This randomized clinical trial compares the rates of use for ready-made vs custom-made spectacles among school-aged children in an eye health program in India.
Key Points
Question
What proportions of children given ready-made vs custom-made spectacles are still wearing the spectacles at 3 to 4 months after testing?
Findings
In this randomized clinical trial of a school-based eye health program in India that included 460 children, the proportion of children wearing spectacles at follow-up included 139 of 184 (75.5%) in the ready-made arm vs 131 of 178 (73.6%) in the custom-made arm.
Meaning
In school-based eye health programs, use of ready-made spectacles may be no different from use of more expensive custom-made spectacles.
Abstract
Importance
Uncorrected refractive errors are the most common cause of visual impairment in children despite correction being highly cost-effective.
Objective
To determine whether less expensive ready-made spectacles produce rates of spectacle wear at 3 to 4 months comparable to those of more expensive custom-made spectacles among eligible school-aged children.
Design, Setting, and Participants
This noninferiority, double-masked, randomized clinical trial recruited children aged 11 to 15 years from January 12 through July 31, 2015, from government schools in urban and periurban areas surrounding Bangalore, India. Follow-up occurred from August 1 through September 31, 2015. Participants met the following eligibility criteria for ready-made spectacles: failed vision screening at the 6/9 level in each eye; refraction was indicated; acuity improved with correction by 2 or more lines in the better-seeing eye; the corrected acuity with the spherical equivalent was not more than 1 line less than with full correction; anisometropia measured less than 1.0 diopter; and an appropriate frame was available.
Interventions
Eligible children were randomized to ready-made or custom-made spectacles.
Main Outcomes and Measures
Proportion of children wearing their spectacles at unannounced visits 3 to 4 months after the intervention.
Results
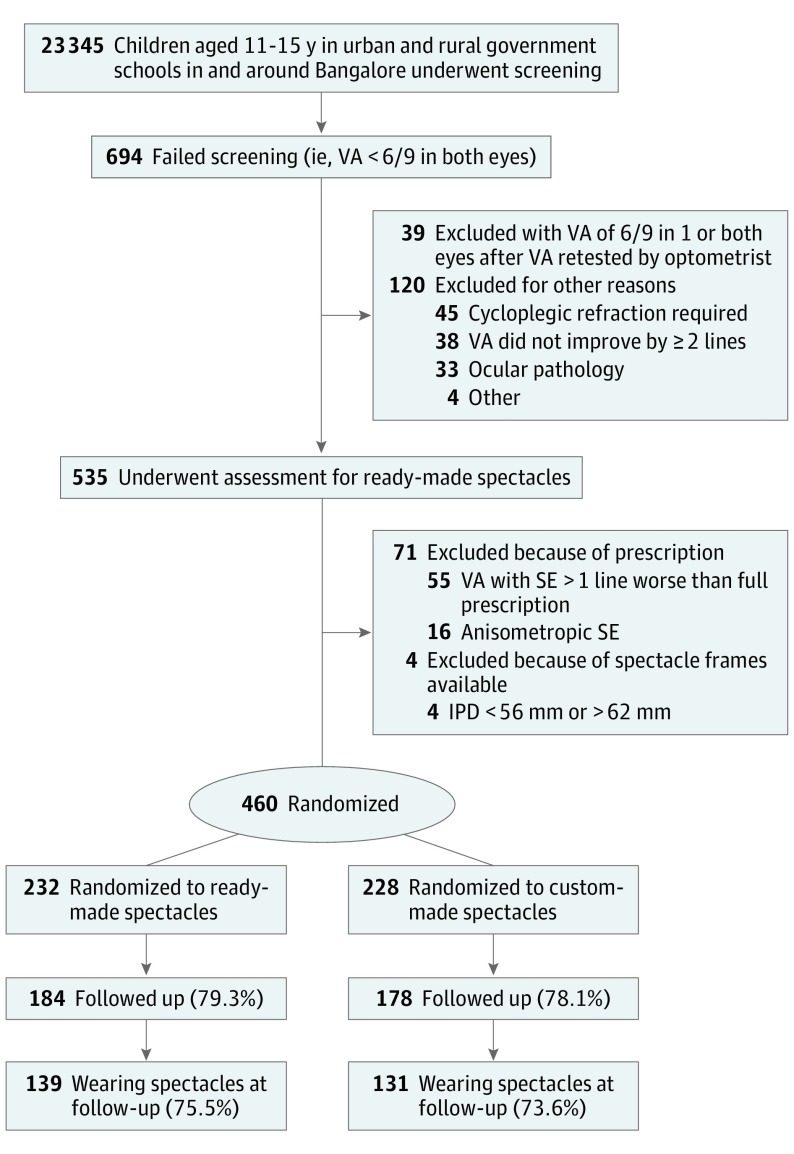
Of 23 345 children aged 11 to 15 years who underwent screening, 694 had visual acuity of less than 6/9 in both eyes, and 535 underwent assessment for eligibility. A total of 460 children (227 female [49.3%] and 233 male [50.7%]; mean [SD] age, 13.4 [1.3] years) were eligible for ready-made spectacles (2.0% undergoing screening and 86.0% undergoing assessment) and were randomized to ready-made (n = 232) or custom-made (n = 228) spectacles. Follow-up rates at 3 to 4 months were similar (184 [79.3%] in the ready-made group and 178 [78.1%] in the custom-made group). Rates of spectacle wear in the 2 arms were similar among 139 of 184 children (75.5%) in the ready-made arm and 131 of 178 children (73.6%) in the custom-made arm (risk difference, 1.8%; 95% CI, −7.1% to 10.8%).
Conclusions and Relevance
Most children were eligible for ready-made spectacles, and the proportion wearing ready-made spectacles was not inferior to the proportion wearing custom-made spectacles at 3 to 4 months. These findings suggest that ready-made spectacles could substantially reduce costs for school-based eye health programs in India without compromising spectacle wear, at least in the short term.
