Abstract
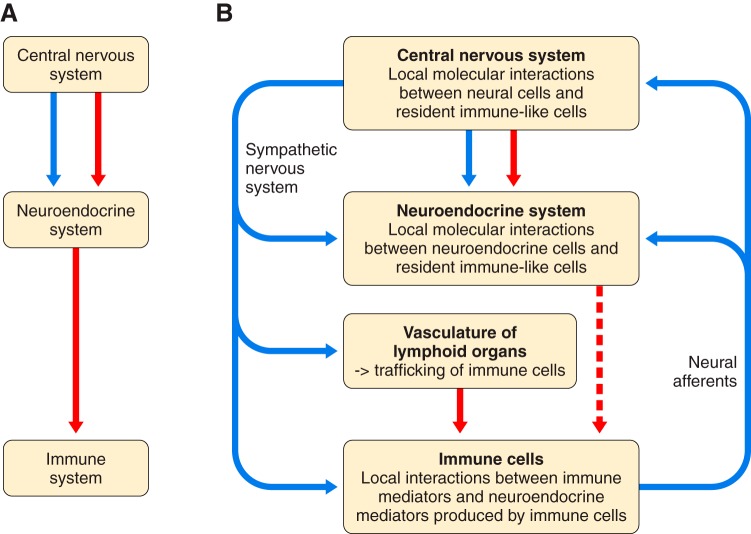
Because of the compartmentalization of disciplines that shaped the academic landscape of biology and biomedical sciences in the past, physiological systems have long been studied in isolation from each other. This has particularly been the case for the immune system. As a consequence of its ties with pathology and microbiology, immunology as a discipline has largely grown independently of physiology. Accordingly, it has taken a long time for immunologists to accept the concept that the immune system is not self-regulated but functions in close association with the nervous system. These associations are present at different levels of organization. At the local level, there is clear evidence for the production and use of immune factors by the central nervous system and for the production and use of neuroendocrine mediators by the immune system. Short-range interactions between immune cells and peripheral nerve endings innervating immune organs allow the immune system to recruit local neuronal elements for fine tuning of the immune response. Reciprocally, immune cells and mediators play a regulatory role in the nervous system and participate in the elimination and plasticity of synapses during development as well as in synaptic plasticity at adulthood. At the whole organism level, long-range interactions between immune cells and the central nervous system allow the immune system to engage the rest of the body in the fight against infection from pathogenic microorganisms and permit the nervous system to regulate immune functioning. Alterations in communication pathways between the immune system and the nervous system can account for many pathological conditions that were initially attributed to strict organ dysfunction. This applies in particular to psychiatric disorders and several immune-mediated diseases. This review will show how our understanding of this balance between long-range and short-range interactions between the immune system and the central nervous system has evolved over time, since the first demonstrations of immune influences on brain functions. The necessary complementarity of these two modes of communication will then be discussed. Finally, a few examples will illustrate how dysfunction in these communication pathways results in what was formerly considered in psychiatry and immunology to be strict organ pathologies.
I. INTRODUCTION
Our understanding of physiology has benefited greatly from the advances in molecular biology that have been at the origin of the explosive development of genetics and -omic techniques. What used to be a rarity a few decades ago, studying the expression and function of a given molecule within a different physiological system from the one in which it was first identified, has now become the norm. Communication signals and signaling pathways are commonly studied in different physiological systems using the same tools. This is the case, for instance, for purinergic signaling, which is investigated by immunologists for its role in macrophage function and plasticity (57) and by neurobiologists for its regulatory activity on synaptic plasticity (203). Blurring of the boundaries between disciplines is probably the main outcome of this wave of research. However, this situation is still relatively new, and the transition to it has been very progressive.
This is well reflected in the history of the research efforts in neural–immune interactions (TABLE 1) (1). What was initially of interest to only a few practitioners in psychosomatic medicine—the influence of personality factors and emotional states on sensitivity to disease, or more generally the interrelationships among mind, body, and environment in health and disease—became an object of scientific investigation in the 1950s, when it was brought into the laboratory to be subjected to a reductionist approach (139). Not surprisingly, retrospectively, but at the time difficult for hardcore pathologists to admit, biobehavioral factors, in the form of exposure to well-defined stressors, were found to influence the initiation and progression of various infectious and noninfectious diseases in animal models of pathology. Once it became possible to assess immune functions in a routine manner using techniques borrowed from clinical immunology, these influences were ascribed to modulation of immune responses by activation of the stress pathways. The predominant stress pathways that were investigated were the hypothalamic-pituitary-adrenal (HPA) axis, the activation of which results in the release of cortisol or corticosterone (depending on the species), and the sympathetic nervous system, the activation of which results in the release of epinephrine and norepinephrine.
Table 1.
The early decades of research that shaped the field of neuroimmune interactions
| Early Neuroimmune Research |
|---|
| 1. The psychosomatic approach: |
| Psychological factors and emotions influence disease onset and progression (allergies, peptic ulcer, cancer, autoimmune diseases, infectious diseases) |
| 2. The biobehavioral approach: |
| Experimental stressors impact immune functions (1964: Solomon proposes the term “psychoimmunology”) |
| The immune system can be modulated by conditioned stimuli (Metalnikov and Chorine, 1926; Ader, 1974) |
| 3. The cellular communication approach: |
| Immune cells express neurotransmitter receptors (Szentivanyi, 1958; Hadden, 1970–5; Pert, 1985) |
| Immune cells produce brain and pituitary peptides (Blalock, 1980) |
| 4. The neuroanatomical approach: |
| Innervation of the spleen and other lymphoid organs by the autonomic nervous system (Felten, 1980) |
| 5. The effect of immune factors on the neuroendocrine system: |
| Interleukin-1 activates the hypothalamic-pituitary-adrenal axis by acting in the brain (Besedovsky and Del Rey, 1975) |
The study of psychological modulation of immunity, initially conducted at Institut Pasteur in Paris, France in the 1920s using Pavlovian conditioned stimuli (157), was revived in the 1970s by Ader and Cohen (2), who rediscovered the phenomenon of conditioned immunosuppression. Working at the University of Rochester Medical Center, they showed that it is possible to increase the immunosuppressive effect of cyclophosphamide by presenting rats with the taste of a saccharin solution previously paired with exposure to the poisonous side effects of cyclophosphamide (2). These were key experiments that indirectly revealed the existence of an intricate network of bidirectional communications between the central nervous and the immune systems. Such communication pathways had been suspected before but not yet demonstrated. Therefore, they were not amenable to mechanistic analysis.
The field of research that studies the basic aspects of neural–immune interactions was variously labeled neuroimmunomodulation, neuroimmunoendocrinology, or psychoneuroimmunology, depending on which scientific discipline predominated at the time. However, this new wave of interdisciplinary research gained momentum in the scientific community at large only when the pathways of communication between the nervous system and the immune system were elucidated. In a nonconcerted effort, neuroanatomists demonstrated the existence of a sympathetic innervation of primary and secondary lymphoid organs (71), neuroendocrinologists described the expression and function of neuroendocrine receptors on immune cells (95, 177), and cell biologists showed that activated immunocytes express and release molecular factors previously identified in the neuroendocrine system, such as adrenocorticotrophin, which is processed from proopiomelanocortin in lymphocytes in the same manner as in the anterior pituitary (212, 213). The emphasis on brain-to-immune, rather than immune-to-brain, communication pathways was mainly due to the active involvement of neuroendocrinologists in the field and to the progress made in the elucidation of the chemical nature and receptor mechanisms of most neuroendocrine factors (93).
Although the existence of an immune-to-brain communication pathway had been inferred by Besedovsky et al. (17), whose elegant physiological studies demonstrated activation of the HPA axis and the sympathetic nervous system during the peak antibody response in mice vaccinated with a T-cell antigen, the molecular nature of this communication pathway took longer to be elucidated. Cloning and recombinant expression of cytokines, the autocrine and paracrine communication factors between immune cells, did not take place before the early 1980s (60). The ability of the first cloned cytokine interleukin (IL)-1β to activate the HPA axis and induce some of the physiological changes observed in a mouse model of antibody response to sheep red blood cells was reported in 1986, shortly after the demonstration of the pyrogenic activity of this cytokine (16).
As previously presented in Physiological Reviews, basic communication mechanisms between the nervous and immune systems include the immune production and function of neuroendocrine peptide hormones (22), the effects of neuroendocrine hormones on the immune system and the innervation of lymphoid organs by the sympathetic nervous system (142), and the regulatory effects of cytokines on the HPA axis (232). The objective of this review is not to update this information but to introduce a new perspective: the fascinating complementarity between short-range and long-range communication mechanisms between the nervous and the immune systems.
Studies of long-range communication mechanisms were initially favored, certainly because of the strong predominance of neuroendocrinology and neuroanatomy in the emerging field of psychoneuroimmunology. Communication from the nervous system to the immune system was believed to take place exclusively via circulating hormones produced by the neuroendocrine system (e.g., cortisol, but also growth hormone and prolactin) and via neurotransmitters (e.g., epinephrine and norepinephrine) released in the vicinity of immune cells by nerve endings in primary and secondary lymphoid organs. However, the discovery that immune cells can themselves produce and release neuroendocrine factors and neuromediators led to a shift in interest from long-range to short-range communication pathways.
Similarly, communication from the immune system to the brain was initially seen as involving circulating immune factors acting indirectly on the brain via the formation of brain-penetrant molecules (prostaglandins) in brain areas where the blood-brain barrier is leaky, the so-called circumventricular organs. This was how endogenous pyrogens were perceived as being responsible for the development of the fever response to infectious pathogens. It took time for neurobiologists to realize that brain innate immune cells actually produce the same cytokines as those originally characterized as endogenous pyrogens and that these locally produced cytokines are responsible for the various components of the response of the host to infection. It took even longer to recognize that cytokines produced locally by brain cells are responsible for intricate functional and structural interactions between endothelial cells, glia, and neurons.
II. NEURAL AND HORMONAL INFLUENCES ON THE IMMUNE SYSTEM
A. Innervation of Lymphoid Organs: Sympathetic Versus Parasympathetic Innervation
There is much anatomic and functional evidence for a role of the autonomic nervous in the regulation of immunity (142). Most of the neuroanatomical studies on innervation of lymphoid organs were carried out during the 1970s–1980s. They revealed the existence of a dense sympathetic innervation of all lymphoid organs. Sympathetic nerves travel with the vasculature but separate from it when entering lymphoid organs. They terminate in close contact with parenchymal T lymphocytes and plasma cells, forming what has been termed “neuroeffector junctions” (71). The nerve fibers that innervate lymphoid organs contain various neuropeptides that are colocalized or not with norepinephrine, including vasoactive intestinal peptide, neuropeptide Y, substance P, Met-enkephalin, and neurotensin.
Most peripheral organs in the body are innervated by branches of both the sympathetic and the parasympathetic nervous systems. The immune system is apparently an exception: no neuroanatomical evidence exists for a parasympathetic or vagal nerve supply to any immune organ, with the possible exception of lymphoid tissue in the respiratory and alimentary tracts (164). This is in contrast to results from earlier tracing studies of innervation (37), which were subsequently corroborated by visualization of the synthesizing enzyme choline-O-acetyltransferase and the degradation enzyme acetylcholinesterase, which act on the neurotransmitter acetylcholine (36). However, these observations were dismissed because of the presence of artifacts in the tracing studies that were caused by the spillover of large doses of tracers (142, 164) and the existence of a nonneuronal acetylcholine expression system in lymphocytes (79). Lymphocytes contain all the components required to constitute an independent, nonneuronal cholinergic system, including acetylcholine, its synthesizing and degrading enzymes, and muscarinic and cholinergic receptors. The fact that expression of the components of this nonneuronal cholinergic system varies during T-cell activation as well as in response to cholinergic agents indicates that acetylcholine synthesized by T cells can act as an autocrine or paracrine factor (115).
The possibility of a parasympathetic innervation of lymphoid organs was reexamined recently, thanks to a new neural-tract tracing methodology based on specific labeling of choline acetyltransferase-expressing cells by the tdTomato fluorescent protein, which can be utilized in appropriate transgenic lines of mice (81). Cholinergic innervation emanating from enteric neurons was apparent only in the intestinal lamina propria of the gastrointestinal tract. Cholinergic fibers were found to come in close contact with macrophages, plasma cells, and lymphocytes located in the intestinal mucosa, and to a lesser degree with immune cells within the gut-associated lymphoid tissue. Cholinergic innervation of the spleen is very sparse and comes from a small subset of cholinergic sympathetic postganglionic neurons located in the paravertebral and/or prevertebral chains. These fibers are often associated with periarteriolar catecholaminergic fibers. A few of them terminate in lymphocyte-containing areas of the white pulp. Nonneuronal choline acetyltransferase cells are clearly visible in the spleen and consist mainly of B cells and fewer T cells.
Another factor of confusion in the identification of cholinergic innervation of lymphoid organs is the existence of a catecholaminergic-to-cholinergic transmission switch in some sympathetic fibers influenced by signals, such as leukemia inhibitory factor, produced by the innervated target. Although this is a marginal phenomenon, it has been described in particular for the sympathetic fibers that innervate sweat glands in mammalian footpads (69) and the periosteum (6). Because the density of catecholaminergic neurons that innervate inflamed tissue decreases in patients with rheumatoid arthritis, the possibility of a catecholamine-to-cholinergic transition of sympathetic nerve fibers was investigated in a murine model of collagen-induced arthritis. Cholinergic sympathetic fibers became apparent several weeks after the induction of arthritis under the influence of leukemia inhibitory factor. However, catecholaminergic-to-cholinergic transition only affected those fibers that innervate healthy tissue adjacent to the inflammatory tissue (217).
The remarkable saga of the anti-inflammatory cholinergic reflex proposed by Kevin Tracey in the 2000s illustrates very well the various ingredients of the controversy about the parasympathetic innervation of lymphoid organs (171). The saga began with the discovery of unexpected pharmacological properties of a new anti-inflammatory drug developed by Tracey for the treatment of sepsis, tetravalent guanylhydrazone (CNI-1493). CNI-1493 was developed on the basis of its ability to inhibit the production of tumor necrosis factor-α (TNF) and other macrophage inflammatory cytokines in response to sepsis induced by administration of lipopolysaccharide (LPS). Tracey discovered that this lead compound was much more potent when injected into the lateral ventricle of the brain than when administered systemically (29). This finding was interpreted to indicate that CNI-1493 activates a neural pathway that links the brain to peripheral macrophages. This neural pathway was claimed to be the vagus nerves, as cutting the vagus nerves abrogated the anti-inflammatory activity of CNI-1493, whereas electrically stimulating the peripheral end of vagal nerves mimicked it (30).
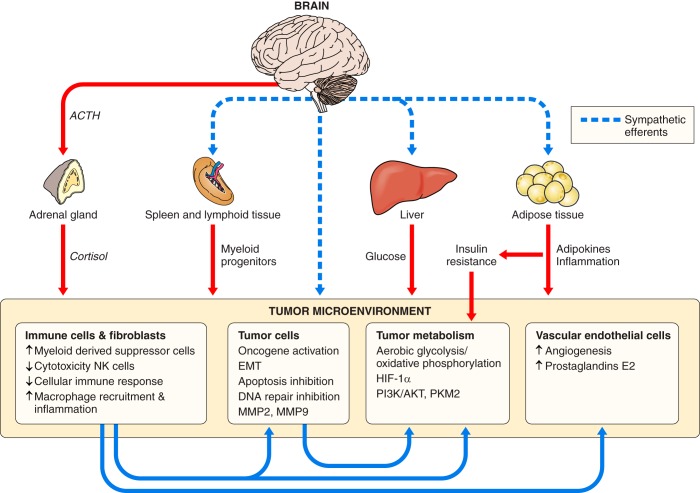
Indifferent to the controversies surrounding the possible existence of a parasympathetic innervation of lymphoid organs, Tracey (231) proposed that cholinergic vagal nerves act on macrophages to suppress the production of TNF and other inflammatory mediators. This neural communication pathway from the central nervous system to the immune system was presented as being part of an anti-inflammatory reflex whose afferent arm was the production of inflammatory cytokines by activated innate immune cells (see sect. III) and whose efferent arm was the activation of cholinergic efferents downregulating cytokine production by innate immune cells (FIGURE 1). Muscarinic cholinergic stimulation was proposed to mediate the central component of the anti-inflammatory pathway, whereas activation of nicotinic receptors containing an α7 receptor subunit mediated the downregulatory effect of acetylcholine on macrophages (242). What was still lacking in the characterization of this anti-inflammatory pathway, however, was an anatomically characterized target for the efferent vagal innervation (137).
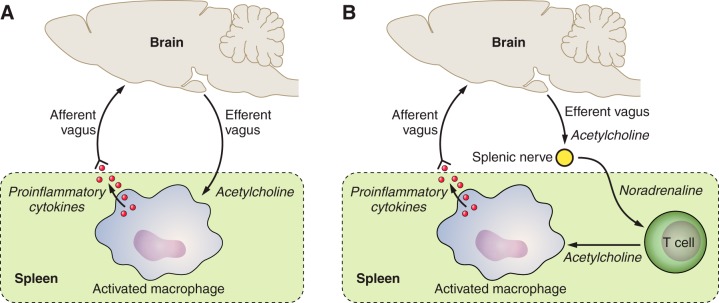
FIGURE 1.
Schematic representation of the inflammatory reflex. A: the initial model of the inflammatory reflex that was proposed originally by Tracey (231). Proinflammatory cytokines released by activated innate immune cells activate the afferent vagus nerves. This sensory input activates in a reflex-like manner neuronal cell bodies of the efferent vagus nerves. The resulting activation of the dorsal vagal complex recruits the efferent cholinergic vagus nerves that downregulate inflammation. B: the revised model of the inflammatory reflex. The parasympathetic branch of the vagus nerves activates the splenic nerves. Activation of this sympathetic nerve results in the recruitment of acetylcholine-producing T cells that downregulate inflammation.
This target was proposed to be the spleen, as sectioning of the splenic nerves abrogated the anti-inflammatory signature of splenic macrophages that developed in response to vagal nerve stimulation (107). In the absence of a direct cholinergic innervation of the spleen, these findings were interpreted to indicate that sympathetic postganglionic splenic nerves indirectly transmitted the cholinergic vagal message to splenic macrophages (192). The problem was that this neuroanatomic circuit implied an adrenergic, instead of cholinergic, transmission of the neural message to macrophages. The missing cholinergic link surfaced later, with the discovery that T cells that produce and release acetylcholine in the spleen could be called to the rescue (FIGURE 1) (193). Microdialysis of the spleen and mass spectrometry analysis of the dialysate samples were used to demonstrate that vagus nerve stimulation leads indirectly to the release of acetylcholine in situ. The lack of an effect of vagus nerve stimulation in nude mice lacking T cells, together with adoptive transfer experiments of acetylcholine containing T cells to nude mice, confirmed the role of T lymphocytes in the anti-inflammatory reflex. Still missing was a demonstration that acetylcholine-containing T cells expressed β2-adrenergic receptors and were located in close proximity to sympathetic splenic nerves. This was subsequently confirmed by immunofluorescence analysis of spleen sections in mice expressing enhanced green fluorescent protein under the control of transcriptional regulatory elements for choline acetyltransferase (193).
Whether this last element of the puzzle puts a triumphant final brick on the saga of the anti-inflammatory reflex (171) is not yet certain. The existence of an indirect vagal innervation of the spleen by splenic nerves has been disputed, because vagal preganglionic neurons do not synaptically connect to sympathetic postganglionic neurons, and vagal nerve stimulation does not recruit splenic neurons (33). These last negative findings are in accordance with the features of the very sparse cholinergic innervation of the spleen described above (81). An alternative is that stimulation of the vagus nerves actually recruits lymphocytes, including acetylcholine-synthesizing cells, from the lymphoid tissue of the gut that is innervated by vagal nerves. These T cells would then be able to migrate to various organs, including the spleen (148), and exert there their local anti-inflammatory activity. As pointed out by Besedovsky a few decades ago, immune-cell trafficking and recirculation require a tight control of blood supply to lymphoid organs, including the spleen. Interactions between locally produced cytokines and sympathetic nerve fibers contribute to this control (187, 188). During sepsis that drives the inflammatory reflex, as studied by Tracey, there is a dramatic increase in splenic blood flow. This increase is secondary to an inhibition of the sympathetic vasoconstrictor tonus at the postganglionic and prejunctional levels. This results in a decrease in the release of norepinephrine, and possibly other neuromediators, by sympathetic nerve fibers in response to locally produced IL-1β (187). In other terms, nerve-driven changes in functionality of immune cells in vivo could well be due to cytokine-induced alterations in the blood supply of the lymphoid organ under investigation, especially when this lymphoid organ is devoid of lymphatic circulation, which is the case with the spleen. This observation necessitates reexamination of the importance of sympathetic nerve endings in controlling immune cell trafficking, circulation, and homing.
