Abstract
This study sought to re-characterize trends and factors affecting electronic dental record (EDR) and technologies adoption by dental practices and the impact of the Health Information Technology for Economic and Clinical Health (HITECH) act on adoption rates through 2012. A 39-question survey was disseminated nationally over 3 months using a novel, statistically-modeled approach informed by early response rates to achieve a predetermined sample. EDR adoption rate for clinical support was 52%. Adoption rates were higher among: (1) younger dentists; (2) dentists ≤ 15 years in practice; (3) females; and (4) group practices. Top barriers to adoption were EDR cost/expense, cost-benefit ratio, electronic format conversion, and poor EDR usability. Awareness of the Federal HITECH incentive program was low. The rate of chairside computer implementation was 72%. Adoption of EDR in dental offices in the United States was higher in 2012 than electronic health record adoption rates in medical offices and was not driven by the HITECH program. Patient portal adoption among dental practices in the United States remained low.
Keywords: Dental Informatics, Dental Records, Dentistry, Electronic Health Records, Meaningful Use
Use of computers in dental offices in the United States has become more commonplace over the last three decades. In 1984, 11% of general dental practices used computers in their offices,1 with rates increasing to >85% of 166,000 dental practices in the United States by 2009.2 While further adoption of electronic dental records (EDRs) by dental practices has been low, substantial growth in adoption specifically of clinical computing and EDRs by U.S. dental practitioners has occurred, especially within the last decade. In a comprehensive investigation through 2006 on adoption, utilization rates, and attitudes toward clinical computing among general U.S. dental practitioners, Schleyer et al1 reported that 25% of dental practitioners used a chairside computer, and 1.8% of dental practitioners were completely paperless. A survey of dentists conducted by the American Dental Association (ADA) from 2006 to 2007 reported further expansion of rates to 55.5% with chairside computers and 9.2% paperless practices.3 A 2010 survey of California dentists4 showed that 23% had fully implemented an EDR in their practice. A recent survey of the Dental Practice-based Research Network reported EDR implementation by 14.3% of solo practitioners and 15.9% of group practitioners.5
The Health Information Technology for Economic and Clinical Health (HITECH) Act authorized $30 billion in incentives to increase the adoption of certified electronic health records (EHRs) for meaningful use.6,7 Incentive payments range from a $44,000 maximum under the Medicare incentive option to $64,000 under the Medicaid program for each eligible provider.6 Although dentists are eligible professionals under the HITECH incentive program, the impact of this program on EDR adoption by dental practices has not been evaluated to date. A proportion of U.S. dentists may not qualify for this incentive program, since they do not meet the minimum requirement of serving a patient population inclusive of a 30% rate of Medicaid beneficiaries. Further, a formal definition of “meaningful use” for dentistry within the context of the regulatory definition is lacking.
Following-up on this historical perspective, this study’s main objective was to gain greater insight into perceptions surrounding current EDR implementation in the dental practice setting and reassess the extent of adoption of EDR systems among a random selection of dental practices in the United States. Two further objectives included: (1) assessing knowledgeability concerning the recent HITECH EHR incentive program and meaningful use among dental practitioners, and (2) obtaining insight into other technology-related practice applications by investigating attitudes towards, and utilization of, clinical computing in dentistry.
Methods
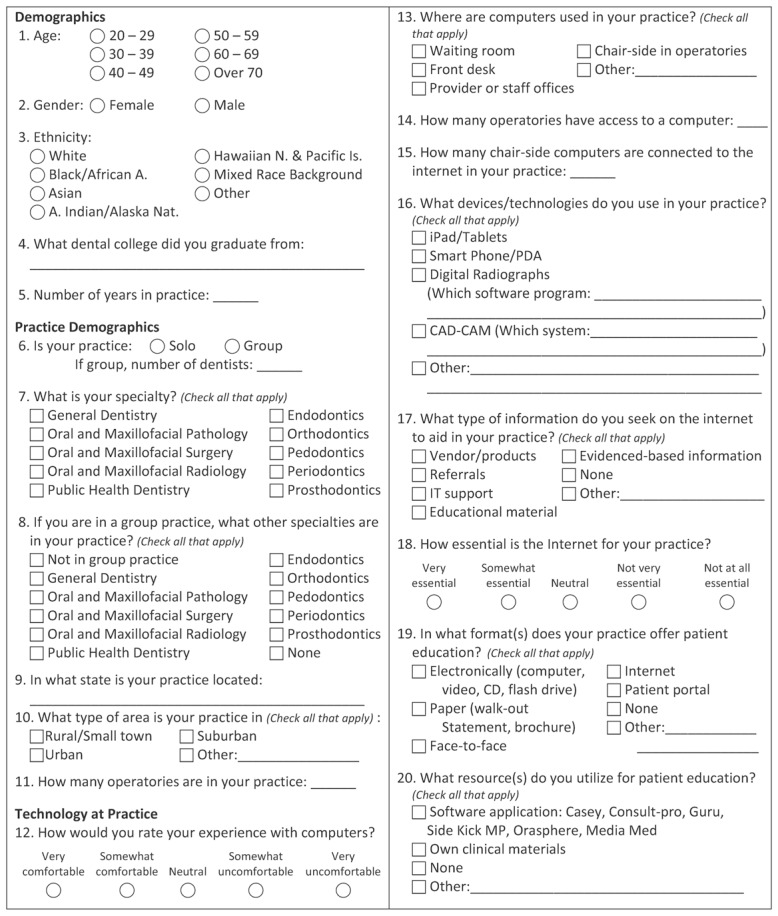
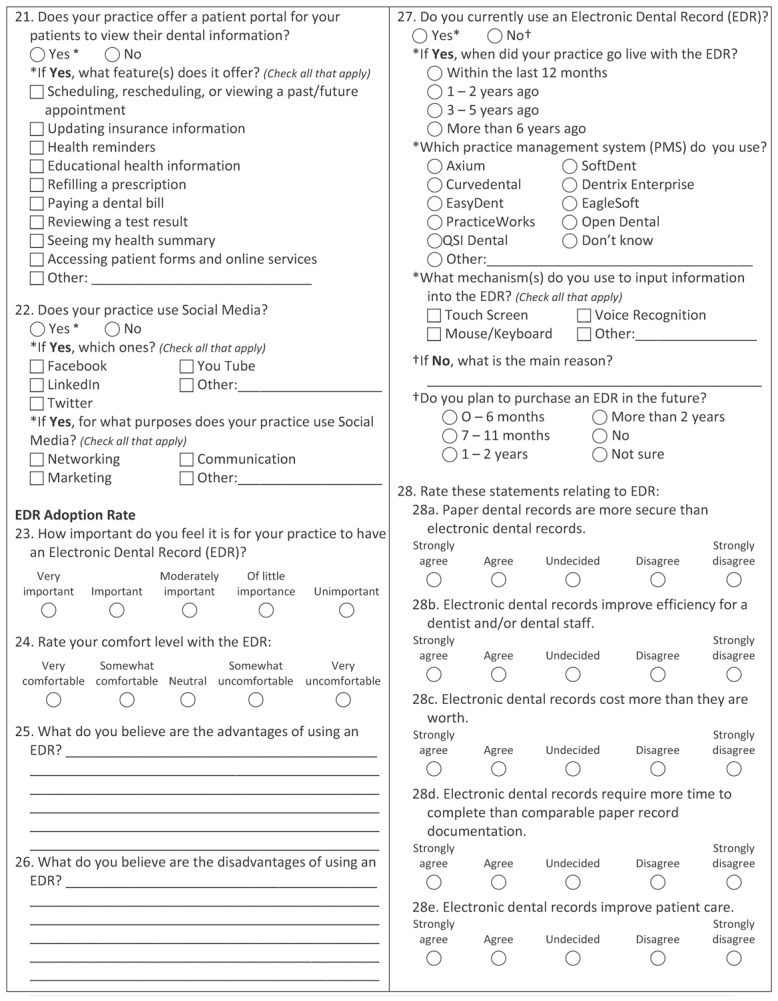
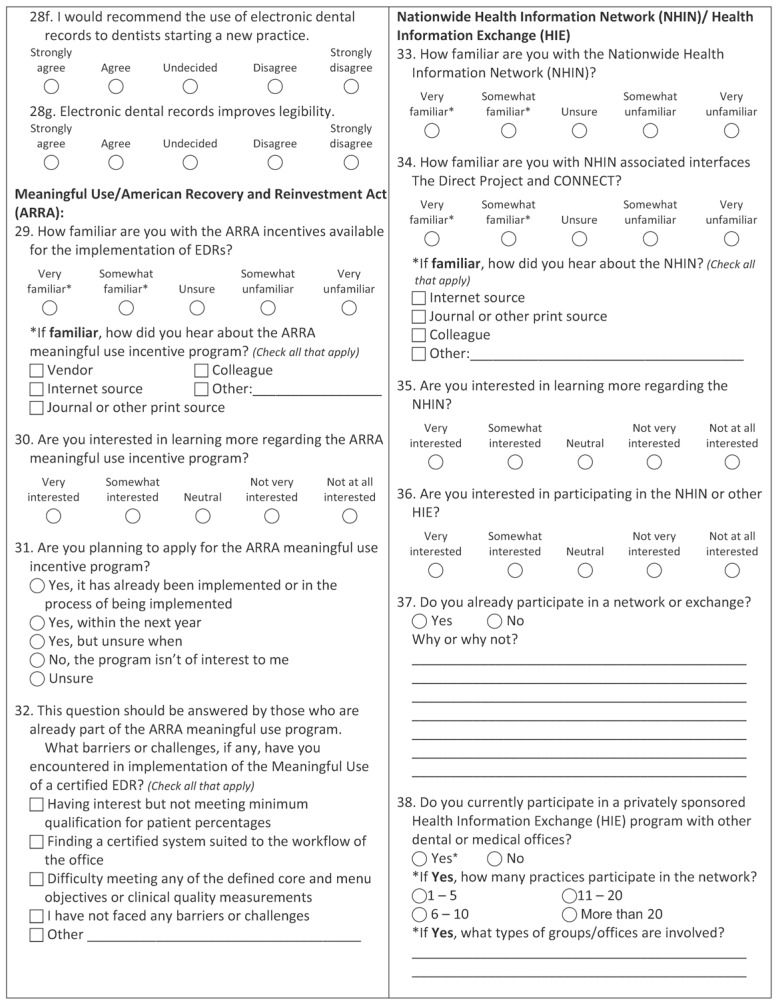
