Abstract
STUDY QUESTION
Would letrozole as a primary ovulation induction agent generate better pregnancy rates than clomiphene citrate (CC) in subfertile women with anovulatory polycystic ovarian syndrome (PCOS)?
SUMMARY ANSWER
Participants receiving letrozole as a primary treatment achieved a significantly (P = 0.022) higher clinical pregnancy rate per patient (61.2%) compared to CC (43.0%).
WHAT IS KNOWN ALREADY
According to a recent Cochrane systematic review (2014), letrozole appears to improve live-birth (LB) and pregnancy rates in anovulatory women with PCOS, compared to CC. However, the review concluded that the quality of evidence was low due to poor reporting of study methods and possible publication bias.
STUDY DESIGN, SIZE, DURATION
This double-blind randomized controlled trial (RCT) included 159 participants between April 2007 and June 2014. Subjects were randomly allocated to either CC (n = 79) or letrozole (n = 80) in a 1:1 ratio. Both drugs were encapsulated to look identical. Randomization was performed in mixed blocks and stratified by patients’ BMI (<30 and 30–35 kg/m2).
PARTICIPANTS/MATERIALS, SETTING, METHODS
The trial included subfertile women diagnosed with PCOS. Treatment started with one tablet (CC 50 mg, letrozole 2.5 mg) increasing to two in non-responders and continuing until pregnancy or for up to six ovulatory cycles. Non-responders were crossed over to the other treatment after a 6-week break. Cycles were initially monitored with ultrasound follicle tracking then mid-luteal serum progesterone measurement in subsequent cycles.
MAIN RESULTS AND THE ROLE OF CHANCE
Amongst the 159 participants included in the intention-to-treat analysis, four women conceived before treatment and six were lost-to-follow-up. The remaining 149 participants (74 on CC and 75 on letrozole) completed at least the first treatment. Women receiving letrozole achieved a significantly (P = 0.022; absolute difference [95% confidence interval] 18% [3–33%]) higher pregnancy rate (61.%) than those on CC (43%). The median number of treatment cycles received until pregnancy was significantly (log rank P = 0.038) smaller with letrozole (4[3–5] cycles) compared to CC (6[4–7] cycles). LB rates were not statistically (P = 0.089) different between the two groups, although there was a trend towards higher rates on letrozole (48.8%) compared to CC (35.4%). After the crossover, pregnancy and LB rates on letrozole (n = 45; 28.9 and 24.4%, respectively) were not statistically (P = 0.539 and P = 0.601) different from CC (n = 31; 22.6 and 19.4%).
LIMITATIONS, REASONS FOR CAUTION
One possible limitation of this trial may be the exclusion of PCOS women with BMI > 35 kg/m2, which would limit the applicability of the results in this subgroup of PCOS. However, this group of women are generally excluded from treatment in the majority of fertility centres, especially in Europe, due to the associated challenges and risks.
WIDER IMPLICATIONS OF THE FINDINGS
The results of this trial are consistent with the recent Cochrane systematic review. However, with its robust design, the current RCT provides more valid and compelling evidence for the superiority of letrozole over CC as a primary ovulation induction agent in PCOS women with 40% increase in pregnancy rates and with a shorter time-to-pregnancy. Furthermore, the participants in this RCT are a good representation of subfertile PCOS population receiving fertility treatment in Europe and worldwide. The results are therefore globally generalizable for clinical practice.
STUDY FUNDING/COMPETING INTEREST(S)
This RCT was mainly funded by the R&D Funding Scheme of Derby Hospitals NHS Foundation Trust. The study also received funds from School of Medicine, University of Nottingham. The Trust R&D department was involved in the development of the protocol and the running of the trial. The trial was sponsored and monitored by the University of Nottingham. The authors have no conflicts of interest.
TRIAL REGISTRATION NUMBER
TRIAL REGISTRATION DATE
Registration was verified on 23/05/2007.
DATE OF FIRST PATIENT'S ENROLMENT
25/04/2007.
Keywords: polycystic ovarian syndrome, letrozole, clomiphene citrate, aromatase inhibitors, ovulation induction, infertility
Introduction
Polycystic ovarian syndrome (PCOS) is a very common ovarian endocrinopathy affecting 6–8% of women and is the commonest cause of anovulatory infertility accounting for >80% of all cases (Asuncion et al., 2000). For decades, clomiphene citrate (CC) has been the standard first line ovulation induction (OI) agent in PCOS women with ovulation rates of ~85% and pregnancy rates of 35–40% (Dickey and Holtkamp, 1996; Kousta et al., 1997; Imani et al., 2002). This discrepancy between ovulation and conception rates has been attributed to the peripheral anti-oestrogenic actions of CC on endometrial development and cervical mucus (Massai et al., 1993; Nakamura et al., 1997).
Letrozole, a specific aromatase inhibitor that reduces oestrogen synthesis, has recently been considered as a potentially better alternative to CC. In contrast to CC, letrozole is not associated with any anti-oestrogenic effects on endometrium. This is supported by recent studies reporting adequate endometrial thickness during letrozole treatment (Mitwally and Casper, 2001; Al-Omari et al., 2004; Atay et al., 2006). Furthermore, unlike CC that accumulates in the body because of its long half-life (2 weeks), letrozole is rapidly eliminated due to its short half-life (45 h), leading to late follicular rise in circulating oestrogen thereby enhancing endometrial development with subsequent increase in the chances of pregnancy (Lipton et al., 1995; Sioufi et al., 1997; Young et al., 1999). The rising oestrogen levels may also result in a shorter FSH window (mimicking the physiological cycle) with subsequent mono-ovulation and a lower risk of multiple pregnancy.
