Abstract
Stress-induced disorders such as anxiety represent the leading causes of adult disability worldwide. Previous studies indicate that yoga and other contemplative practices such as pranayama, or controlled yogic breathing techniques, may be effective in the treatment of mood disorders and stress. In this study, 142 individuals (mean age = 43 years; SD = 13.90) participated in a 3-day retreat program during which they learned Shambhavi Mahamudra kriya, which is a yogic practice that includes both deep breathing and meditation techniques. Participants were instructed to practice the kriya each day for 21 minutes. After 6 weeks of daily practice, participants reported subjectively lower levels of perceived stress (Perceived Stress Scale) and higher levels of general well-being (General Well-Being Scale) compared to baseline. These results support the notion that Shambhavi Mahamudra kriya may represent a natural treatment for stress reduction.
Keywords: meditation, yoga, pranayama, kriya, breathing, stress, well-being, integrative health
Stress-induced disorders such as anxiety represent the leading causes of adult disability worldwide1,2 and account for an estimated 60% to 80% of physician office visits.3 Stress can also exacerbate disorders such as cardiovascular disease, obesity, and chronic pain as well as mental health, gastrointestinal, and sleep disorders. Similarly, anxiety is the strongest risk factor for depression, and both conditions are associated with anomalies in mood-related areas of the brain.4
Stress is a state of disharmony caused by perceived threat and other intrinsic or extrinsic adverse factors that is counteracted by multiple behavioral and physiological responses, which represent an adaptive response to reestablish homeostasis. Chronic stress involves a prolonged or repeated threat to homeostasis that may result in dysregulation of the hypothalamic-pituitary-adrenal axis and autonomic nervous system.5 Chronic stress can lead to premature aging, immunosuppression, mental disorders, reproductive suppression, and a decreased ability to terminate the stress response.6 Chronic stress and increased inflammation may cause or aggravate anxious and depressive disorders.7–9 Stress, hypothalamic-pituitary-adrenal axis deregulation, and increased oxidative stress, or heightened inflammatory burden, have an interconnected relationship and are associated with mood disorders such as anxiety and depression.10 Studies on tricyclic medication used to treat depression and some anxiety symptoms have suggested the mechanism of action to include the modulation of inflammatory cytokines.11–13
Numerous studies have associated yoga- and meditation-based practices with positive psychological and physiological outcomes in both clinical and nonclinical populations.14–17 Increasing evidence suggests that mediation and yoga practices have positive effects on the regulation of the hypothalamic-pituitary-adrenal axis and inflammatory processes.18–20 Studies have suggested that yoga and other contemplative practices may be equally effective as pharmacotherapy in the treatment of mood disorders such as anxiety and depression.21,22
Controlled yogic breathing or pranayama is 1 of 8 practices used in the traditional system of yoga, which also includes meditation and yogic postures. While relatively few studies have been conducted on pranayama, such breathing techniques have been shown to elicit significant changes in both human physiology and psychology. Studies using pranayama interventions have reported changes that include reduction in hypertension, breathing frequency, and stress as well as increased heart rate variability, sympathovagal balance, cognitive performance, central neural processing, dexterity, and motor coordination.23–28 While the burgeoning study of pranayama has been recently established, the full efficacy of various breathing techniques and especially the biological mechanisms mediating the effect of yogic breathing are largely unknown.
Shambhavi Mahamudra kriya is a protocol within the Isha Yoga lineage that includes both pranyanama and meditation-based techniques. A kriya is a yogic action, or inner technique, such as breath control. Shambhavi Mahamudra is an integrative system of several breathing techniques that incorporate multiple limbs of traditional Raja Yoga or the yoga described by Patanjali in the Yoga Sutras.29 The Shambhavi Mahamudra practice is taught by a nonprofit international humanitarian organization. The practice is performed for 21 minutes daily whereby multiple deep, controlled breathing techniques and the engagement of bandhas, or muscular locks in the abdomen and pelvic floor, are applied for 15 minutes; the practice concludes with about 5 minutes of open-monitoring meditation.
Currently, very few studies exist on the Shambhavi Mahamudra practice specifically. However, one study on Isha Yoga in expert practitioners using a set of 6 yogic practices that included the Shambhavi Mahamudra kriya, reported increased heart rate variability and sympathovagal balance in practitioners compared with controls.26 The increased heart rate variability in the absence of increased heart rate revealed balance in vagal afferents during supine rest and deep breathing in the yoga practitioners compared with controls. The authors concluded that the expert yoga practitioners may have improved long-term cardiac responses to daily stresses. In addition, a small pilot study performed real-time electrocardiogram monitoring in expert practitioners during their practice of Shambhavi Mahamudra.30 The authors reported that the various pranayama techniques employed during the kriya elicited unique profiles in terms of vagal and sympathetic tone. Thus, Shambhavi Mahamudra kriya may represent a natural, low-cost breath-based intervention with the potential to decrease stress and increase general well-being.
The present protocol differs from commonly used techniques in mental health improvement such as cognitive behavioral therapy. Cognitive behavioral therapy seeks to alter behavior by focusing on the sensations, thoughts, images, and beliefs of the patient and how these experiences relate to emotional responses and coping. Mind-body practices employ a slightly different approach whereby the patient focuses on only what arises naturally while objectively observing, which leads to personal insight and self-regulation of behavior and thought. Some data suggests a synergistic opportunity in the application of combination therapies that consist of mind-body practices such as yoga with cognitive behavioral therapy for mood disorders such as anxiety.31,32
Yogic breathing practices such as Shambhavi Mahamudra may represent efficacious therapies with few side effects for stress and its associated disorders. To date, the efficacy and biological mechanisms mediating the beneficial effects of pranayama practices on the stress response and mood are not fully understood. Very limited data are currently available on the Shambhavi Mahamudra kriya specifically, and additional studies are warranted. Given that yogic breathing induces relaxation responses,33 it was hypothesized that the Shambhavi Mahamudra practice promotes decreased stress and increased levels of subjective well-being. The present study reports the effects of a daily 21-minute Shambhavi Mahamudra practice for 6 weeks on perceived stress and general well-being in a healthy population.
Materials and Methods
Intervention
Participants attended a nonresidential retreat program in October 2012 in a major Midwestern city hosted by the Isha Foundation for 3 full days. Participants engaged in the Jnana Yoga or knowledge-based educational components of the program, were introduced to Isha Kriya, which is a guided yogic practice, and were taught the self-guided Shambhavi Mahamudra kriya, which was developed by Sadhguru Jaggi Vasudev, in detail. Most of each day was spent listening to lectures on various yogic topics and precepts used to calm the mind. Vegetarian meals were served to all attendees. Participants were encouraged to establish a daily meditation practice and perform the Shambhavi Mahamudra kriya twice daily on completion of the program.
