Abstract
Context:
Few researchers have identified intrinsic risk factors for shoulder injury in team handball players by analyzing measurements of maximal isokinetic rotator muscle strength.
Objective:
To identify possible intrinsic risk factors for shoulder injury by analyzing measurements of maximal isokinetic rotator muscle strength.
Design:
Cross-sectional study.
Setting:
Male team handball senior divisions (the highest level) in France and Belgium.
Patients or Other Participants:
A total of 108 male high-level handball players (age = 24 ± 4 years, height = 189 ± 6 cm, mass = 87 ± 11 kg) were enrolled.
Main Outcome Measure(s):
All players completed a preseason questionnaire and performed a bilateral isokinetic assessment of the shoulder rotator muscles. On a monthly questionnaire, players reported any shoulder injury that they sustained during the season.
Results:
On the preseason questionnaire, 51 of 108 (47%) participants reported a history of dominant-shoulder injury. A total of 106 participants completed the in-season questionnaire, with 22% (n = 23) reporting a shoulder injury on their dominant side during the subsequent season. Fourteen percent (n = 15) sustained microtraumatic injuries, and 8% (n = 8) described a traumatic injury. Backcourt players had a 3.5-times increased risk of injury during the new season compared with players in other positions. Among the isokinetic results, no risk factor for further injury was identified in handball players with microtraumatic injuries. For traumatic injuries, the concentric maximal strength developed by the internal rotators at high speed (240°/s) in the dominant shoulder was a protective factor against the risk of further injury.
Conclusions:
These results can potentially identify intrinsic risk factors for shoulder injury and may be used to determine potential interventions for reducing this risk in handball players.
Key Words: isokinetic strength, risk factors, rotator cuff weakness, prospective study
Key Points
Preseason isokinetic strength assessment of the shoulder internal and external rotators can potentially identify intrinsic risk factors for shoulder injury in handball players.
Weakness of the shoulder internal rotators at high speed was associated with the risk of traumatic injury.
Among the isokinetic results, no risk factor was identified in handball players with microtraumatic injuries.
Team handball is a high-intensity sport with frequent physical contact between players.1,2 The large numbers of throws and passes, as well as hard body tackles directly to the shoulder, make the shoulder region vulnerable to both acute and overuse injuries.2–4 Seil et al5 found that the upper extremity was involved in 37% of injuries in senior-division male team handball players. Langevoort et al1 analyzed injuries during 6 international handball tournaments and observed that the upper extremity was the third most frequent location. Despite this result and the fact that handball is one of the most popular sports in Europe after soccer, volleyball, and basketball,1 only a few researchers2,5,6 have focused specifically on shoulder injuries.
Measures to prevent sports injuries form part of the “sequence of prevention” and have been described by Van Mechelen et al.7 Reeser et al8 divided risk factors for shoulder pain into 2 main categories: intrinsic and extrinsic. Intrinsic risk factors include weakness or imbalance of the rotator muscles.8 The primary role of the rotator cuff muscles is dynamic stability of the humeral head during active upper extremity movements; when force couples induced by the rotator muscles are not properly balanced or equalized, abnormal glenohumeral mechanics occur.9–12 In the current literature, only a few investigators9–11 have identified intrinsic risk factors for shoulder injury by prospectively analyzing maximal isokinetic rotator muscle strength measurements. Wang and Cochrane11 relied on a small sample (16 players) and showed an association between strength imbalance of the rotators and shoulder injuries in elite volleyball athletes. Forthomme et al10 reported that the eccentric maximal strength developed by the internal rotators (IR) and external rotators (ERs) represented a protective factor in volleyball players (n = 66). Edouard et al9 found that, in female youth handball players (n = 16), a higher injury risk was associated with a rotator ratio imbalance as measured by isokinetic dynamometer. Some researchers12–14 who have included measurements of maximal isometric rotator muscle strength found an association between ER weakness and an increased probability of substantial shoulder problems throughout the season among elite male handball players12 and ER : IR ratio imbalance among baseball players.13,14 Therefore, the purpose of our prospective study was to analyze measurements of maximal rotator muscle strength to identify intrinsic risk factors that could put elite handball players at risk for traumatic (injury arising from contact or a fall) and microtraumatic (injury arising from overuse) dominant-shoulder injuries.
METHODS
Participants
We conducted this prospective cohort study during the 2010–2013 indoor handball seasons and over a single 6-month season for each participant. Volunteers were recruited from the male team handball senior divisions (ie, the highest level). The inclusion criteria were that individuals were able to participate fully in training sessions and competitive activity and had no injuries at the time of the study.
