Abstract
Background
Both exercise and vitamin D are recommended means to prevent falls among older adults, but their combined effects on fall-induced injuries are scarcely studied.
Methods
A 2-year follow-up of a previous 2-year randomized controlled trial with vitamin D and exercise (Ex) of 409 older home-dwelling women using a factorial 2 × 2 design (D−Ex−, D+Ex−, D−Ex+, D+Ex+). Besides monthly fall diaries, femoral neck bone mineral density (fn-BMD), and physical functioning were assessed at 1 and 2 years after the intervention.
Results
After the intervention, S-25OHD concentrations declined to baseline levels in both supplement groups. The groups did not differ for change in fn-BMD or physical functioning, except for leg extensor muscle strength, which remained about 10% greater in the exercise groups compared with the reference group (D−Ex−). There were no between-group differences in the rate of all falls, but medically attended injurious falls reduced in D+Ex− and D−Ex+ groups compared with D−Ex−. However, all former treatment groups had less medically attended injured fallers, HRs (95% CI) being 0.62 (0.39–1.00) for D+Ex−, 0.46 (0.28–0.76) for D−Ex+, and 0.55 (0.34–0.88) for D+Ex+, compared with D−Ex−.
Conclusions
Exercise-induced benefits in physical functioning partly remained 2 years after cessation of supervised training. Although there was no difference in the rate of all falls, former exercise groups continued to have lower rate of medically attended injured fallers compared with referents even 2 years after the intervention. Vitamin D without exercise was associated with less injurious falls with no difference in physical functioning.
Keywords: Physical functioning, Injurious falls, Vitamin D, Exercise
Introduction
The number of older people will increase over the next decades, accompanied with increased number of falls and fall-related injuries, and effective means for preventing falls and subsequent consequences are needed. Many risk factors for falls and fall-induced injuries are related to physical inactivity and low functional ability (e.g. mobility limitations, reduced lower limb muscle strength, and balance deficit), and also to bone fragility in case of fractures. Also slow processing speed in the ability to react to perturbation may explain increased risk of injurious falls (1). All these can be modified by exercise (2,3). There is evidence from randomized controlled trials and systematic reviews and meta-analyses that regular strength and balance training can reduce the risk of falling in community-dwelling older adults by 15–50% (4–6). Vitamin D deficiency has also been shown to be associated with lower physical functioning and greater risk of falls and fractures in older people (7–9). However, recent randomized controlled trial (RCTs) with high vitamin D doses have shown either no benefit (10) or even harmful effects on lower extremity physical functioning, falls and fractures (11,12). Nor did a recent RCT of exercise and vitamin D show any synergic effect on falls in older women (13).
Currently, both exercise and vitamin D supplementation are recommended for prevention of falls among older adults. In particular, exercise including strength and balance training has been shown to reduce falls and injurious falls, but the results are yet inconsistent (14–16). There is also some evidence that benefits may last, at least to some extent, after cessation of the intervention as long as the training induced physical performance is maintained (17). So far, only few studies have evaluated rate of falls or injurious falls once the exercise training is stopped (17–20), but it seems that the risk of injurious falls remains reduced even after cessation of the supervised exercise training (19). To our knowledge, there are no follow-ups after ceasing vitamin D supplementation.
Previously, we showed that supervised exercise training reduced medically attended injurious falls among home-dwelling older women, while the rate of all falls was affected by neither exercise nor vitamin D intervention. Exercise also improved physical functioning, while vitamin D did not (13). The aim of this pre-planned 2-year follow-up of the DEX trial was to assess whether the benefits of multimodal supervised exercise training in reducing falls and medically attended injurious falls persist after ceasing the training. In particular, we examined the residual effects of the intervention on falls, fall-induced injuries and physical functioning for up to 2-year after completion of the intervention.
Methods
Trial Design
This study is a 2-year follow-up of the 2-year double-blind, placebo-controlled vitamin D and open exercise DEX trial (NCT00986466). The period of supervised exercise and vitamin D/placebo supplementation denotes the intervention period (0–24 months) (21). The subsequent 2-year period after the intervention (24–48 months) denotes the follow-up period, which is reported here.
