Abstract
OBJECTIVE
Previous work demonstrates the consequences of falling in older adults and the potential of physical activity (PA) to reduce falls, but few studies have used accelerometer-measured PA to compare overall and time-of-day activity patterns of non-fallers, fallers, or subgroups of fallers.
METHODS
In 840 participants (mean age=66.7, s=13.2, range 26–97) of the Baltimore Longitudinal Study of Aging between 2007–2014, PA was measured objectively with Actiheart accelerometers and falling status (faller/non-faller) was assessed during an in-person interview. Differences in daily PA and PA by time-of-day were assessed using multiple linear regression. Differences in PA (multiple linear regression), and functional status (chi-squared) were further examined in subgroups of “risky” or “normal” fallers.
RESULTS
Overall, fallers and non-fallers exhibited similar daily (β=22.6, p=0.48) and time-specific PA; however, those who fell doing risky activities were more active overall (β=243.8, p=0.002), during the morning (β=77.3, p=0.004), afternoon (β=78.4, p=0.001), and late afternoon/evening (β=56.3, p=0.006) than those who fell doing normal activities. “Risky” fallers were significantly higher-functioning than “normal” fallers.
CONCLUSIONS
Persons who fell while engaging in normal activities exhibited lower PA overall and throughout most of the day, and were of lower functional status than persons who fell while engaging in risky or unusual activities, suggesting that engagement in risky or unusual PA is associated with higher functional ability and lower falls risk in older persons.
Keywords: Accidental Falls, Physical Activity, Accelerometry, Actigraphy
INTRODUCTION
Falls are estimated to be the leading cause of both fatal and non-fatal unintentional injuries in older adults.1 Annually, falls are responsible for over $30 billion in healthcare spending in the United States.2 Approximately 30 to 40% of community-dwelling older adults age 65 and older experience a fall annually and half of these falls result in some form of injury leading to declining physical function, loss of independence, illness, or even death.3 To this end, fallers generally report reduced quality of life up to 9 months or more after a fall.4
Physical activity (PA) has been shown to be an important modifiable risk factor in the prevention of falls. There is an abundance of both observational and experimental evidence demonstrating that older adults with a history of falls are less active than non-fallers, and that increasing PA may result in fall reduction.5–8 However until recently, most of these studies have measured PA subjectively with easily administered questionnaires.9 These measures are generally considered inexpensive and valid, but introduce issues like recall bias and social desirability effects.10 Moreover, their validity in older populations is likely lower, given that most older adults spend only 6–10 minutes per day in moderate or higher PA, with the rest of daily PA coming from low intensity activities related to daily living that are difficult to conceptualize and categorize as “physical activity”.11–13 In addition, older adults are more prone to recall bias than younger populations due to a greater risk of cognitive challenges leading to the potential for differential measurement error.12
Accelerometers offer an objective alternative to questionnaires for measuring daily PA, which minimizes the aforementioned biases. These devices allow measurement of total daily movement, and include low intensity activities related to daily living that are generally overlooked when using questionnaires.13 Further, objectively measured PA can help discern subtle differences in daily quantities and patterns of PA that may be important to health and functional status with aging.
To date, the association between objectively measured PA and falls has been under-addressed, apart from a few studies that show a significant inverse association between PA and falls in older adults.14,15 Moreover, this work has concentrated on total amount of daily PA, which leaves daily patterns of PA in fallers and non-fallers unaddressed. Identifying critical differences in the quantities, patterns, and trends of daily PA in fallers and non-fallers could deepen our understanding of the relationship between falls and PA, thus providing a more accurate understanding of the falls-PA relationship, and leading to more comprehensive interventions.
Given the many dire consequences of falls, identifying behaviors and patterns of behavior predictive of falls is important for reducing risk of falls, and preserving mobility and independence into late life. To this end, this study aimed to examine diurnal patterns of physical activity in a well-functioning group of older adults by falls history and corresponding characteristics using objectively measured physical activity data collected in the Baltimore Longitudinal Study of Aging (BLSA).