A total of 108 male players (age = 24 ± 4 years, height = 189 ± 6 cm, mass = 87 ± 11 kg) were enrolled in this study. Of these participants, 56% (n = 60) were backcourt players, 81% (n = 88) were right-hand dominant, and 66% (n = 71) had played handball for more than 13 years. We defined the dominant hand as the hand used for throwing the ball. Most players (47%, n = 51) were involved in practices and games for 9 to 12 hours per week. Eighty-three percent (n = 90) of players were involved in regular resistance-training workouts in addition to their handball training, and 64% (n = 69) routinely followed a specific program dedicated to strengthening the shoulder ERs. All participants provided written informed consent, and the study was approved by the Medical Ethics Committee of the University of Liege.
Procedures
All players completed a standardized preseason questionnaire, including information on previous playing experience and shoulder injury. Among other items, this questionnaire asked about the onset and cause of previous dominant-shoulder injuries, previous treatment, diagnosis received, and any reinjury.
Before the start of the handball season, isokinetic assessments were performed by 3 experienced examiners (B.F., J.L.C., S.G.C.). Isokinetic protocol assessments were standardized, and each examiner received precise instructions on how to apply the test procedure consistently. Moreover, all examiners had experience using this protocol. A high level of reliability between examiners for the isokinetic assessment had been established, with an intraclass correlation coefficient ≥0.890 for all measurements (B.F., unpublished data, 2004).
The dominant- and nondominant-shoulder IRs and ERs were assessed using a dynamometer (model Cybex HUMAC NORM; Computer Sports Medicine, Inc, Stoughton, MA). Players were supine, with the upper extremity abducted to 90° in the frontal plane and the elbow flexed to 90° (Figure 1). We chose the test position of the participants based on reproducibility and specificity criteria.15,16 Range of motion was standardized from 50° of internal rotation to 70° of external rotation.15 The isokinetic speeds were 60°/s (3 repetitions) and 240°/s (5 repetitions) in the concentric mode and 60°/s (4 repetitions) in the eccentric mode. These testing sequences were preceded by warm-up concentric repetitions at 120°/s and 3 submaximal familiarization trials at the selected speed. Successive testing velocities were separated by 1 minute of rest.15,16 During the isokinetic evaluation, no participant reported pain that could have altered the maximal force exerted.
Figure 1. .
Isokinetic evaluation of the rotator muscles.
The isokinetic testing enabled us to measure absolute peak torque (PT in newton meters) and calculate body mass relative to peak torque (PT/kg in Nm/kg). Agonist-to-antagonist ratios (ER : IR) were determined using the same speed and contraction mode for the agonist and antagonist muscle groups.15–17 In addition, a mixed ratio (combining ER PT in the eccentric mode at 60°/s and IR PT in the concentric mode at 240°/s) was designed to more accurately approximate the relationship between the shoulder muscles during throwing.16,17
The data for each player were collected during 1 season (each indoor handball season was 6 months) between 2010 and 2013. All players completed a monthly in-season questionnaire (a total of 6 questionnaires for each participant) about any dominant-shoulder injury (physical harm or damage) that they experienced. This in-season questionnaire provided information about the onset and cause of any shoulder injury and the localization of pain. The questionnaire asked whether the player had received a specific diagnosis from a medical professional and whether he had been examined or received a specific treatment. After an absence from sport because of injury, the players were instructed to describe their conditions on returning to participation. The severity of injury was defined on the basis of sporting time missed: minor (absent from sport <1 week), moderate (absent from sport 1 to 3 weeks), or severe (absent >3 weeks). Exposure information requested from the coaches of each team and recorded on a form included the number of training hours, the average attendance for training sessions, and the number and duration of matches. We calculated the incidence rate of shoulder injury and the number of incident injuries divided by total athlete-time at risk, where athlete-time at risk was computed by multiplying the total number of exposures (eg, games and practices) by the number of athletes participating.18 During the season, we contacted the coaches each month by e-mail to obtain injury and exposure data.
Statistical Analysis
Means and standard deviations were calculated for all variables. The Shapiro-Wilk normality test was used to check the normal distribution of the data. A paired t test (dependent values) was used to identify any differences between the dominant and nondominant sides for the isokinetic results. In the retrospective part of the study, we compared mean values using an unpaired t test (independent between players with and players without a history of injury). The Cohen d effect size was calculated to evaluate the strength of the observed changes. Effect sizes less than 0.2, 0.5, or 0.8 were considered negligible, small, or medium, respectively. Effect sizes greater than 0.8 were considered large.
