Abstract
Objectives
the objectives of this review were (1) to assess whether interventions to support effective communication between maternity care staff and healthy women in labour with a term pregnancy could improve birth outcomes and experiences of care; and (2) to synthesize information related to the feasibility of implementation and resources required.
Design
a mixed-methods systematic review.
Setting and participants
studies which reported on interventions aimed at improving communication between maternity care staff and healthy women during normal labour and birth, with no apparent medical or obstetric complications, and their family members were included. ‘Maternity care staff’ included medical doctors (e.g. obstetricians, anaesthetists, physicians, family doctors, paediatricians), midwives, nurses and other skilled birth attendants providing labour, birth and immediate postnatal care. Studies from all birth settings (any country, any facility including home birth, any resource level) were included.
Findings
two papers met the inclusion criteria. One was a step wedge randomised controlled trial conducted in Syria, and the other a sub-analysis of a randomised controlled trial from the United Kingdom. Both studies aimed to assess effects of communication training for maternity care staff on women's experiences of labour care. The study from Syria reported that a communication skills training intervention for resident doctors was not associated with higher satisfaction reported by women. In the UK study, patient-actors’ (experienced midwives) perceptions of safety and communication significantly improved for postpartum haemorrhage scenarios after training with patient-actors in local hospitals, compared with training using manikins in simulation centres, but no differences were identified for other scenarios. Both studies had methodological limitations.
Key conclusions and implications for practice
the review identified a lack of evidence on impact of interventions to support effective communication between maternity care staff and healthy women during labour and birth. Very low quality evidence was found on effectiveness of communication training of maternity care staff. Robust studies which are able to identify characteristics of interventions to support effective communication in maternity care are urgently needed. Consideration also needs to be given to how organisations prepare, monitor and sustain interventions to support effective communication, which reflect outcomes of priority for women, local culture and context of labour and birth care.
Keywords: Communication, Intrapartum care, Childbirth, Labour, Obstetric delivery, Interpersonal relations
Highlights
-
•
The review found only two studies on interventions for effective communication.
-
•
Neither study considered clinical outcomes of interventions.
-
•
Satisfaction with care was considered in both studies.
-
•
Neither study presented qualitative data on women's and clinicians’ experiences.
-
•
Current evidence is inadequate to inform content of training or practice.
Introduction
Current national (such as in the United Kingdom) and international guidance proposes that effective communication, support and compassion from maternity care staff can help a woman during labour and birth to feel in control, feel her wishes are respected, and contribute to a positive birth experience (e.g. White Ribbon Alliance, 2012; WHO, 2016; NICE, 2017). The provision of good communication is at the core of recent international and national guidance for improving women's outcomes of birth. The recently published World Health Organization (WHO) framework for improving quality of care for mothers and newborns around the time of childbirth in health facilities recognizes two important components of care: the quality of the provision of care and the quality of care as experienced by women and their families (World Health Organization (WHO), 2016, Tuncalp et al., 2015). The framework contains eight domains of quality, one of which is communication, with the standard that ‘communication with women and their families is effective and responds to their needs and preferences’ (Standard 4, WHO, 2016).
The importance of effective communication in healthcare has long been recognised, and there is extensive literature on this in general healthcare. Recent examples include reviews of the role of communication in decision making (Ames et al., 2017) and a review of how patient experiences may impact on clinical safety and effectiveness of outcomes (Doyle et al., 2013). In maternity care, authors have explored the role of communication in the provision of respectful care (Vogel et al., 2016). Communication is at the core of health professional education, with training and assessment in communication skills included in medical, midwifery and nursing curricula in the United States of America (USA), United Kingdom (UK) and some European countries (Deveugele et al., 2005, Butler et al., 2008, Bosse et al., 2010, King and Hoppe, 2013). In some countries, demonstrated competency to provide good communication, including verbal, non-verbal and written communication, is a requirement for registration to practice as a clinician (for example, ‘UK Standards for Pre-Registration Education’, Nursing and Midwifery Council, 2015). However, despite the acknowledged importance of communication, there is no consensus definition of ‘effective communication’ in general health care or in maternity care.
Global support for scaling up midwifery-led care includes the potential to improve women-centred communication (Homer et al., 2014), with women reported as wanting consistent, high quality information, and better communication about their care between maternity staff they encounter (National Maternity Review, 2016). Despite these endeavours, there is widespread evidence of women's perceptions of the continuing failure by clinicians to effectively communicate with them during labour and birth, with adverse consequences including women not feeling in control and not being listened to (Green and Baston, 2003; Care Quality Commission, 2013; Alderdice et al., 2016)). Experiences of poor or disrespectful care, including how women felt they were treated during labour, could trigger the onset of postpartum post-traumatic stress disorder (Ayers et al., 2016), impact on a woman's relationship with her infant (Hauck et al., 2007) and adversely impact on a woman's experiences and satisfaction with her birth (Mannava et al., 2015). Furthermore, if not addressed, these issues could discourage women and communities from using facilities to give birth, particularly in lower-resource settings where access to this care may be vital for maternal and newborn health (Bohren et al., 2014, Bohren et al., 2015).
An initial scoping search for this review identified no clear evidence to underpin recent policy recommendations with respect to the impact of effective communication on labour and birth outcomes or women's experiences. This systematic review therefore aimed to assess whether interventions to support effective communication between maternity care staff and healthy women in labour with a term pregnancy could improve birth outcomes and experiences of care. It also aimed to synthesize information related to the feasibility of implementation and resources required. This formed one of a series of linked reviews commissioned by the WHO to underpin forthcoming global guidance on effective intrapartum care of healthy women going into labour at term (WHO, in press). Other reviews in the WHO series included respectful maternity care during labour and birth, pain relief and the presence of a companion of choice at birth. No current or planned reviews on effective communication during labour and birth were identified through a search of the Cochrane Library, Joanna Briggs Institute and PROSPERO.
Methods
A mixed-methods synthesis methodology was planned (see PROSPERO registration CRD42017070485 for detail). The review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Moher et al., 2009). We refer below to the review questions, search and screening for quantitative and qualitative evidence in line with our protocol. As no qualitative studies met the inclusion criteria, we report below on quality assessment, data extraction, synthesis and findings for the included quantitative papers.
Review questions
The review aimed to address the following questions:
-
(1)
For women during labour, birth and immediately after birth, do interventions to promote effective communication by maternity care staff compared with usual care improve birth and other outcomes, and do these outcomes vary by type of intervention? (See Box 1 for outcomes of interest).
-
(2)
How do women, family members and maternity care staff experience interventions to improve effective communication during labour, birth and immediately after birth in global settings where skilled maternity care is available, compared (where appropriate) to usual care (with no targeted communication intervention)?
-
(3)
What are the characteristics of an effective communication intervention for positive birth outcomes?
-
(4)
What additional resources are needed in birth settings to implement and sustain effective communication interventions?
Box 1. Outcomes of interest.