METHODS
Participants
The BLSA is a study of normative human aging, established in 1958 and conducted in Baltimore, MD by the National Institute on Aging Intramural Research Program. Study sampling and enrollment procedures have been described in detail elsewhere.16 Briefly, the BLSA continuously enrolls healthy volunteers that are required to be free of major chronic conditions and cognitive and functional impairment at baseline. After enrollment, participants are followed for life, attending follow-up visits and in-depth testing every 1 – 4 years depending on participant age. The BLSA began collecting objectively measured physical activity data in 2007. The population for the current study consists of 840 men and women participating in the BLSA between 2007 and 2014 who wore an activity monitor and completed an in-person health interview with a falls questionnaire. The Institutional Review Board of the National Institute of Environmental Health Sciences approved the study protocol, and all volunteers gave written informed consent prior to participation.
Study Procedure
Participants were evaluated at the Clinical Research Unit of the Translational Gerontology Branch of the National Institute on Aging over 3 days of extensive testing. Height and weight were measured according to standard protocols. A trained and certified interviewer and nurse practitioner respectively collected participant social demographic, health practices and general symptom information including falls history and conducted an extensive health history interview and physical examination.
Fall status was assessed with the question, “In the past 12 months, have you fallen and landed on the ground or floor?” This was followed up with questions detailing: (i) how many times the participant fell during the past year, (ii) whether or not an injury was sustained, and (iii) what type of activity was being performed during the fall (normal/usual or unusual/risky). Specifically, interview responses were categorized as follows:
“Fallers” were those who reported falling and landing on the ground or the floor during the previous 12 months
“Single fallers” were those who reported falling once during the previous 12 months
“Multiple fallers” were those who reported falling 2 or more times during the previous 12 months
“Normal fallers” were those who reported falling during normal/usual activities
“Risky fallers” were those who reported falling during perceived unusual or risky activities (e.g., riding a bike, hiking, yard work, major housework)
Participant functional status was assessed during the interview with standard questions asking about difficulty performing daily tasks. Specifically, whether or not a participant had difficulty walking one mile, raising their arms, or standing up from a chair without using their arms for support. Participants with “balance problems” were those who self-reported any level of difficulty keeping their balance while walking on a level surface during their participant interview.
Physical activity was assessed using the Actiheart (Actiheart, CamNtech, Ltd, Papworth, UK) combined heart rate and activity monitor. On the last day of their clinic visit, participants were fitted with the device and asked to continue wearing it at all times for the following seven days except when bathing or swimming. The device was placed horizontally on the chest at the third intercostal space with two standard electrocardiogram electrodes, a valid and reliable placement for measuring free-living physical activity.17,18 Heart rate and activity counts were measured in one-minute epochs for up to seven days, after which time the monitors were returned by express mail. Activity data were downloaded via commercial software (Actiheart, version 4.0.32) into one-minute count epochs. Days with more than 5% of data missing (more than 72 minutes per day) were excluded from the analysis. For the remaining days, missing values were imputed with the average over all of the days at the same time period during the same visit.19
Statistical Analysis
Due to the positively skewed distribution of daily total activity counts, the natural logarithm of each activity count was taken at the minute level. The daily total was then calculated using these log-transformed values, which produced a normal distribution of daily log-transformed activity counts appropriate for linear regression analysis. Although logarithmic values may be less clinically interpretable, the conclusions are the same regarding whether differences in PA exist between groups.
