Abstract
Human embryonic stem (ES) cells are undifferentiated, pluripotent cells that can be maintained indefinitely in culture. Here we demonstrate that human ES cells differentiate to hematopoietic precursor cells when cocultured with the murine bone marrow cell line S17 or the yolk sac endothelial cell line C166. This hematopoietic differentiation requires fetal bovine serum, but no other exogenous cytokines. ES cell-derived hematopoietic precursor cells express the cell surface antigen CD34 and the hematopoietic transcription factors TAL-1, LMO-2, and GATA-2. When cultured on semisolid media with hematopoietic growth factors, these hematopoietic precursor cells form characteristic myeloid, erythroid, and megakaryocyte colonies. Selection for CD34+ cells derived from human ES cells enriches for hematopoietic colony-forming cells, similar to CD34 selection of primary hematopoietic tissue (bone marrow, umbilical cord blood). More terminally differentiated hematopoietic cells derived from human ES cells under these conditions also express normal surface antigens: glycophorin A on erythroid cells, CD15 on myeloid cells, and CD41 on megakaryocytes. The in vitro differentiation of human ES cells provides an opportunity to better understand human hematopoiesis and could lead to a novel source of cells for transfusion and transplantation therapies.
Embryonic stem (ES) cells are pluripotent cells derived from preimplantation embryos. ES cells have the ability to be maintained in culture indefinitely as undifferentiated cells, yet they are capable of forming more differentiated cell types. Because of these properties, mouse ES cells have been instrumental in gaining a better understanding of mammalian development. In studies of hematopoiesis, investigators have used mouse ES cells to derive various hematopoietic lineages in vitro either by formation of “embryoid bodies” (1, 2), coculture with stromal cell lines (3, 4), or culture on collagen-coated plates (5). These studies have used gene expression, cell phenotype, and functional studies to define sequential stages of hematopoietic cell development.
In contrast to work on mouse hematopoietic development, studies of human hematopoiesis have been confined to the use of primary hematopoietic tissue such as bone marrow, peripheral blood, or umbilical cord blood as the starting cell population. The reliance on these heterogeneous tissue samples that are difficult to sustainably expand in vitro has hindered progress in understanding human hematopoiesis. Work on human hematopoiesis typically uses cell surface antigens (such as CD34) to identify putative hematopoietic stem cell (HSC) population(s) within the mixed cell population, and cell sorting methods are used to enrich for the cells of interest (6, 7). Recently, fluorescent dyes that can bind DNA (such as Hoechst 33342) have proven useful in the differential isolation of putative HSCs (8). Although these methods have provided a great deal of information about HSC biology and have facilitated clinical hematopoietic cell transplantation, several important questions remain. For example, recent studies have shown that some CD34− cells also can display HSC properties, including long-term growth, differentiation, and self-renewal when injected into immunodeficient mice (8–11). Moreover, some cells derived from nonhematopoietic tissue appear to have HSC potential (12, 13). The interrelationship between these varying sources and phenotypes of HSCs remains unclear.
Human ES cells (14, 15) provide a unique, homogeneous, unlimited starting population of cells for studying human hematopoiesis. Human ES cells can be cultured for at least 300 population doubling times without observed senescence, while continuing to maintain normal karyotypes, telomere lengths, and pluripotency. Moreover, these cells can be cloned from a single cell without loss of pluripotency (16). Human ES cells give rise to differentiated cells and tissues from all three embryonic germ layers when allowed to form teratomas in immunodeficient mice or when induced to form embryoid bodies in vitro (14, 17). Mouse and human ES cells differ in morphology, population doubling time, and growth factor requirements. Undifferentiated mouse ES cells, for example, can be maintained as undifferentiated “feeder-independent” cells if growth factors such as leukemia inhibitory factor (LIF) or related cytokines are added to the media (1). If human ES cells are grown without feeder cells, but in the presence of LIF, they either differentiate or die (14, 15). Given the unexpected differences in the control of the undifferentiated proliferation of mouse and human ES cells, similar significant differences could exist in the specific factors that direct their differentiation.
Here, we show that coculture of human ES cells with certain stromal cell lines derived from mouse hematopoietic tissue (yolk sac and bone marrow) leads to differentiation into hematopoietic cells. These cells express both cell surface antigens and transcription factors characteristic of cells in primary human hematopoietic tissue. Moreover, hematopoietic cells are present in these differentiating cocultures that can generate myeloid, erythroid, and megakaryocyte colonies in vitro, and the colonies obtained appear identical to those produced from human adult bone marrow cells.
Methods
Culture of ES Cells.
The human ES cell lines H1, H1.1, and H9.2 were derived and maintained as described (14, 16), except that the undifferentiated ES cells were grown in serum-free conditions. Human ES cells were maintained as undifferentiated cells by coculture with irradiated (25 Gy) mouse embryonic fibroblast (MEF) cells in media consisting of DMEM/F12 (GIBCO/BRL) supplemented with 15% KnockOut SR serum replacer (GIBCO/BRL), 2 mM l-glutamine, 0.1 mM β-mercaptoethanol, 1% nonessential amino acids (all from GIBCO/BRL), and 4 ng/ml basic fibroblast growth factor (R & D Systems). ES cells grown under these conditions will begin to show evidence of differentiation after ≈10 days; therefore, ES cells were passaged approximately weekly to maintain undifferentiated growth. To promote hematopoietic differentiation, the human ES cells were cocultured with either the mouse bone marrow stromal cell line S17 (18) (gift of Kenneth Dorshkind, University of California, Los Angeles) or the mouse yolk-sac endothelial cell line C166 (19). S17 and C166 cells were irradiated (30 Gy). Media to support differentiation consisted of DMEM (GIBCO/BRL) supplemented with 20% FBS (from either HyClone or Gencyte, Buffalo, NY), 2 mM l-glutamine, 0.1 mM β-mercaptoethanol, and 1% nonessential amino acids. During differentiation, media were changed every 2–3 days.
