Abstract
Purpose/Objectives
To examine self-reported severity of fatigue and disturbed sleep experienced daily by women with breast cancer during multiple cycles of chemotherapy, exploring potential classes of women experiencing similar symptom trajectories.
Design
In a secondary analysis, classes of women experiencing similar patterns of fatigue and disturbed sleep were identified.
Setting
Oncology clinics in the United States.
Sample
166 women with breast cancer receiving chemotherapy.
Methods
Severity scores were self-reported daily using an automated system. Classes of fatigue and disturbed sleep severity were identified using latent growth mixture modeling.
Main Research Variables
Fatigue, disturbed sleep, age, stage of disease, education, employment, marital status, chemotherapy regimen, hours lying down, and missed work.
Findings
Three fatigue classes were identified: mild decreasing (59% cycle 2, 64% cycle 3), low moderate decreasing (30% cycle 2, 25% cycle 3), and high moderate decreasing (11% both cycles). Two disturbed sleep classes were identified: mild decreasing (89% cycle 2, 81% cycle 3) and increasing (11% cycle 2, 19% cycle 3). Women in the high moderate decreasing fatigue class were more likely to have received doxorubicin (p = 0.02) and spent more hours lying down (p = 0.02).
Conclusions
Patterns of symptom trajectories for fatigue and disturbed sleep were distinguished by baseline symptom severity.
Implications for Nursing
Identification of women at risk for fatigue and disturbed sleep may allow clinicians to intensify symptom management.
Keywords: breast cancer, sleep, fatigue, latent growth mixture modeling, latent class analysis, symptoms
Treatment for breast cancer is associated with toxicities that significantly diminish quality of life, interfere with activity and employment, and interrupt treatment (Bradley, Neumark, Luo, & Schenk, 2007; Cleeland et al., 2003). Considerable evidence suggests variability in symptom trajectories during the course of chemotherapy treatment for breast cancer. However, current evidence has not identified individuals at risk for severe symptom trajectories prior to treatment initiation and symptom escalation (Dodd, Cho, Cooper, & Miaskowski, 2010).
Fatigue and disturbed sleep are common and cause distress in women receiving chemotherapy for breast cancer (Beck et al., 2010; Berger & Higginbotham, 2000; Huang, Chen, Liang, & Miaskowski, 2014; Kuo, Chiu, Liao, & Hwang, 2006). Although fatigue increases with the initiation of treatment, it does not increase with time (Byar, Berger, Bakken, & Cetak, 2006; Jacobsen et al., 1999; Nieboer et al., 2005; Payne, Piper, Rabinowitz, & Zimmerman, 2006). During chemotherapy, the frequency and duration of nighttime awakening and difficulty falling asleep increase and women report the poorest sleep quality on the first night following treatment (Beck et al., 2010; Berger & Higginbotham, 2000; Fortner, Stepanski, Wang, Kasprowicz, & Durrence, 2002). Several potential antecedents to and outcomes of fatigue and disturbed sleep during chemotherapy have been studied. For example, although age is not reported to relate to fatigue during chemotherapy, older adult women experience increased disturbed sleep (Beck et al., 2010; Browall, Ahlberg, Persson, Karlsson, & Danielson, 2008; Colagiuri et al., 2011; de Jong, Candel, Schouten, Abu-Saad, & Courtens, 2004; de Jong, Kester, Schouten, Abu-Saad, & Courtens, 2006; Goldstein et al., 2012; Jacobsen et al., 1999; Von Ah, Kang, & Carpenter, 2008). Reports of the relationship between marital status and fatigue or disturbed sleep during chemotherapy are conflicting (Colagiuri et al., 2011; de Jong et al., 2004; Huang et al., 2014; Jacobsen et al., 1999; Van Onselen et al., 2012). Income and disease stage are not reported to relate to fatigue or sleep disturbance during chemotherapy for breast cancer (Beck et al., 2010; Colagiuri et al., 2011; de Jong et al., 2004; Von Ah et al., 2008). In addition, fatigue and disturbed sleep may predict decreases in activity level during chemotherapy for breast cancer (Berger, 1998; Berger & Farr, 1999; Berger & Higginbotham, 2000; Colagiuri et al., 2011; de Jong et al., 2004; Jacobsen et al., 1999).
The current study was framed by the Dynamic Symptoms Model, which describes the complex nature and longitudinal trajectory of the symptom experience, incorporating the potential for distinct patterns of symptom change with time that may be preceded by antecedent variables and may influence outcomes (Brant, Dudley, Beck, & Miaskowsi, 2016). Consistent with the model, the current study includes specific antecedents (demographic and clinical variables), growth parameters of the symptom experience, and consequences (days of missed work and hours spent lying down). Advances in longitudinal statistical modeling have allowed for newer methodologic approaches to studying classes of symptom trajectories, identifying homogeneous classes of people who share common symptom trajectories. Several investigators have applied subgroup analyses to symptom data for women with breast cancer during various stages of the disease, but only one report of classes of disturbed sleep trajectories and no reports of classes of fatigue trajectories were found in the literature (Dunn et al., 2011; Lam et al., 2010; Langford et al., 2016; Van Onselen et al., 2012).
The purpose of the current study was to examine self-reported severity of fatigue and disturbed sleep experienced daily by women with breast cancer during multiple cycles of chemotherapy and to explore potential classes of women experiencing similar symptom trajectories. The specific aims were to (a) determine the distinct trajectory classes associated with the severity of fatigue and disturbed sleep reported by women undergoing cycles 2 and 3 of chemotherapy for breast cancer, (b) determine if class membership is determined by various antecedent variables, and (c) determine if class membership is associated with days of missed work and hours spent lying down. Understanding trajectories of symptoms may elucidate common etiologies, which may inform the development of targeted symptom interventions.
Methods
Participants and Setting
The current study was a secondary analysis of longitudinal data pooled from three trials of a symptom monitoring and behavioral intervention in women undergoing chemotherapy for breast cancer. Studies 1 and 2 tested the use of an automated system for monitoring and managing symptoms during chemotherapy. Study 3 was an observational study using the same automated system for data collection. A detailed description of the sampling procedures for the parent studies and automated system are provided elsewhere (Mooney, Beck, Friedman, Farzanfar, & Wong, 2014; Mooney et al., 2017).
For study 1, participants were recruited from Cancer Centers of the Carolinas in Greenville, South Carolina, and Intermountain Hematology/Oncology Associates, Wasatch Hematology/Oncology Associates, and Huntsman Cancer Institute, all in Salt Lake City, Utah. For study 2, participants were recruited from Huntsman Cancer Institute and Vanderbilt University Medical Center in Nashville, Tennesee. For study 3, participants were recruited from Huntsman Cancer Institute. Eligibility requirements for this analysis included being a woman diagnosed with breast cancer at initial treatment with chemotherapy, completing study measures through cycles 2 and 3, and reporting data for at least three days during each cycle to allow for application of the analytic methods. Women receiving radiation therapy or biotherapy agents were excluded. Although participants were randomly assigned to a usual care group or a symptom management intervention group in study 1 and 2, differences were found in reported symptoms between groups in study 2 only. Therefore, data collected from eligible participants randomized to the control group in study 2 and data from all eligible participants in studies 1 and 3 were used in this secondary analysis. Cycles 2 and 3 were examined because symptom data were collected during only these cycles in study 1. To accommodate for varying cycle lengths, only data from the first 14 days of each cycle were included.
The original sampling frame consisted of 259 women with breast cancer who were pooled from the three parent studies. Thirteen women who did not complete study measures through cycles 2 and 3 and 80 women who were randomized to the intervention group for study 2 were excluded. This yielded a total data set of 166 women, of which 165 (cycle 2) and 155 (cycle 3) completed measures on at least three days, which was sufficient to apply the analytic methods using Monte Carlo estimation (Muthén & Muthén, 2000).
