomised controlled trial Recruitment: announcements in local newspapers, radio, and on the Internet. Other recruitment methods included posting flyers in mailboxes and handing out flyers Allocation to group: allocated according to evening available |
|
| Participants | 89 participants. Mean age of 50.44 (SD 12.35), 26.4% were male, 33% were overweight or obese, 50.5% had moderate educational level and 41.4% had high | |
| Interventions | Intervention: large poster with portion size and caloric guidelines for daily amounts (GDA) information on soft drinks (n = 48) Control: no label; different portion sizes for soft drinks were displayed indicating only the amount of millilitres that each cup contained (n = 41) |
|
| Outcomes | Soft drink consumed (mL) during film was calculated by electronic weighing of leftovers | |
| Notes | Participants could choose between five portion sizes (200 mL, 250 mL, 400 mL, 500 mL and 750 mL cups). The study took place on two subsequent evenings during which participants could order free soft drinks. Authors were contacted to request information about the energy content of the soft drinks, but this information was not forthcoming. Information on study funding was not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Participants could select which of the two evenings they wanted to take part. On one of the evenings the intervention was implemented and the other evening was the control, but the participants were unaware of this when they chose when to participate |
| Allocation concealment (selection bias) | High risk | No allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Potential participants were told that a marketing study was conducted into consumers' attitudes towards cinemas (so blinded to the purpose of the study). Personnel would have been aware of which participants were in the intervention and comparison groups |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Not reported, but outcome seems to have been objective (weighing food), so lack of blinding may not have influenced the results |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No attrition apparent |
| Selective reporting (reporting bias) | Low risk | All relevant outcomes reported in the Methods section are reported in the Results section |
| Other bias | High risk | Data were collected on only two subsequent evenings, and the sample size is relatively small |
Wansink 2006 ‐ study 1.
| Study characteristics | ||
| Methods | Setting: university campus, USA Design: quasi‐randomised controlled trial Recruitment: new students and their families visiting a display as part of a university open house were approached by a research assistant asking them to take part |
|
| Participants | 269 adults aged over 18 participated. Although further demographic information were collected, no information is given about sample demographics | |
| Interventions | Intervention: glass container labelled 'new low fat M&M's' (sample size not reported) Control: glass container labelled 'new colours of regular M&M's' (sample size not reported) |
|
| Outcomes | Energy (kcal) consumed; assessed by weighing the serving of M&M's that participants had served themselves (97.3% were observed to eat all that they had served themselves) | |
| Notes | Participants helped themselves freely to M&M's in labelled glass containers. The study was conducted over 2 days. The authors stated that "no industry or government agency funds supported this project" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quasi‐randomisation based on the order in which people attended the open house |
| Allocation concealment (selection bias) | High risk | No allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | It is unclear whether participants would have been aware of the other group as both groups seem to have been running at the same time. The M&M's were unusual colours (gold, teal, purple and white), which could have affected consumption behaviour. Research assistants administering the study are likely to have been aware of the different interventions and who was receiving each |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Not reported, but outcome seems to have been objective (weighing M&M's), so lack of blinding may not have influenced the results |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data seem to have been collected from all those who agreed to take part |
| Selective reporting (reporting bias) | Low risk | All relevant outcomes reported in the Methods section are reported in the Results section |
| Other bias | Low risk | No other potential threats to validity identified |
Wansink 2006 ‐ study 3.
| Study characteristics | ||
| Methods | Setting: theatre located on a university campus, USA Design: quasi‐randomised controlled trial Recruitment: university students and staff at a large university campus recruited to be part of a study in which they would evaluate a pilot episode for a television show |
|
| Participants | 179 participants; 49% males, mean age 28.7 years, mean BMI of 25.1 kg/m² with 110 normal‐weight and 69 in the overweight group | |
| Interventions | Intervention: each participant received 160 grams containing 640 kcal of granola in ziplock bags that had an 'attractive' 3.25 × 4 inch (8.26 cm × 10.2 cm) colour label: "Low‐Fat Rocky Mountain Granola" (sample size not reported) Control: as above but the granola was described as "Regular Rocky Mountain Granola". Below this, the label indicated, "Contains 1 Serving" or "Contains 2 Servings", or it provided no serving size information (sample size not reported) |
|
| Outcomes | Energy (kcal) consumed; assessed by weighing of leftovers of granola | |
| Notes | The study was conducted over 10 sessions that lasted from 3:30 to 5:00 pm on each of 10 days (Tuesdays and Thursdays for 5 non‐consecutive weeks). The authors stated that "no industry or government agency funds supported this project" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | By day of the week |
| Allocation concealment (selection bias) | High risk | No allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | The study was also described as evaluating a pilot episode for a television show so there was a low risk of participants being aware of manipulation. Personnel are likely to have been aware of the different interventions and who was receiving each |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Not reported, but outcome seems to have been objective (weighing granola bag), so lack of blinding may not have influenced the results |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 31/210 (15%) participants 'randomised' were not included in the analysis. Participants were excluded for not staying until the end of the show (n = 7), refusing to eat granola because of dietary restrictions or political principles (n = 4), spilling their granola on the floor (n = 3), emptying their granola bags into their pockets (n = 3), and failing to provide height and weight information (n = 14). Exclusions by treatment group were not reported |
| Selective reporting (reporting bias) | Low risk | All relevant outcomes reported in the Methods section are reported in the Results section |
| Other bias | Unclear risk | Not enough methodological information was reported to asses if there were other potential sources of bias |
BMI: body mass index; SD: standard deviation.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Albright 1990 | Intervention: included a leaflet, the effect of which could not be isolated from the labelling intervention |
| Aron 1995 | Study design: controlled before‐and‐after study that did not meet EPOC requirements for implementation in at least 2 intervention and 2 control sites Outcome: purchasing not objectively assessed; participant self‐report used. Consumption only objectively assessed for intervention group, not for control group |
| Babio 2014 | Study design: no no‐label control group; evaluates 2 different types of nutritional labelling schemes |
| Berning 2011 | Study design: controlled before‐and‐after study that did not meet EPOC requirements for implementation in at least 2 intervention and 2 control sites |
| Bleich 2014 | Intervention: 4different types of nutritional labels which were not specific to a particular product but sugar sweetened beverages generally Control: no no‐label control group |
| Bucher 2015 | Outcome: no purchasing or consumption measured (portion size decisions) |
| Callaghan 2010 | Intervention: labelling did not give information about specific nutrient content |
| Cantor 2015 | Study design: controlled before‐and‐after study that did not meet EPOC requirements for implementation in at least 2 intervention and 2 control sites |
| Cawley 2015 | Intervention: guiding stars labels that do not provide information about content of specific nutrients |
| Chu 2012 | Study design: a quasi‐experimental single group, ITS study that did not meet the EPOC criteria of at least 3 data points before and after the intervention |
| Chu 2014 | Study design: a quasi‐experimental single group, ITS study that did not meet the EPOC criteria of at least 3 data points before and after the intervention Control: there was no no‐labelling comparison as a nutrition facts label was already in operation in the cafeteria |
| Dingman 2015 | Intervention: consisted of 3 strategies, not just labelling alone (nutrition information, interpretive signage, and a promotional email) |
| Ducrot 2016 | Outcome: buying intention (virtual web‐based supermarket where virtual purchases were evaluated) |
| Dumanovsky 2011 | Study design: did not meet EPOC criteria for inclusion as an interrupted time series study |
| Elbel 2011 | Study design: controlled before‐and‐after study that did not meet EPOC requirements for implementation in at least 2 intervention and 2 control sites |
| Elbel 2013a | Study design: controlled before‐and‐after study that did not meet EPOC requirements for implementation in at least 2 intervention and 2 control sites |
| Elbel 2013b | Study design: experimental design testing the effects of labelling and taxation Intervention: label did not provide information about content of specific nutrients or energy |
| Ellison 2014 | Study design: did not meet EPOC criteria for ITS: experiments 1 and 2: ITS design, only analysed using t‐tests/multiple regression controlling for background variables (e.g. time of day), but did not account for secular trends/autocorrelation (no data were presented in a graph which would allow re‐analysis) |
| Engbers 2006 | Study design: controlled before‐and‐after study that did not meet EPOC requirements for implementation in at least 2 intervention and 2 control sites Intervention: no attempt to separate out the impact of calorie information and need for physical activity. Outcome: self‐reported consumption of different foods and nutrients |
| Finkelstein 2011 | Study design: controlled before‐and‐after study that did not meet EPOC requirements for implementation in at least 2 intervention and 2 control sites |