Univariate logistic regression models were used to identify independent predictors of shoulder-injury outcome (ie, risk factors for shoulder injury). Odds ratios and 95% confidence intervals (CIs) were determined for each model.
We performed a 2-way analysis of variance with a Bonferroni post hoc test to identify differences between groups of players for game and practice hours and for the number of shots and goals scored. Results were considered to be different at the 5% critical level (P < .05). Statistical analyses were carried out using SAS (version 9.3 for Windows; SAS Institute Inc, Cary, NC).
RESULTS
On the preseason questionnaire, 51 (47%) participants reported a history of injury to the dominant shoulder. Of these shoulder injuries, 10% (n = 5) were traumatic (luxation, instability, or acromioclavicular lesion), and 90% (n = 46) were overuse microtraumatic injuries (rotator cuff tendinopathy). Half (n = 25) of the injured players did not cease sporting activity due to injury, and those who stopped their activity did so for less than 2 weeks (moderate injury). Only 10% (n = 5) of players with previous injuries had undergone isokinetic assessment before returning to play or practice. Half (n = 25) of the players with previous injuries reported playing with residual pain in their dominant shoulder.
The isokinetic performance of the players' dominant and nondominant shoulders are shown in Table 1. We observed a difference between sides for the IRs (P < .001), which were stronger on the dominant side for all isokinetic conditions. The ERs were stronger in the dominant shoulder in the concentric mode (P = .02 at 60°/s and P = .002 at 240°/s) but were not different between sides in the eccentric mode (P = .07). The ER : IR concentric ratios and mixed ratio were different between the dominant and nondominant shoulders (P < .001 for the ER : IR concentric ratio at 60°/s, P = .009 for the ER : IR concentric ratio at 240°/s, and P < .001 for the mixed ratio), with the lowest ratios on the dominant side.
Table 1. .
Isokinetic Results (Peak Torque in Nm/kg and Ratios) for the Dominant and Nondominant Shoulders of Handball Players (N = 108)
| Variable |
Shoulder |
P Value |
Cohen d Effect Size |
|
| Dominant |
Nondominant |
|||
| Mean ± SD |
||||
| Internal rotators, Nm/kg | ||||
| Concentric mode at 60°/s | 0.70 ± 0.15 | 0.62 ± 0.14 | <.001 | 0.77 |
| Concentric mode at 240°/s | 0.55 ± 0.14 | 0.49 ± 0.12 | <.001 | 0.79 |
| Eccentric mode at 60°/s | 0.78 ± 0.20 | 0.69 ± 0.17 | <.001 | 0.59 |
| External rotators, Nm/kg | ||||
| Concentric mode at 60°/s | 0.50 ± 0.09 | 0.49 ± 0.08 | .02 | 0.23 |
| Concentric mode at 240°/s | 0.41 ± 0.08 | 0.39 ± 0.08 | .002 | 0.38 |
| Eccentric mode at 60°/s | 0.63 ± 0.11 | 0.61 ± 0.13 | .07 | 0.18 |
| Ratio of external rotators : internal rotators | ||||
| Concentric mode at 60°/s | 0.73 ± 0.12 | 0.81 ± 0.13 | <.001 | −0.54 |
| Concentric mode at 240°/s | 0.78 ± 0.14 | 0.82 ± 0.17 | .009 | −0.26 |
| Mixed ratio (external rotators in the eccentric mode at 60°/s to internal rotators in the concentric mode at 240°/s) | 1.20 ± 0.30 | 1.30 ± 0.35 | <.001 | −0.43 |
The isokinetic profiles of the players with and the players without a history of shoulder injury appear in Table 2. No difference was found in the isokinetic results (PT/kg of body mass and ratios) between players with and players without previous shoulder injury during the preseason isokinetic assessment (P > .05).
Table 2. .