Primary outcomes of interest:
-
•
Mode of birth (spontaneous vaginal birth, emergency caesarean section, instrumental vaginal birth)
-
•
Mobility in labour
-
•
Perineal/vaginal trauma (1st-4th degree tears, episiotomy)
-
•
Perinatal asphyxia, low Apgar score (<7) at 5 minutes, cord blood acidosis, need for major
resuscitation (respiratory support, intubation at birth), hypoxic ischaemic encephalopathy
-
•
Skin to skin care, latching of baby on breast within first hour of birth
-
•
Initiation of breastfeeding
-
•
Women’s experiences of labour and birth, perspectives of their autonomy and satisfaction with care offered, perspectives on their health and well-being
Secondary outcomes of interest:
-
•
Length of labour (duration of 1st or 2nd stage or as defined by study authors)
-
•
Perception of labour pain, use of pain relief methods (during labour and the immediate postpartum period, non-pharmacological, regional analgesia, epidural)
-
•
Birth position for second stage of labour
-
•
Access to or intake of fluids during labour
-
•
Onset of maternal mental health disorders (PTSD, anxiety, depression) within first 8 weeks of birth
-
•
Use of medical interventions during labour (including amniotomy and oxytocin augmentation)
-
•
Healthcare resource use
-
•
Women’s/family members’ and maternity staff's perceptions and experiences of communication interventions including information about what women value from the intervention offered and women’s preferences for different aspects of communication
-
•
Safety of care, including escalation of concerns by women, their families or maternity care staff
-
•
Acceptability of the communication interventions to the intended recipients such as women, their families and maternity care staff, and feasibility of implementation as perceived by maternity care staff, service commissioners and providers
-
•
Outcome measures relating to the costs of a communication intervention or to cost-effectiveness, (such as cost per facility-based birth) and to cost-utility (such as per quality- or disability-adjusted life year gained) will be included in the review
Eligibility criteria
Eligible studies included primary research studies published from January 1996 to July 2017, to ensure that data reflected contemporary intrapartum care practices. Studies published in scientific journals, studies in the ‘grey literature’ (which reported methods and data) and PhD theses were considered for inclusion. We searched for studies on implementation of interventions to improve communication between maternity care staff and women, to improve birth outcomes and/or enhance women's experiences of care in labour, birth or immediately after birth. No study designs were excluded. Systematic reviews on the topic were excluded, but any papers included in an identified review were checked for eligibility. Papers which only reported family members’ experiences of interventions were not eligible.
Outcomes of interest
Outcomes of interest including perspectives of women and relevant clinical outcomes replicated those used across the linked WHO reviews referred to earlier (WHO, in press). In addition, the review sought to identify evidence about effective communication interventions and women's and family's perspectives of birth (sense of control, shared decision-making), experiences of informed choice, autonomy, feeling safe, including escalation of concerns by women, their families or maternity care staff (see Box 1).
Setting and population
Healthy women during normal labour and birth, with no apparent medical or obstetric complications, and their family members were included. ‘Maternity care staff’ included medical doctors (e.g. obstetricians, anaesthetists, physicians, family doctors, paediatricians), midwives, nurses, and other skilled birth attendants providing labour, birth and immediate postnatal care. All birth settings (any country, facility and home births, and any resource level) were eligible for inclusion.
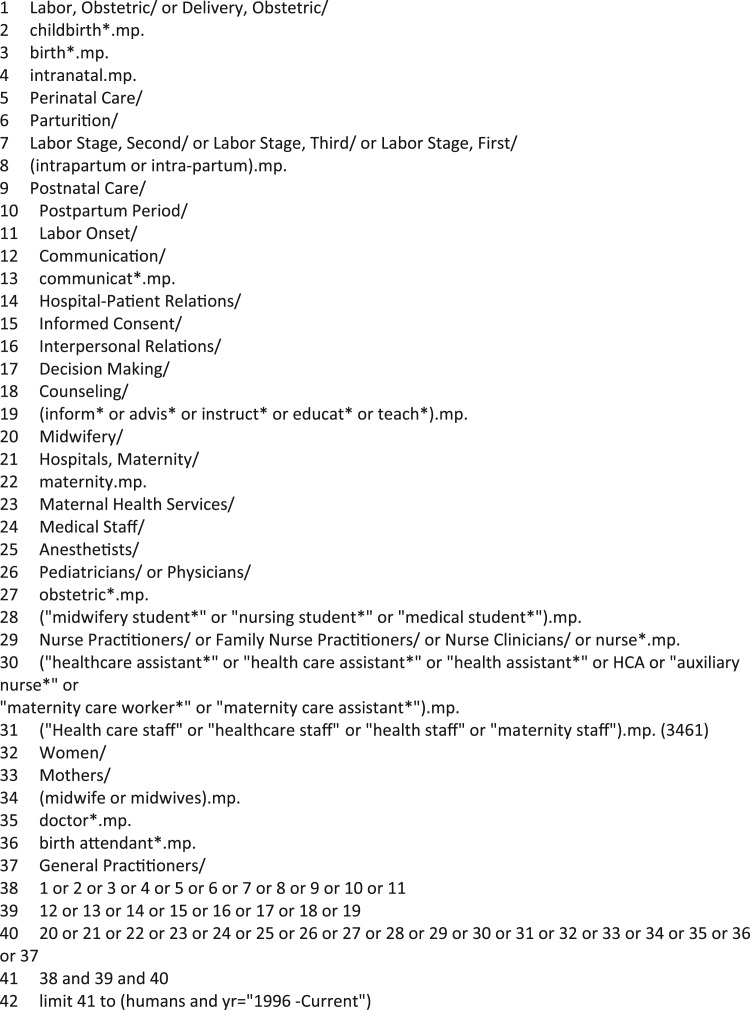
Search strategy
An initial limited search of MEDLINE, CINAHL and SCOPUS was conducted to identify studies published in English during 2014–2016, followed by analysis of the text words contained in the title and abstract and index terms used to describe articles. A second search using identified keywords and index terms was undertaken in the following databases: MEDLINE, CINAHL, PsycINFO, EMBASE, Latin American and Caribbean Health Sciences (LILACS), AJOL (for studies conducted in Africa), Cochrane Central Register of Controlled Trials, and SCOPUS. Initial keywords and index terms included intrapartum care, birth, perinatal care, postnatal care, labour stage, communication, informed consent, interpersonal relations, counselling, maternity, midwifery, medical staff, healthcare assistant, healthcare staff, women and mothers. An example of a search strategy from one bibliographic database is provided in Fig. 1 which also illustrates the use of truncations and Boolean operators. No language restrictions were placed for this search. The reference list of all included publications and identified reviews were searched for additional studies, and for references to grey reports or literature. A call for grey literature was also circulated via the JISCmail ‘midwifery-research’ email group, which reaches international researchers usually based in higher education settings. A citation search of included papers was also conducted.
Fig. 1.
Electronic search strategy (Medline).
Study screening
Identified papers were initially assessed for relevance based on the title by Y-SC, KC and DB. Following the initial assessment, two authors (Y-SC, KC) independently screened all abstracts against inclusion criteria. The abstracts of studies published in languages other than English were translated into English using freely available online software (Google Translate). Y-SC and KC retrieved the full text of all papers considered to be relevant, and independently assessed the papers for relevance according to a priori inclusion criteria as above. A random check of around 1% of the papers at the initial assessment, of around 10% at abstract screening stage, and of 100% at full-text screening stage was undertaken by AGP. Any disagreements were resolved through discussion or through consultation with DB.
Quality appraisal
Two authors (MF, DB) independently assessed the risk of bias of the two included papers which were randomised control trials, adhering to recommendations in the Cochrane Handbook for Systematic Review of Interventions (Higgins and Green, 2011). Any disagreements were resolved through discussion. Papers would not have been excluded based on quality appraisal.
Data extraction
Data were extracted from the included papers by MF and Y-SC, and verified by DB. The data extracted included details about the interventions, populations, study methods, and outcomes of significance to the review question(s) (see Table 1).
Table 1.