In conclusion of this section, innervation of the lymphoid organs is predominantly sympathetic. Parasympathetic innervation of lymphoid organs appears to be limited to the gut lymphoid tissue. The possibility that innervation regulates immune cell functionality by modulating blood supply of lymphoid organs requires further investigation.
B. Influences of Catecholamines on Immune Cells
Innate immune cells express the β2, α1, and α2 subtypes of adrenergic receptors, whereas adaptive immune cells express primarily the β2 subtype of adrenergic receptor (164). Activation of β2-adrenergic receptors triggers a signaling cascade involving the formation of cAMP, which activates either protein kinase A (PKA) or the guanine exchange proteins directly activated by cAMP (EPACs) (124). PKA signals via cytoplasmic kinases such as p38 mitogen-activated protein kinase (MAPK) or the cAMP response element-binding protein (CREB) transcription factor. EPACs further signal via the Rap family of small Ras-like GTPases. Ligation of the β2 adrenergic receptor can also activate β-arrestins that connect to multiple signaling pathways, including p38, extracellular signal-regulated kinase MAPKs, and nuclear factor kappa-B (NF-κB).
Not surprisingly, an abundant literature describes the in vitro effects of various adrenergic receptors agonists and antagonists on immune cells and the signaling pathways involved in these effects. For adaptive immunity, most of the research effort has focused on the consequence of activating β2-adrenergic receptors in CD4+ T cells, Th1, and B cells. Th2 cells do not express β2-adrenergic receptors, at least in the mouse system. Stimulation of β2-adrenergic receptors usually inhibits T-cell responses, although activation effects have also been described. For instance, in vitro exposure of CD4+ T cells to norepinephrine or terbutaline decreased IL-2 production in response to polyclonal activation with anti-CD3 monoclonal antibody (185). However, norepinephrine also promoted naive CD4+ T-cell differentiation into Th1 cells that produced more interferon (IFN)-γ than did nonexposed cells (224). In vivo studies show that chemical sympathetic denervation decreases the intensity of delayed-type hypersensitivity, confirming a positive role of catecholamines in Th1 cell-driven immune responses (143). In B cells, the signaling pathway activated by β2-adrenergic receptor activation involves a PKA-dependent, CREB-mediated pathway that converges with that activated by CD86 ligation to enhance the magnitude of an immunoglobulin (Ig) G1 response. Activation of β2-adrenergic receptors also enhances the IgE response but via a PKA-dependent, hematopoietic tyrosine phosphatase/p38 MAPK-mediated pathway (173).
Because macrophages and monocytes express α1-adrenergic, α2-adrenergic, and β2-adrenergic receptors, their response to adrenergic stimulation is more complex. In general, the production of inflammatory cytokines is inhibited by β2-adrenergic receptor activation, whereas it is enhanced by α1-adrenergic or α2-adrenergic receptor stimulation (108, 110, 173, 215). However, adrenergic stimulation also promotes myeloid cell recruitment and migration to the site of injury, such that β2-adrenergic receptor antagonism might be beneficial. This is the case, for instance, in mice submitted to repeated episodes of social defeat. Activation of β2-adrenergic receptors facilitates the recruitment and trafficking of monocytes to the brain, resulting in prolonged activation of microglia and development of anxiety-like behavior (250).
It is important to note that this effect of β2-adrenergic receptor activation on egress of monocytes from the bone marrow is opposite to that observed on egress of lymphocytes from lymph nodes (163). In the latter case, β2-adrenergic receptor activation actually enhances retention of lymphocytes into lymphoid organs via chemokine receptors (CC-chemokine receptor 7 for B cells and CXC-chemokine receptor type 4 for T cells). Catecholamines acting on endothelial cell adhesion molecules and chemokines produce a similar dissociation in the modulation of the innate and adaptive immune system during the dark-light cycle. This dissociation is orchestrated by molecular clocks via adrenergic nerves (155, 202). Periods of activity associated with high adrenergic tone are characterized by increased recruitment of myeloid cells in tissues and sequestration of lymphocytes from general circulation into lymphoid organs. As proposed by Scheiermann et al. (202), this would help the innate immune system to be prepared for higher risk of infection during the active phase of the cycle while keeping the adaptive immune system at bay.
In addition to serving as coordination molecules between physiological and immune processes when released from autonomic nerves, catecholamines can serve other roles when produced locally (134). Epinephrine and norepinephrine are produced and released by normal T cells and exert their functions in an autocrine or paracrine manner via classic adrenergic receptors on T cells. Lymphocytes contain the machinery to synthesize and degrade catecholamines, and they produce and release more catecholamines when activated (147, 182). This is particularly the case in lymphocytes from the mesenteric lymph nodes (182), where catecholamines modulate lymphocyte trafficking, local vascular perfusion, cytokine production, and functional activity of lymphocytes.
Phagocytic cells (macrophages and neutrophils) also are able to release high levels of epinephrine and norepinephrine when activated. This is associated with enhanced expression of catecholamine synthesizing and degrading enzymes (73). Blockade of α2-adrenoreceptors, but not β2-adrenoreceptors, in a model of inflammation-induced lung injury reduced the intensity of vascular leakage, whereas administration of an α2-adrenergic agonist had the opposite effect. Experiments showing that depletion of T cells and administration of reserpine to achieve sympathetic denervation did not alter the effects of α2-adrenergic agents eliminated the possibility that T cells or sympathetic innervation produce these effects. In addition, blockade of tyrosine hydroxylase or dopamine-β-hydroxylase diminished the inflammatory response, whereas inhibition of the catecholamine-O-methyl transferase enzyme increased lung injury. These results were interpreted by the authors to suggest that the phagocytic system can function as a diffusely expressed adrenergic organ. Enhancement of the local inflammatory response by phagocyte-produced catecholamines was found to be mediated by increased production of inflammatory mediators via activation and translocation of NF-κB (74).
C. Glucocorticoids
1. Anti-inflammatory versus proinflammatory activity of glucocorticoids
In line with the original observation by Selye of an involution of the thymus and other lymphoid organs in response to stress (205) and the subsequent demonstration of the immunosuppressive effects of glucocorticoids (101), glucocorticoids have traditionally been seen as the hormonal mediators of the immunosuppressive effects of stressors. We will not delve into the details of the vast literature on the effects of stress on immunity, as this topic has been reviewed on several occasions and it is not directly relevant to the present review (3, 9, 160, 169, 204, 220).
Glucocorticoids act on their cellular targets by binding to glucocorticoid receptors (GRs). GRs normally reside in the cytosol in the form of a protein complex that brings together heat-shock proteins and FK506 binding protein 52. Upon binding to their ligand, GRs dissociate from this complex to form monomers or dimers and translocate to the nucleus The anti-inflammatory effects of glucocorticoids are mediated by transcriptional repression following nuclear translocation and tethering of monomeric GRs to the glucocorticoid-response elements of transcription factors such as NF-κB, activator protein (AP)-1, and IFN-regulating factor-3 (234). This results in the downregulation of genes coding for inflammatory mediators, enzymes, and adhesion molecules. Although the hypothesis is still controversial, GR dimerization and transactivation are thought to play an important role in the anti-inflammatory activity of glucocorticoids. This phenomenon is illustrated by data obtained in GR(dim/dim) mutant mice that show reduced GR dimerization and increased sensitivity to TNF-induced inflammation, and to experimental models of sepsis induced by LPS or cecal ligation and puncture (123, 235).
Glucocorticoids can be proinflammatory under certain conditions. This effect can be secondary to the selection of corticoid-resistant inflammatory cells, such as pathogenic Th17 cells that overexpress IL-23 receptor and multidrug-resistance protein and that are found in inflamed gut tissue from patients with Crohn’s disease (186). The proinflammatory effect of glucocorticoids may also result from inhibition of the production and release of anti-inflammatory factors, or conversely from enhanced production and release of proinflammatory mediators. In the first case, dexamethasone administered 24 h before LPS was found to enhance the placenta’s proinflammatory cytokine response to LPS as a consequence of the inhibition of lipoxin A4 synthesis (255). In the second case, it is the dose of glucocorticoids that makes the difference: as mentioned above, physiological glucocorticoid levels can be proinflammatory in some circumstances, whereas high or pharmacological levels are anti-inflammatory. For instance, low doses of glucocorticoids increase the production of macrophage migration inhibitory factor, and this effect is sufficient to override glucocorticoid-mediated inhibition of cytokine production and release by LPS-stimulated monocytes (39).
The proinflammatory effects of endogenous levels of corticosteroids have been demonstrated in the brain (214). As in the placenta, these effects are observed only if the glucocorticoid response occurs ahead of the inflammatory stimulus. Maier and his colleagues (76) have repeatedly observed that acute or chronic exposure to stressors 24 h before administration of LPS sensitizes or primes the inflammatory response to LPS. This priming effect is observed not only in peripheral macrophages (112), but also in microglia isolated from the hippocampus of stressed rats (75). The microglial release of high-mobility group box-1 (HMGB1), an endogenous damage-associated molecular pattern, has been proposed to mediate stress-induced priming via activation of Toll-like receptor (TLR)2 and TLR4 and recruitment of the NLRP3 inflammasome (77).
2. Autocrine/paracrine signaling by extra-adrenal glucocorticoids
Glucocorticoids are considered to be prototypical hormonal factors that are produced and released into the general circulation by the adrenal cortex to act on distant target organs. The discovery of extra-adrenal production and release of glucocorticoids acting locally as paracrine or autocrine communication signals was therefore unexpected (226). The very first organ in which extra-adrenal steroidogenesis was identified was the thymus. This ran contrary to the commonly held belief that the thymus is the main target for glucocorticoids produced by the adrenal gland. In the mouse, the thymus typically responds to glucocorticoids by massive apoptosis of CD4+ CD8+ thymocytes and involution (92). However, all the elements necessary for the local production and release of corticosterone are present in murine thymic epithelial cells, as demonstrated in vitro (175). Furthermore, co-culturing of thymic epithelial cells with thymocytes induced apoptosis of thymocytes. This effect was blocked by a GR antagonist as well as by inhibitors of the enzymes involved in the production of corticosterone. Thymocytes produce corticosterone in an age-dependent manner that is concurrent with thymocyte differentiation into CD4+ and CD8+ T cells and thymus involution (181). Several ingenious studies have confirmed the physiological role in vivo of the local production of glucocorticoids in the thymus and have demonstrated their independence from circulating glucocorticoids (226). In general, the findings of these studies confirm that thymic-derived glucocorticoids locally regulate thymocyte development, the rate of naive T-cell formation, and the seeding in the periphery of recent thymic emigrants. This function of thymic glucocorticoids would complement the role of adrenal glucocorticoids in regulating strong and systemic immune responses (226).
Extra-adrenal glucocorticoid synthesis has also been identified in intestinal epithelial cells that are part of the proliferating cells of the crypts of the intestinal mucosa. Locally formed glucocorticoids have both an inhibitory and a costimulatory role in intestinal T-cell activation (45). On the basis of observation that the expression of steroidogenic genes is decreased in colon biopsies of patients with inflammatory bowel diseases, it has been proposed that the local synthesis of glucocorticoids is important for controlling intestinal inflammation and immune responses (48).
Skin inflammation induces glucocorticoid synthesis by keratinocytes. As the skin possesses all the components of a local HPA axis, glucocorticoid synthesis in the skin can act in a manner complementary to the HPA axis to inhibit local inflammation and promote wound healing (257).
D. Other Hormones and Neuropeptides
After showing that human leukocyte IFN-α has strong antigenic relatedness to adrenocorticotropic hormone (ACTH) and endorphins (24), Smith et al. (213) demonstrated that induction of IFN-α in mice by inoculation with a noncytotoxic avian virus, the Newcastle disease virus, simultaneously caused a time-dependent increase in corticosterone production by spleen lymphocytes. The culprit turned out not to be an ACTH-like moiety of IFN-α but leukocyte-derived ACTH produced by the processing of leukocyte proopiomelanocortin in a manner similar to what takes place in the anterior pituitary. As proopiomelanocortin is at the origin of β-endorphin, the stage was set for a quest for ACTH and opioid receptors and their signaling pathways in lymphocytes (23). Classic opioid binding sites had already been described on leukocytes (253), and it did not take long to confirm the presence of ACTH receptors on lymphocytes (31, 46). Other precursors of opioid peptides, prodynorphin, which is at the origin of dynorphin and Leu-enkephalin, and preproenkephalin, which is responsible for Met-enkephalin and Leu-enkephalin, were found to be expressed in leukocytes of several species, together with their receptors (68, 252). Whether opioid peptides produced by immunocytes function as communication signals within the immune system or between the immune system and the neuroendocrine system could then be investigated.
On the basis of the observation that enkephalins promote activity of immunocytes at baseline and suppress activity of activated immune cells, it was proposed that these molecules function as fine tuners of the immune response (68). Evidence of immune-to-nerve communication for immune-derived peptides was extensively described in the field of inflammation-mediated pain. Opioid-containing immunocytes migrate to the site of inflammation, where they release β-endorphin that activates peripheral opioid receptors on sensory nerves to attenuate pain (38, 207, 219). The release of opioid peptides from immune cells is mediated by several signal molecules, including corticotrophin-releasing hormone, norepinephrine, and IL-1β, the production and release of which are upregulated at the site of inflammation (FIGURE 2) (218).
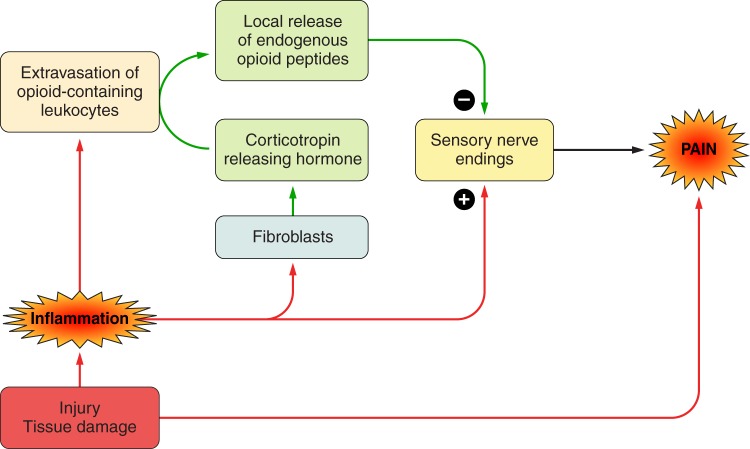
FIGURE 2.
Role of opioid-containing leukocytes in the regulation of inflammation-induced pain. Proinflammatory cytokines released by activated innate immune cells sensitize sensory nerve endings, resulting in an amplification and prolongation of the initial pain reaction triggered by activation of nociceptors in response to the injury. The pain response is downregulated by endogenous opioid peptides released by locally infiltrating opioid containing leukocytes in response to corticotropin releasing hormone produced by fibroblasts. [Adapted from Stein et al. (218).]
The possibility that prolactin and growth hormone regulate immunity by a paracrine/autocrine, rather than hormonal, mechanism was recognized early in the study of the immune properties of these peptides. As with other hormones, the hormonal role of these peptides was described first. The initial observations were made in hypophysectomized rats in which both the deficient antibody response to sheep red blood cells and the delayed-type hypersensitivity response to dinitrochlorobenzene could be restored by replacement treatment with exogenous prolactin or growth hormone (162). This effect could be easily explained by the presence of specific binding sites for prolactin and growth hormone on T and B lymphocytes. Unexpectedly, the potent immunosuppressive drug cyclosporine was found to increase circulating levels of prolactin, and administration of the dopamine agonist bromocriptine blocked cyclosporine’s immunosuppressive properties when administered at doses that abrogated cyclosporine-induced increase in prolactin levels (43). These findings were initially interpreted to suggest that hyperprolactinemia mediates the immunosuppressive effects of cyclosporine. However, further studies showed that cyclosporine and prolactin compete with each other for binding to prolactin receptors on lymphocytes (196) and that part of the signal reaching prolactin receptors is actually a prolactin/growth hormone-related polypeptide produced locally by stimulated lymphocytes (103, 195).
The immunomodulatory activities of growth hormone and prolactin have been reviewed extensively in the past 25 yr (61, 116, 117, 236, 248), and there is no need to reiterate this information. We know now that the production and release of growth hormone and prolactin are regulated by immune factors in both the pituitary gland and in lymphocytes, and the many different effects of these peptides on immune cells can be explained by the intervention of posttranscriptional and posttranslational processes generating various isoforms and variants of these peptides (176, 246).
E. Summary
Numerous studies carried out in vitro and in vivo show that catecholamines released by sympathetic nerve fibers have potent modulatory effects on immune cells. Some of these effects are mediated by alterations in monocyte and lymphocyte trafficking. In addition, immune cells can produce catecholamines that act locally as paracrine or autocrine communication factors in similar or different physiological processes. However, the importance of this last mechanism in immunophysiology and immunopathology has not yet been fully appreciated. Like catecholamines, glucocorticoids can be produced by immune cells in lymphoid tissues and exert local actions on different physiological processes that are in general complementary to those mediated by circulating glucocorticoids produced by the adrenal gland. This action is not necessarily immunosuppressive as glucocorticoids can be proinflammatory in some conditions. The same duality in the modality of action of other hormones and neuropeptides is also apparent.
III. IMMUNE INFLUENCES ON THE NERVOUS SYSTEM
A. Historical Perspective
The existence of immune influences on the nervous system took longer to be recognized and studied than that of neuroendocrine influences on the immune system. The reason is that the molecular nature of immune communication signals (monokines and interleukins, generally grouped together under the name of cytokines) was not elucidated until the 1980s, and these molecules were just not available for physiological studies. The first cytokine to be cloned and produced by recombinant technology was actually a monokine, IL-1. Research on cytokine actions in the brain stemmed from two independent lines of research. The first one was the physiology of fever, which was and still is part of mainstream physiology. The second one was immunophysiology. This last line of research took longer to emerge because of its very marginal place at the boundary between immunology and physiology.
Fever can be defined as a regulated increase in the set point for temperature regulation. Because the set point for temperature regulation is elevated, the feverish organism generates more heat by thermogenesis and actively maintains it by minimizing thermolysis. Fever is not caused by a direct action of microbial pathogens on the brain thermoregulatory centers. It is induced by soluble factors that are released by activated leukocytes, the so-called endogenous pyrogens. The problem faced initially by fever physiologists was that the molecular identity of endogenous pyrogens could not be characterized based solely on their in vivo pyrogenic activity, because available assays lacked specificity. This difficulty was eventually overcome by the development of an appropriate in vitro assay, the lymphocyte activating factor assay (83, 84). Based on this assay, the first endogenous pyrogen, IL-1, was cloned in 1984 (8, 140). Other cytokines that have since been found to act as endogenous pyrogens include IFN- α, TNF, and IL-6 (59). IL-1 represents two different cytokines, IL-1α and IL-1β, produced by two different genes. Most of the early literature on IL-1 refers to IL-1β. Unless mentioned otherwise, we keep this convention in the present review.
The understanding that immune signals could control the immune system via a downregulating neuroendocrine feedback loop involving cytokine action on the brain emerged within the context of immunophysiology. Immunophysiologists reasoned that, like any other physiological system in the body, the immune system requires two levels of regulation: a self-regulatory process that is intrinsic to the immune system, and an external regulatory loop that makes use of the central nervous system and its means of communication with the rest of the body, i.e., the autonomic nervous system and the neuroendocrine system. While mainstream immunologists focused primarily on the self-contained, self-monitored immune system, Besedovsky and Sorkin relentlessly searched for evidence of extrinsic regulation. They hypothesized that if extrinsic regulation exists, it should make use of immune factors able to signal the brain to recruit neuroendocrine factors with immunomodulatory activity. Pivotal to their research was the demonstration that the mounting of an antibody response was associated with increased activity of the HPA axis and the sympathetic nervous system (18); before this discovery, the immune response was believed to be regulated only intrinsically within the immune system. In mice and in rats injected with sheep red blood cells (a T-cell-dependent antigen), the peak of the immune response coincided with an increase in glucocorticoid blood levels (18). In addition, this peak was preceded by decreased norepinephrine in the spleen that was inversely related to the magnitude of the immune response (54). At the functional level, Besedovsky and Sorkin showed that the glucocorticoid response to an antigenic stimulation is required for antigenic competition. Antigenic competition refers to the inhibition exerted by an immune response to a first antigen relative to the immune response to a second non-cross-reactive antigen. This form of competition does not occur in adrenalectomized mice, which are unable to mount a glucocorticoid response to the first antigen (19). To search for the immunological factors that signal the ongoing immune response to the brain neuroendocrine circuits, Besedovsky and Sorkin injected supernatants of in vitro activated lymphocytes into naive mice and identified what they called a “glucocorticoid increasing factor” (20). In collaboration with Dinarello, who had just cloned IL-1 and had obtained sufficient quantities of a recombinant form of it to inject to mice, Besedovsky and his colleagues were then able to demonstrate that this cytokine activated the pituitary-adrenal axis in a manner similar to the glucocorticoid increasing factor (16). Because there was still some uncertainty about the exact site of action of IL-1 to induce glucocorticoid release, it was important to show that this effect was mediated in the hypothalamus, rather than in the pituitary or the adrenal cortex (14). With this demonstration of the role of IL-1 in a brain-mediated immunoregulatory loop, the stage was finally set for further studies on the mechanisms of these regulatory processes.