Isokinetic Results (Peak Torque in Nm/kg and Ratios) for the Dominant Shoulder Between Players With and Without a History of Injury (N = 108)
| Variable |
Injury History (n = 51) |
No Injury History (n = 57) |
P Value |
Cohen d Effect Size |
| Mean ± SD |
||||
| Internal rotators, Nm/kg | ||||
| Concentric mode at 60°/s | 0.70 ± 0.15 | 0.71 ± 0.15 | .77 | 0.06 |
| Concentric mode at 240°/s | 0.55 ± 0.13 | 0.54 ± 0.14 | .56 | 0.12 |
| Eccentric mode at 60°/s | 0.79 ± 0.20 | 0.76 ± 0.20 | .58 | 0.11 |
| External rotators, Nm/kg | ||||
| Concentric mode at 60°/s | 0.50 ± 0.10 | 0.51 ± 0.08 | .58 | 0.11 |
| Concentric mode at 240°/s | 0.42 ± 0.09 | 0.41 ± 0.09 | .75 | 0.06 |
| Eccentric mode at 60°/s | 0.63 ± 0.12 | 0.62 ± 0.10 | .51 | 0.13 |
| Ratio of external rotators : internal rotators | ||||
| Concentric mode at 60°/s | 0.73 ± 0.12 | 0.74 ± 0.12 | .67 | 0.09 |
| Concentric mode at 240°/s | 0.77 ± 0.13 | 0.79 ± 0.16 | .33 | 0.19 |
| Mixed ratio (external rotators in the eccentric mode at 60°/s to internal rotators in the concentric mode at 240°/s) | 1.19 ± 0.28 | 1.21 ± 0.33 | .72 | 0.07 |
A total of 106 (98%) players completed the in-season questionnaire through the end of the season (2 players were obliged to stop practice midseason: 1 due to a finger fracture and 1 due to an anterior cruciate ligament lesion); 22% (n = 23) of the players sustained a shoulder injury on their dominant side during the season. This corresponds to an incidence rate of 1.13 shoulder injuries per 1000 player-hours. Fourteen percent (n = 15) sustained microtraumatic injuries during the season, and 8% (n = 8) experienced traumatic injuries. A total of 74% (n = 17) of the injured players stopped their sport activity due to shoulder injury for a maximum of 1 week, thus the injury was classified as minor.
Backcourt players had 3.5 times more risk of injury during the new season than other player positions (odds ratio = 3.24; 95% CI = 1.306, 8.033; P = .01). Defensive players had 8 times less risk of injury during the following season than offensive players (odds ratio = 0.129; 95% CI = 0.021, 0.812; P = .03).
The players with traumatic injuries during the observed season participated on average in more game hours per month (25.38 ± 11.77 hours) than the players with microtraumatic injuries (19.38 ± 10.05 hours) and uninjured players (22.85 ± 10.27 hours), although no difference was noted among groups (F2,95 = 0.99, P = .38). Players with traumatic injuries showed a trend toward more shooting (F2,78 = 0.30, P = .74) and goal scoring (F2,78 = 0.18, P = .84) than the others, but the values were not different from those of the players with microtraumatic injuries or uninjured players.
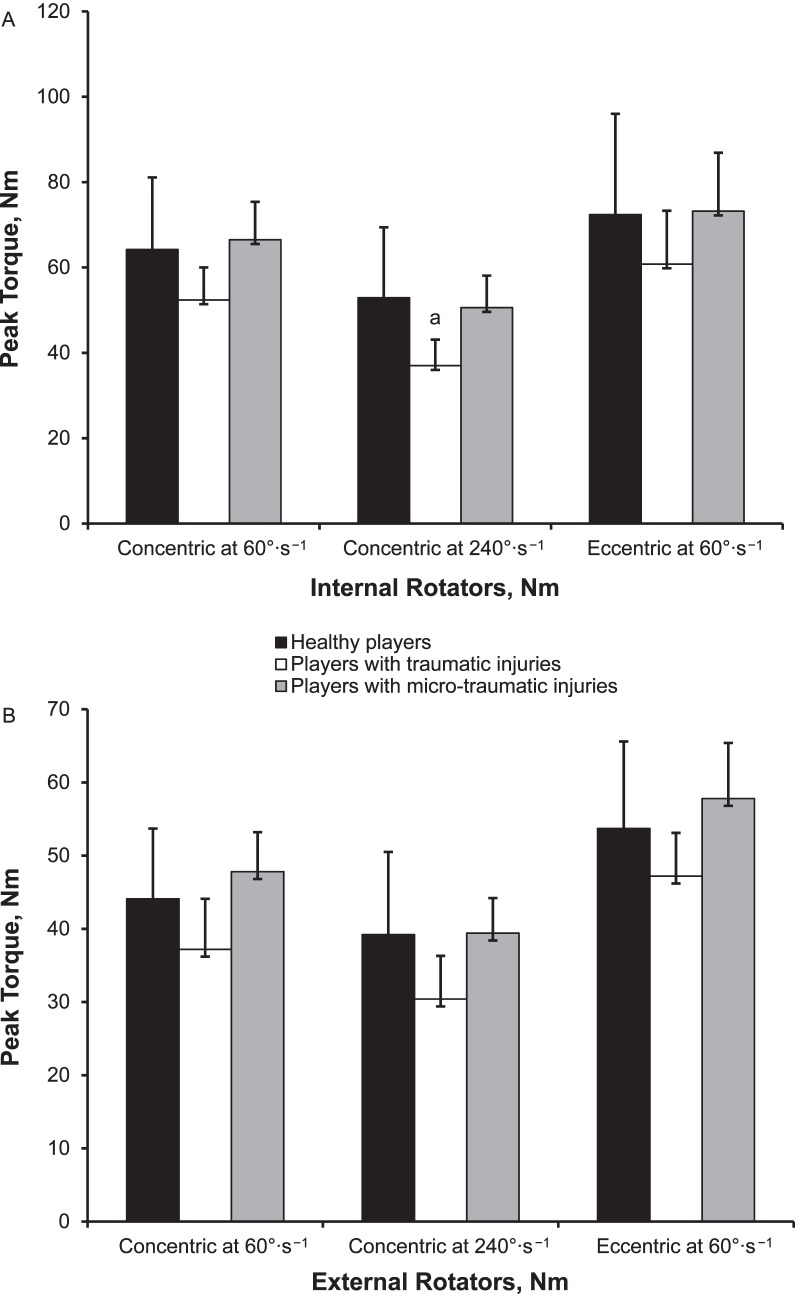
During our study, previous injury was not a risk factor for new injury (P = .28). The isokinetic results (PT in Nm, ratios) for uninjured players, players with traumatic dominant-shoulder injuries (n = 8), and players with microtraumatic dominant-shoulder injuries sustained during the subsequent season (n = 15) are provided in Figure 2. Interestingly, players with traumatic injuries sustained during the following season had weaker IRs (Nm) in the concentric mode at high speed than did uninjured players (identified using univariate logistic regression models). The calculated odds ratio showed that the maximal concentric strength developed by the IRs at high speed (240°/s) was a protective factor (odds ratio = 0.93; 95% CI = 0.865, 1.000; P = .049) against traumatic injury. By contrast, we did not identify any risk factors among the isokinetic results for the handball players with microtraumatic injuries.