Characteristics of included studies.
| Study | Aims of study | Intervention type | Participants | Methodology | Outcome measures | Important results |
|---|---|---|---|---|---|---|
| Bashour et al., 2013 (Syria) | To measure effects of training doctors in interpersonal and communication skills on women’s satisfaction with doctor-women relationship in labour and delivery rooms. | A specially designed training package in communication skills provided to all resident doctors. | Four hospitals (cluster). The intervention was delivered to 137 doctors. A total of 2,000 women participated in the study. | Stepped- wedge cluster randomised trial. | Women’s satisfaction with interpersonal and communication skills of doctors during labour and birth using a Modified Medial Interview Satisfaction Scale (MMISS-21). | The individual level mean satisfaction score was 3.23 (SD 0.72) in the control group and 3.42 (0.73) in the intervention group (a possible score ranged from 1 to 5, with higher values indicating that women were satisfied with the services provided to them). |
| No differences were detected in means for average satisfaction scores of women following use of generalised linear mixed models (95% CI -0.08 to 0.15). | ||||||
| Crofts et al., 2008 (UK) | To measure effects of training on patient-actor perceptions of care (communication, respect and safety) from doctors and midwives during simulated obstetric emergencies. | Four obstetric emergency training: (a) 1 day course at local hospitals; (b) 1 day course at simulation centre; (c) 2 day course with teamwork training at local hospitals; and (d) 2 day course with teamwork training at local simulation centre. | 140 midwives and doctors from six hospitals were randomized to one of four obstetric emergency training interventions. | Randomised control trial | Patient-actors’ (experienced midwives) perceptions of care in relation to communication, safety and respect, were measured using a Likert scale on the 3 simulated emergency scenarios (eclampsia, post-partum haemorrhage, shoulder dystocia). | All patient-actor perception scores in all three emergency scenarios showed statistical significant improvement post-training (p = 0.017 to ˂ 0.001). |
| In terms of perception of communication scores in the three emergency scenarios, statistical significant improvement post-training was only shown during the post-partum haemorrhage scenario (p = 0.035). | ||||||
| There were no statistical significant differences of patient-actor perception scores for participants who received additional teamwork training and those who did not (p = 0.147 to 0.899) |
Assessing the quality of evidence from the review
The GRADE (Grading of Recommendations Assessment, Development and Evaluation) (GRADE Working Group, 2008, Andrews et al., 2013) approach to appraising the quality of quantitative evidence was used for all outcomes identified.
Results
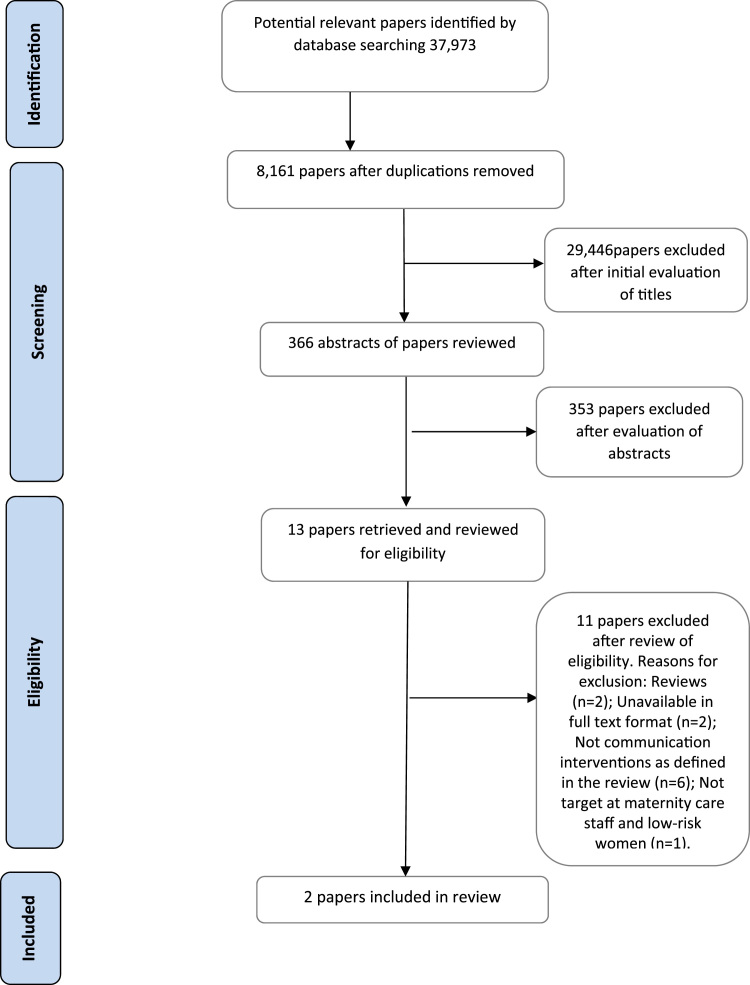
The systematic search identified 37,973 papers. After removing duplicates, 8,161 papers remained, the titles of which were assessed for relevance, after which 366 abstracts were assessed for eligibility. Thirteen papers were retrieved for full-text assessment. Of these, eleven were excluded (see PRISMA diagram Fig. 2). No qualitative studies or grey literature publications were identified. Only two papers met the study eligibility criteria (see Table 1), a step wedge randomised controlled trial (RCT) from Syria (Bashour et al., 2013) and a sub-analysis of a randomised controlled trial conducted in the UK (Crofts et al., 2008). Due to differences in the study designs, contexts of care, study populations and how outcomes were defined and reported in the two studies, meta-analysis could not be undertaken. Data are therefore presented in narrative form.
Fig. 2.
Flow chart of stages of searching.
Bashour et al.'s (2013) trial evaluated a training package designed to strengthen the communication skills of resident doctors (n = 137) at four public maternity hospitals in Damascus. The training content related to characteristics and principles of effective communication, how to overcome barriers to effective communication and improve interactions with women during labour and birth. Data collection included 2,000 women who gave birth between April 2008 and January 2009. Participatory methods were applied in the training workshops, led by a member of the research team described as a national trainer with experience in communication skills who, together with members of the research team, observed and facilitated the training. Each workshop lasted twenty hours in total and was delivered over three days. The training package was rolled out at four time points separated by two months each. Each hospital contributed one cluster to the control arm, and (during the last time period) one to the intervention arm.
Timing of implementation of the training package in each hospital was determined when clusters ‘switched’ from the control to the intervention arm. The primary outcome was women's satisfaction with interpersonal and communication skills of doctors during their labour and birth, as measured at two weeks postnatally using a modified version of the Medical Interview Satisfaction Scale (MISS-21) (Meakin and Weinman, 2002). Secondary outcomes included the communicative behaviour of doctors, as documented using a checklist based on the Al-Galaa observational checklist which was developed in Egypt to record normal labour and birth practices (Sholkamy et al., 2003). Outcomes were measured two to three weeks after implementation of the training package.
Crofts et al.'s (2008) study explored effects of training on patient-actor perceptions of care from doctors and midwives (n = 140) during simulated obstetric emergencies, based on sub-analysis of data from a prospective RCT conducted in six maternity hospitals in the South-West of England. Clinicians were randomized to one of four obstetric emergency training interventions: a one-day course at a local hospital; a one-day course at a simulation centre; a two-day course with teamwork training at a local hospital; and a two-day course with teamwork training at a simulation centre. Training at local hospitals used a patient-actor, while training at the simulation centre was conducted using computerised patient manikins. The two-day training courses included additional teamwork training on communication, roles and responsibilities, and situational awareness (an individual's perception of what is happening around them in terms of surroundings, environment, time, space, and threats to safety which could impact on decision making (Mackintosh et al., 2009)) with lectures, video clips and activities to demonstrate each component of team work.