Trial Registration
isrctn.com Identifier: ISRCTN14715120
Introduction
The proportion of visual impairment due to uncorrected refractive errors (REs) in children aged 3 to 15 years varies from 72.6% in Australia to 82% in India and 97.1% in China. Uncorrected REs are the most common cause of visual impairment in children in all regions, affecting an estimated 12.4 million children, despite correction of RE being highly cost-effective. Incidence of myopia in children is increasing globally in what is now an epidemic in East Asia, Europe, and the United States. In Singapore, China, Taiwan, Hong Kong, Japan, and Korea, 80% to 90% of children completing high school have myopia. Variation in the prevalence of uncorrected RE in children by age and urban or rural location is also evident in India. In a 2002 study in urban India, 7.4% of children aged 5 to 15 years had myopia, and 82% of visual impairment was attributable to uncorrected RE. In a similar study in rural India, 4.1% of children aged 7 to 15 years had myopia, and 61% of visual impairment was due to uncorrected RE. In both studies, older children had a higher prevalence of uncorrected RE than younger children.
Complex refractions require spherical and astigmatic correction, and in clinical practice, these are usually fully corrected. In this trial, these corrections used custom-made spectacles. Simple REs with low or no astigmatism and minimal difference in spherical correction between the 2 eyes can be corrected using low-cost spectacles that have the same spherical equivalent (SE) in both eyes (ie, ready-made spectacles). Two broad criteria need to be fulfilled before dispensing ready-made spectacles: the prescription is suitable, and the available frames are of the correct size and fit.
The high levels of visual impairment due to uncorrected RE have led to school programs for RE in many countries, and organizations are supporting large-scale programs, including in India. However, approaches are not standardized, and most do not use guidelines or prescribing protocols; furthermore, spectacle wear is not usually monitored. Available evidence suggests that the rate of spectacle wear among children with RE is low in many settings, including 13% in Mexico, 29.4% in rural areas near Delhi, and 33.2% among Native American students. Spectacle wear rates are higher among children with more severe uncorrected RE and among girls, but associations between socioeconomic status or parental education are inconclusive. In a recent study in India, only 30% of children dispensed spectacles were wearing them at 6 to 12 months, with higher rates among girls, those with higher REs and poor uncorrected visual acuity (VA), and those whose fathers were better educated.
To our knowledge, school eye-screening programs in India dispense custom-made spectacles regardless of severity or type of RE. These spectacles are more expensive to dispense than ready-made spectacles, require the time of dispensing opticians, and cannot be dispensed immediately in schools. The spectacles must be delivered, which increases costs. Costs are therefore likely to be higher for parents and clinicians if custom-made spectacles are used rather than ready-made.
