Abstract
Inflammation is a complex biological response fundamental to how the body deals with injury and infection to eliminate the initial cause of cell injury and effect repair. Unlike a normally beneficial acute inflammatory response, chronic inflammation can lead to tissue damage and ultimately its destruction, and often results from an inappropriate immune response. Inflammation in the nervous system (“neuroinflammation”), especially when prolonged, can be particularly injurious. While inflammation per se may not cause disease, it contributes importantly to disease pathogenesis across both the peripheral (neuropathic pain, fibromyalgia) and central [e.g., Alzheimer disease, Parkinson disease, multiple sclerosis, motor neuron disease, ischemia and traumatic brain injury, depression, and autism spectrum disorder] nervous systems. The existence of extensive lines of communication between the nervous system and immune system represents a fundamental principle underlying neuroinflammation. Immune cell-derived inflammatory molecules are critical for regulation of host responses to inflammation. Although these mediators can originate from various non-neuronal cells, important sources in the above neuropathologies appear to be microglia and mast cells, together with astrocytes and possibly also oligodendrocytes. Understanding neuroinflammation also requires an appreciation that non-neuronal cell—cell interactions, between both glia and mast cells and glia themselves, are an integral part of the inflammation process. Within this context the mast cell occupies a key niche in orchestrating the inflammatory process, from initiation to prolongation. This review will describe the current state of knowledge concerning the biology of neuroinflammation, emphasizing mast cell-glia and glia-glia interactions, then conclude with a consideration of how a cell's endogenous mechanisms might be leveraged to provide a therapeutic strategy to target neuroinflammation.
Keywords: inflammation, mast cells, microglia, astrocytes, oligodendrocytes, neuro-immune, crosstalk, palmitoylethanolamide
Introduction
Inflammation is a response triggered by damage to living tissues. To quote from Encyclopædia Britannica, Inc., “The inflammatory response is a defense mechanism that evolved in higher organisms to protect them from infection and injury. Its purpose is to localize and eliminate the injurious agent and to remove damaged tissue components so that the body can begin to heal.” An inflammatory response can be either acute (seconds to hours) or a response of longer duration referred to as chronic inflammation. The former is usually beneficial, while the latter may result in tissue destruction caused, for example, when regulatory mechanisms of the inflammatory response are defective or when there is an inappropriate immune response with consequent prolonged and damaging inflammation (Castellheim et al., 2009). As succinctly stated by Nathan and Ding (2010), “the core problem with inflammation is not how often it starts, but how often it fails to subside.” Non-resolving inflammation, without doubt, contributes to the overall medical burden in our society, and is now viewed as a new therapeutic frontier (Fullerton and Gilroy, 2016). Inflammation can be especially perilous where the nervous system is involved (so-called “neuroinflammation”), whether it be of an acute nature or chronic—the latter involving sustained activation of glia and recruitment of immune elements. This phenomenon is recognized as a cardinal element in the pathogenesis of both peripheral nervous system conditions like neuropathic pain and other disorders with chronic pain (Myers et al., 2006; Kim et al., 2007; Ellis and Bennett, 2014; Martini and Willison, 2016), and acute (Iadecola and Anrather, 2011) as well as chronic (McGeer and McGeer, 2013; Freeman and Ting, 2016; Ransohoff, 2016a) central nervous system (CNS) diseases, including mood disorders (Najjar et al., 2013; Castanon et al., 2015; Theoharides et al., 2015a; Calcia et al., 2016; Calsolaro and Edison, 2016; Wohleb et al., 2016) and autism (Noriega and Savelkoul, 2014; Theoharides et al., 2016).
Once thought to be immune-privileged, the CNS now enjoys extensive communication links with the immune system. Indeed, were it not for such interactions it is unlikely that neuroinflammation would occur. Immune cell-derived pro-inflammatory mediators play a key role by regulating host responses to infection, inflammation, and reactions to stress or trauma (Le Thuc et al., 2015; Piirainen et al., 2017). While these inflammatory molecules may originate from a number of non-neuronal cell populations, a large body of evidence points to microglia (the brain's main immune guardians) and mast cells, along with astrocytes (and possibly even oligodendrocytes) as important sources of such agents in the above pathologies (Thacker et al., 2007; Appel et al., 2011; Cunningham, 2013; Silver and Curley, 2013; Amor and Woodroofe, 2014; Harcha et al., 2015; Dong et al., 2017; Kempuraj et al., 2017; Skaper et al., 2017; Spangenberg and Green, 2017; Balducci and Forloni, 2018; Simon et al., 2018). Given the complex nature of cellular involvement in inflammation-associated pathologies across the central and peripheral nervous systems, viewing neuroinflammation in the context of microglia (Masgrau et al., 2017), astrocyte or mast cell involvement alone fails to fully appreciate the homotypic and heterotypic cell—cell interactions that are an integral part of the inflammation process. This review is intended to describe recent contributions in our understanding of the biology and cellular signaling mechanisms of inflammation as it affects the nervous system, with emphasis on a mast cell-glia (microglia, astrocyte, oligodendrocyte) interactions. This will be followed by a consideration of approaches to counteract neuroinflammation that capitalize on natural defense mechanisms and lipid signaling molecules.
Glia
Among the cell types that participate in inflammation of the nervous system, tissue-resident and blood-borne glia and immune system-derived cells comprise key elements. Microglia are the principal immune effector cells of the brain, constantly surveying their environment in preparation for insult or injury (“immunosurveillance”). When activated, they phagocytose cellular debris, present antigens to T cells and release cytokines/chemokines, the latter providing cells with the ability to communicate with one another and orchestrate complex multicellular behavior (Becher et al., 2017). In homeostatic terms, microglia regulate cell death and neurogenesis, and actively engulf synaptic material and play a major role in synaptic pruning during postnatal development, thereby linking microglia surveillance to synaptic maturation (Paolicelli et al., 2011). This synaptic pruning is dependent upon neural activity and the microglia-specific phagocytic signaling pathway, complement receptor 3/C3 (Schafer et al., 2012). Interestingly, this normal developmental synaptic pruning pathway appears to be activated early in the Alzheimer disease (AD) brain and mediates synapse loss (Hong et al., 2016). Yet another role for microglia in CNS development comes from a new study describing a unique phenotype of neonatal (CD11c+) microglia in primary myelinating areas of the developing brain that deliver signals necessary for myelination and neurogenesis (Wlodarczyk et al., 2017).
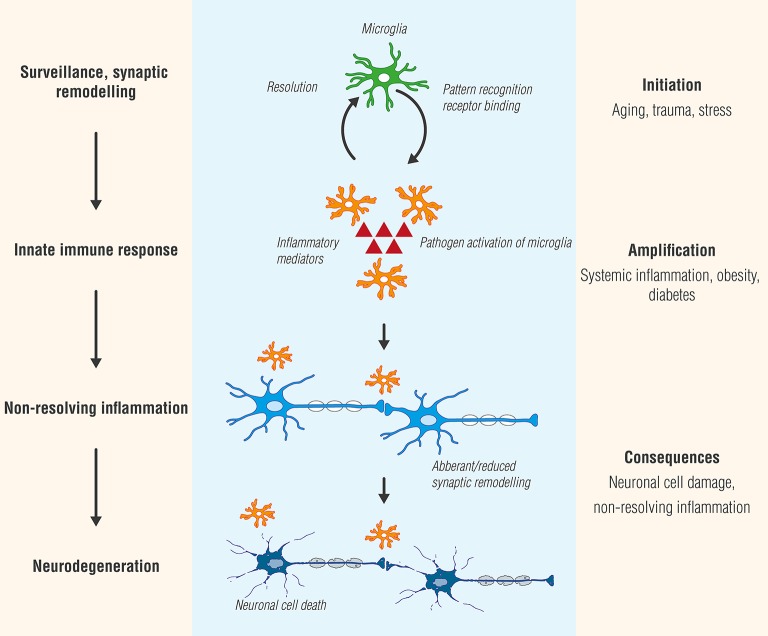
Microglia plasticity is complex, and activation states have generally been classified into two functional subtypes: M1 (classic/pro-inflammatory) and M2 (alternative polarization/neuroprotective) (Tang and Le, 2016). While providing a framework for exploring the diverse functions of microglia, this terminology has been questioned (Ransohoff, 2016b). At least in the case of experimental autoimmune encephalomyelitis (EAE), a widely utilized animal model of MS, inhibiting inflammatory agent secretion by microglia reduces disease severity, while transplanting M2 polarized microglia into the CNS facilitated recovery (Miron et al., 2013; Zhang et al., 2014). Studies by Peferoen et al. (2014) indicate that microglia express an intermediate activation status in all pre- active and remyelinating MS lesions and distinct from microglia profiles in actively demyelinating lesions, thus supporting the view that activation status of microglia is a dynamic process which occurs as a continuum across the M1 and M2 phenotypes. Microglial cell progression from beneficial to detrimental is schematically portrayed in Figure 1.
Figure 1.
Microglia, like Janus, the two-faced Roman god of beginnings and transitions, display two sides—physiological as well as pathological. While microglial cell activation participates in surveillance that functions to maintain homeostasis and promote synaptic maturation, prolonged exposure to pathogen activators or in settings of systemic inflammation, as may occur in conditions such as diabetes or obesity, can culminate in a state of chronic, non-resolving neuroinflammation. Ultimately, these responses will provoke functional and structural changes and neuronal cell death (neurodegeneration).
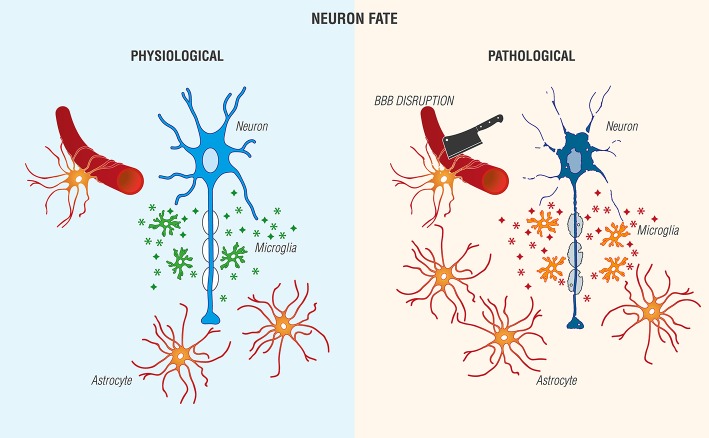
Astrocytes, the most abundant cell type in the CNS and historically viewed as “brain glue,” participate in a number of critical physiological functions, including maintaining blood-brain barrier (BBB) integrity by forming astrocytic end feet around endothelial cells, regulation of axonal outgrowth and myelination (Kiray et al., 2016), and formation of intracellular communication networks, e.g., signaling via Ca2+ release and uptake (Volterra and Meldolesi, 2005; Kimelberg and Nedergaard, 2010). Injury leads to an increase in astrocyte reactivity (Sofroniew and Vinters, 2010) with changes in morphology, increased expression of glial fibrillary acidic protein, proliferation and secretion of pro-inflammatory molecules and growth factors (Jensen et al., 2013; Pekny et al., 2016). Further, these factors may exert autocrine/paracrine actions to promote astrocytic reactivity and impact neighboring cells. Astrocyte-microglia interactions are also possible (Figure 2).
Figure 2.
Reciprocal interactions between microglia and astrocytes provoke beneficial and harmful effects in the brain. (Left) Physiological actions include microglia phagocytosis/debris clearance, release of anti-inflammatory cytokines/chemokines ( ), and trophic agents to favor neuronal cell survival. (Right) Non-resolving neuroinflammation results in a pathological, pro-inflammatory activation profile of microglia/mediator production (
), and trophic agents to favor neuronal cell survival. (Right) Non-resolving neuroinflammation results in a pathological, pro-inflammatory activation profile of microglia/mediator production ( ), blood-brain barrier (BBB) compromise, immune cell infiltration, gliosis, and neuronal cell death [Adapted and extensively modified from Le Thuc et al. (2015). The complex contribution of chemokines to neuroinflammation: switching from beneficial to detrimental effects (Figure 3). Copyright © 2015 John Wiley and Sons. With permission].
), blood-brain barrier (BBB) compromise, immune cell infiltration, gliosis, and neuronal cell death [Adapted and extensively modified from Le Thuc et al. (2015). The complex contribution of chemokines to neuroinflammation: switching from beneficial to detrimental effects (Figure 3). Copyright © 2015 John Wiley and Sons. With permission].
Oligodendrocytes (OLs) are responsible for myelin production in the CNS, and are generated in the germinal zone from migratory bipolar oligodendrocyte precursor cells (OPCs; Grinspan, 2002). Myelinating OLs not only provide trophic support for axons, but also release lactate through the monocarboxylate transporter 1 which is then utilized by axons for mitochondrial ATP generation (Saab et al., 2013). The migration of OPCs is influenced by receptor-ligand adhesions with the extracellular matrix, such as integrins, and signaling molecules (Soliven, 2001) which may provide a critical link between neuronal cell activity and OPCs. Cells of the OL lineage acquire cell surface markers with maturation and respond specifically to factors which regulate proliferation, migration, differentiation, and survival. Moreover, cells of the OL lineage express and respond to a broad range of receptor-ligand pairs, including glutamic acid, γ-aminobutyric acid, ATP, serotonin, acetylcholine, nitric oxide, opioids, prostaglandins, prolactin, cannabinoids, and nuclear receptors (Marinelli et al., 2016). While known for their ability to support axonal functions and long-term integrity (Nave, 2010), OLs participate also in neuropathology, as will be discussed in later sections.
Mast cells
Glial cell participation in inflammation-associated neuropathologies encompasses not only their inflammatory signals, but also their response to mediators produced by other immune system-derived cells, both blood-borne (dendritic cells, lymphocytes, neutrophils), and tissue-resident (mast cells). While receiving comparably less attention than glia, the mast cell nonetheless represents an important peripheral immune signaling link to the brain in an inflammatory setting. Mast cells share a relationship with basophils but have a distinct haematopoietic lineage development, leaving the circulation to enter peripheral tissues where the local environment determines protease phenotype expression packaged in cytoplasmic granules; these also contain histamine and heparin (Table 1; Prussin and Metcalfe, 2003). As a major sensory arm of the body's innate immune system, mast cells function as environmental “sensors” to communicate with other elements in physiological and/or immune responses thanks to their widespread tissue presence near blood vessels and surfaces exposed to the environment (Gilfillan et al., 2011). These immune effector cells are found in tissues innervated by small caliber sensory nerve fibers (A-delta and C-fibers responsible for pain transmission that extend from the periphery to the spinal cord and brain), in meninges, and apposing cerebral blood vessels. Upon activation, mast cells secrete “packaged” or synthesized de novo, numerous vasoactive, neurosensitizing and pro-inflammatory mediators, which include biogenic amines (histamine, serotonin), cytokines, proteolytic enzymes (e.g., chymase, tryptase, acid hydrolases, among others), lipid metabolites (prostaglandin D2, leukotriene C4, platelet-activating factor), ATP, neuropeptides, nerve growth factor (NGF), vascular endothelial growth factor and nitric oxide (Kalesnikoff and Galli, 2008; Silver and Curley, 2013). While more than 50 mediators are known to date, their expression by mast cells is heterogeneous and determined to a large extent by species and tissue location. Additionally, mast cell-derived chemoattractants recruit eosinophils (Wardlaw et al., 1986), monocytes, and neutrophils (Wezel et al., 2015).
Table 1.
Mast cells: a primer.
| Origin and classification: |
|---|
| • First description in 1878, noted for their staining characteristics and abundant cytoplasmic granules • Share some characteristics with circulating basophil granulocytes; thought to arise from distinct bone marrow precursor cells expressing CD34 • Unique hematopoietic lineage development in comparison to other myeloid-derived cells: immature lineage mast cells leave the bone marrow to enter the circulation and immediately undergo transendothelial recruitment into peripheral tissues where formation of secretory granules with a particular protease phenotype is regulated by the peripheral tissue. • Mast cell types are generally divided into connective tissue cells and a distinct set, mucosal mast cells (whose activities are dependent on T-cells) • Broad tissue distribution, often close to blood vessels and prominent near boundaries between the body's external environment and the internal milieu, such as skin, mucosa of lungs and digestive tract, and in mouth, conjunctiva, and nose • Mast cells also found in the nervous system, including meninges, brain parenchyma, and nerve endoneurium |
| Physiology: |
| • Play a key role in the inflammatory process • Upon activation rapidly release mediator-loaded granules into the interstitium • Degranulation is caused by direct injury (e.g., physical or chemical), cross-linking of IgE receptors or by activated complement proteins • Elaborate a vast array of important cytokines and other inflammatory mediators • Express multiple “pattern recognition receptors” (e.g., Toll-like receptors) involved in recognizing broad classes of pathogens • Granules loaded with a plethora of bioactive chemicals, proteoglycans, serine proteases, neuropeptides, and growth factors; can be transferred to nearby immune cells and neurons via transgranulation and their pseudopodia |
| Disease involvement: |
| • Allergic reactions • Anaphylactic shock • Inflammatory pain, chronic (including neuropathic) pain • Acute and chronic neurodegenerative disorders • Mood disorders |
As antigen-presenting cells, mast cells can induce T cell activation, proliferation, and cytokine secretion (Bulfone-Paus and Bahri, 2015). Indeed, the capability of mast cells to present antigens by class I and II major histocompatibility complex molecules, respective, to CD4+ and CD8+ T cells constitutes a major antigen-dependent interaction between mast cells and T cells—the so-called immunological synapse (Monks et al., 1998; Grakoui et al., 1999; Suurmond et al., 2013), and depends on cytoskeletal control of receptor triggering (Comrie and Burkhardt, 2016). Optimal activation of antigen-specific T cells requires interaction between CD28 on T cells and CD86/CD80 on mast cells. Additional interaction between mast cell OX40L and T cell OX40—together with mast cell-derived tumor necrosis factor-α (TNF-α)–promotes antigen-stimulated mast cell enhancement of T cell activation (Nakae et al., 2006) while polarizing T cell secretory machinery toward the mast cell (Gaudenzio et al., 2009). It is not surprising, thus, to see mast cell involvement in T cell-associated immune responses such as EAE (Elieh Ali Komi and Grauwet, 2017).
Neuroinflammation is amplified by mast cell—glia and glia—glia crosstalk
The contribution of mast cells and glia to neuroinflammation is strongly influenced by their potential for mutual interaction and exacerbation of pathology. These cell types are often found in close proximity to each other, facilitating cell-cell communication. Further, ligand-receptor pairings, whose expression may be up-regulated in inflammatory tissues, can facilitate chemotactic actions to bring mast cells and glia in closer contact. Indeed, recruitment and activation of these immune cell populations in a defined temporal pattern necessitates a reciprocal communication between them. Some examples are briefly discussed below.
The complement system appears to play a role in crosstalk between mast cells, microglia, and astrocytes. For example, microglia (and astrocytes) showed up-regulation of the chemoattractant anaphylatoxin peptide C5a and its receptor CD88 in inflamed CNS tissues (Gasque et al., 1997). Complementary expression of C5a receptor on activated mast cells provides a strong chemoattractant signal toward C5a peptide (Pundir et al., 2015). The C5a-C5a receptor pathway plays a vital role in brain inflammatory injury, including intracerebral hemorrhage (Young et al., 2013; Yuan et al., 2017). In the context of AD, the central complement factor C3 secreted from astrocytes interacts with microglial C3a receptor to mediate β-amyloid pathology and neuroinflammation in AD mouse models (Lian et al., 2015, 2016). Neuronal cell overproduction of Aβ activates astroglial nuclear factor-κB (NF-κB) to elicit extracellular release of C3.
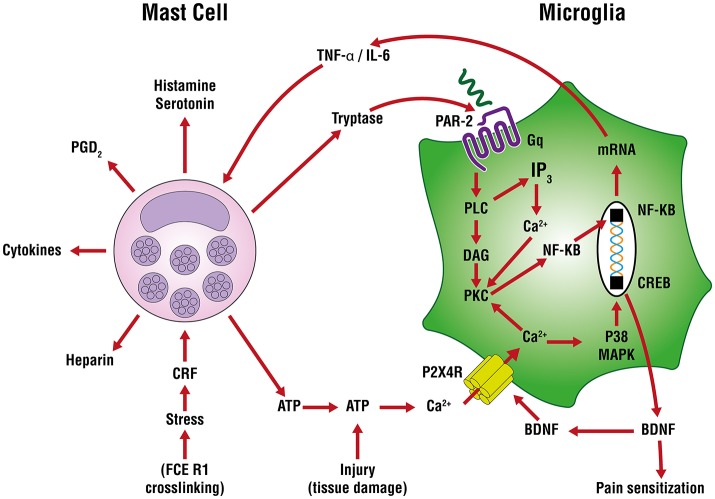
In neuropathic (and other forms of chronic pain) pain, plastic changes in dorsal horn neurons contribute to a phenomenon of hypersensitivity to pain sensation that is maintained over time, known as central sensitization (Constandil et al., 2011). The neurotrophin brain-derived neurotrophic factor (BDNF) is a crucial neuromodulator involved in nociceptive hypersensitivity in the CNS (Coull et al., 2005; Khan and Smith, 2015). BDNF generates a long-lasting neural excitability change in the spinal cord via tyrosine kinase B receptor signaling, similar to that observed in chronic pain models such as neuropathy (Constandil et al., 2011). Peripheral nerve injury up-regulates the purinergic P2X4 receptor in microglia of the sensory part of the spinal cord (Beggs et al., 2012) to mediate BDNF release and neuropathic pain (Ulmann et al., 2008). An important signaling pathway in the development of neuropathic pain is extracellularly-derived ATP, a ubiquitous danger signal released from damaged cells which engages P2 purinoceptors on target cells (Burnstock, 2016). ATP is a potent stimulus for microglia, as well. Distinct P2 receptor subtypes are expressed on mast cells as a function of species and source from which mast calls are derived (Bulanova and Bulfone-Paus, 2010). ATP has a rather large “footprint” and, once released from a mast cell (e.g., FcεR1 cross-linking, stress) can diffuse several hundred micrometers to act on in neighboring cells, including other mast cells as an autocrine/paracrine factor (Osipchuk and Cahalan, 1992). ATP-induced BDNF expression and release is mediated by the P2X4 receptor (Klein et al., 2012) through a mechanism involving Ca2+ entry, induction of Ca2+/inositol 1,4,5-trisphosphate/PKC signaling, phosphorylation of IKKα and IKKβ and activation and nuclear translocation of NF-κB and gene induction (Trang et al., 2009; Figure 3). Another route by which P2X4 receptor acts to release BDNF involves mast cell tryptase cleavage of microglial protease-activated receptor 2 (PAR2) which couples to G proteins and induces canonical phospholipase C/Ca2+/protein kinase C signaling that leads to the activation and nuclear translocation of NF-κB and gene induction (Yuan et al., 2010; Sakamoto et al., 2016; Figure 3). Microglia, by releasing pro-inflammatory cytokines like TNF-α and interleukin-6 (IL-6), amplify mast cell activation/degranulation and numbers (Zhang et al., 2011). An additional mast cell-microglia feedback loop, again linked to ATP, invokes its binding to P2 receptors to stimulate release of IL-33 from microglia pre-activated with pathogen-associated molecular patterns (PAMPs) acting on Toll-like receptors (TLRs), thereby inducing mast cell secretion of IL-6, IL-13, and CCL2 which then modulate microglia activity.
Figure 3.
Mast cell—microglia crosstalk in the release of brain-derived neurotrophic factor (BDNF). ATP-induced BDNF expression and release is mediated by the P2X4 receptor through a mechanism involving Ca2+ entry, induction of Ca2+/inositol 1,4,5-trisphosphate/PKC signaling, phosphorylation of IKKα and IKKβ and activation and nuclear translocation of nuclear factor-κB (NF-κB) and gene induction The purinergic P2X4 receptor acts to release BDNF via mast cell tryptase cleavage/activation of protease-activated receptor 2 (PAR2) on microglia which couples to G proteins and induces canonical phospholipase C (PLC)/Ca2+/protein kinase C (PKC) signaling, activation and nuclear translocation of NF-κB, culminating in BDNF gene induction and translation. The latter cells release tumor necrosis factor-α (TNF-α) and interleukin-6 (IL-6) which can further drive mast cell activation and degranulation and numbers, leading to a potential feedback loop between mast cells and microglia.