As we will see, studies of the influence of immune communication signals on the central nervous system followed the same path of reasoning as the one that led to our understanding of the influence of neuroendocrine communication signals on the immune system. The consideration of long-range interactions between the immune system and the brain via hormonal-like factors predominated for some time; gradually, however, the study of short-range interactions based on immune factors produced locally in the nervous system gained favor.
B. Pyrogenic Effects of Cytokines
The conventional view of fever in infectious diseases holds that the fever response is mediated by endogenous pyrogens released by activated mononuclear phagocytes into the general circulation. This explains why most experimental studies of fever involved intravenous injection of endogenous pyrogens into naive experimental animals. This route of injection continued to be used even after recombinant cytokines became available, despite the fact that cytokines do not behave as circulating communication factors.
The sequence of events leading to the production of inflammatory cytokines by innate immune cells in response to pathogenic microorganisms has been identified. Specialized monocyte/macrophage membrane receptors identified as Toll-like receptors recognize specific molecular moieties of pathogens called pathogen-associated molecular patterns (PAMPs) (72, 191). Activation of Toll-like receptors by PAMPs and by danger-associated molecular patterns (DAMPs) that are released by damaged cells from the host triggers a signaling cascade that culminates in the synthesis and release of proinflammatory cytokines (170). LPS, for instance, activates Toll-like receptor-4 (TLR4) on monocytes and macrophages. This requires the association of LPS to a specific binding protein, LPS-binding protein (LBP). The LPS-LBP protein complex associates with still another membrane protein, cluster of differentiation 14 (CD14), before recruiting another extracellular protein, myeloid differentiation factor 2 (MD-2). Activation of TLR4 recruits two pathways, a myeloid differentiation primary response gene 88 (MyD88)-dependent pathway and a MyD88-independent pathway. MyD88 recruits IL-1 receptor associated kinases (IRAKs) and the adaptor molecules TNF receptor-associated factors (TRAF6) that lead to activation of both mitogen-activated protein kinases Jun NH2-terminal kinase (JNK) and p38, and transcription factor nuclear factor-kappaB (NF-κB). JNK and p38 activate, respectively, CREB and activator protein 1 (AP1). CREB, AP1, and NF-κB are important for the synthesis of proinflammatory cytokines. The MyD88-independent pathway recruits TRAF3 and induces interferon-regulatory factor (IRF3) signaling leading to expression of type I interferons and interferon-inducible genes (170). The MyD88 pathway is shared with other TLRs including TLR2, TLR5, and TLR11 while the MyD88-independent pathway is shared with TLR3.
In terms of communication, the concept that predominated initially was that proinflammatory cytokines were released by innate immune cells into the general circulation and acted at distance. Because of their big molecular size and their hydrophilic nature, proinflammatory cytokines could not cross the blood-brain barrier. They acted instead on those parts of the brain that are devoid of a blood-brain barrier, the so-called circumventricular organs. In the case of the fever response, the target circumventricular organ was the organum vasculosum laminae terminalis (OVLT). At the level of the OVLT, cytokines induced the synthesis of prostaglandins E2 (PGE2). PGE2 are formed from arachidonic acid by cyclooxygenase (COX-1 and COX-2)-dependent synthesis of prostanglandin H2 and further transformation by prostaglandin synthases. PGE2 diffused inside the brain parenchyma and activated PGE2 receptors located on thermosensitive neurons in the anterior preoptic area of the hypothalamus (25). This mode of action of proinflammatory cytokines was well accepted in the scientific community of fever physiologists until further studies revealed a much more complex circuitry than originally anticipated (70, 194, 200).
Fever in response to LPS is characterized actually by a biphasic course. The first wave of fever originates in the liver. It is mediated by activation of the complement cascade and release of constitutive COX-1- and COX-2-dependent PGE2 by liver macrophages (Kupffer cells) (26). The released PGE2 activates vagal afferents that terminate in the nucleus tractus solitarius and project to the ventromedial part of the hypothalamus via the ventral noradrenergic bundle. The second wave is mediated by the production of inflammatory cytokines at the periphery. These cytokines induce the synthesis and release of brain cytokines, including IL-6 which is mainly produced by astrocytes. Brain cytokines ultimately stimulate the production and release of PGE2 by perivascular cells and cerebral endothelial cells; this occurs mainly along venules after induction of the PGE2 synthesizing enzymes COX-2 and microsomal PGE synthase-1 (70, 200). Centrally produced PGE2 activate PGE2 receptors 3 (EP3) that are present on thermosensitive neurons in the median preoptic nucleus of the hypothalamus. This second wave of fever is supported by the synthesis and release of PGE2 by cerebral endothelial cells. The neural circuitry activated by PGE2 acting on EP3 receptors involves two populations of preoptic GABAergic neurons that ultimately control cutaneous vasoconstriction and adipose tissue thermogenesis via the autonomic nervous system (200). The gradual recovery of fever is mediated by the production of anti-inflammatory cytokines both peripherally and centrally (194) and by the dampening of cytokine synthesis in activated macrophages under the effect of heat stress (66, 70).
C. Activation of the Hypothalamo-Pituitary-Adrenal Axis by Cytokines
The neuroendocrine response to an infectious agent cannot be monitored with the same temporal precision as variations in body temperature. This certainly explains why the response of the HPA axis to peripheral immune stimulation is usually described as monophasic rather than multiphasic. Nonetheless, two phases can be distinguished: an earlier phase occurring 1–2 h after injection of LPS, and a sustained response still apparent 6 h after treatment (64). Earlier studies of the ACTH and corticosterone response to an intraperitoneal injection of IL-1 revealed that these responses took longer to develop than the usual response to an exteroceptive stressor, 2 h for the peak ACTH and corticosterone response instead of 15–30 min (16). The sustained phase of the HPA axis response to LPS is dependent on the production and release of PGE2 by the brain vasculature in a COX-2- and mPGES-1-dependent manner (64). PGE2 acts in a paracrine manner to stimulate EP1 and EP3 expressing catecholaminergic neurons in the ventrolateral medulla of the brain (150). These neurons project to CRH containing neurons in the paraventricular nucleus of the hypothalamus (67). The late phase of the HPA axis is temporally dependent on an inducible PGE2 synthesis interacting with an earlier neuronal afferent signal involving constitutive COX-1-dependent PGE2 synthesis in perivascular cells and endothelial cells of the brain vasculature (64, 80). The relative involvement of perivascular cells and endothelial cells depends on the stimulus: IL-1 appears to activate only perivascular cells, while LPS activates both perivascular cells and endothelial cells (206). In addition, perivascular cells exert an inhibitory effect on the response of endothelial cells to LPS that becomes apparent once they are artificially eliminated. However, this account of the role of perivascular cells in the HPA axis response to IL-1 does not fit with immunohistochemistry data showing a selective expression of IL-1 receptors in brain endothelial cells but not in perivascular cells (128). Cell-specific deletion of IL-1 receptors confirms the immunohistochemistry data. Mice lacking IL-1 receptors in hematopoietic cells including perivascular macrophages still respond to IL-1 injected systemically by increased plasma levels of ACTH and corticosterone; this is no longer the case in mice lacking IL-1 receptors in brain vascular cells (151).
The possibility that LPS acts in the adrenal cortex rather than in the hypothalamus to increase circulating corticosterone levels was ruled out by studies of mice with adrenocortical cell-specific deletion of MyD88. This did not impair the HPA axis response to systemic LPS, confirming the effects of LPS take place at the level of the hypothalamus or the pituitary (113). There is evidence that cytokines, including IL-1 and IL-2, can act directly on pituitary cells and increase the release of various pituitary peptides, including ACTH (15, 114). However, the relevance of this activity for the in vivo HPA axis response to immune stimuli is still unclear (154), although there is evidence for direct cytokine action on the pituitary in conditions of prolonged exposure to cytokines after ACTH release has been initiated by CRH (208). Folliculo-stellate cells in the anterior pituitary act as an important source of IL-6 that influences hormonal output from the anterior lobe in a paracrine manner (56, 58).
CRH-containing parvocellular neurons in the rat hypothalamus also produce vasopressin, which strongly potentiates CRH-induced ACTH secretion and augments several actions of extra hypothalamic CRH in the brain. The acute effects of IL-1 on the HPA axis are mediated predominantly by CRH, since they are abolished by CRH immunoneutralization (14). However, CRH immunoneutralization is less effective after repeated administration of IL-1. This is due to phenotypic changes in the expression of CRH and vasopressin in hypothalamic parvocellular neurons, with vasopressin dominating over CRH (230). A similar increase in vasopressin stores in CRH-containing neurons occurs several days after injection of a single dose of IL-1. This phenotypic switch affecting CRH-containing neurons is not specific to IL-1; it is also observed after endotoxin administration and in response to electric foot shocks and social defeat, but not after other types of stressors. The increased expression of vasopressin in CRH-containing neurons is responsible for the cross-sensitization phenomenon that can develop in response to stressors occurring in succession: administration of IL-1 at a given time point sensitizes the response to a different stressor that occurs later (229).
The activating effects of cytokines on the HPA axis are limited by the glucocorticoid resistance that develops in response to inflammation. Glucocorticoid resistance typically occurs in humans in response to repeated injections of IFN-α. It takes place at the level of the hippocampus rather than the pituitary (87). This is not an artifact due to the administration of exogenous cytokines, since it also develops in virus-infected organisms (13, 158). Mechanisms include disruption of glucocorticoid receptor translocation and DNA binding, and alterations in glucocorticoid receptor phosphorylation status (172).
D. Behavioral Effects of Cytokines
The most visible face of the response to an infectious agent is the sickness behavior that develops in ill individuals. Inactivity, decreased responsiveness to external stimuli, sleepiness, decreased appetite, and social withdrawal are the usual signs of a microbial infection. Agitation can occur as a prodrome, but this is rare. These behavioral alterations are often associated with malaise and pain. They are part of a whole repertoire of disease-control strategies that enable organisms to adapt to the very expensive metabolic cost of mounting an immune response and a fever (99, 100). Because behaviorists are usually not interested in the behavior of sick individuals and physiologists rarely engage in lengthy descriptions of behavioral activities, the study of cytokine-induced sickness behavior lagged behind studies of cytokine-induced fever and HPA axis activation. It became more mainstream only after identification of the relationship between sickness behavior and symptoms of depression (53).
The behavioral alterations that develop in animals injected with LPS or cytokines recapitulate those observed in ill individuals (37, 81). The intensity and duration of sickness behavior can be easily measured by reduction in spontaneous activities such as exploration of a novel conspecific or ambulatory activity in a familiar or novel environment (119). Reduced appetite can be measured by decreases in food and water intake. More elaborate indexes of sickness behavior include decreased motivation in tasks requiring an effort to access the reward and impaired cognitive abilities in tasks based on recognition of a novel object, acquisition of context-dependent fear conditioned response, and spatial memory (49, 50, 156, 180).
Neal Miller was the first researcher to propose that the changes in behavior that develop in ill individuals are the expression of a motivational state that competes with usual behavioral activities, rather than just a decrease in these behaviors. He based this hypothesis on the observation that rats injected with endotoxin were less willing to work for food, water, and a rewarding electrical stimulation in their lateral hypothalamus, but they were still able to increase their response rate for gaining some rest when put into a forced wheel-running apparatus (159). This flexibility in the behavioral response to a stimulus depending on the environment and the consequences of the response is typical of a motivated behavior. Competition between the motivational state of sickness and another form of motivated behavior, maternal behavior, was elegantly demonstrated in later studies carried out in lactating mice injected with LPS. LPS-treated dams behaved in a sick way by lying immobile and being apparently indifferent to their pups. However, when their pups were dispersed in the cage and the nest removed and replaced by cotton wool, dams emerged out of their apathy and actively engaged in retrieving pups to the cage location where the cotton wool was placed. They still did not engage in nest building unless submitted to an ambient temperature of 6°C (7). The interoceptive feelings associated with sickness behavior have been studied in human volunteers inoculated with typhoid vaccine or injected with a small dose of LPS. Depressed mood, anhedonia, and fatigue are the typical symptoms that develop in these conditions (35, 63, 97, 130).
The inflammatory signals that mediate sickness behavior are transmitted to the brain by the neural afferents that innervate the site of the body at which the inflammatory response takes place. When LPS is injected into the peritoneal cavity, the vagus nerve is the predominant neural pathway, as demonstrated by subdiaphragmatic vagotomy experiments (27) or by reversible inactivation of the dorsal vagal complex using local injection of bupivacaine (149). Recruitment of neural communication pathways combines with activation of macrophage-like cells in circumventricular organs by circulating pathogen-associated molecular patterns. This results in the local synthesis of proinflammatory cytokines that slowly diffuse into the neural compartment by volume diffusion while actively recruiting macrophages and microglia “en passant” (52, 126, 239). The involvement of brain proinflammatory cytokines in sickness behavior induced by systemic administration of cytokines or LPS has been repeatedly demonstrated by blocking experiments in which cytokine antagonists such as IL-1RA, a specific antagonist of IL-1 type I receptor, have been administered into the lateral ventricle of the brain in rodents injected with cytokines or LPS at the periphery (51, 118, 127). The specific brain areas that mediate sickness behavior have been difficult to delineate. There are several reasons for this, starting with the diffuse nature of microglial activation in the brain in response to systemic inflammation, as evidenced by positron emission tomography with ligands of the 18-kDa translocator protein (TSPO) in monkeys and humans injected with endotoxin (96, 198). TSPO is expressed on the outer mitochondrial membrane of microglia and is prominently upregulated in response to inflammation. Its level of expression in resting microglia is normally low but increases rapidly in activated microglia. This explains why imaging expression of TSPO is used as a marker of microglial activation despite the many limitations of the currently available TSPO radiotracers (240).
The second reason for the difficulties encountered in delineating the brain areas that mediate sickness behavior is that these brain areas differ according to the behavioral process affected by inflammation. Decreases in food intake culminating in anorexia are unlikely to be mediated by the same neuronal networks as fatigue or even anhedonia. Most of the research on neuroanatomy of sickness behavior has focused on endotoxin-induced anorexia and the role of prostaglandins and feeding modulating peptides, including proopiomelanocortin, leptin, neuropeptide Y, agouti-related protein, and ghrelin, and their neural targets in the hypothalamus (e.g., Refs. 62, 178, 200). This field of research has expanded beyond sickness behavior because of the somewhat paradoxical role of hypothalamic inflammation in the resetting of energy homeostasis that is associated with obesity (233). More in tune with the concept of sickness behavior, decreased social interactions in rats in response to LPS have been shown to be mediated by forebrain IL-1 acting on the central amygdala and dorsolateral bed nucleus of the stria terminalis in a prostaglandin-independent manner (127). In addition to causing social withdrawal, LPS has aversive properties that can be evidenced using conditioned taste aversion or conditioned place aversion (78, 247). Acquisition of a conditioned place aversion in response to LPS has been shown to be mediated by COX-1-dependent synthesis of PGE2 by endothelial cells of the blood-brain barrier. PGE2 acts on EP1 receptors located on dopamine D1 receptor-expressing neurons, with expression of the aversion being dependent on GABA-mediated inhibition of dopaminergic cells (78). The predominant involvement of prostaglandins rather than brain cytokines in this behavior is probably due to the time interval between injection of LPS and conditioned place aversion training (10 min). This time interval is much too short for induction of a cytokine cascade in response to LPS both at the periphery and in the brain.
Systemic inflammation caused by injection of LPS or proinflammatory cytokines is associated with motivational deficits that can best be characterized using effort tasks, in which animals have to exert a sustained effort to obtain an expected reward. In mice trained to obtain a sweet milk reward according to a progressive ratio 10 schedule (requiring 1 response for the first reward, 10 for the second, 20 for the third, and so on), administration of IL-1 decreased the breaking point, i.e., the ratio at which mice stopped responding for the reward (131). This was not due to a decreased sensitivity to reward, since LPS-treated mice trained to nose poke a switch key for a highly preferred food (chocolate pellets) by responding 10 times in succession and another key for a less-preferred food (grain pellets) by responding only once continued to respond more on the key giving them access to the highly preferred food than on the key giving them access to grain pellets (237). In terms of neurotransmitters, inflammatory stimuli have a profound depressive effect on activity of orexin-expressing neurons (82, 91). Orexinergic neurons are located in the perifornical lateral hypothalamic area and regulate motivational arousal, thanks to their widespread projections to the rest of the brain. These neurons are inhibited by neurotensin-expressing GABAergic interneurons that sense systemic inflammation indirectly via alterations in leptin (91). The link between orexin and motivation is provided by orexin-dependent glutamatergic projections onto dopaminergic neurons in the ventral tegmental area (28).
Despite its strong relatedness to fever, there is clear evidence that sickness behavior is mediated by mechanisms different from those of fever. The range of behaviorally active cytokines does not fully overlap with that of pyrogens; for instance, IL-6 has no behavioral effect despite its potent pyrogenic activity and its activating effects on the HPA axis (133). In the same manner, subdiaphragmatic vagotomy abrogates decreases in social exploration induced by LPS but has inconsistent effects on the fever response (141). In addition, injections of IL-1RA into the lateral ventricle of the brain abrogate LPS-induced decreases in social interactions but have no effect on fever and activation of the HPA axis (127).
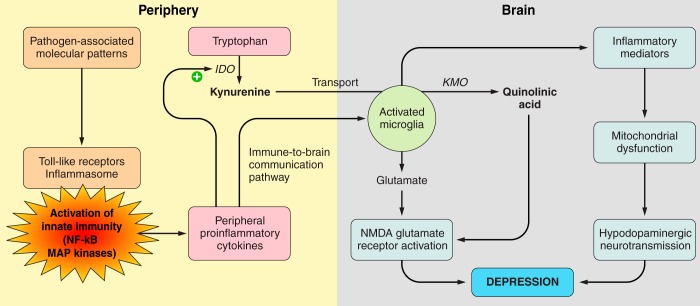
In summary, the effects of pathogenic microorganisms on thermoregulation, the HPA axis, and behavior are dependent on the de novo production of cytokines by activated innate immune cells. Transmission of this peripheral immune message to the brain involves multiple communication pathways with a possible relay in visceral organs such as the liver. These communication pathways ultimately recruit either other communication signals elaborated by brain microvascular endothelial cells, e.g., prostaglandins, or the same communication signals, e.g., IL-1, produced by brain innate immune cells (perivascular macrophages and micoglia). Prostaglandins are prominently involved in very short-term responses to inflammation (<1 h), whereas brain cytokines are more important for relatively longer responses (several hours) (FIGURE 3).
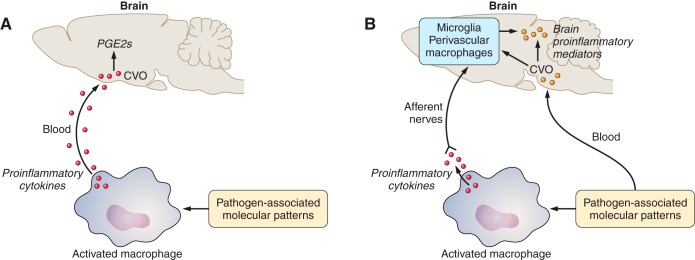
FIGURE 3.
Immune-to-brain communication pathways. In response to pathogen-associated molecular patterns such as lipopolysaccharide sensed by Toll-like receptors and the inflammasome (not represented in the figure), activated macrophages produce and release proinflammatory cytokines in their microenvironment, including IL-1β (red circles). As presented in A, proinflammatory cytokines were initially supposed to be released in the general circulation and act at the level of circumventricular organs (CVO) where the blood-brain barrier is fenestrated. Proinflammatory cytokines were proposed to induce there the release of lipophilic prostaglandin E2 acting as secondary messengers on neurons. However, the demonstration that immunelike cells in the brain including meningeal and perivascular macrophages and microglia produce and release brain proinflammatory cytokines led to a different representation illustrated in B. The peripheral immune signal is relayed to the brain by afferent nerves. This neural message together with slowly diffusing cytokines produced at the level of circumventricular organs and prostaglandins produced by brain endothelial cells in response to circulating pathogen-associated molecular patters results in the production of brain cytokines by activated microglia. Overspill of cytokines in the general circulation can also be transported for some of them into the brain side of the blood-brain barrier (not represented in the figure).
