Abstract
The study aims were to investigate free-living physical activity and sedentary behavior distribution patterns in a group of older women, and assess the cross-sectional associations with body mass index (BMI).
Eleven older women (mean (SD) age: 77 (9) yrs) wore custom-built activity monitors, each containing a triaxial accelerometer ( ± 16 g, 100 Hz), on the waist and ankle for lab-based walking trials and 4 days in free-living. Daily active time, step counts, cadence, and sedentary break number were estimated from acceleration data. The sedentary bout length distribution and sedentary time accumulation pattern, using the Gini index, were investigated. Associations of the parameters’ total daily values and coefficients of variation (CVs) of their hourly values with BMI were assessed using linear regression.
The algorithm demonstrated median sensitivity, positive predictive value, and agreement values > 98% and < 1% mean error in cadence calculations with video identification during lab trials. Participants’ sedentary bouts were found to be power law distributed with 56% of their sedentary time occurring in 20 min bouts or longer. Meaningful associations were detectable in the relationships of total active time, step count, sedentary break number and their CVs with BMI. Active time and step counts had moderate negative associations with BMI while sedentary break number had a strong negative association. Active time, step count and sedentary break number CVs also had strong positive associations with BMI.
The results highlight the importance of measuring sedentary behavior and suggest a more even distribution of physical activity throughout the day is associated with lower BMI.
Keywords: Accelerometer, Wearable sensors, Metabolic syndrome, Body mass index, Older adults
1. Introduction
Physical inactivity is defined as a lack of regular moderate-to-vigorous physical activity (MVPA), whereas sedentary behavior (SB) is defined as sitting/reclining with low energy expenditure while awake. Physical inactivity and SB are recognized as two distinct and separate risk factors for metabolic syndrome and cardiovascular disease (CVD), in addition to not enough low-intensity physical activity (LPA) and sleep [1]. Understanding the health benefits of replacing sedentary time with LPA or sleep is of substantial public health interest, particularly for older adults as physical inactivity and metabolic syndrome prevalence increase with aging [2].
Current objective SB measures involve the use of accelerometers. However, many accelerometer-based studies use methods of limited accuracy, classifying SB using activity count cut-points without considering posture [3,4]. Furthermore, these cut-points differ between studies. Even most studies that consider posture using ActivPAL only look at a limited number of daily mean SB parameters [5,6]. Using only the daily mean values of SB parameters may mean that we are missing important information about individual’s sedentary patterns. Significant sedentary time accumulation pattern differences were reported with no significant total sedentary time differences between active and sedentary young to middle-aged adult participants [7]. Furthermore, reducing SB throughout the day by increasing walking or standing may be more effective at compensating the harmful sedentary time effects on insulin and plasma levels than one hour of daily exercise with equivalent energy expenditure [6]. Therefore, daily sedentary breaks distribution and sedentary time accumulation may be important variables of SB to be examined. The majority of physical activity (PA) and SB research has focused on younger and middle-aged adults, despite older adults being less active and more sedentary [8]. Recent studies have begun to look at PA and SB in older adults [9–12], including PA and SB patterns [8,13–18]. However, these studies also used accelerometer-based tools with cut-points, or for which step detection accuracy has been reported as low for gait velocities < 0.5 m/s [19] which can be typical for lower functioning older adults.
We previously developed an accelerometer-based algorithm to measure active time, steps and cadence for gait velocities as low as 0.1 m/s [20–22]. The study aims were to (1) verify the step detection validity and validate active time and cadence estimations in a new sample of older women, and (2) investigate their PA and SB patterns in their home and community environments. Abdominal obesity, the most prevalent metabolic syndrome factor, is shown by some studies, although not all [13], to be affected by sedentary time [13,23]. This study’s third aim was to determine the cross-sectional associations of PA and SB total daily parameters and their distributions with body mass index (BMI), an indicator of abdominal obesity [24].