| Freedman 2009 | Study design: ITS study that did not meet the EPOC criteria of at least 3 data points before and after the intervention |
| Giesen 2011 | Intervention: this study assessed different prices and calorie information treatment conditions, so that the impact of labelling alone could not be determined |
| Gittelsohn 2013 | Intervention: multi‐component intervention of which nutritional labelling was only one part Outcome: self‐reported outcomes that were not objectively measured (participants were asked about foods and the number of times they had had them in the past 30 days) |
| Gomez 2015 | Intervention: hard‐to‐read vs easy‐to‐read nutrition labelling conditions Control: no no‐label control group Outcome: only purchase intention was assessed |
| Graham 2017 | Outcome: participants did not pay money for items 'chosen' in the 'laboratory' grocery store |
| Hassan 2010 | Outcome: self‐reported choice of food assessed |
| Helfer 2014 | Study design: no no‐label control (4 different types of nutritional labels were assessed) Outcome: only purchase intention was assessed |
| Hobin 2015 | Intervention: evaluated a 'guiding stars' system (foods labelled with different star levels: 0 vs 1 vs 2 vs 3 stars) |
| Hoerr 1993 | Study design: did not meet EPOC criteria for an ITS study |
| Holmes 2011 | Outcome: self‐reported measure of purchasing |
| Kiesel 2013 | Study design: did not meet EPOC criteria for inclusion as a controlled before‐and‐after study |
| Kocken 2012 | Intervention: not possible to isolate the effect of labelling from other interventions |
| Koenigstorfer 2014 | Su: no no‐label control (study 1 and 2); evaluates 2 different types of nutritional labelling schemes |
| Krieger 2013 | Study design: pre‐post design that did not meet EPOC criteria for inclusion as an ITS study |
| Lassen 2014 | Study design: controlled pre‐post study with one intervention site and one control site Intervention: keyhole labelling that did not give information about the content of specific nutrients or energy |
| Mathios 2000 | Study design: the study did not meet EPOC criteria for inclusion as an ITS study |
| McNeill 2014 | Outcome: outcome appears to be hypothetical choice in different scenarios using an on‐line system (authors were contacted for more details, but no response provided) |
| NCT01604954 | Potentially relevant study but not enough information in registry to assess. The study completion date is April 2015, but no associated publications are available. |
| NCT02546505 | Outcome: 'At the end of the shopping session, the respondents proceed to the cashier but don't actually pay for their purchases.' |
| Nikolaou 2014a | Study design: pre‐post study not meeting EPOC criteria for inclusion as a controlled before‐and‐after study |
| Nikolaou 2014b | Study design: pre‐post study not meeting EPOC criteria for inclusion as an interrupted time series study |
| Nikolaou 2016 | Study design: did not meet EPOC criteria for inclusion as an interrupted time series study (not three pre intervention and three post‐intervention periods) |
| Pulos 2010 | Study design: pre‐post study that did not meet the EPOC criteria of at least 2 intervention and 2 control sites |
| Reale 2016 | Study design: repeated measures design (all participant's received the control menu first followed by the experimental conditions which were presented in a randomised order) Outcome: only intention to purchase assessed |
| Sacks 2009 | Study design: pre‐post study that did not meet EPOC criteria for inclusion as an ITS study |
| Sacks 2011 | Study design: pre‐post study that did not meet EPOC criteria for inclusion as a controlled before‐and‐after study |
| Sato 2013 | Study design: pre‐post study that did not meet EPOC criteria for inclusion as an ITS study |
| Schmitz 1986 | Study design: pre‐post study that did not meet EPOC criteria for inclusion as an ITS study |
| Schucker 1992 | Study design: study that did not meet EPOC criteria for inclusion as an ITS study or as a controlled before‐and‐after study |
| Schwartz 2012 | Intervention: the effect of labels could not be isolated from other interventions |
| Seward 2016 | Intervention: labels did not meet inclusion criteria (coloured with no other information) |
| Sharma 2011 | Intervention: healthy menu items were presented on the menu alongside regular items but were labelled with a 'heart‐healthy' symbol only |
| Stutts 2011 | Outcome: self‐reported choice and consumption |
| Sutherland 2010 | Intervention: label consisted of stars which give an indication of overall weighted content of different nutrients based on a summed score |
| Temple 2011a | Intervention: the labelling intervention was associated with a 'taxing' intervention, so that the effect of labelling alone could not be isolated |
| Temple 2011b | Intervention: labels did not provide information about actual nutritional content but were coloured to represent whether the foods were more or less healthy |
| Thorndike 2014 | Intervention: labels did not contain information about specific nutrients or energy and their content in the product |
| Thorndike 2015 | Intervention: all participants were exposed to traffic light labels; intervention group received financial incentives and control group did not |
| Trudel 2015 | Intervention: no no‐label control: red vs green traffic lights was the intervention (study 4) Outcome: rating the health quality of food (study 1 to 3) |
| Vadiveloo 2011 | Study design: controlled before‐and‐after study that did not meet EPOC requirements for implementation in at least 2 intervention and 2 control sites (linked to Elbel 2011) |
| Volkova 2014 | Intervention: no no‐label control; evaluates 2 different types of nutritional labelling schemes |
| Vyth 2011 | Intervention: choices logo provided but information on specific nutrients were not provided |
| Wang 2016 | Study design: a longitudinal analysis. The authors state that they presented weekly retail sales data and product feature records from 2001 to 2011, in order to analyse supply‐side changes in the market for margarine and spreads corresponding to implementation of the 2006 rule (although there is no clear graph showing sales through time that could be used as ITS data – just price or market share) |
| Wardle 1994 | Outcome: food preferences |
| Webb 2011 | Study design: controlled before‐and‐after study but objective purchasing data (electronic till data) are only available for 1 intervention and 1 control store (so did not meet EPOC criteria with at least 2 intervention sites and 2 control sites) |
| Whitaker 1994 | Intervention: intervention schools had both low‐fat labelling and parental information pamphlets; the effects of the 2 parts of the intervention could not be isolated |
EPOC: Cpchrane Effective Practice and Organisation of Care group; ITS: interrupted time series.
Characteristics of ongoing studies [ordered by study ID]
ACTRN12614000964617.
| Study name | The effects of four front‐of‐pack labelling schemes compared to standard Nutrition Information Panel, on mean nutrient profiling score of food purchases among the adult Australian consumers: a randomised trial |
| Methods | Randomised controlled trial |
| Participants |
|
| Interventions | The labelling schemes that will be tested in the study are:
|
| Outcomes | Healthiness of food purchases as evaluated by the mean nutrient profile score of all food and beverage products purchased over the four‐week intervention period. Mean nutrient profiling score will be calculated using the Food Standards Australia New Zealand (FSANZ) nutrient profiling standard. Food purchase information is collected via electronic records (participants will be asked to scan barcodes of purchased items and take photos of the till receipts using the smartphone app and send to the study investigators. The app will then transmit the data to study database. Participants will also be asked to send in the hard copies of their till receipts in a reply‐paid envelop provided by the study. Food purchase information will later be collated from both electronic and paper sources for analysis. |
| Starting date | 15 September 2014 |
| Contact information | Prof Bruce Neal The George Insitute for Global Health, Level 10, King George V Building, 83‐117 Missenden Rd, Camperdown NSW 2050 Australia Phone +61 299934558 |
| Notes | The study intervention includes 4 different front of pack nutrition labelling schemes that will be shown to study participants via a smartphone application. |
Differences between protocol and review
Title: We altered the title to include non‐alcoholic drinks as well as food because relevant studies rarely evaluated food and drink separately. As a consequence, it was not possible to isolate the effect of labelling for these different products and to restrict the inclusion criteria to food only would have let to the exclusion of several potentially relevant studies. We also altered our inclusion criteria to reflect this change.
Background: we made small changes to the Background to bring the review up‐to‐date, including the addition of more recent references, notably Rayner 2013.
Types of studies: the protocol and review state, "Based on Cochrane recommendations, [ITS] studies that reported only a simple pre and post‐intervention comparisons were not included in the review analysis unless a valid justification for their inclusion could be made or a re‐analysis of the data could enable data from multiple observations in the pre and post periods to be analysed using repeated measures methods" (Cochrane Public Health Review Group 2010; EPOC 2015). We added the following sentence to clarify that studies that either presented appropriate data in graphs, or did not present data in graphs, but did present other types of statistical tests (i.e. other than t‐tests) could be eligible for inclusion: "Authors had to present these data within a graph and/or at the very least analyse them using regression analysis, preferably using segmented regression."
Types of interventions: the protocol stated that a label could be compared to a group in which participants see the same food product presented without a label or with an incomplete label. As we found a number of papers in the search that compared two or more types of labels, we added the following text for clarity: "As noted above, the intervention labelling group had to be compared with a no‐labelling (or incomplete) control group. Thus, we excluded studies that only compared two or more different types of labelling schemes without a control group."
Primary outcomes: the protocol specified purchasing or consumption of foods only, but we also included studies that evaluated the effect of labelling on purchasing of non‐alcoholic drinks (for the reasons stated above). We also added the following sentence to this section of the review for clarity: "We excluded studies that evaluated intention to purchase or intention to consume without an objectively assessed measure of the behaviour."