Multiple linear regression was used to assess the continuous association between the daily total log-transformed activity counts and falls adjusting for age, sex, education, employment, cardiovascular, neurological, lung, and kidney disease as well as arthritis, cancer, diabetes, stroke, and hypertension. Subsequent models included covariates for each fall category independently. Based on findings in previous work, interactions by age were also assessed in all models.14
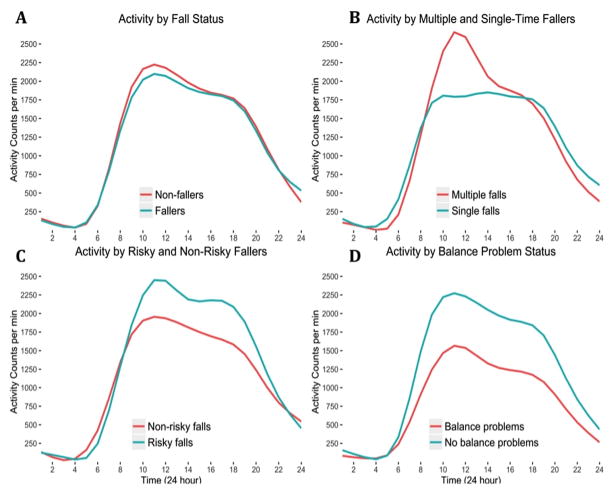
To explore differences in diurnal patterns of PA by fall category, total log-transformed activity counts were calculated and modeled in six 4-hour time bins (12:00 am – 3:59 am, 4:00 am – 7:59 am, 8:00 am – 11:59 am, 12:00 pm – 3:59 pm, 4:00 pm – 7:59 pm, 8:00 pm – 11:59 pm). Smoothed diurnal plots of activity were created to visualize differences in the temporal allocation of daily PA by fall category (Figures 1A – 1D). Based on the appearance of these plots, the association between the total log-transformed activity counts of each time bin and falls was modeled using linear regression, adjusting for age, sex, and BMI. Differences in functional status were assessed by participant self-reported ability to perform daily tasks. Differences in responses for each question were tested using chi-squared tests.
Figure 1.
Smoothed 24-hour median activity counts per minute for (A) fallers vs. non-fallers, (B) multiple vs. single-time fallers, (C) risky vs. non-risky fallers, (D) balance problems vs. no balance problems
Collinearity was examined in all models using the variance inflation factor (VIF). All VIFs were under 3, indicating the presence of little collinearity. Sensitivity analyses were performed to assess the effects of limiting the analysis to those ≥50 years and ≥65 years. Analyses were performed using Stata (version 14; StataCorp, College Station, TX) and the R Statistical software version 3.2 (http://www.r-project.org) and graphs were created with the ggplot2 R package. This study conforms to all STROBE guidelines and reports the required information accordingly (see Supplementary Checklist).
RESULTS
Participant Characteristics
Participant characteristics by fall status can be found in Table 1. The mean age of the 840 participants in the study population was 66.7 (±13.2, range 26 – 97) years. Of these participants, 637 (77.7%) reported no falls in the past 12 months while 203 (22.3%) reported falling at least once. 56 (27.6%) of the fallers fell doing “risky” or “unusual” activities. Non-fallers had a daily activity count of 36,683 (± 22,874) while that of fallers was 35,190 (± 20,382) (p = 0.41). Fallers had significantly worse balance than non-fallers (p < 0.001). Of those who reported falling in the past year, 142 (70.0%) fell during normal or routine activities, 56 (27.6%) fell during “risky” or unusual activities, and 5 (2.5%) fell while intoxicated or for undisclosed reasons. Comparing functional status between “risky” and “normal” fallers, “risky” fallers had significantly better balance (p = 0.04) and were less likely to report difficulty walking one mile (p = 0.03), raising their arms (p = 0.04), or standing up from a chair without using their arms for support (p = 0.01). In addition, those with poor balance were more likely to report a history of CVD (p < 0.001), stroke (p < 0.001), neurological problems (p <0.001), diabetes (p = 0.04), cancer (p < 0.001), and lower extremity arthritis (p < 0.001).
Table 1.
