Abstract
OBJECTIVE
The Qatar Study was designed to examine the efficacy of combination therapy with exenatide plus pioglitazone versus basal/bolus insulin in patients with long-standing poorly controlled type 2 diabetes mellitus (T2DM) on metformin plus a sulfonylurea.
RESEARCH DESIGN AND METHODS
The study randomized 231 patients with poorly controlled (HbA1c >7.5%, 58 mmol/mol) T2DM on a sulfonylurea plus metformin to receive 1) pioglitazone plus weekly exenatide (combination therapy) or 2) basal plus prandial insulin (insulin therapy) to maintain HbA1c <7.0% (53 mmol/mol).
RESULTS
After a mean follow-up of 12 months, combination therapy caused a robust decrease in HbA1c from 10.0 ± 0.6% (86 ± 5.2 mmol/mol) at baseline to 6.1 ± 0.1% (43 ± 0.7 mmol/mol) compared with 7.1 ± 0.1% (54 ± 0.8 mmol/mol) in subjects receiving insulin therapy. Combination therapy was effective in lowering the HbA1c independent of sex, ethnicity, BMI, or baseline HbA1c. Subjects in the insulin therapy group experienced significantly greater weight gain and a threefold higher rate of hypoglycemia than patients in the combination therapy group.
CONCLUSIONS
Combination exenatide/pioglitazone therapy is a very effective and safe therapeutic option in patients with long-standing poorly controlled T2DM on metformin plus a sulfonylurea.
Introduction
The diagnosis of type 2 diabetes mellitus (T2DM) is made based on the plasma glucose concentration. However, progressive β-cell failure and insulin resistance are the principal core defects responsible for development and progression of hyperglycemia in individuals with T2DM (1). Nonetheless, hyperglycemia is the major factor responsible for retinopathy and nephropathy, and every 1% decrease in HbA1c is associated with an ∼35% reduction in risk of microvascular complications (2–5). Microvascular complications are uncommon if the HbA1c is maintained at less than 6.5–7.0% (48–53 mmol/mol) (4). Therefore, the standard of diabetes care recommends maintaining the HbA1c at <7.0% (53 mmol/mol) to minimize the microvascular risk in patients with T2DM (6).
Metformin is the most commonly used first-line antidiabetic agent in T2DM (6). It lowers HbA1c by inhibiting hepatic glucose production (7.8). Because metformin does not halt or prevent the progressive β-cell failure (9,10), after an initial decrease, the HbA1c rises progressively over time. Although the American Diabetes Association (ADA) recommends several therapeutic options in patients in whom metformin is failing, sulfonylureas remains the most commonly used second-line therapy, and similar to metformin, they also lack protective effect on β-cell function (3,9,10).
Insulin is very effective in lowering the plasma glucose concentration, but requires an injection and home glucose monitoring, causes hypoglycemia, and promotes weight gain (11). Nonetheless, insulin is the recommended therapeutic option in patients with poorly controlled T2DM when multiple oral agents fail (e.g., metformin plus a sulfonylurea) (6).
Progressive β-cell failure, weight gain, and hypoglycemia remain major obstacles in maintaining HbA1c within the normal range (2,11), including with insulin therapy. Further, recent clinical trials have reported that hypoglycemia is associated with increased mortality risk (11). This presents a dilemma in patients with poorly controlled T2DM between lowering HbA1c to prevent microvascular complications and minimizing the risk of hypoglycemia. The ADA recommends “lowering HbA1c to <7.0% (53 mmol/mol) in most patients and more stringent targets (6.0–6.5%) (42–48 mmol/mol) in selected patients if achieved without hypoglycemia” (6).
Thiazolidinediones are potent insulin sensitizers (12), improve β-cell function (13–17), and as reviewed by DeFronzo (1), clinical trials have demonstrated durable HbA1c reduction with lower risk of hypoglycemia compared with sulfonylureas (10,18,19).
GLP-1 (glucagon-like peptide 1) receptor agonists (RA) improve β-cell function (20), an effect that lasts for up to 3 years (21). Thus, they produce a durable reduction in HbA1c with a low risk of hypoglycemia.
We recently demonstrated that the addition of exenatide plus pioglitazone, which improve insulin sensitivity and β-cell function, to metformin in patients with newly diagnosed T2DM produces a greater and more durable reduction in the HbA1c and a lower risk of hypoglycemia than the recommended sequential add-on of metformin, followed by a sulfonylurea and insulin (22). Subjects who were started on metformin/pioglitazone/exenatide at the time of diagnosis of T2DM maintained a mean HbA1c of 5.9% (41 mmol/mol) for 2 years compared with HbA1c of 6.5% (48 mmol/mol) in patients in whom metformin, a sulfonylurea, and insulin were sequentially added (22). The group with triple therapy with metformin/pioglitazone/exenatide also experienced much less hypoglycemia and weight gain than the group receiving sequential addition of metformin, followed by glipizide and then a progressively increasing daily dose of glargine insulin (22).
Millions of patients with poorly controlled T2DM worldwide are currently treated with metformin plus a sulfonylurea. Although a third oral agent (e.g., DPP-4 inhibitor) can be added to improve their glycemic control, because of advanced β-cell failure (1), insulin therapy is the most commonly used addition in those patients with poorly controlled T2DM on multiple oral agents.