Review of previously-published survey tools revealed that no existing tool satisfactorily encompassed the total focus of the current study. Thus, expansion of a survey tool created by Schleyer et al1 was undertaken, incorporating multi-level questions germane to analyzing study objectives. The 39 questions were grouped into 7 broad categories (Table 1). Face and content validity analysis of the survey was conducted by coauthors with appropriate expertise before use. The research protocol and survey instrument met exemption criteria from ongoing oversight following Institutional Review Board review. The survey tool (Appendix 1) was beta tested by dentists and staff from dental centers operationalized by the Family Health Center of a multi-specialty clinic, in Wisconsin, USA, before dissemination.
Table 1.
Classification of the 39 multi-level questions across seven broad categories.
| Categories by Subject | Category Description |
|---|---|
| Provider demographics | Provider’s age, gender, ethnicity, graduating dental school; years in practice |
| Practice demographic | Type of practice (solo or group practice), areas of specialty; number of staff, geographic location of practice – state, rural, suburban, urban, number of operatories |
| Technology at practice | Use/location of computers, devices/technologies used, Internet use, patient portal, patient education, use of social media |
| EDR adoption | Adoption rates, practice management systems, input mechanisms, comfort level of staff, input regarding advantages and disadvantages of EDR, attitudes and perceptions of EDRs |
| Meaningful Use/American Recovery and Reinvestment Act (ARRA) | Level of familiarity/interest in Meaningful Use & ARRA, advantages and disadvantages of ARRA, intentions to apply for ARRA incentive program, implementation barriers or challenges |
| Nationwide Health Information Network (NHIN)/Health Information Exchange (HIE) | NHIN level of familiarity, participation, and interest; and other HIE level of familiarity, interest and participation, number of practices in network, type of information shared |
| Method of storage & date entry responsibility/modalities (EDR) | Type of information, storage methods – paper, computer or both, data entry responsibilities |
EDR, electronic dental record
A random list of 8,000 dentists actively practicing in the United States and their contact information was purchased from Hippo Direct, an authorized licensee of the ADA. A novel approach to survey dissemination was piloted10. Briefly, the survey was mailed in phases. Return rates on the first two sub-samples, which randomly targeted the available mailing list, were modeled to determine the number of mailings required in the final distribution of surveys to attain a targeted sample size (n=400). Phasic survey distributions were undertaken over a 3-month window between August and October of 2012. To enhance the probability of response, within a 3-week window respondents were given the option of completing a mailed, paper-based survey; an online survey; or a telephone interview.
All surveys collected during the 3-month window in 2012 were included in the analysis. Data collected in the surveys were entered into the SurveyMonkey tool/database, exported into Excel (Microsoft Corporation, Seattle, WA), and converted to SAS Windows version 9.2, English (SAS Institute Inc., Cary, NC). A data entry/quality assurance clerk manually validated data entry on 10% of surveys to verify accuracy.
Statistical Analysis
For the defined categorical variables, frequency distributions (percentages) were compared, and corresponding P values were derived by Chi-square testing. For specific continuous variables, median values were compared, and corresponding P values were derived using Wilcoxon Rank Sum test. All data analyses were carried out using SAS Windows version 9.2, English.
Content analysis of free-text of open-ended responses from participants was performed to systematically and objectively draw valid inferences from verbal, visual, or written data. An inductive approach was applied to raw data11 to identify and capture detailed factors and categories emerging from open-ended questions.12 Responses to all open-ended questions were iteratively reviewed while developing thematic coding frames for each question. Emergent themes based on content analyses conducted by co-authors with expertise in qualitative analysis were regrouped into larger categories.