Prior to the start of the practice of Shambhavi Mahamudra kriya, a minute of reflection on the basic precepts presented during the program is then observed followed by the performance of 5 minutes of 3 gentle, preparatory yoga asanas (postures). Subsequently, the 21-minute kriya (inner action) begins and is practiced in Siddhasana (accomplished pose), which is a cross-legged posture with left heel pressing the perineum. Shambhavi Mahamudra begins with pranayama (controlled yogic breathing) called Sukha Kriya or Nadi Shodhana, which is an alternate-nostril breathing technique (ie, a slow-paced pranayama) to encourage balance in the mind for 6 to 7 minutes, followed by 21 long repetitions of the bija mantra (root syllable) Om chanted aloud with the thumb and forefinger touching in jnana (wisdom) mudra (seal). Next, the breathing exercise Viparita Swasa or Bhastrika pranayama (ie, a fast-paced pranayama) is practiced for 3 to 4 minutes and concludes with breath retention (kumbhaka or vessel) on both the inhalation and the exhalation while actively engaging the bandhas (muscular and energetic contraction) on the pelvic floor (moola bandha), lower abdomen (uddiyana bandha), and throat (jalandhara bandha). Finally, the Shambhavi kriya practice concludes with a 5-minute period of Vipassana meditation (dhyana) or open-monitoring meditation. The Shambhavi Mahamudra kriya takes approximately 21 minutes to complete. Please note that this outline of the kriya is intended for research purposes only; the Shambhavi Mahamudra practice should be learned under the instruction and observation of a qualified teacher.
The 3-day program in which Shambhavi Mahamudra is taught incorporates Jnana Yoga, or the yoga of the intellect, using simple precepts that calm and center the mind taught over multiple days in a lecture series. The participants spend about 16 hours in didactic lecture on yogic topics and precepts over the course of the program. The precepts encourage personal growth and empowerment through the acceptance of responsibility for the uncertain circumstances encountered throughout the human experience. Participants perform about 10 hours of guided, gentle Isha Hatha Yoga over the course of the retreat program. Participants are also introduced to a guided kriya yoga meditation called Isha Kriya, which focuses on seated meditation and an internal action or kriya, which is a specific thought in this case. Over the 3 days, participants receive about 26 hours of instruction, which includes teacher demonstration, on the Shambhavi Mahamudra kriya. Before the conclusion of the program on day 3, participants complete the Shambhavi Mahamudra kriya twice for about 21 minutes with minimal guidance. The total dosage of the full Shambhavi Mahamudra kriya for this study was 21 minutes performed twice on day 3 of the retreat program (total n = 42 minutes), then at least 21 minutes daily for 6 weeks postretreat.
Survey Setting and Distribution
Survey data were originally collected for quality improvement purposes by the organization that developed and teaches Shambhavi Mahamudra kriya and Isha Kriya; the Isha General Well-Being Surveys were not originally designed for research purposes. The Perceived Stress Scale is one of the most commonly used psychological and psychosomatic research instruments to assess and report perceived stress level.34 Prior to completing the surveys, participants were informed that deidentified survey data may possibly be used in future publications. Institutional review board approval was obtained from Quorum Review in July 2015 for this data to be analyzed for research purposes in accordance with the guidelines of the study of human subjects.
Participants were invited to voluntarily complete baseline and follow-up surveys on SurveyMonkey.com. Two weeks prior to the program, baseline survey links were sent via email to all individuals who had registered to attend. The survey contained demographic questions, including name, age, gender, past meditation experience, frequency and duration of current meditation, and the measures described below (see Outcome Measures section). Baseline survey collection ended 4 days prior to the start of the program.
The follow-up survey was emailed 6 weeks after the program to all persons who attended and for whom baseline data were obtained. Identical measures were used in the follow-up survey with the addition of questions regarding how often respondents practiced Shambhavi Mahamudra or Isha Kriya and the amount of time they meditated each day.
Outcome Measures
Perceived Stress Scale
The Perceived Stress Scale (PSS)35 includes 10 questions devised to ascertain the degree to which respondents perceive their lives to be “unpredictable, uncontrollable, and overwhelming.” Sample items include: “In the past month, how often have you felt that you were on top of things?” and “In the past month, how often have you felt things were going your way?” Items are answered on a 5-point Likert-type scale ranging from 1 = never to 5 = very often; 4 items are reverse scored. The final score is a sum of all items and can range from 10 to 50 with higher scores indicating greater perceived stress.
The PSS has demonstrated good internal validity (α = .78) and good construct validity when compared with other measures of stress.36 The PSS demonstrated high internal reliability within the current sample (baseline α = .907, n = 461; follow-up α = .874, n = 135). Moreover, the PSS has shown predictive validity for symptoms of depression and common physical symptomology.35
General Well-Being Scale
The General Well-Being Scale (GWBS) was created for the quality improvement surveys, and includes 12 items, one of which is reverse scored. Factor analyses of follow-up responses indicate a single factor scale when 4 items are excluded (see Table 1). The 8 remaining items include statements about mental clarity, self-confidence, inner peace, and productivity. Respondents indicate how true each item is for them on a 5-point Likert-type scale ranging from 1 = never true to 5 = always true. Scores are based on a sum of all items, ranging from 10 to 50. In the current sample, the GWBS demonstrated high internal validity (baseline α = .899, n = 467; follow-up α = .913, n = 139).
Table 1.
