Abstract
Background
The new global target for maternal mortality ratio (MMR) is a ratio below 70 maternal deaths per 100 000 live births by 2030. We undertook a systematic review of methods used to measure MMR in low- and middle-income countries.
Sources of data
Systematic review of the literature; 59 studies included.
Areas of agreement
Civil registration (5 studies), census (5) and surveys (16), Reproductive Age Mortality Studies (RAMOS) (4) and the sisterhood methods (11) have been used to measure MMR in a variety of settings.
Areas of controversy
Middle-income countries have used civil registration data for estimating MMR but it has been a challenge to obtain reliable data from low-income countries with many only using health facility data (18 studies).
Growing points and areas for further research
Based on the strengths and feasibility of application, RAMOS may provide reliable and contemporaneous estimates of MMR while civil registration systems are being introduced. It will be important to build capacity for this and ensure implementation research to understand what works where and how.
Keywords: measuring, maternal mortality ratio, RAMOS, low- and middle-income countries
Introduction
Reducing maternal mortality is one of the priority goals on the international agenda—the new global target is to reduce the maternal mortality ratio (MMR) to <70 maternal deaths per 100 000 live births and country should reduce their MMR by at least two-thirds from the 2010 baseline and no country should have an MMR higher than 140 deaths per 100 000 live births by 2030.1,2 A cross-cutting priority for the post-2015 agenda is to move toward counting every birth, maternal death and perinatal death through the establishment of effective national registration and vital statistics systems in every country, as stated within the recommendations of the Commission for Information and Accountability.3
Reliable data are needed so that adequate resources can be allocated to maternal health programmes for countries (or regions in countries) that are not yet accelerating the annual reduction in maternal deaths. These data are also needed to monitor progress toward the targets set for the new Sustainable Development Goals (SDG). Assessing progress has been a challenge because <40% of countries currently have complete civil registration (CR) systems in place or other methods to provide accurate and contemporaneous MMR data. Similarly, although Maternal Death Surveillance and Review is promoted and being implemented in many settings, attribution and reporting of cause of maternal death is not yet systematically in place.4,5 Only 2 of the 49 least developed countries have >50% coverage with regard to death registration.1
The World Health Organization (WHO) publishes global estimates of MMR based on United Nations statistical models, including estimates for countries without reliable data.6 Most of these estimates are subject to greater or lesser degrees of uncertainty and this is a recognized limitation. There are, in addition to modelling, a variety of methods available to measure MMR including via censuses, household surveys, Reproductive Age Mortality Studies (RAMOS) and using the Sisterhood methods. Each method has strengths and weaknesses. This may include cost of application of method, lack of in-country capacity to use the method and requirement for large sample sizes to be able to estimate MMR with reasonable accuracy. Although some of these methods have been used in a number of developing countries, there is a lack of knowledge and guidance regarding which method(s) are the be most appropriate and feasible to use in which settings (e.g. large or small population, national or sub-national application and type of data required to estimate MMR).
We, therefore, conducted a systematic review of the literature to identify which methods have been used to estimate MMR and reviewed their use and applicability to low- and middle-income countries. The specific research questions included: what are the type of data and data sources required, what are the strengths and weaknesses of each method; and which method(s) would be useful and applicable in low- and middle-income settings and able to provide reasonably accurate and contemporaneous data.
Methods
We used the following databases SCOPUS, PUBMED and Institute for Scientific Information (ISI) and MEDLINE to search for studies that measured MMR in low- and middle-income countries. Publications of organizations and programmes such as the United Nations Population Fund (UNFPA), United Nations Children's Fund (UNICEF), World Bank, WHO and the Initiative for Maternal Mortality Programme Assessment (IMMPACT) were included. Internet searches using the Google search engine were conducted to identify relevant literature not published in peer-reviewed journals and the references of all identified, relevant papers were hand-searched.
Search terms used
Medical Subject Headings (MeSH) were searched to identify all relevant terms used to describe maternal mortality and measuring. Boolean operators such as ‘OR’ were used to join keywords and MeSH terms defining the same concepts and different concepts were searched with ‘AND’ to arrive at the final result. We used the search terms ‘maternal mortality OR maternal death OR pregnancy death OR motherhood death OR women deaths’ in combination with ‘measure OR estimate’ OR ‘estimation’. These were then combined using the Boolean operator ‘AND’ with the following search terms: civil registration data, Census, Surveys, health facility data, sisterhood methods, RAMOS and low- and middle-income countries. Star truncation (*) was used where multiple endings of terms were possible.
Inclusion and exclusion criteria
We included papers published between 2000 and October 2016 from low- and middle-income countries as defined by the World Bank income categorization.7 This time period was selected as many countries undertook to assess the MMR to evaluate the burden of maternal mortality and effect of implementation of interventions to achieve MDG5 at this time.8
Studies were included for estimates of MMR obtained at either national or sub-national level regardless of method used. We excluded studies assessing impact of one or more interventions on MMR; demographic health surveys (DHS) as they are included in the direct sisterhood methods and global estimates by WHO, UNICEF, UNFPA and the World Bank (published by the WHO and not countries that use statistical models that may have errors, use unreliable data sources and, in some cases, countries do not use them). We also excluded reviews, posters, editorials and discussion papers, which did not include methodologies and estimates of MMR. DHS were excluded as these use the direct sisterhood method which is already included in the review. Global estimates were excluded when they employed statistical modelling.