The aim of the current study was to compare the efficacy and safety of combination therapy with GLP-1 RA plus thiazolidinedione, which correct the major metabolic defects responsible for the development of progressive hyperglycemia in T2DM (1), versus basal/bolus insulin in patients with long-standing poorly controlled T2DM treated with maximum doses of metformin plus sulfonylurea.
Research Design and Methods
The Qatar Study is an open label, single-center, randomized control trial (ClinicalTrials.gov identifier NCT02887625) that examines the efficacy, durability, and safety of combination therapy with exenatide plus pioglitazone versus basal/bolus insulin in patients with poorly controlled T2DM on metformin plus a sulfonylurea. This is an ongoing study at Hamad General Hospital, Doha, Qatar. Here we report the effect of each therapy on glycemic control and safety parameters at a mean of 1 year of follow-up (range, 6–18 months). The study protocol was approved by the Hamad General Hospital Institutional Review Board, and informed written consent was obtained before patient enrollment.
Subjects
Subjects with poorly controlled (HbA1c >7.5% [58 mmol/mol]) T2DM (age 18–75 years) treated with a maximal/nearly maximal dose of metformin (>1,500 mg/day) plus a sulfonylurea (>4 mg glimepiride or >60 mg gliclazide) were recruited. Patients were in good general health as determined by medical history and physician examination. Participants had normal kidney and liver function, serum chemistry results, electrocardiogram results, and urinalysis, stable body weight (± 3 pounds within preceding year), and a negative pregnancy test. Exclusion criteria were a hematocrit <34%, medications known to affect glucose metabolism other than sulfonylureas and metformin, evidence of diabetic proliferative retinopathy, albumin excretion >300 mg/day, and major organ system disease, as determined by physical examination, medical history, and screening blood tests.
Study Design
Eligible subjects were consecutively randomized by age, sex, BMI, diabetes duration, and HbA1c to receive pioglitazone/exenatide (combination therapy) or basal (glargine)/bolus (aspart) insulin (insulin therapy) to maintain HbA1c <7% (53 mmol/mol). There was no limit on the upper value of HbA1c for enrollment (range of initial HbA1c was 7.5−15.1% [58–142 mmol/mol]).
Subjects randomized to combination therapy were started on weekly exenatide injection (2 mg/week extended-release exenatide [BYDUREON] administered with a pen), and pioglitazone (15 mg/day) was added at week 2, and the dose was increased to 30 mg/day at week 4. Subjects receiving insulin therapy were started on insulin glargine before breakfast. The Treat-to-Target Trial (4T) algorithm was used to calculate the starting glargine dose, and the dose was adjusted weekly to achieve a fasting plasma glucose (FPG) of <110 mg/dL. After the FPG goal was achieved, if the HbA1c was >7.0% (53 mmol/mol), 4–6 units of insulin aspart was started before each meal, and the dose was adjusted to a achieve a plasma glucose concentration of <140 mg/dL at 2 hours after meals.
Patients were seen monthly during the first 4 months or as needed, based on the results of the plasma glucose concentration, and bimonthly thereafter. FPG, body weight, and HbA1c were measured at each follow-up visit, and the medication dose was adjusted to maintain a FPG <110 mg/dL, 2-h postprandial plasma glucose <140 mg/dL, and HbA1c <7% (53 mmol/mol), unless hypoglycemia (blood glucose was <60 mg/dL or symptoms) was encountered. Hypoglycemia was defined as blood glucose concentration of <60 mg/dL, with or without symptoms, or hypoglycemia symptoms that subsided after glucose ingestion. Patients were instructed to perform a 7-point home blood glucose profile level (One Touch, VivaCheck, Wilmington, DE) before and 2 h after a meal and at bedtime 1 day each week. Blood glucose levels measured at home were downloaded at each follow-up visit and verified by the study coordinator. During each follow-up visit, FPG was measured, records of glucose values measured at home were reviewed, and patients were questioned about symptoms of hypoglycemia. Severe hypoglycemia was defined as hypoglycemia requiring third-party assistance. Down titration of medications was allowed to avoid hypoglycemia. If more than three hypoglycemic events per visit on two consecutive visits were encountered, down titration, usually of the sulfonylurea, was done to lower the risk of hypoglycemic events.
Data Analysis and Statistical Analysis
Primary end point was the HbA1c difference between subjects receiving combination therapy and those receiving insulin therapy. Because all patients (N = 231) in the study completed at least 6 months of follow-up, the full effect of therapy on the HbA1c in each treatment arm was achieved. Therefore, the values of HbA1c available at the last follow-up visit (range 6–18 months) were used for the final analysis. Secondary end points included 1) percentage of subjects achieving HbA1c <6.5% (48 mmol/mol) and <7.0% (53 mmol/mol); 2) decrease in FPG concentration; 3) change in body weight; and 4) rate of hypoglycemic events.
The mean value of pre- and postmeal home blood glucose measurements at the last follow-up (range 6–18 months) was used for analysis. Postprandial plasma glucose excursion was calculated as the incremental area above the FPG concentration according to the trapezoid rule.
Overall frequency of hypoglycemia was calculated as total number of hypoglycemic events divided by number of patient-years of follow-up in each arm. The percentage of subjects experiencing hypoglycemia was calculated as number of subjects experiencing at least a single event divided by number of patients in that arm.