Participant characteristics by falling status (N = 840)
| Participant characteristics (2007 – 2014) | Non-fallers (n = 637) | Fallers (n = 203) | p Value* | ||
|---|---|---|---|---|---|
|
| |||||
| Mean | SD (%) | Mean | SD (%) | ||
| Age (y) | 66.4 | 13.1 | 67.9 | 12.9 | 0.16 |
| Male sex, no. | 283 | (44.4) | 85 | (41.9) | 0.52 |
| Body mass index (kg/m2) | 27.2 | 4.6 | 27.8 | 5.5 | 0.15 |
| Usual gait speed (m/s) | 1.18 | 0.24 | 1.15 | 0.22 | 0.07 |
| Balance Difficulty, no. | 58 | (9.1) | 39 | (19.3) | < 0.001 |
| Race, no. | |||||
| White | 412 | (64.7) | 157 | (77.3) | 0.004 |
| Black | 178 | (27.9) | 36 | (17.7) | 0.004 |
| Other | 47 | (7.4) | 10 | (4.9) | 0.004 |
| Education (y) | 16.8 | 2.5 | 17.3 | 2.4 | 0.02 |
| Employed, no. | 314 | (49.4) | 96 | (47.3) | 0.61 |
| Coronary heart disease, no. | 57 | (9.2) | 17 | (8.5) | 0.78 |
| Stroke, no. | 33 | (53.3) | 11 | (55.3) | 0.91 |
| Diabetes, no. | 37 | (6.0) | 22 | (11.1) | 0.02 |
| Cancer, no. | 180 | (29.1) | 54 | (27.1) | 0.60 |
| Hypertension, no. | 240 | (38.8) | 80 | (40.2) | 0.72 |
| Daily activity counts | 36,683 | 22,874 | 35,190 | 20,382 | 0.41 |
Note:
p value for group comparison, analysis of variance for continuous measure, and chi-squared test for proportions
Differences in Daily PA
Consistent with previous results from the BLSA, older age and male sex were negatively associated with total daily activity, while current employment was positively associated (p < 0.002 for all).19,20 Total daily PA did not differ by fall status (faller vs. non-faller; β = 22.6, p = 0.48), although multiple fallers tended to be more active (β = 42.5, p = 0.07). In sub-analyses by type of fall, “risky” fallers were more active than non-fallers (β = 227.8, p < 0.001) and “normal” fallers (β = 243.8, p = 0.002), and were more likely to report falling multiple times (p = 0.07). Those who fell doing normal activities did not differ in daily PA compared to non-fallers (β = −17.3, p = 0.70).
Differences in PA by Time-of-Day
Daily activity patterns were first compared graphically by plotting the unadjusted median activity counts per minute over a 24-hour period (Figures 1A – D). Consistent with the combined analysis, there were no differences in PA between fallers and non-fallers by time-of-day (Figure 1A). Among fallers, those who reported falling multiple times were more active during the morning (8:00 am – 11:59 am [β = 61.2, p = 0.01]) than those who reported falling once (Figure 1B).
In subgroup analyses comparing “risky” to “normal” fallers, “risky” fallers were significantly more active than “normal” fallers in the morning during the 8:00 – 11:59 am interval (β = 77.3, p = 0.004, Figure 1C), maintaining this higher level of PA into the early afternoon period between 12:00 pm – 3:59 pm (β = 78.4, p = 0.001, Figure 1C) as well as the late afternoon and evening hours between 4:00 – 7:59 pm (β = 1618.2, p = 0.03, Figure 1C). When comparing daily activity by balance status, those with poor balance appeared to significantly lag behind those without balance difficulties beginning in the afternoon, lasting into the evening hours (Figure 1D). These differences reached statistical significance in all time intervals except the early (12:00 – 3:59 am, Figure 1D) and late morning (8:00 – 11:59 am, Figure 1D). In general, fallers overall, “normal” fallers, those reporting balance difficulty, and those who reported falling only once had lower peak PA during mid-day than their comparators (Figure 1A – 1D). A summary of regression coefficients representing adjusted differences in total log-counts and significance levels from the linear regressions for each sub-group and time interval is provided in Table 2.
Table 2.
Mean difference in log-transformed total activity counts for various subgroups by time bins from a linear regression model controlling for age, gender, and BMI.
| Subgroups | Time bins | |||||
|---|---|---|---|---|---|---|
| 12:00 – 4:00 am | 4:00 – 8:00 am | 8:00 – 12:00 pm | 12:00 – 4:00 pm | 4:00 – 8:00 pm | 8:00 – 12:00 am | |
| Beta coefficient (p Value) | Beta coefficient (p Value) | Beta coefficient (p Value) | Beta coefficient (p Value) | Beta coefficient (p Value) | Beta coefficient (p Value) | |
| Fallers vs. non-fallers | 0.3* (0.94) | 0.6 (0.95) | 1.4 (0.91) | 17.0 (0.15) | 10.4 (0.32) | 0.7 (0.93) |
| Multiple vs. single falls | −9.6† (0.14) | 0.7 (0.96) | 61.2 (0.01) | 35.7 (0.10) | −16.6 (0.38) | −7.7 (0.63) |
| “Risky” fallers vs. “normal” fallers | 6.2‡ (0.37) | −16.1 (0.40) | 77.3 (0.004) | 78.4 (0.001) | 56.3 (0.006) | 21.8 (0.21) |
| Balance problems vs. no balance problems | −0.8§ (0.89) | −16.4 (0.22) | −27.8 (0.10) | −43.8 (0.008) | −42.8 (0.003) | −24.6 (0.048) |
Note: Log transformation = ln(counts + 1); Bold numbers indicates statistical significance.