Participants
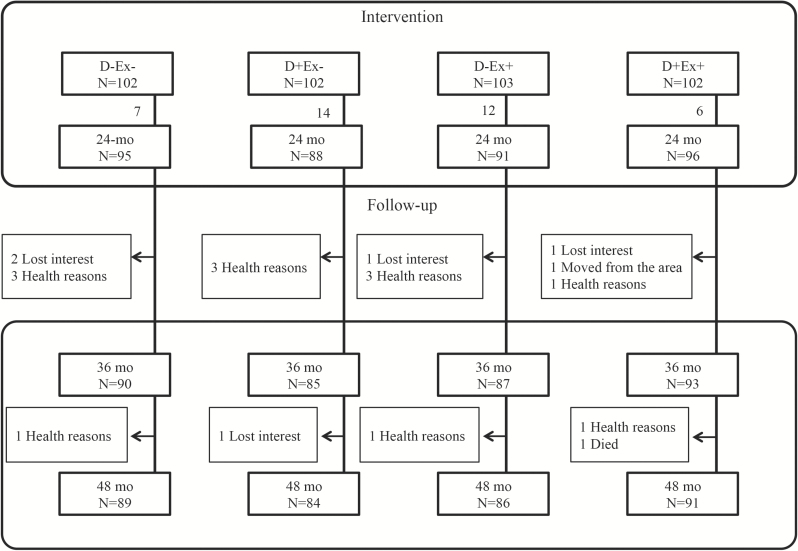
Initially, 409 home-dwelling 70-80-year-old women were randomly assigned to one of four groups: (a) vitamin D 20 µg/day (800 IU) and exercise(D+Ex+) (b) placebo and exercise(D−Ex+) (c) vitamin D 20 µg/day without exercise(D+Ex−), and (d) placebo without exercise (D−Ex−). The intervention results have been reported previously (13,22). Of the 370 women who completed the intervention, 15 were unable or unwilling to continue with the follow-up. Five more women withdrew during the follow-up period (Figure 1).
Figure 1.
Trial profile.
The study protocol was approved by the Ethics Committee of the Pirkanmaa Hospital District, Finland (R09090). Each participant provided her written informed consent prior to randomization.
The exercise training program has been described previously (21). Briefly, exercise consisted of supervised group training classes two times a week for the first year, and once a week for the second year of the intervention. The training program was progressive and consisted of strength, balance, agility, and mobility training, both in the exercise hall and gymnasium. Participants in the non-exercising group were asked to maintain their pre-study level of physical activity during the intervention. All participants received a booklet for home exercise training after the intervention.
Data Collection
The number of falls was obtained from prospective fall diaries returned monthly via mail, and details of each registered fall were ascertained over telephone throughout the 48-month study period. A fall was defined “an unexpected event in which the participant comes to rest on the ground, floor or lower level.” (23) Injurious falls were classified as minor injurious falls and medically attended injurious falls, the latter being those for which participants sought medical care (nurse, physician, or hospital) and included injuries such as bruises, abrasions, contusions, sprains, fractures, and head injuries. This classification conforms with that proposed by Schwenk et al. (24). The Pegasos patient medical records of the City of Tampere were searched for all participants’ utilization of healthcare services due to incident falls during the follow-up period, to find possibly unreported fall injuries for which medical attention was sought.
During follow-up, all measurements were done yearly (at 36 and 48 months from baseline). Dietary intake of calcium and vitamin D were assessed with a validated food frequency questionnaire (25). In addition to height and weight, body composition and areal bone mineral density (fn-BMD) of the left femoral neck was assessed using dual-energy X-ray absorptiometry (DXA, Lunar Prodigy Advance, GE Lunar, Madison. WI) (26).
Physical functioning was assessed by the Short Physical Performance Battery (SPPB) (27), which comprised static balance, 4 m normal walking speed and five-time chair stand tests, and by the Timed up and go (TUG) test (28). Dynamic balance was assessed using backwards walking (29). Maximal isometric leg-extensor strength at a knee angle 110° was measured by a strain gauge dynamometer (Tamtron, Tampere, Finland). The Community Healthy Activities Model Program for Seniors (CHAMPS) physical activity questionnaire for older adults was used to monitor changes in physical activity. In addition, each participant recorded her daily steps with a pedometer (Omron HJ-112-E) over the entire 48-month period.
Analysis of 25-Hydroxy-Vitamin D
Fasting serum 25-hydroxy-vitamin D (S-25OHD) was measured trial with a manual OCTEIA immunoenzymometric assay (IDS, Boldon, UK) during the intervention, and with an automated IDS-iSYS analyzer (IDS) during the follow-up. Reproducibility was ensured by adhering to the Vitamin D External Quality Assessment Scheme, DEQAS (deqas.kmpd.co.uk). Interassay variation was avoided by measuring all samples from the same participants in the same series. According to the manufacturer the results from the two assays correlate very well (r = 0.99). The regression equation between the two methods rendered a positive or negative bias of 1–3 nmol/L between 50–80 nmol/L.
Statistical Analysis
All data were analyzed on an intention-to-treat basis (ITT). Changes from baseline to the end of the intervention (0–24 months) have been reported previously (13). Here we report changes during the follow-up period (24–48 months). Incidence rates of falls were calculated as the total number of falls divided by the time over which falls were monitored (100 person-years) in each group. Negative binomial regression was used to estimate incidence rate ratios (IRR) for falls and injurious falls, and Cox-regression models for calculating hazard ratios (HR) for fallers and injured fallers in each group, with the D−Ex− group as reference. Only HR was analyzed for the entire 48-month period, modeling the time to first fall (i.e. becoming a faller).
For physical functioning and BMD, between-group differences (24–48 months) were estimated by linear mixed models for normally distributed outcomes (fn-BMD, walking speed and isometric muscle strength), and generalized linear mixed models (GLMM) for non-normally distributed outcomes (TUG, backwards walking and chair stand) using possible confounding factors (e.g. age, height and weight) as covariates. These methods allowed the incorporation of incomplete longitudinal data into the analysis.