Measures
Demographic and disease-related data (age, stage of disease, education, employment, marital status, and chemotherapy regimen) were collected at study entry from the participants and their medical record. Participants called the automated system daily to report the presence and severity of fatigue and disturbed sleep, using single-item indicators, with acceptable reliability and validity (Cleeland & Mendoza, 2011; Mooney et al., 2014). Modeled after common symptom assessment tools, the automated system employed conditional branching such that participants were first asked, “During the past 24 hours did you experience (symptoms)?” A “yes” response yielded a question asking the participant to score the symptom severity using a Likert-type scale, with scores ranging from 1 (low) to 10 (high). Participants also reported hours spent lying down; employed participants reported whether they were able to go to work each day.
Procedures
All parent studies and this secondary analysis were approved by the University of Utah Institutional Review Board. Participants were identified only by their original study identification number. All participants signed a written, informed consent to participate in the original parent studies, which included language giving permission for the data collected to be used in additional scientific investigations.
Statistical Analysis
Mplus, version 6.0, was used for mixture model analyses, and SPSS®, version 23.0, was used for data management and analysis of demographic and clinical variables. The data were cleaned and transformed to a person–period data set, containing a participant identifier, a time indicator (time of measurement), outcome variables (symptom scores for each symptom on a Likert-type scale ranging from 0–10), and correlate variables (demographic and disease-related variables, hours spent lying down, and days of missed work). Alpha was set at 0.05, and no adjustments were made for multiplicity in this exploratory study. Descriptive statistics and frequency distributions were generated on the sample characteristics and symptom severity scores.
Latent growth mixture modeling (LGMM) allows for the identification of discrete classes of individuals based on common trajectories of growth. The categorical latent variables represent the class that describes groups of individuals who are homogeneous within that class and are heterogeneous across classes (Muthén & Muthén, 2000). Using LGMM, an initial one-class model was tested, and subsequent classes were added in ascending order to determine the best model fit. Each latent class corresponded to a subpopulation with its own set of parameter values (intercept and slope) (Singer & Willett, 2003). Missing data were accommodated through use of a full information maximum likelihood method. Stepwise models were evaluated on multiple fit indices, including the Bayesian information criterion (BIC) and entropy, with smaller BIC and entropy close to 1 indicating a better model fit (Colder, Campbell, Ruel, Richardson, & Flay, 2002; Jung & Wickerama, 2008; Muthén & Muthén, 2000). In addition, the best-fitting model was examined for the number of participants in each class (greater than 5% of the sample) and graphed visually to determine if the predicted trajectories were clinically and theoretically relevant (Jung & Wickerama, 2008).
After determining the best model fit for the data, the model-predicted class membership for each individual was obtained using posterior probabilities. Although the model-predicted class assignment is uncertain, high entropy and high posterior probabilities suggest that model-predicted class assignments could be considered observed variables. Model-predicted class memberships then were used to test for differences among the classes on antecedents and consequences of class membership. Chi-square was used to test for associations among categories across classes in antecedents (stage of disease, education, employment, marital status, and chemotherapy regimen). Independent-samples t tests and analysis of variance (ANOVA) were used to test for differences between the classes in age and outcomes (hours spent lying down and days of missed work) (de Jong et al., 2004). Daily measures of hours spent lying down during the first 14 days of each cycle separately were averaged for each individual for each cycle 2 and 3. Days of missed work during the first 14 days of each cycle separately were summed for all employed participants. Small cell sizes, with an expected frequency of five or less, were accounted for with use of the more conservative Fisher’s exact chi-square (Green & Salkind, 2008). In cases for which classes did not display homogeneity of variance, the Welch statistic, a robust test that allows violation of this assumption, was used (Green & Salkind, 2008). Where appropriate, follow-up post-hoc contrasts were conducted to evaluate pairwise differences in class membership on antecedents and outcomes. In cases for which equal variances were not assumed, Dunnett’s C test was used (Green & Salkind, 2008).
Results
Patient demographic and clinical characteristics are summarized in Table 1. Participants ranged in age from 24–80 years ( , SD = 10.8). Most participants were White, married, and unemployed. The largest proportion of the sample was diagnosed with stage II disease and had some education beyond high school. Women in the sample received any of 12 different chemotherapy regimens. Daily call compliance was 78.4% (cycle 2) and 78% (cycle 3). The prevalence of fatigue and disturbed sleep and the percentage of days reported with severity of 0, severity of 1–10, and severity of 4–10 (moderate to severe levels) are reported in Table 2.
TABLE 1.
Sample Characteristics (N = 166) Characteristic n %
| Characteristic | n | % |
|---|---|---|
| Ethnicity | ||
| Non-Hispanic | 162 | 98 |
| Hispanic | 2 | 1 |
| Unknown | 2 | 1 |
| Marital status | ||
| Partnered | 123 | 74 |
| Non-partnered | 41 | 25 |
| Unknown | 2 | 1 |
| Employment status | ||
| Not employed | 103 | 62 |
| Full-time | 48 | 29 |
| Part-time | 13 | 8 |
| Unknown | 2 | 1 |
| Education | ||
| Some high school | 6 | 4 |
| High school graduate | 31 | 19 |
| Some college | 52 | 31 |
| Associate degree | 15 | 9 |
| Bachelor’s degree | 36 | 22 |
| Postgraduate | 22 | 13 |
| Unknown | 4 | 3 |
| Income ($) | ||
| Less than 9,999 | 8 | 5 |
| 10,000–29,999 | 16 | 10 |
| 30,000–49,999 | 37 | 22 |
| 50,000–69,999 | 20 | 12 |
| 70,000 or more | 57 | 34 |
| Unknown | 10 | 6 |
| Declined to state | 18 | 11 |
| Stage of disease | ||
| I | 20 | 12 |
| II | 67 | 40 |
| III | 38 | 23 |
| IV | 36 | 22 |
| Unknown | 5 | 3 |
| Chemotherapy regimen | ||
| Cyclophosphamide with doxorubicin | 68 | 41 |
| Docetaxel | 23 | 14 |
| Cyclophosphamide with methotrexate and 5-fluorouracil | 16 | 10 |
| Docetaxel and carboplatin | 13 | 8 |
| Cyclophosphamide with docetaxel | 12 | 7 |
| Cyclophosphamide with doxorubicin and docetaxel | 9 | 5 |
| Cyclophosphamide with doxorubicin and 5-fluorouracil | 6 | 4 |
| Cyclophosphamide with 5-fluorouracil | 4 | 2 |
| Other | 15 | 9 |
Note. Because of rounding, percentages may not total 100.
TABLE 2.