We have identified 2 trials that compared ready-made with custom-made spectacles for children with uncorrected RE, both undertaken in China. The trial by Zeng et al had a superiority design, and children with high degrees of astigmatism or anisometropia were excluded. Children were individually randomized to custom-made or ready-made spectacles. Spectacles were prescribed based on RE and level of uncorrected VA but not corrected VA or improvement in VA, factors known to increase rates of spectacle wear. Subsequent spectacle wear was defined as observation of children wearing their spectacles at an unannounced visit. At 1 month, similar proportions of children were wearing their spectacles (46.9% ready-made vs 51.5% custom-made spectacles, a difference of 5.4%; P = .23). The purpose of the other trial by Zhou et al, which had a noninferiority design, was to assess the effect of spectacle correction on quality of life. The rate of self-reported spectacle wear was high (>94.7%) in all groups, including those dispensed ready-made spectacles.
In our trial, a noninferiority design was used with the null hypothesis that the proportion of children wearing their ready-made spectacles (intervention group) at 3 to 4 months would not be inferior to the proportion wearing custom-made spectacles (standard care group). A noninferiority design was chosen because benefits of ready-made spectacles are the considerably lower cost and the ease of dispensing, which would increase program efficiency. Under these circumstances, a slightly lower acceptance of ready-made spectacles, measured by observed spectacle wear, might be acceptable. The noninferiority margin of 10% was chosen based on the trial by Zeng et al to balance considerations of efficacy and secondary benefits and the maximum difference we were prepared to tolerate if ready-made spectacles were not to be considered as clinically inferior. The trial protocol was published in January 2016.
This prospective, randomized clinical trial was undertaken in government schools in and around Bangalore, India. Reporting follows the CONSORT 2010 Checklist for noninferiority and equivalence trials.
Methods
The trial protocol is available in the Supplement. The study adhered to the Declaration of Helsinki. Children requiring further examination or spectacles for complex REs were not recruited and were referred to Sankara Eye Hospital, Bangalore, India, for free examination and spectacles, if required. The trial was approved by the Interventions and Research Ethics Committee of the London School of Hygiene and Tropical Medicine and the institutional review board of Sankara Eye Hospital. All parents of children eligible to be recruited to the trial provided written informed consent, and the children provided assent.
A list of government secondary schools in urban and periurban areas surrounding Bangalore in Karnataka State was obtained from the district education officer. Schools were excluded if eye screening had taken place within 2 years. Schools were stratified by location (urban or rural) and size (≥200 or <200 children aged 11-15 years) and then randomly selected using block randomization. The principal of each selected school was visited by a field worker who obtained written informed consent for school participation. An information sheet in the local language was given to each child aged 11 to 15 years to take home for parents to sign if they did not want their child to undergo screening and receive spectacles, if required. Field workers who were part of an earlier study were recruited and underwent further training in VA screening, including assessment of interobserver agreement.
Participants and Eligibility
Recruitment took place from January 12 through July 31, 2015. Screening was offered to all children aged 11 to 15 years present at school at the time of screening using the 6/9 row of 5 tumbling Es on an illuminated, distance acuity logMAR chart. Each eye was tested separately. To pass, children had to correctly identify 4 or 5 Es. Children who failed screening (ie, presenting VA<6/9 in each eye) were referred to study optometrists who retested their VA using a full logMAR chart. If a child’s VA was 6/9 in both eyes at the second testing, no further action was taken. Children confirmed with a VA of less than 6/9 in both eyes underwent objective and subjective refraction and assessment for frame size to ascertain whether they fulfilled eligibility criteria for the trial. Because ready-made spectacles have only spherical lenses, SE was calculated for each eye. All children with a VA of less than 6/9 also had a basic eye examination.
To be eligible for recruitment, the following criteria had to be met: (1) VA with full correction improved in the better-seeing eye by 2 or more lines, (2) the SE corrected the VA to not more than 1 line less than best-corrected VA with a full prescription in the better eye, (3) the difference between SE of the right and left eyes was not more than 1.0 diopter (D), (4) interpupillary distance matched that of ready-made spectacle frames available (ie, 54-62 mm), and (5) spectacle frames were of acceptable size and fit. Exclusion criteria consisted of other causes of visual impairment and lack of parental consent. Ineligible children were prescribed custom-made spectacles or referred to Sankara Eye Hospital. Eligible children were recruited by optometrists and given a unique identifier and a red card with the child’s name and identification, class, and father’s name.