Results
Follow-up measurements at 48 months were done for 350 participants (85.6% of the original sample; the main reason for discontinuation was poor health). Descriptive characteristics at baseline (0 months) are given in Table 1, there were no between-group differences in fn-BMD or physical functioning. Dietary intake of calcium and vitamin D were adequately maintained throughout the study, the mean (SD) daily calcium intake was 1098 (378) mg and vitamin D intake 10.4 (3.9) µg at baseline, and 1182 (387) mg and 11.6 (4.9) µg at the end of the follow-up (48 months), respectively. After the intervention, S-25OHD concentrations started to decline towards baseline levels in both supplement groups; mean S-25OHD being 72.5 (18.5) nmol/L at 48 months (see Supplementary Figure 1) showing no difference between the former vitamin D supplemented groups and the placebo groups (p = .15).
Table 1.
Descriptive Group Characteristics (mean, SD) at the Baseline of the 2-Year Intervention (0 months)
| Characteristic | D−Ex− N = 102 |
D+Ex− N=102 |
D−Ex+ N = 103 |
D+Ex+ N = 102 |
|---|---|---|---|---|
| Age, years | 73.8 (3.1) | 74.1 (3.0) | 74.8 (2.9) | 74.1 (2.9) |
| Height, cm | 160.7 (5.4) | 159.2 (5.8) | 159.4 (6.1) | 159.7 (5.9) |
| Weight, kg | 72.0 (12.4) | 73.0 (13.1) | 70·9 (10·6) | 73·2 (10·5) |
| Fat, % | 41.1 (6.7) | 42.0 (7.2) | 41.3 (6.4) | 42.8 (5.3) |
| Calcium intake, mg/day | 1,040 (345) | 1,125 (420) | 1,119 (346) | 1,109 (385) |
| Vitamin D intake, µg/day | 10.2 (4.1) | 10.9 (4.2) | 10.3 (3.6) | 10.4 (3.9) |
| S-25(OH)D, nmol/L | 67.6 (18.8) | 65.8 (17.1) | 69.5 (18.0) | 65.5 (17.5) |
| Cognitive status, MMSE score (0–30)* | 28.5 (1.7) | 28.3 (1.4) | 28.2 (1.4) | 28.3 (1.5) |
| SPPB, range | 10.6 (3–12) | 10.7 (1–12) | 10.9 (7–12) | 10.8 (5–12) |
| ADL score (6–36)† | 6.7 (1.6) | 7.0 (2.2) | 6.8 (1.9) | 6.9 (1.8) |
| IADL score (8–48)† | 9.8 (2.7) | 10.7 (4.9) | 9.9 (3.8) | 10.3 (4.0) |
| Difficulties outdoor mobility, n (%) | 18 (17.6) | 19 (18.6) | 17 (16.5) | 17 (16.7) |
Notes: ADL = Activities of daily living; D−Ex− = placebo; D+Ex− =20 µg vitamin D daily; D−Ex+ = placebo + exercise; D−Ex+ = 20 µg vitamin D daily + exercise; MMSE = Mini Mental State Examination; IADL = Instrumental activities of daily living; SPPB = Short physical performance battery.
*Higher score indicates better functioning.
†Lower score indicates better functioning.
Falls and Injurious Falls
Of 635 falls in 226 fallers, 356 falls (56%) resulted in injuries. Of these 356 injurious falls, 116 (33%) were attended medically. There was no significant difference between groups for the rate of all falls or minor injurious falls, but less medically attended injurious falls occurred in the D+Ex− and D−Ex+ groups compared with the reference group (D−Ex−) (Table 2). All former treatment groups had less medically attended injured fallers HR (95% CI) being 0.62 (0.39–1.00) for D+Ex−, 0.46 (0.28–0.76) for D−Ex+, and 0.55 (0.34–0.88) for D+Ex+, when compared with D−Ex− (see Supplementary Figure 2).
Table 2.
Rate of Falls per 100 Person-Years in Each Study Group During the 2-Year Follow-Up (24–48 months), and Incidence Rate Ratios (IRR) (95% CI) for Falls and Injurious Falls and Hazard Ratio (HR) (95% CI) For Fallers and Injured Fallers
| Outcome | D−Ex− | D+Ex− | D−Ex+ | D+Ex+ |
|---|---|---|---|---|
| Falls, all | 103.0 | 81.5 | 84.2 | 97.1 |
| Minor injurious falls | 29.4 | 20.1 | 20.0 | 24.3 |
| Medically attended injurious falls | 23.8 | 10.6 | 10.6 | 21.4 |
| Falls with fractures | 4.0 | 3.0 | 2.9 | 5.1 |
| IRR | ||||
| All falls | 1 | 0.78 (0.53–1.14) | 0.80 (0.55–1.18) | 0.88 (0.60–1.28) |
| Minor injurious falls | 1 | 0.66 (0.38–1.13) | 0.68 (0.39–1.16) | 0.79 (0.47–1.33) |
| Medically attended injurious falls | 1 | 0.45 (0.23–0.87) | 0.44 (0.23–0.86) | 0.84 (0.48–1.50) |
| HR | ||||
| All fallers | 1 | 0.86 (0.63–1.19) | 1.01 (0.74–1.39) | 0.99 (0.72–1.38) |
| Medically attended injured fallers | 1 | 0.62 (0.39–1.00) | 0.46 (0.28–0.76) | 0.55 (0.34–0.88) |
Note: D−Ex− = placebo; D+Ex− = 20 µg vitamin D daily; D−Ex+ = placebo + exercise; D+Ex+ = 20 µg vitamin D daily + exercise.