Results
Survey Administration
Staged dissemination of surveys achieved a return rate that exceeded the targeted n=400 by 21%, capturing an actual return rate of 484 surveys. Of the 484 respondents returning the survey, 434 (89.7%) completed the mailed, paper-based survey, while the remaining 50 respondents (10.3%) elected to complete the survey online through SurveyMonkey. No respondents engaged telephonic survey completion. Not all 484 respondents answered all the 39 questions
Demographics and Practice Characteristics
Table 2 illustrates the demographics and practice characteristics of survey respondents and highlights observed differences among respondents’ characteristics. Participants were generally older (age > 50 years) with 62% (301/482) reporting their age as over 50 years. Of the respondents, 65% (299/462) reported being in practice for more than 20 years. Only approximately one-quarter of respondents was female. Two-thirds of respondents (324/483) were in solo practice settings. Over half (53/94) of younger respondents (age ≤ 40 years) worked in a group practice, while 73% (282/387) of respondents over age 40 worked in a solo practice. Nearly half (217/474) of respondents practiced in suburban settings, followed by 31% (146/474) in rural/small town areas, and 24% (116/474) in urban areas. US regional representation of the respondents included: Midwest 31% (145/472); South 30% (142/472); West 22% (105/472); and Northeast 15% (72/472).
Table 2.
Demographics and the practice characteristics of the dental providers in the study sample
| No. of years in dental practice | |||||||
|---|---|---|---|---|---|---|---|
|
|
|||||||
| Characteristics | Total No.* | 0–10 | 11–20 | 21–30 | 31–40 | 41–50 | 51+ |
| Gender (response rate: 95.5% (462/484 ) | |||||||
| Male | 356 (77%) | 48 (56%) | 47 (60%) | 108 (78%) | 130 (94%) | 21 (100%) | 2 (100%) |
| Female | 106 (23%) | 37 (44%) | 31 (40%) | 30 (22%) | 8 (6%) | 0 (0%) | 0 (0%) |
| Ethnicity (response rate: 98% (466/484) | |||||||
| White | 405 (87%) | 67 (79%) | 59 (76%) | 122 (88%) | 135 (95%) | 20 (95%) | 2 (100%) |
| Black/African American | 10 (2%) | 1 (1%) | 2 (3%) | 5 (4%) | 2 (1%) | 0 (0%) | 0 (0%) |
| Asian | 33 (7%) | 10 (12%) | 13 (17%) | 7 (5%) | 2 (1%) | 1 (5%) | 0 (0%) |
| Hawaiian & Pacific Islander | 2 (.4%) | 1 (1%) | 0 (0%) | 1 (1%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Mixed Race Background | 4 (.8%) | 0 (0%) | 1 (1%) | 3 (2%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Other | 12 (3%) | 6 (7%) | 3 (4%) | 0 (0%) | 3 (2%) | 0 (0%) | 0 (0%) |
| Location type (response rate: 98% (461/484) | |||||||
| Urban/ sub-urban | 323 (70%) | 54 (65%) | 53 (72%) | 112 (80%) | 89 (63%) | 13 (65%) | 2 (100%) |
| Rural/small town | 138 (30%) | 29 (35%) | 21 (28%) | 28 (20%) | 53 (37%) | 7 (35%) | 0 (0%) |
| Practice type (response rate: 99.8% (475/484) | |||||||
| Solo | 318 (67%) | 39 (46%) | 49 (62%) | 102 (72%) | 111 (76%) | 15 (71%) | 2 (100%) |
| Group | 157 (33%) | 46 (54%) | 30 (38%) | 39 (28%) | 36 (24%) | 6 (29%) | 0 (0%) |
| U.S. Region (response rate: 97.5% (464/484) | |||||||
| Midwest | 145 (31%) | 21 (25%) | 24 (31%) | 40 (29%) | 51 (35%) | 8 (44%) | 1 (50%) |
| Southern | 142 (31%) | 29 (35%) | 26 (34%) | 45 (32%) | 38 (26%) | 3 (17%) | 1 (50%) |
| Western | 105 (23%) | 27 (33%) | 17 (22%) | 29 (21%) | 27 (19%) | 5(28%) | 0(0%) |
| Northeastern | 72 (16%) | 6 (7%) | 10 (13%) | 26(19%) | 28 (19%) | 2 (11%) | 0 (0%) |
Some percentages represent comparisons down columns and due to rounding may not add to 100%.
Values represent the number of respondents out of 484 who supplied a response to a specific question
Table 3 summarizes comparison of study respondents gender, solo/group practice split, and demographic location within the United States, compared to a national sample of dentists from the 2012 ADA National Sample of Dentists Survey.12,13 The current study captured a significantly higher response from Midwestern states compared to ADA response rates from the same region (P < 0.0001).13,14 However, no statistically significant difference was observed in response rates regionally across the nation in the current study, although comparatively higher response rates were achieved among Midwestern and Southern practices compared to those achieved among Northeastern states. Approximately two-thirds of respondents in the current study reported being in solo practice settings.
Table 3.
Study respondents in solo or group practice compared to data reported in the 2012 ADA National Sample of Dentists Survey* (n=188,820).12,13
| Our study | ADA | P value | |
|---|---|---|---|
| Gender | 0.1248 | ||
| Male | 77% | 74% | |
| Female | 23% | 26% | |
| Practice Type | <0.0001 | ||
| Solo | 67% | 57.5% | |
| Group | 33% | 42.5% | |
| Geographical location | <0.0001 | ||
| Midwest | 31% | 20% | |
| Southern | 31% | 32% | |
| Western | 23% | 27% | |
| Northeastern | 16% | 21% |
The denominator for each row of this table is n=475 respondents.
Technology at Practice
Use of computers chairside in operatories was reported by 72% (341/476) of practices, with 46% (158/341) reporting chairside internet connectivity. A majority of respondents reported having computers at the front office desk (458/476) or in provider or staff offices (382/476), and 11% (54/476) reported providing computer access in patient waiting areas. Moderate-to-high comfort levels with computers were reported by 83% (396/477) of respondents, while 9% (41/477) indicated low to very-low comfort levels.
The majority of respondents assigned relatively high importance to internet access in their practices, with 79% (378/476) rating it as ‘somewhat to very essential.’ Practice-related internet searches were reported to access the following: vendor/products (358/474), educational material (358/474), evidence-based information (228/474), referrals (179/474), technology support (175/474), and ‘other purpose’ (54/474). Technologies/devices used in their practice included: iPads/tablets (83/146), Smart Phones/personal digital assistants (104/146), digital radiographs (263/484), and computer-aided design-computer-aided manufacturing (CAD-CAM) (73/484).