Cytokines released following binding of PAMPs to TLR2/TLR4 on mast cells recruits immune cells (e.g., microglia) to the sites of injury that is dependent on signaling pathways involving TLR2/TLR4 (Pietrzak et al., 2011). Further, mast cell activation up-regulates chemokine expression (including CCL5/RANTES); the latter molecules are capable of inducing a pro-inflammatory response in microglia. Microglia-derived IL-6 and CCL5 may, in turn, influence mast cell expression of TLR2/TLR4.
Activation of antigen-presenting cells, including mast cells, requires the co-stimulatory protein CD40 for binding to CD40L. A CD40-CD40L interaction has been described between mast cells and astrocytes which induces cytokine and chemokine production via Rho-family GTPases/Ca2+-dependent protein kinase C isoforms, mitogen-activated protein kinases, NF-κB, and signal transducer and activator of transcription 1 (Kim et al., 2011). These authors observed also a feedback action of the released cytokines on astrocytes to bring about their re-activation. Additional microglia—astrocyte interactions have been demonstrated at the level of translocator protein, a marker of gliosis in neurodegeneration (Wang et al., 2014) and in terms of their ability to exercise a reciprocal interaction through release of pro-inflammatory cytokines/chemokines (Le Thuc et al., 2015). Moreover, several investigators have proposed a crosstalk between oligodendrocytes and microglia involving exosomes—small vesicles containing proteins, lipids, and regulatory RNAs thought to provide a means of intercellular communication and of transmission of macromolecules between cells via membrane vesicle trafficking, thereby influencing the immune system (Peferoen et al., 2014) (Table 2).
Table 2.
Avenues of mast cell—glia and glia—glia communication.
| Biological actions | |||
|---|---|---|---|
| Effector | Microglia/Astrocytes/Oligodendrocytes | Mast cells | References |
| C5a receptor (C5aR) | C5aR up-regulated by microglia activation; C5a peptide released in neuroinflammation; crosstalk between C5a and TLR4 | C5aR up-regulated by activation; strong mast cell chemoattractant signal toward C5a peptide; crosstalk between C5a and TLR4 | Gasque et al., 1997; Griffin et al., 2007; Soruri et al., 2008; Yuan et al., 2017 |
| C3 and C3 receptor (C3aR) | Astrocyte C3 interacts with microglial C3aR to mediate Aβ pathology and neuroinflammation | Lian et al., 2015, 2016 | |
| ATP/P2 receptors | ATP stimulates IL-33 release from microglia pre-activated with pathogen-associate molecular patterns via TLRs | IL-33 binds to mast cell receptor to induce secretion of IL-6, IL-13 and monocyte chemoattractant protein 1 which modulate microglial cell activity | Osipchuk and Cahalan, 1992; Burnstock, 2016 |
| Proteinase-activated receptor 2 (PAR2) | Mast cell tryptase cleaves/activates PAR2 on microglia, resulting in P2X4 receptor up-regulation and release of brain-derived neurotrophic factor | Microglial cell IL-6 and TNF-α up-regulate mast cell expression of PAR2, with mast cell activation and TNF-α release | Osipchuk and Cahalan, 1992; Yuan et al., 2010; Zhang et al., 2010 |
| TLR2, TLR4 | Microglial cell-derived IL-6 and CCL5 affect mast cell expression of TLR2/TLR4 | Up-regulation of cytokine/chemokine release; CCL5/RANTES induces pro-inflammatory profile in microglia; recruitment of immune cells (including mast cells) to site(s) of injury | Orinska et al., 2005; Tanga et al., 2005; Kim et al., 2007; Buchanan et al., 2010; Pietrzak et al., 2011; Skuljec et al., 2011; Liu et al., 2012 |
| CXCR4/CXCL12 | Promotion of microglia migration/activation; CXCR4/CXCL12 up-regulated in hypoxia/ischemia | CXCR4 is a mast cell chemotaxin | Juremalm et al., 2000; Yang et al., 2010; Knerlich-Lukoschus et al., 2011 |
| CD40/CD40L | CD40 up-regulated on activated astrocytes; crosstalk with CD40L leads to production of inflammatory cytokines/chemokines trigger mast cell degranulation | CD40L expression enhanced in activated mast cells; crosstalk with CD40 leads to production of inflammatory cytokines | Kim et al., 2011 |
| IL-33 | Released by oligodendrocytes in neuropathic pain | IL-33 binds to mast cell receptor to induce secretion of TNF-α which up-regulates oligodendrocyte expression of acute phase proteins | Zarpelon et al., 2016; Barbierato et al., 2017 |
| Serum amyloid A (SAA) | Up-regulated by inflammatory cytokines released from glia, mast cells; localized to amyloid β-peptide deposits | SAA is an attractant for mast cells; mast cell-derived cytokines (e.g., TNF-α can uo-regulate SAA expression by glia | Nelson et al., 1993; Olsson et al., 1999; Barbierato et al., 2017 |
| Translocator protein (TSPO) | Retinal inflammation/injury leads to TSPO up-regulation in retinal microglia; TSPO endogenous ligand diazepam-binding inhibitor (DBI) up-regulated in microglia; DBI-TSPO signaling promotes microglia-microglia interactions | Wang et al., 2014 | |
| Cytokines/chemokines (e.g., CCL2) | Reciprocal interactions between microglia and astrocytes | Le Thuc et al., 2015; Xu et al., 2017 | |
| Exosomes | Participate in oligodendrocyte—microglia crosstalk | Peferoen et al., 2014 | |
| IL-18/IL-18 receptor | Nerve injury increases expression of IL-18 in microglia and IL-18R in astrocytes; IL-18 induces astrocytic hypertrophy and release of IL-1β, IL-6, TNF-α | Miyoshi et al., 2008 | |
IL, interleukin; TLR, Toll-like receptor; TNF-α, tumor necrosis factor-α.
Inflammation and neurological disorders
Alzheimer disease
Alzheimer disease is the most prevalent chronic, progressive neurodegenerative disease, and cause of dementia (Selkoe and Hardy, 2016). Principal pathological features are the presence in brain of focal extracellular deposits (senile plaques) of fibrillar amyloid β-peptide (Aβ) and intracellular neurofibrillary tangles composed of hyperphosphorylated tau protein (Selkoe, 2011). The amyloid hypothesis of AD was initially based on the idea that pathogenesis starts with amyloid deposition as senile plaques, although this view has shifted to AD as a disease in which soluble oligomeric forms of Aβ impair synaptic plasticity and behavior (Selkoe, 2008). Disease pathogenesis involves also interactions with immunological mechanisms in the brain. Regional inflammatory responses occur in AD brain with deposits of Aβ as foci, with elevated expression of pro-inflammatory cytokines, acute phase proteins, and complement components (Cameron and Landreth, 2010; Calsolaro and Edison, 2016), along with signs of activated microglia and reactive astrocytes (Wyss-Coray, 2006; Medeiros and LaFerla, 2013; Regen et al., 2017; Balducci and Forloni, 2018). Post-mortem AD brain samples and those of mouse transgenic models of AD bearing deposits of insoluble Aβ display alterations in microglia and astrocytes (Parvathenani et al., 2003; Heneka et al., 2015); Aβ plaques in the frontal cortex of AD brain are surrounded by IL-1β-positive microglia (Heuberger, 2011). Amyloid precursor protein, from which Aβ peptides derive reportedly regulates microglial phenotype (Manocha et al., 2016). In AD brain, activated microglia may phagocytose toxic Aβ and produce survival-promoting trophic factors (Rivest, 2009); however, if prolonged such activation can result in the elaboration of synaptotoxic/neurotoxic cytokines, chemokines, and reactive oxygen/nitrogen species (Wyss-Coray, 2006; Rivest, 2009; Balducci and Forloni, 2018; Simon et al., 2018). Indeed, Biscaro et al. (2012) using a transgenic mouse AD model demonstrated that inhibition of microglial activation protects hippocampal neurogenesis and improves cognitive deficits.
Recent studies have defined a complement-dependent intercellular cross talk whereby Aβ overproduction by neurons activates astroglial cell NF-κB to elicit release of C3 (Lian et al., 2015, 2016). The released C3, in turn, interacts with neuronal and microglial cell C3a receptor (C3aR) to alter cognitive function and impair Aβ phagocytosis—in effect, promoting a pathogenic cycle. Abnormal activation of NF-κB has been implicated in AD (Kaltschmidt et al., 1997), and Lian et al. (2015) showed that exposure to Aβ activates astroglial NF-κB and C3 release.
A role for mast cells in AD disease onset/progression is less well-established. Tryptase-positive mast cells were found in proximity to Aβ plaques in post-mortem AD brain (Maslinska et al., 2007), and fibrillar Aβ was reported to cause CD47-dependent mast cell secretory and phagocytic responses (Niederhoffer et al., 2009). In a more recent study, Harcha et al. (2015) showed that acute treatment of brain mast cells with the 25–35 amino acid fragment of Aβ activates Panx1 and Cx43 hemichannels, accompanied by increases in Ca2+ influx, degranulation, and histamine release. These authors also found raised Panx1 and Cx43 hemichannel activity in a transgenic mouse AD model along with greater mast cell numbers in cortex and hippocampus prior to Aβ plaque formation. Acute phase proteins like serum amyloid A (SAA) are produced in response to inflammation. SAA immunoreactivity co-localized with Aβ deposits in AD brain (Kindy et al., 1999), and SAA concentration was much higher in cerebrospinal fluid (CSF) of AD subjects than in normal controls (Miida et al., 2006). A new study by Barbierato et al. (2017) shows that inflammatory stimuli up-regulate expression of SAA1 by CNS glia—including oligodendrocytes—providing an attractant for mast cells and promoting movement toward Aβ deposits (Nelson et al., 1993; Olsson et al., 1999). The data propose a potential for paracrine/autocrine effects between these cell types. Moreover, Harcha et al. (2015) suggest that mast cells are among the first brain cells to sense Aβ peptides and thus may play a critical role in the onset and progression of AD. Masitinib, a potent and selective oral protein tyrosine kinase inhibitor targeting c-Kit (the receptor for the mast cell growth factor stem cell factor; Dubreuil et al., 2009) that inhibits the survival, migration and activity of mast cells, when administered as add-on therapy to AD patients receiving standard care during 24 weeks was associated with slower cognitive decline (Piette et al., 2011). It is currently in Phase II/III clinical trials for the treatment AD (Folch et al., 2015).
Neuroendocrine and behavioral changes accompanying the stress response can affect homeostasis, over the long term, in terms of detrimental effects such as impairing neuronal cell metabolism, plasticity, and survival. Stress-induced hormonal and behavioral reactions may also indirectly induce neuropathological processes participating in the development and progression of AD (Mravec et al., 2018), in part through mast cell-mediated BBB breakdown (Esposito et al., 2001). Indeed, chronic stress reportedly accelerates AD pathogenesis in human and animal models through increases in inflammatory responses, Aβ accumulation, tau hyperphosphorylation, oxidative stress, mitochondrial impairment, and glucose metabolism (Machado et al., 2014), while early-life stress increases the risk of cognitive disorders in an aged mouse model of AD (Hoeijmakers et al., 2017). Mast cell activation plays a crucial role in stress-dependent inflammatory mechanisms. Human mast cells synthesize and secrete corticotropin releasing hormone (CRH) and express functional CRH receptors (Cao et al., 2005). CRH released from mast cells can act in an autocrine/paracrine manner to activate mast cells and microglia in stress and neuroinflammatory conditions (Karagkouni et al., 2013; Kritas et al., 2014a). Chronic psychological stress is a risk factor for dementia and AD by inducing microglial proinflammatory status (Piirainen et al., 2017) and, conceivably, a crosstalk loop between the former cells and mast cells. These observations propose that mast cells play a crucial role in stress responses associated with inflammation that may predispose to AD pathogenesis in high-risk groups.
Parkinson disease
Parkinson disease (PD) is the first and second most prevalent motor and neurodegenerative disease, respectively (Hirsch et al., 2016). Pathological hallmarks of PD are the progressive death of dopaminergic neurons in the substantia nigra pars compacta and intracellular accumulation of Lewy bodies enriched in α-synuclein protein (Shulman et al., 2011). In addition to motor defects, clinical features of PD comprise non-motor symptoms that become increasingly prevalent during the course of the disease. Although PD is a complex, multisystem disorder, neuroinflammatory responses, and neuroinflammation appear to exacerbate PD pathogenesis (Stojkovska et al., 2015; Wang et al., 2015). A number of studies suggest that microglial cell activation may have a role in PD. For example, Zhang et al. (2017) reported that pathological α-synuclein exacerbates progression of PD through microglial activation via the transcription factor NF-κB and expression of pro-inflammatory cytokines such as TNF-α and IL-1β. Further, expression of major histocompatibility complex II by microglia is needed for activation of these cells by α-synuclein, which can play a role in immune responses (Harms et al., 2013). A number of gene defects have been identified in familial forms of PD, the most commonly mutated gene being that for leucine-rich repeat kinase 2, whose pathogenic mutations influence the ability of microglia to internalize and degrade α-synuclein—thereby exacerbating α-synuclein-induced microglial pathology and neuroinflammation (Recchia et al., 2004; Schapansky et al., 2015). Immunomodulator dysregulation increases microglial activation and the degeneration of dopamine neurons (Zhang et al., 2011). Dopaminergic neurons are especially sensitive to injury by pro-oxidant species, and whose activation of microglia in PD can lead to degeneration of dopaminergic cells (Appel et al., 2010; Herrera et al., 2015).
A role that mast cells may play in PD pathogenesis is, until now, largely lacking. However, recent reports by Kempuraj et al. (2016, 2018) showed that incubation of mouse bone marrow-derived mast cells (BMMCs) and human umbilical cord blood-derived cultured mast cells with the dopaminergic toxin 1-methyl-4-phenylpyridinium (MPP+) led to release of the chemokine CCL2 and matrix metalloproteinase-3 which is claimed to play a role in PD pathogenesis. Moreover, MPP+-treated BMMCs exposed to glia maturation factor (an activator of glia inducing neuroinflammation/neurodegeneration; Zaheer et al., 2007) enhanced CCL2 release. Interestingly, MPP+-induced CCL2 release was greater in BMMCs-astrocyte co-cultures (see also Kim et al., 2010). Based on their findings the authors suggest that mast cells may play role in PD pathogenesis.
Multiple sclerosis
Multiple sclerosis (MS) is the prototypical inflammatory disease of the CNS, whose defining feature is the destruction of myelin (Compston and Coles, 2008). MS is the most frequent cause of chronic neurological impairment in young people (Kamm et al., 2014). Often thought of as a disorder of white matter demyelinating lesions, cortical demyelination contributes greatly to MS disabilities and may even precede the appearance of classic white matter plaques in some MS patients (Lucchinetti et al., 2011). The autoimmune nature of the disease (whether through genetic predisposition or yet to be elucidated environmental triggers) is initiated by myelin-reactive T cells, being then amplified by an inflammatory response involving myeloid cells, including microglia and infiltrating macrophages (Peferoen et al., 2015; Sospedra and Martin, 2016). Triggering receptor expressed on myeloid cells 2 (TREM-2) is a member of the immunoglobulin and lectin-like superfamily and operates as part of the innate immune system. It is highly expressed by microglia (Hickman et al., 2013) and facilitates nervous tissue debris clearance (Takahashi et al., 2007). TREM-2 is cleaved by microglia to produce soluble TREM-2, whose levels are reportedly increased in CSF of patients with relapsing-remitting, secondary progressive, and primary progressive MS, being normalized by treatment with the immunomodulatory drug natalizumab (Öhrfelt et al., 2016).
Mast cells are likely to play an important role in MS pathogenesis (Theoharides et al., 2008b; Kritas et al., 2014b; Conti and Kempuraj, 2016) by mediating inflammation and demyelinization via presentation of myelin antigens to T cells and/or disrupting the BBB, thereby allowing entry of inflammatory cells and cytokines. In the latter instance, expression of the mast cell chemoattractant CXCL12 at the lumen surface of endothelial cells (McCandless et al., 2008) could favor trafficking and accumulation of CXCR4-expressing mast cells. Mast cell tryptase is elevated in CSF from MS patients (Rozniecki et al., 1995), promotes mononuclear cell secretion of TNF-α and IL-6 (Malamud et al., 2003), and stimulates protease-activated receptors (PARs) that may disrupt BBB integrity (Bunnett, 2006). Interestingly, barrier breakdown occurs prior to pathological/clinical signs of MS (Kermode et al., 1990). EAE, a widely utilized animal model of MS based on an immune reaction against myelin oligodendrocyte glycoprotein, evidences degranulating mast cells in brain (Brenner et al., 1994). Mast cell activation and neutrophil recruitment is reported to promote early and robust inflammation in the meninges in EAE (Christy et al., 2013). Myelin activates mast cells (Medic et al., 2008), causing demyelination (Theoharides et al., 1991) and oligodendrocyte cell death (Medic et al., 2010). In spite of the broad use of these mouse EAE models, disagreement remains as to whether mast cell effects on EAE development depend on mouse strain, immunization protocol, or disease type and severity (Nelissen et al., 2013).
Mast cell-derived IL-1 and IL-6 promote transition of regulatory T cells to IL-17-producing active T helper type 17 (Th17) lymphocytes (Dudeck et al., 2011; El-Behi et al., 2011; Ganeshan and Bryce, 2012). IL-17 is elaborated by both adaptive immune cells (e.g., Th17 and cytotoxic T cells; Kolbinger et al., 2016) and innate immune cells (e.g., mast cells; Kan et al., 2016). By synergizing with other pro-inflammatory cytokines (e.g., released by microglia and mast cells themselves), IL-17 can induce release of yet additional cytokines/chemokines to recruit new inflammatory cells, ultimately impacting the function of microglia, astrocytes, oligodendrocytes, neurons, neural precursor cells and endothelial cells (Kolbinger et al., 2016).
The Th17 cytokine granulocyte macrophage-colony stimulating factor (GM-CSF) is a key player in EAE-associated neuroinflammation, as demonstrated by the absence of myelin-specific T cell accumulation in meninges and production of GM-CSF in mast cell-deficient animals (Russi et al., 2016a,b). Using mast cell-T cell co-cultures and selective mast cell reconstitution of the meninges of mast cell-deficient mice, these authors showed meningeal mast cells to be an early source of caspase-1-dependent IL-1β production. IL-1β promotes T cell expression of GM-CSF, thereby enhancing their encephalitogenicity. Interestingly, MS patients in the effector phase display mast cell-T cell co-localization (crosstalk?) in the meninges and CNS (Russi et al., 2016b). Beyond white matter demyelination, plaques in the gray matter also contribute to MS disease pathogenesis, with cortical demyelination being characterized by inflammation in the meninges—where mast cells are resident.
Another member of the IL-1 cytokine family, IL-33, is tied in to inflammatory and autoimmune diseases (Liew et al., 2010). Its receptor is mainly expressed by T helper 2 cells and mast cells. Frequently released from damaged cells, IL-33 is considered a danger signal (“alarmin”). IL-33 released from mast cells may exert autocrine/paracrine actions on these same cells by augmenting the stimulatory effects of IgE and substance P and by triggering their release of cytokines (Theoharides et al., 2015b). IL-33 is up-regulated in both peripheral leukocytes and CNS of MS patients (Christophi et al., 2012), and IL-33 blockade suppresses development of EAE in C57BL/6 mice during the induction phase (Li et al., 2012). Although IL-33 is expressed by neurons, astrocytes, oligodendrocytes and microglia in human brain, its receptor ST2 is mainly neuronal in location. Acute and chronic MS brain lesion tissues show augmented expression levels of IL-33 and ST2 compared to normal brain (Allan et al., 2016). Further, rat myelinating spinal cord co-cultures treated with IL-33 exhibited inhibition of myelination. MS patients frequently suffer from central neuropathic pain (Osterberg et al., 2005; Solaro et al., 2013). An intriguing possibility is that such pain might involve spinal cord oligodendrocyte-derived IL-33 inducing expression of TNF-α and IL-1β in spinal cord (Zarpelon et al., 2016).
Amyotrophic lateral sclerosis
Amyotrophic lateral sclerosis (ALS) is neurodegenerative disease that primarily affects upper and lower motor neurons, resulting in progressive muscular paralysis and typically leading to death within 2–5 years of diagnosis. ALS shows clinical, pathological, and genetic overlap with frontotemporal dementia (FTD; Lall and Baloh, 2017). While ALS appears as a composite syndrome with a number of aberrant cellular pathways (Geloso et al., 2017), neuroinflammation is recognized as a key aspect of ALS pathology (Philips and Robberecht, 2011; Liu and Wang, 2017). Activated microglia are a universal feature of ALS/FTD pathology, together with activation of astrocytes at specific disease stages in mouse models of ALS (Hall et al., 1998; Brites and Vaz, 2014; Lee et al., 2016; Lall and Baloh, 2017) and in humans (Turner et al., 2004). Strong evidence points to impairment of the neurovascular unit, including the blood-brain and blood-spinal cord barriers in patients and animal models of ALS (Rodrigues et al., 2012). Mast cells contain preformed TNF-α (unlike glia) and vasoactive mediators, and so may participate in regulating the function of both blood-brain (Ribatti, 2015) and blood-spinal cord barriers. In so doing, mast cells would facilitate entry of immune cells, including themselves (Sayed et al., 2010) across these barriers when compromised, as happens in ischemic stroke and ALS, respectively. Indeed, ALS spinal cord is reported to contain IL-17-expressing (Fiala et al., 2010) and degranulating mast cells. Regulatory T cells enhance mast cell production of IL-6 via surface-bound transforming growth factor-β (Gao and Ji, 2010), which then promotes Th17 activity (Dudeck et al., 2011). Moreover, serum and CSF of ALS patients display elevated amounts IL-12 and IL-15 (Rentzos et al., 2010), the latter cytokine acting as a mast cell chemoattractant (Jackson et al., 2005), while mast cells are a major source of the former (Nakano et al., 2007). IL-12 up-regulates mast cell surface expression of TLR2/TLR4 (Yang et al., 2010), members of a major class of pattern recognition transmembrane receptors activated by PAMPs. PAMPs are molecules associated with groups of pathogens recognized by cells of the innate immune system (Chakraborty et al., 2010). Mast cell (and microglia) TLR2 and TLR4 respond to molecules called damage associated molecular patterns, for example, the high mobility group box 1 protein that is elevated in spinal cord of ALS patients (Casula et al., 2011). Moreover, IL-6 and CCL5 elaborated by microglia could modulate TLR2 and TLR4 expression by mast cells (Pietrzak et al., 2011) to up-regulate chemokines and induce a pro-inflammatory profile in microglia (Skuljec et al., 2011). IL-12 is able as well to up-regulate expression of PAR2 (Zhang et al., 2007), an emerging target for neuroinflammation (Bushell, 2007). Collectively these data point to mast cell-microglia crosstalk, as well as potential autocrine/paracrine actions of cytokines like IL-12 on mast cells.
Mast cell involvement in the neuromuscular junction (NMJ) denervation of ALS was recently investigated in a rat hereditary ALS model (SOD1G93A), where the authors observed a marked infiltration and degranulation of mast cells that started after paralysis onset and correlated with progressive NMJ denervation (Trias et al., 2017). Further, mast cells accumulated around degenerating motor axons and NMJs, and were also associated with macrophages. Mast cell accumulation and degranulation in paralytic muscle was prevented by systemic treatment with masitinib; motor deficits were reduced as well.