Femoral Neck BMD and Physical Functioning
Absolute baseline values at the end of the intervention (24 months) and percentage changes during follow-up (36 and 48 months) are given in Table 3. Femoral neck BMD declined slightly in all groups during the follow-up period (Table 3).
Table 3.
Baseline Values (SD) and Mean Changes (95% CI) Over Time in BMD and Physical Functioning in Each Study Group (The Rightmost Column, pb, Shows the Significance for Difference in Changes Compared with D−Ex−)
| Outcome | Absolute Baseline Value, Mean (SD) | Change at 24 Months, % | p a Compared with D−Ex− | Change at 36 Months, % | Change at 48 Months, % | p b for the Overall Group-Wise Difference |
|---|---|---|---|---|---|---|
| Femoral neck BMD, g/cm2 | ||||||
| D−Ex− | 0.872 (0.141) | −1.4 (−2.1 to −0.7) | −1.7 (−2.5 to −0.9) | −2.6 (−3.5 to −1.8) | ||
| D+Ex− | 0.821 (0.107) | −0.9 (−1.7 to −0.1) | .017 | −1.2 (−2.1 to −0.4) | −2.7 (−3.6 to −1.8) | .34 |
| D−Ex+ | 0.848 (0.115) | −1.1 (−1.8 to −0.4) | .012 | −1.9 (−2.7 to −1.1) | −2.1 (−3.1 to −1.3) | .93 |
| D+Ex+ | 0.875 (0.134) | −1.1 (−1.8 to −0.5) | .041 | −2.4 (−3.1 to −1.6) | −3.2 (−4.1 to −2.4) | .35 |
| Normal walking speed, m/s | ||||||
| D−Ex− | 1.04 (0.21) | −2.8 (−5.7 to 0.0) | −4.2 (−7.3 to −1.1) | −5.1 (−8.2 to −2.1) | ||
| D+Ex− | 1.00 (0.21) | −3.5 (−6.6 to −0.5) | .72 | −5.0 (−8.2 to −1.7 | −4.9 (−8.2 to −1.5) | .61 |
| D−Ex+ | 1.01 (0.19) | −1.8 (−4.8 to 1.2) | .007 | −0.7 (−3.9 to 2.6) | −0.5 (−3.7 to 2.8) | .11 |
| D+Ex+ | 1.03 (0.20) | −2.1 (−5.0 to 0.7) | .46 | −4.7 (−7.9 to −1.7) | −3.9 (−7.0 to −0.8) | .98 |
| Chair stand time, s | ||||||
| D−Ex− | 12.6 (2.4) | −0.8 (−4.2 to 2.7) | −1.7 (−5.3 to 1.9) | −0.7 (−4.6 to 3.3) | ||
| D+Ex− | 12.6 (3.3) | −4.5 (−8.0 to −0.9) | .46 | −3.3 (−6.9 to 0.4) | −3.9 (−8.0 to 0.2) | .58 |
| D−Ex+ | 12.5 (2.8) | −7.4 (−11.0 to −3.8) | .027 | −5.9 (−9.6 to −2.3) | −6.9 (−10.9 to −2.8) | .95 |
| D+Ex+ | 12.4 (2.5) | −7.7 (−11.2 to −4.3) | .054 | −5.5 (−9.1 to −1.9) | −5.2 (−9.2 to −1.2) | .19 |
| TUG time, s | ||||||
| D−Ex− | 9.31 (2.07) | −0.5 (−3.9 to 2.9) | 4.6 (1.2 to 8.0) | 8.7 (4.7 to 12.7) | ||
| D+Ex− | 9.73 (6.44) | 2.5 (−0.9 to 5.8) | .011 | 7.2 (3.9 to 10.5) | 7.4 (3.4 to 11.4) | .21 |
| D−Ex+ | 8.93 (1.94) | 1.9 (−1.7 to 5.5) | .19 | 4.4 (0.8 to 8.0) | 1.9 (−2.4 to 6.2) | .002 |
| D+Ex+ | 8.89 (1.64) | −1.4 (−4.9 to 2.1) | .63 | 4.3 (0.7 to 7.8) | 5.0 (0.8 to 9.2) | .62 |
| Muscle strength, N/kg | ||||||
| D−Ex− | 23.1 (6.1) | 1.4 (−3.2 to 6.1) | 0.6 (−4.2 to5.5) | 2.3 (−2.5 to 7.2) | ||
| D+Ex− | 23.4 (7.7) | 3.0 (−1.5 to 7.4) | .10 | 3.4 (−1.4 to 8.3) | 2.0 (−2.9 to 6.9) | .68 |
| D−Ex+ | 23.6 (6.0) | 16.7 (12.3 to 21.2) | <.001 | 12.3 (7.7 to 16.9) | 10.2 (5.7 to 14.9) | .003 |
| D+Ex+ | 22.2 (6.6) | 17.3 (12.7 to 21.9) | <.001 | 12.7 (7.9 to 17.5) | 12.4 (7.5 to 17.3) | .007 |
| Backwards walking, proportion of those able to do 6.1 m, % | At baseline | At 24 months | At 36 months | At 48 months | ||
| D−Ex− | 42.2 | 50.0 | 48.3 | 48.1 | ||
| D+Ex− | 30.4 | 40.5 | .68 | 43.9 | 45.9 | .34 |
| D−Ex+ | 45.1 | 72.7 | .001 | 65.9 | 61.7 | .32 |
| D+Ex+ | 51.0 | 78.0 | .026 | 71.6 | 73.8 | .56 |
Notes: D−Ex− = placebo; D+Ex− = 20 µg vitamin D daily; D−Ex+ = placebo + exercise; D+Ex+ = 20 µg vitamin D daily + exercise.