Symptom Prevalence and Mean Number of Days at Moderate to Severe Levels
| Reported Severlty Greater Than 0 at Least Once
|
Days of Severlty Greater Than 0
|
Reported Severlty Greater Than 3 at Least Once
|
Days of Severlty Greater Than 3
|
Days Symptom Reported Level 0
|
Days Symptom Reported Level 1-10
|
Days Symptom Reported Level 4-10
|
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Symptom | n | % |
|
SD | Range | n | % |
|
SD | Range | n | % | n | % | n | % | ||
| Cycle 2 | ||||||||||||||||||
| Fatiguea | 153 | 93 | 7.53 | 3.69 | 1–14 | 115 | 70 | 5.09 | 3.47 | 1–14 | 659 | 36 | 1,152 | 64 | 585 | 32 | ||
| Disturbed sleepb | 126 | 76 | 3.63 | 2.56 | 1–13 | 103 | 62 | 2.87 | 2.07 | 1–13 | 1,354 | 75 | 457 | 25 | 296 | 16 | ||
| Cycle 3 | ||||||||||||||||||
| Fatiguea | 148 | 95 | 7.09 | 3.93 | 1–14 | 105 | 67 | 4.95 | 3.7 | 1–14 | 654 | 38 | 1,050 | 62 | 520 | 31 | ||
| Disturbed sleepb | 110 | 71 | 3.4 | 2.64 | 1–13 | 85 | 55 | 2.46 | 1.76 | 1–11 | 1,330 | 78 | 374 | 22 | 209 | 12 | ||
N = 165 for cycle 2 and 156 for cycle 3; 1,811 (78%) days reported cycle 2; 1,704 (78%) days reported cycle 3; 499 (22%) days missing cycle 2; 480 (22%) days missing cycle 3
N = 84 for cycle 2 and 75 for cycle 3; 948 (81%) days reported cycle 2; 825 (80%) days reported cycle 3; 228 (19%) days missing cycle 2; 211 (20%) days missing cycle 3
Multiclass latent growth mixture models were evaluated for fatigue and disturbed sleep, and fit indices are presented in Table 3. Intercept, slopes, and quadratic terms are presented in Table 4, and trajectory graphs are presented in Figure 1. Class names were based on common category nomenclature for symptom severity: none (0), mild (0–3), moderate (4–7), and severe (7–10) for the intercept and a description of the slope term. For fatigue, a three-class solution was selected during both cycles. Most women were in the mild decreasing fatigue class (59% for cycle 2, 64% for cycle 3), with a low fatigue severity level at day 1 of each cycle ( , SD = 0.29; , SD = 0.24). Individuals in the low moderate decreasing fatigue class (30% for cycle 2, 25% for cycle 3) had a moderate fatigue severity level at day 1 of each cycle ( , SD = 0.52; , SD =0.39), and individuals in the high moderate decreasing fatigue class had a high moderate level of fatigue at day 1 ( , SD = 0.73; , SD = 0.51), maintaining that level through day 5, and then had a slight decline in fatigue to day 14 of each cycle. In both cycles, 11% of participants were in the high moderate fatigue class.
TABLE 3.
Model Fit for Latent Growth Mixture Models
| Modela | Log Likelihood | BIC | Entropy | Posterior Probability | Class Proportions |
|---|---|---|---|---|---|
|
Fatigue
| |||||
| Cycle 2 | |||||
| 1 class | −4,309.41 | 8,651.7 | NA | NA | NA |
| 2 class | −3,954.18 | 7,958.98 | 0.944 | 0.988, 0.989 | 69%, 31% |
|
| |||||
| 3 class | −3,847.23 | 7,742.81 | 0.944 | 0.977, 0.95, 0.982 | 59%, 30%, 11% |
|
| |||||
| 4 class | −3,800.81 | 7,657.7 | 0.943 | 0.95, 0.96, 0.984, 0.935 | 57%, 12%, 22%, 10% |
| Cycle 3 | |||||
| 1 class | −4,062.06 | 8,156.06 | NA | NA | NA |
| 2 class | −3,652.62 | 7,344.68 | 0.963 | 0.998, 0.968 | 72%, 28% |
|
| |||||
| 3 class | −3,570.33 | 7.187.62 | 0.941 | 0.986, 0.95, 0.96 | 64%, 25%, 11% |
|
| |||||
| 4 class | −3,538.36 | 7,131.18 | 0.881 | 0.935, 0.869, 1, 0.956 | 53%, 22%, 22%, 3% |
|
Disturbed sleep | |||||
| Cycle 2 | |||||
| 1 class | −4,067.91 | 8,168.7 | NA | NA | NA |
|
| |||||
| 2 class | −3,906.86 | 7,854.34 | 0.984 | 0.997, 0.995 | 89%, 11% |
|
| |||||
| 3 class | −3,855.66 | 7,759.66 | 0.958 | 0.945, 0.989, 0.968 | 84%, 10%, 5% |
| Cycle 3 | |||||
| 1 class | −3,582.73 | 7,197.38 | NA | NA | NA |
|
| |||||
| 2 class | −3,441.79 | 6,923.02 | 0.925 | 0.981, 0.98 | 81%, 19% |
|
| |||||
| 3 class | −3,385.73 | 6,818.42 | 0.962 | 0.987, 0.995, 0.969 | 82%, 14%, 5% |
Classes were added stepwise to the model to determine the solution that best fit the data, evaluated on the BIC and entropy, and examined for the number of participants in each class and graphed visually.
BIC—Bayesian information criterion; NA—not applicable
Note. Shading indicates the selected model solution.
TABLE 4.
Growth Factor Means and Predicted Frequencies for Each Class
| Class | Intercept | Slope | Quadratic Term | Class Count |
|---|---|---|---|---|
|
Fatigue
| ||||
| Cycle 2 | ||||
| Mild decreasing | 2.25* | ‒0.26* | 0.01* | 97.94 |
| Low moderate decreasing | 3.21* | 0.32 | −0.03* | 51.46 |
| High moderate decreasing | 5.66* | 0.34 | 0.01 | 18.26 |
| Cycle 3 | ||||
| Mild decreasing | 1.76* | −0.12 | 0.00 | 106.24 |
| Low moderate decreasing | 2.52* | 0.65* | −0.06* | 41.5 |
| High moderate decreasing | 5.43* | 0.6* | −0.06* | 18.26 |
|
Disturbed sleep | ||||
| Cycle 2 | ||||
| Mild decreasing | 1.74* | −0.2* | 0.01 | 145.85 |
| Moderate increasing | 3.76* | −0.28 | 0.03 | 18.15 |
| Cycle 3 | ||||
| Mild decreasing | 0.87* | −0.07 | 0.00 | 133.65 |
| Mild increasing | 1.66* | 0.14 | 0.00 | 31.35 |
p < 0.05
FIGURE 1.
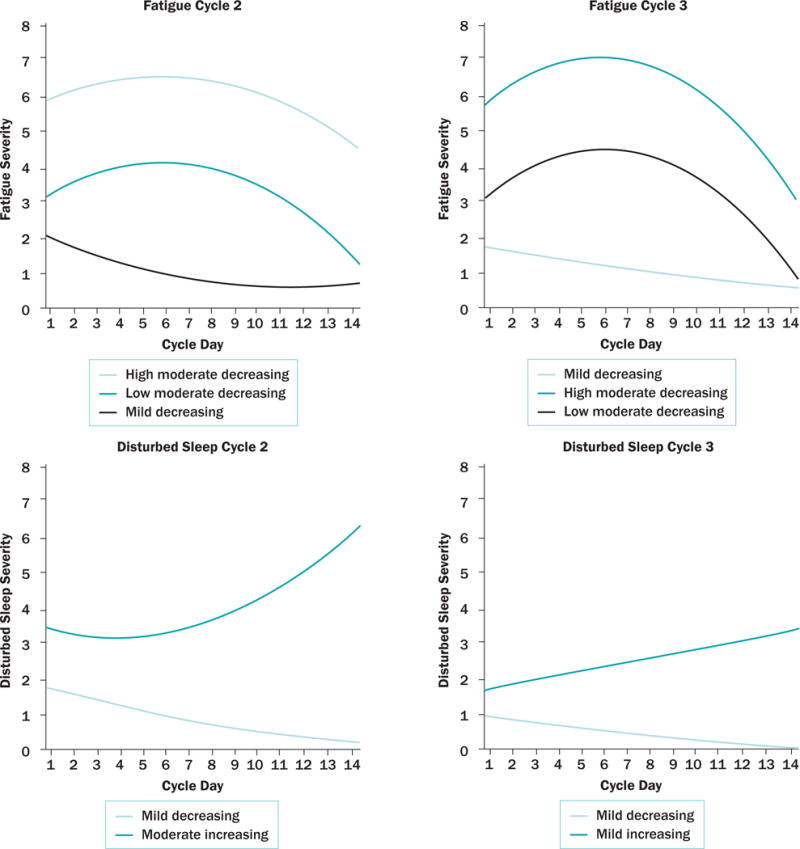
Individual Symptom Trajectory Models
For disturbed sleep, two classes were identified during each cycle. Most participants were in the mild decreasing disturbed sleep classes (89% for cycle 2, 81% for cycle 3) and had a low severity of disturbed sleep at day 1 ( , SD = 0.2; , SD = 0.13) for each cycle and remained stable during the 14 days. A smaller percentage of participants were in the moderate increasing (cycle 2) and mild increasing (cycle 3) disturbed sleep classes (11% in cycle 2, 19% in cycle 3), with a higher severity of disturbed sleep at cycle day 1 in both cycles ( , SD = 1.05; , SD = 0.49) that increased during the 14 days.