Interventions
The intervention consisted of ready-made spectacles (ie, same spherical correction in each eye). The comparator consisted of custom-made spectacles (ie, dispensed on the basis of a prescription from study optometrists). In this study, all spectacles were made at Sankara Eye Hospital. All children had the same choices of frames, and all spectacles were delivered to the school at the same time. The latter procedure masked students to the arm to which they were allocated.
Children recruited to the trial selected the frames they preferred from a range of 6 different colors of plastic and metal frames. Ready-made and custom-made spectacles were delivered to each school by a field worker and optometrist on the same day, within 2 weeks of refraction, to maintain masking. Each child’s identity was confirmed by the teacher and checked against the red card. Spectacle fit was assessed, and corrected distance VA was measured in each eye.
Outcome and Ascertainment of Primary Outcome
Spectacle wear was categorized as follows: children were (1) wearing their spectacles at the time of the unannounced visit, (2) not wearing their spectacles but had them at school, (3) not wearing their spectacles but said they were at home, and (4) no longer had the spectacles because they were broken or lost. Categories 1 and 2 were defined as wearing and categories 3 and 4 as nonwearing.
Field workers made unannounced visits to study schools 3 to 4 months after spectacles were delivered to assess the proportion of children wearing their spectacles (August 1 through September 31, 2015). They were given a list of children dispensed spectacles and went to the relevant classrooms, where teachers identified each child. Whether the child was wearing spectacles was noted. Children not wearing their spectacles were interviewed in another room to explore whether they had their spectacles with them and, if they did, were asked to show them to field workers.
Sample Size Calculation
Sample size was calculated using the Sealed Envelope program, assuming a noninferiority margin (Δ) of 10% and considering a difference of 10% or less in spectacle wear to be acceptable. Other parameters included 95% CI, 80% power, and 1:1 allocation. Sample size was not increased to allow for loss to follow-up, and high follow-up at 3 to 4 months was anticipated because the communities were stable and few study children were expected to leave school during the academic year.
Randomization and Masking
After recruitment, children were randomly assigned to ready-made or custom-made spectacles in a ratio of 1:1. Block randomization with variable block sizes, stratified by school, was computer generated by one of us who was an epidemiologist (J.E.) away from the study site. Sequentially numbered, sealed, stamped opaque envelopes containing labels with unique study identification numbers and random allocation were prepared by persons not involved in the trial. At the study site, the optometrist opened the envelopes.
Children, teachers, and parents were masked to the allocation arm. To maintain masking, a field worker and optometrist not previously involved in the trial were trained to assess the primary outcome.
Statistical Analysis
Data were double entered by the lead investigator at regular intervals to monitor recruitment. After data cleaning and range and consistency checks, primary analysis was undertaken to compare spectacle wear in both arms. Characteristics of children in both arms were compared. All analyses were undertaken according to the group to which the child had been allocated. The outcome is presented as the difference in the proportion wearing spectacles and 95% CI of the difference. Analyses were prespecified. All analyses were performed using STATA software (version 14.1; StataCorp).
Results
All school principals approached agreed that their school would participate in the trial, and no parent or child refused consent. A total of 23 345 children underwent screening at 112 government schools (Figure), 694 (3.0%) of whom had a presenting VA of less than 6/9 in each eye. Thirty-nine children were excluded because their VA was 6/9 or better in 1 or both eyes at a second test. An additional 120 were excluded after refraction and basic eye examination. Of these, 45 required specialist refraction, 38 did not show improvement of VA by 2 or more lines, 33 had pathologic findings that required specialist examination, 1 wanted contact lenses, 1 refused spectacles, and 2 had learning disabilities. Among the 535 children undergoing assessment for eligibility for ready-made spectacles, 75 (14.0%) were excluded because they did not meet all requirements for ready-made spectacles, mainly that their VA with SE was more than 1 line worse than with a full prescription (55 children). Therefore, 460 (86.0%) of the children undergoing assessment were eligible for ready-made spectacles.
Figure. Study Flowchart.
IPD indicates interpupillary distance; SE, spherical equivalent; and VA, visual acuity.
