Abstract
Francisella tularensis is a zoonotic bacterial pathogen that causes severe disease in a wide range of host animals, including humans. Well-developed murine models of F. tularensis pathogenesis are available, but they do not meet the needs of all investigators. However, researchers are increasingly turning to insect host systems as a cost-effective alternative that allows greater increased experimental throughput without the regulatory requirements associated with the use of mammals in biomedical research. Unfortunately, the utility of previously-described insect hosts is limited because of temperature restriction, short lifespans, and concerns about the immunological status of insects mass-produced for other purposes. Here, we present a novel host species, the orange spotted (OS) cockroach (Blaptica dubia), that overcomes these limitations and is readily infected by F. tularensis. Intrahemocoel inoculation was accomplished using standard laboratory equipment and lethality was directly proportional to the number of bacteria injected. Progression of infection differed in insects housed at low and high temperatures and F. tularensis mutants lacking key virulence components were attenuated in OS cockroaches. Finally, antibiotics were delivered to infected OS cockroaches by systemic injection and controlled feeding; in the latter case, protection correlated with oral bioavailability in mammals. Collectively, these results demonstrate that this new host system provides investigators with a new tool capable of interrogating F. tularensis virulence and immune evasion in situations where mammalian models are not available or appropriate, such as undirected screens of large mutant libraries.
Keywords: Francisella, tularemia, insect infection model, Blaptica dubia, cockroach
Introduction
Francisella tularensis is a Gram-negative bacterial pathogen capable of causing disease in a remarkably diverse array of hosts; at least 190 different species of mammals, 23 birds, 3 amphibians and 88 invertebrates are recognized as being susceptible to F. tularensis infection (Morner & Addison, 2001). In experimental animals, F. tularensis invades and replicates within both phagocytic and non-phagocytic cells (Santic & Kwaik, 2013; Steele, Brunton, et al., 2013; Chong & Celli, 2010) and several studies have demonstrated that F. tularensis survives engulfment by bacterivorous protists, often escaping from the food vacuole and replicating within the cytosol (Bradburne, Verhoeven, et al., 201; Abd, Johansson, et al., 2003; Lauriano, Barker, et al., 2004; El-Etr, Margolis, et al., 2009). This ability to survive intracellularly is thought to contribute to the low infectious dose of F. tularensis, which is fewer than 10 bacteria for the highly-virulent strains (Ellis, Oyston, et al., 2002). Due to this high infectivity and an accompanying high rate of mortality and morbidity, F. tularensis is of particular concern as an agent of biological terrorism and is therefore classified as a Tier 1 select agent by the US Centers for Disease Control (Dennis, Inglesby, et al., 2001). An attenuated live vaccine strain (LVS) originally was derived from a virulent isolate in the 1950s (Burke, 1977). Despite its name, LVS is not currently approved by the US Food and Drug Administration for standard human use because of safety and efficacy concerns. However, the LVS strain can be manipulated in biosafety level two laboratories (BSL2) and still causes rapid and severe disease in many hosts, allowing for F. tularensis pathogenesis studies without the need for BSL3 containment.
While experimental models of infectious disease historically have been developed around mammalian host species, non-vertebrate hosts continue to gain attention as an alternative approach for studying pathogenic microorganisms (Hernández, López, et al., 2015; Bangi, 2013; Arvanitis, Glavis-Bloom, & Mylonakis, 2013; Ramarao, Nielsen-Leroux, & Lereclus, 2012). In particular, studies using the fruit fly Drosophila melanogaster (Moule, Monack, & Schneider, 2010; Ahlund, Rydén, et al., 2010) and Greater Wax Moth Galleria mellonella larvae (Dean & Hoek, 2015; Sprynski, Valade, & Neulat-Ripoll, 2014; Aperis, Fuchs, et al., 2007) have significantly advanced our understanding of F. tularensis pathogenesis. D. melanogaster offers powerful host genetic tools but the small body size of this insect makes delivering an exact dose of bacteria difficult without specialized equipment and training. Moreover, D. melanogaster is temperature-restricted and cannot survive at typical mammalian body temperatures, making this host of limited use for analysis of pathogens with temperature-sensitive virulence patterns such as F. tularensis (Horzempa, Carlson, et al., 2008). In contrast, G. mellonella survives well at 37°C and is large enough for confident dosing with a small-gauge syringe. G. mellonella larvae also are readily-available in large quantities from a number of commercial suppliers. However, this insect host also requires investigators to accept certain limitations and tradeoffs. Pupation, the process by which the larvae metamorphesize into adults, typically occurs within a short period of time when the larvae are kept at 37°C, thereby limiting the experimental window available to researchers. Immune function can vary widely before, during, and after pupation (Shaik & Sehnal, 2009; Woltedji, Fang, et al., 2013; Xu, Lu, et al., 2012), thus making it difficult to standardize host immunological status in G. mellonella.
We previously determined that the Madagascar hissing (MH) cockroach (Gromphadorhina laevigata) met the above noted criteria and was a suitable surrogate host for the facultative intracellular pathogens Burkholderia mallei, B. pseudomallei, and B. thailandensis (R Studio Team, 2013). The Orange Spotted (OS) cockroach, (Blaptica dubia Serville 1839) also meets the above criteria as an ideal insect host for pathogenesis studies but is more readily available from commercial suppliers and is more docile compared to the MH cockroach. We sought to determine if tropical cockroach species can serve as experimental hosts for another important bacterial pathogen, namely F. tularensis.. We found the OS cockroach to be a permissive host for F. tularensis LVS. Lethality depended upon the dose of bacteria given, the temperature of incubation, and, interestingly, the developmental stage and gender of the cockroach. Bacterial titers increased throughout the course of infection and several mutant strains lacking factors known to be involved in Francisella pathogenesis were attenuated. Infection could be rescued by systemic or peroral delivery of antibiotics, with protection by the peroral route correlating with known oral absorption profiles in mammals. These results extend our previous findings utilizing the MH cockroach (Fisher, Ribot, et al., 2012) and demonstrate that tropical cockroaches are a favorable alternative to mammals and other insect species for the study of multiple bacterial pathogens.
Materials and Methods
All work described in this manuscript was approved by the appropriate institutional review board prior to completion. Since OS cockroaches are invertebrate animals, IACUC approval was not necessary.
Bacterial Strains and Knockout Construction
F. tularensis LVS strains used in this study were provided by two different laboratories. The strain designated as F. tularensis LVS-1 was provided by the J.F. Huntley laboratory at the University of Toledo (from ATCC). LVS-1 was the parental strain used to generate both ΔdsbA and ΔdipA mutants. The strain designated as F. tularensis LVS-2 was provided by the J. Horzempa laboratory at West Liberty University (originally provided by Karen Elkins). LVS-2 was the parental strain used to generate both ΔdeoB and ΔiglC mutants. None of the mutants used in this study exhibited in vitro growth defects.
Generation of isogenic deletion mutants of dsbA, dipA, and deoB was described previously (Ren, Champion, & Huntley, 2014; Wu, Ren, & Huntley, 2015; Horzempa, Shanks, et al., 2010). Markerless deletion iglC was accomplished by sequentially deleting codons 71-140 of both copies of iglC as previously described (Schmitt, Barnes, et al., 2017). The entire open reading frame was not deleted to preserve elements presumed to be required for expression of neighboring genes (Lai, Golovliov, & Sjöstedt, 2004). This iglC-null mutant is referred to as ΔiglC.
Bacterial Growth Conditions
All F. tularensis isolates and mutant derivatives were maintained as permanent frozen stocks at −80°C in BHI broth supplemented with 15% glycerol. For each experiment, bacteria were recovered by streak plating onto Chocolate II agar (GC base with 1% isovitalex and 1% Hemoglobin) and incubated at 37°C for 48 hours. Since the mutant strains used are genetically stable, antibiotics were not added to the growth media prior to infections.