Franik et al. (2014) published a Cochrane systematic review of clinical trials comparing aromatase inhibitors versus CC. They concluded that the quality of evidence in the reviewed trials was low due to poor reporting of study methods and possible publication bias. One of the trials in that review, which had a good design, included a high proportion of markedly obese women (BMI >40 kg/m2), which does not reflect clinical practice in the majority of fertility centres worldwide (Legro et al., 2014). These results are therefore neither conclusive nor generalizable. The Cochrane review authors stated that further research is needed to compare letrozole with CC as a primary OI agent in PCOS women. Furthermore, none of the reviewed trials was conducted in Europe. Geographical, ethnic, genetic and phenotypical differences in PCOS as well as differences in clinical practices in different parts of the world may limit the generalizability of the review findings in Europe. Therefore, the effectiveness of letrozole versus CC remains uncertain.
The primary objective of this study was to test the hypothesis that letrozole as a primary OI agent will generate higher pregnancy rates than CC in anovulatory women with PCOS. The purpose of the crossover design, was to test the efficacy of each drug as a secondary OI agent.
Materials and Methods
Trial design
This was a single centre, two-arm double-blind RCT. Women not conceiving with the first drug were offered to crossover to the other one.
The trial was approved by West Midlands Research Ethics Committee (Reference: 07/MRE07/5) and by the Medicines and Healthcare Products Regulatory Agency (MHRA). It was sponsored by the University of Nottingham. All participants gave a written informed consent and the trial was monitored by the Sponsor.
Participants
This study was conducted at the Fertility Unit, Derby Teaching Hospitals NHS Foundation Trust between April 2007 and June 2014. Eligible participants were women aged 18–39 years with BMI ≤35 kg/m2, anovulatory infertility, and a diagnosis of PCOS based on Rotterdam consensus (two of three criteria: oligo-/anovulation, hyperandrogenaemia and sonographic appearance of polycystic ovaries) (Rotterdam ESHRE/ASRM-sponsored PCOS consensus workshop group, 2004). Diagnosis of oligo-/anovulation was based on a menstrual pattern of oligo-/amenorrhoea (cycle >35 days) and/or a low mid-luteal serum progesterone concentration. Hyperandrogenaemia was diagnosed either clinically (acne/hirsutism) or biochemically (testosterone ≥2.5 nmol/l or free androgen index [FAI] ≥5). Ultrasound criteria included ≥12 follicles (2–9 mm) and/or an ovarian volume of >10 ml (Jonard et al., 2003). All participants had proven patency of at least one fallopian tube and normal semen analysis of their male partners (WHO, 1999). We excluded patients who have received OI within 6 months and those with uncontrolled thyroid disease or hyperprolactinaemia. Patients with marked hyperandrogenaemia were screened for adult onset congenital adrenal hyperplasia (by measuring serum 17-α-hydroxyl-progesterone concentration) and Cushing syndrome (by measuring urinary free cortisol).
Interventions
Letrozole and CC were prescribed (by the senior investigator, SA) orally daily for 5 days starting on Days 2–4 of a menstrual period or a progestogen-induced bleed (medroxy-progesterone acetate 10 mg twice daily for 5 days). The starting dose was one tablet/day (letrozole 2.5 mg or CC 50 mg) and if ovulation was not achieved, the dose would be doubled in the second cycle. Ovulation was initially monitored by ultrasound follicle tracking (performed by an independent qualified sonographer) and mid-luteal (cycle Day 21 ± 2) serum progesterone measurement. Ovulation was diagnosed with a progesterone level of ≥25 nmol/l, a follicle diameter ≥17 mm and/or occurrence of pregnancy (positive urinary hCG and ultrasound detection of gestational sac). Once ovulation was achieved, further cycles would be monitored mainly by serum progesterone levels with follicle tracking as an option. In case of no ovulation and if the participant remained amenorrheic for ≥6 weeks, bleeding would be induced with progestogen treatment (as above). All participants were advised about timed intercourse during the treatment cycles. Treatment continued until pregnancy or for up to six ovulatory cycles. Participants who failed to ovulate on the maximum dose (two tablets) or to conceive after six ovulatory cycles were crossed over to the other drug (after a 6-week wash-out period) following the same procedures as with the first drug. The obstetric records of those conceiving were reviewed for pregnancy outcomes.
During the course of treatment, if ovulation stopped after an initial positive response, the dose was increased in the subsequent cycle; if already on the high dose, the participant was crossed over to the second drug; or the study was ended if already on the second medicine. The maximum number of cycles per treatment remained seven.
Outcomes
The primary outcome was clinical pregnancy (diagnosed by ultrasonographic visualization of a gestational sac) rate per patient on primary treatment (before the crossover). Secondary outcomes included ovulation, live-birth (LB), pregnancy per ovulating patient, pregnancy per strata, mono-ovulation, endometrial development (thickness and grades), pregnancy outcome and pregnancy complications. Other outcomes included pregnancy and LB rates on secondary and overall (primary and secondary) treatments.
Endometrial grades
Mid-cycle endometrial pattern was assessed and classified into three grades A, B and C according to Zhao et al. (2014). Grade A endometrium has a triple-line pattern, characterized by three hyperechogenic lines (a central and two outer lines) separated by two hypoechogenic areas. Grade C endometrium has a homogenous (non-triple line) hyperechogenic appearance. Grade B endometrium has an intermediate pattern with a poorly defined central echogenic line surrounded by iso- or hypoechogenic layers.