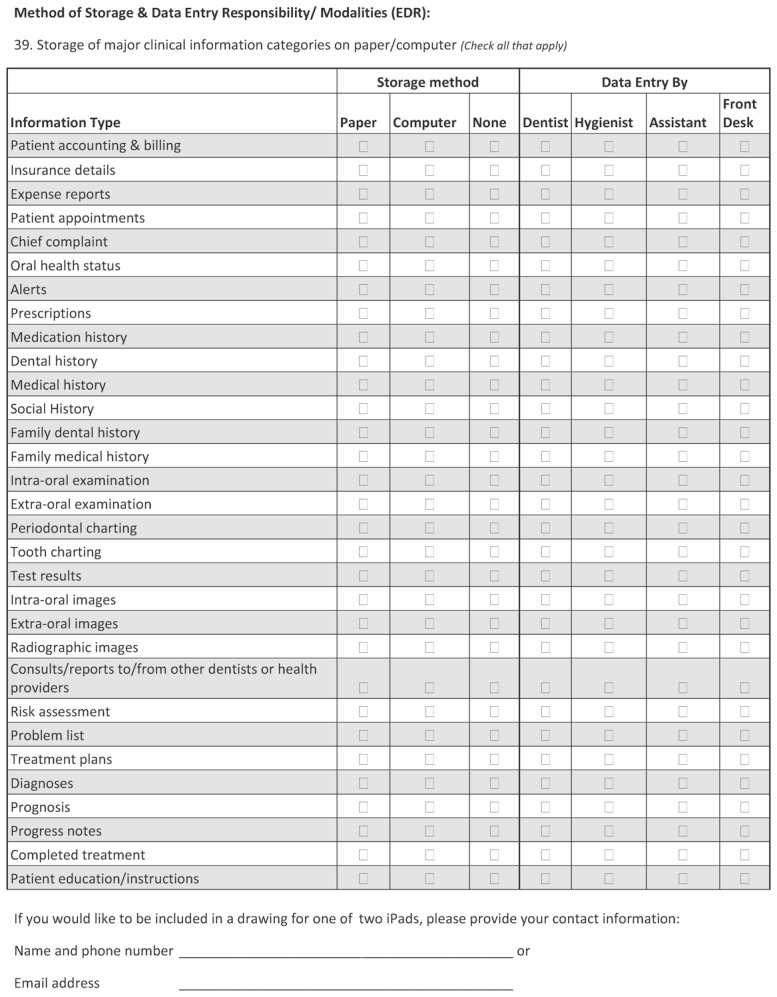
Methods of Information Storage
Table 4 summarizes dental personnel involved in the data entry of various types of information at the dental centers. As indicated by significant P values, activities tend to compartmentalized based on roles. Front desk personnel primarily entered data associated with patient accounting, insurance details, expense reports, and patient appointments. Dental assistants primarily entered intra-oral images and radiographic images. Dental hygienists primarily captured data associated with periodontal charting, and dentists primarily entered oral health status, prescriptions, intra- and extra-oral examinations, test results, consults/reports to/from other dentists or health providers, risk assessment, problem list, treatment plans, diagnosis, prognosis, progress notes, and completed treatment.
Table 4.
Dental personnel responsible for entering data in various information categories
| Information Type | Dentist | Hygienist | Assistant | Front Desk |
|---|---|---|---|---|
| Patient Accounting & Billing | 84 (18%) | 78 (16%) | 88 (19%) | 422 (89%) |
| Insurance Details | 43 (9%) | 30 (6%) | 55 (12%) | 419 (88%) |
| Expense Reports | 169 (36%) | 11 (2%) | 28 (6%) | 252 (53%) |
| Patient Appointments | 96 (20%) | 183 (39%) | 199 (42%) | 409 (86%) |
| Chief complaint | 274 (58%) | 192 (40%) | 201 (42%) | 146 (31%) |
| Oral health status | 328 (69%) | 269 (57%) | 199 (42%) | 84 (18%) |
| Alerts | 244 (51%) | 232 (49%) | 245 (52%) | 307 (65%) |
| Prescriptions | 361 (76%) | 122 (26%) | 141 (30%) | 152 (32%) |
| Medication history | 288 (61%) | 263 (55%) | 244 (51%) | 218 (46%) |
| Dental history | 318 (67%) | 268 (56%) | 255 (54%) | 138 (29%) |
| Medical history | 289 (61%) | 257 (54%) | 239 (50%) | 202 (43%) |
| Social history | 191 (40%) | 172 (36%) | 173 (36%) | 163 (34%) |
| Family dental history | 199 (42%) | 173 (36%) | 168 (35%) | 133 (28%) |
| Family medical history | 210 (44%) | 177 (37%) | 167 (35%) | 129 (27%) |
| Intra-oral examination | 353 (74%) | 257 (54%) | 201 (42%) | 42 (9%) |
| Extra-oral examination | 348 (73%) | 237 (50%) | 183 (39%) | 35 (7%) |
| Periodontal charting | 256 (54%) | 319 (67%) | 188 (40%) | 36 (8%) |
| Tooth charting | 293 (62%) | 292 (61%) | 284 (60%) | 36 (8%) |
| Test results | 271 (57%) | 133 (28%) | 147 (31%) | 119 (25%) |
| Intra-oral images | 259 (55%) | 259 (55%) | 287 (60%) | 45 (9%) |
| Extra-oral images | 241 (51%) | 195 (41%) | 239 (50%) | 51 (11%) |
| Radiographic images | 259 (55%) | 311 (65%) | 336 (71%) | 53 (11%) |
| Consults/reports to/from other dentists or health providers | 293 (62%) | 107 (23%) | 127 (27%) | 248 (52%) |
| Risk assessment | 276 (58%) | 148 (31%) | 92 (19%) | 40 (8%) |
| Problem list | 287 (60%) | 178 (37%) | 164 (35%) | 82 (17%) |
| Treatment plans | 351 (74%) | 192 (40%) | 196 (41%) | 171 (36%) |
| Diagnoses | 379 (80%) | 143 (30%) | 118 (25%) | 40 (8%) |
| Prognosis | 369 (78%) | 132 (28%) | 108 (23%) | 30 (6%) |
| Progress notes | 372 (78%) | 270 (57%) | 204 (43%) | 58 (12%) |
| Completed treatment | 334 (70%) | 227 (48%) | 213 (45%) | 146 (31%) |
| Patient education / instructions | 321 (68%) | 288 (61%) | 278 (59%) | 130 (27%) |
Percent shown in this table were calculated as the # respondents shown in each cell divided by the denominator: the total number of respondents across all 4 categories (n=475) (x100).
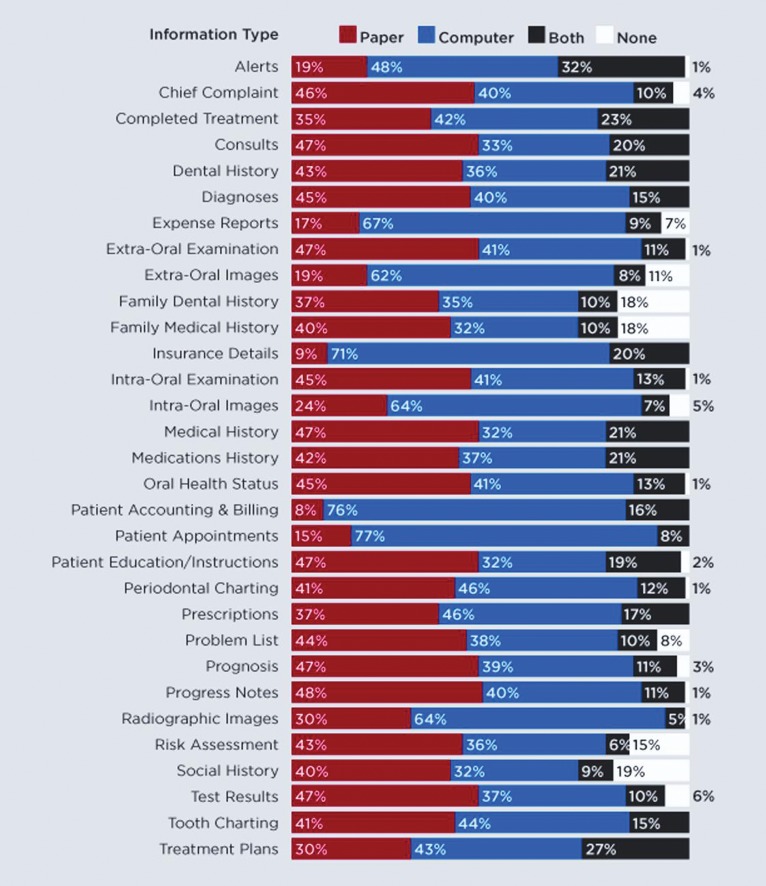
More than two-thirds of respondents stored administrative information such as expense reports, insurance details, patient appointment, patient accounting, and billing entirely on computers. A proportionately large number of respondents stored clinical images completely on computers: intra-oral images 64% (295/458), extra-oral images 62% (280/448), and radiographic images 64% (295/463). Our results showed that dental providers stored administrative information such as insurance details, patient appointment, patient accounting, and billing and treatment plan either on paper, computer, or both, with the exception of expense reports, which were not stored at all among 6% of the respondents. With respect to clinical information, ≤ 5% of respondents neither stored information on paper nor on a computer for the following types of information: alerts, chief complaint, intra-oral and extra-oral examination, intra-oral images, oral health status, patient education/instructions, periodontal charting, prognosis, progress notes, and radiographic images. Between 6%–19% of respondents reported that clinical information including extra-oral images, family medical history, family dental history, problem list, risk assessment, social history, and test results were neither stored on paper nor on computer. Figure 1 captures the different mediums used by the dental providers across the United States to store major clinical and administrative information in their practices.