Values are presented as mean ± SEM. The two-sided t test was used to compare mean differences between the two treatment arms. The χ2 test was used to test the significance of discrete variables.
The study was powered to detect a 0.55% HbA1c difference between treatment arms based on HbA1c difference in our previous Efficacy and Durability of Initial Combination Therapy for Type 2 Diabetes (EDICT) study (22). The EDICT study randomized, patients with new-onset diabetes to receive initial combination therapy with metformin/pioglitazone/exenatide versus sequential add-on of metformin, followed by a sulfonylurea and insulin. At 2 years, >80% of subjects in the sequential add-on therapy group were receiving more than one agent, and subjects who received initial triple therapy had 0.55% lower HbA1c. From these results we assumed that subjects with combination therapy (pioglitazone plus exenatide) would achieve a lower HbA1c by ≥0.55% versus subjects receiving metformin, sulfonylurea, and insulin. We computed that 156 subjects per arm would provide 90% power to detect a 0.55% HbA1c difference between treatment arms at α < 0.05.
Results
The study screened 296 patients and randomized 251 eligible patients, of whom 129 were randomized to combination therapy and 122 to insulin therapy. Six patients in the combination therapy arm and 14 patients in the insulin arm dropped out of the study. This report presents the results of a mean follow-up of 1 year (range, 6–18 months) for 123 patients in the combination therapy group and 108 in the insulin therapy group. Supplementary Figure 1 presents the randomization scheme.
Table 1 presents the baseline characteristics of study participants. Patients in both groups were well matched in age, sex, BMI, disease duration, and baseline HbA1c. Patients were a mean age of 52 ± 1, were mildly obese, had poor glycemic control, with mean baseline HbA1c of 10.0% (86 mmol/mol), and mean diabetes duration of 10.7 years.
Table 1.
Baseline characteristics of study participants
| Combination therapy n = 123 | Insulin therapy n = 108 | P value | |
|---|---|---|---|
| Age (years) | 52 ± 1 | 52 ± 1 | NS |
| Male sex (%) | 40 | 37 | NS |
| BMI (kg/m2) | 31.1 ± 0.5 | 30.5 ± 0.5 | NS |
| Diabetes duration (years) | 10.5 ± 0.5 | 10.9 ± 0.5 | NS |
| HbA1c (%) | 10.0 ± 0.6 | 10.0 ± 0.5 | NS |
| HbA1c (mmol/mol) | 86 ± 5.2 | 86 ± 4.8 | |
| FPG (mg/dL) | 231 ± 8 | 237 ± 7 | NS |
| Ethnicity (%) | |||
| Qataris | 48 | 39 | NS |
| Non-Qatari Arabs | 26 | 29 | NS |
| Asian Indians | 17 | 25 | NS |
| Others | 9 | 7 | NS |
| Background therapy | |||
| Metformin, mg (% of patients) | 1,908 (100) | 1,953 (100) | NS |
| Gliclazide, mg (% of patients) | 101 (58) | 106 (55) | NS |
| Glimepiride, mg (% of patients) | 7.4 (42) | 7.2 (45) | NS |
NS, not significant.
All patients were receiving therapy with metformin. The mean metformin dose was 1,908 ± 50 and 1,953 ± 52 mg/day in combination and insulin therapy groups, respectively. Similarly, all patients were being treated with a sulfonylurea: 58% and 55% of patients were on gliclazide and 42% and 45% of patients were on glimepiride in the combination and insulin therapy groups, respectively. During the study, the sulfonylurea dose could be adjusted downward if symptomatic/biochemical hypoglycemia was experienced. Supplementary Figure 2 demonstrates that the reduction in the sulfonylurea dose was comparable in both treatment groups.
The mean follow-up duration was 12.4 ± 0.5 and 12.1 ± 0.5 months in the combination therapy and insulin therapy groups, respectively.
The mean insulin dose in subjects receiving insulin therapy is shown in Supplementary Fig. 3. The mean glargine dose was 40 ± 1, 47 ± 1, and 47 ± 2 units/day at 6, 12, and 18 months, respectively, and the mean prandial insulin (aspart) dose was 28 ± 1, 40 ± 2, and 49 ± 2 units/day, respectively. Thus, patients in the insulin therapy group received an average of ∼1.1 units/kg of insulin daily.