aBased on analysis of covariance (ANCOVA).
b p value for the overall group-wise difference from the end of intervention (24 months) to 48 months. Based on Generalized Linear Mixed Models (GLMM) or Linear Mixed Models (LMM).
After the end of the intervention, physical functioning showed general decline during the 2-year follow-up with no between-group differences in changes indicating that the achieved mean treatment effects compared with the reference group were largely maintained (Table 3). There were no significant changes in normal walking speed or chair stand time, nor did any of the intervention groups differ from D−Ex−. The TUG test time increased indicating reduced performance in all groups except for D−Ex+, in which it remained unchanged. Isometric leg extensor muscle strength declined significantly in the former exercise groups but was maintained in the non-exercisers. Still, at the end of the follow-up the maximal isometric leg extensor strength was significantly greater in the former exercise groups, mean difference being 10% for D+Ex+ and 8% for D−Ex+ compared with D−Ex−. Change in proportion of the women able to do backwards walking test was similar in all groups, indicating that the former exercise groups had maintained the benefit compared with D−Ex− (Table 3, and Supplementary Figure 3).
Habitual physical activity declined slightly. The frequency of moderate-intensity physical activity (CHAMPS) declined in all four groups from the baseline mean of 6.7 (5.0) to 5.2 (4.3) h/week being similar in all groups at the end of the follow-up (p = .79). Mean number of daily steps also reduced by about 400 steps from the baseline mean of about 6,000 with no between-group differences (p = .77).
Discussion
This 2-year follow-up of the 2-year DEX trial showed no between-group differences in falls or fallers in general, but results were different for medically attended injurious falls. During the follow-up, both D+Ex− and D−Ex+ had significantly less medically attended injurious falls compared with D−Ex−. However, in all intervention groups, including D+Ex−, there were less medically attended injured fallers compared with D−Ex−, in spite of the finding that D+Ex− did not differ from D−Ex− in physical functioning either during the intervention or follow-up and physical functioning declined also in the exercise groups after ceasing the supervised training. Without vitamin D supplementation, also S-25OHD concentrations declined towards baseline levels in both supplemented groups, while there was no significant change in mean concentrations in the former placebo groups.
Femoral neck BMD declined throughout the 4-year study period in all groups. Neither vitamin D nor exercise could prevent bone loss, although its rate reduced slightly during the 2-year intervention. The amount of bone loss was similar to previous studies showing less than 1% annual bone loss among older women (30). Hansen et al. showed that even high dose cholecalciferol did not meaningfully affect BMD suggesting that large increases in calcium absorption are needed to increase BMD (10). Also the intensity of mechanical loading which may result in increased BMD needs likely to be greater than the training given in this study (17,18).
At the end of the 2-year follow-up, some of the exercise-induced gain in physical functioning was maintained; the former exercisers continued to have better balance than the reference group. Also, about a half of training-induced gains in isometric muscle strength remained till the end of the follow-up. Other tests of physical functioning showed slight decline in all groups and between-group differences achieved during the intervention were mostly maintained. However, better physical functioning cannot explain the fewer medically attended injurious falls seen in D+Ex−, because this group did not differ from the reference group either during the intervention or follow-up.
Exercise-induced improvements in lower extremity function, mobility, and balance can reduce the severity of falls (5,14), but not consistently (16,31). Nevertheless, for maintained benefits it is crucial that the improvements are not lost. Previously it has been shown that gains in balance induced strength and balance training can be partly maintained by weekly low-intensity Tai Chi training (32), and even light intensity home-based weight-bearing exercise training may reduce falls and injurious falls compared with controls (17,33). In our previous follow-up of an exercise intervention trial, physical performance was partly maintained in a combination training group, while most of the benefits disappeared in the pure resistance or balance training groups (18). Even 5 years later the combination training group had significantly less medically attended injurious falls. However, physical performance was not measured, and it is not known whether differences in muscle strength or balance still existed and accounted for the observed effect (19).
