Abstract
Objective
To investigate whether virtual autopsy with postmortem CT (PMCT) improves clinical diagnosis of the immediate cause of death.
Design
Retrospective observational cohort study. Inclusion criteria: inhospital and out-of-hospital deaths over the age of 1 year in whom virtual autopsy with PMCT and conventional autopsy were performed. Exclusion criteria: forensic cases, postmortal organ donors and cases with incomplete scanning procedures. Cadavers were examined by virtual autopsy with PMCT prior to conventional autopsy. The clinically determined cause of death was recorded before virtual autopsy and was then adjusted with the findings of virtual autopsy. Using conventional autopsy as reference standard, we investigated the increase in sensitivity for immediate cause of death, type of pathology and anatomical system involved before and after virtual autopsy.
Setting
Tertiary referral centre.
Participants
86 cadavers that underwent conventional and virtual autopsy between July 2012 and June 2016.
Intervention
PMCT consisted of brain, cervical spine and chest–abdomen–pelvis imaging. Conventional autopsy consisted of thoracoabdominal examination with/without brain autopsy.
Primary and secondary outcome measures
Increase in sensitivity for the immediate cause of death, type of pathology (infection, haemorrhage, perfusion disorder, other or not assigned) and anatomical system (pulmonary, cardiovascular, gastrointestinal, other or not assigned) involved, before and after virtual autopsy.
Results
Using PMCT, the sensitivity for immediate cause of death increased with 12% (95% CI 2% to 22%) from 53% (41% to 64%) to 64% (53% to 75%), with 18% (9% to 27%) from 65% (54% to 76%) to 83% (73% to 91%) for type of pathology and with 19% (9% to 30%) from 65% (54% to 76%) to 85% (75% to 92%) for anatomical system.
Conclusion
While unenhanced PMCT is an insufficient substitute for conventional autopsy, it can improve diagnosis of cause of death over clinical diagnosis alone and should therefore be considered whenever autopsy is not performed.
Keywords: cause of death, postmortem, computed tomography, autopsy, sensitivity, specificity
Strengths and limitations of this study.
This study investigated the diagnostic performance for clinical cause of death determination by use of postmortem CT and takes into account the added value over clinical diagnosis alone.
The immediate cause of death (ie, direct cause of death) was the main outcome rather than the primary cause of death (ie, underlying cause of death or basic illness) as from a clinical point of view, diagnosis and treatment of the immediate cause of death is the most urgent.
The sensitivity for clinical cause of death determination, with and without postmortem CT, is investigated on multiple levels of precision; the immediate cause of death as well as the involved type of pathology and anatomical location were investigated.
The retrospective design in a tertiary care centre has probably introduced a selection bias towards patients with diagnostic difficulties or unresolved issues, resulting in an underestimation of the diagnostic performance compared with more general causes of death.
An unexpected low consent rate for postmortem CT in cases with consent for conventional autopsy resulted in a reduction of the statistical power of this study.
Introduction
Autopsies are traditionally regarded as the ‘gold standard’ in quality monitoring of healthcare. It is therefore remarkable that in a time of heightened interest in improving patient safety, healthcare quality and error prevention, worldwide autopsy rates continue to decline from roughly 40% in the 1960s to below 10% nowadays.1–7 Religious and emotional objections to the invasiveness of conventional autopsies, both by the relatives and the doctors, are considered as some of the reasons given for this decline. At present, determination of the cause of death relies heavily on clinical assessment. Despite an increase in the use and improvement of diagnostic techniques in the last decades, major error rates of approximately 25% have not substantially decreased.8–10 According to the Goldman classification system, major errors are defined as clinically missed diagnoses related to the cause of death. In half of these cases, this might have led to a change in therapy and prolonged survival, if known before death.8
National mortality statistics are generally based on the primary cause of death (ie, underlying cause or basic illness), which could be a long-standing, chronic disease.11 However, from an individual and clinical point of view, diagnosis and treatment of the immediate cause of death (ie, direct cause of death) is the most urgent. Accuracy rates for immediate causes of death are probably lower than for underlying causes of death,12 13 due to time constraints of the often acute situations these diagnoses present with. The high error rates emphasise the need to improve clinical diagnoses using techniques that are widely available and acceptable, for example, postmortem CT (PMCT). Previous studies have shown that as yet, PMCT is an insufficient substitute but can be used in adjunct to conventional autopsy.14 15 In order to provide answers and quality control also in cases without consent for conventional autopsy, we investigated whether virtual autopsy with PMCT improves clinical diagnosis of the immediate cause of death.
Material and methods
Study design
All cadavers of inhospital and out-of-hospital deaths over the age of 1 year, who underwent both PMCT and conventional autopsy in our hospital, between July 2012 and June 2016, were included. Forensic cases, postmortal donors and cases with incomplete scanning procedures or without full thorax-abdomen autopsy were excluded. Clinicians had to ask consent from relatives for both PMCT and conventional autopsy in all cases of death.