Pre- and post- training, participants were asked to manage three standardised simulated obstetric emergencies (eclampsia, post-partum haemorrhage (PPH), shoulder dystocia) in a room in the labour ward of their own hospital. Outcomes assessed included the quality of care in relation to communication, safety and respect, in the three simulated emergencies three weeks after training. A five-point Likert scale (1 = strongly disagree to 5 = strongly agree) captured patient-actor responses to statements such as “I felt well informed due to good communication”. The patient-actors were experienced midwives, blinded to the group allocation. All members of the evaluation team were blinded to the participants’ training intervention.
Risk of bias
Both studies had unclear or high risk of bias across several domains (see Table 2). Usual practice was not described in either study. Bashour et al. (2013) failed to report the sequence generation process for hospital randomisation, with uncertainty regarding the selection process of outcome assessors (i.e. women giving birth in the study sites) and characteristics of women (only two of the 2,000 women had a caesarean birth). Due to the nature of the study, blinding of study participants was not possible, with insufficient information regarding blinding of outcome assessors (women). In the study by Crofts et al. (2008), it was not possible to blind clinician participants to the group allocation or blind outcome assessors (patient-actors) to whether participants were being evaluated before or after training.
Table 2.
Risk of bias.
 |
There were no missing outcome data in Bashour et al.'s (2013) trial and a small proportion (5.7%) of missing data in the study by Crofts et al. (2008). Both studies had an unclear risk of bias for selective outcome reporting because study protocols were not publicly available.
Effects of intervention
Impact of interventions for effective communication during labour on women's outcomes
The first question addressed by this review was to report evidence on whether effective communication improved clinical or other outcomes, including satisfaction with care (Box 1). Although neither study reported on the impact of effective communication interventions on clinical outcomes, both studies presented quantitative evidence on ‘satisfaction’ as an outcome.
Bashour et al. (2013) asked postnatal women (two weeks after birth) about their satisfaction with communication by doctors during labour. Crofts et al. (2008) reported patient-actors’ assessments of communication, respect and safety which were recorded immediately after clinical scenarios were completed.
In Bashour et al.'s (2013) trial, women's satisfaction with their birth experience was reported as a primary outcome. The individual level mean satisfaction score was 3.23 (SD 0.72) in the control and 3.42 (0.73) in the intervention group (possible scores ranged from 1 to 5, higher values indicating satisfaction with care), a non-statistically significant difference. Mean for average satisfaction scores also did not differ between the groups (95% CI -0.08 to 0.15) although of note is that mean scores for each group were not provided. Women's views on specific aspects of their doctor's communication with them in labour (for example, did the doctor identify themselves prior to a medical examination; did the doctor greet them; did the doctor look at them when talking to them) were similar across trial groups.
Crofts et al. (2008) evaluated whether patient-actors’ perceptions of care in relation to communication, safety and respect differed after clinical staff completed obstetric emergency training. The authors reported a significant improvement in patient-actors’ perceptions of care after training, regardless of whether they were cared for by a multi-disciplinary team or an individual provider (PPH: Respect, p = 0.007, Safety p<0.001, Communication p = 0.005; Eclampsia: Respect, p = 0.017, Safety p<0.001, Communication p = 0.005; Shoulder dystocia: Respect, p<0.001, Safety p<0.001, Communication p<0.001). Crofts et al. (2008) did not report confidence intervals for these findings.
Women's, partners’ or clinicians’ perceptions or experiences of interventions for effective care in labour
The second review question was designed to identify and synthesise qualitative evidence about the experiences and perceptions of women, family members and maternity care staff in response to interventions to support effective communication during labour and immediately after birth. No qualitative studies were found and neither of the included studies presented qualitative data. Thus no findings for this question are presented.
Characteristics of interventions for effective communication
The third question addressed by this review was to identify characteristics of effective communication interventions for positive birth outcomes, and note any barriers to their implementation. Crofts et al. (2008) provided information on characteristics of the training intervention which we report on below.
Setting of training for effective communication during obstetric emergencies
Crofts et al. (2008) reported evidence on the site of training (local hospital versus simulation centre). During the simulated PPH scenario, safety and communication scores were significantly higher (indicating better perceptions of care) when the patient-actors were cared for by teams trained locally with a patient-actor compared to teams trained at the simulation centre using a computerised patient manikin (safety p = 0.048, communication p = 0.035; confidence intervals were not reported). In the other scenarios, differences in scores did not reach statistical significance.
Clinical training plus teamwork training compared with clinical training only
Crofts et al. (2008) evaluated whether patient-actors’ perceptions of care in relation to communication, safety and respect were influenced by additional training in teamwork (clinical versus clinical and teamwork). The teamwork training comprised a one-day course including lectures, video clips and non-clinical activities which emphasised the importance of effective communication between members of the multi-professional team. There were no significant differences in patient-actors’ perception scores across all scenarios.
Feasibility and acceptability of intervention implementation
The final review question concerned the extent to which an intervention might be considered sustainable, and the resources needed for implementation. No additional quantitative or qualitative studies were found that addressed these aspects. Neither of the included studies presented data on resource requirements needed to undertake the respective training interventions.
However, issues relevant to feasibility, including acceptability to clinicians, were considered. Bashour et al. (2013) included a formal evaluation of the training workshops provided for doctors (n = 137), and although 97% indicated that they would recommend the workshop, 82% reported time pressure, work overload and hospital routine would be barriers to implementation.
Crofts et al. (2008) had relatively low uptake of the training by relevant clinicians. Reasons for this, based on a small number of clinicians’ views (n = 4), included other clinical commitments and illness. Of the 240 staff approached and asked to participate, 158 consented, 18 of whom subsequently withdrew before the first evaluation. Of the remaining 140 participants, 136 attended training and 132 the post-training assessment, with the drop-outs all due to illness.
GRADE assessment: confidence in findings
The quality of evidence for women's satisfaction with their labour and birth was very low when assessed using GRADE criteria, as this result was based on one study (Bashour et al. 2013) which had a number of methodological problems. The quality of the evidence for perceptions of care was also rated as very low, again because the result was based on only one study (Crofts et al. 2008) with several methodological limitations (see Table 3).
Table 3.
A GRADE profile for each quantitative outcome.