Factor Analysis Using the General Well-Being Scale.
| 12 Items | 8 Itemsa | |||||
|---|---|---|---|---|---|---|
| Items | Component 1 | Component 2 | Component 3 | Total Initial Eigen Value | Component 1 | Total Initial Eigen Value |
| I have excellent mental clarity | 0.768 | −0.283 | 0.012 | 5.289 | 0.796 | 4.711 |
| My ability to stay on task is excellent | 0.725 | −0.324 | 0.049 | 1.213 | 0.759 | 0.764 |
| I’m emotionally balanced | 0.776 | −0.189 | −0.049 | 1.004 | 0.797 | 0.630 |
| I have deep inner peace | 0.764 | −0.147 | −0.035 | 0.848 | 0.776 | 0.501 |
| I rarely get up in the middle of the night | 0.480 | 0.575 | −0.388 | 0.739 | — | — |
| My energy level is excellent | 0.759 | 0.144 | 0.042 | 0.604 | 0.739 | 0.471 |
| It is easy for me to fall asleep | 0.548 | 0.554 | −0.239 | 0.528 | — | — |
| I have excellent self-confidence | 0.768 | −0.170 | 0.005 | 0.465 | 0.786 | 0.347 |
| My productivity is excellent | 0.788 | −0.140 | 0.015 | 0.416 | 0.799 | 0.311 |
| I rarely feel anxious | 0.694 | 0.065 | 0.056 | 0.336 | 0.679 | 0.264 |
| I rarely get colds/flu | 0.396 | 0.417 | 0.253 | 0.307 | — | — |
| I have frequent headaches | 0.179 | 0.292 | 0.849 | 0.251 | — | — |
aUsed for analyses.
Statistical Analyses
Paired samples t tests and cross-tabs chi-squares were used to compare those who completed a baseline and follow-up survey (survey responders) to those who only completed a baseline survey (survey nonresponders). To compare frequency and duration of meditation practices across these groups at baseline, data were organized into ordinal scales (see Table 2). Paired samples t tests were used to compare baseline and follow-up scores for the final sample. Repeated-measures analyses of variance were used to compare meditation intensity groups at follow-up while controlling for baseline characteristics. Post hoc analyses included Bonferroni correction to reduce likelihood of type I error (false positive) and to probe intensity group comparisons for significance; planned contrasts were used to further probe intergroup differences when appropriate.
Table 2.
Ordinal Scales and Values for Duration and Frequency of Meditation Practice at Baseline.
| Meditation Descriptora | Value |
|---|---|
| Meditation duration, minutes per day | |
| 1-20 | 1 |
| 21-40 | 2 |
| 40+ | 3 |
| Meditation frequency, times per week | |
| 1-2 | 1 |
| 3-5 | 2 |
| 6-7 | 3 |
| 7+ | 4 |
aRespondents could select more than one descriptor; the lowest value descriptor was considered.
Results
Participants
Survey Response Rate
Baseline surveys were sent via email to 1003 individuals, all of whom had registered for the retreat program; 470 registrants did not respond to the survey, 32 opted out, 10 invites generated a mail delivery failure message, and 491 took the survey of which 483 completed the survey in full.
Six weeks after the conclusion of the program, follow-up surveys were sent to 483 individuals who had completed a baseline survey and had attended the program; 327 did not respond, 7 opted out, 3 invites generated a delivery failure message, and 146 took the survey of which 144 completed the survey in full. Using email addresses as the identifying link between baseline and follow-up surveys, completed baseline and completed follow-up surveys were successfully paired for 142 participants; it is presumed that 2 individuals reported differing email addresses at baseline and follow-up.
Survey Responders and Nonresponders
Of the 483 individuals who completed a baseline survey, 142 completed a baseline and follow-up survey (survey responders, 29.39%) and 341 individuals completed only a baseline survey (survey nonresponders, 70.60%). At baseline, survey responders and nonresponders significantly differed in general well-being, percentage that had no meditation experience, and percentage that were practicing Isha Kriya (see Table 3).
Table 3.
Comparison of Post-Retreat Survey Responders and Nonresponders at Baseline.
| Survey Responders | Survey Nonresponders | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Characteristic | n | Mean | SD | n | Mean | SD | df | t | P | |
| Age, years | 142 | 43.19 | 13.719 | 338 | 41.84 | 13.829 | 478 | 0.976 | .329 | |
| PSS score | 142 | 26.67 | 7.736 | 341 | 27.82 | 7.459 | 481 | −1.520 | .129 | |
| GWBS score | 142 | 26.28 | 5.644 | 341 | 25.14 | 5.717 | 481 | 2.006 | .045 | |
| Frequency | Percentage | Frequency | Percentage | df, n | χ2 | P | ||||
| Gender | 1, 479 | 0.152 | .697 | |||||||
| Male | 64 | 45.4 | 160 | 47.3 | ||||||
| Female | 77 | 54.6 | 178 | 52.7 | ||||||
| Meditation duration, minutes per day | 2, 109 | 8.273 | .016 | |||||||
| 1-20 | 24 | 48.0 | 43 | 72.9 | ||||||
| 21-40 | 19 | 38.0 | 9 | 15.3 | ||||||
| 40+ | 7 | 14.0 | 7 | 11.9 | ||||||
| Meditation frequency, times per week | 3, 136 | 4.666 | .198 | |||||||
| 1-2 | 15 | 30.6 | 36 | 41.4 | ||||||
| 3-5 | 17 | 34.7 | 26 | 29.9 | ||||||
| 6-7 | 7 | 14.3 | 17 | 19.5 | ||||||
| 7+ | 10 | 20.4 | 8 | 9.2 | ||||||
| No meditation experience | 1, 483 | 5.739 | .017 | |||||||
| Selected | 33 | 23.2 | 117 | 34.3 | ||||||
| Did not select | 117 | 76.8 | 224 | 65.7 | ||||||
| Meditated in past | 1, 483 | 0.000 | .984 | |||||||
| Selected | 49 | 34.5 | 118 | 34.6 | ||||||
| Did not select | 93 | 65.5 | 223 | 65.4 | ||||||
| Practice Isha kriya | 1, 483 | 9.119 | .003 | |||||||
| Selected | 33 | 23.2 | 42 | 12.3 | ||||||
| Did not select | 109 | 76.8 | 299 | 87.7 | ||||||
Abbreviations: PSS, Perceived Stress Scale; GWBS, General Well-Being Scale.
Final Sample
The final 142 participants, who had fully completed both the baseline and follow-up survey, ranged in age from 16 to 77 years, with a mean age of 43.19 years (SD = 13.719) and the majority were female (54.2%). At baseline, 33 participants (23.2%) reported having no meditation experience, 49 (34.5%) stated they had meditated in the past, and 83 (58.5%) indicated they currently meditated in some way (see Table 4).
Table 4.