Cerebral ischemia
Eight out of 10 strokes are due to cerebral ischemia, and the remaining ones from cerebral hemorrhage. Stroke is the most common cause of disability, the second commonest cause of dementia and the fourth commonest cause of death in the developed world (Sveinsson et al., 2014) and the leading cause of serious, long-term disability in the United States. Stroke pathology is characterized by an inflammatory response involving microglia activation, cytokine/chemokine release, and macrophage/neutrophil infiltration (Wang et al., 2007; Jordán et al., 2008). Interestingly, in the early phase of the ischemic episode inhibiting microglial cell activation may be of benefit (Hanisch and Kettenmann, 2007), perhaps by phagocytosing debris and/or releasing neurotrophic factors. Another important element in ischemic injury is activation/degranulation of mast cells, a phenomenon that plays a role in initiating the early phase of pathology (Jin et al., 2009; Lindsberg et al., 2010)—even before microglia and astrocyte activation. BBB breakdown accompanies ischemia, allowing for immune inflammatory cell infiltration into brain parenchyma. Mast cells occur within the dura and meninges, and on the brain side of the BBB (Silver and Curley, 2013), and promote BBB breakdown, edema, neutrophil infiltration, and hemorrhage in a rodent model of focal cerebral ischemia (McKittrick et al., 2015). Mast cell degranulation has been observed both in the immature brain after stroke (Biran et al., 2008) and in adult rats undergoing transient global ischemia (Hu et al., 2004). A mast cell role in stroke is strengthened by studies showing that pharmacological mast cell stabilization and genetic mast cell deficiency in rats reduces BBB permeability, brain edema, and neutrophil recruitment (Strbian et al., 2006; Jin et al., 2007; Mattila et al., 2011; Kocic et al., 2015), perhaps by regulating, in part, acute microvascular gelatinase activation (Mattila et al., 2011). Moreover, mast cell blocking limits brain edema and hematoma volume and improves outcome after experimental intracerebral hemorrhage (Strbian et al., 2007). Yet another factor implicated in BBB breakdown is the angiogenic factor vascular endothelial growth factor, which is synthesized, stored, and released by mast cells (Grützkau et al., 2012). In the case of MS, data from EAE models suggest that meningeal (mast cell-mediated) inflammation is a precursor to CNS immune cell (e.g., T cells) infiltration as a consequence of a loss of integrity of both the local BBB and CSF-blood barrier (Sayed et al., 2010; Colloca et al., 2017).
Traumatic brain injury
Traumatic brain injury (TBI) is a non-degenerative, non-congenital insult to the brain from an external mechanical force that causes brain dysfunction. Mild TBI may cause temporary dysfunction of brain cells. More serious injury can result in bruising, torn tissues, bleeding, and other physical damage to the brain followed by secondary pathological processes including excitotoxicity, ischemia, and neuroinflammation that result in long-term complications and/or death (Hagberg et al., 2012; Xiong et al., 2013). Cognitive and behavioral deficits caused by TBI to the immature brain are more severe and persistent than injuries to the adult brain (Rivara et al., 2012). Among the first events of the injury response, in both the adult and the developing brain, is the degranulation of mast cells (Lozada et al., 2005; Stokely and Orr, 2008) that may facilitate a compromised BBB. In addition, mild TBI evoked by closed head injury is associated with persistent (up to 1 month) dura mast cell degranulation (Levy et al., 2016) and a chronic immune response (Ertürk et al., 2016).
Microglia, together with astrocytes and oligodendrocytes, play instrumental roles in shaping the microenvironment after TBI (Koshinaga et al., 2000; Ramlackhansingh et al., 2011; Karve et al., 2016; Kumar et al., 2017; Taib et al., 2017). In a longitudinal study in humans, chronically activated microglia and tissue degeneration was observed even years after injury (Johnson et al., 2013). Experimental studies in rodents are consistent with the above, showing up-regulation of pro-inflammatory markers (Holmin and Mathiesen, 1999), chronic microglial cell activation, lesion expansion, and hippocampal neuron and myelin loss (Loane et al., 2014). Although often overlooked in the context of TBI secondary injury, also the complement system plays a notable role in this multifaceted inflammatory reaction (Hammad et al., 2018). Astrocytes undergo reactive changes in a setting of TBI, becoming hypertrophic with swelling and extension of processes in the first few days, followed by glial scar formation (Villapol et al., 2014) and with reactive gliosis persisting up to several months post-injury. Although scarring is a potentially a protective mechanism against further injury, it can act to inhibit axonal regrowth and regeneration (Silver and Miller, 2004). Another feature of astrocyte reactivity in TBI is that of proliferation, manifested by an up-regulated expression of glial fibrillary acidic protein, close to the lesion site (Bardehle et al., 2013) and which appears to peak in the acute phase after experimental TBI. As discussed earlier astrocytes, like microglia, can elicit both beneficial and detrimental effects. Moreover, as astrocytes render microglia more responsive to pro-inflammatory stimuli (Barbierato et al., 2013, 2017; Facci et al., 2014) and neurotoxic reactive astrocytes are induced by activated microglia (Liddelow et al., 2017), such behaviors could work in concert the affect the local environment after TBI.
Postoperative cognitive dysfunction shares some features with TBI. Neuroinflammation initiated by extra-CNS surgical trauma, followed by release of CNS inflammatory mediators can damage synapses and neurons and may be a critical component of surgery-induced cognitive dysfunction (Riedel et al., 2014). This phenomenon is often seen in the elderly consequent to surgery and hospitalization (Terrando et al., 2011). As with TBI, cerebral mast cells have been suggested to contribute to postoperative cognitive dysfunction and pain after surgical procedure-mediated neuroinflammation (Oliveira et al., 2011; Li et al., 2017) by promoting BBB breakdown (Zhang S. et al., 2016; Zhang X. et al., 2016). In addition, astrocyte-derived CCL2 participates in surgery-induced cognitive dysfunction and neuroinflammation via evoking microglia activation (Xu et al., 2017).
Neuropathic pain
Acute and chronic pain are cardinal features of inflammation, albeit different clinical entities. The former is provoked by a specific disease or injury, serves a useful biologic purpose, and is self-limited. Chronic pain, on the other hand, may be considered a disease state that outlasts the normal time of healing and is thought to result from alterations in neuronal cell plasticity. Such alterations include sensitization of peripheral nociceptors in dorsal root and trigeminal ganglia (Basbaum et al., 2009) and central nociceptive neurons in the spinal cord, trigeminal nucleus, brain stem, and cortex (Ossipov et al., 2010). Together, peripheral sensitization and central sensitization translate into a heightened perception of pain. Chronic pain represents a substantial and rising unmet medical need (Smith and Torrance, 2012), and affects 7–10% of the general population (Colloca et al., 2017).
Neuropathic pain represents, without doubt, the most debilitating type of chronic pain, and is a consequence of damage, degeneration, or dysfunction of the sensory nervous system (Jay and Barkin, 2014). Epidemiological studies place a population prevalence of pain with neuropathic characteristics at between 6.9 and 10% (van Hecke et al., 2014), yet it remains largely untreatable. Neuropathic pain is either peripheral or central, as a function of lesion location caused by disease (e.g., diabetes mellitus), medical intervention (chemotherapy, surgery), and injury, the last most often caused by stroke, spinal cord injury, or MS (Kerstman et al., 2013). Peripheral neuropathic pain (painful neuropathy) is, in effect, a brain disease where alterations in neural networks affect multiple aspects of brain function, structure, and chemistry (Borsook, 2012). Analgesics continue to focus on reducing pain transduction and transmission in neurons, which likely accounts for their limited success in controlling disease progression (Ji et al., 2014). This “neuron-centric” view fails to consider that initiation and maintenance of neuropathic pain depend to a great extent on Schwann cells, spinal microglia, and astrocytes, together with elements of the peripheral immune system (Ren and Dubner, 2010) such as mast cells—as will be discussed below.
Mast cells (Héron and Dubayle, 2013) and microglia are frontline protagonists as primary interlocutors for pain neurons, in the periphery as well as at the spinal/supraspinal levels. In the latter case, a new study (Kissel et al., 2017) demonstrates that spinal nerve ligation corresponds temporally and in magnitude with degranulation of thalamic mast cells—a rich source of these cells (Florenzano and Bentivoglio, 2000). Protracted alterations in these immune cells promote persistent neuroinflammation that ultimately impacts neuron functionality. Mast cell mediators like IL-6 activate/sensitize nociceptors which not only contribute to neuropathic pain (Xanthos et al., 2011) but also activate trigemino-cervical and lumbosacral pain pathways, causing widespread tactile pain hypersensitivity (Levy et al., 2012). Peripheral nerve-resident mast cells (and not microglia) are the responders at the site of damage, where they promote recruitment of neutrophils and macrophages (Zuo et al., 2003). In addition, mast cell-derived NGF (Leon et al., 1994) can not only sensitize nociceptors (Kelleher et al., 2016), but mast cells themselves may respond to NGF in a paracrine/autocrine manner. Mast cells could also help in recruiting other immune cell types (e.g., T-cells) which, in turn, release pro-nociceptive mediators. Rats with chronic constrictive nerve injury and treated with glucocorticoids exhibit a reduction in pain and TNF-α-positive mast cell numbers (Hayashi et al., 2011). Mast cells appear to be crucial mediators of chronic visceral pain, as well (Done et al., 2012), and have been proposed as a target in the treatment of complex regional pain syndrome (Dirckx et al., 2013).
Glia are important interlocutors of pain processes at the spinal level (Grace et al., 2014; Old et al., 2015; Echeverry et al., 2017). For example, spinal microglia, upon activation by either cell surface molecules or pro-inflammatory signals released from peripheral immune cells such as mast cells elaborate IL-1β to modulate neuronal cell activity. Dorsal horn microglia become activated in pathological conditions (e.g., peripheral nerve injury) accompanied by up-regulation of ionotropic P2X and metabotropic P2Y purinergic receptors (Kobayashi et al., 2008; Skaper et al., 2010; Biber et al., 2011) to participate in neuropathic pain (Burnstock, 2016; Tsuda, 2016); indeed, inhibiting the function or expression of these microglial receptors strongly attenuates neuropathic pain (Tsuda, 2016). Interactions between mast cells and glia, as will be discussed in a later section, may contribute to amplification of peripheral pain signals at the spinal level. Astrocytes also are a key contributor to neuropathic pain (Milligan and Watkins, 2009; Ji et al., 2013). A recent study by Peng et al. (2016) suggests that microglia and monocytes may act synergistically to promote the transition from acute to chronic pain after nerve injury. Collectively, these findings propose that moderating mast cell-glia reactivity may be a viable therapeutic direction for treating neuropathic pain (Gao and Ji, 2010; Skaper and Facci, 2012; Popiolek-Barczyk and Mika, 2016). In this context it is interesting to point out that acute intracerebroventricular administration of N-palmitoylethanolamine (PEA), a congener of the endocannabinoid anandamide with analgesic and anti-inflammatory activities linked to mast cell/microglia modulation (Alhouayek and Muccioli, 2014; Petrosino and Di Marzo, 2017), reduced carrageenan-induced paw oedema/hyperalgesia (D'Agostino et al., 2007), and chronic pain in man (Paladini et al., 2016).
While not often considered, intriguing evidence suggests that oligodendrocytes, the myelin-producing cells of the CNS, may also participate in pain mechanisms. Among their other roles, oligodendrocytes support, in a myelin-independent manner, axonal functions, and long-term integrity (Nave, 2010; Bankston et al., 2013). Oligodendrocyte ablation causes spinal axonal pathology, along with induction/maintenance of a heightened nociceptive sensitivity in the absence of innate or adaptive immune responses (Gritsch et al., 2014). Further, they produce and respond to chemokines/cytokines that modulate CNS immune responses, express antigen-presenting molecules, complement and complement receptor molecules, complement regulatory molecules, neuroimmune regulatory proteins as well as extracellular matrix proteins (Peferoen et al., 2014; Zeis et al., 2016), and interact with microglia (Peferoen et al., 2014). Intrathecal administration of N,N-dimethylsphingosine (DMS) in rats, whose dorsal horn production is triggered by inflammation, induces neuropathic pain-like behavior (Patti et al., 2012). Human oligodendrocytes produce DMS, and their levels of DMS rise when challenged with agents that damage white matter (Chen et al., 2014). These authors suggest that damage to oligodendrocytes can result in increased DMS production to drive inflammatory astrocyte responses in sensory neuron sensitization. In the case of MS, for example, autoimmune inflammation driven by invading peripheral immune cells may lead to injury/degeneration of oligodendrocytes and neurons, and play a part in the neuropathic pain often experienced by MS patients. In addition, spinal cord oligodendrocyte-derived IL-33 reportedly mediates neuropathic pain (Zhang et al., 2014). von Büdingen et al. (2015) recently demonstrated that NGF directly binds to myelin oligodendrocyte glycoprotein (which shares structural features with TrkA), a protein localized to the outermost lamellae of compact CNS myelin. These authors posit that myelin oligodendrocyte glycoprotein may serve a protective mechanism to remove excess NGF and prevent aberrant sprouting and neuropathic pain after peripheral nerve injury. It is interesting to note that inflammatory cytokines in peripheral nerves have been implicated in the Wallerian degeneration of peripheral nerves after injury and in certain types of inflammatory neuropathies. In analogy to oligodendrocytes (Barbierato et al., 2017), Schwann cells are the primary source of SAA1 production after peripheral nerve injury (Jang et al., 2012).
Depression
Peripheral immune modulators can induce psychiatric symptoms in animal models and humans. Medical conditions associated with chronic inflammatory and immunological abnormalities, including obesity, diabetes, rheumatoid arthritis, and MS are risk factors for depression (Mezuk et al., 2008; Faith et al., 2011; Matcham et al., 2013; Feinstein et al., 2014). Almost one-half of non-depressed hepatitis C and cancer patients treated with interferon develop depressive symptoms associated with increased serum IL-6 levels (one of the more reliable peripheral biomarkers in major depression) (Loftis and Hauser, 2004), while significantly higher circulating concentrations of TNF-α and IL-6 were reported in depressed subjects compared with controls (Dowlati et al., 2010). Intravenous administration in healthy male volunteers of low-dose endotoxin not only induces a significant increase in peripheral blood concentrations of TNF-α, IL-6, and IL-10 but also results, with some delay, in a selective increase of IL-6 in CSF (Engler et al., 2017). These authors also found a strong association between endotoxin-induced increase of IL-6 in CSF and severity of mood impairment. The cellular mechanisms that underlie depression remain unclear, perhaps due at least in part to the fact that research until now has focused on neuronal cell dysfunction. The role of non-neuronal cells (glia and mast cells especially) in depression has lagged behind. Newer studies indicate that impairment of the normal structure and function of microglia (Prinz and Priller, 2014), caused by either intense inflammatory activation or by decline and senescence of these cells (e.g., during aging), can lead to depression and associated impairments in neuroplasticity and neurogenesis (Brites and Fernandes, 2015; Yirmiya et al., 2015).
Tryptophan catabolism, another important facet of inflammation-induced depression (Hendriksen et al., 2017), involves up-regulation of indoleamine 2,3-dioxygenase (IDO; Maes et al., 2011), the rate-limiting enzyme in the kynurenine pathway. Elevated levels of kynurenine have been linked to depressive-like symptoms in man (Gabbay et al., 2012). As kynurenine has been suggested to enhance IgE-mediated mast cell responses (Kawasaki et al., 2014), it is conceivable that the latter could be affected by alterations in tryptophan metabolism (and, hence, kynurenine levels) (Campbell et al., 2014). Mastocytosis, a rare mast cell activation disorder of both children and adults is characterized by mast cell accumulation in peripheral organs (Valent et al., 2001). Patients with mastocytosis often exhibit not only acute and chronic pain (Wirz and Molderings, 2017) but also psychopathological manifestations such as cognitive impairment; depression appears to be their most common complaint and ranges from 40 to 70% (Rogers et al., 1986; Hermine et al., 2008). Conceivably, systemic brain involvement mediated by mast cell mediators might account for the high prevalence of depression. In this context, mastocytosis patients reportedly display lower levels of tryptophan and serotonin but higher levels of kynurenic and quinolinic acids (Georgin-Lavialle et al., 2016), leading these authors to propose a role for mast cells in the tryptophan pathway leading to depression. Additionally, mast cells have been implicated in mechanisms related to the regulation of emotion (Nautiyal et al., 2008). Masitinib was shown efficacious in treating cutaneous mastocytosis in dogs (Cadot et al., 2011) and in improving recovery from depression associated with mastocytosis (Paul et al., 2010; Moura et al., 2011), suggesting a link between depression in mastocytosis and mast cell activation.
Autism spectrum disorder
Autism spectrum disorder (ASD) is a life-long condition characterized by marked neurological deficits, especially as relates to cognitive function. Although its pathogenesis remains unknown the major hypothesis at present posits that autism is a multifactorial disorder, possibly being associated to some degree with aspects of autoimmune dysfunction (Theoharides et al., 2013). Mast cells, part of the innate immune system, are reportedly activated in autism (Theoharides et al., 2008a, 2012, 2016), and ASD incidence is claimed to be 10-fold higher in children with mastocytosis (Theoharides, 2009). One such mast cell activator is the neuropeptide neurotensin (Carraway et al., 1982), whose circulating levels are elevated in ASD patients (Tsilioni et al., 2014). A growing body of evidence supports the view that a chronic subclinical inflammation involving both the gut and CNS may contribute to autism symptomatology (Vargas et al., 2005; Thacker et al., 2007; Morgan et al., 2010, 2012; Kern et al., 2016), with active neuroinflammatory processes being found throughout the brain in both cerebral cortex and cerebellum of patients with autism. Intriguingly, a new pair of studies in Nature, by Kim et al. (2017) and Shin Yim et al. (2017) describe how infection during pregnancy increases the risk of neurodevelopmental disorders, such as autism, in offspring. These mouse studies now reveal a link between gut bacteria and atypical brain-circuit connections. Brain abnormalities in persons diagnosed with ASD reportedly show significant ongoing neuroinflammation as a central element of the pathology (Herbert, 2005). Areas of abnormally developed cortex have been identified in individuals with autism (Stoner et al., 2014), and suggest dysregulation of layer formation and layer-specific neuronal differentiation at prenatal developmental stages. Tetreault et al. (2012) reported higher densities of microglia throughout cerebral cortex in brains of people with autism. When sustained, microglial activation can contribute to disease progression and injury of healthy brain tissue through release of pro-inflammatory mediators (Smith et al., 2012) and by engulfing synapses (Rodriguez and Kern, 2011) and other neuronal tissue, thereby leading to cell loss and reduced connectivity, both of which are found in ASD brain (Rodriguez and Kern, 2011).
Fibromyalgia syndrome
Fibromyalgia syndrome is a prevalent rheumatic disease, that strikes between 2 and 4% of the general population (Queiroz, 2013), predominantly females. This syndrome is characterized by widespread chronic pain, tenderness in muscles and deep tissues, and fatigue/sleep disturbances. The pain of fibromyalgia is a disabling condition and can become quite marked when provoked by digital pressure at tender points. Pain in fibromyalgia is believed to be associated with a generalized alteration (sensitization) in the central somatosensory system (Kim et al., 2015), a condition most likely sustained by neuroinflammatory processes triggered by microglia (Alfonso Romero-Sandoval and Sweitzer, 2015) and mast cell (Kissel et al., 2017) activation. Interestingly, a recent study identified neuropathy of small nerve fibers in patients with fibromyalgia (Üçeyler et al., 2013). Cross-talk between the nervous and immune systems no doubt plays an important role in the initiation and progression of chronic pain in fibromyalgia syndrome and other central sensitivity syndromes (Staud, 2015).
Neuroinflammation: the risk of growing old
Frailty is a common geriatric syndrome characterized by age-associated declines in physiologic and cognitive reserves across multi-organ systems, resulting in an increased vulnerability for adverse health outcomes (Heuberger, 2011). Chronic (non-resolving) inflammation is likely a key pathophysiologic process that contributes to the frailty syndrome directly and indirectly through other intermediate physiologic systems, and complex multi-factorial etiologies such as obesity and diabetes. Aging is associated with elevated levels of circulating cytokines and pro-inflammatory markers, and age-related changes in the immune system (often referred to as “immunosenescence” or “inflammoaging”) (Michaud et al., 2013; Mate et al., 2014). Hippocampal processing is more easily disrupted in old animals than in younger ones when the peripheral innate immune system is stimulated, suggesting that aging can facilitate neurobehavioral complications associated with peripheral infections (Chen et al., 2008; McManus and Heneka, 2017).
Innate immune cell types, especially mast cells and microglia, are likely to contribute importantly to non-resolving inflammation in the context of aging (Labzin et al., 2018). Although we may think of aging as a general slowing down of the body's cellular activities, the latter cell populations actually appear to become more reactive. For example, as an animal ages, mast cells express alterations in degranulation behavior (e.g., greater sensitivity to prostaglandin E2; Nguyen et al., 2005). Individual microglial cell reactivity/sensitivity appear to persist throughout the entire lifespan, which may explain how stimulation of microglia early in life can induce long-term changes in brain function (Füger et al., 2017). Senescence of resident microglia (and astrocytes) might thus contribute to the age-related increase in risk for neurodegenerative diseases (Hoeijmakers et al., 2016; Labzin et al., 2018; Santoro et al., 2018). In fact, dystrophic (senescent) rather than activated microglia has been noted also in mouse brain with aging (Streit et al., 2009; da Silva et al., 2014; Punzo et al., 2016). Experimental models of aging demonstrate aberrant microglial cell behaviors, in particular in terms of an increased inflammatory state of microglia, in which cells are “primed” to be activated and resistant to regulation (Eggen et al., 2013; Norden and Godbout, 2013; Rawji et al., 2016). Primed microglia are more sensitive to a secondary inflammatory stimulus, thus leading to an exaggerated inflammatory response (Perry and Holmes, 2014). This was demonstrated by culturing microglia-free cerebellar astrocytes together with the addition of increasing numbers of microglia (Facci et al., 2014). The co-cultures displayed a heightened priming response, whereby a classical inflammatory stimulus (lipopolysaccharide, LPS) sensitized (“primes”) the cells to ATP-induced release of IL-1β. Equivalent numbers of microglia alone, however, were essentially devoid of a priming response and IL-1β release. The generality of this phenomenon was shown by the ability of cortical and spinal cord glia to respond to LPS priming in an analogous manner (Facci et al., 2014). These findings serve also to illustrate the concept of glial cell interactions.
Substances other than LPS are capable of effecting a priming behavior. For example, the alarmin high mobility group box 1, released under chronic pathological conditions to initiate inflammatory cascades, mediates neuroinflammatory priming in the aged brain (Fonken et al., 2016). It has also been suggested that microglial priming can be explained by the mechanisms that underlie trained immunity (the latter involving the enhancement of inflammatory responses by epigenetic mechanisms mobilized after first exposure to an inflammatory stimulus) (Haley et al., 2018). When primed, microglia may over-react to a second challenge, resulting in an enhanced pain intensity and duration (Hains et al., 2010). Challenge to the aged brain's immune system leads to amplification/prolongation of microglia activation that may, over a long period of time, manifest itself in deleterious behavioral and cognitive consequences. Xie et al. (2013) found that the age-related decline of myelin proteins is correlated with activation of astrocytes and microglia in rat. In turn, this could disturb microglia clearance function during aging and lead to lysosomal storage, possibly contributing to microglial senescence and immune dysfunction (Safaiyan et al., 2016).
A mast cell—microglia dialogue may likely contribute to exacerbate the effects of aging on their pro-inflammatory behaviors. While not always appreciated as such, both obesity (Theoharides et al., 2015b) and diabetes (Donath, 2014) are states of chronic low-grade inflammation. One might thus predict a general rise in the occurrence of the latter conditions with age, in effect placing the elderly in “harms way” for a condition of low-grade, non-resolving inflammation. Indeed, an endotoxin-induced, persistent state of low-grade inflammation is associated with innate immune “programming” or “memory” (Morris et al., 2015). Given the close link between BBB integrity and cognitive dysfunction in aging (Chan-Ling et al., 2007; Rapp et al., 2008), acute and chronic inflammatory pain states, including neuropathic pain (which is associated with low-grade chronic inflammation), may well alter barrier permeability (Rosenberg, 2012).