Flow Cytometry Analysis.
Undifferentiated H1 cells were washed with Ca2+ and Mg2+-free PBS and dissociated with 0.05% trypsin/0.53 mM EDTA (GIBCO/BRL) for 5–10 min before washing and staining with FACS media consisting of PBS supplemented with 2% FBS and 0.1% sodium azide. To analyze cell surface antigen expression on H1 cells allowed to differentiate as above (H1/S17 and H1/C166 cells), the differentiated cell mixture was dissociated with 1 mg/ml collagenase IV (GIBCO/BRL) and 0.05% trypsin/0.53 mM EDTA supplemented with 2% chick serum (GIBCO/BRL). Dissociated cells were filtered through 85-μm nitex mesh to remove remaining clumps. The single cell suspension was aliquoted and stained with either isotype control or antigen-specific antibodies. Unconjugated isotype control antibodies IgG3 and IgM (Sigma) and directly conjugated isotype control antibodies IgG1-FITC and IgG1-phycoerythrin (PE) (PharMingen) were used. Unconjugated antigen-specific antibodies against SSEA-1 (IgM) and SSEA-4 (IgG3) (Developmental Studies Hybridoma Bank, Iowa City) were detected with a FITC-labeled goat anti-mouse IgG and IgM antibody (Caltag, Burlingame, CA). Other conjugated antibodies were used: CD34-FITC, CD45-PE, CD31-PE, CD38-PE, CD90-FITC, CD117-PE, CD15-FITC, class I-FITC (all IgG1, all from PharMingen), CD133/1-PE (IgG1) (Miltenyi Biotec, Auburn, CA), and glycophorin A-PE (IgG1) (Immunotech, Miami, FL). Cells were analyzed live (without fixation) by using propidium iodide to exclude dead cells on a FACScan (Becton Dickinson) with either pc-lysis or cellquest software.
Magnetic Column (MACS) Separation.
Selection of CD34+ cells was done by labeling the H1/S17 cells with the anti-CD34 antibody QBEND/10 followed by a magnetically labeled secondary antibody (Miltenyi Biotec). The magnetically labeled cells were separated into CD34+ and CD34− populations with a mini-MACS column (Miltenyi Biotec). CD34 enrichment was confirmed by flow cytometry analysis using a different anti-CD34 antibody (PharMingen).
Hematopoietic Colony Assays.
H1/S17 cells, H1/C166 cells, or H1/MEF cells were cultured for the indicated number of days before harvesting and making a single cell suspension as above. Hematopoietic colonies were demonstrated by growing these cells in Methocult GF+ media (StemCell Technologies, Vancouver) consisting of 1% methylcellulose, 30% FBS, 1% BSA, 50 ng/ml stem cell factor, 20 ng/ml granulocyte–macrophage colony-stimulating factor, 20 ng/ml IL-3, 20 ng/ml IL-6, 20 ng/ml granulocyte colony-stimulating factor, and 3 units/ml erythropoietin. Cells were aliquoted in duplicate samples at 1–2 × 105 cell per plate. After 14 days the plates were scored for colony-forming units (CFUs) according to standard criteria (20, 21). To demonstrate CFU-megakaryocyte (CFU-Mk) colonies, the H1/S17 cells were cultured on chamber slides in MegaCult-C media (StemCell Technologies) consisting of 1.1% collagen, 1% BSA, 10 μg/ml bovine pancreatic insulin, 200 μg/ml human transferrin, 2 mM l-glutamine, 0.1 M β-mercaptoethanol, 50 ng/ml thrombopoietin, 10 ng/ml IL-6, and 10 ng/ml IL-3. The Megacult-C media were supplemented with 40 μg/ml low density lipoproteins (Sigma) as recommended by the manufacturer. After 10–14 days, the cells were fixed, dried, and stained with an anti-CD41 (GPIIb)-specific antibody or isotype control antibody, followed by an alkaline phosphatase-conjugated secondary antibody and visualization with Fast Red/Naphthol staining according to the manufacturer's instructions. CFU-Mk cells were identified by red staining.
Cellular morphology and enzyme expression were examined by plucking individual colonies with a pulled Pasteur pipette and spinning onto glass slides by using a Cytospin 2 (Shandon, Pittsburgh). Cells either were stained with Diff-Quik (a modified Wright-Giemsa stain, Dade Behring, Miami) or stained for esterase-containing cells with Naphthol AS-D Chloroacetate esterase and α-Naphthyl acetate esterase (Sigma).
Reverse Transcriptase–PCR (RT-PCR) Analysis.