Data extraction
Two reviewers independently screened all titles and abstracts. When the information provided by title and abstract was insufficient to decide on inclusion or exclusion, full-text versions were retrieved and evaluated. All included papers were reviewed in full. Any discrepancies were resolved through discussion with a third researcher. A summary table was developed and agreed by all authors before full-text review was conducted and all included studies were then summarized. (Supplementary Table S1: Summary Table of included studies)
Results
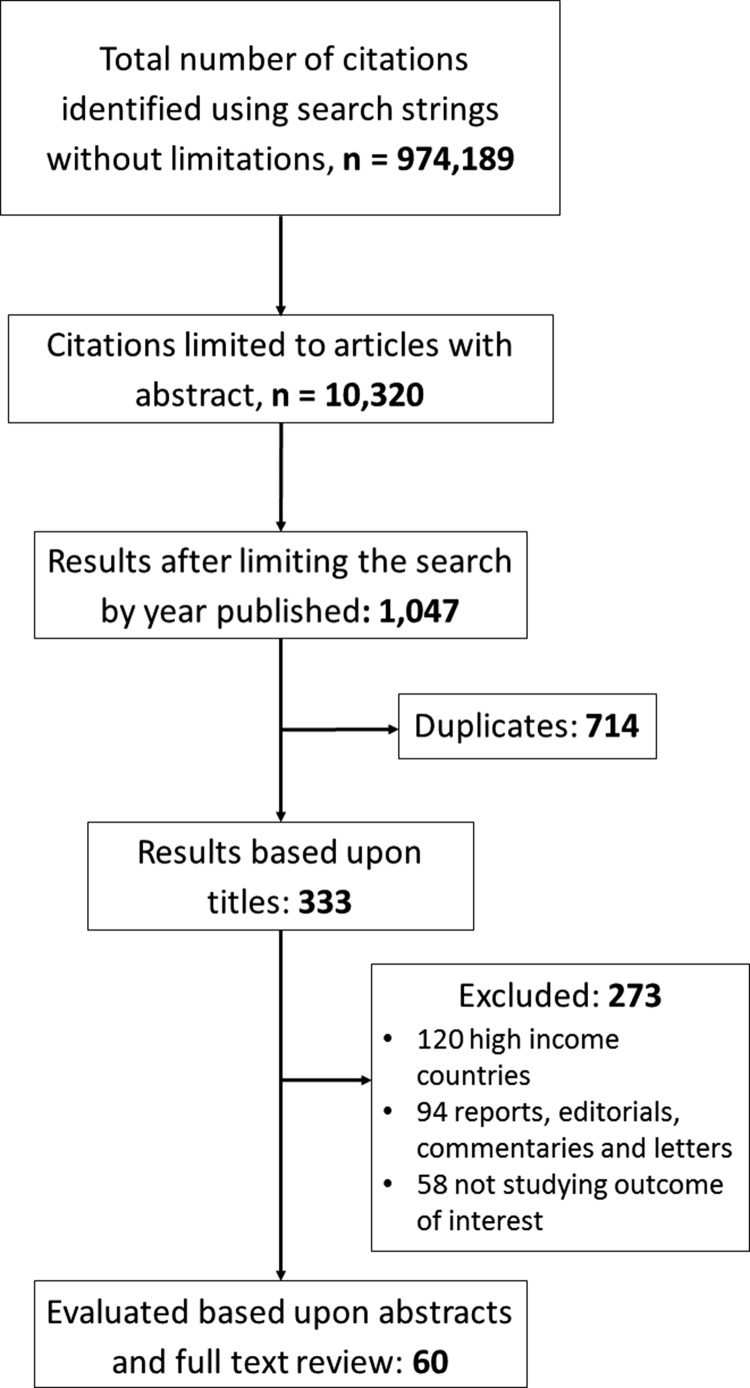
In total, 60 studies meet the inclusion criteria (Fig. 1). Six methods by which MMR or relevant data are obtained in low- and middle-income countries were identified. These include use of existing opportunities which include (i) CR data (5 studies), (ii) health facility data (18 studies), (iii) population census (5 studies), use of special studies which included (iv) population or household surveys (16 studies), (v) direct and indirect sisterhood method (11 studies), and (vi) RAMOS Studies (4 studies).
Fig. 1.
PRISMA diagram for identification of included studies.
CR and vital statistics data
CR is defined as the continuous, permanent, compulsory and universal recording of the occurrence and characteristics of vital events pertaining to the population as provided through decree or regulation in accordance with the legal requirements of a country.9 The data retrieved from CR systems are referred to as vital registration (VR) data. Complete coverage, accuracy and timeliness of CR are essential for quality vital statistics and are the ideal data to count maternal deaths. CR is carried out primarily for the purpose of establishing the legal documents provided by the law. Additionally, registration of births and deaths generates information that has substantial policy utility, especially when the age of the mother giving birth, age and sex of the decedent and underlying cause of death are correctly specified.10 Ideally, CR systems with high coverage and good attribution of cause of death provide accurate data on the level of MM and the causes of maternal deaths. The drawback, however, relates primarily to the availability, reliability, completeness and coverage of the CR data.11 The number of maternal deaths and number of live births recorded are used to calculate MMR (number of MD per 100 000 live births).
Five papers reported using CR data to estimate maternal mortality. These studies were conducted in China, the Dominican Republic, Brazil, Egypt and Guatemala, all middle-income countries.12–16 There were no studies from low-income countries using this method.12–16 In Guatemala, VR data were supplemented with additional information from medical charts and from public healthcare centres which improved the quality of data obtained. The study detected three times the number of maternal deaths compared to using the civil registry data only.15 However, to establish whether the death of a woman of reproductive age (WRA) is a maternal death, information on pregnancy status at time of death is required. It was noted that information on pregnancy status was often either missing or unclear on the death certificates for studies conducted in China, the Dominican Republic, Brazil and Egypt. The authors note that this resulted in misclassification and possibly an underestimation of the number of maternal deaths.12–14,16 Deaths among women living in villages accessible only by foot were not registered in the study in the Dominican Republic.14
Health facility surveys
Health facility data remain the main, routine source of data on MM for many developing countries. Currently, health facility data are not used by academics and by agencies for compiling global mortality estimates, but they are widely used in many countries as they are locally generated and continuously available. Data sources include routinely reported records in health facilities or sentinel sites, reports from healthcare providers and health facility surveys.
Eighteen papers reviewed used health facility data to estimate MMR.17–34 Most studies were conducted in low- and middle-income African countries such as Nigeria, Cameroon, Malawi and Zambia. However, middle-income countries such as India, Pakistan and Turkey also estimated MMR using health facility data.18,23,27 It was noted that 15 studies were conducted in tertiary or teaching hospitals, which are expected to have a significant proportion of high-risk obstetric cases although this proportion was not reported.17,19–23,27–29,31–34 Maternal deaths were identified from maternity ward records in 16 out of 18 facilities. Only two studies identified cases from other wards including the female or gynaecology ward and from operating theatre registers.21,31 Case notes for women who had died were noted to have been missing in some facilities and there were considerable inaccuracies in routine registers noted in most retrospective studies.20,25
Population census
Greater interest has been shown in using data from population censuses to measure maternal mortality. A national census, with the addition of a small number of additional questions, can be used to obtain estimates of maternal mortality.35 This is a result of the endorsement of this method by the United Nations Principles and Recommendations for Population and Housing Censuses.36 The UN principles recommend two follow-up questions in cases where the household being interviewed reports a death during the past 12 months. After ascertaining the name, age and sex of the deceased person and date of death, the interviewer should enquire:
Was the death due to an accident, violence, homicide or suicide?