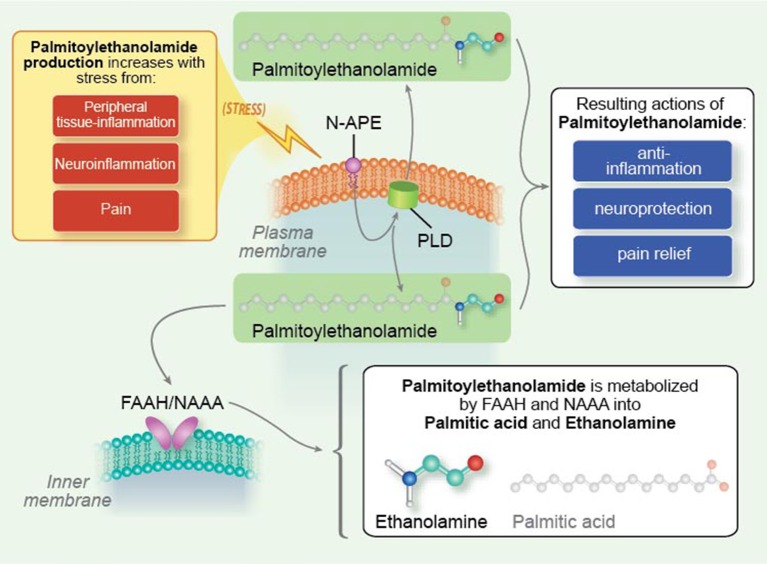
Leveraging endogenous molecules for therapeutic benefit in neuroinflammation
Targeting activation of glia (Gosselin et al., 2010; Möller and Boddeke, 2016; Roser et al., 2017) and mast cells (Graziottin et al., 2014; Hendriksen et al., 2017) is gaining increasing traction as a potential therapeutic avenue for the treatment of nervous system disorders. In addition to small molecule anti-inflammatory agents derived by synthetic chemical routes (Roser et al., 2017), tissue damage and/or stimulation of inflammatory responses activate endogenous protective mechanisms that lead to the elaboration of lipid mediators which function as a program of resolution to switch off inflammation (Buckley et al., 2013; Piomelli and Sasso, 2014). Harnessing such lipid mediators might provide a novel approach to effect a program of resolution (Tabas and Glass, 2013). The mechanism of physiological mast cell regulation, first defined by the Nobel laureate Rita Levi-Montalcini as ALIA (Autocoid Local Injury Antagonism), is the mast cell ability to synthesize on demand the natural mediator PEA. PEA is a member of the N-acylethanolamine (NAE) family, in which a fatty acid is linked to an ethanolamine moiety. NAEs include the endocannabinoid N-arachidonoylethanolamine (anandamide) and its congeners N-stearoylethanolamine, N-oleoylethanolamine and PEA (Pacher et al., 2006). The NAEs (including PEA) are generated principally from by a membrane-associated N-acylated phosphatidylethanolamine (NAPE)-phospholipase D to yield the respective NAE and phosphatidic acid (Figure 4; Leung et al., 2006), although other pathways exist (Ueda et al., 2013). NAEs in the mammalian brain are hydrolyzed to the corresponding fatty acid and ethanolamine by fatty acid amide hydrolase (FAAH; Cravatt et al., 1996) and NAE-hydrolyzing acid amidase (NAAA; Tsuboi et al., 2007; Figure 4). In contrast to FAAH, NAA hydrolyzes NAEs having less than 18 carbon atoms, i.e., PEA (Ueda et al., 2013). The most striking catalytic property of NAAA is a pH optimum at 4.5–5, which is consistent with its immunocytochemical localization in lysosomes (Tsuboi et al., 2007), and with the acidic environment of inflamed tissues.
Figure 4.
Palmitoylethanolamide synthesis and metabolism. N-palmitoyl-phosphatidyl-ethanolamine (N-APE) is converted into palmitoylethanolamide and phosphatidic acid by a plasma membrane-associated N-acylated phosphatidylethanolamine-phospholipase D (PLD). Palmitoylethanolamide (PEA) is broken down to palmitic acid and ethanolamine by fatty acid amide hydrolase (FAAH, which also catabolizes other fatty acid amides) as well as the more selective N-acyl ethanolamine-hydrolyzing acid amidase (NAAA). Tissue levels of palmitoylethanolamide rise under conditions of stress, e.g., peripheral tissue inflammation, neuroinflammation, and pain [Reproduced from Skaper et al. (2014) Mast cells, glia and neuroinflammation: partners in crime? (Figure 2). Copyright © 2013 John Wiley & Sons Ltd. With permission].
PEA is produced/hydrolyzed by microglia and mast cells (Bisogno et al., 1997; Muccioli and Stella, 2008), down-modulates mast cell activation (Facci et al., 1995), and controls microglial cell behaviors (Franklin et al., 2003; Luongo et al., 2013). An expanding body of preclinical studies attest to the anti-neuroinflammatory and neuroprotective actions of PEA (Alhouayek and Muccioli, 2014; Esposito et al., 2014; Fidaleo et al., 2014; Mattace Raso et al., 2014; Petrosino and Di Marzo, 2017), and will not be detailed here. It is worth mentioning, however, that PEA decreased aggression in early adolescent socially isolated mice (a putative rodent model of post-traumatic stress disorder; Locci et al., 2017), and rescued learning and memory impairments in a triple transgenic mouse model of AD (Scuderi et al., 2018). These studies were carried out with micronized/ultramicronized PEA, formulations which favor its oral bioavailability over non-micronized PEA (Impellizzeri et al., 2014). Importantly, PEA has proven efficacious in man in a number of clinical settings, which are summarized in Table 3, including a lower frequency of death and tracheotomy in PEA-treated ALS patients compared to untreated patients in terms of the proportion of ALS patients who survived without tracheotomy. None of the clinical trials with PEA to date have reported treatment-related adverse events (Skaper et al., 2014; Paladini et al., 2016).
Table 3.
Clinical studies demonstrating efficacy of palmitoylethanolamidea.
| Pathology | References |
|---|---|
| Non-surgical lumbar radiculopathies | Chirchiglia et al., 2018 |
| Chronic pain (including neuropathic pain) of differing etiologies | Skaper et al., 2014; Paladini et al., 2016 |
| Endometriosis | Iuvone et al., 2016; Indraccolo et al., 2017 |
| Fibromyalgia | Del Giorno et al., 2015 |
| Parkinson disease (adjuvant therapy) | Brotini et al., 2017 |
| Relapsing-remitting multiple sclerosis (add-on therapy for the treatment of interferon-β1a-related adverse effects) | Orefice et al., 2016 |
| Stroke (adjuvant therapy) | Caltagirone et al., 2016 |
| Amyotrophic lateral sclerosis | Clemente, 2012; Palma et al., 2016 |
| Autism | Antonucci et al., 2015; Bertolino et al., 2017 |
micronized/ultramicronized palmitoylethanolamide.
Inhibiting the enzymatic degradation of PEA by targeting NAAA, in principle, represents another route in treatment of neuroinflammation. A number of selective NAAA inhibitors have been described (Solorzano et al., 2009; Sasso et al., 2013; Ribeiro et al., 2015; Yang et al., 2015) including systemically active compounds which are able to modulate responses induced by inflammatory stimuli in vivo and in vitro. The validity of such an approach in man remains to be demonstrated. PEA is not constitutive but is produced on demand, and its catabolic enzymes are probably intended to modulate substrate availability. Given PEA pleiotropic effects, a modulatory (rather than fully inhibitory) approach would maximize availability of the NAE, while assuring that the NAE's component molecules (palmitic acid and ethanolamine in the case of PEA) are returned to the biological system. In principle, this approach should avoid interfering with further on-demand NAE synthesis.
Epilogue
Inflammation was designed by nature to protect the body in response to injury or infection and promote tissue repair and healing. Uncontrolled, this physiological reaction is transformed into a pathological process that can have profound consequences for nervous system health. Aberrant activation of the innate immune system, in particular involving mast cells and microglia, may occur in either a context-specific fashion or because of the body's inability to resolve a state of protracted inflammation. The former cells are capable of reacting with rapid and longer-term delayed responses, while the latter comprise key sensors for disrupted brain homeostasis and accumulate locally as a consequence of neuronal cell injury or entry of foreign material into the brain parenchyma. We have come to appreciate that a complex interplay exists between non-neuronal cells in the nervous system, including microglia, astrocytes, mast cells and oligodendrocytes. Such cellular behaviors can present a challenge when designing strategies to deal with the resolution of inflammation-associated neurological disorders. This scenario takes on added significance with the knowledge that mast cell and microglia reactivity/responsiveness change with aging. Obesity/metabolic disease and diabetes, for example, with their age-dependent rise in prevalence, can be expected to contribute to low-grade non-resolving inflammation and neuroinflammation. Additionally, acute and chronic inflammatory states may alter BBB permeability and ultimately lead to aging-associated cognitive dysfunction.
We still have much to learn concerning the mechanisms that regulate neuroinflammation. This shortcoming is evident, for example, in current treatments for neuropathic pain; these agents are largely neuron-centric and address the symptoms rather than the underlying pathophysiology. An alternative approach for treating nervous system disorders nay be to focus on endogenous regulators of inflammation. Within this context, the fatty acid amide signaling molecule PEA shows promise by contributing to the resolution of neuroinflammation through modulation of mast cell and glia activity—in other words, a modulator of immuno-neural homeostasis. Molecules capable of modulating activation of both glia and mast cells, without provoking immunosuppression, could be of utility in the resolution of inflammation and restoration of tissue homeostasis.
Author contributions
All authors contributed to the conception, writing, and critical evaluation of the manuscript. All authors read and approved of the final submitted version of the manuscript.
Conflict of interest statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
This study was supported in part by MIUR, PON Ricerca e Competitività 2007–2013 project PON01_02512 and by Regione Veneto project protocol 103173COF/14/LR52001C2/000051.
The authors wish to thank Luca Di Giacomo for his artistic input in the preparation of the illustrations which accompany this manuscript.
References
- Alfonso Romero-Sandoval A., Sweitzer S. (2015). Nonneuronal central mechanisms of pain: glia and immune response. Prog. Mol. Biol. Transl. Sci. 131, 325–358. 10.1016/bs.pmbts.2014.11.007 [DOI] [PubMed] [Google Scholar]
- Alhouayek M., Muccioli G. G. (2014). Harnessing the anti-inflammatory potential of palmitoylethanolamide. Drug Discov. Today 19, 1632–1639. 10.1016/j.drudis.2014.06.007 [DOI] [PubMed] [Google Scholar]
- Allan D., Fairlie-Clarke K. J., Elliott C., Schuh C., Barnett S. C., Lassmann H. (2016). Role of IL-33 and ST2 signalling pathway in multiple sclerosis: expression by oligodendrocytes and inhibition of myelination in central nervous system. Acta Neuropathol. Commun. 4:75. 10.1186/s40478-016-0344-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amor S., Woodroofe M. N. (2014). Innate and adaptive immune responses in neurodegeneration and repair. Immunology 141, 287–291. 10.1111/imm.12134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antonucci N., Cirillo A., Siniscalco D. (2015). Beneficial effects of palmitoylethanolamide on expressive language, cognition, and behaviors in autism: a report of two cases. Case Rep. Psychiatry 2015:325061. 10.1155/2015/325061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Appel S. H., Beers D. R., Henkel J. S. (2010). T cell-microglial dialogue in Parkinson's disease and amyotrophic lateral sclerosis: are we listening? Trends Immunol. 31, 7–17. 10.1016/j.it.2009.09.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Appel S. H., Zhao W., Beers D. R., Henkel J. S. (2011). The microglial-motoneuron dialogue in ALS. Acta Myol 30, 4–8. [PMC free article] [PubMed] [Google Scholar]
- Balducci C., Forloni G. (2018). Novel targets in Alzheimer's disease: a special focus on microglia. Pharmacol. Res. [Epub ahead of print]. 10.1016/j.phrs.2018.01.017 [DOI] [PubMed] [Google Scholar]
- Bankston A. N., Mandler M. D., Feng Y. (2013). Oligodendroglia and neurotrophic factors in neurodegeneration. Neurosci. Bull. 29, 216–228. 10.1007/s12264-013-1321-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barbierato M., Borri M., Facci L., Zusso M., Skaper S. D., Giusti P. (2017). Expression and differential responsiveness of central nervous system glial cell populations to the acute phase protein serum amyloid A. Sci. Rep. 7:12158. 10.1038/s41598-017-12529-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barbierato M., Facci L., Argentini C., Marinelli C., Skaper S. D., Giusti P. (2013). Astrocyte-microglia cooperation in the expression of a pro-inflammatory phenotype. CNS Neurol. Disord. Drug Targets 12, 608–618. 10.2174/18715273113129990064 [DOI] [PubMed] [Google Scholar]
- Bardehle S., Krüger M., Buggenthin F., Schwausch J., Ninkovic J., Clevers H., et al. (2013). Live imaging of astrocyte responses to acute injury reveals selective juxtavascular proliferation. Nat. Neurosci. 16, 580–586. 10.1038/nn.3371 [DOI] [PubMed] [Google Scholar]
- Basbaum A. I., Bautista D. M., Scherrer G., Julius D. (2009). Cellular and molecular mechanisms of pain. Cell 139, 267–284. 10.1016/j.cell.2009.09.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becher B., Spath S., Goverman J. (2017). Cytokine networks in neuroinflammation. Nat. Rev. Immunol. 17, 49–59. 10.1038/nri.2016.123 [DOI] [PubMed] [Google Scholar]
- Beggs S., Trang T., Salter M. W. (2012). P2X4R+ microglia drive neuropathic pain. Nat. Neurosci. 15, 1068–1073. 10.1038/nn.3155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bertolino B., Crupi R., Impellizzeri D., Bruschetta G., Cordaro M., Siracusa R., et al. (2017). Beneficial effects of co-ultramicronized palmitoylethanolamide/luteolin in a mouse model of autism and in a case report of autism. CNS Neurosci. Ther. 23, 87–98. 10.1111/cns.12648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biber K., Tsuda M., Tozaki-Saitoh H., Tsukamoto K., Toyomitsu E., Masuda T., et al. (2011). Neuronal CCL21 up-regulates microglia P2X4 expression and initiates neuropathic pain development. EMBO J. 30, 1864–1873. 10.1038/emboj.2011.89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biran V., Cochois V., Karroubi A., Arrang J. M., Charriaut-Marlangue C., Héron A. (2008). Stroke induces histamine accumulation and mast cell degranulation in the neonatal rat brain. Brain Pathol. 18, 1–9. 10.1111/j.1750-3639.2007.00092.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biscaro B., Lindvall O., Tesco G., Ekdahl C. T., Nitsch R. M. (2012). Inhibition of microglial activation protects hippocampal heurogenesis and improves cognitive deficits in a transgenic mouse model for Alzheimer's disease. Neurodegener. Dis. 9, 187–198. 10.1159/000330363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bisogno T., Maurelli S., Melck D., De Petrocellis L., Di Marzo V. (1997). Biosynthesis, uptake, and degradation of anandamide and palmitoylethanolamide in leukocytes. J. Biol. Chem. 272, 3315–3323. 10.1074/jbc.272.6.3315 [DOI] [PubMed] [Google Scholar]
- Borsook D. (2012). Neurological diseases and pain. Brain 135, 320–344. 10.1093/brain/awr271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brenner T., Soffer D., Shalit M., Levi-Schaffer F. (1994). Mast cells in experimental allergic encephalomyelitis: characterization, distribution in the CNS and in vitro activation by myelin basic protein and neuropeptides. J. Neurol. Sci. 122, 210–213. 10.1016/0022-510X(94)90300-X [DOI] [PubMed] [Google Scholar]
- Brites D., Fernandes A. (2015). Neuroinflammation and depression: microglia activation, extracellular microvesicles and microRNA dysregulation. Front. Cell. Neurosci. 9:476. 10.3389/fncel.2015.00476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brites D., Vaz A. R. (2014). Microglia centered pathogenesis in ALS: insights in cell interconnectivity. Front. Cell. Neurosci. 8:117. 10.3389/fncel.2014.00117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brotini S., Schievano C., Guidi L. (2017). Ultra-micronized palmitoylethanolamide: an efficacious adjuvant therapy for Parkinson's disease. CNS Neurol. Disord. Drug Targets 16, 705–713. 10.2174/1871527316666170321124949 [DOI] [PubMed] [Google Scholar]
- Buchanan M. M., Hutchinson M., Watkins L. R., Yin H. (2010). Toll-like receptor 4 in CNS pathologies. J. Neurochem. 114, 13–27. 10.1111/j.1471-4159.2010.06736.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckley C. D., Gilroy D. W., Serhan C. N., Stockinger B., Tak P. P. (2013). The resolution of inflammation. Nat. Rev. Immunol. 13, 59–66. 10.1038/nri3362 [DOI] [PubMed] [Google Scholar]
- Bulanova E., Bulfone-Paus S. (2010). P2 receptor-mediated signaling in mast cell biology. Purinergic Signal. 6, 3–17. 10.1007/s11302-009-9173-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bulfone-Paus S., Bahri R. (2015). Mast cells as regulators of T cell responses. Front. Immunol. 6:394. 10.3389/fimmu.2015.00394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bunnett N. W. (2006). Protease-activated receptors: how proteases signal to cells to cause inflammation and pain. Semin. Thromb. Hemost. 32, 39–48. 10.1055/s-2006-939553 [DOI] [PubMed] [Google Scholar]
- Burnstock G. (2016). Purinergic mechanisms and pain. Adv. Pharmacol. 7, 91–137. 10.1016/bs.apha.2015.09.001 [DOI] [PubMed] [Google Scholar]
- Bushell T. (2007). The emergence of proteinase-activated receptor-2 as a novel target for the treatment of inflammation-related CNS disorders. J. Physiol. 581, 7–16. 10.1113/jphysiol.2007.129577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cadot P., Hensel P., Bensignor E., Hadjaje C., Marignac G., Beco L., et al. (2011). Masitinib decreases signs of canine atopic dermatitis: a multicentre, randomized, double-blind, placebo-controlled phase 3 trial. Vet. Dermatol. 22, 554–564. 10.1111/j.1365-3164.2011.00990.x [DOI] [PubMed] [Google Scholar]
- Calcia M. A., Bonsall D. R., Bloomfield P. S., Selvaraj S., Barichello T., Howes O. D. (2016). Stress and neuroinflammation: a systematic review of the effects of stress on microglia and the implications for mental illness. Psychopharmacology 233, 1637–1650. 10.1007/s00213-016-4218-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calsolaro V., Edison P. (2016). Neuroinflammation in Alzheimer's disease: current evidence and future directions. Alzheimers Dement. 12, 719–732. 10.1016/j.jalz.2016.02.010 [DOI] [PubMed] [Google Scholar]
- Caltagirone C., Cisari C., Schievano C., Di Paola R., Cordaro M., Bruschetta G., et al. (2016). Co-ultramicronized palmitoylethanolamide/luteolin in the treatment of cerebral ischemia: from rodent to man. Transl. Stroke Res. 7, 54–69. 10.1007/s12975-015-0440-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cameron B., Landreth G. E. (2010). Inflammation, microglia, and Alzheimer's disease. Neurobiol. Dis. 37, 503–509. 10.1016/j.nbd.2009.10.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell B. M., Charych E., Lee A. W., Möller T. (2014). Kynurenines in CNS disease: regulation by inflammatory cytokines. Front. Neurosci. 8:12. 10.3389/fnins.2014.00012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao J., Papadopoulou N., Kempuraj D., Boucher W. S., Sugimoto K., Cetrulo C. L., et al. (2005). Human mast cells express corticotropin-releasing hormone (CRH) receptors and CRH leads to selective secretion of vascular endothelial growth factor. J. Immunol. 174, 7665–7675. 10.4049/jimmunol.174.12.7665 [DOI] [PubMed] [Google Scholar]
- Carraway R., Cochrane D. E., Lansman J. B., Leeman S. E., Paterson B. M., Welch H. J. (1982). Neurotensin stimulates exocytotic histamine secretion from rat mast cells and elevates plasma histamine levels. J. Physiol. 323, 403–414. 10.1113/jphysiol.1982.sp014080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castanon N., Luheshi G., Layé S. (2015). Role of neuroinflammation in the emotional and cognitive alterations displayed by animal models of obesity. Front. Neurosci. 9:229. 10.3389/fnins.2015.00229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castellheim A., Brekke O. L., Espevik T., Harboe M., Mollnes T. E. (2009). Innate immune responses to danger signals in systemic inflammatory response syndrome and sepsis. Scand. J. Immunol. 69, 479–491. 10.1111/j.1365-3083.2009.02255.x [DOI] [PubMed] [Google Scholar]
- Casula M., Iyer A. M., Spliet W. G., Anink J. J., Steentjes K., Sta M., et al. (2011). Toll-like receptor signaling in amyotrophic lateral sclerosis spinal cord tissue. Neuroscience 179, 233–243. 10.1016/j.neuroscience.2011.02.001 [DOI] [PubMed] [Google Scholar]
- Chakraborty S., Kaushik D. K., Gupta M., Basu A. (2010). Inflammasome signaling at the heart of central nervous system pathology. J. Neurosci. Res. 88, 1615–1631. 10.1002/jnr.22343 [DOI] [PubMed] [Google Scholar]
- Chan-Ling T., Hughes S., Baxter L., Rosinova E., McGregor I., Morcos Y., et al. (2007). Inflammation and breakdown of the blood-retinal barrier during “physiological aging” in the rat retina: a model for CNS aging. Microcirculation 14, 63–76. 10.1080/10739680601073451 [DOI] [PubMed] [Google Scholar]
- Chen J., Buchanan J. B., Sparkman N. L., Godbout J. P., Freund G. G., Johnson R. W. (2008). Neuroinflammation and disruption in working memory in aged mice after acute stimulation of the peripheral innate immune system. Brain Behav. Immun. 22, 301–311. 10.1016/j.bbi.2007.08.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y. J., Hill S., Huang H., Taraboletti A., Cho K., Gallo R., et al. (2014). Inflammation triggers production of dimethylsphingosine from oligodendrocytes. Neuroscience 279, 113–121. 10.1016/j.neuroscience.2014.08.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chirchiglia D., Chirchiglia P., Signorelli F. (2018). Nonsurgical lumbar radiculopathies treated with ultramicronized palmitoylethanolamide (umPEA): a series of 100 cases. Neurol. Neurochir. Pol. 52, 44–47. 10.1016/j.pjnns.2017.11.002 [DOI] [PubMed] [Google Scholar]
- Christophi G. P., Gruber R. C., Panos M., Christophi R. L., Jubelt B., Massa P. T. (2012). Interleukin-33 upregulation in peripheral leukocytes and CNS of multiple sclerosis patients. Clin. Immunol. 142, 308–319. 10.1016/j.clim.2011.11.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christy A. L., Walker M. E., Hessner M. J., Brown M. A. (2013). Mast cell activation and neutrophil recruitment promotes early and robust inflammation in the meninges in EAE. J. Autoimmun. 42, 50–61. 10.1016/j.jaut.2012.11.003 [DOI] [PubMed] [Google Scholar]
- Clemente S. (2012). Amyotrophic lateral sclerosis treatment with ultramicronized palmitoylethanolamide: a case report. CNS Neurol. Disord. Drug Targets 11, 933–936. 10.2174/1871527311201070933 [DOI] [PubMed] [Google Scholar]