E. Role of Brain Cytokines in Synaptic Plasticity
Cytokines are not only expressed in the brain in response to peripheral immune stimuli. They are also present constitutively in the brain. Despite their expression levels being much lower than those of their inducible counterparts, they play an important role in synaptic physiology and plasticity. One example is the constitutive regulation by glial TNF of the surface expression of alpha-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA) receptors on hippocampal neurons. Exposure of cultured hippocampal neurons to TNF increased the levels of surface AMPA receptors in the plasma membrane of synapses, whereas blockade of endogenous TNF by treating cultures with a soluble form of the TNF receptor 1 had the reverse effect (12). Similar effects were obtained in hippocampal slices. In both cases, the influence of TNF on AMPA receptor trafficking resulted in rapid changes in synaptic strength at glutamate excitatory synapses. Further studies showed that these effects are specific to TNF and do not generalize to other inflammatory cytokines (221). They are mediated by TNFR1 and phosphoinositol-3-kinase activation. In addition, TNF also increased the endocytosis of surface GABAA receptors, resulting in a decrease in inhibitory synaptic transmission. The adaptive role of TNF in the regulation of synapses varies depending on the brain area. While cortical pyramidal cells and motor neurons behave like hippocampal neurons in their response to TNF, this is not the case for striatal neurons. TNF drives the internalization of AMPA receptors and reduces corticostriatal synaptic strength on GABAergic medium spiny neurons of the dorsolateral striatum (135).
TNF acts not only on neurons but also on astrocytes. Constitutive TNF is able to control glutamate release from astrocytes, as demonstrated by the inability of astrocytes from TNF or TNF receptor knockout mice to release glutamate in response to the activation of P2Y1 receptors by ATP released during synaptic activity. Because of this deficiency, the process of gliotransmission is impaired. The lack of astrocyte-dependent activation of presynaptic N-methyl-d-aspartate (NMDA) receptors compromises both synaptic transmitter release and synaptic strengthening at the level of glutamatergic synapses (199).
In contrast to what was thought originally, constitutive TNF is produced not by neurons but by microglia. Microglia are the resident macrophage population of the central nervous system. Beyond their role as phagocytic cells in the central nervous system when activated by injury or microbial infection, microglial cells are also involved in the development and maintenance of normal synaptic function. Like most tissue macrophages, microglia do not originate from blood monocytes or meningeal macrophages but from yolk sac primitive macrophages during early development (65, 85). They persist by self-renewal in the central nervous system until adulthood and do not need to be replenished by peripheral cells from the circulation (86). Their differentiation and maintenance are dependent on CSF-1 and IL-34 (90, 179, 243), both acting via CSF-1 receptors.
The formation of mature neural circuits requires the activity-dependent elimination or pruning of inactive synapses. Microglia play an important role in this process, as demonstrated by their ability to engulf synaptic material during postnatal development in the mouse (174). They make use of several signaling pathways for this, including the classic complement cascade that is part of the innate immune system. Working on the mouse reticulogeniculate system, Stevens and colleagues (201, 223) demonstrated in an elegant series of experiments that the complement protein C1q, the initiating protein in the classical complement cascade, and the downstream complement protein C3 localize to immature synapses and are necessary for the developmental pruning of nonfunctional reticulogeniculate synapses. C1q and C3 bind to C3 receptors that are expressed by microglia. These receptors are upregulated in microglia during the period of synaptic elimination and are downregulated later on. Furthermore, C3 receptor knockout mice displayed reduced microglial phagocytic function and sustained deficits in eye-specific segregation of synaptic inputs in the reticulogeniculate system and in synaptic connectivity (201). What is remarkable here is the analogy of function in the immune system and in the central nervous system: in both systems, complement proteins clear cellular material that has been tagged at its membrane surface for elimination (222). In the central nervous system, this process requires a close cooperation between synapse targets and microglia.
Microglial cells interact with neurons and synapses via several signaling pathways other than the complement cascade. One of these signaling pathways involves the chemokine CX3CL1, also known as fractalkine, and its receptor CX3CR1. Chemokines are used by hematopoietic and nonhematopoietic tissues to attract immune target cells by chemotaxis. In the central nervous system, CX3CL1 is mostly expressed by neurons and CX3CR1 is uniquely expressed on microglial cells (5, 138). Mice lacking the fractalkine receptor displayed a transient deficit in synaptic pruning during the second and third postnatal weeks, together with electrophysiological signs of synaptic abnormalities (174). However, this was probably due to the role of the CX3CL1/CX3CR1 signaling pathway in microglia migration into the brain during development rather than to the involvement of this pathway in the tagging of synapses to be eliminated, given the reduced microglial density in the brains of CX3CR1 knockout mice compared with littermate controls.
Another signaling pathway makes use of LBP that tags synapses in the developing hippocampus (245). In the innate immune system, LBP acts as an acute phase protein and is necessary for LPS to bind to membrane-bound CD14 on macrophages before being able to activate TLR4 (258). LBP is also temporarily expressed on hippocampal synapses during development, in close association with CD14 surface molecules present on microglia cells (245). In rodents, early life stress in the form of daily brief pup-dam separations is well known to cause increased anxiety-like behavior at adulthood. Early life stress decreased the expression of synaptic but not plasmatic LBP. Genetic deletion of LBP resulted in increased spine density and abnormal spine morphology in the hippocampus, and this was associated with increased anxiety-like behavior at adulthood. These intriguing results point to a possible role for LBP in the development and function of hippocampal synapses during the first weeks of life (245).
F. Summary
The neuroendocrine perspective that initially dominated studies of the neural effects of cytokines left little room for the possibility of a local action of these molecules in the central nervous system despite the fact that cytokines were initially described by immunologists as autocrine and paracrine communication factors. It is only after cytokines were identified in the brain with their receptors that this notion changed. Cytokines are not only induced in the central nervous system in response to peripheral immune stimuli but in addition they are expressed there constitutively and serve as important plasticity factors in the formation and stabilization of neuronal circuits during development.
IV. ALTERATIONS IN THE COMMUNICATION BETWEEN THE IMMUNE AND THE NERVOUS SYSTEM: FROM PHYSIOLOGY TO PATHOLOGY
Because of the bidirectional communication between the brain and the immune system and the reliance of each of these systems on intercellular communication molecules used by the other system, any alteration in one of the systems has the potential to impact the functioning of the other system. It is beyond the scope of this review to describe all possible instances of the reciprocal alterations in the communication between the immune and the nervous system that contribute to pathophysiology. Only two examples will be presented to illustrate this notion, one example of a disorder affecting the brain, major depressive disorder, and one example of a pathology involving the immune system, cancer. In both cases, the research agenda has been the same: long-range communication between systems were investigated first before the possibility of short-range communication mechanisms was considered. In the context of psychiatric disorders, the exact communication mechanisms between the immune system and the brain are not yet fully elucidated, as the research is still mainly at the description level. In the context of stress and cancer, the attention has shifted from long-range to short-range communication mechanisms involving the sympathetic nervous system, These two examples illustrate the important concept that pathological processes develop on the basis of an intricate network of short-range and long-range cellular and molecular mechanisms of communication.
A. Major Depressive Disorder
Given that antidepressant drugs are medications that increase the synaptic availability of serotonin and other monamines in the central nervous system, depression is usually conceived of as resulting from a deficiency in these neurotransmitter systems. However, the monoaminergic theory of depression cannot account for all the features of depression and its response to medication. This has led to a reformulation of the original hypothesis. The modern neurobiology of depression emphasizes the role of neurotrophic factors and synaptic plasticity, making depression the result of long-term alterations in synaptic strength in brain regions that regulate mood, with brain-derived neurotrophic factor (BDNF) as a key transducer of the effect of antidepressant drugs (165).
This brain-centric view of depression leaves little room for mechanisms linking depression to immunity. The first studies on immune functions in depressed subjects focused on the apparent immunosuppression in these subjects, evidenced by reduced proliferative responses of lymphocytes to mitogens, decreased natural killer cell activity, and alterations in numbers of several white blood cell populations (102). However, subsequent studies revealed a much more complex picture with signs of activation of the monocytic and lymphocytic arms of cell-mediated immunity, characterized by increased numbers of peripheral blood leukocytes, monocytes, and neutrophils, and elevated circulating levels of inflammatory cytokines and acute-phase proteins (145). This association between depression and inflammation has been since confirmed by several meta-analyses (94, 104, 106). Such an association is not necessarily surprising, in view of the likely degradation of body care and hygiene habits that occurs in depressed subjects compared with the general population. However, this did not discourage researchers from investigating the possibility that inflammation plays a causal role in depression, given their potent effects on sickness behavior and the similarity between some of the symptoms of sickness and the symptoms of depression (254). In addition, prospective epidemiological studies confirmed that adults with high levels of circulating IL-6 have a higher probability of developing a major depressive disorder within 11–16 yr (122), and the same was true for children aged 9 yr when examined for mental disorders at 18 yr of age (120). In animal studies, some of the behavioral alterations that develop in rodents injected with LPS resemble the anhedonia and decreased sensitivity to reward that are characteristic of depression. In particular, rats injected with LPS displayed a reduction in preference for food, a decrease in consumption of a saccharin solution, and a suppression of sexual behavior. All of these responses were alleviated by chronic but not acute treatment with imipramine, a typical antidepressant drug (254).
Understanding about the mechanisms of inflammation-associated depression began to accrue in the late 1990s with studies in patients with metastatic melanoma or kidney cancer treated with IFN-α and IL-2 to stimulate the immune system and to help eliminate tumor cells that do not respond to chemotherapy or radiation therapy. All patients respond to this form of immunotherapy with sickness symptoms, in the form of fatigue, reduced appetite, and sleep disorders. However, one-third to one-half of patients develop symptoms of depression within a few weeks of treatment (40, 41). These clinical observations indicate that depression develops on a background of immune-mediated sickness, probably via an additional mechanism triggered by inflammation.
Insight into this mechanism came from the observation that the intensity of symptoms of depression is correlated with signs of activation of the tryptophan metabolizing enzyme indoleamine 2,3-dioxygenase (IDO) (42). IDO is an immune-inducible enzyme that metabolizes tryptophan along the kynurenine pathway and plays an important role in immunoregulation (161). The causal involvement of this metabolic pathway in the pathogenesis of inflammation-induced depression was confirmed in mice injected with LPS at a dose that activated IDO. These mice developed depression-like behavior characterized by increased immobility in the forced-swim test and in the tail-suspension test, and decreased sucrose preference when given the choice between a sucrose solution and tap water for drinking. Pharmacological or genetic blockade of IDO activation abrogated depression-like behavior in LPS-treated mice (168). The same effect was obtained in mice inoculated with Bacille Calmette-Guerin, an attenuated form of Mycobacterium bovis, to stimulate the immune system chronically rather than acutely (167).
The initial hypothesis for explaining IDO’s role in inflammation-induced depression was that its activation decreases the bioavailability of tryptophan for the synthesis of the brain neurotransmitter serotonin (53). This hypothesis had the advantage of fitting the monoaminergic theory of depression. However, a fine-grained analysis of the levels of tryptophan, kynurenine, and kynurenine metabolites in the blood and cerebrospinal fluid of IFN-α-treated patients revealed that tryptophan decreased only in the blood but not in the cerebrospinal fluid, whereas kynurenine and its metabolites increased in both compartments (183). These results mean that the brain can compensate for the decrease in peripheral tryptophan levels, probably by allowing more tryptophan to be transported into the brain by the large amino acid transporter LAT1. Blood-brain barrier transport experiments in gerbils showed that nearly all of the kynurenine that is found in the brain in response to systemic LPS comes from the periphery (121).
Brain kynurenine is further metabolized into neurotoxic kynurenine metabolites by the immune-inducible enzyme kynurenine monooxygenase, which is present in microglia. One of these neurotoxic kynurenine metabolites is quinolinic acid, an agonist of the NMDA receptor. When activated in response to immune stimulation, microglia also release glutamate extrasynaptically. This release takes place via the cystine-glutamate exchanger that regulates biosynthesis of the intracellular antioxidant glutathione. In addition, astrocytes that normally uptake glutamate to recycle it via the glutamate-glutamine cycle become much less efficient for doing so in conditions of inflammation, because of the downregulation of their high-affinity glutamate transporters (89). The net result is a spillover of glutamate into the extrasynaptic space, which, in combination with quinolinic acid, activates extrasynaptic NMDA receptor. This explains why blockade of NMDA receptors by ketamine is able to abrogate the depression-like behavior induced by LPS in mice (241). It is important to note that characterization of this glutamatergic pathway does not discard a role for serotonin in inflammation-induced depression. There is evidence in particular that inflammation activates the serotonin transporter, which results in a decrease in the amount of serotonin available at the synapses (10).
During inflammation tetrahydrobiopterin is turned away from its role as a cofactor for the hydroxylase enzymes that catalyze the formation of 5-hydroxy-tryptophan from tryptophan and tyrosine and dihydroxyphenylalanine from phenylalanine, to be mainly consumed for the formation of neopterin and nitric oxide by activated immune cells. This results in a decrease in the biosynthesis of monoamines (216).
The mechanisms of inflammation-induced depression are summarized in FIGURE 4. From this figure it is apparent that much has been learned about how synaptic function is affected by immune mediators produced by brain immunelike cells. Much less is known about the exact nature of the immune-to-brain communication pathways that are ultimately responsible for neuroinflammation. Recruitment of the brain machinery is supposed to be dependent on circulating factors represented either by kynurenine as a consequence of peripheral IDO activation or by pathogen-associated molecular patterns originating from the gut or other barrier organs, especially with alterations in the microbiota (144, 211). These circulating factors do not need to directly reach the brain to induce depression. They can modulate the activity of brain regions involved in the processing of emotions by activating afferent autonomic nerves, as demonstrated very elegantly by neuroimaging experiments in humans experiencing depressed mood in response to typhoid vaccination (98).
FIGURE 4.
Mechanisms of inflammation-induced depression. In addition to activation of the immune-to-brain communication pathways represented in FIGURE 3, peripheral proinflammatory cytokines activate the tryptophan metabolizing enzyme indoleamine 2,3-dioxygenase (IDO) that transforms tryptophan into kynurenine. Kynurenine produced at the periphery is transported into the brain where it is further metabolized into neurotoxic kynurenine metabolites including quinolinic acid by another microglia-associated enzyme, kynurenine monooxygenase (KMO). Together with glutamate released by activated microglia, quinolinic acid activates the N-methyl-d-aspartate (NMDA) receptors. Independently of this pathway, inflammatory mediators released by activated microglia and brain endothelial cells can also downregulate dopaminergic neurotransmission via oxidative stress and mitochondrial dysfunction. Activation of NMDA receptors and deficient dopaminergic neurotransmission both result in depression symptoms.
It is not yet clear whether the mechanisms that underlie the development of inflammation-induced depression also account for depression related to other causal factors, including stress. The issue that still needs to be investigated is how these neuroimmune interactions can be activated in the brain in the absence of overt inflammation. At the clinical level, there is evidence that even relatively minor stressors, such as the Trier social stress test in which participants are asked to prepare and present an impromptu speech and to perform a difficult mental task in front of a nonresponsive, intimating audience, can lead to the increased production of IL-6 (190). The same elevations in circulating IL-6 are found in individuals exposed to chronic stress. It is not known yet whether this IL-6 derives from immune or nonimmune sources. Interestingly, stress-induced elevations in IL-6 are higher in subjects with a history of early life stress (44) and in subjects with low socioeconomic status (34). The fact that these conditions are associated with chronic, low-grade inflammation and activation of immune-to-brain communication pathways (166) makes it very likely that psychosocial stress-induced IL-6 is released by activated innate immune cells, possibly via a β2-adrenergic-dependent mechanism.
Most of the preclinical studies that address the question of how nonimmune stressors can activate the innate immune system rely on the social defeat paradigm, in which a resident male mouse is exposed to attacks and defeat from an aggressor, another male mouse that is larger and trained as a fighter. The defeat episode lasts for only a few minutes, after which mice are typically separated to limit the extent of wounding. Social defeat is repeated daily for several days and in some of these experiments, the resident mouse is forced to cohabit with its aggressor after it has been attacked, although it is protected from further attacks by a perforated divider separating the cage into two compartments. Mice exposed to repeated social defeat show social avoidance when tested with a new male mouse and decreased mobility in potentially frightening environments.
Despite resembling anxiety more so than depression, these behavioral alterations are reversed by chronic but not acute antidepressant treatment (88). In addition, they are associated with reduced synaptic plasticity, chromatin remodeling, and transcriptional activation, which also are responsive to antidepressant treatment. Each defeat episode leads to an intense activation of the HPA axis and the sympathetic nervous system, and this activation is sustained by cohabitation. Socially defeated mice show increased numbers of highly inflammatory and glucocorticoid-insensitive bone marrow-derived myeloid cells in their general circulation. The release of myeloid cells is mediated by activation of β2-adrenergic receptors. Myeloid cells are recruited to the brain in a chemokine-dependent manner (251). This results in the activation of resident microglial cells and the local production of inflammatory cytokines that negatively affect synaptic plasticity (249). These effects could also be mediated downstream of brain cytokines by microglial COX-1-mediated production of PGE2 acting on EP1 receptors on GABAergic neurons located in the medial prefrontal cortex. Activation of EP1 would lead to inhibition of mesocortical dopaminergic neurons (227).
There are individual differences in the response to repeated social defeat. Approximately two-thirds of the mice develop a susceptible behavioral phenotype, whereas other mice are resilient. Mice can be characterized as susceptible or resilient on the basis of their IL-6 response to the first episode of social defeat: those with higher circulating IL-6 levels were more likely to be susceptible than were those with lower IL-6 (105). This elevation in circulating IL-6 was due to a higher number of circulating leukocytes and an increased responsiveness to LPS stimulation. Furthermore, adoptive transfer of bone marrow hematopoietic progenitor cells isolated from susceptible mice into naive wild-type mice or IL-6 knockout mice increased the probability of social avoidance in the bone marrow chimera mice when they were submitted to a subthreshold repeated social stress paradigm. Conversely, transfer of hematopoietic progenitor cells from IL-6-deficient mice into naive wild-type mice decreased the probability of social avoidance. Both IL-6 knockout mice and wild-type mice that were administered IL-6-neutralizing antibodies had a higher probability of resilience (105). These results show that leukocyte-derived sources of IL-6 are critical in mediating the behavioral effects of repeated social stress, although it is not yet clear how peripheral IL-6 modulates susceptibility.
Immunological memory is also affected by repeated social defeat. The experience of repeated social defeat is associated with an augmentation of memory T-cell populations in response to a viral infection occurring after the stress episode (152, 153). These features are not restricted to immunity but extend to immune-to-brain communication. Adoptive transfer of lymphocytes from immunocompetent mice submitted to repeated social defeat into immunocompromised stress-naive mice prevented the development of anxiety-like behavior in these mice, probably by decreasing the inflammatory response to the stress of defeat both at the periphery and in the brain (32). This effect was not limited to social defeat and prevention, as adoptive transfer of lymphocytes from mice exposed to repeated social defeat into immunocompromised mice that had been made anxious by repeated exposure to restraint normalized their behavior. These intriguing findings confirm the idea that exposure to psychological stressors could program the adaptive immune system to confer resistance to stressors (136), but the exact mechanisms remain to be elucidated.
B. Cancer
The nonscientific literature is replete with anecdotal references to the role of personality factors, repressed emotions, and psychosocial stressors in the development of cancer. There have been many attempts to strengthen this narrative through experimental studies of the influence of stressors on the proliferation and dissemination of tumor cells. The golden age of psychoneuroimmunology has produced some examples of this, with publications in high impact factor journals describing the influence of the lack of control over electric shocks on tumor growth in xenograft models of cancer (209, 238). Current research in this field is now decisively mechanistic and builds on our current understanding of tumor biology. In an elegant series of experimental studies on the effect of repeated immobilization stress on the progression and dissemination of cancer in murine models of solid epithelial tumors, oncologists collaborating with psychologists have clearly demonstrated a definitive role for activation of the sympathetic nervous system in modifying the tumor microenvironment and the immune response to the tumor (FIGURE 5) (4, 47, 109, 132, 210, 228).
FIGURE 5.
Mechanism of stress-induced tumor progression and dissemination. Stress facilitates the development of immunotolerance by activation of the hypothalamic pituitary adrenal axis which results in decreased cytotoxicity of natural killer cells (NK cells) and reduced cellular immune responses to the tumor antigens. At the same time, activation of the sympathetic nervous system induces profound alterations in tumor cells and in the tumor microenvironment both directly by sympathetic nerve endings innervating the organ in which the tumor develops and indirectly via the liver and adipose tissue. Red arrows represent communication via the general circulation, dashed blue arrows represent communications via nerves, and blue arrows represent communication within the tumor microenvironment. NK, natural killer; EMT, epithelial-to-mesenchymal translation of cancer cells; DNA, deoxyribonucleic acid; MMP, matrix metalloproteinase; HIF-1α, hypoxia inducible factor-1α; PI3/AKT, phosphatidylinositol 3-kinase/protein kinase B signaling pathway; PKM2, M2 isoform of pyruvate kinase. [Adapted from Cole et al. (47).]
