The incidence of coronary heart disease (CHD) has been declining in the United States,1 but these improvements appear to be lagging in blacks compared to whites.2 To understand race-based patterns in contributions to risk over time, we investigated temporal trends in the prevalence of major risk factors and their attributable hazards for CHD in a large sample of black and white adults living in 4 different communities and followed over the last two decades.
We examined age-adjusted temporal trends in the population attributable risk (PAR) of major CHD risk factors (hypertension, hypercholesterolemia, diabetes, smoking and obesity) using data collected continuously from 14,766 participants (27% black, 56% women) of the multi-center Atherosclerosis Risk in Communities study, who were originally free of CHD and followed from 1987 to 2013.3 Risk factors were defined as follows: hypertension: systolic blood pressure (BP)≥140 mmHg, diastolic BP≥90 mmHg, or anti-hypertensive medication use; hypercholesterolemia: total cholesterol≥200 mg/dL or cholesterol-lowering medication use; obesity: body mass index≥30 kg/m2; diabetes mellitus: fasting glucose≥126 mg/dL, non-fasting glucose≥200 mg/dL, or glucose-lowering medication use; and, current smoking: self-reported active smoking within 1 year. We used a single time-to-event model that considered calendar days as the time scale and treated vital status and all covariates (including risk factors and age) as time-updated while standardizing all results to referent age 65, as previously detailed.3 To account for potential residual confounding by advancing age, all analyses were adjusted for age and any significant age interactions.3 Prevalence of self-reported medication use as well as BP and low-density lipoprotein cholesterol (LDL) levels are presented as rate [95% confidence interval] and mean±standard error, respectively, adjusted for age, sex, and study center and standardized to referent age 65. The study was approved by the Institutional review boards from each site and all participants provided written informed consent.
During a median follow-up of 24.3 (16.7, 25.4) years, we observed 2,020 new-onset CHD cases (592 in blacks), of which 681 were fatal (255 in blacks). The contributions of major risk factors, combined, appeared to decline from years 1990 to 2010 in whites (PAR 73% to 56%) but not in blacks (PAR 77% to 81%). These trends were related to persistent and widening gaps in the contributions of certain risk factors (Figure, Panels A and B). Hypertension was the major risk contributor in both races, and its contribution tended to remain higher in blacks than whites over time. Among participants with hypertension, blacks compared to whites had consistently more elevated systolic BP (139.9±0.8 vs. 137.5±0.5 mmHg in 1990; 136.3±0.8 vs. 128.9±0.5 mmHg in 2010) despite a higher prevalence of anti-hypertensive medication use (71 [66–75]% vs. 66 [63–69]% in 1990; 86 [83–88]% vs. 78 [76–81]% in 2010). Hypercholesterolemia was originally a major risk factor in whites but decreased in its contribution to risk over time (PAR 35% to 9%, P<0.001), due to reductions in both prevalence and hazard; by contrast, hypercholesterolemia in blacks was originally a modest risk factor that tended to increase its risk contribution over time (PAR 14% vs. 31%, P=0.11), given upward trends in both prevalence and hazard. Thus, by 2010, the hypercholesterolemia contribution to CHD risk was 3-fold greater in blacks than whites (Figure, Panels A and B). Although statin use increased (3 [2–4]% to 59 [49–68]% in blacks; 6 [5–7]% to 72 [68–75]% in whites) and LDL levels decreased (160.6±1.5 to 125.3±1.6 mg/dL in blacks; 155.3±0.8 to 119.3±0.8 mg/dL in whites) from 1990 to 2010, among participants with hypercholesterolemia, whites had persistently higher statin use rates and lower LDL levels than blacks over time. With respect to diabetes, its contribution to CHD risk did not substantially change over time in whites (PAR 19% to 16%; P=0.22), but increased in blacks (PAR 19% to 34%; P=0.009), driven by rising prevalence; consequently, the diabetes-related risk was 2-fold higher in blacks than whites by 2010.
Figure. Temporal trends in the contributions of major risk factors to coronary heart disease in whites and blacks.
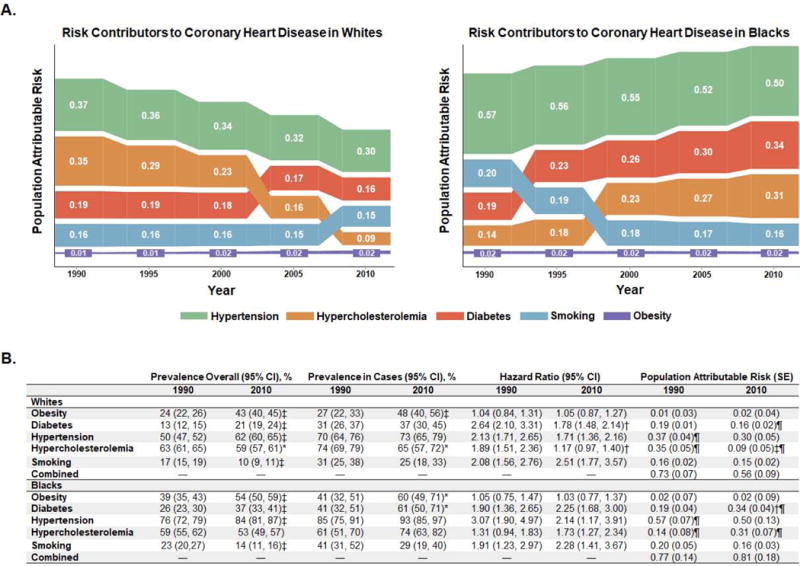
Conceptual Sankey diagrams in Panel A display race-based estimates of each risk factor’s contribution to coronary heart disease incidence over time, where rank order (from top to bottom) is determined by average values. As a result, risk factors with similar population attributable risk (PAR) values may change rank position at different time points. The height of each "bar" is proportional to the PAR value for a given risk factor at a given time point. Prevalence estimates shown in Panel B were based on linear regression analyses accounting for age, sex, and field center and standardized for a sample of persons aged 65 years and with demographics representative of the overall Atherosclerosis Risk in Communities cohort. All hazard ratio and PAR analyses are adjusted for age, sex, field center, hypertension, diabetes, obesity, hypercholesterolemia, and smoking. Linear terms were used to calculate trends in hazard and an age*smoking covariate was included in all Cox-regression models, given an age and smoking interaction (p<0.001 in whites). Combined PAR values were calculated using a multiplicative model assuming no interactions. A coronary heart disease event was defined as a definite or probable hospitalized myocardial infarction, electrocardiographic evidence of an unrecognized prior myocardial infarction, or a definite coronary heart disease death. *P<0.05, †P<0.01, ‡P<0.001 compared to year 1990. ¶P<0.05 compared to PAR of the same risk factor in the other race group at the same time point.