Sample size
To detect a clinically significant difference of 20% between the previously reported pregnancy rate of CC (~35%) and letrozole with a two-sided 5% significance level and power of 80%, a sample size of 212 participants (106 per arm) was required (Dickey and Holtkamp, 1996; Kousta et al., 1997; Imani et al., 2002). In view of the lack of literature data on letrozole before this trial, it was pre-planned in the protocol to perform an interim analysis during the trial with a view to re-calculating the sample size based on the obtained data. An interim blind analysis of the primary outcome after 50% recruitment (n = 106) revealed pregnancy rates of 41.5 and 64.2% for drug A (CC) and B (letrozole), respectively (P = 0.020, rate ratio [RR] 1.5 [1.1–2.3]; absolute difference [AD] 23% [4–40%]). Although, the difference was statistically significant, the power of the study was only 65%. Based on these data, the sample size was recalculated as 75 participants per arm to achieve 80% power with a two-sided 5% significance level. We aimed to recruit 160 participants to allow for 5% drop-outs.
Randomization
An independent pharmacist randomly allocated participants to letrozole or CC, in 1:1 ratio according to a randomization list created by the trial statistician using NQuery Advisor v6.0 software. Randomization was stratified by patients’ BMI (non-obese <30 kg/m2 and obese 30–35 kg/m2) using mixed block sizes. The randomization list included the patient study number and the treatment code (A or B). The participant study number was indicated on the prescription and used by the pharmacist to determine the allocated treatment. Investigators, patients, outcome assessors and the statistician were blinded to the allocation of participants.
Blinding
Letrozole 2.5 mg Tablets (Femara® Novartis Pharmaceuticals UK Ltd) and CC 50 mg Tablets (Clomid® Sanofi UK) were encapsulated in identical opaque capsules by ML(IMP)-licensed Pharmacy Production Units (initially Royal Hallamshire Hospital, Sheffield UK and later St Mary's Pharmaceutical Unit Cardiff and Vale University LHB, Cardiff, UK).
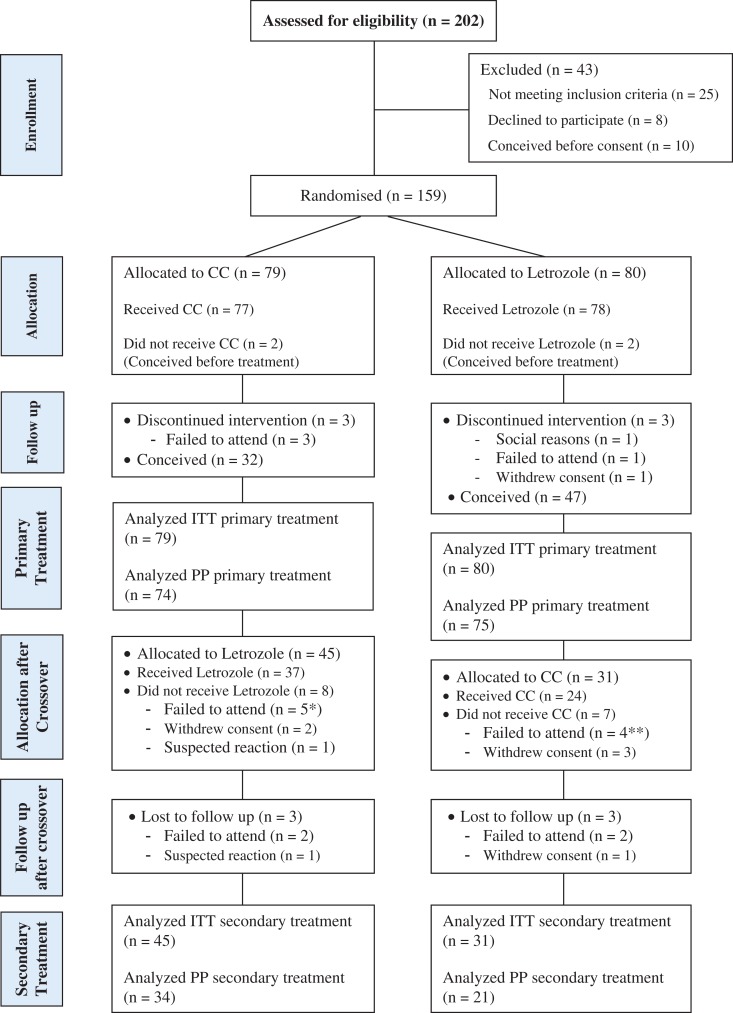
The capsules were packed in identical bottles of five capsules, which were labelled in accordance with Annex 13 of the Rules and Guidance for Pharmaceutical Manufacturers and Distributors. The packs were supplied to the Pharmacy Department, Royal Derby Hospital with additional labels allowing the Pharmacy Staff to identify the contents. At the time of dispensing to the participant these identifiers were removed. While the Pharmacy staff were aware of the patient's allocated treatment throughout the study, the patients and all investigators, including clinicians, research nurses, sonographers and the statistician remained blinded to the treatment. The Pharmacy Department had procedures in place to allow the treatment for any participant to be unblinded at any time in case of emergency. Unblinding was necessary in one case who developed a skin rash, suspected to be a reaction to the trial drug, and she was withdrawn from the study (Fig. 1). Further assessment of the rash excluded any reaction to the trial medicine.