2. Methods
2.1. Experimental design
The step detection accuracy of the accelerometer-based algorithm has previously been validated for 11 young to middle-aged adults and 19 older adults (including 3 participants in the present study) [22]. To further test algorithm robustness, validity was tested for active time, steps and cadence measurements on the present study’s participants using comparison to video recordings during lab-based walking trials. Accelerometer and video data were acquired from 11 ambulatory, community-dwelling older women as they performed 10–14 walking trials at self-selected normal gait velocity over an 8.5 m walkway (with additional acceleration/deceleration room). Participants wore accelerometer-based activity monitors (AMs) on the waist (below the navel) and bilateral ankles. Steps were counted visually by one rater. A total of 119 trials were recorded.
Accelerometer data were also acquired as participants wore the AMs for 4 days in their free-living environments in the week succeeding the lab-based testing. Participants were instructed to wear the AMs at all times except during sleeping, bathing, or swimming. A valid AM hour was defined as ≤30 min of consecutive zero values and a valid day as ≥10 wear hours per day. Participants’ median (min–max) age and mean (SD) BMI were 76 (65–91) years, and 26.1 (4.9) kg m−2, respectively. As participants were recruited from a larger study on fall risk and fracture in older women, exclusion criteria included being on the osteoporosis drugs teriparatide or denosumab, unable to walk for > 1 block without a walking aid, bilateral hip replacements or surgery history, or lower extremity joint replacement within the prior year. The Institutional Review Board approved the protocol and participants provided written informed consent before participating.
2.2. Data collection
The custom-built AMs were secured with straps on the ankles and a clip on the waist. Each AM incorporated a tri-axial MEMS accelerometer (analog, ± 16 g, Analog Devices) with a sampling frequency of 100 Hz, and onboard data storage of up to 0.5 GB [20]. Video data were simultaneously acquired at 60 Hz using a handheld camera during the lab-based data collection. Video and accelerometer data were synchronized by an investigator shaking the AMs three times in view of the handheld camera prior to participant wear.
2.3. Signal processing
All accelerometer data post-processing and analysis were performed offline using MATLAB (Version 7.11.0, Mathworks, MA). The acceleration data were filtered to extract the gravitational component [22]. Subtracting the gravitational component from the original median filtered signal provided the bodily motion component.
2.4. Activity detection
Dynamic activity and steps were detected using algorithms previously developed and validated for 11 younger to middle-aged participants with gait velocities ranging from 0.1–4.8 m/s [20,21] and 19 older adult participants with gait velocities ranging from 0.5 to 2.0 m/s [22]. Upright dynamic activity was identified for 1 s epochs when the angle estimation calculated from the waist acceleration gravitational motion component was < 50°, and the waist acceleration bodily motion component’s signal magnitude area exceeded 0.135 g or the acceleration data within a range of 0.1–2.0 Hz exceeded a scaling threshold of 1.5 when a continuous wavelet transform was applied. In this study, each period of continuous 1 s epochs of detected activity is referred to as an activity segment. Step numbers and heel-strike timings were determined by applying a peak detection algorithm with adaptive acceleration and timing thresholds to the ankle acceleration data for all upright dynamic activity periods detected using the waist AM. Algorithm details can be found in previous studies [20–22].
2.5. Validity
Activity detection, step detection, and cadence calculations were validated against video data. For active time, accelerometer and video data were compared as 1 s windows. For step counts, each step event was compared between accelerometer and video data. Agreement, sensitivity, and positive predictive value (PPV) were used to assess the algorithm’s ability to accurately detect active seconds and steps. Agreement is the percentage of total active time seconds/step number detected using the algorithms compared with those from video data. Sensitivity is the ratio of true positives (steps or active seconds which were detected by the algorithm and from video data) to the sum of true positives and false negatives (steps or active seconds which were not detected by the algorithm but were from video data). PPV is the ratio of true positives to the sum of true positives and false positives (steps or active seconds which were detected by the algorithm but not from video data). Cadence as determined by the algorithm was compared to cadence as determined by video observation by plotting the difference between the two methods, as a percentage of the video-based estimation, against the video-based estimations. Heel-strike times were visually identified to calculate cadence from video data.