|
Quality assessment |
№ of participants |
Effect | Quality/Certainty* | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Outcome | Study design (no. of studies) | Risk of bias | Inconsistency | Indirectness | Imprecision | Other considerations | Intervention | Control | ||
| Training doctors in communication skills (I) compared with no training (C) | ||||||||||
| Birth experience: Satisfaction | Stepped wedge cluster RCT (1) | very serious (-2) † | n/a § | not serious | serious (-1) ¶ | none | 1000 | 1000 | Difference in the average satisfaction scores between the intervention and the control groups = 0.03 (95%CI: – 0.08 to 0.15 | ㊉㊀㊀㊀ |
| VERY LOW | ||||||||||
| Any obstetric emergency training: before intervention compared with after intervention | ||||||||||
| Birth experience: Perception of respect | RCT (1) | serious (-1) ** | n/a § | very serious (-2)‡ | serious (-1)¶ | none | Post-training: | Pre-training: | The mean patient-actor perceptions scores in post-training was 0.5 higher than pre- training for both PPH scenario (p = 0.007) and eclampsia scenario (p = 0.017), and 0.6 higher for shoulder dystocia (p<0.001) | ㊉㊀㊀㊀ |
|
|
VERY LOW | ||||||||
| (95%CI: not reported) | ||||||||||
| Birth experience: Perception of safety | RCT (1) | serious (-1) ** | n/a § | very serious (-2)‡ | serious (-1)¶ | none | Post-training: | Pre-training: | The mean patient-actor perceptions scores in post-training was 0.8 higher than pre-training for both PPH and shoulder dystocia scenarios (p<0.001) and 1.0 higher for eclampsia (p<0.001) | ㊉㊀㊀㊀ |
|
|
VERY LOW | ||||||||
| (95%CI: not reported) | ||||||||||
| Perception of communication | RCT (1) | serious (-1) ** | n/a § | very serious (-2)‡ | serious (-1)¶ | none | Post-training: | Pre-training: | The mean patient-actor perceptions scores in post-training was 0.7 higher than pre-training for both PPH and eclampsia scenarios (p = 0.005), and 0.5 higher for shoulder dystocia (p<0.001) | ㊉㊀㊀㊀ |
|
|
VERY LOW | ||||||||
| (95%CI: not reported) | ||||||||||
| Obstetric emergency training at the local hospital (I) compared with obstetric emergency training at central simulation centre (C) | ||||||||||
| Birth experience: Perception of respect | RCT (1) | n/a § | n/a § | very serious (-2)‡ | serious (-1)¶ | none |
|
|
PPH: P = 0.077 | ㊉㊀㊀㊀ |
| eclampsia: P = 0.14 | VERY LOW | |||||||||
| shoulder dystocia: P = 0.719 | ||||||||||
| (mean difference, 95%CI: not reported) | ||||||||||
| Birth experience: Perception of safety | RCT (1) | Not serious | n/a § | very serious (-2)‡ | serious (-1)¶ | none |
|
|
PPH: P = 0.048 | ㊉㊀㊀㊀ |
| eclampsia: P = 0.214 | VERY LOW | |||||||||
| shoulder dystocia: P = 0.532 | ||||||||||
| (mean difference, 95%CI: not reported) | ||||||||||
| Birth experience: Perception of communication | RCT (1) | Not serious | n/a § | very serious (-2)‡ | serious (-1)¶ | none |
|
|
PPH: P = 0.035 | ㊉㊀㊀㊀ |
| eclampsia: P = 0.071 | VERY LOW | |||||||||
| shoulder dystocia: P = 0.502 | ||||||||||
| (mean difference, 95%CI: not reported) | ||||||||||
| Clinical training plus teamwork training (I) compared with clinical training only (C) | ||||||||||
| Birth experience: Perception of respect | RCT (1) | Not serious | n/a § | very serious (-2)‡ | serious (-1)¶ | none |
|
|
PPH: P = 0.899 | ㊉㊀㊀㊀ |
| eclampsia: P = 0.521 | VERY LOW | |||||||||
| shoulder dystocia: P = 0.82 | ||||||||||
| (mean difference, 95%CI: not reported) | ||||||||||
| Birth experience: Perception of safety | RCT (1) | Not serious | n/a § | very serious (-2)‡ | serious (-1)¶ | none |
|
|
PPH: P = 0.147 | ㊉㊀㊀㊀ |
| eclampsia: P = 0.849 | VERY LOW | |||||||||
| shoulder dystocia: P = 0.68 | ||||||||||
| (mean difference, 95%CI: not reported) | ||||||||||
| Birth experience: Perception of communication | RCT (1) | Not serious | n/a § | very serious (-2)‡ | serious (-1)¶ | none |
|
|
PPH: P = 0.686 | ㊉㊀㊀㊀ |
| eclampsia: P = 0.626 | VERY LOW | |||||||||
| shoulder dystocia: P = 0.345 | ||||||||||
| (mean difference, 95%CI: not reported) | ||||||||||
MMISS: Modified Medical Interview Satisfaction Scale, PPH: postpartum haemorrhage, CI: confidence interval.
Very low: Any estimate of effect is very uncertain.
downgraded by two levels to ‘serious’ because information is from single study (-1) with high risk of bias (-1).
n/a because only one study contributed to this outcome.
downgraded by one level to ‘serious’ – only one study contributed to this outcome.
downgraded by one level to ‘serious’ – although the study design is RCT, for this outcome, the study authors conducted before-after comparison within a group.
downgraded by two levels to ‘very serious’ – measured using patient-actors (an experienced midwife) which may not reflect the real women's perspectives (-1). Also, outcomes were measured using one statement “I felt well informed due to good communication”, which is not a validated measurement and differences in scores before and after the intervention may not reflect clinically significant change accurately (-1).
Population: Healthcare professionals. Setting: Hospitals (UK, Syria) Source: All data are from self-report.
Discussion
The current review only identified two studies of communication interventions specifically aimed at exploring the impact of improving communication between maternity care staff and women during labour and birth, with quality of evidence assessed as very low quality. The evidence gap persists, despite nearly two decades since a review of effectiveness of interventions in maternity care to improve communication between health professionals and women reported a lack of evidence for labour and the postnatal period (Rowe et al., 2002). The absence of evidence in the current review was particularly surprising as the importance of ‘good communication’ has been consistently highlighted in recent studies and successive national and international policy publications.
Evidence of what contributes to ‘effective communication’ remains undefined despite this also being promoted as a core skill for maternity care staff. In Nicholls and Webb's (2006) integrative review which included 33 methodologically diverse studies, the authors reported that good communication skills were considered to be a principal attribute of a good midwife. A later Delphi study from the same researchers which presented women's, midwives’ and midwifery educators’ perceptions of a ‘good midwife’ found ‘communication skills’ was one of the highest scored statements (Nicholls et al., 2011). Communication is persistently cited as a component of high quality maternity care in major policy frameworks to improve women's experiences and other outcomes of maternity care, including WHO Quality of Care Framework for Maternal and Newborn Health (WHO, 2016), Lancet Framework for Quality Maternal and Newborn Care (Renfrew et al., 2014), and respectful maternity care (White Ribbon Alliance, 2012).
Training to improve communication between maternity care staff and women during labour
Both studies included in the review evaluated effectiveness of training interventions to improve communication. Bashour et al. (2013) showed that the training package in communication skills for doctors was not associated with higher satisfaction with labour scores recorded by women, despite high satisfaction with the training workshops reported by the doctors who attended.
Although Crofts et al. (2008) reported that improvements in all scores in the three clinical scenarios were statistically significant after training, this was based on a pre- and post- intervention analysis with no comparison groups. Perceptions of safety and communication significantly improved after training with patient-actors, compared with training using manikins for postpartum haemorrhage scenarios, but it is unclear why no statistically significant improvements were found in perceptions of communication in the eclampsia and shoulder dystocia scenarios using different training methods and settings (patient-actors in local hospitals vs manikins in simulation centres). Furthermore, Crofts et al. (2008) found no benefits of additional teamwork training on patient-actors’ perceptions of care related to safety, communication and respect. Although there seems to be some evidence for simulation training on obstetric emergencies in maternal and neonatal outcomes (Crofts et al. 2011), more robust evaluation is needed to establish not only outcomes of communication and team skills through simulation-based training but content and ‘dose’ of simulation training needed to support effective communication.
Considerations for implementation of communication training
In Bashour et al.'s (2013) trial, possible barriers to implementation of a communication intervention in the clinical environment included long working hours, crowded wards, and high volume of patients. Low social status of women, environment of birth, lack of midwifery support and cultural attitudes were also likely to have impacted on feasibility of implementation. Crofts et al. (2008) had a low take-up of training due to staff illness and clinical commitments. As Bashour et al. (2013) suggest, wider systems change is likely to be needed alongside communication training if outcomes are to improve. How organisations prepare, monitor and sustain interventions to enhance communication, including time to embed and sustain change in practice, require further investigation.