PMCT and conventional autopsy
PMCT was performed as soon as possible after death and prior to autopsy. If scanning within a few hours was not possible, the cadaver was stored in the mortuary at 4°C. CT scanners used were Siemens Somatom Sensation 16, Siemens Sensation 64 (Siemens Healthcare, Germany) and Aquilion ONE (Toshiba Medical Systems, Japan), all with a detector collimation of 1 mm, reconstruction interval of 0.8 mm and 120 kV. The Siemens scanners used a tube current of 400 mA and 1 s rotation time. The Toshiba scanner used Automatic Exposure Control (SD 17.5) with a rotation time of 0.5 s. PMCT protocol consisted of a scan of the head and neck, in bone, soft tissue and cerebral setting, interpreted by a neuroradiologist; a scan of thorax and abdomen in bone, lung and abdominal settings, interpreted by a specialist cardiothoracic and abdominal radiologist; summarised in a single consensus report. All radiologists had minimal previous experience in interpreting PMCT images, as postmortem imaging is a relatively new field of expertise. Conventional autopsy consisted of thoracic-abdominal autopsy with or without examination of the brain, and included full macroscopic and microscopic inspection. Radiologists and pathologists were blinded to each other’s results, but had otherwise full access to electronic patient files. Radiologists and pathologists compiled a report based on their own findings and clinical findings.
Data collection
For each cadaver, the immediate cause of death (ie, direct cause of death), type of pathology and anatomical system involved were collected in retrospect at three moments: before PMCT, after PMCT and based on conventional autopsy findings. The cause of death before virtual autopsy was based on clinical findings only. The cause of death after virtual autopsy was based on both clinical findings and PMCT. If no cause of death could be assigned at PMCT, the cause of death was primarily based on clinical findings. Symptoms (eg, respiratory failure, sepsis, etc) and risk factors (atherosclerosis, hypertension) were not considered as cause of death. Only when the primary source of sepsis (eg, pneumonia) was unknown, sepsis was diagnosed as cause of death. In cases of trauma, the physical injury rather than the mechanism of trauma was assigned as cause of death.
Type of pathology was scored according to the following categories: infection, haemorrhage, perfusion disorder, other or not assigned. Perfusion disorders comprised all cardiac and vascular perfusion disorders not due to infection, haemorrhage or neoplasm (eg, myocardial infarction, heart failure, pulmonary embolism, volvulus, etc). Type A aortic dissections with haemopericardium were grouped in the haemorrhage category. The type of anatomical system was scored as pulmonary, cardiovascular, gastrointestinal, other or not assigned. This strategy and subcategories used were derived from the classification of anatomical regions and groups of pathologies as used by Roberts et al 14 and Wichmann et al.4
Statistical analysis
Cases where the cause of death, type of pathology or anatomical system could not be established after conventional autopsy were excluded from statistical analysis. Sensitivity and specificity were calculated with conventional autopsy as reference standard. 95% confidence intervals (CI) for the difference in proportions before and after PMCT were calculated.16 A sample size of n=113 was required to demonstrate a difference of 15% in sensitivity with α=0.05 and β=0.10. Logistic regression analysis was performed to evaluate radiologists’ improvement in reporting PMCT scans during the 4-year study period. ORs were calculated for each additional year of experience in reporting PMCT scans. P values of 0.05 or less were considered significant. IBM SPSS Statistics V.22 was used.
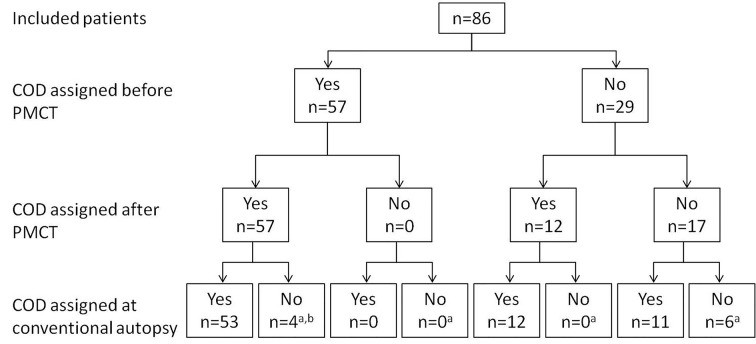
Results
Of 2155 clinically examined inhospital and out-of-hospital deaths in our hospital, a full thorax-abdomen autopsy was performed on 304 (14%) cadavers, a complete PMCT on 120 (6%) cadavers and both on 78 (4%) cadavers. One case was excluded due to postmortem organ donation prior to PMCT. A further nine cases who deceased at home (n=7) or in another hospital (n=2) were brought to the hospital’s mortuary for PMCT and autopsy examination. This led to a total of 86 included cases (51 men, 35 women, with a median age of 62 (IQR: 47 to 74) years (table 1). Fifty-four per cent of the deaths were after a resuscitation attempt. The median postmortem interval between death and PMCT was 7.6 (IQR 3.1 to 18.8) hours. In 69%, there was no consent for brain autopsy and, in those cases, conventional autopsy consisted of a thorax-abdomen examination only. Conventional autopsy, as standard of reference, was not able to assign the immediate cause of death in 10 cadavers (12%) (figure 1). Both the type of pathology and anatomical system involved were not assigned in eight cadavers. Therefore, analyses were based on the remaining 76 or 78 cadavers. Table 2 shows two-by-two tables of the number of correct diagnoses before and after PMCT.
Table 1.
Patient characteristics
| Study population (n=86), n (%) | |
| Sex | |
| Male | 51 (59) |
| Female | 35 (41) |
| Age, median (IQR) | 62 (47–74) |
| Place of death | |
| Emergency room | 31 (36) |
| Intensive care unit | 30 (35) |
| Clinical ward | 18 (21) |
| Out of hospital | 7 (8) |
| CPR performed | |
| Yes | 46 (53) |
| No | 40 (47) |
| Brain autopsy performed | |
| Yes | 27 (31) |
| No | 59 (69) |
| Immediate cause of death | |
| Infectious | 26 (30) |
| Perfusive disorder | 32 (37) |
| Haemorrhage | 13 (15) |
| Other | 5 (6) |
| Uncertain | 10 (12) |
CPR, cardiopulmonary resuscitation.