The mean log-transformed activity counts for fallers was 0.3 log-counts higher than non-fallers, with similar interpretation for other bins.
The mean activity counts for multiple fallers was 9.6 log-counts lower than single fallers.
The mean activity counts for “risky” fallers was 6.2 log-counts higher than normal fallers.
The mean activity counts for those with balance problems was 0.8 log-counts lower than those without balance
DISCUSSION
In combined analyses, there were no differences in levels of total daily PA between fallers and non-fallers. Previous work has reported that the relationship between PA and falls is typically modified by age, and that in younger adults higher PA tends to be associated with more falls while in older adults greater PA tends to be associated with fewer falls.14 This is likely due to fundamental differences in daily quantities, patterns, and trends of PA between younger, healthier individuals and older, less-functionally intact persons. Previous research has supported the dose-response association between PA and falls with aging, but has not examined differences in PA by time of day, relying on daily summary measures that may not accurately reflect differences in daily PA by falling status. The current results expand upon the PA and falls literature by characterizing daily PA quantities, patterns, and trends among several important groups of older adults of varying functional statuses from which unique daily insights can be gleaned and falls-reduction interventions can be tailored to preserve mobility and independence into late life.
Individuals with reported balance difficulties exhibited significantly lower PA beginning in the afternoon into the night and were more likely to report a history of CVD, stroke, neurological problems, diabetes, cancer, and lower extremity arthritis, demonstrating the complexity of the associations among poor balance, chronic conditions, daily PA, and risk of falls. “Risky” fallers had significantly higher PA compared to “normal” fallers throughout most of the day, beginning in the morning (8:00 am) and lasting until night (7:59 pm), with the greatest differences present in the morning and afternoon. Multiple fallers had higher peaks of daily PA, overall, compared to single fallers and interestingly “risky” fallers were more likely to be multiple fallers than “normal” fallers. This consistently lower PA among “normal” fallers may be indicative of greater functional challenges with activities related to daily living or more difficulty managing chronic conditions as well as a greater propensity for fatigue, which may further contribute to the onset and progression of sedentary behaviors with aging.21
Taken together, the current findings suggest that older adults with greater disease burden and poorer functional status may be more easily fatigued or experience a greater fear of falling compared to their healthier, more functional counterparts.22–24 The often substantial differences in PA between groups of varying functional statuses, especially around mid-day, support the hypothesis that these time-of-day differences can be quite informative regarding health and functioning in older adults. Though cross-sectional, these findings highlight time-of-day differences that may be helpful in designing interventions to reduce falls by targeting PA increases for times where PA is typically lower. Given the established success of PA interventions in older populations, these targeted interventions could potentially enhance and add to the ability to increase mobility and quality of life.5–8 In addition, identifying time of day differences in PA by functional status will allow more focused efforts and directed clinical discussions with patients to overcome the obstacles potentially contributing to lower PA during these times.
This study has several limitations. First, participants in the BLSA are healthier than the general population. This may attenuate the differences in PA between fallers and non-fallers, resulting in an underestimation of the true relationships among comorbidities, employment, and PA with aging. To account for the high-functioning level of participants, the current analysis compared activity levels of those that fell doing “risky” or unusual activities with those that fell doing normal routine activities. These two groups represent two very different types of individuals as demonstrated by the significantly higher PA, better balance, and lower prevalence of reported functional challenges in the “risky” fallers compared to the “normal” fallers. Those that are able to engage in activities they perceive to be risky are likely functionally superior to those who fall doing normal activities like getting out of bed or into the shower. Thus, by comparing differences in PA in these two groups, it is possible to examine how highly functioning individuals differ by total daily PA as well as PA throughout the day, compared to less functional individuals more prone to falling during routine tasks, highlighting differences that are important for sustaining PA and function later into life. Second, the measurement of falls with a health interview questionnaire is subject to substantial recall bias. Importantly, those who remember their falls are more likely to have sustained injuries, and less-intense falls may not be reported. Finally, the cross-sectional design of this analysis prevents causal inference and direction of associations from being determined.