We also clarified that purchasing had to involve payment with money, as we found some studies in the evidence base that evaluated choices in the settings of interest (e.g. grocery stores), but did not involve purchasing per se.
Food consumption: the protocol specified that where the food consumed was heterogeneous (e.g. a meal comprising various elements with different nutritional content), the amount of each separate element consumed within the meal needed to be assessed for the study to be included. However, this approach would have excluded a number of otherwise good‐quality studies. Thus, we ended up including studies that evaluated multiple food elements and consumption by weighing the meal before and after consumption.
Search methods for identification of studies: we also searched for trials in progress, which was an additional source not specified in the study protocol.
Selection of studies: the protocol stated that "[w]here studies are excluded only on the basis of an incomplete label, the details of these studies will be tabulated separately." We did not identify any incomplete labels, so there was no need to tabulate any details separately.
Data extraction and management: we planned to extract data on any measures relating to the process of implementing the intervention, including data on cost of implementing the intervention in any of the included studies. We did not do this in the final review due to lack of data.
Assessment of risk of bias in included studies:
We added detection bias to this section, which we had omitted. We also removed the risk of bias domain of outcome measurement assessment, as objective outcome measurement was an inclusion criterion for the review. Moreover, we added information to the review regarding how we determined an overall assessment of risk of bias for each study (which we had not specified in the protocol).
The protocol specified that we would use the Quality Assessment Tool for Quantitative Studies (EPHPP 2009) to estimate the risk of bias in controlled before‐and‐after studies and to compare the risk between different types of studies. We did not end up using this tool because we did not identify any eligible controlled before‐and‐after studies.
In addition to the quality assessment strategies specified in the protocol, we conducted a GRADE assessment of the evidence for each outcome according to Cochrane guidance.
Measures of treatment effect: we added the following two paragraphs to the review, which we did not present in the protocol. We added the first paragraph to help quantify the results, and the second because many of the ITS studies were of poor quality, so we considered re‐analysis of the data to be of limited value:
"In order to re‐express effect sizes using a more familiar metric, we calculated the percentage reduction in energy consumed over a typical meal, using an average of 600 kcal as a baseline. This amount was based on mean daily energy intake across the UK population of 1727 kcal or 7226 kJ (standard deviation (SD) 537 kcal or 2247 kJ, using data from the UK National Diet and Nutrition Survey (National Centre for Social Research 2012). Our approach to re‐expressing effect sizes was based on Hollands 2015.
"For ITS studies, we aimed to present statistical comparisons of time trends before and after the intervention (EPOC 2015). In all of the ITS studies, we present the results as described by the study authors, typically as regression analyses. When studies also presented data graphically, we did not attempt any re‐analysis using segmented time series regression techniques if the data were already appropriately analysed by the study authors or if we did not consider the study to be of sufficient quality to warrant re‐analysis. We considered one ITS study to be at low risk of bias (Bollinger 2011), but we could not re‐analyse the data presented graphically due to a lack of information. The figures presented weekly calories per transaction, but there were no data on the number of transactions per week; this means that the absolute and relative variability of each point was unknown and could not be modelled with time series to provide unbiased estimates."
Unit of analysis issues: we updated this section to reflect current methodology. This section now states, "For eligible cluster‐randomised trials, we planned to adjust the data to account for clustering if the study authors had not already done so. However, we only included one cluster‐RCT in the review, and the appropriate data needed to report and adjust the results were not available."
Assessment of heterogeneity: we added a sentence to the review regarding how we would deal with non‐statistical heterogeneity as well as statistical heterogeneity (the protocol only described the latter).
Assessment of reporting biases: the protocol stated that we would use funnel plots to assess reporting biases. However, we could not do this because none of the meta‐analyses included more than 10 studies.
Data synthesis: the protocol stated, "[W]e will only include studies considered to be at lower risk of bias in the meta‐analysis". We included all available evidence in one meta‐analysis but also did a separate sensitivity analysis for studies considered to be at lower risk of bias. We did this in order to present a comprehensive overview of all of the evidence and because we considered very few studies to be at low risk of bias.
A number of unanticipated data synthesis challenges emerged once we identified the included papers. In order to describe how we dealt with these, we added the following text to the review:
"For included studies with more than one eligible intervention arm, we combined data when studies contained information about the same product characteristic (e.g. energy), albeit in multiple ways (e.g. varying in whether presented as numbers, colour coded, activity‐equivalents, and whether presented with recommended daily energy intake).
"Where studies assessed the impact of nutritional labelling adjacent to a range of food products and it was not possible to extract an effect summary for the range of food products, we included the data for the product representing the most complete meal, for example, sales of entrées (as opposed to sales of a side dish) (e.g. Dubbert 1984). If no products represented more or less complete meals, we extracted data for products containing the greatest amount of energy.
"Where studies reported a number of outcomes, such as consumption of a range of different nutrients, we used the most frequently reported outcome among the included studies (e.g. Harnack 2008a). Had outcomes been reported in the same study that related to both increased consumption of healthier foods and decreased consumption of less healthy foods, we would have prioritised the latter."
In addition, after examination of the included studies, we decided to conduct separate analyses for laboratory studies that offered multiple and single food options (which we did not specify in the protocol). We added the following text to the section on data synthesis to describe our rationale: "In the process of conducting the review, it became apparent that the studies also differed in terms of how many labelled options participants had to choose from and what kind(s) of nutritional content the labels described. Participants had to make absolute judgments when given only one labelled option and relative judgments when provided with a myriad of options labelled differently. Thus, we analysed these studies separately."
The exploration of effect modifiers: the protocol specified exploration of 10 possible effect moderators of nutritional labelling using subgroup analysis.
Body weight: overweight (> BMI 25 kg/m²) or not overweight (< BMI 25 kg/m²).
Dietary restraint in individuals intending to diet: restrained eater or unrestrained eater.
Gender: male or female.
Label amount formats: relative amounts or absolute amounts of the nutrient or energy.
Label signposting: signposting present or absent.
The national context in which food was purchased or consumed. Initial examination of the literature indicated that a large proportion of the current research originates in the USA. Thus we compared the effects of nutritional labelling in the USA versus other countries. If there were sufficient variation in the country of study, we would make comparisons between countries.
Socioeconomic status: more socially deprived or less socially deprived.
Expectations of the taste the food: tastes bad or tastes good.
Price of the food: more expensive or less expensive.
Immediate context in which food is: purchased in a fast food restaurant or non‐fast food restaurant; or consumed in a real‐world or laboratory setting.
There were sufficient data to analyse only two of these effects (dietary restraint and country). Further, the protocol described the procedure for analysing moderating effects for both continuous and dichotomous outcomes. Given that all data included in the meta‐analysis were continuous, we removed the information about the analysis of dichotomous outcomes and added information about the analysis of the continuous outcomes.
Assessment of heterogeneity: the protocol considers three potential sources of heterogeneity for exploration in subgroup analysis.
The impact of the positioning of the label, comparing those that appear on the food package with those appearing in another location, such as on a supermarket shelf.
The impact of the information given on the label. First, we planned to compare labels giving information about a range of nutrients versus those giving information about one nutrient. Second, as labels most frequently give energy information, we planned to compare the impact of labels giving information about energy content with labels giving information about other nutrients.
The impact of the definitions of healthy purchasing and healthy consumption used in this review. More healthy purchasing is considered to be decreased purchasing of less healthy foods or increased purchasing of more healthy foods, but these may be two separate behaviours. We planned to use subgroup analysis to identify whether they were separate behaviours and this a source of heterogeneity. Similarly, we planned to investigate possible heterogeneity as a consequence of defining more healthy consumption as either decreased consumption of less healthy foods or increased consumption of healthier foods.
Due to lack of information (e.g. many studies did not report on the positioning of the label) and/or lack of differences in label format between the studies, we did not conduct these planned subgroup analyses. Also, given that there were only four studies at low risk of bias, various further subgroup analyses were not possible.
Sensitivity analysis: the protocol stated, "Sensitivity analyses will be conducted to explore the impact of missing data comparing results from available‐case and ITT analysis. Sensitivity analyses will also be used to assess the effects of nutritional labelling on behaviour across studies at both high and low risk of bias, specifically the meta‐analyses will be re‐run including all studies regardless of their risk of bias. Additionally, the impact of the definition of nutritional labels used in this review will be explored. The meta‐analyses will be re‐run including the studies excluded from the main analyses due to the presentation of an incomplete label rather than a complete label (as described in the 'Description of the intervention')."
We did not conduct these analyses because only four studies at low risk of bias were available for analysis, which is not enough to enable comparison in the above variables.
Contributions of authors
Writing the protocol: RAC, GJH, SAJ, TMM.
Searching for studies: NR, RAC.
Selecting studies: RAC, SEK, BS, GB.
Extracting data from studies: RAC, SEK, BS, GB.
Entering data into RevMan: SEK, RAC.
Analysing data: SEK, RAC, ATP.
Interpreting the analysis: SEK, ATP, SAJ, GJH, TMM.