Results of the tests of differences and associations among categories across classes on the demographic variables are presented in Table 5 for the fatigue classes and Table 6 for the disturbed sleep classes. All tests were nonsignificant, except for chemotherapy regimen. Women who received doxorubicin were more likely to be in the high moderate decreasing fatigue class when compared to the mild decreasing fatigue class in both cycles 2 (χ2= 7.75, p = 0.02) and 3 (χ2 = 8.59, p = 0.01).
TABLE 5.
Tests of Difference in Means and Associations Among Categories for Antecedents and Outcomes of Fatigue Class Membership
| Mild Decreasing (N = 95)
|
Low Moderate Decreasing (N = 50)
|
High Moderate Decreasing (N = 19)
|
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Characteristic |
|
SD |
|
SD |
|
SD | Omnibus Test | |||
| Cycle 2 | ||||||||||
|
| ||||||||||
| Age (years) | 51.79 | 10.7 | 53.56 | 10.2 | 57.51 | 11.76 | F(2, 159) = 2.35, p = 0.1 | |||
| Hours spent lying down | 10 | 2.54 | 10.79 | 2.64 | 12.36 | 3.77 | F(2, 44) = 2.03, p = 0.02* | |||
| Days missed work (n = 20) | 1.9 | 1.52 | 3.13 | 2.03 | 2.5 | 2.12 | F(2, 17) = 1.05, p = 0.37 | |||
|
| ||||||||||
| Characteristic | n | % | n | % | n | % | Omnibus Test | |||
|
| ||||||||||
| Education | χ2 = 2.16, p = 0.99 | |||||||||
| Less than high school | 4 | 4 | 1 | 2 | 1 | 5 | ||||
| High school | 20 | 21 | 8 | 16 | 3 | 16 | ||||
| Undergraduate | 57 | 60 | 33 | 66 | 13 | 68 | ||||
| Postgraduate | 12 | 13 | 7 | 14 | 2 | 11 | ||||
| Unknown | 2 | 2 | 1 | 2 | – | – | ||||
| Marital status | χ2 = 1.54, p = 0.85 | |||||||||
| Married | 72 | 76 | 37 | 74 | 13 | 68 | ||||
| Not married | 23 | 24 | 12 | 24 | 6 | 32 | ||||
| Unknown | – | – | 1 | 2 | – | – | ||||
| Employment | χ2 = 2.91, p = 0.58 | |||||||||
| Employed | 32 | 34 | 22 | 44 | 6 | 32 | ||||
| Not employed | 63 | 66 | 27 | 54 | 13 | 68 | ||||
| Unknown | – | – | 1 | 2 | – | – | ||||
| Stage | χ2 = 4.6, p = 0.8 | |||||||||
| I | 13 | 14 | 5 | 10 | 2 | 11 | ||||
| II | 34 | 36 | 25 | 50 | 8 | 42 | ||||
| III | 24 | 25 | 10 | 20 | 4 | 21 | ||||
| IV | 21 | 22 | 10 | 20 | 5 | 26 | ||||
| Unknown | 3 | 3 | – | – | – | – | ||||
| Doxorubicin | χ2 = 7.75, p = 0.02* | |||||||||
| Yes | 41 | 43 | 27 | 54 | 14 | 74 | ||||
| No | 47 | 50 | 20 | 40 | 3 | 16 | ||||
| Unknown | 7 | 7 | 3 | 6 | 2 | 11 | ||||
| Taxane | χ2 = 3.01, p = 0.22 | |||||||||
| Yes | 34 | 36 | 14 | 28 | 3 | 15 | ||||
| No | 54 | 57 | 33 | 66 | 14 | 74 | ||||
| Unknown | 7 | 7 | 3 | 6 | 2 | 11 | ||||
|
| ||||||||||
|
Mild Decreasing (N = 97)
|
Low Moderate Decreasing (N = 39)
|
High Moderate Decreasing (N = 18)
|
||||||||
| Characteristic |
|
SD |
|
SD |
|
SD | Omnibus Test | |||
|
| ||||||||||
| Cycle 3 | ||||||||||
|
| ||||||||||
| Age (years) | 52.9 | 10.31 | 52.53 | 12 | 54.13 | 12 | F(2, 150) = 0.13, p = 0.88 | |||
| Hours spent lying down | 10.44 | 2.94 | 10.71 | 2.51 | 10.05 | 2.51 | F(2, 150) = 0.35, p = 0.7 | |||
| Days missed work (n = 27) | 1.33 | 1.5 | 1.43 | 1.72 | 2.2 | 1.65 | F(2, 24) = 0.51, p = 0.61 | |||
|
| ||||||||||
| Characteristic | n | % | n | % | n | % | Omnibus Test | |||
|
| ||||||||||
| Education | χ2 = 3.47, p = 0.75 | |||||||||
| Less than high school | 3 | 3 | 1 | 3 | 1 | 5 | ||||
| High school | 20 | 21 | 5 | 13 | 5 | 28 | ||||
| Undergraduate | 58 | 60 | 26 | 66 | 10 | 56 | ||||
| Postgraduate | 12 | 12 | 7 | 18 | 2 | 11 | ||||
| Unknown | 4 | 4 | – | – | – | – | ||||
| Marital status | χ2 = 0.78, p = 0.74 | |||||||||
| Married | 69 | 71 | 29 | 74 | 15 | 83 | ||||
| Not married | 26 | 27 | 10 | 26 | 3 | 17 | ||||
| Unknown | 2 | 2 | – | – | – | – | ||||
| Employment | χ2 = 0.06, p = 1.00 | |||||||||
| Employed | 36 | 37 | 15 | 38 | 7 | 39 | ||||
| Not employed | 59 | 61 | 24 | 62 | 11 | 61 | ||||
| Unknown | 2 | 2 | – | – | – | – | ||||
| Stage | χ2 = 7.69, p = 0.25 | |||||||||
| I | 11 | 11 | 6 | 15 | – | – | ||||
| II | 37 | 38 | 20 | 51 | 9 | 50 | ||||
| III | 27 | 28 | 5 | 13 | 6 | 33 | ||||
| IV | 22 | 23 | 7 | 18 | 3 | 17 | ||||
| Unknown | – | – | 1 | 3 | – | – | ||||
| Doxorubicin | – | – | χ2 = 8.59, p = 0.01* | |||||||
| Yes | 45 | 46 | 22 | 56 | 15 | 83 | ||||
| No | 51 | 53 | 16 | 41 | 3 | 17 | ||||
| Unknown | 1 | 1 | 1 | 3 | – | – | ||||
| Taxane | χ2 = 6.06, p = 0.05 | |||||||||
| Yes | 38 | 39 | 11 | 28 | 2 | 11 | ||||
| No | 58 | 60 | 27 | 69 | 16 | 89 | ||||
| Unknown | 1 | 1 | 1 | 3 | – | – | ||||
p < 0.05
TABLE 6.