The environment and context of maternity care in the two studies (i.e. centres in Syria and UK) are likely to be different to those in other settings. Bashour et al. (2013) reported that labour and childbirth largely took place in overcrowded hospitals (two participating hospitals had over 10,000 births per year) and in most cases, the women were not allowed to be accompanied by any relatives during labour and birth. Eye-to-eye contact was not acceptable between the woman and her care provider if this was a male. This suggests that there is a need to consider context and culturally specific communication training when developing and implementing interventions. Communication interventions which reflect ‘cultural norms’ as perceived by local women and maternity care staff, could more appropriately inform outcomes of importance for both groups.
Women's, family members’ and maternity care staff's experiences and views of communication interventions
No qualitative evidence was found on women's, family members’ or maternity care staff's experiences or views of interventions to improve communication during labour. Considering the limited research identified, this is perhaps not surprising. How communication is defined, when and how outcomes are assessed and whether assessment is to provide an overall view of maternity care, or to inform a specific component of care (for example, antenatal screening tests) differs between published studies (Rowe et al., 2002, Nieuwenhuijze et al., 2013, O'Brien et al., 2017). A review of literature from developing countries which aimed to identify determinants of women's satisfaction with maternity care showed that therapeutic communication which included components such as listening, politeness, prompt pain relief, kindness, approachability and a smiling demeanour, could enhance maternal satisfaction with care (Srivastava et al., 2015).
A systematic qualitative review of evidence of what women want and need during childbirth highlighted that women expected staff to be sensitive, caring and kind, and fear of staff being distant, insensitive or rude (Downe et al., in preparation). A recently conducted qualitative evidence synthesis aimed to develop a conceptualization of respectful maternity care during childbirth in health facilities globally from the perspectives of key stakeholders (including women, providers, and administrators); this review included 67 studies from 32 countries ranging from high to low income settings (Shakibazadeh et al., 2017). One of the domains of respectful maternity identified was ‘engaging with effective communication’ which was assessed as including interventions such as ‘talking and listening to women’, ‘practicing and encouraging effective non-verbal communication’, ‘being honest’, ‘availability of interpreters due to language proficiency and cultural differences’, and ‘providing empathy’. These were clearly important to women and their maternity carers in a range of settings. However, the extent to which women experienced this level of care and how it could be supported by their care providers remains unknown. Furthermore, there was evidence that negative impacts of maltreatment during labour and birth included increased risk of maternal and infant morbidity and mortality (Mannava et al., 2015), and may dissuade women in some country settings from planning a subsequent birth in a facility setting (Kumbani et al., 2013, Moyer et al., 2014).
National maternity surveys in England of women's experiences of maternity care, including care in labour, have included questions on communication, including ‘At the very start of your labour, did you feel that you were given appropriate advice and support when you contacted a midwife or the hospital?’, ‘Thinking about your care during labour and birth, were you spoken to in a way you could understand?’ (e.g. Care Quality Commission, 2015, Care Quality Commission, 2013). In the USA, national surveys of women's experiences of childbearing have also included questions relevant to communication in labour, including women's views of involvement in decision making (Maternity Center Association, 2002, Declercq et al., 2007). These illustrate how effective communication may be perceived from the perspectives of different stakeholders, including maternity service funders or providers. Communication in maternity care is usually more likely to be assessed as part of a ‘package’ of questions aimed at supporting overall feedback, as illustrated by these national surveys. This is perhaps why this current review which specifically targeted communication interventions between maternity care staff and healthy women at term during labour, birth and the immediate postnatal period found so few relevant studies.
Recent studies have started to explore the extent to which women, partners and families feel able to ‘speak up’ when, for example, women are aware of a deterioration in their health (Carter et al., 2017) or that their safety is at risk as a consequence of staff failing to listen and respond to them (Rance et al., 2013). This area of work could potentially support and inform effective communication in labour to enhance women's experiences and outcomes of birth. Organisational support to achieve and sustain effective communication by maternity care staff is likely to be crucial, with evidence of level, type and characteristics of intervention urgently needed.
Implications for future research
This review identified a lack of studies on interventions to support effective communication between healthy women with a term pregnancy in labour and maternity care staff, despite communication being referred to as a ‘core’ component of high quality, respectful maternity care. This is a major and unexpected research gap that needs to be addressed. The gap suggests an assumption that benefits are self-evident, or taken for granted by stakeholders; potentially research has not been prioritized for this area. We suggest there is an urgent need to improve understanding of key components of effective communication and robust studies to test these. The evidence identified in this review was assessed as very low quality, and the two included studies provided contrasting findings.
The constraints in practice reported in the two studies (Crofts et al., 2008, Bashour et al., 2013) demonstrate the importance of a systems perspective which reflects political, cultural, social and economic factors and impact on the preparation, delivery, impact and sustainability of the intervention. Research is needed from different resource and infrastructure settings to build a body of evidence to inform global policy and practice. As no qualitative studies on women's or providers’ experiences of such interventions were identified, effectiveness studies might usefully incorporate high quality qualitative evidence. In the context of resource limitations in many maternity settings, evidence on resource use, feasibility of implementation for staff and providers, and implementation of different approaches to support effective communication would also be useful. Suggestions for future research are presented in Box 2.
Box 2. Suggestions for future research.
-
•
What are the characteristics of an effective communication in labour, birth and immediate postnatal period as defined from the perspectives of women and their families?
-
•
What outcomes of an effective communication intervention in labour, birth and immediate postnatal period do women and their families consider to be of high priority?
-
•
When and how should clinical and other outcomes be assessed following an intervention to enhance effective communication during labour, birth and immediate postnatal period?
-
•
What additional resources are needed in birth settings to prepare, monitor and sustain implementation of effective communication interventions by maternity care staff to women during labour, birth and the immediate postnatal period?
Strengths and limitations
This review was undertaken using a robust search strategy with the guidance of a University information specialist to identify all relevant evidence to answer the review questions. Included papers were subject to critical review and appraisal to meet planned aims and objectives. No restrictions on languages or countries of origin were placed, although the searches were conducted in English. Although the two included studies were randomised trials, methodological limitations resulted in high risk of bias and very low quality evidence, which prevented conclusive recommendations for practice being made. Due to heterogeneity of included studies, findings could not be statistically pooled which further prevented generalisability of the results. As the current review targeted interventions to promote effective communication between maternity care staff and healthy women at term during labour, birth and the immediate postnatal period, our remit was specific. This meant that research evidence which considered communication in other areas of maternity care, newborn and child health care or health care more generally was not included. A future broader review on maternal and newborn health might usefully provide evidence to inform research and training as a basis for communication interventions and allow integration of evidence from other related areas including breastfeeding.
Conclusion
There is a dearth of evidence on interventions to inform effective communication between maternity care staff and healthy women with term pregnancies during labour, birth and immediate postnatal period. Policy ambitions which recommend effective communication to support high quality, safe maternity care may not be achievable unless robust research is undertaken which reflects women's preferences, birth setting, care providers and the context of care in which labour and birth take place.
Potential barriers to implementation of effective communication interventions would need to be addressed at individual, health facility and system level if outcomes associated with benefit are to be achieved. Some barriers (ie high workload) may be common across all settings, whilst other barriers (e.g. role of women in society) are likely to be specific to particular cultures or settings and would need to be addressed individually. Research is needed to define what an effective communication intervention in labour means to women and their families, what outcomes women and their families consider to be high priority, how outcomes are assessed and timing of assessment in relation to the birth.