Cockroach Housing
The original laboratory stock of Blaptica dubia cockroaches was purchased from Backwater Reptiles (www.backwaterreptiles.com). Subsequent generations that were reared in the lab were used for most experiments, although we did supplement our stock with additional orders from Backwater Reptiles, as necessary. Cockroaches were stored in vented 18- or 32-gallon plastic containers and kept at 30°C in the dark. Since B. dubia cockroaches do not climb vertical glass or slick plastic surfaces, no chemical or physical restrains are needed to keep the insects in the rearing containers. Pressed paper egg cartons or paper-based cat litter (www.yesterdaysnews.com) was used as a substrate in the rearing containers. Rearing containers were cleaned and cockroaches were sorted into new containers according to their developmental stage at least monthly, or more frequently as needed. Dry dog chow (Purina) was provided ad libitum and fresh fruits or vegetables including carrots, oranges, bananas and apples were given periodically as a source of water. After infection, groups of 4 or 5 cockroaches were kept in 100 mm Petri dishes with dry dog food and carrot slices, which were changed daily.
Bacterial Infection
Newly molted, sixth-instar cockroaches weighing 0.7-1.0 g were transferred to the challenge temperature (usually 37°C) at least seven days prior to infection in order to allow them to acclimate. We found this acclimation step to be critical– cockroaches that experienced a simultaneous temperature shift and injection trauma tended to have unpredictable deaths in control groups and dose-independent deaths in experimental groups. All data reported here is from temperature-acclimated insects. Bacteria cultivated on Chocolate II agar that had been incubated at 37°C for 48 hours were suspended in PBS to a concentration of approximately 108 colony forming units (CFU) per mL. These initial suspensions were serial diluted in PBS and aliquots (20 μl) of each dilution were delivered by intrahemoceol injection to the right of the midline at the base of the third tergum (Figure 1). A 28-gauge needle-syringe combination was used for all experiments except those testing for antibiotic rescue. Those experiments used a sharpened pipette tip, made by cutting a 60° bevel into a gel-loading pipette with a razor blade prior to sterilization, for inoculation of bacteria. The rate of mortality in groups receiving 106 CFU of F. tularensis LVS by each method was not significantly different (p>0.05), but we have not yet compared the two methods at lower doses. In either case, the abdomen was swabbed with 70% isopropanol prior to injection in order to lessen the risk of external contamination. For each experiment, a control group was injected with PBS to observe effects of trauma alone. Groups of 8 to 10 cockroaches were used for each experiment. Cockroaches were stored at the temperature indicated and observed for survival up to 10 days post-inoculation. Cockroaches were considered dead when they displayed no response to touch. Unless otherwise mentioned, juvenile cockroaches were used (unable to differentiate gender until roaches reach adulthood).
Figure 1.
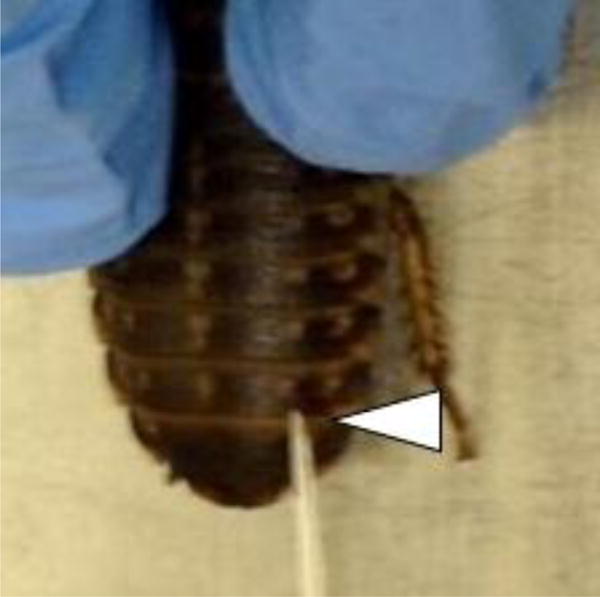
Typical site of injection to the right of the midline along the base of the third tergum (arrowhead) from the posterior. Note that sharpened pipette tips can be used for inoculation, instead of needles.
Antibiotic Administration
Groups of 10 cockroaches were injected with F. tularensis LVS using sharpened gel-loading pipette tips and treated with antibiotics at 2, 48, and 96 hours post infection. Two methods of delivery were used for antibiotic administration; systemic injection and controlled feeding. For systemic injection, 20 μl of each antibiotic suspension was injected into the base of the third terga (abdominal plate) on the ventral side of the body, on the right side halfway between the midline and the spiracle (Figure 2A) using a needle and syringe combination. For the second and third injections, the left side of the same tergum and the right side of the next anterior tergum were used, respectively. For controlled feeding, antibiotics were prepared and diluted to the appropriate concentration in a sterile 50% sucrose solution. Cockroaches were placed on their back and a 10 μl aliquot of the sucrose solution containing antibiotic was slowly dispensed onto the mouth (Figure 2B). This resulted in the rapid consumption of the entire dose. Antibiotics were delivered at the following total doses, regardless of route: Streptomycin, 32 μg; Gentamicin, 32 μg; Doxycycline, 32 μg; Azithromycin, 100 μg; Resazurin; 11 μg.
Figure 2. Antibiotic delivery to OS cockroaches.
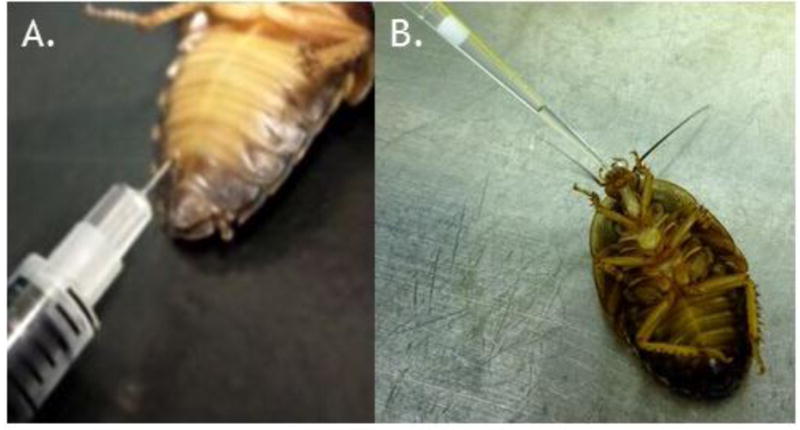
(A) For systemic delivery, a 20 μl aliquot of each antibiotic or PBS vehicle control was injected at the base of the 3rd (shown) or 4th tergum on the ventral side of the abdomen. (B) For oral delivery, cockroaches were placed on their backs and were fed a solution containing either 50% sucrose or 50% sucrose containing the specified antibiotic. In both cases, antibiotics were delivered at 2-, 48-, and 96-hours post infection.
Enumeration of bacteria in hemolymph
B. dubia roaches were inoculated with 106 F. tularensis LVS cells as described previously. Cockroaches were incubated at 37°C with access to dry dog chow and carrot slices (to prevent dehydration). Hemolymph was extracted from insects at each designated time point of 6, 12, 24, 50, 72, and 96 hours post initial infection. Two groups were used for each extraction time point. One group of cockroaches received a 16 μg dose of gentamicin 2 hours prior to hemolymph extraction, and a second group received an equal volume of sterile PBS in parallel. At the time of harvest, cockroaches were cleansed with 70% isopropyl alcohol and decapitated using sterile surgical scissors. Hemolymph was immediately drained into a 1.5 mL Eppendorf tube containing 10 μl chilled PBS with anticoagulant (0.05% N-Phenylthiourea). Tubes were weighed before and after addition of hemolymph in order to estimate the volume of hemolymph collected from each cockroach. (This approach is necessary because cockroach hemolyph is extremely viscous and cannot be accurately measured volumetrically. We estimate that 1 ml ≈ 1 g at room temperature). In order to quantify the number of F. tularensis LVS CFU present in the hemolymph, the harvested samples were serial diluted 1:10 in PBS and aliquots of each dilution were plated on Chocolate II agar plates supplemented with ampicillin and trimethoprim. The total number of F. tularensis LVS per mL of hemolymph was determined based on the number of CFU observed from PBS-treated cockroaches and the number of intracellular F. tularensis LVS per mL of hemolymph was determined based on the number of CFU observed from gentamicin-treated cockroaches.