Our longitudinal community data suggest widening racial disparities in the contributions of major risk factors to CHD. We found that, in blacks compared to whites, hypertension has persisted while hypercholesterolemia and diabetes have increased in their contributions to CHD risk over the last two decades. When investigating possible explanations for the raced-based differences in hypertension-related risk, we observed persistently worse BP control in blacks compared to whites, despite blacks reporting higher anti-hypertensive medication use. With respect to the hypercholesterolemia trends, we observed that blacks compared to whites had higher LDL levels and lower statin use over time. These results coincide with evidence that blacks compared to whites have lower rates of access or adherence to interventions aimed at controlling cardiovascular risk factors.4,5 Multiple psychosocial and socioeconomic factors may contribute to the observed racial disparities in CHD risk. Together, our findings suggest that further investigations and targeted efforts, including those focused on improving adherence and access to therapy, are needed to achieve more effective CHD risk factor modification across the population at large – and particularly among blacks.
Acknowledgments
Sources of Funding: Supported by grants from the National Heart, Lung, and Blood Institute (HHSN268201100005C, HHSN268201100006C, HHSN268201100007C, HHSN268201100008C, HHSN268201100009C, HHSN268201100010C, HHSN268201100011C, and HHSN268201100012C, to the Atherosclerosis Risk in Communities study, R01-HL131532 and R01-HL134168, to Dr. Cheng), and the Brazilian National Council for Scientific and Technological Development (249481/2013-8, to Dr. Nadruz).
Footnotes
Data sharing: The data and study materials have been made available to the scientific community via BioLINCC* and analytic methods specific to the current report are provided herein.
* National Heart Lung and Blood Institute (2017). Atherosclerosis Risk in Communities Study (ARIC). Biologic Specimen and Data Repository Information Coordinating Center. NCT00005131.
Disclosures: No potential conflicts of interest relevant to this article were reported.
References
- 1.Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R, de Ferranti SD, Floyd J, Fornage M, Gillespie C, Isasi CR, Jiménez MC, Jordan LC, Judd SE, Lackland D, Lichtman JH, Lisabeth L, Liu S, Longenecker CT, Mackey RH, Matsushita K, Mozaffarian D, Mussolino ME, Nasir K, Neumar RW, Palaniappan L, Pandey DK, Thiagarajan RR, Reeves MJ, Ritchey M, Rodriguez CJ, Roth GA, Rosamond WD, Sasson C, Towfighi A, Tsao CW, Turner MB, Virani SS, Voeks JH, Willey JZ, Wilkins JT, Wu JH, Alger HM, Wong SS, Muntner P, American Heart Association Statistics Committee and Stroke Statistics Subcommittee Heart Disease and Stroke Statistics-2017 Update: A Report From the American Heart Association. Circulation. 2017;135:e146–e603. doi: 10.1161/CIR.0000000000000485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chen J, Normand SL, Wang Y, Drye EE, Schreiner GC, Krumholz HM. Recent declines in hospitalizations for acute myocardial infarction for Medicare fee-for-service beneficiaries: progress and continuing challenges. Circulation. 2010;121:1322–1328. doi: 10.1161/CIRCULATIONAHA.109.862094. [DOI] [PubMed] [Google Scholar]
- 3.Nadruz W, Jr, Claggett B, Henglin M, Shah AM, Skali H, Rosamond WD, Folsom AR, Solomon SD, Cheng S. Racial Disparities in Risks of Stroke. N Engl J Med. 2017;376:2089–2090. doi: 10.1056/NEJMc1616085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mochari-Greenberger H, Liao M, Mosca L. Racial and ethnic differences in statin prescription and clinical outcomes among hospitalized patients with coronary heart disease. Am J Cardiol. 2014;113:413–417. doi: 10.1016/j.amjcard.2013.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kressin NR, Orner MB, Manze M, Glickman ME, Berlowitz D. Understanding contributors to racial disparities in blood pressure control. Circ Cardiovasc Qual Outcomes. 2010;3:173–180. doi: 10.1161/CIRCOUTCOMES.109.860841. [DOI] [PMC free article] [PubMed] [Google Scholar]