Figure 1.
CONSORT diagram showing the flow of participants through each stage of the crossover randomized trial. ITT, intention-to-treat; PP, per protocol. *Three of the five participants failed to attend before the crossover. **Three of the four participants failed to attend before the crossover.
Neither letrozole nor CC manufacturers were involved in the trial.
Participant compliance monitoring
Participants were asked to return all study packs (including empty bottles) to Pharmacy. Details of returns were recorded on the dispensing log. All participants who completed the study complied well to their prescriptions.
Statistical analysis
Statistical analysis was performed using PASW Statistics 18. Intention-to-treat (ITT) analysis included all randomized subjects, regardless of whether or not they received the study drug. Per protocol (PP) analysis included all randomized subjects who received the study drug and were not lost to follow-up. Participants who were lost to follow-up were assumed neither to be pregnant nor to have given LB in the ITT analysis.
Three groups were analysed including primary, secondary and strategy treatment groups. The ‘primary’ treatment group was defined as the group of participants who received the first treatment before the crossover. The ‘secondary’ treatment group was defined as the group of patients who received the second treatment after the crossover. The ‘strategy’ treatment group was defined as the group of women who received the primary treatment followed by the secondary one.
Per cycle analysis was conducted for the primary treatment including pregnancy, LB, ovulation, mono-ovulation (cycles with one follicle ≥18) and endometrial parameters (grades and thickness).
Participants’ characteristics in the two allocated treatment sequences were described without formal statistical testing at baseline. Categorical data were compared using the chi-squared test. In addition, the RR and the AD (95% CI) were estimated for pregnancy, ovulation and LB rates (Miettinen and Nurminen, 1985; Newcombe, 1998). The length of time (measured as number of treatment cycles) from randomization to pregnancy during the ‘primary’ treatment was compared using Kaplan Maier plot and the log rank test. The endometrial thickness was compared using independent t-test.
Results
Participant flow
Figure 1 shows the flow of participants through the trial. A total of 202 eligible women were invited, of whom 159 were randomized. Four women (two in each group) conceived before starting treatment and six (three in each group) were lost to follow-up before completing the first treatment. The remaining 149 participants (CC, n = 74 on; letrozole, n = 75) completed at least the first treatment as per protocol. In total, 79 women conceived during the first treatment and the remaining 76 participants (letrozole, n = 31; CC, n = 45) were eligible to crossover to the second treatment and were included in the ITT analysis for the secondary treatment.
Baseline data
Baseline demographic, clinical and endocrine characteristics of the two trial groups were similar (Table I).
Table I.
Baseline characteristics of participants.
| Letrozole (n = 80) | CC (n = 79) | |
|---|---|---|
| Age (years) | 28.3 (4.4) | 28.1 {(4.2)} |
| BMI (kg/m2) | 27.5 (23.4 to 32.2) | 27.7 (23.0 to 31.0) |
| Infertility duration (years) | 1.5 (1.0 to 2.0) | 1.5 (1.0 to 2.0) |
| LH (iu/l) | 11.8 (8.9 to 15.2) | 10.2 (6.2 to 13.3) |
| FSH (iu/l) | 5.0 (1.6) | 5.1 {(1.4)} |
| Testosterone (nmol/l) | 1.8 (1.4 to 2.3) | 1.9 (1.2 to 2.4) |
| FAI (%) | 5.5 (3.0 to 7.8) | 5.0 (3.0 to 8.0) |
| Prolactin (nmol/l) | 219.5 (170 to 302.5) | 214.0 (154 to 271) |
| Fasting insulin (mIU/L) | 7.7 (4.2 to 11.6) | 7.4 (4.5 to 20.4) |
| Fasting glucose (mM) | 4.9 (4.6 to 5.1) | 4.9 (4.6 to 5.3) |
| Rt Ovarian volume (ml) | 11.5 (9.2 to 15.0) | 12.0 (9.1 to 15.5) |
| Lt Ovarian volume (ml) | 10.5 (7.0 to 13.3) | 11.8 (8.3 to 13.6) |
| Menses | ||
| Oligomenorrhoea | 51 (63.8%) | 44 (55.7%) |
| Amenorrhoea | 21 (26.2%) | 19 (24.1%) |
| Irregular | 7 (8.8% | 11 (13.9%) |
| Regular | 1 (1.2%) | 5 (6.3%) |
| Hirsutism | 33 (38.8%) | 40 (50.6%) |
| Acne | 30 (36.2%) | 31 (39.2%) |
| Primary infertility | 54 (67.5)% | 58 (5873.4%) |
| Primiparity | 63 (78.8%) | 65 (82.3%) |
| Ethnicity | ||
| Caucasian | 68 (85.0%) | 62 (78.5%) |
| South Asian | 11 (13.8%) | 13 (16.5%) |
| Other | 1 (1.2%) | 4 (5.0%) |
Numerical data presented as mean (SD) or median (25th to 75th percentile).
Categorical data presented as n (%).
CC, clomiphene citrate; FAI, free androgen index; Rt, right; Lt, left.
Primary outcome (pregnancy rates on primary treatment)
ITT analysis revealed significantly (P = 0.022) higher pregnancy rates on letrozole compared to CC (Table II). The PP analysis revealed similar results (P = 0.018) as shown in Supplementary Table SI.
Table II.