LD50 Estimation and Statistical analysis
The R programming environment (version 3.2.1; (R Core Team, 2013)), accessed via the RStudio interactive development environment (R Studio Team, 2013), was used for all comparisons. Lethal doses 50% and corresponding 95% confidence intervals were estimated by non-linear regression using the ‘drc’ package. Differences in survival outcome between groups that received equivalent doses of F. tularensis with or without antibiotics were determined by log-rank (Mantel-Cox) analysis using the ‘survival’ package (Therneau & Grambsch, 2000; Therneau, 2015). For analysis of in vivo growth patterns of F. tularensis LVS, the mean, median, and interquartile range of each group was calculated using plot.ly (Plotly Technologies Inc., 2015).
Results
Infection of OS cockroaches with F. tularensis LVS
To determine if OS cockroach survival was proportional to the number of bacteria present in the inoculum, serial dilutions of F. tularensis LVS were injected into the hemocoel of juvenile cockroaches that weighed between 0.7 and 1.0 grams. Following infection, cockroaches were housed at 37°C and survival was monitored over the course of 7 days. Overall, the percentage of cockroaches in each group that survived infection and the rates of death were dose-dependent. None of the cockroaches inoculated with 106 or 105 CFU of F. tularensis LVS survived beyond day 4 (Figure 3). In comparison, 5 out of 8 cockroaches infected with 104 CFU of F. tularensis LVS survived through day seven post-infection (p=0.0141; compared to 105 CFU group) and 7 out of 8 cockroaches infected with 103 CFU of F. tularensis LVS survived through day seven post-infection (p<0.001; compared to 105CFU group). Injection of PBS alone did not result in any cockroach deaths.
Figure 3. B. dubia survival is proportional to the F. tularensis LVS infection dose.
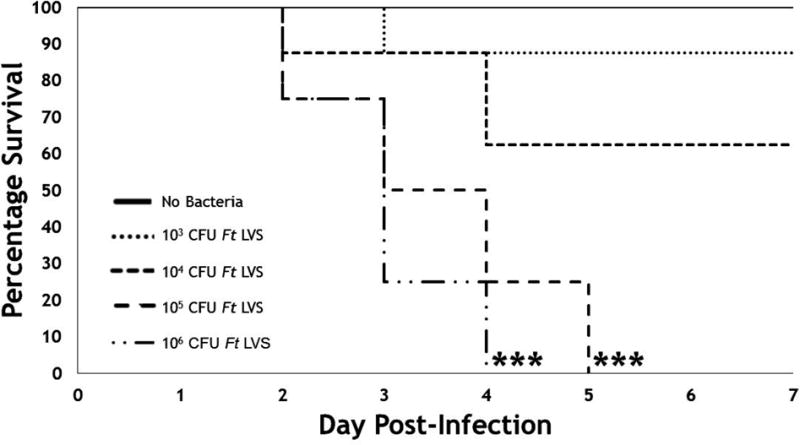
Groups of juvenile OS cockroaches (n=8) were injected with either PBS (no bacteria) or serial dilutions of F. tularensis LVS (1.7 × 106 to 103 CFU), incubated at 37°C, and monitored for survival over the course of 7 days. LVS was grown on CHOCII agar for 48 hours, harvested, and diluted in PBS. Statistical differences between groups were calculated by log-rank (Mantel-Cox) analysis. Asterisks indicate significant difference from the no bacteria control group (***=p<0.001).
Effect of temperature on F. tularensis virulence
Transcriptional activation of F. tularensis virulence factors is at least partially controlled by temperature (Horzempa, Carlson, et al., 2008). Since insects are ectothermic, taking on the ambient temperature of their surroundings, we sought to determine the impact of varied temperatures on F. tularensis pathogenesis in this system. Serial dilutions of F. tularensis were injected into the hemocoel of juvenile OS cockroaches and their survival rates were monitored over the course of 8 days at 22°C, 30°C, 37°C, or 40°C. We found that higher temperatures correlated with higher rates of mortality (Figure 4A, Table 1). Following infection with 106 CFU, incubation at either 37°C or 40°C resulted in rapid OS cockroach death (mean time-to-death of 3.6 and 3.2 days, respectively), with no survivors at either temperature (Figure 4A). By comparison, incubation at the lower temperatures of 22°C or 30°C resulted in delayed time-to-death and increased survival, despite slightly higher inoculums (Figure 4A). At 30°C, 20 percent of cockroaches survived F. tularensis LVS infection with a mean time-to-death of 6.14 days. At 22°C, 30 infection with a mean time-to-death of 6.33 days. There were no significance differences between cockroach survival at 22°C and 30°C or between cockroach survival at 37°C and 40°C. However, cockroach survival at both of the lower temperatures (22°C and 30°C) was significantly different from cockroach survival at both of the higher temperatures (37°C and 40°C; all p<0.001).
Figure 4. F. tularensis LVS lethality in B. dubia is temperature-dependent.
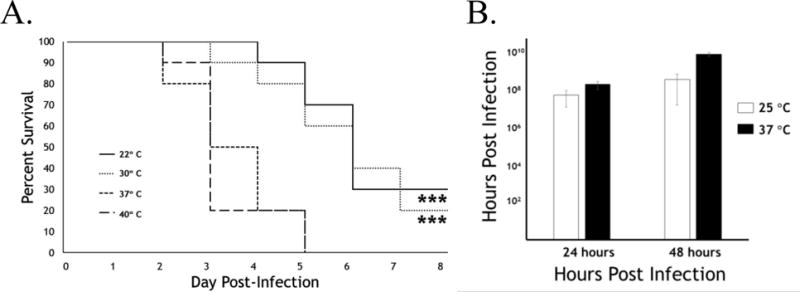
A. Groups of juvenile B. dubia cockroaches (n=10) were injected with 6.0 × 106 CFU, 8.8 × 106 CFU, 4.5 × 106 CFU, or 3.0 × 106 CFU F. tularensis LVS (approx. 100 × LD50) and incubated at 22°C, 30°C, 37°C, or 40°C, respectively. Statistical differences between groups were calculated by log-rank (Mantel-Cox) analysis. Asterisks indicate statistical differences from the 37°C and 40°C groups (***=p<0.001). B. Groups of juvenile B. dubia cockroaches were injected with 1.72 × 107 CFU of F. tularensis LVS and incubated at 25°C (open bars) or 37°C (closed bars). At 24 hours and 48 hours after infection, the total hemolymph was harvested from five roaches in each group and bacterial burden was determined by serial dilution and plating on agar plates. Data were log-transformed and analyzed via two-way ANOVA with the Sidak’s multiple comparison’s test. CFU were significantly higher in roaches incated at 37°C relative to 25°C at both 24 h and 48 h (*,p<0.05; ***,p<0.0001).
Table 1. Median lethal dose of F. tularensis LVS and derivatives in OS cockroaches and wax worms.