A total of 460 children eligible for ready-made spectacles were recruited from January 12 through July 31, 2015, of whom 227 (49.3%) were female and 233 (50.7%) were male (mean [SD] age, 13.4 [1.3] years). Two hundred thirty-two children were randomized to ready-made and 228 to custom-made spectacles. All children received the correct spectacles and had a corrected VA of at least 6/9 in each eye with their new spectacles at the time of delivery 2 weeks later. The mean SE was similar in both arms of the trial (ready-made: −1.51 D; custom-made: −1.42 D), but the range of SE in the better eye was wider in the custom-made than ready-made arms (Table 1). All other baseline variables were similar in both arms.
Table 1. Baseline Characteristics of Children Randomized to Ready-Made or Custom-Made Spectacles.
| Characteristic | Study Group, No. (%)a | |
|---|---|---|
| Ready-Made Spectacles (n = 232) |
Custom-Made Spectacles (n = 228) |
|
| Sociodemographic | ||
| Age, mean (SD) [range], y | 13.4 (1.28) [11 to 15] | 13.6 (1.28) [11 to 15] |
| Female | 111 (47.8) | 116 (50.9) |
| Rural location | 73 (31.5) | 70 (30.7) |
| Parental | ||
| Literacy | ||
| Father only | 38 (16.4) | 57 (25.0) |
| Mother only | 38 (16.4) | 42 (18.4) |
| Both parents | 90 (38.8) | 80 (35.1) |
| Neither parent | 66 (28.4) | 49 (21.5) |
| Spectacle wear | ||
| Father only | 25 (10.8) | 29 (12.7) |
| Mother only | 18 (7.8) | 19 (8.3) |
| Both parents | 6 (2.6) | 3 (1.3) |
| Neither parent | 183 (78.9) | 177 (77.6) |
| Clinical | ||
| Presenting VA in better eye | ||
| <6/9 to 6/12 | 62 (26.7) | 63 (27.6) |
| <6/12 to 6/18 | 75 (32.3) | 72 (31.6) |
| <6/18 to 6/60 | 91 (39.2) | 85 (37.3) |
| <6/60 | 4 (1.7) | 8 (3.5) |
| SE (better eye), mean (SD) [range] | −1.51 (0.92) [0.50 to −5.50] | −1.42 (1.20) [2.25 to −9.50] |
Abbreviations: SE, spherical equivalent; VA, visual acuity.
Percentages have been rounded and may not total 100.
Overall, 362 of 460 children (78.7%) were identified in their schools at follow-up (Table 2). Follow-up was similar in both arms, with 184 of 232 (79.3%) in the ready-made and 178 of 228 (78.1%) in the custom-made arms. All children not followed up in school (n = 98) had changed schools and moved to a different area. Children not followed up in the ready-made arm were more likely to be male (30 of 48 [62.5%] vs 21 of 50 [42.0%]) and to have parents who did not wear spectacles (43 of 48 [89.6%] vs 37 of 50 [74.0%]). Children not followed up in the custom-made arm were more likely to have a literate father (33 of 50 [66.0%] vs 27 of 48 [56.3%]) and better presenting VA (32 of 50 [64.0%] vs 29 of 48 [60.4%]).
Table 2. Characteristics of Children in Both Arms of the Trial by Follow-up Status.