Not surprisingly, most of these effects are mediated by β2-adrenergic activation of multiple local intracellular signaling pathways involving protein kinases, CREB, EPAC, and MAPK. The net results include inhibition of DNA damage repair and p53-associated apoptosis, activation of oncogenic signaling pathways, increased inflammation by enhanced expression of proinflammatory cytokines, recruitment of macrophages into the tumor parenchyma, production of tumor growth factors (including transforming growth factor-β, vascular endothelial growth factor, and matrix metalloproteases), activation of mesenchymal cells present in tumor stroma, promotion of angiogenesis, inhibition of anoikis, and increased resistance to chemotherapy. In addition, activation of sympathetic nervous system signaling contributes to the escape of tumors from immunosurveillance by inhibiting type I and II interferon signaling and by suppressing the cytotoxic function of T lymphocytes and natural killer cells.
Nerves innervating solid tumors and their microenvironment mediate the influences of stress on tumor progression and dissemination. Female mice with orthotopic or spontaneous mammary tumors responded to restraint stress by increased turnover of norepinephrine in sympathetic nerves innervating the tumor (225). The peripheral nerves that innervate the tumor are not restricted to those preexisting in the tissue in which the tumor develops: tumor cells can actually promote neurogenesis. In two murine models of cancer, including an orthotopic xenograft model of human prostate cancer cells in nude mice and a genetic model of prostate cancer in immunocompetent mice, tumor growth was associated with infiltration of autonomic nerve fibers into the tumor mass. Chemical or surgical sympathectomy as well as genetic deletion of β2-adrenergic receptors prevented the early phase of tumor development. Pharmacological blockade or genetic disruption of the stromal type 1 muscarinic receptor abrogated tumor dissemination (146). Similar results have been obtained in a mouse model of gastric cancer (256). Sensory neurons can also play a role, as demonstrated by the slower initiation and progression of cancer after sensory neuron ablation by neonatal injection of capsaicin in a model of pancreatic ductal adenocarcinoma (197).
In general, the notion that the peripheral nervous system is able to adapt to an ongoing disease process and contribute to its evolution is not totally new. For instance, complex interactions between neurons, glial cells, immune cells, and endocrine cells have been shown to take place during pancreatitis. They modulate inflammation and cancer growth, while at the same time undergoing plastic changes in the proportion of autonomic and sensory fibers innervating the affected organ and in the quantity of mediators they release. This form of neural plasticity has been well studied in pancreatitis and its progression to pancreatic cancer (55). The outgrowth of nerves in solid tumors is driven by the production of neurotrophic factors, such as nerve growth factor (NGF), by cancer cells (111). Knocking down NGF or its receptors, or administering an NGF receptor inhibitor, attenuated the proliferation and migration of pancreatic cancer cells in vitro (11). This dependence on neurotrophins could account for the perineural invasion that characterizes tumor metastasis in several solid malignancies, such as head and neck squamous cell carcinoma (189).
C. Summary
We have restricted ourselves to only two examples to illustrate the possibility that pathological processes develop on the basis of an intricate network of short- and long-range cellular and molecular mechanisms of communication. These examples are not the only ones, and there are many other instances of altered communication mechanisms between the immune system and the nervous system in the pathophysiology of many disorders. This intricacy explains at least in part the important psychological comorbidity of physical illness and provides some clues as to how to better treat these disorders.
V. CONCLUSIONS AND PERSPECTIVES
In the earlier ages of psychoneuroimmunology, Blalock (21) proposed that the immune system may function as a diffuse sensory organ specialized in the detection of the nonself in a manner complementary to that employed by classic sensory organs. He speculated that “in the future, it may be difficult to distinguish the receptors and signals that these systems use for communication within and between one another.” Because of the reluctance of the scientific community to accept this concept despite the convincing examples of communication Blalock provided, the original review paper he submitted was ultimately published as an opinion piece. This reluctance was still apparent a few years later, when the first review paper on the neuroimmune mechanisms of sickness behavior was submitted (119).
Thanks to the research work that has been carried out since then, the situation has changed considerably. It is now fully recognized that the nervous system and the immune system do not function independently from one another, but that the central nervous system utilizes cellular and molecular elements of immune communication for its own purposes, while the immune response is regulated in part by neuroendocrine mediators produced by immunocytes (FIGURE 6). The intricate interactions between these two systems play a key role in health and disease. Several examples of this necessary communication between immune cells and neuronal cells have been provided in this review, and their implications for pathology have been discussed. Not only does the immune system have a considerable impact on neural functions, but conversely the somatosensory and autonomic nervous systems play an active role in the coordination of the organism’s defense to infection and injury via positive and negative modulation of immune responses. Pathology can emerge either from the dysfunction of one of these interacting systems or from the deflection of the molecular or cellular mechanisms specifically involved in their reciprocal regulation.
FIGURE 6.
Schematic representation of neuroimmune interactions. A: the initial notion that neuroimmune interactions take place via mediators released in the general circulation by the neuroendocrine system. B: summary of the knowledge presented in this review showing that long-distance communication between the central nervous system and the immune system takes place mainly via neural pathways and much less so via circulating neuroendocrine factors. Long-distance communication via neural pathways is bidirectional, from the central nervous system to the immune system and vice versa. Long-distance communication pathways modulate the functioning of local or short-range communication pathways that involve intricate interactions between resident immunelike cells (mainly microglia and astrocytes, but also endothelial cells) and neuronal cells in the nervous system, and between immune mediators and neuroendocrine mediators produced locally by immune cells in the immune system in addition to mediators released locally by nerve endings. The immune phenotype of the microenvironment of the affected organ can be modified by alterations in immune cell trafficking induced by noradrenergic or more rarely cholinergic modulation (not represented in the figure) of the vasculature of lymphoid organs. This is more likely to take place at the periphery than in the nervous system that is protected by the blood-brain barrier even if it can become leaky in some conditions. Blue arrows correspond to neural communication pathways and red arrows to humoral communication pathways.
It is generally agreed that the knowledge gained from these studies will help to clarify pathophysiology and inform future therapeutics, thanks to the emergence of new targets. For example, who would have thought a few years ago that it would be possible to treat depression with the TNF antagonist infliximab, at least in patients with low-grade chronic inflammation (184), or that the use of beta-blockers could prolong overall survival in patients with ovarian cancer (244)? Nonetheless, adding such approaches to the therapeutic horizon will require detailed investigation into which patients will likely benefit from them and at what time point in the course of the disease they are more likely to succeed.
Concerning this last aspect, it is important to note that we still know very little, if anything at all, about the temporal aspect of neuroimmune interactions. As just one example, a recent study demonstrated that, although the neuropathic pain induced by chemotherapeutic agents such as paclitaxel is mediated at the very early stage of its development by activation of the innate immune system, its resolution is actually dependent on the involvement of the adaptive immune system and more specifically the trafficking of CD8+ T cells into the dorsal root ganglia (129). This means that a treatment targeting the immune system could actually be detrimental when given at the wrong time point in the disease process.
GRANTS
This work was supported by National Cancer Institute Grants R01CA193522 and CA183736, National Institute of Mental Health Grant R21MH104694, and National Institute of Neurological Disorders and Stroke Grant R01NS073939.
DISCLOSURES
No conflicts of interest, financial or otherwise, are declared by the author.
ACKNOWLEDGMENTS
Address for reprint requests and other correspondence: R. Dantzer, Dept. of Symptom Research, Univ. of Texas MD Anderson Cancer Center, Houston, TX 77005 (e-mail: rdantzer@mdanderson.org).
REFERENCES
- 1.Ader R. Historical perspectives on psychoneuroimmunology. In: Psychoneuroimmunology, Stress, and Infection, edited by Friedman H, Klein TW, Friedman AL. Boca Raton, FL: CRC, 1995, p. 1–21. [Google Scholar]
- 2.Ader R, Cohen N. Behaviorally conditioned immunosuppression. Psychosom Med 37: 333–340, 1975. doi: 10.1097/00006842-197507000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Antoni MH. Psychosocial intervention effects on adaptation, disease course and biobehavioral processes in cancer. Brain Behav Immun 30, Suppl: S88–S98, 2013. doi: 10.1016/j.bbi.2012.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Armaiz-Pena GN, Allen JK, Cruz A, Stone RL, Nick AM, Lin YG, Han LY, Mangala LS, Villares GJ, Vivas-Mejia P, Rodriguez-Aguayo C, Nagaraja AS, Gharpure KM, Wu Z, English RD, Soman KV, Shahzad MM, Zigler M, Deavers MT, Zien A, Soldatos TG, Jackson DB, Wiktorowicz JE, Torres-Lugo M, Young T, De Geest K, Gallick GE, Bar-Eli M, Lopez-Berestein G, Cole SW, Lopez GE, Lutgendorf SK, Sood AK. Src activation by β-adrenoreceptors is a key switch for tumour metastasis. Nat Commun 4: 1403, 2013. doi: 10.1038/ncomms2413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Arnoux I, Audinat E. Fractalkine Signaling and Microglia Functions in the Developing Brain. Neural Plast 2015: 689404, 2015. doi: 10.1155/2015/689404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Asmus SE, Parsons S, Landis SC. Developmental changes in the transmitter properties of sympathetic neurons that innervate the periosteum. J Neurosci 20: 1495–1504, 2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Aubert A, Goodall G, Dantzer R, Gheusi G. Differential effects of lipopolysaccharide on pup retrieving and nest building in lactating mice. Brain Behav Immun 11: 107–118, 1997. doi: 10.1006/brbi.1997.0485. [DOI] [PubMed] [Google Scholar]
- 8.Auron PE, Webb AC, Rosenwasser LJ, Mucci SF, Rich A, Wolff SM, Dinarello CA. Nucleotide sequence of human monocyte interleukin 1 precursor cDNA. Proc Natl Acad Sci USA 81: 7907–7911, 1984. doi: 10.1073/pnas.81.24.7907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Avitsur R, Levy S, Goren N, Grinshpahet R. Early adversity, immunity and infectious disease. Stress 18: 289–296, 2015. doi: 10.3109/10253890.2015.1017464. [DOI] [PubMed] [Google Scholar]
- 10.Baganz NL, Blakely RD. A dialogue between the immune system and brain, spoken in the language of serotonin. ACS Chem Neurosci 4: 48–63, 2013. doi: 10.1021/cn300186b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bapat AA, Munoz RM, Von Hoff DD, Han H. Blocking Nerve Growth Factor Signaling Reduces the Neural Invasion Potential of Pancreatic Cancer Cells. PLoS One 11: e0165586, 2016. doi: 10.1371/journal.pone.0165586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Beattie EC, Stellwagen D, Morishita W, Bresnahan JC, Ha BK, Von Zastrow M, Beattie MS, Malenka RC. Control of synaptic strength by glial TNFalpha. Science 295: 2282–2285, 2002. doi: 10.1126/science.1067859. [DOI] [PubMed] [Google Scholar]
- 13.Bener D, Wohlman A, Itzik A, Yirmiya R, Ben-Hur T, Weidenfeld J. Glucocorticoid resistance following herpes simplex-1 infection: role of hippocampal glucocorticoid receptors. Neuroendocrinology 85: 207–215, 2007. doi: 10.1159/000102976. [DOI] [PubMed] [Google Scholar]
- 14.Berkenbosch F, van Oers J, del Rey A, Tilders F, Besedovsky H. Corticotropin-releasing factor-producing neurons in the rat activated by interleukin-1. Science 238: 524–526, 1987. doi: 10.1126/science.2443979. [DOI] [PubMed] [Google Scholar]
- 15.Bernton EW, Beach JE, Holaday JW, Smallridge RC, Fein HG. Release of multiple hormones by a direct action of interleukin-1 on pituitary cells. Science 238: 519–521, 1987. doi: 10.1126/science.2821620. [DOI] [PubMed] [Google Scholar]
- 16.Besedovsky H, del Rey A, Sorkin E, Dinarello CA. Immunoregulatory feedback between interleukin-1 and glucocorticoid hormones. Science 233: 652–654, 1986. doi: 10.1126/science.3014662. [DOI] [PubMed] [Google Scholar]
- 17.Besedovsky H, Sorkin E. Network of immune-neuroendocrine interactions. Clin Exp Immunol 27: 1–12, 1977. [PMC free article] [PubMed] [Google Scholar]
- 18.Besedovsky H, Sorkin E, Keller M, Müller J. Changes in blood hormone levels during the immune response. Proc Soc Exp Biol Med 150: 466–470, 1975. doi: 10.3181/00379727-150-39057. [DOI] [PubMed] [Google Scholar]
- 19.Besedovsky HO, Del Rey A, Sorkin E. Antigenic competition between horse and sheep red blood cells as a hormone-dependent phenomenon. Clin Exp Immunol 37: 106–113, 1979. [PMC free article] [PubMed] [Google Scholar]
- 20.Besedovsky HO, Del Rey A, Sorkin E, Lotz W, Schwulera U. Lymphoid cells produce an immunoregulatory glucocorticoid increasing factor (GIF) acting through the pituitary gland. Clin Exp Immunol 59: 622–628, 1985. [PMC free article] [PubMed] [Google Scholar]
- 21.Blalock JE. The immune system as a sensory organ. J Immunol 132: 1067–1070, 1984. [PubMed] [Google Scholar]
- 22.Blalock JE. A molecular basis for bidirectional communication between the immune and neuroendocrine systems. Physiol Rev 69: 1–32, 1989. [DOI] [PubMed] [Google Scholar]
- 23.Blalock JE. Proopiomelanocortin and the immune-neuroendocrine connection. Ann N Y Acad Sci 885: 161–172, 1999. doi: 10.1111/j.1749-6632.1999.tb08673.x. [DOI] [PubMed] [Google Scholar]
- 24.Blalock JE, Smith EM. Human leukocyte interferon: structural and biological relatedness to adrenocorticotropic hormone and endorphins. Proc Natl Acad Sci USA 77: 5972–5974, 1980. doi: 10.1073/pnas.77.10.5972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Blatteis CM. Neuromodulative actions of cytokines. Yale J Biol Med 63: 133–146, 1990. [PMC free article] [PubMed] [Google Scholar]
- 26.Blatteis CM. The onset of fever: new insights into its mechanism. Prog Brain Res 162: 3–14, 2007. doi: 10.1016/S0079-6123(06)62001-3. [DOI] [PubMed] [Google Scholar]
- 27.Bluthé RM, Michaud B, Kelley KW, Dantzer R. Vagotomy blocks behavioural effects of interleukin-1 injected via the intraperitoneal route but not via other systemic routes. Neuroreport 7: 2823–2827, 1996. doi: 10.1097/00001756-199611040-00083. [DOI] [PubMed] [Google Scholar]
- 28.Borgland SL, Chang SJ, Bowers MS, Thompson JL, Vittoz N, Floresco SB, Chou J, Chen BT, Bonci A. Orexin A/hypocretin-1 selectively promotes motivation for positive reinforcers. J Neurosci 29: 11215–11225, 2009. doi: 10.1523/JNEUROSCI.6096-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Borovikova LV, Ivanova S, Nardi D, Zhang M, Yang H, Ombrellino M, Tracey KJ. Role of vagus nerve signaling in CNI-1493-mediated suppression of acute inflammation. Auton Neurosci 85: 141–147, 2000. doi: 10.1016/S1566-0702(00)00233-2. [DOI] [PubMed] [Google Scholar]
- 30.Borovikova LV, Ivanova S, Zhang M, Yang H, Botchkina GI, Watkins LR, Wang H, Abumrad N, Eaton JW, Tracey KJ. Vagus nerve stimulation attenuates the systemic inflammatory response to endotoxin. Nature 405: 458–462, 2000. doi: 10.1038/35013070. [DOI] [PubMed] [Google Scholar]
- 31.Bost KL, Smith EM, Wear LB, Blalock JE. Presence of ACTH and its receptor on a B lymphocytic cell line: a possible autocrine function for a neuroendocrine hormone. J Biol Regul Homeost Agents 1: 23–27, 1987. [PubMed] [Google Scholar]
- 32.Brachman RA, Lehmann ML, Maric D, Herkenham M. Lymphocytes from chronically stressed mice confer antidepressant-like effects to naive mice. J Neurosci 35: 1530–1538, 2015. doi: 10.1523/JNEUROSCI.2278-14.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bratton BO, Martelli D, McKinley MJ, Trevaks D, Anderson CR, McAllen RM. Neural regulation of inflammation: no neural connection from the vagus to splenic sympathetic neurons. Exp Physiol 97: 1180–1185, 2012. doi: 10.1113/expphysiol.2011.061531. [DOI] [PubMed] [Google Scholar]
- 34.Brydon L, Edwards S, Mohamed-Ali V, Steptoe A. Socioeconomic status and stress-induced increases in interleukin-6. Brain Behav Immun 18: 281–290, 2004. doi: 10.1016/j.bbi.2003.09.011. [DOI] [PubMed] [Google Scholar]
- 35.Brydon L, Harrison NA, Walker C, Steptoe A, Critchley HD. Peripheral inflammation is associated with altered substantia nigra activity and psychomotor slowing in humans. Biol Psychiatry 63: 1022–1029, 2008. doi: 10.1016/j.biopsych.2007.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bulloch K, Damavandy T, Badamchian M. Characterization of choline O-acetyltransferase (ChAT) in the BALB/C mouse spleen. Int J Neurosci 76: 141–149, 1994. doi: 10.3109/00207459408985999. [DOI] [PubMed] [Google Scholar]
- 37.Bulloch K, Moore RY. Innervation of the thymus gland by brain stem and spinal cord in mouse and rat. Am J Anat 162: 157–166, 1981. doi: 10.1002/aja.1001620207. [DOI] [PubMed] [Google Scholar]
- 38.Cabot PJ, Carter L, Gaiddon C, Zhang Q, Schäfer M, Loeffler JP, Stein C. Immune cell-derived beta-endorphin. Production, release, and control of inflammatory pain in rats. J Clin Invest 100: 142–148, 1997. doi: 10.1172/JCI119506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Calandra T, Bernhagen J, Metz CN, Spiegel LA, Bacher M, Donnelly T, Cerami A, Bucala R. MIF as a glucocorticoid-induced modulator of cytokine production. Nature 377: 68–71, 1995. doi: 10.1038/377068a0. [DOI] [PubMed] [Google Scholar]