In this study, habitual physical activity estimated as daily steps, or time spent in moderate physical activity was consistent with the general older Finnish population (34). Habitual physical activity estimated by pedometers and questionnaires (CHAMPS) declined over time in all groups. During the intervention, the exercisers were more physically active (by about the amount of supervised training; 1–2 h per week) than the non-exercisers, but after cessation of the training, the exercisers’ physical activity returned to the level of their control counterparts.
Vitamin D has been positively associated with better musculoskeletal health and physical functioning, and fewer fractures (35,36). However, there is also evidence that vitamin D has no effect, or may even be harmful in terms of falls or fractures (10–12). Recently, Hansen et al. (10) found that compared with placebo, high-dose cholecalciferol did not translate to better physical functioning or fewer falls. Similarly, Bischoff-Ferrari et al. (11) found that monthly high-dose vitamin D treatment did not improve physical functioning and was associated with increased risk of falls compared with 24,000 IU given monthly (a dose corresponding to 800 IU/day).
Only a few studies have evaluated effects of both vitamin D and exercise on physical functioning (37), and none of these studies had a follow-up after the intervention, nor reported falls. These results indicated no effect of vitamin D supplementation on muscle strength or function following exercise. This is in accordance with the DEX trial, which showed that vitamin D intervention with or without exercise had no effect on physical functioning or falls compared with the reference group during the intervention. However, during follow-up D+Ex− had 55% less medically attended injurious falls and nearly 40% less medically attended injured fallers than the reference group. One explanation could be that vitamin D conferred a delayed preventive effect on severe falls through an unknown mechanism. There was no corresponding effect on physical functioning, which declined similarly in both non-exercise groups with or without vitamin D. Furthermore, though the achieved benefit in physical functioning was partly maintained after cessation of training, it declined in both exercise groups, and exercisers with vitamin D did not differ from exercisers without vitamin D. Also, S-25OHD concetrations returned to baseline levels in both supplemented groups with no significant difference compared with the reference group. These findings do not support the delayed benefit of vitamin D concentrations on falls.
A major strength of this study is the long 2-year follow-up after the 2-year intervention. The drop-out rate was low; only 15 women (4%) of the original cohort who completed the intervention were not willing to continue in the follow-up, and five more discontinued after the first follow-up year mainly due to declined health status. Physical functioning was objectively measured, and falls were assessed with prospective and controlled monthly fall diaries, free of recall bias, over the entire 48 months. Medical records were scrutinized for confirming self-reported medically attended injurious falls. Vitamin D concentrations were also assessed annually during the follow-up in winter when concentrations are expected to be at their lowest levels.
A limitation was that detailed information on participants’ physical activity in the four study groups was not available during the follow-up. Our study did not include older men or institutionalized persons, and the results can only be generalized to older home-dwelling women. Also, the study was powered for falls, and results regarding injurious falls or fallers should be interpreted cautiously, though are consistent with current literature (14,19). Vitamin D supplementation may be more effective among people with vitamin D insufficiency. In this study, despite the decline in vitamin D concentrations after stopping supplementation, participants still had adequate vitamin D status (38).
In conclusion, exercise-induced benefits in physical functioning partly remained 2 years after cessation of supervised exercise training. Although there was no difference in the rate of all falls, former exercise groups had less medically attended injured fallers compared with referents even 2 years after the intervention. Vitamin D without exercise was also associated with less injurious falls with no corresponding difference in physical functioning.
In the absence of a structured exercise training program, training effects are likely to reduce with time, as do habitual physical activity. Training programs focusing on balance and resistance training and adequate vitamin D intake should be an integral part of daily life in older adults for preventing injurious falls.
Supplementary Material
Supplementary data is available at The Journals of Gerontology, Series A: Biomedical Sciences and Medical Sciences online
Funding
This work was supported by the Academy of Finland (grant no. 131524); Juho Vainio Foundation, Helsinki, Finland; and Finnish Cultural Foundation, Pirkanmaa Regional fund, Finland.
Conflict of interest
The authors declare no conflict of interest.