- Colloca L., Ludman T., Bouhassira D., Baron R., Dickenson A. H., Yarnitsky D., et al. (2017). Neuropathic pain. Nat. Rev. Dis. Primers 16:3 10.1038/nrdp.2017.2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compston A., Coles A. (2008). Multiple sclerosis. Lancet 372, 1502–1517. 10.1016/S0140-6736(08)61620-7 [DOI] [PubMed] [Google Scholar]
- Comrie W. A., Burkhardt J. K. (2016). Action and traction: cytoskeletal control of receptor triggering at the immunological synapse. Front. Immunol. 7:68. 10.3389/fimmu.2016.00068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Constandil L., Aguilera R., Goich M., Hernández A., Alvarez P., Infante C., et al. (2011). Involvement of spinal cord BDNF in the generation and maintenance of chronic neuropathic pain in rats. Brain Res. Bull. 86, 454–459. 10.1016/j.brainresbull.2011.08.008 [DOI] [PubMed] [Google Scholar]
- Conti P., Kempuraj D. (2016). Important role of mast cells in multiple sclerosis. Mult. Scler. Relat. Disord. 5, 77–80. 10.1016/j.msard.2015.11.005 [DOI] [PubMed] [Google Scholar]
- Coull J. A., Beggs S., Boudreau D., Boivin D., Tsuda M., Inoue K., et al. (2005). BDNF from microglia causes the shift in neuronal anion gradient underlying neuropathic pain. Nature 438, 1017–1021. 10.1038/nature04223 [DOI] [PubMed] [Google Scholar]
- Cravatt B. F., Giang D. K., Mayfield S. P., Boger D. L., Lerner R. A., Gilula N. B. (1996). Molecular characterization of an enzyme that degrades neuromodulatory fatty-acid amides. Nature 384, 83–87. 10.1038/384083a0 [DOI] [PubMed] [Google Scholar]
- Cunningham C. (2013). Microglia and neurodegeneration: the role of systemic inflammation. Glia 61, 71–90. 10.1002/glia.22350 [DOI] [PubMed] [Google Scholar]
- D'Agostino G., La Rana G., Russo R., Sasso O., Iacono A., Esposito E., et al. (2007). Acute intracerebroventricular administration of palmitoylethanolamide, an endogenous peroxisome proliferator-activated receptor-alpha agonist, modulates carrageenan-induced paw edema in mice. J. Pharmacol. Exp. Ther. 322, 1137–1143. 10.1124/jpet.107.123265 [DOI] [PubMed] [Google Scholar]
- da Silva E. Z., Jamur M. C., Oliver C. (2014). Mast cell function: a new vision of an old cell. J. Histochem. Cytochem. 62, 698–738. 10.1369/0022155414545334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Del Giorno R., Skaper S., Paladini A., Varrassi G., Coaccioli S. (2015). Palmitoylethanolamide in fibromyalgia: results from prospective and retrospective observational studies. Pain Ther. 4, 169–178. 10.1007/s40122-015-0038-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dirckx M., Groeneweg G., van Daele P. L., Stronks D. L., Huygen F. J. (2013). Mast cells: a new target in the treatment of complex regional pain syndrome? Pain Pract. 13, 599–603. 10.1111/papr.12049 [DOI] [PubMed] [Google Scholar]
- Donath M. Y. (2014). Targeting inflammation in the treatment of type 2 diabetes: time to start. Nat. Rev. Drug Discov. 13, 465–476. 10.1038/nrd4275 [DOI] [PubMed] [Google Scholar]
- Done J. D., Rudick C. N., Quick M. L., Schaeffer A. J., Thumbikat P. (2012). Role of mast cells in male chronic pelvic pain. J. Urol. 187, 1473–1482. 10.1016/j.juro.2011.11.116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong H., Zhang X., Wang Y., Zhou X., Qian Y., Zhang S. (2017). Suppression of brain mast cells degranulation inhibits microglial activation and central nervous system inflammation. Mol. Neurobiol. 54, 997–1007. 10.1007/s12035-016-9720-x [DOI] [PubMed] [Google Scholar]
- Dowlati Y., Herrmann N., Swardfager W., Liu H., Sham L., Reim E. K., et al. (2010). A meta-analysis of cytokines in major depression. Biol. Psychiatry 67, 446–457. 10.1016/j.biopsych.2009.09.033 [DOI] [PubMed] [Google Scholar]
- Dubreuil P., Letard S., Ciufolini M., Gros L., Humbert M., Castéran N., et al. (2009). Masitinib (AB1010), a potent and selective tyrosine kinase inhibitor targeting KIT. PLoS ONE 4:7258. 10.1371/journal.pone.0007258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dudeck A., Suender C. A., Kostka S. L., von Stebut E., Maurer M. (2011). Mast cells promote Th1 and Th17 responses by modulating dendritic cell maturation and function. Eur. J. Immunol. 41, 1883–1893. 10.1002/eji.201040994 [DOI] [PubMed] [Google Scholar]
- Echeverry S., Shi X. Q., Yang M., Huang H., Wu Y., Lorenzo L. E., et al. (2017). Spinal microglia are required for long-term maintenance of neuropathic pain. Pain 158, 1792–1801. 10.1097/j.pain.0000000000000982 [DOI] [PubMed] [Google Scholar]
- Eggen B. J., Raj D., Hanisch U. K., Boddeke H. W. (2013). Microglial phenotype and adaptation. J. Neuroimmune Pharmacol. 8, 807–823. 10.1007/s11481-013-9490-4 [DOI] [PubMed] [Google Scholar]
- El-Behi M., Ciric B., Dai H., Yan Y., Cullimore M., Safavi F., et al. (2011). The encephalitogenicity of T(H)17 cells is dependent on IL-1- and IL-23-induced production of the cytokine GM-CSF. Nat. Immunol. 12, 568–575. 10.1038/ni.2031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elieh Ali Komi D., Grauwet K. (2017). Role of mast cells in regulation of T cell responses in experimental and clinical settings. Clin. Rev. Allergy Immunol. [Epub ahead of print]. 10.1007/s12016-017-8646-z [DOI] [PubMed] [Google Scholar]
- Ellis A., Bennett D. L. (2014). Neuroinflammation and the generation of neuropathic pain. 2013. Br. J. Anaesth. 111, 26–37. 10.1093/bja/aet128 [DOI] [PubMed] [Google Scholar]
- Engler H., Brendt P., Wischermann J., Wegner A., Röhling R., Schoemberg T., et al. (2017). Selective increase of cerebrospinal fluid IL-6 during experimental systemic inflammation in humans: association with depressive symptoms. Mol. Psychiatry 22, 1448–1454. 10.1038/mp.2016.264 [DOI] [PubMed] [Google Scholar]
- Ertürk A., Mentz S., Stout E. E., Hedehus M., Dominguez S. L., Neumaier L., et al. (2016). Interfering with the chronic immune response rescues chronic degeneration after traumatic brain injury. J. Neurosci. 36, 9962–9975. 10.1523/JNEUROSCI.1898-15.2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esposito E., Cordaro M., Cuzzocrea S. (2014). Roles of fatty acid ethanolamides (FAE) in traumatic and ischemic brain injury. Pharmacol. Res. 86, 26–31. 10.1016/j.phrs.2014.05.009 [DOI] [PubMed] [Google Scholar]
- Esposito P., Gheorghe D., Kandere K., Pang X., Connolly R., Jacobson S., et al. (2001). Acute stress increases permeability of the blood-brain-barrier through activation of brain mast cells. Brain Res. 888, 117–127. 10.1016/S0006-8993(00)03026-2 [DOI] [PubMed] [Google Scholar]
- Facci L., Barbierato M., Marinelli C., Argentini C., Skaper S. D., Giusti P. (2014). Toll-like receptors 2,−3 and−4 prime microglia but not astrocytes across central nervous system regions for ATP-dependent interleukin-1β release. Sci. Rep. 4:6824 10.1038/srep06824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Facci L., Dal Toso R., Romanello S., Buriani A., Skaper S. D., Leon A. (1995). Mast cells express a peripheral cannabinoid receptor with differential sensitivity to anandamide and palmitoylethanolamide. Proc. Natl. Acad. Sci. U.S.A. 92, 3376–3380. 10.1073/pnas.92.8.3376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faith M. S., Butryn M., Wadden T. A., Fabricatore A., Nguyen A. M., et al. (2011). Evidence for prospective associations among depression and obesity in population-based studies. Obes. Rev. 12:e438-53. 10.1111/j.1467-789X.2010.00843.x [DOI] [PubMed] [Google Scholar]
- Feinstein A., Magalhaes S., Richard J. F., Audet B., Moore C. (2014). The link between multiple sclerosis and depression. Nat. Rev. Neurol. 10, 507–517. 10.1038/nrneurol.2014.139 [DOI] [PubMed] [Google Scholar]
- Fiala M., Chattopadhay M., La Cava A., Tse E., Liu G., Lourenco E., et al. (2010). IL-17A is increased in the serum and in spinal cord CD8 and mast cells of ALS patients. J. Neuroinflammation 7:76. 10.1186/1742-2094-7-76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fidaleo M., Fanelli F., Ceru M. P., Moreno S. (2014). Neuroprotective properties of peroxisome proliferator-activated receptor alpha (PPARα) and its lipid ligands. Curr. Med. Chem. 21, 2803–2821. 10.2174/0929867321666140303143455 [DOI] [PubMed] [Google Scholar]
- Florenzano F., Bentivoglio M. (2000). Degranulation, density, and distribution of mast cells in the rat thalamus: a light and electron microscopic study in basal conditions and after intracerebroventricular administration of nerve growth factor. J. Comp. Neurol. 424, 651–669. [DOI] [PubMed] [Google Scholar]
- Folch J., Petrov D., Ettcheto M., Pedrós I., Abad S., Beas-Zarate C., et al. (2015). Masitinib for the treatment of mild to moderate Alzheimer's disease. Expert Rev. Neurother. 15, 587–596. 10.1586/14737175.2015.1045419 [DOI] [PubMed] [Google Scholar]
- Fonken L. K., Frank M. G., Kitt M. M., D'Angelo H. M., Norden D. M., Weber M. D., et al. (2016). The alarmin HMGB1 mediates age-induced neuroinflammatory priming. J. Neurosci. 36, 7946–7956. 10.1523/JNEUROSCI.1161-16.2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freeman L. C., Ting J. P. (2016). The pathogenic role of the inflammasome in neurodegenerative diseases J. Neurochem. 136(Suppl. 1), 29–38. 10.1111/jnc.13217 [DOI] [PubMed] [Google Scholar]
- Franklin A., Parmentier-Batteur S., Walter L., Greenberg D. A., Stella N. (2003). Palmitoylethanolamide increases after focal cerebral ischemia and potentiates microglial cell motility. J. Neurosci. 23, 7767–7775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Füger P., Hefendehl J. K., Veeraraghavalu K., Wendeln A. C., Schlosser C., Obermüller U., et al. (2017). Microglia turnover with aging and in an Alzheimer's model via long-term in vivo single-cell imaging. Nat. Neurosci. 20, 1371–1376. 10.1038/nn.4631 [DOI] [PubMed] [Google Scholar]
- Fullerton J. N., Gilroy D. W. (2016). Resolution of inflammation: a new therapeutic frontier. Nat. Rev. Drug Discov. 15, 551–567. 10.1038/nrd.2016.39 [DOI] [PubMed] [Google Scholar]
- Gabbay V., Ely B. A., Babb J., Liebes L. (2012). The possible role of the kynurenine pathway in anhedonia in adolescents. J. Neural Transm. 119, 253–260. 10.1007/s00702-011-0685-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ganeshan K., Bryce P. J. (2012). Regulatory T cells enhance mast cell production of IL-6 via surface-bound TGF-β. J. Immunol. 188, 594–603. 10.4049/jimmunol.1102389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao Y. J., Ji R. R. (2010). Targeting astrocyte signaling for chronic pain. Neurotherapeutics 27, 482–493. 10.1016/j.nurt.2010.05.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gasque P., Singhrao S. K., Neal J. W., Götze O., Morgan B. P. (1997). Expression of the receptor for complement C5a (CD88) is up-regulated on reactive astrocytes, microglia, and endothelial cells in the inflamed human central nervous system. Am. J. Pathol. 150, 31–41. [PMC free article] [PubMed] [Google Scholar]
- Gaudenzio N., Espagnolle N., Mars L. T., Liblau R., Valitutti S., Espinosa E. (2009). Cell-cell cooperation at the T helper cell/mast cell immunological synapse. Blood 114, 4979–4988. 10.1182/blood-2009-02-202648 [DOI] [PubMed] [Google Scholar]
- Geloso M. C., Corvino V., Marchese E., Serrano A., Michetti F., D'Ambrosi N. (2017). The dual role of microglia in ALS: mechanisms and therapeutic approaches. Front. Aging Neurosci. 9:242. 10.3389/fnagi.2017.00242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Georgin-Lavialle S., Moura D. S., Salvador A., Chauvet-Gelinier J. C., Launay J. M., Damaj G., et al. (2016). Mast cells' involvement in inflammation pathways linked to depression: evidence in mastocytosis. Mol. Psychiatry 21, 1511–1516. 10.1038/mp.2015.216 [DOI] [PubMed] [Google Scholar]
- Gilfillan A. M., Austin S. J., Metcalfe D. D. (2011). Mast cell biology: introduction and overview. Adv. Exp. Med. Biol. 716, 2–12. 10.1007/978-1-4419-9533-9_1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gosselin R. D., Suter M. R., Ji R. R., Decosterd I. (2010). Glial cells and chronic pain. Neuroscientist 16, 519–531. 10.1177/1073858409360822 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grace P. M., Hutchinson M. R., Maier S. F., Watkins L. R. (2014). Pathological pain and the neuroimmune interface. Nat. Rev. Immunol. 14, 217–231. 10.1038/nri3621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grakoui A., Bromley S. K., Sumen C., Davis M. M., Shaw A. S., Allen P. M., et al. (1999). The immunological synapse: a molecular machine controlling T cell activation. Science 285, 221–227. 10.1126/science.285.5425.221 [DOI] [PubMed] [Google Scholar]
- Graziottin A., Skaper S. D., Fusco M. (2014). Mast cells in chronic inflammation, pelvic pain and depression in women. Gynecol. Endocrinol. 30, 472–477. 10.3109/09513590.2014.911280 [DOI] [PubMed] [Google Scholar]
- Griffin R. S., Costigan M., Brenner G. J., Ma C. H., Scholz J., Moss A., et al. (2007). Complement induction in spinal cord microglia results in anaphylatoxin C5a-mediated pain hypersensitivity. J. Neurosci. 27, 8699–8708. 10.1523/JNEUROSCI.2018-07.2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grinspan J. (2002). Cells and signaling in oligodendrocyte development. J. Neuropathol. Exp. Neurol. 61, 297–306. 10.1093/jnen/61.4.297 [DOI] [PubMed] [Google Scholar]
- Gritsch S., Lu J., Thilemann S., Wörtge S., Möbius W., Bruttger J., et al. (2014). Oligodendrocyte ablation triggers central pain independently of innate or adaptive immune responses in mice. Nat. Commun. 5:5472 10.1038/ncomms6472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grützkau A., Krüger-Krasagakes S., Baumeister H., Schwarz C., Kögel H., Welker P., et al. (2012). Synthesis, storage, and release of vascular endothelial growth factor/vascular permeability factor (VEGF/VPF) by human mast cells: implications for the biological significance of VEGF206. Mol. Biol. Cell 9, 875–884. 10.1091/mbc.9.4.875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagberg H., Gressens P., Mallard C. (2012). Inflammation during fetal and neonatal life: implications for neurologic and neuropsychiatric disease in children and adults. Ann. Neurol. 71, 444–457. 10.1002/ana.22620 [DOI] [PubMed] [Google Scholar]
- Hains L. E., Loram L. C., Weiseler J. L., Frank M. G., Bloss E. B., Sholar P., et al. (2010). Pain intensity and duration can be enhanced by prior challenge: initial evidence suggestive of a role of microglial priming. J. Pain 11, 1004–1114. 10.1016/j.jpain.2010.01.271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haley M. J., Brough D., Quintin J., Allan S. M. (2018). Microglial priming as trained immunity in the brain. Neuroscience. [Epub ahead of print]. 10.1016/j.neuroscience.2017.12.039 [DOI] [PubMed] [Google Scholar]
- Hall E. D., Oostveen J. A., Gurney M. E. (1998). Relationship of microglial and astrocytic activation to disease onset and progression in a transgenic model of familial ALS. Glia 23, 249–256. [DOI] [PubMed] [Google Scholar]
- Hammad A., Westacott L., Zaben M. (2018). The role of the complement system in traumatic brain injury: a review. J. Neuroinflammation 15:24 10.1186/s12974-018-1066-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanisch U. K., Kettenmann H. (2007). Microglia: active sensor and versatile effector cells in the normal and pathologic brain. Nat. Neurosci. 10, 1387–1394. 10.1038/nn1997 [DOI] [PubMed] [Google Scholar]
- Harcha P. A., Vargas A., Yi C., Koulakoff A. A., Giaume C., Sáez J. C. (2015). Hemichannels are required for amyloid β-peptide-induced degranulation and are activated in brain mast cells of APPswe/PS1dE9 mice. J. Neurosci. 35, 9526–9538. 10.1523/JNEUROSCI.3686-14.2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harms A. S., Cao S., Rowse A. L., Thome A. D., Li X., Mangieri L. R., et al. (2013). MHCII is required for α-synuclein-induced activation of microglia, CD4 T cell proliferation, and dopaminergic neurodegeneration. J. Neurosci. 33, 9592–9600. 10.1523/JNEUROSCI.5610-12.2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayashi R., Xiao W., Kawamato M., Yuge O., Bennett G. J. (2011). Systemic glucocorticoid therapy reduces pain and the number of endoneurial tumor necrosis factor-alpha (TNFα)-positive mast cells in rats with a painful peripheral neuropathy. J. Pharmacol. Sci. 106, 559–565. 10.1254/jphs.FP0072181 [DOI] [PubMed] [Google Scholar]
- Hendriksen E., van Bergeijk D., Oosting R. S., Redegeld F. A. (2017). Mast cells in neuroinflammation and brain disorders. Neurosci. Biobehav. Rev. 79, 119–133. 10.1016/j.neubiorev.2017.05.001 [DOI] [PubMed] [Google Scholar]
- Heneka M. T., Carson M. J., El Khoury J., Landreth G. E., Brosseron F., Feinstein D. L., et al. (2015). Neuroinflammation in Alzheimer's disease. Lancet Neurol. 14, 388–405. 10.1016/S1474-4422(15)70016-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herbert M. R. (2005). Large brains in autism: the challenge of pervasive abnormality. Neuroscientist 11, 417–440. 10.1177/0091270005278866 [DOI] [PubMed] [Google Scholar]
- Hermine O., Lortholary O., Leventhal P. S., Catteau A., Soppelsa F., Baude C., et al. (2008). Case-control cohort study of patients' perceptions of disability in mastocytosis. PLoS ONE 3:e2266. 10.1371/journal.pone.0002266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Héron A., Dubayle D. (2013). A focus on mast cells and pain. J. Neuroimmunol. 264, 1–7. 10.1016/j.jneuroim.2013.09.018 [DOI] [PubMed] [Google Scholar]
- Herrera A. J., Espinosa-Oliva A. M., Carrillo-Jiménez A., Oliva-Martín M. J., García-Revilla J., García-Quintanilla A., et al. (2015). Relevance of chronic stress and the two faces of microglia in Parkinson's disease. Front. Cell. Neurosci. 9:312. 10.3389/fncel.2015.00312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heuberger R. A. (2011). The frailty syndrome: a comprehensive review. J. Nutr. Gerontol. Geriatr. 30, 315–368. 10.1080/21551197.2011.623931 [DOI] [PubMed] [Google Scholar]
- Hickman S. E., Kingery N. D., Ohsumi T. K., Borowsky M. L., Wang L. C., Means T. K., et al. (2013). The microglial sensome revealed by direct RNA sequencing. Nat. Neurosci. 16, 1896–1905. 10.1038/nn.3554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirsch L., Jette N., Frolkis A., Steeves T., Pringsheim T. (2016). The incidence of Parkinson's disease: a systematic review and meta-analysis. Neuroepidemiology 46, 292–300. 10.1159/000445751 [DOI] [PubMed] [Google Scholar]
- Hoeijmakers L., Heinen Y., van Dam A. M., Lucassen P. J., Korosi A. (2016). Microglial priming and Alzheimer's disease: a possible role for (early) immune challenges and epigenetics? Front. Hum. Neurosci. 10:398. 10.3389/fnhum.2016.00398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoeijmakers L., Ruigrok S. R., Amelianchik A., Ivan D., Van Dam A. M., Lucassen P. J., et al. (2017). Early-life stress lastingly alters the neuroinflammatory response to amyloid pathology in an Alzheimer's disease mouse model. Brain Behav. Immun. 63, 160–175. 10.1016/j.bbi.2016.12.023 [DOI] [PubMed] [Google Scholar]
- Holmin S., Mathiesen T. (1999). Long-term intracerebral inflammatory response after experimental focal brain injury in rat. Neuroreport 10, 1889–1891. 10.1097/00001756-199906230-00017 [DOI] [PubMed] [Google Scholar]
- Hong S., Beja-Glasser V. F., Nfonoyim B. M., Frouin A., Li S., Ramakrishnan S., et al. (2016). Complement and microglia mediate early synapse loss in Alzheimer mouse models. Science 352, 712–716. 10.1126/science.aad8373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu W., Xu L., Pan J., Zheng X., Chen Z. (2004). Effect of cerebral ischemia on brain mast cells in rats. Brain Res. 1019, 275–280. 10.1016/j.brainres.2004.05.109 [DOI] [PubMed] [Google Scholar]
- Iadecola C., Anrather J. (2011). The immunology of stroke: from mechanisms to translation. Nat. Med. 17, 796–808. 10.1038/nm.2399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Impellizzeri D., Bruschetta G., Cordaro M., Crupi R., Siracusa R., Esposito E., et al. (2014). Micronized/ultramicronized palmitoylethanolamide displays superior oral efficacy compared to non-micronized palmitoylethanolamide in a rat model of inflammatory pain. J. Neuroinflammation 11:136 10.1186/s12974-014-0136-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Indraccolo U., Indraccolo S. R., Mignini F. (2017). Micronized palmitoylethanolamide/trans-polydatin treatment of endometriosis-related pain: a meta-analysis. Ann. Ist Super. Sanita 53, 125–134. 10.4415/ANN_17_02_08 [DOI] [PubMed] [Google Scholar]
- Iuvone T., Affaitati G., De Filippis D., Lopopolo M., Grassia G., Lapenna D., et al. (2016). Ultramicronized palmitoylethanolamide reduces viscerovisceral hyperalgesia in a rat model of endometriosis plus ureteral calculosis: role of mast cells. Pain 157, 80–91. 10.1097/j.pain.0000000000000220 [DOI] [PubMed] [Google Scholar]
- Jackson N. E., Wang H. W., Tedla N., McNeil H. P., Geczy C. L., Collins A., et al. (2005). IL-15 induces mast cell migration via a pertussis toxin-sensitive receptor. Eur. J. Immunol. 35, 2376–2385. 10.1002/eji.200526154 [DOI] [PubMed] [Google Scholar]
- Jang S. Y., Shin Y. K., Lee H. Y., Park J. Y., Suh D. J., Kim J. K., et al. (2012). Local production of serum amyloid a is implicated in the induction of macrophage chemoattractants in Schwann cells during wallerian degeneration of peripheral nerves. Glia 60, 1619–1628. 10.1002/glia.22382 [DOI] [PubMed] [Google Scholar]
- Jay G. W., Barkin R. L. (2014). Neuropathic pain: etiology, pathophysiology, mechanisms, and evaluations. Dis. Mon. 60, 6–47. 10.1016/j.disamonth.2013.12.001 [DOI] [PubMed] [Google Scholar]
- Jensen C. J., Massie A., De Keyser J. (2013). Immune players in the CNS: the astrocyte. J. Neuroimmune Pharmacol. 8, 824–839. 10.1007/s11481-013-9480-6 [DOI] [PubMed] [Google Scholar]