Meditation Practice Duration and Frequency at Baseline and Follow-up (n = 142).
| Descriptora | n | Percentage |
|---|---|---|
| Baseline | ||
| No meditation experience | 33 | 23.2 |
| Meditated in past | 49 | 34.5 |
| Isha kriya | 33 | 23.2 |
| 1-20 minutes per day | 24 | 16.9 |
| 21-40 minutes per day | 19 | 13.4 |
| 40+ minutes per day | 7 | 4.9 |
| 1-2 times per week | 15 | 10.6 |
| 3-5 times per week | 17 | 12.0 |
| 6-7 times per week | 7 | 4.9 |
| 7+ times per week | 10 | 7.0 |
| Follow-up | ||
| Shambhavi 6+ times per week | 96 | 67.6 |
| Shambhavi 1-6 times per week | 33 | 23.2 |
| Did not practice Shambhavi | 8 | 5.6 |
| Isha kriya 4+ times per week | 11 | 7.7 |
| Isha kriya 1-3 times per week | 7 | 4.9 |
| 10-30 minutes per day | 74 | 52.1 |
| 31-60 minutes per day | 54 | 38.0 |
| Other practice | 17 | 12.0 |
| Did not meditate | 14 | 9.9 |
aRespondents could select more than one descriptor.
Practice Intensity Groups
At follow-up, participants were asked to select an option that described the frequency, duration, and type of meditation they practiced following the program (see Table 4). Participants were divided into 3 groups based on the descriptor they selected: optimum kriya practice intensity, moderate practice intensity, or low practice intensity. The optimum practice intensity group included those who practiced Shambhavi 6 or more times per week (96 participants, 67.6%); the moderate practice intensity group included participants who practiced Shambhavi 1 to 6 times per week (33 participants, 23.2%); and the low practice intensity group included those who practiced Isha Kriya or other practices besides Shambhavi regardless of frequency (13 participants, 9.2%).
At baseline, kriya practice intensity groups differed significantly at baseline in gender, percentage with prior meditation experience, and percentage who had meditated in the past (see Table 5). At follow-up, program participants reported lower perceived stress (change mean = −4.05, SD = 6.529), t(141) = −7.393, P < .001) and a higher level of general well-being (change mean = 2.39, SD = 5.128), t(141) = 5.564, P < .001).
Table 5.
Comparison of Practice Intensity Groups at Baseline.
| Optimum Intensity | Moderate Intensity | Low Intensity | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Characteristic | n | Mean | SD | n | Mean | SD | n | Mean | SD | df | F | P |
| Age, years | 96 | 42.44 | 12.738 | 33 | 43.18 | 15.735 | 13 | 48.77 | 15.117 | 2,139 | 1.223 | .297 |
| PSS score | 96 | 26.73 | 7.462 | 33 | 26.88 | 9.226 | 13 | 25.77 | 5.862 | 2,139 | 0.102 | .903 |
| GWBS score | 96 | 26.41 | 5.812 | 33 | 25.39 | 5.825 | 13 | 27.62 | 3.477 | 2,139 | 0.792 | .455 |
| Frequency | Percentage | Frequency | Percentage | Frequency | Percentage | df, n | χ2 | P | ||||
| Gender | 2, 141 | 8.128 | .017 | |||||||||
| Male | 51 | 53.7 | 9 | 27.3 | 4 | 30.8 | ||||||
| Female | 44 | 46.3 | 24 | 72.7 | 9 | 69.2 | ||||||
| Meditation duration, minutes per day | 4, 50 | 8.800 | .066 | |||||||||
| 1-20 | 19 | 47.5 | 2 | 28.6 | 3 | 100.0 | ||||||
| 21-40 | 17 | 42.5 | 2 | 28.6 | 0 | 0.0 | ||||||
| 40+ | 4 | 10.0 | 3 | 42.9 | 0 | 0.0 | ||||||
| Meditation frequency, times per week | 6, 49 | 10.829 | .094 | |||||||||
| 1-2 | 6 | 17.6 | 7 | 63.6 | 2 | 50.0 | ||||||
| 3-5 | 14 | 41.2 | 2 | 18.2 | 1 | 25.0 | ||||||
| 6-7 | 6 | 17.6 | 0 | 0.0 | 1 | 25.0 | ||||||
| 7+ | 8 | 23.5 | 2 | 18.2 | 0 | 0.0 | ||||||
| No meditation experience | 2, 142 | 7.222 | .027 | |||||||||
| Selected | 21 | 21.9 | 12 | 36.4 | 0 | 0.0 | ||||||
| Did not select | 75 | 78.1 | 21 | 63.6 | 13 | 100.0 | ||||||
| Meditated in past | 2, 142 | 8.533 | .014 | |||||||||
| Selected | 32 | 33.3 | 8 | 24.2 | 9 | 69.2 | ||||||
| Did not select | 64 | 66.7 | 25 | 75.8 | 4 | 30.8 | ||||||
| Practice Isha kriya | 2, 142 | 1.345 | .510 | |||||||||
| Selected | 25 | 26.0 | 6 | 18.2 | 2 | 15.4 | ||||||
| Did not select | 71 | 74.0 | 27 | 81.8 | 11 | 84.6 | ||||||
Abbreviations: PSS, Perceived Stress Scale; GWBS, General Well-Being Scale.
Practice Intensity Group Comparisons
Change in Perceived Stress
Controlling for baseline differences, participants, overall, experienced a significant reduction in perceived stress from baseline to follow-up, F(1, 139) = 14.076, P < .001, and practice intensity group had a significant effect on this change, F(2, 139) = 3.466, P = .034; however, post hoc analyses indicated that no 2 practice intensity groups significantly differed from one another in how much their perceived stress had changed. Further examination of these findings in a line plot (see Figure 1) suggested a significant difference may exist between the low practice intensity group and the moderate and optimum practice groups combined, F(1, 140) = 6.389, P = .013.
Figure 1.
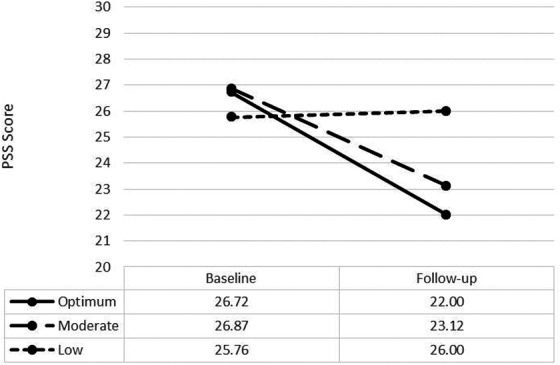
Perceived Stress Scale (PSS) scores at baseline and follow-up by meditation intensity group. PSS scores range from 10 to 50.