If the deceased was a woman aged 15–49, did the death occur while she was pregnant, during childbirth or during the six weeks after the end of pregnancy?
As a result, in the 1990s several countries included questions intended to ascertain if any WRA had died during pregnancy or within a defined period postpartum, usually 6 weeks. In principle, a census allows the identification of deaths in a household in a relatively short reference period (1–2 years) and thereby provides estimates of recent maternal mortality.
Population census data were used to estimate maternal mortality in five studies.37–41 Questions regarding the time of circumstance of death among WRA who died during pregnancy, labour and in the postpartum period (usually 6 weeks after delivery) were included during census data collection. The studies were conducted in Latin America (Honduras, Nicaragua and Paraguay), South Africa, Burkina Faso, Honduras (only) and Indonesia. A study conducted in Burkina Faso used this approach and obtained an estimate of the MMR, the results of which were similar to a previous study which had used the direct sisterhood method.41 In Latin America, there was a greater number of reported pregnancy-related deaths in census data when compared with the number reported during a household survey which was conducted at the same time.39 Similarly, in the Republic of South Africa, an increase in maternal death was observed.40 Narrow confidence intervals were obtained: MMR: 519 per 100 000 (95% CI: 454, 584) in Damage and MMR: 353 per 100 000 (95% CI: 295, 411) in Orangey in Burkina Faso.41 Similarly, there was a greater number of reported pregnancy-related deaths using census data than obtained via sample surveys in Latin America.
Population or household surveys
Population or household surveys are one of the most important data capturing methods for maternal deaths in settings where routine information systems are weak or non-existent. These surveys are administered at the household level to collect information about maternal deaths. Names and residences are cross-checked to avoid double counting. Sometimes, they are complemented with verbal autopsies where the family members or other people with knowledge about the death could be asked to describe the situation surrounding the death relatives. The WHO has devised a standard verbal autopsy tool to collect information on signs, symptoms, medical history and circumstances preceding death,42 which countries can adapt according to their situation. In both population or household surveys and verbal autopsies, names and residences are cross-checked to avoid double counting. These methods are only appropriate for settings in which the sampling unit is a complete village and the geographical scope of the study is quite limited. Surveys, however, require a relatively large sample size to obtain statistically significant findings for occurrences that are relatively rare such as maternal deaths.35 Sixteen studies included in this review estimated the number of maternal deaths using population and/or household surveys.38,43–57 Out of the 16 studies, only 5 were conducted in Africa (Ethiopia, Kenya, Malawi, Senegal and Tanzania).44,52,56,57 Six were conducted prospectively (Colombia, Sri Lanka, Ethiopia, Indonesia, Jamaica and Pakistan).38,43,48,50,51,53 For cultural reasons, family members and birth attendants in Cambodia were reported to have felt ashamed of deaths that had occurred and, therefore, did not report all deaths. There were sampling problems in some of the studies and very wide confidence intervals were obtained for the MMR estimates.55,57 For example, in India, only a small area was covered because it was considered too expensive to conduct a household survey covering a bigger, geographical area.
Direct and indirect sisterhood methods
In sisterhood surveys, adult respondents report on the aggregate numbers of surviving sisters and of sisters who have died.58 There are two types of sisterhood methods, the indirect and the direct method.
The original (indirect) sisterhood method was developed in the late 1980s by Graham et al.58 In the indirect sisterhood method, adult respondents are asked four questions pertaining to the survival (or not) of all their adult sisters born to the same mother. By enquiring about female siblings in a high fertility setting, one effectively expands the sample size with very little additional cost. The method also reduces the need for large sample sizes because there may be more than one respondent per household and more than one sister per respondent. The questions for which responses are required in the indirect sisterhood method are listed in Box 1. As this method identifies any death that occurs during pregnancy, childbirth or the postpartum period; the indirect sisterhood approach identifies pregnancy-related deaths rather than true maternal deaths. Overestimation of maternal mortality due to the inclusion of deaths that are coincidental and/or non-maternal deaths is likely. Conversely, abortion-related maternal deaths are often not captured. It has been suggested that the omission of induced abortions a compensate for the inclusion of non-maternal deaths. However, the extent of the compensation is unknown. Finally, estimates obtained using the indirect sisterhood method relate to the previous 10–12 years and are, therefore, not contemporaneous and cannot be used for evaluating the effectiveness or impact of an intervention programme.
Box 1. Indirect sisterhood.
How many sisters (born to the same mother) have you ever had who reached age 15 (who were ever-married) including those who are now dead?
How many of these ever-married sisters are alive now?
How many of these are dead?
How many of these dead sisters died while they were pregnant, or during childbirth, or during the six weeks after the end of the pregnancy?
Rutenburg and Sullivan proposed the direct sisterhood method,59 which has been widely used in DHS programmes. This is a variant of the indirect sisterhood method based on a detailed sibling history obtained from each respondent. The four questions listed above for the original indirect sisterhood method are expanded to 11 questions. In addition, the formulation of the original questions was altered. For example, the fourth question on timing of death in relation to pregnancy, childbirth and the postpartum period was changed to include three separate questions (Box 2).
Box 2. Direct sisterhood.
How many children did your mother give birth to?
How many of these births did your mother have before you were born?
What was the name given to your oldest (next oldest) brother or sister?
Is (NAME) male or female?
Is (NAME) still alive?
How old is (NAME)?
In what year did (NAME) die? OR how many years ago did (NAME) die?
-
How old was (NAME) when she died?
For dead sisters only:
Was (NAME) pregnant when she died?
Did (NAME) die during childbirth?
Did (NAME) die within two months after the end of pregnancy or
Source: World Health Organization (1997). The Sisterhood method for estimating maternal mortality: guidance potential users. Available on http://apps.who.int/iris/bitstream/10665/64007/1/WHO_RHT_97.28.pdf. Accessed on November 21, 2016.