Supplementary Material
References
- 1. Welmer AK, Rizzuto D, Laukka EJ, Johnell K, Fratiglioni L. Cognitive and physical function in relation to the risk of injurious falls in older adults: a population-based study. J Gerontol A Biol Sci Med Sci. 2016. [DOI] [PubMed] [Google Scholar]
- 2. Karinkanta S, Piirtola M, Sievänen H, Uusi-Rasi K, Kannus P. Physical therapy approaches to reduce fall and fracture risk among older adults. Nat Rev Endocrinol. 2010;6:396–407. doi:10.1038/nrendo.2010.70. [DOI] [PubMed] [Google Scholar]
- 3. Ferrucci L, Cooper R, Shardell M, Simonsick EM, Schrack JA, Kuh D. Age-Related Change in Mobility: Perspectives From Life Course Epidemiology and Geroscience. J Gerontol A Biol Sci Med Sci. 2016;71:1184–1194. doi:10.1093/gerona/glw043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Gillespie LD, Robertson MC, Gillespie WJ, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2012;9:CD007146. doi:10.1002/14651858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Palvanen M, Kannus P, Piirtola M, Niemi S, Parkkari J, Järvinen M. Effectiveness of the Chaos Falls Clinic in preventing falls and injuries of home-dwelling older adults: a randomised controlled trial. Injury. 2014;45:265–271. doi:10.1016/j.injury.2013.03.010. [DOI] [PubMed] [Google Scholar]
- 6. Sherrington C, Michaleff ZA, Fairhall N, et al. Exercise to prevent falls in older adults: an updated systematic review and meta-analysis. Br J Sports Med. 2016. [DOI] [PubMed] [Google Scholar]
- 7. Bischoff-Ferrari HA, Dawson-Hughes B, Willett WC, et al. Effect of vitamin D on falls: a meta-analysis. JAMA. 2004;291:1999–2006. doi:10.1001/jama.291.16.1999. [DOI] [PubMed] [Google Scholar]
- 8. Bischoff-Ferrari HA, Willett WC, Orav EJ, et al. A pooled analysis of vitamin D dose requirements for fracture prevention. N Engl J Med. 2012;367:40–49. doi:10.1056/NEJMoa1109617. [DOI] [PubMed] [Google Scholar]
- 9. Pfeifer M, Begerow B, Minne HW, Suppan K, Fahrleitner-Pammer A, Dobnig H. Effects of a long-term vitamin D and calcium supplementation on falls and parameters of muscle function in community-dwelling older individuals. Osteoporos Int. 2009;20:315–322. doi:10.1007/s00198-008-0662-7. [DOI] [PubMed] [Google Scholar]
- 10. Hansen KE, Johnson RE, Chambers KR, et al. Treatment of vitamin D insufficiency in postmenopausal women: a randomized clinical trial. JAMA Intern Med. 2015;175:1612–1621. doi:10.1001/jamainternmed.2015.3874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bischoff-Ferrari HA, Dawson-Hughes B, Orav EJ, et al. Monthly high-dose vitamin D treatment for the prevention of functional decline: a randomized clinical trial. JAMA Intern Med. 2016;176:175–183. doi:10.1001/jamainternmed.2015.7148. [DOI] [PubMed] [Google Scholar]
- 12. Sanders KM, Stuart AL, Williamson EJ, et al. Annual high-dose oral vitamin D and falls and fractures in older women: a randomized controlled trial. JAMA. 2010;303:1815–1822. doi:10.1001/jama.2010.594. [DOI] [PubMed] [Google Scholar]
- 13. Uusi-Rasi K, Patil R, Karinkanta S, et al. Exercise and vitamin D in fall prevention among older women: a randomized clinical trial. JAMA Intern Med. 2015;175:703–711. doi:10.1001/jamainternmed.2015.0225. [DOI] [PubMed] [Google Scholar]
- 14. El-Khoury F, Cassou B, Charles MA, Dargent-Molina P. The effect of fall prevention exercise programmes on fall induced injuries in community dwelling older adults: systematic review and meta-analysis of randomised controlled trials. BMJ. 2013;347:f6234. doi:10.1136/bmj.f6234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Freiberger E, Häberle L, Spirduso WW, Zijlstra GA. Long-term effects of three multicomponent exercise interventions on physical performance and fall-related psychological outcomes in community-dwelling older adults: a randomized controlled trial. J Am Geriatr Soc. 2012;60:437–446. doi:10.1111/j.1532-5415.2011.03859.x. [DOI] [PubMed] [Google Scholar]
- 16. Gianoudis J, Bailey CA, Ebeling PR, et al. Effects of a targeted multimodal exercise program incorporating high-speed power training on falls and fracture risk factors in older adults: a community-based randomized controlled trial. J Bone Miner Res. 2014;29:182–191. doi:10.1002/jbmr.2014. [DOI] [PubMed] [Google Scholar]
- 17. Korpelainen R, Keinänen-Kiukaanniemi S, Nieminen P, Heikkinen J, Väänänen K, Korpelainen J. Long-term outcomes of exercise: follow-up of a randomized trial in older women with osteopenia. Arch Intern Med. 2010;170:1548–1556. doi:10.1001/archinternmed.2010.311. [DOI] [PubMed] [Google Scholar]
- 18. Karinkanta S, Heinonen A, Sievänen H, Uusi-Rasi K, Fogelholm M, Kannus P. Maintenance of exercise-induced benefits in physical functioning and bone among elderly women. Osteoporos Int. 2009;20:665–674. doi:10.1007/s00198-008-0703-2. [DOI] [PubMed] [Google Scholar]
- 19. Karinkanta S, Kannus P, Uusi-Rasi K, Heinonen A, Sievänen H. Combined resistance and balance-jumping exercise reduces older women’s injurious falls and fractures: 5-year follow-up study. Age Ageing. 2015;44:784–789. doi:10.1093/ageing/afv064. [DOI] [PubMed] [Google Scholar]