Tests of Difference in Means and Associations Among Categories for Antecedents and Outcomes of Disturbed Sleep Class Membership
| Mild Decreasing (N = 139)
|
Moderate Increasing (N = 25)
|
||||||
|---|---|---|---|---|---|---|---|
| Characteristic |
|
SD |
|
SD | Omnibus Test | ||
| Cycle 2 | |||||||
|
| |||||||
| Age (years) | 53.06 | 10.63 | 52.03 | 11.54 | t(159) = 0.19, p = 0.66 | ||
| Hours spent lying down | 10.66 | 2.59 | 9.87 | 3.88 | t(28.1) = 0.98, p = 0.33 | ||
| Days missed work (n = 20) | 2.44 | 1.93 | 2.5 | 1.29 | t(18) = 0.00, p = 0.95 | ||
|
| |||||||
| Characteristic | n | % | n | % | Omnibus Test | ||
|
| |||||||
| Education | χ2 = 1.08, p = 0.94 | ||||||
| Less than high school | 6 | 4 | – | – | |||
| High school | 26 | 19 | 4 | 16 | |||
| Undergraduate | 85 | 61 | 18 | 72 | |||
| Postgraduate | 18 | 13 | 3 | 12 | |||
| Unknown | 4 | 3 | – | – | |||
| Marital status | χ2 = 1.01, p = 0.61 | ||||||
| Married | 104 | 75 | 17 | 68 | |||
| Not married | 33 | 24 | 8 | 32 | |||
| Unknown | 2 | 1 | – | – | |||
| Employment | χ2 = 0.87, p = 0.64 | ||||||
| Employed | 48 | 35 | 11 | 44 | |||
| Not employed | 88 | 63 | 14 | 56 | |||
| Unknown | 3 | 2 | – | – | |||
| Stage | χ2 = 3.8, p = 0.4 | ||||||
| I | 14 | 10 | 6 | 24 | |||
| II | 57 | 41 | 10 | 40 | |||
| III | 33 | 24 | 4 | 16 | |||
| IV | 31 | 22 | 5 | 20 | |||
| Unknown | 4 | 3 | – | – | |||
| Doxorubicin | χ 2 = 0.22, p = 0.66 | ||||||
| Yes | 68 | 49 | 14 | 56 | |||
| No | 60 | 43 | 10 | 40 | |||
| Unknown | 11 | 8 | 1 | 4 | |||
| Taxane | χ2 = 0.25, p = 0.65 | ||||||
| Yes | 44 | 32 | 7 | 28 | |||
| No | 84 | 60 | 17 | 68 | |||
| nknown | 11 | 8 | 1 | 4 | |||
|
| |||||||
|
Mild Decreasing (N = 137)
|
Mild Increasing (N = 18)
|
||||||
| Characteristic |
|
SD |
|
SD | Omnibus Test | ||
|
| |||||||
| Cycle 3 | |||||||
|
| |||||||
| Age (years) | 52.79 | 10.95 | 52.7 | 9.18 | t(150) = 0.00, p = 0.97 | ||
| Hours spent lying down | 10.69 | 2.74 | 9.65 | 3.23 | t(150) = 1.48, p = 0.14 | ||
| Days missed work (n = 27) | 1.5 | 1.71 | 1.6 | 1.52 | t(25) = 0.01, p = 0.91 | ||
|
| |||||||
| Characteristic | n | % | n | % | Omnibus Test | ||
|
| |||||||
| Education | χ2 = 2.31, p = 0.62 | ||||||
| Less than high school | 5 | 4 | 1 | 6 | |||
| High school | 26 | 19 | 2 | 11 | |||
| Undergraduate | 86 | 63 | 12 | 66 | |||
| Postgraduate | 17 | 12 | 2 | 11 | |||
| Unknown | 3 | 2 | 1 | 6 | |||
| Marital status | χ2 = 2.25, p = 0.41 | ||||||
| Married | 103 | 75 | 11 | 61 | |||
| Not married | 32 | 24 | 7 | 39 | |||
| Unknown | 2 | 1 | – | – | |||
| Employment | χ2 = 0.29, p = 1.00 | ||||||
| Employed | 53 | 39 | 7 | 39 | |||
| Not employed | 82 | 60 | 11 | 61 | |||
| Unknown | 2 | 1 | – | – | |||
| Stage | χ2 = 1.83, p = 0.77 | ||||||
| I | 17 | 13 | 2 | 11 | |||
| II | 58 | 42 | 7 | 39 | |||
| III | 32 | 23 | 3 | 17 | |||
| IV | 27 | 20 | 6 | 33 | |||
| Unknown | 3 | 2 | – | – | |||
| Doxorubicin | χ2 = 0.18, p = 0.67 | ||||||
| Yes | 72 | 53 | 10 | 56 | |||
| No | 63 | 46 | 7 | 39 | |||
| Unknown | 2 | 1 | 1 | 5 | |||
| Taxane | χ2 = 0.5, p = 0.59 | ||||||
| Yes | 44 | 33 | 7 | 39 | |||
| No | 91 | 66 | 10 | 56 | |||
| Unknown | 2 | 1 | 1 | 5 | |||
Independent-samples t tests and ANOVAs for hours spent lying down and days of missed work were nonsignificant, except for hours spent lying down during cycle 2 for fatigue class. During cycle 2, the number of hours spent lying down was statistically significantly higher in the high moderate decreasing fatigue class ( , SD = 3.77) when compared to the mild decreasing fatigue class ( , SD = 2.54) (F[2, 44] = 2.03, p = 0.02).
Discussion
Results of the current study contribute to a growing body of literature concerned with the trajectories of symptoms experienced by women receiving chemotherapy for breast cancer. Distinct patterns of fatigue and disturbed sleep were identified and antecedents and consequences to those patterns were studied, consistent with the Dynamic Symptoms Model (Brant et al., 2016). Fatigue was reported at a severity greater than 0 by more than 90% of women, consistent with the high prevalence of fatigue during chemotherapy found in other studies (Bender, Ergÿn, Rosenzweig, Cohen, & Sereika, 2005; Bower et al., 2011; Browall, Persson, Ahlberg, Karlsson, & Danielson, 2009; Downie, Mar Fan, Houédé-Tchen, Yi, & Tannock, 2006; Gaston-Johansson, Fall-Dickson, Bakos, & Kennedy, 1999; Given, Given, Azzouz, & Stommel, 2001; Jacobsen et al., 1999; Kim, Barsevick, Tulman, & McDermott, 2008; Liu et al., 2009; Nieboer et al., 2005; So et al., 2009; Tchen et al., 2003). In contrast to previous studies, this analysis used fatigue severity rather than occurrence to model change. Three patterns of fatigue were described, including mild decreasing fatigue, low moderate decreasing fatigue, and high moderate decreasing fatigue classes. Across all three classes, fatigue improved during the first 14 days of chemotherapy during both cycles but remained present at day 14, consistent with previous findings that fatigue persists throughout treatment but does not worsen with time (Byar et al., 2006; de Jong et al., 2004; Jacobsen et al., 1999; Payne et al., 2006; Sitzia & Huggins, 1998). In addition, the growth factors during the two cycles of chemotherapy suggest that fatigue in cycle 2 did not differ in pattern during cycle 3, similar to previously reported findings that fatigue does not differ in subsequent chemotherapy cycles (Berger, 1998; Jacobsen et al., 1999).
Disturbed sleep was reported by more than 70% of women, which is slightly higher than previous reports (Beck et al., 2010; Bender et al., 2005; Berger & Higginbotham, 2000; Bower et al., 2011; Fortner et al., 2002; Given et al., 2001; Janz et al., 2007; Kim et al., 2008; Lee, Dibble, Pickett, & Luce, 2005). Two patterns of disturbed sleep were described, including a mild decreasing disturbed sleep class during both cycles, a moderate increasing disturbed sleep class during cycle 2, and a mild increasing disturbed sleep class during cycle 3. Although the severity of disturbed sleep improved slightly with time in the mild decreasing disturbed sleep class during both cycles, the severity of disturbed sleep worsened in the increasing disturbed sleep classes during both cycles, suggesting that some women experienced disturbed sleep progression.