The data requirements for the direct sisterhood method are considerably more demanding than those for the indirect approach. In the direct approach, a respondent is asked to provide the birth history of her mother, including the current age of all living siblings and the age at death and years since death for all deceased siblings. These data allow deaths and births to be placed in calendar time and, therefore, permit the calculation of sex and age-specific death rates for reference periods.59 Unlike the indirect sisterhood method, the direct sisterhood method targets a more limited reference period for sister deaths: the previous 0–6 years compared with the previous 10–12 years for the indirect sisterhood method. Point estimates for maternal mortality are obtainable. The approach also allows for the calculation of rates/ratios for the reference period of interest and monitor trends. The direct sisterhood method is currently used during DHS. This method requires larger sample sizes than the indirect method. It also requires an additional 8–10 min per interview on average and additional training and supervision in the field.
Both methods measure the ICD-10 concept of pregnancy-related mortality rather than maternal mortality on the grounds that respondents would not be easily able to distinguish between maternal and pregnancy-related deaths.39
We did not find any peer-reviewed studies that use the direct sisterhood method apart from the DHS. An analysis of the quality of maternal health indicators for DHS studies is not part of this review and has been described elsewhere.60 Eleven included studies used the indirect sisterhood method to estimate MMR. Ten studies were conducted in Africa (Liberia, Nigeria (2 studies), Mali, Tanzania (3 studies), Swaziland, Uganda and Ghana).61–69 One study was conducted in India.70
In Ghana and Uganda, the MMR estimates identified through the indirect sisterhood method were higher than those obtained as national estimates (modelling, UN global estimates) conducted at the same time.68,69 All studies registered pregnancy-related deaths and include death due to accidental or incidental causes (i.e. not maternal deaths). Cause of death is not determined and data collected refers to the previous 10–12 years.
Reproductive age mortality studies
A RAMOS has been identified as a relatively robust method, which uses both active and passive data collection methods to estimate the MMR in countries without VR data and are often considered to be the gold standard.35 The approach involves retrospective or prospective identification and investigating the causes of all deaths of WRA in a defined area/population by using multiple sources of data such as existing records (CR and health facility data), census, surveys and surveillance. RAMOS are conducted in two phases. The first phase, involves identification of all deaths among WRA in a population. In the second phase, all deaths are investigated (using verbal autopsy, health facility reports or medical record reviews death certificates with medical cause and interview with household members and relatives) to ascertain if there are pregnancy-related or maternal deaths.71
Four studies conducted in Malawi, Sudan, Jordan and Ghana estimated MMR using the RAMOS method.72–75 Three studies were prospective and one study retrospective.73 A list of all deaths of WRA was collected using data collated at health facilities (e.g. admission and discharge books, death certificate books, death registers and mortuary logbooks) and individual case notes when necessary, available census data or any other relevant data e.g. the number of births from the most recent DHS and from the Health Management Information System (HMIS). Deaths that occurred in the community were identified by local key informants, traditional birth attendants and community workers. A study in Malawi used the existing health staff (nurses, doctors, medical assistants and community health workers known as health surveillance assistants) at both health facility and community level to identify and report all deaths of WRA. One study in Pakistan included interviews with graveyard caretakers as an additional source of data. In most studies, verbal autopsies where family members or other people with knowledge about the death were interviewed to describe the situation surrounding the death.
All RAMOS studies highlight that this method identifies more maternal deaths than obtained via any one of the existing reporting mechanisms alone (e.g. HMIS and facility death reports). Underreporting of maternal deaths (by 44 and 43%) documented via survey and CR was reported in Ghana and Malawi, respectively.72,75 In Sudan and Jordan, the RAMOS study was conducted at state level, while in Malawi and Ghana the studies were conducted at district and city level, respectively.73,74 In Malawi, verbal autopsy was only done for deaths that were identified as maternal deaths. Maternal deaths were identified using the ICD-10 version 10 definition of MD.76
Discussion
Accurate levels of maternal mortality are difficult to measure in a population for it is challenging to identify maternal deaths precisely, particularly in settings where routine recording of deaths is not complete within CR systems.6 The woman's pregnancy status is usually missed even if such a death was recorded and may not be reported as a maternal death even if the woman was pregnant. Even in countries where routine registration of deaths is in place, maternal deaths may be unidentified due to misclassification of ICD-10 coding and identification of the true numbers of maternal deaths may require special investigations into the causes of deaths.59,77 This review shows that even in high-middle income countries such mechanisms are only now in process of being fully developed. A variety of other methods are used in low- and middle-income settings. Very often the only contemporaneous data available are health facility-based MMR estimates which do not apply to the whole population or estimates obtained via the sisterhood method which are not contemporaneous and report pregnancy-related rather than maternal deaths per se.
Birth and death registration
For birth and death registration systems to provide data on the number of maternal deaths among all deaths of WRA, it is important that pregnancy status is known. Although a tick box has been included on the death notification from, underreporting of the number of maternal deaths and misreporting (misclassification of death of a WRA as a maternal death or not) has been identified as a problem of CR data.78,79 In this review, information on pregnancy status was often either missing or unclear in the identified deaths.12–16 Although countries such as Sweden, the Netherlands, the UK and USA, which have documented reduction in MMR over several decades, have relied on adequate CR systems, misclassification and underreporting exist.4,79 Revision of the death certificate to include information on pregnancy status improves the quality of data and helps to reduce misclassification of maternal deaths. CR data can be compared with data obtained via other systems specific to the evaluation or audit of maternal deaths; countries such as the UK and South Africa have used the Confidential Enquiry into Maternal Deaths (CEMD) to ensure any death missed by the CR system are captured.2,80,81,82
Health facility data
Valuable information can be obtained when maternal deaths that occur in a health facility are reviewed specifically to identify where the health system needs to improve.22,83 However, in low- and middle-income countries unless >95% of women give birth in a health facility (as opposed to at home), findings from hospital-based studies cannot be generalized to the entire population. However, the majority of the studies from developing country settings reported hospital-based MMR. These only apply to the hospital itself and reflect the type of services provided; large referral hospitals with a large proportion of referred and complicated cases (rather than uncomplicated deliveries) can expect the MMR to be higher than for lower level hospitals (from where patients who are severely ill will be referred out). Thus, facility-based MMR can only be used at the facility level to monitor trends over time and if the proportion of women with potentially life threatening obstetric complications is taken into consideration. It is also crucial that all deaths of WRA are identified and an assessment is made to classify them as maternal deaths or not.