Cells used for initial RT-PCR studies were: H1 cells allowed to differentiate on S17 cells (H1/S17), H1 cells allowed to differentiate on MEFs (H1/MEF day 17), H1 cells on MEFs for 6 days and harvested before differentiation was seen (H1/MEF day 6), irradiated S17 cells alone, irradiated MEF cells alone, and the erythroleukemia cell line K562 (American Type Culture Collection). Adherent cells were harvested with 1 mg/ml collagenase IV, washed with PBS, and pelleted. Total RNA was extracted by using a RNeasy mini kit (Qiagen, Valencia, CA) with homogenization with a Qiashredder (Qiagen) according to the manufacturer's instructions. Total RNA was quantified by UV spectrophotometer and 1 μg was used for each RT reaction. For time-course experiments, 0.5 μg RNA was used for each RT sample. RT reactions were done by using Omniscript RT (Qiagen) according to the manufacturer's instructions. Duplicate samples with and without addition of RT enzyme were done for all studies to control for contaminating genomic DNA. RT reactions were primed by using oligo(dT) primers (Promega), and 20 units RNase inhibitor was added to each reaction (Promega). PCRs were done with HotStarTaq (Qiagen) using 2 μl of RT product per reaction according to the manufacturer's instructions. PCR conditions consisted of: 15 min at 95°C (hot start), 25–40 cycles (actual number noted below) of: 94°C for 1 min, annealing temperature (Ta, noted below) for 1 min, 72°C for 1 min. A final 10-min extension at 72°C was done at the end. Oligonucleotide-specific conditions were: TAL-1, 40 cycles, Ta 53°C; GATA-2: 31 cycles, Ta 53°C; Flk-1, 35 cycles, Ta 53°C; LMO-2, 40 cycles, Ta 53°C; and β-actin, 25 cycles, Ta 58°C. Products were analyzed on 1.5% agarose gel and visualized with ethidium bromide staining. DNA sequencing was done to confirm bands corresponded with the appropriate human genes. Oligonucleotide primers were: TAL-1 (331 bp), forward, 5′-ATGGTGCAGCTGAGTCCTCC-3′, reverse, 5′-TCTCATTCTTGCTGAGCTTC-3′; GATA-2 (242 bp), forward, 5′- AGCCGGCACCTGTTGTGCAA-3′, reverse, 5′-TGACTTCTCCTGCATGCACT-3′; Flk-1 (537 bp), forward, 5′-ATGCACGGCATCTGGGAATC-3′, reverse, 5′-GCTACTGTCCTGCAAGTTGCTGTC-3′; LMO-2 (289 bp), forward, 5′-GGATCCTGCCGGAGAGACTATCTC-3′, reverse, 5′-GAATTCAGTGAACACCTCCGCAAA-3′; and β-actin, (838 bp), forward, 5′-ATCTGGCACCACACCTTCTACAATGAGCTGCG-3′, reverse, 5′-CGTCATACTCCTGCTTGCTGATCCACATCTGC-3′.
Results
Hematopoietic Differentiation of Human ES Cells.
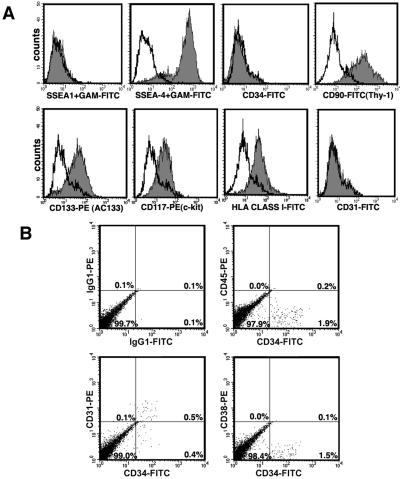
The majority of these experiments were done by using the human ES cell line H1 (14). These cells were maintained in the undifferentiated state by coculture on irradiated MEF “feeder cells” in serum-free media. Flow cytometric analysis of undifferentiated H1 cells demonstrates they are SSEA-1−, SSEA-4+, as previously demonstrated by immunohistochemical staining (14) (Fig. 1A). Here, we further characterized these human undifferentiated ES cells as expressing CD90 (thy-1), CD133 (AC133), and CD117 (c-kit). However, H1 cells fail to express CD34, CD31, CD45, and CD38 (Fig. 1A and data not shown). Interestingly, CD90, CD133, and CD117 (c-kit) are well recognized to be present on HSCs, and recently CD133 was identified on purified human neural stem cells (7, 22, 23).
Figure 1.
Flow cytometric analysis of undifferentiated human ES (H1) cells and differentiated H1 cells. (A) Undifferentiated H1 cells analyzed by single-color flow cytometry. Appropriate isotype control antibody is demonstrated by line and indicated antibody by filled plot. SSEA-1 and SSEA-4 were unconjugated antibodies and a secondary FITC-conjugated goat anti-mouse (GAM) antibody was used. All other antibodies were directly conjugated to flurochrome. (B) H1 cells allowed to differentiate on S17 cells (H1/S17 cells) analyzed by two-color flow cytometry. Percentages of positive cells are indicated in each quadrant.
To promote hematopoiesis, the undifferentiated H1 cells were cocultured with irradiated S17 cells (originally derived from mouse bone marrow; ref. 18), or with C166 cells (originally derived from embryonic day 12 mouse yolk sac; ref. 19). The media contained 20% FBS, but no other exogenously added cytokines or growth factors. Both the S17 and C166 cell lines have been shown to support the growth of bone marrow-derived hematopoietic progenitor cells (24, 25). After 3–5 days in culture under these conditions, the H1 cells differentiated into a variety of cell types. Within these areas of differentiation were regions of cobblestone-type cells and other areas of small, round loosely adherent cells. The appearance of these cells is reminiscent of early hematopoietic cells derived from other sources (7).