Outcomes for letrozole versus CC as a primary treatment—intention-to-treat analysis
| Outcome | Letrozole (N = 80) | CC (N = 79) | Rate ratio (95% CI) | Absolute difference (95% CI) | P |
|---|---|---|---|---|---|
| Pregnancy rate | 49/80 (61.2%) | 34/79 (43.0%) | 1.4 (1.1, 2.0) | 18% (3–33%) | 0.022 |
| Live birth rate | 39/80 (48.8%) | 28/79 (35.4%) | 1.4 (0.95, 2.0) | 13% (−2 to 28%) | 0.089 |
| Ovulation rate | 67/80 (83.8%) | 63/79 (79.7%) | 1.1 (0.9, 1.2) | 4% (−8 to 16%) | 0.513 |
| Pregnancies per ovulating patient | 47/67 (70.1%) | 32/63 (50.8%) | 1.4 (1.04, 1.9) | 20% (3–30%) | 0.024 |
| Pregnancies—strata 1 (BMI <30) | 37/54 (68.5%) | 25/53 (47.2%) | 1.5 (1.04, 2.1) | 21% (3–38%) | 0.025 |
| Pregnancies—strata 2 (BMI 30–35) | 12/26 (46.2%) | 9/26 (34.6%) | 1.3 (0.7, 2.7) | 12% (−14 to 35%) | 0.397 |
| Live births—strata 1 (BMI <30) | 29/54 (53.7%) | 20/53 (37.7%) | 1.4 (0.9, 2.2) | 15% (−3 to 30%) | 0.122 |
| Live births—strata 2 (BMI 30–35) | 10/26 (38.5%) | 8/26 (30.8%) | 1.3 (0.6, 2.7) | 8% (−20 to 30%) | 0.771 |
| Pregnancies per cycle | 49/261 (19.0%) | 34/278 (12%) | 1.5 (1.03, 2.3) | 7% (0.4–13%) | 0.036 |
| Live births per cycle | 39/261 (15%) | 28/278 (10%) | 1.48 (0.95, 2.33) | 5% (−0.7 to 11%) | 0.087 |
| Ovulation per cycle | 196/261 (75%) | 187/278 (67%) | 1.1 (1.01, 1.2) | 8% (1–15%) | 0.045 |
| Mono-ovulation* | 80/94 (85.1%) | 64/77 (83.1%) | 0.88 (0.4, 1.7) | −2% (−13 to 9%) | 0.723 |
| ET (mm) [median (IQR)] | 8.4 (7.0, 10.2) | 9.0 (8.0, 11.0) | 0.002 | ||
| EG | |||||
| A | 67 (46.5%) | 50 (36.2%) | 0.141 | ||
| B | 50 (34.7%) | 51 (37.0%) | |||
| C | 27 (18.8%) | 37 (26.8%) | |||
CC, clomiphene citrate; IQR, interquartile; ET, midcycle endometrial thickness; EG, endometrial grade.
*Mono-ovulation rate per ovulatory cycles, proportion of cycles with one follicle ≥18 mm.
Secondary outcomes on primary treatment
Table II illustrates secondary outcomes including LB (overall and per strata), ovulation, pregnancy per ovulating patient and pregnancy per strata (ITT analysis). In addition, per cycle success rates including pregnancy, ovulation and LB are also shown. PP analysis results were similar as shown in Supplementary Table SI.
There was no statistically significant difference in the LB rates between the two drugs neither in the overall groups nor in different BMI strata, although there was a trend towards higher rates in the letrozole arm.
Pregnancy rate per ovulating woman was significantly (P = 0.024) higher with letrozole compared to CC. In strata one, women receiving letrozole achieved 50% (P = 0.025) higher pregnancy rate than those receiving CC. With regards to strata 2, there was no statistically significant difference in pregnancy rates between the two groups. Ovulation rates per patient were not statistically different.
Sub-analysis of pregnancy rates based on different PCOS phenotypes (e.g. presence of hyperandrogenaemia/ultrasound features) revealed no statistically significant difference between the two drugs (Supplementary Table SII).
Per cycle analysis revealed significantly higher pregnancy (P = 0.036) and ovulation (P = 0.045) rates in the letrozole group, whilst LB rates were not statistically (P = 0.087) different.
Outcomes on secondary and strategy treatment
After the crossover, 45 women with CC-resistance/failure were allocated to letrozole and 31 with letrozole-resistance/failure were allocated to CC (Fig. 1). Pregnancy and LB rates were not significantly (ITT, P = 0.539 and P = 0.601, respectively) different between letrozole (28.9 and 24.4%, respectively) and CC (22.6 and 19.4%).
Pregnancy and LB rates achieved with letrozole followed by CC (70.0 and 56.2%, respectively) were not statistically (ITT, P = 0.166 and P = 0.369, respectively) different from those (59.5 and 49.4%) achieved with CC followed by letrozole.
Follicular and endometrial development
Mono-ovulation rates were similar between the two groups (Table II). The median (IQR) mid-cycle endometrial thickness was significantly (P = 0.002) greater during CC treatment compared to letrozole. Midcycle endometrial grades were not statistically (P = 0.141) different between the two groups (Table II).
Dose and duration of treatment
Amongst the 49 letrozole pregnancies, 32 (65.3%) were achieved on the low dose and 17 (34.7%) on the high dose. This was not significantly (P = 0.613) different from the dosages of 34 CC pregnancies (low, 24 [70.6%] and high, 10 [29.4%]).