The median lethal dose (LD50) of F. tularensis LVS parental strains, LVS-1 or LVS-2, and deletion mutants of those LVS strains lacking known virulence factors, and E. coli DH5α. LD50 and corresponding 95% confidence intervals were estimated by non-linear regression using the ‘drc’ package in the R programming environment (Version 3.2.1).
| Strain | Host | Temperature | LD50 (95% Cl), CFU |
|---|---|---|---|
| F. tularensis LVS-1 | Juvenile cockroaches | 22°C | 3.2 × 106 (5.6 × 105−1.2 × 107) |
| Juvenile cockroaches | 30°C | 2.9 × 105 (4.6 × 104−1.8 × 106) | |
| Juvenile cockroaches | 37°C | 3.5 × 104 (1.1 × 104−1.0 × 105) | |
| Juvenile cockroaches | 40°C | 1.2 × 104 (4.2 × 103−3.3 × 104) | |
| Adult female cockroaches | 37°C | 5.4 × 104 (9.7 × 103−3.0 × 105) | |
| Adult male cockroaches | 37°C | 1.3 × 103 (4.0 × 102−4.2 × 103) | |
| F. tularensis LVS-1 ΔdsbA | Juvenile cockroaches | 37°C | 2.2 × 106 (1.0 × 106−4.7 × 106) |
| F. tularensis LVS-1 ΔdipA | Juvenile cockroaches | 37°C | 8.1 × 105 (4.0 × 105−1.6 × 106) |
| F. tularensis LVS-2 | Juvenile cockroaches | 37°C | 1.7 × 104 (6.7 × 103−4.4 × 104) |
| F. tularensis LVS-2 ΔiglC | Juvenile cockroaches | 37°C | 1.3 × 106 (2.8 × 105−5.7 × 106) |
| F. tularensis LVS-2 ΔdeoB | Juvenile cockroaches | 37°C | 5.6 × 105 (2.1 × 105−1.8 × 106) |
| E. coli DH5α | Juvenile cockroaches | 37°C | 8.7 × 106 (3.0 × 106−2.5 × 107) |
We further examined F. tularensis LVS pathogenicity with respect to temperature by measuring the in vivo growth kinetics at 25°C and 37°C. Because there was no statistical difference is survival between insects incubated at 22°C and 30°C, we selected an intermediate value (25°C) as the lower temperature for this experiment. At 24 and 48 hours post infection, hemolymph was extracted, diluted, and plated for CFU. At each time point, significantly more CFU were recovered from roaches incubated at 37°C (Figure 4B), indicating that changes in the F. tularensis growth rate may partially explain the differences in survival seen in Figure 4A. Other contributing factors could include temperature-regulated activation of F. tularensis LVS virulence factors (Horzempa, Carlson, et al., 2008) or temperature-induced changes in insect immunity (Lazzaro, Flores, et al., 2008).
F. tularensis genes required for virulence in mammals are required for virulence in OS cockroaches
In order to determine if virulence factors known to be required for F. tularensis pathogenicity in mammals also are required in our cockroach model, we determined the LD50 value for several mutant strains of F. tularensis LVS. Juvenile OS cockroaches were infected by intrahemocoel injection followed by incubation at 37°C. Survival was monitored for 8 days post-infection and the LD50 value for each strain was determined by non-linear regression. Since the various LVS mutants were generated by two different laboratories, we excluded the possibility of inherent differences in LVS virulence by infecting cockroaches with either LVS parental strain, LVS-1 and LVS-2. Indeed, LVS-1 and LVS-2 did not exhibit any significant LD50 differences in juvenile cockroaches at 37°C (Table 1). In contrast, loss of dsbA, dipA, iglC, or deoB resulted in substantially decreased virulence in cockroaches (Table 1), similar to trends previously observed in mice (Ren, Champion, & Huntley, 2014; Schmidt, Klimentova, et al., 2013; Chong, Child, et al., 2013; Golovliov, Sjöstedt, et al., 2003) and chick embryos (Horzempa, Carlson, et al., 2008). More specifically, dipA and deoB mutants were more than 1-log attenuated in cockroaches and dipA and iglC were nearly 2-log attenuated in cockroaches. These results suggest that, despite obvious differences between mice and cockroaches, there are significant overlaps in how F. tularensis causes disease and death in hosts from diverse phyla.
In vivo growth of F. tularensis LVS
In order to monitor the kinetics of F. tularensis LVS growth during infection, we harvested hemolymph from infected OS cockroaches at various time points post-infection and used serial dilution to enumerate the number of viable bacterial cells in each sample. In one set of experimentally infected cockroaches, we measured the total number of bacteria present at each time point. After an initial inoculum of 106 CFU, F. tularensis LVS quickly replicated, reaching 109 CFU per ml of hemolymph by 96 hours (Figure 5). Since the antibiotic gentamicin does not penetrate eukaryotic host cells, it is lethal only to extracellular bacteria (Moule, Monack, & Schneider, 2010; Horzempa, O’Dee, et al., 2010). Therefore, we administered it to a second set of infected cockroaches 2 hours prior to harvesting hemolymph in order to distinguish between F. tularensis LVS cells located in intracellular and extracellular environments. Interestingly, most bacteria in the hemolymph were sensitive to gentamicin, indicating that they were exposed to the extracellular environment at some time during the 2 hours prior to harvest (Figure 5).
Figure 5. In vivo growth of intracellular and total F. tularensis LVS in OS cockroaches.
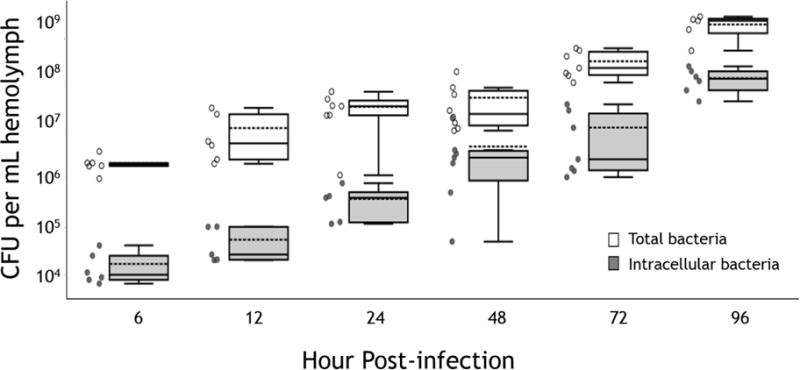
Total (open symbols) and gentamicin-protected (intracellular; shaded symbols) F. tularensis LVS from at least 5 infected OS cockroaches per time point. Bacterial CFU were determined by serial dilution of hemolymph and enumeration on CHOCII agar plates. Intracellular bacterial numbers were determined by injecting gentamicin into infected cockroaches 2 hours prior to each time point. Results from individual insects are shown as open (total CFU) and closed (intracellular CFU) circles. Boxes indicate the median (solid line), mean (dotted line) and interquartile ranges (IQR; box boundaries) for each group. Upper and lower whiskers correspond with the largest and smallest data points, respectively, within 1.5 × IQR for each group.
Effect of OS cockroach development on F. tularensis virulence
Because insect immune responses are known to vary by age and developmental stage (Booth, Cambron, et al., 2015; Eleftherianos, Baldwin, et al., 2008; Tian, Guo, et al., 2010), we sought to determine if there were any differences in susceptibility to F. tularensis LVS in juvenile and adult cockroaches. Injections in adults were performed using the same method described for the juveniles. Cockroaches cannot be separated by gender as juveniles, but anatomical differences (Figure 1C) make gender determination possible in adults. We, therefore, analyzed survival in adult female and adult male cockroaches separately. We found that although the overall percentages of surviving cockroaches differed slightly between adult female (50 percent survival) and juvenile (30 percent survival) cockroaches, both groups were equally susceptible to F. tularensis LVS infections (juvenile mean time-to-death 4.7 days; adult female mean time-to-death 4.8 days; no statistical difference between groups). By comparison, adult male cockroaches were more sensitive to killing by F. tularensis LVS, with rapid death rates (mean time-to-death 3.8 days) and 100% mortality by day 6 post-infection (p=0.0169 compared with juveniles; p<0.001 compared with adult females; Figure 6). The LD50 of adult males was determined to be 1.3 × 103 CFU, which is a 1.4- and 1.6-log decrease from that of juvenile and adult female cockroaches, respectively (Table 1).