Initially, to characterize potential hematopoietic cells, the H1 cells allowed to differentiate on either S17 cells (H1/S17 cells) or C166 cells (H1/C166 cells) for 17 days were analyzed by flow cytometry (Fig. 1B). Approximately 1–2% of the differentiated H1 cells were shown to be CD34+CD38−, consistent with the phenotype of early hematopoietic cells (7, 26). Interestingly, roughly 50% of the CD34+ cells also expressed CD31 on the cell surface. Other studies have shown that CD34 and CD31 can be coexpressed on both HSCs and endothelial cells, and both cell types are thought to be derived from the same hemangioblast precursor cells (27–29). Therefore, it is possible that endothelial cells or endothelial precursors are also present within these cultures of differentiated H1 cells. These CD34+CD38− cells also were found to be CD45− (Fig. 1B). Although CD45 is commonly expressed on mature hematopoietic cells, expression of CD45 on HSCs and hematopoietic colony-forming cells (CFCs) is unclear. Studies of both human and murine hematopoiesis have identified CD45− hematopoietic precursors. This includes work on differentiated mouse ES cells and day 9.5 mouse embryonic yolk sac that demonstrate hematopoietic CFCs from CD45− cell populations (5).
Hematopoietic Colony Assays.
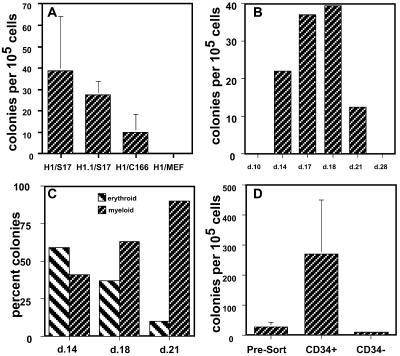
Cells that form hematopoietic colonies (so-called CFUs or CFCs) represent a stage of hematopoietic differentiation between HSCs and more terminally differentiated cells (such as erythrocytes, granulocytes, monocytes, or platelets). These CFCs are identified by culturing them in a semisolid media (typically methylcellulose or agar) supplemented with cytokines that promote the localized expansion and differentiation of hematopoietic cells in discrete colonies. In methylcellulose assays, on average, H1/S17 cells gave rise to 30.4 colonies per 105 input cells, and H1/C166 gave rise to 4.3 colonies per 105 input cells (Fig. 2A). H1/S17 cells produced CFCs after 14 days of coculture (but not at earlier times), produced a maximal number of CFCs at 17–18 days, and produced no CFCs at 28 days (Fig. 2B). This finding demonstrates the transient nature of hematopoietic differentiation within this system and suggests that long-term self-renewal of HSCs is not supported by this stromal coculture method. The clonally derived human ES cell lines H1.1 and H9.2 gave similar results when allowed to differentiate on S17 cells (Fig. 2A and data not shown). Importantly, none of the following conditions lead to generation of CFCs: undifferentiated H1 cells (harvested after 6 days on MEFs without evidence of differentiation), H1 cells allowed to differentiate on MEF cells for 17 days (H1/MEF), H1 cells allowed to differentiate on S17 cells in serum-free media, and S17 cells or C166 stromal cells alone (Fig. 2A and data not shown). H1/S17 cells and H1/C166 cells gave rise to both erythroid and myeloid (nonerythroid) colonies (Fig. 2C). Interestingly, after 14 days of differentiation H1/S17 cells produced mostly erythroid CFCs, whereas after 21 days of differentiation H1/S17 cells produced mostly myeloid CFCs (Fig. 2C).
Figure 2.
Methylcellulose hematopoietic colony-forming assays. (A) Production of CFCs from human ES cells. H1/S17 cells, H1.1/S17, H1/C166 cells, and differentiated H1/MEF cells were harvested after 14–20 days of culture, placed in methylcellulose-based media supplemented with hematopoietic growth factors, and scored for total hematopoietic colonies after 14 days. Results are mean ± SE of seven trials with H1/S17, four trials with H1.1/S17, four trials with H1/C166, and three trials with H1/MEF. Data are presented as colonies per 105 cells harvested from the differentiated H1 cultures. (B) Time course of H1/S17 cell differentiation into hematopoietic CFCs. H1 cells cocultured with S17 cells for the indicated number of days before colony assay. (C) Percent of erythroid (burst-forming unit-erythroid) and myeloid (CFU-GM, CFU-M, and CFU-G) colonies derived from H1/S17 cells harvested at day indicated. (D) CD34+ H1/S17 cells are enriched for CFCs. Unsorted H1/S17 cells and H1/S17 cells sorted for CD34+ cells and CD34− cells by magnetic column were placed in hematopoietic colony assay. These results are mean ± SE of three separate trials.
Because CD34 is the best identified surface antigen expressed on hematopoietic precursor cells, the H1/S17 cells were enriched for CD34+ cells by magnetic selection. Here, the CD34-enriched cells gave rise to on average 270 colonies per 105 H1/S17 cells and the CD34-depleted cells gave rise to only 10 colonies per 105 H1/S17 cells (Fig. 2D). Therefore CD34 selection markedly enriched CFCs compared with the unselected H1/S17 cells, whereas the CD34-depleted cell population was reduced in CFCs. Because the CD34-depleted cells still contained ≈0.5% CD34+ cells (postdepletion), the CFCs from the CD34-depleted cells may have come from either CD34− cells or contaminating CD34+ cells.