Unless a country has a healthcare system like Saudi Arabia, where almost all maternal deaths take place in the hospital or where all women are brought into hospital soon after death outside the facility, hospital-based data cannot be used to provide accurate estimates of MMR for the population.84
Census and population or household surveys
The United Nations recommend the use of a population censuses for estimating MMR, without considering this a substitute for VR.85 Use of census data to calculate MMR is cost-effective as the data can be obtained as part of an already agreed country census. Census data should provide a complete picture of the whole population and results in an estimate with relatively normal confidence indicators due to the large sample sizes. However, a census is usually only conducted every 10 years and cannot be used for routine monitoring. Furthermore, they identify pregnancy-related deaths (not maternal deaths). Early pregnancy deaths may remain under-reported if pregnancy status was not known and maternal mortality can be over-estimated where death was incidental and not due to the pregnancy. This is illustrated in a study conducted in the Republic of South Africa where an increase in maternal deaths was identified when census data were used as compared with a previous MMR estimate which was obtained using a survey method.40 Despite these limitations, census data still offer the opportunity to measure pregnancy-related mortality as a proxy for maternal mortality in countries with poor or no death registration systems in place.
When specific, planned surveys are used, capturing deaths and births is more complete than with routinely gathered statistics. However, survey methods require prohibitively large sample sizes to obtain statistically significant findings. Such surveys could, however, be used to estimate MMR in resource-limited countries in smaller subsets of populations where the other data sources are not available and/or RAMOS cannot be conducted.
Sisterhood methods
The sisterhood method is cost-effective and easier to perform than prospective population-based methods. Specifically, with the indirect sisterhood method, the number of households that need to be visited in order to obtain information on large numbers of women who have reached reproductive age is relatively small.58 Given that questions are asked about the deaths of adult sisters, both methods actually measure pregnancy-related deaths rather than maternal deaths, on the grounds that respondents (sisters) would not easily be able to distinguish between maternal and non-maternal deaths and/or usually unable to assign cause of death with certainty. Both methods provide estimates of maternal mortality in orders of magnitude rather than precise ratios since both can have wide margins of error (wide confidence intervals). Neither method provides a current estimate for the year of the survey. For these reasons, sisterhood studies cannot be used to monitor changes in maternal mortality or to assess the impact of safe motherhood programmes in the short term. The sisterhood method has been recommended by the WHO for countries without other reliable source of data and this method is frequently used as part of the 5-year DHS in low- and middle-income countries.
Reproductive Age Mortality Studies (RAMOS)
In the absence of a CR system with/without additional data collection mechanisms such as a CEMD, the RAMOS approach probably provides the most complete and contemporaneous estimation of MMR because information regarding the number of maternal deaths is obtained from a variety of sources and each death among WRA is evaluated to assess whether the death is a maternal death or not. However, the RAMOS approach is difficult in the absence of a reasonably complete initial list of deaths. Inadequate identification of all deaths among WRA results in an underestimation of maternal mortality levels. For example, Surinam had a reliable registration system for deaths which made identification of deaths of WRA relatively easy.86 Similarly, during the prospective RAMOS in Pakistan, good population-based systems were in place for tracking deaths.48 This meant that the number of maternal death among deaths of WRA could be assessed. RAMOS studies can be expensive and time consuming when conducted on a larger scale.14 A RAMOS may, therefore, be considered to provide accurate MMR data for a sub-national population.
Conclusion
To end preventable maternal deaths, it is crucial that countries develop systems and processes to ensure the ability to count every maternal death and identify the cause of death and contributing conditions. This will help identify where and how the availability or coverage as well as quality of care need to be improved. Ideally, MMR estimates should be obtained from CR data, which provide both numerator and denominator data. This would also assist in monitoring any trends in MMR over time. Many low- and middle-income countries are in the process of introducing CR systems for births and deaths. For countries without reliable systems in place, a RAMOS can be an effective method that can be used to obtain recent data and provides better estimates of MMR.
A RAMOS approach can also help illustrate what is needed to support the introduction of a full-scale Maternal Death Surveillance and Response (MDSR) process. The MDSR builds on the principles of public health surveillance and response by collecting accurate information on cause of maternal deaths so lessons can be learnt and actions taken to prevent similar deaths in the future and to improve quality of care.
Author Biographies
Florence Mgawadere PhD Florence, a nurse-midwife from Malawi with over 12 years of international experience in teaching, research and technical assistance. Florence's current research interests include quality of care, application of the ICD-MM cause classification for maternal deaths, maternal death audit or review and strengthening of Maternal Death Surveillance and Response (MDSR). Florence has carried out research on maternal health, including at the community and facility levels and programme evaluations. Florence works as a Senior Research Associate at the Centre for Maternal and Newborn Health at the Liverpool School of Tropical Medicine.
Terry Kana MSc Terry, an experienced teacher in midwifery and public health from community to postgraduate level, has worked in a wide variety of hospital and community settings with over 10 years of international programme management and research experience. Her current research interests include assessment of the effectiveness of competency based ‘skills and drills’ training in emergency obstetric care, the role, scope of work and workload of nurse-midwives working in low- and middle-income settings. Terry works as a Senior Research Associate at the Centre for Maternal and Newborn Health at the Liverpool School of Tropical Medicine.
Nynke van den Broek MBBS, DTMH, PhD, FRCOG Professor van den Broek is a recognized international expert in global maternal and newborn health who established and leads the Centre for Maternal and Newborn Health (CMNH), one of the largest academic groups in Europe with an internationally recognized portfolio of work that incorporates priority interventions for reducing maternal and newborn mortality and morbidity. Four key thematic areas include skilled birth attendance, emergency obstetric care, quality of care and maternal morbidity. Professor van den Broek has designed and conducted large population-based randomized controlled trials of single interventions for improved maternal and newborn outcomes. She has used this experience to develop complex packages of interventions and to design and conduct operational research programmes in multi-country settings.
Supplementary Material
Supplementary material
Supplementary material is available at BRIMED Journal online.
Conflict of interest statement
The authors have no potential conflicts of interest.