The health benefits of PA are well established, but a more comprehensive understanding of the benefit of the overall amount of time spent ambulatory, as well as the diurnal patterns of daily PA will aid in the establishment of improved recommendations, interventions for maintaining daily PA into late life, and focused clinician-assisted interventions to overcome specific patient obstacles responsible for these time-specific differences. The current findings use such metrics to add to the substantial literature on PA and falls by highlighting fundamental differences in objectively measured total and time of day PA in a well-functioning population of older adults. Future longitudinal research on the directionality of the associations presented in these analyses, as well as interventions to improve daily nadirs of activity is warranted.
Supplementary Material
Acknowledgments
FUNDING
This work was supported by the Intramural Research Program of the NIH, National Institute on Aging. Data for these analyses were obtained from the Baltimore Longitudinal Study of Aging, an ongoing study of normative aging conducted by the National Institute on Aging.
Author Contributions:
Anthony Nastasi: Study design, analysis, interpretation of data, preparation of manuscript
Alka Ahuja: Analysis, interpretation of data, preparation of manuscript
Vadim Zippunikov: Analysis, interpretation of data, preparation of manuscript
Eleanor Simonsick: Interpretation of data, preparation of manuscript
Stephanie Studenski: Interpretation of data, preparation of manuscript
Luigi Ferrucci: Interpretation of data, preparation of manuscript
Jennifer Schrack: Data acquisition, study design, analysis, interpretation of data, preparation of manuscript
Sponsor’s Role: Not applicable.
Footnotes
This work was presented at the Johns Hopkins 3rd Annual Research on Aging Showcase, winning 3rd place.
Conflict of interest: The authors declare that they have no sources of funding or conflicts of interest relevant to the analysis to report.
References
- 1.Stevens JA, Mack KA, Paulozzi LJ, et al. Self-reported falls and fall-related injuries among persons aged>or=65 years--United States, 2006. Journal of safety research. 2008;39:345–9. doi: 10.1016/j.jsr.2008.05.002. [DOI] [PubMed] [Google Scholar]
- 2.Bohl AA, Fishman PA, Ciol MA, et al. A longitudinal analysis of total 3-year healthcare costs for older adults who experience a fall requiring medical care. Journal of the American Geriatrics Society. 2010;58:853–60. doi: 10.1111/j.1532-5415.2010.02816.x. [DOI] [PubMed] [Google Scholar]
- 3.Hausdorff JM, Rios DA, Edelberg HK. Gait variability and fall risk in community-living older adults: a 1-year prospective study. Archives of physical medicine and rehabilitation. 2001;82:1050. doi: 10.1053/apmr.2001.24893. [DOI] [PubMed] [Google Scholar]
- 4.Hartholt KA, van Beeck EF, Polinder S, et al. Societal consequences of falls in the older population: injuries, healthcare costs, and long-term reduced quality of life. The Journal of trauma. 2011;71:748–53. doi: 10.1097/TA.0b013e3181f6f5e5. [DOI] [PubMed] [Google Scholar]
- 5.Robertson MC, Gillespie LD. Fall prevention in community-dwelling older adults. Jama. 2013;309:1406–7. doi: 10.1001/jama.2013.3130. [DOI] [PubMed] [Google Scholar]
- 6.El-Khoury F, Cassou B, Charles MA, et al. The effect of fall prevention exercise programmes on fall induced injuries in community dwelling older adults: systematic review and meta-analysis of randomised controlled trials. BMJ (Clinical research ed) 2013;347:f6234. doi: 10.1136/bmj.f6234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gillespie LD, Robertson MC, Gillespie WJ, et al. Interventions for preventing falls in older people living in the community. The Cochrane database of systematic reviews. 2012;9:Cd007146. doi: 10.1002/14651858.CD007146.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Greenwood-Hickman MA, Rosenberg DE, Phelan EA, et al. Participation in Older Adult Physical Activity Programs and Risk for Falls Requiring Medical Care, Washington State, 2005–2011. Preventing chronic disease. 2015;12:E90. doi: 10.5888/pcd12.140574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pereira CL, Baptista F, Infante P. Role of physical activity in the occurrence of falls and fall-related injuries in community-dwelling adults over 50 years old. Disability and rehabilitation. 2014;36:117–24. doi: 10.3109/09638288.2013.782355. [DOI] [PubMed] [Google Scholar]