Figure 2. .
Isokinetic results for, A, internal-rotator muscles and, B, external-rotator muscles in uninjured players, players with traumatic injuries, and players with microtraumatic injuries. a Independent predictor of shoulder-injury outcome (univariate logistic regression models, P < .05).
DISCUSSION
The aim of our study was to retrospectively and prospectively identify risk factors for dominant-shoulder injury among high-level handball players using isokinetic measures. A total of 108 male team handball players, mainly from the highest division level, were enrolled. At the preseason assessment, 51 (47%) players had already experienced a dominant-shoulder injury. Most (90%, n = 46) injuries resulted from overuse. Only half (n = 25) of injured players had stopped their sport activity due to pain for up to 2 weeks (moderate injury). Myklebust et al3 reported that 57% of 179 female Norwegian top-level handball players surveyed were affected by previous shoulder pain. In our study, half of the players with a history of shoulder injury said they played with residual pain in their dominant shoulder. Myklebust et al3 confirmed that a substantial number of handball players continued to play despite shoulder pain. Nevertheless, our participants with a history of shoulder injury were at no more risk of experiencing another injury in their dominant shoulder (P = .28).
At the beginning of the season, all players performed a bilateral isokinetic shoulder assessment. The positioning of the participants was chosen based on reproducibility and specificity criteria. Isokinetic assessment of the IRs and ERs was conducted in the supine position with the extremity in 90° of abduction in the frontal plane to simulate, in a reproducible manner, the motion of throwing or shooting.10,15 The supine position in 90° of abduction is associated with the lowest coefficient of variation (7.1%–11.8%) and smallest detectable difference (7–15.9 Nm) for PT and strength ratios.15 We do not recommend using the seated position, as Forthomme et al15 found this offered relatively poor reproducibility for ER PT and the ER : IR ratios. The concentric and eccentric modes of contraction used in our protocol reflected the different modes of contraction used during a throwing motion, although testing speeds during the isokinetic evaluation were far lower than those that occur during throwing.16 Successive testing velocities were separated by a 1-minute rest period to allow complete phosphagen recovery, given the duration of maximal effort (less than 12 seconds) for each muscle group.15
The handball players in our study had stronger IRs on the dominant side than on the nondominant side because the dominant extremity is required to generate a larger amount of torque in internal rotation to project the ball with sufficient velocity.19 Consequently, the ER : IR ratios were lower in the dominant than in the nondominant shoulder. Andrade et al20 also reported muscular imbalances in handball players resulting from daily sport practice; the lower ER : IR ratios in the dominant shoulder reflected greater strengthening of the IRs than the ERs.