Primary Outcome
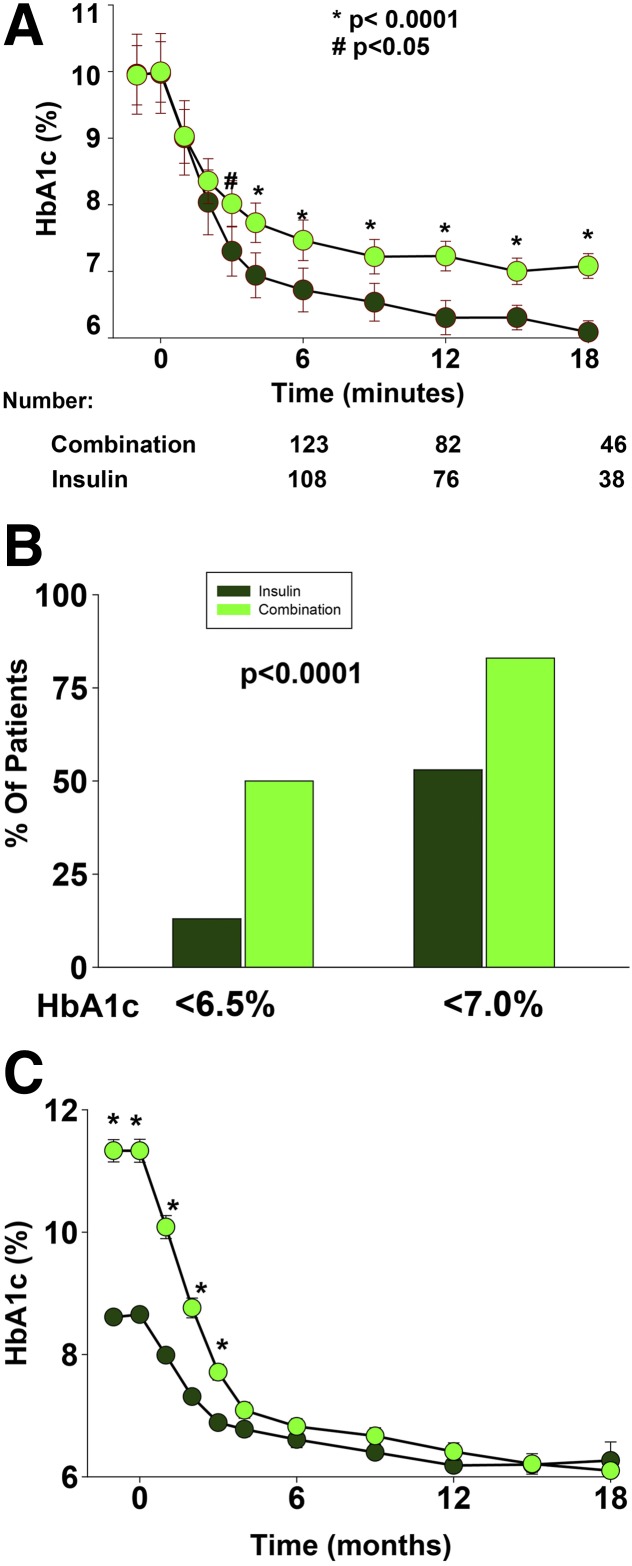
The primary outcome was the HbA1c difference between the two treatment arms (Fig. 1A). Baseline HbA1c was identical in both groups (10.0% [86 mmol/mol]) and progressively decreased in both treatment groups during the first 6 months. However, the decrease in HbA1c was greater in subjects receiving combination therapy. At 6 months, there was a statistically significant difference in the HbA1c (0.7%, P < 0.0001) between the combination therapy (6.7% [50 mmol/mol]) and insulin therapy (7.4% [57 mmol/mol]) groups. After 6 months, HbA1c continued to decrease in both groups; however, the difference in HbA1c continued to widen with time (0.9 at 12 months and 1% at 18 months, both P < 0.0001).
Figure 1.
Effect of combination therapy and insulin therapy on glycemic control. A: The change over time in the mean HbA1c is shown in subjects receiving combination therapy or insulin therapy. B: The percentage of subjects is shown in each treatment group achieving HbA1c <7.0% (53 mmol/mol) and 6.5% (48 mmol/mol). C: The change in HbA1c over time is shown in subjects in the combination therapy group stratified by baseline HbA1c into the upper 50% (n = 62) and lower 50% (n = 61). *P < 0.0001; **P = 0.001.
More subjects receiving combination therapy achieved the ADA treatment goal (HbA1c <7.0% [53 mmol/mol]) versus those receiving insulin therapy (83% vs. 53%, P = 0.003) (Fig. 1B). Similarly, more patients achieved HbA1c <6.5 (48 mmol/mol) in the combination therapy group (50% vs. 13%, P < 0.0001).
To examine the efficacy of combination therapy on glycemic control in relation to baseline HbA1c, we divided subjects into two equal groups by their starting HbA1c. Subjects in the upper half (HbA1c >9.5% [80 mmol/mol], n = 62) had a mean baseline HbA1c of 11.3 ± 0.2% (100 mmol/mol) compared with a mean HbA1c of 8.5 ± 0.1% (69 mmol/mol) in subjects in the lower half (HbA1c 7.5–9.5% [58–80 mmol/mol], n = 61). Figure 2C demonstrates that the combination therapy was equally effective in lowering the HbA1c in both treatment groups independent of baseline HbA1c. After 3 months, the difference in HbA1c in subjects in the upper half was not statistically different from the mean HbA1c in subjects in the lower half. Similarly, combination therapy was equally effective in lowering the HbA1c in the three ethnic groups in the study (Qatari nationals, non-Qatari Arabs, and Indians) (Supplementary Fig. 4). The efficacy of combination therapy in lowering HbA1c was independent of age, sex, BMI, or diabetes duration.