Figure 6. OS cockroach susceptibility to F. tularensis infection varies by life stage.
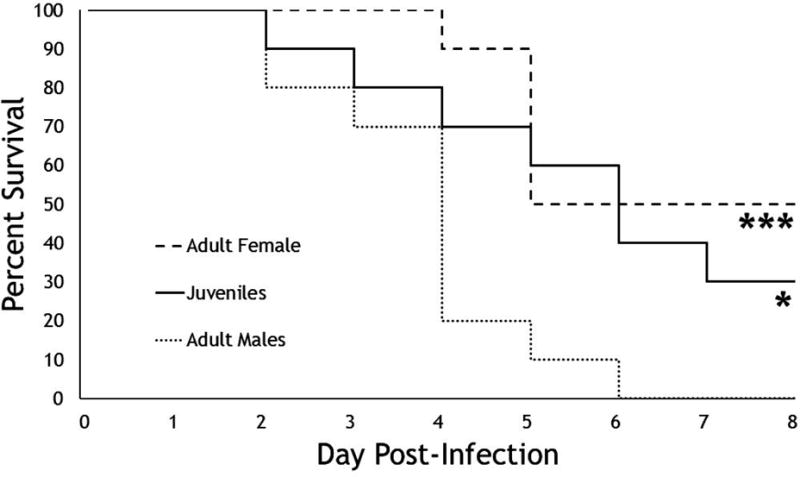
Groups of juvenile, adult male, or adult female cockroaches (n=10) were injected with 3.4 × 104 CFU F. tularensis LVS prior to incubation at 37°C. Statistical differences between groups were calculated by log-rank (Mantel-Cox) analysis. Asterisks indicate statistical differences from the adult male group (*=p<0.05; ***=p<0.001). Survival in the adult female and juvenile groups was not significantly different (p>0.05).
Antibiotic rescue of infected OS cockroaches
To explore whether OS cockroaches may be useful in the drug development pipeline, we infected cockroaches with a high dose (1.3 × 106 CFU to 3.4 × 106 CFU) of F. tularensis LVS by intrahemocoel injection and then administered antibiotics either by injection or by controlled feeding. All cockroaches in the vehicle only control groups died by day 7 post-infection (Table 2). Doxycycline, an antibiotic known to absorb well through mucus membranes, effectively prevented cockroach death when delivered by either route (Table 2, p<0.001). F. tularensis LVS is resistant to azithromycin (Ahmad, Hunter, et al., 2010) and this antibiotic failed to protect OS cockroaches from infection, illustrating the specificity of protection in the assay (Table 2). Streptomycin and gentamicin, which have poor oral bioavailbility in mammals, were effective at preventing cockroach mortality when injected directly into the hemocoel (80 percent survival with streptomycin; 90 percent survival with gentamicin; p<0.001 for both antibiotics compared to no antibiotic treatment; Table 2). However, neither of these antibiotics rescued OS cockroaches when delivered perorally (p=0.00199 for injection of streptomycin compared to forced feeding; p<0.001 for injection of gentamicin compared to forced feeding). Finally, resazurin, an experimental drug candidate that has anti-F. tularensis activity in vitro (Schmitt, O’Dee, et al., 2013), failed to protect OS cockroaches from infection (no survival by either delivery route; Table 2).
Table 2. Rescue of OS cockroaches with antibiotics after lethal dose of F. tularensis LVS.
Groups of OS cockroaches (n=8-18) were infected with approximately 100 × LD50 (between 1.3 × 106 CFU and 3.4 × 106 CFU) F. tularensis LVS using sharpened pipette tips. Then at 2, 48, and 96 hours post-infection, infected cockroaches were treated by intrahemocoel injection (i.h.) or peroral feeding (p.o.) of the antibiotics indicated. Statistical differences in survival endpoints were determined by log-rank (Mantel-Cox) analysis.
| Antibiotic | Route | Dosea | Survival Rate | Log-rank Comparison
|
|
|---|---|---|---|---|---|
| to Vehicle Control | between Routes | ||||
| Vehicle only | i.h. | 0/18 | n.s. | ||
| p.o | 0/10 | ||||
| Doxycydine | i.h. | 32 μg | 9/10 | *** | n.s. |
| p.o | 32 μg | 10/10 | *** | ||
| Streptomycin | i.h. | 32 μg | 8/10 | *** | ** |
| p.o | 32 μg | 0/10 | n.s. | ||
| Gentamicin | i.h. | 32 μg | 7/8 | *** | *** |
| p.o | 32 μg | 0/10 | n.s. | ||
| Azithromycin | i.h. | 100 μg | 0/10 | n.s. | n.s. |
| p.o | 100 μg | 0/10 | n.s. | ||
| Resazurin | i.h. | 11 μg | 0/10 | n.s. | n.s. |
| p.o | 11 μg | 0/10 | n.s. | ||
| Additional control groups
|
|||||
| Bacteria only | No manipulation | 0/10 | n.s.b | ||
| No Bacteria | No manipulation | 10/10 | |||
| i.h. vehicle | 18/18 | ||||
| p.o. vehicle | 6/6 | ||||
Asterisks indicate significant differences compared to the corresponding vehicle control group or alternative route of delivery (**=p<0.01, ***=p<0.001).
=this dose was administered three times during the study.
=survival outcome in the no manipulation group was not statistically different than survival in either vehicle control group (i.h. or p.o.; p>0.05 for all comparisons).
Discussion
F. tularensis is a highly-virulent zoonotic pathogen that causes significant morbidity and mortality globally. To facilitate future advances in our understanding of this important bacterium, we sought to develop an improved insect host system that eliminates undesirable biological and logistical trade-offs that accompany other popular host species such as D. melanogaster and G. mellonella. In this manuscript, we provide data indicating that B. dubia OS cockroach can function as an experimental host for F. tularensis that is (Morner & Addison, 2001) readily-available, (Santic & Kwaik, 2013) simple to rear in the laboratory, (Steele, Brunton, et al., 2013) tolerant of mammalian body temperatures, (Chong & Celli, 2010) large enough in size to allow consistent delivery of bacterial inoculations using standard needle-syringe combinations, (Bradburne, Verhoeven, et al., 2013) long-lived with low background mortality, and (Abd, Johansson, et al., 2003) hardy enough to withstand multiple injections of bacteria and/or antibiotics.
Temperature is known to regulate expression of F. tularensis virulence factors (Horzempa, Carlson, et al., 2008). One of the advantages of insect models, in comparison with mammals, is the ability to experimentally manipulate the temperature at which host-pathogen interactions occur. When we varied the temperature at which infection took place, we observed that higher temperatures correlated with higher mortality (Figure 4, Table 1). Others have shown that temperature can effect insect immune pathways (Lazzaro, Flores, et al., 2008; Woida & Taszłow, 2013; Kaunisto, Härkönen, et al., 2015; Torson, Yocum, et al., 2015; Browne, Surlis, & Kavanagh, 2014; Telsonis-Scott, van Heerwaarden, et al., 2013), making it likely that here are also differences in the immune response of OS cockroaches infected at different temperatures. To date, the biological underpinnings of the observed correlation between temperature and survival remain unknown and are an active area of investigation.