2.6. Parameters to evaluate physical and sedentary behavior in the free-living environment
The PA parameters of interest were: (1) active time, (2) step counts, and (3) cadence. Activity segments were classified as LPA, moderate physical activity (MPA), or vigorous physical activity (VPA) using previously defined cadence cut-points [13]: LPA < 93 steps min−1, MPA ≥93 steps min−1 and ≤124 steps min−1, and VPA > 124 steps min−1.
SB parameters of interest were: (1) daily number of breaks in sedentary time, (2) sedentary breaks distribution, (3) sedentary bout length distribution, and (4) sedentary time accumulation pattern. Some accelerometry-based studies define sedentary time as all minutes for which the activity count per minute is less than a defined cut-point and a sedentary break as any sedentary time interruption for which the activity count per minute is equal to or exceeds the defined cut-point [3,4]. However, in addition to no cut-point value agreement, cut-point methodology introduces issues such as the inability to differentiate between sitting and standing, or to accurately and repeatedly separate out low versus no acceleration activities both within and between participants. In this study, acceleration data were classified as either active or sedentary time on a second by second basis and a sedentary break was identified when an activity segment of ≥30 s (at least 1 min of activity when rounding to the nearest minute) was detected using our activity detection algorithm [20–22] with at least one second of sedentary time preceding it. Studies vary in their definition of minimum time duration required to classify sedentary bouts typically choosing 1, 2, 5, or 10 min or greater [14–17]. In this study, a sedentary bout was defined as a segment where no activity was detected for at least 10 min, consistent with previous sedentary bout length distribution studies [7].
2.7. Statistics
The coefficient of variation (CV) was used to investigate active time, steps and sedentary breaks distributions based on hourly values throughout the day. Simple linear regression with Pearson correlation analysis was used to assess the associations of each PA and SB parameter with BMI across participants using JMP Pro 9.0.1 (SAS Institute Inc., NC). Bivariable multiple regression was used to assess the significance of age in each association and to adjust for age if necessary. Significance level was set at 0.05 for two-tailed analyses.
Sedentary bout length distribution was examined by investigating the relationship between sedentary bout length and density on a logarithmic scale [7]. The sedentary bouts’ power distribution, estimated from the histogram shape, is characterized by exponent α, which can be used to quantify different SB strategies. Cohorts which accumulate sedentary time with larger percentages of long sedentary bouts yield a lower α exponent. Similarly, the Lorenz curve and Gini index were used to describe the pattern of sedentary time accumulation [7]. The Gini index, a standardized statistic for accumulation pattern comparisons, ranges from 0 (all sedentary bouts lengths contribute equally to sedentary time) to 1 (the longest sedentary bouts make up a very small percentage of total sedentary time).
3. Results
The mean (SD) time to complete the lab-based protocol and step number were 659 (42) s and 139 (36), respectively.
3.1. Lab-based validation
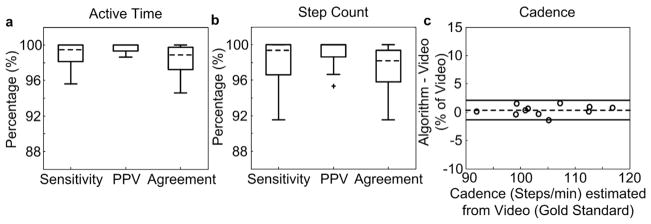
The median (interquartile range (IQR)) sensitivity, PPV, and agreement of active time (in s) and step detection were > 98 (96–100) % for lab-based walking trials (Fig. 1a and b). Mean percentage error was < 1% for cadence with 95% limits of agreement of −1 to 2% (Fig. 1c).
Fig. 1.
Sensitivity, positive predictive value (PPV), and agreement with video identification for (a) active time and (b) step count. The central line (dashed) represents the median, the edges of the box are the 25th and 75th percentiles, and the error bars extend to ± 1.5 of the interquartile range from the median value. Outliers beyond this range are labeled as +. (c) The percentage difference for cadence when using the activity monitoring system algorithm compared to video identification. The dashed line represents the mean, while the solid lines represent the limits of agreement ( ± 1.96 SD).