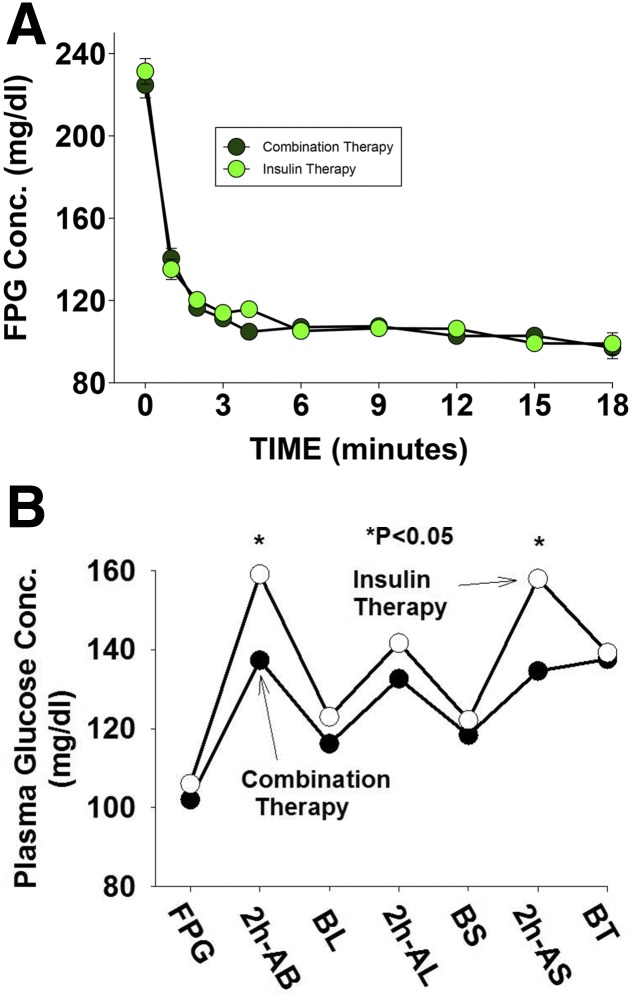
Figure 2.
Effect of combination therapy and insulin therapy on FPG concentration (Conc.) (A) and postprandial plasma glucose concentration (B) in The Qatar Study. AB, after breakfast; AL, after lunch; AS, after supper; BL, before lunch; BS, before supper; BT, bedtime.
Fasting and Postprandial Glucose
Baseline FPG was similar in the combination and insulin therapy groups (224 ± 7 vs. 234 ± 7 mg/dL, respectively; P = not significant) and decreased rapidly after therapy started (Fig. 2A). The decrease in HbA1c was similar in both groups (Fig. 2A), and at 6 months, the FPG was 107 ± 2 vs. 105 ± 3 mg/dL (P = not significant) in the combination and insulin therapy groups, respectively.
Figure 2B depicts the postprandial plasma glucose excursion curves in subjects in the combination and insulin therapy groups. Subjects in the combination therapy group experienced a lower postmeal plasma glucose concentration. The mean incremental area under the curve for the plasma glucose concentration during the day was 28% lower in subjects receiving combination therapy (410 ± 17 vs. 536 ± 23 mg/dL/h in the insulin therapy group; P < 0.01). Further, the plasma glucose concentration after breakfast and dinner was significantly lower in subjects receiving combination therapy compared with insulin therapy (Fig. 2B).
Body Weight
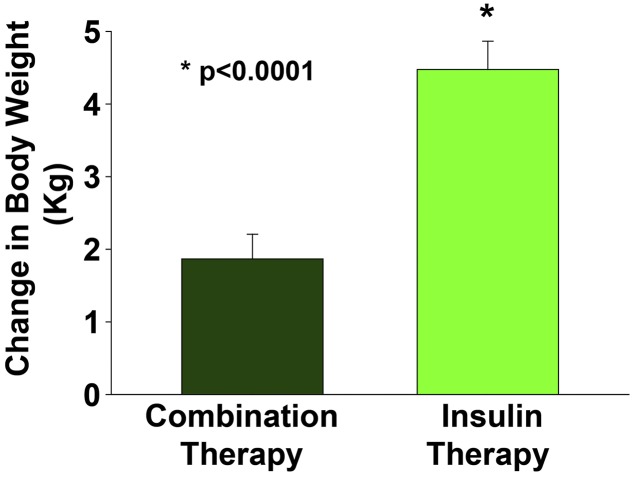
The mean body weight increased in both groups. However, subjects in the combination therapy group experienced half as much weight gain as subjects in the insulin therapy group (2.1 ± 1.1 vs. 4.2 ± 1.0 kg, P < 0.0001) (Fig. 3).
Figure 3.
Effect of combination therapy and insulin therapy on body weight.
Adverse Events
In general, both treatments were well tolerated, and a small number (<2%) of patients dropped out of the study because of adverse events. At least one adverse event occurred in ∼90% of patients in both groups (Supplementary Table 1); most adverse events were mild and unrelated to study treatment. Hypoglycemia was the most common adverse events related to study treatments, being reported by 91% and 66% of participants receiving insulin therapy and combination therapy, respectively. The overall frequency of hypoglycemic events was approximately threefold greater in the insulin therapy versus combination therapy group (2.3 vs. 6.6 events per patient-year, P < 0.0001). All hypoglycemic events were mild, and the only episode of severe hypoglycemia occurred in a subject in the insulin therapy group.