Figure 1.
Information storage methods of major clinical and administrative information in dental practices.
Patient-centric Practice
Formats used most frequently for patient education by respondents included: face-to-face 93% (447/480); take-away paper-brochures/walk-out statements 89% (427/480); electronic—computer/video/CDs 42% (203/480); and Internet 31% (150/480). When asked what resources were used for patient education, 79% (373/471) cited their own clinical materials; 30% (141/471) listed software applications; and 14% (64/471) listed other resources.
Among the 15% (70/476) of respondents who had patient portals at their practice, the following features/capacities were available: patient forms and online services 68% (46/68); viewing and/or scheduling appointments 53% (36/68); updating insurance information 53% (36/68); bill payment 41% (28/68); health reminders 40% (27/68); educational health information 40% (27/68); health summary 21% (14/68); refilling prescriptions 9% (6/68); and reviewing test results 1% (1/68).
Among respondents, 38% (184/480) used social media including the following venues: Facebook, 95% (175/184); Twitter, 26% (48/184); LinkedIn, 23% (42/184); and YouTube, 15% (28/184). Dental practices indicated using social media for marketing (87%, 154/177), communication (71%, 125/177), and networking (60%, 106/177).
Electronic Dental Record Adoption and Usage
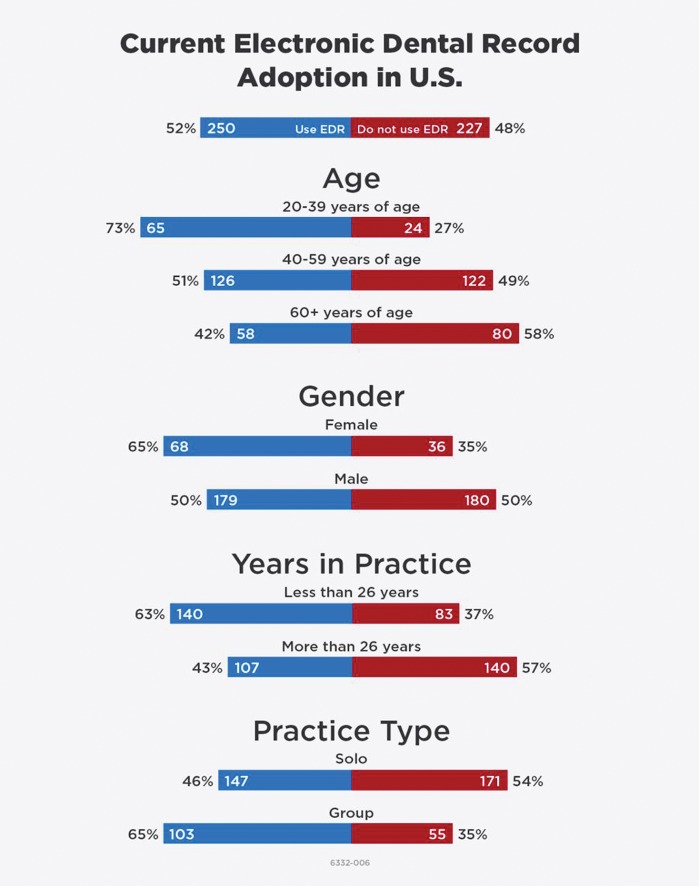
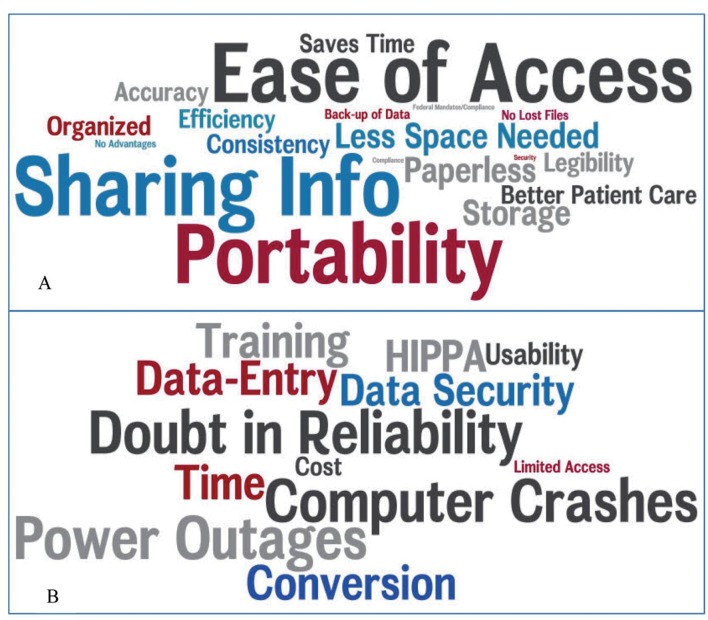
Figure 2 illustrates demographics and practice characteristics of responding practices reporting EDR use versus no EDR use. Among respondents with EDRs, 73% (347/475) indicated EDRs were ‘moderately to very important’ for their practice. Comfort level with use of EDRs was ranked as, ‘very or somewhat comfortable’ by 53% (248/472), while 23% (109/472) selected ‘somewhat or very uncomfortable’. Figure 3 depicts word clouds that summarize emergent themes representing perceived advantages (Figure 3a) and disadvantages (Figure 3b) of EDRs as described by the respondents.
Figure 2.
Demographics and practice characteristics of dentists who are using electronic dental records (EDRs) versus the dentists not engaging EDRs.
Figure 3.
(A) Word cloud summarizing key themes described by the respondents that represent the advantages of electronic dental records (EDRs). (B) Word cloud reflecting key themes advanced by respondents surrounding disadvantages of EDRs. Thematic emphasis is shown proportionately by the size of the words depicting the theme reflecting frequency of expression of the theme by participants.