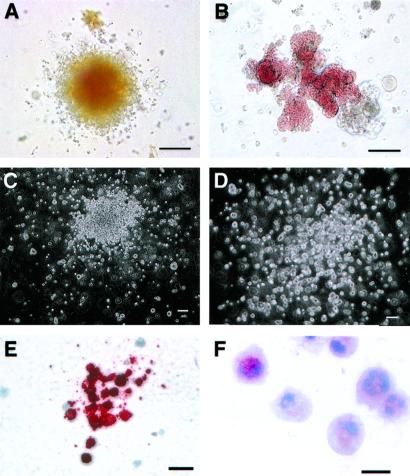
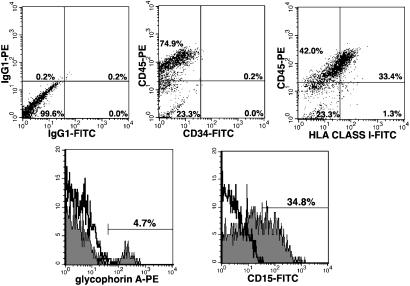
The colonies formed in methylcellulose had the same highly characteristic morphologies of colonies derived from human bone marrow cells placed in similar culture conditions (Fig. 3 A–E)(20, 21). The phenotypes of the CFCs included CFU-macrophage (CFU-M), CFU-granulocyte, mixed CFU-macrophage/granulocyte (CFU-GM), burst-forming unit-erythroid, and CFU-erythroid. Occasional experiments also demonstrated mixed CFU-granulocyte, erythroid, macrophage, megakaryocyte (CFU-GEMM), an early multipotent progenitor cell. CFU-Mks were demonstrated by culture of the H1/S17 cells in a collagen based-media designed to support CFU-Mk growth. The CFU-Mk were specifically identified by immunostaining with an antibody against CD41 (GPIIb of the GPIIb/IIIa complex), specific for megakaryocytes and platelets (Fig. 3E). Staining of the CFU-M- and CFU-GM-derived colonies with nonspecific esterase demonstrated granules typical of these lineages (Fig. 3F). Mature neutrophils also could be identified within the CFU-GM-derived cells by their typical nuclear morphology (Fig. 3F). Flow cytometric analysis of cells within these colonies demonstrates expression of surface antigens typical of normal human blood cells. These cells are CD45+, HLA class I+, and CD34−. The erythroid cells express glycophorin A, and the myeloid cells express CD15 (Fig. 4).
Figure 3.
Photographs of hematopoietic colonies and cells derived from H1/S17 cells. H1 cells allowed to differentiate on S17 cells for ≈17 days, harvested, and allowed to form colonies in semisolid media for 14 days before scoring colony phenotypes. (A) CFU-granulocyte, erythroid, macrophage, megakaryocyte (CFU-GEMM). Colony of mixed erythroid and myeloid cells. (B) Burst-forming unit-erythroid. Large unstained, red (hemoglobin) colony. (C) CFU-GM, unstained myeloid colony. (D) CFU-M, unstained myeloid colony, less dense than CFU-GM colony. (E) CFU-Mk. Colony of cells stained with platelet/megakaryocyte-specific antibody against CD41 (GPIIb/IIIa) with alkaline phosphatase-conjugated secondary antibody and Fast Red/naphthol reagent to provide red stain. (F) Cytospin of CFU-GM cells demonstrating granulocytes with esterase-positive red granules. (Scale bars: A–D, 100 μm; E, 40 μm; F, 20 μM.)
Figure 4.
Flow cytometric analysis of hematopoietic cells derived from methylcellulose colony assay of H1/S17 cells. Cells were washed free of methylcellulose before incubation with indicated antibodies and analyzed by two-color (Upper) or one-color (Lower) flow cytometry. (Upper) Isotype controls are shown (Left), and percent positive cells in each quadrant is indicated. (Lower) Isotype control is demonstrated by line, and indicated antibody is demonstrated by filled plot. Percent positive cells are shown by labeled marker.
Hematopoietic Gene Expression.
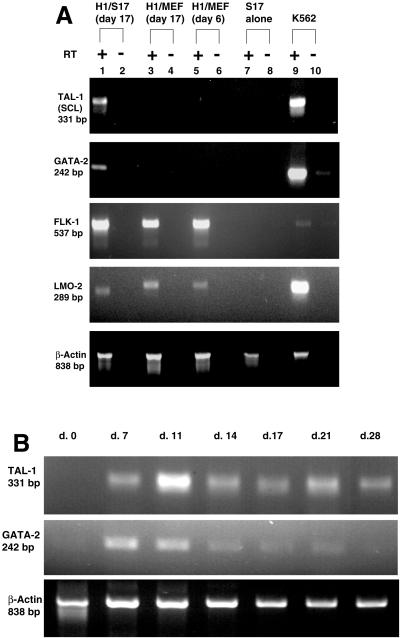
To further characterize the H1 cells differentiated to hematopoietic cells by coculture with S17 cells (H1/S17 cells), we examined genes known to be expressed at an early stage of hematopoietic differentiation by using RT-PCR. H1/S17 cells expressed mRNA for TAL-1 and GATA-2, confirming the presence of early hematopoietic cells uniquely within this population (Fig. 5A). The vascular endothelial growth factor receptor Flk-1 and the transcription factor LMO-2 were expressed in undifferentiated H1 cells, H1/S17 cells, and H1/MEF cells. This finding suggests that Flk-1 and LMO-2 may have important roles in cells other than hematopoietic cells, including undifferentiated ES cells. The S17 and MEF feeder cells alone do not express any of these genes (Fig. 5 and data not shown). Time-course analysis found expression of TAL-1 and GATA-2 as early as day 7, before the appearance of CFCs. However, expression of GATA-2 was not detectable after day 21, corresponding to loss of CFC generation (Fig. 5B).