Drafting final review: all.
Updating the review: all.
Sources of support
Internal sources
-
King's College London, UK
Provides support and resources for two authors (RAC, TMM)
-
University of Cambridge, UK
Provides support for three authors (GJH, TMM, SAJ)
-
University of Stirling, UK
Provides support and resources for one author (RAC)
External sources
-
National Institutes for Health Research, UK
Postdoctoral Research Fellowship (RAC)
National Institute of Health Research Senior Investigator Award (NF‐SI‐0513‐10101) (TM)
Declarations of interest
Rachel Crockett: none known. Sarah King: none known. Theresa Marteau: none known. AT Prevost: none known. Giacomo Bignardi: none known. Nia Roberts: none known. Brendon Stubbs: none known. Gareth Hollands: none known. Susan Jebb: Chaired the Public Health Responsibility Deal Food Network (2011‐2015) which encouraged the adoption of front of pack nutritional labelling and energy labelling on menus.
Crockett, King and Marteau have contributed equally to this review, thus should be considered joint first authors.
Hollands and Jebb contributed equally to this review.
Edited (no change to conclusions)
References
References to studies included in this review
Allan 2015 {published data only}
- Allan JL, Johnston M, Campbell N. Snack purchasing is healthier when the cognitive demands of choice are reduced: a randomized controlled trial. Health Psychology 2015;34(7):750–5. [DOI] [PubMed] [Google Scholar]
Balasubramanian 2002 {published data only}
- Balasubramanian SK, Cole C. Consumers' search and use of nutrition information: the challenge and promise of the Nutrition Labeling and Education Act. Journal of Marketing 2002;66(3):112-27. [Study 3 in published paper] [Google Scholar]
Bergen 2006 {published data only}
- Bergen D, Yeh M-C. Effects of energy-content labels and motivational posters on sales of sugar-sweetened beverages: stimulating sales of diet drinks among adults study. Journal of the American Dietetic Association 2006;106(11):1866-9. [DOI] [PubMed] [Google Scholar]
Bollinger 2011 {published data only}
- Bollinger B, Leslie P, Sorensen A. Calorie posting in chain restaurants. American Economic Journal-Economic Policy 2011;3(1):91-128. [Google Scholar]
Cavanagh 2014 {published data only}
- Cavanagh KV, Kruja B, Forestall CA. The effect of brand and caloric information on flavor perception and food consumption in restrained and unrestrained eaters. Appetite 2014;82:1-7. [DOI] [PubMed] [Google Scholar]
Chu 2009 {published data only}
- Chu YH, Frongillo EA, Jones SJ, Kaye GL. Improving patrons' meal selections through the use of point-of-selection nutrition labels. American Journal of Public Health 2009;99(11):2001-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu YH, Frongillo EA, Jones SJ, Kaye GL. Nutrition labels at point-of-selection in a food-service operation improves patrons' meal selection. FASEB Journal 2009;23:No. 1 Supplement 336.5. [Google Scholar]
Cioffi 2015 {published and unpublished data}
- Cioffi CE, Levitsky. An examination of the effect of nutrition labels on food purchasing behavior in Cornell dining units [Honors degree research paper]. Cornell (USA): University of Cornell, 2012. [Google Scholar]
- Cioffi CE, Levitsky D, Pacanowski CR, Bertz F. A nudge in a healthy direction. The effect of nutrition labels on food purchasing behaviors in university dining facilities. Appetite 2015;92:7-14. [DOI] [PubMed] [Google Scholar]
Crockett 2014 {published and unpublished data}
- Crockett RA, Jebb S A, Hankins M, Marteau TM. The impact of nutritional labels and socioeconomic status on energy intake: an experimental field study. Appetite 2014;81:12-19. [DOI] [PubMed] [Google Scholar]
Dubbert 1984 {published data only}
- Dubbert PM, Johnson WG, Schlundt DG, Montague NW. The influence of caloric information on cafeteria food choices. Journal of Applied Behavior Analysis 1984;17(1):85-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ebneter 2013 {published data only}
- Ebneter D, Latner J, Nigg C. Is less always more? The effects of low fat labeling and caloric information on food intake, calorie estimates, taste preference, and health attributions. Appetite 2013;68:92-7. [DOI] [PubMed] [Google Scholar]
Ellison 2013 {published data only}
- Ellison B, Lusk J, Davis D. Looking at the label and beyond: the effects of calorie label, health consciousness and demographics on calorie intake in restaurants. International Journal of Behavioural Nutrition and Physical Activity 2013;10(21):1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ellison 2014a {published data only}
- Ellison B, Lusk J, Davis D. The impact of restaurant calorie labels on food choice: results from a field experiment. Economic Inquiry 2014;52(2):666-81. [Google Scholar]
Girz 2012 ‐ study 1 {published data only}
- Girz L, Polivy J, Herman C P, Lee H. The effects of calorie information on food selection and intake. International Journal of Obesity 2012;36(10):1340-5. [DOI] [PubMed] [Google Scholar]
Girz 2012 ‐ study 2 {published data only}
- Girz L, Polivy J, Herman C P, Lee H. The effects of calorie information on food selection and intake. International Journal of Obesity 2012;36(10):1340-1345. [DOI] [PubMed] [Google Scholar]
Girz ongoing {unpublished data only}
- Girz L. The Impact of calorie labels and a confederate on ordering behaviour. In process.
Hammond 2013 {published data only}
- Hammond D, Goodman S, Hanning R, Danel S. A randomised trial of calorie labeling on menus. Preventive Medicine 2013;57(6):860-6. [DOI] [PubMed] [Google Scholar]
- NCT01948752. Clinical trial of menu labeling. clinicaltrials.gov/ct2/show/NCT01948752 (first received 24 September 24 2013).
Harnack 2008a {published data only}
- Harnack LJ, French SA, Oakes JM, Story MT, Jeffery RW, Rydell SA. Effects of calorie labeling and value size pricing on fast food meal choices: results from an experimental trial. International Journal of Behavioral Nutrition and Physical Activity 2008;5(63):[13 p.]. [DOI] [PMC free article] [PubMed]
- NCT00127660. Effect of nutrition labeling on fast food choices. clinicaltrials.gov/ct2/show/NCT00127660 (first received 8 August 2005).
Holmes 2013 {published data only}
- Holmes AS, Serrano EL, Machin JE, Duetsch T, Davis GC. Effect of different children's menu labeling designs on family purchases. Appetite 2013;62:198-202. [DOI] [PubMed] [Google Scholar]
James 2015 {published data only}
- James A, Adams-Huet MS, Shah M. Menu labels displaying the kilocaloric content or the exercise equivalent: effects on energy ordered and consumed in young adults. American Journal of Health Promotion 2015;29(5):294-302. [DOI] [PubMed] [Google Scholar]
Kral 2002 {published data only}
- Kral TVE, Roe LS, Rolls BJ. Does nutrition information about the energy density of meals affect food intake in normal-weight women? Appetite 2002;39:137-45. [DOI] [PubMed] [Google Scholar]
Platkin 2014 {published data only}
- Platkin C, Yeh M-C, Hirsch K, Weiss Wiewel E, Lin C-Y, Tung H-J, et al. The effect of menu labeling with calories and exercise equivalents on food selection and consumption. BMC Obesity 2014;1:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
Roberto 2010 {published data only}
- NCT01626729. Facts-up-front versus traffic-light food labels. clinicaltrials.gov/ct2/show/NCT01626729 (first received 25 June 2012).
- Roberto CA, Larsen PD, Agnew H, Baik J, Brownell KD. Evaluating the impact of menu labeling on food choices and intake. American Journal of Public Health 2010;100(2):312-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Roberto 2012 {published data only}
- Roberto C A, Shivaram M, Martinez O, Boles C, Harris JL, Brownell K D. The Smart Choices front-of-package nutrition label. Influence on perceptions and intake of cereal. Appetite 2012;58:651-7. [DOI] [PubMed] [Google Scholar]
Temple 2010 {published data only}
- Temple JL, Johnson K, Recupero K, Suders H. Nutrition labels decrease energy intake in adults consuming lunch in the laboratory. Journal of the American Dietetic Association 2010;110:1094-7. [DOI] [PubMed] [Google Scholar]
VanEpps 2016 {published data only}
- NCT01473225. Can calorie labels increase caloric intake? clinicaltrials.gov/ct2/show/NCT01473225 (first received 17 November 2011).