Figure 1.
Flow chart of whether or not an immediate cause of death could be assigned before and after PMCT and during conventional autopsy. aNo cause of death could be assigned at autopsy in 10 cases, and were excluded from the sensitivity analysis for cause of death. bIn four cases, where clinicians and radiologists were able to assign a cause of death, autopsy did not reveal the cause of death. In one case, this was due to lack of consent to a brain autopsy in a case with an intracerebral haemorrhage. In another case, the pulmonary embolisms were not diagnosed at autopsy, but identified with ultrasonography during resuscitation as well as on PMCT (figure 2). In two other cases with unknown cause of death at autopsy, aspiration and cardiac failure were diagnosed as the cause of death after imaging, whereas previously sepsis with unknown abdominal focus and myocardial infarction were diagnosed by the clinicians. COD, immediate cause of death; PMCT, postmortem CT.
Table 2.
Cross tabulations of correct and incorrect assigned immediate COD (A), type of pathology (B) and anatomical system (C), before and after PMCT
| (A) | COD after PMCT | |||
| Correct | Incorrect | |||
| COD before PMCT | Correct | 36 | 4 | 40 |
| Incorrect | 13 | 23 | 36 | |
| 49 | 27 | 76 | ||
| (B) | Type of pathology after PMCT | |||
| Type of pathology before PMCT | Correct | 50 | 1 | 51 |
| Incorrect | 15 | 12 | 27 | |
| 65 | 13 | 78 | ||
| (C) | Type of anatomical system after PMCT | |||
| Type of anatomical system before PMCT | Correct | 48 | 3 | 51 |
| Incorrect | 18 | 9 | 27 | |
| 66 | 12 | 78 | ||
COD, immediate cause of death; PMCT, postmortem CT.
Sensitivity for immediate cause of death
The overall sensitivity for immediate cause of death increased with 12% (2% to 22%) from 53% (41% to 64%) to 64% (53% to 75%) after performing a PMCT scan. Sensitivities specified per type of pathology or anatomical system are shown in table 3. All autopsy causes of death, and whether or not they were correctly appointed before and after PMCT, are shown in table 4.
Table 3.
Sensitivity for immediate cause of death before and after virtual autopsy with PMCT
| Sensitivity | |||
| Before PMCT (95% CI) | After PMCT (95% CI) | Difference (95% CI) | |
| Immediate cause of death (n=76)* | 53% (41 to 64) | 64% (53 to 75) | 12% (2 to 22) |
| Per subgroup of type of pathology | |||
| Infection (n=26) | 65% (44 to 83) | 69% (48 to 86) | 4% (–16 to 24) |
| Haemorrhage (n=13) | 69% (39 to 91) | 85% (55 to 98) | 15% (–4 to 35) |
| Perfusion disorder (n=32) | 31% (16 to 50) | 47% (29 to 65) | 16% (0 to 31) |
| Other (n=5) | 80% (28 to 99) | 100% (48 to 100) | 20% (–15 to 55) |
| Per subgroup of anatomical system | |||
| Pulmonary (n=18) | 56% (31 to 78) | 67% (41 to 87) | 11% (–3 to 26) |
| Cardiovascular (n=37) | 43% (27 to 61) | 54% (37 to 71) | 11% (–4 to 25) |
| Gastrointestinal (n=13) | 54% (25 to 81) | 85% (55 to 98) | 31% (–2 to 64) |
| Other (n=8) | 88% (47 to 100) | 75% (35 to 97) | –13% (–35 to 10) |
*Conventional autopsy was not able to establish a cause of death in 10 cases.
PMCT, postmortem CT.
Table 4.
Overview of all COD diagnosed at autopsy, classified by type pathology and whether they were correctly diagnosed as the immediate COD before and after virtual autopsy
| Correct COD, both before and after PMCT | Incorrect COD before PMCT. Correct COD after PMCT | Correct COD before PMCT. Incorrect COD after PMCT | Incorrect COD, both before and after PMCT | |
| Infections | 10× pneumonia 1× infected liver cysts 1× sepsis e.c.i.† 1× pancreatitis 1× cholecystitis/cholangitis |
1× pneumonia 2× peritonitis* 1× diverticulitis and pancreatitis |
1× endocarditis 1× HSV hepatitis 1× cerebral aspergillosis |
4× pneumonia 1× endocarditis / pericarditis |
| Perfusion disorders | 7× myocardial infarction 1× heart failure 1× pulmonary embolism |
2× pulmonary embolism 2× arrhythmia 1× volvulus 1× heart failure |
1× heart failure | 9× myocardial infarction 3× arrhythmia 2× heart failure 1× pulmonary veno-occlusive disease 1× bowel ischaemia due to adhesions |
| Haemorrhages | 4× type A aortic dissection 1× subarachnoid haemorrhage 1× gastric haemorrhage 1× arteria carotis haemorrhage 1× arteria iliaca communis sinistra haemorrhage 1× haemorrhage from fistula; gastric tube versus aorta |
1× type A aortic dissection 1× haemothorax+ intrapulmonary haemorrhage |
1× haemothorax 1× liver and kidney rupture+ haemothorax |
|
| Other | 1× pleural carcinomatosis 1× cachexia 1× anaphylaxis 1× (auto-)intoxication |
1× epileptic seizure due to brain metastases |
*Peritonitis was due to a misplaced gastrostomy button in one case, and due to a misplaced ventriculoperitoneal drain in another case.