The median number of treatment cycles received until pregnancy was significantly (log rank P = 0.038) smaller with letrozole (4[3–5] cycles) compared to CC (6[4–7] cycles).
Pregnancy outcome and complications on primary treatment
Pregnancy outcome and complications on primary treatment are detailed in Table III. There were no significant differences in fetal, maternal, or neonatal complication rates. No fetal anomaly was detected on primary treatment, but only one minor fetal anomaly (dilated left kidney) was reported in the 20-week anatomy scan in a CC pregnancy as secondary treatment. Amongst the 49 letrozole pregnancies, there were three (6.1%) sets of twins (one identical and two non-identical), which were not significantly different from that (0/34, 0%) in the CC pregnancies. Another set of identical twins was achieved with letrozole as a secondary treatment. Two of the four sets of twins were delivered at 33 and 36 weeks due to intrauterine growth restriction, but there were no neonatal problems.
Table III.
Pregnancy outcome and complications on primary treatment
| Letrozole n (%) | CC n (%) | P | |
|---|---|---|---|
| Pregnancy outcome | |||
| Miscarriage | 9 (18.4) | 6 (17.6) | 0.822 |
| Ectopic | 1 (2.0) | 0 (0.0) | |
| Preterm | 4 (8.2) | 2 (5.9) | |
| Term | 35 (71.4) | 26 (76.5) | |
| Twins | 3* (6.1) | 0 (0) | 0.201 |
| Fetal anomalies** | 0 (0) | 0 (0) | |
| Fetal complications | 3 (11.1) | 3 (7.9) | 0.521 |
| IUGR | 2 (7.4) | 2 (5.3) | |
| Macrosomia | 1 (3.7) | 0 (0) | |
| Malpresentation | 0 (0) | 1 (2.6) | |
| Maternal complications | 2† (7.4) | 7‡ (18.4) | 0.205 |
| IOL | 9 (32.1) | 13 (33.3) | 0.199 |
| CS | 7 (24.1) | 7 (17.9) | 0.124 |
| Delivery complications | 0 (0) | 1¶ (2.6) | 0.591 |
| Neonatal hypoglycaemia | 1 (3.7) | 2 (5.3) | 0.663 |
IOL, induction of labour; CS, caesarean section; IUGR, intrauterine growth restriction.
*One set was identical twins—there was an additional set of identical twins on letrozole as a secondary treatment.
**No anomalies on primary treatment as reported by 20-week anatomy fetal scan. There was one Minor anomaly (Dilated left kidney) on CC as a secondary treatment with no neonatal problems.
†1 case of gestational diabetes; 1 case of impaired glucose tolerance.
‡1 case of gestational diabetes; 2 cases of pregnancy induced hypertension; 3 cases of antepartum haemorrhage; 1 case of premature rupture of membranes.
¶Shoulder dystocia.
The preterm rates were not different between the two drugs as primary treatments (Table III). Amongst the four preterm births in the letrozole group, three were near term (33–36 weeks) with good neonatal outcome. The remaining one was severely premature (26 weeks) and the neonate survived after 20 weeks in neonatal intensive care unit (NICU). The two preterm births of the CC group were severely premature (27 and 23 weeks gestation) and both survived after several months in NICU.
Adverse events
Serious adverse events included two cases of haemorrhagic cysts (one in each arm) and one acute cholecystitis (CC group), requiring hospitalization. Both haemorrhagic cysts resolved spontaneously. Twelve participants on letrozole developed minor adverse events including cyst formation (n = 3), diarrhoea, nausea and vomiting (n = 2), hot hands, heavy leg, headache, neck pain, urinary tract infection and skin spots. Eleven women on CC experienced minor adverse events including cyst formation (n = 3), hot flushes (n = 3), migraine, low mood, elevated lever enzymes and skin rash.
Discussion
To the best of our knowledge, this is the first sufficiently powered double-blind RCT comparing letrozole versus CC in Europe. We have found letrozole to generate a pregnancy rate of 61%, which is 40% (RR, 1.4) higher than that (43%) of the standard first line CC in anovulatory women with PCOS. Furthermore, letrozole also resulted in a 40% (RR, 1.4) increase in the LB rate compared to CC (49 versus 35%, respectively), although this did not reach statistical significance as the study was not powered to address this outcome (power 36%, alpha level 0.05). We also found that letrozole has significantly shortened the time-to-pregnancy compared to CC (four versus six treatment cycles, respectively). In addition, we have reported relatively low pregnancy rates on both drugs as secondary treatments (after the crossover). This finding suggests a cross-resistance between the two drugs. The incidence of twins with letrozole (6%) was not different from the previously published 5–10% incidence of CC twins (Scialli, 1986; Imani et al., 1999). There were no differences in the other pregnancy outcomes, but the trial was not powered to assess these parameters. These data should therefore be considered preliminary.
Our PCOS participants fulfilled the universally accepted Rotterdam diagnostic criteria of PCOS and had a median BMI of ~27 kg/m2. We believe that this cohort is a good representation of PCOS women receiving fertility treatment in most fertility centres. Our results are therefore globally generalizable for clinical practice.