Change in General Well-Being
Controlling for baseline differences, participants overall experienced a significant improvement in general well-being from baseline to follow-up, F(1, 139) = 4.469, P = .036. Practice intensity group had a significant effect on this change, F(2, 139) = 5.608, P = .005; however, post hoc analyses indicated that no 2 practice intensity groups significantly differed from one another in how much their general well-being had changed. Further examination of these findings in a line plot (see Figure 2) suggested a significant difference exists between the low intensity group and the moderate and optimum groups combined, F(1, 140) = 11.274, P = .001.
Figure 2.
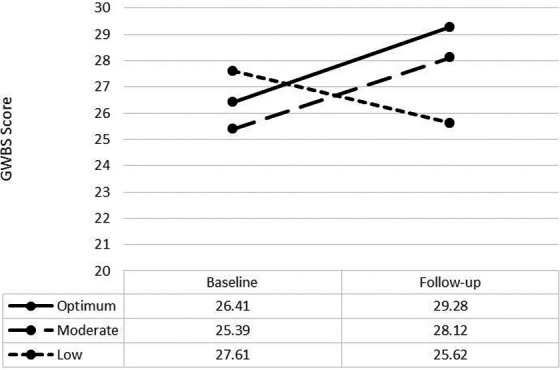
General Well-Being Scale (GWBS) scores at baseline and follow-up by meditation intensity group. GWBS scores range from 10 to 50.
Discussion
The dysregulation of the stress response may lead to mental disorders such as anxiety or depression as well as chronic inflammatory processes. The present study investigated the effects of Shambhavi Mahamudra practice, which is essentially composed of a simple 21-minute protocol of breath regulation techniques, on perceived stress and general well-being in a healthy population. Participants in a yogic retreat program, which included Shambhavi Mahamudra training, who subsequently practiced the kriya daily, reported significantly reduced perceived stress and increased general well-being at 6-weeks follow-up compared with baseline. These results support the notion that Shambhavi Mahamudra kriya may represent a complementary therapy in the treatment of anxiety and stress reduction as well as for general well-being enhancement. Thus, further studies on this kriya and the associated pranayama, or yogic breathing techniques, are warranted.
Conventional drug treatment for stress-related disorders such as anxiety and depression can lead to a number of undesirable side effects. Both chronic stress and selective serotonin reuptake inhibitor drug treatment for depression and anxiety are associated with the development of obesity and metabolic disorders.37,38 In addition, patients presenting with a high inflammatory burden may exhibit reduced response to drug intervention.39 These treatment risks as well as conditions of nonresponse to conventional treatments suggest that integrative therapies for stress and related disorders are needed.40,41 Studies have demonstrated that yoga practice can, at least in part, reduce stress responses and related cardiovascular, immunological, and endocrine changes as well as promote an improved psychological response to stress.20,42
Previous studies suggest that yoga and other contemplative practices such as the yogic breath-based techniques may be equally effective compared to conventional treatments for anxiety and depression.21,22,43 Several studies employing yoga or meditation interventions report improvement in mood disorders, physiology, stress response regulation, and well-being.44–48 For example, a breath-based kriya yoga intervention in patients diagnosed with mood and/or anxiety disorders utilized a similar set of breath practices as those employed in Shambhavi Mahamudra. The authors reported a significant reduction in anxiety and depression related symptoms postintervention.49 Another kriya yoga intervention using these breath-based techniques reported reduced perception of stress and pain in breast cancer patients compared with controls.50
In addition, these pranayama techniques promoted improved stress regulation and antioxidant status in healthy participants practicing a set of breathing techniques similar to Shambhavi Mahamudra.51 Another study using these techniques reported improved stress regulation, sympathovagal balance, and workload tolerance compared with controls.52 A randomized controlled trial using this set of practices also reported that the controlled breathing techniques were also shown to reduce examination stress and improve blood lipid profiles in stressed college students compared with controls.53 Interestingly, a Qigong intervention incorporating a similar bandha, or abdominal retraction technique, reported increased mood, comfort, and sociability following the practice.54 Studies also indicate that Isha Yoga and Iyengar yoga practices restore balance to autonomic nervous system function by modulating vagal afferents.26,42 Deep breathing, specific breath patterns, and the engagement of these abdominal and pelvic floor muscular locks (bandhas) may stimulate the vagus nerve, a key mediator of the stress response, and thus help correct reduced parasympathetic nervous system activity55–57; however, additional studies are needed to elucidate these mechanisms.
Previous research has also focused separately on the fast- and slow-breathing techniques in the context of perceived stress. Shambhavi Mahamudra incorporates both fast- and slow-pranayama methods, which are both considered deep breathing techniques practiced at different frequencies of respiration. Different types of pranayama techniques promote beneficial effects yet distinct physiological responses in healthy populations.58 A study in healthy students compared the effects of slow, fast, and no pranayama for 12 weeks on cardiovascular parameters and stress.59 The results demonstrated that both the fast and slow pranayama promoted significant decreases in perceived stress as measured by the PSS, which was also employed in the current study; however, only the slow pranayama was reported to promote a statistically significant decrease in heart rate, blood pressure, rate pressure product and double product thus indicating increased parasympathetic dominance and vagal tone in the slow compared with the fast and no practice groups. Another study in healthy students comparing slow, fast, and no pranayama for 12 weeks on perceived stress and cognitive functions reported improved executive function, perceived stress, and reaction time in both pranayama groups compared with controls.27 Perceived stress negatively affects executive functions such as memory, concentration, and information retrieval.60 The authors concluded that since perceived stress alters signaling in the prefrontal cortex during cognitive tasks, the perception of reduced stress as measured by the PSS in both pranayama groups compared with controls may promote the observed improved cognitive function in the domains of attention, visuomotor speed, and memory retention capacity. Therefore, while yogic breathing techniques promote beneficial effects, specific types and sequences of pranayama appear to produce more distinct effects. Additional research is needed to further compare the physiological and psychological effects of various types of pranayama separately and specific sequences of pranayama.
To date, the biological mechanisms by which yogic breathing practices facilitate stress reduction or mood alteration are not fully known and represent an area in need of further research. Pranayama increase thoracic volume, which produces inhibitory signals that may induce changes in the autonomic nervous system to increase parasympathetic dominance.61 While engaging the abdominal bandha (uddiyana bandha), both the volume and the hydrostatic pressure in the large intestine decreases.54 We speculate that these controlled breath practices and the engagement of the bandhas, or muscular and energetic locks, also stimulate the vagus nerve and thus facilitate correction of the reduced parasympathetic nervous system activity observed in stress-related disorders such as anxiety. One of the key pathways for the bidirectional signaling between the viscera and the brain is via the vagus nerve. The majority of the vagal nerve fibers are afferent, and communicate peripheral information, including signals from the gut and gut microbiota, to the brain.62 Moreover, gut-brain signaling affects homeostasis and may modulate behavior, mood, and mental health disorders.63 Accordingly, the neurobiological mechanisms of the beneficial effects of pranayama practices should be investigated in greater depth to facilitate a broader understanding of their potential clinical application as integrative therapies.