- VanEpps EM, Downs JS, Loewenstein G. Calorie label formats: using numeric and traffic light calorie labels to reduce lunch calories. Journal of Public Policy & Marketing 2016;35(1):26-36. [Google Scholar]
Vermeer 2011 {published data only}
- Vermeer WM, Steenhuis IHM, Leeuwis FH, Bos AER, De Boer M, Seidell JC. View the label before you view the movie: a field experiment into the impact of portion size and Guideline Daily Amounts labelling on soft drinks in cinemas. BMC Public Health 2011;11:438. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wansink 2006 ‐ study 1 {published data only}
- Wansink B, Chandon P. Can "Low-Fat" nutrition labels lead to obesity? Journal of Marketing Research 2006;43(4):605-17. [Study 1 of three presented in the paper] [Google Scholar]
Wansink 2006 ‐ study 3 {published data only}
- Wansink B, Chandon P. Can "Low-Fat" nutrition labels lead to obesity? Journal of Marketing Research 2006;43(4):605-17. [Study 3 of three presented in the paper] [Google Scholar]
References to studies excluded from this review
Albright 1990 {published data only}
- Albright CL, Flora JA, Fortmann SP. Restaurant menu labeling: impact of nutrition information on entree sales and patron attitudes. Health Education Quarterly 1990;17(2):157-67. [DOI] [PubMed] [Google Scholar]
Aron 1995 {published data only}
- Aron JI, Evans RE, Mela DJ. Paradoxical effect of a nutrition labelling scheme in a student cafeteria. Nutrition Research 1995;15(9):1251-61. [Google Scholar]
Babio 2014 {published data only}
- Babio N, Vicent P, Lopez L, Benito A, Basulto J, Salas-Salvado, J. Adolescents' ability to select healthy food using two different front-of-pack food labels: a cross-over study. Public Health Nutrition 2014;17(6):1403-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Berning 2011 {published data only}
- Berning JP, Chouinard HH, McCluskey JJ. Do positive nutrition shelf labels affect consumer behavior? Findings from a field experiment with scanner data. American Journal of Agricultural Economics 2011;93:364-9. [Google Scholar]
Bleich 2014 {published data only}
- Bleich SN, Barry CL, Gary-Webb TL, Herring BJ. Reducing sugar-sweetened beverage consumption by providing caloric information: how Black adolescents alter their purchases and whether the effects persist. American Journal of Public Health 2014;104(12):2417-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bucher 2015 {published data only}
- Bucher T, De Vlieger N, Brown H, Collins C. Do energy labels influence served portion sizes and meal composition? Annals of Nutrition and Metabolism 2015;67:147. [Google Scholar]
Callaghan 2010 {published data only}
- Callaghan C, Mandich G, He M. Healthier snacks in school vending machines: a pilot project in four Ontario high schools. Canadian Journal of Dietetic Practice and Research 2010;71(4):186-91. [DOI] [PubMed] [Google Scholar]
Cantor 2015 {published data only}
- Cantor J, Torres A, Abrams C, Elbel B. Five years later: awareness of New York City's calorie labels declined, with no changes in calories purchased. Health Affairs 2015;34(11):1893-1900. [DOI] [PubMed] [Google Scholar]
Cawley 2015 {published data only}
- Cawley J, Sweeney MJ, Sobal J, Just DR, Kaiser HM, Schulze WD, et al. The impact of a supermarket nutrition rating system on purchases of nutritious and less nutritious foods. Public Health Nutrition 2015;18(1):8-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chu 2012 {published data only}
- Chu YH, Jones SJ, Frongillo EA, Thrasher JF, DiPietro RB. Modifying placement and simplifying menu labels in a food service operation reduces the energy content purchased by patrons. FASEB Journal 2012;26:No. 1 Supplement 32.8. [Google Scholar]
Chu 2014 {published data only}
- Chu YH, Jones SJ, Frongillo EA, DiPietro RB, Thrasher JF. Investigating the impact of menu labeling on revenue and profit in a foodservice operation. Journal of Foodservice Business Research 2014;17:215-27. [Google Scholar]
Dingman 2015 {published data only}
- Dingman DA, Schulz MR, Wyrick DL, Bibeau DL, Gupta SN. Does providing nutrition information at vending machines reduce calories per item sold? Journal of Public Health Policy 2015;36(1):110-22. [DOI] [PubMed] [Google Scholar]
Ducrot 2016 {published data only}
- Ducrot P, Julia C, Mejean C, Kesse-Guyot E, Touvier M, Fezeu LK, et al. Impact of different front-of-pack nutrition labels on consumer purchasing intentions: a randomized controlled trial. American Journal of Preventive Medicine 2016;50(5):627-36. [DOI] [PubMed] [Google Scholar]
Dumanovsky 2011 {published data only}
- Dumanovsky T, Huang CY, Nonas CA, Matte TD, Bassett MT, Silver LD. Changes in energy content of lunchtime purchases from fast food restaurants after introduction of calorie labelling: cross sectional customer surveys. BMJ 2011;343:d4464. [DOI] [PMC free article] [PubMed] [Google Scholar]
Elbel 2011 {published data only}
- Elbel B, Gyamfi J, Kersh R. Child and adolescent fast-food choice and the influence of calorie labeling: a natural experiment. International Journal of Obesity 2011;35(4):493-500. [DOI] [PMC free article] [PubMed] [Google Scholar]
Elbel 2013a {published data only}
- Elbel B, Mijanovich T, Dixon B, Kersh R, Abrams C, Weitzman B. Calorie labeling and food choice: results from Philadelphia. In: Obesity. Vol. 19. 2011:S53.
Elbel 2013b {published data only}
- Elbel B, Taksler GB, Mijanovich T, Abrams CB, Dixon LB. Promotion of healthy eating through public policy: a controlled experiment. American Journal of Preventive Medicine 2013;45(1):49-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ellison 2014 {published data only}
- Ellison B, Lusk JL, Davis D. The effect of calorie labels on caloric intake and restaurant revenue: evidence from two full-service restaurants. Journal of Agricultural and Applied Economic 2014;46(2):173-91. [Google Scholar]
Engbers 2006 {published data only}
- Engbers LH, Van Poppel MNM, Paw MCA, Van Mechelen W. The effects of a controlled worksite environmental intervention on determinants of dietary behavior and self-reported fruit, vegetable and fat intake. BMC Public Health 2006;6:253. [DOI] [PMC free article] [PubMed] [Google Scholar]
Finkelstein 2011 {published data only}
- Finkelstein EA, Strombotne KL, Chan NL, Krieger J. Mandatory menu labeling in one fast-food chain in King County, Washington. American Journal of Preventive Medicine 2011;40:122-7. [DOI] [PubMed] [Google Scholar]
Freedman 2009 {published data only}
- Freedman MR, Mishra S. Effect of Point of Selection Nutrition Information (POSNI) on Food Choices in an All-You-Care-to-Eat University Dining Facility. Obesity 2009;17:S161-S162. [Google Scholar]
Giesen 2011 {published data only}
- Giesen JC, Payne CR, Havermans RC, Jansen A. Exploring how calorie information and taxes on high-calorie foods influence lunch decisions. American Journal of Clinical Nutrition 2011;93(4):689-94. [DOI] [PubMed] [Google Scholar]
Gittelsohn 2013 {published data only}
- Gittelsohn J, Kim EM, He S, Pardilla M. A food store-based environmental intervention is associated with reduced BMI and improved psychosocial factors and food-related behaviors on the Navajo nation. Journal of Nutrition 2013;143(9):1494-500. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gomez 2015 {published data only}
- Gomez P, Werle COC, Corneille O. The pitfall of nutrition facts label fluency: easier-to-process nutrition information enhances purchase intentions for unhealthy food products. Marketing Letters 2015;28(1):15-27. [Google Scholar]
Graham 2017 {published data only}
- Graham DJ, Lucas-Thompson RG, Mueller MP, Jaeb M, Harnack L. Impact of explained v. unexplained front-of-package nutrition labels on parent and child food choices: a randomized trial. Public Health Nutrition 2017;20(5):774-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hassan 2010 {published data only}
- Hassan LM, Shiu EM, Michaelidou N. The influence of nutrition information on choice: the roles of temptation, conflict and self-control. Journal of Consumer Affairs 2010;44:499-515. [Google Scholar]
Helfer 2014 {published data only}
- Helfer P, Shultz TR. The effects of nutrition labeling on consumer food choice: a psychological experiment and computational model. Annals of the New York Academy of Sciences 2014;1331:174-185. [DOI] [PubMed] [Google Scholar]
Hobin 2015 {published data only}
- Hobin E, Sacco J, Vanderlee L, Rosella L, L'Abbe M, Bollinger B, Manson H, Hammond D. Can an on-shelf nutrition labelling system improve the nutritional quality of food purchases in supermarkets? Canadian Journal of Diabetes 2015;39(S1):S32. [Google Scholar]
Hoerr 1993 {published data only}
- Hoerr S M, Louden V A. Can nutrition information increase sales of healthful vended snacks? Journal of School Health 1993;63:386-90. [DOI] [PubMed] [Google Scholar]
Holmes 2011 {published data only}
- Holmes A, Serrano E, Davis G. The effect of alternative nutrition menu labels on children's meals purchases and parent-child decision-making. In: Annual Meeting, July 24-26, 2011, Pittsburgh, Pennsylvania, Agricultural and Applied Economics Association, No 103816. 2011.