- Ji R. R., Berta T., Nedergaard M. (2013). Glia and pain: is chronic pain a gliopathy? Pain 154(Suppl. 1), S10–S28. 10.1016/j.pain.2013.06.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ji R. R., Xu Z. Z., Gao Y. J. (2014). Emerging targets in neuroinflammation-driven chronic pain. Nat. Rev. Drug Discov. 13, 533–548. 10.1038/nrd4334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jin Y., Silverman A. J., Vannucci S. J. (2007). Mast cell stabilization limits hypoxic-ischemic brain damage in the immature rat. Dev. Neurosci. 29, 373–384. 10.1159/000105478 [DOI] [PubMed] [Google Scholar]
- Jin Y., Silverman A. J., Vannucci S. J. (2009). Mast cells are early responders after hypoxia-ischemia in immature rat brain. Stroke 40, 3107–3112. 10.1161/STROKEAHA.109.549691 [DOI] [PubMed] [Google Scholar]
- Johnson V. E., Stewart J. E., Begbie F. D., Trojanowski J. Q., Smith D. H., Stewart W. (2013). Inflammation and white matter degeneration persist for years after a single traumatic brain injury. Brain 136, 28–42. 10.1093/brain/aws322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jordán J., Segura T., Brea D., Galindo M. F., Castillo J. (2008). Inflammation as therapeutic objective in stroke. Curr. Pharm. Des. 14, 3549–3564. 10.2174/138161208786848766 [DOI] [PubMed] [Google Scholar]
- Juremalm M., Hjertson M., Olsson N., Harvima I., Nilsson K., Nilsson G. (2000). The chemokine receptor CXCR4 is expressed within the mast cell lineage and its ligand stromal cell-derived factor-1alpha acts as a mast cell chemotaxin. Eur. J. Immunol. 30, 3614–3622. 10.1002/1521-4141(200012)30:12 [DOI] [PubMed] [Google Scholar]
- Khan N., Smith M. T. (2015). Neurotrophins and neuropathic pain: role in pathobiology. Molecules 20, 10657–10688. 10.3390/molecules200610657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalesnikoff J., Galli S. J. (2008). New developments in mast cell biology. Nat. Immunol. 9, 1215–1223. 10.1038/ni.f.216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaltschmidt B., Uherek M., Volk B., Baeuerle P. A., Kaltschmidt C. (1997). Transcription factor NF-κB is activated in primary neurons by amyloid beta peptides and in neurons surrounding early plaques from patients with Alzheimer disease. Proc. Natl. Acad. Sci. U.S.A. 94, 2642–2647. 10.1073/pnas.94.6.2642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamm C. P., Uitdehaag B. M., Polman C. H. (2014). Multiple sclerosis: current knowledge and future outlook. Eur. Neurol. 72, 132–141. 10.1159/000360528 [DOI] [PubMed] [Google Scholar]
- Kan J., Mishima S., Kashiwakura J. I., Sasaki-Sakamoto T., Seki M., Saito S., et al. (2016). Interleukin-17A expression in human synovial mast cells in rheumatoid arthritis and osteoarthritis. Allergol. Int. 65, S11–S16. 10.1016/j.alit.2016.04.007 [DOI] [PubMed] [Google Scholar]
- Karagkouni A., Alevizos M., Theoharides T. C. (2013). Effect of stress on brain inflammation and multiple sclerosis. Autoimmun. Rev. 12, 947–953. 10.1016/j.autrev.2013.02.006 [DOI] [PubMed] [Google Scholar]
- Karve I. P., Taylor J. M., Crack P. J. (2016). The contribution of astrocytes and microglia to traumatic brain injury. Br. J. Pharmacol. 173, 692–702. 10.1111/bph.13125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawasaki H., Chang H. W., Tseng H. C., Hsu S. C., Yang S. J., Hung C. H., et al. (2014). A tryptophan metabolite, kynurenine, promotes mast cell activation through aryl hydrocarbon receptor. Allergy 69, 445–452. 10.1111/all.12346 [DOI] [PubMed] [Google Scholar]
- Kelleher J. H., Tewari D., McMahon S. B. (2016). Neurotrophic factors and their inhibitors in chronic pain treatment. Neurobiol. Dis. 97, 127–138. 10.1016/j.nbd.2016.03.025 [DOI] [PubMed] [Google Scholar]
- Kempuraj D., Thangavel R., Fattal R., Pattani S., Yang E., Zaheer S., et al. (2016). Mast cells release chemokine CCL2 in response to parkinsonian toxin 1-methyl-4-phenyl-pyridinium (MPP(+)). Neurochem. Res. 41, 1042–1049. 10.1007/s11064-015-1790-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kempuraj D., Thangavel R., Selvakumar G. P., Zaheer S., Ahmed M. E., Raikwar S. P., et al. (2017). Brain and peripheral atypical inflammatory mediators potentiate neuroinflammation and neurodegeneration. Front. Cell. Neurosci. 11:216. 10.3389/fncel.2017.00216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kempuraj D., Selvakumar G. P., Zaheer S., Thangavel R., Ahmed M. E., Raikwar S., et al. (2018). Cross-talk between glia, neurons and mast cells in neuroinflammation associated with Parkinson's disease. J. Neuroimmune Pharmacol. 13, 100–112. 10.1007/s11481-017-9766-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kermode A. G., Thompson A. J., Tofts P., MacManus D. G., Kendall B. E., Kingsley D. P. E., et al. (1990). Breakdown of the blood-brain barrier precedes symptoms and other MRI signs of new lesions in multiple sclerosis. Brain 113, 1477–1489. 10.1093/brain/113.5.1477 [DOI] [PubMed] [Google Scholar]
- Kern J. K., Geier D. A., Sykes L. K., Geier M. R. (2016). Relevance of neuroinflammation and encephalitis in autism. Front. Cell. Neurosci. 9:519. 10.3389/fncel.2015.00519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerstman E., Ahn S., Battu S., Tariq S., Grabois M. (2013). Neuropathic pain. Handb. Clin. Neurol. 110, 175–187. 10.1016/B978-0-444-52901-5.00015-0 [DOI] [PubMed] [Google Scholar]
- Kim D. Y., Hong G. U., Ro J. Y. (2011). Signal pathways in astrocytes activated by cross-talk between of astrocytes and mast cells through CD40-CD40L. J. Neuroinflammation 8:25. 10.1186/1742-2094-8-25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim D. Y., Jeoung D., Ro J. Y. (2010). Signaling pathways in the activation of mast cells cocultured with astrocytes and colocalization of both cells in experimental allergic encephalomyelitis. J. Immunol. 185, 273–283. 10.4049/jimmunol.1000991 [DOI] [PubMed] [Google Scholar]
- Kim D., Kim M. A., Cho I. H., Kim M. S., Lee S., Jo E. K., et al. (2007). A critical role of toll-like receptor 2 in nerve injury-induced spinal cord glial cell activation and pain hypersensitivity. J. Biol. Chem. 282, 14975–14983. 10.1074/jbc.M607277200 [DOI] [PubMed] [Google Scholar]
- Kim S., Kim H., Yim Y. S., Ha S., Atarashi K., Tan T. G., et al. (2017). Maternal gut bacteria promote neurodevelopmental abnormalities in mouse offspring. Nature 549, 528–532. 10.1038/nature23910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J., Loggia M. L., Cahalan C. M., Harris R. E., Beissner F., Garcia R. G., et al. (2015). The somatosensory link in fibromyalgia: functional connectivity of the primary somatosensory cortex is altered by sustained pain and is associated with clinical/autonomic dysfunction. Arthritis Rheumatol. 67, 1395–1405. 10.1002/art.39043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimelberg H. K., Nedergaard M. (2010). Functions of astrocytes and their potential as therapeutic targets. Neurotherapeutics 7, 338–353. 10.1016/j.nurt.2010.07.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kindy M. S., Yu J., Guo J. T., Zhu H. (1999). Apolipoprotein serum amyloid A in Alzheimer's disease. J. Alzheimers Dis. 1, 155–167. 10.3233/JAD-1999-1303 [DOI] [PubMed] [Google Scholar]
- Kissel C. L., Kovács K. J., Larson A. A. (2017). Evidence for the modulation of nociception in mice by central mast cells. Eur. J. Pain. 21, 1743–1755. 10.1002/ejp.1086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiray H., Lindsay S. L., Hosseinzadeh S., Barnett S. C. (2016). The multifaceted role of astrocytes in regulating myelination. Exp. Neurol. 283, 541–549. 10.1016/j.expneurol.2016.03.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein K., Aeschlimann A., Jordan S., Gay R., Gay S., Sprott H. (2012). ATP induced brain-derived neurotrophic factor expression and release from osteoarthritis synovial fibroblasts is mediated by purinergic receptor P2X4. PLoS ONE 7:36693. 10.1371/journal.pone.0036693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knerlich-Lukoschus F., von der Ropp-Brenner B., Lucius R., Mehdorn H. M., Held-Feindt J. (2011). Spatiotemporal CCR1, CCL3(MIP-1α), CXCR4, CXCL12(SDF-1α) expression patterns in a rat spinal cord injury model of posttraumatic neuropathic pain. J. Neurosurg. Spine 14, 583–597. 10.3171/2010.12.SPINE10480 [DOI] [PubMed] [Google Scholar]
- Kobayashi K., Yamanaka H., Fukuoka T., Dai Y., Obata K., Noguchi K. (2008). P2Y12 receptor upregulation in activated microglia is a gateway of p38 signaling and neuropathic pain. J. Neurosci. 28, 2892–2902. 10.1523/JNEUROSCI.5589-07.2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kocic I., Kowianski P., Rusiecka I., Lietzau G., Mansfield C., Moussy A., et al. (2015). Neuroprotective effect of masitinib in rats with postischemic stroke. Naunyn Schmiedebergs Arch. Pharmacol. 388, 79–86. 10.1007/s00210-014-1061-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kolbinger F., Huppertz C., Mir A., Padova F. D. (2016). IL-17A and multiple sclerosis: signaling pathways, producing cells and target cells in the central nervous system. Curr. Drug Targets 17, 1882–1893. 10.2174/1389450117666160307144027 [DOI] [PubMed] [Google Scholar]
- Koshinaga M., Katayama Y., Fukushima M., Oshima H., Suma T., Takahata T. (2000). Rapid and widespread microglial activation induced by traumatic brain injury in rat brain slices. J. Neurotrauma 17, 185–192. 10.1089/neu.2000.17.185 [DOI] [PubMed] [Google Scholar]
- Kritas S. K., Saggini A., Cerulli G., Caraffa A., Antinolfi P., Pantalone A., et al. (2014a). Corticotropin-releasing hormone, microglia and mental disorders. Int. J. Immunopathol. Pharmacol. 27, 163–167. 10.1177/039463201402700203 [DOI] [PubMed] [Google Scholar]
- Kritas S. K., Saggini A., Cerulli G., Caraffa A., Antinolfi P., Pantalone A., et al. (2014b). Impact of mast cells on multiple sclerosis: inhibitory effect of natalizumab. Int. J. Immunopathol. Pharmacol. 27, 331–335. 10.1177/039463201402700303 [DOI] [PubMed] [Google Scholar]
- Kumar A., Stoica B. A., Loane D. J., Yang M., Abulwerdi G., Khan N., et al. (2017). Microglial-derived microparticles mediate neuroinflammation after traumatic brain injury. J. Neuroinflammation 14:47. 10.1186/s12974-017-0819-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Labzin L. I., Heneka M. T., Latz E. (2018). Innate immunity and neurodegeneration. Annu. Rev. Med. 69, 437–449. 10.1146/annurev-med-050715-104343 [DOI] [PubMed] [Google Scholar]
- Lall D., Baloh R. H. (2017). Microglia and C9orf72 in neuroinflammation and ALS and frontotemporal dementia. J. Clin. Invest. 127, 3250–3258. 10.1172/JCI90607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J., Hyeon S. J., Im H., Ryu H., Kim Y., Ryu H. (2016). Astrocytes and microglia as non-cell autonomous players in the pathogenesis of ALS. Exp. Neurobiol. 25, 233–240. 10.5607/en.2016.25.5.233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leon A., Buriani A., Dal Toso R., Fabris M., Romanello S., Aloe L., et al. (1994). Mast cells synthesize, store, and release nerve growth factor. Proc. Natl. Acad. Sci. U.S.A. 91, 3739–3743. 10.1073/pnas.91.9.3739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Thuc O., Blondeau N., Nahon J. L., Rovère C. (2015). The complex contribution of chemokines to neuroinflammation: switching from beneficial to detrimental effects. Ann. N.Y. Acad. Sci. 1351, 127–140. 10.1111/nyas.12855 [DOI] [PubMed] [Google Scholar]
- Leung D., Saghatelian A., Simon G. M., Cravatt B. F. (2006). Inactivation of N-acyl phosphatidylethanolamine phospholipase D reveals multiple mechanisms for the biosynthesis of endocannabinoids. Biochemistry 45, 4720–4726. 10.1021/bi060163l [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy D., Edut S., Baraz-Goldstein R., Rubovitch V., Defrin R., Bree D. (2016). Responses of dural mast cells in concussive and blast models of mild traumatic brain injury in mice: potential implications for post-traumatic headache. Cephalalgia 36, 915–923. 10.1177/0333102415617412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy D., Kainz V., Burstein R., Strassman A. M. (2012). Mast cell degranulation distinctly activates trigemino-cervical and lumbosacral pain pathways and elicits widespread tactile pain hypersensitivity. Brain Behav. Immun. 26, 311–317. 10.1016/j.bbi.2011.09.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li M., Li Y., Liu X., Gao X., Wang Y. (2012). IL-33 blockade suppresses the development of experimental autoimmune encephalomyelitis in C57BL/6 mice. J. Neuroimmunol. 247, 25–31. 10.1016/j.jneuroim.2012.03.016 [DOI] [PubMed] [Google Scholar]
- Li N., Zhang X., Dong H., Hu Y., Qian Y. (2017). Bidirectional relationship of mast cells-neurovascular unit communication in neuroinflammation and its involvement in POCD. Behav. Brain Res. 322(Pt A), 60–69. 10.1016/j.bbr.2017.01.006 [DOI] [PubMed] [Google Scholar]
- Lian H., Litvinchuk A., Chiang A. C., Aithmitti N., Jankowsky J. L., Zheng H. (2015). Astrocyte-microglia cross talk through complement activation modulates amyloid pathology in mouse models of Alzheimer's disease. J. Neurosci. 36, 577–589. 10.1523/JNEUROSCI.2117-15.2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lian H., Yang L., Cole A., Sun L., Chiang A. C., Fowler S. W., et al. (2016). NFκB-activated astroglial release of complement C3 compromises neuronal morphology and function associated with Alzheimer's disease. Neuron 85, 101–115. 10.1016/j.neuron.2014.11.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liddelow S. A., Guttenplan K. A., Clarke L. E., Bennett F. C., Bohlen C. J., Schirmer L., et al. (2017). Neurotoxic reactive astrocytes are induced by activated microglia. Nature 541, 481–487. 10.1038/nature21029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liew F. Y., Pitman N. I., McInnes I. B. (2010). Disease-associated functions of IL-33: the new kid in the IL-1 family. Nat. Rev. Immunol. 10, 103–110. 10.1038/nri2692 [DOI] [PubMed] [Google Scholar]
- Lindsberg P. J., Strbian D., Karjalainen-Lindsberg M. L. (2010). Mast cells as early responders in the regulation of acute blood-brain barrier changes after cerebral ischemia and hemorrhage. J. Cereb. Blood. Flow Metab. 30, 689–702. 10.1038/jcbfm.2009.282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu S., Liu Y., Hao W., Wolf L., Kiliaan A. J., Penke B., et al. (2012). TLR2 is a primary receptor for Alzheimer's amyloid β-peptide to trigger neuroinflammatory activation. J. Immunol. 188, 1098–1107. 10.4049/jimmunol.1101121 [DOI] [PubMed] [Google Scholar]
- Liu J., Wang F. (2017). Role of neuroinflammation in amyotrophic lateral sclerosis: cellular mechanisms and therapeutic implications. Front. Immunol. 8:1005. 10.3389/fimmu.2017.01005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Locci A., Geoffroy P., Miesch M., Mensah-Nyagan A. G., Pinna G. (2017). Social isolation in early versus late adolescent mice is associated with persistent behavioral deficits that can be improved by neurosteroid-based treatment. Front. Cell. Neurosci. 11:208. 10.3389/fncel.2017.00208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loane D. J., Kumar A., Stoica B. A., Cabatbat R., Faden A. I. (2014). Progressive neurodegeneration after experimental brain trauma: association with chronic microglial activation. J. Neuropathol. Exp. Neurol. 73, 14–29. 10.1097/NEN.0000000000000021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loftis J. M., Hauser P. (2004). The phenomenology and treatment of interferon-induced depression. J. Affect. Disord. 82, 175–190. 10.1016/j.jad.2004.04.002 [DOI] [PubMed] [Google Scholar]
- Lozada A., Maegele M., Stark H., Neugebauer E. M., Panula P. (2005). Traumatic brain injury results in mast cell increase and changes in regulation of central histamine receptors. Neuropathol. Appl. Neurobiol. 31, 150–162. 10.1111/j.1365-2990.2004.00622.x [DOI] [PubMed] [Google Scholar]
- Lucchinetti C. F., Popescu B. F., Bunyan R. F., Moll N. M., Roemer S. F., Lassmann H., et al. (2011). Inflammatory cortical demyelination in early multiple sclerosis. N. Engl. J. Med. 365, 2188–2197. 10.1056/NEJMoa1100648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luongo L., Guida F., Boccella S., Bellini G., Gatta L., Rossi F., et al. (2013). Palmitoylethanolamide reduces formalin-induced neuropathic-like behaviour through spinal glial/microglial phenotypical changes in mice. CNS Neurol. Disord. Drug Targets 12, 45–54. 10.2174/1871527311312010009 [DOI] [PubMed] [Google Scholar]
- Machado A., Herrera A. J., De Pablos R. M., Espinosa-Oliva A. M., Sarmiento M., Ayala A., et al. (2014). Chronic stress as a risk factor for Alzheimer's disease. Rev. Neurosci. 25, 785–804. 10.1515/revneuro-2014-0035 [DOI] [PubMed] [Google Scholar]
- Maes M., Leonard B. E., Myint A. M., Kubera M., Verkerk R. (2011). The new ‘5-HT’ hypothesis of depression: cell-mediated immune activation induces indoleamine 2,3-dioxygenase, which leads to lower plasma tryptophan and an increased synthesis of detrimental tryptophan catabolites (TRYCATs), both of which contribute to the onset of depression. Prog. Neuropsychopharmacol. Biol. Psychiatry 35, 702–721. 10.1016/j.pnpbp.2010.12.017 [DOI] [PubMed] [Google Scholar]
- Malamud V., Vaaknin A., Abramsky O., Mor M., Burgess L. E., Ben-Yehudah A., et al. (2003). Tryptase activates peripheral blood mononuclear cells causing the synthesis and release of TNF-alpha, IL-6 and IL-1 beta: possible relevance to multiple sclerosis. J. Neuroimmunol. 138, 115–122. 10.1016/S0165-5728(03)00090-0 [DOI] [PubMed] [Google Scholar]
- Manocha G. D., Floden A. M., Rausch K., Kulas J. A., McGregor B. A., Rojanathammanee L., et al. (2016). APP regulates microglial phenotype in a mouse model of Alzheimer's disease. J. Neurosci. 36, 8471–8486. 10.1523/JNEUROSCI.4654-15.2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marinelli C., Bertalot T., Zusso M., Skaper S. D., Giusti P. (2016). Systematic review of pharmacological properties of the oligodendrocyte lineage. Front. Cell. Neurosci. 10:27. 10.3389/fncel.2016.00027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martini R., Willison H. (2016). Neuroinflammation in the peripheral nerve: cause, modulator, or bystander in peripheral neuropathies? Glia 64, 475–486. 10.1002/glia.22899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masgrau R., Guaza C., Ransohoff R. M., Galea E. (2017). Should we stop saying ‘glia’ and ‘neuroinflammation’? Trends Mol. Med. 23, 486–500. 10.1016/j.molmed.2017.04.005 [DOI] [PubMed] [Google Scholar]
- Maslinska D., Laure-Kamionowska M., Maslinski K. T., Gujski M., Maslinski S. (2007). Distribution of tryptase-containing mast cells and metallothionein reactive astrocytes in human brains with amyloid deposits. Inflamm. Res. 56, S17–S18. 10.1007/s00011-006-0508-8 [DOI] [PubMed] [Google Scholar]
- Matcham F., Rayner L., Steer S., Hotopf M. (2013). The prevalence of depression in rheumatoid arthritis: a systematic review and meta-analysis. Rheumatology 52, 2136–2148. 10.1093/rheumatology/ket169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mate I., Madrid J. A., De la Fuente M. (2014). Chronobiology of the neuroimmunoendocrine system and aging. Curr. Pharm. Des. 20, 4642–4655. 10.2174/1381612820666140130201131 [DOI] [PubMed] [Google Scholar]
- Mattace Raso G., Russo R., Calignano A., Meli R. (2014). Palmitoylethanolamide in CNS health and disease. Pharmacol. Res. 86, 32–41. 10.1016/j.phrs.2014.05.006 [DOI] [PubMed] [Google Scholar]
- Mattila O. S., Strbian D., Saksi J., Pikkarainen T. O., Rantanen V., Tatlisumak T., et al. (2011). Cerebral mast cells mediate blood-brain barrier disruption in acute experimental ischemic stroke through perivascular gelatinase activation. Stroke 42, 3600–3605. 10.1161/STROKEAHA.111.632224 [DOI] [PubMed] [Google Scholar]
- McCandless E. E., Piccio L., Woerner B. M., Schmidt R. E., Rubin J. B., Cross A. H., et al. (2008). Pathological expression of CXCL12 at the blood-brain barrier correlates with severity of multiple sclerosis. Am. J. Pathol. 172, 799–808. 10.2353/ajpath.2008.070918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGeer P. L., McGeer E. G. (2013). The amyloid cascade-inflammatory hypothesis of Alzheimer disease: implications for therapy. Acta Neuropathol. 126, 479–497. 10.1007/s00401-013-1177-7 [DOI] [PubMed] [Google Scholar]
- McKittrick C. M., Lawrence C. E., Carswell H. V. (2015). Mast cells promote blood brain barrier breakdown and neutrophil infiltration in a mouse model of focal cerebral ischemia. J. Cereb. Blood Flow Metab. 35, 638–647. 10.1038/jcbfm.2014.239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McManus R. M., Heneka M. T. (2017). Role of neuroinflammation in neurodegeneration: new insights. Alzheimers Res. Ther. 9:14. 10.1186/s13195-017-0241-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medeiros R., LaFerla F. M. (2013). Astrocytes: conductors of the Alzheimer disease neuroinflammatory symphony. Exp. Neurol. 239, 133–138. 10.1016/j.expneurol.2012.10.007 [DOI] [PubMed] [Google Scholar]
- Medic N., Lorenzon P., Vita F., Trevisan E., Marchioli A., Soranzo M. R., et al. (2010). Mast cell adhesion induces cytoskeletal modifications and programmed cell death in oligodendrocytes. J. Neuroimmunol. 218, 57–66. 10.1016/j.jneuroim.2009.10.011 [DOI] [PubMed] [Google Scholar]
- Medic N., Vita F., Abbate R., Soranzo M. R., Pacor S., Fabbretti E., et al. (2008). Mast cell activation by myelin through scavenger receptor. J. Neuroimmunol. 200, 27–40. 10.1016/j.jneuroim.2008.05.019 [DOI] [PubMed] [Google Scholar]
- Mezuk B., Eaton W. W., Albrecht S., Golden S. H. (2008). Depression and type 2 diabetes over the lifespan: a meta-analysis. Diabetes Care 31, 2383–2390. 10.2337/dc08-0985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michaud M., Balardy L., Moulis G., Gaudin C., Peyrot C., Vellas B., Cesari M., et al. (2013). Proinflammatory cytokines, aging, and age-related diseases. J. Am. Med. Dir. Assoc. 14, 877–882. 10.1016/j.jamda.2013.05.009 [DOI] [PubMed] [Google Scholar]
- Miida T., Yamada T., Seino U., Ito M., Fueki Y., Takahashi A., et al. (2006). Serum amyloid A (SAA)-induced remodeling of CSF-HDL. Biochim. Biophys. Acta 1761, 424–433. 10.1016/j.bbalip.2006.03.013 [DOI] [PubMed] [Google Scholar]