We did not find any muscle-strength differences in the isokinetic profiles (PT, PT/kg, ratios) between players with and players without a history of injury. Forthomme et al10 observed similar results in a cross-sectional study among high-level volleyball players, reporting no isokinetic differences between players with and those without a history of shoulder injury.
Ninety-eight percent (n = 106) of our players completed the prospective protocol, and 22% (n = 23) of these players presented with a dominant-shoulder injury during the following season. Chronic shoulder injuries appeared to be the most frequent injury among the players (14%, n = 15), although acute shoulder injuries were not uncommon (8%, n = 8), as noted by Seil et al5 and Langevoort et al.1
We found that backcourt players were more at risk of injury (3.5 times more) than other positions, and a defensive role in the game protected against injury (8 times less risk of injury than for offensive roles). In fact, backcourt players are physically different from other players in handball and have different roles in practice. They are larger and undertake many more physical collisions with other large players. The injury pattern varied by player position and contact situation, a pattern Seil et al5 also demonstrated. They5 showed an increased rate of upper extremity injuries in wing and backcourt players; 89% of participants with shoulder-injury symptoms related to overuse were backcourt players. Olsen et al21 found that most injuries occurred during the attacking phase to backcourt players, and more than half occurred during contact with an opponent. In our study, the handball players with traumatic injuries showed a trend toward more game hours of participation and more shooting and goal scoring than those with microtraumatic injuries or uninjured players, but the values were not significantly different. Seil et al5 also observed that the majority of acute shoulder injuries were in players who threw the most (backcourt players). According to Olsen et al,22 the factors most strongly associated with injury among baseball pitchers were overuse and fatigue. High pitch velocity and participation in showcases were also associated with increased risk for injury.22 Similarly, Lyman et al23 identified risk factors among youth baseball pitchers for shoulder pain, which included decreased satisfaction with one's pitching, arm fatigue while pitching during games, throwing more than 75 pitches per game, and throwing fewer than 300 pitches per season.
In a recent study, Clarsen et al12 found an association between isometric ER weakness and an increased probability of substantial shoulder problems throughout the season among elite handball players. Similar findings have been reported in studies of baseball pitchers, in whom preseason weakness or ER and supraspinatus abduction strength were associated with in-season throwing-related injury resulting in surgical intervention.14 Trakis et al13 found a relationship between ER weakness or a low ER : IR ratio and throwing-related injury. Those results cannot be directly compared with those of other studies, as different methods were used to measure strength. Edouard et al9 showed that the relative risk of injury was 2.57 when handball players had an imbalanced muscle-strength profile as measured by isokinetic dynamometer. In 16 female elite handball players, they found a lower ER : IR ratio for the dominant than the nondominant side. We did not identify this association between agonist : antagonist imbalances and dominant-shoulder injury among our 106 male elite handball players. In a study of risk factors for tendinopathy among high-level volleyball players,10 the eccentric maximal strength developed by the IRs and ERs represented a protective factor in volleyball players. Wang and Cochrane11 showed that dominant-side average eccentric ER strength was weaker than the concentric IR strength in elite volleyball athletes and that this was associated with shoulder injury. We did not observe this association between eccentric maximal weakness of the rotator cuff and injury to the dominant shoulder among elite handball players. This result could be due to the maximal eccentric IR and ER performance measured during the isokinetic evaluation, which was higher than in volleyball players.10 The preventive training program that was followed by 64% (n = 69) of our 108 participants or the difference in specific movements used could explain the better eccentric results among handball players.