Kiesel 2013 {published data only}
- Kiesel K, Villas-Boas SB. Can information costs affect consumer choice? Nutritional labels in a supermarket experiment. International Journal of Industrial Organization 2013;31(2):115-63. [Google Scholar]
- Kiesel K. What do I buy now? Essays on consumer response to food labeling. Dissertation Abstracts International Section A: Humanities and Social Sciences 2009;69(9-A):3668. [Google Scholar]
Kocken 2012 {published data only}
- Kocken PL, Eeuwijk J, Van Kesteren NMC, Dusseldorp E, Buijs G, Bassa-Dafesh Z, et al. Promoting the purchase of low-calorie foods from school vending machines: a cluster-randomized controlled study. Journal of School Health 2012;82(3):115-22. [DOI] [PubMed] [Google Scholar]
Koenigstorfer 2014 {published data only}
- Koenigstorfer J, Groeppel-Klein A, Kamm F. Healthful food decision-making in response to traffic light color-coded nutrition labeling. Journal of Public Policy and Marketing 2014;33(1):65-77. [Google Scholar]
Krieger 2013 {published data only}
- Krieger JW, Chan NL, Saelens BE, Ta ML, Solet D, Fleming DW. Menu labeling regulations and calories purchased at chain restaurants. American Journal of Preventive Medicine 2013;44:595-604. [DOI] [PubMed] [Google Scholar]
Lassen 2014 {published data only}
- Lassen AD, Beck A, Leedo E, Andersen EW, Christensen T, Mejborn H, et al. Effectiveness of offering keyhole labelled meals in improving the nutritional quality of lunch meals eaten in worksite canteens. Appetite 2014;75:128-134. [DOI] [PubMed] [Google Scholar]
Mathios 2000 {published data only}
- Mathios AD. Socioeconomic factors, nutrition, and food choices: an analysis of the salad dressing market. Journal of Public Policy and Marketing 1996;15(1):45-54. [Google Scholar]
- Mathios AD. The impact of mandatory disclosure laws on product choices: an analysis of the salad dressing market. Journal of Law and Economics 2000;43(2):651-77. [Google Scholar]
McNeill 2014 {published data only}
- McNeill R, Odishoo E, Seesaengnom D. The efficacy of different nutrition labels for improving healthier food choices. International Journal of Behavioral Medicine 2014;21:S77. [Google Scholar]
NCT01604954 {published and unpublished data}
- NCT01604954. Does food labeling influence long-term food intake and eating-related variables in women? (MENU). clinicaltrials.gov/ct2/show/NCT01604954 (first received 24 May 2012).
NCT02546505 {published and unpublished data}
- NCT02546505. Impact of front-of-pack nutrition labelling on consumer purchases. clinicaltrials.gov/ct2/show/NCT02546505 (first received 11 September 2015).
Nikolaou 2014a {published data only}
- Nikolaou CK, Lean ME, Hankey C. Calorie-labelling in catering outlets: acceptability and impacts on food sales. Preventive Medicine 2014;67:160-5. [DOI] [PubMed] [Google Scholar]
Nikolaou 2014b {published data only}
- Nikolaou C, Lean M, Hankey C. Can calorie labels nudge the 'Freshman 15' phenomenon away? Obesity Reviews 2014;15:184-5. [Google Scholar]
Nikolaou 2016 {published data only}
- Nikolaou CK, Hankey CR, Lean ME. Effects of calorie labelling on macro- and micro-nutrients in main-meal choices made by young adults. European Journal of Clinical Nutrition 2016;70(3):386-92. [DOI] [PubMed] [Google Scholar]
Pulos 2010 {published data only}
- Pulos E, Leng K. Evaluation of a voluntary menu-labeling program in full-service restaurants. American Journal of Public Health 2010;100(6):1035-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Reale 2016 {published data only}
- Reale S, Flint SW. Menu labelling and food choice in obese adults: a feasibility study. BMC Obesity 2016;3:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sacks 2009 {published data only}
- Sacks G, Rayner M, Swinburn B. Impact of front-of-pack 'traffic-light' nutrition labelling on consumer food purchases in the UK. Health Promotion International 2009;24(4):344-52. [DOI] [PubMed] [Google Scholar]
Sacks 2011 {published data only}
- Sacks G, Tikellis K, Millar L, Swinburn B. Impact of 'traffic-light' nutrition information on online food purchases in Australia. Australian and New Zealand Journal of Public Health 2011;35(2):122-6. [DOI] [PubMed] [Google Scholar]
Sato 2013 {published data only}
- Sato JN, Wagle A, McProud L, Lee L. Food label effects on customer purchases in a hospital cafeteria in northern california. Journal of Foodservice Business Research 2013;16:155-68. [Google Scholar]
Schmitz 1986 {published data only}
- Schmitz MF, Fielding JE. Point-of-choice nutritional labeling - evaluation in a work site cafeteria. Journal of Nutrition Education 1986;18(2):S65-8.
Schucker 1992 {published data only}
- Schucker RE, Levy AS, Tenney JE, Mathews O. Nutrition shelf labeling and consumer purchase behavior. Journal of Nutrition Education 1992;24(2):75-81. [Google Scholar]
Schwartz 2012 {published data only}
- Schwartz J, Riis J, Elbel B, Ariely D. Inviting consumers to downsize fast-food portions significantly reduces calorie consumption. Health Affairs 2012;31(3):399-407. [DOI] [PubMed] [Google Scholar]
Seward 2016 {published data only}
- Seward MW, Block JP, Chatterjee A. A traffic-light label intervention and dietary choices in college cafeterias. American Journal of Public Health 2016;106(10):1808-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sharma 2011 {published data only}
- Sharma S, Wagle A, Sucher K, Bugwadia N. Impact of point of selection nutrition information on meal choices at a table-service restaurant. Journal of Foodservice Business Research 2011;14:146-61. [Google Scholar]
Stutts 2011 {published data only}
- Stutts MA, Zank GM, Smith KH, Williams SA. Nutrition information and children's fast food menu choices. Journal of Consumer Affairs 2011;45:52-86. [Google Scholar]
Sutherland 2010 {published data only}
- Sutherland LA, Kaley LA, Fischer L. Guiding stars: the effect of a nutrition navigation program on consumer purchases at the supermarket. American Journal of Clinical Nutrition 2010;91(4):1090S-4S. [DOI] [PubMed] [Google Scholar]
Temple 2011a {published data only}
- Temple JL, Johnson KM, Archer K, LaCarte A, Yi C, Epstein LH. Influence of simplified nutrition labeling and taxation on laboratory energy intake in adults. Appetite 2011;57:184-92. [DOI] [PubMed] [Google Scholar]
Temple 2011b {published data only}
- Temple JL, Johnson KM, Archer K, LaCarte A, Yi C, Epstein LH. Influence of simplifies nutrition labeling and taxation on laboratory energy intake in adults. Appetite 2011;57:184-192. [DOI] [PubMed] [Google Scholar]
Thorndike 2014 {published data only}
- Thorndike AN, Riis J, Sonnenberg LM, Levy DE. Traffic-light labels and choice architecture promoting healthy food choices. American Journal of Preventive Medicine 2014;46(2):143-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Thorndike 2015 {published data only}
- Thorndike A, Levy DE, Macias-Navarro L, Franckle RL, Rimm EB. Traffic-light labels and financial incentives reduce purchase of sugar-sweetened beverages by low-income, Latino families: a randomized controlled trial. Circulation 2015;131(S1):A34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Trudel 2015 {published data only}
- Trudel R, Murray KB, Kim S, Chen S. The impact of traffic light color-coding on food health perceptions and choice. Journal of Experimental Psychology Applied 2015;21(3):255-75. [DOI] [PubMed] [Google Scholar]
Vadiveloo 2011 {published data only}
- Vadiveloo MK, Dixon LB, Elbel B. Consumer purchasing patterns in response to calorie labeling legislation in New York City. International Journal of Behavioral Nutrition and Physical Activity 2011;8(51):[9 p.]. [DOI] [PMC free article] [PubMed] [Google Scholar]
Volkova 2014 {published data only}
- Volkova E, Neal B, Rayner M, Swinburn B, Eyles H, Jiang Y, et al. Effects of interpretive front-of-pack nutrition labels on food purchases: protocol for the Starlight randomised controlled trial. BMC Public Health 2014;14:968. [DOI] [PMC free article] [PubMed] [Google Scholar]
Vyth 2011 {published data only}
- Vyth EL, Steenhuis IHM, Heymans MW, Roodenburg AJC, Brug J, Seidell JC. Influence of placement of a nutrition logo on cafeteria menu items on lunchtime food Choices at Dutch work sites. Journal of the American Dietetic Association 2011;111(1):131-6. [DOI] [PubMed] [Google Scholar]
Wang 2016 {published data only}
- Wang EY, Wei HL, Caswell JA. The impact of mandatory trans fat labeling on product mix and consumer choice: a longitudinal analysis of the US Market for margarine and spreads. Food Policy 2016;64:63-81. [Google Scholar]
Wardle 1994 {published data only}
- Wardle J, Solomons W. Naughty but nice: a laboratory study of health information and food preferences in a community sample. Health Psychology 1994;13(2):180-3. [DOI] [PubMed] [Google Scholar]
Webb 2011 {published data only}
- Webb KL, Solomon LS, Sanders J, Akiyama C, Crawford PB. Menu labeling responsive to consumer concerns and shows promise for changing patron purchases. Journal of Hunger and Environmental Nutrition 2011;6(2):166-78. [Google Scholar]
Whitaker 1994 {published data only}
- Whitaker RC, Wright JA, Koepsell TD, Finch AJ, Psaty BM. Randomized intervention to increase children's selection of low-fat foods in school lunches. Journal of Pediatrics 1994;125(4):535-40. [DOI] [PubMed] [Google Scholar]
References to ongoing studies
ACTRN12614000964617 {unpublished data only}
- ACTRN12614000964617. The effects of four front-of-pack labelling schemes compared to standard Nutrition Information Panel, on the healthiness of food Purchases among adult Australian consumers [The effects of four front-of-pack labelling schemes compared to standard Nutrition Information Panel, on mean nutrient profiling score of food purchases among the adult Australian consumers: A Randomised Trial]. www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=366945 (first received 21 August 2014).