One of the main limitations of the current study is that the survey questionnaires were not created for research purposes, although the PSS is a commonly used instrument in psychology. The surveys include inherent methodological weaknesses, including that participants may select multiple and sometimes contradictory descriptors of their home practice after the program. Although factor analysis demonstrated that the GWBS, when shortened, displayed a single factor and good internal validity in the current sample, there is currently no other measure of the reliability or validity of the scale. Another limitation of the study was a high frequency of survey nonresponse or noncompletion; of the 1003 individuals who were sent a survey, baseline data was collected from only 491 participants, and complete follow-up data was collected from only 142 of those participants since many participants did not choose to complete a survey. Additionally, the number of participants in each practice intensity group varied widely (n = 96, 33, 13 individuals), which may have affected inter-group comparisons, and there was not a no-treatment control group included in the study. This study should be replicated in a large randomized controlled trial to ensure equal groups and include additional standard psychological questionnaires as well as assessment of biological markers of stress, anxiety, and inflammation.
In conclusion, participation in a yogic retreat program that included pranayama training and the subsequent practice of Shambhavi Mahamudra kriya for 6 weeks led to significant reductions in perceived stress and anxiety as well as increases in general well-being. Shambhavi Mahamudra kriya and other breath-based practices may represent potentially efficacious natural treatments for stress reduction and the promotion of general well-being. Yoga research is underrepresented and additional studies regarding clinical utility and mechanistic bases should be conducted. Further research is also needed to confirm the reported effects of these breathing practices on mood and the stress response. Future studies are also required in the field of pranayama research to fully understand the efficacy of the various techniques and the biological mechanisms involved.
Footnotes
Authors’ Note: The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
Author Contributions: RJK designed and ran the study. SMB processed the data and performed statistical analyses. CTP wrote the manuscript. CTP, RJK, SMB, DC, and PJM performed data analysis, wrote, and edited the manuscript.
Declaration of Conflicting Interests: The authors declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: CTP is a postdoctoral fellow at the University of California, San Diego partially funded by the Chopra Foundation. DC is a founder of the Chopra Foundation and Chopra Center and a co-owner of the Chopra Center. PM is the Scientific Director of the Chopra Foundation.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
Ethical Approval: Institutional review board approval was obtained from Quorum Review in July 2015 for these data to be analyzed for research purposes in accordance with the guidelines of the study of human subjects. This study was carried out in accordance with the recommendations of the Quorum Review committee.
References
- 1. Whiteford HA, Degenhardt L, Rehm J, et al. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet. 2013;382:1575–1586. doi:10.1016/S0140-6736(13)61611-6. [DOI] [PubMed] [Google Scholar]
- 2. Whiteford HA, Ferrari AJ, Degenhardt L, Feigin V, Vos T. The global burden of mental, neurological and substance use disorders: an analysis from the Global Burden of Disease Study 2010. PLoS One. 2015;10:e0116820 doi:10.1371/journal.pone.0116820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Nerurkar A, Bitton A, Davis RB, Phillips RS, Yeh G. When physicians counsel about stress: results of a national study. JAMA Intern Med. 2013;173:76–77. doi:10.1001/2013.jamainternmed.480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Mathew AR, Pettit JW, Lewinsohn PM, Seeley JR, Roberts RE. Co-morbidity between major depressive disorder and anxiety disorders: shared etiology or direct causation? Psychol Med. 2011;41:2023–2034. doi:10.1017/S0033291711000407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Charmandari E, Tsigos C, Chrousos G. Endocrinology of the stress response. Annu Rev Physiol. 2005;67:259–284. doi:10.1146/annurev.physiol.67.040403.120816 [DOI] [PubMed] [Google Scholar]
- 6. Sapolsky RM, Krey LC, McEwen BS. The adrenocortical stress-response in the aged male rat: impairment of recovery from stress. Exp Gerontol. 1983;18:55–64. [DOI] [PubMed] [Google Scholar]
- 7. Dantzer R. Depression and inflammation: an intricate relationship. Biol Psychiatry. 2012;71:4–5. doi:10.1016/j.biopsych.2011.10.025. [DOI] [PubMed] [Google Scholar]
- 8. Hou R, Baldwin DS. A neuroimmunological perspective on anxiety disorders. Hum Psychopharmacol. 2012;27:6–14. doi:10.1002/hup.1259. [DOI] [PubMed] [Google Scholar]
- 9. Salim S, Chugh G, Asghar M. Inflammation in anxiety. Adv Protein Chem Struct Biol. 2012;88:1–25. doi:10.1016/B978-0-12-398314-5.00001-5. [DOI] [PubMed] [Google Scholar]
- 10. Furtado M, Katzman MA. Neuroinflammatory pathways in anxiety, posttraumatic stress, and obsessive compulsive disorders. Psychiatry Res. 2015;229:37–48. doi:10.1016/j.psychres.2015.05.036. [DOI] [PubMed] [Google Scholar]
- 11. Fonseka TM, McIntyre RS, Soczynska JK, Kennedy SH. Novel investigational drugs targeting IL-6 signaling for the treatment of depression. Expert Opin Investig Drugs. 2015;24:459–475. doi:10.1517/13543784.2014.998334. [DOI] [PubMed] [Google Scholar]
- 12. Kohler O, Benros ME, Nordentoft M, et al. Effect of anti-inflammatory treatment on depression, depressive symptoms, and adverse effects: a systematic review and meta-analysis of randomized clinical trials. JAMA Psychiatry. 2014;71:1381–1391. doi:10.1001/jamapsychiatry.2014.1611. [DOI] [PubMed] [Google Scholar]
- 13. Kubera M, Holan V, Mathison R, Maes M. The effect of repeated amitriptyline and desipramine administration on cytokine release in C57BL/6 mice. Psychoneuroendocrinology. 2000;25:785–797. [DOI] [PubMed] [Google Scholar]