3.2. Free-living environment
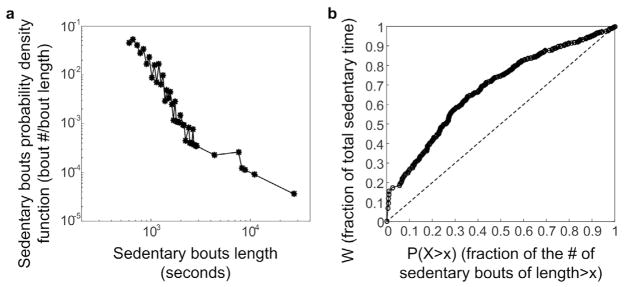
The median (IQR) daily step count, cadence, and active time were 7689 (6544–11950) steps, 73 (64–80) steps min−1, and 109 (92–173) min, respectively. Fig. 2 and Supplementary Table 1 show the distribution of steps, cadence, active time, and sedentary break number per hour throughout one day for a sample participant.
Fig. 2.
Data from a sample participant of (a) total number of steps per hour, (b) boxplots demonstrating the distributions of cadence during each hour (the dotted grey lines mark the cadence cut-points to classify activity as low (< 93 steps min−1), moderate, or vigorous (> 124 steps min−1) intensity) throughout one day, (c) minutes of low and moderate activity per hour (no vigorous activity was detected for this participant), and (d) breaks in sedentary time per hour. For the boxplots in (b) the central line (grey) represents the median, the edges of the box are the 25th and 75th percentiles, and the error bars extend to ± 1.5 of the interquartile range from the median value. Outliers beyond this range are labeled as +. Actual values are presented in Supplementary Table 1.
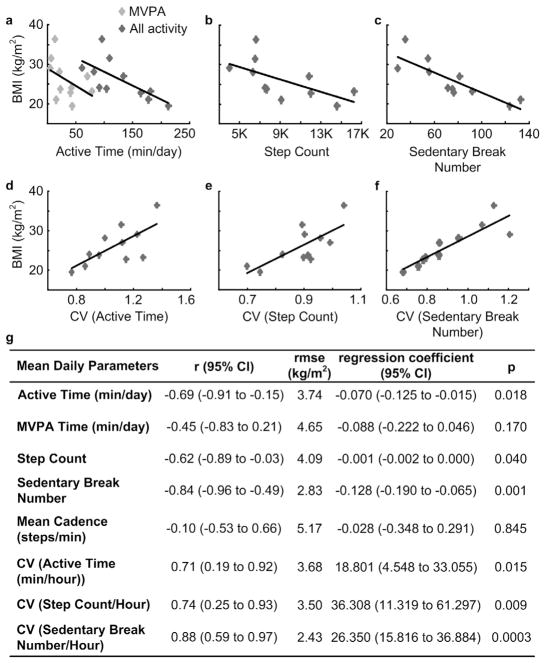
Participants spent a mean (SD) of 68 (10) % of their time in SB. The sedentary bouts’ distribution with respect to their length was similar to a power law distribution (Fig. 3a). The power law characteristic exponent α was 2.83 with a standard error σ of 0.10 and the median (IQR) sedentary bout length was 15.8 (12.3–21.4) min. The majority of bouts were < 20 min but bouts > 20 min contributed to 56% of total sedentary time across participants. The Gini index estimated from the Lorenz curve (Fig. 3b) was 0.36.
Fig. 3.
(a) Distribution of sedentary bout per bout length, and (b) the Lorenz curve linking the fraction of sedentary time to the proportion of sedentary bouts above a certain length × for all participants. The dashed line in (b) represents the line of perfect equality and the Gini index is estimated as the area between the Lorenz curve and the line of perfect equality.