- 10.Prince SA, Adamo KB, Hamel ME, et al. A comparison of direct versus self-report measures for assessing physical activity in adults: a systematic review. The international journal of behavioral nutrition and physical activity. 2008;5:56. doi: 10.1186/1479-5868-5-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sallis JF, Saelens BE. Assessment of physical activity by self-report: status, limitations, and future directions. Research quarterly for exercise and sport. 2000;71:S1–14. [PubMed] [Google Scholar]
- 12.Washburn RA. Assessment of physical activity in older adults. Research quarterly for exercise and sport. 2000;71(Suppl 2):79–87. doi: 10.1080/02701367.2000.11082790. [DOI] [PubMed] [Google Scholar]
- 13.Troiano RP, Berrigan D, Dodd KW, et al. Physical activity in the United States measured by accelerometer. Medicine and science in sports and exercise. 2008;40:181–8. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 14.Cauley JA, Harrison SL, Cawthon PM, et al. Objective measures of physical activity, fractures and falls: the osteoporotic fractures in men study. Journal of the American Geriatrics Society. 2013;61:1080–8. doi: 10.1111/jgs.12326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jefferis BJ, Iliffe S, Kendrick D, et al. How are falls and fear of falling associated with objectively measured physical activity in a cohort of community-dwelling older men? BMC geriatrics. 2014;14:114. doi: 10.1186/1471-2318-14-114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stone JL, Norris AH. Activities and attitudes of participants in the Baltimore longitudinal study. Journal of gerontology. 1966;21:575–80. doi: 10.1093/geronj/21.4.575. [DOI] [PubMed] [Google Scholar]
- 17.Brage S, Brage N, Ekelund U, et al. Effect of combined movement and heart rate monitor placement on physical activity estimates during treadmill locomotion and free-living. European journal of applied physiology. 2006;96:517–24. doi: 10.1007/s00421-005-0112-6. [DOI] [PubMed] [Google Scholar]
- 18.Villars C, Bergouignan A, Dugas J, et al. Validity of combining heart rate and uniaxial acceleration to measure free-living physical activity energy expenditure in young men. Journal of applied physiology (Bethesda, Md : 1985) 2012;113:1763–71. doi: 10.1152/japplphysiol.01413.2011. [DOI] [PubMed] [Google Scholar]
- 19.Schrack JA, Zipunnikov V, Goldsmith J, et al. Assessing the “physical cliff”: detailed quantification of age-related differences in daily patterns of physical activity. The journals of gerontology Series A, Biological sciences and medical sciences. 2014;69:973–9. doi: 10.1093/gerona/glt199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Xiao L, Huang L, Schrack JA, et al. Quantifying the lifetime circadian rhythm of physical activity: a covariate-dependent functional approach. Biostatistics. 2015;16(2):352–367. doi: 10.1093/biostatistics/kxu045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nagano H, James L, Sparrow WA, et al. Effects of walking-induced fatigue on gait function and tripping risks in older adults. J Neuroeng Rehabil. 2014 Nov 15;11:155. doi: 10.1186/1743-0003-11-155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Landers MR, Oscar S, Sasaoka J, et al. Balance Confidence and Fear of Falling Avoidance Behavior Are Most Predictive of Falling in Older Adults: Prospective Analysis. Phys Ther. 2016 Apr;96(4):433–42. doi: 10.2522/ptj.20150184. [DOI] [PubMed] [Google Scholar]
- 23.Sibley Km, Voth J, Munce SE, et al. Chronic disease and falls in community-dwelling Canadians over 65 years old: a population-based study exploring associations with number and pattern of chronic conditions. BMC Geriatr. 2014 Feb 14;14:22. doi: 10.1186/1471-2318-14-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Oh E, Hong GS, Lee S, Han S. Fear of falling and its predictors among community-living older adults in Korea. Aging Ment Health. 2015 Oct 19;:1–10. doi: 10.1080/13607863.2015.1099034. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.