Figure 5.
Hematopoietic gene expression by RT-PCR of H1/S17 cells. (A) H1 cells were allowed to differentiate on either S17 cells for 17 days (lanes 1 and 2) or to differentiate on MEF cells for 17 days (lanes 3 and 4), or harvested after culture on MEFs for 6 days, before evidence of differentiation (undifferentiated H1 cells, lanes 5 and 6) and subjected to RT-PCR analysis. Irradiated S17 cells were examined to demonstrate positive bands in the H1/S17 samples were not from these feeder cells (lanes 7 and 8). The erythroleukemia cell line K562 was used as a positive control (lanes 9 and 10). Oligonucleotide primers specific for genes of interest are shown. Each sample was done with RT added (+, lanes 1, 3, 5, 7, and 9) and without RT added (−, lanes 2, 4, 6, 8, and 10) to demonstrate positive bands are not caused by genomic DNA. (B) Time course of hematopoietic gene expression. H1 cells were allowed to differentiate on S17 cells for the number of days indicated prior isolation of RNA for RT-PCR analysis. Day 0 (d. 0) indicates undifferentiated H1 cells. Controls of PCR done on samples without RT added did not have any positive bands (data not shown).
Because the ES cell-derived erythroid colonies could potentially express globin genes from any stage of development (embryonic, fetal, or adult), we used RT-PCR to evaluate this gene expression. RNA was prepared from erythroid colonies harvested from methylcellulose culture of differentiated H1/S17 cells and compared with erythroid colonies formed by normal adult bone marrow. As expected, the adult bone marrow-derived colonies expressed ample α and β RNA, as well as some γ and δ RNA. In contrast, the H1/S17-derived colonies also expressed α, β, and δ globin, but did not express fetal γ globin. No embryonic (ɛ or ζ) globin gene expression was detected (data not shown). These results show that the ES cell-derived erythoid cells can express mature, adult-type hemoglobin.
Discussion
We have demonstrated in vitro differentiation of human ES cells to multiple hematopoietic lineages. Although in vitro colony assays are commonly used to study human hematopoiesis (30, 31), one concern about using colony assays to identify ES cell-derived hematopoietic cells is that the colonies could consist of nonhematopoietic cells that are able to grow in clusters that merely resemble hematopoietic colonies. However, we have used several complementary methods to demonstrate that these colonies consist of hematopoietic cells. The hemoglobin (red) of the burst-forming unit-erythroid colonies provide a distinct marker of terminally differentiating erythroid cells. Moreover, these cells are glycophorin A+ and express normal adult globin genes as detected by RT-PCR. The esterase-positive granules in the CFU-GM-derived colonies are characteristic of granulocytes and macrophages. Additionally, the cells within the myeloid-derived (CFU-GM and CFU-M) colonies are CD45+ and CD15+. The CFU-Mk-derived cells (megakaryocytes) are CD41+. Sorting the H1/S17 cells into CD34+ and CD34− populations demonstrates enrichment of CFCs within the CD34+ population, as expected for hematopoietic precursors. Although the frequency of CFCs is relatively low under the conditions of differentiation described, the yield using CD34-enriched populations is close to the number of CFCs derived from human bone marrow samples (≈100–1,000 CFCs per 105 bone marrow cell). Further studies to evaluate methods to derive more highly purified populations of HSCs and CFCs from human ES cells will be of interest.
The hematopoietic differentiation of human ES cells has important therapeutic implications, including the derivation of erythrocytes and platelets for transfusions, and the derivation of HSCs for hematopoietic cell transplantation. Because ES cells can be expanded without apparent limit (16), ES cell-derived blood products could be created in virtually unlimited amounts. These cells could be screened for pathogenic organisms and even potentially be genetically engineered to treat specific patients or to combat specific diseases. ES cell-derived HSCs could dramatically increase both the availability and the effectiveness of HSC transplantation for the treatment of hematologic malignancies. Recent work in mice suggests that highly purified HSCs can provide long-term engraftment across complete allogeneic barriers (32, 33). However, the dose of purified HSCs required to obtain engraftment across these allogeneic MHC barriers is high. By using human ES cells as the starting cell population, a sufficiently large dose of pure HSCs could be generated, which would permit allogeneic engraftment. Importantly, the in vitro derivation of HSCs capable of long-term, multilineage engraftment from mouse ES cells has so far proven an elusive goal. Mouse ES cells, however, clearly have this potential, as they routinely contribute to the definitive hematopoietic system in vivo when formed into chimeras with preimplantation embryos (34). Thus, the failure of hematopoietic cells derived in vitro from mouse ES cells to support long-term, multilineage engraftment reflects our current ignorance of hematopoietic differentiation, but does not reflect a defect in the developmental potential of ES cells.