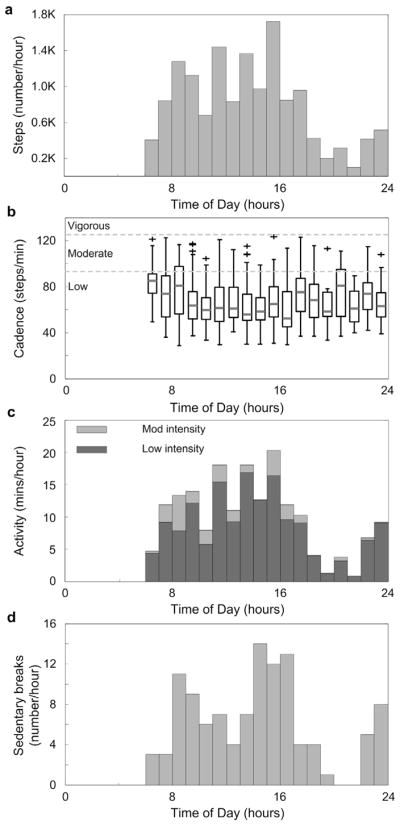
Meaningful associations were detectable in the relationships of daily total active time, step count, sedentary break number and their CVs per hour with BMI. Daily active time and step counts had moderate [25] and significant negative associations with BMI while daily MVPA time demonstrated a weak negative association with BMI which was not statistically significant (Fig. 4a and b). The number of breaks in sedentary time had a strong and significant negative association with BMI (Fig. 4c). The CV per hour of active time, step count, and sedentary break number also had strong and significant positive associations with BMI (Fig. 4d–f). Mean daily cadence had a very weak association with BMI which was not statistically significant (Fig. 4g). Age had weak positive associations with all investigated variables but none were statistically significant (r: 0.01–0.35 and p-values: 0.290–0.983). Using bivariable multiple regression, age was only significant in the model of CV of sedentary break number and BMI. After adjusting for age, the CV of sedentary break number still had a strong positive association with BMI (r = 0.97 (0.89 to 0.99), rmse = 1.47 kg/m2, CV of sedentary break number: regression coefficient (95% CIs) = 25.397 (18.950–31.843), p-value = 0.0001; age: regression coefficient (95% CIs) = −0.147 (−0.271 to −0.023), p-value = 0.0314).
Fig. 4.
Associations with body mass index (BMI) of mean daily (a) active time (all intensity levels: dark grey, moderate to vigorous physical activity time; light grey), (b) step count, and (c) sedentary break number, and the coefficients of variation (CVs) of (d) active time, (e) step count, and (f) sedentary break number per hour. (g) Pearson’s correlation coefficients with 95% confidence intervals (CIs), root mean square errors (rmse), regression coefficients with 95% CIs per unit of standard error (SE), and p-values for all investigated parameters.
4. Discussion
The study aims were to (1) verify algorithm robustness in a new sample of older women, (2) investigate the PA and SB distribution and accumulation pattern in their home and community environments, and (3) examine the associations of PA and SB parameters with BMI.
The lab-based walking trials’ validation results demonstrate the algorithm’s robustness to accurately track PA and SB in older women. The daily step count range was higher than expected for older adults, however, most participants were self-reportedly very active. The calculated cadences and the mean calculation error (caused by missed steps) were similar to previous estimates [26]. The mean daily sedentary break numbers were also comparable [4]. The present study’s participants spent a similar percentage (68%) of their day in sedentary time compared to previous studies on young to middle-aged (60%) [27] and older adults (72–77%) [10,14,15] which used cut-points to identify SB, and for middle-aged (65%) [4]; and older (78%) [12]; adults in posture-based studies using ActivPAL. The small differences between studies may be due to algorithm differences, participant age or employment status. While the present study’s algorithm includes posture detection, participants were not compliant with thigh AM wear which is required to distinguish standing from sitting postures. Therefore, fidgeting during sitting may have been identified as activity rather than SB. Nonetheless, even fidgeting while sitting may be important in maintaining weight [28].
The dose-response relationship between different behavior distributions and cardiovascular health remains to be established. While few studies have investigated more complex SB measures, some suggest that more detailed SB pattern examination incorporating distribution, variability, time of day, and accumulation is needed [7]. Sedentary time accumulation strategy differences have been observed using ActivPAL between healthy young to middle-aged active and sedentary workers and chronic low back pain and chronic fatigue syndrome participants [7]. The power law characteristic distribution exponent decreased with more sedentary groups, particularly those with chronic diseases. In the present study, the distribution exponent was even higher than for healthy active participants in Chastin and Granat [7]. This may be due to the use of different algorithms that do not necessarily measure sedentary bouts equivalently. Without a thigh AM, standing still is misclassified as SB using our algorithm. Increasing standing time in place of sitting may result in cardiometabolic markers improvements [29]. ActivPAL ignores activity while sitting. Even though SB is characterized as sitting or lying postures, increased activity during sitting can improve cardiometabolic risk factors [30]. Currently, no field-based tool directly and accurately measures all aspects although our algorithm has the potential with thigh AM wear. The present study’s Gini index was similar to that of healthy active participants [7] with 56% of sedentary time occurring in bouts > 20 min.