References
- 1. WHO Strategies towards Ending Preventable Maternal Mortality (EPMM). Geneva: World Health Organization, 2015. Available from: http://who.int/reproductivehealth/topics/maternal_perinatal/epmm/en/ [Google Scholar]
- 2. United Nations Sustainable Development Goals. Geneva: World Health Organization, 2015. Available from: http://www.un.org/sustainabledevelopment/sustainable-development-goals/ [Google Scholar]
- 3. WHO Commission on Information and Accountability for Women's and Children's Health. Keeping Promises, Measuring Results. Geneva: World Health Organization, 2011. Available from: http://www.who.int/topics/millennium_development_goals/accountability_commission/Commission_Report_advance_copy.pdf?ua=1 [Google Scholar]
- 4. WHO Maternal Death Surveillance and Response. Geneva: World Health Organization, 2016. Available from: http://www.who.int/maternal_child_adolescent/epidemiology/maternal-death-surveillance/en/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ameh CA, Adegoke A, Pattinson R, et al. Using the new ICD-MM classification system for attribution of cause of maternal death-a pilot study. Brit J Obstet Gynaecol 2014;121:32–40. [DOI] [PubMed] [Google Scholar]
- 6. WHO, UNICEF, UNFPA, World Bank, United Nations Population Division . Trends in Maternal Mortality 1990 to 2015: Estimates by the WHO, UNICEF, UNFPA, The World Bank and the United Nations Population Division. Geneva: World Health Organization, 2015. Available from: http://www.who.int/reproductivehealth/publications/monitoring/maternal-mortality-2015/en/ [Google Scholar]
- 7. World Bank New Country Classifications. Washington, DC: World Bank, 2015. Available from: http://data.worldbank.org/news/new-country-classifications-2015 [Google Scholar]
- 8. United Nations United Nations Millennium Declaration, vol. 37, UN Chronicle, 2000;38. [Google Scholar]
- 9. Phillips DE, Abou Zahr C, Lopez AD, et al. Counting births and deaths: Are well functioning civil registration and vital statistics systems associated with better health outcomes. Lancet 2015;386:1386–94. [DOI] [PubMed] [Google Scholar]
- 10. Setel PW, MacFarlane SB, Szreter S, et al. A scandal of invisibility: making everyone count by counting everyone. Lancet 2007;370:1569–77. [DOI] [PubMed] [Google Scholar]
- 11. Graham WJ, Ahmed S, Stanton C, et al. Measuring maternal mortality: an overview of opportunities and options for developing countries. BMC Med 2008;6:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Zhu L, Qin M, Du L, et al. Comparison of maternal mortality between migrating population and permanent residents in Shanghai, China, 1996–2005. Brit J Obstet Gynaecol 2009;116:401–7. [DOI] [PubMed] [Google Scholar]
- 13. Alves SV. Maternal mortality in Pernambuco, Brazil: what has changed in ten years. Reprod Health Matters 2007;15:134–44. [DOI] [PubMed] [Google Scholar]
- 14. Westoff W, Calcagno E, McDermott R, et al. Estimating maternal mortality in Monseñor Nouel Province, Dominican Republic. Matern Child Health J 2009;13:707–714. [DOI] [PubMed] [Google Scholar]
- 15. Kestler E, Ramírez L. Pregnancy-related mortality in Guatemala, 1993–1996. Rev Panam Salud Publ 2000;7:41–6. [DOI] [PubMed] [Google Scholar]
- 16. Hamza S. The maternal mortality. Egyptian Natl Matern Mortality Study 2005;2:306. [Google Scholar]
- 17. Agan TU, Archibong EI, Ekabua JE. Trends in maternal mortality at the University of Calabar Teaching Hospital, Nigeria, 1999–2009. Int J Womens Health 2010;2:249–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Aggarwal AR, Pandey A, Kar R. Estimates of maternal mortality ratio and the associated medical causes in Orissa and Rajasthan states - A cross sectional study. Ind J Comm Health 2015;27:18–24. [Google Scholar]
- 19. Omo-Aghoja LO, Aisien OA, Akuse JT, et al. Maternal mortality and emergency obstetric care in Benin City, South-south Nigeria. J Chin Clin Med 2010;5:164–7. [Google Scholar]
- 20. Bergsjø P, Vangen S, Lie RT, et al. Recording of maternal deaths in an East African university hospital. Acta Obstet Gynecol Scand 2010;89:789–93. [DOI] [PubMed] [Google Scholar]
- 21. Malik FR, Swati AA, Akhter S, et al. Retrospective Analysis of Maternal Mortality at a Tertiary Care Hospital of Peshawar, Pakistan. Khyber Med Univ J 2015;7:25–9. [Google Scholar]
- 22. Gumanga SK, Kolbila DZ, Gandau BBN. Trends in maternal mortality in Tamale teaching hospital, Ghana.Ghana Med J 2011;45:105–10. [PMC free article] [PubMed] [Google Scholar]
- 23. Iftikhar R. A study of maternal mortality. J Surg Pakistan 2009;14:177. [Google Scholar]
- 24. Igwegbe AO, Eleje GU, Ugboaja JO, et al. Improving maternal mortality at a university teaching hospital in Nnewi, Nigeria. Int J Gynecol Obstet 2012;116:197–200. [DOI] [PubMed] [Google Scholar]
- 25. Lema VM, Changole J, Kanyighe C, et al. Maternal mortality at the Queen Elizabeth Central Teaching Hospital, Blantyre, Malawi. East Afr Med J 2005;82:3–9. [DOI] [PubMed] [Google Scholar]
- 26. Li N, Matchi E, Spiegelman D, et al. Maternal mortality among HIV-infected pregnant women in Tanzania. Acta Obstet Gynecol Scand 2014;93:463–8. [DOI] [PubMed] [Google Scholar]
- 27. Malatyalioglu E, Kokcu A, Cetinkaya MB, et al. Maternal mortality rates in the last eight years: a university hospital-based study from Turkey. J Matern Fetal Neo Med 2006;19:353–6. [DOI] [PubMed] [Google Scholar]
- 28. Mundkur A, Rai L. Prepare and prevent rather than repair and repent: Study of maternal mortality in tertiary care hospital. Int J Med Public Health 2013;3:163–7. [Google Scholar]
- 29. Okeh UM. Statistical analysis of the maternal death rate at the Ebonyi State University Teaching Hospital, Abakaliki for the year ending 31 December 2007. Afr J Prim Health Care Fam Med 2009;1:118–20. [Google Scholar]
- 30. Olopade FE, Lawoyin TO. Maternal mortality in a Nigerian Maternity Hospital. Afr J Biomed Res 2010;11:267–73. [Google Scholar]