Considering the risk factors in our isokinetic results, players with traumatic dominant-shoulder injury during the subsequent season showed IR weakness at 240°/s in the concentric mode on the dominant side. In fact, the maximal concentric strength developed by the IRs at high speed represented a protective factor in the handball players. A collision-type injury is more likely to occur during throwing or blocking; the shooter's extremity may be pulled during the cocking phase or blocked during the acceleration, deceleration, or follow-through phase.6 The link between traumatic injury and IR weakness at high concentric speed could correspond to increased difficulty for shooters when moving their extremity to rapidly escape blocking actions imposed by a defender during shooting. Moreover, internal rotation at high speed is of paramount importance for the acceleration phase of throwing. The strength developed by the IRs at fast speed in the concentric mode should also protect the shoulder against traumatic injury by providing a well-centered glenohumeral position. Myers et al24 reported that patients with instability demonstrated suppressed pectoralis major and biceps brachii mean reflexive activation and suppressed supraspinatus-subscapularis co-activation. These muscle-activation alterations identified in patients with glenohumeral instability may contribute to recurrent instability episodes and traumatic injuries during throwing activities.24 We did not find any risk factors for the other aspects of isokinetic assessment (other speed, mode of contraction, or direction of movement) among handball players. A preventive program with controlled concentric contractions, including internal rotation at high speed, may benefit individual handball players with IR weakness, and future research in this area is needed.
Our study had limitations. The isokinetic evaluation should have been accompanied by morphostatic assessment, such as glenohumeral passive rotation, scapular position, or posterior rotator cuff stiffness. Another limitation was the retrospective nature of the preseason questionnaire and possible inaccurate reporting of some events. In addition, the diagnoses received from different medical practitioners in the absence of a clear guideline for reporting may have led to variations in the data. Moreover, the information obtained from the questionnaire was subjective and provided by the athletes rather than by medical professionals.
CONCLUSIONS
Our results clearly documented different injury demographics according to field position (3.5 times or 350% higher risk for backcourt players). We reported a preliminary finding of reduced risk (8%) for traumatic but not overuse shoulder injury.
ACKNOWLEDGMENTS
We thank Mrs A. Depaifve for her kind and efficient technical assistance; Lucas Giacomino, Clement Gault, Delphine Schiettecatte, Nicolas Wauters, and Catherine Theunissen for their help with the experiment; and Laurence Seidel from Adelin Albert's team for assisting with statistical analysis. We also thank the French and Belgium Handball National Federations and the French and Belgium Handball Leagues. We thank the medical staff and the players of the teams who took part in the study.
REFERENCES
- 1. Langevoort G, Myklebust G, Dvorak J, Junge A. . Handball injuries during major international tournaments. Scand J Med Sci Sports. 2007; 17 4: 400– 407. [DOI] [PubMed] [Google Scholar]
- 2. Vlak T, Pivalica D. . Handball: the beauty or the beast. Croat Med J. 2004; 45 5: 526– 530. [PubMed] [Google Scholar]
- 3. Myklebust G, Hasslan L, Bahr R, Steffen K. . High prevalence of shoulder pain among elite Norwegian female handball players. Scand J Med Sci Sports. 2013; 23 3: 288– 294. [DOI] [PubMed] [Google Scholar]
- 4. Reckling C, Zantop T, Petersen W. . Epidemiology of injuries in juvenile handball players [in German]. Sportverl Sportschad. 2003; 17 3: 112– 117. [DOI] [PubMed] [Google Scholar]
- 5. Seil R, Rupp S, Tempelhof S, Kohn D. . Sports injuries in team handball: a one-year prospective study of sixteen men's senior teams of a superior nonprofessional level. Am J Sports Med. 1998; 26 5: 681– 687. [DOI] [PubMed] [Google Scholar]