Current EDR use was reported by 52% (250/477) of respondents with 40% of practices (101/250) reporting “going live” with their EDR more than 6 years ago, 29% (73/250) 3–5 years ago, while 28% (70/250) reported startup within the last 2 years. The remaining 48% (227/477) of respondents that indicated they were not currently using EDRs in their practice were asked to provide a rationale for lack of adoption. The top four reasons indicated for not using EDRs were: cost/expense 28% (33/116); low value placed on EDR implementation 16% (19/116); time investment to convert/train staff 16% (18/116); and poor usability/comfort level with computers 8% (9/116). Of the current non-adopters, 40% (91/227) were unsure of whether they would adopt an EDR in the future, and 33% (74/277) indicated no interest in adopting an EDR. Among the respondents planning potential future EDR adoption, 4% (10/227) were planning adoption in the next 6 months, 4% (8/227) in the next 7–11 months, 10% (23/227) in the next 1–2 years, and 4% (8/227) in > 2 years.
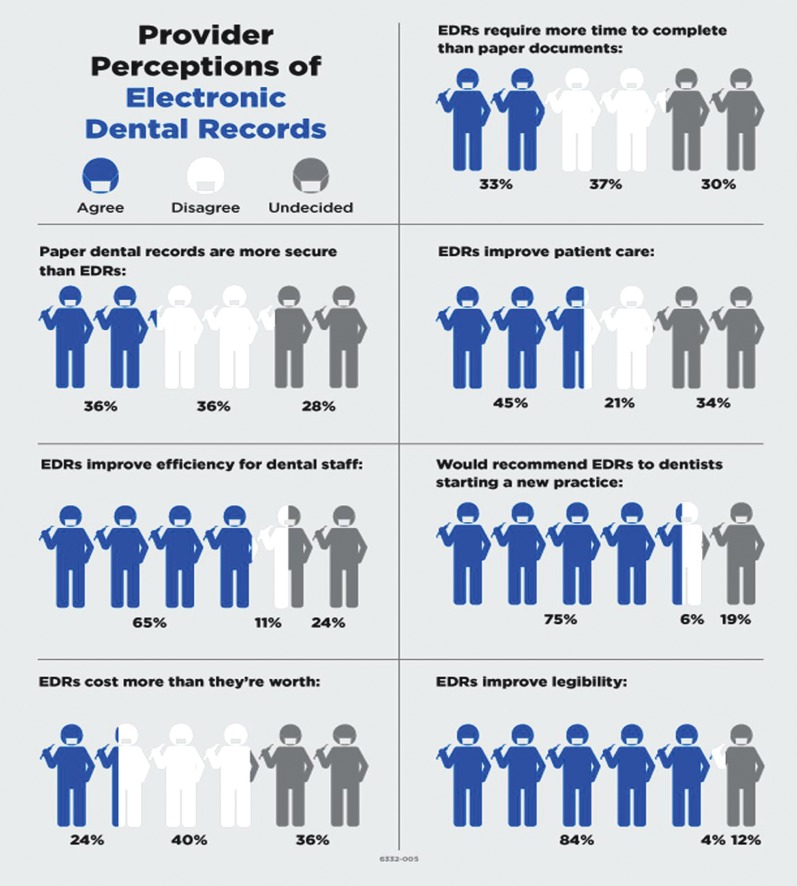
Provider’s Perception of EDRs
With respect to perceptions on the relative security offered by paper versus EDRs, 36% (173/276) of respondents felt the paper version offered more security, while an additional 36% (173/276) of respondents electronic dental records provided a higher level of security. Among respondents, 64% (308/478) agreed that EDRs improve efficiency among dental staff. When asked about cost benefit, 25% (117/468) agreed that EDR cost exceeds the relative value to the practice, while 41% (191/468) disagreed. Regarding data entry, 37% (176/474) of respondents disagreed that more time is required to enter data into EDRs than to a paper record, while 33% (159/477) agreed. When asked whether EDRs improve patient care, 44% (212/478) of the respondents agreed. When asked whether they would recommend EDRs to dentists starting a new practice, 75% (359/477) of respondents noted they would, and 85% (402/474) agreed that EDRs improve legibility. Figure 4 illustrates dental providers’ perceptions of EDRs.
Figure 4.
Dental providers’ perception of electronic dental records (EDRs) summarized in this figure depicts extent of agreement (or disagreement) with statements presented to them about EDRs.
Electronic Health Record Incentive Program
Among respondents, 75% (357/474) were unfamiliar with the National Health Information Network (NHIN)/Health Information Exchange (HIE). Further, 73% (348/478) of respondents lacked familiarity with the Meaningful Use/American Reinvestment and Recovery Act (MU/ARRA) incentives available for implementation of EHRs. When asked if they planned to apply for the MU/ARRA incentive program, 59% (273/459) were unsure, and 25% (117/459) did not plan to apply. For those respondents already participating in MU/ARRA (n=22), 45% (10/22) reported no barriers or challenges to certification for MU, while 27% (6/22) reported not meeting the minimum qualification for patient coverage. Among practitioners who identified barriers to EDR adoption, 18% (4/22) named inability to identify a certified EDR system to suit their practice as a core barrier, while 0.5% (1/22) noted difficulty in meeting the defined MU core/menu objectives and clinical quality measures as barriers.
Discussion
The results of this study contributed to better understanding of the current knowledge, trends, extent of adoption of EDR systems, perceptions, and attitudes regarding the utilization of clinical computing among U.S. dental practices. Our study represents the most current national survey study relative to EDR adoption among dental practices in the United States conducted at the national level since the HITECH Act adoption in 2009.
Among the sample of nationwide respondents, high rates of computer utilization to support office and practice management in dental practices were captured, especially in the context of patient appointing and billing. Further, introduction of computer access in patient waiting areas is slowly emerging in dental practices, with potential to support patient check-in, providing an alternative venue for patients to access educational materials, as well as the availability of a patient portal to support updates to medical, medication, and dental history in the future. Our study results reported a 72% rate of chairside computer use, increasing the rates of 25% and 55% reported in 2005 and 2006–2007, respectively. An increased trend in internet access via chair-side computers among dental providers was noted, with practitioners electronically accessing products/vendor information, patient educational materials, and evidence-based data for clinical decision support.
Our results supported findings from a previous study1 that reported administrative information storage was predominantly captured by computers in dental practices. Our study noted an increase of ≥ 20% in computer use for storing chief complaint, dental history, medical history, and radiographic images by U.S. dental providers since the previous study conducted by Schleyer et al in 2006.1 However, several important differences should be noted between the methodological approaches of the two studies.
Whereas the study by Schleyer et al1 used a telephonic interview approach and required interviewees to have a computer to achieve study eligibility, the current study used a survey approach and had no similar exclusion criteria. Further, Schleyer’s study screened 1039 practices to identify 256 practices that indicated potential willingness to engage the study and completed 102 interviews among eligible receptive practices.1 Our study engaged a novel approach, which screened historical dental survey literature for definitions of sample sizes and response rates achieved in previous dental survey studies, to identify a robust sample size and then statistically modeled the estimated response rate required to achieve the target.10 Response rate projection was informed by true response rates achieved by two initial mailings and then estimating total numbers of mailing required to achieve the targeted sample. This approach was highly successful in achieving the targeted response, requiring only two-thirds of potential recipients to be targeted, while still exceeding the targeted goal by 20%.
To examine whether the approach targeted a representative population, we compared our demographic data with that captured by a large national ADA survey relative to respondents’ gender, solo/group practice split, and demographic location within the United States to see if statistically significant differences were observable. As shown in Table 3, statistical differences were noted between our respondents and those of the ADA survey for geographic location and practice type (solo vs group practice). Our study achieved a significantly higher response rate from Midwestern institutions compared to those achieved for the national ADA survey (Figure 4). Higher response to our survey may be attributable to our Midwestern geographic location and its regional visibility to Midwest practices. Notably, among the surveys returned, a range of EDR adoption rates across practices was noted, increasing the likelihood that the sample was representative. However, the reproducibility of this approach remains to be further validated in future studies.