The derivation of engraftable HSCs from human ES cells will have implications for human medicine far beyond the treatment of hematologic malignancies, as these HSCs may provide a powerful method to prevent immune rejection of other ES cell-derived tissues (35). Use of hematopoietic cell transplantation as a means to create tolerance to a solid organ transplant has been studied since the 1950s (36). Recent studies have shown that transplantation of highly purified mouse HSCs across allogeneic barriers creates tolerance to other tissues that share the same genetic background as the HSCs (37). Other studies in both primates and humans demonstrate that hematopoietic chimerism can create a state of tolerance that permits long-term survival of transplanted organs without continued immunosuppression (38, 39). If human ES cell-derived HSCs can be used to create hematopoietic chimerism in a patient, that patient should be tolerant to other tissues derived from the same ES cells and would not require any continuous immunosuppressive treatment.
The clinical promise of human ES cell-based therapies is great; however, because these therapies will be entirely novel, serious concerns about safety and efficacy will need to be addressed before human clinical trials can be initiated. The malignant transformation of cells that have been cultured for extended periods is a particular concern. Because we also have isolated ES cells from rhesus monkeys (40), it will be possible to use these primate cells as an accurate, preclinical transplantation model for human ES cell-based therapies. Recently, the hematopoietic potential of the rhesus monkey ES cells has been demonstrated (41). These animal models, as well as continued study of methods to promote lineage specific differentiation, will facilitate the potential clinical applications of human ES cell-based therapies.
Acknowledgments
We thank Christine Daigh and Michelle Waknitz for expert technical assistance, and Drs. Deane Mosher and Connie Eaves for review of the manuscript. This work was supported in part by a program pilot grant from the University of Wisconsin Comprehensive Cancer Center and used facilities supported by the WiCell Research Institute.
Abbreviations
- ES
embryonic stem
- HSC
hematopoietic stem cell
- MEF
mouse embryonic fibroblast cell
- CFC
colony-forming cell
- RT-PCR
reverse transcriptase–PCR
- PE
phycoerythrin
- CFU
colony-forming unit
- CFU-Mk
CFU-megakaryocyte
- CFU-M
CFU-macrophage
- CFU-G
CFU-granulocyte
- CFU-GM
CFU-macrophage/granulocyte
References
- 1.Keller G M. Curr Opin Cell Biol. 1995;7:862–869. doi: 10.1016/0955-0674(95)80071-9. [DOI] [PubMed] [Google Scholar]
- 2.Keller G, Kennedy M, Papayannopoulou T, Wiles M V. Mol Cell Biol. 1993;13:473–486. doi: 10.1128/mcb.13.1.473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nakano T, Kodama H, Honjo T. Science. 1994;265:1098–1101. doi: 10.1126/science.8066449. [DOI] [PubMed] [Google Scholar]
- 4.Palacios R, Golunski E, Samaridis J. Proc Natl Acad Sci USA. 1995;92:7530–7534. doi: 10.1073/pnas.92.16.7530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ogawa M, Kizumoto M, Nishikawa S, Fujimoto T, Kodama H, Nishikawa S I. Blood. 1999;93:1168–1177. [PubMed] [Google Scholar]
- 6.Baum C M, Weissman I L, Tsukamoto A S, Buckle A M, Peault B. Proc Natl Acad Sci USA. 1992;89:2804–2808. doi: 10.1073/pnas.89.7.2804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Morrison S J, Uchida N, Weissman I L. Annu Rev Cell Dev Biol. 1995;11:35–71. doi: 10.1146/annurev.cb.11.110195.000343. [DOI] [PubMed] [Google Scholar]
- 8.Goodell M A, Rosenzweig M, Kim H, Marks D F, DeMaria M, Paradis G, Grupp S A, Sieff C A, Mulligan R C, Johnson R P. Nat Med. 1997;3:1337–1345. doi: 10.1038/nm1297-1337. [DOI] [PubMed] [Google Scholar]
- 9.Bhatia M, Bonnet D, Murdoch B, Gan O I, Dick J E. Nat Med. 1998;4:1038–1045. doi: 10.1038/2023. [DOI] [PubMed] [Google Scholar]
- 10.Nakamura Y, Ando K, Chargui J, Kawada H, Sato T, Tsuji T, Hotta T, Kato S. Blood. 1999;94:4053–4059. [PubMed] [Google Scholar]
- 11.Sato T, Laver J H, Ogawa M. Blood. 1999;94:2548–2554. [PubMed] [Google Scholar]
- 12.Jackson K A, Mi T, Goodell M A. Proc Natl Acad Sci USA. 1999;96:14482–14486. doi: 10.1073/pnas.96.25.14482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bjornson C R, Rietze R L, Reynolds B A, Magli M C, Vescovi A L. Science. 1999;283:534–537. doi: 10.1126/science.283.5401.534. [DOI] [PubMed] [Google Scholar]