- 40.Capuron L, Miller AH. Cytokines and psychopathology: lessons from interferon-alpha. Biol Psychiatry 56: 819–824, 2004. doi: 10.1016/j.biopsych.2004.02.009. [DOI] [PubMed] [Google Scholar]
- 41.Capuron L, Neurauter G, Musselman DL, Lawson DH, Nemeroff CB, Fuchs D, Miller AH. Interferon-alpha-induced changes in tryptophan metabolism. Relationship to depression and paroxetine treatment. Biol Psychiatry 54: 906–914, 2003. doi: 10.1016/S0006-3223(03)00173-2. [DOI] [PubMed] [Google Scholar]
- 42.Capuron L, Ravaud A, Neveu PJ, Miller AH, Maes M, Dantzer R. Association between decreased serum tryptophan concentrations and depressive symptoms in cancer patients undergoing cytokine therapy. Mol Psychiatry 7: 468–473, 2002. doi: 10.1038/sj.mp.4000995. [DOI] [PubMed] [Google Scholar]
- 43.Cardon SB, Larson DF, Russell DH. Rapid elevation of rat serum prolactin concentration by cyclosporine, a novel immunosuppressive drug. Biochem Biophys Res Commun 120: 614–618, 1984. doi: 10.1016/0006-291X(84)91299-3. [DOI] [PubMed] [Google Scholar]
- 44.Carpenter LL, Gawuga CE, Tyrka AR, Lee JK, Anderson GM, Price LH. Association between plasma IL-6 response to acute stress and early-life adversity in healthy adults. Neuropsychopharmacology 35: 2617–2623, 2010. doi: 10.1038/npp.2010.159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cima I, Corazza N, Dick B, Fuhrer A, Herren S, Jakob S, Ayuni E, Mueller C, Brunner T. Intestinal epithelial cells synthesize glucocorticoids and regulate T cell activation. J Exp Med 200: 1635–1646, 2004. doi: 10.1084/jem.20031958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Clarke BL, Bost KL. Differential expression of functional adrenocorticotropic hormone receptors by subpopulations of lymphocytes. J Immunol 143: 464–469, 1989. [PubMed] [Google Scholar]
- 47.Cole SW, Nagaraja AS, Lutgendorf SK, Green PA, Sood AK. Sympathetic nervous system regulation of the tumour microenvironment. Nat Rev Cancer 15: 563–572, 2015. doi: 10.1038/nrc3978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Coste A, Dubuquoy L, Barnouin R, Annicotte JS, Magnier B, Notti M, Corazza N, Antal MC, Metzger D, Desreumaux P, Brunner T, Auwerx J, Schoonjans K. LRH-1-mediated glucocorticoid synthesis in enterocytes protects against inflammatory bowel disease. Proc Natl Acad Sci USA 104: 13098–13103, 2007. doi: 10.1073/pnas.0702440104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cunningham C, Sanderson DJ. Malaise in the water maze: untangling the effects of LPS and IL-1beta on learning and memory. Brain Behav Immun 22: 1117–1127, 2008. doi: 10.1016/j.bbi.2008.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Czerniawski J, Miyashita T, Lewandowski G, Guzowski JF. Systemic lipopolysaccharide administration impairs retrieval of context-object discrimination, but not spatial, memory: Evidence for selective disruption of specific hippocampus-dependent memory functions during acute neuroinflammation. Brain Behav Immun 44: 159–166, 2015. doi: 10.1016/j.bbi.2014.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Dantzer R. Cytokine-induced sickness behavior: mechanisms and implications. Ann N Y Acad Sci 933: 222–234, 2001. doi: 10.1111/j.1749-6632.2001.tb05827.x. [DOI] [PubMed] [Google Scholar]
- 52.Dantzer R, Konsman JP, Bluthe RM, Kelley KW. Neural and humoral pathways of communication from the immune system to the brain: parallel or convergent? Auton Neurosci 85: 60–65, 2000. doi: 10.1016/S1566-0702(00)00220-4. [DOI] [PubMed] [Google Scholar]
- 53.Dantzer R, O’Connor JC, Freund GG, Johnson RW, Kelley KW. From inflammation to sickness and depression: when the immune system subjugates the brain. Nat Rev Neurosci 9: 46–56, 2008. doi: 10.1038/nrn2297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Del Rey A, Besedovsky H, Sorkin E. Endogenous blood levels of corticosterone control the immunologic cell mass and B cell activity in mice. J Immunol 133: 572–575, 1984. [PubMed] [Google Scholar]
- 55.Demir IE, Friess H, Ceyhan GO. Neural plasticity in pancreatitis and pancreatic cancer. Nat Rev Gastroenterol Hepatol 12: 649–659, 2015. doi: 10.1038/nrgastro.2015.166. [DOI] [PubMed] [Google Scholar]
- 56.Denef C. Paracrinicity: the story of 30 years of cellular pituitary crosstalk. J Neuroendocrinol 20: 1–70, 2008. doi: 10.1111/j.1365-2826.2007.01616.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Desai BN, Leitinger N. Purinergic and calcium signaling in macrophage function and plasticity. Front Immunol 5: 580, 2014. doi: 10.3389/fimmu.2014.00580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Devnath S, Inoue K. An insight to pituitary folliculo-stellate cells. J Neuroendocrinol 20: 687–691, 2008. doi: 10.1111/j.1365-2826.2008.01716.x. [DOI] [PubMed] [Google Scholar]
- 59.Dinarello CA. Cytokines as endogenous pyrogens. J Infect Dis 179, Suppl 2: S294–S304, 1999. doi: 10.1086/513856. [DOI] [PubMed] [Google Scholar]
- 60.Dinarello CA. Interleukin-1 and the pathogenesis of the acute-phase response. N Engl J Med 311: 1413–1418, 1984. doi: 10.1056/NEJM198411293112205. [DOI] [PubMed] [Google Scholar]
- 61.Dorshkind K, Horseman ND. The roles of prolactin, growth hormone, insulin-like growth factor-I, and thyroid hormones in lymphocyte development and function: insights from genetic models of hormone and hormone receptor deficiency. Endocr Rev 21: 292–312, 2000. [DOI] [PubMed] [Google Scholar]
- 62.Dwarkasing JT, Marks DL, Witkamp RF, van Norren K. Hypothalamic inflammation and food intake regulation during chronic illness. Peptides 77: 60–66, 2016. doi: 10.1016/j.peptides.2015.06.011. [DOI] [PubMed] [Google Scholar]
- 63.Eisenberger NI, Inagaki TK, Rameson LT, Mashal NM, Irwin MR. An fMRI study of cytokine-induced depressed mood and social pain: the role of sex differences. Neuroimage 47: 881–890, 2009. doi: 10.1016/j.neuroimage.2009.04.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Elander L, Engström L, Ruud J, Mackerlova L, Jakobsson PJ, Engblom D, Nilsberth C, Blomqvist A. Inducible prostaglandin E2 synthesis interacts in a temporally supplementary sequence with constitutive prostaglandin-synthesizing enzymes in creating the hypothalamic-pituitary-adrenal axis response to immune challenge. J Neurosci 29: 1404–1413, 2009. doi: 10.1523/JNEUROSCI.5247-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Epelman S, Lavine KJ, Randolph GJ. Origin and functions of tissue macrophages. Immunity 41: 21–35, 2014. doi: 10.1016/j.immuni.2014.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ericsson A, Arias C, Sawchenko PE. Evidence for an intramedullary prostaglandin-dependent mechanism in the activation of stress-related neuroendocrine circuitry by intravenous interleukin-1. J Neurosci 17: 7166–7179, 1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ericsson A, Kovács KJ, Sawchenko PE. A functional anatomical analysis of central pathways subserving the effects of interleukin-1 on stress-related neuroendocrine neurons. J Neurosci 14: 897–913, 1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Eriksson F, Kavelaars A, Heijnen C. Preproenkephalin: an unappreciated neuroimmune communicator. In: Psychoneuroimmunology (3rd ed.), edited by Ader R, Felten D, Chohen N. San Diego, CA: Academic, 2001, p. 391–403. [Google Scholar]
- 69.Ernsberger U, Rohrer H. Development of the cholinergic neurotransmitter phenotype in postganglionic sympathetic neurons. Cell Tissue Res 297: 339–361, 1999. doi: 10.1007/s004410051363. [DOI] [PubMed] [Google Scholar]
- 70.Evans SS, Repasky EA, Fisher DT. Fever and the thermal regulation of immunity: the immune system feels the heat. Nat Rev Immunol 15: 335–349, 2015. doi: 10.1038/nri3843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Felten DL, Felten SY, Carlson SL, Olschowka JA, Livnat S. Noradrenergic and peptidergic innervation of lymphoid tissue. J Immunol 135, Suppl: 755s–765s, 1985. [PubMed] [Google Scholar]
- 72.Ferrandon D, Imler JL, Hoffmann JA. Sensing infection in Drosophila: Toll and beyond. Semin Immunol 16: 43–53, 2004. doi: 10.1016/j.smim.2003.10.008. [DOI] [PubMed] [Google Scholar]
- 73.Flierl MA, Rittirsch D, Nadeau BA, Chen AJ, Sarma JV, Zetoune FS, McGuire SR, List RP, Day DE, Hoesel LM, Gao H, Van Rooijen N, Huber-Lang MS, Neubig RR, Ward PA. Phagocyte-derived catecholamines enhance acute inflammatory injury. Nature 449: 721–725, 2007. doi: 10.1038/nature06185. [DOI] [PubMed] [Google Scholar]
- 74.Flierl MA, Rittirsch D, Nadeau BA, Sarma JV, Day DE, Lentsch AB, Huber-Lang MS, Ward PA. Upregulation of phagocyte-derived catecholamines augments the acute inflammatory response. PLoS One 4: e4414, 2009. doi: 10.1371/journal.pone.0004414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Frank MG, Baratta MV, Sprunger DB, Watkins LR, Maier SF. Microglia serve as a neuroimmune substrate for stress-induced potentiation of CNS pro-inflammatory cytokine responses. Brain Behav Immun 21: 47–59, 2007. doi: 10.1016/j.bbi.2006.03.005. [DOI] [PubMed] [Google Scholar]
- 76.Frank MG, Watkins LR, Maier SF. Stress-induced glucocorticoids as a neuroendocrine alarm signal of danger. Brain Behav Immun 33: 1–6, 2013. doi: 10.1016/j.bbi.2013.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Frank MG, Weber MD, Watkins LR, Maier SF. Stress sounds the alarmin: the role of the danger-associated molecular pattern HMGB1 in stress-induced neuroinflammatory priming. Brain Behav Immun 48: 1–7, 2015. doi: 10.1016/j.bbi.2015.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Fritz M, Klawonn AM, Nilsson A, Singh AK, Zajdel J, Wilhelms DB, Lazarus M, Löfberg A, Jaarola M, Kugelberg UÖ, Billiar TR, Hackam DJ, Sodhi CP, Breyer MD, Jakobsson J, Schwaninger M, Schütz G, Parkitna JR, Saper CB, Blomqvist A, Engblom D. Prostaglandin-dependent modulation of dopaminergic neurotransmission elicits inflammation-induced aversion in mice. J Clin Invest 126: 695–705, 2016. doi: 10.1172/JCI83844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Fujii T, Takada-Takatori Y, Kawashima K. Basic and clinical aspects of non-neuronal acetylcholine: expression of an independent, non-neuronal cholinergic system in lymphocytes and its clinical significance in immunotherapy. J Pharmacol Sci 106: 186–192, 2008. doi: 10.1254/jphs.FM0070109. [DOI] [PubMed] [Google Scholar]
- 80.García-Bueno B, Serrats J, Sawchenko PE. Cerebrovascular cyclooxygenase-1 expression, regulation, and role in hypothalamic-pituitary-adrenal axis activation by inflammatory stimuli. J Neurosci 29: 12970–12981, 2009. doi: 10.1523/JNEUROSCI.2373-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Gautron L, Rutkowski JM, Burton MD, Wei W, Wan Y, Elmquist JK. Neuronal and nonneuronal cholinergic structures in the mouse gastrointestinal tract and spleen. J Comp Neurol 521: 3741–3767, 2013. doi: 10.1002/cne.23376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Gaykema RP, Goehler LE. Lipopolysaccharide challenge-induced suppression of Fos in hypothalamic orexin neurons: their potential role in sickness behavior. Brain Behav Immun 23: 926–930, 2009. doi: 10.1016/j.bbi.2009.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Gery I, Gershon RK, Waksman BH. Potentiation of the T-lymphocyte response to mitogens. I. The responding cell. J Exp Med 136: 128–142, 1972. doi: 10.1084/jem.136.1.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Gery I, Waksman BH. Potentiation of the T-lymphocyte response to mitogens. II. The cellular source of potentiating mediator(s). J Exp Med 136: 143–155, 1972. doi: 10.1084/jem.136.1.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Ginhoux F, Greter M, Leboeuf M, Nandi S, See P, Gokhan S, Mehler MF, Conway SJ, Ng LG, Stanley ER, Samokhvalov IM, Merad M. Fate mapping analysis reveals that adult microglia derive from primitive macrophages. Science 330: 841–845, 2010. doi: 10.1126/science.1194637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Ginhoux F, Prinz M. Origin of microglia: current concepts and past controversies. Cold Spring Harb Perspect Biol 7: a020537, 2015. doi: 10.1101/cshperspect.a020537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Gisslinger H, Svoboda T, Clodi M, Gilly B, Ludwig H, Havelec L, Luger A. Interferon-alpha stimulates the hypothalamic-pituitary-adrenal axis in vivo and in vitro. Neuroendocrinology 57: 489–495, 1993. doi: 10.1159/000126396. [DOI] [PubMed] [Google Scholar]
- 88.Golden SA, Covington HE III, Berton O, Russo SJ. A standardized protocol for repeated social defeat stress in mice. Nat Protoc 6: 1183–1191, 2011. doi: 10.1038/nprot.2011.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Gras G, Samah B, Hubert A, Léone C, Porcheray F, Rimaniol AC. EAAT expression by macrophages and microglia: still more questions than answers. Amino Acids 42: 221–229, 2012. doi: 10.1007/s00726-011-0866-6. [DOI] [PubMed] [Google Scholar]
- 90.Greter M, Lelios I, Pelczar P, Hoeffel G, Price J, Leboeuf M, Kündig TM, Frei K, Ginhoux F, Merad M, Becher B. Stroma-derived interleukin-34 controls the development and maintenance of langerhans cells and the maintenance of microglia. Immunity 37: 1050–1060, 2012. doi: 10.1016/j.immuni.2012.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Grossberg AJ, Zhu X, Leinninger GM, Levasseur PR, Braun TP, Myers MG Jr, Marks DL. Inflammation-induced lethargy is mediated by suppression of orexin neuron activity. J Neurosci 31: 11376–11386, 2011. doi: 10.1523/JNEUROSCI.2311-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Gruber J, Sgonc R, Hu YH, Beug H, Wick G. Thymocyte apoptosis induced by elevated endogenous corticosterone levels. Eur J Immunol 24: 1115–1121, 1994. doi: 10.1002/eji.1830240516. [DOI] [PubMed] [Google Scholar]
- 93.Guillemin R. Peptides in the brain: the new endocrinology of the neuron. Science 202: 390–402, 1978. doi: 10.1126/science.212832. [DOI] [PubMed] [Google Scholar]
- 94.Haapakoski R, Mathieu J, Ebmeier KP, Alenius H, Kivimäki M. Cumulative meta-analysis of interleukins 6 and 1β, tumour necrosis factor α and C-reactive protein in patients with major depressive disorder. Brain Behav Immun 49: 206–215, 2015. doi: 10.1016/j.bbi.2015.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Hadden JW, Hadden EM, Middleton E Jr. Lymphocyte blast transformation. I. Demonstration of adrenergic receptors in human peripheral lymphocytes. Cell Immunol 1: 583–595, 1970. doi: 10.1016/0008-8749(70)90024-9. [DOI] [PubMed] [Google Scholar]
- 96.Hannestad J, Gallezot JD, Schafbauer T, Lim K, Kloczynski T, Morris ED, Carson RE, Ding YS, Cosgrove KP. Endotoxin-induced systemic inflammation activates microglia: [11C]PBR28 positron emission tomography in nonhuman primates. Neuroimage 63: 232–239, 2012. doi: 10.1016/j.neuroimage.2012.06.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Harrison NA, Brydon L, Walker C, Gray MA, Steptoe A, Critchley HD. Inflammation causes mood changes through alterations in subgenual cingulate activity and mesolimbic connectivity. Biol Psychiatry 66: 407–414, 2009. doi: 10.1016/j.biopsych.2009.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Harrison NA, Brydon L, Walker C, Gray MA, Steptoe A, Dolan RJ, Critchley HD. Neural origins of human sickness in interoceptive responses to inflammation. Biol Psychiatry 66: 415–422, 2009. doi: 10.1016/j.biopsych.2009.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Hart BL. Behavioural defences in animals against pathogens and parasites: parallels with the pillars of medicine in humans. Philos Trans R Soc Lond B Biol Sci 366: 3406–3417, 2011. doi: 10.1098/rstb.2011.0092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Hart BL. Biological basis of the behavior of sick animals. Neurosci Biobehav Rev 12: 123–137, 1988. doi: 10.1016/S0149-7634(88)80004-6. [DOI] [PubMed] [Google Scholar]
- 101.Hench PS, Slocumb CH, Polley HF, Kendal EC. Effect of cortisone and pituitary adrenocorticotropic hormone (ACTH) on rheumatic diseases. J Am Med Assoc 144: 1327–1335, 1950. doi: 10.1001/jama.1950.02920160001001. [DOI] [PubMed] [Google Scholar]
- 102.Herbert TB, Cohen S. Depression and immunity: a meta-analytic review. Psychol Bull 113: 472–486, 1993. doi: 10.1037/0033-2909.113.3.472. [DOI] [PubMed] [Google Scholar]
- 103.Hiestand PC, Mekler P, Nordmann R, Grieder A, Permmongkol C. Prolactin as a modulator of lymphocyte responsiveness provides a possible mechanism of action for cyclosporine. Proc Natl Acad Sci USA 83: 2599–2603, 1986. doi: 10.1073/pnas.83.8.2599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Hiles SA, Baker AL, de Malmanche T, Attia J. A meta-analysis of differences in IL-6 and IL-10 between people with and without depression: exploring the causes of heterogeneity. Brain Behav Immun 26: 1180–1188, 2012. doi: 10.1016/j.bbi.2012.06.001. [DOI] [PubMed] [Google Scholar]
- 105.Hodes GE, Pfau ML, Leboeuf M, Golden SA, Christoffel DJ, Bregman D, Rebusi N, Heshmati M, Aleyasin H, Warren BL, Lebonté B, Horn S, Lapidus KA, Stelzhammer V, Wong EH, Bahn S, Krishnan V, Bolaños-Guzman CA, Murrough JW, Merad M, Russo SJ. Individual differences in the peripheral immune system promote resilience versus susceptibility to social stress. Proc Natl Acad Sci USA 111: 16136–16141, 2014. doi: 10.1073/pnas.1415191111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Howren MB, Lamkin DM, Suls J. Associations of depression with C-reactive protein, IL-1, and IL-6: a meta-analysis. Psychosom Med 71: 171–186, 2009. doi: 10.1097/PSY.0b013e3181907c1b. [DOI] [PubMed] [Google Scholar]
- 107.Huston JM, Ochani M, Rosas-Ballina M, Liao H, Ochani K, Pavlov VA, Gallowitsch-Puerta M, Ashok M, Czura CJ, Foxwell B, Tracey KJ, Ulloa L. Splenectomy inactivates the cholinergic antiinflammatory pathway during lethal endotoxemia and polymicrobial sepsis. J Exp Med 203: 1623–1628, 2006. doi: 10.1084/jem.20052362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Ignatowski TA, Gallant S, Spengler RN. Temporal regulation by adrenergic receptor stimulation of macrophage (M phi)-derived tumor necrosis factor (TNF) production post-LPS challenge. J Neuroimmunol 65: 107–117, 1996. doi: 10.1016/0165-5728(96)00004-5. [DOI] [PubMed] [Google Scholar]
- 109.Inbar S, Neeman E, Avraham R, Benish M, Rosenne E, Ben-Eliyahu S. Do stress responses promote leukemia progression? An animal study suggesting a role for epinephrine and prostaglandin-E2 through reduced NK activity. PLoS One 6: e19246, 2011. doi: 10.1371/journal.pone.0019246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Izeboud CA, Mocking JA, Monshouwer M, van Miert AS, Witkamp RF. Participation of beta-adrenergic receptors on macrophages in modulation of LPS-induced cytokine release. J Recept Signal Transduct Res 19: 191–202, 1999. doi: 10.3109/10799899909036645. [DOI] [PubMed] [Google Scholar]