We took a genetic approach to determine if virulence factors known to be required for pathogenesis against mammals are also required in the OS cockroach (at 37°C). We examined survival of insects challenged with a small panel of F. tularensis LVS mutants that are attenuated in other model systems. The proteins DsbA and DipA are both associated with the normal structure and function of the F. tularensis membrane and their loss results in severe attenuation in mammals (Ren, Champion, & Huntley, 2014; Chong & Celli, 2010). DeoB is a metabolic protein (a phosphopentomutase) required for cellular invasion and virulence toward macrophages, dendritic cells, and chick embryos in F. tularensis (Horzempa, Carlson, et al., 2008; Horzempa, O’Dee, et al., 2010) and virulence toward mice in the closely related Francisella novicida (Weiss, Brotcke, et al., 2007). Finally, IglC is a virulence factor encoded on the Francisella pathogenicity island that is required for intracellular survival and virulence toward mice (Eleftherianos, Baldwin, et al., 2008; Law, Sriram, et al., 2014; Bröms, Meyer, et al., 2012). These strains were chosen for testing based on availability within the collaborating laboratories and the availability of correlating data in mammals. We found that mutants lacking each of these proteins to be attenuated in OS cockroaches (Table 1). Since these proteins play essential roles in distinct components of the F. tularensis virulence program, this finding supports the idea that F. tularensis uses similar mechanisms to evade immune clearance and cause disease in diverse host organisms. Thus, the OS cockroach model should be useful in identifying additional regulators and effectors of F. tularensis pathogenesis. For example, large mutant libraries can be screened in this model without the regulatory or cost burdens associated with similar studies in mammals.
Classically, F. tularensis is considered a facultative intracellular pathogen and it is known to invade both mammalian and insect cells (Moule, Monack, & Schneider, 2010; Sprynski, Valade, & Neulat-Ripoll, 2014; Ahmad, Hunter, et al., 2010). As seen in Figure 5, gentamicin-resistant bacteria can be recovered as early as six hours post injection, which is likely to indicate successful invasion of OS cockroach cells as has been previously reported for D. melanogaster (Moule, Monack, & Schneider, 2010). As expected, the population of intracellular bacteria continued to grow throughout the infection process. Importantly, the method of analysis used here only allowed for recovery of intracellular bacteria located within circulating hemocytes. Bacteria that invaded non-circulating hemocytes or other cell, tissue-associated cell types would not have been recovered.
It is now recognized that, in addition to the classic intracellular phase, F. tularensis also goes through a distinct extracellular phase that is critical for pathogenecity in mammals (Silva & Pestana, 2013; Forestral, Malik, et al., 2007). Interestingly, the majority of F. tularensis cells recovered from infected OS cockroaches were killed by injection of gentamicin prior to harvest, indicating that they were located in the extracellular environment. This finding mirrors what others have observed for F. novicida in D. melanogaster (Moule, Monack, & Schneider, 2010), indicating that insects may be useful experimental hosts for understanding the extracellular phase of Francisella virulence.
Host immune function is not static; it can vary dramatically across developmental stages in wax worms and other lepidopterans (Meylaers, Freitak, & Schoofs, 2007; Beetz, Holthusen, et al., 2008) and fruit flies (Horn, Leips, & Starz-Gaiano, 2014; Verma & Tapadia, 2012). Importantly, Meylaers, et al, found that wax worm immunity dramatically increases as larvae progress through the wandering stage, in which they are typically used, and enter pupation (Meylaers, Freitak, & Schoofs, 2007). We therefore sought to determine if OS cockroach susceptibility to F. tularensis LVS varied by developmental stage. We determined the killing kinetics and LD50 of F. tularensis LVS against juvenile, adult female, and adult male OS cockroaches. The susceptibility pattern of juveniles (which we used for all other experiments reported here) and adult females were highly similar. In comparison, adult males showed enhanced susceptibility, with a shorter mean time-to-death (Figure 5) and a lower LD50 (Table 1). Other insect hosts have demonstrated gender-specific differences in innate immune responses (Klein & Flanagan, 2016) which could explain the observed differences in CFU demonstrated here. Interestingly, Horn, et al, found that the phagocytic ability of D. melanogaster hemocytes, migratory cells similar in function to mammalian macrophages, decreases with age (Horn, Leips, & Starz-Gaiano, 2014) and it will be important to examine this and other possible causes of the increased susceptibility that we observed in adult males. Revealing these causes may illuminate key host factors that differentiate protective and unprotective immune responses to F. tularensis infection, information that could aid in developing a much-needed safe and effective vaccine.
Finally, we tested the ability of five different antibiotics to protect OS cockroaches from F. tularensis LVS infection (Table 2). Doxycycline is readily absorbed orally and was able to protect OS cockroaches from infection when delivered by either route. This protection was specific to antibiotics with anti-Francisella activity since azithromycin, to which F. tularensis LVS is resistant, failed to protect from lethality. Streptomycin and gentamicin are aminoglycoside antibiotics with poor oral bioavailability in mammals. Interestingly, these antibiotics protected OS cockroaches only when delivered by systemic injection and not when provided perorally. These findings indicate that oral absorption of antibiotics is similar in both mammals and insects and that OS cockroaches can provide a preliminary screening platform for identification of new antibiotics with anti-Francisella activity. As an example, we examined the ability of resazurin, which has been shown to have potent anti-F. tularensis LVS activity in vitro (Schmitt, O’Dee, et al., 2013), to rescue OS cockroaches from lethality. Unfortunately, resazurin failed to protect OS cockroaches from infection likely due to inactivation by host proteins (Schmitt, Connolly et al., 2016). Future experimentation will allow us to determine whether modifying the resazurin molecule will preserve activity in the OS cockroach infection model similarly to what was demonstrated in the gonococcal mouse model (Schmitt, Connolly et al., 2016). It is thought-provoking to consider how screening for in vivo activity in insects prior to substantial investments in mammalian models could change the cost profile of early stage antibiotic development efforts.
We suggest that, collectively, these results show that the OS cockroach offers significant biological and logistical advantages compared to other experimental host choices. Importantly, the OS cockroach provides researchers with a non-mammalian, thermotolerant host suitable for the examining the extracellular phase of F. tularensis pathogenesis. Thus, the OS cockroach model is an important new addition to the repertoire of invertebrate hosts for mammalian pathogens.
Acknowledgments
B.E.E. and O.M. were partially supported by NIH Grant Number 5P30 GM103332 from the National Institute of General Medicine (NIGMS) and the North Dakota State University Agricultural Research Station (NDSU ARS). Generation of the iglC mutant was funded in part by an Institutional Development Award (IDeA) from the National Institute of General Medical Sciences of the National Institutes of Health (P20GM103434) and a grant from the National Institutes of Health, National Institute of Allergy and Infectious Diseases (5K22AI087703). Generation of the dsbA and dipA mutants was supported by the National Institute of Allergy and Infectious Disease of the National Institutes of Health grants K22AI083372 and R01AI093351 to J.F.H. The contents of this manuscript are solely the responsibility of the authors and do not necessarily represent the official views of the NIH or the NDSU ARS. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Footnotes
Conflict of Interest
J.H. abstained from editorial responsibilities associated with the review of this manuscript.