†Sepsis e causa ignota.
COD, immediate cause of death; PMCT, postmortem CT.
Pneumonia was the most common infectious cause of death. It was correctly assigned as cause of death in 11/15=73% after PMCT, compared with 10/15=67% before PMCT. In the other 27% (n=4), pneumonia was recognised, but not assigned as cause of death. Vice versa, in two other patients who had died from cerebral aspergillosis and heart failure, the ancillary pneumonia was incorrectly assigned as cause of death on PMCT. Furthermore, two cases of peritonitis (due to a misplaced gastrostomy button and ventriculoperitoneal drain) and one pancreatitis which were clinically missed (ie, major errors) were correctly diagnosed at PMCT as cause of death.
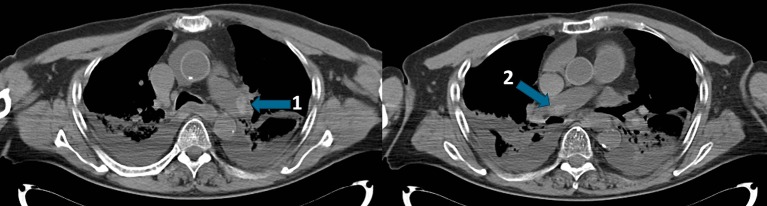
In the group of perfusion disorders, all three pulmonary embolisms diagnosed at autopsy were also assigned as cause of death at PMCT. In a further three cases, including one with pulmonary embolism diagnosis on antemortem ultrasound (figure 2), PMCT diagnosed pulmonary embolisms which were not confirmed during autopsy. Moreover, radiologists correctly diagnosed two arrhythmias, one heart failure and one volvulus which were initially missed as cause of death by the clinicians. Cardiac arrhythmia was suspected based on left ventricular hypertrophy and aortic valve stenosis or local hyperdensity of myocardial tissue corresponding to fibrosis in the absence of other significant findings. In the other case, heart failure was also based on the presence of secondary characteristics (dilated atria and pleural effusion) in the absence of other significant findings. Myocardial infarction was correctly diagnosed as cause of death in 7/16=44% after PMCT. However, in 5/7=71% of these cases, the myocardial infarction was not directly visible on PMCT and was based on the combination of clinical findings and absence of significant pathologies at PMCT. In the two other cases, imaging was suspect for myocardial infarction: once due to an intravascular hypodensity proximal of a coronary stent, which might indicate a (fat) embolism, and once due to the combination of significant coronary calcifications, enlarged right atrium, clinical history and absence of other significant findings.
Figure 2.
Example where pulmonary embolisms were diagnosed at antemortem ultrasound and postmortem CT but were not confirmed during autopsy. This patient died after a resuscitation attempt, 3 days after re-laparotomy due to a hernia cicatricalis correction with invagination complications. An ultrasound scan during resuscitation revealed pulmonary embolisms. Postmortem CT (postmortem interval of 2 hours) confirmed embolisms in the left (1) and right (2) pulmonary arteries. Autopsy did not assign a cause of death.
Using PMCT, haemorrhagic causes of death were correctly diagnosed in 11/13=85%. All five aortic dissections were correctly diagnosed on PMCT, including a clinically missed dissection. In a traumatic case, radiologists diagnosed haemothorax and a spleen rupture where pathologists diagnosed haemothorax and a liver and kidney rupture (figure 3). In another traumatic case where death was attributed to haemorrhagic shock due to haemothorax, radiologists diagnosed an air embolus in the left coronary artery (figure 4).
Figure 3.
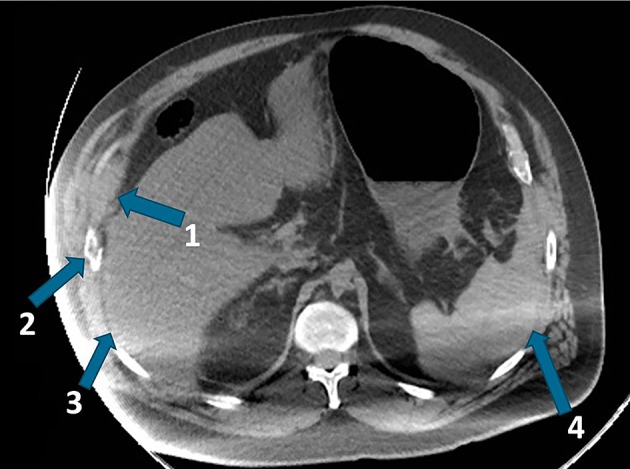
Example of discrepant diagnosis of the cause of traumatic exsanguination. This patient died after a resuscitation attempt following a scooter accident with impact on the right side. Initial trauma screening revealed no significant pathologies. Postmortem CT suggested exsanguinations due to a spleen laceration. Autopsy diagnosed exsanguinations due to lacerations of the liver and right kidney. Further findings are (1) abdominal wall haematoma, (2) rib fracture, (3) small rim of blood along the liver and (4) intra-abdominal blood along the spleen.
Figure 4.