Due to reports that response rates to surveys among dental practices are declining,15 an alternative strategy was developed for modeling survey return rates to achieve a projected sample size proved to be a novel, cost-effective approach to achieving a representative response free of bias to achieve valid survey outcomes10. When compared to the alternative approach involving enrollment of special populations to increase the probability of a high response rate,5 which is potentially prone to bias because the targeted population may not represent the national experience and may therefore not be generalizable, this approach supported random sampling nationally and yielded representative outcomes despite targeting a more modest sample size.
More than 20% of respondents indicated storage of alerts, completed treatment, dental history, medical history, medication history, and treatment plan on both paper and computers, indicating continued existence of hybrid data storage among some dental practices. The family medical/dental history provides an opportunity to connect with the patient as an individual and can be used to monitor for the presence of disease, guide physical examination, and inform strategies for clinical testing to support provision of cost effective, evidence-based care.16 Although family medical history, family dental history, and social history were stored in electronic and/or paper format by the majority of the respondents in their practice, nearly 18% of respondents reported not storing the information in these formats.
Notably, our findings were in good agreement with a study published by Schleyer et al5 who conducted a study similar in approximately the same time frame among the Dental Practice-Based Research Network (DPBRN), a subset of dental practitioners with membership in a research network, surrounding EDR and computer use in the dental clinical setting. The authors reported a robust response rate of 74% among the 991 DPBRN participants of their web-based survey approach and reported rates of computer use for management of clinical information at 74% and 78.7% among solo and group practitioners, respectively. Similarly, our study reported an average rate of chairside computer use of 72% across all practice types in our national survey of dental clinicians. Notably, our ratio of solo practice to group practice participants was approximately 2:1. Close agreement in the findings reported by both studies further validated capacity of our targeted sample size approach to accurately quantify adoption of technology in the clinical setting.
A main focus of this study, which has not been examined to date, was to explore whether rising EHR adoption rates among physicians and hospitals in the United States may be partially attributable to incentivisation by the HITECH Act passed in February 2009.17 Although our study data indicated that U.S. dentists were generally unfamiliar with the EHR incentive program18,19 available to them, it nevertheless documented a higher adoption rate of EDRs by U.S. dentists in the same time frame compared to medical practices rates reported in the study by Hsaio et al,20 which was based on data surrounding rates of basic EHR system adoption reported by the Office of National Coordinator reported in 201221 (data summarized in Table 5). The U.S. dentists surveyed in our study in 2012 reported a 52% EDR adoption rate, with the dentists in the Midwest showing highest adoption rates. Highest EHR adoption rates in 2012 were also reported among Midwestern practitioners. By comparison, a 2016 systematic review22 that explored trends in EHR adoption cited a study reporting only 55% of providers nationwide were in compliance with the HITECH act at the end of 2014.23 The systematic review further identified 25 facilitating factors and 23 barriers to EHR adoption.22 Cost of EHR adoption was noted as a leading barrier to EHR adoption and was also identified among the leading barriers in our study.
Current EDR use is higher among younger dentists in the United States, likely due to adoption of EDRs by U.S. dental schools for training dental students.24 Adopting an unfamiliar paper-based environment in their private practices is highly unlikely for this subset of dentists. Notably, demographic evaluation of the 33% of dental practices with no EDR that indicated no plans for adoption determined they were largely older, male, engaged in solo practices, and in practice for >26 years (Figure 2).
Ramoni et al25 surveyed 814 dental team practitioners of a large private dental practice with offices in three states across the Pacific Northwest regarding their attitudes/beliefs related to establishment and use of standardized diagnostic terminology.25 With a robust response rate of 92%, their study reported an overarchingly positive attitude towards clinical implementation of diagnostic terminology for improving intradisciplinary communication and communication between practitioners and patients. Increasingly, a growing interest in platforms reinforcing interdisciplinary interoperability to support integrated medical-dental care delivery models is an emergent factor that may further drive health record adoption in the future.26 These reports reflect further positive directions associated with increased implementation of clinical computing as reported in the current study.
Cost/expense of the EDRs, cost-benefit ratio, time to convert from paper-based to computer-based practice, and poor usability of the current EDRs remained as the top barriers cited for adoption of EDRs. Notably, within the time frame that approximately parallels that of our survey study, Walji et al27 identified usability issues and, in collaboration with vendors, set up timelines to systematically solve identified problems. Such studies are strategic in achieving high functioning EDRs for use in the clinical setting and diminishing barriers to EDR adoption. Our results indicate there is still debate over the relative security of paper-based versus computer-based patient dental records, and the opinions of U.S. dental providers are divided equally around this issue. Despite mixed perception surrounding EDRs, 75% of survey responders indicated they would recommend EDRs to dentists starting a new practice. Ease of access to patient information emerged as the top advantage of EDRs, while concerns regarding technology reliability as the top disadvantage.
Notably, only 15% of respondents had adopted the use of patient portals in their practice based on survey data. A patient health portal is a web-based resource that provides a secure, HIPAA-compliant, two-way communication channel between patients and their health care providers.28,29 A patient health portal offers potential benefits to patients and provider organizations by improving both quality and access to care through features that enable patients to communicate electronically and securely with providers.30,31 Generally, patients using patient health portals tend to report greater satisfaction with provider communications and overall care.32 This trend is important to follow in future studies.
Conclusion
Although the majority of dentists surveyed in the United States were unfamiliar with the HITECH EHR incentive program available to them, the rate of adoption of EDRs by U.S. dentists to support chairside practice out-distanced the adoption rate by medical practitioners to support clinical practice in 2012. It would be important to determine the direction of this trend in the future. Use of EDRs is higher among younger dentists in the United States. Top barriers for adoption of EDRs identified in this survey included cost/expense of EDRs, cost-benefit ratio, time to convert from paper-based to computer-based practice, and poor usability of current EDRs. Adoption rates of patient portals among dental practices in the United States were low. Finally, the approach piloted for targeting a defined sample of returned responses through modeling return rates from multiple mailings was effective in achieving the targeted national sample. However, more studies will be needed to further validate this alternative approach for survey research.
Acknowledgements
The authors thank Crystal Gumz, Lauren Janes, Neel Shimpi, and Cathy Schneider of the Biomedical Informatics Research Center for their assistance with the mailings conducted for this study. The authors thank Cathy Schneider for helping with the manual validation of the data entry process to verify accuracy of the data. Finally, the authors also thank Dr. Ingrid Glurich, Institute for Oral and Systemic Health project scientist and Marie Fleisner from the Office of Scientific Writing at Marshfield Clinic Research Foundation for assistance with reviewing and editing this manuscript.
Appendix 1. Marshfield Clinic Research Institute’s Electronic Dental Record Adoption Survey Tool
Footnotes
Financial Support: This study was supported in part by funds from Marshfield Clinic Research Institute, Family Health Center of Marshfield, Inc., and Delta Dental of Wisconsin.