- 14. Cahn BR, Polich J. Meditation states and traits: EEG, ERP, and neuroimaging studies. Psychol Bull. 2006;132:180–211. doi:10.1037/0033-2909.132.2.180. [DOI] [PubMed] [Google Scholar]
- 15. Chiesa A, Serretti A. A systematic review of neurobiological and clinical features of mindfulness meditations. Psychol Med. 2010;40:1239–1252. doi:10.1017/S0033291709991747. [DOI] [PubMed] [Google Scholar]
- 16. Davidson RJ, McEwen BS. Social influences on neuroplasticity: stress and interventions to promote well-being. Nat Neurosci. 2012;15:689–695. doi:10.1038/nn.3093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Rubia K. The neurobiology of meditation and its clinical effectiveness in psychiatric disorders. Biol Psychol. 2009;82:1–11. doi:10.1016/j.biopsycho.2009.04.003. [DOI] [PubMed] [Google Scholar]
- 18. Bower JE, Irwin MR. Mind-body therapies and control of inflammatory biology: a descriptive review. Brain Behav Immun. 2016;51:1–11. doi:10.1016/j.bbi.2015.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kaliman P, Alvarez-Lopez MJ, Cosin-Tomas M, Rosenkranz MA, Lutz A, Davidson RJ. Rapid changes in histone deacetylases and inflammatory gene expression in expert meditators. Psychoneuroendocrinology. 2014;40:96–107. doi:10.1016/j.psyneuen.2013.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kiecolt-Glaser JK, Christian L, Preston H, et al. Stress, inflammation, and yoga practice. Psychosom Med. 2010;72:113–121. doi:10.1097/PSY.0b013e3181cb9377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Chen KW, Berger CC, Manheimer E, et al. Meditative therapies for reducing anxiety: a systematic review and meta-analysis of randomized controlled trials. Depress Anxiety. 2012;29:545–562. doi:10.1002/da.21964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. da Silva TL, Ravindran LN, Ravindran AV. Yoga in the treatment of mood and anxiety disorders: a review. Asian J Psychiatry. 2009;2:6–16. doi:10.1016/j.ajp.2008.12.002. [DOI] [PubMed] [Google Scholar]
- 23. Bernardi L, Wdowczyk-Szulc J, Valenti C, et al. Effects of controlled breathing, mental activity and mental stress with or without verbalization on heart rate variability. J Am Coll Cardiol. 2000;35:1462–1469. [DOI] [PubMed] [Google Scholar]
- 24. Dhruva A, Miaskowski C, Abrams D, et al. Yoga breathing for cancer chemotherapy-associated symptoms and quality of life: results of a pilot randomized controlled trial. J Altern Complement Med. 2012;18:473–479. doi:10.1089/acm.2011.0555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Froeliger B, Garland EL, McClernon FJ. Yoga meditation practitioners exhibit greater gray matter volume and fewer reported cognitive failures: results of a preliminary voxel-based morphometric analysis. Evid Based Complement Alternat Med. 2012;2012:821307 doi:10.1155/2012/821307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Muralikrishnan K, Balakrishnan B, Balasubramanian K, Visnegarawla F. Measurement of the effect of Isha Yoga on cardiac autonomic nervous system using short-term heart rate variability. J Ayurveda Integr Med. 2012;3:91–96. doi:10.4103/0975-9476.96528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Sharma VK, Rajajeyakumar M, Velkumary S, et al. Effect of fast and slow pranayama practice on cognitive functions in healthy volunteers. J Clin Diagn Res. 2014;8:10–13. doi:10.7860/JCDR/2014/7256.3668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Telles S, Yadav A, Kumar N, Sharma S, Visweshwaraiah NK, Balkrishna A. Blood pressure and Purdue pegboard scores in individuals with hypertension after alternate nostril breathing, breath awareness, and no intervention. Med Sci Monit. 2013;19:61–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Satchidananda, Patañjali. The Yoga Sutras of Patanjali. Yogaville, VA: Integral Yoga; 1990. [Google Scholar]
- 30. Selvaraj N, Shivplara N, Bhatia M, Santosh J, Deepak K, Anand S. Heart rate dynamics during Shambhavi Mahamudra—a practice of Isha Yoga. J Complement Integr Med. 2008;5(1). doi:10.2202/1553-3840.1137. [Google Scholar]
- 31. Khalsa MK, Greiner-Ferris JM, Hofmann SG, Khalsa SB. Yoga-enhanced cognitive behavioural therapy (Y-CBT) for anxiety management: a pilot study. Clin Psychol Psychother. 2015;22:364–371. doi:10.1002/cpp.1902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Vorkapic CF, Range B. Reducing the symptomatology of panic disorder: the effects of a yoga program alone and in combination with cognitive-behavioral therapy. Front Psychiatry. 2014;5:177 doi:10.3389/fpsyt.2014.00177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Sinha AN, Deepak D, Gusain VS. Assessment of the effects of pranayama/alternate nostril breathing on the parasympathetic nervous system in young adults. J Clin Diagn Res. 2013;7:821–823. doi:10.7860/JCDR/2013/4750.2948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Lee EH. Review of the psychometric evidence of the perceived stress scale. Asian Nurs Res. 2012;6:121–127. doi:10.1016/j.anr.2012.08.004. [DOI] [PubMed] [Google Scholar]
- 35. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–396. [PubMed] [Google Scholar]
- 36. Cohen S, Williamson G. Perceived stress in a probability sample of the United States In: Spacapam S, Oskamp S, eds. The Social Psychology of Health: Claremont Symposium on Applied Social Psychology. Newbury Park, CA: Sage; 1988:31–67. [Google Scholar]
- 37. Kyrou I, Chrousos GP, Tsigos C. Stress, visceral obesity, and metabolic complications. Ann N Y Acad Sci. 2006;1083:77–110. doi:10.1196/annals.1367.008. [DOI] [PubMed] [Google Scholar]
- 38. McIntyre RS, Park KY, Law CW, et al. The association between conventional antidepressants and the metabolic syndrome: a review of the evidence and clinical implications. CNS Drugs. 2010;24:741–753. doi:10.2165/11533280-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 39. Raison CL, Rutherford RE, Woolwine BJ, et al. A randomized controlled trial of the tumor necrosis factor antagonist infliximab for treatment-resistant depression: the role of baseline inflammatory biomarkers. JAMA Psychiatry. 2013;70:31–41. doi:10.1001/2013.jamapsychiatry.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Balestri M, Calati R, Souery D, et al. Socio-demographic and clinical predictors of treatment resistant depression: a prospective European multicenter study. J Affect Disord. 2016;189:224–232. doi:10.1016/j.jad.2015.09.033. [DOI] [PubMed] [Google Scholar]