| Characteristic | Study Group, No. (%)a | |||
|---|---|---|---|---|
| Ready-Made Spectacles (n = 232) |
Custom-Made Spectacles (n = 228) |
|||
| Followed Up (n = 184) | Lost to Follow-up (n = 48) |
Followed Up (n = 178) | Lost to Follow-up (n = 50) |
|
| Sociodemographic | ||||
| Age, mean (SD) [range] | 13.3 (1.3) [11 to 15] | 13.8 (1.2) [11 to 15] | 13.6 (1.3) [11 to 15] | 13.7 (1.1) [11 to 15] |
| Female | 93 (50.5) | 18 (37.5) | 87 (48.9) | 29 (58.0) |
| Rural school | 56 (30.4) | 17 (35.4) | 56 (31.5) | 17 (34.0) |
| Parental | ||||
| Literacy | ||||
| Father only | 31 (16.8) | 7 (14.6) | 41 (23.0) | 16 (32.0) |
| Mother only | 31 (16.8) | 7 (14.6) | 33 (18.5) | 9 (18.0) |
| Both parents | 70 (38.0) | 20 (41.7) | 63 (35.4) | 17 (34.0) |
| Neither parent | 52 (28.3) | 14 (29.2) | 41 (23.0) | 8 (16.0) |
| Spectacle wear | ||||
| Father only | 21 (11.4) | 4 (8.3) | 21 (11.8) | 8 (16.0) |
| Mother only | 17 (9.2) | 1 (2.1) | 15 (8.4) | 4 (8.0) |
| Both parents | 6 (3.3) | 0 | 2 (1.1) | 1 (2.0) |
| Neither parent | 140 (76.1) | 43 (89.6) | 140 (78.7) | 37 (74.0) |
| Clinical | ||||
| Presenting VA in better eye | ||||
| <6/9 to 6/12 | 47 (25.5) | 15 (31.3) | 46 (25.8) | 17 (34.0) |
| <6/12 to 6/18 | 61 (33.2) | 14 (29.2) | 57 (32.0) | 15 (30.0) |
| <6/18 to 6/60 | 73 (39.7) | 18 (37.5) | 68 (38.2) | 17 (34.0) |
| <6/60 | 3 (1.6) | 1 (2.1) | 7 (3.9) | 1 (2.0) |
| SE (better eye), mean (SD) [range] | −1.49 (0.88) [0.50 to −4.50] | −1.58 (1.07) [−0.50 to −5.50] | −1.46 (1.28) [2.50 to −9.50] | −1.30 (0.93) [2.00 to −3.50] |
Abbreviations: SE, spherical equivalent; VA, visual acuity.
Percentages have been rounded and may not total 100.
Overall, 270 of 362 children (74.6%) were wearing their spectacles or had them at school, including 139 of 184 (75.5%) in the ready-made arm and 131 of 178 (73.6%) in the custom-made arm. The risk difference between the 2 arms was 1.8% (95% CI, −7.1% to 10.8%). The proportion of children given spectacles and wearing them were 126 (68.5%) in the ready-made arm and 112 (62.9%) in the custom-made arm. Other children had their spectacles with them (13 [7.1%] in the ready-made and 19 [10.7%] in the custom-made arms).
Discussion
In our trial, most of the children undergoing assessment were eligible for ready-made spectacles, as reported in the 2 previous studies. At the 3- to 4-month follow-up, spectacle wear was similar in both arms. These important findings suggest that ready-made spectacles, which can be purchased in bulk at very low cost, would be suitable for most children with uncorrected REs in this setting without compromising spectacle wear. In addition to the lower purchase cost, ready-made spectacles can be dispensed on site at the time of refraction, which reduces the cost of dispensing the optician’s time and visits to schools by clinicians. In some programs, children are given a prescription for spectacles that parents collect from the opticians or the eye department. Ready-made spectacles delivered on site would, therefore, reduce travel and opportunity costs for parents. However, dispensing ready-made spectacles in schools would require a relatively large inventory of frames (sizes, colors, and shapes) with a range of powers. A recent innovation, termed clip-and-go spectacles, would reduce the inventory required. Lenses of the same shape are used for each eye, and lenses of relevant powers are clipped into frames. Pilot studies could provide information on frame preference, sizes needed, and range of powers required, all of which are likely to be context dependent.
Strengths
The rate of spectacle wear in our trial was much higher than in other studies of children of similar ages. Several explanations may exist. First, in our trial, only children with significant uncorrected RE who had improvement of 2 or more lines in VA in the better-seeing eye were prescribed spectacles, unlike the trial by Zeng at al. Second, children underwent refraction only if both eyes had a presenting VA of less than 6/9. Most other studies define screening failure as a reduced VA in 1 or both eyes, and in the absence of prescribing guidelines, many children are prescribed spectacles when they already have good VA in 1 eye. This practice decreases spectacle wear because children do not perceive any benefit. How screening failure is defined and use of prescribing guidelines are important to ensure that children are only prescribed spectacles if they have the potential to benefit. Another difference was that children were given the opportunity to choose spectacle frames they preferred. Studies frequently report that if children do not like the appearance of their spectacles, they are less likely to wear them. Comparison with other studies is difficult because definitions of spectacle wear and intervals from dispensing to follow-up vary among studies. The trial by Zeng et al had a superiority design and was powered to detect a 15% difference in spectacle wear; the study had a short follow-up, and the definition of significant RE was not based on improvement in VA with correction. In our trial, significant RE was clearly defined, follow-up was 3 to 4 months, and we used more established ways of assessing spectacle wear.