The current findings conflict with a report by Van Onselen et al. (2012), in which three classes of women with sleep disturbance during the six months following surgery for breast cancer were identified: a low and high class, but also a decreasing class that represented 5.3% of their sample (N = 398). The conflicting number of classes may be a result of differing instrumentation and timing of measures and use of model constraints.
None of the demographic or clinical characteristics was found to be associated with class membership, except for chemotherapy regimen. The current findings are consistent with several reports that age and fatigue are not related (Browall et al., 2008; de Jong et al., 2004, 2006; Goldstein et al., 2012; Jacobsen et al., 1999; Von Ah et al., 2008). Findings relating age and disturbed sleep are inconsistently reported, and this relationship was not found in the current sample (Beck et al., 2010; Browall et al., 2008; Colagiuri et al., 2011; Van Onselen et al., 2012). Similarly, the relationship between marital status and fatigue is inconsistently reported, with no relationship being found in the current sample (de Jong et al., 2004; Huang et al., 2014; Jacobsen et al., 1999). The lack of relationship between marital status and disturbed sleep is similar to findings of Colagiuri et al. (2011) and Van Onselen et al. (2012). Although the current finding that employment status does not predict fatigue is supported in the literature, Van Onselen et al. (2012) found an association between unemployment and disturbed sleep trajectory (de Jong et al., 2004, 2006; Huang et al., 2014). The lack of association between stage of disease and either fatigue or disturbed sleep has been previously reported (Beck et al., 2010; Colagiuri et al., 2011; de Jong et al., 2004; Jacobsen et al., 1999; Van Onselen et al., 2012; Von Ah & Kang, 2008). A lack of sample variation on these demographics and a relatively small sample size in the current study may explain some conflicting findings. Additional research is needed to explore other personal characteristics, including molecular determinants (Cleeland et al., 2003; Miaskowski et al., 2014).
Women in the current sample who received doxorubicin were more likely to be in the high moderate decreasing fatigue class when compared to the mild decreasing fatigue class. The effects of chemotherapy type on fatigue severity have been reported with inconsistent findings (Berger, 1998; Berger & Farr, 1999; de Jong et al., 2006). Although doxorubicin use had a significant effect on fatigue class membership in the current sample, whether that effect is dose-dependent or related to other agents received in combination with doxorubicin is unknown, and additional studies are needed.
Although days of missed work were not significantly associated with class membership, examination of the mean days of missed work for the three classes of fatigue severity suggests an upward trend in the number of days missed as fatigue severity increases. However, only 37% of the sample was employed. A larger cohort of employed participants may have revealed a significant relationship between these variables.
Increased hours spent lying down was associated with membership in the high moderate decreasing fatigue class when compared to the mild decreasing fatigue class during cycle 2 only, consistent with other studies (Berger & Farr, 1999; Berger & Higginbotham, 2000; de Jong et al., 2004; Downie et al., 2006). However, the upward trend and statistical association of hours spent lying down and fatigue severity class was not seen during cycle 3, and further examination with larger samples may better highlight this association.
Limitations
Particular care should be given to the nature of the data in the current study and the usefulness of LGMM in modeling symptom trajectories with daily reporting. In the identified models, and given the use of daily symptom severity reporting, more variability is likely within the classes than the presented growth factors adequately represent. In addition, many days for which women reported 0 severity on symptoms may have decreased the aggregate means for the growth factors. The current study was limited by a lack of data for several relevant variables of interest, including comorbidities, menopausal status, symptom management, and previous sleep patterns, and the inability to separate varying chemotherapy regimens because of sample size. The use of a single-item measure for symptom severity has limitations, including the risk of increased measurement error when compared to measures using multiple items. However, single-item measures are reliable and valid for collecting symptom data and minimize participant burden when monitoring multiple symptoms over time. In addition, the sample size was modest and the sample was fairly homogenous in demographic variables, including marital status and ethnicity. Although data were collected from multiple sites across the United States, findings may not generalize to all populations of women receiving initial treatment for breast cancer.
Implications for Nursing
The findings of the current study suggest that clinical practice must incorporate assessment and management of fatigue and disturbed sleep early during the course of chemotherapy. Recognizing the existence of a percentage of women who experience fatigue and disturbed sleep at moderate to severe levels across multiple cycles of chemotherapy is important, because not all women will need the same level of symptom management. The identified trajectory classes suggest that women who report an initial value of moderate or greater severity of fatigue or disturbed sleep may continue with the symptom. Many of the classes showed an improvement in trajectory, but not always to a mild level. In addition, the existence of increasing disturbed sleep class trajectories suggests that some women experienced a worsening in disturbed sleep. Clinicians should be aware that women who report an initial symptom severity at moderate to severe levels may benefit from increased symptom surveillance and management. This is particularly important because these women may be at increased risk for poorer outcomes, including decreased activity and missed work as in the current sample, as well as decreased quality of life and increased healthcare resource use (Beck et al., 2010; Bradley et al., 2007; Byar et al., 2006; Cleeland, 2000). Potential interventions for at-risk women may include patient and caregiver education regarding self-care, careful monitoring and assessment, and referral or pharmacologic intervention. Additional research should focus on determining whether these classes are replicable and stable across multiple cycles and continue to study potential antecedents of class membership, including sleep-related variables, comorbidities, and genetic and molecular factors (Miaskowski et al., 2014).
Conclusion
The current results suggest that women receiving chemotherapy for breast cancer experience distinct trajectories of severity of fatigue and disturbed sleep. Regardless of class membership, and except for a small percentage of women in the worsening disturbed sleep classes, severity of symptoms remained fairly stable or improved during the chemotherapy cycle. Additional research should focus on replication of the current study and identifying potential correlates of class membership to clarify which individuals are likely to experience severe fatigue and disturbed sleep during chemotherapy.
Knowledge Translation.
Fatigue and disturbed sleep occur at moderate to severe levels for a percentage of women throughout chemotherapy.
Women receiving chemotherapy for breast cancer experience distinct trajectories of severity of fatigue and disturbed sleep.
Clinicians should be aware that women who report an initial symptom severity on the first day of chemotherapy at moderate to severe levels may benefit from increased symptom surveillance and management.
Acknowledgments
Data used in this analysis were collected as part of National Institutes of Health (NIH)/Department of Health and Human Services (DHHS) (R01 CA8947) and NIH/DHHS (R01 CA120558). Whisenant was supported, in part, by a T32 Institutional Training Grant in Cancer, Aging, and End-of-Life Care (T32NR013456). Wong is supported by a grant from the NIH.
Footnotes
Whisenant, Beck, and Mooney completed the data collection. Whisenant, Wong, Mitchell, and Mooney provided the analysis. All authors contributed to the conceptualization and design, provided statistical support, and contributed to the manuscript preparation.
Contributor Information
Meagan Whisenant, Postdoctoral fellow in the Division of Internal Medicine, Department of Symptom Research, at the University of Texas MD Anderson Cancer Center in Houston.
Bob Wong, Research associate professor in the College of Nursing at the University of Utah in Salt Lake City.
Sandra A. Mitchell, Research scientist in the Outcomes Research Branch at the National Cancer Institute in Rockville, MD.
Susan L. Beck, Professor, College of Nursing at the University of Utah.
Kathi Mooney, Distinguished professor, College of Nursing at the University of Utah.