- 41. Taylor S, Abramowitz JS, McKay D. Non-adherence and non-response in the treatment of anxiety disorders. J Anxiety Disord. 2012;26:583–589. doi:10.1016/j.janxdis.2012.02.010. [DOI] [PubMed] [Google Scholar]
- 42. Khattab K, Khattab AA, Ortak J, Richardt G, Bonnemeier H. Iyengar yoga increases cardiac parasympathetic nervous modulation among healthy yoga practitioners. Evid Based Complement Alternat Med. 2007;4:511–517. doi:10.1093/ecam/nem087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Hofmann SG, Andreoli G, Carpenter JK, Curtiss J. Effect of hatha yoga on anxiety: a meta-analysis [published online May 20, 2016]. J Evid Based Med. doi:10.1111/jebm.12204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Cahn BR, Goodman MS, Peterson CT, Maturi R, Mills PJ. Yoga, meditation and mind-body health: increased BDNF, cortisol awakening response, and altered inflammatory marker expression after a 3-month yoga and meditation retreat. Front Hum Neurosci. 2017;11:315 doi:10.3389/fnhum.2017.00315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Kirkwood G, Rampes H, Tuffrey V, Richardson J, Pilkington K. Yoga for anxiety: a systematic review of the research evidence. Br J Sports Med. 2005;39:884–891. doi:10.1136/bjsm.2005.018069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Mills PJ, Wilson KL, Pung MA, et al. The self-directed biological transformation initiative and well-being. J Altern Complement Med. 2016;22:627–634. doi:10.1089/acm.2016.0002. [DOI] [PubMed] [Google Scholar]
- 47. Pilkington K, Kirkwood G, Rampes H, Richardson J. Yoga for depression: the research evidence. J Affect Disord. 2005;89:13–24. doi:10.1016/j.jad.2005.08.013. [DOI] [PubMed] [Google Scholar]
- 48. Rod K. Observing the effects of mindfulness-based meditation on anxiety and depression in chronic pain patients. Psychiatr Danub. 2015;27(suppl 1):S209–S211. [PubMed] [Google Scholar]
- 49. Doria S, de Vuono A, Sanlorenzo R, Irtelli F, Mencacci C. Anti-anxiety efficacy of Sudarshan Kriya Yoga in general anxiety disorder: a multicomponent, yoga based, breath intervention program for patients suffering from generalized anxiety disorder with or without comorbidities. J Affect Disord. 2015;184:310–317. doi:10.1016/j.jad.2015.06.011. [DOI] [PubMed] [Google Scholar]
- 50. Kumar N, Bhatnagar S, Velpandian T, et al. Randomized controlled trial in advance stage breast cancer patients for the effectiveness on stress marker and pain through Sudarshan Kriya and pranayam. Indian J Palliat Care. 2013;19:180–185. doi:10.4103/0973-1075.121537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Sharma H, Datta P, Singh A, et al. Gene expression profiling in practitioners of Sudarshan Kriya. J Psychosom Res. 2008;64:213–218. doi:10.1016/j.jpsychores.2007.07.003. [DOI] [PubMed] [Google Scholar]
- 52. Chandra S, Sharma G, Sharma M, Jha D, Mittal AP. Workload regulation by Sudarshan Kriya: an EEG and ECG perspective. Brain Inform. 2008;4:13–25. doi:10.1007/s40708-016-0055-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Subramanian S, Elango T, Malligarjunan H, Kochupillai V, Dayalan H. Role of sudarshan kriya and pranayam on lipid profile and blood cell parameters during exam stress: a randomized controlled trial. Int J Yoga. 2012;5:21–27. doi:10.4103/0973-6131.91702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Voroshilov AP, Volinsky AA, Wang Z, Marchenko EV. Modified qigong breathing exercise for reducing the sense of hunger on an empty stomach. J Evid Based Complementary Altern Med. 2017;22(4):687–695. doi:10.1177/2156587217707143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Brown RP, Gerbarg PL. Sudarshan Kriya yogic breathing in the treatment of stress, anxiety, and depression. Part II—clinical applications and guidelines. J Altern Complement Med. 2005;11:711–717. doi:10.1089/acm.2005.11.711. [DOI] [PubMed] [Google Scholar]
- 56. Brown RP, Gerbarg PL. Sudarshan Kriya yogic breathing in the treatment of stress, anxiety, and depression: Part I—neurophysiologic model. J Altern Complement Med. 2005;11:189–201. doi:10.1089/acm.2005.11.189. [DOI] [PubMed] [Google Scholar]
- 57. Jerath R, Edry JW, Barnes VA, Jerath V. Physiology of long pranayamic breathing: neural respiratory elements may provide a mechanism that explains how slow deep breathing shifts the autonomic nervous system. Med Hypotheses. 2006;67:566–571. doi:10.1016/j.mehy.2006.02.042. [DOI] [PubMed] [Google Scholar]
- 58. Madanmohan Udupa K, Bhavanani AB, Vijayalakshmi P, Surendiran A. Effect of slow and fast pranayams on reaction time and cardiorespiratory variables. Indian J Physiol Pharmacol. 2005;49:313–318. [PubMed] [Google Scholar]
- 59. Sharma VK, Trakroo M, Subramaniam V, Rajajeyakumar M, Bhavanani AB, Sahai A. Effect of fast and slow pranayama on perceived stress and cardiovascular parameters in young health-care students. Int J Yoga. 2013;6:104–110. doi:10.4103/0973-6131.113400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Ohman L, Nordin S, Bergdahl J, Slunga Birgander L, Stigsdotter Neely A. Cognitive function in outpatients with perceived chronic stress. Scand J Work Environ Health. 2007;33:223–232. [DOI] [PubMed] [Google Scholar]
- 61. Nivethitha L, Mooventhan A, Manjunath NK. Effects of various pranayama on cardiovascular and autonomic variables. Anc Sci Life. 2016;36:72–77. doi:10.4103/asl.ASL_178_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Berthoud HR, Neuhuber WL. Functional and chemical anatomy of the afferent vagal system. Autonom Neurosci. 2000;85:1–17. [DOI] [PubMed] [Google Scholar]
- 63. Montiel-Castro AJ, Gonzalez-Cervantes RM, Bravo-Ruiseco G, Pacheco-Lopez G. The microbiota-gut-brain axis: neurobehavioral correlates, health and sociality. Front Integr Neurosci. 2013;7:70 doi:10.3389/fnint.2013.00070. [DOI] [PMC free article] [PubMed] [Google Scholar]