An example that gas-related diagnoses can be more confidently diagnosed with PMCT than autopsy. This patient died during a midtransport resuscitation attempt following a car accident. Initial clinical examination found a haemothorax; however, it was unclear if the patient died due to blood loss or from some other underlying pathology which may have caused the accident. During air ambulance transportation, ventricular fibrillation occurred. PMCT showed an air embolus in the left anterior descending artery (1), probably due to extensive lung trauma and the decrease in atmospheric pressure during the flight. This was not diagnosed at autopsy, with death being attributed to a haemorrhagic shock due to haemothorax. Also, the pneumothorax, pneumopericardium and pneumomediastinum were not mentioned in the autopsy report. PMCT, postmortem CT.
In the category of other pathologies, there were three patients who died from malignant disease. The cause of death was correctly diagnosed before and after PMCT in two of these cases, one with pleural carcinomatosis in breast cancer and one with respiratory failure due to cachexia in metastasised oesophageal cancer. In the other case, the patient died after an epileptic seizure due to (unidentified) brain metastases. There were three other cases with cancer at time of death died, but those patients died from complications (septic cholecystitis, carotid artery bleeding and endocarditis due to immunodeficiency).
Sensitivity and specificity for type of pathology and anatomical system involved in the immediate cause of death
The overall sensitivity for type of pathology increased with 18% (9% to 27%) from 65% (54% to 76%) to 83% (73% to 91%) and with 19% (9% to 30%) from 65% (54% to 76%) to 85% (75% to 92%) for the anatomical system (table 5). These improvements were statistically significant. In the subgroups of cardiovascular causes and perfusion disorders as cause of death, where the sensitivity for immediate cause of death was rather low, we observed significant improvements of 21% (6% to 35%) and 21% (5% to 36%) for the identification of the involved anatomical system and type of pathology, respectively. This illustrates that PMCT can indicate a cardiovascular or perfusive cause of death, even in cases when the exact cause of death within that subgroup cannot be differentiated. There were no significant differences in specificity within the subgroups before and after PMCT.
Table 5.
Sensitivity and specificity for type of pathology and anatomical system diagnosed before and after virtual autopsy with PMCT
| Sensitivity | Specificity | |||||
| Before PMCT (95% CI) |
After PMCT (95% CI) |
Difference (95% CI) |
Before PMCT (95% CI) |
After PMCT (95% CI) |
Difference (95% CI) |
|
| A. Type of pathology (n=78)* | 65% (54 to 76) | 83% (73 to 91) | 18% (9 to 27) | N/A | N/A | |
| Per subgroup | ||||||
| Infection (n=26) | 69% (48 to 86) | 85% (65 to 96) | 15% (2 to 29) | 96% (87 to 100) | 92% (81 to 98) | −4% (−9 to 1) |
| Haemorrhage (n=13) | 69% (39 to 91) | 92% (64 to 100) | 23% (0 to 46) | 9% (92 to 100) | 100% (94 to 100) | 2% (−1 to 5) |
| Perfusion disorder (n=34) | 56% (38 to 73) | 76% (59 to 89) | 21% (5 to 36) | 95% (85 to 99) | 93% (81 to 99) | −2% (−12 to 87) |
| Other (n=5) | 100% (48 to 100) | 100% (48 to 100) | 0% (0 to 0) | 99% (93% to 100%) | 99% (93% to 100%) | 0% (0 to 0) |
| B. Anatomical system (n=78)* | 65% (54 to 76) | 85% (75 to 92) | 19% (9 to 30) | N/A | N/A | |
| Per subgroup | ||||||
| Pulmonary (n=18) | 72% (47 to 90) | 89% (65 to 99) | 17% (−1 to 34) | 95% (86 to 99) | 95% (86 to 99) | 0% (−8 to 8) |
| Cardiovascular (n=39) | 62% (45 to 77) | 82% (66 to 92) | 21% (6 to 35) | 100% (91 to 100) | 95% (82 to 99) | −5% (−12 to 2) |
| Gastrointestinal (n=13) | 54% (25 to 81) | 85% (55 to 98) | 31% (−2 to 64) | 98% (92 to 100) | 100% (94 to 100) | 2% (−1 to 5) |
| Other (n=8) | 88% (48 to 100) | 88% (48 to 100) | 0% (−35 to 35) | 97% (90 to 100) | 94% (86 to 98) | −3% (−7 to 1) |
*Autopsy was not able to establish the involved type of pathology and anatomical system in eight cases.
N/A, not applicable; PMCT, postmortem CT.
Performance of radiologists
Logistic regression analysis showed no significant improvement in the performance of radiologists in assigning the correct cause of death over the 4-year study period. ORs for each year of additional experience in reporting PMCT scans were 0.85 (95% CI 0.56 to 1.27, P=0.41) for correct assignment of the immediate cause of death, 0.95 (95% CI 0.61 to 1.48, P=0.81) for type of pathology and 0.82 (95% CI 0.51 to 1.32, P=0.41) for anatomical system involved.
Discussion
The sensitivity for immediate cause of death increased from 53% to 64% after performing PMCT. Analyses showed that the value of PMCT is variable per subcategory and depends on the cause of death. Unfortunately, subgroups were a lot smaller than expected, resulting in a lower statistical power and large CIs. We had predicted to include 272 cases (4 years of inclusion × average 80 thoracoabdominal autopsies each year × 0.85 PMCT consent rate). The main reason for the limited number of included patients was the unexpected low consent rate (78/304=26%) for PMCT in cases with consent for conventional autopsy. We did not investigate the reason for this low consent rate as motives for performing or not performing a PMCT scan were not extensively documented. In case of death, clinicians had to ask consent for both PMCT and autopsy. Though some clinicians mentioned that they only requested for PMCT in case of refusal of conventional autopsy.