Literature Cited
- Abd H, Johansson T, Golovliov I, Sandström G, Forsman M. Survival and growth of Francisella tularensis in Acanthamoeba castellanii. Appl Environ Microbiol. 2003;69:600–6. doi: 10.1128/AEM.69.1.600-606.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahlund MK, Rydén P, Sjöstedt A, Stöven S. Directed screen of Francisella novicida virulence determinants using Drosophila melanogaster. Infect Immun. 2010;78:3118–28. doi: 10.1128/IAI.00146-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmad S, Hunter L, Qin A, Mann BJ, van Hoek ML. Azithromycin effectiveness against intracellular infections of Francisella. BMC Microbiol. 2010;10:123. doi: 10.1186/1471-2180-10-123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aperis G, Fuchs BB, Anderson CA, Warner JE, Calderwood SB, Mylonakis E. Galleria mellonella as a model host to study infection by the Francisella tularensis live vaccine strain. Microbes Infect. 2007;9:729–34. doi: 10.1016/j.micinf.2007.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arvanitis M, Glavis-Bloom J, Mylonakis E. Invertebrate models of fungal infection. Biochim Biophys Acta. 2013;1832:1378–83. doi: 10.1016/j.bbadis.2013.03.008. [DOI] [PubMed] [Google Scholar]
- Bangi E. Drosophila at the intersection of infection, inflammation, and cancer. Front Cell Infect Microbiol. 2013;3:103. doi: 10.3389/fcimb.2013.00103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beetz S, Holthusen TK, Koolman J, Trenczek T. Correlation of hemocyte counts with different developmental parameters during the last larval instar of the tobacco hornworm, Manduca sexta. Arch Insect Biochem Physiol. 2008;67:63–75. doi: 10.1002/arch.20221. [DOI] [PubMed] [Google Scholar]
- Booth K, Cambron L, Fisher N, Greenlee KJ. Immune Defense Varies within an Instar in the Tobacco Hornworm, Manduca sexta. Physiol Biochem Zool. 2015;88:226–36. doi: 10.1086/680054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradburne CE, Verhoeven AB, Manyam GC, Chaudhry SA, Chang EL, Thach DC, Bailey CL, Hoek van ML. Temporal transcriptional response during infection of type II alveolar epithelial cells with Francisella tularensis live vaccine strain (LVS) supports a general host suppression and bacterial uptake by macropinocytosis. J Biol Chem. 2013;288:10780–91. doi: 10.1074/jbc.M112.362178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bröms JE, Meyer L, Sun K, Lavander M, Sjöstedt A. Unique substrates secreted by the type VI secretion system of Francisella tularensis during intramacrophage infection. PLoS One. 2012;7:e50473. doi: 10.1371/journal.pone.0050473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Browne N, Surlis C, Kavanagh K. Thermal and physical stresses induce a short-term immune priming effect in Galleria mellonella larvae. J Insect Physiol. 2014;63:21–6. doi: 10.1016/j.jinsphys.2014.02.006. [DOI] [PubMed] [Google Scholar]
- Burke DS. Immunization against tularemia: analysis of the effectiveness of live Francisella tularensis vaccine in prevention of laboratory-acquired tularemia. J Infect Dis. 1977;135:55–60. doi: 10.1093/infdis/135.1.55. [DOI] [PubMed] [Google Scholar]
- Chong A, Celli J. The Francisella intracellular life cycle: toward molecular mechanisms of intracellular survival and proliferation. Front Microbiol. 2010;1:138. doi: 10.3389/fmicb.2010.00138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chong A, Child R, Wehrly TD, Rockx-Brouwer D, Qin A, Mann BJ, Celli J. Structure-Function Analysis of DipA, a Francisella tularensis Virulence Factor Required for Intracellular Replication. PLoS One. 2013;8:e67965. doi: 10.1371/journal.pone.0067965. 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dean SN, Hoek van ML. Screen of FDA-approved drug library identifies maprotiline, an antibiofilm and antivirulence compound with QseC sensor-kinase dependent activity in Francisella novicida. Virulence. 2015;6:487–503. doi: 10.1080/21505594.2015.1046029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis DT, Inglesby TV, Henderson DA, Bartlett JG, Ascher MS, Eitzen E, Fine AD, Friedlander AM, Hauer J, Layton M, Lillibridge SR, McDade JE, Osterholm MT, O’Toole T, Parker G, Perl TM, Russell PK, Tonat K. Tularemia as a biological weapon: medical and public health management. JAMA. 2001;285:2763–73. doi: 10.1001/jama.285.21.2763. [DOI] [PubMed] [Google Scholar]
- El-Etr SH, Margolis JJ, Monack D, Robison RA, Cohen M, Moore E, Rasley A. Francisella tularensis type A strains cause the rapid encystment of Acanthamoeba castellanii and survive in amoebal cysts for three weeks postinfection. Appl Environ Microbiol. 2009;75:7488–500. doi: 10.1128/AEM.01829-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eleftherianos I, Baldwin H, ffrench-Constant RH, Reynolds SE. Developmental modulation of immunity: changes within the feeding period of the fifth larval stage in the defence reactions of Manduca sexta to infection by Photorhabdus. J Insect Physiol. 2008;54:309–18. doi: 10.1016/j.jinsphys.2007.10.003. [DOI] [PubMed] [Google Scholar]
- Ellis J, Oyston PC, Green M, Titball RW. Tularemia. Clin Microbiol Rev. 2002;15:631–46. doi: 10.1128/CMR.15.4.631-646.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher NA, Ribot WJ, Applefeld W, DeShazer D. The Madagascar hissing cockroach as a novel surrogate host for Burkholderia pseudomallei, B. mallei and B. thailandensis. BMC Microbiol. 2012;12:117. doi: 10.1186/1471-2180-12-117. Jun 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forestral CA, Malik M, Catlett SV, Savitt AG, Benach JL, Sellati TJ, Furie MB. Francisella tularensis has a significant extracellular phase in infected mice. J infect Dis. 2007;196:134–7. doi: 10.1086/518611. [DOI] [PubMed] [Google Scholar]
- Golovliov I, Sjöstedt A, Mokrievich A, Pavlov V. A method for allelic replacement in Francisella tularensis. FEMS Microbiol Lett. 2003;222:273–80. doi: 10.1016/S0378-1097(03)00313-6. [DOI] [PubMed] [Google Scholar]
- López Hernández Y, Yero D, Pinos-Rodríguez JM, Gibert I. Animals devoid of pulmonary system as infection models in the study of lung bacterial pathogens. Front Microbiol. 2015;6:38. doi: 10.3389/fmicb.2015.00038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horn L, Leips J, Starz-Gaiano M. Phagocytic ability declines with age in adult Drosophila hemocytes. Aging Cell. 2014;13:719–28. doi: 10.1111/acel.12227. Aug 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horzempa J, Carlson PE, Jr, O’Dee DM, Shanks RM, Nau GJ. Global transcriptional response to mammalian temperature provides new insight into Francisella tularensis pathogenesis. BMC Microbiol. 2008;8:172. doi: 10.1186/1471-2180-8-172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horzempa J, O’Dee DM, Shanks RM, Nau GJ. Francisella tularensis ∆pyrF mutants show that replication in nonmacrophages is sufficient for pathogenesis in vivo. Infect Immun. 2010;78:2607–19. doi: 10.1128/IAI.00134-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horzempa J, Shanks RM, Brown MJ, Russo BC, O’Dee DM, Nau GJ. Utilization of an unstable plasmid and the I-SceI endonuclease to generate routine markerless deletion mutants in Francisella tularensis. J Microbiol Methods. 2010;80:106–8. doi: 10.1016/j.mimet.2009.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaunisto S, Härkönen L, Rantala MJ, Kortet R. Early-life temperature modifies adult encapsulation response in an invasive ectoparasite. Parasitology. 2015;142:1290–6. doi: 10.1017/S0031182015000591. [DOI] [PubMed] [Google Scholar]