References
- Beck SL, Berger AM, Barsevick AM, Wong B, Stewart KA, Dudley WN. Sleep quality after initial chemotherapy for breast cancer. Supportive Care in Cancer. 2010;18:679–689. doi: 10.1007/s00520-009-0662-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bender CM, Ergÿn FS, Rosenzweig MQ, Cohen SM, Sereika SM. Symptom clusters in breast cancer across 3 phases of the disease. Cancer Nursing. 2005;28:219–225. doi: 10.1097/00002820-200505000-00011. [DOI] [PubMed] [Google Scholar]
- Berger AM. Patterns of fatigue and activity and rest during adjuvant breast cancer chemotherapy. Oncology Nursing Forum. 1998;25:51–62. [PubMed] [Google Scholar]
- Berger AM, Farr L. The influence of daytime inactivity and nighttime restlessness on cancer-related fatigue. Oncology Nursing Forum. 1999;26:1663–1671. [PubMed] [Google Scholar]
- Berger AM, Higginbotham P. Correlates of fatigue during and following adjuvant breast cancer chemotherapy: A pilot study. Oncology Nursing Forum. 2000;27:1443–1448. [PubMed] [Google Scholar]
- Bower JE, Ganz PA, Irwin MR, Kwan L, Breen EC, Cole SW. Inflammation and behavioral symptoms after breast cancer treatment: Do fatigue, depression, and sleep disturbance share a common underlying mechanism? Journal of Clinical Oncology. 2011;29:3517–3522. doi: 10.1200/JCO.2011.36.1154. https://doi.org/10.1200/jco.2011.36.1154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradley CJ, Neumark D, Luo Z, Schenk M. Employment and cancer: Findings from a longitudinal study of breast and prostate cancer survivors. Cancer Investigation. 2007;25:47–54. doi: 10.1080/07357900601130664. [DOI] [PubMed] [Google Scholar]
- Brant JM, Dudley WN, Beck S, Miaskowski C. Evolution of the dynamic symptoms model. Oncology Nursing Forum. 2016;43:651–654. doi: 10.1188/16.ONF.651-654. https://doi.org/10.1188/16.ONF.651-654. [DOI] [PubMed] [Google Scholar]
- Browall M, Persson LO, Ahlberg K, Karlsson P, Danielson E. Daily assessment of stressful events and coping among post-menopausal women with breast cancer treated with adjuvant chemotherapy. European Journal of Cancer Care. 2009;18:507–516. doi: 10.1111/j.1365-2354.2008.00994.x. [DOI] [PubMed] [Google Scholar]
- Browall MM, Ahlberg KM, Persson LO, Karlsson PO, Danielson EB. The impact of age on Health-Related Quality of Life (HRQoL) and symptoms among postmenopausal women with breast cancer receiving adjuvant chemotherapy. Acta Oncologica. 2008;47:207–215. doi: 10.1080/02841860701621258. https://doi.org/10.1080/02841860701621258. [DOI] [PubMed] [Google Scholar]
- Byar KL, Berger AM, Bakken SL, Cetak MA. Impact of adjuvant breast cancer chemotherapy on fatigue, other symptoms, and quality of life [Online exclusive] Oncology Nursing Forum. 2006;33:E18–E26. doi: 10.1188/06.ONF.E18-E26. https://doi.org/10.1188/06.ONF.E18-E26. [DOI] [PubMed] [Google Scholar]
- Cleeland CS. Cancer-related symptoms. Seminars in Radiation Oncology. 2000;10:175–190. doi: 10.1053/srao.2000.6590. [DOI] [PubMed] [Google Scholar]
- Cleeland CS, Bennett GJ, Dantzer R, Dougherty PM, Dunn AJ, Meyers CA, Lee BN. Are the symptoms of cancer and cancer treatment due to a shared biologic mechanism? A cytokine-immunologic model of cancer symptoms. Cancer. 2003;97:2919–2925. doi: 10.1002/cncr.11382. [DOI] [PubMed] [Google Scholar]
- Cleeland CS, Mendoza TR. Symptom measurement by patient report. In: Cleeland CS, Fisch MJ, Dunn AJ, editors. Cancer symptom science: Measurement, mechanisms, and management. New York, NY: Cambridge University Press; 2011. pp. 268–284. [Google Scholar]
- Colagiuri B, Christensen S, Jensen AB, Price MA, Butow PN, Zachariae R. Prevalence and predictors of sleep difficulty in a national cohort of women with primary breast cancer three to four months postsurgery. Journal of Pain and Symptom Management. 2011;42:710–720. doi: 10.1016/j.jpainsymman.2011.02.012. [DOI] [PubMed] [Google Scholar]
- Colder CR, Campbell RT, Ruel E, Richardson JL, Flay BR. A finite mixture model of growth trajectories of adolescent alcohol use: Predictors and consequences. Journal of Consulting and Clinical Psychology. 2002;70:976–985. doi: 10.1037//0022-006x.70.4.976. [DOI] [PubMed] [Google Scholar]
- de Jong N, Candel MJ, Schouten HC, Abu-Saad HH, Courtens AM. Prevalence and course of fatigue in breast cancer patients receiving adjuvant chemotherapy. Annals of Oncology. 2004;15:896–905. doi: 10.1093/annonc/mdh229. [DOI] [PubMed] [Google Scholar]
- de Jong N, Kester AD, Schouten HC, Abu-Saad HH, Courtens AM. Course of fatigue between two cycles of adjuvant chemotherapy in breast cancer patients. Cancer Nursing. 2006;29:467–477. doi: 10.1097/00002820-200611000-00007. [DOI] [PubMed] [Google Scholar]
- Dodd MJ, Cho MH, Cooper BA, Miaskowski C. The effect of symptom clusters on functional status and quality of life in women with breast cancer. European Journal of Oncology Nursing. 2010;14:101–110. doi: 10.1016/j.ejon.2009.09.005. https://doi.org/10.1016/j.ejon.2009.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Downie FP, Mar Fan HG, Houédé-Tchen N, Yi Q, Tannock IF. Cognitive function, fatigue, and menopausal symptoms in breast cancer patients receiving adjuvant chemotherapy: Evaluation with patient interview after formal assessment. Psycho-Oncology. 2006;15:921–930. doi: 10.1002/pon.1035. https://doi.org/10.1002/pon.1035. [DOI] [PubMed] [Google Scholar]
- Dunn LB, Cooper BA, Neuhaus J, West C, Paul S, Aouizerat B, Miaskowski C. Identification of distinct depressive symptom trajectories in women following surgery for breast cancer. Health Psychology. 2011;30:683–692. doi: 10.1037/a0024366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fortner BV, Stepanski EJ, Wang SC, Kasprowicz S, Durrence HH. Sleep and quality of life in breast cancer patients. Journal of Pain and Symptom Management. 2002;24:471–480. doi: 10.1016/s0885-3924(02)00500-6. [DOI] [PubMed] [Google Scholar]
- Gaston-Johansson F, Fall-Dickson JM, Bakos AB, Kennedy MJ. Fatigue, pain, and depression in pre-autotransplant breast cancer patients. Cancer Practice. 1999;7(5):240–247. doi: 10.1046/j.1523-5394.1999.75008.x. [DOI] [PubMed] [Google Scholar]
- Given B, Given C, Azzouz F, Stommel M. Physical functioning of elderly cancer patients prior to diagnosis and following initial treatment. Nursing Research. 2001;50:222–232. doi: 10.1097/00006199-200107000-00006. [DOI] [PubMed] [Google Scholar]
- Goldstein D, Bennett BK, Webber K, Boyle F, de Souza PL, Wilcken NR, Lloyd AR. Cancer-related fatigue in women with breast cancer: Outcomes of a 5-year prospective cohort study. Journal of Clinical Oncology. 2012;30:1805–1812. doi: 10.1200/JCO.2011.34.6148. [DOI] [PubMed] [Google Scholar]