Pneumonia was the most common missed infectious cause of death, both before and after PMCT. Resuscitation induced changes and normal postmortem changes, such as the occurrence of pulmonary oedema, could mask pneumonia (figure 5).17 In the subgroup of perfusion disorders, diagnosis of pulmonary embolism at unenhanced PMCT is challenging as it is notoriously difficult to distinguish an antemortem thrombus from a postmortem blood clot.18–20 This, or the possibility that the embolus was lost during the autopsy procedure, may explain why in three cases the pulmonary embolism was not confirmed during autopsy. Postmortem angiography, now being developed and validated, can be effective in demonstrating any obstructing thrombi.21 Most causes of death in the subgroup of perfusion disorders were cardiac related. Clinicians are often restricted in their ability to differentiate a cause of death due to the acute nature and time constraints of the situations (resuscitation setting) these patients present with. On the contrary, cardiac arrhythmia and heart failure are impossible to diagnose by postmortem examinations only. Furthermore, an autopsy can only detect a myocardial infarction in cases where patients have survived 2 to 3 hours postinfarction.22 Therefore, radiologists and pathologists had access to clinical information in order to assign the most probable cause of death based on postmortem findings and clinical findings as well. Accordingly, both PMCT and autopsy could indicate a cardiac cause of death, based on clinical findings and secondary characteristics observed during postmortem examination in the absence of other significant pathologies.
Figure 5.
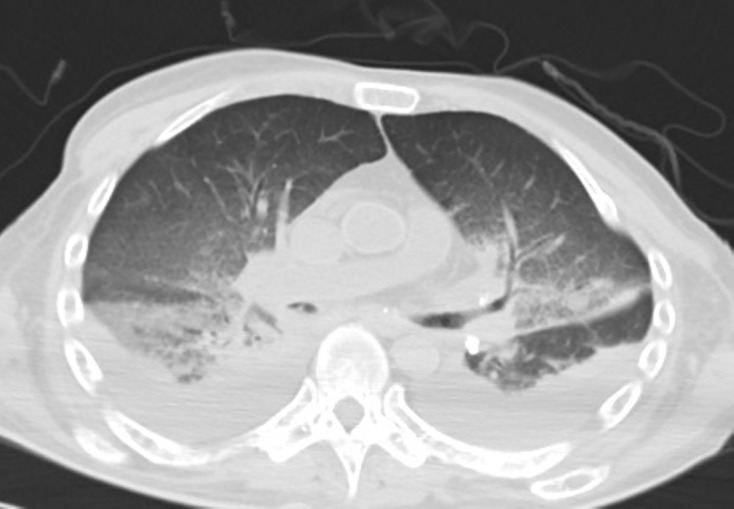
Normal postmortem changes could mask underlying pathology This patient had a clinical history of allogeneic stem cell transplantation due to multiple myeloma. Clinical examination and antemortem MRI of the brain suggested a post-transplant lymphoproliferative disorder (PTLD). Autopsy diagnosed bronchopneumonia (left upper lobe and right lower lobe) as the cause of death and did not show PTLD, nor recurrence of multiple myeloma or other malignancy. PMCT showed pleural fluid and interstitial pulmonary oedema, which were interpreted as normal postmortem findings. Bronchopneumonia was not diagnosed at PMCT. PMCT, postmortem CT.
Tables 3 and 5 show an increase in overall sensitivity from 64% to 83 or 85% when PMCT is used for identification of the type of pathology or anatomical system involved rather than for assigning the exact immediate cause of death. This indicates that even when the cause of death is uncertain after PMCT, it is still a valuable tool in targeting the region of interest or excluding some of the differential diagnostic possibilities. Clinical evaluation of the cause of death often indicates the failing system (eg, respiratory failure) rather than the underlying illness or structural changes, whereas radiologists appear to be more adept at ascertaining the involved anatomical system. Based on how confident radiologists are of their findings, they can guide the pathologist to the region(s) of interest. Among non-invasive techniques, Blokker et al 15 concluded that PMCT in combination with postmortem MRI yields the highest diagnostic performance in adults, with PMCT performing somewhat better when only one of the modalities is used.14 PMCT is less expensive than a conventional autopsy; however, cost-effective analyses have not been formulated.23 Images can be stored digitally (useful for legal or educational purposes) and results can be audited and promptly reviewed by one or more radiologists. Among minimally invasive methods, the highest performance is reported in studies combining PMCT and CT angiography. PMCT, enhanced with targeted coronary angiography, showed a sensitivity of 92% for cause of death.20 Two studies combining CT, CT angiography and CT-guided tissue biopsies achieved a pooled sensitivity of 91% for cause of death.24 25
To our knowledge, this is the second study which has investigated the additional value of unenhanced PMCT compared with clinical diagnoses. The first study by Inai et al 26 showed a significant increase in sensitivity from 46% to 74% for the immediate cause of death in 50 non-forensic deaths. This is somewhat higher than we found in our study, one reason could be the fact that less specific causes of death were used. Other previous studies have investigated the diagnostic accuracy of PMCT compared with autopsy and not to clinical diagnoses. Those studies are difficult to compare, as some use broadly defined categorisations and others use well-defined specific causes of death, or some use the immediate cause of death and others the intermediate or underlying cause of death, or do not state their definition of cause of death at all. Furthermore, most previous studies consisted of small sample sizes (n<50) and used different study populations, different outcome parameters (eg, cause of death, major or minor diagnoses) and different parameters of accuracy.4 27–29 A large prospective study of 182 adult deaths by Roberts et al 14 showed a major discrepancy rate of 32% in determining the cause of death with PMCT compared with autopsy. Another study showed a sensitivity of 82% and a specificity of 97% for PMCT regarding the categorisation of cause death in 101 cases.30 This is in accordance with our results regarding the categorisation of cause of death per type of pathology or anatomical system. Westphal et al 27 showed a sensitivity of 18/27=67% for cause of death and a sensitivity of 5/17=19% for a more specific description of the involved pathogenetic mechanism. Takahashi et al 28 found a sensitivity of 12% for definite findings and 53% for both definite and possible findings with PMCT as to cause of death. The study by Puranik et al 29 supports our results regarding the difficulty in diagnosing cardiac causes of death with unenhanced PMCT. A sensitivity of 25% for cause of death was found in a population of 17 young patients with sudden cardiac death.