Other strengths of our study include the noninferiority design; the large sample size, which was representative of the school-going population in the study area; and the primary outcome assessed by direct observation, as in other studies, instead of self-report, which may induce response bias, particularly because the trial involved children. The findings can, therefore, be extrapolated to other children aged 11 to 15 years attending school in this part of India. However, the proportion of children eligible for ready-made spectacles is likely to vary across India because the type and degree of REs vary.
Limitations
A limitation of this study was loss to follow-up of children who had left school or moved to another school in a different location. However, characteristics of those followed up and those lost to follow-up are similar. Another limitation was assessment of spectacle wear at 3 to 4 months rather than a longer period. Although longer follow-up would be desirable, children often move schools at the end of the academic year, making follow-up difficult.
Conclusions
Our study is the first, to our knowledge, to use clearly defined prescribing guidelines, which may explain the high rates of spectacle wear at follow-up. However, because this approach was used in both arms, other factors may also have been important. Additional studies may be of value to address the effect of prescribing guidelines on spectacle wear among children.
Trial Protocol.
References
- 1.Robaei D, Huynh SC, Kifley A, Mitchell P. Correctable and non-correctable visual impairment in a population-based sample of 12-year-old Australian children. Am J Ophthalmol. 2006;142(1):112-118. [DOI] [PubMed] [Google Scholar]
- 2.Murthy GVS, Gupta SK, Bachani D. The Principles and Practices of Community Ophthalmology. New Delhi, India: Community Ophthalmology Section, RP Centre, All India Institute of Medical Sciences; 2002. [Google Scholar]
- 3.He M, Huang W, Zheng Y, Huang L, Ellwein LB. Refractive error and visual impairment in school children in rural southern China. Ophthalmology. 2007;114(2):374-382. [DOI] [PubMed] [Google Scholar]
- 4.Resnikoff S, Pascolini D, Mariotti SP, Pokharel GP. Global magnitude of visual impairment caused by uncorrected refractive errors in 2004. Bull World Health Organ. 2008;86(1):63-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fricke TR, Holden BA, Wilson DA, et al. . Global cost of correcting vision impairment from uncorrected refractive error. Bull World Health Organ. 2012;90(10):728-738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kodjebacheva G, Brown ER, Estrada L, Yu F, Coleman AL. Uncorrected refractive error among first-grade students of different racial/ethnic groups in southern California: results a year after school-mandated vision screening. J Public Health Manag Pract. 2011;17(6):499-505. [DOI] [PubMed] [Google Scholar]
- 7.Pizzarello L, Tilp M, Tiezzi L, Vaughn R, McCarthy J. A new school-based program to provide eyeglasses: ChildSight. J AAPOS. 1998;2(6):372-374. [DOI] [PubMed] [Google Scholar]
- 8.Morgan IG, Ohno-Matsui K, Saw SM. Myopia. Lancet. 2012;379(9827):1739-1748. [DOI] [PubMed] [Google Scholar]
- 9.Pan CW, Ramamurthy D, Saw SM. Worldwide prevalence and risk factors for myopia. Ophthalmic Physiol Opt. 2012;32(1):3-16. [DOI] [PubMed] [Google Scholar]
- 10.Dandona R, Dandona L, Srinivas M, et al. . Refractive error in children in a rural population in India. Invest Ophthalmol Vis Sci. 2002;43(3):615-622. [PubMed] [Google Scholar]
- 11.Kalikivayi V, Naduvilath TJ, Bansal AK, Dandona L. Visual impairment in school children in southern India. Indian J Ophthalmol. 1997;45(2):129-134. [PubMed] [Google Scholar]
- 12.Murthy GV, Gupta SK, Ellwein LB, et al. . Refractive error in children in an urban population in New Delhi. Invest Ophthalmol Vis Sci. 2002;43(3):623-631. [PubMed] [Google Scholar]
- 13.Maul E, Barroso S, Munoz SR, Sperduto RD, Ellwein LB. Refractive error study in children: results from La Florida, Chile. Am J Ophthalmol. 2000;129(4):445-454. [DOI] [PubMed] [Google Scholar]