- 31. Onakewhor JUE, Gharoro EP. Changing trends in maternal mortality in a developing country. Nigerian J Clin Pract 2008;11:111–20. [PubMed] [Google Scholar]
- 32. Rulisa S, Umuziranenge I, Small M, et al. Maternal near miss and mortality in a tertiary care hospital in Rwanda. BMC Pregnancy Childbirth 2015;15:203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Sule-Odu AO. Maternal deaths in Sagamu, Nigeria. Int J Gynaecol Obstet 2000;69:47. [DOI] [PubMed] [Google Scholar]
- 34. Tebeu PM, Ngassa P, Kouam L, et al. Maternal mortality in Maroua Provincial Hospital, Cameroon (2003–2005). West Indian Med J 2007;56:502–7. [PubMed] [Google Scholar]
- 35. WHO WHO Guidance for Measuring Maternal Mortality from Census Data. New York: World Health Organization, 2013. Available from: http://apps.who.int/iris/bitstream/10665/87982/1/9789241506113_eng.pdf [Google Scholar]
- 36. United Nations Statistics Division, Department of Economic and Social Affairs Principles and Recommendations for Population and Housing Censuses. New York: United Nations, 2007. [Google Scholar]
- 37. Queiroz BL. Estimating maternal mortality differentials using census data: experience in Honduras. J Popul Res 2011;28:75–87. [Google Scholar]
- 38. Qomariyah SN, Braunholtz D, Achadi EL, et al. An option for measuring maternal mortality in developing countries: a survey using community informants. BMC Pregnancy Childbirth 2010;10:74–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Hill K, Queiroz BL, Wong L, et al. Estimating pregnancy-related mortality from census data: experience in Latin America. Bull World Health Organ 2009;87:288–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Garenne M, McCaa R, Nacro K. Maternal mortality in South Africa in 2001: from demographic census to epidemiological investigation. Popul Health Metr 2008;6:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Bell JS, Byass P, Fitzmaurice AE, et al. The epidemiology of pregnancy outcomes in rural Burkina Faso. Trop Med Int Health 2008;13:31–43. [DOI] [PubMed] [Google Scholar]
- 42. World Health Organization Verbal Autopsy Standards: The 2012 WHO Verbal Autopsy Instrument. Geneva: WHO, 2012. [Google Scholar]
- 43. Agampodi S, Wickramage K, Agampodi T, et al. Maternal mortality revisited: the application of the new ICD-MM classification system in reference to maternal deaths in Sri Lanka. Reprod Health 2014;11:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Ba MG, Kodio B, Etard JF. [Verbal autopsy to measure maternal mortality in rural Senegal]. J Gynecol Obstet Biol Reprod (Paris) 2003;32:728–35. [PubMed] [Google Scholar]
- 45. Barnett S, Nair N, Tripathy P, et al. A prospective key informant surveillance system to measure maternal mortality – findings from indigenous populations in Jharkhand and Orissa, India. BMC Pregnancy Childbirth 2008;8:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Chandy H, Heng YV, Samol H, et al. Comparing two survey methods for estimating maternal and perinatal mortality in rural Cambodia. Women Birth 2008;21:9–12. [DOI] [PubMed] [Google Scholar]
- 47. Farooq N, Jadoon H, Masood TI, et al. An assessment study of maternal mortality ratio databank in five districts of North Western Frontier Province Pakistan. J Ayub Med Co Abbottabad 2006;18:64–8. [PubMed] [Google Scholar]
- 48. Jafarey RN, Rizvi T, Koblinsky M, et al. Verbal autopsy of maternal deaths in two districts of Pakistan – filling information gaps. J Health Popul Nutr 2009;27:170–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Karabulut A, Çalişkan A, Özcan. Maternal mortality in Denizli region: three years’ evaluation. Turkiye Klinikleri Jinekoloji Obstetrik 2010;20:29–34. [Google Scholar]
- 50. McCaw-Binns A, Lindo JL, Lewis-Bell KN, et al. Maternal mortality surveillance in Jamaica. Int J Gynaecol Obstet 2008;100:31–6. [DOI] [PubMed] [Google Scholar]
- 51. Mohammed AA, Elnour MH, Mohammed EE, et al. Maternal mortality in Kassala State - Eastern Sudan: community-based study using reproductive age mortality survey (RAMOS). BMC Pregnancy Childbirth 2011;11:102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Olsen BE, Hinderaker SG. Estimates of maternal mortality by the sisterhood method in rural northern Tanzania: a household sample and an antenatal clinic sample. Brit J Obstet Gynaecol 2000;107:1290–7. [DOI] [PubMed] [Google Scholar]
- 53. Prata N, Gerdts C, Gessessew A. An innovative approach to measuring maternal mortality at the community level in low-resource settings using mid-level providers: a feasibility study in Tigray, Ethiopia. Reprod Health Matters 2012;20:196–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Saleem S, McClure EM, Goudar SS, et al. A prospective study of maternal, fetal and neonatal deaths in low- and middle-income countries. Bull World Health Organ 2014;92:605–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Singh P, Pandey A, Aggarwal A. House-to-house survey vs. snowball technique for capturing maternal death in India: a search for a cost-effective method. Indian J Med Res 2007;125:550–6. [PubMed] [Google Scholar]
- 56. van den Broek NR, White SA, Ntonya C, et al. Reproductive health in rural Malawi a population-based survey. Brit J Obstet Gynaecol 2003;110:902–8. [DOI] [PubMed] [Google Scholar]
- 57. Ziraba AK, Madise N, Mills S, et al. Maternal mortality in the informal settlements of Nairobi city: what do we know. Reprod Health 2009;22:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Graham W, Brass W, Snow RW. Estimating maternal mortality: the sisterhood method. Stud Family Plann 1989;20:125–35. [PubMed] [Google Scholar]
- 59. Rutenberg N, Sullivan J Direct and indirect estimates of maternal mortality from the sisterhood method, Proceedings of the Demographic and Health Surveys World Conference, 5–7 August 1991. Vol. 3. Washington, DC, USA: Institute for Resource. 1991.