- 6. Miskulin PM, Jaklinovic Z, Vrgoc G. . Shoulder issues in handball: are there any or are handball players either lucky, well-prepared or just under-investigated? Aspetar Sports Med J. 2014; 3 targeted topic 3: 160– 165. [Google Scholar]
- 7. Van Mechelen W, Hlobil H, Kemper HC. . Incidence, severity, aetiology and prevention of sports injuries. Sports Med. 1992; 14 2: 82– 99. [DOI] [PubMed] [Google Scholar]
- 8. Reeser JC, Verhagen E, Briner WW, Askeland TI, Bahr R. . Strategies for the prevention of volleyball related injuries. Br J Sports Med. 2006; 40 7: 594– 600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Edouard P, Degache F, Oullion R, Plessis JY, Gleizes-Cervera S, Calmels P. . Shoulder strength imbalances as injury risk in handball. Int J Sports Med. 2013; 34 7: 654– 660. [DOI] [PubMed] [Google Scholar]
- 10. Forthomme B, Wieczorek V, Frisch A, Crielaard JM, Croisier JL. . Shoulder pain among high-level volleyball players and preseason features. Med Sci Sports Exerc. 2013; 45 10: 1852– 1860. [DOI] [PubMed] [Google Scholar]
- 11. Wang HK, Cochrane T. . Mobility impairment, muscle imbalance, muscle weakness, scapular asymmetry and shoulder injury in elite volleyball athletes. J Sports Med Phys Fitness. 2001; 41 3: 403– 410. [PubMed] [Google Scholar]
- 12. Clarsen B, Bahr R, Andersson SH, Munk R, Myklebust G. . Reduced glenohumeral rotation, external rotation weakness and scapular dyskinesis are risk factors for shoulder injuries among elite male handball players: a prospective cohort study. Br J Sports Med. 2014; 48 17: 1327– 1333. [DOI] [PubMed] [Google Scholar]
- 13. Trakis JE, McHugh MP, Caracciolo PA, Busciacco L, Mullaney M, Nicholas SJ. . Muscle strength and range of motion in adolescent pitchers with throwing-related pain: implications for injury prevention. Am J Sports Med. 2008; 36 11: 2173– 2178. [DOI] [PubMed] [Google Scholar]
- 14. Byram IR, Bushnell BD, Dugger K, Charron K, Harrell FE Jr, Noonan TJ. . Preseason shoulder strength measurements in professional baseball pitchers: identifying players at risk for injury. Am J Sports Med. 2010: 38 7: 1375– 1382. [DOI] [PubMed] [Google Scholar]
- 15. Forthomme B, Dvir Z, Crielaard JM, Croisier JL. . Isokinetic assessment of the shoulder rotators: a study of optimal test position. Clin Physiol Funct Imaging. 2011; 31 3: 227– 232. [DOI] [PubMed] [Google Scholar]
- 16. Forthomme B, Croisier JL, Ciccarone G, Crielaard JM, Cloes M. . Factors correlated with volleyball spike velocity. Am J Sports Med. 2005; 33 10: 1513– 1519. [DOI] [PubMed] [Google Scholar]
- 17. Scoville CR, Arciero RA, Taylor DC, Stoneman PD. . End range eccentric antagonist/concentric agonist strength ratios: a new perspective in shoulder strength assessment. J Orthop Sports Phys Ther. 1997; 25 3: 203– 207. [DOI] [PubMed] [Google Scholar]
- 18. Knowles SB, Marshall SW, Guskiewicz KM. . Issues in estimating risks and rates in sports injury research. J Athl Train. 2006; 41 2: 207– 215. [PMC free article] [PubMed] [Google Scholar]
- 19. Bayios IA, Anastasopoulou EM, Sioudris DS, Boudolos KD. . Relationship between isokinetic strength of the internal and external shoulder rotators and ball velocity in team handball. J Sports Med Phys Fitness. 2001; 41 2: 229– 235. [PubMed] [Google Scholar]
- 20. Andrade MS, Vancini RL, de Lira CA, Mascarin NC, Fachina RJ, da Silva AC. . Shoulder isokinetic profile of male handball players of the Brazilian National Team. Braz J Phys Ther. 2013; 17 6: 572– 578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Olsen OE, Myklebust G, Engebretsen L, Bahr R. . Injury pattern in youth team handball: a comparison of two prospective registration methods. Scand J Med Sci Sports. 2006; 16 6: 426– 432. [DOI] [PubMed] [Google Scholar]
- 22. Olsen SJ 2nd, Fleisig GS, Dun S, Loftice J, Andrews JR. . Risk factors for shoulder and elbow injuries in adolescent baseball pitchers. Am J Sports Med. 2006; 34 6: 905– 912. [DOI] [PubMed] [Google Scholar]
- 23. Lyman S, Fleisig GS, Waterbor JW, et al. Longitudinal study of elbow and shoulder pain in youth baseball pitchers. Med Sci Sports Exerc. 2001; 33 11: 1803– 1810. [DOI] [PubMed] [Google Scholar]
- 24. Myers JB, Ju YY, Hwang JH, McMahon PJ, Rodosky MW, Lephart SM. . Reflexive muscle activation alterations in shoulders with anterior glenohumeral instability. Am J Sports Med. 2004; 32 4: 1013– 1021. [DOI] [PubMed] [Google Scholar]