The negative associations of daily active time, step counts, and sedentary break number with BMI are consistent with greater activity being associated with healthier weight [30]. The higher association of total active time at any intensity level with BMI compared to time spent in MVPA supports recent findings that considering LPA is crucial [1]. A parameter’s CV not only takes the number of events into account but also how the events are distributed throughout the day. Interestingly, the CVs per hour of active seconds, steps, and sedentary breaks had stronger associations with BMI than their total daily values. This suggests a more even distribution of activity throughout the day to break up prolonged sedentary time may be beneficial to adiposity in addition to total daily activity volume. This agrees with previous observations of the activity distribution effect on insulin and plasma levels [6] and of an association between less fragmented sedentary time with higher % body fat [13]. Both the sedentary break number and the CV of sedentary break number per hour had the strongest associations with BMI compared to traditional PA variables, consistent with previous reports that BMI and abdominal obesity are affected by sedentary time [13]. As this is a cross-sectional study, causality cannot be inferred. While lower activity volumes can lead to higher adiposity, higher adiposity can act as a barrier (or motivator) to increasing PA.
This study was not powered to detect significant differences between the associations observed for the parameters examined. The small sample size may have also lead to the inability to detect an association of MVPA time or mean daily cadence with BMI. However, meaningful associations were detectable in the relationships of daily total active time, step count, sedentary break number and their CVs per hour with BMI. Larger variations in BMI and activity volume (particularly in the less active range) would be expected in the general older adult female population. Therefore, these relationships need to be investigated with much larger sample sizes to determine generalizability among this population and also separately in different patient populations. As male participants were not included, this study’s results are not generalizable to the older adult male population. Previous studies including both sexes have reported differences in PA and SB [10] and in their relationships with obesity measures for older adults [13,16]. Therefore, studies often report sex-based results [10,13,16] or include one gender [15,18]. Nonetheless, this is one of a small number of studies to investigate older adult females’ PA and SB distribution and accumulation patterns and uses a novel algorithm with high accuracy for gait velocities as low as 0.1 m/s.
Our data suggest that activity variation may be an important weight management factor to consider in future larger studies. Our findings also highlight the importance of measuring SB, since a more uniform PA distribution to break up SB throughout the day to avoid prolonged sedentary bouts appears to be associated with a lower BMI.
Supplementary Material
Acknowledgments
Funding was provided by DOD DM090896 and NIH R01 AR027065. The body-worn motion detection and recording units were provided by Dr. Barry Gilbert, James Bublitz, Kevin Buchs, Charles Burfield, Christopher Felton, Dr. Clifton Haider, Michael Lorsung, Shaun Schreiber, Steven Schuster, and Daniel Schwab from the Mayo Clinic Special Purpose Processor Development Group. The information or content and conclusions do not necessarily represent the official position of, nor should any official endorsement be inferred by the National Institutes of Health, the United States Navy, the Department of Defense, or the U.S. Government.
Appendix A. Supplementary data
Supplementary data associated with this article can be found, in the online version, at http://dx.doi.org/10.1016/j.gaitpost.2017.05.014.
Footnotes
Conflict of interest
The authors report no conflict of interest.