Additional references
Australian Dept Health and Aging 2013
- Department of Health and Aging (Australia). Final Communiqué - Legislative and Governance Forum on Food Regulation. 2013. www.health.gov.au/internet/ministers/publishing.nsf/Content/mr-yr13-sn-sn014.htm (accessed prior to 20 November 2017).
Balshem 2011
- Balshem H, Helfand M, Schunemann HJ, Oxman AD, Zunz R, Brozek J, et al. GRADE guidelines: 3. Rating the quality of evidence. Journal of Clinical Epidemiology 2011;64(4):401-6. [DOI] [PubMed] [Google Scholar]
Bleich 2017
- Bleich SN, Economos CD, Spiker ML, Vercammen KA, VanEpps EM, Block JP, Elbel B, Story M, Roberto CA. A systematic review of calorie labeling and modified calorie labeling interventions: impact on consumer and restaurant behavior. Obesity (Silver Spring) 2017;25(12):2018-2044. [DOI] [PMC free article] [PubMed] [Google Scholar]
Blewett 2011
- Blewett N, Goddard N, Pettigrew S, Reynolds C, Yeatman H. Labelling logic: review of food labelling law and policy. Canberra: Commonwealth of Australia, 2011. Available at www.foodlabellingreview.gov.au/internet/foodlabelling/publishing.nsf/content/labelling-logicGovernment Report.
Brownell 2006
- Brownell K, Yach D. Lessons from a small country about the global obesity crisis. Globilization and Health 2006;2(1):11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Campos 2011
- Campos S, Doxey J, Hammond D. Nutrition labels on pre-packaged foods: a systematic review. Public Health Nutrition 2011;14(8):1496-1506. [DOI] [PubMed] [Google Scholar]
Cantu‐Jungles 2017
- Cantu-Jungles TM, McCormack LA, Slaven JE, Slebodnik M, Eicher-Miller HA. A meta-analysis to determine the impact of restaurant menu labeling on calories and nutrients (ordered or consumed) in U.S. adults. Nutrients 2017;9(1088):18 p. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cecchini 2016
- Cecchini M, Warin L. Impact of food labelling systems on food choices and eating behaviours: a systematic review and meta-analysis of randomized studies. Obesity Reviews 2016;17(3):201-10. [DOI] [PubMed] [Google Scholar]
Cochrane Public Health Review Group 2010
- Cochrane Public Health Group. Developing a Cochrane Protocol. In: Jackson N. Systematic Reviews of Health Promotion and Public Health Interventions. Cochrane Collaboration, 2010. Available at ph.cochrane.org/sites/ph.cochrane.org/files/uploads/HPPH_systematic_review_handbook.pdf.
Cohen 1988
- Cohen J. Statistical Power Analysis in the Behavioural Sciences. 2nd edition. Hillsdale (NJ): Lawrence Erlbaum Associates Inc., 1988. [Google Scholar]
Commonwealth of Australia 2016
- About Health Star Ratings. healthstarrating.gov.au/internet/healthstarrating/publishing.nsf/Content/About-health-stars (accessed prior to 20 November 2017).
Cowburn 2005
- Cowburn G, Stockley L. Consumer understanding and use of nutrition labelling: a systematic review. Public Health Nutrition 2005;8(1):21-8. [DOI] [PubMed] [Google Scholar]
Das 2012
- Das P, Horton R. Rethinking our approach to physical activity. Lancet 2012;380(9838):189–90. [DOI] [PubMed] [Google Scholar]
Deeks 2011
- Deek JJ, Higgins JPT, Altman DG. Chapter 9: Analysing data and undertaking meta-analyses. In: Higgins JPT, Green S, editors(s). Cochrane Handbook for Systematic Reviews of interventions. Wiley-Blackwell, 2011:243-296. [Google Scholar]
DeGroot 2012
- DeGroot MH, Schervish MJ. Probability and Statistics. 4th edition. Boston: Addison-Wesley, 2012. [Google Scholar]
Dobbs 2014
- Dobbs R, Sawers C, Thompson F, et al. Overcoming obesity: An initial economic analysis. McKinsey Global Institute, 2014. http://www.mckinsey.com/insights/economic_studies/how_the_world_could_better_fight_obesity (accessed prior to 20 November 2017).
EEC 1990
- European Commission. Council Directive 90/496/EEC on nutrition labelling for foodstuffs of 24 September 1990. Official Journal of the European Communities 1990:40-4.
EPHPP 2010
- Effective Public Health Practice Project. Quality assessment tool for quantitative studies. 2010. www.ephpp.ca/PDF/Quality%20Assessment%20Tool_2010_2.pdf (accessed prior to 20 November 2017).
EPOC 2015
- EPOC. Effective Practice and Organisation of Care (EPOC). EPOC Resources for review authors. Oslo: Norwegian Knowledge Centre for the Health Services. Available at epoc.cochrane.org/epoc-specific-resources-review-authors 2015.
EUFIC 2013
- European Food Information Council. Global update on nutrition labelling. 2013. www.eufic.org (accessed prior to 20 November 2017).
European Commission 2011
- European Commission. Provision of Food Information to Consumers - Proposed Legislation. 2011. ec.europa.eu/food/food/labellingnutrition/foodlabelling/proposed_legislation_en.htm (accessed prior to 20 November 2017).
European Union 2011
- European Union. Regulation (EU) No 1169/2011 Of the European Parliament and of the Council of 25 October 2011. Official Journal of the European Union L304 of November 2011:18-63.
FDA 1994
- US Food and Drug Administration. Guide to Nutrition Labelling and Education Act (NLEA) requirements. 1994. www.fda.gov/ICECI/Inspections/InspectionGuides/ucm074948.htm (accessed prior to 20 November 2017).
FDA 2016
- US Food and Drug Administration. Menu and vending machines labeling requirements. 2016. www.fda.gov/Food/GuidanceRegulation/GuidanceDocumentsRegulatoryInformation/LabelingNutrition/ucm217762.htm (accessed prior to 20 November 2017).
Food Standards 2002
- New Zealand (Australia New Zealand Food Standards Code) Food Standards 2002. http://www.foodsafety.govt.nz/elibrary/industry/zealand-australia-zealand-food-standards/nz-food-standards-2002.pdf.
Foresight 2007
FTC 2016
- Federal Trade Commission. Fair Packaging and Labeling Act. 2016. www.ftc.gov/enforcement/rules/rulemaking-regulatory-reform-proceedings/fair-packaging-labeling-act (accessed prior to 20 November 2017).
Grech 2015
- Grech A, Allman-Farinelli M. A systematic literature review of nutrition interventions in vending machines that encourage consumers to make healthier choices. Obesity Reviews 2015;16(12):1030-41. [DOI] [PubMed] [Google Scholar]
Grunert 2007
- Grunert KG, Wills JM. A review of European research on consumer response to nutrition information on food labels. Journal of Public Health 2007;15(5):385-99. [Google Scholar]
Harnack 2008b
- Harnack LJ, French SA. Effect of point-of-purchase calorie labeling on restaurant and cafeteria food choices: a review of the literature. International Journal of Behavioral Nutrition and Physical Activity 2008;5(51):[6 p.]. [DOI] [PMC free article] [PubMed] [Google Scholar]
Health Canada 2016
- Health Canada. Final amendments to the Food and Drug Regulations - Nutrition Labelling, Other Labelling Provisions and Food Colours. www.hc-sc.gc.ca/fn-an/label-etiquet/nutrition/reg/index-eng.php (accessed prior to 20 November 2017).