Funding
This work was commissioned to King’s College London, UK by the UNDP/UNFPA/UNICEF/WHO/World Bank Special Programme of Research, Development and Research Training in Human Reproduction (HRP), Department of Reproductive Health and Research, World Health Organization, Switzerland as part of the evidence base preparation for the WHO recommendations on intrapartum care. The development of the WHO recommendations on intrapartum care was financially supported by The United States Agency for International Development (USAID). AGP is a staff member of the Department of Maternal, Newborn, Child and Adolescent Health, World Health Organization. She alone is responsible for the views expressed in this article and they do not necessarily represent the decisions, policy or views of the World Health Organization. DB is a staff member of the Department of Women and Children’s Health, School of Life Course Sciences, Faculty of Life Sciences and Medicine, King’s College London, UK and Y-SC is a staff member of Florence Nightingale Faculty of Nursing, Midwifery and Palliative Care, King’s College London, UK. KC is a staff member of Faculty of Health, Social Care and Education, a joint Faculty at Kingston University and St George’s, University of London, UK. MF is a staff member of Kyoto University, Japan. The paper represents the views of the named authors only.
Conflicts of interest
Debra Bick is the Editor-in-Chief of the Midwifery and Marie Furuta is an Associate Editor of Midwifery but neither were involved in the peer review, or editorial decisions, regarding this manuscript. There are no other conflicts of interest.
Acknowledgements
The authors would like to thank the World Health Organization (WHO) which commissioned this review and the WHO intrapartum care steering group, in particular Olufemi T. Oladapo who reviewed the protocol and the manuscript. DB and KC are supported by the National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care South London.
Contributor Information
Yan-Shing Chang, Email: yan-shing.chang@kcl.ac.uk.
Kirstie Coxon, Email: K.Coxon@sgul.kingston.ac.uk.
Anayda Gerarda Portela, Email: portelaa@who.int.
Marie Furuta, Email: furuta.marie.8r@kyoto-u.ac.jp.
Debra Bick, Email: debra.bick@kcl.ac.uk.
References
- Alderdice F., Hamilton K., McNeill J., Lynn F., Curran R., Redshaw M. School of Nursing and Midwifery, Queen's University of Belfast; Belfast: 2016. Birth NI: A Survey of Women's Experience of Maternity Care in Northern Ireland.〈http://www.qub.ac.uk/schools/SchoolofNursingandMidwifery/FileStore/Filetoupload,670193,en.pdf?platform=hootsuite〉 Available from. [Google Scholar]
- Ames H.M.R., Glenton C., Lewin S. Parents' and informal caregivers' views and experiences of communication about routine childhood vaccination: a synthesis of qualitative evidence. Cochrane Database of Systematic Reviews. 2017 doi: 10.1002/14651858.CD011787.pub2. (Art. No.: CD011787) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrews J., Guyatt G., Oxman A.D., Alderson P., Dahm P., Falck-Ytter Y., Nasser M., Meerpohl J., Post P.N., Kunz R., Brozek J., Vist G., Rind D., Akl E.A., Schünemann H.J. GRADE guidelines: 14. Going from evidence to recommendations: the significance and presentation of recommendations. Journal of Clinical Epidemiology. 2013;66:719–725. doi: 10.1016/j.jclinepi.2012.03.013. [DOI] [PubMed] [Google Scholar]
- Ayers S., Bond R., Bertullies S., Wijma K. The aetiology of post-traumatic stress following childbirth: a meta-analysis and theoretical framework. Psychological Medicine. 2016;46:1121–1134. doi: 10.1017/S0033291715002706. [DOI] [PubMed] [Google Scholar]
- Bashour H.N., Kanaan M., Kharouf M.H., Abdulsalam A.A., Tabbaa M.A., Cheikha S.A. The effect of training doctors in communication skills on women's satisfaction with doctor–woman relationship during labour and delivery: a stepped wedge cluster randomised trial in Damascus. BMJ Open. 2013;3:e002674. doi: 10.1136/bmjopen-2013-002674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bohren M.A., Hunter E.C., Munthe-Kaas H.M., Souza J.P., Vogel J.P., Gülmezoglu A.M. Facilitators and barriers to facility-based delivery in low- and middle-income countries: a qualitative evidence synthesis. Reproductive Health. 2014;11:71. doi: 10.1186/1742-4755-11-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bohren M.A., Vogel J.P., Hunter E.C., Lutsiv O., Makh S.K., Souza J.P., Aguiar C., Saraiva Coneglian F., Diniz A.L., Tunçalp Ö., Javadi D., Oladapo O.T., Khosla R., Hindin M.J., Gülmezoglu A.M. The mistreatment of women during childbirth in health facilities globally: a mixed-methods systematic Review. PLoS Medicine. 2015;12:e1001847. doi: 10.1371/journal.pmed.1001847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bosse H.M., Nickel M., Huwendiek S., Jünger J., Schultz J.H., Nikendei C. Peer role-play and standardised patients in communication training: a comparative study on the student perspective on acceptability, realism, and perceived effect. BMC Medical Education. 2010;10:27. doi: 10.1186/1472-6920-10-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler M., Fraser D., Murphy R. What are the essential competencies required of a midwife at the point of registration? Midwifery. 2008;24:260–269. doi: 10.1016/j.midw.2006.10.010. [DOI] [PubMed] [Google Scholar]
- Care Quality Commission. National findings from the 2013 survey of women’s experiences of maternity care, 2013, Care Quality Commission, Newcastle Upon Tyne.
- Care Quality Commission. Survey of women’s experiences of maternity care, 2015, Care Quality Commission, Newcastle Upon Tyne.
- Carter W., Bick D., Mackintosh N., Sandall J.A. Narrative synthesis of factors that affect women speaking up about early warning signs and symptoms of pre-eclampsia and responses of healthcare staff. BMC Pregnancy and Childbirth. 2017;17:63. doi: 10.1186/s12884-017-1245-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crofts J.F., Bartlett C., Ellis D., Donald F., Winter C.J., Hunt L.P., Draycott T.J. Patient-actor perception of care: a comparison of obstetric emergency training using manikins and patient-actors. Quality and Safety in Health Care. 2008;17:20–24. doi: 10.1136/qshc.2006.021873. [DOI] [PubMed] [Google Scholar]
- Crofts J.F., Winter C., Sowter M.C. Practical simulation training for maternity care – where we are and where next. BJOG: An International Journal of Obstetrics&Gynaecology. 2011;118:11–16. doi: 10.1111/j.1471-0528.2011.03175.x. [DOI] [PubMed] [Google Scholar]
- Declercq E.R., Sakala C., Corry M.P., Applebaum S. Listening to mothers II: report of the second national U.S. survey of women's childbearing experiences: conducted January–February 2006 for Childbirth Connection by Harris Interactive® in partnership with Lamaze International. The Journal of Perinatal Education. 2007;16:9–14. doi: 10.1624/105812407X244769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deveugele M., Derese A., De Maess-chalck S., Willems S., Van Driel M., De Maeseneer J. Teaching communication skills to medical students, a challenge in the curriculum? Patient Education and Counselling. 2005;58:265–270. doi: 10.1016/j.pec.2005.06.004. [DOI] [PubMed] [Google Scholar]
- Downe, S., Finlayson, K., Oladapo, O., Bonet, M., Gülmezoglu, A., What matters to women during childbirth: a systematic qualitative review (in preparation). [DOI] [PMC free article] [PubMed]
- Doyle C., Lennox L., Bell D. A systematic review of evidence on the links between patient experience and clinical safety and effectiveness. BMJ Open. 2013;3:e001570. doi: 10.1136/bmjopen-2012-001570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green J.M., Baston H.A. Feeling in control during labor: concepts, correlates, and consequences. Birth. 2003;30:235–247. doi: 10.1046/j.1523-536x.2003.00253.x. [DOI] [PubMed] [Google Scholar]
- Guyatt G.H., Oxman A.D., Kunz R., Yngve F.-Y., Vist G.E., Liberati A., Schünemann H.J., GRADE Working Group Going from evidence to recommendations. British Medical Journal. 2008;336:1049–1051. doi: 10.1136/bmj.39493.646875.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hauck Y., Fenwick J., Downie J., Butt J. The influence of childbirth expectations of Western Australian women's perceptions of their birth experience. Midwifery. 2007;23:235–247. doi: 10.1016/j.midw.2006.02.002. [DOI] [PubMed] [Google Scholar]
- Higgins, J.P.T. and Green, S., Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0, 2011, The Cochrane Collaboration. Available from: 〈www.handbook.cochrane.org〉 (Accessed 18 June 2017).