Two subjects in the combination therapy group experienced a local reaction at the injection site. Subjects receiving combination therapy experienced more frequent gastrointestinal adverse effects and ankle edema. Nausea occurred in 31% of combination therapy subjects at the initiation of exenatide therapy; the nausea was mild and subsided after 2–3 months. Only two patients discontinued treatment as a result of nausea.
The incidence of peripheral edema was low, at 3.4% vs. 9.3% in insulin and combination therapy, respectively. Peripheral edema was mild and easily controlled with the addition of a distally acting diuretic. Two patients discontinued combination therapy because of peripheral edema.
There were no cases of congestive heart failure. Five cardiovascular events occurred (4 myocardial infarctions, 1 of which was fatal; and 1 cerebrovascular accident). The five subjects with cardiovascular disease (CVD) events were in the insulin therapy group. No CVD events were recorded in the combination therapy group. The number of subjects who withdrew because of adverse events was small: four receiving combination therapy and none receiving insulin therapy.
Conclusions
The major new finding of the current study is that combination therapy with pioglitazone plus exenatide produces a robust reduction in the HbA1c in patients with poorly controlled (mean HbA1c 10% [86 mmol/mol]) long-standing (mean duration of 10 years) T2DM treated with maximal/nearly maximal doses of metformin plus a sulfonylurea.
It should be noted that subjects in both treatment arms, despite very poor glycemic control at baseline (HbA1c 10% [86 mmol/mol]), generally experienced very good glycemic control. As anticipated, insulin therapy, which is very powerful in lowering the plasma glucose concentration, produced a robust reduction in mean HbA1c (∆ = 2.9%), and half of the subjects receiving insulin therapy achieved the ADA treatment goal of HbA1c <7.0% (53 mmol/mol) without significant hypoglycemia. The mean FPG concentration in insulin-treated subjects reached the target (110 mg/dL) at ∼2 months, confirming rigorous insulin intensification in the insulin-treated group. However, the glycemic goal (HbA1c<7.0% [53 mmol/mol]) was achieved in only half of the patients because hypoglycemia precluded further escalation of the insulin dose. Subjects receiving combination therapy experienced a more robust reduction in mean HbA1c (∆ = 3.9%). Because neither pioglitazone nor exenatide are associated with an increased risk of hypoglycemia, subjects receiving combination therapy experienced a threefold lower risk of hypoglycemia despite an HbA1c that was 1% lower compared with the insulin therapy group. Of note, most of the hypoglycemic events in subjects receiving combination therapy were related to the use of sulfonylureas, because down titration or stopping the sulfonylurea in these patients eliminated most of the hypoglycemic events.
The combination of pioglitazone plus exenatide was very effective in lowering the HbA1c independent of ethnicity, BMI, sex, or baseline HbA1c. Remarkably, the HbA1c in subjects in the upper half of the HbA1c range (baseline HbA1c 9.5–15% [80–140 mmol/mol], mean 11.3% [100 mmol/mol]) in the combination therapy group decreased at 4 months to the same level as patients with baseline HbA1c between 7.5 and 9.5% (58 and 80 mmol/mol) (mean HbA1c 8.5% [69 mmol/mol]); there was no difference in the mean HbA1c between groups after 3 months (Fig. 1C). These results demonstrate that the combination of once-weekly exenatide plus pioglitazone, antidiabetic agents that have been shown in previous studies to correct the underlying core defects responsible for the development of hyperglycemia in T2DM (i.e., β-cell dysfunction and insulin resistance) (12–20), reduces the mean plasma glucose concentration close to the normal range, regardless of the starting HbA1c, and with a low risk of hypoglycemia.
Subjects receiving combination therapy experienced half of the weight gain compared with subjects receiving insulin therapy (2.1 vs. 4.2 kg) (Fig. 3). Although pioglitazone therapy resulted in weight gain, 32% of patients receiving combination therapy experienced weight loss compared with only 13% (P < 0.01) in the insulin treatment group. This most likely is explained by the concomitant use of exenatide, which is well documented to suppress appetite and cause weight loss (20,21). It also should be pointed out that with pioglitazone, the greater the weight gain, the greater are the improvements in HbA1c, insulin sensitivity, and β-cell function (17).
Both treatments were well tolerated, and few subjects (<3% in combination therapy; 0% in insulin therapy) withdrew because of adverse events. Most of the adverse events were mild and unrelated to study treatment. Hypoglycemia was the most common adverse event; the absolute hypoglycemia rate was relatively low (Supplementary Table 1) compared with other studies that have used intensive insulin therapy in T2DM (23–25). The relatively low rate of peripheral edema (Supplementary Table 1) with combination therapy most likely is explained by the lower dose of pioglitazone (30 mg/day) used in the current study. The natriuretic effect of exenatide also could have reduced the incidence of peripheral edema. Most of edema that occurred was mild and easily controlled with the addition of a distally acting diuretic to the treatment regimen. Only two subjects discontinued combination therapy because of ankle edema. No congestive heart failure or fractures occurred in either group.
Although the study was not powered to detect the effect of therapy on cardiovascular events, five cardiovascular events, one fatal, occurred in the insulin therapy group. Because of the small sample size in the current study and short follow-up duration, it is impossible to determine whether this result was due to chance or to a potential protective cardiovascular effect of pioglitazone (26) or GLP-1 RA (27), both of which have been shown to reduce CVD events, but longer monitoring will be required to see the CVD benefit. A much larger and longer cardiovascular outcome study will be required to answer this question.