Certain diagnoses, for example, fractures or those related to the accumulation of gasses or air (figure 4), are more confidently diagnosed with PMCT than autopsy.14 31 Therefore, the presented performance of PMCT will probably be underestimated in cases were pathologies are difficult to confirm due to the limitations of autopsy. Generally, in our experience we find that autopsy can no longer be considered as the gold standard for all postmortem diagnoses, due to the limitations of dissection, and due to the decline in the number of autopsies performed, leading to a decrease in pathologists’ expertise. We would suggest a gold standard involving a multidisciplinary consensus evaluation among clinicians, radiologists and pathologists. Prospective studies with larger sample sizes are required to investigate the additional value of PMCT in specific subgroups of causes of death. Even with the aid of improved non-minimally or minimally invasive techniques, conventional autopsy will still be required in complex cases where clinical and radiological diagnosis as to cause of death is inconclusive.
Conclusion
While virtual autopsy with PMCT is an insufficient substitute for conventional autopsy, it can improve diagnosis of the cause of death over clinical diagnosis alone. Even in cases where no immediate cause of death can be assigned after virtual autopsy, radiologists may indicate a region of interest, so directing pathologists at autopsy. Future studies are needed to investigate whether PMCT is able to reduce the invasiveness of autopsy or even avoid an autopsy altogether.
Supplementary Material
Footnotes
Contributors: LJPS had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. LJPS acquired and analysed the data. LJPS, WMK, BK and MP interpreted the data. LJPS drafted the manuscript. WMK and MP supervised the study. LJPS, WMK and MP contributed to the overall conception and design of the study. All authors revised the manuscript for intellectual content.
Funding: This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Disclaimer: The lead author affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Competing interests: None declared.
Patient consent: Parental/guardian consent obtained.
Ethics approval: This retrospective study was approved by the local ethical committee in the form of a waiver in accordance with Dutch national law.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Details on how to obtain additional data from the study (eg, statistical code, datasets) are available from the corresponding author.
References
- 1.Harrington DE, Sayre EA. Managed care and measuring medical outcomes: did the rise of HMOs contribute to the fall in the autopsy rate? Soc Sci Med 2010;70:191–8. 10.1016/j.socscimed.2009.09.018 [DOI] [PubMed] [Google Scholar]
- 2.Blokker BM, Weustink AC, Hunink MGM, et al. Autopsy rates in the Netherlands: 35 years of decline. PLoS One 2017;12:e0178200 10.1371/journal.pone.0178200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kretzschmar H. Brain banking: opportunities, challenges and meaning for the future. Nat Rev Neurosci 2009;10:70–8. 10.1038/nrn2535 [DOI] [PubMed] [Google Scholar]
- 4.Wichmann D, Obbelode F, Vogel H, et al. Virtual autopsy as an alternative to traditional medical autopsy in the intensive care unit: a prospective cohort study. Ann Intern Med 2012;156:123–30. 10.7326/0003-4819-156-2-201201170-00008 [DOI] [PubMed] [Google Scholar]
- 5.Burton JL, Underwood J. Clinical, educational, and epidemiological value of autopsy. Lancet 2007;369:1471–80. 10.1016/S0140-6736(07)60376-6 [DOI] [PubMed] [Google Scholar]
- 6.Royal College of Pathologists of Australasia Autopsy Working Party. The decline of the hospital autopsy: a safety and quality issue for healthcare in Australia. Med J Aust 2004;180:281–5. [DOI] [PubMed] [Google Scholar]
- 7.Chariot P, Witt K, Pautot V, et al. Declining autopsy rate in a French hospital: physician’s attitudes to the autopsy and use of autopsy material in research publications. Arch Pathol Lab Med 2000;124:739–45. [DOI] [PubMed] [Google Scholar]
- 8.Goldman L, Sayson R, Robbins S, et al. The value of the autopsy in three medical eras. N Engl J Med 1983;308:1000–5. 10.1056/NEJM198304283081704 [DOI] [PubMed] [Google Scholar]
- 9.Shojania KG, Burton EC, McDonald KM, et al. Changes in rates of autopsy-detected diagnostic errors over time: a systematic review. JAMA 2003;289:2849–56. 10.1001/jama.289.21.2849 [DOI] [PubMed] [Google Scholar]
- 10.Kuijpers CC, Fronczek J, van de Goot FR, et al. The value of autopsies in the era of high-tech medicine: discrepant findings persist. J Clin Pathol 2014;67:512–9. 10.1136/jclinpath-2013-202122 [DOI] [PubMed] [Google Scholar]
- 11.Office for National Statistics. Guidance for doctors completing medical certificates of cause of death in England and Wales. 2010. https://www.gro.gov.uk/Images/medcert_July_2010.pdf (accessed 3 Jun 2016).