Higgins 2011
- Higgins JPT, Altman DG, Sterne JA. Chapter 8: Assessing risk of bias in included studies. In: Higgins JPT, Green S, editors(s). Cochrane Handbook for Systematic Reviews of Interventions. Wiley-Blackwell, 2011:187-241. [Google Scholar]
Hollands 2013a
- Hollands GJ, Shemilt I, Marteau TM, Jebb SA, Kelly MP, Nakamura R, et al. Altering micro-environments to change population health behaviour: towards an evidence base for choice architecture interventions. BMC Public Health 2013a;13:1218. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hollands 2013b
- Hollands GJ, Shemilt I, Marteau TM, Jebb SA, Kelly MP, Nakamura R, et al. Altering Choice Architecture to Change Population Health Behaviour: a Large-Scale Conceptual and Empirical Scoping Review of Interventions Within Micro-Environments. Cambridge: University of Cambridge, 2013. [Google Scholar]
Hollands 2015
- Hollands GJ, Shemilt I, Marteau TM, Jebb SA, Lewis HB, Wei Y, et al. Portion, package or tableware size for changing selection and consumption of food, alcohol and tobacco. Cochrane Database of Systematic Reviews 2015, Issue 9. Art. No: CD011045. [DOI: 10.1002/14651858.CD011045.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hollands 2016
- Hollands GJ, Marteau TM, Fletcher PC. Non-conscious processes in changing health-related behaviour: a conceptual analysis and framework. Health Psychology Review 2016;10(4):381-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hollands 2017a
- Hollands GJ, Carter P, Shemilt I, Marteau TM, Jebb SA, Higgins J, et al. Altering the availability or proximity of food, alcohol and tobacco products to change their selection and consumption. Cochrane Database of Systematic Reviews 2017, Issue 3. Art. No: CD012573. [DOI: 10.1002/14651858.CD012573] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hollands 2017b
- Hollands GJ, Bignardi G, Johnston M, Kelly MP, Ogilvie D, Petticrew M, et al. The TIPPME intervention typology for changing environments to change behaviour. Nature Human Behaviour 2017;1:0140. [Google Scholar]
Horgen 2002
- Horgen KB, Brownell KD. Comparison of price change and health message interventions in promoting healthy food choices. Health Psychology 2002;21(5):505-12. [DOI] [PubMed] [Google Scholar]
Malam 2009
- Malam S, Clegg S, Kiwan S, McGinigal S, BMRB Social Research. Comprehension and use of UK nutritional signpost labelling schemes. 2009. www.food.gov.uk/multimedia/pdfs/pmpreport.pdf (accessed prior to 20 November 2017).
Marteau 2012
- Marteau TM, Hollands GJ, Fletcher PC. Changing human behaviour to prevent disease: the importance of targeting automatic processes. Science 2012;337(6101):1492–5. [DOI] [PubMed] [Google Scholar]
Marteau 2015
- Marteau TM, Hollands GJ, Shemilt I, Jebb SA. Downsizing: policy options to reduce portion sizes to help tackle obesity. BMJ 2015;351:h5863. [DOI] [PubMed] [Google Scholar]
Mhurchu 2007
- Mhurchu C, NiGorton D. Nutrition labels and claims in New Zealand and Australia: a review of use and understanding. Australian & New Zealand Journal of Public Health 2007;31(2):105-12. [DOI] [PubMed] [Google Scholar]
National Centre for Social Research 2012
- National Centre for Social Research. National Diet andNutrition Survey Years 1-4, 2008/09-2011/12. London: National Centre for Social Research, 2012. [Google Scholar]
Newton 2015
- Newton JN, Briggs ADM, Murray CJL, Dicker D, Foreman KJ, Wang H et al. Changes in health in England, with analysis by English regions and areas of deprivation, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015;386(10010):2257–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ng 2014
- Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014;384(9945):766-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nordic Council of Ministers 2016
- About keyhole. www.norden.org/en/nordic-council-of-ministers/council-of-ministers/nordic-council-of-ministers-for-fisheries-and-aquaculture-agriculture-foodstuffs-and-forestry-mr-fjls/keyhole-nutrition-label/about-keyhole (accessed prior to 20 November 2017).
Obesity Policy Coalition 2014
- Obesity Policy Coalition. Policy brief: Kilojoule labelling in chain food outlets. 2014. www.opc.org.au/downloads/positionpapers/policy-brief-kJ-labelling-food-chain-outlets.pdf (accessed prior to 20 November 2017).
Ogden 2007
- Ogden J, Karim L, Choudry A, Brown K. Understanding successful behaviour change: the role of intentions, attitudes to the target and motivations and the example of diet. Health Education Research 2007;22(3):397-405. [DOI] [PubMed] [Google Scholar]
Public Health England 2015
- Public Health England. Sugar Reduction: The Evidence for Action. London: Public Health England, 2015. [Google Scholar]
Rayner 2013
- Rayner M, Wood A, Lawrence M, Mhurchu CN, Albert J, Barquera S, et al. Monitoring the health-related labelling of foods and non-alcoholic beverages in retail settings. Obesity 2013;14(Supp 1):70-81. [DOI] [PubMed] [Google Scholar]
Reeves 2011
- Reeves B, Deeks J, Higgins J, Wells G. Chapter 13: Including non-randomized studies. In: Higgins JPT, Green S, editors(s). Cochrane Handbook for Systematic Reviews of interventions. Wiley-Blackwell, 2011:391-432. [Google Scholar]
RevMan 2014 [Computer program]
- Nordic Cochrane Centre, The Cochrane Collaboration Review Manager (RevMan). Version 5.3. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Schünemann 2011
- Schünemann HJ, Oxman AD, Vist GE, Higgins JPT, Deeks JJ, Glasziou P, et al. Chapter 12: Interpreting results and drawing conclusions. In: Higgins JPT, Green S, editors(s). Cochrane Handbook for Systematic Reviews of Interventions. Wiley-Blackwell, 2011:259-387. [Google Scholar]
Shemilt 2017
- Shemilt I, Hendry V, Marteau TM. What do we know about the effects of exposure to 'Low alcohol' and equivalent product labelling on the amounts of alcohol, food and tobacco people select and consume? A systematic review. BMC Public Health 2017;17(1):29. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sinclair 2014
- Sinclair S, Cooper M, Mansfiled E. The influence of menu labelling on calories selected or consumed: a systematic review and meta-analysis. Journal of the Academy of Nutrition and Dietetics 2014;114(9):1375-88. [DOI] [PubMed] [Google Scholar]
Sterne 2011
- Sterne J AC, Egger M, Moher D, on behalf of the Cochrane Bias Methods Group. Chapter 10: Addressing reporting biases. In: Higgins JPT, Green S, editors(s). Cochrane Handbook for Systematic Reviews of Interventions. Wiley-Blackwell, 2011:297-333. [Google Scholar]
Swartz 2011
- Swartz JJ, Braxton D, Viera AJ. Calorie menu labeling on quick-service restaurant menus: an updated systematic review of the literature. International Journal of Behavioral Nutrition and Physical Activity 8;135:[8 p.]. [DOI] [PMC free article] [PubMed] [Google Scholar]
UK Dept Health 2013
- Department of Health (UK). Technical guidance on nutritional labelling. 2013. www.gov.uk/government/uploads/system/uploads/attachment_data/file/207842/2013-06-19_Nutrition_Technical_Guidance.pdf (accessed prior to 20 November 2017).
Wansink 2004
- Wansink B, Ittersum K, Painter JE. How diet and health labels influence taste and satiation. Journal of Food Science 2004;69(9):S340-6. [Google Scholar]
WHO 2004
- World Health Organization. Global Strategy, on Diet, Physical Activity and Health. Geneva: World Health Organization, 2004. [www.who.int/dietphysicalactivity/en/] [Google Scholar]
WHO 2013
- World Health Organisation. Global Action for the Prevention and Control of Non-communicable Disease 2013-2020. Geneva: World Health Organization, 2013. [ www.who.int/nmh/events/ncd_action_plan/en/] [http://apps.who.int/iris/bitstream/10665/94384/1/9789241506236_eng.pdf?ua=1] [Google Scholar]
WHO Obesity Fact Sheet
- World Health Organization. 10 Facts on Obesity. www.who.int/features/factfiles/obesity/facts/en/index1.html (accessed prior to 20 November 2017).
Yach 2006
- Yach D, Stuckler D, Brownell K. Epidemiological and economic consequences of the global epidemics of obesity and diabetes. Nature Medicine 2006;12(1):62-6. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Crockett 2011
- Crockett RA, Hollands GJ, Jebb SA, Marteau TM. Nutritional labelling for promoting healthier food purchasing and consumption [protocol]. Cochrane Database of Systematic Reviews 2011, Issue 9. Art. No: CD009315. [DOI: 10.1002/14651858.CD009315] [DOI] [PMC free article] [PubMed] [Google Scholar]