The current study has several limitations. The therapies used (weekly exenatide and multiple daily insulin injections) prohibited the study from being blinded. Because study was performed in a single center, it included a relatively small number of participants, primarily of Arab origin (∼70% of participants). Thus, a larger multiethnic study is warranted to examine the generalizability of this novel treatment approach in individuals with poorly controlled, long-standing T2DM. Further, longer follow-up is required to determine the durability of glycemic control achieved in the combination therapy group. Whether the HbA1c difference (6.1% [43 mmol/mol] in combination therapy vs. 7.1% [54 mmol/mol] in insulin therapy) in this range of HbA1c will be translated into greater prevention of diabetic microvascular complications also remains to be determined.
Nonetheless, the present results are impressive and, contrary to standard dogma, demonstrate that even in individuals with very poorly controlled, long-standing T2DM, combination therapy with a GLP-1 RA plus pioglitazone can achieve nearly normal/normal HbA1c levels. We believe that the robust results observed in the current study should foster a larger multiethnic study with longer duration to validate the findings in the current study and examine their benefit on diabetic microvascular and macrovascular complications.
In summary, the present results demonstrate that combination therapy with pioglitazone plus exenatide is a very effective and safe therapeutic option in patients with poorly controlled, long-standing T2DM on metformin plus a sulfonylurea. Continued follow-up will be required to ascertain how long the beneficial effects of combination therapy are maintained.
Supplementary Material
Article Information
Acknowledgments. The authors thank Evette Ibrahim, RN, Sanaa Mansy, RN, and Huda Mejri, RN, (Hamad General Hospital) for their excellent care of patients and Huda Esam, Mariam Al-Malaheem, and Kirollos Magdi (Hamad General Hospital) for technical and logistic support throughout the study. The authors also thank the pharmacy team led by Dr. Enas Abdoun and the team of diabetes educators at Hamad General Hospital for dispensing the study medications and for training patients on the use of insulin and BYDUREON pens, respectively.
Funding. This study was supported by a Qatar Foundation grant NPRP 5-273-3-079. R.A.D.’s salary is paid in part by the South Texas Veterans Health Care System.
Duality of Interest. R.A.D. is on the advisory boards of AstraZeneca, Novo Nordisk, Janssen, Intarcia, and Boehringer-Ingelheim; receives research support from Bristol-Myers Squibb, Boehringer-Ingelheim, Takeda, and AstraZeneca; and is on the speaker's bureaus of Novo Nordisk and AstraZeneca. AstraZeneca provided the exenatide. No other potential conflicts of interest relevant to this article were reported.
Author Contributions. M.A.-G. designed the study, wrote the protocol, contributed to data generation and data analysis, and wrote the manuscript. O.M., A.M., J.A., and C.T. generated the data. R.A.D., M.Z., and A.J. reviewed and revised the manuscript. M.A.-G. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
Clinical trial reg. no. NCT02887625, clinicaltrials.gov.
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc16-1738/-/DC1.
This article is featured in a podcast available at http://www.diabetesjournals.org/content/diabetes-core-update-podcasts.
References
- 1.DeFronzo RA. Banting Lecture. From the triumvirate to the ominous octet: a new paradigm for the treatment of type 2 diabetes mellitus. Diabetes 2009;58:773–795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.The Diabetes Control and Complications Trial Research Group The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 1993;329:977–986 [DOI] [PubMed] [Google Scholar]
- 3.UK Prospective Diabetes Study (UKPDS) Group Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet 1998;352:837–853 [PubMed] [Google Scholar]
- 4.Nakagami T, Kawahara R, Hori S, Omori Y. Glycemic control and prevention of retinopathy in Japanese NIDDM patients. A 10-year follow-up study. Diabetes Care 1997;20:621–622 [DOI] [PubMed] [Google Scholar]
- 5.Klein R, Klein BE, Moss SE. Relation of glycemic control to diabetic microvascular complications in diabetes mellitus. Ann Intern Med 1996;124:90–96 [DOI] [PubMed] [Google Scholar]
- 6.Inzucchi SE, Bergenstal RM, Buse JB, et al.; American Diabetes Association (ADA); European Association for the Study of Diabetes (EASD) . Management of hyperglycemia in type 2 diabetes: a patient-centered approach: position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care 2012;35:1364–1379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.DeFronzo RA, Goodman AM; The Multicenter Metformin Study Group . Efficacy of metformin in patients with non-insulin-dependent diabetes mellitus. N Engl J Med 1995;333:541–549 [DOI] [PubMed] [Google Scholar]
- 8.Rossetti L, DeFronzo RA, Gherzi R, et al. . Effect of metformin treatment on insulin action in diabetic rats: in vivo and in vitro correlations. Metabolism 1990;39:425–435 [DOI] [PubMed] [Google Scholar]