- Homer C.S., Friberg I.K., Dias M.A., ten Hoope-Bender P., Sandall J., Speciale A.M., Bartlett L. The projected effect of scaling up midwifery. The Lancet. 2014;384 doi: 10.1016/S0140-6736(14)60790-X. (1164-1157) [DOI] [PubMed] [Google Scholar]
- King A., Hoppe R.B. “Best Practice” for patient-centered communication: a narrative review. Journal of Graduate Medical Education. 2013;5:385–393. doi: 10.4300/JGME-D-13-00072.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumbani L., Bjune G., Chirwa E., Malata A., Odland J. Why some women fail to give birth at health facilities: a qualitative study of women's perceptions of perinatal care from rural Southern Malawi. Reproductive Health. 2013;10:9. doi: 10.1186/1742-4755-10-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackintosh N.J., Berridge E.-J., Freeth D.S. Supporting structures for team situation awareness and decision making: insights from four delivery suites. Journal of Evaluation in Clinical Practice. 2009;15:46–54. doi: 10.1111/j.1365-2753.2008.00953.x. [DOI] [PubMed] [Google Scholar]
- Mannava P., Durrant K., Fisher J., Chersich M., Luchters S. Attitudes and behaviours of maternal health care providers in interactions with clients: a systematic review. Globalization and Health. 2015;11:36. doi: 10.1186/s12992-015-0117-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maternity Center Association . Maternity Center Association,; New York: 2002. Listening to Mothers: Report of the First National U.S. Survey of Women's Childbearing Experiences Executive Summary and Recommendations Issued by the Maternity Center Association. [Google Scholar]
- Meakin R., Weinman J. The Medical Interview Satisfaction Scale (MISS-21) adapted for British general practice. Family Practice. 2002;19:257–263. doi: 10.1093/fampra/19.3.257. [DOI] [PubMed] [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., Altman D.G., The PRISMA Group Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA Statement. PLoS Medicine. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moyer C.A., Adongo P.B., Aborigo R.A., Hodgson A., Engmann C.M. ‘They treat you like you are not a human being’: maltreatment during labour and delivery in rural northern Ghana. Midwifery. 2014;30:262–268. doi: 10.1016/j.midw.2013.05.006. [DOI] [PubMed] [Google Scholar]
- National Insitute for Health and Care Excellence (NICE), Intrapartum Care for Healthy Women and Babies. CG 190, 2017, NICE, London.
- National Maternity Review, Better Births: Improving Outcomes of Maternity Services in England. A five Year Forward View for Maternity Care, 2016, Available from 〈https://www.england.nhs.uk/wp-content/uploads/2016/02/national-maternity-review-report.pdf〉 (Accessed 18th August 2017) .
- Nicholls L., Webb C. What makes a good midwife? An integrative review of methodologically-diverse research. Journal of Advanced Nursing. 2006;56:414–429. doi: 10.1111/j.1365-2648.2006.04026.x. [DOI] [PubMed] [Google Scholar]
- Nicholls L., Skirton H., Webb C. Establishing perceptions of a good midwife: a Delphi study. British Journal of Midwifery. 2011;19:230–236. [Google Scholar]
- Nieuwenhuijze M.J. dA., Korstjent I., Bude L., Lagro-Janssen T.L.M. Influence on birthing positions affects women's sense of control in second stage of labour. Midwifery. 2013;29:e107–e114. doi: 10.1016/j.midw.2012.12.007. [DOI] [PubMed] [Google Scholar]
- Nursing and Midwifery Council . NMC; London: 2015. The Code. Professional Standards of Practice and Behaviour for Nurses and Midwives. [Google Scholar]
- O'Brien D., Butler M.M., Casey M. A participatory action research study exploring women's understandings of the concept of informed choice during pregnancy and childbirth in Ireland. Midwifery. 2017;46:1–7. doi: 10.1016/j.midw.2017.01.002. [DOI] [PubMed] [Google Scholar]
- Rance S., McCourt C., Rayment J., Mackintosh N., Carter W., Watson K., Sandall J. Women's safety alerts in maternity care: is speaking up enough? BMJ Quality and Safety. 2013;22:348–355. doi: 10.1136/bmjqs-2012-001295. [DOI] [PubMed] [Google Scholar]
- Renfrew M.J., McFadden A., Bastos M.H., Campbell J., Channon A.A., Cheung N.F., Silva D.R.A.D., Downe S., Kennedy H.P., Malata A., McCormick F., Wick L., Declercq E. Midwifery and quality care: findings from a new evidence-informed framework for maternal and newborn care. Lancet. 2014;384:1129–1145. doi: 10.1016/S0140-6736(14)60789-3. [DOI] [PubMed] [Google Scholar]
- Rowe R.E., Garcia J., Macfarlane A.J., Davidson L.L. Improving communication between health professionals and women in maternity care: a structured review. Health Expectations. 2002;5:63–83. doi: 10.1046/j.1369-6513.2002.00159.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shakibazadeh E., Namadian M., Bohren M.A., Vogel J.P., Rashidian A., Pileggi V.N., Madeira S., Leathersich S., Tunçalp O¨., Oladapo O.T., Souza J.P., Gülmezoglu A.M. Respectful care during childbirth in health facilities globally: a qualitative evidence synthesis. BJOG: An International Journal of Obstetrics&Gynaecology. 2017 doi: 10.1111/1471-0528.15015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sholkamy H., Khalil K., Cherine M., Elnoury A., Breebaart M., Khalil K. The Population Council, Cairo; Cairo: 2003. An Observation Checklist for Facility-Based Normal Labour and Delivery Practices: The Galaa Study. Monographs in Reproductive Health 5. [Google Scholar]
- Srivastava A., Bilal I., Avan B.I., Rajbangshi P., Bhattacharyya S. Determinants of women's satisfaction with maternal health care: a review of literature from developing countries. BMC Pregnancy and Child birth. 2015;15:97. doi: 10.1186/s12884-015-0525-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tuncalp O¨., Were W.M., MacLennan C., Oladapo O.T., Gulmezoglu A.M., Bahl R., Daelmans B., Mathai M., Say L., Kristensen F., Temmerman M., Bustreo F. Quality of care for pregnant women and newborns-the WHO vision. BJOG: An International Journal of Obstetrics&Gynaecology. 2015;122:1045–1049. doi: 10.1111/1471-0528.13451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vogel J., Bohren M., Tunçalp O¨., Oladapo O., Gülmezoglu A. Promoting respect and preventing mistreatment during childbirth. BJOG: An International Journal of Obstetrics&Gynaecology. 2016;123:671–674. doi: 10.1111/1471-0528.13750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White Ribbon Alliance, Respectful maternity care: The Universal Rights of Childbearing Women., 2012, Washington, DC, White Ribbon Alliance.
- World Health Organization (WHO) World Health Organization; Geneva: 2016. Standards for Improving Quality of Maternal and Newborn Care in Healthcare Facilities. [Google Scholar]
- World Health Organization (WHO),2018 WHO Recommendations on Intrapartum Care for A Positive Childbirth Experience, World Health Organization, Geneva (in press). [PubMed]