- 20. Liu-Ambrose TY, Khan KM, Eng JJ, Gillies GL, Lord SR, McKay HA. The beneficial effects of group-based exercises on fall risk profile and physical activity persist 1 year postintervention in older women with low bone mass: follow-up after withdrawal of exercise. J Am Geriatr Soc. 2005;53:1767–1773. doi:10.1111/j.1532-5415.2005.53525.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Uusi-Rasi K, Kannus P, Karinkanta S, et al. Study protocol for prevention of falls: a randomized controlled trial of effects of vitamin D and exercise on falls prevention. BMC Geriatr. 2012;12:12. doi:10.1186/1471-2318-12-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Patil R, Karinkanta S, Tokola K, Kannus P, Sievänen H, Uusi-Rasi K. Effects of vitamin D and exercise on the wellbeing of older community-dwelling women: a randomized controlled trial. Gerontology. 2016;62:401–408. doi:10.1159/000442441. [DOI] [PubMed] [Google Scholar]
- 23. Lamb SE, Jørstad-Stein EC, Hauer K, Becker C; Prevention of Falls Network Europe and Outcomes Consensus Group Development of a common outcome data set for fall injury prevention trials: the Prevention of Falls Network Europe consensus. J Am Geriatr Soc. 2005;53:1618–1622. doi:10.1111/j.1532-5415.2005.53455.x. [DOI] [PubMed] [Google Scholar]
- 24. Schwenk M, Lauenroth A, Stock C, et al. Definitions and methods of measuring and reporting on injurious falls in randomised controlled fall prevention trials: a systematic review. BMC Med Res Methodol. 2012;12:50. doi:10.1186/1471-2288-12-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Outila TA, Kärkkäinen MU, Lamberg-Allardt CJ. Vitamin D status affects serum parathyroid hormone concentrations during winter in female adolescents: associations with forearm bone mineral density. Am J Clin Nutr. 2001;74:206–210. [DOI] [PubMed] [Google Scholar]
- 26. Uusi-Rasi K, Rauhio A, Kannus P, et al. Three-month weight reduction does not compromise bone strength in obese premenopausal women. Bone. 2010;46:1286–1293. doi:10.1016/j.bone.2009.10.013. [DOI] [PubMed] [Google Scholar]
- 27. Guralnik JM, Simonsick EM, Ferrucci L, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49:M85–M94. [DOI] [PubMed] [Google Scholar]
- 28. Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39:142–148. [DOI] [PubMed] [Google Scholar]
- 29. Husu P, Suni J, Pasanen M, Miilunpalo S. Health-related fitness tests as predictors of difficulties in long-distance walking among high-functioning older adults. Aging Clin Exp Res. 2007;19:444–450. [DOI] [PubMed] [Google Scholar]
- 30. Uusi-Rasi K, Sievänen H, Pasanen M, Oja P, Vuori I. Maintenance of body weight, physical activity and calcium intake helps preserve bone mass in elderly women. Osteoporos Int. 2001;12:373–379. doi:10.1007/s001980170105. [DOI] [PubMed] [Google Scholar]
- 31. Gill TM, Pahor M, Guralnik JM, et al. ; LIFE Study Investigators. Effect of structured physical activity on prevention of serious fall injuries in adults aged 70-89: randomized clinical trial (LIFE Study). BMJ. 2016;352:i245. doi:10.1136/bmj.i245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Wolfson L, Whipple R, Derby C, et al. Balance and strength training in older adults: intervention gains and Tai Chi maintenance. J Am Geriatr Soc. 1996;44:498–506. [DOI] [PubMed] [Google Scholar]
- 33. Hwang HF, Chen SJ, Lee-Hsieh J, Chien DK, Chen CY, Lin MR. Effects of home-based Tai Chi and lower extremity training and self-practice on falls and functional outcomes in older fallers from the Emergency Department-A Randomized Controlled Trial. J Am Geriatr Soc. 2016;64:518–525. doi:10.1111/jgs.13952. [DOI] [PubMed] [Google Scholar]
- 34. Husu P, Suni J, Vähä-Ypyä H, et al. Objectively measured sedentary behavior and physical activity in a sample of Finnish adults: a cross-sectional study. BMC Public Health. 2016;16:920. doi:10.1186/s12889-016-3591-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Bischoff-Ferrari HA, Dawson-Hughes B, Platz A, et al. Effect of high-dosage cholecalciferol and extended physiotherapy on complications after hip fracture: a randomized controlled trial. Arch Intern Med. 2010;170:813–820. doi:10.1001/archinternmed.2010.67. [DOI] [PubMed] [Google Scholar]
- 36. Bischoff-Ferrari HA, Dietrich T, Orav EJ, et al. Higher 25-hydroxyvitamin D concentrations are associated with better lower-extremity function in both active and inactive persons aged > or =60 y. Am J Clin Nutr. 2004;80:752–758. [DOI] [PubMed] [Google Scholar]
- 37. Minshull C, Biant LC, Ralston SH, Gleeson N. A systematic review of the role of vitamin d on neuromuscular remodelling following exercise and injury. Calcif Tissue Int. 2016;98:426–437. doi:10.1007/s00223-015-0099-x. [DOI] [PubMed] [Google Scholar]
- 38. Lamberg-Allardt C, Brustad M, Meyer HE, Steingrimsdottir L. Vitamin D - a systematic literature review for the 5th edition of the Nordic Nutrition Recommendations. Food Nutr Res. 2013;57. doi:10.3402/fnr.v57i0.22671. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.