Our data are consistent with the recent Cochrane systematic review, which reported 44% higher pregnancy rates with the letrozole compared to CC alone with no adjuvants (OR = 1.44, 95% CI: 1.20–1.73, n = 2286) (Franik et al., 2014). However, the quality of evidence presented in that review was deemed poor by the review authors as most of the trials were neither randomized nor double blinded. The only well-designed trial by Legro et al. (2014) had a selection bias towards markedly obese PCOS women, with two-thirds of their cohort having BMI >30 kg/m2 (one-third over 40 kg/m2). This may explain their significantly lower pregnancy and LB rates compared to our trial. They, however, reported (graphically) cumulative LB data in 250 non-obese women (BMI ≤30.3 kg/m2) showing no significant (P = 0.39) difference between the two drugs. Although we have also found no statistically significant difference in LB rates in non-obese women, our results showed an obvious trend towards markedly higher LB rates with letrozole (53%) compared to CC (37%) (Table II). In contrast, the difference in Legro's trial was only small in favour of letrozole. It is worth mentioning, however, that both Legro's trial and ours are underpowered for this outcome in non-obese PCOS women.
As far as time-to-pregnancy and multiple pregnancy data are concerned, our findings seem to differ from those of Legro's trial. However, this could simply be due to lack of sufficient statistical power to assess these outcomes in either of our trials (Legro et al., 2014). Our letrozole safety data are consistent with several previous studies showing no increase in fetal/neonatal anomalies in letrozole pregnancies (Tulandi et al., 2006; Legro et al., 2014).
With regards to endometrial parameters, mid-cycle endometrium was slightly thicker with CC compared to letrozole. However, this difference is unlikely to affect the chances of pregnancy. Although endometrial thickness and pattern have been widely utilized as markers of endometrial receptivity, more recent research does not support their usefulness (Zhao et al., 2014). Our endometrial data therefore neither support nor exclude an endometrial factor for the differences in pregnancy rates between the two drugs.
A possible explanation of the higher success of letrozole is the greater ovulation rate per cycle in the letrozole group. Legro et al. (2014) hypothesized that the higher pregnancy rate with letrozole could be due to lower mid-luteal serum estradiol level and higher progesterone levels (probably due to sustained aromatase inhibition into the luteal phase) (Scialli, 1986; Dickey and Holtkamp, 1996; Imani et al., 1999; Legro et al., 2007, 2014).
It may be argued that excluding women with BMI >35 kg/m2 could limit the applicability of our results in obese women. However, the majority of fertility centres worldwide, especially in Europe, tend to exclude markedly obese women from fertility treatment due to the well-known associated challenges and risks (Zachariah et al., 2006). Another possible limitation of this RCT may be argued to be using pregnancy rather than LB as the primary outcome. However, we believe that pregnancy rate is clinically important and relevant and is commonly used in practice. A further slight concern is the long duration of the trial spanning over a 7-year period with potential differences in responses between the early and late recruits. However, the results of the interim analysis, which included the early recruits, are consistent with the final results.
In conclusion, this trial provides compelling evidence for the superiority of letrozole over clomiphene citrate as a primary OI agent in PCOS women with a 40% increase in pregnancy rates and with a shorter time-to-pregnancy. We, therefore, recommend that letrozole should replace CC as the first line OI agent in PCOS. Further research is required to investigate possible mechanisms of the increased pregnancy rates with letrozole and of the cross-resistance between the two drugs.
Supplementary data
Supplementary data are available at Human Reproduction online.
Supplementary Material
Acknowledgements
We are grateful to all participants and to all staff who have helped with the trial including Pharmacy staff, Fertility Nurses, Sonographers and R&D staff at Royal Derby Hospital. In particular, we are indebted to Margaret Harper, Jane Watson, Wendy Abbott, Diane Jamison, Carole Cooper, Jeanette Dawson and Liz Bedford for their valuable contributions to the trial. We also thank staff at the Research Department of the University of Nottingham for their support. We are grateful to the Pharmacy Production Units at Royal Hallamshire Hospital, Sheffield and Princes of Wales hospitals, Cardiff.
Authors’ roles
S.A.A.: conception of the idea, study design, recruitment, follow-up of treatment, data collection, interpretation of results and writing the article. J.S.: recruitment, data collection and article review. P.F.: randomization, sourcing and dispensing of the trial medicines and article review. A.M.: patient recruitment, data collection and entry into statistics software and article review. A.F.: study design, sample size estimations, randomization schedule, statistical analyses, study results reports and article preparation.
Funding
General Research Grant Scheme of Derby Hospitals NHS Foundation Trust. The trial also received funds from the Division of Medical Sciences & Graduate Entry Medicine, School of Medicine, University of Nottingham.
Conflict of interest
None declared.