References
- 1.Wijndaele K, Duvigneaud N, Matton L, Duquet W, Delecluse C, Thomis M, et al. Sedentary behaviour, physical activity and a continuous metabolic syndrome risk score in adults. Eur J Clin Nutr. 2009;63:421–429. doi: 10.1038/sj.ejcn.1602944. [DOI] [PubMed] [Google Scholar]
- 2.Ford ES, Giles WH, Mokdad AH. Increasing prevalence of the metabolic syndrome among U.S. adults. Diabetes Care. 2004;27:2444–2449. doi: 10.2337/diacare.27.10.2444. [DOI] [PubMed] [Google Scholar]
- 3.Cooper AR, Sebire S, Montgomery AA, Peters TJ, Sharp DJ, Jackson N, et al. Sedentary time, breaks in sedentary time and metabolic variables in people with newly diagnosed type 2 diabetes. Diabetologia. 2012;55:589–599. doi: 10.1007/s00125-011-2408-x. [DOI] [PubMed] [Google Scholar]
- 4.Bankoski A, Harris TB, McClain JJ, Brychta RJ, Caserotti P, Chen KY, et al. Sedentary activity associated with metabolic syndrome independent of physical activity. Diabetes Care. 2011;34:497–503. doi: 10.2337/dc10-0987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stephens BR, Granados K, Zderic TW, Hamilton MT, Braun B. Effects of 1 day of inactivity on insulin action in healthy men and women: interaction with energy intake. Metabolism. 2011;60:941–949. doi: 10.1016/j.metabol.2010.08.014. [DOI] [PubMed] [Google Scholar]
- 6.Duvivier BM, Schaper NC, Bremers MA, van Crombrugge G, Menheere PP, Kars M, et al. Minimal intensity physical activity (standing and walking) of longer duration improves insulin action and plasma lipids more than shorter periods of moderate to vigorous exercise (cycling) in sedentary subjects when energy expenditure is comparable. PLOS ONE. 2013;8:e55542. doi: 10.1371/journal.pone.0055542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chastin SF, Granat MH. Methods for objective measure, quantification and analysis of sedentary behaviour and inactivity. Gait Posture. 2010;31:82–86. doi: 10.1016/j.gaitpost.2009.09.002. [DOI] [PubMed] [Google Scholar]
- 8.Lord S, Chastin SF, McInnes L, Little L, Briggs P, Rochester L. Exploring patterns of daily physical and sedentary behaviour in community-dwelling older adults. Age Ageing. 2011;40:205–210. doi: 10.1093/ageing/afq166. [DOI] [PubMed] [Google Scholar]
- 9.Aguilar-Farias N, Brown WJ, Peeters GM. ActiGraph GT3X+ cut-points for identifying sedentary behaviour in older adults in free-living environments. J Sci Med Sport. 2014;17:293–299. doi: 10.1016/j.jsams.2013.07.002. [DOI] [PubMed] [Google Scholar]
- 10.Arnardottir NY, Koster A, Van Domelen DR, Brychta RJ, Caserotti P, Eiriksdottir G, et al. Objective measurements of daily physical activity patterns and sedentary behaviour in older adults: Age, Gene/Environment Susceptibility-Reykjavik Study. Age Ageing. 2013;42:222–229. doi: 10.1093/ageing/afs160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gennuso KP, Gangnon RE, Matthews CE, Thraen-Borowski KM, Colbert LH. Sedentary behavior, physical activity, and markers of health in older adults. Med Sci Sports Exerc. 2013;45:1493–1500. doi: 10.1249/MSS.0b013e318288a1e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Godfrey A, Lord S, Galna B, Mathers JC, Burn DJ, Rochester L. The association between retirement and age on physical activity in older adults. Age Ageing. 2014;43:386–393. doi: 10.1093/ageing/aft168. [DOI] [PubMed] [Google Scholar]
- 13.Chastin SF, Ferriolli E, Stephens NA, Fearon KC, Greig C. Relationship between sedentary behaviour, physical activity, muscle quality and body composition in healthy older adults. Age Ageing. 2012;41:111–114. doi: 10.1093/ageing/afr075. [DOI] [PubMed] [Google Scholar]