- 60. Stanton C, Abderrahim N, Hill K. DHS Maternal Mortality Indicators: An Assessment of Data Quality and Implications for Data Use. Calverton, MD: Demographic and Health Surveys, Macro International, Inc., 1997. Available from: https://dhsprogram.com/pubs/pdf/AR4/AR4.pdf [Google Scholar]
- 61. Moseson H, Massaquoi M, Bawo L, et al. Estimation of maternal and neonatal mortality at the subnational level in Liberia. Int J Gynecol Obstet 2014;127:194–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Adegoke AA, Campbell M, Thomson AM, et al. Community study of maternal mortality in south west Nigeria: How applicable is the sisterhood method. Matern Child Hlth J 2013;17:319–29. [DOI] [PubMed] [Google Scholar]
- 63. Oye-Adeniran BA, Odeyemi KA, Gbadegesin A, et al. The use of the sisterhood method for estimating maternal mortality ratio in Lagos state, Nigeria. J Obstet Gynaecol 2011;31:315–9. [DOI] [PubMed] [Google Scholar]
- 64. Aa I, Grove MA, Haugsjå AH, et al. High maternal mortality estimated by the sisterhood method in a rural area of Mali. BMC Pregnancy Childbirth 2011;11:56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Mbaruku G, Vork F, Vyagusa D, et al. Estimates of maternal mortality in western Tanzania by the sisterhood method. Afr J Reprod Health 2003;7:84–91. [PubMed] [Google Scholar]
- 66. Font F, Alonso González M, Nathan R, et al. Maternal mortality in a rural district of south Eastern Tanzania: an application of the sisterhood method. Int J Epidemiol 2000;29:107–12. [DOI] [PubMed] [Google Scholar]
- 67. Lech MM, Zwane A. Survey on maternal mortality in Swaziland using the sisterhood method. Paediatr Perinat Epidemiol 2002;16:101–7. [DOI] [PubMed] [Google Scholar]
- 68. Orach CG. Maternal mortality estimated using the Sisterhood method in Gulu district, Uganda. Trop Doct 2000;30:72–4. [DOI] [PubMed] [Google Scholar]
- 69. Smith JB, Fortney JA, Wong E, et al. Estimates of the maternal mortality ratio in two districts of the Brong-Ahafo region, Ghana. Bull World Health Organ 2001;79:400–8. [PMC free article] [PubMed] [Google Scholar]
- 70. Bhat PNM. Maternal mortality in India: an update. Stud Family Plann 2002;33:227–36. [DOI] [PubMed] [Google Scholar]
- 71. AbouZahr C. Global burden of maternal death and disability. Brit Med Bull 2003;67:1–11. [DOI] [PubMed] [Google Scholar]
- 72. Mgawadere F, Unkels R, Adegoke A, et al. Measuring maternal mortality using a Reproductive Age Mortality Study (RAMOS). BMC Pregnancy Childbirth 2016;16:291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Mohammed AA, Elnour MH, Mohammed EE, et al. Maternal mortality in Kassala State - Eastern Sudan: community-based study using Reproductive age mortality survey (RAMOS). BMC Pregnancy Childbirth 2011;16:102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Amarin Z, Khader Y, Okour A, et al. National maternal mortality ratio for Jordan, 2007–2008. Int J Gynecol Obstet 2010;111:152–56. [DOI] [PubMed] [Google Scholar]
- 75. Zakariah AY, Alexander S, van Roosmalen J, et al. Reproductive age mortality survey (RAMOS) in Accra, Ghana. Reprod Health 2009;6:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. WHO ICD-10, the ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines. Geneva: World Health Organization, 1992. [Google Scholar]
- 77. Hogan MC, Foreman KJ, Naghavi M, et al. Maternal mortality for 181 countries, 1980–2008: a systematic analysis of progress towards Millennium Development Goal 5. Lancet 2010;375:1609–1623. [DOI] [PubMed] [Google Scholar]
- 78. Deneux-Tharaux C, Berg C, Bouvier-Colle MH, et al. Underreporting of pregnancy-related mortality in the United States and Europe. Obstet Gynecol 2005;106:684–92. [DOI] [PubMed] [Google Scholar]
- 79. Hoyert DL, Danel I, Tully P. Maternal mortality, United States and Canada, 1982–1997. Birth 2000;27:4–11. [DOI] [PubMed] [Google Scholar]
- 80. MBRRACE-UK Saving Lives, Improving Mothers’ Care Surveillance of maternal deaths in the UK 2011-13 and lessons learned to inform maternity care from the UK and Ireland Confidential Enquiries into Maternal Deaths and Morbidity 2009-13. Oxford: National Perinatal Epidemiology Unit, 2015. Available from: https://www.npeu.ox.ac.uk/downloads/files/mbrrace-uk/reports/MBRRACE-UK%20Maternal%20Report%202015.pdf [Google Scholar]
- 81. Moodley J, Pattinson RC, Fawcus S, et al. The confidential enquiry into maternal deaths in South Africa: a case study. Brit J Obstet Gynaec 2014;121:S53–60. [DOI] [PubMed] [Google Scholar]
- 82. World Health Organisation Beyond the Numbers: Reviewing Maternal Deaths and Complications to Make Pregnancy Safer. Geneva: Department of Reproductive Health and Research, WHO, 2004. [Google Scholar]
- 83. Yego F, D'Este C, Byles J, et al. Risk factors for maternal mortality in a Tertiary Hospital in Kenya: A case control study. BMC Pregnancy Childbirth 2014;14:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. al-Meshari A, Chattopadhyay SK, Younes B, et al. Trends in maternal mortality in Saudi Arabia. Int J Gynecol Obstet 1996;52:25–32. [DOI] [PubMed] [Google Scholar]
- 85. United Nations Statistical Division Principles and recommendations for population and housing censuses / Department of Economic and Social Affairs, Statistics Division. New York: United Nations Publications, 2008. [Google Scholar]
- 86. Mungra A, Van Bokhoven SC, Florie J. Reproductive age mortality survey to study under-reporting of maternal mortality in Surinam. Eur J Obstet Gynecol Reprod Biol 1998;77:37–9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.