- Milligan E. D., Watkins L. R. (2009). Pathological and protective roles of glia in chronic pain. Nat. Rev. Neurosci. 10, 23–36. 10.1038/nrn2533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miron V. E., Boyd A., Zhao J. W., Yuen T. J., Ruckh J. M., Shadrach J. L., et al. (2013). M2 microglia and macrophages drive oligodendrocyte differentiation during CNS remyelination. Nat. Neurosci. 16, 1211–1218. 10.1038/nn.3469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miyoshi K., Obata K., Kondo T., Okamura H., Noguchi K. (2008). Interleukin-18-mediated microglia/astrocyte interaction in the spinal cord enhances neuropathic pain processing after nerve injury. J. Neurosci. 28, 12775–12787. 10.1523/JNEUROSCI.3512-08.2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Möller T., Boddeke H. W. (2016). Glial cells as drug targets: what does it take? Glia 64, 1742–1754. 10.1002/glia.22993 [DOI] [PubMed] [Google Scholar]
- Monks C. R., Freiberg B. A., Kupfer H., Sciaky N., Kupfer A. (1998). Three-dimensional segregation of supramolecular activation clusters in T cells. Nature 395, 82–86. 10.1038/25764 [DOI] [PubMed] [Google Scholar]
- Morgan J. T., Chana G., Abramson I., Semendeferi K., Courchesne E., Everall I. P. (2012). Abnormal microglial-neuronal spatial organization in the dorsolateral prefrontal cortex in autism. Brain Res. 1456, 72–81. 10.1016/j.brainres.2012.03.036 [DOI] [PubMed] [Google Scholar]
- Morgan J. T., Chana G., Pardo C. A., Achim C., Semendeferi K., Buckwalter J., et al. (2010). Microglial activation and increased microglial density observed in the dorsolateral prefrontal cortex in autism. Biol. Psychiatry 68, 368–376. 10.1016/j.biopsych.2010.05.024 [DOI] [PubMed] [Google Scholar]
- Morris M. C., Gilliam E. A., Li L. (2015). Innate immune programing by endotoxin and its pathological consequences. Front. Immunol. 5:680. 10.3389/fimmu.2014.00680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moura D. S., Sultan S., Georgin-Lavialle S., Pillet N., Montestruc F., Gineste P., et al. (2011). Depression in patients with mastocytosis: prevalence, features and effects of masitinib therapy. PLoS ONE 6:26375. 10.1371/journal.pone.0026375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mravec B., Horvathova L., Padova A. (2018). Brain under stress and Alzheimer's disease. Cell. Mol. Neurobiol. 38, 73–84. 10.1007/s10571-017-0521-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muccioli G. G., Stella N. (2008). Microglia produce and hydrolyze palmitoylethanolamide. Neuropharmacology 54, 16–22. 10.1016/j.neuropharm.2007.05.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers R. R., Campana W. M., Shubayev V. I. (2006). The role of neuroinflammation in neuropathic pain: mechanisms and therapeutic targets. Drug Discov. Today 11, 8–20. 10.1016/S1359-6446(05)03637-8 [DOI] [PubMed] [Google Scholar]
- Najjar S., Pearlman D. M., Alper K., Najjar A., Devinsky O. (2013). Neuroinflammation and psychiatric illness. J. Neuroinflammation 10:43. 10.1186/1742-2094-10-43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakae S., Suto H., Iikura M., Kakurai M., Sedgwick J. D., Tsai M., et al. (2006). Mast cells enhance T cell activation: importance of mast cell costimulatory molecules and secreted TNF. J. Immunol. 176, 2238–2248. 10.4049/jimmunol.176.4.2238 [DOI] [PubMed] [Google Scholar]
- Nakano N., Nishiyama C., Kanada S., Niwa Y., Shimokawa N., Ushio H., et al. (2007). Involvement of mast cells in IL-12/23 p40 production is essential for survival from polymicrobial infections. Blood 109, 4846–4855. 10.1182/blood-2006-09-045641 [DOI] [PubMed] [Google Scholar]
- Nathan C., Ding A. (2010). Nonresolving inflammation. Cell 140, 871–882. 10.1016/j.cell.2010.02.029 [DOI] [PubMed] [Google Scholar]
- Nautiyal K. M., Ribeiro A. C., Pfaff D. W., Silver R. (2008). Brain mast cells link the immune system to anxiety-like behavior. Proc. Natl. Acad. Sci. U.S.A. 105, 18053–18057. 10.1073/pnas.0809479105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nave K. A. (2010). Myelination and support of axonal integrity by glia. Nature 468, 244–252. 10.1038/nature09614 [DOI] [PubMed] [Google Scholar]
- Nelissen S., Lemmens E., Geurts N., Kramer P., Maurer M., Hendriks J., et al. (2013). The role of mast cells in neuroinflammation. Acta Neuropathol. 125, 637–650. 10.1007/s00401-013-1092-y [DOI] [PubMed] [Google Scholar]
- Nelson R. B., Siman R., Iqbal M. A., Potter H. (1993). Identification of a chymotrypsin-like mast cell protease in rat brain capable of generating the N-terminus of the Alzheimer amyloid beta-protein. J. Neurochem. 61, 567–577. [DOI] [PubMed] [Google Scholar]
- Nguyen M., Pace A. J., Koller B. H. (2005). Age-induced reprogramming of mast cell degranulation. J. Immunol. 175, 5701–5707. 10.4049/jimmunol.175.9.5701 [DOI] [PubMed] [Google Scholar]
- Niederhoffer N., Levy R., Sick E., Andre P., Coupin G., Lombard Y., et al. (2009). Amyloid beta peptides trigger CD47-dependent mast cell secretory and phagocytic responses. Int. J. Immunopathol. Pharmacol. 22, 473–483. 10.1177/039463200902200224 [DOI] [PubMed] [Google Scholar]
- Norden D. M., Godbout J. P. (2013). Review: microglia of the aged brain: primed to be activated and resistant to regulation. Neuropathol. Appl. Neurobiol. 39, 19–34. 10.1111/j.1365-2990.2012.01306.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noriega D. B., Savelkoul H. F. (2014). Immune dysregulation in autism spectrum disorder. Eur. J. Pediatr. 173, 33–43. 10.1007/s00431-013-2183-4 [DOI] [PubMed] [Google Scholar]
- Öhrfelt A., Axelsson M., Malmeström C., Novakova L., Heslegrave A., Blennow K. (2016). Soluble TREM-2 in cerebrospinal fluid from patients with multiple sclerosis treated with natalizumab or mitoxantrone. Mult. Scler. 22, 1587–1595. 10.1177/1352458515624558 [DOI] [PubMed] [Google Scholar]
- Old E. A., Clark A. K., Malcangio M. (2015). The role of glia in the spinal cord in neuropathic and inflammatory pain. Handb. Exp. Pharmacol. 227, 145–170. 10.1007/978-3-662-46450-2_8 [DOI] [PubMed] [Google Scholar]
- Oliveira S. M., Drewes C. C., Silva C. R., Trevisan G., Boschen S. L., Moreira C. G., et al. (2011). Involvement of mast cells in a mouse model of postoperative pain. Eur. J. Pharmacol. 672, 88–95. 10.1016/j.ejphar.2011.10.001 [DOI] [PubMed] [Google Scholar]
- Olsson N., Siegbahn A., Nilsson G. (1999). Serum amyloid A induces chemotaxis of human mast cells by activating a pertussis toxin-sensitive signal transduction pathway. Biochem. Biophys. Res. Commun. 254, 143–146. 10.1006/bbrc.1998.9911 [DOI] [PubMed] [Google Scholar]
- Orefice N. S., Alhouayek M., Carotenuto A., Montella S., Barbato F., Comelli A. (2016). Oral palmitoylethanolamide treatment is associated with reduced cutaneous adverse effects of interferon-β1a and circulating proinflammatory cytokines in relapsing-remitting multiple sclerosis. Neurotherapeutics 13, 428–438. 10.1007/s13311-016-0420-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orinska Z., Bulanova E., Budagian V., Metz M., Maurer M., Bulfone-Paus S. (2005). TLR3-induced activation of mast cells modulates CD8+ T-cell recruitment. Blood 106, 978–987. 10.1182/blood-2004-07-2656 [DOI] [PubMed] [Google Scholar]
- Osipchuk Y., Cahalan M. (1992). Cell-to-cell spread of calcium signals mediated by ATP receptors in mast cells. Nature 359, 241–244. 10.1038/359241a0 [DOI] [PubMed] [Google Scholar]
- Ossipov M. H., Dussor G. O., Porreca F. (2010). Central modulation of pain. J. Clin. Invest. 120, 3779–3787. 10.1172/JCI43766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osterberg A., Boivie J., Thuomas K. A. (2005). Central pain in multiple sclerosis–prevalence and clinical characteristics. Eur. J. Pain 9, 531–542. 10.1016/j.ejpain.2004.11.005 [DOI] [PubMed] [Google Scholar]
- Pacher P., Bátkai S., Kunos G. (2006). The endocannabinoid system as an emerging target of pharmacotherapy. Pharmacol. Rev. 58, 389–462. 10.1124/pr.58.3.2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paladini A., Fusco M., Cenacchi T., Schievano C., Piroli A., Varrassi G. (2016). Palmitoylethanolamide, a special food for medical purposes, in the treatment of chronic pain: a pooled data meta-analysis. Pain Physician 19, 11–24. [PubMed] [Google Scholar]
- Palma E., Reyes-Ruiz J. M., Lopergolo D., Roseti C., Bertollini C., Ruffolo G. (2016). Acetylcholine receptors from human muscle as pharmacological targets for ALS therapy. Proc. Natl. Acad. Sci. U.S.A. 113, 3060–3065. 10.1073/pnas.1600251113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paolicelli R. C., Bolasco G., Pagani F., Maggi L., Scianni M., Panzanelli P., et al. (2011). Synaptic pruning by microglia is necessary for normal brain development. Science 333, 1456–1458. 10.1126/science.1202529 [DOI] [PubMed] [Google Scholar]
- Parvathenani L. K., Tertyshnikova S., Greco C. R., Roberts S. B., Robertson B., Posmantur R. (2003). P2X7 mediates superoxide production in primary microglia and is up-regulated in a transgenic mouse model of Alzheimer's disease. J. Biol. Chem. 278, 13309–13317. 10.1074/jbc.M209478200 [DOI] [PubMed] [Google Scholar]
- Patti G. J., Yanes O., Shriver L. P., Courade J. P., Tautenhahn R., Manchester M., et al. (2012). Metabolomics implicates altered sphingolipids in chronic pain of neuropathic origin. Nat. Chem. Biol. 8, 232–234. 10.1038/nchembio.767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paul C., Sans B., Suarez F., Casassus P., Barete S., Lanternier F., et al. (2010). Masitinib for the treatment of systemic and cutaneous mastocytosis with handicap: a phase 2a study. Am. J. Hematol. 85, 921–925. 10.1002/ajh.21894 [DOI] [PubMed] [Google Scholar]
- Peferoen L., Kipp M., van der Valk P., van Noort J. M., Amor S. (2014). Oligodendrocyte-microglia cross-talk in the central nervous system. Immunology 141, 302–313. 10.1111/imm.12163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peferoen L. A., Vogel D. Y., Ummenthum K., Breur M., Heijnen P. D., Gerritsen W. H., et al. (2015). Activation status of human microglia is dependent on lesion formation stage and remyelination in multiple sclerosis. J. Neuropathol. Exp. Neurol. 74, 48–63. 10.1097/NEN.0000000000000149 [DOI] [PubMed] [Google Scholar]
- Pekny M., Pekna M., Messing A., Steinhäuser C., Lee J. M., Parpura V., et al. (2016). Astrocytes: a central element in neurological diseases. Acta Neuropathol. 131, 323–345. 10.1007/s00401-015-1513-1 [DOI] [PubMed] [Google Scholar]
- Peng J., Gu N., Zhou L., Eyo U. B., Murugan M., Gan W. B., et al. (2016). Microglia and monocytes synergistically promote the transition from acute to chronic pain after nerve injury. Nat. Commun. 7:12029. 10.1038/ncomms12029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perry V. H., Holmes C. (2014). Microglial priming in neurodegenerative disease. Nat. Rev. Neurol. 10, 217–224. 10.1038/nrneurol.2014.38 [DOI] [PubMed] [Google Scholar]
- Petrosino S., Di Marzo V. (2017). The pharmacology of palmitoylethanolamide and first data on the therapeutic efficacy of some of its new formulations. Br. J. Pharmacol. 174, 1349–1365. 10.1111/bph.13580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Philips T., Robberecht W. (2011). Neuroinflammation in amyotrophic lateral sclerosis: role of glial activation in motor neuron disease. Lancet Neurol. 10, 253–263. 10.1016/S1474-4422(11)70015-1 [DOI] [PubMed] [Google Scholar]
- Pietrzak A., Wierzbicki M., Wiktorska M., Brzezinska-Błaszczyk E. (2011). Surface TLR2 and TLR4 expression on mature rat mast cells can be affected by some bacterial components and proinflammatory cytokines. Mediators Inflamm. 2011:427473. 10.1155/2011/427473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piette F., Belmin J., Vincent H., Schmidt N., Pariel S., Verny M., et al. (2011). Masitinib as an adjunct therapy for mild-to-moderate Alzheimer's disease: a randomised, placebo-controlled phase 2 trial. Alzheimers Res. Ther. 3:16. 10.1186/alzrt75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piirainen S., Youssef A., Song C., Kalueff A. V., Landreth G. E., et al. (2017). Psychosocial stress on neuroinflammation and cognitive dysfunctions in Alzheimer's disease: the emerging role for microglia? Neurosci. Biobehav. Rev. 77, 148–164. 10.1016/j.neubiorev.2017.01.046 [DOI] [PubMed] [Google Scholar]
- Piomelli D., Sasso O. (2014). Peripheral gating of pain signals by endogenous lipid mediators. Nat. Neurosci. 17, 164–174. 10.1038/nn.3612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Popiolek-Barczyk K., Mika J. (2016). Targeting the microglial signaling pathways: new insights in the modulation of neuropathic pain. Curr. Med. Chem. 23, 2908–2928. 10.2174/0929867323666160607120124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prinz M., Priller J. (2014). Microglia and brain macrophages in the molecular age: from origin to neuropsychiatric disease. Nat. Rev. Neurosci. 15, 300–312. 10.1038/nrn3722 [DOI] [PubMed] [Google Scholar]
- Prussin C., Metcalfe D. D. (2003). IgE, mast cells, basophils, and eosinophils. J. Allergy Clin. Immunol. 111(Suppl. 2), S486–S494. 10.1067/mai.2003.120 [DOI] [PubMed] [Google Scholar]
- Pundir P., MacDonald C. A., Kulka M. (2015). The novel receptor C5aR2 is required for C5a-mediated human mast cell adhesion, migration, and proinflammatory mediator production. J. Immunol. 195, 2774–2787. 10.4049/jimmunol.1401348 [DOI] [PubMed] [Google Scholar]
- Punzo D., Errico F., Cristino L., Sacchi S., Keller S., Belardo C., et al. (2016). Age-related changes in D-aspartate oxidase promoter methylation control extracellular D-aspartate levels and prevent precocious cell death during brain aging. J. Neurosci. 36, 3064–3078. 10.1523/JNEUROSCI.3881-15.2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Queiroz L. P. (2013). Worldwide epidemiology of fibromyalgia. Curr. Pain Headache Rep. 17:356. 10.1007/s11916-013-0356-5 [DOI] [PubMed] [Google Scholar]
- Ramlackhansingh A. F., Brooks D. J., Greenwood R. J., Bose S. K., Turkheimer F. E., Kinnunen K. M., et al. (2011). Inflammation after trauma: microglial activation and traumatic brain injury. Ann. Neurol. 70, 374–383. 10.1002/ana.22455 [DOI] [PubMed] [Google Scholar]
- Ransohoff R. M. (2016a). How neuroinflammation contributes to neurodegeneration. Science 353, 777–782. 10.1126/science.aag2590 [DOI] [PubMed] [Google Scholar]
- Ransohoff R. M. (2016b). A polarizing question: do M1 and M2 microglia exist? Nat. Neurosci. 19, 987–991. 10.1038/nn.4338 [DOI] [PubMed] [Google Scholar]
- Rapp J. H., Pan X. M., Neumann M., Hong M., Hollenbeck K., Liu J. (2008). Microemboli composed of cholesterol crystals disrupt the blood-brain barrier and reduce cognition. Stroke 39, 2354–2361. 10.1161/STROKEAHA.107.496737 [DOI] [PubMed] [Google Scholar]
- Rawji K. S., Mishra M. K., Michaels N. J., Rivest S., Stys P. K., Yong V. W. (2016). Immunosenescence of microglia and macrophages: impact on the ageing central nervous system. Brain 139, 653–661. 10.1093/brain/awv395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Recchia A., Debetto P., Negro A., Guidolin D., Skaper S. D., Giusti P. (2004). Alpha-synuclein and Parkinson's disease. FASEB J. 18, 617–626. 10.1096/fj.03-0338rev [DOI] [PubMed] [Google Scholar]
- Regen F., Hellmann-Regen J., Costantini E., Reale M. (2017). Neuroinflammation and Alzheimer's disease: implications for microglial activation. Curr. Alzheimer Res. 14, 1140–1148. 10.2174/1567205014666170203141717 [DOI] [PubMed] [Google Scholar]
- Ren K., Dubner R. (2010). Interactions between the immune and nervous systems in pain. Nat. Med. 16, 1267–1276. 10.1038/nm.2234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rentzos M., Rombos A., Nikolaou C., Zoga M., Zouvelou V., Dimitrakopoulos A., et al. (2010). Interleukin-15 and interleukin-12 are elevated in serum and cerebrospinal fluid of patients with amyotrophic lateral sclerosis. Eur. Neurol. 63, 285–290. 10.1159/000287582 [DOI] [PubMed] [Google Scholar]
- Ribatti D. (2015). The crucial role of mast cells in blood-brain barrier alterations. Exp. Cell. Res. 338, 119–125. 10.1016/j.yexcr.2015.05.013 [DOI] [PubMed] [Google Scholar]
- Ribeiro A., Pontis S., Mengatto L., Armirotti A., Chiurchiù V., Capurro V., et al. (2015). A potent systemically active N-acylethanolamine acid amidase inhibitor that suppresses inflammation and human macrophage activation. ACS Chem. Biol. 10, 1838–1846. 10.1021/acschembio.5b00114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riedel B., Browne K., Silbert B. (2014). Cerebral protection: inflammation, endothelial dysfunction, and postoperative cognitive dysfunction. Curr. Opin. Anaesthesiol. 27, 89–97. 10.1097/ACO.0000000000000032 [DOI] [PubMed] [Google Scholar]
- Rivara F. P., Vavilala M. S., Durbin D., Temkin N., Wang J., O'Connor S. S., et al. (2012). Persistence of disability 24 to 36 months after pediatric traumatic brain injury: a cohort study. J. Neurotrauma 29, 2499–2504. 10.1089/neu.2012.2434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rivest S. (2009). Regulation of innate immune responses in the brain. Nat. Rev. Immunol. 9, 429–439. 10.1038/nri2565 [DOI] [PubMed] [Google Scholar]
- Rodriguez J. I., Kern J. K. (2011). Evidence of microglial activation in autism and its possible role in brain underconnectivity. Neuron Glia Biol. 7, 205–213. 10.1017/S1740925X12000142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodrigues M. C., Hernandez-Ontiveros D. G., Louis M. K., Willing A. E., Borlongan C. V., Sanberg P. R., et al. (2012). Neurovascular aspects of amyotrophic lateral sclerosis. Int. Rev. Neurobiol. 102, 91–106. 10.1016/B978-0-12-386986-9.00004-1 [DOI] [PubMed] [Google Scholar]
- Rogers M. P., Bloomingdale K., Murawski B. J., Soter N. A., Reich P., Austen K. F. (1986). Mixed organic brain syndrome as a manifestation of systemic mastocytosis. Psychosom. Med. 48, 437–447. 10.1097/00006842-198607000-00006 [DOI] [PubMed] [Google Scholar]
- Rosenberg G. A. (2012). Neurological diseases in relation to the blood–brain barrier. J. Cereb. Blood Flow Metab. 32, 1139–1151. 10.1038/jcbfm.2011.197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roser A. E., Tönges L., Lingor P. (2017). Modulation of microglial activity by rho-kinase (ROCK) inhibition as therapeutic strategy in Parkinson's disease and amyotrophic lateral sclerosis. Front. Aging Neurosci. 9:94. 10.3389/fnagi.2017.00094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rozniecki J. J., Hauser S. L., Stein M., Lincoln R., Theoharides T. C. (1995). Elevated mast cell tryptase in cerebrospinal fluid of multiple sclerosis patients. Ann. Neurol. 37, 63–66. 10.1002/ana.410370112 [DOI] [PubMed] [Google Scholar]
- Russi A. E., Walker-Caulfield M. E., Brown M. A. (2016a). Mast cell inflammasome activity in the meninges regulates EAE disease severity. Clin. Immunol. [Epub ahead of print]. 10.1016/j.clim.2016.04.009 [DOI] [PubMed] [Google Scholar]
- Russi A. E., Walker-Caulfield M. E., Guo Y., Lucchinetti C. F., Brown M. A. (2016b). Meningeal mast cell-T cell crosstalk regulates T cell encephalitogenicity. J. Autoimmun. 73, 100–110. 10.1016/j.jaut.2016.06.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saab A. S., Tzvetanova I. D., Nave K. A. (2013). The role of myelin and oligodendrocytes in axonal energy metabolism. Curr. Opin. Neurobiol. 23, 1065–1072. 10.1016/j.conb.2013.09.008 [DOI] [PubMed] [Google Scholar]
- Safaiyan S., Kannaiyan N., Snaidero N., Brioschi S., Biber K., Yona S. (2016). Age-related myelin degradation burdens the clearance function of microglia during aging. Nat. Neurosci. 19, 995–998. 10.1038/nn.4325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sakamoto A., Andoh T., Kuraishi Y. (2016). Involvement of mast cells and proteinase-activated receptor 2 in oxaliplatin-induced mechanical allodynia in mice. Pharmacol. Res. 105, 84–92. 10.1016/j.phrs.2016.01.008 [DOI] [PubMed] [Google Scholar]
- Santoro A., Spinelli C. C., Martucciello S., Nori S. L., Capunzo M., Puca A. A., et al. (2018). Innate immunity and cellular senescence: the good and the bad in the developmental and aged brain. J. Leukoc. Biol. 103, 509–524. 10.1002/JLB.3MR0118-003R [DOI] [PubMed] [Google Scholar]
- Sasso O., Moreno-Sanz G., Martucci C., Realini N., Dionisi M., Mengatto L., et al. (2013). Antinociceptive effects of the N-acylethanolamine acid amidase inhibitor ARN077 in rodent pain models. Pain 154, 350–360. 10.1016/j.pain.2012.10.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sayed B. A., Christy A. L., Walker M. E., Brown M. A. (2010). Meningeal mast cells affect early T cell central nervous system infiltration and blood-brain barrier integrity through TNF: a role for neutrophil recruitment? J. Immunol. 184, 6891–6900. 10.4049/jimmunol.1000126 [DOI] [PubMed] [Google Scholar]
- Schafer D. P., Lehrman E. K., Kautzman A. G., Koyama R., Mardinly A. R., Yamasaki R., et al. (2012). Microglia sculpt postnatal neural circuits in an activity and complement-dependent manner. Neuron 74, 691–705. 10.1016/j.neuron.2012.03.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schapansky J., Nardozzi J. D., LaVoie M. J. (2015). The complex relationships between microglia, alpha-synuclein, and LRRK2 in Parkinson's disease. Neuroscience 302, 74–88. 10.1016/j.neuroscience.2014.09.049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scuderi C., Bronzuoli M. R., Facchinetti R., Pace L., Ferraro L., Broad K. D., et al. (2018). Ultramicronized palmitoylethanolamide rescues learning and memory impairments in a triple transgenic mouse model of Alzheimer's disease by exerting anti-inflammatory and neuroprotective effects. Transl. Psychiatry. 8:32. 10.1038/s41398-017-0076-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selkoe D. J. (2008). Soluble oligomers of the amyloid beta-protein impair synaptic plasticity and behavior. Behav. Brain Res. 192, 106–113. 10.1016/j.bbr.2008.02.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selkoe D. J. (2011). Alzheimer's disease. Cold Spring Harb. Perspect. Biol. 3, 7 10.1101/cshperspect.a004457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selkoe D. J., Hardy J. (2016). The amyloid hypothesis of Alzheimer's disease at 25 years. EMBO Mol. Med. 8, 595–608. 10.15252/emmm.201606210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shin Yim Y., Park A., Berrios J., Lafourcade M., Pascual L. M., Soares N., et al. (2017). Reversing behavioural abnormalities in mice exposed to maternal inflammation. Nature 549, 482–487. 10.1038/nature23909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shulman J. M., De Jager P. L., Feany M. B. (2011). Parkinson's disease: genetics and pathogenesis. Annu. Rev. Pathol. 6, 193–222. 10.1146/annurev-pathol-011110-130242 [DOI] [PubMed] [Google Scholar]