References
- Al-Omari WR, Sulaiman WR, Al-Hadithi N. Comparison of two aromatase inhibitors in women with clomiphene-resistant polycystic ovary syndrome. Int J Gynecol Obstet 2004;85:289–291. [DOI] [PubMed] [Google Scholar]
- Asuncion M, Calvo RM, San Millan JL, Sancho J, Avila S, Escobar-Morreale HF. A prospective study of the prevalence of the polycystic ovary syndrome in unselected Caucasian women from Spain. J Clin Endocrinol Metab 2000;85:2434–2438. [DOI] [PubMed] [Google Scholar]
- Atay V, Cam C, Muhcu M, Cam M, Karateke A. Comparison of letrozole and clomiphene citrate in women with polycystic ovaries undergoing ovarian stimulation. J Int Med Res 2006;34:73–76. [DOI] [PubMed] [Google Scholar]
- Dickey RP, Holtkamp DE. Development, pharmacology and clinical experience with clomiphene citrate. Hum Reprod Update 1996;2:483–506. [DOI] [PubMed] [Google Scholar]
- Franik S, Kremer JA, Nelen WL, Farquhar C. Aromatase inhibitors for subfertile women with polycystic ovary syndrome. Cochrane Database Syst Rev 2014:CD010287. [DOI] [PubMed] [Google Scholar]
- Imani B, Eijkemans MJ, te Velde ER, Habbema JD, Fauser BC. A nomogram to predict the probability of live birth after clomiphene citrate induction of ovulation in normogonadotropic oligoamenorrheic infertility. Fertil Steril 2002;77:91–97. [DOI] [PubMed] [Google Scholar]
- Imani B, Eijkemans MJ, te Velde ER, Habbema JD, Fauser BC. Predictors of chances to conceive in ovulatory patients during clomiphene citrate induction of ovulation in normogonadotropic oligoamenorrheic infertility. J Clin Endocrinol Metab 1999;84:1617–1622. [DOI] [PubMed] [Google Scholar]
- Jonard S, Robert Y, Cortet C, Decanter C, Dewailly D. Ultrasound examination of polycystic ovaries: is it worth counting the follicles. Hum Reprod 2003;18:598–603. [DOI] [PubMed] [Google Scholar]
- Kousta E, White DM, Franks S. Modern use of clomiphene citrate in induction of ovulation. Hum Reprod Update 1997;3:359–365. [DOI] [PubMed] [Google Scholar]
- Legro RS, Barnhart HX, Schlaff WD, Carr BR, Diamond MP, Carson SA, Steinkampf MP, Coutifaris C, McGovern PG, Cataldo NA et al. Clomiphene, metformin, or both for infertility in the polycystic ovary syndrome. N Engl J Med 2007;356:551–566. [DOI] [PubMed] [Google Scholar]
- Legro RS, Brzyski RG, Diamond MP, Coutifaris C, Schlaff WD, Casson P, Christman GM, Huang H, Yan Q, Alvero R et al. Letrozole versus clomiphene for infertility in the polycystic ovary syndrome. N Engl J Med 2014;10:119–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipton A, Demers LM, Harvey HA, Kambic KB, Grossberg H, Brady C, Adlercruetz H, Trunet PF, Santen RJ. Letrozole (CGS 20267). A phase I study of a new potent oral aromatase inhibitor of breast cancer. Cancer 1995;75:2132–2138. [DOI] [PubMed] [Google Scholar]
- Massai MR, de Ziegler D, Lesobre V, Bergeron C, Frydman R, Bouchard P. Clomiphene citrate affects cervical mucus and endometrial morphology independently of the changes in plasma hormonal levels induced by multiple follicular recruitment. Fertil Steril 1993;59:1179–1186. [DOI] [PubMed] [Google Scholar]
- Miettinen OS, Nurminen M. Comparative analysis of two rates. Stat Med 1985;4:213–226. [DOI] [PubMed] [Google Scholar]
- Mitwally MF, Casper RF. Use of an aromatase inhibitor for induction of ovulation in patients with an inadequate response to clomiphene citrate. Fertil Steril 2001;75:305–309. [DOI] [PubMed] [Google Scholar]
- Nakamura Y, Ono M, Yoshida Y, Sugino N, Ueda K, Kato H. Effects of clomiphene citrate on the endometrial thickness and echogenic pattern of the endometrium. Fertil Steril 1997;67:256–260. [DOI] [PubMed] [Google Scholar]
- Newcombe RG. Interval estimation for the difference between independent proportions: comparison of eleven methods. Stat Med 1998;17:873–890. [DOI] [PubMed] [Google Scholar]
- Rotterdam ESHRE/ASRM-Sponsored PCOS consensus workshop group Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome (PCOS). Hum Reprod 2004;19:41–47. [DOI] [PubMed] [Google Scholar]
- Scialli AR. The reproductive toxicity of ovulation induction. Fertil Steril 1986;45:315–323. [DOI] [PubMed] [Google Scholar]
- Sioufi A, Gauducheau N, Pineau V, Marfil F, Jaouen A, Cardot JM, Godbillon J, Czendlik C, Howald H, Pfister C et al. Absolute bioavailability of letrozole in healthy post-menopausal women. Biopharm Drug Dispos 1997;18:779–789. [DOI] [PubMed] [Google Scholar]
- Tulandi T, Martin J, Al-Fadhli R, Kabli N, Forman R, Hitkari J, Librach C, Greenblatt E, Casper RF. Congenital malformations among 911 newborns conceived after infertility treatment with letrozole or clomiphene citrate. Fertil Steril 2006;85:1761–1765. [DOI] [PubMed] [Google Scholar]
- World Health Organization WHO Laboratory Manual for the Examination of Human Semen and Semen-Cervical Mucus Interaction, 4th edn Cambridge (UK): Cambridge University Press, 1999. [Google Scholar]
- Young SL, Opsahl MS, Fritz MA. Serum concentrations of enclomiphene and zuclomiphene across consecutive cycles of clomiphene citrate therapy in anovulatory infertile women. Fertil Steril 1999;7:639–644. [DOI] [PubMed] [Google Scholar]
- Zachariah M, Fleming R, Acharya U. Management of obese women in assisted conception units: a UK survey. Hum Fertil 2006;9:101–105. [DOI] [PubMed] [Google Scholar]
- Zhao J, Zhang Q, Wang Y, Li Y. Endometrial pattern, thickness and growth in predicting pregnancy outcome following 3319 IVF cycle. Reprod Biomed Online 2014;29:291–298. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.