- Klein SL, Flanagan KL. Sex differences in immune responses. Nat Rev Immunol. 2016;16(10):626–38. doi: 10.1038/nri.2016.90. [DOI] [PubMed] [Google Scholar]
- Lai XH, Golovliov I, Sjöstedt A. Expression of IglC is necessary for intracellular growth and induction of apoptosis in murine macrophages by Francisella tularensis. Microb Pathog. 2004;37:225–30. doi: 10.1016/j.micpath.2004.07.002. [DOI] [PubMed] [Google Scholar]
- Lauriano CM, Barker JR, Yoon SS, Nano FE, Arulanandam BP, Hassett DJ, Klose KE. MglA regulates transcription of virulence factors necessary for Francisella tularensis intraamoebae and intramacrophage survival. Proc Natl Acad Sci USA. 2004;101:4246–9. doi: 10.1073/pnas.0307690101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Law HT, Sriram A, Fevang C, Nix EB, Nano FE, Guttman JA. IglC and PdpA are important for promoting Francisella invasion and intracellular growth in epithelial cells. PLoS One. 2014;9:e104881. doi: 10.1371/journal.pone.0104881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazzaro BP, Flores HA, Lorigan JG, Yourth CP. Genotype-by-environment interactions and adaptation to local temperature affect immunity and fecundity in Drosophila melanogaster. PLOS Pathog. 2008;4(3):e1000025. doi: 10.1371/journal.ppat.1000025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meylaers K, Freitak D, Schoofs L. Immunocompetence of Galleria mellonella: sex- and stage-specific differences and the physiological cost of mounting an immune response during metamorphosis. J Insect Physiol. 2007;53:146–56. doi: 10.1016/j.jinsphys.2006.11.003. [DOI] [PubMed] [Google Scholar]
- Morner T, Addison E. Tularemia. In: Williams ES, Barker IK, editors. Infectious Diseases of Wild Mammals. 3. Iowa State University Press; Ames, Iowa, USA: 2001. chapter 18. [DOI] [Google Scholar]
- Moule MG, Monack DM, Schneider DS. Reciprocal analysis of Francisella novicida infections of a Drosophila melanogaster model reveal host-pathogen conflicts mediated by reactive oxygen and imd-regulated innate immune response. PLoS Pathog. 2010;6:e1001065. doi: 10.1371/journal.ppat.1001065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plotly Technologies Inc. Collaborative data science. 2015. [Google Scholar]
- R Core Team. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing; Vienna, Austria: 2013. [Google Scholar]
- R Studio Team. RStudio: Integrated Development Environment for R. RStudio, Inc.; Boston, MA: 2015. [Google Scholar]
- Ramarao N, Nielsen-Leroux C, Lereclus D. The insect Galleria mellonella as a powerful infection model to investigate bacterial pathogenesis. J Vis Exp. 2012:e4392. doi: 10.3791/4392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ren G, Champion MM, Huntley JF. Identification of disulfide bond isomerase substrates reveals bacterial virulence factors. Mol Microbiol. 2014;94:926–44. doi: 10.1111/mmi.12808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steele S, Brunton B, Ziehr B, Taft-Benz S, Moorman N, Kawula T. Francisella tularensis harvests nutrients derived via ATG5-independent autophagy to support intracellular growth. PLoS Pathog. 2013;9:e1003562. doi: 10.1371/journal.ppat.1003562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santic M, Kwaik YA. Nutritional virulence of Francisella tularensis. Front Cell Infect Microbiol. 2013;3:112. doi: 10.3389/fcimb.2013.00112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt M, Klimentova J, Rehulka P, Straskova A, Spidlova P, Szotakova B, Stulik J, Pavkova I. Francisella tularensis subsp. holarctica DsbA homologue: a thioredoxin-like protein with chaperone function. Microbiology. 2013;159:2364–74. doi: 10.1099/mic.0.070516-0. [DOI] [PubMed] [Google Scholar]
- Schmitt DM, Barnes R, Rogerson T, Haught A, Mazzella LK, Ford M, Gilson T, Birch JW-M, Sjöstedt A, Reed DS, Franks JM, Stolz DB, Denvir J, Fan J, Rekulapally S, Primerano DA, Horzempa J. The role and mechanism of erythrocyte invasion by Francisella tularensis. Frontiers in Cellular and Infection Microbiology. 2017;7:1–173. doi: 10.3389/fcimb.2017.00173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmitt DM, Connolly KL, Jerse AE, Detrick MS, Horzempa J. Antibacterial activity of resazurin-based compounds against Neisseria gonorrhoeae in vitro and in vivo. Int J Antimicrob Agents. 2016;48(4):367–72. doi: 10.1016/j.ijantimicag.2016.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmitt DM, O’Dee DM, Cowan BN, Birch JW, Mazzella LK, Nau GJ, Horzempa J. The use of resazurin as a novel antimicrobial agent against Francisella tularensis. Front Cell Infect Microbiol. 2013;3:93. doi: 10.3389/fcimb.2013.00093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaik HA, Sehnal F. Hemolin expression in the silk glands of Galleria mellonella in response to bacterial challenge and prior to cell disintegration. J Insect Physiol. 2009;55:781–7. doi: 10.1016/j.jinsphys.2009.04.010. [DOI] [PubMed] [Google Scholar]
- Silva MT, Pestana NT. The in vivo extracellular life of facultative intracellular bacterial parasites: role in pathogenesis. Immunobiology. 2013;218:325–37. doi: 10.1016/j.imbio.2012.05.011. [DOI] [PubMed] [Google Scholar]
- Sprynski N, Valade E, Neulat-Ripoll F. Galleria mellonella as an infection model for select agents. Methods Mol Biol. 2014;1197:3–9. doi: 10.1007/978-1-4939-1261-2_1. [DOI] [PubMed] [Google Scholar]
- Therneau TM, Grambsch PM. Modeling Survival Data: Extending the Cox Model. Springer; New York: 2000. [Google Scholar]
- Therneau TM. A Package for Survival Analysis in S. version 2.38. 2015. [Google Scholar]
- Tian L, Guo E, Diao Y, Zhou S, Peng Q, Cao Y, Ling E, Li S. Genome-wide regulation of innate immunity by juvenile hormone and 20-hydroxyecdysone in the Bombyx fat body. BMC Genomics. 2010;11:549. doi: 10.1186/1471-2164-11-549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torson AS, Yocum GD, Rinehart JP, Kemp WP, Bowsher JH. Transcriptional responses to fluctuating thermal regimes underpinning differences in survival in the solitary bee Megachile rotundata. J Exp Biol. 2015;218:1060–8. doi: 10.1242/jeb.113829. [DOI] [PubMed] [Google Scholar]
- Verma P, Tapadia MG. Immune response and anti-microbial peptides expression in Malpighian tubules of Drosophila melanogaster is under developmental regulation. PLoS One. 2012;7:e40714. doi: 10.1371/journal.pone.0040714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss DS, Brotcke A, Henry T, Margolis JJ, Chan K, Monack DM. In vivo negative selection screen identifies genes required for Francisella virulence. Proc Natl Acad Sci U S A. 2007;104:6037–42. doi: 10.1073/pnas.0609675104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woltedji D, Fang Y, Han B, Feng M, Li R, Lu X, Li J. Proteome analysis of hemolymph changes during the larval to pupal development stages of honeybee workers (Apis mellifera ligustica) J Proteome Res. 2013;12:5189–98. doi: 10.1021/pr400519d. [DOI] [PubMed] [Google Scholar]
- Wu X, Ren G, Huntley JF. Generating Isogenic Deletions (Knockouts) in Francisella tularensis, a Highly-infectious and Fastidious Gram-negative Bacterium. Bio Protoc. 2015;5:e1500. doi: 10.21769/bioprotoc.1500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu Q, Lu A, Xiao G, Yang B, Zhang J, Li X, Guan J, Shao Q, Beerntsen BT, Zhang P, Wang C, Ling E. Transcriptional profiling of midgut immunity response and degeneration in the wandering silkworm, Bombyx mori. PLoS One. 2012;7:e43769. doi: 10.1371/journal.pone.0043769. [DOI] [PMC free article] [PubMed] [Google Scholar]