- 14.Diaz KM, Howard VJ, Hutto B, Colabianchi N, Vena JE, Blair SN, et al. Patterns of sedentary behavior in US middle-age and older adults: the REGARDS study. Med Sci Sports Exerc. 2016;48:430–438. doi: 10.1249/MSS.0000000000000792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jefferis BJ, Sartini C, Shiroma E, Whincup PH, Wannamethee SG, Lee IM. Duration and breaks in sedentary behaviour: accelerometer data from 1566 community-dwelling older men (British Regional Heart Study) Br J Sports Med. 2015;49:1591–1594. doi: 10.1136/bjsports-2014-093514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Judice PB, Silva AM, Santos DA, Baptista F, Sardinha LB. Associations of breaks in sedentary time with abdominal obesity in Portuguese older adults. Age (Dordr) 2015;37:23. doi: 10.1007/s11357-015-9760-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Leask CF, Harvey JA, Skelton DA, Chastin SF. Exploring the context of sedentary behaviour in older adults (what, where, why, when and with whom) Eur Rev Aging Phys Act. 2015;12:4. doi: 10.1186/s11556-015-0146-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shiroma EJ, Freedson PS, Trost SG, Lee IM. Patterns of accelerometer-assessed sedentary behavior in older women. JAMA. 2013;310:2562–2563. doi: 10.1001/jama.2013.278896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stansfield B, Hajarnis M, Sudarshan R. Characteristics of very slow stepping in healthy adults and validity of the activPAL3 activity monitor in detecting these steps. Med Eng Phys. 2015;37:42–47. doi: 10.1016/j.medengphy.2014.10.003. [DOI] [PubMed] [Google Scholar]
- 20.Lugade V, Fortune E, Morrow M, Kaufman K. Validity of using tri-axial accelerometers to measure human movement – Part I: Posture and movement detection. Med Eng Phys. 2014;36:169–176. doi: 10.1016/j.medengphy.2013.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fortune E, Lugade V, Morrow M, Kaufman K. Validity of using tri-axial accelerometers to measure human movement – Part II: Step counts at a wide range of gait velocities. Med Eng Phys. 2014;36:659–669. doi: 10.1016/j.medengphy.2014.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fortune E, Lugade VA, Amin S, Kaufman KR. Step detection using multi-versus single tri-axial accelerometer-based systems. Physiol Meas. 2015;36:2519–2535. doi: 10.1088/0967-3334/36/12/2519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yang X, Telama R, Viikari J, Raitakari OT. Risk of obesity in relation to physical activity tracking from youth to adulthood. Med Sci Sports Exerc. 2006;38:919–925. doi: 10.1249/01.mss.0000218121.19703.f7. [DOI] [PubMed] [Google Scholar]
- 24.Bozeman SR, Hoaglin DC, Burton TM, Pashos CL, Ben-Joseph RH, Hollenbeak CS. Predicting waist circumference from body mass index. BMC Med Res Methodol. 2012;12:115. doi: 10.1186/1471-2288-12-115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vincent W, Weir J. Statistics in Kinesiology. 4. Human Kinetics; Champaign: 2012. [Google Scholar]
- 26.Blanc Y, Balmer C, Landis T, Vingerhoets F. Temporal parameters and patterns of the foot roll over during walking: normative data for healthy adults. Gait Posture. 1999;10:97–108. doi: 10.1016/s0966-6362(99)00019-3. [DOI] [PubMed] [Google Scholar]
- 27.Healy GN, Dunstan DW, Salmon J, Cerin E, Shaw JE, Zimmet PZ, et al. Breaks in sedentary time: beneficial associations with metabolic risk. Diabetes Care. 2008;31:661–666. doi: 10.2337/dc07-2046. [DOI] [PubMed] [Google Scholar]
- 28.Levine JA. Non-exercise activity thermogenesis (NEAT) Best Pract Res Clin Endocrinol Metab. 2002;16:679–702. doi: 10.1053/beem.2002.0227. [DOI] [PubMed] [Google Scholar]
- 29.Dunstan DW, Kingwell BA, Larsen R, Healy GN, Cerin E, Hamilton MT, et al. Breaking up prolonged sitting reduces postprandial glucose and insulin responses. Diabetes Care. 2012;35:976–983. doi: 10.2337/dc11-1931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Carr LJ, Dunsiger SI, Lewis B, Ciccolo JT, Hartman S, Bock B, et al. Randomized controlled trial testing an internet physical activity intervention for sedentary adults. Health Psychol. 2013;32:328–336. doi: 10.1037/a0028962. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.