- 14.Wedner S, Masanja H, Bowman R, Todd J, Bowman R, Gilbert C. Two strategies for correcting refractive errors in school students in Tanzania: randomised comparison, with implications for screening programmes. Br J Ophthalmol. 2008;92(1):19-24. [DOI] [PubMed] [Google Scholar]
- 15.Castanon Holguin AM, Congdon N, Patel N, et al. . Factors associated with spectacle-wear compliance in school-aged Mexican children. Invest Ophthalmol Vis Sci. 2006;47(3):925-928. [DOI] [PubMed] [Google Scholar]
- 16.Rustagi N, Uppal Y, Taneja DK. Screening for visual impairment: outcome among schoolchildren in a rural area of Delhi. Indian J Ophthalmol. 2012;60(3):203-206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Li L, Song Y, Liu X, et al. . Spectacle acceptance among secondary school students in rural China: the Xichang Pediatric Refractive Error Study (X-PRES)—report 5. Invest Ophthalmol Vis Sci. 2008;49(7):2895-2902. [DOI] [PubMed] [Google Scholar]
- 18.Messer DH, Mitchell GL, Twelker JD, Crescioni M; CLEERE Study Group . Spectacle wear in children given spectacles through a school-based program. Optom Vis Sci. 2012;89(1):19-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Congdon N, Zheng M, Sharma A, et al. . Prevalence and determinants of spectacle nonwear among rural Chinese secondary schoolchildren: the Xichang Pediatric Refractive Error Study Report 3. Arch Ophthalmol. 2008;126(12):1717-1723. [DOI] [PubMed] [Google Scholar]
- 20.Robaei D, Kifley A, Rose KA, Mitchell P. Refractive error and patterns of spectacle use in 12-year-old Australian children. Ophthalmology. 2006;113(9):1567-1573. [DOI] [PubMed] [Google Scholar]
- 21.Gogate P, Mukhopadhyaya D, Mahadik A, et al. . Spectacle compliance amongst rural secondary school children in Pune district, India. Indian J Ophthalmol. 2013;61(1):8-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zeng Y, Keay L, He M, et al. . A randomized, clinical trial evaluating ready-made and custom spectacles delivered via a school-based screening program in China. Ophthalmology. 2009;116(10):1839-1845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.von-Bischhoffshausen FB, Muñoz B, Riquelme A, Ormeño MJ, Silva JC. Spectacle-wear compliance in school children in Concepción Chile. Ophthalmic Epidemiol. 2014;21(6):362-369. [DOI] [PubMed] [Google Scholar]
- 24.Zhou Z, Chen T, Jin L, et al. . Self-refraction, ready-made glasses and quality of life among rural myopic Chinese children: a non-inferiority randomized trial [published online June 20, 2016]. Acta Ophthalmol. doi:10.1111/aos.13149 [DOI] [PubMed] [Google Scholar]
- 25.National Institute for Health Research Non-inferiority trials. http://www.rds-sc.nihr.ac.uk/planning-a-study/study-design/quantitative-studies/clinical-trials/non-inferiority-trials/ Updated August 11, 2016. Accessed January 22, 2017.
- 26.Morjaria P, Murali K, Evans J, Gilbert C. Spectacle wearing in children randomised to ready-made or custom spectacles, and potential cost savings to programmes: study protocol for a randomised controlled trial. Trials. 2016;17:36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Piaggio G, Elbourne DR, Pocock SJ, Evans SJ, Altman DG; CONSORT Group . Reporting of noninferiority and equivalence randomized trials: extension of the CONSORT 2010 statement. JAMA. 2012;308(24):2594-2604. [DOI] [PubMed] [Google Scholar]
- 28.World Medical Association World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191-2194. doi: 10.1001/jama.2013.281053 [DOI] [PubMed] [Google Scholar]
- 29.Sealed Envelope Ltd. Power calculator for binary outcome non-inferiority trial. https://www.sealedenvelope.com/power/binary-noninferior/. 2012. Accessed September 22, 2014.
- 30.Aldebasi YH. A descriptive study on compliance of spectacle-wear in children of primary schools at Qassim Province, Saudi Arabia. Int J Health Sci (Qassim). 2013;7(3):291-299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Khandekar R, Mohammed AJ, Al Raisi A. Compliance of spectacle wear and its determinants among schoolchildren of Dhakhiliya region of Oman: a descriptive study. J Sci Res Med Sci. 2002;4(1-2):39-43. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Trial Protocol.