- 14.Thomson J A, Itskovitz-Eldor J, Shapiro S S, Waknitz M A, Swiergiel J J, Marshall V S, Jones J M. Science. 1998;282:1145–1147. doi: 10.1126/science.282.5391.1145. [DOI] [PubMed] [Google Scholar]
- 15.Reubinoff B E, Pera M F, Fong C Y, Trounson A, Bongso A. Nat Biotechnol. 2000;18:399–404. doi: 10.1038/74447. [DOI] [PubMed] [Google Scholar]
- 16.Amit M, Carpenter M K, Inokuma M S, Chiu C, Harris C P, Waknitz M A, Itskovitz-Eldor J, Thomson J A. Dev Biol. 2000;227:271–278. doi: 10.1006/dbio.2000.9912. [DOI] [PubMed] [Google Scholar]
- 17.Schuldiner M, Yanuka O, Itskovitz-Eldor J, Melton D A, Benvenisty N. Proc Natl Acad Sci USA. 2000;97:11307–11312. doi: 10.1073/pnas.97.21.11307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Collins L S, Dorshkind K. J Immunol. 1987;138:1082–1087. [PubMed] [Google Scholar]
- 19.Wang S J, Greer P, Auerbach R. In Vitro Cell Dev Biol Anim. 1996;32:292–299. doi: 10.1007/BF02723062. [DOI] [PubMed] [Google Scholar]
- 20.Eaves C, Lambie K. Atlas of Human Hematopoietic Colonies. Vancouver: StemCell Technologies; 1995. [Google Scholar]
- 21.Coutinho L M, Gilleece M H, de Wynter E A, Will A, Testa N G. In: Hematopoiesis: A Practical Approach. Testa N G, Molineux G, editors. New York: Oxford Univ. Press; 1993. pp. 75–106. [Google Scholar]
- 22.Uchida N, Buck D W, He H, Reitsma M J, Masek M, Phan T V, Tsukamoto A S, Gage F H, Weissman I L. Proc Natl Acad Sci USA. 2000;97:14720–14725. doi: 10.1073/pnas.97.26.14720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yin A H, Miraglia S, Zanjani E D, Almeida-Porada G, Ogawa M, Leary A G, Olweus J, Kearney J, Buck D W. Blood. 1997;90:5002–5012. [PubMed] [Google Scholar]
- 24.Wineman J, Moore K, Lemischka I, Muller-Sieburg C. Blood. 1996;87:4082–4090. [PubMed] [Google Scholar]
- 25.Lu L S, Wang S J, Auerbach R. Proc Natl Acad Sci USA. 1996;93:14782–14787. doi: 10.1073/pnas.93.25.14782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ramsfjell V, Bryder D, Bjorgvinsdottir H, Kornfalt S, Nilsson L, Borge O J, Jacobsen S E. Blood. 1999;94:4093–4102. [PubMed] [Google Scholar]
- 27.Fina L, Molgaard H V, Robertson D, Bradley N J, Monaghan P, Delia D, Sutherland D R, Baker M A, Greaves M F. Blood. 1990;75:2417–2426. [PubMed] [Google Scholar]
- 28.Watt S M, Williamson J, Genevier H, Fawcett J, Simmons D L, Hatzfeld A, Nesbitt S A, Coombe D R. Blood. 1993;82:2649–2663. [PubMed] [Google Scholar]
- 29.Choi K, Kennedy M, Kazarov A, Papadimitriou J C, Keller G. Development (Cambridge, UK) 1998;125:725–732. doi: 10.1242/dev.125.4.725. [DOI] [PubMed] [Google Scholar]
- 30.Dexter T M, Allen T D, Lajtha L G. J Cell Physiol. 1977;91:335–344. doi: 10.1002/jcp.1040910303. [DOI] [PubMed] [Google Scholar]
- 31.Sutherland H J, Lansdorp P M, Henkelman D H, Eaves A C, Eaves C J. Proc Natl Acad Sci USA. 1990;87:3584–3588. doi: 10.1073/pnas.87.9.3584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shizuru J A, Jerabek L, Edwards C T, Weissman I L. Biol Blood Marrow Transplant. 1996;2:3–14. [PubMed] [Google Scholar]
- 33.Wang B, El-Badri N S, Cherry, Good R A. Proc Natl Acad Sci USA. 1997;94:14632–14636. doi: 10.1073/pnas.94.26.14632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nagy A, Rossant J, Nagy R, Abramow-Newerly W, Roder J C. Proc Natl Acad Sci USA. 1993;90:8424–8428. doi: 10.1073/pnas.90.18.8424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kaufman D S, Odorico J S, Thomson J A. e-biomed: J Regenerative Med. 2000;1:11–15. [Google Scholar]
- 36.Main J M, Prehn R T. J Natl Cancer Inst. 1955;15:1023–1029. [PubMed] [Google Scholar]
- 37.Gandy K L, Weissman I L. Transplantation. 1998;65:295–304. doi: 10.1097/00007890-199802150-00001. [DOI] [PubMed] [Google Scholar]
- 38.Spitzer T R, Delmonico F, Tolkoff-Rubin N, McAfee S, Sackstein R, Saidman S, Colby C, Sykes M, Sachs D H, Cosimi A B. Transplantation. 1999;68:480–484. doi: 10.1097/00007890-199908270-00006. [DOI] [PubMed] [Google Scholar]
- 39.Wekerle T, Sykes M. Transplantation. 1999;68:459–467. doi: 10.1097/00007890-199908270-00001. [DOI] [PubMed] [Google Scholar]
- 40.Thomson J A, Kalishman J, Golos T G, Durning M, Harris C P, Becker R A, Hearn J P. Proc Natl Acad Sci USA. 1995;92:7844–7848. doi: 10.1073/pnas.92.17.7844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Li F, Lu S, Vida L, Thomson J A, Honig G R. Blood. 2001;98:335–342. doi: 10.1182/blood.v98.2.335. [DOI] [PubMed] [Google Scholar]