- 111.Jobling P, Pundavela J, Oliveira SM, Roselli S, Walker MM, Hondermarck H. Nerve-Cancer Cell Cross-talk: A Novel Promoter of Tumor Progression. Cancer Res 75: 1777–1781, 2015. doi: 10.1158/0008-5472.CAN-14-3180. [DOI] [PubMed] [Google Scholar]
- 112.Johnson JD, O’Connor KA, Deak T, Stark M, Watkins LR, Maier SF. Prior stressor exposure sensitizes LPS-induced cytokine production. Brain Behav Immun 16: 461–476, 2002. doi: 10.1006/brbi.2001.0638. [DOI] [PubMed] [Google Scholar]
- 113.Kanczkowski W, Alexaki VI, Tran N, Großklaus S, Zacharowski K, Martinez A, Popovics P, Block NL, Chavakis T, Schally AV, Bornstein SR. Hypothalamo-pituitary and immune-dependent adrenal regulation during systemic inflammation. Proc Natl Acad Sci USA 110: 14801–14806, 2013. doi: 10.1073/pnas.1313945110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Karanth S, McCann SM. Anterior pituitary hormone control by interleukin 2. Proc Natl Acad Sci USA 88: 2961–2965, 1991. doi: 10.1073/pnas.88.7.2961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Kawashima K, Fujii T, Moriwaki Y, Misawa H, Horiguchi K. Reconciling neuronally and nonneuronally derived acetylcholine in the regulation of immune function. Ann N Y Acad Sci 1261: 7–17, 2012. doi: 10.1111/j.1749-6632.2012.06516.x. [DOI] [PubMed] [Google Scholar]
- 116.Kelley KW, Arkins S, Li YM. Growth hormone, prolactin, and insulin-like growth factors: new jobs for old players. Brain Behav Immun 6: 317–326, 1992. doi: 10.1016/0889-1591(92)90031-I. [DOI] [PubMed] [Google Scholar]
- 117.Kelley KW, Weigent DA, Kooijman R. Protein hormones and immunity. Brain Behav Immun 21: 384–392, 2007. doi: 10.1016/j.bbi.2006.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Kent S, Bluthe RM, Dantzer R, Hardwick AJ, Kelley KW, Rothwell NJ, Vannice JL. Different receptor mechanisms mediate the pyrogenic and behavioral effects of interleukin 1. Proc Natl Acad Sci USA 89: 9117–9120, 1992. doi: 10.1073/pnas.89.19.9117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Kent S, Bluthé RM, Kelley KW, Dantzer R. Sickness behavior as a new target for drug development. Trends Pharmacol Sci 13: 24–28, 1992. doi: 10.1016/0165-6147(92)90012-U. [DOI] [PubMed] [Google Scholar]
- 120.Khandaker GM, Pearson RM, Zammit S, Lewis G, Jones PB. Association of serum interleukin 6 and C-reactive protein in childhood with depression and psychosis in young adult life: a population-based longitudinal study. JAMA Psychiatry 71: 1121–1128, 2014. doi: 10.1001/jamapsychiatry.2014.1332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Kita T, Morrison PF, Heyes MP, Markey SP. Effects of systemic and central nervous system localized inflammation on the contributions of metabolic precursors to the l-kynurenine and quinolinic acid pools in brain. J Neurochem 82: 258–268, 2002. doi: 10.1046/j.1471-4159.2002.00955.x. [DOI] [PubMed] [Google Scholar]
- 122.Kivimäki M, Shipley MJ, Batty GD, Hamer M, Akbaraly TN, Kumari M, Jokela M, Virtanen M, Lowe GD, Ebmeier KP, Brunner EJ, Singh-Manoux A. Long-term inflammation increases risk of common mental disorder: a cohort study. Mol Psychiatry 19: 149–150, 2014. doi: 10.1038/mp.2013.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Kleiman A, Hübner S, Rodriguez Parkitna JM, Neumann A, Hofer S, Weigand MA, Bauer M, Schmid W, Schütz G, Libert C, Reichardt HM, Tuckermann JP. Glucocorticoid receptor dimerization is required for survival in septic shock via suppression of interleukin-1 in macrophages. FASEB J 26: 722–729, 2012. doi: 10.1096/fj.11-192112. [DOI] [PubMed] [Google Scholar]
- 124.Kolmus K, Tavernier J, Gerlo S. β2-Adrenergic receptors in immunity and inflammation: stressing NF-κB. Brain Behav Immun 45: 297–310, 2015. doi: 10.1016/j.bbi.2014.10.007. [DOI] [PubMed] [Google Scholar]
- 125.Konsman J. Immune-to-brain signaling and substrates of altered behavior during inflammation. Neuroimmunol Neuroinflamm 3: 207–214, 2016. doi: 10.20517/2347-8659.2016.19. [DOI] [Google Scholar]
- 126.Konsman JP, Parnet P, Dantzer R. Cytokine-induced sickness behaviour: mechanisms and implications. Trends Neurosci 25: 154–159, 2002. doi: 10.1016/S0166-2236(00)02088-9. [DOI] [PubMed] [Google Scholar]
- 127.Konsman JP, Veeneman J, Combe C, Poole S, Luheshi GN, Dantzer R. Central nervous action of interleukin-1 mediates activation of limbic structures and behavioural depression in response to peripheral administration of bacterial lipopolysaccharide. Eur J Neurosci 28: 2499–2510, 2008. doi: 10.1111/j.1460-9568.2008.06549.x. [DOI] [PubMed] [Google Scholar]
- 128.Konsman JP, Vigues S, Mackerlova L, Bristow A, Blomqvist A. Rat brain vascular distribution of interleukin-1 type-1 receptor immunoreactivity: relationship to patterns of inducible cyclooxygenase expression by peripheral inflammatory stimuli. J Comp Neurol 472: 113–129, 2004. doi: 10.1002/cne.20052. [DOI] [PubMed] [Google Scholar]
- 129.Krukowski K, Eijkelkamp N, Laumet G, Hack CE, Li Y, Dougherty PM, Heijnen CJ, Kavelaars A. CD8+ T Cells and Endogenous IL-10 Are Required for Resolution of Chemotherapy-Induced Neuropathic Pain. J Neurosci 36: 11074–11083, 2016. doi: 10.1523/JNEUROSCI.3708-15.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Kullmann JS, Grigoleit JS, Lichte P, Kobbe P, Rosenberger C, Banner C, Wolf OT, Engler H, Oberbeck R, Elsenbruch S, Bingel U, Forsting M, Gizewski ER, Schedlowski M. Neural response to emotional stimuli during experimental human endotoxemia. Hum Brain Mapp 34: 2217–2227, 2013. doi: 10.1002/hbm.22063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Larson SJ, Romanoff RL, Dunn AJ, Glowa JR. Effects of interleukin-1beta on food-maintained behavior in the mouse. Brain Behav Immun 16: 398–410, 2002. doi: 10.1006/brbi.2001.0634. [DOI] [PubMed] [Google Scholar]
- 132.Le CP, Nowell CJ, Kim-Fuchs C, Botteri E, Hiller JG, Ismail H, Pimentel MA, Chai MG, Karnezis T, Rotmensz N, Renne G, Gandini S, Pouton CW, Ferrari D, Möller A, Stacker SA, Sloan EK. Chronic stress in mice remodels lymph vasculature to promote tumour cell dissemination. Nat Commun 7: 10634, 2016. doi: 10.1038/ncomms10634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Lenczowski MJ, Bluthé RM, Roth J, Rees GS, Rushforth DA, van Dam AM, Tilders FJ, Dantzer R, Rothwell NJ, Luheshi GN. Central administration of rat IL-6 induces HPA activation and fever but not sickness behavior in rats. Am J Physiol Regul Integr Comp Physiol 276: R652–R658, 1999. [DOI] [PubMed] [Google Scholar]
- 134.Levite M. NeuroImmunoTransmitters: neurotransmitters that induce numerous direct and powerful effects on immune cells, via their receptors. Psychoneuroendocrinology. In press. [Google Scholar]
- 135.Lewitus GM, Pribiag H, Duseja R, St-Hilaire M, Stellwagen D. An adaptive role of TNFα in the regulation of striatal synapses. J Neurosci 34: 6146–6155, 2014. doi: 10.1523/JNEUROSCI.3481-13.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Lewitus GM, Schwartz M. Behavioral immunization: immunity to self-antigens contributes to psychological stress resilience. Mol Psychiatry 14: 532–536, 2009. doi: 10.1038/mp.2008.103. [DOI] [PubMed] [Google Scholar]
- 137.Libert C. Inflammation: a nervous connection. Nature 421: 328–329, 2003. doi: 10.1038/421328a. [DOI] [PubMed] [Google Scholar]
- 138.Limatola C, Ransohoff RM. Modulating neurotoxicity through CX3CL1/CX3CR1 signaling. Front Cell Neurosci 8: 229, 2014. doi: 10.3389/fncel.2014.00229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Lipowski ZJ. Psychosomatic medicine: past and present. Part I. Historical background. Can J Psychiatry 31: 2–7, 1986. doi: 10.1177/070674378603100102. [DOI] [PubMed] [Google Scholar]
- 140.Lomedico PT, Gubler U, Hellmann CP, Dukovich M, Giri JG, Pan YC, Collier K, Semionow R, Chua AO, Mizel SB. Cloning and expression of murine interleukin-1 cDNA in Escherichia coli. Nature 312: 458–462, 1984. doi: 10.1038/312458a0. [DOI] [PubMed] [Google Scholar]
- 141.Luheshi GN, Bluthe RM, Rushforth D, Mulcahy N, Konsman JP, Goldbach M, Dantzer R. Vagotomy attenuates the behavioural but not the pyrogenic effects of interleukin-1 in rats. Auton Neurosci 85: 127–132, 2000. doi: 10.1016/S1566-0702(00)00231-9. [DOI] [PubMed] [Google Scholar]
- 142.Madden KS, Felten DL. Experimental basis for neural-immune interactions. Physiol Rev 75: 77–106, 1995. [DOI] [PubMed] [Google Scholar]
- 143.Madden KS, Felten SY, Felten DL, Sundaresan PR, Livnat S. Sympathetic neural modulation of the immune system. I. Depression of T cell immunity in vivo and vitro following chemical sympathectomy. Brain Behav Immun 3: 72–89, 1989. doi: 10.1016/0889-1591(89)90007-X. [DOI] [PubMed] [Google Scholar]
- 144.Maes M, Kubera M, Leunis JC. The gut-brain barrier in major depression: intestinal mucosal dysfunction with an increased translocation of LPS from gram negative enterobacteria (leaky gut) plays a role in the inflammatory pathophysiology of depression. Neuro Endocrinol Lett 29: 117–124, 2008. [PubMed] [Google Scholar]
- 145.Maes M, Smith R, Scharpe S. The monocyte-T-lymphocyte hypothesis of major depression. Psychoneuroendocrinology 20: 111–116, 1995. doi: 10.1016/0306-4530(94)00066-J. [DOI] [PubMed] [Google Scholar]
- 146.Magnon C, Hall SJ, Lin J, Xue X, Gerber L, Freedland SJ, Frenette PS. Autonomic nerve development contributes to prostate cancer progression. Science 341: 1236361, 2013. doi: 10.1126/science.1236361. [DOI] [PubMed] [Google Scholar]
- 147.Marino F, Cosentino M. Adrenergic modulation of immune cells: an update. Amino Acids 45: 55–71, 2013. doi: 10.1007/s00726-011-1186-6. [DOI] [PubMed] [Google Scholar]
- 148.Martelli D, McKinley MJ, McAllen RM. The cholinergic anti-inflammatory pathway: a critical review. Auton Neurosci 182: 65–69, 2014. doi: 10.1016/j.autneu.2013.12.007. [DOI] [PubMed] [Google Scholar]
- 149.Marvel FA, Chen CC, Badr N, Gaykema RP, Goehler LE. Reversible inactivation of the dorsal vagal complex blocks lipopolysaccharide-induced social withdrawal and c-Fos expression in central autonomic nuclei. Brain Behav Immun 18: 123–134, 2004. doi: 10.1016/j.bbi.2003.09.004. [DOI] [PubMed] [Google Scholar]
- 150.Matsuoka Y, Furuyashiki T, Bito H, Ushikubi F, Tanaka Y, Kobayashi T, Muro S, Satoh N, Kayahara T, Higashi M, Mizoguchi A, Shichi H, Fukuda Y, Nakao K, Narumiya S. Impaired adrenocorticotropic hormone response to bacterial endotoxin in mice deficient in prostaglandin E receptor EP1 and EP3 subtypes. Proc Natl Acad Sci USA 100: 4132–4137, 2003. doi: 10.1073/pnas.0633341100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Matsuwaki T, Eskilsson A, Kugelberg U, Jönsson JI, Blomqvist A. Interleukin-1β induced activation of the hypothalamus-pituitary-adrenal axis is dependent on interleukin-1 receptors on non-hematopoietic cells. Brain Behav Immun 40: 166–173, 2014. doi: 10.1016/j.bbi.2014.03.015. [DOI] [PubMed] [Google Scholar]
- 152.Mays JW, Bailey MT, Hunzeker JT, Powell ND, Papenfuss T, Karlsson EA, Padgett DA, Sheridan JF. Influenza virus-specific immunological memory is enhanced by repeated social defeat. J Immunol 184: 2014–2025, 2010. doi: 10.4049/jimmunol.0900183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Mays JW, Powell ND, Hunzeker JT, Hanke ML, Bailey MT, Sheridan JF. Stress and the anti-influenza immune response: repeated social defeat augments clonal expansion of CD8(+)T cells during primary influenza A viral infection. J Neuroimmunol 243: 34–42, 2012. doi: 10.1016/j.jneuroim.2011.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Melmed S. gp130-Related cytokines and their receptors in the pituitary. Trends Endocrinol Metab 8: 391–397, 1997. doi: 10.1016/S1043-2760(97)00156-2. [DOI] [PubMed] [Google Scholar]
- 155.Méndez-Ferrer S, Lucas D, Battista M, Frenette PS. Haematopoietic stem cell release is regulated by circadian oscillations. Nature 452: 442–447, 2008. doi: 10.1038/nature06685. [DOI] [PubMed] [Google Scholar]
- 156.Merali Z, Brennan K, Brau P, Anisman H. Dissociating anorexia and anhedonia elicited by interleukin-1beta: antidepressant and gender effects on responding for “free chow” and “earned” sucrose intake. Psychopharmacology (Berl) 165: 413–418, 2003. doi: 10.1007/s00213-002-1273-1. [DOI] [PubMed] [Google Scholar]
- 157.Metalnikov S, Chorine V. Rôle des réflexes conditionnels dans l’immunité. Ann Inst Pasteur (Paris) XL: 1640–1647, 1926. [Google Scholar]
- 158.Miller AH, Pariante CM, Pearce BD. Effects of cytokines on glucocorticoid receptor expression and function. Glucocorticoid resistance and relevance to depression. Adv Exp Med Biol 461: 107–116, 1999. doi: 10.1007/978-0-585-37970-8_7. [DOI] [PubMed] [Google Scholar]
- 159.Miller N. Some psychophysiological studies of the motivation and of the behavioral effects of illness. Bull Br Psychol Soc 17: 1–20, 1964. [Google Scholar]
- 160.Moynihan JA, Ader R. Psychoneuroimmunology: animal models of disease. Psychosom Med 58: 546–558, 1996. doi: 10.1097/00006842-199611000-00003. [DOI] [PubMed] [Google Scholar]
- 161.Munn DH, Mellor AL. Indoleamine 2,3 dioxygenase and metabolic control of immune responses. Trends Immunol 34: 137–143, 2013. doi: 10.1016/j.it.2012.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Nagy E, Berczi I, Friesen HG. Regulation of immunity in rats by lactogenic and growth hormones. Acta Endocrinol (Copenh) 102: 351–357, 1983. [DOI] [PubMed] [Google Scholar]
- 163.Nakai A, Hayano Y, Furuta F, Noda M, Suzuki K. Control of lymphocyte egress from lymph nodes through β2-adrenergic receptors. J Exp Med 211: 2583–2598, 2014. doi: 10.1084/jem.20141132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Nance DM, Sanders VM. Autonomic innervation and regulation of the immune system (1987-2007). Brain Behav Immun 21: 736–745, 2007. doi: 10.1016/j.bbi.2007.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Nestler EJ, Barrot M, DiLeone RJ, Eisch AJ, Gold SJ, Monteggia LM. Neurobiology of depression. Neuron 34: 13–25, 2002. doi: 10.1016/S0896-6273(02)00653-0. [DOI] [PubMed] [Google Scholar]
- 166.Nusslock R, Miller GE. Early-Life Adversity and Physical and Emotional Health Across the Lifespan: A Neuroimmune Network Hypothesis. Biol Psychiatry 80: 23–32, 2016. doi: 10.1016/j.biopsych.2015.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.O’Connor JC, Lawson MA, André C, Briley EM, Szegedi SS, Lestage J, Castanon N, Herkenham M, Dantzer R, Kelley KW. Induction of IDO by bacille Calmette-Guérin is responsible for development of murine depressive-like behavior. J Immunol 182: 3202–3212, 2009. doi: 10.4049/jimmunol.0802722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.O’Connor JC, Lawson MA, André C, Moreau M, Lestage J, Castanon N, Kelley KW, Dantzer R. Lipopolysaccharide-induced depressive-like behavior is mediated by indoleamine 2,3-dioxygenase activation in mice. Mol Psychiatry 14: 511–522, 2009. doi: 10.1038/sj.mp.4002148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.O’Leary A. Stress, emotion, and human immune function. Psychol Bull 108: 363–382, 1990. doi: 10.1037/0033-2909.108.3.363. [DOI] [PubMed] [Google Scholar]
- 170.O’Neill LA, Golenbock D, Bowie AG. The history of Toll-like receptors: redefining innate immunity. Nat Rev Immunol 13: 453–460, 2013. doi: 10.1038/nri3446. [DOI] [PubMed] [Google Scholar]
- 171.Olofsson PS, Rosas-Ballina M, Levine YA, Tracey KJ. Rethinking inflammation: neural circuits in the regulation of immunity. Immunol Rev 248: 188–204, 2012. doi: 10.1111/j.1600-065X.2012.01138.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Pace TW, Hu F, Miller AH. Cytokine-effects on glucocorticoid receptor function: relevance to glucocorticoid resistance and the pathophysiology and treatment of major depression. Brain Behav Immun 21: 9–19, 2007. doi: 10.1016/j.bbi.2006.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Padro CJ, Sanders VM. Neuroendocrine regulation of inflammation. Semin Immunol 26: 357–368, 2014. doi: 10.1016/j.smim.2014.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Paolicelli RC, Bolasco G, Pagani F, Maggi L, Scianni M, Panzanelli P, Giustetto M, Ferreira TA, Guiducci E, Dumas L, Ragozzino D, Gross CT. Synaptic pruning by microglia is necessary for normal brain development. Science 333: 1456–1458, 2011. doi: 10.1126/science.1202529. [DOI] [PubMed] [Google Scholar]
- 175.Pazirandeh A, Xue Y, Rafter I, Sjövall J, Jondal M, Okret S. Paracrine glucocorticoid activity produced by mouse thymic epithelial cells. FASEB J 13: 893–901, 1999. [DOI] [PubMed] [Google Scholar]
- 176.Pereira Suarez AL, López-Rincón G, Martínez Neri PA, Estrada-Chávez C. Prolactin in inflammatory response. Adv Exp Med Biol 846: 243–264, 2015. doi: 10.1007/978-3-319-12114-7_11. [DOI] [PubMed] [Google Scholar]
- 177.Pert CB, Ruff MR, Weber RJ, Herkenham M. Neuropeptides and their receptors: a psychosomatic network. J Immunol 135, Suppl: 820s–826s, 1985. [PubMed] [Google Scholar]
- 178.Pimentel GD, Ganeshan K, Carvalheira JB. Hypothalamic inflammation and the central nervous system control of energy homeostasis. Mol Cell Endocrinol 397: 15–22, 2014. doi: 10.1016/j.mce.2014.06.005. [DOI] [PubMed] [Google Scholar]
- 179.Pixley FJ, Stanley ER. CSF-1 regulation of the wandering macrophage: complexity in action. Trends Cell Biol 14: 628–638, 2004. doi: 10.1016/j.tcb.2004.09.016. [DOI] [PubMed] [Google Scholar]
- 180.Pugh CR, Kumagawa K, Fleshner M, Watkins LR, Maier SF, Rudy JW. Selective effects of peripheral lipopolysaccharide administration on contextual and auditory-cue fear conditioning. Brain Behav Immun 12: 212–229, 1998. doi: 10.1006/brbi.1998.0524. [DOI] [PubMed] [Google Scholar]
- 181.Qiao S, Chen L, Okret S, Jondal M. Age-related synthesis of glucocorticoids in thymocytes. Exp Cell Res 314: 3027–3035, 2008. doi: 10.1016/j.yexcr.2008.06.014. [DOI] [PubMed] [Google Scholar]
- 182.Qiu YH, Peng YP, Jiang JM, Wang JJ. Expression of tyrosine hydroxylase in lymphocytes and effect of endogenous catecholamines on lymphocyte function. Neuroimmunomodulation 11: 75–83, 2004. doi: 10.1159/000075316. [DOI] [PubMed] [Google Scholar]
- 183.Raison CL, Dantzer R, Kelley KW, Lawson MA, Woolwine BJ, Vogt G, Spivey JR, Saito K, Miller AH. CSF concentrations of brain tryptophan and kynurenines during immune stimulation with IFN-alpha: relationship to CNS immune responses and depression. Mol Psychiatry 15: 393–403, 2010. doi: 10.1038/mp.2009.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Raison CL, Rutherford RE, Woolwine BJ, Shuo C, Schettler P, Drake DF, Haroon E, Miller AH. A randomized controlled trial of the tumor necrosis factor antagonist infliximab for treatment-resistant depression: the role of baseline inflammatory biomarkers. JAMA Psychiatry 70: 31–41, 2013. doi: 10.1001/2013.jamapsychiatry.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Ramer-Quinn DS, Swanson MA, Lee WT, Sanders VM. Cytokine production by naive and primary effector CD4+ T cells exposed to norepinephrine. Brain Behav Immun 14: 239–255, 2000. doi: 10.1006/brbi.2000.0603. [DOI] [PubMed] [Google Scholar]