- Silver R., Curley J. P. (2013). Mast cells on the mind: new insights and opportunities. Trends Neurosci. 36, 513–521. 10.1016/j.tins.2013.06.001 [DOI] [PubMed] [Google Scholar]
- Silver J., Miller J. H. (2004). Regeneration beyond the glial scar. Nat. Rev. Neurosci. 5, 146–156. 10.1038/nrn1326 [DOI] [PubMed] [Google Scholar]
- Simon E., Obst J., Gomez-Nicola D. (2018). The evolving dialogue of microglia and neurons in Alzheimer's disease: microglia as necessary transducers of pathology. Neuroscience. [Epub ahead of print]. 10.1016/j.neuroscience.2018.01.059 [DOI] [PubMed] [Google Scholar]
- Skaper S. D., Debetto P., Giusti P. (2010). The P2X7 purinergic receptor: from physiology to neurological disorders. FASEB J. 24, 337–453. 10.1096/fj.09-138883 [DOI] [PubMed] [Google Scholar]
- Skaper S. D., Facci L. (2012). Mast cell-glia axis in neuroinflammation and therapeutic potential of the anandamide congener palmitoylethanolamide. Philos. Trans. R. Soc. Lond. B Biol. Sci. 367, 3312–3325. 10.1098/rstb.2011.0391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skaper S. D., Facci L., Fusco M., Della Valle M. F., Zusso M., Costa B., et al. (2014). Palmitoylethanolamide, a naturally occurring disease-modifying agent in neuropathic pain. Inflammopharmacology 22, 79–94. 10.1007/s10787-013-0191-7 [DOI] [PubMed] [Google Scholar]
- Skaper S. D., Facci L., Zusso M., Giusti P. (2017). Neuroinflammation, mast cells, and glia: dangerous liaisons. Neuroscientist 23, 478–498. 10.1177/1073858416687249 [DOI] [PubMed] [Google Scholar]
- Skuljec J., Sun H., Pul R., Bénardais K., Ragancokova D., Moharregh-Khiabani D., et al. (2011). CCL5 induces a pro-inflammatory profile in microglia in vitro. Cell. Immunol. 270, 164–171. 10.1016/j.cellimm.2011.05.001 [DOI] [PubMed] [Google Scholar]
- Smith J. A., Das A., Ray S. K., Banik N. L. (2012). Role of pro-inflammatory cytokines released from microglia in neurodegenerative diseases. Brain Res. Bull. 87, 10–20. 10.1016/j.brainresbull.2011.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith B. H., Torrance N. (2012). Epidemiology of neuropathic pain and its impact on quality of life. Curr. Pain Headache Rep. 16, 191–198. 10.1007/s11916-012-0256-0 [DOI] [PubMed] [Google Scholar]
- Sofroniew M. V., Vinters H. V. (2010). Astrocytes: biology and pathology. Acta Neuropathol. 119, 7–35. 10.1007/s00401-009-0619-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solaro C., Trabucco E., Messmer Uccelli M. (2013). Pain and multiple sclerosis: pathophysiology and treatment. Curr. Neurol. Neurosci. Rep. 131:320 10.1007/s11910-012-0320-5 [DOI] [PubMed] [Google Scholar]
- Soliven B. (2001). Calcium signalling in cells of oligodendroglial lineage. Microsc. Res. Tech. 52, 672–679. 10.1002/jemt.1051 [DOI] [PubMed] [Google Scholar]
- Solorzano C., Zhu C., Battista N., Astarita G., Lodola A., Rivara S., et al. (2009). Selective N-acylethanolamine-hydrolyzing acid amidase inhibition reveals a key role for endogenous palmitoylethanolamide in inflammation. Proc. Natl. Acad. Sci. U.S.A. 106, 20966–20971. 10.1073/pnas.0907417106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soruri A., Grigat J., Kiafard Z., Zwirner J. (2008). Mast cell activation is characterized by upregulation of a functional anaphylatoxin C5a receptor. BMC Immunol. 9:29. 10.1186/1471-2172-9-29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sospedra M., Martin R. (2016). Immunology of multiple sclerosis. Semin. Neurol. 36, 115–127. 10.1055/s-0036-1579739 [DOI] [PubMed] [Google Scholar]
- Spangenberg E. E., Green K. N. (2017). Inflammation in Alzheimer's disease: lessons learned from microglia-depletion models. Brain Behav. Immun. 61, 1–11. 10.1016/j.bbi.2016.07.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Staud R. (2015). Cytokine and immune system abnormalities in fibromyalgia and other central sensitivity syndromes. Curr. Rheumatol. Rev. 11, 109–115. 10.2174/1573397111666150619094819 [DOI] [PubMed] [Google Scholar]
- Stojkovska I., Wagner B. M., Morrison B. E. (2015). Parkinson's disease and enhanced inflammatory response. Exp. Biol. Med. 240, 1387–1395. 10.1177/1535370215576313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stokely M. E., Orr E. L. (2008). Acute effects of calvarial damage on dural mast cells, pial vascular permeability, and cerebral cortical histamine levels in rats and mice. J. Neurotrauma 25, 52–61. 10.1089/neu.2007.0397 [DOI] [PubMed] [Google Scholar]
- Stoner R., Chow M. L., Boyle M. P., Sunkin S. M., Mouton P. R., Roy S., et al. (2014). Patches of disorganization in the neocortex of children with autism. N. Engl. J. Med. 370, 1209–1219. 10.1056/NEJMoa1307491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strbian D., Karjalainen-Lindsberg M. L., Tatlisumak T., Lindsberg P. J. (2006). Cerebral mast cells regulate early ischemic brain swelling and neutrophil accumulation. J. Cereb. Blood Flow Metab. 26, 605–612. 10.1038/sj.jcbfm.9600228 [DOI] [PubMed] [Google Scholar]
- Strbian D., Tatlisumak T., Ramadan U. A., Lindsberg P. J. (2007). Mast cell blocking reduces brain edema and hematoma volume and improves outcome after experimental intracerebral hemorrhage. J. Cereb. Blood Flow Metab. 27, 795–802. 10.1038/sj.jcbfm.9600387 [DOI] [PubMed] [Google Scholar]
- Streit W. J., Braak H., Xue Q. S., Bechmann I. (2009). Dystrophic (senescent) rather than activated microglial cells are associated with tau pathology and likely precede neurodegeneration in Alzheimer's disease. Acta Neuropathol. 118, 475–485. 10.1007/s00401-009-0556-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suurmond J., van Heemst J., van Heiningen J., Dorjée A. L., Schilham M. W., van der Beek F. B., et al. (2013). Communication between human mast cells and CD4+ T cells through antigen-dependent interactions. Eur. J. Immunol. 43, 1758–1768. 10.1002/eji.201243058 [DOI] [PubMed] [Google Scholar]
- Sveinsson O. A., Kjartansson O., Valdimarsson E. M. (2014). Cerebral ischemia/infarction - epidemiology, causes and symptoms. Laeknabladid 100, 271–279. [DOI] [PubMed] [Google Scholar]
- Tabas I., Glass C. K. (2013). Anti-inflammatory therapy in chronic disease: challenges and opportunities. Science 166, 166–172. 10.1126/science.1230720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taib T., Leconte C., Van Steenwinckel J., Cho A. H., Palmier B., Torsello E., et al. (2017). Neuroinflammation, myelin and behavior: temporal patterns following mild traumatic brain injury in mice. PLoS ONE 12:e0184811. 10.1371/journal.pone.0184811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takahashi K., Prinz M., Stagi M., Chechneva O., Neumann H. (2007). TREM2-transduced myeloid precursors mediate nervous tissue debris clearance and facilitate recovery in an animal model of multiple sclerosis. PLoS Med. 4:e124. 10.1371/journal.pmed.0040124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang Y., Le W. (2016). Differential roles of M1 and M2 microglia in neurodegenerative diseases. Mol. Neurobiol. 53, 1181–1194. 10.1007/s12035-014-9070-5 [DOI] [PubMed] [Google Scholar]
- Tanga F. Y., Nutile-McMenemy N., DeLeo J. A. (2005). The CNS role of Toll-like receptor 4 in innate neuroimmunity and painful neuropathy. Proc. Natl. Acad. Sci. U.S.A. 102, 5856–5861. 10.1073/pnas.0501634102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terrando N., Brzezinski M., Degos V., Eriksson L. I., Kramer J. H., Leung J. M., et al. (2011). Perioperative cognitive decline in the aging population. Mayo Clin. Proc. 86, 885–893. 10.4065/mcp.2011.0332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tetreault N. A., Hakeem A. Y., Jiang S., Williams B. A., Allman E., Wold B. J., et al. (2012). Microglia in the cerebral cortex in autism. J. Autism Dev. Disord. 42, 2569–2584. 10.1007/s10803-012-1513-0 [DOI] [PubMed] [Google Scholar]
- Thacker M. A., Clark A. K., Marchand F., McMahon S. B. (2007). Pathophysiology of peripheral neuropathic pain: immune cells and molecules. Anesth. Analg. 105, 838–847. 10.1213/01.ane.0000275190.42912.37 [DOI] [PubMed] [Google Scholar]
- Theoharides T. C. (2009). Autism spectrum disorders and mastocytosis. Int. J. Immunopathol. Pharmacol. 22, 859–865. 10.1177/039463200902200401 [DOI] [PubMed] [Google Scholar]
- Theoharides T. C., Angelidou A., Alysandratos K. D., Zhang B., Asadi S., Francis K. (2012). Mast cell activation and autism. Biochim. Biophys. Acta 1822, 34–41. 10.1016/j.bbadis.2010.12.017 [DOI] [PubMed] [Google Scholar]
- Theoharides T. C., Asadi S., Panagiotidou S., Weng Z. (2013). The “missing link” in autoimmunity and autism: extracellular mitochondrial components secreted from activated live mast cells. Autoimmun. Rev. 12, 1136–1142. 10.1016/j.autrev.2013.06.018 [DOI] [PubMed] [Google Scholar]
- Theoharides T. C., Baloyannis S. J., Manolidis L. S. (1991). Activated rat peritoneal mast cells can cause syngeneic brain demyelination in vitro. Int. J. Immunopathol. Pharmacol. 4, 137–144. [Google Scholar]
- Theoharides T. C., Doyle R., Francis K., Conti P., Kalogeromitros D. (2008a). Novel therapeutic targets for autism. Trends Pharmacol. Sci. 29, 375–382. 10.1016/j.tips.2008.06.002 [DOI] [PubMed] [Google Scholar]
- Theoharides T. C., Kempuraj D., Kourelis T., Manola A. (2008b). Human mast cells stimulate activated T cells: implications for multiple sclerosis. Ann. N.Y. Acad. Sci. 1144, 74–82. 10.1196/annals.1418.029 [DOI] [PubMed] [Google Scholar]
- Theoharides T. C., Petra A. I., Taracanova A., Panagiotidou S., Conti P. (2015a). Targeting IL-33 in autoimmunity and inflammation. J. Pharmacol. Exp. Ther. 354, 24–31. 10.1124/jpet.114.222505 [DOI] [PubMed] [Google Scholar]
- Theoharides T. C., Stewart J. M., Hatziagelaki E., Kolaitis G. (2015b). Brain “fog,” inflammation and obesity: key aspects of neuropsychiatric disorders improved by luteolin. Front. Neurosci. 9:225 10.3389/fnins.2015.00225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Theoharides T. C., Stewart J. M., Panagiotidou S., Melamed I. (2016). Mast cells, brain inflammation and autism. Eur. J. Pharmacol. 778, 96–102. 10.1016/j.ejphar.2015.03.086 [DOI] [PubMed] [Google Scholar]
- Trang T., Beggs S., Wan X., Salter M. W. (2009). P2X4-receptor-mediated synthesis and release of brain-derived neurotrophic factor in microglia is dependent on calcium and p38-mitogen-activated protein kinase activation. J. Neurosci. 29, 3518–3528. 10.1523/JNEUROSCI.5714-08.2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trias E., Ibarburu S., Barreto-Núñez R., Varela V., Moura I. C., Dubreuil P., et al. (2017). Evidence for mast cells contributing to neuromuscular pathology in an inherited model of ALS. JCI Insight. 2:95934. 10.1172/jci.insight.95934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsilioni I., Dodman N., Petra A. I., Taliou A., Francis K., Moon-Fanelli A., et al. (2014). Elevated serum neurotensin and CRH levels in children with autistic spectrum disorders and tail-chasing Bull Terriers with a phenotype similar to autism. Transl. Psychiatry 4:e466. 10.1038/tp.2014.106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsuboi K., Takezaki N., Ueda N. (2007). The N-acylethanolamine-hydrolyzing acid amidase (NAAA). Chem. Biodivers. 4, 1914–1925. 10.1002/cbdv.200790159 [DOI] [PubMed] [Google Scholar]
- Tsuda M. (2016). P2 receptors, microglial cytokines and chemokines, and neuropathic pain. J. Neurosci. Res. 95, 1319–1329. 10.1002/jnr.23816 [DOI] [PubMed] [Google Scholar]
- Turner M. R., Cagnin A., Turkheimer F. E., Miller C. C., Shaw C. E., Brooks D. J., et al. (2004). Evidence of widespread cerebral microglial activation in amyotrophic lateral sclerosis: an [11C](R)-PK11195 positron emission tomography study. Neurobiol. Dis. 15, 601–609. 10.1016/j.nbd.2003.12.012 [DOI] [PubMed] [Google Scholar]
- Üçeyler N., Zeller D., Kahn A. K., Kewenig S., Kittel-Schneider S., Schmid A., et al. (2013). Small fibre pathology in patients with fibromyalgia syndrome. Brain 136, 1857–1867. 10.1093/brain/awt053 [DOI] [PubMed] [Google Scholar]
- Ueda N., Tsuboi K., Uyama T. (2013). Metabolism of endocannabinoids and related N-acylethanolamines: canonical and alternative pathways. FEBS J. 280, 1874–1894. 10.1111/febs.12152 [DOI] [PubMed] [Google Scholar]
- Ulmann L., Hatcher J. P., Hughes J. P., Chaumont S., Green P. J., Conquet F. (2008). Up-regulation of P2X4 receptors on spinal microglia after peripheral nerve injury mediates BDNF release and neuropathic pain. J. Neurosci. 28, 11263–11268. 10.1523/JNEUROSCI.2308-08.2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valent P., Horny H. P., Escribano L., Longley B. J., Li C. Y., Schwartz L. B., et al. (2001). Diagnostic criteria and classification of mastocytosis: a consensus proposal. Leuk. Res. 25, 603–625. 10.1016/S0145-2126(01)00038-8 [DOI] [PubMed] [Google Scholar]
- van Hecke O., Austin S. K., Khan R. A., Smith B. H., Torrance N. (2014). Neuropathic pain in the general population: a systematic review of epidemiological studies. Pain 155, 654–662. 10.1016/j.pain.2013.11.013 [DOI] [PubMed] [Google Scholar]
- Vargas D. L., Nascimbene C., Krishnan C., Zimmerman A. W., Pardo C. A. (2005). Neuroglial activation and neuroinflammation in the brain of patients with autism. Ann. Neurol. 57, 67–81. 10.1002/ana.20315 [DOI] [PubMed] [Google Scholar]
- Villapol S., Byrnes K. R., Symes A. J. (2014). Temporal dynamics of cerebral blood flow, cortical damage. Apoptosis 5:82. 10.3389/fneur.2014.00082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volterra A., Meldolesi J. (2005). Astrocytes, from brain glue to communication elements: the revolution continues. Nat. Rev. Neurosci. 6, 626–640. 10.1038/nrn1722 [DOI] [PubMed] [Google Scholar]
- von Büdingen H. C., Mei F., Greenfield A., Jahn S., Shen Y. A., Reid H. H., et al. (2015). The myelin oligodendrocyte glycoprotein directly binds nerve growth factor to modulate central axon circuitry. J. Cell Biol. 210, 891–898. 10.1083/jcb.201504106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Q., Liu Y., Zhou J. (2015). Neuroinflammation in Parkinson's disease and its potential as therapeutic target. Transl. Neurodegener. 4:19. 10.1186/s40035-015-0042-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Q., Tang X. N., Yenari M. A. (2007). The inflammatory response in stroke. J. Neuroimmunol. 184, 53–68. 10.1016/j.jneuroim.2006.11.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang M., Wang X., Zhao L., Ma W., Rodriguez I. R., Fariss R. N., et al. (2014). Macroglia-microglia interactions via TSPO signaling regulates microglial activation in the mouse retina. J. Neurosci. 34, 3793–3806. 10.1523/JNEUROSCI.3153-13.2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wardlaw A. J., Moqbel R., Cromwell O., Kay A. B. (1986). Platelet-activating factor. A potent chemotactic and chemokinetic factor for human eosinophils. J. Clin. Invest. 78, 1701–1706. 10.1172/JCI112765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wezel A., Lagraauw H. M., van der Velden D., de Jager S. C., Quax P. H., Kuiper J. (2015). Mast cells mediate neutrophil recruitment during atherosclerotic plaque progression. Atherosclerosis 241, 289–296. 10.1016/j.atherosclerosis.2015.05.028 [DOI] [PubMed] [Google Scholar]
- Wirz S., Molderings G. J. (2017). A practical guide for treatment of pain in patients with systemic mast cell activation disease. Pain Physician 20, E849–E861. [PubMed] [Google Scholar]
- Wlodarczyk A., Holtman I. R., Krueger M., Yogev N., Bruttger J., Khorooshi R., et al. (2017). A novel microglial subset plays a key role in myelinogenesis in developing brain. EMBO J. 36, 3292–3308. 10.15252/embj.201696056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wohleb E. S., Franklin T., Iwata M., Duman R. S. (2016). Integrating neuroimmune systems in the neurobiology of depression. Nat. Rev. Neurosci. 17, 497–511. 10.1038/nrn.2016.69 [DOI] [PubMed] [Google Scholar]
- Wyss-Coray T. (2006). Inflammation in Alzheimer disease: driving force, bystander or beneficial response? Nat. Med. 12, 1005–1015. 10.1038/nm1484 [DOI] [PubMed] [Google Scholar]
- Xanthos D. N., Gaderer S., Drdla R., Nuro E., Abramova A., Ellmeier W., et al. (2011). Central nervous system mast cells in peripheral inflammatory nociception. Mol. Pain 7:42. 10.1186/1744-8069-7-42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie F., Zhang J. C., Fu H., Chen J. (2013). Age-related decline of myelin proteins is highly correlated with activation of astrocytes and microglia in the rat CNS. Int. J. Mol. Med. 32, 1021–1028. 10.3892/ijmm.2013.1486 [DOI] [PubMed] [Google Scholar]
- Xiong Y., Mahmood A., Chopp M. (2013). Animal models of traumatic brain injury. Nat. Rev. Neurosci. 14, 128–142. 10.1038/nrn3407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu J., Dong H., Qian Q., Zhang X., Wang Y., Jin W., et al. (2017). Astrocyte-derived CCL2 participates in surgery-induced cognitive dysfunction and neuroinflammation via evoking microglia activation. Behav. Brain Res. 332, 145–153. 10.1016/j.bbr.2017.05.066 [DOI] [PubMed] [Google Scholar]
- Yang L., Li L., Chen L., Li Y., Chen H., Li Y., et al. (2015). Potential analgesic effects of a novel N-acylethanolamine acid amidase inhibitor F96 through PPAR-α. Sci. Rep. 5:13565. 10.1038/srep13565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang H., Wei J., Zhang H., Song W., Wei W., Zhang L., et al. (2010). Upregulation of Toll-like Receptor (TLR) expression and release of cytokines from mast cells by IL-12. Cell Physiol. Biochem. 26, 337–346. 10.1159/000320557 [DOI] [PubMed] [Google Scholar]
- Yirmiya R., Rimmerman N., Reshef R. (2015). Depression as a microglial disease. Trends Neurosci. 38, 637–658. 10.1016/j.tins.2015.08.001 [DOI] [PubMed] [Google Scholar]
- Young K. M., Psachoulia K., Tripathi R. B., Dunn S. J., Cossell L., Attwell D., et al. (2013). Oligodendrocyte dynamics in the healthy adult CNS: evidence for myelin remodeling. Neuron 77, 873–885. 10.1016/j.neuron.2013.01.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan B., Fu F., Huang S., Lin C., Yang G., Ma K., et al. (2017). C5a/C5aR pathway plays a vital role in brain inflammatory injury via initiating Fgl-2 in intracerebral hemorrhage. Mol. Neurobiol. 54, 6187–6197. 10.1007/s12035-016-0141-7 [DOI] [PubMed] [Google Scholar]
- Yuan H., Zhu X., Zhou S., Chen Q., Zhu X., Ma X., et al. (2010). Role of mast cell activation in inducing microglial cells to release neurotrophin. J. Neurosci. Res. 88, 1348–1354. 10.1002/jnr.22304 [DOI] [PubMed] [Google Scholar]
- Zaheer A., Zaheer S., Sahu S. K., Knight S., Khosravi H., Mathur S. N., et al. (2007). A novel role of glia maturation factor: induction of granulocyte-macrophage colony-stimulating factor and pro-inflammatory cytokines. J. Neurochem. 101, 364–376. 10.1111/j.1471-4159.2006.04385.x [DOI] [PubMed] [Google Scholar]
- Zarpelon A. C., Rodrigues F. C., Lopes A. H., Souza G. R., Carvalho T. T., Pinto L. G., et al. (2016). Spinal cord oligodendrocyte-derived alarmin IL-33 mediates neuropathic pain. FASEB J. 30, 54–65. 10.1096/fj.14-267146 [DOI] [PubMed] [Google Scholar]
- Zeis T., Enz L., Schaeren-Wiemers N. (2016). The immunomodulatory oligodendrocyte. Brain Res. 1641, 139–148. 10.1016/j.brainres.2015.09.021 [DOI] [PubMed] [Google Scholar]
- Zhang X., Dong H., Li N., Zhang S., Sun J., Zhang S., et al. (2016). Activated brain mast cells contribute to postoperative cognitive dysfunction by evoking microglia activation and neuronal apoptosis. J. Neuroinflammation 13:127. 10.1186/s12974-016-0592-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang S., Dong H., Zhang X., Li N., Sun J., Qian Y. (2016). Cerebral mast cells contribute to postoperative cognitive dysfunction by promoting blood brain barrier disruption. Behav. Brain Res. 298, 158–166. 10.1016/j.bbr.2015.11.003 [DOI] [PubMed] [Google Scholar]
- Zhang Q. S., Heng Y., Yuan Y. H., Chen N. H. (2017). Pathological α-synuclein exacerbates the progression of Parkinson's disease through microglial activation. Toxicol. Lett. 265, 30–37. 10.1016/j.toxlet.2016.11.002 [DOI] [PubMed] [Google Scholar]
- Zhang X. M., Lund H., Mia S., Parsa R., Harris R. A. (2014). Adoptive transfer of cytokine-induced immunomodulatory adult microglia attenuates experimental autoimmune encephalomyelitis in DBA/1 mice. Glia 62, 804–817. 10.1002/glia.22643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang S., Wang X. J., Tian L. P., Pan J., Lu G. Q., Zhang Y. J., et al. (2011). CD200-CD200R dysfunction exacerbates microglial activation and dopaminergic neurodegeneration in a rat model of Parkinson's disease. J. Neuroinflammation 8:154. 10.1186/1742-2094-8-154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang H., Yang H., He S. (2010). TNF increases expression of IL-4 and PARs in mast cells. Cell. Physiol. Biochem. 26, 327–336. 10.1159/000320556 [DOI] [PubMed] [Google Scholar]
- Zhang H., Yang X., Yang H., Zhang Z., Lin Q., Zheng Y., et al. (2007). Modulation of mast cell proteinase-activated receptor expression and IL-4 release by IL-12. Immunol. Cell Biol. 85, 558–566. 10.1038/sj.icb.7100085 [DOI] [PubMed] [Google Scholar]
- Zuo Y., Perkins N. M., Tracey D. J., Geczy C. L. (2003). Inflammation and hyperalgesia induced by nerve injury in the rat: a key role of mast cells. Pain 105, 467–479. 10.1016/S0304-3959(03)00261-6 [DOI] [PubMed] [Google Scholar]