- 12.Attems J, Arbes S, Böhm G, et al. The clinical diagnostic accuracy rate regarding the immediate cause of death in a hospitalized geriatric population; an autopsy study of 1594 patients. Wien Med Wochenschr 2004;154:159–62. 10.1007/s10354-004-0057-0 [DOI] [PubMed] [Google Scholar]
- 13.Ermenc B. Comparison of the clinical and post mortem diagnoses of the causes of death. Forensic Sci Int 2000;114:117–9. 10.1016/S0379-0738(00)00329-7 [DOI] [PubMed] [Google Scholar]
- 14.Roberts IS, Benamore RE, Benbow EW, et al. Post-mortem imaging as an alternative to autopsy in the diagnosis of adult deaths: a validation study. Lancet 2012;379:136–42. 10.1016/S0140-6736(11)61483-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Blokker BM, Wagensveld IM, Weustink AC, et al. Non-invasive or minimally invasive autopsy compared to conventional autopsy of suspected natural deaths in adults: a systematic review. Eur Radiol 2016;26:1159–79. 10.1007/s00330-015-3908-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.University College London. Chapter 7: Paired Data. 2018. http://www.ucl.ac.uk/ich/short-courses-events/about-stats-courses/stats-rm/Chapter_7 (accessed 19 Jan 2018).
- 17.Klein WM, Kunz T, Hermans K, et al. The common pattern of postmortem changes on whole body CT scans. Journal of Forensic Radiology and Imaging 2016;4:47–52. 10.1016/j.jofri.2015.11.006 [DOI] [Google Scholar]
- 18.Jackowski C, Thali M, Aghayev E, et al. Postmortem imaging of blood and its characteristics using MSCT and MRI. Int J Legal Med 2006;120:233–40. 10.1007/s00414-005-0023-4 [DOI] [PubMed] [Google Scholar]
- 19.Ross SG, Bolliger SA, Ampanozi G, et al. Postmortem CT angiography: capabilities and limitations in traumatic and natural causes of death. Radiographics 2014;34:830–46. 10.1148/rg.343115169 [DOI] [PubMed] [Google Scholar]
- 20.Rutty GN, Morgan B, Robinson C, et al. Diagnostic accuracy of post-mortem CT with targeted coronary angiography versus autopsy for coroner-requested post-mortem investigations: a prospective, masked, comparison study. Lancet 2017;390:145–54. 10.1016/S0140-6736(17)30333-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Grabherr S, Grimm J, Baumann P, et al. Application of contrast media in post-mortem imaging (CT and MRI). Radiol Med 2015;120:824–34. 10.1007/s11547-015-0532-2 [DOI] [PubMed] [Google Scholar]
- 22.Kubat K, Smedts F. The usefulness of the lactate dehydrogenase macroreaction in autopsy practice. Mod Pathol 1993;6:743–7. [PubMed] [Google Scholar]
- 23.Weustink AC, Hunink MG, van Dijke CF, et al. Minimally invasive autopsy: an alternative to conventional autopsy? Radiology 2009;250:897–904. 10.1148/radiol.2503080421 [DOI] [PubMed] [Google Scholar]
- 24.Ross SG, Thali MJ, Bolliger S, et al. Sudden death after chest pain: feasibility of virtual autopsy with postmortem CT angiography and biopsy. Radiology 2012;264:250–9. 10.1148/radiol.12092415 [DOI] [PubMed] [Google Scholar]
- 25.Bolliger SA, Filograna L, Spendlove D, et al. Postmortem imaging-guided biopsy as an adjuvant to minimally invasive autopsy with CT and postmortem angiography: a feasibility study. AJR Am J Roentgenol 2010;195:1051–6. 10.2214/AJR.10.4600 [DOI] [PubMed] [Google Scholar]
- 26.Inai K, Noriki S, Kinoshita K, et al. Postmortem CT is more accurate than clinical diagnosis for identifying the immediate cause of death in hospitalized patients: a prospective autopsy-based study. Virchows Arch 2016;469:101–9. 10.1007/s00428-016-1937-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Westphal SE, Apitzsch J, Penzkofer T, et al. Virtual CT autopsy in clinical pathology: feasibility in clinical autopsies. Virchows Arch 2012;461:211–9. 10.1007/s00428-012-1257-4 [DOI] [PubMed] [Google Scholar]
- 28.Takahashi N, Higuchi T, Shiotani M, et al. The effectiveness of postmortem multidetector computed tomography in the detection of fatal findings related to cause of non-traumatic death in the emergency department. Eur Radiol 2012;22:152–60. 10.1007/s00330-011-2248-6 [DOI] [PubMed] [Google Scholar]
- 29.Puranik R, Gray B, Lackey H, et al. Comparison of conventional autopsy and magnetic resonance imaging in determining the cause of sudden death in the young. J Cardiovasc Magn Reson 2014;16:44 10.1186/1532-429X-16-44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ampanozi G, Thali YA, Schweitzer W, et al. Accuracy of non-contrast PMCT for determining cause of death. Forensic Sci Med Pathol 2017;13:284–92. 10.1007/s12024-017-9878-1 [DOI] [PubMed] [Google Scholar]
- 31.Dirnhofer R, Jackowski C, Vock P, et al. VIRTOPSY: minimally invasive, imaging-guided virtual autopsy. Radiographics 2006;26:1305–33. 10.1148/rg.265065001 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.