- 186.Ramesh R, Kozhaya L, McKevitt K, Djuretic IM, Carlson TJ, Quintero MA, McCauley JL, Abreu MT, Unutmaz D, Sundrud MS. Pro-inflammatory human Th17 cells selectively express P-glycoprotein and are refractory to glucocorticoids. J Exp Med 211: 89–104, 2014. doi: 10.1084/jem.20130301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Rogausch H, del Rey A, Kabiersch A, Reschke W, Ortel J, Besedovsky H. Endotoxin impedes vasoconstriction in the spleen: role of endogenous interleukin-1 and sympathetic innervation. Am J Physiol Regul Integr Comp Physiol 272: R2048–R2054, 1997. [DOI] [PubMed] [Google Scholar]
- 188.Rogausch H, Zwingmann D, Trudewind M, del Rey A, Voigt KH, Besedovsky H. Local and systemic autonomic nervous effects on cell migration to the spleen. J Appl Physiol (1985) 94: 469–475, 2003. doi: 10.1152/japplphysiol.00411.2002. [DOI] [PubMed] [Google Scholar]
- 189.Roh J, Muelleman T, Tawfik O, Thomas SM. Perineural growth in head and neck squamous cell carcinoma: a review. Oral Oncol 51: 16–23, 2015. doi: 10.1016/j.oraloncology.2014.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Rohleder N, Aringer M, Boentert M. Role of interleukin-6 in stress, sleep, and fatigue. Ann N Y Acad Sci 1261: 88–96, 2012. doi: 10.1111/j.1749-6632.2012.06634.x. [DOI] [PubMed] [Google Scholar]
- 191.Ronald PC, Beutler B. Plant and animal sensors of conserved microbial signatures. Science 330: 1061–1064, 2010. doi: 10.1126/science.1189468. [DOI] [PubMed] [Google Scholar]
- 192.Rosas-Ballina M, Ochani M, Parrish WR, Ochani K, Harris YT, Huston JM, Chavan S, Tracey KJ. Splenic nerve is required for cholinergic antiinflammatory pathway control of TNF in endotoxemia. Proc Natl Acad Sci USA 105: 11008–11013, 2008. doi: 10.1073/pnas.0803237105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Rosas-Ballina M, Olofsson PS, Ochani M, Valdés-Ferrer SI, Levine YA, Reardon C, Tusche MW, Pavlov VA, Andersson U, Chavan S, Mak TW, Tracey KJ. Acetylcholine-synthesizing T cells relay neural signals in a vagus nerve circuit. Science 334: 98–101, 2011. doi: 10.1126/science.1209985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Roth J, Blatteis CM. Mechanisms of fever production and lysis: lessons from experimental LPS fever. Compr Physiol 4: 1563–1604, 2014. doi: 10.1002/cphy.c130033. [DOI] [PubMed] [Google Scholar]
- 195.Russell DH. New aspects of prolactin and immunity: a lymphocyte-derived prolactin-like product and nuclear protein kinase C activation. Trends Pharmacol Sci 10: 40–44, 1989. doi: 10.1016/0165-6147(89)90106-5. [DOI] [PubMed] [Google Scholar]
- 196.Russell DH, Kibler R, Matrisian L, Larson DF, Poulos B, Magun BE. Prolactin receptors on human T and B lymphocytes: antagonism of prolactin binding by cyclosporine. J Immunol 134: 3027–3031, 1985. [PubMed] [Google Scholar]
- 197.Saloman JL, Albers KM, Li D, Hartman DJ, Crawford HC, Muha EA, Rhim AD, Davis BM. Ablation of sensory neurons in a genetic model of pancreatic ductal adenocarcinoma slows initiation and progression of cancer. Proc Natl Acad Sci USA 113: 3078–3083, 2016. doi: 10.1073/pnas.1512603113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Sandiego CM, Gallezot JD, Pittman B, Nabulsi N, Lim K, Lin SF, Matuskey D, Lee JY, O’Connor KC, Huang Y, Carson RE, Hannestad J, Cosgrove KP. Imaging robust microglial activation after lipopolysaccharide administration in humans with PET. Proc Natl Acad Sci USA 112: 12468–12473, 2015. doi: 10.1073/pnas.1511003112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Santello M, Volterra A. TNFα in synaptic function: switching gears. Trends Neurosci 35: 638–647, 2012. doi: 10.1016/j.tins.2012.06.001. [DOI] [PubMed] [Google Scholar]
- 200.Saper CB, Romanovsky AA, Scammell TE. Neural circuitry engaged by prostaglandins during the sickness syndrome. Nat Neurosci 15: 1088–1095, 2012. doi: 10.1038/nn.3159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Schafer DP, Lehrman EK, Kautzman AG, Koyama R, Mardinly AR, Yamasaki R, Ransohoff RM, Greenberg ME, Barres BA, Stevens B. Microglia sculpt postnatal neural circuits in an activity and complement-dependent manner. Neuron 74: 691–705, 2012. doi: 10.1016/j.neuron.2012.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Scheiermann C, Kunisaki Y, Lucas D, Chow A, Jang JE, Zhang D, Hashimoto D, Merad M, Frenette PS. Adrenergic nerves govern circadian leukocyte recruitment to tissues. Immunity 37: 290–301, 2012. doi: 10.1016/j.immuni.2012.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Sebastião AM, Ribeiro JA. Neuromodulation and metamodulation by adenosine: Impact and subtleties upon synaptic plasticity regulation. Brain Res 1621: 102–113, 2015. doi: 10.1016/j.brainres.2014.11.008. [DOI] [PubMed] [Google Scholar]
- 204.Segerstrom SC. Personality and the immune system: models, methods, and mechanisms. Ann Behav Med 22: 180–190, 2000. doi: 10.1007/BF02895112. [DOI] [PubMed] [Google Scholar]
- 205.Selye H. A syndrome produced by diverse nocuous agents. Nature 138: 32, 1936. doi: 10.1038/138032a0. [DOI] [PubMed] [Google Scholar]
- 206.Serrats J, Schiltz JC, García-Bueno B, van Rooijen N, Reyes TM, Sawchenko PE. Dual roles for perivascular macrophages in immune-to-brain signaling. Neuron 65: 94–106, 2010. doi: 10.1016/j.neuron.2009.11.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Sharp B, Yaksh T. Pain killers of the immune system. Nat Med 3: 831–832, 1997. doi: 10.1038/nm0897-831. [DOI] [PubMed] [Google Scholar]
- 208.Silverman MN, Pearce BD, Biron CA, Miller AH. Immune modulation of the hypothalamic-pituitary-adrenal (HPA) axis during viral infection. Viral Immunol 18: 41–78, 2005. doi: 10.1089/vim.2005.18.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Sklar LS, Anisman H. Stress and coping factors influence tumor growth. Science 205: 513–515, 1979. doi: 10.1126/science.109924. [DOI] [PubMed] [Google Scholar]
- 210.Sloan EK, Priceman SJ, Cox BF, Yu S, Pimentel MA, Tangkanangnukul V, Arevalo JM, Morizono K, Karanikolas BD, Wu L, Sood AK, Cole SW. The sympathetic nervous system induces a metastatic switch in primary breast cancer. Cancer Res 70: 7042–7052, 2010. doi: 10.1158/0008-5472.CAN-10-0522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Slyepchenko A, Maes M, Jacka FN, Köhler CA, Barichello T, McIntyre RS, Berk M, Grande I, Foster JA, Vieta E, Carvalho AF. Gut Microbiota, Bacterial Translocation, and Interactions with Diet: Pathophysiological Links between Major Depressive Disorder and Non-Communicable Medical Comorbidities. Psychother Psychosom 86: 31–46, 2017. doi: 10.1159/000448957. [DOI] [PubMed] [Google Scholar]
- 212.Smith EM, Blalock JE. Human lymphocyte production of corticotropin and endorphin-like substances: association with leukocyte interferon. Proc Natl Acad Sci USA 78: 7530–7534, 1981. doi: 10.1073/pnas.78.12.7530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Smith EM, Meyer WJ, Blalock JE. Virus-induced corticosterone in hypophysectomized mice: a possible lymphoid adrenal axis. Science 218: 1311–1312, 1982. doi: 10.1126/science.6183748. [DOI] [PubMed] [Google Scholar]
- 214.Sorrells SF, Sapolsky RM. An inflammatory review of glucocorticoid actions in the CNS. Brain Behav Immun 21: 259–272, 2007. doi: 10.1016/j.bbi.2006.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Spengler RN, Allen RM, Remick DG, Strieter RM, Kunkel SL. Stimulation of alpha-adrenergic receptor augments the production of macrophage-derived tumor necrosis factor. J Immunol 145: 1430–1434, 1990. [PubMed] [Google Scholar]
- 216.Sperner-Unterweger B, Kohl C, Fuchs D. Immune changes and neurotransmitters: possible interactions in depression? Prog Neuropsychopharmacol Biol Psychiatry 48: 268–276, 2014. doi: 10.1016/j.pnpbp.2012.10.006. [DOI] [PubMed] [Google Scholar]
- 217.Stangl H, Springorum HR, Muschter D, Grässel S, Straub RH. Catecholaminergic-to-cholinergic transition of sympathetic nerve fibers is stimulated under healthy but not under inflammatory arthritic conditions. Brain Behav Immun 46: 180–191, 2015. doi: 10.1016/j.bbi.2015.02.022. [DOI] [PubMed] [Google Scholar]
- 218.Stein C, Clark JD, Oh U, Vasko MR, Wilcox GL, Overland AC, Vanderah TW, Spencer RH. Peripheral mechanisms of pain and analgesia. Brain Res Brain Res Rev 60: 90–113, 2009. doi: 10.1016/j.brainresrev.2008.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Stein C, Hassan AH, Przewłocki R, Gramsch C, Peter K, Herz A. Opioids from immunocytes interact with receptors on sensory nerves to inhibit nociception in inflammation. Proc Natl Acad Sci USA 87: 5935–5939, 1990. doi: 10.1073/pnas.87.15.5935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Stein M, Schiavi RC, Camerino M. Influence of brain and behavior on the immune system. Science 191: 435–440, 1976. doi: 10.1126/science.1108202. [DOI] [PubMed] [Google Scholar]
- 221.Stellwagen D, Beattie EC, Seo JY, Malenka RC. Differential regulation of AMPA receptor and GABA receptor trafficking by tumor necrosis factor-alpha. J Neurosci 25: 3219–3228, 2005. doi: 10.1523/JNEUROSCI.4486-04.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Stephan AH, Barres BA, Stevens B. The complement system: an unexpected role in synaptic pruning during development and disease. Annu Rev Neurosci 35: 369–389, 2012. doi: 10.1146/annurev-neuro-061010-113810. [DOI] [PubMed] [Google Scholar]
- 223.Stevens B, Allen NJ, Vazquez LE, Howell GR, Christopherson KS, Nouri N, Micheva KD, Mehalow AK, Huberman AD, Stafford B, Sher A, Litke AM, Lambris JD, Smith SJ, John SW, Barres BA. The classical complement cascade mediates CNS synapse elimination. Cell 131: 1164–1178, 2007. doi: 10.1016/j.cell.2007.10.036. [DOI] [PubMed] [Google Scholar]
- 224.Swanson MA, Lee WT, Sanders VM. IFN-gamma production by Th1 cells generated from naive CD4+ T cells exposed to norepinephrine. J Immunol 166: 232–240, 2001. doi: 10.4049/jimmunol.166.1.232. [DOI] [PubMed] [Google Scholar]
- 225.Szpunar MJ, Belcher EK, Dawes RP, Madden KS. Sympathetic innervation, norepinephrine content, and norepinephrine turnover in orthotopic and spontaneous models of breast cancer. Brain Behav Immun 53: 223–233, 2016. doi: 10.1016/j.bbi.2015.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Talabér G, Jondal M, Okret S. Extra-adrenal glucocorticoid synthesis: immune regulation and aspects on local organ homeostasis. Mol Cell Endocrinol 380: 89–98, 2013. doi: 10.1016/j.mce.2013.05.007. [DOI] [PubMed] [Google Scholar]
- 227.Tanaka K, Furuyashiki T, Kitaoka S, Senzai Y, Imoto Y, Segi-Nishida E, Deguchi Y, Breyer RM, Breyer MD, Narumiya S. Prostaglandin E2-mediated attenuation of mesocortical dopaminergic pathway is critical for susceptibility to repeated social defeat stress in mice. J Neurosci 32: 4319–4329, 2012. doi: 10.1523/JNEUROSCI.5952-11.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Thaker PH, Han LY, Kamat AA, Arevalo JM, Takahashi R, Lu C, Jennings NB, Armaiz-Pena G, Bankson JA, Ravoori M, Merritt WM, Lin YG, Mangala LS, Kim TJ, Coleman RL, Landen CN, Li Y, Felix E, Sanguino AM, Newman RA, Lloyd M, Gershenson DM, Kundra V, Lopez-Berestein G, Lutgendorf SK, Cole SW, Sood AK. Chronic stress promotes tumor growth and angiogenesis in a mouse model of ovarian carcinoma. Nat Med 12: 939–944, 2006. doi: 10.1038/nm1447. [DOI] [PubMed] [Google Scholar]
- 229.Tilders FJ, Schmidt ED. Cross-sensitization between immune and non-immune stressors. A role in the etiology of depression? Adv Exp Med Biol 461: 179–197, 1999. doi: 10.1007/978-0-585-37970-8_11. [DOI] [PubMed] [Google Scholar]
- 230.Tilders FJ, Schmidt ED. Interleukin-1-induced plasticity of hypothalamic CRH neurons and long-term stress hyperresponsiveness. Ann N Y Acad Sci 840: 65–73, 1998. doi: 10.1111/j.1749-6632.1998.tb09550.x. [DOI] [PubMed] [Google Scholar]
- 231.Tracey KJ. The inflammatory reflex. Nature 420: 853–859, 2002. doi: 10.1038/nature01321. [DOI] [PubMed] [Google Scholar]
- 232.Turnbull AV, Rivier CL. Regulation of the hypothalamic-pituitary-adrenal axis by cytokines: actions and mechanisms of action. Physiol Rev 79: 1–71, 1999. [DOI] [PubMed] [Google Scholar]
- 233.Valdearcos M, Xu AW, Koliwad SK. Hypothalamic inflammation in the control of metabolic function. Annu Rev Physiol 77: 131–160, 2015. doi: 10.1146/annurev-physiol-021014-071656. [DOI] [PubMed] [Google Scholar]
- 234.Vandevyver S, Dejager L, Tuckermann J, Libert C. New insights into the anti-inflammatory mechanisms of glucocorticoids: an emerging role for glucocorticoid-receptor-mediated transactivation. Endocrinology 154: 993–1007, 2013. doi: 10.1210/en.2012-2045. [DOI] [PubMed] [Google Scholar]
- 235.Vandevyver S, Dejager L, Van Bogaert T, Kleyman A, Liu Y, Tuckermann J, Libert C. Glucocorticoid receptor dimerization induces MKP1 to protect against TNF-induced inflammation. J Clin Invest 122: 2130–2140, 2012. doi: 10.1172/JCI60006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Velkeniers B, Dogusan Z, Naessens F, Hooghe R, Hooghe-Peters EL. Prolactin, growth hormone and the immune system in humans. Cell Mol Life Sci 54: 1102–1108, 1998. doi: 10.1007/s000180050239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Vichaya EG, Hunt SC, Dantzer R. Lipopolysaccharide reduces incentive motivation while boosting preference for high reward in mice. Neuropsychopharmacology 39: 2884–2890, 2014. doi: 10.1038/npp.2014.141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Visintainer MA, Volpicelli JR, Seligman ME. Tumor rejection in rats after inescapable or escapable shock. Science 216: 437–439, 1982. doi: 10.1126/science.7200261. [DOI] [PubMed] [Google Scholar]
- 239.Vitkovic L, Konsman JP, Bockaert J, Dantzer R, Homburger V, Jacque C. Cytokine signals propagate through the brain. Mol Psychiatry 5: 604–615, 2000. doi: 10.1038/sj.mp.4000813. [DOI] [PubMed] [Google Scholar]
- 240.Vivash L, O’Brien TJ. Imaging Microglial Activation with TSPO PET: Lighting Up Neurologic Diseases? J Nucl Med 57: 165–168, 2016. doi: 10.2967/jnumed.114.141713. [DOI] [PubMed] [Google Scholar]
- 241.Walker AK, Budac DP, Bisulco S, Lee AW, Smith RA, Beenders B, Kelley KW, Dantzer R. NMDA receptor blockade by ketamine abrogates lipopolysaccharide-induced depressive-like behavior in C57BL/6J mice. Neuropsychopharmacology 38: 1609–1616, 2013. doi: 10.1038/npp.2013.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Wang H, Yu M, Ochani M, Amella CA, Tanovic M, Susarla S, Li JH, Wang H, Yang H, Ulloa L, Al-Abed Y, Czura CJ, Tracey KJ. Nicotinic acetylcholine receptor alpha7 subunit is an essential regulator of inflammation. Nature 421: 384–388, 2003. doi: 10.1038/nature01339. [DOI] [PubMed] [Google Scholar]
- 243.Wang Y, Szretter KJ, Vermi W, Gilfillan S, Rossini C, Cella M, Barrow AD, Diamond MS, Colonna M. IL-34 is a tissue-restricted ligand of CSF1R required for the development of Langerhans cells and microglia. Nat Immunol 13: 753–760, 2012. doi: 10.1038/ni.2360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Watkins JL, Thaker PH, Nick AM, Ramondetta LM, Kumar S, Urbauer DL, Matsuo K, Squires KC, Coleman RL, Lutgendorf SK, Ramirez PT, Sood AK. Clinical impact of selective and nonselective beta-blockers on survival in patients with ovarian cancer. Cancer 121: 3444–3451, 2015. doi: 10.1002/cncr.29392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Wei L, Simen A, Mane S, Kaffman A. Early life stress inhibits expression of a novel innate immune pathway in the developing hippocampus. Neuropsychopharmacology 37: 567–580, 2012. doi: 10.1038/npp.2011.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Weigent DA. Lymphocyte GH-axis hormones in immunity. Cell Immunol 285: 118–132, 2013. doi: 10.1016/j.cellimm.2013.10.003. [DOI] [PubMed] [Google Scholar]
- 247.Weingarten S, Senn M, Langhans W. Does a learned taste aversion contribute to the anorectic effect of bacterial lipopolysaccharide? Physiol Behav 54: 961–966, 1993. doi: 10.1016/0031-9384(93)90309-4. [DOI] [PubMed] [Google Scholar]
- 248.Wilder RL. Neuroendocrine-immune system interactions and autoimmunity. Annu Rev Immunol 13: 307–338, 1995. doi: 10.1146/annurev.iy.13.040195.001515. [DOI] [PubMed] [Google Scholar]
- 249.Wohleb ES, Franklin T, Iwata M, Duman RS. Integrating neuroimmune systems in the neurobiology of depression. Nat Rev Neurosci 17: 497–511, 2016. doi: 10.1038/nrn.2016.69. [DOI] [PubMed] [Google Scholar]
- 250.Wohleb ES, McKim DB, Sheridan JF, Godbout JP. Monocyte trafficking to the brain with stress and inflammation: a novel axis of immune-to-brain communication that influences mood and behavior. Front Neurosci 8: 447, 2015. doi: 10.3389/fnins.2014.00447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Wohleb ES, Powell ND, Godbout JP, Sheridan JF. Stress-induced recruitment of bone marrow-derived monocytes to the brain promotes anxiety-like behavior. J Neurosci 33: 13820–13833, 2013. doi: 10.1523/JNEUROSCI.1671-13.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Wybran J. Enkephalins and endorphins as modifiers of the immune system: present and future. Fed Proc 44: 92–94, 1985. [PubMed] [Google Scholar]
- 253.Wybran J, Appelboom T, Famaey JP, Govaerts A. Suggestive evidence for receptors for morphine and methionine-enkephalin on normal human blood T lymphocytes. J Immunol 123: 1068–1070, 1979. [PubMed] [Google Scholar]
- 254.Yirmiya R. Endotoxin produces a depressive-like episode in rats. Brain Res 711: 163–174, 1996. doi: 10.1016/0006-8993(95)01415-2. [DOI] [PubMed] [Google Scholar]
- 255.Zhang D, Li Y, Peng H, Liu H, Cheng Q, Cheng X, Zeng P, Wu P, Chen H, Huang Y, Ye D. Glucocorticoids sensitize rat placental inflammatory responses via inhibiting lipoxin A4 biosynthesis. Biol Reprod 90: 74, 2014. doi: 10.1095/biolreprod.113.116384. [DOI] [PubMed] [Google Scholar]
- 256.Zhao CM, Hayakawa Y, Kodama Y, Muthupalani S, Westphalen CB, Andersen GT, Flatberg A, Johannessen H, Friedman RA, Renz BW, Sandvik AK, Beisvag V, Tomita H, Hara A, Quante M, Li Z, Gershon MD, Kaneko K, Fox JG, Wang TC, Chen D. Denervation suppresses gastric tumorigenesis. Sci Transl Med 6: 250ra115, 2014. doi: 10.1126/scitranslmed.3009569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Zmijewski MA, Slominski AT. Neuroendocrinology of the skin: an overview and selective analysis. Dermatoendocrinol 3: 3–10, 2011. doi: 10.4161/derm.3.1.14617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Zweigner J, Schumann RR, Weber JR. The role of lipopolysaccharide-binding protein in modulating the innate immune response. Microbes Infect 8: 946–952, 2006. doi: 10.1016/j.micinf.2005.10.006. [DOI] [PubMed] [Google Scholar]