- 9.Kahn SE, Haffner SM, Heise MA, et al.; ADOPT Study Group . Glycemic durability of rosiglitazone, metformin, or glyburide monotherapy. N Engl J Med 2006;355:2427–2443 [DOI] [PubMed] [Google Scholar]
- 10.United Kingdom Prospective Diabetes Study (UKPDS) United Kingdom Prospective Diabetes Study (UKPDS). 13: relative efficacy of randomly allocated diet, sulphonylurea, insulin, or metformin in patients with newly diagnosed non-insulin dependent diabetes followed for three years. BMJ 1995;310:83–88 [PMC free article] [PubMed] [Google Scholar]
- 11.Seaquist ER, Anderson J, Childs B, et al. . Hypoglycemia and diabetes: a report of a workgroup of the American Diabetes Association and the Endocrine Society. Diabetes Care 2013;36:1384–1395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bays H, Mandarino L, DeFronzo RA. Role of the adipocyte, free fatty acids, and ectopic fat in pathogenesis of type 2 diabetes mellitus: peroxisomal proliferator-activated receptor agonists provide a rational therapeutic approach. J Clin Endocrinol Metab 2004;89:463–478 [DOI] [PubMed] [Google Scholar]
- 13.Rasouli N, Kern PA, Reece EA, Elbein SC. Effects of pioglitazone and metformin on beta-cell function in nondiabetic subjects at high risk for type 2 diabetes. Am J Physiol Endocrinol Metab 2007;292:E359–E365 [DOI] [PubMed] [Google Scholar]
- 14.Xiang AH, Peters RK, Kjos SL, et al. . Effect of pioglitazone on pancreatic beta-cell function and diabetes risk in Hispanic women with prior gestational diabetes. Diabetes 2006;55:517–522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jin J, Yu Y, Yu H, Wang C, Zhang X. Effects of pioglitazone on beta-cell function in metabolic syndrome patients with impaired glucose tolerance. Diabetes Res Clin Pract 2006;74:233–241 [DOI] [PubMed] [Google Scholar]
- 16.DeFronzo RA, Tripathy D, Schwenke DC, et al.; ACT NOW Study . Pioglitazone for diabetes prevention in impaired glucose tolerance. N Engl J Med 2011;364:1104–1115 [DOI] [PubMed] [Google Scholar]
- 17.Gastaldelli A, Ferrannini E, Miyazaki Y, Matsuda M, Mari A, DeFronzo RA. Thiazolidinediones improve beta-cell function in type 2 diabetic patients. Am J Physiol Endocrinol Metab 2007;292:E871–E883 [DOI] [PubMed] [Google Scholar]
- 18.Mazzone T, Meyer PM, Feinstein SB, et al. . Effect of pioglitazone compared with glimepiride on carotid intima-media thickness in type 2 diabetes: a randomized trial. JAMA 2006;296:2572–2581 [DOI] [PubMed] [Google Scholar]
- 19.Hanefeld M, Pfützner A, Forst T, Lübben G. Glycemic control and treatment failure with pioglitazone versus glibenclamide in type 2 diabetes mellitus: a 42-month, open-label, observational, primary care study. Curr Med Res Opin 2006;22:1211–1215 [DOI] [PubMed] [Google Scholar]
- 20.Drucker DJ. The biology of incretin hormones. Cell Metab 2006;3:153–165 [DOI] [PubMed] [Google Scholar]
- 21.Bunck MC, Cornér A, Eliasson B, et al. . Effects of exenatide on measures of β-cell function after 3 years in metformin-treated patients with type 2 diabetes. Diabetes Care 2011;34:2041–2047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Abdul-Ghani MA, Puckett C, Triplitt C, et al. . Initial combination therapy with metformin, pioglitazone and exenatide is more effective than sequential add-on therapy in subjects with new-onset diabetes. Results from the Efficacy and Durability of Initial Combination Therapy for Type 2 Diabetes (EDICT): a randomized trial. Diabetes Obes Metab 2015;17:268–275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lingvay I, Legendre JL, Kaloyanova PF, Zhang S, Adams-Huet B, Raskin P. Insulin-based versus triple oral therapy for newly diagnosed type 2 diabetes: which is better? Diabetes Care 2009;32:1789–1795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fritsche A, Larbig M, Owens D, Häring HU; GINGER study group . Comparison between a basal-bolus and a premixed insulin regimen in individuals with type 2 diabetes-results of the GINGER study. Diabetes Obes Metab 2010;12:115–123 [DOI] [PubMed] [Google Scholar]
- 25.Bowering K, Reed VA, Felicio JS, Landry J, Ji L, Oliveira J. A study comparing insulin lispro mix 25 with glargine plus lispro therapy in patients with type 2 diabetes who have inadequate glycaemic control on oral anti-hyperglycaemic medication: results of the PARADIGM study. Diabet Med 2012;29:e263–e272 [DOI] [PubMed] [Google Scholar]
- 26.Dormandy JA, Charbonnel B, Eckland DJ, et al.; PROactive Investigators . Secondary prevention of macrovascular events in patients with type 2 diabetes in the PROactive Study (PROspective pioglitAzone Clinical Trial In macroVascular Events): a randomised controlled trial. Lancet 2005;366:1279–1289 [DOI] [PubMed] [Google Scholar]
- 27.Marso SP, Daniels GH, Brown-Frandsen K, et al.; LEADER Steering Committee; LEADER Trial Investigators . Liraglutide and cardiovascular outcomes in type 2 diabetes. N Engl J Med 2016;375:311–322 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.