- Green SB, Salkind NJ. Using SPSS for Windows and Macintosh: Analyzing and understanding data. 5th. Upper Saddle River, NJ: Pearson Prentice Hall; 2008. [Google Scholar]
- Huang HP, Chen ML, Liang J, Miaskowski C. Changes in and predictors of severity of fatigue in women with breast cancer: A longitudinal study. International Journal of Nursing Studies. 2014;51:582–592. doi: 10.1016/j.ijnurstu.2013.09.003. https://doi.org/10.1016/j.ijnurstu.2013.09.003. [DOI] [PubMed] [Google Scholar]
- Jacobsen PB, Hann DM, Azzarello LM, Horton J, Balducci L, Lyman GH. Fatigue in women receiving adjuvant chemotherapy for breast cancer: Characteristics, course, and correlates. Journal of Pain and Symptom Management. 1999;18:233–242. doi: 10.1016/s0885-3924(99)00082-2. [DOI] [PubMed] [Google Scholar]
- Janz NK, Mujahid M, Chung LK, Lantz PM, Hawley ST, Morrow M, Katz SJ. Symptom experience and quality of life of women following breast cancer treatment. Journal of Women’s Health. 2007;16:1348–1361. doi: 10.1089/jwh.2006.0255. https://doi.org/10.1089/jwh.2006.0255. [DOI] [PubMed] [Google Scholar]
- Jung T, Wickerama KA. An introduction to latent class growth analysis and growth mixture modeling. Social and Personality Psychology Compass. 2008;2:302–317. [Google Scholar]
- Kim HJ, Barsevick AM, Tulman L, McDermott PA. Treatment-related symptom clusters in breast cancer: A secondary analysis. Journal of Pain and Symptom Management. 2008;36:468–479. doi: 10.1016/j.jpainsymman.2007.11.011. [DOI] [PubMed] [Google Scholar]
- Kuo HH, Chiu MJ, Liao WC, Hwang SL. Quality of sleep and related factors during chemotherapy in patients with stage I/II breast cancer. Journal of the Formosan Medical Association. 2006;105:64–69. doi: 10.1016/S0929-6646(09)60110-8. https://doi.org/10.1016/S0929-6646(09)60110-8. [DOI] [PubMed] [Google Scholar]
- Lam WW, Bonanno GA, Mancini AD, Ho S, Chan M, Hung WK, Fielding R. Trajectories of psychological distress among Chinese women diagnosed with breast cancer. Psycho-Oncology. 2010;19:1044–1051. doi: 10.1002/pon.1658. https://doi.org/10.1002/pon.1658. [DOI] [PubMed] [Google Scholar]
- Langford DJ, Paul SM, Cooper B, Kober KM, Mastick J, Melisko M, Miaskowski C. Comparison of subgroups of breast cancer patients on pain and co-occurring symptoms following chemotherapy. Supportive Care in Cancer. 2016;24:605–614. doi: 10.1007/s00520-015-2819-1. [DOI] [PubMed] [Google Scholar]
- Lee J, Dibble SL, Pickett M, Luce J. Chemotherapy-induced nausea/vomiting and functional status in women treated for breast cancer. Cancer Nursing. 2005;28(4):249–255. doi: 10.1097/00002820-200507000-00002. [DOI] [PubMed] [Google Scholar]
- Liu L, Fiorentino L, Natarajan L, Parker BA, Mills PJ, Sadler GR, Ancoli-Israel S. Pre-treatment symptom cluster in breast cancer patients is associated with worse sleep, fatigue and depression during chemotherapy. Psycho-Oncology. 2009;18:187–194. doi: 10.1002/pon.1412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miaskowski C, Cooper BA, Melisko M, Chen LM, Mastick J, West C, Aouizerat BE. Disease and treatment characteristics do not predict symptom occurrence profiles in oncology outpatients receiving chemotherapy. Cancer. 2014;120:2371–2378. doi: 10.1002/cncr.28699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mooney KH, Beck SL, Friedman RH, Farzanfar R, Wong B. Automated monitoring of symptoms during ambulatory chemotherapy and oncology providers’ use of the information: A randomized controlled clinical trial. Supportive Care in Cancer. 2014;22:2343–2350. doi: 10.1007/s00520-014-2216-1. https://doi.org/10.1007/s00520-014-2216-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mooney KH, Beck SL, Wong B, Dunson W, Wujcik D, Whisenant M, Donaldson G. Automated home monitoring and management of patient-reported symptoms during chemotherapy. Cancer Medicine. 2017;6:537–546. doi: 10.1002/cam4.1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén B, Muthén LK. Integrating person-centered and variable-centered analyses: Growth mixture modeling with latent trajectory classes. Alcoholism, Clinical and Experimental Research. 2000;24:882–891. [PubMed] [Google Scholar]
- Nieboer P, Buijs C, Rodenhuis S, Seynaeve C, Beex LV, van der Wall E, de Vries EG. Fatigue and relating factors in high-risk breast cancer patients treated with adjuvant standard or high-dose chemotherapy: A longitudinal study. Journal of Clinical Oncology. 2005;23:8296–8304. doi: 10.1200/JCO.2005.10.167. https://doi.org/10.1200/jco.2005.10.167. [DOI] [PubMed] [Google Scholar]
- Payne J, Piper B, Rabinowitz I, Zimmerman B. Biomarkers, fatigue, sleep, and depressive symptoms in women with breast cancer: A pilot study. Oncology Nursing Forum. 2006;33:775–783. doi: 10.1188/06.ONF.775-783. [DOI] [PubMed] [Google Scholar]
- Singer JD, Willett JB. Applied longitudinal data analysis. New York, NY: Oxford University Press; 2003. [Google Scholar]
- Sitzia J, Huggins L. Side effects of cyclophosphamide, methotrexate, and 5-fluorouracil (CMF) chemotherapy for breast cancer. Cancer Practice. 1998;6:13–21. doi: 10.1046/j.1523-5394.1998.1998006013.x. [DOI] [PubMed] [Google Scholar]
- So WK, Marsh G, Ling WM, Leung FY, Lo JC, Yeung M, Li GK. The symptom cluster of fatigue, pain, anxiety, and depression and the effect on the quality of life of women receiving treatment for breast cancer: A multicenter study [Online exclusive] Oncology Nursing Forum. 2009;36:E205–E214. doi: 10.1188/09.ONF.E205-E214. [DOI] [PubMed] [Google Scholar]
- Tchen N, Juffs HG, Downie FP, Yi QL, Hu H, Chemerynsky I, Tannock IF. Cognitive function, fatigue, and menopausal symptoms in women receiving adjuvant chemotherapy for breast cancer. Journal of Clinical Oncology. 2003;21:4175–4183. doi: 10.1200/JCO.2003.01.119. [DOI] [PubMed] [Google Scholar]
- Van Onselen C, Cooper BA, Lee K, Dunn L, Aouizerat BE, West C, Miaskowski C. Identification of distinct subgroups of breast cancer patients based on self-reported changes in sleep disturbance. Supportive Care in Cancer. 2012;20:2611–2619. doi: 10.1007/s00520-012-1381-3. [DOI] [PubMed] [Google Scholar]
- Von Ah D, Kang DH. Correlates of mood disturbance in women with breast cancer. Journal of Advanced Nursing. 2008;61:676–689. doi: 10.1111/j.1365-2648.2007.04563.x. [DOI] [PubMed] [Google Scholar]
- Von Ah DM, Kang DH, Carpenter JS. Predictors of cancer-related fatigue in women with breast cancer before, during, and after adjuvant therapy. Cancer Nursing. 2008;31:134–144. doi: 10.1097/01.NCC.0000305704.84164.54. [DOI] [PubMed] [Google Scholar]