References
- 1.Schleyer TK, Thyvalikakath TP, Spallek H, Torres-Urquidy MH, Hernandes P, Yuhaniak J. Clinical computing in general dentistry. J Am Med Inform Assoc. 2006;13:344–352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Irwin JY, Tores-Uquidy MH, Schleyer T, Monaco V. A preliminary model of work during initial examination and treatment planning appointments. Br Dent J. 2009;206:E1. [DOI] [PubMed] [Google Scholar]
- 3.American Dental Association Survey Center. In: 2006 Technology Survey. Chicago: American Dental Association; 2007. 22–37. [Google Scholar]
- 4.Dental Health Information Technology Survey. Edge Research. April 2010. [Google Scholar]
- 5.Schleyer T, Song M, Gilbert GH, Rindal DB, Fellows VV, Gordan VV, Funkhouser E.Electronic dental record use and clinical information management patterns among practitioner-investigators in The Dental Practice-Based Research Network. J Am Dent Assoc. 2013;144:49–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Blumenthal D. Launching HITECH. N Engl J Med. 2010;362:382–385. [DOI] [PubMed] [Google Scholar]
- 7.Blumenthal D. Implementation of the federal health information technology initiative. N Engl J Med. 2011;365:2426–2431. [DOI] [PubMed] [Google Scholar]
- 8.American Dental Association News, June 21, 2010, Electronic Health Record: Will federal government require it by 2014? Available at: http://www.ada.org/news/4306.aspx Accessed February 4, 2017.
- 9.Edlestein BL. Federal supports for state oral health plans. J Publ Health Dent. 2012;72:S54–S59. [DOI] [PubMed] [Google Scholar]
- 10.Chyou PH, Schroeder D, Schwei K, Acharya A. Statistical application and cost saving in a dental survey. Clin Med Res. 2017;15:1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Elo S, Kyngäs H. The qualitative content analysis process. J Adv Nurs. 2008;62:107–115. [DOI] [PubMed] [Google Scholar]
- 12.Forman J, Damschroder L. Qualitative content analysis. In: Jacoby L, Siminoff LA, eds. Empirical Research for Bioethics: A Primer. Oxford, UK: Elsevier; Publishing; 2008. 39–62. [Google Scholar]
- 13.American Dental Association Survey Center. 2012 Distribution of Dentists survey. Chicago: American Dental Association; 2011. [Google Scholar]
- 14.American Dental Association. Health Policy Institute. Supply of dentists. 2015. Available at: http://www.ada.org/en/scienceresearch/health-policy-institute/data-center/supply-of-dentists Accessed February 4, 2017.
- 15.Cook JV, Dickinson HO, Eccles MP. Response rates in postal surveys of healthcare professionals between 1996 and 2005: an observational study. BMC Health Services Res. 2009;9:160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Anderson R, Schiedermayer D. The social history matters! Acad Med. 2010;85:1103. [DOI] [PubMed] [Google Scholar]
- 17.DesRoches CM, Charles D, Furukawa MF, Joshi MS, Kralovec P, Mostashari F, Worzala C, Jha AK. Adoption Of electronic health records grows rapidly, but fewer than half of US hospitals had at least a basic system in 2012. Health Affairs (Millwood). 2013;32:1478–1485. [DOI] [PubMed] [Google Scholar]
- 18.Kalenderian E, Walji M, Ramoni RB. “Meaningful use” of EHR in dental school clinics: how to benefit from the U.S. HITECH Act’s Financial and quality improvement incentives. J Dent Educ. 2013;77:401–415. [PubMed] [Google Scholar]
- 19.Powell VJ, Acharya A, Mahnke A, Din FM, Thyvalikakath TP. Metrics and Measurements. In: Powell VJ, Din FM, Achary A, Torres-Uquidy MH, eds. Integration of Medical and Dental Care and Patient Data. London: Springer, Health Informatics Series; 2012. Vol 3:139–165. Isbn: 978-1-4471-2185-5 10.1007/978-1-4471-2185-5_3; [DOI] [Google Scholar]
- 20.Hsiao C-J, Hing E, Ashman J. Trends in electronic health record system adoption among office-based physicians: United States, 2007–2012. National Health Statistics Report # 75, May 20, 2014. Available at: http://www.cdc.gov/nchs/data/nhsr/nhsr075.pdf Accessed April 20, 2016. [PubMed]
- 21.Health IT Dashboard. Electronic Health Record Adoption. EHR Adoption by Office-Based Providers. 2012. Available at: http://dashboard.healthit.gov/HHSONCHIEVIEWSLAB/ Accessed February 4, 2017.
- 22.Kruse CS, Kothman K, Anerobi K, Abanaka L. Adoption Factors of the Electronic Health Record: a systematic review. JIMR Med Inform 2016;4(2):e19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hamid F, Cline TW. Providers’ acceptance factors and their perceived barriers to electronic health record (EHR) adoption. Online Journal of Nursing Informatics 2013;17 Available at: http://ojni.org/issues/?p=2837 Accessed November 7, 2017.
- 24.White JM, Kalenderian E, Stark PC, Ramoni RL, Vaderhobli R, Walji MF. Evaluating a dental diagnostic terminology in an electronic health record. J Dent Educ. 2011;75:605–615. [PMC free article] [PubMed] [Google Scholar]
- 25.Ramoni RB, Walji MF, Kim S, McClellan L, Simmons K, Skourtes E, Yansane A, White JM, Kalenderian E. Attitudes toward and beliefs about the use of a dental diagnostic terminology: a survey of dental care providers in a dental practice. J Am Dent Assoc 2015;146:390–397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kalenderian E, Halamka JD, Spallek H. An EHR with teeth. Appl Clin Inform 2016;7:425–429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Walji MF, Kalenderian E, Tran D, Kookal KK, Nguyen V, Tokede O, White JM, Vaderhobli R, Ramoni R, Stark PC, Kimmes NS, Schoonheim-Klein ME, Patel VL. Detection and characterization of usability problems in structured data entry interfaces in dentistry. Int J Med Inform 2013;82:128–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Horowitz AM, Robinson LA, Ng MW, Acharya A. After Visit Summaries: A Tool Whose Time Has Come for Use in Dentistry. Institute of Medicine of the National Academies: 2014. Avaialble at: http://www.iom.edu/~/media/Files/Perspectives-Files/2014/Discussion-Papers/aftervisitsummaries.pdf Accessed February 4, 2017.
- 29.Tang PC, Ash JS, Bates DW, Overhage JM, Sands DZ. Personal health records: definitions, benefits, and strategies for overcoming barriers to adoption. J Am Med Inform Assoc. 2006;13:121–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Emont S. Measuring the Impact of Patient Portals: What the Literature Tells Us. Oakland, CA: California HealthCare Foundation; 2011. Avaialble at: http://www.chcf.org/~/media/MEDIA%20LIBRARY%20Files/PDF/M/PDF%20MeasuringImpactPatientPortals.pdf Accessed Feburary 4, 2017. [Google Scholar]
- 31.Lin CT, Wittevrongel L, Moore L, Beaty BL, Ross SE. An Internet-based patient-provider communication system: randomized controlled trial. J Med Internet Res. 2005;7:e47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zickmund SL, Hess R, Bryce CL, Mc Tigue K, Olshansky E, Fitzerald K, Fisher GS. Interest in the use of computerized patient portals: role of the provider-patient relationship. J Gen Intern Med. 2008;23:20–26. [DOI] [PMC free article] [PubMed] [Google Scholar]